SUMMARY
This study was carried out to determine the prevalence of falls, their etiology and risk factors in neurological patients admitted to the hospital in northern Turkey. A cross-sectional, descriptive design was used. Data were collected by survey that identified socio-demographic and clinical features of the subjects, Hendrich II fall risk model and Berg Balance Scale (BBS). Study results revealed approximately one-third of the study patients (33.1%) to have sustained falls before. Concerning the timing of falls, 24.9% of these incidents had occurred within the last year. The most common reason for falling was dizziness (14.3%). The mean score on the Hendrich II fall risk model was 2.7±0.1 for those who had fallen and 2.3±0.1 for those who had not fallen. The respective mean BBS score was 20.7±1.9 and 18.4±1.3. It was found that approximately one-third of neurological patients had fallen before and had restricted their activities due to fear of falls; the great majority of them had a chronic disease and permanently used medicines; and the most important risk factors for falls were advanced age, fear of falls and impaired balance.
Key words: Balance, Etiology, Fall, Neurology, Prevalence, Prevention, Risk
Introduction
Falls are common health problems, which might result in significant injuries and complications in health care settings, extend hospitalization, decrease functional capacity of patients and increase health care costs (1). Giles et al. report that falls were the most common critical event reported in inpatients that led to tragic outcomes affecting mortality and morbidity (2). A previous research found that accidental falls in inpatients caused serious injuries and complications (1). Falls might be affected by various factors in inpatients. Healey reports that falls among inpatients were caused by a combination of many risk factors involving acute diseases and long-term effects of these diseases, the process of aging, and adverse effects of medication and hospital environment unfamiliar to patients (3). Lovallo et al. report that the majority of patients were exposed to many risk factors and therefore they would probably experience falls, while the nature and prevalence of these factors varied in different hospitalized groups (4). In another study, it was found that the fall risk profiles of inpatients varied when compared to those in the community; that hospital setting was much different from house setting; and that inpatients were generally more frail due to hospitalization (2).
Previous studies on falls report that neurological patients had a high risk of falling (5), and that falls were more prevalent in neurological services (6, 7). Hunderfund et al. found the rate of falls in neurology departments to be 5.69 per 1000 patients/day, with neurological inpatients to have a high percentage of falls (8). Albernaz and Dos Santos Cabral report that 32.5% of their study participants had fallen before; 60% of them fell accidentally, 20% fell due to neurological disorder and another 20% due to vestibular disorder, while 40% had neurological disorder and vertigo. They also report that vertigo, imbalance and dizziness were very common in individuals with neurological disorder (9). Stolze et al. found falls in neurological patients to be linked with disorders affecting gait and balance and use of medication (10).
Aim
There is a lack of epidemiological data on falls concerning risk factors and characteristics of neurological patients that affect proneness to falls among neurological patients in northern Turkey. This situation stimulated our embarking upon this study. The present study aimed to determine the prevalence of falls, their etiology and risk factors in neurological patients admitted to the hospital. The research was expected to answer the following questions:
What is the prevalence of falls, their etiology and risk factors among neurological patients?
What is the balance status among neurological patients?
What characteristics of neurological patients affect the fall situation?
Patients and Methods
Study design and sampling method
A cross-sectional, descriptive design was used to determine the prevalence of falls, their etiology and risk factors in neurological patients. It was carried out at a hospital neurology department between May 20, 2011 and April 30, 2012 in Samsun province in northern Turkey. A total of 534 patients were admitted to the department as inpatients during the study. The authors aimed to recruit the entire population of patients admitted to the hospital neurology service due to various neurological problems. However, patients who were not willing to participate in the study (n=24), who failed to complete the questionnaire and did not respond clearly to the questions (n=12), and who were unconscious (n=253) were excluded. The study included 245 patients who gave their consent to take part in the study. The response rate was 45.9%. All subjects were able to answer the questions independently and had no memory problems.
The sample criteria were as follows: age ≥18 years; admission to the neurology department as inpatients; being able to communicate verbally with us; being able to understand the study and provide their informed consent; not taking any psychiatric drugs that would affect his/her mental status; not being too confused to complete the questionnaire; and being able to read and write, a literacy level education. Exclusion criteria were as follows: bedridden and unconscious patients; mental or legal incapacity to provide an informed consent; having communication difficulties (inability to speak) or cognitive impairment; terminal illness; and history of illness or a condition that would affect balance test (e.g., disability).
Procedures
Data were collected via a questionnaire prepared by the researchers to determine the patient socio-demographic and clinical specifications, in addition to the Hendrich II fall risk model and the Berg Balance Scale (BBS). The study commenced upon approval granted by the Hospital Scientific Committee. The study followed the principles of the Declaration of Helsinki. We obtained consent from each study participant. This process was carried out in a separate room by the researchers. In the data collection phase, the aims of the research were explained to the patients and their willingness to participate was ensured. Before data collection, the questionnaire was tested in a pilot study on a group of 10 patients. The response and practice time was estimated to 25-30 min.
Instruments
Data were collected using a questionnaire. The first part of the questionnaire contained 30 questions on the patient socio-demographic characteristics, clinical characteristics, and fall characteristics (e.g., status of having fear of falling, the place where they mostly have fear of falling, taking precautions against falling at home, conditions of restricting activities due to fear of falling, condition of experiencing falling incident before, fall time, when the fall occurred, hours of falling, the place where the incident of falling occurred, reasons for falling, states aftermath falling, and number of falling incidents).
Socio-demographic factors collected in the study included age, gender, marital status, education level, family type (large or nuclear), and living arrangements (living with a spouse, family member, or alone). In this study, a city referred to an urban area that was the largest residential area. A town referred to a semi-urban area with an approximate population of 5,000 to 10,000 people. A village was a rural area with an approximate population of 2,000 to 3,000 people. The sample was stratified by age (40-51, 52-63, 64-75, and 76-88 years). Sex was coded as male or female. Marital status was married or single. The study grouped educational levels as literate, elementary school, secondary school, high school, and university.
Clinical characteristics and health behaviors included any chronic illnesses, previous hospitalizations, having a sensory disorder (yes/no), and type of sensory disorders (visual or auditory). Researchers asked about the subject perception of health. Respondents rated their own current health as good, fair, or poor. Data were also collected using the Hendrich II fall risk model and BBS.
Hendrich II Fall Risk Model
The Hendrich II fall risk model is fast to administer and provides determination of the risk of falling (11, 12). The validity and reliability of the Hendrich II fall risk model were tested for Turkish samples by Atay et al. in 2009 (13). They assessed data using appropriate statistical methods and found the kappa values obtained for the first seven items on the scale to range from 0.77 to 1.00. The Spearman’s rho value obtained for the eighth item, related to standing up and walking, was 0.91. The reliability of the Turkish version of the Hendrich II fall risk model was found to be acceptably high in their study (13). In our study, the alpha coefficient for patients was 0.79.
Berg Balance Scale
Balance was measured using the BBS (14, 15). The validity and reliability of the BBS were tested for Turkish samples by Sahin et al. in 2008. In their research, internal consistency (Cronbach’s alpha) of the BBS total score was calculated as 0.93 (16). In our study, the alpha coefficient for patients was 0.85.
Data analysis
On data evaluation, percentage calculation, one-way ANOVA, Student’s t-test, Pearson correlation analysis, and logistic regression analysis were used.
Results
Sample characteristics
Study results revealed that 37.6% of the subjects were 64-75 years of age; 53.9% were female and 46.1% were male; 86.1% were married; 58.8% were literate; 62.0% had income less than expenses; 90.2% did not work; 70.2% had a nuclear family; 97.6% had social security; 35.5% lived with a spouse; and 49.8% lived in a city (Table 1).
Table 1. Demographic characteristics of patients (N=245).
| Characteristic | n | % |
|---|---|---|
| Age group (years) | 66.5±0.9 | |
| 40-51 | 28 | 11.4 |
| 52-63 | 48 | 19.6 |
| 64-75 | 92 | 37.6 |
| 76-88 | 77 | 31.4 |
| Gender | ||
| Female | 132 | 53.9 |
| Male | 113 | 46.1 |
| Marital status | ||
| Married | 211 | 86.1 |
| Single | 34 | 13.9 |
| Education | ||
| Literate | 144 | 58.8 |
| Primary school | 60 | 24.5 |
| Secondary school | 14 | 5.7 |
| High school | 21 | 8.6 |
| University | 6 | 2.4 |
| Socioeconomic status | ||
| Income less than expenses | 152 | 62.0 |
| Income equal to expenses | 85 | 34.7 |
| Income more than expenses | 8 | 3.3 |
| Working status | ||
| Yes | 24 | 9.8 |
| No | 221 | 90.2 |
| Family type | ||
| Large | 73 | 29.8 |
| Nucleus | 172 | 70.2 |
| Social security | ||
| Present | 239 | 97.6 |
| Absent | 6 | 2.4 |
| Living with | ||
| Spouse | 87 | 35.5 |
| Spouse and children | 73 | 29.8 |
| Children | 72 | 29.4 |
| No one | 13 | 5.3 |
| Place of residence | ||
| City | 122 | 49.8 |
| Town | 63 | 25.7 |
| Village | 60 | 24.5 |
Clinical characteristics
In this study, 75.5% of patients reported that their health condition was fair; 89.8% had chronic disease; 20.4% had diabetes: 46.5% had hypertension disease; 83.3% had been previously hospitalized; 29.4% had a sensory disorder: 21.2% had a visual disorder; and 89.8% used maintenance medicines for chronic diseases (Table 2).
Table 2. Clinical characteristics of patients (N=245).
| Characteristic | n | % |
|---|---|---|
| Type of neurological disorder | ||
| Cerebrovascular disease | 168 | 68.6 |
| Vertigo | 22 | 9.0 |
| Epilepsy | 11 | 4.5 |
| Headache | 9 | 3.7 |
| Alzheimer’s disease | 9 | 3.7 |
| Multiple sclerosis | 7 | 2.8 |
| Dementia | 16 | 6.5 |
| Parkinson’s disease | 3 | 1.2 |
| Perceived health | ||
| Good | 33 | 13.5 |
| Fair | 185 | 75.5 |
| Poor | 27 | 11.0 |
| Chronic disease condition | ||
| Yes | 220 | 89.8 |
| No | 25 | 10.2 |
| *Has chronic illness | ||
| Hypertension | 114 | 46.5 |
| Diabetes | 50 | 20.4 |
| Coronary arterial disease | 17 | 6.9 |
| Renal failure | 3 | 1.2 |
| Asthma | 8 | 3.3 |
| Chronic obstructive pulmonary disease | 12 | 4.9 |
| Others | 8 | 3.3 |
| Previous hospitalization | ||
| Yes | 204 | 83.3 |
| No | 41 | 16.7 |
| Status of heaving sensory disorder | ||
| Yes | 72 | 29.4 |
| No | 173 | 70.6 |
| *Sensory disorders (n=72) | ||
| Visual | 52 | 21.2 |
| Auditory | 11 | 4.5 |
| Visual-auditory | 9 | 3.7 |
| Status of using continuous medicine | ||
| Yes | 220 | 89.8 |
| No | 25 | 10.2 |
*More than one answer given.
Falling status among neurological patients
Study results showed that 32.2% of study patients had a fear of falling, mostly while having bath; 72.2% took precautions against falling at home; 14.3% restricted their activities because they were afraid of falling; and 33.1% had fallen during the previous three years. For the falls, 24.9% of the falling incidents occurred in the last year, 21.6% of the falling incidents occurred at daytime and 12.2% occurred in the afternoon. The most common reason for falling was dizziness (14.3%) and 7.3% had a lesion after falling (Table 3).
Table 3. Distribution of patient features according to falling incidents (N=245).
| Characteristic | n | % |
|---|---|---|
| Having fear of falling | ||
| Yes | 79 | 32.2 |
| No | 166 | 67.8 |
| *The place where patients mostly had fear of falling (n=79) | ||
| While going downstairs | 27 | 11.0 |
| While having bath | 39 | 15.9 |
| Other | 18 | 7.3 |
| Taking precaution against falling at home | ||
| Yes | 177 | 72.2 |
| No | 68 | 27.8 |
| *Precautions taken against falling at home (n=177) | ||
| Grab irons on the stairs | 153 | 62.4 |
| Grab irons in the bathroom and toilet | 3 | 1.2 |
| Smooth floor surface | 21 | 8.6 |
| Anti-skid matting in the bathroom | 60 | 24.5 |
| Restricting activities due to fear of falling | ||
| Yes | 35 | 14.3 |
| No | 210 | 85.7 |
| Having experienced falling incident before | ||
| Yes | 81 | 33.1 |
| No | 164 | 66.9 |
| Fall time (n=81) | ||
| Night | 28 | 11.4 |
| Daytime | 53 | 21.6 |
| When the fall occurred? (n=81) | ||
| Last year | 61 | 24.9 |
| 1 year ago | 4 | 1.6 |
| 2 years ago | 8 | 3.3 |
| 3 years ago | 8 | 3.2 |
| *Hours of falling (n=81) | ||
| Getting up in the morning | 5 | 2.0 |
| Before noon | 26 | 10.6 |
| Afternoon | 30 | 12.2 |
| Evening | 19 | 7.8 |
| At night | 10 | 4.1 |
| *The place where the falling incident occurred (n=81) | ||
| On the street | 15 | 6.1 |
| In the room | 48 | 19.6 |
| In the bathroom | 13 | 5.3 |
| In the toilet | 12 | 4.9 |
| On the stairs at home | 3 | 1.2 |
| On the stairs outside home | 4 | 1.6 |
| *Reason for falling (n=81) | ||
| Dizziness | 35 | 14.3 |
| Stumbling | 13 | 5.3 |
| Imbalance | 17 | 6.9 |
| Gait and balance disorder | 15 | 6.1 |
| Wet floor | 4 | 1.6 |
| Movement and strength problems | 7 | 2.8 |
| State aftermath falling (n=81) | ||
| Lesion | 18 | 7.3 |
| Laceration | 4 | 1.6 |
| Fracture | 6 | 2.4 |
| Hematoma | 4 | 1.6 |
| Nothing | 49 | 20.0 |
| Average of falling incident | 1.4±.1 | |
*More than one answer given.
Balance status and falling risk among neurological patients
In the present study, 11.4% of neurological patients had a high risk of falling. The mean score on the Hendrich II fall risk model was 2.4±0.1. The mean score on the Hendrich II fall risk model was 2.7±0.1 for those who had fallen and 2.3±0.1 for those who had not fallen, yielding no statistically significant difference between the two groups (t=1.590, p=0.116). The mean score on the BBS among all neurological patients was 19.2±1.1, with 89.0% scoring ≤45 points. The mean BBS score was 20.7±1.9 for those who had fallen and 18.4±1.3 for those who had not fallen, thus yielding no statistically significant difference between the two groups (t=1.027, p=0.308) (Fig. 1).
Fig. 1.
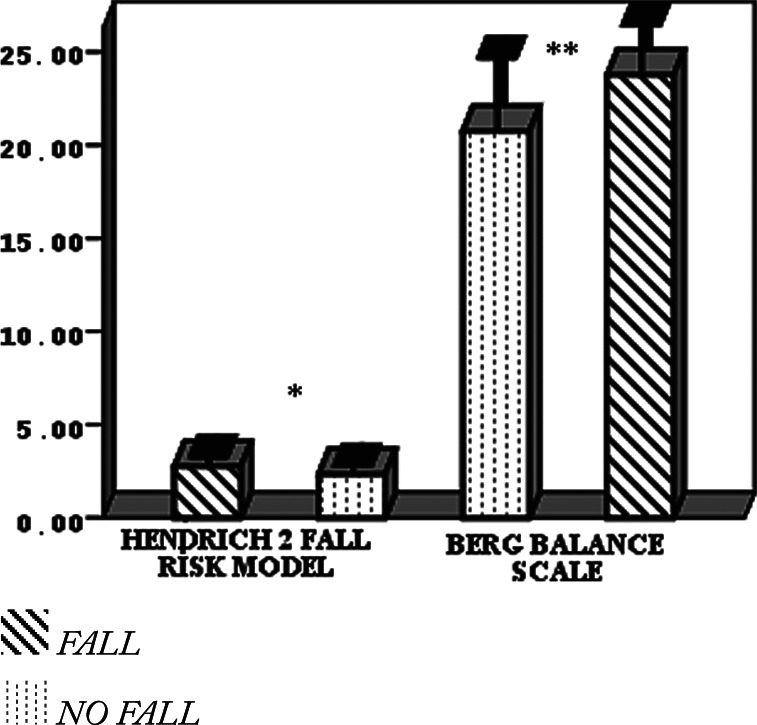
Distribution of total score of Hendrich II fall risk model and Berg balance scale of patients with and without falls (*t=1.590, p=0.116; **t=1.027, p=0.308).
Logistic regression analysis was performed to determine some risk factors affecting falls in neurological patients. Logistic regression analysis showed that the model accurately estimated the risk of falls at 88.2% and each increase in age unit increased the risk of falls (p=0.000); the residence unit where the patients lived had a significant impact on the risk of falls, and compared to the patients living in villages, those living in town districts had a 7.9-fold higher risk of falling; the state of health perception also affected falls (p=0.001); compared to the patients with negative perception of health, the risk of falls was 0.09 times higher in those with good health perception; it was 0.08 times higher in those with moderate level of health perception and 0.18 times higher in those with fear of falling (p=0.013). Logistic regression analysis showed that the model accurately estimated balance risk in 89.0% and that like in falls, each increase in age unit affected balance and increased the risk of falls (p=0.000) (Table 4).
Table 4. Some risk factors affecting the status of falls and balance and odds ratio.
| Risk factor | Hendrich II fall risk model | Berg balance scale | ||
|---|---|---|---|---|
| Odds ratio (95% confidence interval) | p | Odds ratio (95% confidence interval) | p | |
| Age | 1.111 (1.052-1.172) |
0.000 | 0.922 (0.887-0.958) |
0.000 |
| Gender | ||||
| Female | 0.450 (0.175-1.157) |
0.097 | 0.831 (0.331-2.087) |
0.694 |
| Male | 2.00 | 2.00 | ||
| Place of residence | 0.015 | |||
| City | 2.917 (0.761-11.190) |
0.119 | 3.895 (0.772-19.653) |
0.100 |
| Town | 7.972 (1.868-34.027) |
0.005 | 2.342 (0.382-14.378) |
0.358 |
| Village | 3.00 | 3.00 | ||
| Perceived health | 0.001 | |||
| Good | 0.096 (0.014-0.664) |
0.018 | 3.421 (0.560-20.886) |
0.183 |
| Fair | 0.086 (0.024-0.313) |
0.000 | 0.883 (0.157-4.968) |
0.888 |
| Poor | 3.00 | 3.00 | ||
| Status of having fear of falling | ||||
| Yes | 0.189 (0.051-0.700) |
0.013 | 0.821 (0.296-2.282) |
0.706 |
| No | 2.00 | 2.00 | ||
Discussion
Although it has been reported that falls in inpatients cause serious injuries and complications (1), it was found that the literature contained a limited number of research on the prevalence of risk factors and diagnosis of falls (8, 10, 17). This study will contribute to understanding the prevalence, etiology and risk factors in neurological patients in northern Turkey and help develop appropriate guidelines to reduce patient falls.
In the present study, it was found that 11.4% of neurological patients had a high risk of falling. Lovallo et al. report that 29.69% of patients had the risk of falling; 70.31% had no risk of falling; neurology department ranked third in the prevalence of falls (18.6%) following oncology (35.6%) and rehabilitation (20.3%) departments (4). Other studies found that neurological patients had a risk of falling (8); when compared to other services, the rate of fall cases was higher in neurology services (5-7). As indicated in the literature, arrangements in interior structure of hospitals (5) and implementation of programs to prevent falls and injuries is of great importance to reduce falls among neurological patients (5, 6).
In the present study, the majority (89.8%) of patients had a chronic disease, particularly hypertension and diabetes, and they were taking medication for their chronic diseases regularly. Similarly, Özden et al. report that patients had chronic diseases, mainly hypertension, coronary artery disease, diabetes mellitus (83.7%, 41.8% and 28.3%, respectively) and that almost all of them (94.6%) used medication (18). Stolze et al. report that antidepressants, antihypertensives, diuretics and digitalis are risk factors for falls (10). Results of the present study suggest that, considering that the majority of neurological patients had chronic diseases and used medication for these diseases, these patients should be closely monitored for the risk of falling and adverse effects of medicines.
It was found that approximately one-third of the study patients (33.1%) had fallen during the previous three years. Previous studies determining falls in neurological patients report that fall prevalence varied between 7.2% and 89.2% (1, 9, 10, 18-20). On the other hand, comparison of our findings with those of other studies with similar research methodology showed the prevalence of falls in neurological patients to be higher in other studies (10, 18, 19); however, in some other studies, the prevalence of falls was lower as compared with our study (9, 20).
We found that falls occurred mostly in rooms (19.6%) and that the most significant cause of falls was dizziness (14.3%). On the other hand, other studies found that falls generally occurred inside houses (10, 18, 19), outside (10), in other buildings (10), in the street (18), in patient bathroom (7), toilet (18), corridor (18); and that they had fallen due to wet floor (10), poor lighting (10), inadequate shoes (10), walking bare foot (10), slippery ground (7, 10), posture and gait disorders (10), malfunction of wheelchair (18), fainting (7), and vertigo (9). Similar to these findings, previous studies report that falls occurred mostly in patient rooms (1, 6, 7, 18) and that the most important causes of falling were loss of balance and dizziness (7, 9, 18). Albernaz and Dos Santos Cabral report that neurological patients experienced loss of balance and dizziness very often, therefore falls were frequent among them (9).
In the present study, lesion, fracture, laceration and hematoma occurred in patients after falling (7.3%, 2.4%, 1.6% and 1.6%, respectively). Although types and rates of injuries after falling showed variation in other studies, fractures (10, 18), contusions (6, 10), soft tissue damage (10), trauma (6), abrasion (6), laceration (6, 18), head injury (6, 18) and chest trauma (18) occurred after falling.
In the present study, the most important risk factors for falls were age, status of balance and fear of falling. In another study that determined the prevalence, etiology and risk factors for falls it was found that factors such as old age (8, 10, 18, 19), stroke (21), dementia (21), Parkinson’s disease (21), peripheral neuropathy (21), depression (19), vertigo and dizziness (8, 9), posture disorders (10), gait disorders (8, 10, 18, 19, 21), balance disorders (8-10, 18, 19, 21), history of the last fall (8, 18, 21), fear of falls (10), use of psychotropic medication (8), antidepressant treatment (10), neuroepileptics (10), cardiovascular medicines (10), use of antihypertensive medicines (18), change in the level of consciousness (18), adverse environmental factors in patient house (10), use of walking aids (10, 21), lower extremity weakness (21), muscle weakness (8), use of inappropriate walking aid (19), sensory losses (21), problems in bowel and bladder movements (8), and significant loss of vision (8, 18, 21) increased the risk of falls in neurological patients. Although the prevalence, etiology and risk factors in neurological patients varied, we believe that this variation might have resulted from research methodology, socio-demographic and clinical characteristics of the study groups.
We found that patients feared of falls mostly while taking bath; they restricted their movements due to this fear and the rate of falls was increased 0.18 times in those that had fear of falls. In previous studies, 10.9% of falls occurred in the bathroom (7); fear of falls was an intrinsic risk factor for falls (10); and fear of falls might cause reluctance in daily life activities of patients (1).
In the present study, it was found that falls mostly occurred during the day and in the afternoon. On the other hand, Hitcho et al. report that 58.5% of falls occurred between 7 p.m. and 6 a.m. (7). The fact that falls occurred during the day might result from meeting personal care needs when they are more active. The fact that previous studies found that falls mostly occurred at night might result from problems of patients due to bowel and bladder movements (8), or they wanted to use bathroom. Lovallo et al. report that 32.2% of falls occurred at night and 34% occurred on their way to bathroom; accordingly, going to toilette was a significant risk factor for falls (4).
Logistic regression analysis performed to determine some risk factors affecting falls of patients revealed the risk of falls to have increased in patients who felt fear of falls and at each age unit increase. Similar to our findings, previous studies have reported that age (10, 18, 22) and fear of falls (10) were important risk factors affecting falls. Giles et al. conducted logistic regression analysis and report that confusion, incontinence, mediation, movement and sleep disorders were significant risk factors affecting patient safety among inpatients (2).
It was found that like in falls, each unit increase of age affected status of balance and increased the risk of falls. Some of the studies report that loss of balance (8-10, 18, 21), vertigo (23) and gait disorder were the most important risk factors in neurological patients, while many risk factors for falls such as gait and balance problems can be modified (24). Morse reports that due to iatrogenic nature of hospital settings, they are risky places for patients in terms of falls, injuries and deaths, and that health care professionals are responsible for taking protective and preventive measures to eliminate and reduce these risks (25). As indicated in the literature, considering each etiologic target in hospitals, it is of great importance to understand the use of fall preventive principles and to implement them comprehensively and systematically.
Comparison of the risk profiles of inpatients with those in the society showed variations; hospital environment was found to be much different from home environment, inpatients were generally more frail due to hospitalization, and therefore the measures to reduce falls in hospitalized subjects should be different from those in home setting (2). In this context, since the present study was carried out in neurological inpatients, it cannot be generalized to different neurological patients in the community. For this reason, future studies should be planned to include neurological patients in the community, as indicated in the literature (17); studies should be conducted in individuals with special neurological conditions that might affect gait, movement and balance.
Conclusions
It was found that approximately one-third of neurological patients had fallen before and they restricted their activities due to fear of falls; in addition, the great majority of them had a chronic disease and permanently used medicines; the most important risk factors for falls were age, fear of falls and balance disorder. Based on these findings, health care professionals are suggested to diagnose fall risk factors with comprehensive assessment (including chronic diseases, medicines, functional condition, house safety, etc.) to reduce the risk of falls, upgrade patient safety and increase mobility of neurological patients. Nurses are recommended to diagnose the risk of falls in all inpatients and to make assessments using fast, easy and practical monitoring tools to reduce and prevent falls in neurological patients. In addition, as indicated in the literature, we suggest the use of exercise programs for balance training (17). On the other hand, it is of great importance to organize training programs for patients, health care providers and health care professionals to prevent falls.
Acknowledgment
We would like to thank the elderly for taking part in this study.
References
- 1.Schwendimann R. Patient Falls: a Key Issue in Patient Safety in Hospitals. Zürich: Basel University, 2006, doi: 10.5451/unibas-004036746 [DOI] [Google Scholar]
- 2.Giles LC, Whitehead CH, Jeffers L, McErlean B, Thompson D, Crotty M. Falls in hospitalized patients. Comput Inform Nurs. 2006;24(3):167–72. 10.1097/00024665-200605000-00014 [DOI] [PubMed] [Google Scholar]
- 3.Healey F. A guide on how to prevent falls and injury in hospital. Nurs Older People. 2010;22(9):16–22. 10.7748/nop2010.11.22.9.16.c8060 [DOI] [PubMed] [Google Scholar]
- 4.Lovallo C, Rolandi S, Rossetti AM, Lusignani M. Accidental falls in hospital inpatients: evaluation of sensitivity and specificity of two risk assessment tools. J Adv Nurs. 2010;66(3):690–6. 10.1111/j.1365-2648.2009.05231.x [DOI] [PubMed] [Google Scholar]
- 5.Diccini S, Gomes de Pinho P, Oliveira da Silva F. Assessment of risk and incidence of falls in neurosurgical inpatients. Rev Lat Am Enfermagem. 2008;16(4):752–7. 10.1590/S0104-11692008000400016 [DOI] [PubMed] [Google Scholar]
- 6.Rohde JM, Myers AH, Vlahov D. Variation in risk for falls by clinical department: implications for prevention. Infect Control Hosp Epidemiol. 1990;11(10):521–4. 10.2307/30151319 [DOI] [PubMed] [Google Scholar]
- 7.Hitcho EB, Krauss M, Brige S, Dunagan WC, Fischer I, Johnson S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732–9. 10.1111/j.1525-1497.2004.30387.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hunderfund ANL, Sweeney CM, Mandrekar JN, Johnson LM, Britton JW. Effect of multidisciplanary fall risk assessment on falls among neurology inpatients. Mayo Clin Proc. 2011;86(1):19–24. 10.4065/mcp.2010.0441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albernaz PLM, Dos Santos Cabral FS. Vertigo and dizziness in elderly patients with neurological disorders. Einstein (Sao Paulo). 2011;9(4):466–9. 10.1590/s1679-45082011ao2131 [DOI] [PubMed] [Google Scholar]
- 10.Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G. Falls in frequent neurological diseases – prevalence, risk factors and aetiology. J Neurol. 2004;251(1):79–84. 10.1007/s00415-004-0276-8 [DOI] [PubMed] [Google Scholar]
- 11.Hendrich AL, Bender PS, Nyhuis A. Validation of the Hendrich II fall risk model: a large concurrent case/control study of hospitalized patients. Appl Nurs Res. 2003;16(1):9–21. 10.1053/apnr.2003.016009 [DOI] [PubMed] [Google Scholar]
- 12.Hendrich A. How to try this: predicting patient falls. Using the Hendrich II fall risk model in clinical practice. Am J Nurs. 2007;107(11):50–8. 10.1097/01.NAJ.0000298062.27349.8e [DOI] [PubMed] [Google Scholar]
- 13.Atay S, San AT, Aycan Ö. Validity and reliability study of Hendrich II Fall Risk Model. 12th National Nursing Congress, 20-24 October, 2009, pp. 217-8; Sivas (in Turkish). [Google Scholar]
- 14.Berg K, Wood-Dauphinee S, Williams JI, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304–11. 10.3138/ptc.41.6.304 [DOI] [Google Scholar]
- 15.Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg balance scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88(4):449–59. 10.2522/ptj.20070251 [DOI] [PubMed] [Google Scholar]
- 16.Sahin F, Yılmaz F, Ozmaden A, Kotevoglu N, Sahin T, Kuran B. Reliability and validity of the Turkish version of the Berg Balance Scale. J Geriatr Phys Ther. 2008;31(1):32–7. 10.1519/00139143-200831010-00006 [DOI] [PubMed] [Google Scholar]
- 17.Thurman DJ, Stevens JA, Rao JK. Practice parameter: assessing patients in a neurology practice for risk of falls (an evidence-based review). Neurology. 2008;70(6):473–9. 10.1212/01.wnl.0000299085.18976.20 [DOI] [PubMed] [Google Scholar]
- 18.Özden D, Karagözoğlu Ş, Kurukız S. Determination of fall risk according to Hendrich II and Morse Fall Scale: a pilot study. Anadolu Hemşirelik ve Sağlık Bilimleri Dergisi. 2012;15(1):80–8. [in Turkish] [Google Scholar]
- 19.Soyuer F, Ünalan D, Erdoğan F. The prevalence and risk factors of fall of the patients applying to the Department of Neurology in Erciyes University Medical Faculty. Turk Noroloji Dergisi. 2006;12(4):269–74. [in Turkish] [Google Scholar]
- 20.Savcı C, Kaya H, Acaroğlu R, Kaya N, Bilir A, Kahraman H, et al. The determination of patients’ falling risk and taken preventive measures in neurology and neurosurgery clinics. Maltepe Üniversitesi Hemşirelik Bilim ve Sanatı Dergisi. 2009;2(3):19–25. [in Turkish] [Google Scholar]
- 21.American Academy of Neurology. AAN Summary of Evidence Based Guideline for Clinicians, 2008. Assessing patients in a neurology practice for risk of falls. [cited 2012 September 11]. Available from: www.aan.com.
- 22.Nakai A, Akeda M, Kawabata I. Incidence and risk factors for inpatient falls in an academic acute-care hospital. J Nippon Med Sch. 2006;73(5):265–70. 10.1272/jnms.73.265 [DOI] [PubMed] [Google Scholar]
- 23.Moylan KC, Binder EF. Falls in older adults: risk assessment, management, and prevention. Am J Med. 2007;120(6):493.e1–7.e6. 10.1016/j.amjmed.2006.07.022 [DOI] [PubMed] [Google Scholar]
- 24.Matejcic A, Bekavac-Belin M, Ivica M, Tomljenovic M, Krolo I, Vucetic B. Fractures of the proximal femur in the elderly. Acta Clin Croat. 2002;41:15–23. [Google Scholar]
- 25.Morse JM. Enhancing the safety of hospitalization by reducing patient falls. Am J Infect Control. 2002;30(6):376–80. 10.1067/mic.2002.125808 [DOI] [PubMed] [Google Scholar]


