Abstract
Objective:
Using inpatient data from a 1,160-bed health system, we aimed to assess the positive predictive value (PPV) of ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) codes included in a traumatic brain injury (TBI) surveillance definition proposed by the Centers for Disease Control and Prevention in 2016.
Methods:
A random sample of 196 records with ICD-10-CM TBI codes was reviewed. The PPVs for the ICD-10-CM codes’ ability to capture true TBI cases were calculated as the percentage of records with confirmed clinical provider-documented TBI and reported with their 95% confidence intervals [95%CIs].
Results:
The estimated overall PPV was 74% [67.9%, 80.1%] when the codes were listed in any diagnostic field position, but 91.5% [86.2%, 96.8%] when listed as the principal diagnosis. S06 codes (intracranial injury) had an overall PPV of 80.2% [74.3%, 86.1%] and 96.9% [93.3%, 100%] when listed as the principal diagnosis. S02.0-.1 codes (vault/base skull fractures) in any position without co-existing S06 codes had a PPV of 15.8% [0%, 33.2%].
Conclusions:
Intracranial injury codes (S06) in any diagnostic position had a very high estimated PPV. Further research is needed to determine the utility of other codes currently included in the CDC proposed definition for TBI surveillance.
Keywords: surveillance definition, traumatic brain injury, positive predictive value, ICD-10-CM, medical record review
Introduction
Traumatic brain injury (TBI) is a temporary or permanent disruption of the normal function of the brain due to an external force (1, 2). Public health agencies in the United States have conducted TBI surveillance using health care administrative data sets coded in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), for more than two decades. The initial set of TBI surveillance ICD-9-CM codes proposed by the Centers for Disease Control and Prevention (CDC) (800.0–801.9 Fracture of vault or base of skull; 803.0–804.9 Other unqualified and multiple fractures of skull; 850.0–854.1 Intracranial injury, including concussion, contusion, laceration, and hemorrhage) was expanded with 950.1–950.3 Injury to optic nerve and pathways; 995.55 Shaken infant syndrome; and 959.01 Head injury, unspecified (3–7).
The validity of the ICD-9-CM diagnosis codes used in TBI morbidity surveillance has been assessed over the years in different populations and clinical settings (8–10). A 2005 study by Shore et al. found that the ICD-9-CM data performed well in capturing anatomic injuries such as skull fractures, but fell short in accurately assessing cases with neurologic abnormalities, ultimately underestimating TBI severity and prevalence (10). Carlson et al. compared the ability of ICD-9-CM diagnosis codes in U.S. Department of Veterans Affairs (VA) data to capture clinician-confirmed TBI cases. The authors found the VA codes to have an overall sensitivity of 70% and concordance of 75% (8). However, Faul et al. noted that the CDC’s ICD-9-CM-based TBI surveillance definition, while useful for approximating disease burden, was not always consistent with the clinical diagnosis of TBI (11). Bazarian et al. compared emergency department records of patients with documented mild TBI to corresponding ICD-9-CM data and found the positive predictive value of the CDC TBI surveillance definition to be only 23% (9).
On October 1, 2015, health systems in the United States transitioned from ICD-9-CM to the ICD-10-CM coding system (12). In 2016, the CDC proposed an updated surveillance definition for TBI using ICD-10-CM diagnosis codes that excluded the diagnosis code Unspecified injury of head (S09.90), although its analog (959.01) in ICD-9-CM was part of the ICD-9-CM-based TBI surveillance definition (7, 13). The differences between the ICD-10-CM- and the ICD-9-CM-based TBI surveillance definitions are reviewed by Hedegaard et al (13). The new definition was developed before data coded in ICD-10-CM was available to validate it. Recent multi-site medical record review studies have evaluated the positive predictive value (PPV) of some of the ICD-10-CM TBI surveillance codes for capturing TBIs treated in emergency department (ED) settings (14, 15). This current study builds on the previous work to estimate the PPV of proposed ICD-10-CM codes for TBI surveillance in the inpatient setting using data from one health care system.
Methods
Study Population
The study population included all patients treated in the two acute care hospitals within the University of Kentucky health care system between October 2015 and March 2019. Hospital discharge records were provided by the Office of Health Data and Analytics, Kentucky Cabinet for Health and Family Services. The Kentucky inpatient discharge records include one principal diagnosis field and up to 24 secondary fields. Encounters of care for treatment of TBI were identified as records that had at least one ICD-10-CM diagnosis code (principal or secondary) in the range: S02.0, S02.1 (vault/base skull fractures); S02.8, S02.91 (fracture of other specified skull and facial bones, unspecified fracture of skull); S04.02, S04.03, S04.04 (injury of optic chiasm, optic tract and pathways; injury of visual cortex); S06 (intracranial injury); S07.1 (crushing injury of skull); or T74.4 (shaken infant syndrome) (13). Only records representing encounters for initial treatment (i.e., ICD-10-CM diagnosis code with a 7th character “A” or “B”) were included in the sampling frame.
During the study period (October 1, 2015- March 31, 2019), there were 3,259 inpatient discharge records with at least one ICD-10-CM code for initial treatment encounter for TBI, including 292 (9%) records with a code S02.0; 706 (21.7%) with a code S02.1; 296 (9.1%) with S02.8; 28 (0.9%) with a code S02.91; 2.946 (90.4%) with a code S06; 5 (0.2%) with a code T74.4, less than 5 with a code S07.1; and no records with a code in the range S04.02-.04 (the percentages add up to more than 100% as some records had more than one TBI code). The study sample size was calculated (using normal approximation to binomial distribution) to guarantee a margin of error no larger than 7% for the 95% confidence interval (95% CI) of the estimated PPV under the assumption that the true PPV was 50%. A sample size of 196 inpatient records was sufficient for the desired precision of the PPV estimation. A simple random sample of 196 inpatient discharge records was taken from the eligible 3,259 inpatient discharge records with at least one ICD-10-CM discharge code for initial treatment of TBI.
Ascertainment of TBI documentation
The primary goal of the study was to estimate the PPV of the TBI surveillance codes for capturing TBI-related hospitalizations. According to the medical coding guidelines for code assignment and clinical criteria (12), when assigning ICD-10-CM discharge diagnosis codes, medical coders are allowed to use only notes and diagnostic statements of the clinical provider who is legally accountable for establishing the patient’s diagnosis. Information indicating the presence of a TBI (e.g., imaging test positive for TBI) that is not reflected in the clinical provider’s notes cannot be used by the medical coder. Therefore, clear documentation for a TBI in the clinical provider notes is the sole criterion that could justify the assignment of a TBI-related ICD-10-CM code.
This study assessed cases captured by the ICD-10-CM surveillance codes via medical record chart review, similar to previous validation studies (10, 15). A medical student was trained as a reviewer to collect information from the electronic medical record on the documentation of TBI by the patient’s clinical provider. Relevant information regarding patient demographics, injury mechanism, and TBI-related symptoms was also recorded in an abstract form (Appendix 1) that was initially developed by a CDC-funded multi-state study on TBI (14). The abstracted data were collected via a secure, web-based application, REDCap (Research Electronic Data Capture) (16).
Documentation of a TBI-related diagnosis was taken from clinical provider-authored notes within the electronic medical record. Clinical provider notes for the inpatient stay included the discharge summary, admission note, and any progress or consult notes authored and signed by the clinical provider. The reviewer used the clinical provider notes as the main source of information to gather evidence and respond to the following question: “TBI, concussion or similar diagnosis documented in the clinical provider’s note (No; Yes, known; Yes, suspected)”. Medical terms indicating documentation of a TBI diagnosis within the clinical provider notes (e.g., intracranial hemorrhage (subdural, epidural, subarachnoid, intracerebral, intraventricular), traumatic intracerebral hemorrhage, acute traumatic intracerebral hemorrhage, delayed traumatic intracerebral hemorrhage, traumatic brain injury, traumatic intracranial hemorrhage, concussion) were adapted from the previously mentioned multi-state study (14). The reviewer consulted a trauma surgeon when the interpretation of medical record notes was ambiguous. If the study reviewer responded “Yes, known”, we considered this record a true positive record for TBI, justifying the assignment of a TBI surveillance code.
The PPV for the ICD-10-CM TBI surveillance codes to capture records for TBI encounters in inpatient hospitalizations was estimated as the percentage of true positive cases out of the total sample (n=196). Additionally, the study estimated the PPVs for the most TBI-relevant ICD-10-CM diagnosis code of intracranial injury, S06, using the subsample of records with a diagnosis of S06 in any diagnosis position and separately, in the principal diagnosis position only. The estimated PPVs and their 95% confidence intervals were calculated with statistical software SAS v.9.4 (17).
Determining TBI likelihood
The secondary goal of the study was to determine, based on all the information available in the medical record, whether the patient experienced a TBI. Of specific interest were cases with a discrepancy between the information recorded in the provider’s diagnostic statement and the information in other parts of the medical record (e.g., imaging results, consultation notes). The study reviewer used information from the entire medical record authored by a clinical provider (e.g., discharge notes, medical consult notes, imaging reports, etc.) to answer the question: “Based on complete record review, reviewer’s assessment is: TBI, Probable TBI, Possible TBI, or No TBI”. The reviewer was allowed to use personal clinical knowledge to interpret documented clinical signs and symptoms (e.g., loss of consciousness, headache, memory problems), imaging results, Glasgow Coma Scale (GCS) scores, and other documented symptom inventories (e.g., Post-Concussion Symptom Scale, Health and Behavior Inventory, Acute Concussion Evaluation) that could indicate the presence or absence of a TBI (14, 15, 18–20). Thus, the study reviewer could categorize a case as a documented TBI (“Yes, documented”) if the presence of a TBI diagnosis was clearly stated in the patient’s clinical provider notes, but then categorize the same case as “Possible TBI” if the diagnosis of TBI was not supported by documentation of any relevant symptom or test. This approach supported identification of areas for documentation improvement.
The most significant factors contributing to the reviewer’s decision of TBI likelihood were the following: a diagnosis of TBI in the clinical provider notes; documentation of an injury event; positive imaging findings (Appendix 2); and number and severity of TBI-related symptoms (including loss of consciousness, memory problems, nausea or vomiting, noise or light sensitivity, headache, coordination and balance issues, and others). Injury event was defined as “any external strike, force of acceleration/deceleration, or explosive force/shock wave” documented directly as likely or as suspected. Positive imaging findings were obtained from the radiologist’s “impression” section. For the purposes of this study, the reviewer considered imaging positive for TBI if the radiologist’s impression section documented a traumatic intracranial injury (Appendix 2). Other abnormal findings, such as skull fractures or facial fractures, were recorded in the abstract form if present, but not considered positive for TBI unless concurrent intracranial injury was present or explicit language indicating positive imaging for traumatic brain injury was stated in the radiologist’s report.
Laboratory information was collected from either clinical provider notes or the results tab in the electronic medical record. Time of injury and time of admission were collected from either clinical provider notes or the patient care flowsheet and arrival information tabs in the electronic medical record. Injury events were categorized as documented present, documented not present, or not documented. When the medical record did not include documentation of clinically relevant symptoms (e.g., loss of consciousness or headache), the study reviewer categorized the symptom as not documented.
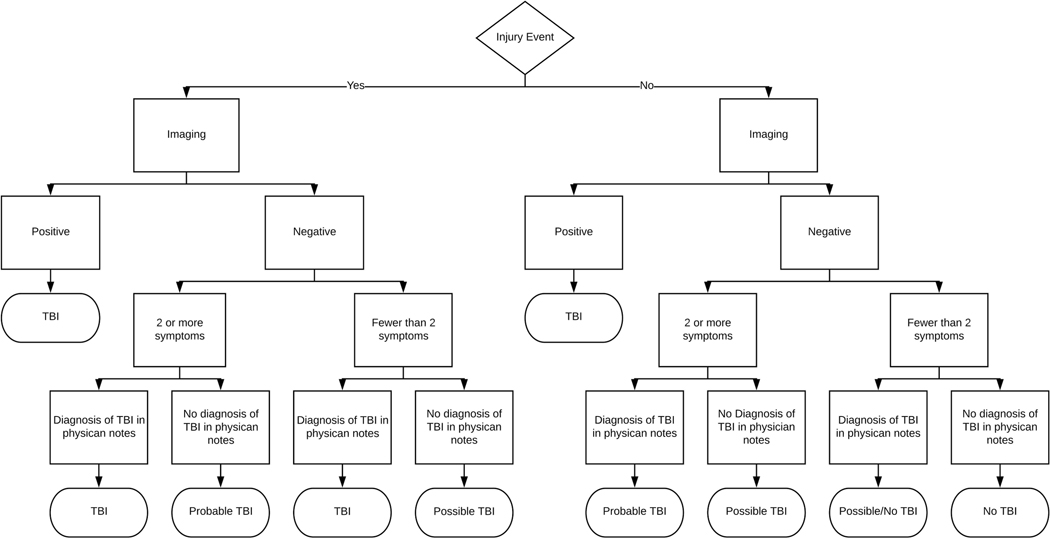
Figure 1 serves as a schematic of the decision-making process that went into the reviewer’s final assessment of TBI likelihood, but it does not list all factors that were accounted for. Due to variation in presentation and documentation, factors such as duration and severity of symptoms were taken into account on a case-by-case basis (6). These variable factors were most often used to differentiate “possible TBI” and “no TBI” when the objective information in the medical record was not definitive. The decision scheme outlined in Figure 1 differentiates TBI likelihood based on number of TBI-related symptoms. However, our review found that relevant symptoms might be recorded in one clinical note but not in subsequent notes, or be recorded as “suspected” only. Symptoms that were consistently documented throughout the medical record were considered more reliable than symptoms inconsistently reported, as were symptoms that were definitively recorded as present rather than suspected.
Figure 1:
Flowchart for assessing if medical record documentation provides evidence for traumatic brain injury-related encounter of care for a random sample of 196 inpatient records from one Kentucky healthcare system between October 2015 and March 2019.
The presence of potentially confounding factors such as dementia and drug or alcohol intoxication were also considered when assessing TBI likelihood (9). For instance, the symptom of “confusion” was often documented alongside alcohol intoxication. This was considered a potential confounder, and in these cases the reviewer would examine subsequent medical record notes to see if confusion continued to be documented after the patient’s blood alcohol levels normalized. Confusion in the absence of such confounders would be considered much more likely to be due to TBI, and thus more reliably applied to the decision scheme outlined in Figure 1.
This study was approved by the University of Kentucky Institutional Review Board.
Results
The study sample (n=196) included 106 (54.1%) records with a principal diagnosis code among the group proposed for the ICD-10-CM definition of TBI, including 87 records with a principal diagnosis code S06 (intracranial injury), and 19 records with a principal diagnosis code S02.0-.1,.8-.91 (fracture of skull, base of skull, other specified skull and facial bones, unspecified fracture of skull) (Table 1). The sample did not capture records with diagnosis codes (principal or secondary) of S04.0-S04.4 or S07.1 due to the rarity of these codes. There were fewer than 5 records with both T74.4 (shaken infant syndrome) and S06 in secondary diagnosis positions. Overall, 177 (90.3%) of the records had a principal (n= 87) or a secondary (n=90) diagnosis of intracranial injury (S06). The median age of patients in the sample was 44 years (ranging from 0 to 99); and male patients made up 68.4% of the sample (data not shown). Based on the abstracted information, in 177 (90.3%) cases, a direct injury event that led to hospital admission was known and documented, and in 15 (7.7%), an injury event was suspected. In 7 cases the injury was documented as resulting from known or suspected abuse. The majority of the abuse cases were in children, and a workup for intentional trauma was documented in the records for those cases (data not shown).
Table 1:
Estimated positive predictive values (PPV) and 95% confidence intervals (95% CIs) for ICD-10-CM case definition for capturing traumatic brain injuries (TBIs) using a random sample of inpatient hospitalizations from one Kentucky health care system, 2016–2019.
| Inpatient sample of TBI-related records | Number records | TBI documented by clinical provider | Estimated PPV % (95% CI) |
|---|---|---|---|
| All | 196 | 145 | 74.0 (67.8–80.1) |
| With a principal diagnosis of TBI | 106 | 97 | 91.5 (86.2–96.8) |
| Principal ICD-10-CM diagnosis S06 (intracranial injury) | 87 | 84 | 96.9 (92.7–100) |
| Principal ICD-10-CM diagnosis S02.0-.1 (vault/base skull fractures) or S02.8-.91 (other specified skull or facial bone fracture or unspecified fracture of skull)
with co-present secondary S06 without co-present secondary S06 |
14 5 |
12 1 |
85.7 (67.4–100) a |
| With a secondary (but no principal) diagnosis of TBI | 90 | 48 | 53.3 (43.0–63.6) |
| Secondary S06 (with or without other TBI codes) | 76 | 46 | 60.5 (49.5–71.5) |
| Secondary S02.0-.1 or S02.8-.91 without co-present S06 | 14 | 2 | 14.3 (0, 34.5) |
| With S06 in any diagnosis position | 177 | 142 | 80.2 (74.4–86.1) |
| With S02.0-.1,S02.9-.91 (without co-present S06) in any diagnosis position | 19 | 3 | 15.8 (0.0–33.2) |
Note:
Estimated PPV and 95%CI not informative due to a large margin of error
Positive predictive value
The study reviewer confirmed that a TBI was documented by the clinical provider in 145 (74.0%) of the 196 sampled cases (Table 1). Thus, the estimated PPV of the ICD-10-CM-based TBI surveillance definition for capturing true recorded TBI cases was 74.0%, 95% CI [67.9%, 80.1%]. Among the 106 cases with a principal diagnosis of TBI, 97 (91.5%) were documented as TBI cases. Thus the estimated PPV for the ICD-10-CM-based TBI surveillance definition to capture TBI cases using the principal diagnosis only is 91.5%, 95% CI [86.2%, 96.8%]. There were 177 cases with a diagnosis code S06 (intracranial injury) and of these, 142 (80.2%) were documented by the clinical provider as TBIs, yielding an estimated 95% CI for the PPV of [74.3%, 86.1%]. The estimated PPV for the code S06 when listed as a principal diagnosis was 96.9%, 95% CI [93.3%, 100%], and 60.5%, 95% CI [49.5%, 71.5 %] when listed as a secondary diagnosis (regardless of the principal diagnosis). Cases with a principal diagnosis in the range S02.0-.1, .8-.91 and concurrent secondary diagnosis of S06 had a PPV of 85.7%, 95% CI [67.4%, 100%]. Without a secondary S06 code, cases with a principal diagnosis code of S02.0-.1, .8-.91 had a PPV of 53.3%, 95% CI [43.0%, 63.6%]. The estimated PPV for the S02.0-.1, .8-.91 codes in any position, without concurrent S06 code, was 15.8%, 95% CI [0, 33.2%].
For 48 (24.5%) of the 196 sampled records, the study reviewer found no documentation of TBI diagnosis in the clinical provider’s notes. Twenty-two of these cases were captured by S02.0-.1 (vault/base skull fracture) or S02.8-.91 (other specified skull or facial bone fracture or unspecified fracture of skull) codes, but the majority had a concurrent code for an intracranial injury. Thirty--two of the 48 unconfirmed cases had a code S06, with the most common being S06.9X (unspecified intracranial injury), which appeared in 17 of the unconfirmed cases. The clinical presentations in the unconfirmed cases varied widely (e.g., epileptic or alcohol withdrawal seizures, embolic infarct or stroke, transfers from other hospitals with concern for TBI in which either no TBI was found or confirmation of TBI was not documented). Numerous cases documented potentially TBI-related symptoms, such as loss of consciousness, headache, or confusion, but none had a documented physician-authored TBI diagnosis.
Likelihood of TBI based on the entire inpatient medical record
The study reviewer followed the decision tree described in the Methods section and Figure 1 to evaluate the likelihood that the sampled records captured TBI-related encounters of care.
The frequency of documented relevant clinical symptoms is presented in Table 2. Loss of consciousness (LOC) was very common (n=118, 60.2%), with 99 (83.9%) of these cases documented as known and 19 (16.1%) as suspected. Memory problems were documented in 103 cases (66% known, 34% suspected). Headache was recorded in 55 cases and suspected in 34 more cases, frequently documented as “head pain” or “gripping head.” The study abstractor identified 80 (40.8%) patients meeting the description of “dazed, foggy, confused, disoriented, or not able to think clearly” and additional 41 (20.9%) cases with suspected symptoms related to this group. Vision changes were entirely negative or not documented. Dizziness or balance changes, concentration changes, sensitivity to noise or light, sleep disturbances, and tinnitus were rarely documented as present. Documented cases of mood change were usually in conjunction with drug or alcohol use. In 31 cases speech problems were noted, but many of these had low GCS scores or were intubated at time of admission. Drug or alcohol use was documented in 35 (17.9%) cases and confirmed by either clinical provider notes or laboratory results records; dementia was noted in 10 (5%) cases and often coincided with memory symptoms (data not shown). In those cases, histories of injury mechanism and symptoms could have been difficult to obtain and the final assessment and documentation of TBI in the record could be questioned. Patients with low GCS scores (<9) upon admission often had no explicit documentation of multiple symptom categories. No patient records documented the use of a TBI-specific inventory (e.g., Post-Concussion Symptom Scale, Health and Behavior Inventory, Post-Concussion Symptom Inventory, Acute Concussion Evaluation). Non-contrast head CT was performed in 193 (98.5%) cases (data not shown). Contrast CT imaging was performed in addition to non-contrast CT in 103 (54.4%) of the sampled cases. MRIs were performed in 17 (8.7%) cases, primarily pediatric patients. Additional potential TBI symptoms, such as combativeness, seizures, or pupillary changes were noted in 38 cases (19.4%). The occurrence of these symptoms with confounding factors such as intoxication or a pre-existing seizure disorder was noted by the reviewer and accounted for in the final assessment of TBI likelihood.
Table 2:
Documentation of symptoms with clinical relevance to traumatic brain injuries (TBI) and results from a review of the medical record review on the likelihood for the presence of a TBI in a random sample (n=196) of inpatient hospital discharge records with an ICD-10-CM code for TBI surveillance
| Symptom Documenteda | Reviewer assessment of present TBIb N (%) | ||
|---|---|---|---|
| Symptom | Yes, Known N (%) | Yes, Suspected N (%) | |
| Dazed or disoriented: Dazed, foggy, confused, disoriented, or not able to think clearly (n=121; 61.7%) | 80 (66.1) | 41(33.9) | 90 (74.4) |
| Memory problems: Difficulty remembering what happened just before or after the injury event, difficulty recognizing people or places or learning new things (n=103; 52.6%) | 68 (66.0) | 35 (34.0) | 69 (70.0) |
| Loss of consciousness: also referred to as syncope or fainting (n=118; 60.2%) | 99 (83.9) | 19 (16.1) | 75 (63.6) |
| Nausea or vomiting: Nausea or vomiting that occurred early on following the injury event (n=22; 11.2%) | 22 (100) | 0 | 19 (86.4) |
| Headache: Headache, including pain or feeling pressure in the head subsequent to injury event (n=89; 45.4%) | 55 (61.8) | 34 (38.2) | 69 (77.5) |
| Coordination or balance issues: Dizzy, uncoordinated, had poor balance, was stumbling around, was moving more slowly than usual, or had imbalance on gait testing (e.g., tandem walk ability normal/able vs abnormal; speed normal vs decreased) (n=30; 15.3%) | 20 (66.7) | 10 (33.3) | 23 (76.7) |
| Vision changes: Blurred vision, double vision, or decreased vision as compared to pre-injury state (n=15) | 11 (73.3) | 4 (26.7) | 13 (86.7) |
| Difficulty concentrating: Difficulty concentrating or easily distractible (n=25; 12.8%) | 10 (40.0) | 15 (60.0) | 20 (80.0) |
| Noise or light sensitivity: Sensitivity to noise or light (Noise or light are disturbing or painful to the patient) (n=0) | 0 | 0 | 0 |
| Mood changes: Change in mood or personality such as irritability, nervousness, anxiety, feeling more or less emotional or sad, or feeling more bothered by things (n=30; 15.3%) | 18 (60.0) | 12 (40.0) | 23 (76.7) |
| Speech changes: Slurred speech, inability to speak (aphasia) or other speech problem (n=38; 19.4%) | 31 (81.6) | 7 (18.4) | 32 (84.2) |
| Sleep changes: Difficulty falling asleep, more drowsy than usual, or sleep quantity is noticeably more or less than usual (n=16; 8.2%) | 13 (81.3) | 3 (18.7) | 13 (81.3) |
| Hearing changes: Ringing in the ears (tinnitus) or other change in hearing (n=2; 1%) | 2 (100) | 0 | 2 (100) |
| Motor or sensory loss: Motor or sensory loss including weakness, numbness or tingling (n=21; 10.7%) | 15 (71.4) | 6 (28.6) | 16 (76.2) |
Within the medical record, was there mention of the following signs and/or symptoms by anyone? (Answer: No; Yes, known; Yes, suspected; No documentation)
Based on complete record review, reviewer’s assessment is: TBI; Probable TBI; Possible TBI; No TBI
Based on the review of the entire medical record pertaining to the sampled inpatient stay, the study reviewer classified the cases as TBI (n=135; 68.9%), Probable TBI (n=8; 4%), Possible TBI (n=13; 6.6%), or No TBI (n=40; 20.4%) encounters (Table 3). In ten cases within our 196-case sample, the clinical provider documented a TBI diagnosis in the medical record, but the reviewer determined TBI likelihood as only “probable” or “possible.” All of these instances documented mild TBI, usually in the setting of multiple injuries, but the medical record included no documentation of TBI-related symptoms or imaging. Within the 48 unconfirmed cases, the study reviewer categorized eight cases as “Possible” TBI due to documented injury events and TBI-related symptoms, despite no physician-authored TBI diagnosis being present in the medical record (Table 3).
Table 3:
Concordance between TBI diagnosis documented in the clinical provider notes and reviewer assessment of TBI likelihood based on review of the entire medical record
| TBI diagnosis documented in the clinical provider’s notes |
Based on complete record review, reviewer’s assessment is: | ||||
|---|---|---|---|---|---|
| TBI | Probable TBI | Possible TBI | No TBI | Total | |
| No | 0 | 0 | 8 | 40 | 48 |
| Yes, known | 135 | 5 | 5 | 0 | 145 |
| Yes, suspected | 0 | 3 | 0 | 0 | 3 |
| Total | 135 | 8 | 13 | 40 | 196 |
Discussion
Identification of TBI, particularly mild cases and those in patients with polytrauma, has been the subject of substantial international investigation (14–17). However, variation in country-specific implementation of the ICD-10-based coding system for morbidity data and surveillance definitions complicates comparisons of international studies (21). Greater accuracy in case identification is important because epidemiological datasets are used for internal and external resource allocation. This study adds to the existing literature by assessing the positive predictive value (PPV) of the United States CDC’s proposed ICD-10-CM TBI surveillance codes for hospitalized patients.
The code for unspecified head injuries was previously included in the CDC’s TBI definition for ICD-9-CM coded data. Bazarian et al. reported that 58.5% of the TBIs in their study sample were captured by the code for unspecified head injuries. The proposed TBI surveillance definition for ICD-10-CM-coded data does not include the ICD-10-CM code for unspecified head injuries. More than 90% of the cases in our study sample were captured by a code for an intracranial injury (S06).
Diagnosis of TBI documented in the clinical provider notes was confirmed in 145 of 196 total reviewed cases, resulting in an overall estimated PPV of 74% [67.8%, 80.1%]. The estimated PPV using the principal diagnosis only was 91.5% [86.2%, 96.8%]. Trauma patients often present with multiple injuries, so many TBIs would occur concurrently with other injuries. It is therefore reasonable that the PPV of a TBI surveillance code would decrease when listed as a secondary rather than a principal diagnosis, because a principal diagnosis of TBI would likely be the subject of more detailed documentation. Codes for vault/base skull fracture (S02.0-.1) demonstrated high PPV of 85.7% [67.4%, 100%] when assigned as principal diagnoses with concurrent secondary diagnosis code of intracranial injury (S06). This high PPV is likely due to the secondary intracranial injury diagnosis code. However, when vault/base skull fracture codes (S02.0-.1) were used alone, without a code for intracranial injury, skull fracture codes in any position resulted in a very low PPV of 15.8% [0%, 33.2%]. It is important to understand that while fractures of the skull, face, or orbit may, and often do, accompany traumatic brain injury, the presence of the fracture itself is not necessarily indicative of brain injury (11). A less severe fracture, demonstrating no abnormal intracranial findings on imaging and having minimal TBI-related signs or symptoms, may not be indicative of a true TBI. A recent multi-site review of the CDC TBI surveillance definition in the emergency department setting found consistently high PPV’s for intracranial injury codes across all study sites, but significantly lower PPV’s for skull fracture codes (15). The difference in PPV for skull fracture codes was even more pronounced in sites that used clinical reviewers, highlighting the potential for misclassification skull fracture codes have in capturing TBI. Further study on the incorporation of skull fracture codes into the surveillance definition for capturing true TBI cases in inpatient discharge data is warranted.
The ten cases in which the reviewer’s assessment of TBI likelihood did not align with the documented clinical provider diagnosis of TBI involved mild TBI (concussion), usually with multiple injuries. The clinical presentation of mild TBI varies widely, and symptoms can be transient, making definitive diagnosis difficult. Although there are several available mild TBI symptom inventories, there is no consensus on the diagnosis of mild TBI, and no cases in our study documented the use of any TBI-specific symptom inventories. When patients present with multiple injuries, diagnosis of mild TBI may be missed, delayed, or simply not documented as clinicians prioritize more severe injuries (22, 23).
In this retrospective record review, confirmation of TBI was not always possible due to incomplete clinical documentation, a limitation of the retrospective review studies addressed by other authors as well (18, 24). Variation and inconsistency in documentation of mild TBI cases, particularly in the context of multiple injury inpatient cases, characterized the majority of discordant cases in our study.
Our study sample included 48 cases identified by the proposed TBI surveillance definition codes that had no documentation in the medical record supporting confirmation of a TBI. Some of these cases were captured by codes for skull fracture, and as previously shown by another recent study, skull fracture codes without the concurrent intracranial injury code S06 had lower PPV for identifying TBIs in emergency department settings (15). Other unconfirmed cases, such as those captured by the unspecified intracranial injury code S06.9, did not have an explicit TBI diagnosis in the clinical provider’s notes but included documentation of potentially TBI-related symptoms such as loss of consciousness, confusion, and headache that likely triggered the code assignment (possibly due to the lack of more appropriate code in these situations). A future study with a larger sample size of cases coded S06.9 could support systematic evaluation and identification of language in the medical record that triggers this coding. Specific examples could then be included in continuing education for medical coders and clinical providers with the aim to improve documentation and coding of TBI hospitalizations.
Limitations
The study had several limitations. The study used only one reviewer, although a trauma surgery faculty member also reviewed the cases where the clinical documentation was ambiguous. The study was retrospective and the accuracy of the reviewer’s assessment of “true” TBI likelihood depended on the extent of the clinical documentation in the medical record. The absence of a validated, standardized method for retrospective analysis of potentially transient signs and symptoms makes assessment of TBI likelihood difficult. Variation in clinician practices and the presence of multiple injuries likely contributed to variation in medical record completeness. The inconsistent TBI documentation introduces a subjective element into interpretation of certainty regarding a TBI diagnosis. For example, a skull fracture resulting from a known injury mechanism may have been considered and treated as a TBI by the clinical provider, but in the absence of explicit TBI documentation, the case could not have been counted as “confirmed” in our study. Efforts to standardize how and when TBI is documented clinically would greatly benefit retrospective TBI surveillance data quality. The study period and study sample were not large enough to capture records with other codes currently included in the proposed TBI surveillance definition (e.g,. S04.02-.04 or S07.1), and was limited to inpatient records from one health care system. Our results are not generalizable beyond this population, but can serve to inform the design of future studies with different populations and in different clinical settings.
Our study evaluated the utility of a single ICD-10-CM surveillance definition of TBI developed by the United States CDC; many other code definitions are used by different institutions both within the United States and internationally (18–21). However, the predictive value of individual codes reported in this study can be considered when assessing the validity of various TBI surveillance definitions.
In this inpatient study, confirmed cases of TBI were commonly identified as “traumatic brain injury” in provider notes, and were almost always assigned of an intracranial injury code, S06. The intracranial injury code S06 in any diagnostic field (principal or secondary) had a high PPV for capturing true TBI cases. The low PPV for the skull fracture codes S02.0-.1, although based on a small subsample, signals the need for further study addressing the ability of these codes to capture true TBI cases and their utility for TBI surveillance.
Supplementary Material
Acknowledgements
The authors gratefully acknowledge Andrew Bernard, MD, MS for his clinical expertise and assistance in answering clinical questions involved in this review. The authors acknowledge support from the Office of Health Data and Analytics, Kentucky Cabinet for Health and Family Services, for providing administrative billing data for this study.
Footnotes
Disclosure of Interest
The authors report no conflicts of interests. The research described was supported in part by the NIH National Center for Advancing Translational Science, through training grant number TL1TR001997. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This work was also supported by a Grant (U17 CE924846) funded by the Centers for Disease Control and Prevention and awarded to the Kentucky Injury Prevention and Research Center as bona fide agent for the Kentucky Department for Public Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention, the Department of Health and Human Services.
References
- 1.Misch MR, Raukar NP. Sports Medicine Update: Concussion. Emergency medicine clinics of North America. 2020;38(1):207–22. [DOI] [PubMed] [Google Scholar]
- 2.Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2017;66(9):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998−−2000. Brain Inj. 2005;19(2):85–91. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Traumatic Brain Injuries in the United States. A Report to Congress Atlanta, GA; 1999. [Google Scholar]
- 5.Control CfD, Prevention. Traumatic Brain Injury in the United States: A Report to Congress Atlanta, GA: Department of Health and Human Services (US), CDC. National Center for Injury Prevention and Control; 1999. [Google Scholar]
- 6.Faul M. Traumatic Brain Injury in the United States ; emergency department visits, hospitalizations and deaths. http://wwwcdcgov/traumaticbraininjury/statisticshtml. 2010.
- 7.CDC. Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014.: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2019. [Google Scholar]
- 8.Carlson KF, Barnes JE, Hagel EM, Taylor BC, Cifu DX, Sayer NA. Sensitivity and specificity of traumatic brain injury diagnosis codes in United States Department of Veterans Affairs administrative data. Brain Inj. 2013;27(6):640–50. [DOI] [PubMed] [Google Scholar]
- 9.Bazarian JJ, Veazie P, Mookerjee S, Lerner EB. Accuracy of Mild Traumatic Brain Injury Case Ascertainment Using ICD-9 Codes. Academic Emergency Medicine. 2006;13(1):31–8. [DOI] [PubMed] [Google Scholar]
- 10.Shore AD, McCarthy ML, Serpi T, Gertner M. Validity of administrative data for characterizing traumatic brain injury-related hospitalizations. Brain Inj. 2005;19(8):613–21. [DOI] [PubMed] [Google Scholar]
- 11.Faul M, Coronado V. Epidemiology of traumatic brain injury. Handbook of clinical neurology. 2015;127:3–13. [DOI] [PubMed] [Google Scholar]
- 12.PMIC. International Classification of Diseases 10th Revision Clinical Modification: Practice Management Information Corporation (PMIC); 2016. [Google Scholar]
- 13.Hedegaard H, Johnson RL, Warner M, Chen LH, Annest JL. Proposed Framework for Presenting Injury Data Using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Diagnosis Codes. National health statistics reports. 2016(89):1–20. [PubMed] [Google Scholar]
- 14.Peterson AB, Gabella B, Johnson J, Hume B, Liu A, Costich J, et al. Multi-site medical record review of emergency department visits for unspecified injury of head following the ICD-10-CM coding transition. ICD-10-CM Injury Epidemiology and Surveillance Methods Supplement. Injury Prevention. 2020;(accepted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gabella B, Hathaway J, Hume B, Johnson J, Johnson RL, Liu A, et al. , editors. Assessment of the Proposed ICD-10-CM Traumatic Brain Injury Definition in Emergency Department Discharge Data: A Multi-State Medical Record Review. CSTE Annual Conference; 2019; Raleigh, NC. [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.SAS. SAS Version 9.4. SAS Institute Inc; Cary, NC: 2012. [Google Scholar]
- 18.Pozzato I, Meares S, Kifley A, Craig A, Gillett M, Vu KV, et al. Challenges in the acute identification of mild traumatic brain injuries: results from an emergency department surveillance study. BMJ Open. 2020;10(2):e034494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McChesney-Corbeil J, Barlow K, Quan H, Chen G, Wiebe S, Jette N. Validation of a Case Definition for Pediatric Brain Injury Using Administrative Data. The Canadian journal of neurological sciences Le journal canadien des sciences neurologiques. 2017;44(2):161–9. [DOI] [PubMed] [Google Scholar]
- 20.Pozzato I, Cameron ID, Meares S, Kifley A, Vu KV, Liang A, et al. A surveillance study to determine the accuracy of mild traumatic brain injury diagnosis in an emergency department: protocol for a retrospective cohort study. BMJ Open. 2017;7(8):e016222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen AY, Colantonio A. Defining neurotrauma in administrative data using the International Classification of Diseases Tenth Revision. Emerging themes in epidemiology. 2011;8(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buduhan G, McRitchie DI. Missed injuries in patients with multiple trauma. J Trauma. 2000;49(4):600–5. [DOI] [PubMed] [Google Scholar]
- 23.NASEM. Evaluation of the Disability Determination Process for Traumatic Brain Injury in Veterans. Washington (DC): National Academies Press (US): National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on the Review of the Department of Veterans Affairs Examinations for Traumatic Brain Injury; 2019. [PubMed] [Google Scholar]
- 24.Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9(4):231–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.