Abstract
Background
The surge of coronavirus 2019 (COVID-19) hospitalizations in New York City required rapid discharges to maintain hospital capacity.
Objective
To determine whether lenient provisional discharge guidelines with remote monitoring after discharge resulted in safe discharges home for patients hospitalized with COVID-19 illness.
Design
Retrospective case series
Setting
Tertiary care medical center
Patients
Consecutive adult patients hospitalized with COVID-19 illness between March 26, 2020, and April 8, 2020, with a subset discharged home
Interventions
COVID-19 Discharge Care Program consisting of lenient provisional inpatient discharge criteria and option for daily telephone monitoring for up to 14 days after discharge
Measurements
Fourteen-day emergency department (ED) visits and hospital readmissions
Results
Among 812 patients with COVID-19 illness hospitalized during the study time period, 15.5% died prior to discharge, 24.1% remained hospitalized, 10.0% were discharged to another facility, and 50.4% were discharged home. Characteristics of the 409 patients discharged home were mean (SD) age 57.3 (16.6) years; 245 (59.9%) male; 27 (6.6%) with temperature ≥ 100.4 °F; and 154 (37.7%) with oxygen saturation < 95% on day of discharge. Over 14 days of follow-up, 45 patients (11.0%) returned to the ED, of whom 31 patients (7.6%) were readmitted. Compared to patients not referred, patients referred for remote monitoring had fewer ED visits (8.3% vs 14.1%; OR 0.60, 95% CI 0.31–1.15, p = 0.12) and readmissions (6.9% vs 8.3%; OR 1.15, 95% CI 0.52–2.52, p = 0.73).
Limitations
Single-center study; assignment to remote monitoring was not randomized.
Conclusions
During the COVID-19 surge in New York City, lenient discharge criteria in conjunction with remote monitoring after discharge were associated with a rate of early readmissions after COVID-related hospitalizations that was comparable to the rate of readmissions after other reasons for hospitalization before the COVID pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-020-06340-w.
INTRODUCTION
In March of 2020, the COVID-19 pandemic resulted in a massive surge in hospitalizations across New York City, from one case on March 2 to nearly 30,000 by mid-April 2020.1–4 Limited knowledge about the clinical course of COVID-19 illness contributed to unclear discharge criteria for hospitalized patients.5 At the same time, social distancing policies limited options for usual outpatient follow-up at post-discharge clinic visits or by home-based programs such as visiting nurses. Concerns about these gaps in post-discharge care for patients with COVID-19 illness and an uncertain clinical course had the potential to delay hospital discharges.
In response to this pressing need to maximize hospital capacity through rapid discharges, a multidisciplinary team of clinicians and hospital leaders created a COVID-19 Discharge Care Program consisting of provisional discharge criteria and remote monitoring. At the time, there were few published guidelines for safe discharge parameters for patients hospitalized with COVID-19 illness6 and few known risk factors for readmission.7 The major goals of the COVID-19 Discharge Care Program were to (1) promote a lenient strategy toward discharges; (2) provide monitoring to prevent unnecessary emergency department (ED) visits while fostering early detection of deteriorating patients; (3) support patients’ social and psychological needs; and (4) standardize the care of COVID-19 patients after discharge home. This report describes the characteristics and outcomes of patients discharged home following institution of the COVID-19 Discharge Care Program, which we hypothesized would be associated with a low rate of return to hospital among discharged patients.
METHODS
Patients
The total sample was comprised of consecutive adult patients, excluding those admitted to the obstetric or labor and delivery services, with COVID-19-related illness that were hospitalized at Columbia-New York Presbyterian Hospital (New York, New York) from March 26 to April 8, 2020. COVID-19 status was determined based on a confirmed severe acute respiratory syndrome coronavirus 2 infection by positive result on polymerase chain reaction testing of a nasopharyngeal sample. Clinical outcomes were assessed until April 22, 2020, to allow for 14 days of follow-up on all patients discharged home. The institutional review board of Columbia University Irving Medical Center (CUIMC) approved this case series as minimal-risk research using data collected as part of routine clinical practice and waived the requirement for informed consent.
Interventions
The COVID-19 Discharge Care Program, launched on March 26, consisted of provisional discharge criteria for patients hospitalized with COVID-19 illness and daily telephone monitoring of patients discharged home using a structured protocol. To establish provisional discharge criteria, a multidisciplinary team of hospitalists, primary care providers, pulmonologists, infectious disease experts, and health system leaders came to consensus on provisional discharge criteria (Table 1). Notable components of these criteria included allowance for fever at time of discharge so long as the fever curve was improving and allowance for mild hypoxia so long as the resting oxygen saturation was ≥ 92% on room air at time of discharge. Criteria involving exertional oxygen saturation were not included due to the practical difficulties of exercising patients with COVID-19 illness in the hospital and the lack of evidence demonstrating prognostic significance of exertional desaturation in patients with acute illnesses.8,9 Oxygen saturation was required to be at room air as home oxygen was not readily available during the time period described.
Table 1.
Provisional Criteria for Hospital Discharge to Home for Patients with COVID-19 Illness
| Characteristic | Criteria for discharge to home |
|---|---|
| Vital signs |
• Stable measured respiratory rate (< 20 breaths per minute) • Stable blood pressure • Temperature afebrile or improving fever curve • Resting oxygen saturation ≥ 92% on room air |
| Social considerations |
• Access to resources such as food, pharmacy, and other necessities for daily living • Access to appropriate caregivers if limited ability to engage in self-care • Transmission risk within the home (e.g., the availability of a separate bedroom to minimize sharing of immediate living spaces with others, ability to adhere to home isolation, respiratory and hand hygiene, and the presence of household members at increased risk for COVID-19 complications) |
| Risk enhancers |
• Age ≥ 60 years • Comorbid illnesses (chronic lung disease, heart disease, poorly controlled diabetes mellitus, body mass index (BMI) ≥ 40 kg/m2, chronic kidney disease (stage 3 or higher), immunosuppression—e.g., transplant, other immunosuppression (transplant, other immunosuppressive medications, poorly controlled HIV, malignancy if patient underwent chemotherapy or surgery in the past month) |
All vital sign and social consideration criteria had to be met for patients to qualify for discharge home. Risk enhancers indicated patient characteristics that should be considered when deciding whether to follow the lenient provisional criteria
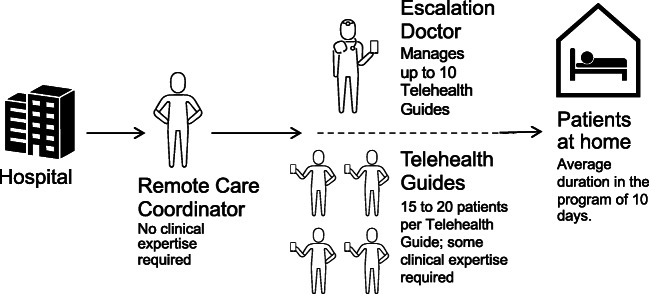
Concurrently, a multidisciplinary team of hospitalists, primary care providers, health system leaders, and experts in human-centered design used an agile process to create the COVID Remote Care Program (Appendix). Inpatient teams were made aware of the eligibility criteria and referral process to this remote monitoring program through communications from hospitalist leadership. Eligibility criteria included age 18 years or older, admitted with COVID-19 illness, discharged home, and capable of being contacted by telephone. Patients admitted to the obstetrics or labor and delivery services and those discharged to home hospice were ineligible. Referrals were made by emailing patient contact information to a Remote Care Coordinator that distributed cases to a team of Telehealth Guides (Fig. 1). Telehealth Guides were expected to have some clinical experience; third- and fourth-year medical students served in this role during the described time period. Telehealth Guides conducted daily telephone calls to discharged patients following a structured assessment tool that investigated COVID-19-related symptoms (cough, shortness of breath, fever) expected to be associated with readmission risk (Appendix). Body temperature, oxygen saturation, and pulse were also monitored if corresponding devices were available in the home. Assessments had the potential to trigger flags that indicated a need for Telehealth Guides to escalate review of patients’ need to return to the hospital with a more experienced clinician, called the Escalation Doctor (Table 2). Escalation Doctors, comprised of general internists, directly contacted flagged patients on a case by case basis, after discussion with the Telehealth Guide. Telehealth Guides were also responsible for screening patients for emotional distress, counseling on self-quarantining, identifying other social or medical needs, and scheduling patients for remote visits with primary care providers or specialists if needed. Examples of actions taken by Telehealth Guides or Escalation Doctors that could have averted returns to the ED included prescribing medications for refractory COVID symptoms, linking patients to community resources for delivery of food or medical supplies, and providing reassurance to those with distressing symptoms. Telehealth Guides followed patients for up to 14 days after discharge with the option of completing follow-up after 7 days if patients had become asymptomatic.
Figure 1.
The COVID Remote Care Program for Patients Discharged Home after Hospitalization for COVID-19 Illness. The Remote Care Coordinator receives patient referrals to the program from the inpatient teams and distributes patients to a team of Telehealth Guides. Telehealth Guides then make daily telephone calls to patients in their home following a structured protocol that includes flags that identify patients potentially at risk for readmission. The Escalation Doctor reviews patients that flag with the Telehealth Guides, and directly contact patients when indicated.
Table 2.
Criteria for Flagging Patients for Escalation During Remote Monitoring of Recently Hospitalized Patients with COVID-19 Illness
| Characteristic | Criteria for flagging patients for escalation during remote monitoring |
|---|---|
| Symptoms |
• New or worsening shortness of breath with light activities • New or worsening cough • New or worsening subjective fever (if no thermometer available) |
| Vital signs |
• Temperature ≥ 100.4 °F (if thermometer available) • O2 saturation < 95% (if pulse oximeter available) • Pulse ≥ 110 beats per minute (if pulse oximeter available) |
| Other reasons | • At discretion of the Telehealth Guide. Examples of other reasons included other concerning signs (e.g., low blood pressure) or symptoms (e.g., syncope, chest pain, severe anxiety), prescribing needs, and assistance with organizing home care and specialty referrals |
Measurements
Patient sociodemographic, medical characteristics, and clinical outcomes including discharge disposition, and 14-day ED visits, readmissions, and mortality were extracted from the CUIMC data warehouse. Race and ethnicity were self-reported by patients. Vital signs were extracted from the last recorded vital signs prior to discharge. Symptoms of new or worsening cough, new or worsening shortness of breath with light activities, subjective or objectively measured fever, oxygen saturation, and pulse (if devices available) were assessesed daily by the Telehealth Guides. Emotional distress was assessed 1 week after discharge using the validated Generalized Anxiety Disorder-2 item (GAD-2)10 and the Patient Health Questionnaire-2 item (PHQ-2).11 Loneliness was assessed using a single item that asked patients how often they felt lonely since returning from the hospital (“not at all” to “nearly every day”).12 Patient satisfaction with remote monitoring was assessed at the completion of the program by asking patients how likely they would be to recommend the program to other patients who had been hospitalized with COVID-19 illness (0, not at all likely; 10, extremely likely).
Statistical analysis
Descriptive statistics were used to describe patient characteristics and clinical outcomes. Gradual diffusion of information about the remote monitoring program led to incomplete uptake in its first 2 weeks and created an opportunity to compare patients who were and were not referred. Chi-squared and Mann–Whitney U tests were used to compare characteristics of discharged patients who were and were not referred for remote monitoring. Logistic regression models were applied to estimate the associations between remote monitoring and two binary outcomes: return to the ED and readmission. In addition to the multivariable analysis that adjusted for potentially confounding factors (demographics, comorbidities, vital signs at discharge), inverse probability weighting (IPW) based on propensity score was used. Conventional covariate adjustment using a multivariable regression model may yield biased estimation when the functional form of the outcome model is unspecified; applying IPW can be more robust in this case. The individual propensities for being referred for remote monitoring were estimated based on a logistic regression model. The predicted probabilities from the propensity score model were used to calculate the stabilized IPW weight. To control for potential confounding that was not fully addressed after weighting, we fitted multivariable logistic regression models concurrently adjusting for IPW and covariates. Analyses were performed using SAS 9.4 (Cary, NC) and R (version 3.6.1). The significance threshold was 0.05 and two-side p values are reported.
Role of the Funding Source
Individual authors received support from the National Institutes of Health, Agency for Healthcare Research and Quality, and the Health Resources and Services Administration. None of the funders had a role in the conduct or interpretation of the study.
RESULTS
Between March 26 and April 8, 812 patients were hospitalized with COVID-19 illness (mean age 63 years, 60.6% male). Of these patients, 15.5% died in hospital, 24.1% remained hospitalized, 5.0% were discharged to a skilled nursing facility or nursing home, 4.9% were discharged to hospice, and 50.4% were discharged home.
Patients who were discharged home had a mean age of 57 years, 59.9% were men, 51.1% were Hispanic, and 22.8% were Black (Table 3). The most common comorbidities were hypertension (39.1%) and diabetes (26.2%). Consistent with the lenient discharge criteria, a substantial proportion of patients that were discharged home had abnormal vital signs on the day of discharge. Specifically, 6.6% had a last recorded temperature ≥ 100.4 °F, 23.5% had a respiratory rate ≥ 20 breaths per minute, 11.0% had a pulse ≥ 100 beats per minute, and 37.7% had an oxygen saturation < 95%. Furthermore, a substantial number of patients were discharged home even though the last recorded vital sign did not meet the lenient discharge criteria (i.e., respiratory rate ≥ 20 breaths per minute, 23.5%; pulse ≥ 110 beats per minute, 2.4%; oxygen saturation < 92%, 4.2%).
Table 3.
Characteristics of Patients Hospitalized with COVID-19 Illness
| Characteristic | All hospitalized patients (N = 812) | Patients discharged home (N = 409) | Patients readmitted after discharge home (N = 31) |
|---|---|---|---|
| Age, years | 62.8 ± 16.9 | 57.3 ± 16.6 | 66.3 ± 19.3 |
| Male sex | 492 (60.6%) | 245 (59.9%) | 19 (61.3%) |
| Race | |||
| White | 161 (19.8%) | 80 (19.6%) | 7 (22.6%) |
| Black | 185 (22.8%) | 95 (23.2%) | 4 (12.9%) |
| Other | 264 (32.5%) | 139 (34.0%) | 13 (41.9%) |
| Unknown | 202 (24.9%) | 95 (23.2%) | 7 (22.6%) |
| Ethnicity | |||
| Hispanic | 409 (50.4%) | 209 (51.1%) | 21 (67.7%) |
| Non-Hispanic | 195 (24.0%) | 93 (22.7%) | 6 (19.4%) |
| Unknown | 208 (25.6%) | 107 (26.2%) | 4 (12.9%) |
| Comorbidities | |||
| Hypertension | 363 (44.7%) | 160 (39.1%) | 21 (67.7%) |
| Diabetes | 277 (34.1%) | 107 (26.2%) | 10 (32.3%) |
| Coronary artery disease | 159 (19.6%) | 61 (14.9%) | 10 (32.3%) |
| Chronic lung disease | 134 (16.5%) | 64 (15.7%) | 6 (19.4%) |
| Heart failure | 114 (14.0%) | 39 (9.5%) | 6 (19.4%) |
| Chronic kidney disease | 149 (18.4%) | 58 (14.2%) | 12 (38.7%) |
| Body mass index*, kg/m2 | |||
| <30 | 368 (58.7%) | 186 (59.1%) | 20 (64.5%) |
| 30–40 | 203 (32.4%) | 102 (32.4%) | 10 (32.3%) |
| >40 | 56 (8.9%) | 27 (8.6%) | 1 (3.2%) |
| Invasive mechanical ventilation | 98 (12.1%) | 0 | 0 |
| Vitals on discharge | |||
| Temperature, °F | – | 98.7 ± 1.0 | 99.0 ± 1.2 |
| < 100.4 | – | 382 (93.4%) | 27 (87.1%) |
| ≥ 100.4 | – | 27 (6.6%) | 4 (12.9%) |
| Systolic blood pressure, mmHg | – | 123.2 ± 17.3 | 123.4 ± 19.1 |
| Diastolic blood pressure, mmHg | – | 74.7 ± 9.2 | 72.6 ± 8.5 |
| Respiratory rate, breaths per minute | – | 18.4 ± 2.0 | 18.4 ± 1.7 |
| < 20 | – | 313 (76.5%) | 23 (74.2%) |
| ≥ 20 | – | 96 (23.5%) | 8 (25.8%) |
| Pulse, beats per minute | – | 83.2 ± 16.0 | 85.5 ± 13.7 |
| < 100 | – | 364 (89.0%) | 25 (80.7%) |
| 100–110 | – | 35 (8.6%) | 4 (12.9%) |
| ≥ 110 | – | 10 (2.4%) | 2 (6.5%) |
| Oxygen saturation (room air), % | – | 95.2 ± 2.3 | 95.5 ± 2.4 |
| < 92 | – | 17 (4.2%) | 1 (3.2%) |
| 92–94 | – | 137 (33.5%) | 8 (25.8%) |
| 95–96 | – | 136 (33.3%) | 12 (38.7%) |
| ≥ 97 | – | 119 (29.1%) | 10 (32.3%) |
Data are presented as mean ± standard deviation or as N (%). Chronic lung disease was defined as any of the following: asthma, chronic obstructive pulmonary disease, emphysema, chronic bronchitis, or interstitial lung disease. Invasive mechanical ventilation was defined as being placed on a ventilator at any time during hospital admission.
*Data were missing on body mass index for 185 patients
Among the 409 patients that were discharged home after initiating the COVID Discharge Care Program, 45 patients (11.0%) returned to the ED within 14 days, and of these, 31 patients (7.6%) were readmitted. Seven patients (1.7%) died in hospital after being readmitted. The median [IQR] days to readmission was 4 [3, 7], range 0–14 days. Compared to patients that were discharged home but not readmitted, patients who were readmitted were significantly older (66.3 years vs 56.6 years, p = 0.002), more likely to have hypertension (67.7% vs 36.8%, p < 0.001), chronic kidney disease (38.7% vs 12.2%, p < 0.001), coronary artery disease (32.3% vs 13.5%, p = 0.01), and heart failure (19.4% vs 8.7%, p = 0.10), but not diabetes (32.3% vs 25.7%, p = 0.42) or chronic lung disease (19.4% vs 15.3%, p = 0.61). There were no differences in day of discharge body temperature (99.0 °F vs 98.7 °F, p = 0.32), respiratory rate (18.4 vs 18.4, p = 0.56), pulse (85.5 vs 83.0, p = 0.30), or oxygen saturation (95.5% vs 95.2%, p = 0.58) between those who were and were not readmitted, respectively.
Of the 409 patients discharged home, 217 patients (53.1%) were referred for remote monitoring (41.3% of all discharges in week 1 and 64.4% of all discharges in week 2). Patients discharged home with a referral for remote monitoring were similar to those who were discharged without such a referral, but had lower rates of hypertension, diabetes, and chronic kidney disease; longer length of stay during the index hospitalization; and lower oxygen saturation at discharge (Table 4).
Table 4.
Characteristics of Patients Discharged Home, With and Without Referral to Remote Monitoring Program
| Characteristic | Patients discharged home with remote monitoring (N = 217) | Patients discharged home without remote monitoring (N = 192) | p value |
|---|---|---|---|
| Age, years | 56.7 ± 15.2 | 58.0 ± 18.0 | 0.40 |
| Male sex | 137 (63.1%) | 108 (56.3%) | 0.16 |
| Race | 0.48 | ||
| White | 39 (18.0%) | 41 (21.4%) | |
| Black | 46 (21.2%) | 49 (25.5%) | |
| Other | 79 (36.4%) | 60 (31.3%) | |
| Unknown | 53 (24.4%) | 42 (21.9%) | |
| Ethnicity | 0.81 | ||
| Hispanic | 111 (51.2%) | 98 (51.0%) | |
| Non-Hispanic | 47 (21.7%) | 46 (24.0%) | |
| Unknown | 59 (27.2%) | 48 (25.0%) | |
| Comorbidities | |||
| Hypertension | 73 (33.6%) | 87 (45.3%) | 0.02 |
| Diabetes | 47 (21.7%) | 60 (31.3%) | 0.03 |
| Chronic lung disease | 34 (15.7%) | 30 (15.6%) | 0.99 |
| Coronary artery disease | 31 (14.3%) | 30 (15.6%) | 0.70 |
| Chronic kidney disease | 19 (8.8%) | 39 (20.3%) | < .001 |
| Heart failure | 19 (8.8%) | 20 (10.4%) | 0.57 |
| Body mass index, kg/m2 | 30.1 ± 7.3 | 29.6 ± 6.4 | 0.64 |
| Vitals on discharge | |||
| Temperature | 98.6 ± 1.0 | 98.8 ± 1.0 | 0.01 |
| < 100.4 °F | 204 (94.0%) | 178 (92.7%) | |
| ≥ 100.4 °F | 13 (6.0%) | 14 (7.3%) | |
| Systolic blood pressure, mmHg | 122.6 ± 16.9 | 123.9 ± 17.8 | 0.45 |
| Diastolic blood pressure, mmHg | 74.9 ± 8.8 | 74.4 ± 9.6 | 0.80 |
| Respiratory rate, breaths per minute | 18.5 ± 2.1 | 18.4 ± 1.8 | 0.65 |
| < 20 | 163 (75.1%) | 150 (78.1%) | |
| ≥ 20 | 54 (24.9%) | 42 (21.9%) | |
| Pulse, beats per min | 82.1 ± 13.8 | 84.4 ± 18.0 | 0.21 |
| < 100 | 196 (90.3%) | 168 (87.5%) | |
| 100–110 | 17 (7.8%) | 18 (9.4%) | |
| ≥ 110 | 4 (1.8%) | 6 (3.1%) | |
| Oxygen saturation at room air, mean ± SD, % | 95.0 ± 2.3 | 95.5 ± 2.3 | 0.05 |
| < 92% | 9 (4.2%) | 8 (4.2%) | |
| 92–94% | 79 (36.4%) | 58 (30.2%) | |
| 95–96% | 71 (32.7%) | 65 (33.9%) | |
| ≥ 97% | 58 (26.7%) | 61 (31.8%) | |
| Length of stay for index hospitalization, days | 5.0 ± 3.9 | 4.2 ± 3.2 | 0.05 |
| 14-day readmission | 15 (6.9%) | 16 (8.3%) | 0.59 |
| 14-day emergency department visit | 18 (8.3%) | 27 (14.1%) | 0.06 |
| 14-day mortality (all in hospital) | 3 (1.4%) | 4 (2.1%) | 0.59 |
Data are presented as mean ± standard deviation or as N (%).Chronic lung disease was defined as any of the following: asthma, chronic obstructive pulmonary disease, emphysema, chronic bronchitis, or interstitial lung disease
The majority of patients referred for remote monitoring (86.2%) completed at least one call with the Telehealth Guide. Reasons for not completing any calls included inability to contact (11.0%), completed early due to improved health (0.9%), readmitted before first call (0.5%), and declined to participate (1.4%). Among patients who completed at least one call, the median [IQR] number of calls completed per patient was 4 [3, 5] and the median [IQR] duration of follow-up was 5 [4, 7] days. Reasons for completing fewer phone calls than expected included challenges reaching patients by telephone, patients declining daily phone calls, or patients returning to the ED early. Overall, 1406 calls were completed, of which 7.9% were associated with at least 1 flag, relevant to 28.1% of all patients. The most common reasons for flags pertained to new or worsening cough (2.8%), new or worsening shortness of breath (2.2%), oxygen saturation < 95% (1.9%), and new or increased fever (1.6%). While the number of times Escalation Doctors directly contacted patients was not tracked, this occurred for a minority of flagged Telehealth Guide encounters.
Emotional distress questionnaires were completed by 90 patients. A substantial percentage of patients did not complete these assessments as they were scheduled on days calls were not completed. Among patients that completed the questionnaires, 12.4% screened positive for anxiety (GAD-2 ≥ 3), 7.9% screened positive for depression (PHQ2 ≥ 3) and 11.1% were lonely on more than half the days since discharge. Of 105 patients that completed a program satisfaction question, 86.7% reported they would be very likely to recommend the monitoring program to others (score of 9 or 10), 10.5% scored the program a 7 or 8, and 2.8% scored the program < 7.
There was a trend toward a lower percentage of patients with an ED visit within 14 days of discharge in patients that were referred to remote monitoring versus those not referred (8.3% vs 14.1%, p = 0.06; Table 4). Among patients referred for remote monitoring, 61.1% (11 of 18) of those with an ED visit were flagged by one or more escalation criteria. There were no significant differences in the percentage of patients referred versus not referred that were readmitted (6.9% vs 8.3%, p = 0.59) or that died (1.4% vs 2.1%, p = 0.59) within 14 days. In the unweighted, multivariable analysis, remote monitoring was associated with a decreased risk of an ED visit (OR 0.63, 95% CI 0.32–1.24, p = 0.18) and an increased risk of readmission (OR 1.29, 95% CI 0.55–3.01, p = 0.56), but these differences were not statistically significant. In the main IPW analysis, remote monitoring was similarly associated with risk of returning to hospital (OR 0.60, 95% CI 0.31–1.15, p = 0.12) and risk of readmission (OR 1.15, 95% CI 0.52–2.52, p = 0.73). No covariates were significantly associated with return to the ED or readmission in these models (data not shown).
DISCUSSION
The implementation of a COVID-19 Discharge Care Program consisting of lenient discharge criteria and remote telephone monitoring after discharge was associated with a low rate of 14-day readmission and mortality. To our knowledge, this study represents one of the first case series of patients with COVID-19 illness that reports on follow-up after discharge. While the rate of readmission in this sample was higher than that found in another recent case series of patients from New York, our sample was followed for 14 days after discharge, whereas the prior study had a mean follow-up of only 3 days.13 The 14-day readmission rate was similar to the readmission rate for other common reasons for hospitalization.14 Accordingly, the discharge criteria used in this program, which were substantially more lenient than those used by the National Health Commission of China,6 appeared to be safe with respect to readmissions and mortality.
The remote monitoring component of the COVID-19 Discharge Care Program was associated with rapid uptake by inpatient teams, with two thirds of discharged patients referred to the program by its second week. There was also a high rate of participation by patients, with less than 2% declining remote follow-up. A bigger challenge was having accurate contact information for patients, of particular relevance in our socioeconomically diverse patient population. Though the program was designed to provide patients with phone calls on at least 7 days after discharge, a lower number of phone calls were typically completed. Patients that participated rated the remote monitoring program highly, suggesting it may be an important part of a patient-centered approach to post-discharge care in patients hospitalized with COVID-19 illness. While referral to remote monitoring was not associated with a statistically significant reduction in 14-day readmissions, referral was associated with a trend toward an approximately 40% reduction in patients returning for an ED visit. This reduction in return visits to the hospital may be particularly important in the context of new surges in COVID-19 infections that arise when social distancing measures are relaxed.15,16
Though results were only available for a subset of patients that participated in remote monitoring, only about 1 in 10 surveyed patients screened positive for anxiety, depression, and loneliness in the week after discharge. This is one of the first studies to assess mental health outcomes in patients discharged home after COVID-19 hospitalization. For context, prior studies suggest that at least 20% of patients have elevated anxiety and depressive symptoms after hospitalizations for pneumonia and acute coronary syndromes.17,18
Limitations
There were several limitations to our study. First, the study evaluated patients hospitalized at a single hospital in New York City, and home oxygen was not available during the study period, limiting generalizability. Second, data on readmissions and mortality were missing for patients that had events occur outside the health system. Third, the follow-up period was limited to 14 days after discharge. Fourth, less than half of patients were referred for remote monitoring, likely due to incomplete dissemination of the referral process to busy inpatient providers during the roll-out of the program. Fifth, even among patients referred to the program, there were incomplete responses to emotional assessments such that data on mental health screening should be interpreted cautiously. Further, mental health assessments were made by Telehealth Guides, which may have led to underreporting on mood questionnaires. Sixth, comparisons between patients who were and were not referred for remote monitoring should be interpreted cautiously given differences in patient characteristics between members of these groups and the lack of randomization; nevertheless, we sought to control for these differences by incorporating covariates and IPW into multivariable analyses. Seventh, some patients may have been discharged without meeting the lenient discharge criteria; nevertheless, these criteria were not intended to replace clinical judgment of inpatient teams and chart extraction from flowsheets may have missed vital sign data recorded elsewhere in the medical record. Finally, while older age and comorbidities were associated with readmission risk on bivariate analyses, too few patients had early readmissions to reliably identify predictors of these adverse outcomes; future studies should re-examine these predictors as outcomes accrue.
Conclusions
A COVID-19 Discharge Care Program comprised of lenient discharge criteria and post-discharge remote monitoring via telephone was associated with a low rate of readmissions and high patient satisfaction. Other health systems may wish to create similar programs, particularly when surges in the volume of patients hospitalized with COVID-19 illness outpace hospital capacity.
Supplementary Information
(DOCX 1317 kb)
Acknowledgments
The authors wish to acknowledge the dedication, commitment, and sacrifice of the staff, providers, and personnel at our institutions through the local COVID crisis and the suffering, loss, and resilience of our patients, their families, and our community.
Author Contributions
Dr. Kronish had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Kronish, Moise
Acquisition, analysis, or interpretation of data: All authors
Drafting of the manuscript: Kronish
Critical revision of the manuscript for important intellectual content: All authors
Statistical analysis: Kronish, Hiura, Sun
Obtained funding: Not applicable
Administrative, technical, or material support: Kronish
Supervision: Kronish
Funding
Dr. Kronish received support from the National Heart, Lung, and Blood Institute (NHLBI, R01-HL123368, and R01-HL117832) and the Agency for Healthcare Research and Quality (AHRQ, R01-HS024262). Mr. Hiura and Dr. Sun received support from NHLBI (R01-HL093081, R01-HL077612, and R01-HL121270). Dr. Liyanage-Don received support from the Health Resources and Services Administration (T32-HP10260). Dr. Moise received support from NHLBI (R01-HL141609) and AHRQ (R01-HS025198).
Compliance with Ethical Standards
The institutional review board of Columbia University Irving Medical Center (CUIMC) approved this case series as minimal-risk research using data collected as part of routine clinical practice and waived the requirement for informed consent.
Conflict of Interest
Dr. Geleris reports non-financial support from Allergan Inc, Alexion Pharmaceuticals, Inc, Boehringer Inhelheim Pharmaceuticals, Inc, Jansen Pharmaceuticals, Inc, Pfizer, Inc, outside the submitted work.
Footnotes
Key Points
Question: What are the short-term outcomes of patients hospitalized with coronavirus 19 (COVID-19) that are discharged home following the institution of lenient discharge criteria in conjunction with a remote monitoring program after discharge?
Findings: In this case series that included 812 consecutive patients hospitalized at a hospital in New York City, 7.6% of the 409 patients discharged home were readmitted within 14 days. The remote monitoring component of the program consisting of daily telephone surveillance of patients discharged home was associated with high patient satisfaction, a lower rate of return to the emergency department, and fewer 14-day readmissions, though these differences were not statistically significant.
Meaning: Lenient discharge criteria that allow patients with fever and mild hypoxia to be discharged home with remote monitoring after discharge can be safely used as an approach to maximizing hospital capacity during surges in COVID-19 infections.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Goldstein J, McKinley J. Coronavirus in N.Y.: Manhattan woman is first confirmed case in state. The New York Times. March 1, 2020. Accessed March 30, 2020. https://www.nytimes.com/2020/03/01/nyregion/new-york-coronvirus-confirmed.html
- 2.New York City Department of Health and Mental Hygiene. Coronavirus disease 2019 (COVID-19) - daily data summary. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-daily-data-summary-hospitalizations-04152020-1.pdf. Updated April 14, 2020. Accessed April 14, 2020.
- 3.Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). COVID-19 dashboard: coronavirus COVID-19 global cases. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Updated March 30, 2020. Accessed March 30, 2020.
- 4.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hupert N, Horn EM, Martinez FJ, Gulick RM, Safford MM. Clinical characteristics of COVID-19 in New York City. N Engl J Med. 2020;382:2372–2374. [DOI] [PMC free article] [PubMed]
- 5.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7(1):4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang X, Xu H, Jiang H, et al. Follow-up study of 131 COVID-19 discharged patients: is the current Chinese discharge criteria reliable? Preprint at: https://ssrn.com/abstract=3551342. Posted March 18, 2020.
- 8.Hardinge M, Annandale J, Bourne S, et al. British Thoracic Society guidelines for home oxygen use in adults. Thorax. 2015;70(Suppl 1):i1–43. doi: 10.1136/thoraxjnl-2015-206865. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs SS, Lederer DJ, Garvey CM, et al. Optimizing home oxygen therapy. an official American Thoracic Society Workshop report. Ann Am Thorac Soc. 2018;15(12):1369–1381. doi: 10.1513/AnnalsATS.201809-627WS. [DOI] [PubMed] [Google Scholar]
- 10.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 12.Gruenewald TL, Crosswell AD, Epel E, et al. Measures of stress in the Health and Retirement Study (HRS) and the HRS family of studies: user guide. https://164f89be-6459-4649-bea5-b3d3fcc248ee.filesusr.com/ugd/890fda_66d3318e858045559cfd85cccbd92724.pdf. Updated April 2020. Accessed April 14, 2020.
- 13.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. [DOI] [PMC free article] [PubMed]
- 14.Lindenauer PK, Rothberg MB, Pekow PS, Kenwood C, Benjamin EM, Auerbach AD. Outcomes of care by hospitalists, general internists, and family physicians. N Engl J Med. 2007;357(25):2589–2600. doi: 10.1056/NEJMsa067735. [DOI] [PubMed] [Google Scholar]
- 15.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. [DOI] [PMC free article] [PubMed]
- 16.Vahidy FS, Drews AL, Masud FN, et al. Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area. JAMA;324:998–1000. [DOI] [PMC free article] [PubMed]
- 17.Davydow DS, Hough CL, Levine DA, Langa KM, Iwashyna TJ. Functional disability, cognitive impairment, and depression after hospitalization for pneumonia. Am J Med. 2013;126(7):615-624.e615. doi: 10.1016/j.amjmed.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen BE, Edmondson D, Kronish IM. State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28(11):1295–1302. doi: 10.1093/ajh/hpv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 1317 kb)