Learning objectives.
By reading this article the reader should be able to:
-
•
Identify the importance of data collection and risk stratification in patients needing an emergency laparotomy.
-
•
Explain the principles and importance of a care pathway that extends into the postoperative period.
-
•
Describe the management of anaesthesia for these cases.
-
•
Discuss that these patients require significant resources but if managed properly mortality can be improved.
Key points.
-
•
Emergency laparotomy is a common surgical procedure with significant economic impact and a 30-day mortality approaching 15%.
-
•
Patients are often elderly with comorbidities that might not be treated optimally.
-
•
Key goals of anaesthesia are to secure the airway rapidly; maintain cardiovascular stability; and use goal-directed fluid therapy and critical care facilities appropriately, guided by risk scoring.
-
•
Postoperative pain relief is very important and all modalities should be considered.
-
•
The use of the nine key standards of care identified by the UK National Emergency Laparotomy Audit has decreased mortality, saving an estimated 300 lives per year.
An emergency laparotomy is a common surgical procedure, performed for a wide variety of intra-abdominal pathologies, which has a significant associated morbidity and mortality. Included under this umbrella term are a heterogenous collection of conditions and presentations, often in patients with significant physiological derangement and comorbidities. These cases represent a significant challenge to both clinicians and organisations involved with their management.
Each year, approximately 30,000 emergency laparotomies are performed in the UK.1 In 2012, there was a reported 30-day mortality of 14.9% for all patients undergoing an emergency laparotomy, increasing to 25% in those aged >80 yrs.2 A report from the Royal College of Surgeons in 2011 suggested that patients presenting for emergency general surgery were a ‘forgotten group’, but accounted for the largest proportion of surgical admissions to hospital and surgical deaths. These patients had a high complication and mortality rate, and intensive care costs of £88 million per year nationally.3, 4, 5 Delays in access to investigations, lack of access to senior clinicians, and time to surgery are several modifiable factors that contribute to poor outcomes.
The issues described above were addressed in the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report, ‘Knowing the risk’, which highlighted that emergency surgery outcomes in the UK were worse than those seen in the USA, suggesting an 8-fold increase in mortality in patients who had a predicted mortality rate of 0–5%.6 The report suggested that the differences could be overcome by better identification of high-risk patients; improved triage and preassessment; better intraoperative care; and improved postoperative care, including increased use of critical care. Since then, several ventures and collaborations have attempted to address these issues. These include the Emergency Laparotomy Network, National Emergency Laparotomy Audit (NELA), and the Emergency Laparotomy Collaborative (ELC).
Preoperative management
Indications for laparotomy
There are a wide variety of indications for emergency laparotomy. Advances in medical imaging and minimally invasive surgical techniques have decreased the need for exploratory laparotomy; in most cases the diagnosis and intended operation are known beforehand.
Common indications for laparotomy are listed in Table 1.
Table 1.
Recorded indications for performing emergency laparotomy. Data from the first report of the National Emergency Laparotomy Audit, 20157
| Indication for surgery | Number of patients | Frequency (%) |
|---|---|---|
| Intestinal obstruction | 9,811 | 49 |
| Perforation | 4,744 | 24 |
| Peritonitis | 4,116 | 20 |
| Ischaemia | 1,720 | 9 |
| Abdominal abscess | 1,332 | 7 |
| Sepsis: other | 1,474 | 7 |
| Haemorrhage | 819 | 4 |
| Colitis | 748 | 4 |
| Anastomotic leak | 618 | 3 |
| Intestinal fistula | 326 | 2 |
| Abdominal wound dehiscence | 116 | 0.6 |
| Abdominal compartment syndrome | 55 | 0.3 |
| Planned relook | 51 | 0.3 |
| Other | 1,758 | 9 |
| Total | 27,688 |
Patients with perforation, peritonitis, and obstruction are highly likely to need emergency laparotomy. However, in some instances initial conservative treatment is appropriate, for example: (i) obstruction secondary to adhesions, when conservative management up to 72 h in the absence of bowel ischaemia is acceptable; (ii) localised abscess amenable to ultrasound or CT-guided drainage; (iii) malignant large bowel obstruction, which can be treated with a stent if there is no perforation or peritonism; and (iv) colitis or inflammatory bowel disease that can be managed medically in the first instance. Although these are indications for laparotomy, many types of intra-abdominal surgery are not included (appendicectomy, cholecystectomy, emergency abdominal aortic aneurysm repair, obstetric and gynaecological laparotomies).
Preoperative preparation
Anaesthetic assessment will begin the process of risk stratification through history, examination, and tests. Routine investigations include blood tests (including a pregnancy test if appropriate), arterial or venous blood gas and serum lactate, a chest X-ray, ECG, and usually a CT scan. In addition to pre-existing comorbidities, the diverse pathologies mandating the laparotomy can have profound effects on the patient, all of which influence the choice of anaesthetic agents, monitoring, and perioperative management. These include profound hypovolaemia in patients with bowel obstruction, sepsis in patients with bowel perforation or ischaemia; and effects secondary to these changes such as acute kidney injury and pulmonary atelectasis.
In many patients requiring a laparotomy, it is important to consider and treat sepsis. The Surviving Sepsis Campaign guidelines, most recently updated in 2016, report that early antibiotics, given within 1 h, have been shown to reduce mortality in septic shock.8 A recommendation by NELA is to administer antibiotics within the first hour of diagnosis of sepsis. Other Surviving Sepsis Campaign recommendations of relevance include preoperative resuscitation with fluids in volumes of up to 30 ml kg−1, aiming for a mean arterial pressure of >65 mm Hg, and the need for frequent reassessment of resuscitation priorities. It should be emphasised that in the majority of emergency laparotomies, resuscitation must not delay access to surgery, and should be managed concurrently with timely access to the operating theatre. For patients requiring urgent surgery, the aim is for definitive surgery within 6 h of decision to perform surgery, although the most life-threatening cases require surgery within 2 h.
The pathophysiological changes encountered in patients requiring an emergency laparotomy are multifactorial. Sepsis, encountered in many patients needing an emergency laparotomy, is a state defined by the pathophysiological changes of arterial and venous vasoplegia, increased tissue oedema caused by disruption of endothelial glycocalyx, and ventricular dysfunction.9 This combination of factors, and the potential for significant fluid shifts and fluid losses, reflect the fact that although early resuscitation is important, assessment of fluid balance and fluid requirements in this group of patients is challenging, and overzealous administration of fluids may have detrimental effects. This highlights the importance of cardiac output monitoring and the early use of vasopressors.
Management of anaesthesia
Management of anaesthesia is centred around: (i) rapidly securing of the airway, minimising the risks of pulmonary aspiration; (ii) haemodynamic stability during rapid sequence induction of anaesthesia and throughout the perioperative period; (iii) optimal volume and type of fluids; (iv) protective lung ventilation strategies; (v) analgesia; and (vi) postoperative considerations.
Airway securement and rapid sequence induction of anaesthesia
In the Royal College of Anaesthetist's Fourth National Audit Project (NAP4), the most common 'anaesthetic' cause of death was pulmonary aspiration of gastric contents; the incidences of aspiration syndromes were one in 400,000 cases for elective anaesthesia and as high as one in 900 cases for emergency anaesthesia.
There are several options for the agents used for induction of anaesthesia. Whichever anaesthetic technique is chosen, it must deliver the following: rapid onset anaesthesia and neuromuscular blockade, good conditions for tracheal intubation, and haemodynamic stability. Measures to avoid hypotension at induction of anaesthesia include the use of a large dose of short-acting opioid (such as alfentanil) to reduce the dose of thiopental or propofol; the use of ketamine (at a dose of 1–2 mg kg−1) as the iv induction agent, and the use of a vasopressor after induction to maintain arterial pressure. The use of rocuronium 1.2 mg kg−1 instead of succinylcholine has gained popularity for neuromuscular block, mainly because of the increased availability of sugammadex to reverse dense rocuronium-induced neuromuscular block, and the adverse effects of succinylcholine, such as hyperkalaemia, succinylcholine apnoea, and malignant hyperthermia.10 It is imperative that whichever induction agents and neuromuscular blocking agents are used, the anaesthetist must be familiar in their use in these high-risk patients.
If an indwelling nasogastric tube is present, it should be suctioned to further minimise the risk of pulmonary aspiration of gastric contents. Maintenance of anaesthesia can be with volatile agents or total intravenous anaesthesia, depending on the clinician's preference and the clinical situation.
Management of fluids and haemodynamic support
There are several measures that can guide intravenous fluid therapy during a laparotomy. These include haemodynamic features such as heart rate and arterial pressure, and markers of organ perfusion such as serial serum lactate and base excess. An arterial catheter is strongly advised, usually sited before induction of anaesthesia because of the risk of hypotension at induction. A central venous catheter, inserted either before or after induction of anaesthesia, may be indicated if the patient has sepsis and is requiring vasopressors (see below). A urinary catheter is mandated for monitoring of urine output.
The choice of fluid depends on the clinical situation; although balanced crystalloid solutions offer the mainstay of therapy, blood products may be considered in patients with anaemia, thrombocytopaenia, or coagulopathies. Because of their association with kidney injury, synthetic colloids such as hydroxyl ethyl starches (HES) are no longer indicated.11
It is important that the patient undergoing emergency laparotomy receives an adequate, but not excessive, volume of intravenous fluid. Too little risks hypovolaemia, inadequate tissue perfusion, metabolic acidosis, and organ dysfunction. Too much results in tissue oedema, pulmonary oedema, and impaired oxygenation, and the risk of anastomotic breakdown. Current evidence suggests that the use of goal-directed fluid therapy (GDFT) techniques can reduce both the complications associated with surgery and length of hospital stay, but has no effect on mortality compared with conventional fluid administration.12, 13 An ongoing randomised trial, the Fluid Optimisation in Emergency Laparotomy (FLO-ELA) trial, will attempt to address whether goal directed fluid is of benefit in patients undergoing acute laparotomy. Despite this, the use of GDFT techniques, such as pulse contour analysis techniques and the oesophageal Doppler, is widespread, and is advocated by the ELC. Discussion of the application and pitfalls of each technique is outside the scope of this article.14
A vasopressor infusion may be required in the face of fluid-resistant hypotension, especially in patients with sepsis. Noradrenaline (norepinephrine) is the first-line vasopressor in this group of patients. Other vasopressors for peripheral use include phenylephrine and metaraminol.
Other perioperative targets include the maintenance of normothermia using fluid warmers and surface air warmers. This prevents the sequelae of hypothermia such as coagulopathy and increased risk of wound infection.
Patients with a significant degree of compromise, comorbidity, or ongoing sepsis, may require organ support and high dependency care. It is recommended by NELA that patients with a mortality risk of more than 10% are admitted to intensive care, as calculated using the NELA risk calculator. This tool has been validated in this group of patients and is the recommended risk calculator for patients undergoing laparotomy.15
Protective lung ventilation
The concept of lung protective ventilation has arisen from the management of patients with acute respiratory distress syndrome (ARDS); it suggests low tidal volumes of 6–8 ml kg−1 to avoid volutrauma, inflation pressure limited to 30 cm H2O to avoid barotrauma and optimum positive end expiratory pressure (PEEP). It has been suggested that a low tidal volume technique (6–8 ml kg−1) without high PEEP may be a good starting point in the patient without ARDS, with optimisation of PEEP and the use of recruitment manoeuvres as indicated.16
Acute lung injury is the most common cause of postoperative respiratory failure, and the incidence of respiratory complications may exceed that of cardiac complications. The nature and extent of the intra-abdominal pathology may have a significant impact on the ability to ventilate the patient's lungs effectively; permissive hypercapnia, as sometimes used in patients with ARDS, may not be appropriate in a patient with a pre-existing metabolic acidosis.
Postoperative care
Analgesia
Poorly managed pain after a laparotomy is a leading contributor to postoperative complications and mortality. Inadequate analgesia may lead to distress and an increased risk of postoperative pulmonary complications such as atelectasis and pneumonia; cardiac complications such as myocardial ischaemia; thromboembolic events; and a greater stress response. Pain after laparotomy has two sources, both of which need to be addressed using appropriate analgesics. The pain from somatic afferent nerve fibres associated with skin and muscle incision is different from the visceral pain from stretch and inflammation of the peritoneum. This principle should be remembered when treating post laparotomy pain—the visceral deeper pain resolves more rapidly than the somatic pain from the incision. Management of the somatic ‘incision’ pain, so that the patient may deep breathe, cough, move around the bed, and walk, should be the goal of analgesia. This is often best managed, as far as is possible, without the use of high dose opioids, either during or after surgery. Opioids are associated with postoperative cognitive dysfunction, respiratory depression and gastrointestinal dysfunction.17 Techniques to minimise the use of opioids include central neuraxial analgesia, transversus abdominus plane (TAP), or posterior rectus sheath blocks, either single shot or catheter, placed by the surgeon directly or the anaesthetist using ultrasound. These techniques are usually very effective at managing postoperative pain, even in complicated situations.18 However, each of these strategies is associated with risks, especially in these high-risk patients. Central neuraxial strategies, such as epidural and spinal analgesia, may be especially hazardous—concerns include hypotension caused by vasodilatation in a patient with sepsis or hypovolaemia; and the presence of contraindicating factors such as coagulopathy or systemic sepsis that increase the risks of epidural haematoma or abscess formation. However, thoracic epidural analgesia can provide superior analgesia for abdominal, thoracic, and pelvic surgery and also reduce the incidence of postoperative ileus.
Other effective options for analgesia to reduce the need for opioids include the intraoperative administration of lidocaine i.v., ketamine, and magnesium. The use of these agents is increasing, but is not universal, and evidence for their use is mainly derived from patients undergoing elective abdominal surgery. Lidocaine i.v., given initially as a bolus (1–2 mg kg−1) then as an infusion (0.5–3 mg kg−1 h−1), can reduce opioid requirements and improve postoperative gastrointestinal motility.19 Ketamine is efficacious as an analgesic in abdominal surgery, reduces opioid requirement, and can reduce the risk of the development of postoperative chronic pain.20 However, ketamine is associated with the risk of postoperative psychiatric adverse effects.21 Magnesium reduces the requirement for opioids, improves analgesia, and can reduce the hyperalgesia seen with remifentanil. Potential adverse effects of magnesium include hypotension and the prolongation of neuromuscular block.22
After operation, oxycodone or morphine can be used via a patient-controlled analgesia (PCA) system. Paracetamol is used during operation. Given the high incidence of hypovolaemia and acute kidney injury in these patients, NSAIDs are often contraindicated.
Other postoperative considerations
There is an increased recognition of the importance of postoperative intensive care after an emergency laparotomy. NELA suggests all patients with a predicted mortality of 10% should be admitted to ICU after laparotomy, whereas the ELC group suggests that all patients should be admitted to ICU after a laparotomy. Decisions around whether the patient is suitable for tracheal extubation, or whether a period of postoperative lung ventilation is required, will be guided by several factors at the end of laparotomy. These include the patient's acid base status, oxygen requirement, vasopressor requirements, and temperature. It may be that resuscitation will be required after the end of the procedure.
If tracheal extubation is indicated, the risk of pulmonary aspiration is significant around the time of extubation itself. Before extubation, it is prudent to again aspirate an indwelling nasogastric tube, and suction the pharynx. In the patient undergoing emergency laparotomy, tracheal extubation should be delayed until the patient is awake with the return of protective airway reflexes.
Other postoperative considerations include the avoidance of hyperglycaemia and optimising nutritional status. Sepsis and the surgical stress response are hypercatabolic states, leading to loss of muscle mass and deconditioning. After laparotomy, it may be that enteral nutrition is avoided for a period, and parenteral nutrition is used to attempt to prevent malnutrition, sarcopenia, and weakness. Thromboprophylaxis is also important in the postoperative period.
National laparotomy collaboratives
In response to a statement from the Association of Surgeons of Great Britain and Ireland (ASGBI), which highlighted the unacceptably high mortality rate in emergency cases, the Emergency Laparotomy Network was formed. In 2012, they published their first report into emergency laparotomies. This report concluded that emergency laparotomy cases were associated with a high mortality, and highlighted the need for a national quality improvement programme. Recent developments have attempted to address this. These included the NELA and the ELC.
National Emergency Laparotomy Audit
Having started in 2012, NELA is a joint national audit between the Royal College of Anaesthetists, National Institute of Academic Anaesthesia (NIAA), Royal College of surgeons, and Health Quality improvement Project (HQIP). The stated aim of NELA is to describe and compare inpatient care of those undergoing emergency bowel surgery to promote quality improvement. Standards revised from the first report in 2015 to the third report in 2017 (Table 2) include a greater focus on formal risk assessment, prompt consultant-led investigation and surgery provided by consultant surgeons and anaesthetists, and increased utilisation of critical care after operation. Aside from annual national reports, participating hospitals are able to review their performance against other hospitals.
Table 2.
National Emergency Laparotomy Audit (NELA) care standards from the third NELA report, 2017.1 RAG = Red Amber Green (red, not met, amber partially met and green met).
| Key standards currently subject to RAG rating |
|---|
|
The fourth report, published in 2018, demonstrated a reduced 30-day mortality in participating hospitals of 9.5%.23 It also reported reduced length of stay, improved access to operating theatre, and improved access to critical care facilities. However, it states that further improvements need to be made in provision of geriatrician-led care to elderly patients undergoing laparotomy, and timely antibiotic provision in patients with sepsis needing a laparotomy. There is now a web-based application from NELA, which is validated in this group of patients.
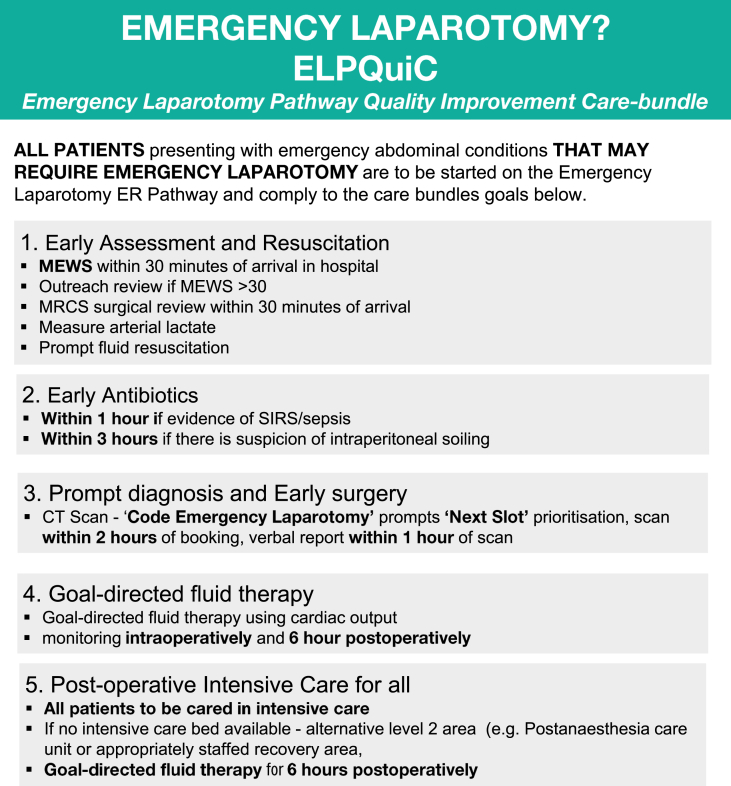
ELC and Emergency Laparotomy Pathway Quality Improvement Care
The Emergency Laparotomy Pathway Quality Improvement Care (ELPQuiC) bundle project commenced in 2011 and utilised a formalised pathway for emergency laparotomy patients at four UK hospitals.24 Features of the bundle are reproduced in Figure 1. This approach significantly reduced mortality in the hospitals studied. This led to the development of the ELC, which incorporated 28 UK hospitals, all of which utilised the same bundle. The project, which ran for 2 yrs, led to a mortality rate of 8.1% for emergency laparotomy cases, compared to a mortality of 10.6% for the same period for hospitals participating in NELA.
Fig 1.
Emergency Laparotomy Pathway Quality Improvement Care (ELPQuiC) bundle. From the Emergency Laparotomy Collaborative with permission.
Both NELA and the ELC highlight the success of the use of a protocolised approach. These protocols, also highlighted elsewhere, incorporate consultant-led care and ICU care for all patients, early antibiotics, and GDFT.25, 26 It has been shown repeatedly that these protocols should form the cornerstone of management for the patient undergoing emergency laparotomy. The third NELA report stated that a best practice tariff is to be introduced in the UK for emergency laparotomy, which should lead to sustained improvements, as seen in patients with fractured neck of femur.
Summary
Emergency laparotomies are performed in high numbers for a diverse range of pathologies, and are associated with significant morbidity, mortality, and complications. Patients presenting for laparotomy may have significant pre-existing comorbidity, compounded by the haemodynamic and metabolic effects of organ hypoperfusion, hypovolaemia, and sepsis. A detailed, but timely, approach to preoperative assessment and resuscitation will help elucidate the need for further investigation, perioperative management techniques, and required levels of support, both during and after surgery. Optimal administration of fluids, haemodynamic support, and effective analgesia are crucial to a good outcome.
Although the mortality associated with emergency laparotomy remains high, progress is being made because of the work of NELA and the ELC. These ‘bundled’ approaches highlight the importance of risk stratification, consultant input throughout the patient's hospital stay, and the increased utilisation of critical care. It is hoped that with greater uptake of this approach, outcomes will continue to improve.
Declaration of interests
The authors declare that they have no conflict of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
John Jones FRCA is a consultant at Leeds Teaching Hospitals, a Final FRCA examiner and the regional advisor in anaesthesia for West Yorkshire. His clinical interests include anaesthesia for major colorectal and urology cases and provision of emergency anaesthesia.
Carl Ilyas FRCA is a specialty trainee in anaesthesia in the West Yorkshire Deanery who is currently at St James University Hospital, Leeds.
Scott Fortey FANZCA is a consultant at Gosford and Wyong hospitals in the Central Coast Local Health District of NSW, Australia. He is the current chairman of the ANZCA Scholar Role Subcommittee and a member of the ANZCA NSW Regional Committee. His interests include education, quality improvement, and research initiation for new centres.
Matrix codes: 1I05; 2A03; 3A03
References
- 1.NELA Project Team . RCoA; London: 2017. Third Patient Report of the National Emergency Laparotomy Audit.https://www.nela.org.uk/Third-Patient-Audit-Report#pt Available from: (Last accessed 29th January) [Google Scholar]
- 2.Saunders D.I., Murray D., Peden C.J. Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth. 2012;109:368–375. doi: 10.1093/bja/aes165. [DOI] [PubMed] [Google Scholar]
- 3.Anderson I., Eddleston J., Grocott M. Royal College of Surgeons of England; London: 2011. The higher risk general surgical patient: towards improved care for a forgotten group. [Google Scholar]
- 4.Tengberg L.T. Complications after emergency laparotomy beyond the immediate postoperative period — a retrospective, observational cohort study of 1139 patients. Anaesthesia. 2017;72:309–316. doi: 10.1111/anae.13721. [DOI] [PubMed] [Google Scholar]
- 5.Vester-Andersen M., Lundstrøm L.H., Møller M.H. Mortality and postoperative care pathways after emergency gastrointestinal surgery in 2904 patients: a population-based cohort study. Br J Anaesth. 2014;112:60–70. doi: 10.1093/bja/aet487. [DOI] [PubMed] [Google Scholar]
- 6.NCEPOD knowing the risk — a review of the peri-operative care of surgical patients. A report by the National Confidential Enquiry into Patient Outcome and Death. 2011. London, Available from: https://www.ncepod.org.uk/2011report2/downloads/POC_fullreport.pdf. [Google Scholar]
- 7.NELA project team . RCoA; London: 2015. First patient report of the National Emergency Laparotomy Audit. Available from: https://www.nela.org.uk/All-Patient-Reports#pt (Last accessed 31st January 2019) [Google Scholar]
- 8.Rhodes A., Evans L., Alhazzani W. Surviving sepsis Campaign: international guidelines for management of sepsis and septic shock 2016. Crit Care Med. 2017;45:486–552. doi: 10.1097/CCM.0000000000002255. [DOI] [PubMed] [Google Scholar]
- 9.Marik P., Bellomo R. A rational approach to fluid therapy in sepsis. Br J Anaesth. 2016;116:339–349. doi: 10.1093/bja/aev349. [DOI] [PubMed] [Google Scholar]
- 10.Sørensen M.K., Bretlau C., Rasmussen L.S. Rapid sequence induction and intubation with rocuronium–sugammadex compared with succinylcholine: a randomized trial. Br J Anaesth. 2012;108:682–689. doi: 10.1093/bja/aer503. [DOI] [PubMed] [Google Scholar]
- 11.Lewis S.R., Pritchard M.W., Roberts I. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst Rev. 2018;8:CD000567. doi: 10.1002/14651858.CD000567.pub7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grocott M.P.W., Dushianthan A., Rowan K. Perioperative increase in global blood flow to explicit defined goals and outcomes following surgery. Cochrane Database Syst Rev. 2012;11:CD004082. doi: 10.1002/14651858.CD004082.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Neal J., Shaw A. Goal-directed therapy: what we know and what we need to know. Periop Med. 2015;4:1–3. doi: 10.1186/s13741-015-0012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drummond K.E., Murphy E. Minimally invasive cardiac output monitors. Br J Anaesth Educ. 2012;12:5–10. [Google Scholar]
- 15.Eugene N., Cripps M. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: the National Emergency Laparotomy Audit risk model. Br J Anaesth. 2018;4:739–748. doi: 10.1016/j.bja.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 16.Güldner A., Kiss T., Serpa Neto A. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuver. Anesthesiology. 2015;123:692–713. doi: 10.1097/ALN.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 17.Brown C., Deiner S. Perioperative cognitive protection. Br J Anaesth. 2016;117:iii52–iii61. doi: 10.1093/bja/aew361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Niraj G., Kelkar A., Jeyapaln I. Comparison of analgesic efficacy of subcostal transversus abdominus plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66:465–471. doi: 10.1111/j.1365-2044.2011.06700.x. [DOI] [PubMed] [Google Scholar]
- 19.Eipe N., Gupta S., Penning J. Intravenous lidocaine for acute pain: an evidence-based clinical update. BJA Educ. 2016;16:292–298. [Google Scholar]
- 20.Laskowski K., Stirling A., McKay W.P. A systematic review of intravenous ketamine for postoperative analgesia. J Can Anesth. 2011;58:911–923. doi: 10.1007/s12630-011-9560-0. [DOI] [PubMed] [Google Scholar]
- 21.Tsui P.Y., Chu M.C. Ketamine: an old drug revitalized in pain medicine. Br J Anaesth Educ. 2017;17:84–87. [Google Scholar]
- 22.Albrecht E., Kirkham K.R., Brull R. Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia. 2013;68:79–90. doi: 10.1111/j.1365-2044.2012.07335.x. [DOI] [PubMed] [Google Scholar]
- 23.NELA Project Team . RCoA; London: 2018. Fourth Patient Report of the National Emergency Laparotomy Audit. Available from: https://www.nela.org.uk/Fourth-Patient-Audit-Report#pt. [Google Scholar]
- 24.Huddart S., Peden C.J., Swart M. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg. 2015;102:57–66. doi: 10.1002/bjs.9658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tengberg L.T., Bay-Nielsen M., Bisgaard T. Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg. 2017;104:463–471. doi: 10.1002/bjs.10427. [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal G., Peden C., Quiney N. Improving outcomes in emergency general surgery patients: what evidence is out there? Anesth Analg. 2017;125:1403–1405. doi: 10.1213/ANE.0000000000002190. [DOI] [PubMed] [Google Scholar]