Supplemental Digital Content is available in the text
Keywords: continuous circular capsulorhexis, limbus-centered, marker
Abstract
To introduce a limbus-centered continuous circular capsulorhexis (CCC) marking technique.
Compared with traditional capsulotomy diameter mark technique, a self-designed limbus-centered capsulotomy mark (LCM) was used to perform the routine cataract surgery in this observational study. Ten eyes were included in each group. The area outer/inner 5.5-mm CCC ring, the furthest/nearest distance from the capsule margin to the intraocular lens (IOL) margin, the CCC total coverage IOL area were measured and compared between this 2 groups.
No significant differences were found for all the comparison parameters between the 2 groups (all P > .05). However, the capsule total coverage area, area inner 5.5-mm ring was lower in the LCM group, which demonstrated advantage of LCM.
The limbus-centered capsulotomy diameter mark, as an inexpensive and convenient method, helps to perform limbus-centered capsulorhexis with not only a 360° overlapping capsular edge but also well-centered IOL optics.
1. Introduction
Previous studies demonstrated that a complete anterior capsule overlap on the intraocular lens (IOL) has a greater effect compared to a sharp-edge IOL design for reducing posterior capsule opacification (PCO).[1] Based on Wallace's report, even with an experienced cataract surgeon, imperfect contact of the anterior capsule rim with the IOL optic is observed in around 20% cases.[2] An incomplete contact deteriorates the function of a sharp square optic edge, which impedes cells migration and proliferates fibrosis toward the central posterior capsule.[3] Therefore, Wallace introduced a rapid and easy method to provide better anterior capsule size and location, called the capsulotomy diameter mark (CDM).[2] Kellen found that CDM works well in the clinic.[4] Generally, most surgeons perform continuous circular capsulorhexis (CCC) using the pupil center as a reference. However, the pupil center shifts when the pupil dilates,[5] and is a less reliable landmark compared to the limbus center for ocular alignment measurement (Fig. 1).[6] Therefore, the limbus center would be a good reference point in CCC. However, CDM focuses on the center of the optic zone, which may be less repeatable and precise, based on the surgeon's experience.
Figure 1.
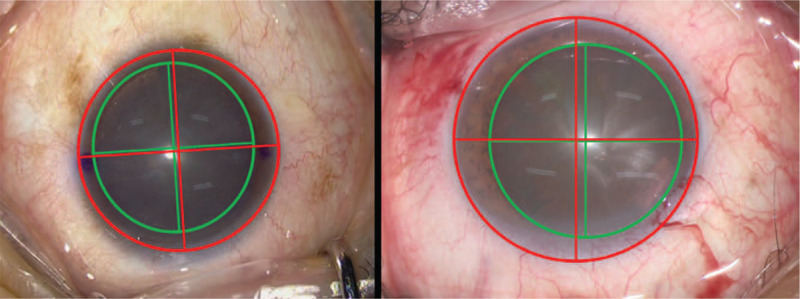
The degree of inconsistency between corneal center (red circle and red crisscross line) and dilated pupil center (green circle and green crisscross line) in different surgical eyes.
With the advent of premium IOLs, centration of high-end IOLs became favorable. Decentrated capsulotomy is associated with asymmetric capsular shrinkage after cataract surgery, which may cause severe IOL tilt and decentration.[7] Moreover, a decentered diffractive multifocal IOL or a toric IOL may induce high-order aberrations, defocusing, and astigmatism, which may decrease patients’ postoperative visual quality or reduce the magnitude of astigmatism correction.[8]
We recently found a more convenient and precise method for routine cataract surgical procedures to make sure that CCC is well-centered at the limbus. The method is called limbus-centered capsulotomy mark (LCM).
2. Methods
2.1. Subjects
This observational study was performed at the Linfen Yaodu Eye Hospital (Linfen, Shanxi, China). The research protocol was approved by the institutional review board of Linfen Yaodu Eye Hospital and carried out according to the tenets of the Declaration of Helsinki. Written informed consent was obtained from each subject after explaining the nature of this study.
Consecutive patients diagnosed with cataract were retrospectively enrolled between April 2019 and July 2019. The inclusion criteria were as follows: senile cataracts without systemic disease, nuclear cataract grade 3 (Lens Opacities Classification System III), no pathological alteration of the anterior segment (such as keratoconus, zonular dialysis, pseudoexfoliation syndrome, or corneal opacity), no retinal diseases impairing visual function, and no previous anterior or posterior segment surgery.
2.2. Surgical technique
Similar to an important step in toric IOL surgery (see Video1, Supplemental Video, http://links.lww.com/MD/F511, which demonstrates the surgical technique of LCM), we marked the 0 to 180° axis using a slit lamp in the natural pupil size before the cataract surgery. The horizontal axis marking was as follows:
-
(1)
narrow the slit-lamp beam to a thin slit and align it with the 0 to 180° marks on the calibrator;
-
(2)
keep the patient's head to the right of the slit lamp;
-
(3)
ask the patient to look into the slit-lamp light with the surgical eye;
-
(4)
make sure the slit beam pass through the first bright Purkinje image;
-
(5)
mark the junction point where the slit beams interact with the limbus using a sterile 1 mL syringe.
Place the lid speculum beneath the eyelid and bring the microscope in the surgical position. With the reference of 0 to 180° limbus mark and a horizontally scaled connecting rod, indent a 6.0-mm central corneal mark on the corneal surface when the patient's gaze is fixated on the microscope light. Moreover, apply the toric manual marker on the opposite side of the corneal mark to make sure that the indentation mark is more distinct and maintained until the end of the surgery (Fig. 2).
Figure 2.
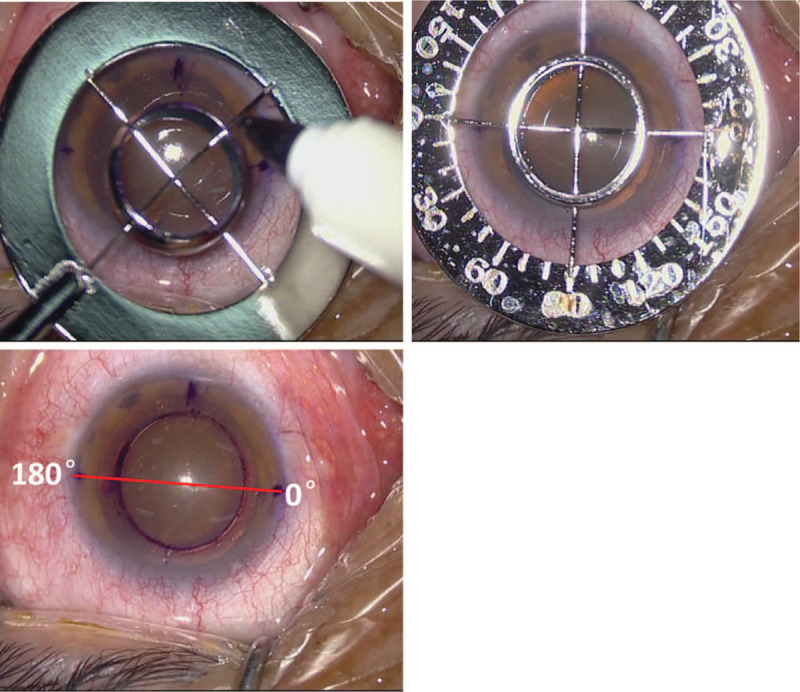
(Minghui Deng) The limbus-centered colored indentation is marked on the corneal surface using the limbus-centered capsulotomy mark (LCM). Note: 1) the toric manual marker is applied on the opposite side of the corneal mark to make sure that the indentation mark is more distinct (top left); 2) the LCM device is combined with the capsulotomy diameter mark device using an astigmatism marker plate, keeping the distance from the inner ring margin to the horizontal and vertical limbus equal to make sure that LCM is well-centered at the limbus as a reference during the surgery (top right); 3) after indentation, coaxially sighted corneal reflex is confirmed to be centered in the corneal indentation circle, and the 0–180° horizontal line passes through it.
After a clear corneal incision is made, and the anterior chamber is filled with a viscoelastic material, CCC is performed using 1.8-mm capsule forceps and following the indentation path on the cornea (Fig. 3).
Figure 3.
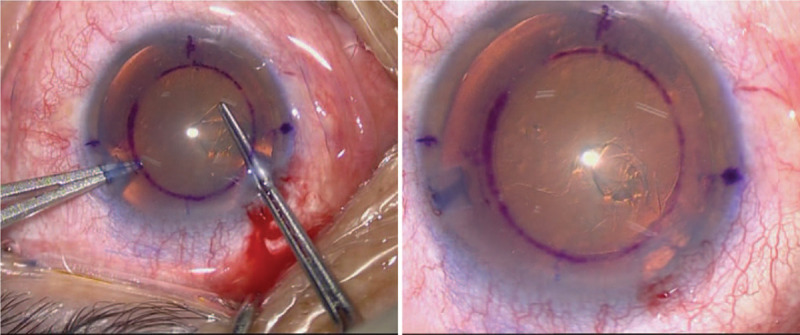
(Minghui Deng) Anterior capsulotomy inside the limbus-centered capsulotomy mark indentation and the finished continuous circular capsulorhexis margin following the indentation.
After phacoemulsification and cortex removal, a foldable IOL was implanted in the bag. The anterior capsule margin overlapped with the IOL optic edge and was well-centered (Fig. 4).
Figure 4.
(Minghui Deng) After phacoemulsification and cortex removal, the continuous circular capsulorhexis margin is identical with the indentation (top left), and the well-centered intraocular lens (IOL) and capsule overlap after IOL implantation with a 6.0-mm optical diameter during the surgery (top right). After 1 postoperative week, the intraocular lens was well-centered, and the anterior capsule margin evenly covered the IOL optic edges.
2.3. Method evaluation
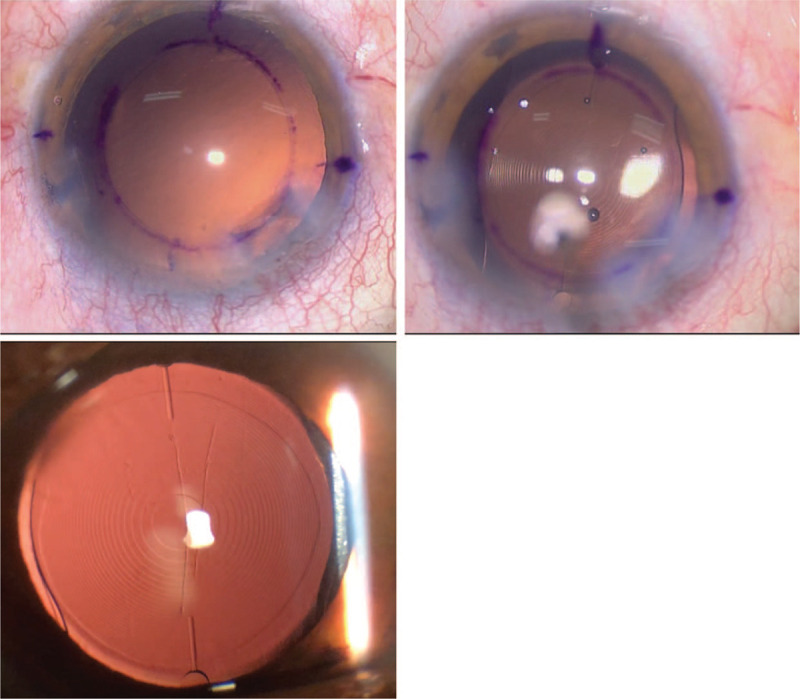
The routine cataract surgery was done by the same surgeon (MHD) with the device of CDM or LCM. Ten eyes were included in each group. The area outer/inner 5.5-mm CCC ring, the furthest/nearest distance from the capsule margin to the IOL margin, the CCC total coverage IOL area were measured with self-designed analysis software (Fig. 5).
Figure 5.
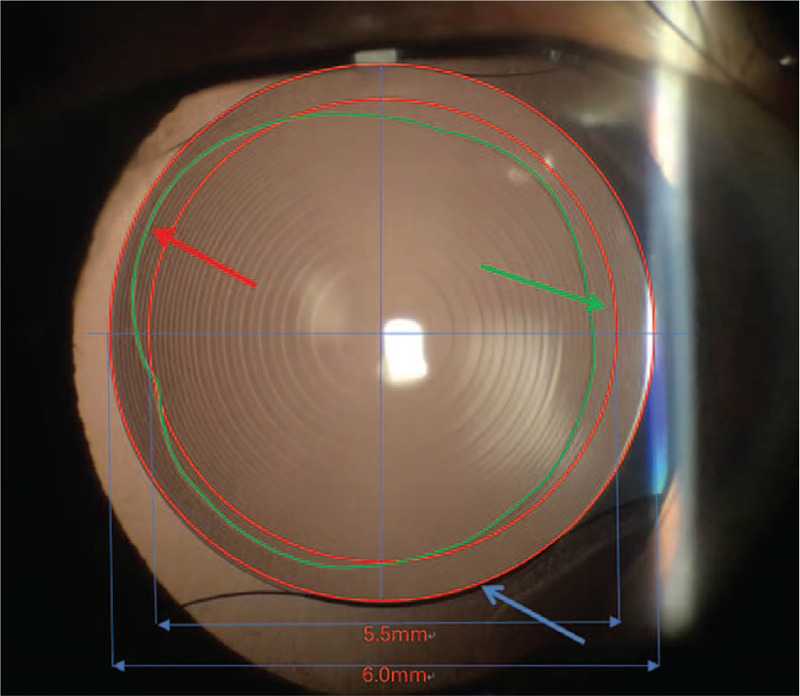
The area outer/inner 5.5-mm CCC ring (the irregular area circled by the ideal 5.5-mm CCC ring and the actual CCC margin demonstrated with the red and green arrows), the furthest/nearest distance from the capsule margin to the IOL margin (6.0 mm ring), the CCC total coverage IOL area (the area between IOL optic margin and the actual CCC margin) were measured for final analysis.
Statistical analyses were performed with commercial software (SPSS ver. 13.0; SPSS Inc.). An independent sample t test was performed to compare the quantitative measurement results between groups. All tests had a significance level of 5%.
3. Results
Ten eyes in each group were included in the first observation. After 1 postoperative week, IOL was well-centered, and the anterior capsule margin covered the IOL optic edges in all eyes (Fig. 6).
Figure 6.
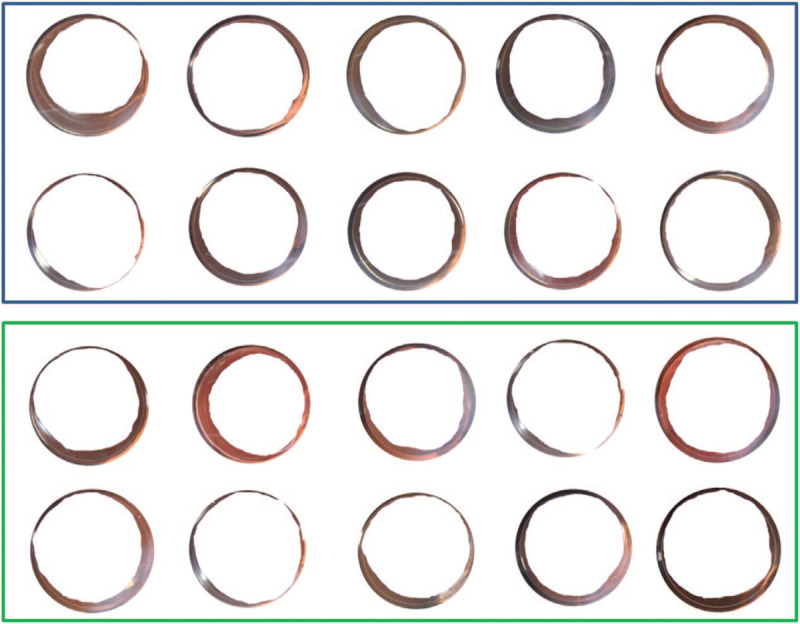
Total coverage area of each case in CDM group (blue rectangle) and LCM group (green rectangle).
The analysis result was demonstrated in Table 1. No significant differences were found between the 2 groups (all P > .05). However, the capsule total coverage area, area inner 5.5-mm ring was lower in the LCM group, which demonstrated advantage of LCM. Moreover, all the capsule related parameters demonstrated relatively lower standard deviation in the LCM group.
Table 1.
Analysis parameters in each group.
| CDM (n = 10) | LCM (n = 10) | Difference (M ± SE) | P | |
| Area outer 5.5-mm ring (mm2) | 0.19 ± 0.33 | 0.35 ± 0.30 | −0.17 ± 0.14 | .254 |
| Area inner 5.5-mm ring (mm2) | 2.95 ± 1.37 | 2.48 ± 1.23 | 0.47 ± 0.58 | .433 |
| Furthest distance from capsule margin to IOL margin (mm) | 0.68 ± 0.20 | 0.66 ± 0.12 | 0.02 ± 0.07 | .775 |
| Nearest distance from capsule margin to IOL margin (mm) | 0.14 ± 0.09 | 0.07 ± 0.08 | 0.06 ± 0.04 | .109 |
| Capsule total coverage area (mm2) | 8.01 ± 2.47 | 6.34 ± 1.53 | 1.67 ± 0.92 | .087 |
CDM = capsulotomy diameter mark, IOL = intraocular lens, LCM = limbus-centered capsulotomy mark, M = mean, SE = standard error.
4. Discussion
Traditional CCC marking methods used in cataract surgery mostly take the dilated pupil center as the subjective reference for the CCC center. Due to the pupil center shift, CCC center shift may occur, which may induce incomplete anterior capsule overlap on the IOL optics and IOL tilt and decentration due to postoperative capsule shrinkage.[5–7]
Although the CDM method uses the optic zone center as the CCC center, based on experience, it is hard to maintain a precise and repeatable result in each case, especially in misalignment cases.[9] Moreover, eye rotation from the sitting to the supine position also potentially affects the location choice of the optic zone center in the CDM method.[10] The aforementioned factors also affect the CCC reference center choice when using other device-dependent CCC methods, such as femtosecond laser-assisted capsulorhexis, Zepto-rhexis, and ring-shaped caliper.[11–13]
The corneal arcus, especially at the superior and inferior poles of the cornea will also affect the subjective choice of the limbus center during CCC. Therefore, we mark the 0–180° limbus rim in the sitting position and the natural pupil size before the cataract surgery to make sure that the final LCM method works well with limbus center positioning.
Refractive outcomes, especially for premium IOLs, are affected by not only proper size but also the centration of CCC.[8,14] A previous study demonstrated that CCC decentration of over 0.4 mm will cause a change of 0.25 D in spherical equivalence, and a capsulorhexis-IOL optic gap will induce astigmatism of 0.5 D after 1 postoperative year.[15] Therefore, a well limbus-centered and proper-sized CCC with the complete anterior capsule rim overlapping the IOL optic reduces the risks of IOL tilt and decentration, postoperative myopic shift, and PCO.[15–17] The LCM method, with the combination of astigmatism marker plate and corneal indented ring, could provide well limbus-centered and proper-sized CCC for cataract surgery. CCC of 5.5-mm diameter using the LCM method could provide a 0.3–0.5-mm anterior capsule overlap on the IOL optic edge, which would help prevent PCO. A relatively smaller capsulorhexis size compared to the IOL (normally 6.0 mm in diameter) is useful for ciliary sulcus IOL placement in posterior capsule rupture cases. Moreover, the small CCC size also provides IOL optic capture manipulation in sulcus placement cases. Furthermore, it is also useful in some cases that need marking of the toric IOL implantation axis and limbal relaxing incision location to correct ocular astigmatism.
Although the corneal curvature, light refraction from the cornea to the anterior capsule, and magnification may slightly have an influence on CCC size and location, with the help of double concentric rings, LCM can still provide well-centered and proper-sized CCC, even in cases of slight misalignment of the microscope and eye axis.[9] Moreover, more cases with long follow-ups should be studied to monitor and assess the long-term effects of the LCM method on PCO, IOL tilt and decentration prevention.
5. Conclusions
This limbus-centered capsulotomy diameter mark technique could provide limbus-centered capsulorhexis with not only a 360° overlapping capsular edge but also well-centered IOL optics.
Author contributions
XGW: conception, design, data acquisition, analysis, drafting, critical revision. JD: conception design, data acquisition, drafting, critical revision. MHD: conception, design, data acquisition, analysis, drafting, critical revision. All authors: final approval of the manuscript.
Conceptualization: xiaogang wang, jing dong, minghui Deng.
Data curation: xiaogang wang, jing dong, minghui Deng.
Formal analysis: xiaogang wang, jing dong, minghui Deng.
Funding acquisition: xiaogang wang.
Investigation: xiaogang wang, minghui Deng.
Methodology: xiaogang wang, jing dong, minghui Deng.
Project administration: minghui Deng.
Resources: minghui Deng.
Software: xiaogang wang, minghui Deng.
Supervision: xiaogang wang, jing dong, minghui Deng.
Validation: xiaogang wang, jing dong, minghui Deng.
Writing – original draft: xiaogang wang, minghui Deng.
Writing – review & editing: xiaogang wang, jing dong, minghui Deng.
Glossary
Abbreviations: CCC = continuous circular capsulorhexis, CDM = capsulotomy diameter mark, IOL = intraocular lens, PCO = posterior capsule opacification.
References
- [1].Smith SR, et al. The effect of lens edge design versus anterior capsule overlap on posterior capsule opacification. Am J Ophthalmol 2004;138:521–6. [DOI] [PubMed] [Google Scholar]
- [2].Wallace RB, 3rd. Capsulotomy diameter mark. J Cataract Refract Surg 2003;29:1866–8. [DOI] [PubMed] [Google Scholar]
- [3].Sacu S, et al. Effect of intraocular lens optic edge design and material on fibrotic capsule opacification and capsulorhexis contraction. J Cataract Refract Surg 2004;30:1875–82. [DOI] [PubMed] [Google Scholar]
- [4].Kellen RI. Capsulotomy diameter mark. J Cataract Refract Surg 2004;30:2031–2. [DOI] [PubMed] [Google Scholar]
- [5].Camellin M, Gambino F, Casaro S. Measurement of the spatial shift of the pupil center. J Cataract Refract Surg 2005;31:1719–21. [DOI] [PubMed] [Google Scholar]
- [6].Barry JC, Backes A. Limbus versus pupil center for ocular alignment measurement with corneal reflexes. Invest Ophthalmol Vis Sci 1997;38:2597–607. [PubMed] [Google Scholar]
- [7].Ohmi S, Uenoyama K. Decentration associated with asymmetric capsular shrinkage and intraocular lens design in a rabbit model. J Cataract Refract Surg 1995;21:293–6. [DOI] [PubMed] [Google Scholar]
- [8].Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol 2012;23:269–75. [DOI] [PubMed] [Google Scholar]
- [9].Jasinskas V, Galdikas A, Zemaitiene R. Novel capsulotomy diameter marking capability. J Cataract Refract Surg 2005;31:1675. [DOI] [PubMed] [Google Scholar]
- [10].Prickett AL, et al. Cyclotorsional and non-cyclotorsional components of eye rotation observed from sitting to supine position. Br J Ophthalmol 2015;99:49–53. [DOI] [PubMed] [Google Scholar]
- [11].Thompson VM, et al. Comparison of Manual, Femtosecond Laser, and Precision Pulse Capsulotomy Edge Tear Strength in Paired Human Cadaver Eyes. Ophthalmology 2016;123:265–74. [DOI] [PubMed] [Google Scholar]
- [12].Nagy ZZ, Mastropasqua L, Knorz MC. The use of femtosecond lasers in cataract surgery: review of the published results with the LenSx system. J Refract Surg 2014;30:730–40. [DOI] [PubMed] [Google Scholar]
- [13].Tassignon MJ, Rozema JJ, Gobin L. Ring-shaped caliper for better anterior capsulorhexis sizing and centration. J Cataract Refract Surg 2006;32:1253–5. [DOI] [PubMed] [Google Scholar]
- [14].Wang L, Koch DD. Effect of decentration of wavefront-corrected intraocular lenses on the higher-order aberrations of the eye. Arch Ophthalmol 2005;123:1226–30. [DOI] [PubMed] [Google Scholar]
- [15].Okada M, et al. Effect of centration and circularity of manual capsulorrhexis on cataract surgery refractive outcomes. Ophthalmology 2014;121:763–70. [DOI] [PubMed] [Google Scholar]
- [16].Hollick EJ, Spalton DJ, Meacock WR. The effect of capsulorhexis size on posterior capsular opacification: one-year results of a randomized prospective trial. Am J Ophthalmol 1999;128:271–9. [DOI] [PubMed] [Google Scholar]
- [17].Ram J, et al. Effect of in-the-bag intraocular lens fixation on the prevention of posterior capsule opacification. J Cataract Refract Surg 2001;27:1039–46. [DOI] [PubMed] [Google Scholar]


