TO THE EDITOR: Oxygen is among the most frequently administered medical therapies, with a level that is commonly adjusted according to the reading on a pulse oximeter that measures patients’ oxygen saturation. Questions about pulse oximeter technology have been raised, given its original development in populations that were not racially diverse.1,2 The clinical significance of potential racial bias in pulse oximetry measurement is unknown.
Our study involved adult inpatients who were receiving supplemental oxygen at the University of Michigan Hospital (from January through July 2020) and patients in intensive care units at 178 hospitals (from 2014 through 2015).3 We analyzed paired pulse oximetry measures of oxygen saturation and measures of arterial oxygen saturation in arterial blood gas, with all evaluations performed within 10 minutes of each other. To ensure that the arterial oxygen saturation was directly measured by co-oximetry, we limited analyses to measures of arterial blood gas that included carboxyhemoglobin and methemoglobin saturations.
We tested for occult hypoxemia (i.e., an arterial oxygen saturation of <88% despite an oxygen saturation of 92 to 96% on pulse oximetry) among patients who identified their race as Black or White. Since a low level of peripheral perfusion could lower the accuracy of oxygen saturation values,4 we also estimated the percentage of patients with occult hypoxemia after adjusting for age, sex, and cardiovascular score on the Sequential Organ Failure Assessment (SOFA) in the University of Michigan cohort. Additional details regarding the methods that were used in the study are provided in the Supplementary Appendix, available with the full text of this letter at NEJM.org.
We analyzed 10,789 pairs of measures of oxygen saturation by pulse oximetry and arterial oxygen saturation in arterial blood gas obtained from 1333 White patients and 276 Black patients in the University of Michigan cohort and 37,308 pairs obtained from 7342 White patients and 1050 Black patients in the multicenter cohort. In the University of Michigan cohort, among the patients who had an oxygen saturation of 92 to 96% on pulse oximetry, an arterial oxygen saturation of less than 88% was found in 88 of 749 arterial blood gas measurements in Black patients (11.7%; 95% confidence interval [CI], 8.5 to 16.0) and in 99 of 2778 measurements in White patients (3.6%; 95% CI, 2.7 to 4.7) (Fig. 1). The findings in the adjusted analyses were similar to those in the unadjusted analyses, with an arterial blood gas oxygen saturation of less than 88% in 11.4% (95% CI, 7.6 to 15.2) of the measurements in Black patients and in 3.6% (95% CI, 2.5 to 4.6) of those in White patients. Results were also consistent after the exclusion of patients with an elevated carboxyhemoglobin level or diabetes. (Details are provided in the Supplementary Appendix.)
Figure 1. Accuracy of Pulse Oximetry in Measuring Arterial Oxygen Saturation, According to Race.
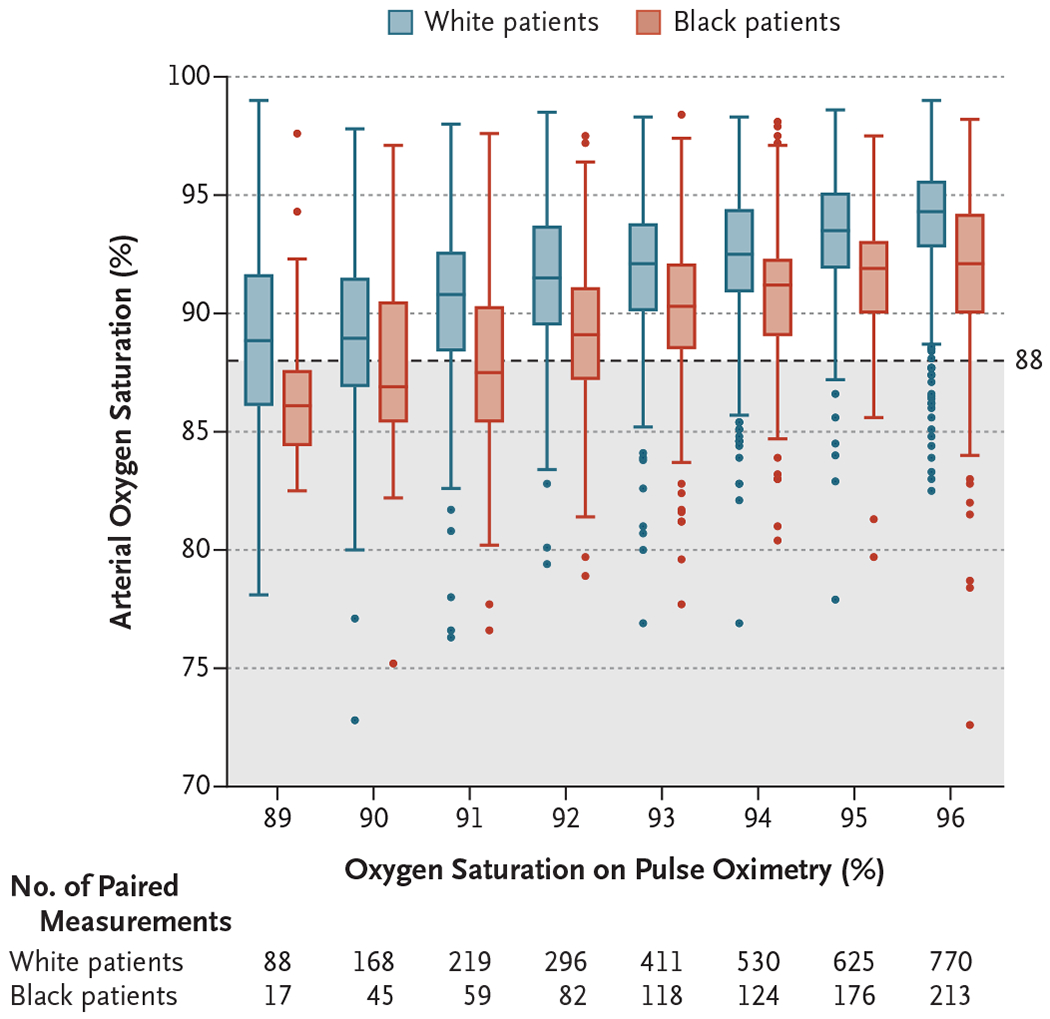
Shown is a comparison of paired measurements of pulse oximetry readings of oxygen saturation and time-matched directly measured arterial oxygen saturation among hospitalized patients who were stratified according to race. The shaded area indicates an arterial oxygen saturation of less than 88%. In the box plot, the horizontal line within each box represents the median, the top and bottom of each box represent the upper and lower limits of the interquartile range, and the whiskers represent 1.5 times the interquartile range. Outliers outside this range are indicated by data points.
In unadjusted analyses, the area under the receiver-operating-characteristic curve for detecting an arterial blood gas oxygen saturation of less than 88% according to the oxygen saturation on pulse oximetry was 0.84 (95% CI, 0.81 to 0.87) among Black patients and 0.89 (95% CI, 0.87 to 0.91) among White patients (P = 0.003). In the multicenter cohort, the unadjusted analyses involving patients with an oxygen saturation of 92 to 96% on pulse oximetry showed an arterial blood gas oxygen saturation of less than 88% in 160 of 939 measurements in Black patients (17.0%; 95% CI, 12.2 to 23.3) and in 546 of 8795 measurements in White patients (6.2%; 95% CI, 5.4 to 7.1).
Thus, in two large cohorts, Black patients had nearly three times the frequency of occult hypoxemia that was not detected by pulse oximetry as White patients. Given the widespread use of pulse oximetry for medical decision making, these findings have some major implications, especially during the current coronavirus disease 2019 (Covid-19) pandemic. Our results suggest that reliance on pulse oximetry to triage patients and adjust supplemental oxygen levels may place Black patients at increased risk for hypoxemia. It is important to note that not all Black patients who had a pulse oximetry value of 92 to 96% had occult hypoxemia. However, the variation in risk according to race necessitates the integration of pulse oximetry with other clinical and patient-reported data.
In device applications, the Food and Drug Administration requires reporting of demographic subgroups to mitigate risk. However, our findings highlight an ongoing need to understand and correct racial bias in pulse oximetry and other forms of medical technology.
Supplementary Material
THIS WEEK’S LETTERS.
2477 Racial Bias in Pulse Oximetry Measurement
2479 Risk Factors for SARS-CoV-2 in a Statewide Correctional System
2480 Capping or Suctioning for Tracheostomy Decannulation
2482 Avelumab Maintenance for Urothelial Carcinoma
2484 A Randomized Trial of Closed-Loop Control in Children with Type 1 Diabetes
2485 Spectrum of Fibrotic Lung Diseases
2486 Racial Disproportionality in Covid Clinical Trials
Acknowledgments
Supported by grants (K01 HL136687 and R01 LM013325, to Dr. Sjoding; R01 HL144599, to Dr. Dickson; K12 HL138039, to Dr. Iwashyna; and K23 HL140165, to Dr. Valley) from the National Institutes of Health and a grant (VA HSR&D IIR 17-045, to Dr. Iwashyna) from the Department of Veterans Affairs.
Footnotes
A complete list of authors is available with the full text of this letter at NEJM.org.
This letter reflects the views of the authors and does not necessarily represent the view of the U.S. Government or the Department of Veterans Affairs.
Disclosure forms provided by the authors are available with the full text of this letter at NEJM.org.
References
- 1.Moran-Thomas A How a popular medical device encodes racial bias. Boston Review. August 5, 2020. (http://bostonreview.net/science-nature-race/amy-moran-thomas-how-popular-medical-device-encodes-racial-bias).
- 2.Bickler PE, Feiner JR, Severinghaus JW. Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology 2005;102:715–9. [DOI] [PubMed] [Google Scholar]
- 3.Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Sci Data 2018;5:180178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Louie A, Feiner JR, Bickler PE, Rhodes L, Bernstein M, Lucero J. Four types of pulse oximeters accurately detect hypoxia during low perfusion and motion. Anesthesiology 2018;128:520–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


