Supplemental Digital Content is available in the text
Keywords: bariatric surgery, sleeve gastrectomy, complications, orogastric tube, nasogastric tube, bougie
Abstract
Background:
Entrapment of an orally introduced tube by stapling/stitching is an intra-operative complication of bariatric surgery with grave consequences. Incidence is unknown. No prevention/management strategy is available. A systematic review was performed to assess the absolute reported observed risk and incidence. Additionally, data on 3 cases during our entire sleeve gastrectomy (SG) experience is evaluated.
Methods:
Literature is reviewed using PubMed/Web of science data-bases. Data was recorded prospectively. Videos of orally introduced tube staplings were re-watched, presentation/recognition/management were re-evaluated. A protocol ensuring the removal of the small caliber orogastric tube (OGT) by the surgeons direct inspection was introduced after the 3rd entrapment.
Results:
Review revealed OGT as the most commonly entrapped tube following temperature probe and bougie. SG/stapling were the most common causative operation/reason, respectively. Leak rates over 20%, conversion, early-late re-operations and mortality were reported. During our 948 consecutive SGs, 3 OGT entrapments (0.32%), third one with double stapling, occurred. All were recognized/managed intraoperatively by freeing the entrapped-end of the OGT from the sleeve part of the staple-line. In doubly stapled case, second transected end could only be recognized when routine reinforcement suturing come in proximity. Defects were continuously stitched with barbed suture. No morbidity occurred. One-year excess-weight-loss was 82%. A pre-protocol incidence of 0.56% (n: 3/534) dropped to nil in the remaining 414.
Conclusion:
Iatrogenic stapling of the OGT during SG is rare, but morbid. It must be avoided by a strict protocol. Upon occurrence/recognition, stapling must immediately stop until the “entirety” of the tube, including the “specimen-part”, is retrieved, to avoid double entrapment.
1. Introduction
Bariatric operations, sleeve gastrectomy (SG) in particular, are being increasingly performed world-wide during the obesity pandemic. Decompression of the stomach by a small-caliber orogastric-tube (OGT), which is frequently accomplished by a nasogastric, is almost routine during the start of all laparoscopic bariatric procedures since evacuation of the gastric content is immediately needed, before the insertion of the first trocar. Although the OGT must be removed prior to stapling as a rule, not only OGTs but thermal probes and even bougies were reportedly stapled and transected.[1–11] These iatrogenic misadventures, besides causing longer operations, were associated with major sequelae such as increased leak risk,[1,4,7] early[2,4] or late re-operations[8] and even death.[7] Published data is surprisingly scarce. An excellent editorial has rightly commented on the underreported nature of this complication[10] and the real incidence remains unknown. No specific guidelines for prevention/management are available.
Besides a systematic review of the incidence/outcome data of the available reports, we present 3 cases with inadvertent stapling of OGTs during 948 consecutive SGs. A double stapling, which can easily be missed unless looked for, is described. A strategy to eliminate the possibility of double stapling is suggested. Finally, we report our experience with a prevention protocol.
2. Materials and methods
2.1. Systematic review
2.1.1. Inclusion criteria
The search subject was orally introduced tube (OGT, temperature probe, bougie) entrapments resulting from inadvertent stitching/stapling during a bariatric procedure. Reports including outcome data and were published in peer reviewed journals were included.
2.1.2. Exclusion criteria
Similar tube entrapments that were reported to occur during other upper abdominal surgical procedures rather than bariatric surgery and bariatric cases without outcome data were excluded.
In accordance with Gosseen et al literature search strategy for reviews in surgery [12], PubMed-MEDLINE and Web of Science databases were used without language restriction by combining key words “nasogastric”, “orogastric”, “bougie”, “sleeve gastrectomy”, “gastric bypass”, “duodenal switch”.
2.2. Clinical data
All data, including intraoperative problems such as OGT entrapment and operative footage were recorded/stored in digital platform prospectively. The same tube (Levin-nasogastric, 6x1210 mm, Biçakcilar A.Ş., İstanbul, Turkey) was routinely used trans-orally to decompress the stomach prior to trocar insertions. No esophageal thermal probes were used.
2.2.1. Surgery
All SGs were performed by the senior author or under his direct supervision by3 primary surgeons. Using an optical trocar for first entry, after full mobilization, an SG over a bougie was done starting 3 to 4 cm from the pylorus. The 36-Fr compressible bougie was abandoned after the 522nd case and a blunt tipped, flexible, incompressible 42-Fr bougie (Hurst, tungsten-filled esophageal bougie, Teleflex-Pilling, Morrisville-NC, USA) was used in the remaining 426. Manually and electrically driven staplers were used in 909 (95.9%) and 39 (4.1%) patients respectively. During all SGs, the staple line was reinforced with full-thickness, continuous stitching utilizing 000, 6 inches, barbed suture material (V-Loc 180; Medtronic, Minneapolis, MN, USA). Methylene blue leak test was not routine but was performed selectively as in the presented cases. All SGs were drained with a 7 mm Jackson-Pratt drain which was withdrawn on the 3rd postoperative day, before discharge, in accordance with our protocol. No nasogastric tube was used postoperatively. Postoperative day one upper gastrointestinal series was routine.
Videos of OGT entrapment cases were re-watched in detail to assess how the incident first presented itself, when it was recognized, at which stapling it occurred, and how it was managed. Results on duration of surgery, discharge day, complications and weight loss were retrieved from the prospective database.
After the third case, a protocol on OGT usage was developed. Once all the trocars were in place and the stomach was seen to be adequately decompressed, dissection was only allowed after the primary surgeon saw the disposed OGT in the bin. The nurse was not allowed to open a stapler without re-confirming this disposal with the surgeon.
The study is approved by the institutional review board and written informed consent is obtained from all patients.
3. Results
3.1. Systematic review
The review initially identified 11 articles reporting on orally introduced tube entrapments during a bariatric surgery.[1–11] PRISMA chart is presented in Figure 1. One was an editorial comment, admitting to 2 previous bariatric operations where small-caliber OGTs were inadvertently stapled, without any further data[10] and excluded. Another was a review based on the Food and Drug Administrations Manufacturer and User Facility Device Experience (MAUDE) data which revealed 7 GastriSailTM bougie entrapments without any outcome information.[11] Although excluded from the analysis, it is important to note that none of these GastriSaiLTM bougie entrapments have been reported in the medical literature. Nine articles provided data to analyze; 6 were anecdotal case reports[2,3,5–7,9] and 3 were case series including a national survey from Israel[4] and 2 retrospective analyses reporting on consecutive series of patients[1,8] (Table 1). This limited dataset on 36 patients showed that; small-caliber OGT was the most commonly entrapped tube, stapling was the main reason of entrapment and SG was the most common causative operation. In addition, both reported[4,8] and unreported[11] data emphasized that bougie transections are real, highly morbid and underreported (Table 1).
Figure 1.
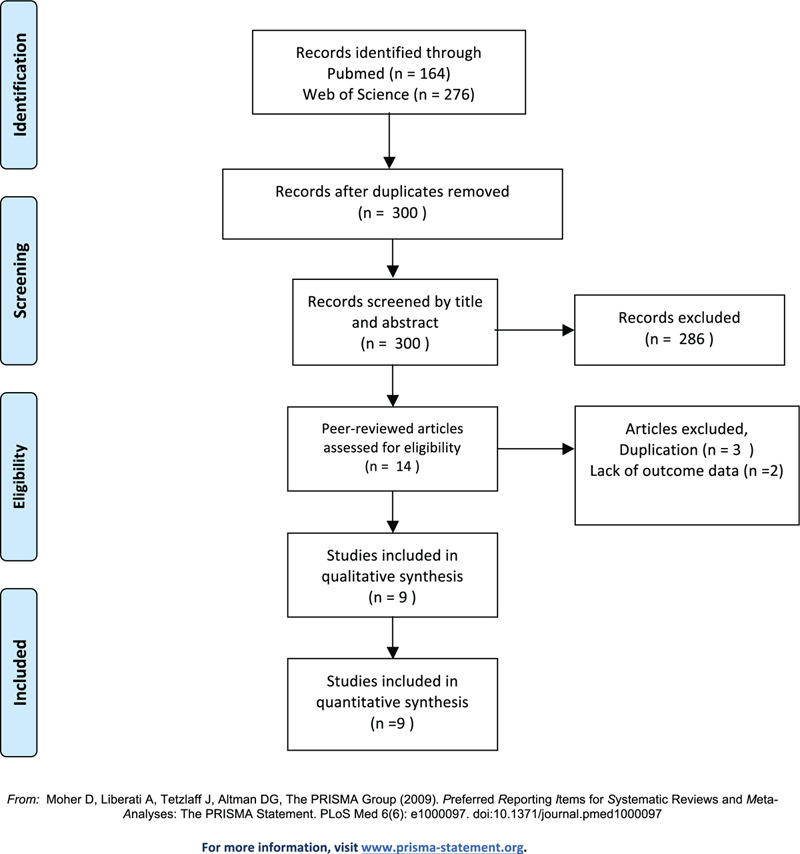
PRISMA flow chart.
Table 1.
All publications reporting data on orally introduced and inadvertently entrapped tubes during bariatric operations in chronological order.
| Author | Study type | Number of entrapments/total cases (%) | Type of operation (n) | Small-caliber OGT/Temperature probe/Bougie | Stapled/Stitched | Morbidity and Mortality |
| Sanchez[1] | Two centers Retrospective analysis of consecutive cases | 9/727 (1.2) | RYGB (727) | 7/2/0 | 7/2 | 22% open conversion 22% leak |
| Péquignot[2] | Case report | 1 (NA) | SG (1) | 1/0/0 | 1/0 | Not recognized intraoperatively Re-surgery + endoscopically managed |
| Sucandy[3] | Case report | 1 (NA) | DS anastomosis (1) | 1/0/0 | 0/1 | Not recognized intraoperatively Endoscopically managed |
| Abu-Gazala[4] | National survey | 17/2444 (0.69) | SG (1847) RYGB (597) | 8/6/3 | 17/0 | 17.6% leak Resurgery (n:1) Unplanned RYGB (n:1) Open conversion (n:1) |
| Higa[5] | Case report | 1 (NA) | SG to RYGB conversion (1) | 1/0/0 | 1/0 | No |
| Shivaram[6] | Case report | 1 (NA) | SG (1) | 1/0/0 | 1/0 | No |
| Kayaalp[7] | Case series | 2 (NA) | RYGB (2) | 2/0/0 | 2/0 | No |
| Baltasar[8] | Single center Retrospective analysis of consecutive cases | 3/1284 (0.23) | SG (312) SG part of DS (972) | 0/0/3 | 3/0 | 66.6% leak Mortality (n:1) |
| Rizk[9] | Case report | 1 (NA) | RYBG (1) | 1/0/0 | 1/0 | Gastro-gastric fistula required re-surgery (n:1) |
| Çalikoğlu | Single center Observational study from prospective data base | 3/948 (0.32) | SG (948) | 3/0/0 | 3/0 | No |
OGT = orogastric tube; RYGB = Roux-en-Y gastric bypass; NA = not applicable; SG = sleeve gastrectomy; DS = duodenal switch.
3.2. Clinical data
Between January 2012 and February 2020, 948 consecutive SGs were performed. No bougie entrapment occurred. Three small-caliber OGT staplings occurred during the 13th, 417th, and 534th SG. Three primary surgeons had one entrapment each, occurring at 12th, 145th, and 52nd cases of their entire experience. Patient demographics are summarized in Table 2. The third case had a doubly stapled OGT. The overall incidence was 0.32% (3/948). Before the protocol, the incidence was 0.56% (3/534) which dropped to zero in the remaining 414 cases.
Table 2.
Demographics and outcome data.
| SG number | Sex | Age | BMI prior to SG (kg/m2) | Operation | Duration of surgery (minutes) | Length of stay (days) | %EWL at 1 year |
| 13th | Male | 52 | 39 | SG | 165 | 3 | 84.2 |
| 417th | Female | 39 | 45 | SG | 150 | 3 | 82.6 |
| 534th | Female | 36 | 42 | SG/cholecystectomy | 245 | 3 | 80 |
SG = sleeve gastrectomy; BMI = body mass index; %EWL = excess weight loss.
The incident was never recognized by the surgeon before cutting the OGT, although a manually driven stapler was used at each instance (60 mm, ECHELON FLEX ENDOPATH Staplers, Ethicon, Cincinnati, OH, USA). The complication was immediately recognized upon opening the first stapler, when the transected ends of the OGT became obviously visible in 2 patients (Fig. 2, Fig. 3). They were managed by freeing the stapled OGT end within the sleeve and sewing this defect (see Video, Supplemental Video 1 (http://links.lww.com/MD/F517), footages on OGT entrapment in cases 1 and 2). The specimen part of the transected tube was not addressed, further stapling was carried out and the distal OGT was retrieved with the specimen. In doubly stapled case, entrapments occurred at the 4th and 5th staplings (Fig. 4). The entrapment was visible after the opening of the 4th stapler when the video is re-watched, but that was overlooked. It became evident a few minutes later when the anesthesiologist pulled on the tube as shown in the video (see Video, Supplemental Video 2 (http://links.lww.com/MD/F518), footage on doubly entrapped OGT in the third case). After managing this obvious entrapment similarly, we fired the 5th stapler without making sure the entirety of OGT was out, since the possibility of double stapling never occurred to us. The second entrapped/cut end was not seen immediately and could be recognized only when reinforcement stitching came in proximity to the stapled OGT (Fig. 4B). No intraoperative gastroscopy was used. No conversions occurred and drainage was standard. Operative and follow-up data is presented in Table 2. The concomitant cholecystectomy added 50 minutes to the duration of surgery in case 3. Trocar site infection, the sole complication, resolved with drainage and antibiotics.
Figure 2.
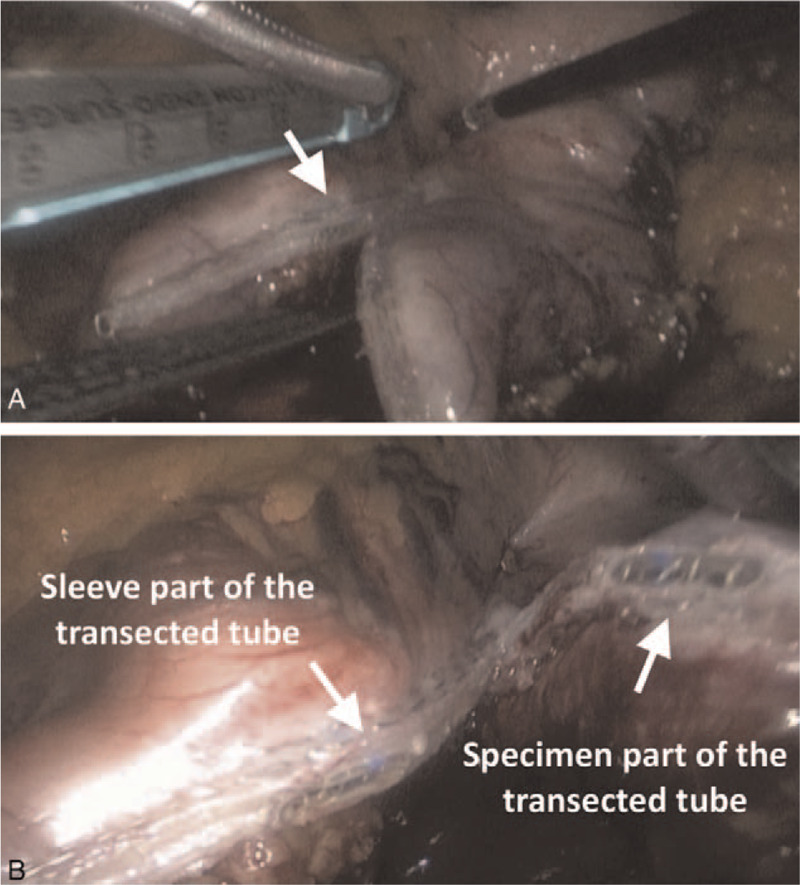
Case 1. (A) Transection becoming immediately obvious upon opening the first stapler, (B) both transected ends of the orogastric tube.
Figure 3.
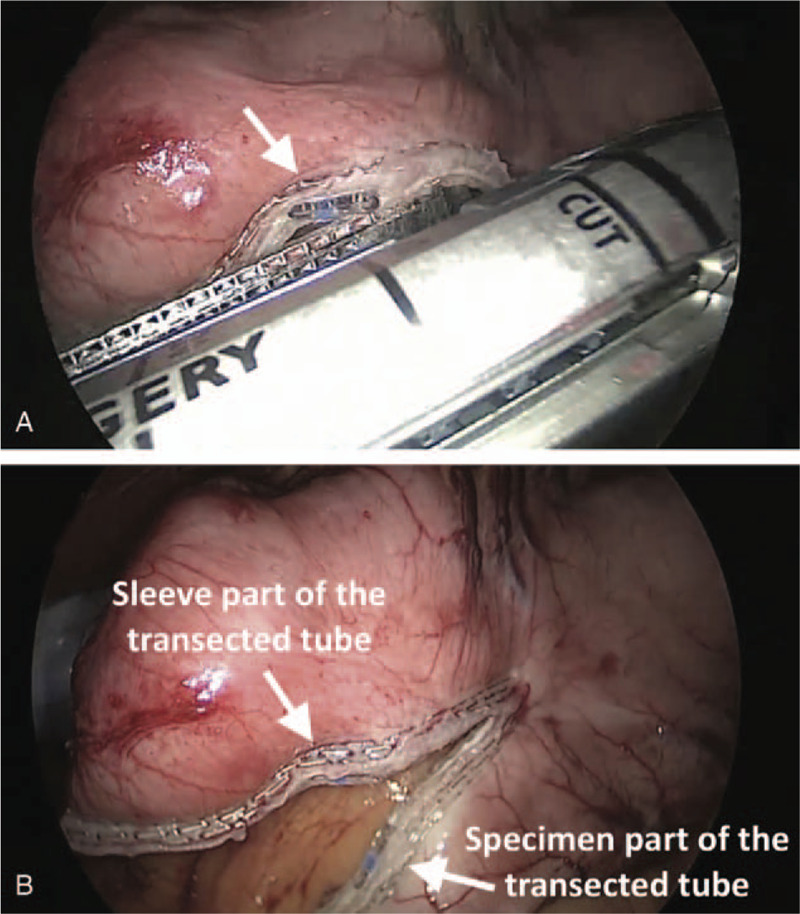
Case 2. (A) Transection becoming immediately obvious upon opening the first stapler, (B) both transected ends of the orogastric tube.
Figure 4.
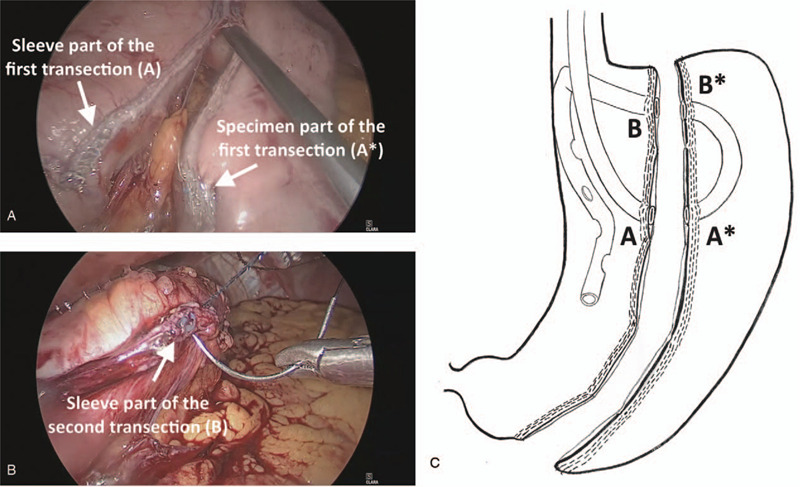
Case 3. (A) Overlooked first transection which became evident when the anesthetist pulled the orogastric tube, (B) recognition of the second transection during routine reinforcement stitching. Note that this end of the tube was not in reach for the anesthetist, (C) Depiction of the doubly entrapped case. A-A∗ corresponds to the first, B-B∗ corresponds to the second transection.
4. Discussion and conclusion
The review identified 36 reported cases of iatrogenic stapling of an intraluminal tube during various bariatric procedures (i.e.,: SG,[2,4,6,8] Roux-en-Y gastric bypass (RYGB)[1,4,5,7,9] and duodenal switch[3,8]). However, it also raised concern that such incidents are more common than reported as shown by the MAUDE data[11] and also noted by others[6,10]. Besides self-admitting to 2 “unreported” small-caliber OGT staplings, an editorial[10] stated that; “the true number of surgeons who are willing to acknowledge the event in public is low; however, 25% to 50% of many seminar participants acknowledged having stapled a “tube” during laparoscopic bariatric surgery, although published reports never listed this intraoperative complication”.
However, “the shame” upon inadvertently transecting a tube, must not result in underreporting given the grave nature of the reported outcomes (Table 1). In terms of incidence, 1.2% incidence in 727 consecutive RYGBs[1] and very recently, a 0.23% incidence in 1284 consecutive SGs have been reported.[8] In a multi-center survey including all 43 bariatric surgeons of Israel,[4] responders reported 17 entrapments with 0.5% and 0.75% incidences in RYGB and SG respectively. If we assume non-responders had zero entrapments, the incidence was 0.45% in 3092 SGs. The rates mentioned above[1,4,8] and the 0.32% rate presented herein deserve attention since they reflect unbiased incidences, because of zero exclusions and impossibility of duplicate cases. Similar to our experience, both the Israeli[4] and Sanchez et al[1] data also showed that, the entrapments had occurred early on during the primary surgeons over-all experience or early in the surgeons experience in a new hospital setting. Hence, all available information suggests that a few cases in every thousand may be expected, especially during the early phase of multi-surgeon bariatric programs that are booming world-wide. Arguably, absence of tactile feed-back during laparoscopy, may be responsible.
Reported management strategy includes; freeing the entrapped end within the sleeve, removal the tube by the anesthetist and laparoscopic repair of the defect by suturing or re-stapling.[1,4,8] In the Israeli survey reporting on 17 entrapments, the described approach resulted in; open conversion; re-operation; an unplanned RYGB instead of an SG in 3 different patients and a 17.6% leak rate[4] (Table 1). Duration of surgery and hospital stay were 105.4 minutes and 6.2 days respectively in SGs. In the single report on RYGBs, 7 OGTs and 2 thermal probes were entrapped.[1] No mortality, but a 33% rate of life-threatening complications (2 leaks, 1 pulmonary insufficiency requiring tracheostomy) occurred with a 22% open conversion rate. Average operating time and length of stay were 318 minutes and 10.7 days respectively. Baltasar et al[8], recently, reported 3 compressible bougie staplings during 1284 SGs. Management was similar. Two patients leaked and 1 died (Table 1). One leak could only be finalized with total gastrectomy 3 years later. All 6 anecdotal reports addressed entrapped OGTs. Importantly, 3 reported intra-operatively overlooked entrapments requiring endoscopic removal [2,3], emergency[2] or late[9] re-surgery. A stapled OGT remnant was found to be entrapped 3 years later at the blind part of the RYGB, during an assessment of a gastro-gastric fistula.[9] Surgical management strategy was similar in all, including the first case of a double entrapment recently reported.[7]
Surprisingly, not only OGTs[1–7,9–11] and temperature probes,[1,4] but also bougies[4,8,11] were stapled during bariatric procedures. The MAUDE data[11] commenting on 7 “unreported” bougie entrapments and the extreme morbidity associated with bougie entrapments in Baltasar et al series[8] is alarming. Even a mortality was reported due to a stapled bougie after an SG.[8] Clearly, compressible/hollow bougies having parts that a stapler can easily close on must be abandoned to eliminate their transection. Blunt tipped, flexible, incompressible bougies, if used with caution and good cooperation with the anesthesiologist, are almost void of complications.
One national survey[4] and 2 available consecutive series[1,8] reported very high morbidity and 3 of 5 case-reports, referring to intraoperatively overlooked entrapments, required further interventions, in contrast to our experience. However, our operating time also increased more than an hour compared to our average (103.3 ± 23.6 minutes in 944 SGs, unpublished data) and the double entrapment case lasted 3 hours excluding the duration of cholecystectomy (Table 2). We are aware that the situation is far more complex during a RYGB and higher morbidity in Sanchez et al paper is understandable.[1] Since the remnant stomach is to be preserved, retrieval of the distal tube with repair of this second defect is essential and a gastrostomy may be needed as stated.[1,9] The bougie, instead of a small-caliber OGT may be the reason for the extreme morbidity in Baltasar et al report[8] since it caused a larger defect. It is also noteworthy that one of the SGs were performed as a part of a more complicated, switch procedure. Outcome comparison with the Israeli survey[4] is also not possible because it included RYGBs and bougie entrapments. Nevertheless, continuous, full-thickness suturing with barbed suture satisfactorily repaired all 4 defects. Avoiding knot formation and the self-locking property of the suture matched expectations. In contrast to meticulous stitching, re-stapling may cause functional stenosis if used at the mid-gastric portion and was avoided.
The double stapling case taught us a lesson. As a rule, upon recognition of an OGT stapling during SG, stapling must immediately stop. First, both transected ends of the tube must be freed and retrieved. The proximal part which is in reach to the anesthetist will be removed by pulling it out orally. The distal part, however, must be removed laparoscopically by the surgeon. If both parts are taken out with ease and the entirety of OGT is out, then double entrapment cannot occur and stapling may resume. This detail has not been reported before and we also failed to observe this practice in our patients. We avoided double entrapment in the first 2 cases, only by luck. If an OGT is already stapled multiple times, the end which is not in reach for the anesthetist may be easily overlooked intraoperatively, since withdrawing the tube will have no visual effect. Fortunately, our routine stitching practice made it possible for us to recognize the 2th stapling. Intraoperative recognition is mandatory to prevent additional morbidity. Entrapped thermal probes and OGTs, diagnosed after bariatric surgery were reported to require endoscopic interventions[2,3] and emergency[2] or late re-surgeries.[9]
Since OGT stapling is totally preventable, if considered like “retention of foreign body” or “wrong side surgery”, can become a subject of litigation, as rightly stated.[4] For better prevention, increased cooperation between the anesthesiologist and the surgeon is repeatedly emphasized.[1–9] Dr. Champion enforced a special prevention protocol after experiencing 2 small-caliber OGT entrapments.[10] We adopted a similar strategy. We never use esophageal thermal probes and only blunt tipped, flexible, incompressible bougies are currently utilized. Similar to Dr. Champions protocol, the surgeon has full responsibility to ensure the entire OGT is withdrawn by his direct visual confirmation before starting the dissection. Nurse will also ask for a “time-out” prior to staple opening to re-ensure. Reportedly, the OGTs were inadvertently pushed back into the stomach during bougie insertions if they were not completely removed when asked.[2,4] This may also have been the case in our pre-protocol experience. Although increased awareness and experience may also have had an influence, our new protocol resulted in the elimination of any entrapment.
In conclusion, intraluminal tube stapling during bariatric surgery is a rare, but potentially serious complication which is underreported. Abandonment of thermal esophageal probes and compressible bougies in bariatric practice will certainly reduce the incidence. Incompressible bougies, on the other hand, must be certainly used with great care to avoid perforation but this complication is extremely rare with blunt tipped, flexible ones.
Unless a hollow/compressible bougie is used for both decompression and calibration, we cannot abandon OGTs, and bariatric surgery, SG in particular, is on the rise. Surgeons who are developing new programs must be extremely cautious since OGT or bougie entrapments are completely preventable and can become a judicial issue. For prevention, specific protocols must be implemented. If a tube is entrapped, prompt recognition and stopping further stapling is essential to avoid double entrapment. Retrieval of the entire OGT (both ends) and then closing the defect by continuous, full-thickness suturing seems to be satisfactory for management.
Acknowledgments
The authors would like to thank Murat Akyol M.D., F.R.C.S. for reviewing the manuscript.
Author contributions
Conceptualization: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Data curation: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Investigation: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Methodology: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Resources: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Supervision: Mehmet Ali Yerdel.
Visualization: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Writing – original draft: Mehmet Ali Yerdel.
Writing – review & editing: İsmail Çalikoğlu, Görkem Özgen, Mehmet Ali Yerdel.
Glossary
Abbreviations: MAUDE = manufacturer and user facility device experience, OGT = orogastric tube, RYGB = Roux en Y Gastric Bypass, SG = sleeve gastrectomy.
References
- [1].Sanchez BS, Safadi BY, Kieran JA, et al. Orogastric tube complications in laparoscopic Roux-en-Y gastric bypass. Obes Surg 2006;16:443–7. [DOI] [PubMed] [Google Scholar]
- [2].Péquignot A, Dhahri A, Mensah E, et al. Stapling and section of the nasogastric tube during sleeve gastrectomy: how to prevent and recover? Case Rep Gastroenterol 2011;5:350–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sucandy I, Antanavicius G. A novel use of endoscopic cutter: endoscopic retrieval of a retained nasogastric tube following a robotically assisted laparoscopic biliopancreatic diversion with duodenal switch. N Am J Med Sci 2011;3:486–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Abu-Gazala S, Donchin Y, Keidar A. Nasogastric tube, temperature probe, and bougie stapling during bariatric surgery: a multicenter survey. Surg Obes Relat Dis 2012;8:595–600. [DOI] [PubMed] [Google Scholar]
- [5].Higa G, Szomstein S, Rosenthal R. Stapling of orogastric tube during gastrojejunal anastomosis: an unusual complication after conversion of sleeve gastrectomy to laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 2012;8:116–8. [DOI] [PubMed] [Google Scholar]
- [6].Shivaram HV, Kumar A, Channappa M. Stapling and section of nasogastric tube during sleeve gastrectomy. Obes Surg 2012;22:1327–8. [Google Scholar]
- [7].Kayaalp C, Aydin C, Gozeneli O. Stapled nasogastric tube during Roux-en-Y gastric bypass: two cases. Obes Surg 2013;23:1120. [Google Scholar]
- [8].Baltasar A, Bou R, Serra C, et al. Stapling the bougie in sleeve gastrectomy: video. Surg Obes Relat Dis 2016;12:1136–8. [DOI] [PubMed] [Google Scholar]
- [9].Rizk S, El Hajj Moussa W, Assaker N, et al. Case report about the management of a late Gastro-Gastric Fistula after Laparoscopic Gastric Bypass, with the finding of an unexpected foreign body. Int J Surg Case Rep 2020;67:117–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Champion JK. Editorial comment on: nasogastric tube, temperature probe, and bougie stapling during bariatric surgery: a multi-center survey. Surg Obes Relat Dis 2012;8:600–1. [DOI] [PubMed] [Google Scholar]
- [11].Nandra K, Ing R. Safety of orogastric tubes in foregut and bariatric surgery. Surg Endosc 2018;32:4068–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Gooseen K, Tenckhoff S, Probst P, et al. Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg 2018;403:119–29. [DOI] [PubMed] [Google Scholar]


