Key points.
-
•
Epidermolysis bullosa is a group of rare genetic conditions characterized by extreme skin fragility. Even trivial shearing forces to the skin lead to blister formation and skin injury
-
•
The main challenges for anaesthetists are the prevention of new skin blister formation, management of previously scarred tissues (especially the airway), and perioperative pain management
-
•
Where concerns exist there should be an explicit strategy for airway management, agreed jointly with a senior Ear Nose and Throat (ENT) clinician
-
•
Active input from a dermatologist is very useful
-
•
Adhesive dressings and tapes in contact with the skin should be avoided at all costs and all airway equipment including facemasks should be well lubricated.
Epidermolysis bullosa (EB) is a group of rare genetic conditions characterized by severe skin fragility. Patients are extremely prone to developing bullae caused by separation of the skin and mucosa from underlying tissues with even gentle contact. The challenge to anaesthetists is preventing new skin or membrane injury whilst managing previously scarred or deformed tissues and pain. Patients with EB tend to present for diagnostic or therapeutic procedures in specialist centres, but may present for an unrelated surgical condition in a local hospital, hence the anaesthetic management of the condition should be well known to all. Whilst acquired forms of bullous skin disease have been described, this article is confined to inherited EB.
Background
EB was first described in 1870 by Ferdinand Ritter Von Hebra, an Austrian physician and dermatologist, who, incidentally also discovered the causative organism in scabies.1 These early descriptions were soon subclassified into discrete sub-types of EB and since then geneticists have discovered at least 18 different genes resulting in more than 30 clinical subtypes of EB.2 Genes encoding for keratin, collagen, and laminin proteins are the most commonly implicated.3 All of these proteins play important roles as anchors providing structural stability at various layers of the skin. A loss in function of any of these proteins leads to inherent weakness, fragility, and dehiscence at the dermal layer at which they are prevalent. In addition, the skin becomes a less effective functional barrier to infection and there is impaired healing.2 A study from the USA spanning 1986–2002 estimated the overall incidence of inherited EB at 19 cases per 1 million live births.4
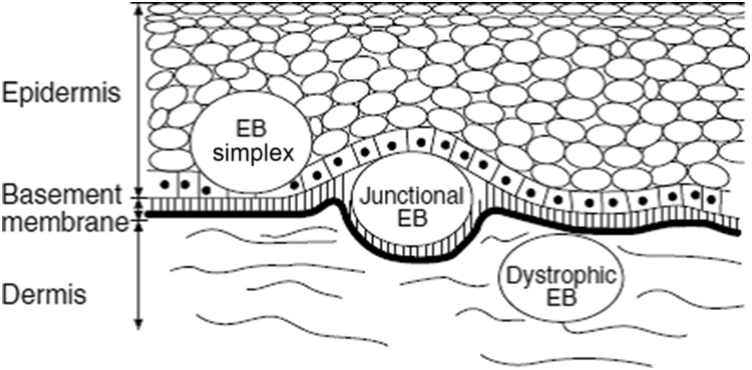
Given the myriad of different genetic types of EB, three major histological groups have been described: dystrophic EB (DEB), EB simplex (EBS), and junctional EB (JEB).5 These groups are based on the precise ultrastructural level of the dermis at which the weakness and hence dehiscence occurs.
EBS
This is the most common sub-type of EB, accounting for up to 70% of cases.6 Fragility is limited to the epidermis and the ‘cleavage plane’ is either within or above the basal keratinocytes (Fig. 1). It is usually inherited in an autosomal dominant manner; in most patients the clinical picture is mild with a good prognosis.
Fig 1.
Dermal layers implicated in the major forms of EB. Reproduced, with permission, from Herod et al.7
Blistering occurs most frequently in the hands and feet (those areas experiencing the greatest frictional forces on a repetitive basis) and whilst severe generalized forms also exist, oral involvement is rarely seen.
JEB
Here, the structural defect occurs at the dermo-epidermo junction (Fig. 1). It accounts for 10% of cases and unlike EBS is usually inherited in a recessive manner, leading to carrier states. As such, there is a spectrum of severity, but patients with JEB will often have significant skin and mucosal involvement including pharyngeal and upper oesophageal blistering and scarring (the distal oesophagus being ciliated columnar epithelium is not affected as opposed to the squamous epithelium of the proximal one third). The most common subgroup of JEB is the Herlitz type and is characterized by laryngeal involvement causing a hoarse cry and stridor.7 Partial and complete upper airway obstruction and asphyxiation has been described in JEB and indeed up to 50% of patients with generalized, severe JEB may show symptoms or signs of laryngotracheal stenosis secondary to granulation, not necessarily blistering.8 In its most severe form, patients die in infancy from malnutrition (due to pain and difficult feeding), anaemia, and infection due to chronic ulceration.
DEB
In this subtype, the fragility is deep to the basement membrane in the upper dermis (see Fig. 1). Inheritance is again variable. Mutations in genes encoding collagen VII are commonly encountered. Unlike other forms of EB it is characterized by a tendency for the bullae to heal forming significant amounts of scar tissue. This often leads to fusion of digits and significant amounts of cutaneous scar tissue, but in addition, since collagen VII is found in many non-cutaneous membranes, oesophageal, joint, and peri-orbital contractures are seen. As a result, DEB is the most common subtype presenting for surgical treatment.7 As with JEB, the spectrum of disease is wide, but often these patients will survive into adulthood where squamous cell carcinomas before the age of 35 years are common and are a major cause of death in adulthood.9 Oral and upper oesophageal blistering is commonly seen and leads to progressive contractures of the mouth, ankyloglossia, dysphagia, poor oral intake, and gastro-oesophageal reflux. This all contributes to painful and limited nutritional intake and subsequent malnutrition and anaemia.
A fourth, rarer group called Kindler Syndrome was also described whereby there can be multiple levels of blistering. Other rare and severe forms exist that are not necessarily confined to one histologically described group.
There is considerable variation in the prognosis for EB. Patients with severe forms of EBS and JEB subtypes tend to die in early childhood, whilst those with DEB can live into early adulthood, but this is variable and dependent upon the precise genetic mutation.9, 10 In all but the most mild forms of the condition, life expectancy is reduced. Since sufferers often present for surgical interventions in childhood, the wealth of experience in the management of these complex cases is held by paediatric anaesthetists.
Anaesthetic management
General considerations
Due to the rare and complex nature of EB, patients requiring elective surgery should be managed in a specialist paediatric centre with the necessary experience and personnel present. Common surgical procedures being carried out in this population involve contracture releases, separation of syndactyly, oesophageal or urethral dilatations, dental or ophthalmic surgery.7, 11, 12 Gastrostomy formation is another commonly performed operation in this population and an open as opposed to an endoscopic technique is utilized due to the risk of bullae formation from the endoscope. Patients may, however, attend with a surgical problem unrelated to EB and not necessarily to a specialist centre, and thus regardless of the surgery being undertaken, meticulous planning and involvement of multidisciplinary clinicians in paramount.
Anaesthesia
Preoperative
It should be remembered that surgery for EB is often carried out in young children and all the usual paediatric anatomical, physiological, and pharmacological considerations apply. A thorough preoperative assessment enquiring about all co-morbidities should be completed and previous anaesthetic records obtained. The clinical subtype of EB, the severity and extracutaneous extent of the disease must be sought, and admissions should ideally involve joint care including dermatologists.
There should be careful preoperative assessment of oral contractures causing microstomia or ankyloglossia and any airway involvement, e.g. poor dentition or existing mucosal bullae, to predict a potential difficult airway. Patients with oesophageal strictures and scarring will have a degree of gastro-oesophageal reflux, and antacid prophylaxis is advised either orally or i.v. Discussions with child and carers are useful to yield the best place for venous cannulation placement, and often they will expose the skin area removing the bandages prior to attendance in the anaesthetic room. Topical local anaesthetic is possible as long as no adhesive dressing is used (suggest cling film).7, 11 The use of sedative premedication has previously been reported as beneficial with reduced patient movement, improved compliance, and overall reduced skin trauma, especially amongst younger children undergoing inhalational induction.11, 12, 13, 14
Preoperative blood tests may be necessary as the majority of severe EB patients are malnourished and anaemic.11 The decision as to whether to transfuse preoperatively will depend upon the haemoglobin level, local protocols, and the intended surgery.11 Signs and symptoms of intercurrent infection should be sought, as recurrent infections due to impaired skin barrier function are commonplace. In addition, some patients may be taking long-term oral corticosteroids, and perioperative supplementation should be considered.
Intraoperative
When anaesthetizing children with EB, great care should be undertaken to prevent formation of new bullae, caused by friction and shearing forces. Preparation for potentially difficult airway management and/or intubation in many subgroups secondary to contractures and granulation tissue is also important.7, 12
To reduce the incidence of new skin trauma and bullae formation, minimal patient handling and transferring should be undertaken. Induction of a younger child should take place on a crease free sheet to ensure easy lifting once asleep. Older children and adults can be anaesthetized in theatre on the operating table. The use of an ‘egg crate’ mattress or similar on the operating table is useful and helps to reduce skin injury. Clearly manual handling aids such as the Patslide patient transfer should be avoided as these can create shearing forces.
Monitoring
Monitoring is an essential part of safe anaesthetic delivery but can also cause great harm to a patient with EB if not applied in the correct manner: thus, a pragmatic approach is often employed. The avoidance of any adhesive part in contact with the skin is paramount. Clip-on pulse oximeters are preferable, however if self-adhesive probes are necessary then the digit to be used should be amply lubricated with petroleum or paraffin-based lubricants, such as Vaseline, covered with a clear polyvinylchloride (PVC) film or finger part of a glove before attaching the probe. Placement of these pegs can be limited by lesions where syndactyly is present and use of ear clips may be necessary.7, 12, 14 Similarly, an ECG electrode should have either paraffin gauze/gel pads or a silicone mesh placed between it and the skin; alternatively the electrode can be attached to a staple placed in the skin once the child is anaesthetized.7, 12 Non-invasive blood pressure monitoring can be used as long as there is application of PVC film and padding underneath the cuff, the same applies to tourniquet use during surgery. Occasionally it may be recommended by a patient's dermatology team that non-invasive blood pressure monitoring should not be used because of disease severity. In these instances a manual blood pressure measurement can be obtained as necessary, or alternatively, invasive arterial pressure monitoring can be used for longer procedures. Invasive temperature monitoring devices should be avoided.
Induction should be as calm and as smooth as possible; sedative premedication should be considered for some, as children with EB are often anxious from repeated dressing changes and/or surgical procedures. Psychologically, these children are often frequent theatre attendees and have formed their own opinions as to how they prefer anaesthesia to be induced. If a cannula is in situ then i.v. induction is preferable. Cannulation can be performed by gentle direct pressure to distend the veins with utmost care to avoid shearing forces, but this can be difficult with overlying ulceration/scarring or bandages. Cannulae or invasive lines can be secured using non-adhesive dressing, or if required for longer-term use, then sutured or stapled in place. If i.v. access is deemed difficult, then an inhalational induction with sevoflurane is an acceptable alternative. In this situation, the facemask cushion should be liberally covered with paraffin gauze or lubricated with Vaseline or similar petroleum jelly to reduce friction and torsional forces, as well as the contact area with the skin (especially the mandible where anaesthetist fingers will lie) and the anaesthetist's gloves and fingers should also be well lubricated.11 All airway adjuncts, intubation aids, and blades should be well lubricated. Eye protection should avoid adhesive taping and consist of the application of a gel pad.
By far the most complex and hazardous part of anaesthetizing EB patients is airway management. This is for a number of reasons: (i) mouth, pharyngeal, and laryngeal EB involvement, which may hinder visualization of the larynx, endotracheal tube, or supraglottic airway device placement; (ii) contractures of the mouth or neck can affect positioning; and (iii) significant swelling and blister formation can be caused by trivial mucosal and skin contact during anaesthesia.
Where upper airway distortion or symptoms and signs of airway obstruction (e.g. stridor) are present, preoperative ENT input should be sought and a joint strategy for airway management agreed. The difficulty in airway management is a consideration of whether to instrument the airway or not. Facemask, orotracheal intubation, nasotracheal intubation, tracheostomy, and supraglottic airway device techniques have all been described in patients with EB.11, 13 Facemask anaesthesia avoids airway manipulation, but the potential for laryngeal bullae formation must be balanced against complications from prolonged facial manipulation. Maintenance of a hand-held airway is not usually a problem as the tongue is usually tethered so does not tend to fall back and obstruct the airway.14 It must be remembered, however, that patients with EB often have an increased risk of gastro-oesophageal reflux: this and a prolonged anticipated length of surgery may preclude facemask anaesthesia. Furthermore, the liberal use of lubrication for the facemask represents the challenge of holding a slippery mask in position for an extended period of time. If tracheal intubation is deemed necessary, then a tracheal tube half a size smaller is advocated, preferably uncuffed, but if cuffed is used, then the cuff should be inflated gently.7, 12, 14 Intubation represents the gold standard with regard to protection from gastro-oesophageal reflux and the facility to ventilate the patient's lungs for a prolonged period in longer duration surgeries. Tracheal intubation may be achieved by direct laryngoscopy, indirect video-laryngoscopy, and via oral or nasal fibreoptic techniques. Fibreoptic intubation has an important role where difficult intubation via direct laryngoscopy is known or suspected. Nasal fibreoptic intubation is often performed for dental surgery. Where fibreoptic intubation is used, it is better performed after induction of anaesthesia (as opposed to awake) because paediatric patients often have difficulty co-operating with the procedure and there is the potential for tissue injury if the patient moves on the trolley. During intubation, the lips should be protected with paraffin gauze and all blades and tubes must be lubricated fully, with careful attention to how the tube is secured. It must be stressed that adhesive taping should be avoided at all costs and a common strategy includes using lubricated ribbon/paraffin gauze with an underlay of further lubricated gauze to prevent shearing. The lubricated gauze can be secured adhesively to the actual endotracheal tube to prevent inadvertent migration of this.7 Laryngeal mask airways have been used successfully with minimal sequelae as long as they are well lubricated and applied gently.14 Pharyngeal suctioning should be done gently and only under direct vision, taking care to avoid direct trauma to the oral mucosa.
Surgery under both local and general anaesthesia has been described although it is rare to encounter regional-only techniques.14 Neuromuscular blockade (both depolarizing and non-depolarizing) is not contra-indicated despite previous concerns, and should be managed as per any other paediatric patient.7, 11, 12, 13 Central neuraxial and peripheral regional techniques were once feared for causing introduced infections and new bullae, but have been used successfully without reported complications.7, 12, 15, 16 Antiseptic/chlorhexidine spray should be used to ensure sterility, as rubbing the skin is prohibited.7, 14, 15, 16 However, the use of local anaesthetic skin infiltration is to be avoided.7, 14 Regional anaesthesia provides excellent postoperative pain relief and if frequent dressing changes are envisaged then placement of a catheter (epidural or block) may be particularly helpful.7
Postoperative management
Smooth emergence is as important as smooth induction of anaesthesia. All airway adjuncts should be removed before emergence and all hard plastic oxygen face masks should be avoided. Oxygen during recovery should be delivered with the cushioned and lubricated anaesthetic mask or towards the patient without direct skin contact, guided by SpO2 values. Methods to avoid overstimulation include maintaining a darkened and quiet recovery area and allowing the child to waken up naturally without stimulation.
Analgesia
Analgesia is especially key to smooth emergence from anaesthesia. Any distress is likely to manifest as excessive movement or tugging at bandages and cause new blister formation. EB is an inherently painful condition with elements of both acute and chronic pain and is difficult to treat effectively. Multimodal analgesia is the mainstay of treatment with care to the use of non-steroidal anti-inflammatory drugs where gastro-oesophageal reflux is present. Often the route of delivery is limited to i.v. or oral (rectal suppositories are to be avoided as they may lead to perianal trauma).7, 14, 16 If the oral route is unlikely to be available then IV administration is likely to be preferable, even in those surgeries that do not warrant this usually, e.g. dental procedures. There is no evidence to contradict the use of strong opioids and nurse- or patient-controlled analgesia are often used. However, this may exacerbate the chronic itching that is associated with the healing blisters in some forms and which is notoriously difficult to treat.7, 12 Intraoperative regional anaesthetic blocks should be considered, as outlined above.
It is crucial that there is excellent communication perioperatively between the anaesthetic and surgical teams to ensure that all staff are aware of the complex issues involved, especially the extreme care required to move, position, and care for the child with EB. In some centres, there is an EB liaison nurse who may bring a wealth of invaluable information, practical help and advice. In many specialist centres there is a designated EB trolley (Fig. 2) in theatre, stocked with all required materials (Fig. 3) and an attached aide-memoire to facilitate safe anaesthetic practise (Table 1).
Fig 2.
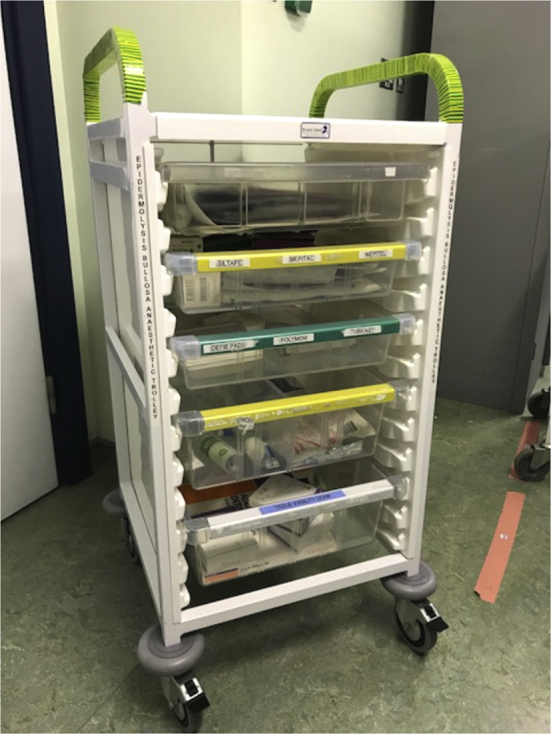
A designated EB trolley containing equipment necessary for management.
Fig 3.
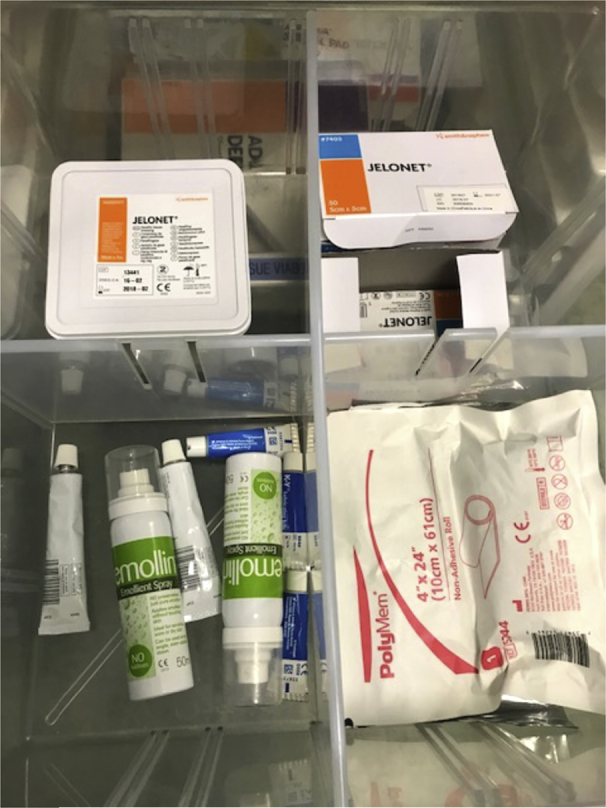
Equipment and dressings required.
Table 1.
Aide-memoire of equipment to use and avoid in patients with EB
| Recommended | Avoid |
|---|---|
| Clip on oxygen saturation probe | All self-adhesive products, e.g. medical tape |
| Clear PVC film, e.g. Clingfilm | Directly applying ECG electrodes/peripheral temperature electrode |
| Lubrication e.g. paraffin or petroleum based jelly (Vaseline) | Friction causing devices, e.g. manual handling aids |
| Eye gel pads | Hard rigid plastics, e.g. oxygen face masks, nasogastric tubes |
| Silicone based dressings (low adherent) | |
| Gel/soft foam padding for pressure areas | |
| Non-invasive blood pressure cuff/tourniquet (with soft padding underneath) | |
| Bipolar/dry pad diathermy |
Summary
Patients with EB are usually cared for in specialist centres, but may present to other hospitals for emergency surgery. They provide a unique and complex challenge for anaesthetists both anaesthetically and for pain management. All anaesthetists should be aware of the basic principles to provide safe and effective care for EB patients wherever they present. With meticulous preoperative planning and extreme attention to detail to protect mucous membrane and skin, and to prevent shearing or frictional forces, anaesthesia can be delivered with few sequelae.
Declaration of interest
None declared.
MCQs
The associated MCQs (to support CME/CPD activity) can be accessed at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Lowri Bowen MRCSEng FRCA is a consultant paediatric anaesthetist at the Children's Hospital for Wales, Cardiff.
Mark Burtonwood FRCA MAcadMEd is a specialty registrar at University Hospital of Wales, Cardiff.
Matrix codes: 1A01, 2D02, 3A01
References
- 1.Pai-Dhungat J.V. Ferdinand Von Hebra–founder of classical dermatology. J Assoc Phys India. 2014;62:80–81. [PubMed] [Google Scholar]
- 2.Uitto J., Richard G. Progress in epidermolysis bullosa: genetic classification and clinical implications. Am J Med Genet C Semin Med Genet. 2004;131:61–74. doi: 10.1002/ajmg.c.30035. [DOI] [PubMed] [Google Scholar]
- 3.Aumailley M., Has C., Tunggal L., Bruckner-Tuderman L. Molecular basis of inherited skin-blistering disorders and therapeutic implications. Expert Rev Mol Med. 2006;24:1–21. doi: 10.1017/S1462399406000123. [DOI] [PubMed] [Google Scholar]
- 4.Fine J.D. Epidemiology of inherited epidermolysis bullosa based on incidence and prevalence estimates from the national epidermolysis bullosa registry. JAMA Dermatol. 2016;152:1231. doi: 10.1001/jamadermatol.2016.2473. [DOI] [PubMed] [Google Scholar]
- 5.Fine J.D., Eady R.A.J., Bauer J.A. The classification of inherited epidermolysis bullosa: report of the third international consensus meeting on diagnosis and classification of EB. J Am Acad Dermatol. 2008;58:931–950. doi: 10.1016/j.jaad.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Dystrophic Epidermolysis Bullosa Research Association. About EB, Berkshire, 2017. Available from: http://www.debra.org.uk. [Accessed 20 June 2017].
- 7.Herod J., Denyer J., Goldman A. Epidermolysis bullosa in children: pathophysiology, anaesthesia and pain management. Paediatr Anaesth. 2002;12:388–397. doi: 10.1046/j.1460-9592.2002.00768.x. [DOI] [PubMed] [Google Scholar]
- 8.Fine J.D., Mellerio J.E. Extracutaneous manifestations and complications of inherited epidermolysis bullosa: part I. Epithelial associated tissues. J Am Acad Dermatol. 2009;61:367–384. doi: 10.1016/j.jaad.2009.03.052. [DOI] [PubMed] [Google Scholar]
- 9.Fine J.D. Inherited epidermolysis bullosa. Orphanet J Rare Dis. 2010;5:12. doi: 10.1186/1750-1172-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hon K.L.E., Li J.J., Cheng B.L. Age and etiology of childhood epidermolysis bullosa mortality. J Dermatolog Treat. 2014;26:178–182. doi: 10.3109/09546634.2014.915002. [DOI] [PubMed] [Google Scholar]
- 11.Iohom G., Lyons B. Anaesthesia for children with epidermolysis bullosa: a review of 20 years' experience. Eur J Anaesth. 2001;18:745–754. doi: 10.1046/j.1365-2346.2001.00916.x. [DOI] [PubMed] [Google Scholar]
- 12.Nandi R., Howard R. Anaesthesia and epidermolysis bullosa. Dermatol Clin. 2010;28:319–324. doi: 10.1016/j.det.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Griffin R.P., Mayou B.J. The anaesthetic management of patients with dystrophic epidermolysis bullosa. Anaesthesia. 1993;48:810–815. doi: 10.1111/j.1365-2044.1993.tb07599.x. [DOI] [PubMed] [Google Scholar]
- 14.Ames W.A., Mayou B.J., Williams K. Anaesthetic management of epidermolysis bullosa. Br J Anaesth. 1999;82:746–751. doi: 10.1093/bja/82.5.746. [DOI] [PubMed] [Google Scholar]
- 15.Boughton R., Crawford M.R., Vonwiller J.B. Epidermolysis bullosa – a review of 15 year's experience, including experience with combined general and regional anaesthetic techniques. Anaesth Intens Care. 1988;16:260–264. doi: 10.1177/0310057X8801600304. [DOI] [PubMed] [Google Scholar]
- 16.Lloyd-Thomas A.R., Howard R.F. A pain service for children. Paediatr Anaesth. 1994;4:3–15. [Google Scholar]