Abstract
Renal transplant recipients are at an increased risk of atypical nontuberculous mycobacterial (NTM) infections. Infections caused by NTM are uncommon in the general population, rarely occurring in immunocompetent individuals. NTM infections are an uncommon cause of tenosynovitis. Mycobacterium marseillense is a rare, atypical mycobacteria that has been reported to cause pulmonary and cutaneous infections; however, no previous reports of this pathogen causing tenosynovitis exist. This case reports a 73-year-old male renal transplant recipient who presented with chronic extensor tenosynovitis of the right hand caused by M marseillense. The patient was treated with radical extensor tenosynovectomy and 6 months of antibiotic treatment. A review of literature on tenosynovitis caused by atypical mycobacteria was performed. The patient successfully responded to treatment with no complications or recurrence of infection at the 18-month follow-up. Tenosynovitis of the hand caused by atypical mycobacteria is rare. A high index of suspicion is required to prevent a delay in diagnosis, particularly in immunocompromised individuals.
Immunocompromised patients including renal transplant recipients are at an increased risk of atypical nontuberculous mycobacterial (NTM) infections. Nontuberculous mycobacteria (NTM) are omnipresent environmental organisms, consisting of over 150 distinct species, found in soil, water, and other reservoirs.1 Infections caused by NTM are uncommon in the general population, rarely occurring in immunocompetent individuals.2,3 Manifestations of NTM infections can be observed as cutaneous disease, osteoarticular disease, pulmonary disease, or disseminated disease. The most observed species causing NTM infections in renal transplant recipients are Mycobacterium chelonae and Mycobacterium kansasii.2,4 Recently, Mycobacterium marseillense has been reported as the cause of pulmonary and cutaneous infections; however, there have been no previous reports of this pathogen causing tenosynovitis.
Case Report
This case reports a 73-year-old man with a history of polycystic kidney disease after deceased donor kidney transplantation on tacrolimus, mycophenolic acid, and prednisone who presented to the office with a 1-year history of a progressively enlarging painless right dorsal wrist mass. He first noticed the mass a few weeks after his kidney transplant. He denied pain, weakness, or paresthesia in his right hand and wrist. His primary concern included the dorsal, painless mass. Examination revealed a soft-tissue mass 5 × 7 cm in size overlying the fourth dorsal compartment. The mass was soft, mobile, and nonpulsatile. The mass moved with flexion and extension of the digits. No neurovascular deficits were appreciated. MRI of the wrist demonstrated innumerable rice bodies within the fourth dorsal compartment with distension of the tendon sheath and a partial rupture of the extensor digitorum communis (EDC) tendon to the index finger (Figure 1). There was no preoperative detectable weakness in extension of the index finger. These findings along with a history of immunosuppression were strongly suggestive of infectious extensor tenosynovitis. Surgical intervention consisting of right dorsal wrist irrigation and débridement and extensor tenosynovectomy of the fourth dorsal compartment was proposed, and the patient elected to proceed.
Figure 1.
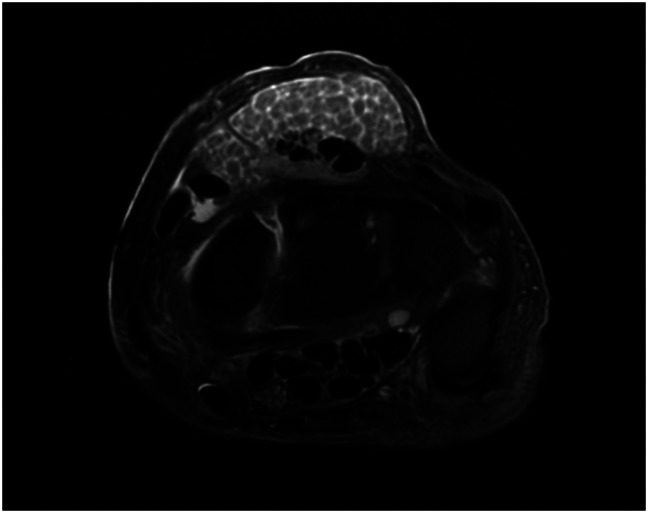
T2-weighted axial MRI of the right wrist demonstrate innumerable rice bodies within the fourth dorsal compartment with distension of the tendon sheath and a partial rupture of the extensor digitorum communis.
A fourth dorsal compartment tenosynovectomy was performed, revealing innumerable tan-yellow rice bodies. The rice bodies were sent for culture and pathology. A partial rupture of the EDC tendon to the index finger (>50% intact) as previously seen on the MRI was identified and was treated with débridement alone. He tolerated the procedure well with no immediate complications and was discharged on the same day.
Histopathologic Findings/Cultures
Histological examination of the specimen revealed synovial hyperplasia and numerous palisading granulomas with focal necrosis. Grocott methenamine silver and acid-fast bacilli (AFB) stains were performed and were negative for microorganisms. This pattern was suggestive of necrotizing granulomatous tenosynovitis. AFB culture yielded M marseillense after 10 days with susceptibility to all tested antibiotics (amikacin, linezolid, clarithromycin, and moxifloxacin). Aerobic, anaerobic, and fungal cultures yielded no growth after 3 days per our institutional protocol.
Follow-up
Because the culture yielded M marseillense, the infectious disease service recommended treatment with azithromycin 500 mg daily, rifabutin 300 mg daily, and ethambutol 400 mg daily to be taken for 6 months. At the 3-, 6-, 10-, and 18-month follow-ups, the incision was well-healed with no recurrence of mass (Figure 2). He tolerated the antibiotic treatment regimen well. His EDC function remained intact and had no neurovascular deficits.
Figure 2.
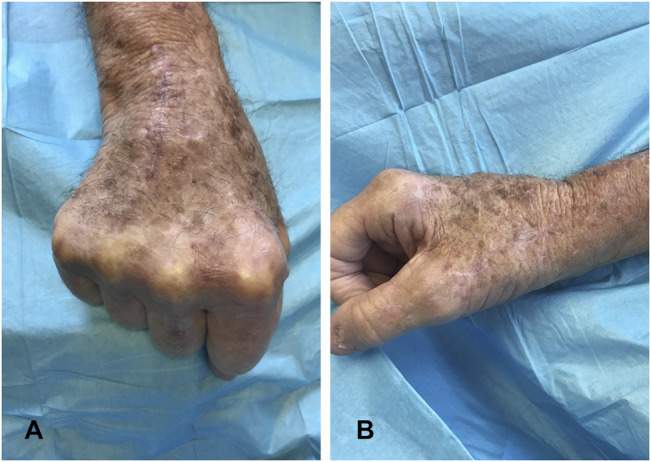
Photograph showing the dorsal (A) and lateral (B) aspects of the right wrist 3 months after radical extensor tenosynovectomy.
Discussion
To our knowledge, this is the first reported case of tenosynovitis caused by M marseillense. Among renal transplant patients, the reported incidence of NTM infections is between 0.16% and 0.38%.5 Atypical NTM infections in immunocompetent patients are uncommon, and when they occur, 90% of cases commonly affect the lungs, making NTM tenosynovitis an even rarer occurrence.6 These infections often occur because of previous trauma, surgery, corticosteroid injections, or nonapparent inoculation from contaminated sources. The most commonly reported site for NTM tenosynovitis is the fourth dorsal extensor compartment because of the highest risk of penetrating injury to this area in the hand and wrist.6-8 Previous case reports demonstrate favorable outcomes with no recurrence with adequate débridement and tenosynovectomy.6-8 In the case of our patient, no report of previous trauma or penetrating injury to the hand as a potential source for inoculation was observed. A variety of fast- and slow-growing NTM species have been isolated as causes of tenosynovitis, including M chelonae, Mycobacterium malmoense, Mycobacterium abscessus and more commonly, Mycobacterium marinum and M kansasii.6-12 M marseillense is a more recent discovery that until now has been described as causing infections with pulmonary, lymphatic, and cutaneous involvement.3,13-15,21
Mycobacterium marseillense was first described in 2009 as a new species belonging to the Mycobacterium avium complex phylogenetic group, originally isolated from respiratory specimens. It is a small, slow-growing, acid-fast, gram-positive bacilli showing close similarity to Mycobacterium chimaera and Mycobacterium intracellulare.3,9,13,16 Although NTM infections are generally uncommon in immunocompetent patients, there have been multiple reported cases of M marseillense occurring in immunocompromised patients. Therefore, one should include M marseillense in the differential diagnosis in treating individuals presenting with a slowly growing mass in the hand of an immunocompromised patient.
Clinical awareness of this entity is essential for diagnosis of atypical NTM tenosynovitis. Because M marseillense is slow-growing and painless, the time from onset to diagnosis can be anywhere from 6 months to 1 year. This delay in diagnosis and treatment can ultimately lead to tendinous disruption and bony involvement resulting in other complications. As noted in our patient, a partial tear of the EDC to the index finger was reported on the MRI and confirmed intraoperatively. The absence of clinical signs such as pain, fever, and erythema along with negative inflammatory markers such as a normal erythrocyte sedimentation rate and C-reactive protein make the diagnosis of M marseillense challenging.12,17 MRI can be helpful for diagnosis as well, showing synovial thickening around the tendons and fluid within the tendon sheaths. Rice bodies, seen on MRI or on gross intraoperative inspection may be suggestive but not pathognomonic for M marseillense as rice bodies can also be seen in other inflammatory conditions such as rheumatoid arthritis and seronegative inflammatory arthritis.12,17,18 Perioperatively, AFB cultures are essential for the diagnosis of M marseillense. Although AFB stains may be useful for immediate diagnosis of an NTM infection with >95% positive predictive value, it has been shown to have a 20% to 90% sensitivity depending on mycobacterial burden.19 Thus, current guidelines recommend continuing AFB cultures for 18 to 24 days to confirm negative growth after a negative AFB stain.20 Based on this case report, the authors propose consideration for tenosynovectomy and multidrug antimycobaterial therapy in the treatment of M marseillense in the hand and wrist.
Conclusion
Tenosynovitis of the hand caused by atypical mycobacteria is rare. To our knowledge, this is the first reported case of M marseillense infection causing tenosynovitis in an immunocompromised patient. Diagnosis of tenosynovitis can be difficult because often no physical signs of acute or chronic infections exist, and erythrocyte sedimentation rate and C-reactive protein levels are typically normal. A high index of suspicion is required to prevent a delay in diagnosis and treatment, particularly in immunocompromised individuals.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Hirase, Dr. Le, Dr. Jack, Dr. Siff, and Dr. Liberman.
References
- 1.Saiman L: The mycobacteriology of non-tuberculous mycobacteria. Paediatr Respir Rev 2004;5(suppl A):S221-S223. [DOI] [PubMed] [Google Scholar]
- 2.Abad CL, Raymund RR: Non-tuberculous mycobacterial infections in solid organ transplant recipients: An update. J Clin Tuberc Other Mycobact Dis 2016;4:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azzali A, Montagnani C, Simonetti MT, et al. : First case of Mycobacterium marseillense lymphadenitis in a child. Ital J Pediatr 2017;43:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho TA, Rommelaere M, Coche E, et al. : Nontuberculous mycobacterial pulmonary infection in renal transplant recipients. Transpl Infect Dis 2010;12:138-142. [DOI] [PubMed] [Google Scholar]
- 5.Doucette K, Fishman JA: Nontuberculous mycobacterial infection in hematopoietic stem call and solid organ transplant recipients. Clin Infect Dis 2004;38:1428-1439. [DOI] [PubMed] [Google Scholar]
- 6.Yoon HJ, Kwon JW, Yoon YC, et al. : Nontuberculous mycobacterial tenosynovitis in the hand: Two case reports with the MR imaging findings. Korean J Radiol 2011;12:745-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blood TD, Morrell NT, Weiss AP: Tenosynovitis of the hand and wrist: A critical analysis review. JBJS Rev 2016;4:e7. [DOI] [PubMed] [Google Scholar]
- 8.Mahajan NP, Palange ND, Pawar E, et al. : Surgical treatment of tenosynovitis of extensor tendons of fourth compartment of wrist in nonrheumatoid patients: A case series of 10 patients in India. J Hand Microsurg 2019;11:45-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salah B, Cayrou C, Raoult D, et al. : Mycobacterium marseillense sp. nov., Mycobacterium timonense sp. nov. and Mycobacterium bouchedurhonense sp. nov., members of the Mycobacterium avium complex. Int J Syst Evol Microbiol 2009;59:2803-2808. [DOI] [PubMed] [Google Scholar]
- 10.Chan E, Bagg M: Atypical hand infections. Orthop Clin North Am 2017;48:229-240. [DOI] [PubMed] [Google Scholar]
- 11.van Grootveld R, Scherer HU, Peters EEM, et al. : Tenosynovitis caused by Mycobacterium malmoense in two kidney transplant recipients and review of the literature. Transpl Infect Dis 2018;20:e12810. [DOI] [PubMed] [Google Scholar]
- 12.van Mechelen M, van der Hilst J, Gyssens IC, Messiaen P: Mycobacterial skin and soft tissue infections: TB or not TB? Neth J Med 2018;76:269-274. [PubMed] [Google Scholar]
- 13.van Ingen J, Turenne CY, Tortoli E, et al. : A definition of the Mycobacterium avium complex for taxonomical and clinical purposes, a review. Int J Syst Evol Microbiol 2018;68:3666-3677. [DOI] [PubMed] [Google Scholar]
- 14.Kim SY, Yoo H, Jeong BH, et al. : First case of nontuberculous mycobacterial lung disease caused by Mycobacterium marseillense in a patient with systemic lupus erythematosus. Diagn Microbiol Infect Dis 2014;79:355-357. [DOI] [PubMed] [Google Scholar]
- 15.Grottola A, Roversi P, Fabio A, et al. : Pulmonary disease caused by Mycobacterium marseillense, Italy. Emerg Infect Dis 2014;20:1769-1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tortoli E: Microbiological features and clinical relevance of new species of the genus Mycobacterium. Clin Microbiol Rev 2014;27:727-752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanal HT, Zor F, Kocaoğlu M, Bulakbaşi N: Atypical mycobacterial tenosynovitis and bursitis of the wrist. Diagn Interv Radiol 2009;15:266-268. [DOI] [PubMed] [Google Scholar]
- 18.Chau CL, Griffith JF, Chan PT, Lui TH, Yu KS, Ngai WK: Rice-body formation in atypical mycobacterial tenosynovitis and bursitis: Findings on sonography and MR imaging. AJR Am J Roentgenol 2003;180:1455-1459. [DOI] [PubMed] [Google Scholar]
- 19.Lipsky BA, Gates J, Tenover FC, Plorde JJ: Factors affecting the clinical value of microscopy for acid-fast bacilli. Rev Infect Dis 1984;6:214-222. [DOI] [PubMed] [Google Scholar]
- 20.Caulfield AJ, Wengenack NL: Diagnosis of active tuberculosis disease: From microscopy to molecular techniques. J Clin Tuberc Other Mycobact Dis 2016;4:33-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xie B, Chen Y, Wang J, et al. : Mycobacterium marseillense infection in human skin, China, 2018. Emerg Infect Dis 2019;25:1991-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]


