Supplemental Digital Content is Available in the Text.
Chronic pain severity and interference worsened under conditions of social distancing, with certain sociodemographic factors and high pain catastrophizing associated with greater impact.
Keywords: Chronic pain, Social distancing, COVID-19, Isolation, Psychosocial factors
Abstract
The COVID-19 pandemic has had a tremendous impact, including on individuals with chronic pain. The social distancing policies necessary to slow the spread of SARS-CoV-2 have involved increased levels of social isolation. This cross-sectional survey study examined pain severity and interference among individuals with chronic pain during an early phase of social distancing mandates and identified characteristics of individuals who were most impacted. Approximately 4 to 8 weeks after social distancing mandates commenced in the state of Massachusetts, 150 patients with fibromyalgia, chronic spine, and postsurgical pain completed demographic, pain, social distancing, and validated psychosocial questionnaires. Patients self-reported an overall significant increase in pain severity and pain interference, compared with before social distancing, although both pain severity and interference were quite variable among individuals under conditions of social distancing. Several demographic, socioeconomic, and psychosocial factors were associated with greater pain severity and interference during social distancing. Multivariable linear regression demonstrated that female sex, nonwhite race, lower education, disability, fibromyalgia, and higher pain catastrophizing were independently associated with greater pain severity, while female sex and pain catastrophizing were independently associated greater pain interference. The findings suggest that individual differences among patients with chronic pain should be considered in the planning, development, and prioritization of interventions to improve pain care and to prevent worsening of symptoms during the continuing COVID-19 pandemic.
1. Introduction
Pain is modulated not only by sensory, emotional, and cognitive components but also by social factors including social connection.68 Despite the recognition of the importance of social factors in shaping the pain experience under the biopsychosocial model,46 their influence remains understudied. Unfortunately, the COVID-19 pandemic has imposed significant changes in social conditions of the majority of individuals worldwide, including persons with chronic pain. The World Health Organization has encouraged governments to regard slowing the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as a top priority,55 in which social distancing mandates have become an essential tool. As a result, individuals were relatively suddenly subjected to elevated levels of social isolation.9,54,69,72 Although the first wave of COVID-19 has abated in some areas, spread continues in other areas. It is projected that subsequent waves of recurrence may necessitate social distancing to varying degrees in years to come, possibly into 2022.38
Previous research has suggested that social isolation can result in adverse health outcomes in general, including worsening mental and physical health, and is associated with increased likelihood of emergency department admissions and greater length of hospital stay.20,30,61 Social interactions may also play an important role in modulating pain and the ability to cope with chronic pain.46 Thus, individuals with chronic pain may be at an increased risk of both physical and mental health deterioration31 during social distancing.36 Worsening of pain may contribute to a reliance on maladaptive coping strategies, such as substance abuse and increased suicidal ideation, which are already elevated among individuals with chronic pain.35 In addition, social distancing mandates have restricted or eliminated access to many adjunctive therapies for pain, including acupuncture, massage, physical therapy, rehabilitation therapy, and counseling services, potentially further contributing to worsening pain and stress.3,7,23
The aim of this study was to measure the impact of the externally imposed social isolation during the COVID-19 pandemic on pain. We queried patients with chronic pain about the degree of current social and physical isolation as well as patient pain severity and interference under the social distancing mandate and compared current reports with patient recalled isolation and pain from before social distancing. We hypothesized that current pain severity and interference would be greater while under conditions of increased social isolation. In addition, as an exploratory analysis to see whose current pain was impacted the most by changes imposed by social distancing, we carefully assessed the relationship between pain outcomes and psychosocial factors known to be important to impact the modulation of pain with the intentions of gaining greater insight into where to focus innovative pain management during future waves of COVID-19.
2. Methods
2.1. Study design and participants
This observational cross-sectional cohort study was conducted at an academic medical center in Boston, Massachusetts, between April 28, 2020, and May 22, 2020. The study was approved by the Partners Human Research Committee (PHRC)/Institutional Review Board (IRB). Participants were recruited through Partners Healthcare Rally website, an online platform that provides the public with information about current research studies they may be eligible to participate in. In addition, we contacted patients from our previous studies that belonged to cohorts that had postsurgical pain (mastectomy, TKA, C-section, thoracotomy, and spine surgery), fibromyalgia, and/or low back pain and invited them to complete the survey. Individuals who expressed interest in participating in the study were emailed a link to a secure data entry system to complete the eligibility survey.
Individuals were eligible to participate if they self-reported persistent pain for 3 months or longer, were English speaking, were ≥18 years of age, and were Massachusetts residents under the statewide social distancing rules at the time of survey. All participants (N = 150) who completed the survey provided consent and were compensated with a $20 Amazon electronic gift code. The study survey took approximately 30 to 45 minutes to complete.
2.2. Measures
Participants completed a series of questionnaires assessing sociodemographic, clinical, psychosocial characteristics, as well as degree of social and physical distancing, pain severity, and pain interference, which included both free form questions and validated questionnaires.
2.2.1. Sociodemographic and social distancing questions
In addition to basic demographics, participants completed the Brief Basic Needs Questionnaire. This questionnaire contains items relevant to basic needs security.27 This measure included 1 question with a 5-point Likert scale (very hard, hard, somewhat hard, not very hard, or not hard at all) on financial resource strain in which participants were asked how challenging it is for them to afford basic necessities such as food, housing, medical care, and heating. In addition, there were 2 items assessing food insecurity, 2 items examining transportation needs, and 3 items specific to housing stability. The questionnaire has a range of 1 to 14 in which higher score suggests increased challenges in obtaining basic needs. Participants also reported number of household residents, changes in employment, and whether they received a stimulus check. Patients were also asked if they got tested for COVID-19 and also if they had a positive test result. Participants were queried regarding perceived changes in physical and social isolation during COVID-19, access to health care, use of pain self-management techniques, and methods of social communication and connection since social distancing, including social media usage. Specifically, participants were also asked to indicate a percentage (operated a slider initially set at 50% to indicate %) of both social and physically isolation, with anchors at 0% being “not isolated at all” and 100% being “completely isolated.” Participants also reported utilization of various self-management techniques, physical and behavioral pain management resources, from a checklist. For those selected, they further indicated one of 3 choices regarding their utilization of the modality (it has decreased, it has stayed the same, or it has increased). Social contact was also examined by asking patients to indicate one of 6 options regarding video chat, phone calls or texting, connecting with social media, online classes, and in-person events (N/A—I have never performed this, I stopped doing this completely since I started social distancing, I do this less now than before social distancing, I do this the same amount now as before social distancing, I do this more often now than before social distancing, or I only started doing this since I started social distancing).
2.2.2. Pain outcomes
The 9-item Brief Pain Inventory (BPI) questionnaire was used to assess the primary outcomes of pain severity and pain interference with general functioning. The BPI has high test–retest reliability, construct validity, and criterion validity in chronic pain populations.21 Patients filled out this questionnaire twice consecutively, once with the text of each item referring to the time “before social distancing,” and once with the text referring to “Now, since social distancing.” Participants were asked to provide a 5-point Likert-scale (0 = “strongly disagree” to 4 = “strongly agree”) rating to indicate how much they attributed changes in pain to different elements of social distancing, including loneliness, mood, exercise, and access to pain treatments or self-management practices.
2.2.3. Psychosocial characteristics
The Pain Catastrophizing Scale (PCS) was used to examine catastrophic thinking associated with pain, including the domains of magnification, helplessness, and rumination. The PCS consists of 13 items scored from 0 to 4, resulting in a total possible score of 52, with higher scores indicating greater pain-related catastrophic thinking. The PCS has been widely validated in populations within both pain and controls.64,65 The validated 3-item UCLA Loneliness Scale (Version 3) was used to assess loneliness and has been found to be highly reliable, both in terms of internal consistency and test–retest reliability. Each question is rated on a 3-point scale, and all items are summed to give a total score of up to 9, with higher scores indicating greater loneliness.32,57 The 10-item extroversion and introversion subscale from the Myers–Briggs Type Indicator (MBTI) was used to assess introversion. The MBTI has been found to have construct validity. The introversion subscale has a range of 0 to 10, with higher scores indicating a preference towards higher levels of introversion.27 The Distress Intolerance Index is a 10-item tool which was used to examine participants’ ability to tolerate distress, with scores ranging from 10 to 40 with higher scores representing higher distress intolerance, and has demonstrated good internal consistency and reliability in pain patients and has been used to assess cognitive/affective responses and avoidance behaviors in response to distress.44 The Perceived Stress Scale (PSS) is a 10-item validated questionnaire used to assess the extent patients find their lives unpredictable, uncontrollable, and overloaded,17 with higher scores indicating greater perceived stress. The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) was used to capture the prevalence of PTSD in our sample. The PC-PTSD-5 is a 5-item measure that reflects the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) PTSD diagnostic criteria and has demonstrated validity, with a score of 3 or higher considered as positive for PTSD.10 In addition, validated short-form instruments from the Patient-Reported Outcome Measurement Information System (PROMIS) were used to assess anxiety, depressive symptoms, and sleep disturbance.12,16
2.3. Statistical approach
Descriptive statistics were used to examine frequencies, percentages, and measures of central tendency for demographics and behavioral health characteristics. Paired t tests were used to compare participants' current vs recalled ratings of outcomes (social isolation, physical isolation, pain severity, and pain interference), and effect sizes are reported as differences in the means with 95% confidence intervals (CI). Our power analysis was based on our previous chronic pain study where patients reported a worst pain severity with mean of 6.5 with SD of 2.6.58 Using a power of 80% and 2-sided level of significance of 5%, we calculated that to detect a small effect size16 in a paired group comparison, 135 subjects would be needed, so we planned to recruit 150 patients in case of missing questionnaire items. To correct for multiple testing of changes related to the social distancing mandate across 4 outcomes (social isolation, physical isolation, pain severity, and pain interference), we used a Bonferroni correction and considered P < 0.0125 significant for these outcomes.
We used linear regression to assess associations between patient characteristics and both pain outcomes (pain severity and pain interference). Categorical variables were dichotomized or made continuous when possible to decrease degrees of freedom. First, we performed univariable (simple) linear regression analyses for each individual baseline characteristic and each pain outcome. Next, we conducted a multivariable (multiple) linear regression analysis for each pain outcome, including all variables that were associated with the outcome in the univariable analyses at the P < 0.1 level. Multicollinearity between candidate predictors in the multivariable linear regression models was assessed using variable inflation factor (VIF) values, with a score of VIF > 5 considered problematic for model stability.63 VIF score ranges for predictor variables included in each model indicated minimal instability from multicollinearity amongst predictors (VIF range 1.11-3.52). All statistical analyses were performed using SPSS version 26.
3. Results
3.1. COVID-19 in Massachusetts, stay at home advisory, and phased reopening
Figure 1 depicts the development of the COVID-19 pandemic in Massachusetts from March 10, 2020, to June 15, 2020. Importantly, participants completed the survey between April 28 and May 22, representing a time of early social distancing in MA. All residents were required to practice proper hygiene, maintain social distancing, and use facial coverings when it was absolutely necessary to go to public places. Individuals who were at a higher risk of contracting COVID-19 (eg, people older than 65 years and those with underlying health conditions) were given additional guidance that strongly encouraged them to stay at home, with the exception of essential errands such as going grocery shopping and attending to health care needs.
Figure 1.
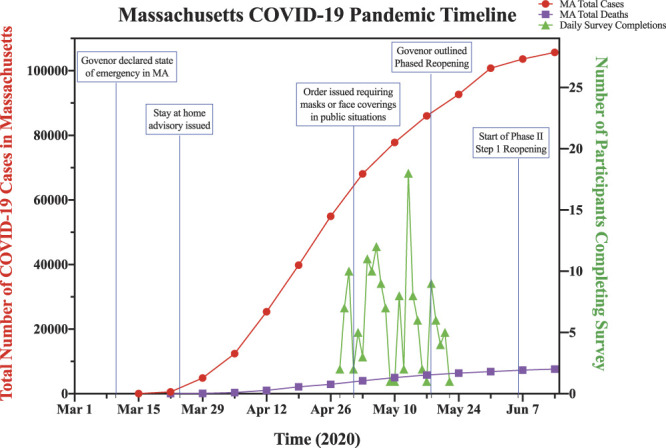
Study timeline in relation to COVID-19 pandemic in Massachusetts. All study surveys were completed between April 28 and May 22. The timeline includes key dates relevant to social distancing mandates in Massachusetts around the time of survey administration.
3.2. Participant recruitment and study flow
Figure 2 outlines the process of study recruitment, which included email invitations to patients with chronic pain including a general email blast through the Partners Healthcare System (Rally) research enrollment site, as well as outreach to patients participating in previous studies. Of the eligibility surveys completed, 204 eligible participants were emailed the main study survey, and 150 ultimately completed the study survey.
Figure 2.
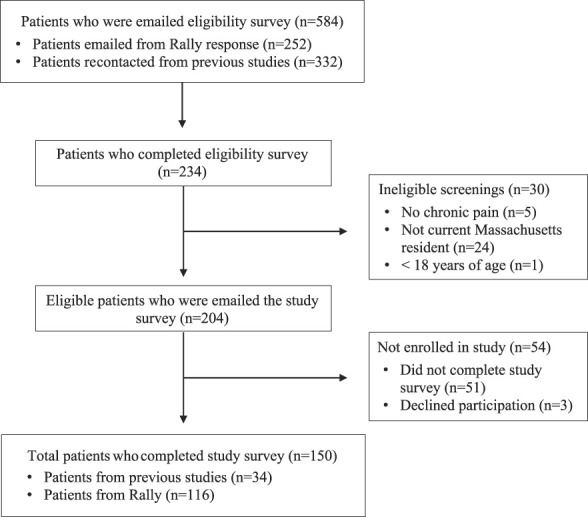
Study flow chart.
3.3. Participant demographics
Participants had a mean age of 41 years, were female majority, and predominantly non-Hispanic Anglo-American, with most having some postsecondary education (Table 1). Employment status before the pandemic included 60.1% employed full-time and 10.8% reporting receiving disability benefits. A range of incomes were reported, with relatively few participants reported outright job loss due to the pandemic. Most participants (72%) received a COVID-19 economic stimulus check. Questions regarding economic hardship indicated some difficulty with transportation to medical care or employment (10%-12%), as well as difficulty with food (14%), or housing (11%) security. Approximately 18% of participants reported being tested for COVID-19 and, only 1 participant screened positive for SARS-CoV-2. When participants were asked to self-report the nature of their chronic pain, 57% reported back pain, 25% fibromyalgia, 11% persistent postsurgical pain, and 58.7% other pain, with many participants reporting multiple sites/types of chronic pain (Appendix Figure 1, available at http://links.lww.com/PAIN/B221). A minority reported taking opioid medications (12.7%) for their pain condition.
Table 1.
Baseline patient characteristics.
| Variables | N (total) | N, mean | %, SD |
|---|---|---|---|
| Demographics | |||
| Age | 150 | 40.6 | ± 15.7 |
| Sex | 150 | ||
| Female | 125 | 83.3 | |
| Male | 21 | 14.0 | |
| Other | 4 | 2.7 | |
| Race | 149 | ||
| White | 126 | 84.6 | |
| Black | 11 | 7.4 | |
| Other | 12 | 8.1 | |
| Hispanic ethnicity | 149 | 5 | 3.4 |
| Education | 150 | ||
| High school diploma | 11 | 7.3 | |
| Associate's degree or trade/tech school | 15 | 10.0 | |
| Bachelor's degree | 65 | 43.3 | |
| Graduate degree | 59 | 39.3 | |
| Employment | 148 | ||
| Full-time | 89 | 60.1 | |
| Part-time | 15 | 10.1 | |
| Unemployed | 6 | 4.1 | |
| Student | 12 | 8.1 | |
| Disability | 16 | 10.8 | |
| Retired | 10 | 6.8 | |
| Employment changed since COVID | 150 | 108 | 72.0 |
| Received a stimulus check | 149 | 106 | 71.1 |
| Annual household income | 135 | ||
| < $25,000 | 16 | 11.9 | |
| $25,000 to $34,999 | 17 | 12.6 | |
| $35,000 to $49,999 | 24 | 17.8 | |
| $50,000 to $74,999 | 23 | 17.0 | |
| $75,000 to $99,999 | 23 | 17.0 | |
| $100,000 to $149,999 | 12 | 8.9 | |
| ≥ $150,000 | 20 | 14.8 | |
| Brief Basic Needs Questionnaire (1-14) | 150 | 2.86 | ±2.2 |
| Nature of chronic pain | 150 | ||
| Back pain | 86 | 57.3 | |
| Fibromyalgia | 38 | 25.3 | |
| Postsurgical pain | 17 | 11.3 | |
| Taking opioids for pain | 19 | 12.7 | |
| Isolation factors | |||
| Duration of social distancing | 150 | ||
| 3-6 weeks | 30 | 20.0 | |
| 7-8 weeks | 70 | 46.7 | |
| 9-10 weeks | 29 | 19.3 | |
| 11-12 weeks | 16 | 10.7 | |
| ≥ 3 mo | 5 | 3.3 | |
| Total number of household residents | 147 | 1.72 | ± 1.2 |
| Lives alone | 21 | 14.3 | |
| Degree of social isolation (0-100) | 146 | 68.9 | ± 21.8 |
| Degree of physical isolation (0-100) | 148 | 76.5 | ± 24.0 |
| Loneliness (3-9) | 150 | 6.2 | ± 2.0 |
| Psychosocial characteristics | |||
| Pain catastrophizing (0-52) | 150 | 17.8 | ± 13.5 |
| Distress tolerance (10-40) | 150 | 20.7 | ± 7.6 |
| Perceived stress (0-40) | 150 | 9 | ± 2.0 |
| Sleep disturbance (4-20) | 150 | 13.2 | ± 4.1 |
| Anxiety (7-35) | 150 | 21.8 | ± 7.1 |
| Depression (8-40) | 150 | 19.5 | ± 8.3 |
| Introversion (0-10) | 150 | 4.9 | ± 3.1 |
| PTSD | 150 | 32 | 21.3 |
| Substance use frequency | |||
| Tobacco use frequency | 147 | ||
| Never | 131 | 89.1 | |
| Less than monthly | 5 | 3.4 | |
| Daily or almost daily | 11 | 7.5 | |
| Alcohol use frequency | 150 | ||
| Never | 109 | 72.7 | |
| Less than monthly | 18 | 12.0 | |
| Monthly | 8 | 5.3 | |
| Weekly | 9 | 6.0 | |
| Daily or almost daily | 6 | 4.0 | |
| Drug use frequency | 150 | ||
| Never | 119 | 79.3 | |
| Less than monthly | 2 | 1.3 | |
| Monthly | 3 | 2.0 | |
| Weekly | 9 | 6.0 | |
| Daily or almost daily | 17 | 11.3 |
3.4. Degree of social and physical distancing, loneliness, and use of social media and technology
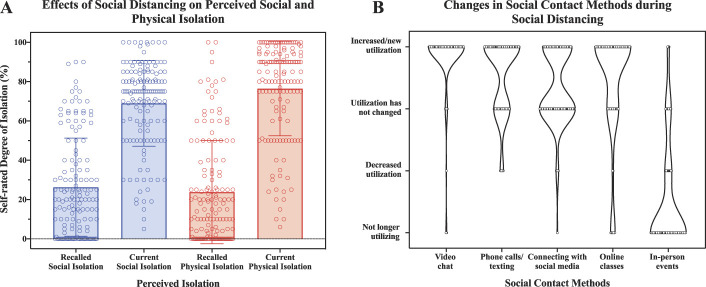
The majority of participants reported engaging in social distancing practices for an average of 4 to 8 weeks at the time of survey completion. Comparing current state with recalled state from before social distancing, most respondents reported a significant increase in both physical (t = 20.50, P < 0.001) and social isolation (t = 16.80, P < 0.001) at the time of survey completion (Fig. 3A). On average, participants reported feeling 54% more physically isolated (95% CI: 49%-59.11%) and 42% more socially isolated (95% CI: 37%-47%) compared with before social distancing. Participants reported changes in use of electronic means of communication and connection (Fig. 3B). Compared with before social distancing, 65% of participants reported an increase in phone usage (talking or texting), 91% reported an increase in video chatting, 43% reported an increase in using social media to connect with others, and 67% reported taking online classes. Unsurprisingly, 71.2% of participants reported no longer attending in-person community or religious gatherings. Approximately 14% of the study sample reported living alone, with the remaining participants reporting a mean of 2 ± 1 other household members. Participants reported a mean loneliness score of 6.2 ± 2 (range 1-9) and average introversion scores of 4.9 ± 3 (range 0-10).
Figure 3.
Effects of social distancing on isolation and social contact methods. (A) compares participants' recalled perceived social and physical isolation before social distancing to perceived isolation at the time of survey completion under conditions of social distancing. (B) depicts reported changes in how often participants use various social contact methods since they started distancing, compared with how often they recall using the method before social distancing.
3.5. Changes in pain severity and interference under social distancing
Participants' average pain severity and pain interference, measured by the Brief Pain Inventory, was quite variable (Fig. 4). Compared with patients' recall of pain before social distancing, both current pain severity and pain interference significantly increased (pain severity: t = 7.15, P < 0.001; pain interference: t = 3.93, P < 0.001). Current pain severity increased an average of 8% (0.79/10 points; 95% CI: 0.53-1.01), and current pain interference increased by 6% (4.28/70 points; 95% CI: 2.13-6.43), although this was quite variable between participants.
Figure 4.
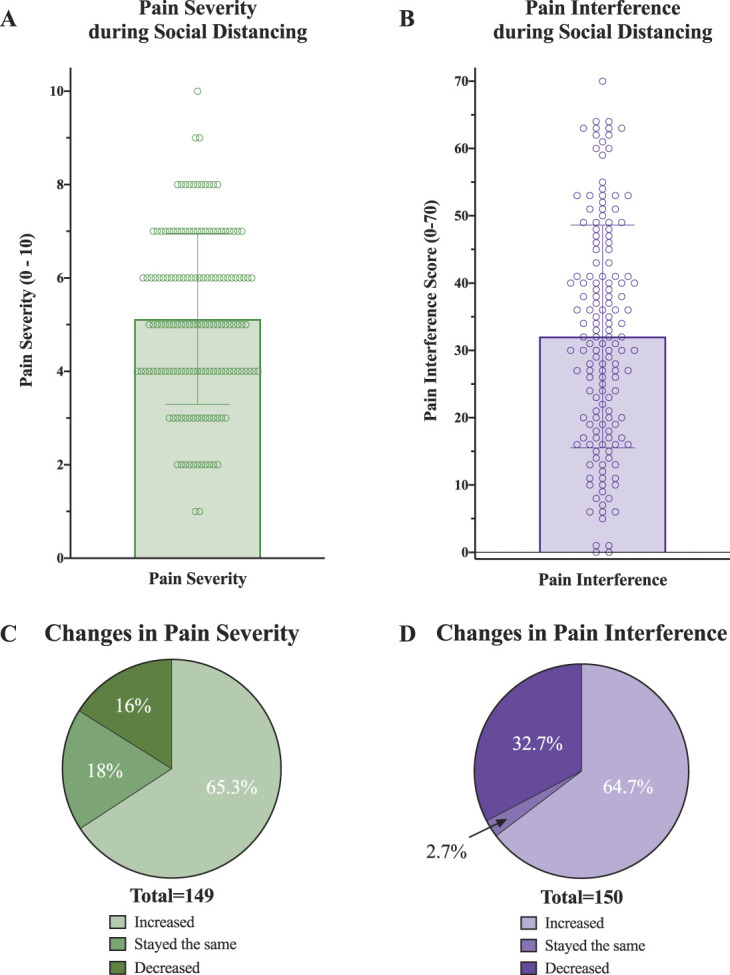
Participants' average pain severity and pain interference under social distancing conditions. (A) shows the distribution of current pain severity scores amongst participants during social distancing. (B) shows the distribution of current pain interference scores amongst participants during social distancing. (C) reports proportion of patients with changes in perceived pain severity since starting social distancing compared with their recalled pain. (D) reports proportion of patients with change in perceived pain interference since starting social distancing.
3.6. Factors associated with worse pain severity and interference under social distancing
Univariable (simple) regression analyses were performed to assess patient characteristics associated with greater pain severity and interference during social distancing (Table 2), revealing association of several factors with worse pain. Female sex, lower education, and higher Brief Basic Needs Questionnaire scores were associated with both worse pain severity and interference. Older age was associated with greater pain interference, but not pain severity, while nonwhite race was associated with greater pain, but not pain interference. Regarding isolation, a greater degree of social and physical isolation was weakly associated with greater pain severity, but more strongly associated with greater pain interference. Similarly, self-reported loneliness was related to pain interference but not to pain severity. Psychological factors were also variably related to pain severity and interference. Higher pain catastrophizing, sleep disturbance, anxiety, and depression were associated with greater pain severity and interference. Perceived stress was associated only with pain interference. More frequent drug use was associated with greater pain severity and interference, while alcohol use was only marginally related to pain severity.
Table 2.
Univariable association of patient characteristics with pain severity and pain interference during social distancing.
| Variable | BPI pain severity (0-10) | BPI pain interference (0-70) | ||
|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | |
| Demographics | ||||
| Age | 0.01 (−0.01 to 0.03) | 0.471 | 0.02 (−0.15 to 0.20) | 0.786 |
| Female | 1.11 (0.33 to 1.88) | 0.005 | 8.68 (1.63 to 15.73) | 0.016 |
| White, Non-Hispanic | −1.00 (−1.76 to −0.25) | 0.010 | −4.60 (−11.56 to 2.36) | 0.194 |
| Bachelor's degree | −1.48 (−2.23 to −0.74) | <0.001 | −8.24 (−15.19 to −1.29) | 0.021 |
| Employment status as disability | 2.37 (1.49 to 3.26) | <0.001 | 16.44 (8.12 to 24.76) | <0.001 |
| Brief Basic Needs Questionnaire | 0.32 (0.20 to 0.45) | <0.001 | 3.38 (2.27 to 4.49) | <0.001 |
| Fibromyalgia | 1.43 (0.79 to 2.07) | <0.001 | 8.43 (2.42 to 14.44) | 0.006 |
| Isolation factors | ||||
| Duration of social distancing | −0.05 (−0.34 to 0.24) | 0.715 | 1.99 (−0.61 to 4.58) | 0.133 |
| Degree of social isolation | 0.01 (0.00 to 0.03) | 0.056 | 0.29 (0.17 to 0.40) | <0.001 |
| Degree of physical isolation | 0.01 (0.00 to 0.02) | 0.204 | 0.20 (0.09 to 0.30) | <0.001 |
| Loneliness | 0.08 (−0.07 to 0.23) | 0.298 | 2.90 (1.61 to 4.20) | <0.001 |
| Psychosocial characteristics | ||||
| Pain catastrophizing | 0.07 (0.05 to 0.09) | <0.001 | 0.79 (0.64 to 0.94) | <0.001 |
| Perceived stress | 0.11 (−0.04 to 0.26) | 0.146 | 2.25 (0.93 to 3.58) | 0.001 |
| Sleep disturbance | 0.14 (0.07 to 0.21) | <0.001 | 1.69 (1.08 to 2.29) | <0.001 |
| Anxiety | 0.04 (0.00 to 0.08) | 0.070 | 0.94 (0.59 to 1.28) | <0.001 |
| Depression | 0.06 (0.02 to 0.09) | 0.002 | 0.99 (0.71 to 1.27) | <0.001 |
| Introversion | −0.04 (−0.14 to 0.05) | 0.403 | 0.25 (−0.61 to 1.10) | 0.566 |
| PTSD | 0.40 (−0.32 to 1.12) | 0.271 | 10.99 (4.70 to 17.28) | 0.001 |
| Substance use frequency | ||||
| Alcohol use | 0.23 (−0.04 to 0.50) | 0.096 | −0.02 (−2.48 to 2.43) | 0.985 |
| Drug use | 0.21 (0.00 to 0.41) | 0.054 | 2.02 (0.14 to 3.90) | 0.035 |
3.7. Multivariable linear regression of factors predicting worse pain outcomes under social distancing
Recognizing that many of the variables in the univariable analysis are closely related, we used multivariable (multiple) linear regression to examine factors that were independently associated with worse pain outcomes during social distancing, including variables that were significantly associated with the outcomes on univariable (simple) regression analysis at the P < 0.1 level. Model 1 explained 43.3% of the variance in pain severity and revealed female sex, nonwhite race, lower education, disability employment status, fibromyalgia, and higher pain catastrophizing scores as independently associated with worse pain severity (Table 3). Similarly, model 2 explained 48.4% of the variance in pain interference and revealed only female sex and higher pain catastrophizing as significant independent predictors.
Table 3.
Multivariable analyses.
| Model 1: pain severity | Model 2: pain interference | ||||
|---|---|---|---|---|---|
| β (95% CI) | P | β (95% CI) | P | ||
| Female | 0.82 (0.16 to 1.49) | 0.015 | Female | 6.31 (0.53 to 12.09) | 0.033 |
| White, Non-Hispanic | −0.85 (−1.47 to −0.23) | 0.007 | Bachelor's degree | −4.77 (−10.77 to 1.24) | 0.119 |
| Bachelor's degree | −0.86 (−1.54 to −0.18) | 0.014 | Brief Basic Needs Questionnaire | 0.73 (−0.47 to 1.93) | 0.231 |
| Brief Basic Needs Questionnaire | 0.00 (−0.14 to 0.14) | 0.980 | Employment status as disability | 4.36 (−3.07 to 11.80) | 0.248 |
| Employment status as disability | 1.00 (0.17 to 1.83) | 0.019 | Fibromyalgia | 2.91 (−2.09 to 7.90) | 0.252 |
| Fibromyalgia | 0.73 (0.16 to 1.30) | 0.012 | Degree of social isolation | 0.12 (−0.02 to 0.25) | 0.088 |
| Degree of social isolation | 0.00 (−0.01 to 0.02) | 0.562 | Degree of physical isolation | 0.04 (−0.08 to 0.15) | 0.557 |
| Pain catastrophizing | 0.05 (0.03 to 0.07) | 0.001 | Loneliness | 0.25 (−1.11 to 1.60) | 0.719 |
| Sleep disturbance | 0.05 (−0.02 to 0.11) | 0.198 | Pain catastrophizing | 0.41 (0.20 to 0.63) | 0.001 |
| Anxiety | −0.02 (−0.07 to 0.03) | 0.391 | Perceived stress | 0.86 (−0.30 to 2.01) | 0.145 |
| Depression | −0.01 (−0.06 to 0.04) | 0.760 | Sleep disturbance | 0.47 (−0.12 to 1.06) | 0.119 |
| Alcohol use | −0.03 (−0.25 to 0.20) | 0.829 | Anxiety | −0.05 (−0.49 to 0.40) | 0.835 |
| Drug use | 0.12 (−0.05 to 0.29) | 0.177 | Depression | 0.13 (−0.31 to 0.58) | 0.551 |
| PTSD | −1.30 (−7.16 to 4.57) | 0.662 | |||
| Drug use | 0.60 (−0.87 to 2.07) | 0.422 | |||
CI, confidence intervals.
3.8. Perceived impact on care and causes for pain worsening
Generally, participants reported decreased usage of pain management services and at the same time reported overall increased use of self-management techniques for pain (Fig. 5A and B). Patients endorsed the importance of treatment restrictions (70.7% agreed or strongly agreed) and decreased activity levels (66.7% agreed or strongly agreed) due to social distancing as an important reason for their pain worsening. In addition, increased stress (67.3% agreed or strongly agreed) and lower mood (53.4% agreed or strongly agreed) due to social distancing was cited as important to pain worsening as well. Interestingly, fewer participants cited loneliness (46.7% agreed or strongly agreed) as responsible for worsening pain (Fig. 5C).
Figure 5.
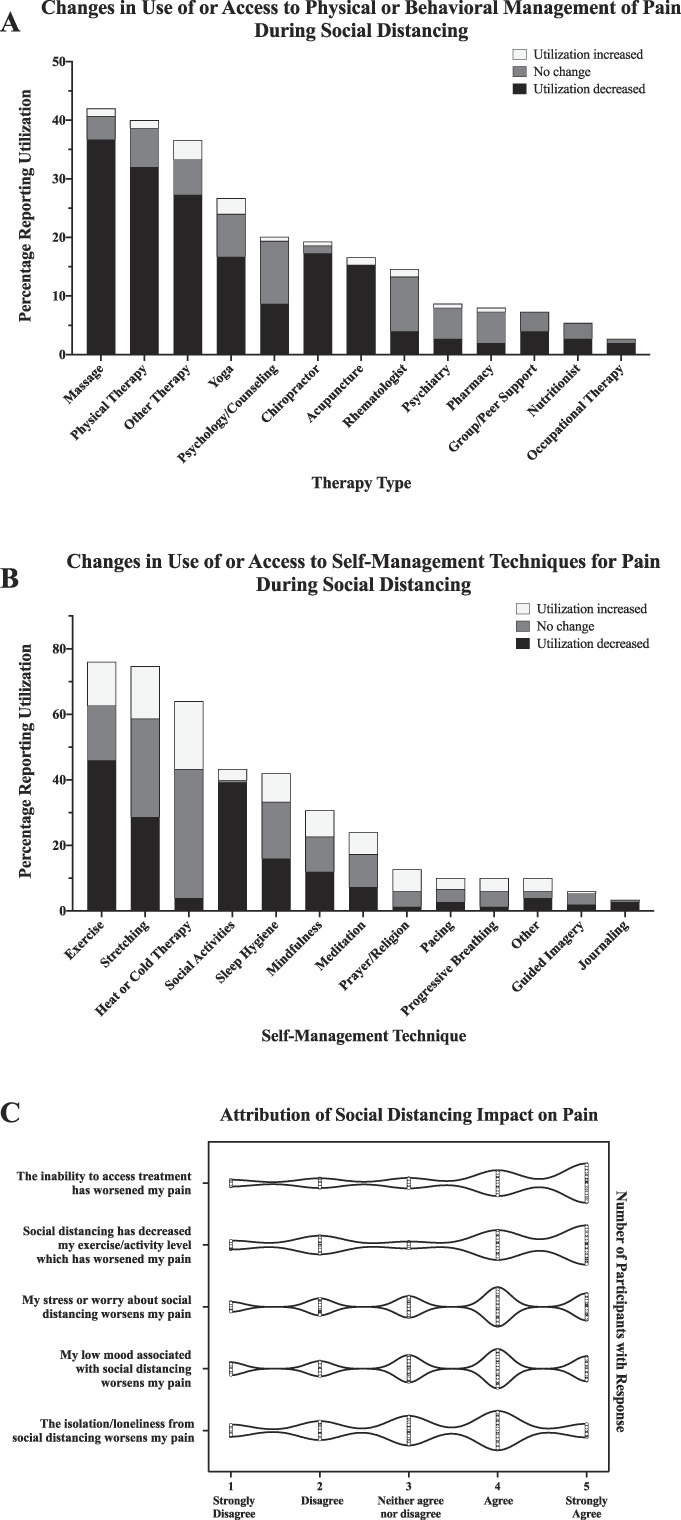
Effects of social distancing on utilization of pain management strategies, access to treatments, and quality of life. (A) shows what physical and behavioral pain management resources patients recalled using before social distancing and whether utilization of the resource has been affected since social distancing. (B) shows what self-management techniques for pain participants recalled engaging in before social distancing and how usage of each technique has been affected by social distancing. (C) depicts the extent participants attribute social distancing changes to factors contributing to changes in reported pain.
4. Discussion
This study examined the natural social experiment imposed on patients with chronic pain by the COVID-19 pandemic. We observed a self-reported increase in both pain severity and interference under social distancing conditions. Notably, pain severity and interference were quite variable among individuals with chronic pain during social distancing. Our subsequent exploratory assessment of factors that were related to greater pain severity with social distancing implicated a number of sociodemographic and psychosocial factors known from previous work to be related to pain. These exploratory findings may suggest that certain demographics (female sex, nonwhite race, lower education, and disability status) and psychosocial characteristics (higher pain catastrophizing) convey higher risk under conditions of social isolation. If there are future waves requiring another social distancing mandate, patients with these characteristics may benefit more from curated, targeted interventions.
4.1. Sociodemographic factors impacting pain
Although chronic pain is common, some individuals are at higher risk.62 Pain susceptibility seems to be influenced by sociodemographic factors, including sex,26,47,50,52 race and ethnicity,11,37,55 education,29,51,56 and employment,22 making individuals with these characteristics more vulnerable.4,8,21,33,34 In addition, the impact of social context in which an individual experiences pain has been understudied compared with biological and psychological constructs.39,45 The current study examined pain severity and interference in a sample of individuals with chronic pain during a period of newly imposed social isolation, shortly after the institution of social distancing mandates to prevent SARS-CoV-2 spread in Massachusetts. We observed that female sex, nonwhite race, lower education, and disability employment status were independently associated with greater pain severity during newly imposed social isolation. This effect was seen despite the study having a relatively small number of nonwhite participants and a large proportion of female participants.
Throughout the COVID-19 pandemic, sociodemographic factors have played an important role, with inequities in case incidence, morbidity, and mortality amongst minorities, and this pattern is expected to worsen.59 COVID-19 has revealed broader disparities within our society, providing an opportunity to prioritize strategic efforts to address inequity, including basic needs, access to medical services, and appropriate pain care.1,48 Despite our study sample having a relatively small number of minority participants, we still observed an association with greater pain severity, which suggests that it would be beneficial to develop additional research and programs targeting and rectifying this inequity. Furthermore, it is a priority is to combat the structural inequity of resources for marginalized populations, which lead to greater risk of chronic pain incidence, as well impact their ability to self-manage their pain. More proximal changes include targeting pain research to underrepresented minorities and involving researchers with diverse backgrounds in study design and conduct.54 This would allow for a more informed understanding of what mechanisms may be distinctly at work among minority patients, thus allowing also more effective and inclusive therapies for them.5 Furthermore, increasing the recognition of diversity of pain processing pain between individuals (even within a given demographic group) will support better-informed and more personalized medicine.6
4.2. Psychosocial characteristics, including pain catastrophizing
We were interested in investigating how psychosocial characteristics may interact with the social isolation imposed by the COVID-19 pandemic, which is itself associated with significant uncertainty and fear.40,67 Interestingly, although loneliness was associated with worse pain interference on the univariable regression analysis, we did not observe that loneliness per se was independently associated with worse pain outcomes in the multivariable regression analysis. This is consistent with the fact that patients did not cite feelings of loneliness per se as the most important drivers of pain increase during social distancing.
Under normal conditions, anxiety, depression, and stress are frequently comorbid with chronic pain and may in turn exacerbate and meaningfully worsen the experience of painful symptoms.13,44 Although we found that anxiety, stress, depression, and sleep disturbance were all associated with worse pain under conditions of social isolation, pain catastrophizing was the only psychosocial variable that was independently predictive of worsening of pain severity and interference. It seems plausible that being physically and socially isolated may contribute to higher levels of catastrophic thinking, including feelings of helplessness, rumination, and magnification. Catastrophic thinking has also been shown to be higher amongst many individuals with fibromyalgia, which was also associated with worse pain outcomes in our sample.9 Pain catastrophizing may represent an essential communicative function during socializing for patients with chronic pain. Collectively, it may be that the heightened pain expression exemplified by catastrophizing serves a useful purpose, allowing the individual's distress about pain to be recognized and managed within their social context.36 Pain catastrophizing may therefore simultaneously fulfill adaptive functions (eg, recruiting social support) and maladaptive functions (eg, amplifying pain severity and disability),35 a process that is consistent with our study findings.
4.3. Implications for pain management services
Our study findings suggested that fibromyalgia was independently associated with greater pain severity during newly imposed social isolation. This is consistent with previous research demonstrating that in patients with fibromyalgia, increased stress has a potent impact on symptom severity,2,28,49 and suggests that targeting individuals with fibromyalgia during social distancing may be of particular importance. However, many patients with chronic pain will likely benefit from the development and targeting of novel approaches to help improve care. Before the pandemic, telemedicine and eHealth approaches to chronic pain were already under development,15,24 and the current pandemic has accelerated the development and implementation of these approaches. There has been an increased demand and recommendation to use remotely supported eHealth pain management services with the outbreak, which brings unique changes in service delivery of pain management.18,25 A recent systematic review found that teletherapy and remote online cognitive behavioral therapy (CBT) strategies can be effective in improving quality of life among persons with chronic pain,41 with 1 study suggesting that online group CBT may be as effective in improving coping among persons with chronic pain as in-person groups.42 Such findings are promising, although additional research is needed to evaluate the impact of eHealth while recognizing the unique challenges created by the pandemic. Our study sample reported a significant disruption to their lives, including restricted access to pain-related service, and a need to increasingly rely on self-management techniques and remote/online forms of communication for social support.66 The increase in global use of social media platforms to maintain connections while social distancing14,19,43,53 suggests that people are becoming more accustomed and open to remote formats, perhaps making it an ideal time to implement these therapies into regular practices. Pandemic conditions aside, improvements in eHealth services could provide lasting impact on addressing the current dearth in necessary providers needed to meet overwhelming rates of individuals with chronic pain.
5. Limitations
Although this study offers valuable information regarding the experience of patients with chronic pain during social distancing, some important limitations should be considered when interpreting these findings. This study recruited participants with chronic pain from an urban academic medical center in Massachusetts, and participants were predominately white and female with higher formal education, thus limiting the generalizability to a broader population of patients with chronic pain across the United States or in other countries. The sample size was relatively small, likely precluding sufficient power for the exploratory regression analysis investigating who was had worse pain under social distancing mandates. Despite both these limitations, however, this analysis still observed racial, sex, and educational differences in pain under social distancing, hinting at the perhaps great extent of this problem. In addition, it should be acknowledged that our study participants had online access, as the survey required an email and an Internet connection. Thus, this study may not be adequately representative of individuals who do not have as much access to technologies and who also, unfortunately, would be less likely or unable to participate in remote-based therapies. Further research is needed to better understand the needs of these marginalized patients. In addition, it is possible that a self-selection bias may have impacted findings, with an overrepresentation of participants who were more impacted by the pandemic being willing to participate. Another important limitation is that the cross-sectional study design is open to the potential for recall bias, as we asked patients to reflect back to their condition weeks before the survey. Future research should use a longitudinal design within larger samples, including collection of preratings and postratings in real time, to limit issues around recall bias. In addition, it is important to note that there was a potential for confirmation bias present in the questions regarding social and physical isolation during social distancing mandates. The unforeseen circumstances of the rapidly imposed social distancing precluded this type of design in the current study, making a cross-sectional design a more feasible option to rapidly collect data, and to provide a snapshot of how social distancing impacts chronic pain.
6. Conclusion
In planning for the future of service delivery for patients with chronic pain, it is imperative to develop a more comprehensive understanding regarding the impact of social distancing amongst different types of patients with pain in other geographic locations variably impacted by COVID-19, specifically allowing for identification of those for whom it is most problematic. This information could be beneficial in better understanding the impact of social isolation on pain and guide development of innovative approaches to support this vulnerable population in the case of potential subsequent waves of COVID-19 where social distancing mandates may continue to be in effect.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Appendix A. Supplemental digital content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B221.
Acknowledgements
The authors thank the patients who took the time to participate in this study. The conduct of this study was supported by a grant from the NIH/NIGMS: R35 GM128691. There were no relevant conflicts of interests for any of the authors.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
Contributor Information
K. Mikayla Flowers, Email: kmflowers@bwh.harvard.edu.
Desiree R. Azizoddin, Email: desiree_azizoddin@dfci.harvard.edu.
Robert N. Jamison, Email: rjamison@bwh.harvard.edu.
Robert R. Edwards, Email: rredwards@bwh.harvard.edu.
Kristin L. Schreiber, Email: klschreiber@bwh.harvard.edu.
References
- [1].Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8:659–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Alok R, Das S, Agarwal G, Salwahan L, Srivastava R. Relationship of severity of depression, anxiety and stress with severity of fibromyalgia. Clin Exp Rheumatol Incl Supplements 2011;29:S70. [PubMed] [Google Scholar]
- [3].Blyth FM, March LM, Brnabic AJ, Cousins MJ. Chronic pain and frequent use of health care. PAIN 2004;111:51–8. [DOI] [PubMed] [Google Scholar]
- [4].Booher L. The impact of low socioeconomic status in adults with chronic pain: an integrative review. Orthopaedic Nurs 2019;38:381–9. [DOI] [PubMed] [Google Scholar]
- [5].Brady B, Veljanova I, Andary T, Southwell T, Chipchase L. Recognising ethnocultural diversity in chronic pain assessment: validation of the Pictorial Representation of Illness and Self Measure (PRISM) for use with culturally diverse communities. Health Qual Life Outcomes 2019;17:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Brady B, Veljanova I, Chipchase L. An exploration of the experience of pain among culturally diverse migrant communities. Rheumatol Adv Pract 2017;1: rkx002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Braunack-Mayer AJ, Street JM, Rogers WA, Givney R, Moss JR, Hiller JE. Including the public in pandemic planning: a deliberative approach. BMC public health 2010;10:501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Breivik H. A major challenge for a generous welfare system: a heavy socio‐economic burden of chronic pain conditions in Sweden – and how to meet this challenge. Eur J Pain 2012;16:167–9. [DOI] [PubMed] [Google Scholar]
- [9].Caley P, Philp DJ, McCracken K. Quantifying social distancing arising from pandemic influenza. J R Soc Interf 2008;5:631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cameron RP, Gusman D. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry 2003;9:9–14. [Google Scholar]
- [11].Campbell CM, France CR, Robinson ME, Logan HL, Geffken GR, Fillingim RB. Ethnic differences in the nociceptive flexion reflex (NFR). PAIN 2008;134:91–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 2010;63:1179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Charles S, Carayannopoulos AG, Pathak S. Anxiety and Depression in Patients with Chronic Pain. In: Deer's Treatment of Pain. Springer Nature Switzerland: Springer, 2019. pp. 125–9. [Google Scholar]
- [14].Chen Q, Min C, Zhang W, Wang G, Ma X, Evans R. Unpacking the black box: how to promote citizen engagement through government social media during the COVID-19 crisis. Comput Hum Behav 2020;110:106380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Clauw DJ, Häuser W, Cohen SP, Fitzcharles MA. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. PAIN 2020;161:1694–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates Publishers, 1988. [Google Scholar]
- [17].Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983:385–96. [PubMed] [Google Scholar]
- [18].Cohen SP, Baber ZB, Buvanendran A, McLean L, Chen Y, Hooten WM, Laker SR, Wasan WAD, Kennedy DJ, Sandbrink F. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 2020;21:1730–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Courtet P, Olié E, Debien C, Vaiva G. Keep socially (but not physically) connected and carry on: preventing suicide in the age of COVID-19. J Clin Psychiatry 2020;81:e20com13370–e13320com13370. [DOI] [PubMed] [Google Scholar]
- [20].Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community 2017;25:799–812. [DOI] [PubMed] [Google Scholar]
- [21].Davies KA, Silman AJ, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, McBeth J. The association between neighbourhood socio-economic status and the onset of chronic widespread pain: results from the EPIFUND study. Eur J Pain 2008;13:635–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].de Sola H, Salazar A, Dueñas M, Ojeda B, Failde I. Nationwide cross-sectional study of the impact of chronic pain on an individual's employment: relationship with the family and the social support. BMJ Open 2016;6:e012246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Degli Atti MLC, Merler S, Rizzo C, Ajelli M, Massari M, Manfredi P, Furlanello C, Tomba GS, Iannelli M. Mitigation measures for pandemic influenza in Italy: an individual based model considering different scenarios. PLoS One 2008;3:1–11. doi: 10.1371/journal.pone.0001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].DeMonte CM, DeMonte WD, Thorn BE. Future implications of eHealth interventions for chronic pain management in underserved populations. Pain Manag 2015;5:207–14. [DOI] [PubMed] [Google Scholar]
- [25].Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid MC, de C Williams AC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. PAIN 2020;161:889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Edwards R, Augustson E, Fillingim R. Differential relationships between anxiety and treatment-associated pain reduction among male and female chronic pain patients. Clin J Pain 2003;19:208–16. [DOI] [PubMed] [Google Scholar]
- [27].Gadhoke P, Pemberton S, Foudeh A, Brenton BP. Development and validation of the social determinants of health questionnaire and implications for “promoting food security and healthy lifestyles” in a complex urban food ecosystem. Ecol Food Nutr 2018;57:261–81. [DOI] [PubMed] [Google Scholar]
- [28].Gracely R, Geisser M, Giesecke T, Grant M, Petzke F, Williams D, Clauw D. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 2004;127:835–43. [DOI] [PubMed] [Google Scholar]
- [29].Grol-Prokopczyk H. Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. PAIN 2017;158:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hämmig O. Health risks associated with social isolation in general and in young, middle and old age. PLoS One 2019;14:e0222124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Harris RA. Chronic pain, social withdrawal, and depression. J pain Res 2014;7:555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging 2004;26:655–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and socioeconomic disparities in disabling chronic pain: findings from the health and retirement study. J Pain 2017;18:1459–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain 2010;11:1230–9. [DOI] [PubMed] [Google Scholar]
- [35].Karayannis NV, Baumann I, Sturgeon JA, Melloh M, Mackey SC. The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med 2019;53:65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Karos K, McParland JL, Bunzli S, Devan H, Hirsh A, Kapos FP, Keogh E, Moore D, Tracy LM, Ashton-James CE. The social threats of COVID-19 for people with chronic pain. PAIN 2020;161:2229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kim HJ, Yang GS, Greenspan JD, Downton KD, Griffith KA, Renn CL, Johantgen M, Dorsey SG. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. PAIN 2017;158:194–211. [DOI] [PubMed] [Google Scholar]
- [38].Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020;368:860–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Krahé C, Springer A, Weinman JA, Fotopoulou A. The social modulation of pain: others as predictive signals of salience - a systematic review. Front Hum Neurosci 2013;7:386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Long NJ. From social distancing to social containment: reimagining sociality for the coronavirus pandemic. Med Anthropol Theor 2020;7:247–60. [Google Scholar]
- [41].Mariano TY, Wan L, Edwards RR, Jamison RN. Online teletherapy for chronic pain: a systematic review. J Telemed Telecare 2019. doi: 10.1177/1357633X19871746 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [42].Mariano TY, Wan L, Edwards RR, Lazaridou A, Ross EL, Jamison RN. Online group pain management for chronic pain: preliminary results of a novel treatment approach to teletherapy. J Telemed Telecare 2019. doi: 10.1177/1357633X19870369. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [43].Marston HR, Musselwhite C, Hadley R. COVID-19 vs Social Isolation: the impact technology can have on communities, social connections and citizens. Br Soc Gerontol 2020. Available at: https://ageingissues.wordpress.com/2020/03/18/covid-19-vs-social-isolation-the-impact-technology-can-have-on-communities-social-connections-and-citizens/. [Google Scholar]
- [44].Mitsi V, Zachariou V. Modulation of pain, nociception, and analgesia by the brain reward center. Neuroscience 2016;338:81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Mogil JS. Social modulation of and by pain in humans and rodents. PAIN 2015;156(suppl 1):S35–41. [DOI] [PubMed] [Google Scholar]
- [46].Mogil JS. Social modulation of and by pain in humans and rodents. PAIN 2015;156:S35–41. [DOI] [PubMed] [Google Scholar]
- [47].Mogil JS, Bailey AL. Sex and gender differences in pain and analgesia. In: Progress in Brain Research. Vol. 186: Elsevier, 2010. pp. 140–57. [DOI] [PubMed] [Google Scholar]
- [48].Mossey JM. Defining racial and ethnic disparities in pain management. Clin orthopaedics Relat Res 2011;469:1859–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Murray TL, Jr, Daniels MH, Murray CE. Differentiation of self, perceived stress, and symptom severity among patients with fibromyalgia syndrome. Families Syst Health 2006;24:147. [Google Scholar]
- [50].Nandi M, Schreiber KL, Martel MO, Cornelius M, Campbell CM, Haythornthwaite JA, Smith MT, Wright J, Aglio LS, Strichartz G, Edwards RR. Sex differences in negative affect and postoperative pain in patients undergoing total knee arthroplasty. Biol Sex differences 2019;10:23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Núñez-Cortés R, Chamorro C, Ortega-Palavecinos M, Mattar G, Paredes O, Besoaín-Saldaña Á, Cruz-Montecinos C. Social determinants associated to chronic pain after total knee arthroplasty. Int Orthopaedics 2019;43:2767–71. [DOI] [PubMed] [Google Scholar]
- [52].Paller CJ, Campbell CM, Edwards RR, Dobs AS. Sex-based differences in pain perception and treatment. Pain Med 2009;10:289–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Pappot N, Taarnhøj GA, Pappot H. Telemedicine and e-health solutions for COVID-19: patients' perspective. Telemed J E Health; 2020;26:847–9. [DOI] [PubMed] [Google Scholar]
- [54].Peacock S, Patel S. Cultural influences on pain. Rev Pain 2008;1:6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Rahim-Williams FB, Riley JL, III, Herrera D, Campbell CM, Hastie BA, Fillingim RB. Ethnic identity predicts experimental pain sensitivity in African Americans and Hispanics. PAIN 2007;129:177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Roth RS, Punch MR, Bachman JE. Educational achievement and pain disability among women with chronic pelvic pain. J Psychosomatic Res 2001;51:563–9. [DOI] [PubMed] [Google Scholar]
- [57].Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess 1996;66:20–40. [DOI] [PubMed] [Google Scholar]
- [58].Schreiber KL, Campbell C, Martel MO, Greenbaum S, Wasan AD, Borsook D, Jamison RN, Edwards RR. Distraction analgesia in chronic pain patients: the impact of catastrophizing. Anesthesiology 2014;121:1292–301. [DOI] [PubMed] [Google Scholar]
- [59].Shah GH, Shankar P, Schwind JS, Sittaramane V. The detrimental impact of the COVID-19 crisis on health equity and social determinants of health. J Public Health Manage Pract 2020;26:317–19. [DOI] [PubMed] [Google Scholar]
- [60].Simons JS, Gaher RM. The distress tolerance scale: development and validation of a self-report measure. Motiv Emot 2005;29:83–102. [Google Scholar]
- [61].Smith TO, Dainty JR, MacGregor A. Changes in social isolation and loneliness following total hip and knee arthroplasty: longitudinal analysis of the English Longitudinal Study of Ageing (ELSA) cohort. Osteoarthritis Cartilage 2017;25:1414–19. [DOI] [PubMed] [Google Scholar]
- [62].Steglitz J, Buscemi J, Ferguson MJ. The future of pain research, education, and treatment: a summary of the IOM report Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Transl Behav Med 2012;2:6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Stine RA. Graphical interpretation of variance inflation factors. Am Statistician 1995;49:53–6. [Google Scholar]
- [64].Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995;7:524. [Google Scholar]
- [65].Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. PAIN 2002;96:319–24. [DOI] [PubMed] [Google Scholar]
- [66].Wentzel J, van der Vaart R, Bohlmeijer ET, van Gemert-Pijnen JE. Mixing online and face-to-face therapy: how to benefit from blended care in mental health care. JMIR Ment Health 2016;3:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Wilder-Smith A, Freedman D. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Trav Med 2020;27:taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Williams AC, Craig KD. Updating the definition of pain. PAIN 2016;157:2420–23. [DOI] [PubMed] [Google Scholar]
- [69].Williams SN, Armitage CJ, Tampe T, Dienes K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: a UK-based focus group study. BMJ Open 2020;20:e039334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].World Health Organization. Coronavirus disease 2019 (COVID-19): situation report. 63, 2020. Available at: https://apps.who.int/iris/handle/10665/331607 [Google Scholar]
- [71].World Health Organization. Coronavirus disease 2019 (COVID-19): situation report. 67, 2020. Available at: https://apps.who.int/iris/handle/10665/331613. [Google Scholar]
- [72].Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B221.