Learning objectives.
By reading this article, you should be able to:
-
•
Describe the key anatomy of the sciatic nerve and lumbosacral plexus.
-
•
Discuss the clinical indications for different approaches to the sciatic nerve block.
-
•
Explain four ultrasound-guided approaches to the sciatic nerve at different anatomical levels.
-
•
Illustrate the typical sonographic landmarks relevant to the safe performance of each approach.
Key points.
-
•
A sciatic nerve block can provide analgesia or anaesthesia for a wide range of lower-limb procedures.
-
•
Ultrasound guidance allows visualisation of the sciatic nerve and surrounding anatomical structures.
-
•
Understanding the relevant anatomy of the sciatic nerve is vital when considering the level at which to perform the block.
-
•
An additional block of the lumbar plexus or its branches is required to provide complete anaesthesia for lower-limb surgery.
-
•
Motor-sparing ultrasound-guided local anaesthetic injection techniques for the posterior knee are gaining popularity for total knee arthroplasty.
Anatomy
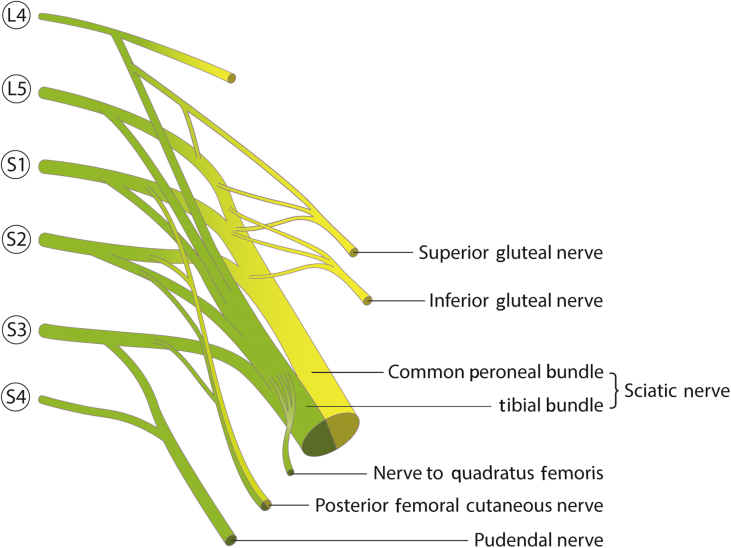
The sacral plexus is derived from the lumbosacral trunk (L4–L5) and the first to fourth sacral anterior rami. The plexus emerges within the pelvis, lying anterior to the piriformis muscle and posterior to the presacral fascia. The major branch of the sacral plexus is the sciatic nerve (SN), although other clinically relevant branches include the posterior femoral cutaneous nerve (PFCN), the superior gluteal nerve, and the nerve to quadratus femoris. The PFCN provides cutaneous innervation to the posterior thigh, whilst the superior gluteal nerve and the nerve to quadratus femoris supply the posterior hip capsule along with articular branches from the SN (Fig. 1).
Fig 1.
Abbreviated lumbosacral plexus showing the major branches relevant when performing a SN/sacral plexus block. Yellow- dorsal divisions; green- ventral divisions.
The SN exits the pelvis via the greater sciatic foramen, and after emerging from the inferior edge of the piriformis muscle it descends inferolaterally through the gluteal region. The nerve subsequently crosses the posterior surface of the superior gemellus, obturator internus, inferior gemellus, and quadratus femoris muscles. The SN descends dorsal to the quadratus femoris muscle between the medial border of the greater trochanter (GT) of the femur and the lateral border of the ischial tuberosity (IT), anterior to the gluteus maximus muscle. It then enters the posterior compartment of the thigh, anterior to the long head of the biceps femoris, but posterior to the adductor magnus muscle, running posteromedially to the femur.
As it approaches the popliteal fossa, the SN divides into the tibial nerve (TN) and the common peroneal nerve (CPN). This bifurcation commonly occurs at the apex of the popliteal fossa, but the SN can divide anywhere from the sacral plexus to the popliteal skin crease.1
Although the SN appears to run as a single entity, it is composed of two major components: the TN and CPN bundles. These independent bundles do not mix fibres and have their own epineurium, separated by the Compton–Cruveilhier septum. They descend together in a paraneural sheath consisting of multiple circular layers of extra-neural fascial connective tissue.2,3
The larger tibial branch remains enveloped in this paraneural sheath and descends vertically through the popliteal fossa. It gives rise to many collateral branches, including muscular branches to the major ankle flexors, the sural nerve (cutaneous), and articular branches to the knee and ankle joints, before splitting into its terminal branches: the medial and lateral plantar nerves.
The smaller CPN peels off laterally and descends along the head and then neck of the fibula. It gives off articular branches to the knee joint and branches to the sural nerve before splitting into its terminal components: the superficial and deep peroneal nerves.
The PFCN, also known as the posterior cutaneous nerve of the thigh, is a purely sensory branch of the sacral plexus derived from the first to third anterior sacral rami. It innervates the buttock, posterior scrotum/labia, and posterior thigh as distal as the popliteal fossa. Like the SN, the PFCN also exits the pelvis via the greater sciatic foramen, travelling anterior to the piriformis muscle before descending anterior to the gluteus maximus muscle alongside the inferior gluteal artery. It gradually moves more medial and closer to the skin than the SN. It then descends superficial to the long head of the biceps femoris in a separate fascial plane to the SN. As the PFCN approaches the popliteal fossa, it pierces the fascia lata. It was previously thought to terminate here, however, a recent cadaveric study has reported this nerve to commonly terminate at the proximal or distal lower leg, with only 9.7% of nerves terminating at the level of the popliteal fossa. The clinical significance of this is unknown.4
Traditional landmark approaches to the sciatic nerve
Several landmark approaches to the SN block (SNB) have been described (Table 1), which allow nerve localisation using peripheral nerve stimulation (PNS). When seeking the SN with PNS, an appropriate endpoint is either plantar flexion and inversion, primarily mediated by the TN supplying gastrocnemius and soleus, or dorsiflexion and eversion primarily mediated by the deep peroneal nerve supplying tibialis anterior.
Table 1.
Most common traditional landmark approaches to SNB, including the name of the approach, position of the patient, and the landmarks used
| Approach | Position of patient | Landmarks |
|---|---|---|
| Labat (1923) | Lateral decubitus position Operative side up, knee flexed |
A line is drawn between the GT and PSIS. At the midpoint of this line, a second perpendicular line is drawn caudad for 3 cm marking the point of needle insertion. |
| Winnie (1975) (modification of Labat's approach) | Lateral decubitus position Operative side up, knee flexed |
A line is drawn between the GT and PSIS. A second line is drawn from the GT to the sacral hiatus. The point of needle insertion is defined by drawing a line perpendicular from the midpoint of the first line to its intersection with the second line. This is usually 3–5 cm from the midpoint of the line drawn from the GT to the PSIS. |
| Raj (1975) | Lithotomy position (only the limb to be blocked) Hip and knee flexed maximally to 90–120 degrees |
A line is drawn between the GT and IT. The midpoint marks the point of needle insertion. |
| Beck (1963) (anterior approach) | Supine position | First line is drawn from the anterior superior iliac spine to the pubic tuberosity. A second line is then drawn from the GT parallel to the first line towards the inside thigh. A third perpendicular line is drawn from the midpoint of the first line to meet the second line. This intersection is the point of needle insertion. |
| Mansour (1993) (sacral plexus block) | Lateral decubitus position Operative side up |
A line is drawn between the midpoints of the PSIS and IT. The point of needle insertion is 6 cm along this line from the PSIS. The needle is slowly advanced in a sagittal plane using nerve stimulation. |
When PNS is used in isolation for SNB, a starting current of 1–2 mA is typically used to seek the nerve before lowering to 0.5 mA to ensure appropriate proximity to the nerve before injection. Peripheral nerve stimulation is a useful adjunct to use in combination with ultrasound (US) guidance for proximal SNBs, a technique known as dual location.
Ultrasound-guided approaches to the sciatic nerve
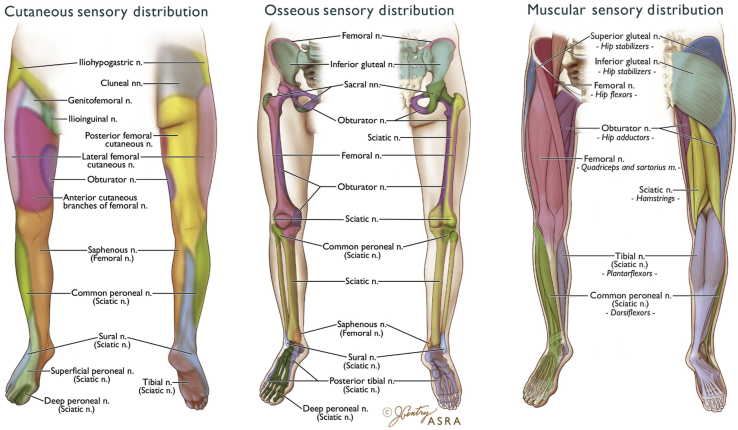
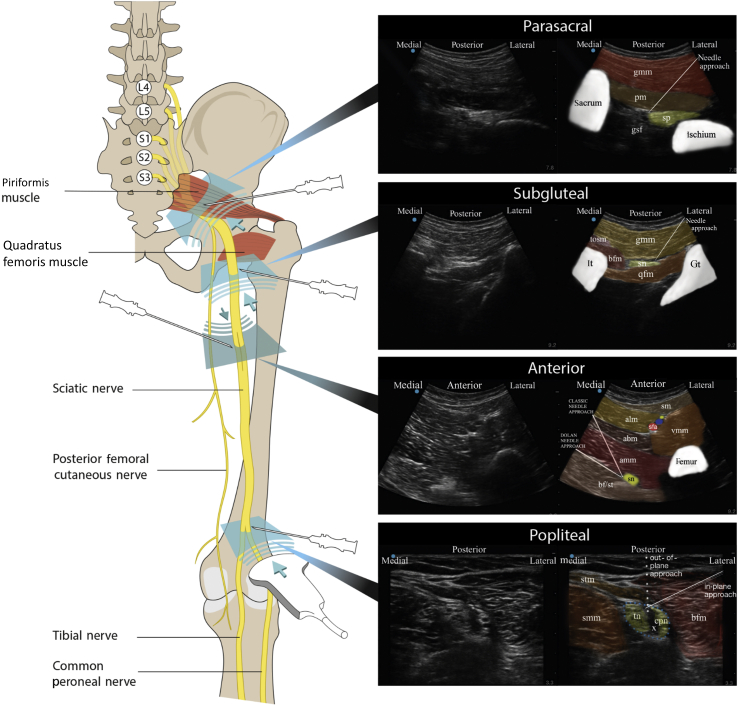
The increasing availability of US has facilitated more targeted approaches to the SN with concurrent visualisation of surrounding anatomical structures. The SN can be targeted at any point along its proximal to distal course. However, consideration must be given to the cutaneous, muscular, and osseous innervation of structures involved in the surgical procedure (Fig. 2). This review will discuss four commonly cited and practical US-guided approaches: parasacral, subgluteal, anterior and popliteal (Fig. 3).
Fig 2.
Cutaneous, muscular, and osseous innervation of the lower limb. Reproduced with permission from the American Society of Regional Anesthesia and Pain Medicine.
Fig 3.
Four US-guided approaches to the SN (parasacral, subgluteal, anterior, and popliteal). Each approach includes the US transducer position, angle of needle insertion, original US image, and coloured US image highlighting the key anatomy relevant to performing the block. Parasacral: gmm, gluteus maximus muscle; gsf, greater sciatic foramen; pm, piriformis muscle; sp, sacral plexus. Subgluteal: bfm, biceps femoris muscle; gt, greater trochanter; it, ischial tuberosity; qfm, quadratus femoris muscle; sn, sciatic nerve; tosm, tendon of semimembranosus muscle. Anterior: abm, adductor brevis muscle; alm, adductor longus muscle; amm, adductor magnus muscle; bf/st, biceps femoris/semitendinosus; sfa, superficial femoral artery; sm, sartorius muscle; sn, sciatic nerve; vmm, vastus medialis muscle. Popliteal: bfm, biceps femoris muscle; blue dotted line, common paraneural sheath; cpn, common peroneal nerve; smm, semimembranosus muscle; stm, semitendinosus muscle; tn, tibial nerve; X, space within common paraneural sheath.
The anisotropic properties of the SN can make it difficult to visualise. The nerve appears more distinct when the US transducer is perpendicular to it, and even small changes in transducer angle can significantly impair visibility. Small adjustments of the transducer, including alterations in pressure, alignment, rotation, and tilt, should be used to optimise the view.
All techniques discussed should be performed in a fully monitored environment as per the guidelines of the Association of Anaesthetists, with secure i.v. access, ‘stop before you block’ check, appropriate sterility, and practical ergonomics.
Local anaesthetic (LA) 20–30 ml is typically used for these approaches. Surgical anaesthesia requires higher concentrations, such as levobupivacaine 0.5%, whilst lower concentrations, such as levobupivacaine 0.25%, may be used for postoperative analgesia.
Parasacral approach
Anatomy
The landmark parasacral approach was first described by Mansour in 1993 and involved blocking the SN at a point distal to the lateral edge of the sacrum and caudal to the sacroiliac joint.5 Although commonly cited as an SNB, the parasacral approach is actually a sacral plexus block that targets branches of the entire sacral plexus before the true SN is formed at the inferior edge of the piriformis muscle. This block is performed at the level of the greater sciatic foramen.5
Advantages
In addition to targeting the SN, this approach blocks other clinically relevant branches of the sacral plexus, including the PFCN, superior gluteal nerve, and the nerve to quadratus femoris. The PFCN must be targeted for any awake surgery involving skin incision to the posterior thigh, such as an above-knee amputation.
Clinical indications
Pelvic surgery, hip surgery, above-knee amputation, surgery below the knee.
Pitfalls
Unrestricted needle advancement deep to the sacral plexus risks injury to the inferior gluteal vessels or rectum.
Technique
The patient is positioned in the lateral decubitus position with the operative side uppermost. The dependant limb should be straightened at the knee and hip with the limb to be blocked flexed at both hip and knee.
The authors' preferred technique is that of the parasacral parallel shift. A curvilinear transducer (2–5 MHz) is placed on the line connecting the posterior superior iliac spine (PSIS) and the GT, between the midpoint of this line and the PSIS. The continuous hyperechoic rim of the iliac bone is identified before the transducer is guided inferomedially until a gap appears in the bone: the greater sciatic foramen. This is the point where the sacral plexus leaves the pelvis.6
Visualisation of the sacral plexus between the sacrum and ischial bone, deep to piriformis, is aided by tilting the transducer slightly caudad. Small changes in probe orientation can achieve a better sonographic nerve appearance. Before needling, colour Doppler should be utilised to visualise pelvic vasculature, such as the inferior gluteal vessels. An in-plane approach is preferred, using dual guidance with PNS. Motor twitch of the SN at 0.5 mA via the nerve stimulator combined with appropriate needle tip position confirms proximality to the sacral plexus, and LA 20 ml is typically injected superficial to the plexus.
Subgluteal approach
Anatomy
This approach targets the SN as it traverses the subgluteal space, between the IT and the GT. The subgluteal space is a well-defined anatomical space between the anterior surface of gluteus maximus and the posterior surface of quadratus femoris. The quadratus femoris muscle attaches to the posterior surface of the GT and IT, and runs deep to the subgluteal space.7,8
Advantages
Reliable bony landmarks aid the identification of the SN at this location. However, injection of LA into the subgluteal space will provide an adequate block even if visualisation of the nerve is difficult.
Pitfalls
Several vascular structures are present within the subgluteal space, including the inferior gluteal vessels, the comitans artery, vein of the SN, and the ascending branch of the medial circumflex femoral artery. Colour Doppler should be utilised before block performance to aid identification of potentially hazardous structures.
The subgluteal approach does not reliably block the PFCN, with one study only reporting 68% coverage. A cadaveric study described a deep investing muscular fascia of the thigh at the subgluteal level, which impeded spread between the SN and PFCN, requiring two separate injections. A targeted US-guided approach to the PFCN block has been recently described.9, 10, 11
Clinical indications
Above-knee amputation (analgesia), knee surgery, surgery below the knee.
Technique
The patient is positioned in the lateral position with the operative side uppermost, hip and knee flexed. A curvilinear transducer (2–5 MHz) is placed between the palpable anatomical landmarks of the GT and IT. The IT (medial) and the GT (lateral) are seen on US as hypoechoic shadows with a thin superficial hyperechoic rim. The large gluteus maximus muscle lies superficial to these bony landmarks and traverses the entire image. The subgluteal space is seen as a hypoechoic space between the hyperechoic borders of the gluteus maximus and quadratus femoris muscles, extending from the GT to the IT. The SN is visualised as an oval hyperechoic structure, sitting on top of the hypoechoic quadratus femoris muscle.
A needle is advanced in-plane from lateral to medial. A subtle needle ‘click’ may be felt as the needle tip passes through the gluteus maximus muscle into the subgluteal space. Distension of the subgluteal space is seen during LA injection with spread of injectate around the nerve. Dual location can be used to aid detection of the nerve if visualisation is difficult. An LA volume of 20 ml is typically used, and rotation of the transducer through 90 degrees seeking a longitudinal plane to the nerve can demonstrate LA in the subgluteal space surrounding it.
Anterior approach
Anatomy
The anterior approach targets the SN in the proximal thigh as it descends medial to the femur between the adductor magnus anteriorly and the biceps femoris and semitendinosus posteriorly.
Advantages
The main advantage of the anterior approach is the ability to perform a proximal SNB with the patient supine. This can be useful where lateral positioning or knee elevation is unsuitable because of pain or trauma, or in the presence of external fixation devices.
Pitfalls
This is an advanced technique because of the depth of the target, difficulty in visualising the anisotropic nerve, and potentially difficult needle visualisation attributable to the steep angle of insertion. Dual localisation is therefore commonly used, even in experienced hands. The anterior approach does not reliability block the PFCN with a reported coverage of 15%.7,12
Clinical indications
Surgery at or below the knee.
Technique
With the patient supine, the leg is slightly abducted and externally rotated. A curvilinear transducer (2–5 MHz) and a 100–150 mm echogenic needle are required because of the target depth (usually between 6 and 9 cm in an average 70 kg patient). Needle tip visualisation technology can also be considered because of the target depth. The transducer is initially placed transversely over the medial thigh around 8 cm distal to the inguinal crease to first visualise the femur before sliding medially to identify the adductor muscles inserting onto the medial femur. Other important structures to note are the superficial femoral artery (SFA) in the sub-sartorial canal, surrounded by the sartorius, vastus medialis, and adductor longus muscles. The SN is located deep to the adductor magnus and posteromedial to the femur. Visualisation of the nerve can be difficult in some patients. The location of the SN can be estimated by plotting it as the apex of a triangle where the SFA and the femur make up its base corners. Although the posterior border of the femur cannot be seen on US, the SN usually lies just deep and medial to this.
The needle is inserted in-plane from anteromedial to posterolateral direction through the adductor muscles taking care not to transect any vital superficial structures (femoral vessels and obturator nerve). As the SN lies just deep to the adductor magnus, using a high current on the PNS to induce adductor magnus muscle twitching indicates correct needle plane position. The adductor muscle twitching disappears as the needle tip enters into the fascial plane containing the SN. Local anaesthetic 20 ml is typically used.
Dolan described a modification of this approach to improve needle visibility.13 By measuring the depth of the SN from the skin using US and inserting the needle at the observed depth in the medial thigh, the needle trajectory becomes more parallel to the transducer in the fascial plane between the dductor magnus and the hamstring muscles (Fig. 3).13
Popliteal approach
Anatomy
This approach targets the SN as it divides into the TN and the CPN in the region of the popliteal fossa, commonly 5–12 cm from the popliteal crease, although this division may occur more proximally.2
In the popliteal fossa, the SN lies superficial to the popliteal vein and artery, and is bordered laterally by the biceps femoris and medially by the semitendinosus and semimembranosus. As the SN divides, the larger TN lies more medially, whilst the smaller CPN courses laterally and more superficially.
The paraneural sheath is a key anatomical structure relevant to the correct performance of this approach. It is a fibrous sheath made of multiple circular layers of extraneural fascial connective tissue surrounding the SN from the lumbosacral plexus to its bifurcation. To facilitate timely onset of block, LA deposition should ideally occur within the paraneural sheath, but external to the separate epineuria of the TN and CPN bundles. However, if this space is difficult to identify on US, circumferential spread around the nerve is adequate.14
Advantages
The distal nature of the block results in preservation of hamstring motor function. The block is also much more superficial compared with the more proximal approaches making the block easier to learn for less experienced practitioners.
Clinical pitfalls
The most common mistake amongst novices when performing the popliteal approach is to block only one of either the TN or CPN. This can occur if the operator performs the block distal to the sciatic bifurcation, mistaking either the TN or CPN for the true SN. This can be avoided by scanning proximally until both nerves can be seen to join within the common paraneural sheath. Cutaneous innervation to the medial aspect of the lower leg is supplied by the saphenous nerve, and this must be blocked separately to provide complete anaesthesia below the level of the knee.
Clinical indications
Ankle surgery, hindfoot surgery, midfoot surgery, below-knee amputation, total knee replacement.
Position
The patient can be placed in three positions depending on the operator's preference and experience:
-
(i)
Supine: The knee is flexed or straight with a support under the lower leg to facilitate transducer placement and manipulation.
-
(ii)
Lateral: The side to be blocked is uppermost.
-
(iii)
Prone: Extra care must be taken to ensure the correct side is blocked.
Each of these positions can facilitate an in-plane or out-of-plane approach. The authors commonly place this block with the patient supine or lateral using an in-plane approach. An out-of-plane approach with lateral or prone positioning may better facilitate a perineural catheter approach with lower reported rates of displacement.15
Technique
A linear transducer (6–15 MHz) is placed transversely at the level of the popliteal crease. A typical starting depth of 4 cm is utilised, attempting to visualise the popliteal artery, and using colour Doppler if necessary. The popliteal vein is seen superficial to the artery if transducer pressure is reduced, and the TN and CPN lie superficially. These nerves appear hyperechoic. However, because of their anisotropic nature, they can be difficult to visualise if the transducer is not perpendicular to the nerve, as the nerve does not travel parallel to the skin. The angle of the transducer usually needs to be adjusted to aim slightly caudally to improve nerve visualisation.
Once both branches are visualised, the transducer is moved proximally until both nerves are seen to converge within the common paraneural sheath. If nerve visualisation proves difficult, asking the patient to plantarflex and dorsiflex the foot is helpful, thus creating the ‘see-saw’ sign as the TN and CPN slide in opposite directions (Video 1).
Supplementary video related to this article can be found at https://doi.org/10.1016/j.bjae.2020.04.004
The following is the supplementary data related to this article:
1
The distance between the nerves and the skin is calculated from the US image, with the needle inserted in-plane at this distance below the US transducer. This aids needle visualisation by reducing the angle between the needle and the transducer. The needle is inserted to a point where both components of the nerve are seen within the common paraneural sheath, but slightly separated by adipose tissue. Single injection at this point may produce adequate spread. However, additional needle positioning and injection may be required to provide optimal circumferential spread. A volume of 20–30 ml LA is typically used.
Motor-sparing ultrasound-guided local anaesthetic infiltration techniques
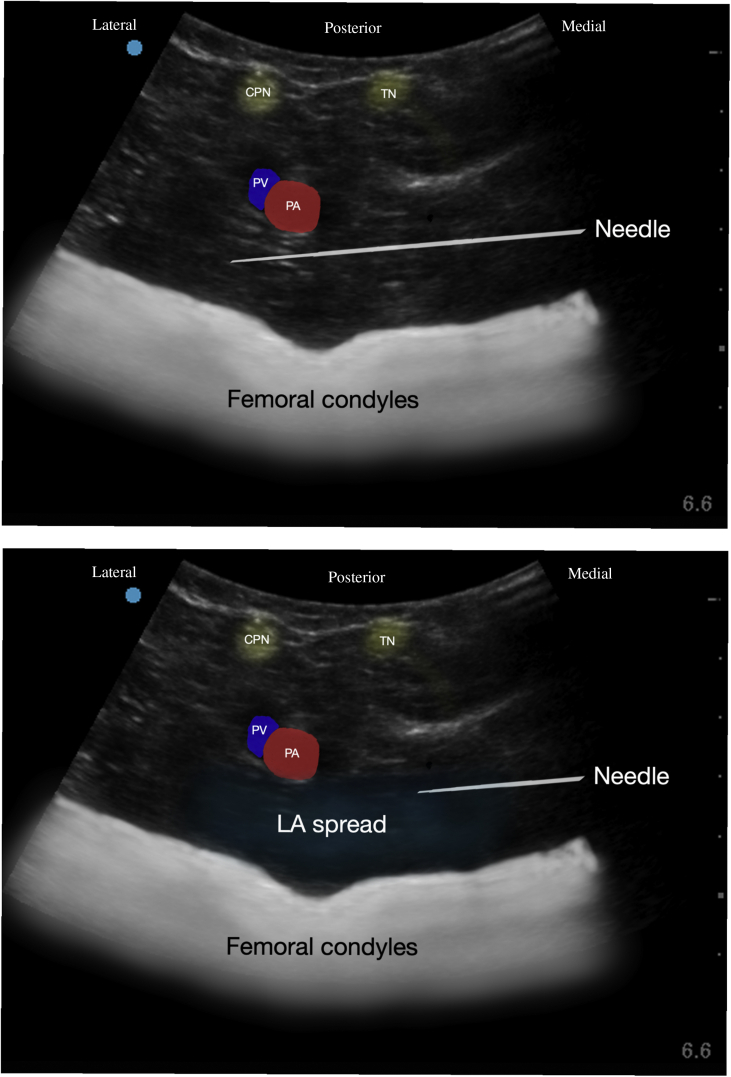
The infiltration of the interspace between the popliteal artery and capsule of the knee (iPACK) block is a novel US-guided approach for postoperative analgesia after total knee arthroplasty. It targets the genicular nerves innervating the posterior knee joint capsule, which are supplied by articular branches of the sciatic and posterior obturator nerves. Postoperative analgesia is therefore provided to the posterior knee, with motor sparing of the TN and CPN.16
The patient is positioned in the supine position with the knee flexed and hip abducted. A curvilinear transducer (2–5 MHz) is placed on the medial aspect of the thigh just proximal to the popliteal crease, and the probe is then slid towards the posterior aspect of the popliteal fossa aiming to visualise the femoral condyles and popliteal artery. Injection of LA targets the interspace between these structures where the genicular branches lie.
Both proximal (one finger breadth above the patella) and distal (at the superior border of the femoral condyles) injection points have been described. In both techniques, the needle is inserted in-plane in a medial-to-lateral direction between the popliteal artery and the femur/femoral condyles until the needle tip is 1–2 cm beyond the lateral edge of the popliteal artery. At this point, LA is injected, observing for a hypoechoic pool between the aforementioned structures. The needle is slowly withdrawn with a continuing injection to coat the entire area deep to the artery. In total, 20–30 ml of a low-concentration long-acting LA is given (Fig. 4).17
Fig 4.
Top image: annotated US image of an iPACK block taken with relevant anatomy labelled (CPN, common peroneal nerve; PA, popliteal artery; PV, popliteal vein; TN, tibial nerve) with needle approach. Bottom image: same image with ideal LA spread on needle withdrawal.
Potential complications of this technique include spread of injectate to the TN and CPN, and the theoretical risk of infection attributable to proximity to the surgical site. Further research is required, but emerging evidence suggests improved analgesia and reduced opioid consumption after total knee arthroplasty.18
Clinical application
For surgery below the knee, a popliteal approach provides adequate analgesia or anaesthesia in combination with a saphenous nerve block if required. However, this will not provide coverage for a thigh tourniquet.
For surgery above the knee, consideration should be given to the PFCN. A proximal parasacral approach is required to reliably block both the SN and PFCN, which is vital for awake surgery where total anaesthesia of the surgical site is required.
Regional anaesthesia for total knee arthroplasty has evolved in favour of motor-sparing techniques, such as US-guided infiltration of the posterior capsule (iPACK) in combination with an adductor canal block to facilitate earlier postoperative mobilisation. However, an SNB remains a useful technique for patients at high risk of significant acute pain or postoperative opioid requirements.19,20
Placement of a perineural catheter may be considered for certain lower-limb surgical procedures associated with significant postoperative pain, such as hind-foot surgery, ankle fusion, and ankle replacement.
Conclusions
Sciatic nerve blocks can be used to provide anaesthesia or postoperative analgesia for a wide range of lower-limb procedures. When considering which SN approach to use, it is vital to understand the anatomy of the SN itself, and the cutaneous, osseous, and muscular innervation provided by the nerve. Ultrasound guidance allows visualisation of typical sonographic landmarks relevant to the safe performance of each approach.
Declaration of interests
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) are accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Sean Shevlin FRCA PG Dip Med Ed is currently a fellow in regional anaesthesia in Belfast. He is currently undertaking the MSc in Regional Anaesthesia through the University of East Anglia.
Lloyd Turbitt FRCA MSc (RA) is a consultant at the Royal Victoria Hospital, Belfast. He has undertaken a fellowship in regional anaesthesia in Toronto and is on the teaching faculty for the MSc in regional anaesthesia at the University of East Anglia. He is a board member of Regional Anaesthesia UK and was lead organiser for their 2019 annual scientific meeting.
David Johnston FRCA EDRA is a consultant at the Royal Victoria Hospital, Belfast. He completed a fellowship in regional anaesthesia at London Health Sciences Centre, Ontario. He has multiple publications and research interests related to regional anaesthesia.
Matrix codes: 1D02, 2G02, 3A09
References
- 1.Vloka J.D., Hadžić A., April E., Thys D.M. The division of the sciatic nerve in the popliteal fossa: anatomical implications for popliteal nerve blockade. Anesth Analg. 2001;92:215–217. doi: 10.1097/00000539-200101000-00041. [DOI] [PubMed] [Google Scholar]
- 2.Sladjana U.Z., Ivan J.D., Bratislav S.D. Microanatomical structure of the human sciatic nerve. Surg Radiol Anat. 2008;30:619–626. doi: 10.1007/s00276-008-0386-6. [DOI] [PubMed] [Google Scholar]
- 3.Abdallah F.W., Chan V.W. The paraneural compartment: a new destination? Reg Anesth Pain Med. 2013;38:375–377. doi: 10.1097/AAP.0b013e3182a34dfa. [DOI] [PubMed] [Google Scholar]
- 4.Feigl G.C., Schmid M., Zahn P.K., Gonzalez C.A., Litz R.J. The posterior femoral cutaneous nerve contributes significantly to the sensory innervation of the lower leg: an anatomical investigation. Br J Anaesth. 2020;124:308–313. doi: 10.1016/j.bja.2019.10.026. [DOI] [PubMed] [Google Scholar]
- 5.Mansour N.Y. Re-evaluating the sciatic nerve blocks: another landmark for consideration. Reg Anesth. 1993;18:322–323. [PubMed] [Google Scholar]
- 6.Bendtsen F., Lönnqvist P.A., Jepsen K.V., Petersen M., Knudsen L., Børglum J. Preliminary results of a new ultrasound-guided approach to block the sacral plexus: the parasacral parallel shift. Br J Anaesth. 2011;107:278–280. doi: 10.1093/bja/aer216. [DOI] [PubMed] [Google Scholar]
- 7.Chan V.W., Nova H., Abbas S., McCartney C.J., Perlas A., Xu D.Q. Ultrasound examination and localization of the sciatic nerve: a volunteer study. Anesthesiology. 2006;104:309–314. doi: 10.1097/00000542-200602000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Karmakar M.K., Kwok W.H., Ho A.M., Tsang K., Chui P.T., Gin T. Ultrasound-guided sciatic nerve block: description of a new approach at the subgluteal space. Br J Anaesth. 2007;98:390–395. doi: 10.1093/bja/ael364. [DOI] [PubMed] [Google Scholar]
- 9.Ota J., Sakura S., Hara K., Saito Y. Ultrasound-guided anterior approach to sciatic nerve block: a comparison with the posterior approach. Anesth Analg. 2009;108:660–665. doi: 10.1213/ane.0b013e31818fc252. [DOI] [PubMed] [Google Scholar]
- 10.Johnson C.S., Johnston R.L., Niessen A.D., Stoike D.E., Pawlina W. Ultrasound-guided posterior femoral cutaneous nerve block: a cadaveric study. J Ultrasound Med. 2018;37:897–903. doi: 10.1002/jum.14429. [DOI] [PubMed] [Google Scholar]
- 11.Meng S., Lieba-Samal D., Reissig L.F. High-resolution ultrasound of the posterior femoral cutaneous nerve: visualization and initial experience with patients. Skeletal Radiol. 2015;44:1421–1426. doi: 10.1007/s00256-015-2177-6. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida T., Nakamoto T., Hashimoto C., Aihara S., Nishimoto K., Kamibayashi T. An ultrasound-guided lateral approach for proximal sciatic nerve block: a randomized comparison with the anterior approach and a cadaveric evaluation. Reg Anesth Pain Med. 2018;43:712–719. doi: 10.1097/AAP.0000000000000835. [DOI] [PubMed] [Google Scholar]
- 13.Dolan J. Ultrasound-guided anterior sciatic nerve block in the proximal thigh: an in-plane approach improving the needle view and respecting fascial planes. Br J Anaesth. 2013;110:319–320. doi: 10.1093/bja/aes492. [DOI] [PubMed] [Google Scholar]
- 14.Perlas A., Wong P., Abdallah F., Hazrati L.N., Tse C., Chan V. Ultrasound-guided popliteal block through a common paraneural sheath versus conventional injection: a prospective, randomized, double-blinded study. Reg Anesth Pain Med. 2013;38:218–225. doi: 10.1097/AAP.0b013e31828db12f. [DOI] [PubMed] [Google Scholar]
- 15.Hauritz R.W., Pedersen E.M., Linde F.S. Displacement of popliteal sciatic nerve catheters after major foot and ankle surgery: a randomized controlled double-blinded magnetic resonance imaging study. Br J Anaesth. 2016;117:220–227. doi: 10.1093/bja/aew172. [DOI] [PubMed] [Google Scholar]
- 16.Thobhani S., Scalercio L., Elliot C.E. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J. 2017;17:233–238. [PMC free article] [PubMed] [Google Scholar]
- 17.Tran J., Giron-Arango L., Peng P.W.H., Sidha S.K., Agur A., Chan V. Evaluation of the iPACK block injectate spread: a cadaveric study. Reg Anesth Pain Med. 2019;44:689–694. doi: 10.1136/rapm-2018-100355. [DOI] [PubMed] [Google Scholar]
- 18.Kim D.H., Beathe J.C., Lin Y. Addition of infiltration between the popliteal artery and the capsule of the posterior knee and adductor canal block to periarticular injection enhances postoperative pain control in total knee arthroplasty: a randomized controlled trail. Anesth Analg. 2019;129:526–535. doi: 10.1213/ANE.0000000000003794. [DOI] [PubMed] [Google Scholar]
- 19.O’Donnell R., Dolan J. Anaesthesia and analgesia for knee joint arthroplasty. BJA Educ. 2018;18:8–15. doi: 10.1016/j.bjae.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zorrilla-Vaca A., Li J. The role of sciatic nerve block to complement femoral nerve block in total knee arthroplasty: a meta-analysis of randomized controlled trials. J Anesth. 2018;32:341–350. doi: 10.1007/s00540-018-2480-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1