Learning objectives.
By reading this article, you should be able to:
-
•
Explain the differences between ECGs in adults and children.
-
•
Evaluate a child's ECG with a structured approach and identify common patterns associated with specific childhood pathologies.
-
•
Characterise and treat major arrhythmias in children.
Key points.
-
•
Use age-appropriate reference ranges when interpreting a child's ECG.
-
•
The right ventricle can be dominant up to the age of 3 yrs, and this is reflected by dominant R waves in Lead V1.
-
•
T waves are normally upright in Lead V1 for the first week of life, after which they become inverted and then revert back upright during adolescence.
-
•
A superior axis on ECG in a cyanotic patient provides a clue for diagnosing tricuspid atresia; in an acyanotic patient, it would suggest an atrioventricular septal defect.
-
•
Supraventricular tachycardias caused by increased automaticity are resistant to treatments used for re-entrant supraventricular tachycardias.
The ECG is a source of invaluable information for the perioperative physician. When interpreted wisely, it aids in the diagnosis of conduction and anatomical abnormalities, and also gives the physician clues to metabolic or electrolyte abnormalities that might be present. Preoperatively, this information will help with creating a tailored anaesthetic plan. Intra- and postoperatively, the physician must be able to recognise and treat pathological rhythms presented to them on the ECG.
Electrocardiogram interpretation in paediatric patients is challenging. The heart of a neonate differs significantly physiologically from an adult's; the developing heart also undergoes continuous change until adulthood.
At birth, the right ventricle is dominant because of the high pulmonary vascular resistance present in utero; this dominance can persist up to the age of 3 yrs. This is reflected on the ECG by the presence of a right axis and dominant R waves in the right precordial leads. (R wave voltages are greater than S wave voltages, but do not exceed normal limits for age.) T waves are upright for the first week after birth, and then become inverted. The T waves gradually become upright again during adolescence.1
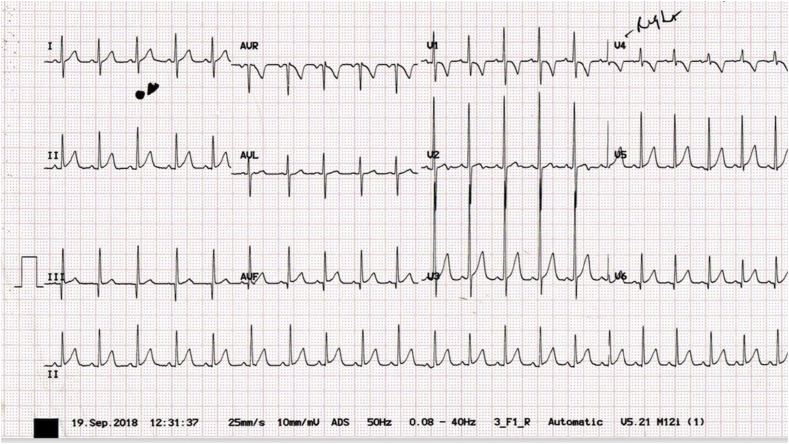
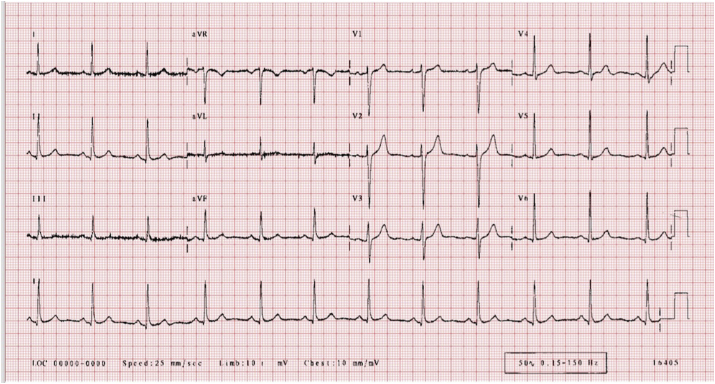
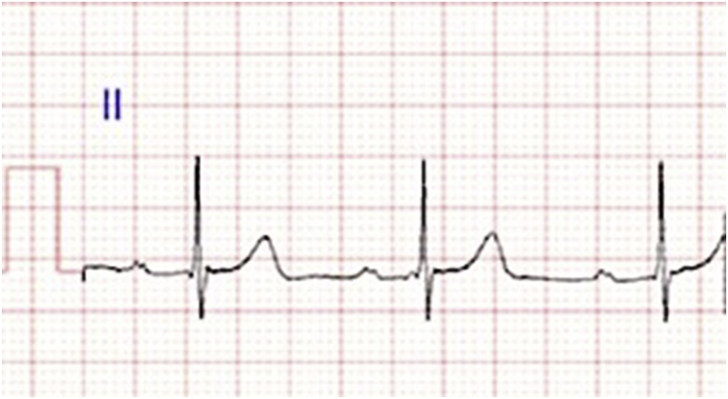
Fig 1, Fig 2 demonstrate the differences between a normal neonatal and an adult ECG.
Fig 1.
Normal neonatal ECG with dominant R waves and inverted T waves in V1.
Fig 2.
Normal adult ECG.
The physician needs to be aware of the effects that normal physiological changes will have on the ECG, and use age-appropriate reference ranges when interpreting a paediatric ECG.
Approach to an ECG
Technical aspects
Always start by assessing the technical quality of the ECG. The clinician must be able to obtain an accurate and good-quality ECG, and recognise when there have been deviations from standard practice in standardisation or paper speed. Failure to do this will lead to erroneous diagnosis and treatments.
Technical checklist:
-
(i)
Identification of patient's name and age
-
(ii)
Lead placement
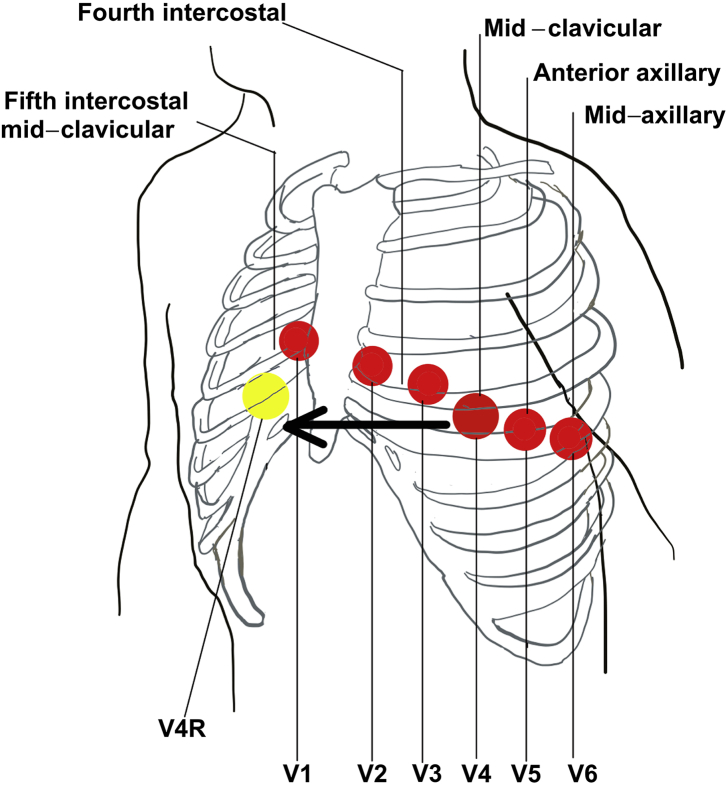
Landmarks for correct ECG lead placement are demonstrated in Figure 3.
Fig 3.
Landmarks for standard and V4R ECG lead placement.
In the younger child, the right ventricle is dominant, and therefore, additional right-sided leads may be recorded (e.g. V3R and V4R). Recording V4R entails placing the V4 cable in the V4R position (right-sided mirror image of V4). Some guidelines recommend omitting V3 when recording V4R.2,3
An additional posterior lead that may be recorded is V7. The V7 electrode position can be found in the posterior axillary line and horizontal to the V4 electrode position.
Incorrect lead placement should be suspected when the lead AvR becomes positive or if any of Lead I, II or III reads as a flatline. Left arm/right arm lead reversal will appear as a completely inverted Lead I and a possible positive AVR, which may mimic dextrocardia.4
-
(iii)Machine recording settings
-
(a)Paper speed (standard: 25 mm s−1): Paper speed is sometimes changed to 50 mm s−1 to unmask hidden P waves during tachyarrhythmias. At this speed, every small square on the ECG paper is therefore now equivalent to 20 ms and not 40 ms. All waveforms and intervals will thus appear prolonged, and care should be taken not to misdiagnose atrial enlargement, bradycardias, atrioventricular (AV) and bundle branch blocks, or long QT syndrome.
-
(b)Voltage gain/sensitivity (standard: 10 mm mV−1): Be careful not to miss ventricular hypertrophy or wrongly diagnose a pericardial effusion (suggested by small complexes) when the gain has been set to 5 mm mV−1.
-
(c)Filters: Filters can lead to loss of ECG information and should only be used after all attempts to reduce the interference have failed.3
-
(d)Recognising artefacts: Important artefacts to be aware of are muscle tremors (baseline appears irregular and spiky) and electromagnetic interference (baseline appears thick as a result of regular oscillations from alternating current).
-
(a)
Structured approach to interpreting a paediatric ECG
A structured approach to examining and interpreting a paediatric ECG will ensure that important abnormalities are not missed. Although no standardised sequence is enforced, we recommend interrogating the ECG in the following sequence:
-
(i)
Rate
-
(ii)
Rhythm
-
(iii)
Axis: P and QRS
-
(iv)
P waves
-
(v)
QRS complex
-
(vi)
T segment and T waves
-
(vii)
Intervals: PR, QRS and QT
Rate
Assess the heart rate according to age-related normal ranges to diagnose bradycardia or tachycardia (Table 1). With regular sinus rhythm and the standard recording speed of 25 mm s−1, heart rate can be calculated by using one of the following formulas: 1,500 divided by the RR interval in small blocks (mm), or 300 divided by the RR interval in big blocks. When the heart rate is irregular, the rate can be calculated by multiplying the number of QRS complexes in the rhythm strip by 6 (an A4 size ECG at normal speed records 10 s of ECG activity).
Table 1.
Normal heart rate ranges for age. Adapted from the Advanced Paediatric Life Support guidelines5
| Heart rate (beats min–1) | |
|---|---|
| Neonate6 | 90–180 |
| Infant | 110–160 |
| 1–5 yrs | 100–150 |
| 6–12 yrs | 80–120 |
| Above 12 yrs | 60–100 |
Rhythm
Normal sinus rhythm is characterised by a P wave preceding every QRS complex and a normal P-wave axis.
Sinus arrhythmia with variation during respiration is a completely normal presentation in the paediatric population.
Axis: P wave
Normal conduction from the sinoatrial node in the right atrium will result in a P-wave axis between 0 and +90°; this is reflected as a positive P wave in Leads I, II and aVF.
Axis: QRS
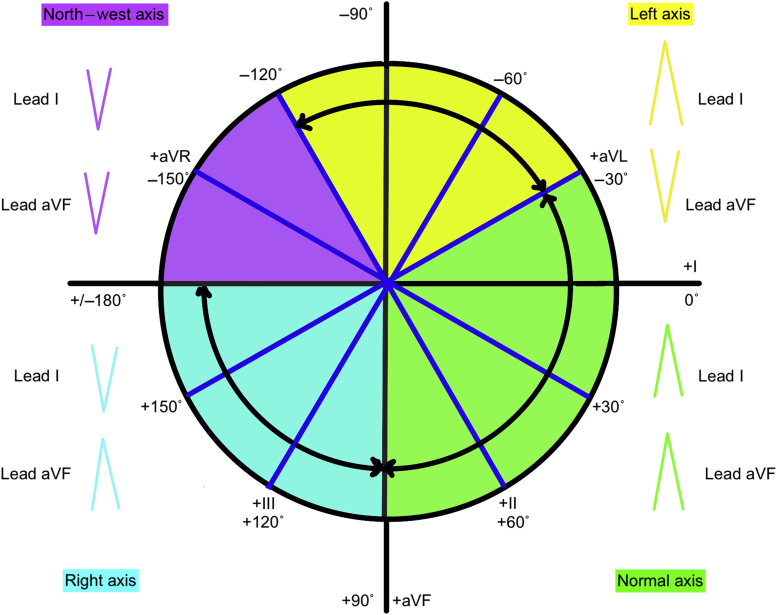
In this article, we define a normal axis as –30 to 90°, a right axis as 90 to 180°, a left axis as –30 to –120°, a north-west axis as –120 to –180°, and a superior axis as –30 to –180° (Table 2).
Table 2.
Normal QRS axis ranges for age. Adapted from Park and colleagues7
| QRS axis (°) | |
|---|---|
| Neonate | 30–180 |
| Infant | 5–125 |
| 1–5 yrs | 5–110 |
| 6–12 yrs | 20–120 |
| >12 yrs | –30 to 105 |
The QRS axis can be calculated using the net vector of ventricular depolarisation in Leads I and aVF. The net R–S vector for Lead I is plotted on 0° and the net R–S vector for Lead aVF is plotted on 90°. The resultant vector gives the QRS axis.
Another method is to look whether the QRS net deflection is positive or negative in Lead I and aVF (Fig. 4).
Fig 4.
QRS axis reference diagram.
P waves
P waves represent atrial depolarisation and are best viewed in Leads II and V1. Left atrial enlargement is suggested by the presence of a notched, widened P wave of more than 2.5 mm or a biphasic P wave in V1. In contrast, a tall P wave of more than 3 mm in infants below 6 months and 2.5 mm in older children suggests right atrial enlargement.
QRS complex
The QRS complex represents ventricular depolarisation and is assessed in Leads V1 and V6. In neonates, the right ventricle is dominant; therefore, the R wave is dominant in V1 and the S wave is dominant in V6 (Table 3). This right ventricular dominance gradually changes to an adult-type left ventricular dominance, which is commonly recognised by the age of 3 yrs.
Table 3.
R wave amplitude (upper limit of normal). Adapted from Saarel and colleagues8
| V1 (mm) | V6 (mm) | |
|---|---|---|
| Neonate | 23 | 19 |
| Infant | 25 | 31 |
| 1–5 yrs | 21 | 35 |
| 6–12 yrs | 17 | 37 |
| >12 yrs | 13 | 33 |
Right ventricular hypertrophy presents as abnormal tall R waves (R waves exceeding upper limits for age) in V1 with abnormal deep S waves in V6. The reverse is seen in left ventricular hypertrophy. Other criteria for right ventricular hypertrophy are right QRS axis, positive T waves in V1 (positive T waves are normal in the first week of life and after adolescence), qR pattern in V1 and an R/S ratio of <1 in V6.
Criteria for left ventricular hypertrophy are decreased R/S ratio (less than lower limit of normal) in V1 and V2, abnormal Q waves in V5 and V6 and inverted T waves in Lead I and aVL.
Depolarisation of the interventricular septum is represented by Q waves on the ECG. Normally, Q waves are seen in Leads I, II, III, aVF, V5 and V6, but their duration should not be longer than 0.03 s and they should not be deeper than 5 mm in children above 3 yrs of age. In children younger than 3 yrs, Q wave amplitude of up to 8 mm can be normal.
ST segments and T waves
It is normal for there to be elevation or depression of ST segments of up to 1 mm in the limb leads and 2 mm in the left precordial leads. Pathological ST segment depression or elevation may occur in myocarditis and the rare congenital cardiovascular malformation called anomalous left coronary artery from the pulmonary artery. Convex-shaped ST segment elevation is a sign of pericarditis. Digoxin causes downsloping of the ST segment and inverted T waves.
T waves are usually upright in Lead V1 in the first week of life, after which they become inverted and then only change back to the upright position at around 8 yrs of age.
U waves
U waves are an additional positive wave at the end of the T wave. U waves can be a normal finding at slow heart rates or can be seen in hypokalaemia.
PR, QRS and QT intervals
Normal values for all these intervals vary with age and heart rate.
PR interval
Normal values are between 90 and 210 ms (Table 4). Delayed AV conduction causes a prolonged PR interval, and can be seen in acute rheumatic fever, digitalis toxicity, hyperkalaemia and certain congenital lesions (AV septal defect [AVSD], atrial septal defect and Ebstein's anomaly). A long PR interval may be a manifestation of high vagal tone and can also occur during sleep, whilst pre-excitation and glycogen storage diseases cause a short PR interval.
Table 4.
Normal PR interval for age (upper limit of normal). Adapted from Saarel and colleagues8
| PR interval (ms) | |
|---|---|
| Neonate | 120 |
| Infant | 140 |
| 1–5 yrs | 170 |
| 6–12 yrs | 190 |
| >12 yrs | 210 |
QRS duration
In children, the QRS duration is much shorter than in adults and varies with age (Table 5). QRS prolongation can be seen in bundle branch blocks, pre-excitation, electrolyte abnormalities, drug toxicity and certain ventricular arrhythmias.
Table 5.
Normal QRS duration for age (upper limit of normal). Adapted from Davignon and colleagues6
| QRS duration (ms) | |
|---|---|
| Neonate | 70 |
| Infant | 75 |
| 1–5 yrs | 75 |
| 6–12 yrs | 85 |
| >12 yrs | 100 |
QT interval
This interval, defined as the start of Q (or R, in the absence of Q) to the end of the T wave, will shorten with a faster heart rate. The corrected QT (QTc) interval is used to standardise the values. The most commonly used formula used to calculate QTc is Bazett's formula:
| (1) |
where QTc is the corrected QT interval, QT is the absolute QT interval, and RR is the preceding RR interval.
Values of up to 440 ms in children and 490 ms in neonates are accepted as normal. In neonates, the Fridericia formula (cube root of RR) is used instead of the Bazett's formula.
A prolonged QTc may occur in congenital long QT syndromes or may be acquired. Congenital syndromes known to cause long QT are Romano–Ward syndrome and Jervell–Lange-Nielsen syndrome (associated with deafness).
Causes of acquired long QT are electrolyte abnormalities (hypokalaemia, hypocalcaemia and hypomagnesaemia), myocarditis, head injury and drugs. Multiple drugs are known to cause a long QT, but the most commonly used ones are amiodarone, macrolide antibiotics, fluconazole, quinidine, haloperidol, droperidol, metoclopramide, 5-HT3 antagonists and tricyclic antidepressants.9 Warning signs on history that should prompt ECG investigation for long QT syndrome are syncope that occurs with exertion, or a history of near drowning.10
The typical dysrhythmia associated with long QT syndrome is a polymorphic ventricular tachycardia (torsade de pointes). Torsade de pointes without a pulse should be treated with defibrillation. Magnesium sulfate should be given to suppress further episodes. Transvenous pacing can be considered in magnesium-resistant torsade.
The reference we recommend for normal paediatric ECG values is by Saarel and colleagues, published in 2018, which obtained these reference ranges using new digital ECG recordings and analysis, as Davignon and colleagues obtained their data using older analogue technology.6,8
Pattern recognition in paediatric ECGs
It is important to interpret the ECG in combination with the history and clinical examination. Common paediatric cardiovascular pathologies, both congenital and acquired, can present with very distinct patterns on an ECG. This is also true for non-cardiovascular pathologies, such as electrolyte abnormalities, neuromuscular disorders and lung disease.
Congenital cardiac lesions
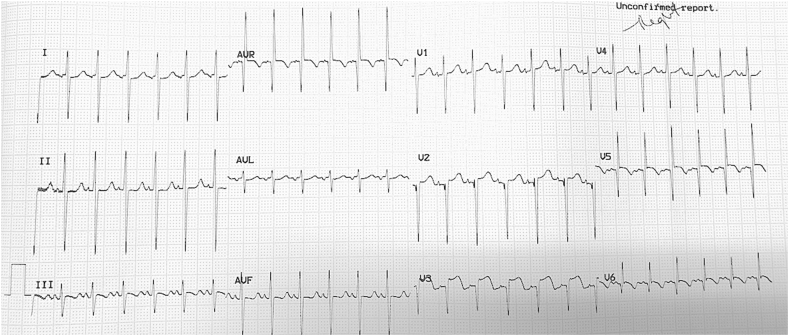
Determining the QRS axis is important in children with suspected congenital cardiac lesions. A superior axis deviation (between –30 and –180°) should be regarded as abnormal. A superior axis in a patient with trisomy-21 presenting with cardiac failure is almost always diagnostic of an AVSD (Fig. 5). Patients that present with cyanosis and a superior QRS axis could have tricuspid atresia or an unbalanced AVSD.
Fig 5.
Superior axis in a patient with an AVSD.
In patients with tetralogy of Fallot, the most common finding on ECG are signs of right ventricular hypertrophy (Fig. 6).11 In patients with Ebstein's anomaly, the most striking feature on ECG are prominent peaked P waves and small R waves in Leads V1 and V2 (Fig. 7).12
Fig 6.
Right-axis deviation with dominant R waves (above the upper limit of normal) and upright T waves in V1 as seen in patients with tetralogy of Fallot.
Fig 7.
Typical peaked P waves as seen in Ebstein's anomaly.
Anomalous left coronary artery from the pulmonary artery is a rare congenital anomaly that can cause myocardial ischaemia and dilated cardiomyopathy early in infancy. The typical ECG changes will be pathological Q waves in the lateral leads with associated ST changes. With a severely dilated left ventricle, there will be deep S waves in V1 and tall R waves in V6.
Acquired cardiac lesions
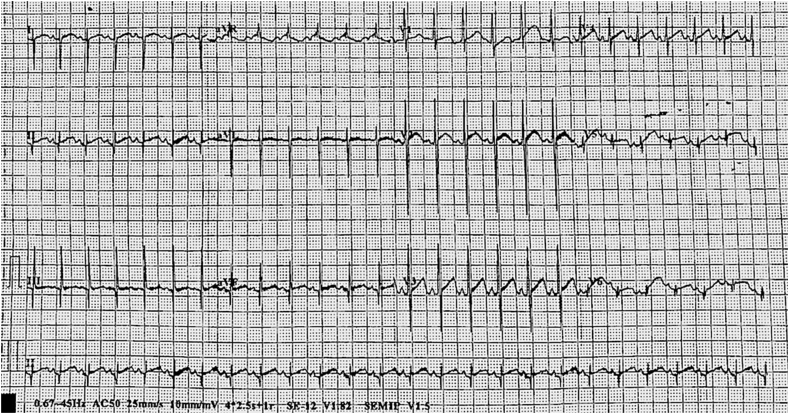
In patients with acute rheumatic fever, the PR interval is usually prolonged on ECG (Fig. 8). This is also one of the minor criteria for the diagnosis of acute rheumatic fever in the modified Jones criteria.
Fig 8.
Prolonged PR interval in acute rheumatic fever.
Patients with acute pericarditis typically have concave ST segment elevation and PR segment depression in limb Leads I, II, III, aVL and aVF, and precordial Leads V1–V6 with the reverse in aVR (Fig. 9).13
Fig 9.
Concave ST segment elevation seen in patients with pericarditis.
Pulmonary hypertension
Common cardiac causes of pulmonary hypertension are large left-to-right shunts, such as ventricular septal defects, AVSDs, patent ductus arteriosus and mixing lesions (such as truncus arteriosus). Non-cardiac causes include lung disease and upper airway obstruction. Typical ECG changes found in pulmonary hypertension are a tall peaked P wave more than 3 mm, features of right ventricular hypertrophy and right-axis deviation (Fig. 10).
Fig 10.
Peaked P waves and right-axis deviation seen with severe pulmonary hypertension.
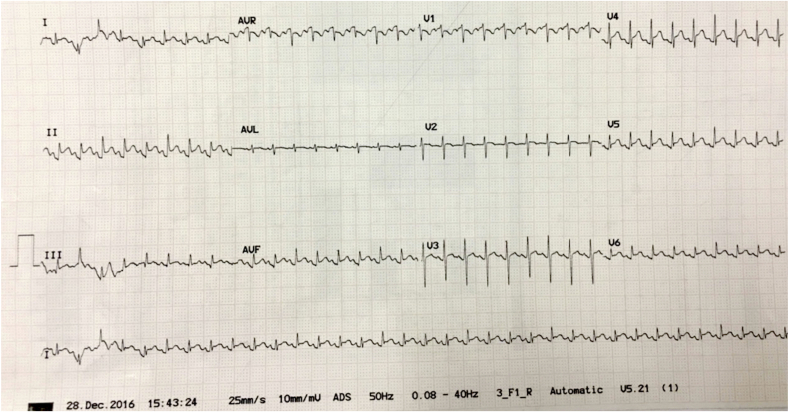
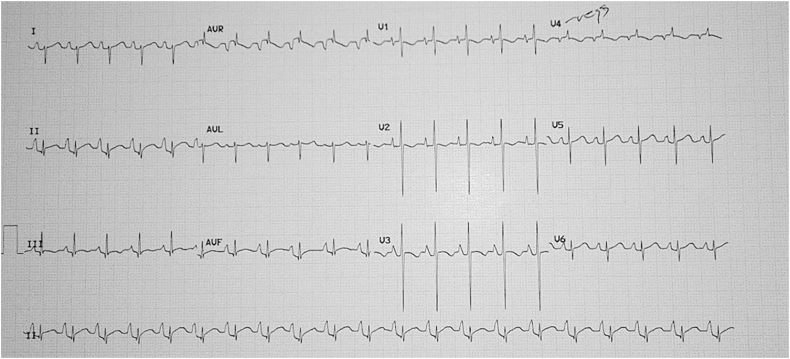
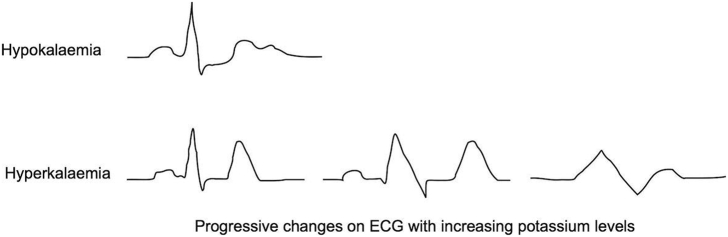
Electrolyte abnormalities
Potassium is essential for normal conduction, and both hypokalaemia and hyperkalaemia cause significant changes on the ECG. With potassium concentrations below 2.5 mmol L−1, U waves typically develop and the QTc will prolong. This is followed by flattening of the T waves, which may become biphasic, and eventual ST segment depression.14
With serum potassium concentrations >6 mmol L−1, the typical progression of changes on ECG are peaked tall T waves seen especially in the precordial leads, prolongation of the QRS and PR interval, disappearance of the P wave, wide biphasic QRS complexes (sine wave) and eventually asystole (Fig. 11).
Fig 11.
ECG changes seen in hypo- and hyperkalaemia.
Duchenne muscular dystrophy
Electrocardiogram changes are commonly seen in patients with Duchenne muscular dystrophy. The most common changes are a shortened PR interval; right ventricular hypertrophy; prominent Q waves in Lead I, aVL, V5 and V6; and a prolonged QTc.15
QRS fragmentation on ECG can be a useful marker of early cardiac involvement in younger patients with Duchenne muscular dystrophy.16
Arrhythmias
Tachyarrhythmias
Supraventricular tachyarrhythmias
Supraventricular tachycardias (SVTs) are summarised in Table 6. As a group, they are also frequently classified as narrow QRS complex tachycardias. This classification system simplifies the process of making a diagnosis. Unfortunately, there are some SVTs, specifically in the AV re-entry tachycardia (AVRT) group that do not fit this description, causing potential confusion. A basic understanding of the two main underlying mechanisms causing SVTs helps with ECG diagnosis and with the emergency treatment of these tachyarrhythmias.
Table 6.
Classification of supraventricular tachyarrhythmias. Adapted from the Paediatric Critical Care Study Guide and the Advanced Paediatric Life Support treatment guidelines5,17,18
|
Unstable 1. Cardioversion
1. Vagal manoeuvre 2. Adenosine
|
||
|
|||
|
|
 |
|
|
|
 |
|
|
|
||
|
|
 |
|
|
|
 |
|
|
|
 |
|
|
|
 |
|
| |||
|
|
 |
Treat underlying cause |
|
|
 |
Slow automaticity
|
|
|
 |
|
|
|
 |
|
Kadam and colleagues.18
The first mechanism, re-entry, occurs when a single heartbeat can regenerate itself by following a circular conduction pathway.
The prerequisites for a re-entry tachycardia are:
-
(i)
A conduction pathway that contains both a fast pathway (fast conduction velocity, but a slow refractory period) and a slow pathway (slow conduction velocity, but a fast refractory period)
-
(ii)
A premature beat that arrives when one of the pathways is refractory
This circular pathway can form in the atrial tissue and lead to the atrial re-entry tachycardias, atrial fibrillation and atrial flutter. In AVRT and AV nodal re-entry tachycardias (AVNRTs), the fast pathway is the normal AV pathway, whilst the additional slow pathway is either in the AV node itself (AVNRT) or totally separate from the AV node (AVRT). Adenosine will slow conduction through the AV node, and thus conduction through the one limb of the circular re-entry pathway, which will lead to the termination of the re-entry circuit in AVRT and AVNRT.
In atrial re-entry tachycardias, the circular pathway exists in the atria above the AV node; as such, adenosine will not terminate the circuit. However, by slowing the impulses conducted through the AV node, adenosine might unmask flutter or fibrillation waves, and is a diagnostic rather than a therapeutic agent in this scenario.
The distinguishing factor between AVRT and AVNRT is the position of the retrograde P wave. In AVRT, there is a larger circuit within which the impulse must travel before the atria are reactivated as the accessory pathway is outside of the AV node. This leads to a retrograde P wave that will either appear halfway between two QRS complexes or on top of a T wave. In AVNRT, the circuit is much smaller as the accessory pathway is within the AV node. This gives rise to a retrograde P wave that is either hidden within the QRS complex, or appears shortly after the QRS complex.2
Atrioventricular re-entry tachycardia can give rise to either a narrow complex SVT or a wide complex SVT attributable to orthodromic or antidromic conduction. Orthodromic conduction is the most common, where the impulse conducts through the normal AV node and the His bundle, resulting in a narrow QRS complex. In antidromic conduction, the impulse spreads through the accessory pathway, which means depolarisation is partially via the ventricular myocardium, and thus results in a broad QRS complex.
The second mechanism that may lead to an SVT is automaticity. It can be very difficult to distinguish an AVRT from an automatic junctional ectopic tachycardia (JET). Some distinguishing signs are that, in a JET, there is a gradual rate increase, whereas in a re-entry SVT, the dysrhythmia begins suddenly, with a heart rate that varies little from one episode to another.
Junctional ectopic tachycardia occurs mostly postoperatively and is quite resistant to re-entry tachycardia treatment modalities. It will potentially slow down, but does not terminate with vagal manoeuvres, adenosine or cardioversion. Treatment is aimed at slowing automaticity and restoring AV synchrony.
Ventricular tachyarrhythmias
The two main ventricular tachyarrhythmias to recognise are ventricular tachycardia and ventricular fibrillation.
Ventricular tachycardia
Ventricular tachycardia is typified by a broad complex monomorphic tachycardia. P waves are absent or retrograde.
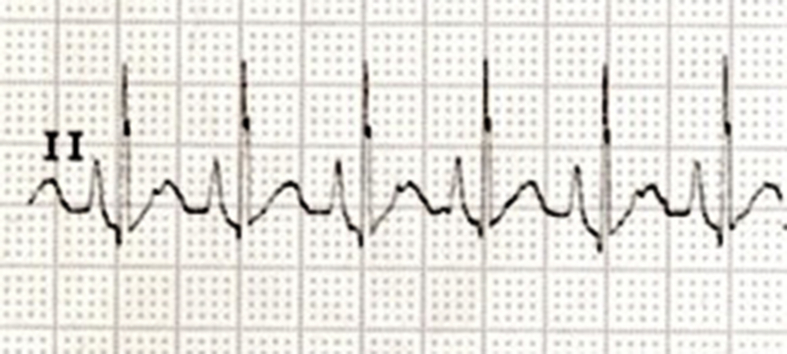
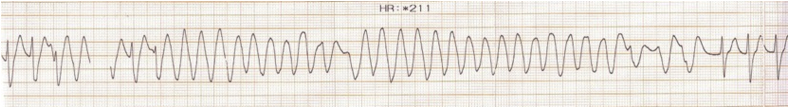
Torsade de pointes is a form of ventricular tachycardia, in which the QRS complexes are wide and polymorphic, and appear to be twisting around the ECG baseline (Fig. 12). Torsade de pointes is associated with prolonged QT syndrome, which was discussed previously.
Fig 12.
Torsade de pointes.
The emergency treatment of a patient with a ventricular tachycardia who has a pulse, but is unstable, is cardioversion with 1–2 J kg−1.5 The treatment in a stable patient is amiodarone 5 mg kg−1 over 30 min, with correction of electrolyte abnormalities, especially magnesium. Cardioversion can also be considered. The treatment of the patient with a pulseless ventricular tachycardia is according to the ventricular fibrillation protocol, discussed next.
Ventricular fibrillation
Ventricular fibrillation is a life-threatening rhythm, and thus needs urgent diagnosis and treatment.
Ventricular fibrillation is characterised on ECG by rapid, chaotic, irregular and wide oscillations of the baseline. There are no recognisable P waves, QRS complexes or T waves.
Emergency treatment is to commence cardiopulmonary resuscitation immediately and follow with unsynchronised defibrillation (4 J kg−1).5
Bradyarrhythmias
Sinus bradycardia
Diagnostic ECG features are a sinus rhythm that is slower than the lower limit of normal for age.
Management of a sinus bradycardia is to seek and treat the underlying causes, which include hypoxia, electrolyte disturbances (hyperkalaemia or hypercalcaemia), hypothermia, hypothyroidism, raised intracranial pressure and certain drugs (beta blockers and digoxin). If the heart rate is less than 60 and shock is present, chest compressions should be started. Hypoxia should be urgently addressed and vagal overactivity managed with atropine 0.02 mg kg−1. If shock and bradycardia persist, adrenaline and pacing may be indicated.5
AV junctional/nodal bradycardia
Diagnostic ECG features are inverted P waves that occur before, during or after the QRS complex with a regular QRS rate between 40 and 60.2 Asymptomatic patients do not need treatment, but if there are signs of shock, atropine or pacing may be indicated.10
Conduction abnormalities
-
(i)
First-degree AV block: Diagnostic ECG features are normal P waves with a prolonged PR interval.
-
(ii)
Second-degree AV block Type I: This block is diagnosed when there is progressive lengthening of the PR interval leading to a P wave that is not followed by a QRS complex.
-
(iii)
Second-degree AV block Type II: Diagnostic ECG features are a constant PR interval with occasional non-conducted P waves.
-
(iv)
Third-degree AV block/complete heart block: Here, the atria and ventricles work independently of each other with no atrial impulses being conducted to the ventricles. On the ECG, this translates into regular atrial and ventricular rhythms with regular RR and PP intervals, respectively (Fig. 13). A bradycardia in an asymptomatic patient should prompt the performance of a 12-lead ECG with a rhythm strip to exclude a third-degree AV block. The cause can be congenital or acquired, most commonly secondary to cardiac surgery. In a neonate with complete heart block, the mother should be tested for anti-Ro and anti-La antibodies to rule out neonatal lupus.19 Symptomatic congenital or acquired (post-surgical) AV blocks will require permanent pacing.20
Fig 13.
Complete heart block.
Conclusions
Whilst pattern recognition is a useful skill, this should not prevent the clinician from following a structured approach when interpreting a paediatric ECG. If any abnormality is detected on ECG, then further investigation and review by an expert may be indicated.
Declaration of interests
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) are accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Lelanie Lambrechts Dip PEC (SA) DA (SA) FCA (SA) Cert Critical Care (SA)Paed is a consultant anaesthetist at Groote Schuur Hospital and Red Cross War Memorial Children's Hospital. She has a special interest in paediatric intensive care and perioperative medicine.
Barend Fourie FC Paed (SA) Cert Cardiology (SA)Paed is a consultant paediatric cardiologist at Tygerberg Hospital and senior lecturer at the University of Stellenbosch. His major interests are interventional cardiology and advanced imaging.
Matrix codes: 1A03, 2D02, 3D00
References
- 1.Dickinson D.F. The normal ECG in childhood and adolescence. Heart. 2005;91:1626–1630. doi: 10.1136/hrt.2004.057307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowbrick S., Borg A.N. Edinburgh, UK, Churchill Livingstone; 2006. ECG complete. [Google Scholar]
- 3.Campbell B., Richley D., Ross C., Eggett C. 2017. Clinical guidelines by consensus: recording a standard 12-lead electrocardiogram, an approved methodology by the Society for Cardiological Science & Technology (SCST)https://www.bmj.com/sites/default/files/response_attachments/2016/09/CAC_SCST_Recording_a_12-lead_ECG_final_version_2014_CS2v2.0.pdf Available from: [Google Scholar]
- 4.Batchvarov V.N., Malik M., Camm A.J. Incorrect electrode cable connection during electrocardiographic recording. Europace. 2007;9:1081–1090. doi: 10.1093/europace/eum198. [DOI] [PubMed] [Google Scholar]
- 5.Samuels M., Wieteska S. Wiley-Blackwell; West Sussex, UK: 2011. Advanced paediatric life support: a practical approach. [Google Scholar]
- 6.Davignon A., Rautaharju P., Boisselle E., Soumis F., Mégélas M., Choquette A. Normal ECG standards for infants and children. Pediatr Cardiol. 1980;1:123–131. [Google Scholar]
- 7.Park M.K., Guntheroth W.G. Mosby/Elsevier; Philadelphia, PA: 2006. How to read pediatric ECGs. [Google Scholar]
- 8.Saarel E.V., Granger S., Kaltman J.R. Electrocardiograms in healthy North American children in the digital age. Circ Arrhythm Electrophysiol. 2018;11 doi: 10.1161/CIRCEP.117.005808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Hare M., Maldonado Y., Munro J., Ackerman M.J., Ramakrishna H., Sorajja D. Perioperative management of patients with congenital or acquired disorders of the QT interval. Br J Anaesth. 2018;120:629–644. doi: 10.1016/j.bja.2017.12.040. [DOI] [PubMed] [Google Scholar]
- 10.Doniger S.J., Sharieff G.Q. Pediatric dysrhythmias. Pediatr Clin North Am. 2006;53:85–105. doi: 10.1016/j.pcl.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Roberts D.L., Wagner H.R., Lambert E.C. The electrocardiogram in tetralogy of fallot. J Electrocardiol. 1972;5:155–161. doi: 10.1016/s0022-0736(72)80031-1. [DOI] [PubMed] [Google Scholar]
- 12.Attenhofer Jost C.H., Connolly H.M., Edwards W.D., Hayes D., Warnes C.A., Danielson G.K. Ebstein’s anomaly—review of a multifaceted congenital cardiac condition. Swiss Med Wkly. 2005;135:269–281. doi: 10.4414/smw.2005.10985. [DOI] [PubMed] [Google Scholar]
- 13.Spodick D.H. Acute pericarditis. JAMA. 2003;289:1150. doi: 10.1001/jama.289.9.1150. [DOI] [PubMed] [Google Scholar]
- 14.Diercks D.B., Shumaik G.M., Harrigan R.A., Brady W.J., Chan T.C. Electrocardiographic manifestations: electrolyte abnormalities. J Emerg Med. 2004;27:153–160. doi: 10.1016/j.jemermed.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Thrush P.T., Allen H.D., Viollet L., Mendell J.R. Re-examination of the electrocardiogram in boys with Duchenne muscular dystrophy and correlation with its dilated cardiomyopathy. Am J Cardiol. 2009;103:262–265. doi: 10.1016/j.amjcard.2008.08.064. [DOI] [PubMed] [Google Scholar]
- 16.Yoo W.H., Cho M.J., Chun P., Kim K.H., Lee J.S., Shin Y.B. The evolution of electrocardiographic changes in patients with duchenne muscular dystrophies. Korean J Pediatr. 2017;60:196–201. doi: 10.3345/kjp.2017.60.6.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lucking S.E. Springer; London, UK: 2012. Pediatric critical care Study Guide: text and review. [Google Scholar]
- 18.Kadam S., Tailor K., Kulkarni S., Mohanty S., Joshi P., Rao S. Effect of dexmedetomidine on postoperative junctional ectopic tachycardia after complete surgical repair of tetralogy of Fallot: a prospective randomized controlled study. Ann Card Anaesth. 2015;18:323–328. doi: 10.4103/0971-9784.159801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salomonsson S., Strandberg L. Autoantibodies associated with congenital heart block. Scand J Immunol. 2010;72:185–188. doi: 10.1111/j.1365-3083.2010.02442.x. [DOI] [PubMed] [Google Scholar]
- 20.Singh H.R., Batra A.S., Balaji S. Pacing in children. Ann Pediatr Cardiol. 2013;6:46–51. doi: 10.4103/0974-2069.107234. [DOI] [PMC free article] [PubMed] [Google Scholar]