Learning objectives.
By reading this article you should be able to:
-
•
Describe the anatomy of the anterior and posterior abdominal wall in relation to the performance of abdominal wall blocks for intra-abdominal surgery.
-
•
Understand the indications for, and how to undertake transversus abdominis plane, quadratus lumborum, and transversalis fascia blocks.
-
•
Recognise that newer blocks are emerging that may be applicable to intra-abdominal surgery.
Key points.
-
•
Abdominal wall blocks are performed on the principle of high-volume local anaesthetic deposition within a fascial plane.
-
•
Ultrasound-guided performance with constant visualisation of the needle increases the accuracy of placement and reduces inadvertent visceral or neurovascular injury.
-
•
Abdominal wall blocks provide primarily somatic analgesia, but newer blocks may also block visceral nerves.
-
•
Abdominal wall blocks provide a relatively safe alternative to epidural analgesia with no motor block, hypotension, or risk to the central neuraxis.
-
•
Novel blocks, such as the erector spinae plane and quadratus lumborum, are gaining popularity, but the evidence is limited.
Abdominal wall blocks provide analgesia in a number of clinical situations and the use of ultrasound has enabled variations of existing blocks to be developed, and new blocks to be introduced. Thoracic epidural analgesia (TEA) has traditionally been used in intra-abdominal surgery, but concerns with this technique include hypotension, motor block, and the risk of neurological damage, particularly in the presence of anticoagulant or antiplatelet therapy. Abdominal wall blocks avoid the risks and adverse effects of central neuraxial blockade and provide a relatively safe alternative to TEA. These blocks may therefore be warranted where epidural anaesthesia has not been possible either for technical reasons or patient wishes; where the risk of complications is increased (e.g. sepsis, coagulopathy, or pre-existing neurological conditions); or in circumstances such as unexpected conversion to an open surgical procedure. The duration of abdominal wall blockade can also be prolonged by catheter placement and may be a viable alternative to TEA, especially where enhanced recovery protocols are used and not just in situations where TEA may be contraindicated.
This article outlines the ultrasound-guided techniques of some of the popular and newer abdominal wall blocks for intra-abdominal surgery: the transversus abdominis plane (TAP), quadratus lumborum (QL), erector spinae plane (ESP), and transversalis fascia plane (TFP) blocks. The indications, risks, clinical applications, and available evidence are detailed below. Ilioinguinal and iliohypogastric blocks are not included whereas rectus sheath blocks have been discussed recently in this journal.1
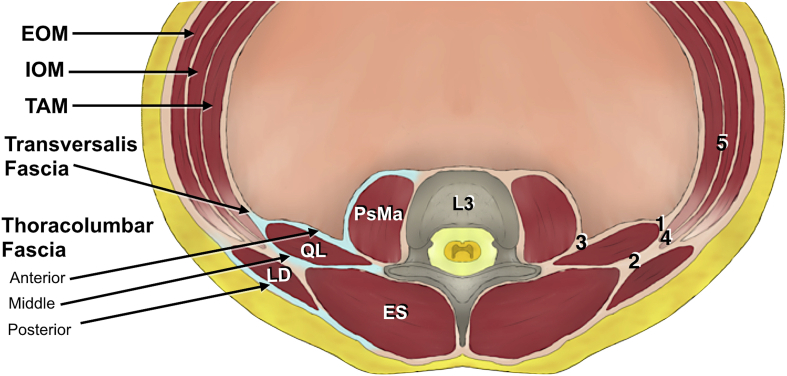
Anatomy of the anterior and posterior abdominal wall
Figure 1 shows a cross section through the posterolateral aspect of the abdominal wall at the level of L3. On each side, the anterior abdominal wall is bounded superiorly by the costal margin and xiphoid process, inferiorly by the inguinal ligament and pelvic bone, and laterally by the posterior axillary line. The lateral aspect of the anterior abdominal wall is composed of three main muscle layers, each with an associated fascial sheath. These muscles are the external oblique most superficially, internal oblique and then transversus abdominis. Deep to the muscle layers lie the transversalis fascia, extraperitoneal fat, and parietal peritoneum.2
Fig 1.
Cross section of posterolateral abdominal wall at L3 level showing the transversalis fascia and the anterior, middle and posterior layers of the thoracolumbar fascia. Numbers relate to the needle endpoints: 1) lateral QL (QL1) block, 2) posterior QL (QL2) block, 3) transmuscular QL (QL3 or anterior) block, 4) posterior TAP block, and 5) lateral TAP block. We thank Dr Parthipan Jegendirabose for his assistance with generating this image. EOM, external oblique muscle; ES, erector spinae; IOM, internal oblique muscle; LD, latissimus dorsi; PsMa, psoas major; QL, quadratus lumborum; TAM, transversus abdominis muscle.
The external oblique muscle (EOM) arises from the fifth to 12th ribs, passing inferomedially to insert into the iliac crest and pubic tubercle. It becomes aponeurotic at the midclavicular line, with the inferior edge forming the inguinal ligament. The internal oblique muscle (IOM) arises from the iliac crest, passing superomedially to the 10–12th ribs and linea alba. It blends with the medial edge of the EOM aponeurosis to form the rectus sheath. The transversus abdominis muscle (TAM) fibres originate from the internal aspect of the seventh to 12th costal cartilages, thoracolumbar fascia (TLF), and iliac crest, and run transversely to insert into the linea alba. Its aponeurosis also contributes to the rectus sheath.2
The rectus abdominis muscle (RAM) is a paired muscle, arising from the pubic crest and passing to the xiphoid process and fifth to seventh costal cartilages.2 It is covered by the rectus sheath and separated in the midline by the linea alba. Superiorly the anterior rectus sheath is composed of the aponeuroses of EOM and IOM, whereas the posterior rectus sheath is formed by the IOM aponeurosis (this splits into two layers) and the TAM aponeurosis. The RAM attaches to the anterior rectus sheath via transverse tendinous insertions, which divide the muscle into its typical ‘six-pack’ appearance. This prevents spread of local anaesthetic, and therefore rectus sheath blocks are placed posterior to the RAM where the sheath is undivided.1, 2 Inferior to the arcuate line (level of the anterior superior iliac spine) the aponeuroses of the EOM, IOM, and TAM pass anteriorly, meaning the rectus sheath is deficient posteriorly and the RAM is lined only by the thin transversalis fascia.2
The thoracoabdominal nerves supplying the abdomen are derived from the anterior rami of T6 to T12. A lateral cutaneous branch supplies the lateral abdominal wall, whereas anteriorly the nerves lie in the TAP between the IOM and TAM, along with the L1 anterior ramus. T6 to T9 enter the TAP medial to the anterior axillary line, with the subsequent nerves entering progressively more laterally. The nerves appear to communicate freely in the TAP forming an anteriorly positioned ‘intercostal plexus’. T9 to L1 form a ‘TAP plexus’ near the deep circumflex iliac artery, which can lead to substantial individual variation of traditional dermatomal patterns. T9 to L1 also form a ‘rectus sheath plexus’ alongside the deep inferior epigastric artery.3
The posterior abdominal wall is loosely defined as the area bounded medially by the thoracolumbar vertebrae, laterally by the lateral abdominal walls, anteriorly by the parietal peritoneum, and inferiorly by the pelvic girdle. The QL muscle arises from the iliac crest and extends to the L1 to L4 transverse processes and the 12th rib. The psoas major muscle is anterior and medial to the QL, originating from the T12 to L5 transverse processes and attaching to the lesser trochanter. The TLF arises from the spinous processes of the thoracic and lumbar vertebrae and is most commonly described as dividing into three layers. The anterior layer of the TLF is known as the transversalis fascia, and it lines the peritoneal surface of the TAM, following the QL and psoas major cephalad through the diaphragm.2 The ilioinguinal and iliohypogastric nerves, arising from L1 (and sometimes contributed to by T12), emerge at the lateral border of the psoas major muscle before passing inferiorly over the anterior surface of QL and deep to TAM, commonly entering the TAP close to the anterior third of the iliac crest.2
Pain from intra-abdominal surgery is a combination of somatic and visceral pain. Visceral pain is transmitted by the autonomic nervous system via sympathetic fibres that form plexuses in close proximity to the viscera themselves. This pain tends to be diffuse, poorly localised, and dull, and may be associated with autonomic symptoms such as nausea, vomiting, and sweating.4 Nerve blocks of the abdominal wall generally only treat somatic pain, which is more localised; hence they should be used as part of a multimodal approach to analgesia. Newer blocks, however, as described below, may have the potential to contribute to visceral pain through spread to the paravertebral space where the sympathetic chain lies.
Specific blocks and their clinical applications
Transversus abdominis plane (TAP)
The aim is to block the T7–L1 spinal nerves within the TAP, for which there are a variety of approaches. Traditionally, the posterior TAP block is performed with a landmark technique in the triangle of Petit (area defined inferiorly by the iliac crest, anteriorly by the EOM, and posteriorly by the latissimus dorsi muscle).5 ‘Two pops’ are felt as the needle passes through the plane between the EOM and IOM and then between the IOM and TAM. However, cadaver studies have demonstrated large variability in the anatomy of this region, rendering this technique unreliable.
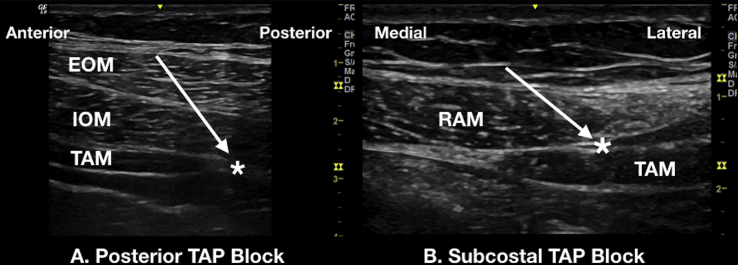
Ultrasound guidance allows for a more definitive execution of the block, with the most common ultrasound approach being the lateral TAP block. A high-frequency (5–13 MHz) linear array probe and a 50 or 80 mm needle is adequate for most patients. With the patient supine, the probe is placed transversely in the mid-axillary line between the 12th rib and iliac crest with in-plane needling from anterior to posterior.6 Usual local anaesthetic volumes are between 20 and 30 ml with spread seen between the IOM and TAM. As the block is usually performed bilaterally, caution must be exercised to not exceed the maximum dose. Nerves above T10 are not consistently blocked with this approach because of their more medial entry into the TAP and injectate rarely spreading beyond the anterior axillary line.2, 7 The posterior TAP block may also be performed with ultrasound (Fig. 2a).
Fig 2.
Ultrasound images of (a) posterior transversus abdominis plane (TAP) block and (b) subcostal TAP block. Arrow indicates needle trajectory; asterisk (*) indicates needle tip position for local anaesthetic deposition. EOM, external oblique muscle; IOM, internal oblique muscle; RAM, rectus abdominis muscle; TAM, transversus abdominis muscle.
The subcostal TAP block aims to cover the lower thoracic nerves but also T6 to T9, which enter medial to the anterior axillary line.2 The ultrasound probe is obliquely placed, parallel to the costal margin, close to the midline. It is then moved obliquely and laterally along the subcostal margin until the TAM is identified posterior to the RAM. A 100 or 150 mm needle is passed medial to lateral in-plane to deposit local anaesthetic in the TAP (Fig. 2b).8 A more common approach has the needle entry point at the anterior axillary line and passing superomedially towards the xiphoid process, termed the oblique subcostal TAP block.2, 9 Both the lateral and subcostal TAP blocks allow catheter placement for continuous analgesia, and combining them as a ‘dual TAP’ block may provide superior analgesia for the whole abdominal wall when performed bilaterally. However, prolonged analgesia with this technique would, in essence, require four catheters, as opposed to one if epidural analgesia was used.
Indications for TAP block include colonic, urological, gynaecological, and obstetric surgery, with a recent systematic review demonstrating marginally reduced opioid consumption at 6 h after laparotomy, laparoscopy, and Caesarean section (CS).10 The ultrasound-guided lateral approach has been the most widely studied technique in CS, where analgesic benefit has been demonstrated after general anaesthesia, but not in addition to regional anaesthesia including intrathecal opioid.10 Although the ultrasound-guided lateral TAP block has become a popular approach, another recent meta-analysis demonstrated that the anatomically-guided posterior TAP block produces a longer duration of analgesia (up to 48 h) than the lateral TAP block after lower abdominal transverse incision surgery.11 One suggested explanation for this is that injectate spreads to the thoracic paravertebral space with the anatomically guided posterior TAP but not with the lateral ultrasound approach.2 However, the studies in this meta-analysis did not directly compare the two techniques, and further work is necessary to establish if a difference exists.11
Quadratus lumborum (QL)
The various QL blocks (QLBs) can be viewed as ultrasound-guided variations of the initial landmark posterior TAP block through the triangle of Petit. The ventral rami of the spinal nerves pass over the anterior aspect of QL, with the potential for T7–L1 to be covered by this block.12 The main mechanism of action for this block, however, is thought to be thoracic paravertebral spread. The transversalis fascia, which lines the TAM and QL, is continuous with the endothoracic fascia in the thoracic cage, and therefore local anaesthetic can spread posterior to the transversalis fascia into the thoracic paravertebral space. This spread, however, has not been demonstrated in all cadaver studies. Nonetheless, of all the ultrasound-guided abdominal wall blocks, the QLBs may have the greatest potential to provide both somatic and visceral analgesia.2
Generally, QLBs are performed with the patient in the supine or lateral position, using a low-frequency (2–5 MHz) curvilinear probe (although a high-frequency linear probe has been used12) and an 80–100 mm block needle with 20–30 ml of local anaesthetic. The first described QLB—later called the lateral (or QL1) QLB—is believed by some to be a TFP block (see below). The needle is passed in an anterior (lateral) to posterior (medial) direction to the junction of the IOM and TAM aponeurosis and the transversalis fascia. Local anaesthetic is deposited at this position at the tapered end of the TAM, at the anterolateral aspect of the QL, with spread seen along its anterior edge. The second QL block—later called the posterior (or QL2) QLB—has a similar needle path, but a shallower angle, with the point of injection towards the posterior part of the QL. Local anaesthetic is deposited between the QL and latissimus dorsi and spread is seen along its posterior aspect (Fig. 1 online video). This block has been proved to work in one RCT, but the explanation for its effectiveness remains unclear.13 The transmuscular quadratus lumborum (TQL) block (QL3 block or anterior QLB), depends upon depositing local anaesthetic posterior to the transversalis fascia (Fig. 2 online video). The needle is passed in a posterior to anterior direction passing through QL, and local anaesthetic should be seen pooling in the plane between it and psoas major.
The QLB, being a more recent development than the TAP, is less clearly understood in terms of spread and the potential differences in efficacy (if any) between the approaches.2 Emerging evidence has demonstrated the use of lateral or posterior QLBs in providing analgesia after CS, midline laparotomy, and laparoscopic procedures. Additionally, the utility of the lateral QLB in hip surgery has also been highlighted, with the caudal extension of the transversalis fascia over psoas major and iliacus being the mechanism of injectate spread to the lumbar plexus, explaining its potential efficacy in this scenario. To date, less evidence exists regarding the efficacy of TQL blocks in abdominal surgery. However, a recent cadaveric study demonstrated thoracic paravertebral spread with the TQL block.14 The efficacy of the block in randomised clinical trials is soon to be published (Clinicaltrials.gov registration numbers NCT03068260 and NCT02818140).
Transversalis fascia plane (TFP)
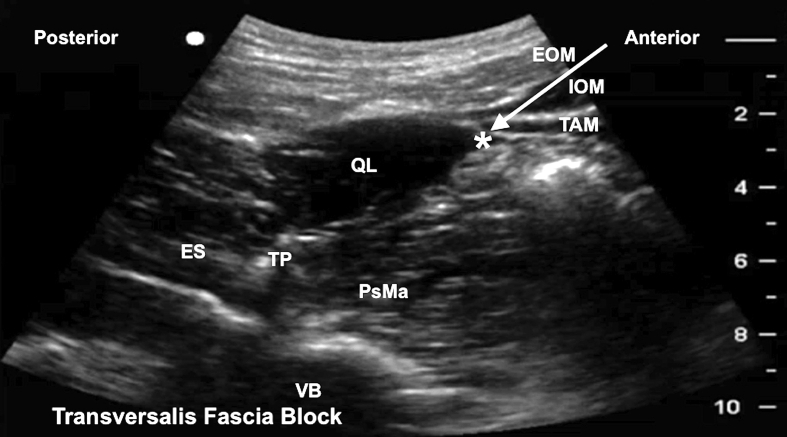
The TFP block was developed as a means of reliably blocking the lateral cutaneous branches of T12 and L1, commonly missed by the TAP block,6 because these branches leave the TAP more proximally.15 The TFP block is argued to be different to the QL1 as the injection point is beneath the tip of TAM and not the TAM/IOM aponeurosis.2
The block is performed using a low-frequency curvilinear or high-frequency linear probe and 80 mm needle, with the patient lateral, with the side to be blocked uppermost, or in the supine position (Fig. 3).16
Fig 3.
Ultrasound image for transversalis fascia plane (TFP) block. Arrow indicates needle trajectory; * indicates needle tip position for local anaesthetic deposition. The probe is placed transversely in the mid-axillary line just above the iliac crest. The IOM and TAM are traced posteriorly until they taper off as the TLF anterior to the QL. The needle is advanced in-plane in an anterior to posterior direction, and injection of 20 ml local anaesthetic underneath the TAM at this point produces a spread in the transversalis fascia plane. EOM, external oblique muscle; ES, erector spinae; IOM, internal oblique muscle; PsMa, psoas major; QL, quadratus lumborum; TAM, transversus abdominis muscle; TP, transverse process; VB, vertebral body.
Case reports, observational studies, and a sole randomised trial have cited indications for the TFP block to include open appendicectomy, inguinal hernia repair, and anterior iliac bone graft harvesting.16
Risks of abdominal wall blocks
A study of needle tip placement for landmark-guided TAP blocks determined that under a quarter of performed blocks were in the correct plane when assessed with ultrasound and, in fact, a high proportion had inadvertently breached the peritoneal cavity.17 Ultrasound should therefore in theory reduce the risk of visceral and neurovascular injury, as long as the needle is seen throughout the block; there may be an argument for abandoning blind techniques altogether.17 Performance of abdominal wall blocks under general or neuraxial anaesthesia is widely accepted, and there have so far been no reports of neurological injury. This is likely to be because fascial planes are the site of target instead of specific nerve bundles.2
Local anaesthetic systemic toxicity is a concern as these are high-volume blocks and generally bilateral. Maximum doses of local anaesthetic should not be exceeded, also taking into consideration physiological or pathological changes that may affect sensitivity or metabolism, such as pregnancy or renal impairment. Systemic absorption of local anaesthetics from abdominal wall blocks is high because of well-vascularised large surface area fascial planes and ideally less cardiotoxic agents should be used.2 It is possible that systemic absorption contributes to some of the effects of large volume abdominal wall blocks, especially as i.v. lidocaine has been shown to be of clear benefit in reducing pain and opioid consumption after abdominal surgery.18
A specific risk with the QL and TFP blocks is the spread of local anaesthetic to the lumbar plexus, or spread to the femoral nerve with TAP blocks, because injectate may pass close to psoas major and track under the iliopsoas fascia.19 As a result, patients should always be informed of the risk of quadriceps weakness when consent is being obtained.2 In addition, QLB may risk renal injury as the kidney lies anterior to the QL, separated only by perinephric fat and fascia. Any difficulties delineating the anatomy around the QL may also increase the risk of inadvertent visceral injury.
Current controversies and future trends
The ESP block is a novel and theoretically low-risk technique first performed at the T5 transverse process level.20 The aim is to deposit a high volume of local anaesthetic deep to the erector spinae muscle (ESM) at the tip of the transverse process, close to the costotransverse foramina and the dorsal and ventral rami as they emerge from the intervertebral foramen,20 potentially providing somatic analgesia to the entire thoracic and abdominal walls.21
The block is performed with the patient in the sitting, lateral, or prone position using either a high-frequency linear probe, or a low-frequency curvilinear probe in larger patients. The block is performed at the level of T7 for abdominal wall analgesia. Placing the probe longitudinally to see the transverse processes reveals the trapezius and ESM. Above T5–6, the rhomboid major muscle is also visible between the trapezius and ESM; hence its absence confirms the T7 level.21 An 80 mm needle is usually adequate, inserting at a 30–45° angle in-plane cranial to caudal approach aiming to make contact with the T7 transverse process. Hydrolocation with normal saline is advocated to ensure correct needle placement before injection of 20–30 ml local anaesthetic underneath the ESM such that the muscle is seen ‘lifting’ off the transverse process (Fig. 3 online video). Catheter techniques have been used to prolong analgesia. Cadaver studies demonstrate injection at T7 can spread to as low as L2 to L3, although this is a variable outcome and may not necessarily translate to the clinical effect.
The ESP block may have analgesic potential for abdominal procedures, including nephrectomy, hysterectomy, and laparotomies and has also been used as analgesia for rib fractures and chronic pain. Current evidence in abdominal surgery, however, remains limited to case reports supporting its use for laparoscopic ventral hernia repair.21 Further evidence on the efficacy and clinical utility of this technique is awaited.
Declaration of interest
A. Pawa consults for B Braun Medical Ltd and has received honoraria from GE Healthcare for teaching.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Desire Onwochei BSc (Hons) FRCA MSc is a consultant anaesthetist at Guy's & St Thomas' NHS Foundation Trust who completed fellowships and research in regional anaesthesia, obstetrics and airway management. She has a keen interest in the application of regional anaesthesia in obstetrics.
Jens Børglum MD PhD is an associate professor and consultant anaesthetist at Copenhagen University Hospital. He has been working in the area of ultrasound in anaesthesia since 2005 and has published a large number of papers on regional anaesthesia. He has extensive experience as teacher of ultrasound-guided regional anaesthesia and as an invited speaker worldwide.
Amit Pawa BSc (Hons) FRCA EDRA is a consultant anaesthetist and lead for regional anaesthesia at Guy's & St Thomas' NHS Foundation Trust who is also the current president of Regional Anaesthesia UK. In addition to helping create a series of video tutorials on ultrasound-guided regional anaesthesia, he has authored numerous articles on different aspects of regional anaesthesia.
Matrix codes: 1D02, 2G01, 3A09
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.bjae.2018.07.002.
Appendix A. Supplementary data
The following are the supplementary data related to this article:
Ultrasound image of the quadratus lumborum (QL) muscle for a posterior QL (QL2) block. Arrow indicates needle trajectory; * indicates needle tip position for local anaesthetic deposition. If reading the pdf online, click on the image to view the video. EOM, external oblique muscle; ES, erector spinae; IOM, internal oblique muscle; PsMa, psoas major; QL, quadratus lumborum; TAM, transversus abdominis muscle; TP, transverse process; VB, vertebral body.
Ultrasound image of the transmuscular QL block (QLB). If reading the pdf online, click on the image to view the video. ES, erector spinae muscle; L4, vertebral body of L4; PMM, psoas major; QL, quadratus lumborum; TP, transverse process.
Ultrasound image for the erector spinae plane (ESP) block. Note the presence of the rhomboid major muscle indicating the level to be above T5–6. Arrow indicates needle trajectory, asterisk (*) indicates needle tip position for local anaesthetic deposition. If reading the pdf online, click on the image to view the video. Video reproduced with permission from Dr Ki Jinn. TP, transverse process.
References
- 1.Rucklidge M., Beattie E. Rectus sheath catheter analgesia for patients undergoing laparotomy. BJA Educ. 2018;18:166–172. doi: 10.1016/j.bjae.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chin K.J., McDonnell J.G., Carvalho B., Sharkey A., Pawa A., Gadsden J. Essentials of our current understanding: abdominal wall blocks. Reg Anesth Pain Med. 2017;42:133–183. doi: 10.1097/AAP.0000000000000545. [DOI] [PubMed] [Google Scholar]
- 3.Rozen W.M., Tran T.M.N., Ashton M.W., Barrington M.J., Ivanusic J.J., Taylor G.I. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21:325–333. doi: 10.1002/ca.20621. [DOI] [PubMed] [Google Scholar]
- 4.Kansal A., Hughes J. Visceral pain. Anaesth Intensive Care Med. 2016;17:543–547. [Google Scholar]
- 5.McDonnell J.G., O’Donnell B.D., Farrell T. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32:399–404. doi: 10.1016/j.rapm.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Hebbard P., Fujiwara Y., Shibata Y.R.C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–617. [PubMed] [Google Scholar]
- 7.Carney J., Finnerty O., Rauf J., Bergin D., Laffey J.G., Mc Donnell J.G. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66:1023–1030. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 8.Hebbard P.D., Barrington M.J., Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical technique. Reg Anesth Pain Med. 2010;35:436–441. doi: 10.1097/aap.0b013e3181e66702. [DOI] [PubMed] [Google Scholar]
- 9.Sondekoppam R.V., Brookes J., Morris L., Johnson M., Ganapathy S. Injectate spread following ultrasound-guided lateral to medial approach for dual transversus abdominis plane blocks. Acta Anaesthesiol Scand. 2015;59:369–376. doi: 10.1111/aas.12459. [DOI] [PubMed] [Google Scholar]
- 10.Baeriswyl M., Kirkham K.R., Kern C., Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121:1640–1654. doi: 10.1213/ANE.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 11.Abdallah F.W., Laffey J.G., Halpern S.H., Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111:721–735. doi: 10.1093/bja/aet214. [DOI] [PubMed] [Google Scholar]
- 12.Murouchi T., Iwasaki S., Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. 2016;41:146–150. doi: 10.1097/AAP.0000000000000349. [DOI] [PubMed] [Google Scholar]
- 13.Blanco R., Ansari T., Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlled trial. Eur J Anaesthesiol. 2015;32:812–818. doi: 10.1097/EJA.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 14.Dam M., Moriggl B., Hansen C.K., Hoermann R., Bendtsen T.F., Børglum J. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. 2017;125:303–312. doi: 10.1213/ANE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 15.Hebbard P.D. Transversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve block. Can J Anesth. 2009;56:618–620. doi: 10.1007/s12630-009-9110-1. [DOI] [PubMed] [Google Scholar]
- 16.Chin K.J., Chan V., Hebbard P., Tan J.S., Harris M., Factor D. Ultrasound-guided transversalis fascia plane block provides analgesia for anterior iliac crest bone graft harvesting. Can J Anesth. 2012;59:122–123. doi: 10.1007/s12630-011-9610-7. [DOI] [PubMed] [Google Scholar]
- 17.McDermott G., Korba E., Mata U. Should we stop doing blind transversus abdominis plane blocks? Br J Anaesth. 2012;108:499–502. doi: 10.1093/bja/aer422. [DOI] [PubMed] [Google Scholar]
- 18.Eipe N., Gupta S., Penning J. Intravenous lidocaine for acute pain: an evidence-based clinical update. BJA Educ. 2016;16:292–298. [Google Scholar]
- 19.Rosario D.J., Jacob S., Luntley J., Skinner P.P., Raftery A.T. Mechanism of femoral nerve palsy complicating percutaneous ilioinguinal field block. Br J Anaesth. 1997;78:314–316. doi: 10.1093/bja/78.3.314. [DOI] [PubMed] [Google Scholar]
- 20.Forero M., Adhikary S.D., Lopez H., Tsui C., Chin K.J. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–627. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 21.Chin K.J., Adhikary S., Sarwani N., Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–460. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Ultrasound image of the quadratus lumborum (QL) muscle for a posterior QL (QL2) block. Arrow indicates needle trajectory; * indicates needle tip position for local anaesthetic deposition. If reading the pdf online, click on the image to view the video. EOM, external oblique muscle; ES, erector spinae; IOM, internal oblique muscle; PsMa, psoas major; QL, quadratus lumborum; TAM, transversus abdominis muscle; TP, transverse process; VB, vertebral body.
Ultrasound image of the transmuscular QL block (QLB). If reading the pdf online, click on the image to view the video. ES, erector spinae muscle; L4, vertebral body of L4; PMM, psoas major; QL, quadratus lumborum; TP, transverse process.
Ultrasound image for the erector spinae plane (ESP) block. Note the presence of the rhomboid major muscle indicating the level to be above T5–6. Arrow indicates needle trajectory, asterisk (*) indicates needle tip position for local anaesthetic deposition. If reading the pdf online, click on the image to view the video. Video reproduced with permission from Dr Ki Jinn. TP, transverse process.