Abstract
Background In March 2020, the COVID-19 pandemic led to a national lockdown and quarantine in Italy. The aim of this study was to assess the perceived change in anxiety levels and its predictors in a non-clinical, non-infected, home-quarantined Italian sample in the very first weeks of the lockdown. Methods Online survey data on perceived change in anxiety symptoms since the beginning of the lockdown, health anxiety, social anxiety, depression, and obsessive-compulsive symptomatology before the lockdown, and background information were anonymously collected between March 26 and April 9 2020 on 660 Italian participants. Results Overall, participants reported a substantial increase of anxiety levels. Women reported more increased levels of anxiety symptoms than men. Increase of anxiety was also predicted by higher pre-existing levels of health anxiety and lower socio-economic status. Having lost the job was not associated with a perceived change in anxiety levels. Limitations Crosssectional design; sample of mostly female, young, highly educated, and not infected participants; use of self-report measures. Conclusions The results suggest the need to address mental health issues as a core element of the response to a pandemic, in order to prevent long-term social, psychological, and economic costs to society.
Keywords: COVID-19, Pandemics, Anxiety, Health anxiety, Mental health, Quarantine
1. Introduction
The COVID-19 (SARS-CoV-2) disease is an infectious disease caused by a coronavirus, whose most common symptoms are fever, dry cough, fatigue, shortness of breath, and loss of smell and taste. While it can be often treated at home like a common flu, in some cases there might be severe complications, such as acute respiratory distress syndrome, that can cause death (World Health Organization [WHO], 2020a,b). This disease was unknown before December 2019, when an outbreak began in Wuhan, China. Being an airborne disease, it quickly spread worldwide, and the WHO declared it a pandemic on March 11, 2020. The rapid increase of cases in Northern Italy during the last week of February 2020 lead to quarantine two main regions and on March 8 the Prime Minister announced that the quarantine was extended nationwide. This decision imposed the lockdown of all businesses and activities that were not supplying basic goods and services. The population was forced to stay at home. Going outside was permitted for essential workers and necessary errands . Being the Italian national health care system open and free to everyone, the access to hospitals was regulated in order to prioritize the patients in most critical conditions that required urgent treatments, and the availability of intensive care beds soon showed to be inadequate.
At the end of March 2020, in Italy there were more than 100,000 confirmed cases and more than 10,000 deaths. During the early days of the pandemic, Italian news reported almost exclusively pandemic-related information, such as the high risk of contagion, the deadliness of the disease, the difficulties of the national and local governments in dealing with it, and nobody knew when the emergency, and, consequently, the lockdown would have ended. As pointed out by Wheaton et al. (2012), such media attention can be a double-edged sword, as the information about the risks of infection can promote healthy behaviors and reduce the spread of contagion, but it can lead to mass hysteria and fear, too. In March 2020, surveys (e.g. Nielsen, 2020) revealed that the situation in Italy was highly stressful for the whole population, as people became increasingly worried not only for their health and for their loved ones, but also for their jobs and finances. We thus hypothesized that these circumstances could lead to an increase in anxiety symptoms.
Anxiety can be defined as "an emotion characterized by apprehension and somatic symptoms of tension in which an individual anticipates impending danger, catastrophe, or misfortune" (American Psychological Association [APA], 2020). During a pandemic these symptoms may exacerbate. As reported by Rubin et al. (2009), one in four Britons reported a significant increase in anxiety during the 2009 H1N1 influenza outbreak. Other studies on the effects of pandemics on anxiety have reported that higher levels of anxiety are predicted by health anxiety (i.e., a form of anxiety that leads to interpret bodily sensations and changes as indicative of a disease (Taylor and Asmundson, 2004), to an overestimation of the likelihood of being infected, and to an inflated perception of the negative consequences of having a severe illness (Wheaton et al., 2010), contamination cognition, the tendency to exaggerate the likelihood and severity of contamination and to excessively monitor physical reactions, disgust sensitivity, and obsessive-compulsive symptoms or beliefs (Brand et al., 2013; Wheaton et al., 2012). The psychological consequences of pandemics can also be related to post-traumatic stress disorder (PTSD) and depression (e.g., Hawryluck et al., 2004).
A major role in developing a psychological distress during a pandemic is thought to be played by being quarantined (but see Wang et al., 2011). A review by Brooks et al. (2020) pointed out that the negative psychological effects of quarantine included PTSD symptoms, confusion, and anger, while risk factors were quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. However, most of the studies reviewed enrolled health care workers, undergraduates, or infected individuals, and only a minority included the general population. The differences in sampling strategies, in the data collected, in the country where the study was performed, and in the specific pandemic considered make it hard to find conclusive results.
The investigation of the predictors of change in anxiety symptoms in quarantined individuals can be useful to understand the roots of the distress and the functional impairment that may occur in these circumstances. Previous studies (e.g., Wheaton et al., 2012) showed that one key factor is health anxiety. While moderate degrees of health anxiety are adaptive, excessive levels are not, as they can impair psychological, social, and occupational functioning, and lead to needless utilization of health care services (Asmundson and Taylor, 2007). As the COVID-19 is a highly contagious virus, the experts and the mass-media insistently recommended frequent hand washing and use of disinfectants to prevent infection. Such recommendations, however, might trigger fears of contamination comparable to the ones typically observed in individuals with obsessive-compulsive disorder (OCD), which can cause an overestimation of the likelihood of being contaminated and the dangerousness of the disease itself (Wheaton et al., 2012).
The aim of this study was to investigate the perceived change in anxiety symptoms and its predictors in the very first weeks of a quarantine in a non-clinical, non-infected sample (i.e., participants that did not report any COVID-19 symptoms at the time of the study). Most previous studies focused on quarantined individuals that had been infected or had a concrete possibility to have been infected. In these cases increased levels of anxiety can be expected mainly due to a higher perceived likelihood to be infected. Conversely, in this study we enrolled non-infected participants and administered them a questionnaire in order to investigate the predictive power of retrospectively rated levels of specific forms of anxiety (i.e., health anxiety, contamination fears, social anxiety), other dimensions of OCD, and depression, on the perceived change in anxiety levels during the quarantine, while controlling for background variables and exposure to infected individuals.
2. Method
2.1. Participants and procedure
A link to an online survey was sent to a list of 800 Italian adult personal and work contacts of the authors. Between March 26 and April 9, 2020, 755 participants anonymously accessed the survey, 95 of which reported not to have answered honestly to all questions. Their data was not used in subsequent analyses, which were performed on a sample of 660 participants (Table 1 ). The research was conducted in accordance with the Helsinki Declaration.
Table 1.
Descriptive statistics of the variables considered in this study, bivariate associations of Beck Anxiety Inventory (BAI) scores with the other variables (in r metric), and results of the general linear model (GLM) analysis predicting BAI scores. (in r metric). More details about these analyses are reported in the Supplementary Materials.
| Variable | Statistic | Bivariate association coefficient | GLM effect size / EMMs |
|---|---|---|---|
| Gender identified with (N (%)) | −.11** [−.19; −.03] | −.11** [−.18; −.03] | |
| Male | 87 (13.18%) | 0.10 [0.00; 0.21]b | |
| Female | 569 (86.21%) | 0.25 [0.20; 0.30]a | |
| Missing | 4 (0.61%) | ||
| Age (years; M ± SD, range) | 31.08 ± 10.30 (18; 79) | −.15*** [−.23; −.08] | −.03 [−.11; .05] |
| Education (completed years; M ± SD, range) | 15.44 ± 3.14 (5; 21) | −.01 [−.09; .06] | |
| Socioeconomic status (M ± SD, range)° | 5.88 ± 1.66 (1; 10) | −.10* [−.18; −.02] | −.09* [−.17; −.01] |
| Relationship status (N (%)) | .13** [.04; .20]^ | .05 [.00; .12] | |
| No relationship | 173 (26.21%) | 0.16 [0.07; 0.24]a | |
| Stable relationship, no cohabiting | 224 (33.94%) | 0.22 [0.13; 0.30]a | |
| Living with partner / spouse | 263 (39.85%) | 0.16 [0.07; 0.24]a | |
| Occupational status during quarantine (N (%))° | .19*** [.08; .24]^ | .15* [.00; .21] | |
| Working as before | 51 (7.73%) | 0.22 [0.08; 0.35]ab | |
| Working from home | 166 (25.15%) | 0.24 [0.15; 0.32]a | |
| Forced to take time off | 62 (9.39%) | 0.27 [0.15; 0.40]a | |
| Unemployement insurance | 56 (8.48%) | 0.11 [-0.02; 0.23]ab | |
| Lost work | 32 (4.85%) | −0.03 [-0.20; 0.14]b | |
| Student | 216 (32.73%) | 0.26 [0.18; 0.34]a | |
| Not working nor studying | 77 (11.67%) | 0.17 [0.05; 0.29]ab | |
| People living with (N (%)) | |||
| Parents | 299 (45.30%) | .14*** [.06; .21] | .02 [−.06; .10] |
| Children | 123 (18.64%) | −.03 [−.11; .04] | |
| Partner | 263 (39.85%) | NCa | |
| Relations | 72 (10.91%) | .03 [−.05; .11] | |
| Friends | 7 (1.06%) | NC | |
| Flatmates | 26 (3.94%) | .03 [−.05; .10] | |
| Nobody | 50 (7.58%) | −.05 [−.13; .03] | |
| Infected by Covid-19 (N (%)) | NC | ||
| No | 653 (98.94%) | ||
| Yes | 7 (1.06%) | ||
| Severity of infection (N (%))a | NC | ||
| Asymptomatic | 1 (0.15%) | ||
| Weak symptoms | 5 (0.76%) | ||
| Moderate symptoms | 1 (0.15%) | ||
| People participant knows having being infected by Covid-19 (N (%))^ | |||
| Nobody | 277 (41.97%) | −.01 [−.08; .07] | |
| Partner | 3 (0.45%) | NCb | |
| Parent | 7 (1.06%) | NCb | |
| Child | 1 (0.15%) | NCb | |
| Sibling | 1 (0.15%) | NCb | |
| Relation | 30 (4.55%) | .07 [−.00; .15] | |
| Friend | 85 (12.88%) | −.04 [−.12; .03] | |
| Colleague | 49 (7.42%) | −.00 [−.08; .08] | |
| Acquaintance | 312 (47.27%) | .05 [−.02; .13] | |
| Psychological measures (M ± SD, range, omega) | |||
| CES-D | 1.87 ± 0.61 (1.00; 4.00), .89 | .08* [.00; .16] | −.03 [−.11; .04] |
| SAM | 2.05 ± 0.57 (1.00; 3.86),.93 | .06 [−.02; .14] | |
| HAS | 1.67 ± 0.53 (1.00; 3.67),.96 | .18*** [.11; .25] | .13*** [.06; .21] |
| OCI-Checking | 0.60 ± 0.72 (1.00; 5.00),.83 | .07 [−.00; .15] | |
| OCI-Washing | 0.37 ± 0.61 (1.00; 5.00),.78 | .04 [−.04; .11] | |
| OCI-Ordering | 0.89 ± 0.92 (1.00; 5.00),.89 | .03 [−.05; .11] | |
| OCI-Obsessing | 1.04 ± 1.03 (1.00; 5.00),.92 | .11** [.03; .19] | .03 [−.05; .10] |
| OCI-Neutralizing | 0.28 ± 0.58 (1.00; 5.00),.88 | −.02 [−.09; .06] | |
| OCI-Hoarding | 0.98 ± 0.89 (1.00; 5.00),.87 | .09* [.02; .17] | .04 [−.04; .12] |
| BAI | 0.26 ± 0.48 (-2.00; 1.95),.95 |
Note: ***: p < .001; **: p < .01; *: p < .05; N: observed count; %: percentage on the total (660); M: mean; SD: standard deviation; °: measured using Adler et al. (2000) subjective socioeconomic status scale
: not considered since redundant with the information in the relationship status variable
: not computed due to the low frequency of "yes" responses; omega: McDonald (1999) reliability index; unless otherwise specified, bivariate association coefficients are Pearson's rs with their 95% confidence interval [CI]; ^ square root of the eta-squared with its 95% CI; GLM effect sizes: General Linear Model effect sizes, that are the square root of eta-squareds (categorical predictors) or the partial correlations (metric predictors) along with their 95%CI; indented italicized values are Estimated Marginal Means (EMMs) with their 95% CI; the compact letter display notation has been used to highlight significant post-hoc tests for categorical predictors.
2.2. Measures
Participants were initially presented with a question that showed an informed consent form and asked whether they had read it and voluntary confirmed their willingness to participate. If they answered positively, they could access the questionnaires, that were presented in randomized order and included the Health Anxiety questionnaire (HAQ, Lucock and Morley, 1996), a newly developed social anxiety inventory (SAI; Author, in preparation), and the short versions of the Center for Epidemiologic Studies Depression Scale (CES-D; Andresen et al., 1994) and of the Obsessive–Compulsive Inventory (OCI; Foa et al., 2002). For these questionnaires, participants were asked to answer thinking about how they felt before the quarantine. Then they were presented with the Beck Anxiety Inventory (BAI, Beck et al., 1988) and asked to report if and how each symptom had changed since the beginning of the quarantine (-2= Much decreased, -1=A bit decreased, 0=Unchanged, +1=A bit increased, +2=Much increased). More details about these measures are reported in Section 1 of the Supplementary Materials (SM1). A form collecting background and exposure information was then administered (Table 1). Finally, participants were asked whether they answered carefully and honestly to all questions and were presented with a note on the final page that thanked them for participating and provided debriefing information and contact details for queries about the survey.
3. Results
Seven cases were excluded from the analyses as they reported being infected by the COVID-19. The BAI mean change score was significantly higher than 0, with a moderate effect size (one-sample t-test: t(652)=14.17, p < .001, d = 0.55 [0.47;0.63]), suggesting that participants perceived an increased level of anxiety. We performed the same analysis on item scores and those who showed a strong (d>|0.80|) increase were item5 ("Fear of worst happening"), item10 ("Nervous"), and item17 ("Scared") (Fig. 1 ).
Fig. 1.
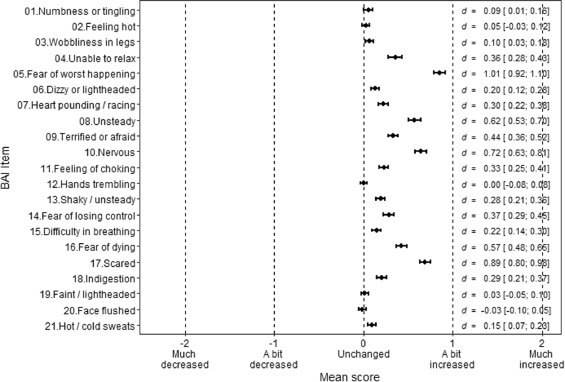
Mean change scores of Beck Anxiety Inventory items and their effect size (difference from zero).
We then computed bivariate associations of BAI scores with the other variables, and found that they were significantly associated with gender, age, relationship status, socioeconomic status (SES), occupational status during quarantine, living with parents, depression, health anxiety, obsessing, and hoarding (Table 1; SM2). These variables were subsequently entered as predictors in a general linear model predicting BAI scores. Results showed that women reported a higher increase in anxiety levels than men. While in all categories of occupation an increase in anxiety was observed, participants who lost their job did not report a significant change. The increase in anxiety was also predicted by higher levels of health anxiety and by lower levels of SES (Table 1; SM3).
4. Discussion
This study aimed at assessing the perceived change in anxiety symptoms and its predictors in a non-clinical and non-infected Italian sample in the very first weeks of the COVID-19 quarantine. Measuring the extent of this phenomenon and investigating the factors that contribute to it are useful in understanding how the population responds to large scale illness threats. While we were finalizing this manuscript, the WHO (2020b) published a document that reported an increase in symptoms of depression and anxiety in several countries, especially in women. The results of this study are consistent with those ones, as we found a substantial increase in anxiety that was higher in women. We also observed that a perceived increase in anxiety was significantly predicted by higher levels of health anxiety and lower levels of SES. Both results are consistent with previous studies. Health anxiety depends on how likely and how severe a feared illness is perceived to be (Wheaton et al., 2010), and a media portrayal of the COVID-19 as an easily communicable virus possibly induced a perception of a high likelihood of exposure and of becoming infected. The daily press conferences of health authorities reporting the count of new cases and deaths could also have contributed to an increase in health anxiety, and consequently, in anxiety symptoms. A few previous studies found that lower SES predicted higher anxiety (e.g., Mwinyi et al., 2017), and speculated that low SES may, in a vicious circle, contribute to an increase in anxiety. Although the cross-sectional design used here does not allow causal inferences, this result could be ascribed to several factors, potentially stressful and threatening in this situation, such as: have to face a lower income or a wider economic crisis; a perceived decreased possibility of receiving proper treatments in case of infection; having an inadequate living space where to spend the quarantine. However, having lost a job was not associated with a perceived change in anxiety symptoms: it is possible that some people felt relieved not to have to deal with the uncertainty of losing their job, and/or felt safer having the possibility of staying at home.
This work has some limitations. First, the generalizability of the results, since participants were recruited among the personal contacts of the authors. Although we sought to sample a group of participants as much diverse as possible in terms of background variables, they were mostly females, young, and highly educated. Second, the use of self-report measures might have caused an inflation of the relationships between study variables due to common method variance. Third, recall bias might have influenced the scores on the psychological predictors, and the scores on the perceived change in anxiety symptoms might have depended on the unknown participants' pre-quarantine level.
That said, the present research allowed an assessment of the psychological functioning of individuals in the early days of a pandemic-driven quarantine as it unfolded, and the results supported the WHO (2020b) claim that mental health needs must be treated as a core element of the response to a pandemic, since a failure to take them account can lead to long-term social, psychological, and economic costs to society.
Declaration of Competing Interest
The authors declare that they do not have any interests that could constitute a real, potential or apparent conflict of interest with respect to their involvement in the publication. The authors also declare that they do not have any financial or other relations (e.g. directorship, consultancy or speaker fee) with companies, trade associations, unions or groups (including civic associations and public interest groups) that may gain or lose financially from the results or conclusions in the study. The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jadr.2021.100078.
Appendix. Supplementary materials
References
- Adler N.E., Epel E.S., Castellazzo G., Ickovics J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. 2000;19(6):586–592. doi: 10.1037/0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- American Psychological Association. (2020). Anxiety. In APA Dictionary of Psychology. https://dictionary.apa.org/anxiety
- Andresen E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am. J. Prevent. Med. 1994;10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J.G., Taylor S. Health anxiety and its disorders. In: Hersen M., Rosqvist J., editors. Handbook of Assessment, Conceptualization, and Treatment. Wiley; 2007. pp. 701–727. [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Brand J., McKay D., Wheaton M.G., Abramowitz J.S. The relationship between obsessive compulsive beliefs and symptoms, anxiety and disgust sensitivity, and Swine Flu fears. J. Obsessive-Compuls. Relat. Disord. 2013;2(2):200–206. doi: 10.1016/j.jocrd.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E.B., Huppert J.D., Leiberg S., Langner R., Kichic R., Hajcak G., Salkovskis P.M. The obsessive-compulsive inventory: development and validation of a short version. Psychol. Assess. 2002;14(4):485–496. doi: 10.1037/1040-3590.14.4.485. [DOI] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucock M.P., Morley S. The health anxiety questionnaire. Br. J. Health Psychol. 1996;1:137–150. doi: 10.1111/j.2044-8287.1996.tb00498.x. [DOI] [Google Scholar]
- McDonald R.P. Lawrence Erlbaum Associates Publishers; New York: 1999. Test Theory: a Unified Treatment. [Google Scholar]
- Mwinyi J., Pisanu C., Castelao E., Stringhini S., Preisig M., Schiöth H.B. Anxiety disorders are associated with low socioeconomic status in women but not in men. Women's Health Issues. 2017;27(3):302–307. doi: 10.1016/j.whi.2017.01.001. [DOI] [PubMed] [Google Scholar]
- Nielsen (2020, March 14). Coronavirus: Il pensiero degli italiani post DPCM. https://www.nielsen.com/it/it/insights/article/2020/coronavirus-il-pensiero-degli-italiani-post-dpcm/
- Rubin G.J., Amlôt R., Page L., Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339:b2651. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., Asmundson G.J.G. Guilford; 2004. Treating Health Anxiety: a Cognitive-Behavioral Approach. [Google Scholar]
- Wang Y., Xu B., Zhao G., Cao R., He X., Fu S. Is quarantine related to immediate negative psychological consequences during the 2009 H1N1 epidemic? Gen. Hosp. Psychiatry. 2011;33(1):75–77. doi: 10.1016/j.genhosppsych.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit. Ther. Res. 2012;36(3):210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Wheaton M.G., Berman N.C., Franklin J.C., Abramowitz J.S. Health anxiety: latent structure and associations with anxiety-related psychological processes in a student sample. J. Psychopathol. Behav. Assess. 2010;32:565–574. doi: 10.1007/s10862-010-9179-4. [DOI] [Google Scholar]
- World Health Organization. (2020a). Q&A on coronaviruses (COVID-19). April 17, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses.
- World Health Organization. (2020b). Substantial investment needed to avert mental health crisis. May 14, 2020. https://www.who.int/news-room/detail/14-05-2020-substantial-investment-needed-to-avert-mental-health-crisis.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


