Learning objectives.
By reading this article you should be able to:
-
•
Appreciate the principles of quality improvement.
-
•
Describe how to start a quality improvement project.
-
•
Describe the different types of quality improvement measures.
Key points.
-
•
Take steps to truly understand a problem before trying to solve it.
-
•
Involve all members of the multidisciplinary team, including patients where possible.
-
•
Make small-scale changes and review their impact before moving on.
-
•
Measurement is the ruler of improvement.
-
•
Collect ‘just enough’ data to know if interventions are working.
Clinical scenario.
You notice that a number of patients on your regular elective orthopaedic list need to be actively warmed in recovery because they are hypothermic after leaving the operating theatre. You wonder if anyone else is experiencing the same and discover that 2 yr ago a departmental audit was conducted.
In the second of three articles we discuss the key factors in starting a quality improvement project.
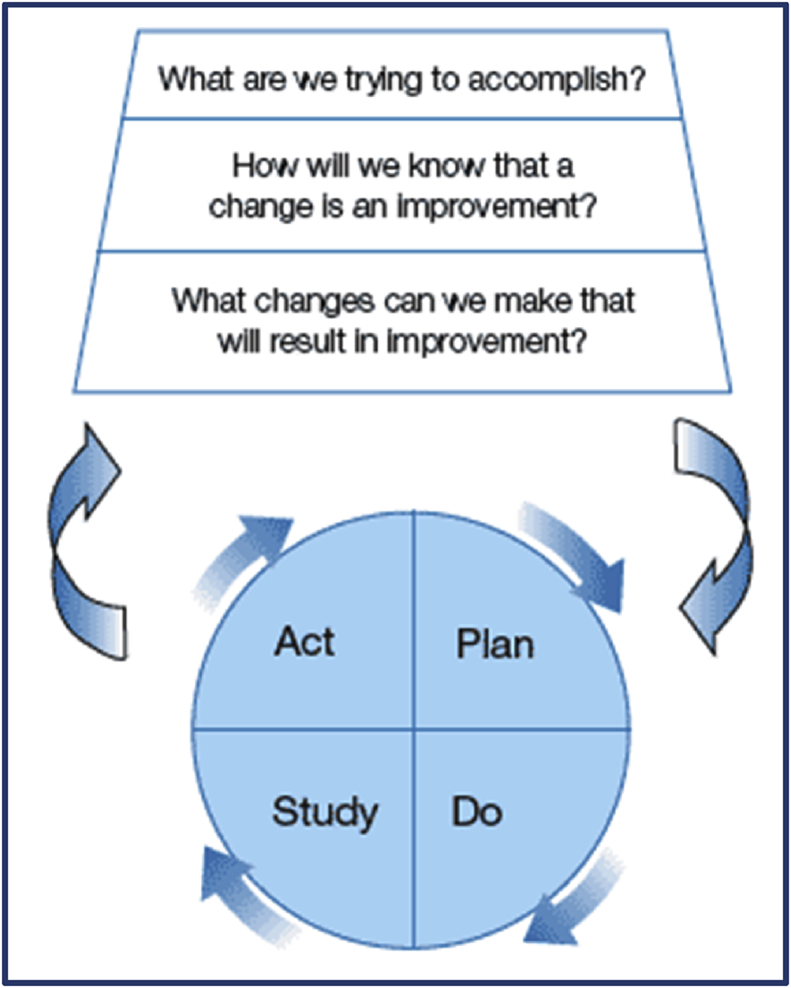
Modern quality improvement builds upon the work of W. Edwards Deming in the mid 20th century. He was an engineer and statistician who is widely regarded as the father of quality improvement, and many models that have been developed draw upon his work. There are a wide variety of improvement methods and they are all mutually beneficial, although some have a greater appeal and are more intuitive. The Model for Improvement1 (Fig. 1) has gained widespread acceptance in healthcare and is the model upon which the Institute for Healthcare Improvement bases its methodology. It is widely used within the National Health Service, and consists of three essential questions followed by Plan-Do-Study-Act (PDSA) cycles (discussed in more detail later).2 The simple appearance of this and other improvement models belies the rigorous application required to ensure success and the complex nature of most healthcare-related problems.
Fig 1.
Project initiation
Improvement projects have a natural life cycle and flow through the phases of Initiation→ Planning→Delivery→Evaluation → Closure.
The first step in many improvement projects is frustration with the status quo. It is important that the frustration is converted into a clear aim to provide the answer to the Model for Improvement's question ‘What are we trying to accomplish?’3 The accuracy of the aim provides focus for the other phases of the project and prevents potential misinterpretation by others. It will also help you articulate the case for change and get others involved in your project.
Consider the following aim:
‘This organisation wants to reduce the number of patients leaving theatre hypothermic’
This statement is non-specific and is unlikely to focus attention or generate a sense of urgency to improve. Project aims should be SMART:
-
(i)
Specific
-
(ii)
Measurable
-
(iii)
Attainable
-
(iv)
Relevant
-
(v)
Time bound
An improved goal might therefore be:
‘This organisation wants to reduce the number of patients leaving orthopaedic theatres with a temperature of less than 36°C by 30% over the next 3 months in order to reduce postoperative wound infections’
More generically, this may be considered as a multipart statement:
‘This organisation wants to [increase/decrease outcome measure] in [this setting/these patients] by [amount] over [time frame] because [reason for change].’
Once the aim is articulated it is important to consider who else may need to be involved in the project to make it a success. Ideally, this should be multi-disciplinary involving all the major stakeholders, including patients where feasible.
Project planning
Understanding the problem
The true origin of a problem may not be what is initially expected. It is important to identify the root causes of the problem before introducing changes. It is very easy to jump directly to potential solutions without taking time to investigate root causes; such solutions are unlikely to be successful.
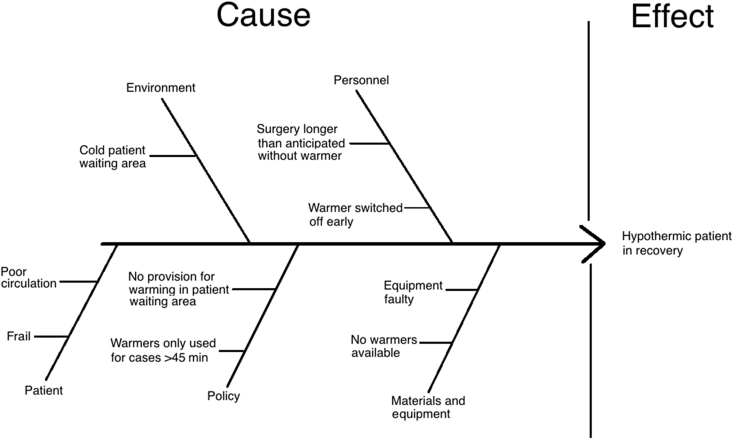
There are many methods to help find the underlying cause. Two commonly used ones are the ‘Five Whys’ approach, combined with a fishbone, or Ishikawa, diagram.4, 5 In simple terms, the five whys approach consists of continuing to ask why until the root cause is identified.
Start by precisely defining the question. In answering the question, keep asking why until the root cause(s) are addressed. For example:
Because they arrive cold in the anaesthetic room why?
Because they are changed into gowns early why?
Because there are insufficient staff to help patients later why?
Because the staff nurses are busy administering premedication.
‘Why do 30% of elective surgical patients enter recovery after general anaesthesia with a temperature under 36°C?’
Potential solutions can then be tailored to the root causes identified; in this case, it might be that there is a different time or person to give the premedication.
There will usually be other explanations for the issue which can be explored in seeking alternative answers to the ‘why’ questions, and the overall results can often be grouped according to common themes. These thematic explanations may be displayed using a fishbone diagram (Fig. 2) that is constructed by:
-
(i)
Identifying a problem.
-
(ii)
Drawing an arrow pointing to the problem.
-
(iii)
Identifying who and what are involved in the problem and when and where it occurs.
-
(iv)Adding categories for causes, which may include:
- Patient, personnel, policy, equipment, and environment.
-
(v)
Brainstorming, exploring and gradually building up each category with primary and secondary causes.
-
(vi)
The diagram should now show all possible causes of the problem.
-
(vii)
The team should now identify and prioritise the main causes.
Fig 2.
Fishbone or Ishikawa diagram.
Process mapping
Systems are complex entities and in order to improve systems within them, we need to answer a few questions about individual elements:
-
(i)
How does a process work?
-
(ii)
What components are involved?
-
(iii)
How does the process flow?
A process map can help a team visualise both individual elements of a process and the process as a whole; two such tools are swim-lane diagrams and spaghetti diagrams.4 The first step is to define the start and end points of the process to be mapped, otherwise mapping may become unmanageable. Stakeholders must then list the individual steps in the process including decisions and delays, and who is involved at each stage. These steps are then visualised as a flowchart and edited as necessary. Swim-lane diagrams (Fig. 3) have the added benefit of dividing the process into ‘lanes’ illustrating who is responsible for various actions. Do not be tempted to take a short cut and do this on your own, as one person rarely understands all the processes involved in healthcare.
Fig 3.
Swim lane diagram showing the process from a patient arriving to the start of the anaesthetic. Pre-op (pre-operative), WHO (World Health Organisation), ODP (Operating Department Practitioner).
A broader approach to process mapping is the A3 method.5, 6 Named for the size of paper typically used to capture data on a single-sheet, this tool focuses on understanding the problem with a strong emphasis on data acquisition and analysis, but also encourages collaboration between the team and stakeholders and allows changes to be tracked. An A3 sheet can also be used as an overarching project planning document. Once a project has been completed, an A3 chart acts as a record as to how a change was successfully introduced.
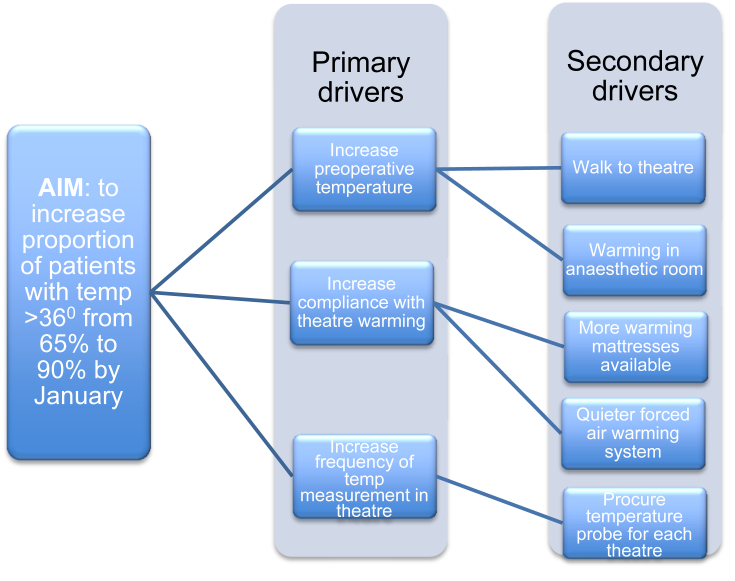
Driver diagrams
Driver diagrams (Fig. 4) can help to show where improvements can be made that will impact upon the outcome.7 They support the Model for Improvement by helping to delineate the answers to the question: ‘What change(s) can we make that will result in an improvement?’3 They are particularly useful when the underlying stimulus for improvement is organisational rather than personal, as it clearly aligns the relevant system components with the aims of the project.
Fig 4.
Driver diagram.
Measurement
‘How will we know that a change is an improvement?’
Measurement could be described as the defining principle of quality improvement methodology. Instead of traditional audit methods, based on complete data capture at discrete intervals, improvement tools rely on frequent sampling and assessing simple, often surrogate, measures of improvement. According to the Institute for Healthcare Improvement, there are three main types of measure:1, 3
-
(i)
Outcome: patient based—what are the outcomes for the patient population being studied?
For example: what percentage of patients have surgical site infections?
-
(ii)
Process: is the system working as it should?
For example: what percentage of patients enter the recovery room with a temperature of greater than 360C?
What percentage of patients have their temperature recorded on the preadmission ward, and in the anaesthetic room?
-
(iii)
Balancing: has improvement in one area led to a decline in performance in another?
For example: is there an increased cost from warming patients intraoperatively?
Data collection principles
-
(i)
Agree with the team on what exactly is being measured and ensure everyone uses the same definition(s).
-
(ii)
Confirm whether raw counts, percentages, ratios, or intervals are most appropriate.
Counts are useful when the background population is relatively static; for example, the number of patients on a ward. Percentages are used when there is a recognised occurrence of a problem that needs to be reduced. Ratios help to show incidence compared with risk (i.e. number of surgical site infections per 1000 operations). Intervals can be used to collect data where the absolute numbers are low (e.g. number of days between episodes of MRSA bacteraemia).8
-
(i)
Consider using data that is already electronically collected as opposed to that which requires detailed review of notes, for example consider time of surgical booking (which is likely to be available from theatre information systems) to provide a surrogate marker of decision-to-operate time (which can only be obtained from the physical notes).
-
(ii)
Take a baseline measurement before your intervention; if it proves difficult to capture, then consider undertaking PDSA cycles to develop a more practical indicator (but do not allow the main aims of the project to be overshadowed by improving data quality).
-
(iii)
Collect only enough data to be able to show whether or not the intervention has made a difference.
-
(iv)
Patient outcome measures are preferable to process measures where available.
Longitudinal measurement of small samples of data therefore allows for:
-
(i)
Feedback on the results of small changes during PDSA cycles.
-
(ii)
Statistical analysis.
-
(iii)
Visual representation of performance.
-
(iv)
Confirmation of long-lasting change.
If, in the longer term, the project aims are being met consistently, then it may be feasible to decrease sampling frequency.
Documentation
A project plan document should be created which details:
-
(i)
Actions to be undertaken and anticipated results of those actions.
-
(ii)
Who will undertake them?
-
(iii)
Over what time frame?
-
(iv)
Where ideas will be tested?
-
(v)
A single change should be tested in a single location (e.g. an individual ward or theatre), so that change can happen in a timely manner and the effects of failure are minimised.
-
(vi)
How effective communication with stakeholders will be achieved?
Project delivery
Changes laid out on the project plan should be implemented using PDSA cycles. PDSA cycles are a way of implementing and testing small changes in a structured way.2, 3, 9 These small-scale tests of change build upon each other in an iterative process. Because they are small-scale changes they are ‘low stakes’ as each one does not involve a large investment of time to plan or deliver. The learning from the outcome, if it is not as expected in your carefully planned test of change, is as important as the successes, and these provide a great insight into the process.
PDSA
-
(i)
PLAN how to explicitly test a small change
-
(ii)
DO what is planned
-
(iii)
STUDY the outcomes (expected and unexpected) of the test
-
(iv)
ACT on the results to modify and improve
In the past, there has been criticism of healthcare workers trying to create a perfect plan before starting a test of change. This delays the start of the project and leads to a loss of motivation. More recently, this has shifted to a situation where there is too much ‘doing’ and not enough ‘planning’ or ‘studying’.10 All parts of the PDSA cycle are important.
Timely collection, analysis, and feedback of the data are crucial to maintaining team motivation. They allow the opportunity to make regular reviews of progress and perform rapid intervention when problems have been identified.
This delivery phase is where projects are most likely to fail, and it may be necessary to take action to reinvigorate the project if momentum is lost.
Project evaluation
Were the aims of the project achieved? If not, what prevented this from happening?
Were the resources used justifiable in light of the results?
How has the project improved patient and staff experience?
Project closure
The project should be formally closed to ensure that:
-
(i)
Those involved in the project are satisfied with its outcome.
-
(ii)
Learning or procedural changes have been disseminated as intended.
Summary
Quality improvement (QI) is a systematic way of creating positive change. Its effective deployment requires a conceptual shift away from the audit methodology with which most healthcare providers are comfortable. QI's core tenets of truly understanding: (i) the problem, (ii) the system, (iii) variation, and (iv) the psychology of change, drive its methodology:
-
(i)
Get the right people involved from the start.
-
(ii)
Take time to understand the problem without leaping first to solutions.
-
(iii)
Make small, reversible changes and test their efficacy in a defined location or population.
-
(iv)
Collect ‘just enough’ data, and use existing sources where possible.
Biographies
Lauren Weekes FRCA is a final year specialty trainee in anaesthesia in the South West Peninsula deanery. She has undertaken an advanced module in quality improvement, and is a member of the Health Foundation's Q Community.
Tom Lawson FRCA is Consultant at Plymouth Hospitals NHS Trust. His interests include quality improvement methodology and basic science for FRCA.
Matt Hill BMedSci, MRCPCH, FRCA, MSc is a Consultant at Plymouth Hospitals NHS Trust and Honorary Fellow at Plymouth University Peninsula School of Medicine and Dentistry, where he teaches Quality Improvement. He has an MSc in Quality and Safety in Healthcare and been faculty for the IHI. He was a founding member of the Health Foundation's Q community and is the Clinical Lead for the safety culture work stream of the national Patient Safety Collaborative.
Matrix codes: 1H02, 2H02, 3J00
Declaration of interest
There is no declaration of interest to be declared.
MCQs
The associated MCQs (to support CME/CPD activity) can be accessed at www.bjaed.org/cme/home by subscribers to BJA Education.
References
- 1.Langley G., Moen R.D., Nolan K.M., Nolan T.W., Norman C.L., Provost L.P. Jossey–Boss; San Francisco: 2009. The improvement guide: a practical approach to enhancing organizational performance; p. 512. [Google Scholar]
- 2.The Scottish Government Health Delivery Directorate: Improvement and support Team . 2009. The scottish primary care collaborative summary.http://www.gov.scot/Publications/2008/01/14161901/3 Available from: [Google Scholar]
- 3.Institute for Healthcare Improvement. Science of Improvement: Establishing Measures. Available from: http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementEstablishingMeasures.aspx [Accessed 22 December 2017]
- 4.Panesar S.S., Carson-Stevens A., Salvilla S.A., Sheikh A. 1st ed. Wiley Blackwell; Chichester: 2014. Patient safety and healthcare improvement at a glance. [Google Scholar]
- 5.NHS Institute for Innovation and Service . New Audience Limited; Aldridge: 2010. The handbook of quality and Service improvement tools. [Google Scholar]
- 6.Health Foundation . 2013. Improving patient flow.http://www.health.org.uk/sites/health/files/ImprovingPatientFlow_fullversion.pdf Available from: [Google Scholar]
- 7.Joint Royal Colleges of Physicians Training Board, & Health Education England . 2014. Learning to Make a Difference Quality improvement in practice: a core competence of medical training in the 21st century.https://www.rcplondon.ac.uk/guidelines-policy/ltmd-trainees Available from: [Google Scholar]
- 8.Clarke J., Davidge M., James L. 2010. The how-to guide for measurement for improvement.https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/How-to-Guide-for-Measurement-for-Improvement.pdf Available from: [Google Scholar]
- 9.NHS Improvement . 2014. First steps towards quality improvement: a simple guide to improving services.https://www.england.nhs.uk/improvement-hub/publication/first-steps-towards-quality-improvement-a-simple-guide-to-improving-services/ Available from: [Google Scholar]
- 10.Reed J.E., Card A.J. The problem with Plan-Do-Study-Act cycles. BMJ Qual Saf. 2016;25:147–152. doi: 10.1136/bmjqs-2015-005076. [DOI] [PMC free article] [PubMed] [Google Scholar]
Further reading
- 11.How to improve, Institute for Healthcare Improvement, http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx.
- 12.Quality Improvement Zone, NHS Education for Scotland, https://learn.nes.nhs.scot/741/quality-improvement-zone.
- 13.Quality improvement made simple, Health Foundation, 2013, http://www.health.org.uk/publication/quality-improvement-made-simple.
- 14.Context for Successful Quality Improvement, Health Foundation, 2015, http://www.health.org.uk/sites/health/files/ContextForSuccessfulQualityImprovement.pdf.
- 15.Improvement Hub, NHS Improvement, https://improvement.nhs.uk/improvement-hub/.