Abstract
Background
The estimated annual global perinatal and neonatal death is four million. Stillbirths are almost equivalent to neonatal mortality, yet they have not received the same attention. Antenatal care is generally thought to be an effective method of improving pregnancy outcomes, but its effectiveness as a means of reducing perinatal mortality has not been evaluated in Ethiopia. Therefore, we will identify the pooled effect of antenatal care on perinatal outcomes in Ethiopia.
Methods
Medline, Embase, Cinahl, African journal online and Google Scholar was searched for articles published in English language between January 1990 and May 2020. Two independent assessors selected studies and extracted data from eligible articles. The Risk of Bias Assessment tool for Non-Randomized Studies was used to assess the quality of each included study. Data analysis was performed using RevMan 5.3. Heterogeneity and publication bias were assessed using I2 test statistical significance and Egger's test for small-study effects respectively. The random effect model was employed, and forest plot was used to present the risk ratio (RR) with 95% confidence interval (CI).
Results
Thirteen out of seventeen included studies revealed antenatal care utilization had a significant association with perinatal outcomes. The pooled risk ratio by the random-effects model for perinatal death was 0.42 (95% CI: 0.34, 0.52); stillbirth 0.34 (95% CI: 0.25, 0.46); early neonatal death 0.85 (95% CI: 0.21. 3.49).
Conclusion
Women who attended at least one antenatal care visit were more likely to give birth to an alive neonate that survives compared to their counterpart. Therefore, the Ethiopian Ministry of health and other stakeholders should design tailored interventions to increase antenatal care utilization since it has been shown to reduce perinatal mortality.
Introduction
Globally, an estimated four million perinatal and neonatal deaths occur annually [1–3]. In addition, an estimated 2.6 million babies were stillborn in 2015, only a 19% decrease since 2000. Ninety eight percent of stillbirth occurred in low and middle income countries (LMICs) and 77% of these occurred in the south Asia and Sub-Saharan Africa (SSA), thus showing little progress in SSA [2]. Majority of the stillbirths (60%) occurred during the antepartum period were mainly due to untreated maternal infection, hypertension, and poor fetal growth [2], which are preventable. The perinatal mortality rate across SSA was 35 per 1000 live births [4]. In Ethiopia, there are high proportions of stillbirths and early neonatal deaths [5,6], being one of the top ten countries with highest stillbirth numbers, and the high perinatal mortality rate (33 per 1000 live births) is coupled with high percent of low birth weight babies (13% of babies weighing less than 2500 grams at birth) [2,7,8].
The increase in perinatal mortality is more likely due to increased stillbirths and reduced antenatal visits [9]. ANC is a vital intervention for successful maternal and child health, globally [10]. Attending less than 50% of recommended or inadequate ANC visits was associated with adverse pregnancy outcomes [11–17]. Stillbirths are a reflection of ANC accessibility and utilization [18]. Women with no ANC had significantly increased risk of stillbirths [19]; mortality and morbidity of mothers and newborns was reduced for those who had optimal utilization of ANC services [20]. Furthermore, the risk of developing neonatal mortality was decreased for women who received as little as one ANC follow up [21–27], but the effect on perinatal outcomes is unknown.
Studies revealed that low birth weight (LBW) was associated with not attending at least five to eight ANC visits, not receiving any ANC during the first trimester and not having access to certain ANC contents [28–30]; LBW is a contributing factor to stillbirths [31]. However, there are conflicting results on the effectiveness of ANC interventions on maternal and newborn health outcomes [32–36]. There are inconsistencies in the studies regarding the benefits of ANC in reducing perinatal mortality [17,36–40]; studies revealed perinatal mortality was not affected by no and inadequate ANC [41]; other studies showed improved ANC did not reduce perinatal or neonatal mortality [42]. Benefits of ANC were reported by some but not all care programs regarding perinatal mortality [43]; however, ANC has not been compellingly shown to improve birth outcomes [44]. Furthermore, the focused ANC model is associated with more perinatal deaths than models comprised of at least eight ANC contacts [45].
Reduction in an availability and utilization’s gaps of ANC practice is needed to end preventable deaths of newborns [46]. Failure to improve birth outcomes by 2035 will result in an estimated 116 million deaths, 99 million survivors with disability [47], and an additional 52 million stillbirths [47,48]. There are no pooled estimates of the effect of ANC on perinatal outcomes in Ethiopia; therefore, we aimed to assess the effect of ANC on perinatal outcomes in Ethiopia in this systematic review and meta-analysis.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist was used in the preparation of the systematic review methodology [49]. The systematic review was registered on the PROSPERO prospective register of systematic reviews after piloting the study selection process (registration number PROSPERO 2020: CRD42020188340).
Eligibility criteria
Assessment for eligibility was conducted and studies were included in this review if (i) the study involved a delivering/laboring women or newborn babies or women of child-bearing age or pregnant women or postpartum women; (ii) the study reported the outcomes (perinatal death, stillbirth, early neonatal death); (iii) the ANC utilization was considered as factors/exposure for the outcomes; (iv) the study was done in the perinatal period and the author(s) defined perinatal outcomes (perinatal mortality) as death of newborn between 28 weeks’ of gestation and seven days postpartum; (v) it was an observational study design (cross-sectional, case-control or cohort study design) and (v) English language article.
We excluded studies from the review that focused only on the number of ANC visits based on full-text assessment.
PICO. Population: Newborn after 28 weeks’ gestation and survived seven days postpartum.
Intervention: utilized at least one ANC visit.
Comparison: Newborns whose mothers received at least one ANC service as compared to newborns whose mothers did not.
Outcome: Newborn death during perinatal period (from 28 weeks’ of gestation to 7 days postpartum).
Information sources and search strategy
Medline (via PubMed), EMBASE, and CINAHL were searched for (S1–S3 Tables) articles published in the English language between January 1990 and June 2020, using the keywords “antenatal care”, “prenatal care”, "maternity care", “maternal health care”, “obstetrics”, “maternal health services”, "pregnancy care", "perinatal mortality", "perinatal death", "early neonatal mortality", "early neonatal death" "stillbirth", "newborn mortality", "newborn death", "perinatal outcomes", “fetal death” "infant death", “infant mortality” AND "Ethiopia”. Moreover; we thorough literatures search was performed on Google Scholar and African Journal Online (AJOL). A search combining MeSH and key terms connecting population, intervention and outcomes of interest was performed.
Study selection
The study selection involved several steps. First, the title and abstract were selected independently by the review authors using the inclusion criteria. Second, after removing the duplicates, the full reports of all titles that met the inclusion criteria were independently identified by review authors. Third, the review authors screened the full text reports to decide whether the studies meet the eligibility criteria. Finally, any disagreements among review authors were resolved through discussion or review authors who did not participate in step one thru three decided whether to include or exclude the article. An attempt was made to meet study authors for additional information by email and in order to have put reasons for excluding studies (Fig 1).
Fig 1. Flowchart of search results for included studies.
Data extraction
Each studies’ relevance was checked based on their topic, objectives and methodology. Two independent reviewers (KS & BM) completed and verified the data extraction, using a standardized form with explicit inclusion and exclusion criteria. If not resolved by discussion of reviewers, the third or fourth author was consulted to decide on the disagreement. For each study, the first author’s last name, publication year, design, setting, sample size, study period, sample age, the definition of outcomes, population, outcome and comparison groups were documented.
In this review, our evaluation of perinatal outcomes related to the death of the newborn from 28 weeks’ of gestation to seven days postpartum (i.e., fetal death, stillbirth, and early neonatal death) were reported [50–52]. Antenatal care ‘no ANC visit at all’ or ‘one or more ANC visit’ were the two classifications of the exposure variable. An attempt to contact study authors to request information, such as missing data, was made, if necessary and unfortunately there was no study which was excluded do to missing data.
Data items
Antenatal care is defined as ‘a woman having one or more health facility visits for a pregnancy check-up by a skilled attendant during her pregnancy’ [12,23,53–58].
Focused ANC model is four visits providing essential evidence based interventions–a package to achieve the full life-saving potential that ANC promises for women and babies [59].
Perinatal outcomes/mortality refers to the number of stillbirths and deaths in the first week of life [23,42,60,61]. In this review, perinatal death (as study authors defined) or reviewers added the number of stillbirths and early neonatal deaths or available outcomes between stillbirths and early neonatal deaths to estimate overall perinatal outcomes/mortality rate.
Stillbirth was defined as fetal deaths after 28 weeks of gestation [5,62,63].
Skilled attendant refers to a midwife, doctor or nurse who has been educated, trained and accredited to manage normal pregnancies, childbirth and the immediate postnatal period and identify, manage and/or refer women and newborns with complications [64].
Early neonatal mortality was defined as neonatal deaths in the first week of life after being delivered in the age of viability (28 weeks of gestation and above) [5,56].
Individual study’s risk of bias
The review authors assessed all selected studies rigorously for inclusion in the review. The Risk of Bias Assessment Tool for Non-Randomized Studies (RoBANS) [65] was used to assess the quality of each included study. Studies were evaluated across six groups (selection bias, attrition bias, detection bias, performance bias, confounding bias and reporting bias). Each domain was assigned one of three possible groups for each of the involved studies: ‘low risk’, ‘high risk’ and ‘unclear’. RoBANS is shown in S4 Table.
Synthesis and analysis of data
Statistical analysis was carried out in RevMan version 5.3. A DerSimonian and Laird random effects model [66] was used to measure ANC’s overall effect on perinatal mortality and the risk ratio was measured with a 95% confidence interval. We calculated the I2 statistic which describes the percentage of total variation among studies to assess heterogeneity among studies. An I2 statistical value of 25%, 50% and 75% representing low, moderate and high heterogeneity respectively [67]. A p-value less than 0.05 was considered as statistically significant both for risk ratio and heterogeneity.
Sensitivity analysis was conducted to assess the stability of results and test individual study effects on the meta-analysis using leave one out method. Furthermore, possible sources of heterogeneity were explored using subgroup analysis. Egger's test for small-study effects was used to investigate potential publication bias (p-value > 0.1) [68].
Results
Search results
The initial search identified 1918 unique citations. Of these, 1824 and 53 were excluded on title/abstract alone and following full-text review respectively. Furthermore, 6 articles classified ANC based on number of visits [69–74], 6 articles defined their outcomes differently [62,75–79], 6 articles did not determine outcome at all [26,53,80–83] and 6 articles had no ANC follow-up status [84–89] and therefore they all were excluded. Lastly, 17 articles were retained for final review (Fig 1).
Characteristics of studies
The review included studies from all regions in Ethiopia; the majority were from Amhara and Oromia. Nine cross-sectional, six case-control and two cohort studies were included in the meta-analysis. The sample size of the studies ranged from 300 to 12560. Among the included studies, 5 and 12 were community-based and facility-based, respectively. A total of 51729 study samples were included, of which 2951 newborns died during the perinatal period, making the perinatal mortality rate 41 per 1000 total births (total deliveries, total stillbirths and total early neonatal deaths), excluding case-control studies in which total numbers of live births at the time of the study were unknown. Similarly, the stillbirth rate and early neonatal mortality rate were 38 per 1000 total births (stillbirths and live births) and 19 per 1000 live births. Table 1 displays the characteristics of the 17 included primary studies.
Table 1. Characteristics of studies revealing the effect of ANC on perinatal outcomes in Ethiopia.
| No | Authors | Design | Study setting | Study period | Sample size | Population | Sample age | Outcomes variable | Operational definition | ANC status | Perinatal outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | |||||||||||
| 1 | Adane etal. 2014 [90] | Cross-sectional study | Facility-based | February 2013 | 481 | Laboring women | <20, 20–35, 35+ | Stillbirth | Stillbirth was defined as the birth of an infant that has died in the womb or during intra-partum after 28 weeks of gestation. | Yes | 18 | 397 |
| No | 16 | 50 | ||||||||||
| 2 | Goba et al. 2017 [91] | Case-control study | Facility-based study | From February 1 to September 30, 2016 | 378 | Delivering women | <24, 25–34, 35+ | Perinatal death | Patients who experienced stillbirth or early neonatal death were classified as the case group and those whose neonates survived until discharge or for at least 7 days were control group. | 0 visits | 19 | 9 |
| 1–3 visits | 89 | 149 | ||||||||||
| ≥4 visits | 18 | 94 | ||||||||||
| 3 | Roro et al. 2018 [92] | Nested case-control study | Community-based study | Between March 2011 to December 2012 | 4438 | Newborn babies | 15–19, 20–24, 25–29, 30–34, 35+ | Perinatal mortality | Perinatal death is defined as the sum of stillbirth and early neonatal death. | Yes | 56 | 121 |
| No | 17 | 25 | ||||||||||
| 4 | Welegebriel et al. 2017 [93] | Case-control study | Facility-based study | From January 2011 to 2015 | 540 | Mothers registered in for maternal health service utilization | <20, 20–34, 35+ | Stillbirth | Not defined | Yes | 69 | 278 |
| No | 66 | 127 | ||||||||||
| 5 | Worede and Dagnew 2019 [94] | Unmatched case-control | Facility-based study | From 1st January to 30th April 2019 | 420 | Delivering women | <20, 20–34, 35+ | Stillbirth | Case is defined as fetal death after 28 weeks of pregnancy (either pre-partum or intra-partum stillbirth) | Yes | 47 | 284 |
| No | 37 | 52 | ||||||||||
| 6 | Getiye and Fantahun 2017 [95] | Unmatched case-control study | Facility-based study | From January 1/ 2014 to Dec 31/ 2014 | 1113 | Delivering women | 15–19, 20–24, 25–29, 30–34, 35+ | Perinatal outcome | Perinatal mortality is total number of deaths in the perinatal period | Yes | 354 | 724 |
| No | 22 | 13 | ||||||||||
| 7 | Tilahun & Assefa 2017 [96] | Cross-sectional study | Facility-based | Not specified | 413 | Delivering women | <20, 20–34, 35–45 | Stillbirth | Not defined | Yes | 17 | 321 |
| No | 16 | 59 | ||||||||||
| 8 | Berhie and Gebresilassie 2016 [97] | Cross-sectional study | Community-based study | From September 2010 through June 2011 | 12,560 | Women of child-bearing age | 15–24, 25–34, 35+ | Stillbirth | Pregnancy losses occurring after seven completed months of gestation are defined as stillbirths. | No ANC visit | 273 | 3828 |
| Visited at least once | 118 | 3172 | ||||||||||
| 9 | Tilahun and Gaym 2008 [98] | Case-control study | Facility-based | From May 15, 2006 to August 15, 2006 | 390 | Delivering mothers | <20, 20–34, 35+ | Perinatal Mortality | Perinatal mortality (case) were mothers with a singleton pregnancy who were admitted to the labor ward and had a stillbirth or suffered an early neonatal death after delivery. | Unbooked | 43 | 14 |
| Booked | 87 | 246 | ||||||||||
| 10 | Ballard et al. 2016 [99] | Cross-sectional study | Community-based | Between May and December 2014 | 4442 | Women of child-bearing age | Not mentioned | Stillbirth | The stillbirth was delivering a dead neonate after a pregnancy lasting 7 months or more. | Received ANC | 42 | 2437 |
| Not received ANC | 53 | 1921 | ||||||||||
| 11 | Eyob and Worku 2003 [100] | Cross-sectional study | Facility-based | From lstJanuary 1995 to December 31, 1996 | 8986 | Delivering mothers | Not mentioned | Perinatal death | Not defined | Unbooked | 283 | 1770 |
| Booked | 301 | 6632 | ||||||||||
| 12 | Worku et al. 2013 [14] | Prospective cohort study | Community-based | From December 1, 2011 to August 31, 2012 | 727 | Pregnant women | <20, 20–34, 35+ | Perinatal death | Definition taken from WHO guideline monitoring emergency obstetric care | Yes | 13 | 240 |
| No | 23 | 451 | ||||||||||
| 13 | Lakew et al. 2017 [101] | Cross-sectional | Community-based | 2014 | 2555 | Women of child-bearing age | <24, 25–34, 35+ | Stillbirth | Stillbirth outcomes was characterized as the introduction of a newborn child that has passed on in the womb or amid intra-partum following 28 weeks of growth | No ANC visit | 9 | 138 |
| ANC 1+ visit | 7 | 231 | ||||||||||
| 14 | Berhan 2014 [102] | Retrospective cohort study | Facility-based | Between January 2006 and December 2011 | 9619 | Women that gave birth | <20, 20–34, 35+ | Perinatal death | Perinatal status defined the fetal or early neonatal survival (from 28 weeks of pregnancy age up to the first 7 days of newborn age) | Yes | 124 | 283 |
| No | 90 | 149 | ||||||||||
| 15 | Chekol A., 2011 [103] | Cross-sectional | Facility-based | From September 2008 to August 2009 | 581 | Laboring women | 15–19, 20–29, 30–42 | Perinatal death | It is fetal death starting from 28 weeks of gestational age and the death of new born in the first week of life, which comprises late fetal and early neonatal deaths. | No | 36 | 93 |
| Yes | 33 | 419 | ||||||||||
| 16 | Aragaw Y., 2016 [104] | Cross-sectional | Facility-based | From September 11, 2012 to 10, 2013 | 3786 | Newborn babies | <20, 20–34, 35+ | Perinatal death | Not defined | Yes | 204 | 2765 |
| No | 169 | 648 | ||||||||||
| 17 | Mihiretu A. et al, 2017 [105] | Cross-sectional | Facility-based | July, 2015 | 300 | Mothers who gave birth | <18, 18–34, 35+ | Perinatal death | Not defined | Yes | 10 | 142 |
| No | 42 | 107 | ||||||||||
Individual study’s risk of bias
The risk of bias assessment for all included studies is shown in Table 2. The risk of bias in selection of participants into the study was low for all studies. The bias due to missing or incomplete data was low in most of the studies, although a few studies have unclear explanation. The performance bias during measurement of exposure variable was low in fourteen and unclear in three studies. However, the risk of detection bias was high in all studies. The risk of confounding bias was low in thirteen, high in three and unclear in one study. The bias due to reporting of results was low in fifteen and unclear in two studies. See S4 Table.
Table 2. Individual studies risk of bias on effect of ANC on perinatal outcomes in Ethiopia.
| Studies | Selection bias | Attrition bias | Performance bias | Detection bias | Confounding bias | Reporting bias |
|---|---|---|---|---|---|---|
| Adane et al. 2014 | Low | Low | Low | High | Low | Low |
| Ballard et al. 2016 | Low | Low | Low | High | High | Low |
| Berhan 2014 | Low | Low | Unclear | High | High | Low |
| Berhie and Gebresilassie 2016 | Low | Low | Low | High | Low | Low |
| Eyob and Worku 2003 | Low | Low | Unclear | High | High | Low |
| Getiye and Fantahun 2017 | Low | Low | Low | High | Low | Low |
| Goba et al. 2017 | Low | Low | Unclear | High | Low | Low |
| Lakew et al. 2017 | Low | Low | Low | High | Low | Low |
| Roro et al. 2018 | Low | Unclear | Low | High | Low | Low |
| Tilahun & Assefa 2017 | Low | Low | Low | High | Low | Low |
| Tilahun and Gaym 2008 | Low | Unclear | Low | High | Low | Low |
| Welegebriel et al. 2017 | Low | Unclear | Low | High | Low | Low |
| Worede and Dagnew 2019 | Low | Low | Low | High | Low | Low |
| Worku et al. 2013 | Low | Low | Low | High | Unclear | Low |
| Chekol A., 2011 | Low | Low | Low | High | Low | Low |
| Aragaw Y., 2016 | Low | Low | Low | High | Low | Unclear |
| Mihiretu A. et al, 2017 | Low | Low | Low | High | Low | Unclear |
Pooled effect size of ANC on perinatal outcomes
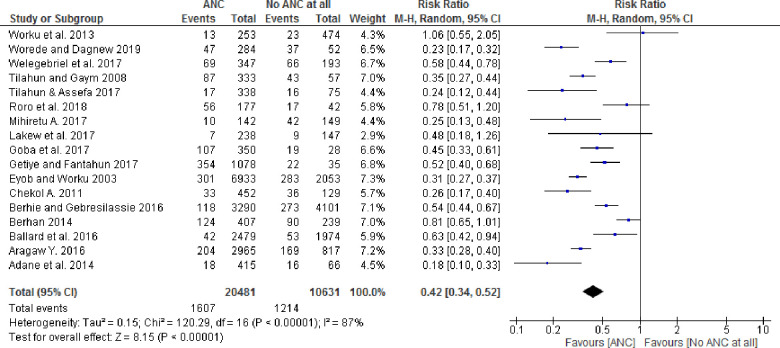
Among the seventeen studies included in the analysis, thirteen studies with at least one ANC visit showed statistically significant associations with perinatal outcomes, whereas four studies had no statistically significant association. Similarly, the pooled effect size for perinatal death by the random-effect model was 0.42 (95% CI: 0.34, 0.52) for babies born to women who received at least one ANC follow-up as compared to newborns whose mothers did not receive any ANC follow-up (Fig 2). Furthermore, the pooled stillbirth and early neonatal death effect size by random effects model was 0.34 (95% CI: 0.25, 0.46) and 0.85 (95% CI: 0.21. 3.49) respectively.
Fig 2. Forest plot showing pooled effect of ANC on the perinatal outcomes in Ethiopia.
Heterogeneity of the studies
There was overall substantial heterogeneity across studies (I2 = 87%, p-value < 0.001), as well as within subgroups for sample size, design and place. Heterogeneity that was present in the overall meta-analysis was partially explained with stratification by study design and place. For example, in a subgroup analysis, cohort studies’ (RR = 0.83[95% CI: 0.67–1.02]; p-value = 0.45 for heterogeneity test, I2 = 0%) and community-based studies (RR = 0.64[95% CI: 0.51–0.80]; p-value = 0.23 for heterogeneity test, I2 = 29%) were not statistically heterogeneous (p-value > 0.10); however, heterogeneity was present when the subgroup analysis was performed by sample size (Table 3).
Table 3. Studies’ subgroup analysis modifying the effect of ANC on perinatal outcomes in Ethiopia.
| Subgroup | Random effects RR(95% CI) | I-squared, p-value |
|---|---|---|
| Study design | ||
| Cross-sectional study | 0.34(0.27–0.44) | 78%, p-value < 0.001 |
| Case-control study | 0.45(0.33–0.61) | 85%, p-value < 0.001 |
| Cohort study | 0.83(0.67–1.02) | 0%, p-value = 0.45 |
| Study place | ||
| Community-based study | 0.64(0.51–0.80) | 29%, p-value = 0.23 |
| Facility-based study | 0.36(0.28–0.46) | 88%, p-value < 0.001 |
| Sample size | ||
| < 500 | 0.29(0.22–0.38) | 67%, p-value = 0.009 |
| 500–1000 | 0.53(0.26–1.05) | 86%, p-value = 0.0006 |
| > 1000 | 0.52(0.39–0.69) | 90%, p-value < 0.001 |
Sensitivity analysis was performed for the outcome variable to observe a significant change in risk ratio and confidence interval. The meta-analysis resulted in no substantial difference in the overall risk ratio during the sequential removal of each study from the analysis. For instance, when a statistically insignificant study [14] and those study with wide confidence interval were excluded [101], the risk ratio of the effect of ANC did not change significantly or are within the confidence interval of pooled effect of ANC (0.32, 0.52).
An Egger's test for small-study effects showed no publication bias (p-value = 0.49). Therefore, there was no significant threat to the validity of the review.
Discussion
The purpose of this review was to evaluate the effectiveness of focused ANC as a means of reducing perinatal mortality among women (pregnant, delivering, postpartum, and mothers) in Ethiopia. Seventeen eligible primary studies were identified evaluating ANC with a range of populations including pregnant women, laboring women and postpartum mothers and their perinatal outcomes. Literature throughout Ethiopia support the benefits of ANC’s that provided by skilled attendants for the health of newborns. To improve ANC’s effectiveness, numerous approaches and strategies have been employed in LMICs [106–108]. The focused ANC approach, developed in the 1990s by WHO has been implemented by most LMICs including Ethiopia [109,110].
The perinatal mortality and stillbirth rate were 41 and 38 per 1000 total births respectively in this meta-analysis which were slightly higher than the perinatal mortality rate in SSA (34.7 per 1000 total births) [4] however, lower than the pooled perinatal mortality rate (51.3 per 1000 total births) and slightly higher than stillbirth rate in Ethiopia (37 per 1000 total births) [6]. The review in SSA utilized only demographic health survey data whereas the pooled perinatal mortality in Ethiopia included both demographic health survey and study data. The difference may be attributed to not only a variation in the study nature, sample size, and setting but also maternal and child health utilization and access to quality maternal and newborn health services [6]. However, early neonatal mortality rate was 19 per 1000 live births in this review which was lower than systematic reviews found in Ethiopia (30 per 1000 live births).
A global multipartner movement to end preventable maternal and newborn deaths and stillbirths, setting a target for national stillbirths less than 12 per 1000 live births and will reduce death and disability continuously, ensuring no newborn is left behind in all countries by 2030 [2,19]; however, this review, along with the EDHS [5] and another systematic review in Ethiopia [6] revealed that the perinatal mortality has remained stable for two decades. Using this study’s perinatal mortality rate as a benchmark, the annual rate of reduction (ARR) must increase to achieve The Every Newborn Action Plan.
Pregnant women’s attendance of at least one ANC follow-up had a statistically significant effect on perinatal mortality. This study found a 58% and 66% lower risk of perinatal mortality and stillbirth among women who attended at least one ANC by a skilled attendant in Ethiopia. The basic finding of this study was even limited ANC (as little as one visit) leads to better newborn outcomes compared with no ANC, and encouraging pregnant women to seek ANC would significantly impact perinatal mortality rate (PMR) and would be an important strategy to incorporate in planning initiatives aimed at reducing PMR; this appears to be consistent with studies from another countries [56,111]. The finding was also in line with the global network’s population-based birth registry results in Africa, India, Pakistan and Guatemala [19]. A review in Asia also revealed a protective effect on perinatal mortality for women who used ANC and health facility delivery [39].
Antenatal care utilization and delivery at a health facility by a skilled attendant [112] who provides quality care are established as an intervention to reduce perinatal mortality [113–115]. This may be due to the women receiving interventions during her pregnancy, [116–118] which have a positive effect on lowering mortality; ANC also has an indirect impact since those women attending ANC are more likely to have a skilled birth attendant [39,112,119,120] hence, their newborns have access to basic neonatal resuscitation [121,122] which prevent perinatal mortality. Therefore, receiving high quality and an accessible health care services to reduce perinatal mortality is critical for pregnant women [123]. Skilled training of health care providers and resources of local primary healthcare facilities should be strengthened [124].
The factors associated with perinatal mortality (preterm labor, hypertensive disorders of pregnancy, intrauterine growth restriction, gestational diabetes) can be identified in the prenatal period, thus reinforcing the need to upgrade the continuum of care from initiation of ANC to complication management at health facilities [113,125].
A comprehensive database search was conducted to include all pertinent studies, and subgroup analysis was conducted to determine whether any specific study level factor described the outcomes. The large sample size of the analysis, could detect the effect of ANC on perinatal outcomes since the review included all studies conducted in Ethiopia. As a limitation, the systematic review and meta-analysis were based on English language and observational studies associated with inherent biases. We were unable to pool the overall effect of ANC for those studies that were based on the number of visits, since they did not define zero visits and therefore that were excluded. The study authors defined stillbirth and early neonatal death based on gestational age and the days of life of the newborn. The future research should focus on visits and specific ANC interventions that may affect perinatal outcomes.
Conclusion
This review showed that women who received at least one ANC follow-up by a skilled attendant were less likely to experience perinatal mortality than those who did not. Thus, increasing a woman’s ANC utilization by a skilled attendant is mandatory in Ethiopia to reduce perinatal mortality. Furthermore, to address perinatal mortality in the country, strategies should focus on women’s mobilization to seek ANC services and facility-based deliveries.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOC)
Acknowledgments
We would like to acknowledge Haramaya University for providing a scholarship and stipend. We also thank Tara Wilfong for her constructive comments and language edition.
Data Availability
All relevant data are within the manuscript and Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet. 2015;385(9966):430–40. 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 2.Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. The Lancet Global Health. 2016;4(2):e98–e108. 10.1016/S2214-109X(15)00275-2 [DOI] [PubMed] [Google Scholar]
- 3.Leisher SH, Teoh Z, Reinebrant H, Allanson E, Blencowe H, Erwich JJ, et al. Seeking order amidst chaos: a systematic review of classification systems for causes of stillbirth and neonatal death, 2009–2014. BMC pregnancy and childbirth. 2016;16(1):295 10.1186/s12884-016-1071-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akombi BJ, Renzaho AM. Perinatal Mortality in Sub-Saharan Africa: A Meta-Analysis of Demographic and Health Surveys. Annals of global health. 2019;85(1):1–8. 10.5334/aogh.2411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berhan YB, Asres. Perinatal mortality trends in Ethiopia. Ethiopian journal of health sciences. 2014;24:29–40. 10.4314/ejhs.v24i0.4s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jena BH, Biks GA, Gelaye KA, Gete YK. Magnitude and trend of perinatal mortality and its relationship with inter-pregnancy interval in Ethiopia: a systematic review and meta-analysis. BMC pregnancy and childbirth. 2020;20(1):432–. 10.1186/s12884-020-03089-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Central Statistical Agency ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016.
- 8.World Health Organization. Global nutrition targets 2025: low birth weight policy brief (WHO/NMH/NHD/14.5). Avenue Appia 20, CH-1211 Geneva 27, Switzerland: World Health Organization, Development NfHa; 2014. [Google Scholar]
- 9.Vogel JP, Habib NA, Souza JP, Gülmezoglu AM, Dowswell T, Carroli G, et al. Antenatal care packages with reduced visits and perinatal mortality: a secondary analysis of the WHO Antenatal Care Trial. Reproductive health. 2013;10(1):19 10.1186/1742-4755-10-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ataguba JE-O. A reassessment of global antenatal care coverage for improving maternal health using sub-Saharan Africa as a case study. PloS one. 2018;13(10):e0204822 10.1371/journal.pone.0204822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stacey T, Thompson JM, Mitchell EA, Zuccollo JM, Ekeroma AJ, McCOWAN LM. Antenatal care, identification of suboptimal fetal growth and risk of late stillbirth: F indings from the A uckland S tillbirth S tudy. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2012;52(3):242–7. 10.1111/j.1479-828X.2011.01406.x [DOI] [PubMed] [Google Scholar]
- 12.Gumede S, Black V, Naidoo N, Chersich MF. Attendance at antenatal clinics in inner-city Johannesburg, South Africa and its associations with birth outcomes: analysis of data from birth registers at three facilities. BMC Public Health. 2017;17(3):443 10.1186/s12889-017-4347-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heaman MI, Martens PJ, Brownell MD, Chartier MJ, Derksen SA, Helewa ME. The association of inadequate and intensive prenatal care with maternal, fetal, and infant outcomes: A population-based study in Manitoba, Canada. Journal of Obstetrics and Gynaecology Canada. 2019;41(7):947–59. 10.1016/j.jogc.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 14.Worku AG, Yalew AW, Afework MF. The contributions of maternity care to reducing adverse pregnancy outcomes: a cohort study in Dabat District, Northwest Ethiopia. Maternal and child health journal. 2014;18(6):1336–44. 10.1007/s10995-013-1367-x [DOI] [PubMed] [Google Scholar]
- 15.Van Dijk JAW, Anderko L, Stetzer F. The impact of prenatal care coordination on birth outcomes. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2011;40(1):98–108. 10.1111/j.1552-6909.2010.01206.x [DOI] [PubMed] [Google Scholar]
- 16.Rosário EVN, Gomes MC, Brito M, Costa D. Determinants of maternal health care and birth outcome in the Dande Health and Demographic Surveillance System area, Angola. PloS one. 2019;14(8). 10.1371/journal.pone.0221280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blondel B, Dutilh P, Delour M, Uzan S. Poor antenatal care and pregnancy outcome. European Journal of Obstetrics & Gynecology and Reproductive Biology. 1993;50(3):191–6. 10.1016/0028-2243(93)90200-v [DOI] [PubMed] [Google Scholar]
- 18.Cotzias CS, Paterson-Brown S, Fisk NM. Prospective risk of unexplained stillbirth in singleton pregnancies at term: population based analysis. Bmj. 1999;319(7205):287–8. 10.1136/bmj.319.7205.287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saleem S, Tikmani SS, McClure EM, Moore JL, Azam SI, Dhaded SM, et al. Trends and determinants of stillbirth in developing countries: results from the Global Network’s Population-Based Birth Registry. Reproductive health. 2018;15(1):100 10.1186/s12978-018-0526-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurniasih NID, Sulistyaningsih I, editors. EFFORT FOR UTILIZATION ANTENATAL CARE (ANC) IN PREGNANT WOMEN: systematic literature review. Proceeding International Conference; 2019.
- 21.Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: A systematic review and meta-analysis. PloS one. 2019;14(9):1–15. 10.1371/journal.pone.0222566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wondemagegn AT, Alebel A, Tesema C, Abie W. The effect of antenatal care follow-up on neonatal health outcomes: a systematic review and meta-analysis. Public health reviews. 2018;39(1):33 10.1186/s40985-018-0110-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arunda M, Emmelin A, Asamoah BO. Effectiveness of antenatal care services in reducing neonatal mortality in Kenya: analysis of national survey data. Global Health Action. 2017;10(1):1328796 10.1080/16549716.2017.1328796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roy S, Haque MA. Effect of antenatal care and social well-being on early neonatal mortality in Bangladesh. BMC pregnancy and childbirth. 2018;18(1):485 10.1186/s12884-018-2129-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kidus F, Woldemichael K, Hiko D. Predictors of neonatal mortality in Assosa zone, Western Ethiopia: a matched case control study. BMC pregnancy and childbirth. 2019;19(1):108 10.1186/s12884-019-2243-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Orsido TT, Asseffa NA, Berheto TM. Predictors of Neonatal mortality in Neonatal intensive care unit at referral Hospital in Southern Ethiopia: a retrospective cohort study. BMC pregnancy and childbirth. 2019;19(1):83 10.1186/s12884-019-2227-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belachew A, Tewabe T, Dessie G. Neonatal mortality and its association with antenatal care visits among live births in Ethiopia: a systematic review and meta-analysis. The Journal of Maternal-Fetal & Neonatal Medicine. 2020:1–8. 10.1080/14767058.2020.1718093 [DOI] [PubMed] [Google Scholar]
- 28.Zhou H, Wang A, Huang X, Guo S, Yang Y, Martin K, et al. Quality antenatal care protects against low birth weight in 42 poor counties of Western China. PloS one. 2019;14(1). 10.1371/journal.pone.0210393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yaya S, Bishwajit G, Ekholuenetale M, Shah V. Inadequate utilization of prenatal care services, socioeconomic status, and educational attainment are associated with low birth weight in Zimbabwe. Frontiers in public health. 2017;5:35 10.3389/fpubh.2017.00035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tayebi T, Hamzehgardeshi Z, Shirvani MA, Dayhimi M, Danesh M. Relationship between Revised Graduated Index (R-GINDEX) of prenatal care utilization & preterm labor and low birth weight. Global journal of health science. 2014;6(3):131 10.5539/gjhs.v6n3p131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, Van Den Broek N. Causes of and factors associated with stillbirth in low‐and middle‐income countries: a systematic literature review. BJOG: An International Journal of Obstetrics & Gynaecology. 2014;121:141–53. 10.1111/1471-0528.12995 [DOI] [PubMed] [Google Scholar]
- 32.Adam T, Lim SS, Mehta S, Bhutta ZA, Fogstad H, Mathai M, et al. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. Bmj. 2005;331(7525):1107 10.1136/bmj.331.7525.1107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hollowell J, Oakley L, Kurinczuk JJ, Brocklehurst P, Gray R. The effectiveness of antenatal care programmes to reduce infant mortality and preterm birth in socially disadvantaged and vulnerable women in high-income countries: a systematic review. BMC pregnancy and childbirth. 2011;11(1):13 10.1186/1471-2393-11-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carroli G, Villar J, Piaggio G, Khan-Neelofur D, Gülmezoglu M, Mugford M, et al. WHO systematic review of randomised controlled trials of routine antenatal care. The Lancet. 2001;357(9268):1565–70. 10.1016/S0140-6736(00)04723-1 [DOI] [PubMed] [Google Scholar]
- 35.Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, De Bernis L, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? The Lancet. 2005;365(9463):977–88. 10.1016/S0140-6736(05)71088-6 [DOI] [PubMed] [Google Scholar]
- 36.Tesema GA, Gezie LD, Nigatu SG. Trends of stillbirth among reproductive-age women in Ethiopia based on Ethiopian demographic and health surveys: a multivariate decomposition analysis. BMC pregnancy and childbirth. 2020;20(193):1–11. 10.1186/s12884-020-02880-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kapoor SKR, Lobo V. P, J Antenatal care and perinatal mortality. the Indian Journal of Pediatrics. 1985;52:159–62. 10.1007/BF02754777 [DOI] [PubMed] [Google Scholar]
- 38.Haque SRaA. Effect of antenatal care and social well-being on early neonatal mortality in Bangladesh. BMC pregnancy and childbirth. 2018;18(485). 10.1186/s12884-018-2129-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghimire PR, Agho KE, Akombi BJ, Wali N, Dibley M, Raynes-Greenow C, et al. Perinatal mortality in south Asia: Systematic Review of Observational Studies. International Journal of Environmental Research and Public Health. 2018;15(7):1428 10.3390/ijerph15071428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Australia nstitute of Health and walfare. Perinatal death in Australia: 2013–2014 Cat.no. PER 94. Camberra: AIHW: 2018. [Google Scholar]
- 41.Tuladhar H, Dhakal N. Impact of antenatal care on maternal and perinatal utcome: a study at Nepal medical college teaching hospital. Nepal Journal of Obstetrics and Gynaecology. 2011;6(2):37–43. 10.3126/njog.v6i2.6755. [DOI] [Google Scholar]
- 42.Pasha O, McClure EM, Wright LL, Saleem S, Goudar SS, Chomba E, et al. A combined community-and facility-based approach to improve pregnancy outcomes in low-resource settings: a Global Network cluster randomized trial. BMC medicine. 2013;11(1):215 10.1186/1741-7015-11-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rumbold AR, Cunningham J. A review of the impact of antenatal care for Australian Indigenous women and attempts to strengthen these services. Maternal and child health journal. 2008;12(1):83–100. 10.1007/s10995-007-0216-1 [DOI] [PubMed] [Google Scholar]
- 44.Fiscella K. Does prenatal care improve birth outcomes? A critical review. Obstetrics & Gynecology. 1995;85(3):468–79. 10.1016/0029-7844(94)00408-6 [DOI] [PubMed] [Google Scholar]
- 45.Dowswell T, Carroli G, Duley L, Gates S, Gülmezoglu AM, Khan‐Neelofur D, et al. Alternative versus standard packages of antenatal care for low‐risk pregnancy. Cochrane Database of Systematic Reviews. 2015;(7). 10.1002/14651858.CD000934.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shukla VV, Carlo WA. Review of the evidence for interventions to reduce perinatal mortality in low-and middle-income countries. International Journal of Pediatrics and Adolescent Medicine. 2020. 10.1016/j.ijpam.2020.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every Newborn: progress, priorities, and potential beyond survival. The Lancet. 2014;384(9938):189–205. 10.1016/S0140-6736(14)60496-7. [DOI] [PubMed] [Google Scholar]
- 48.Qureshi ZU, Millum J, Blencowe H, Kelley M, Fottrell E, Lawn JE, et al. Stillbirth should be given greater priority on the global health agenda. Bmj. 2015;351:h4620 10.1136/bmj.h4620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4(1):1 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta A, Cecilia A. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA. 2006;295 (15): 1837–8. 10.1001/jama.295.15.1837 [DOI] [PubMed] [Google Scholar]
- 51.Ota E, Ganchimeg T, Morisaki N, Vogel JP, Pileggi C, Ortiz-Panozo E, et al. Risk factors and adverse perinatal outcomes among term and preterm infants born small-for-gestational-age: secondary analyses of the WHO Multi-Country Survey on Maternal and Newborn Health. PloS one. 2014;9(8). 10.1371/journal.pone.0105155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pileggi‐Castro C, Camelo J Jr, Perdoná G, Mussi‐Pinhata M, Cecatti J, Mori R, et al. Development of criteria for identifying neonatal near‐miss cases: analysis of two WHO multicountry cross‐sectional studies. BJOG: An International Journal of Obstetrics & Gynaecology. 2014;121:110–8. 10.1111/1471-0528.12637 [DOI] [PubMed] [Google Scholar]
- 53.Debelew GT, Afework MF, Yalew AW. Determinants and causes of neonatal mortality in Jimma zone, southwest Ethiopia: a multilevel analysis of prospective follow up study. PloS one. 2014;9(9):e107184 10.1371/journal.pone.0107184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karthik L, Kumar G, Keswani T, Bhattacharyya A, Chandar SS, Rao KB. Protease inhibitors from marine actinobacteria as a potential source for antimalarial compound. PloS one. 2014;9(3):e90972 10.1371/journal.pone.0090972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meier PP, Engstrom JL, Janes JE, Jegier BJ, Loera F. Breast pump suction patterns that mimic the human infant during breastfeeding: greater milk output in less time spent pumping for breast pump-dependent mothers with premature infants. Journal of Perinatology. 2012;32(2):103–10. 10.1038/jp.2011.64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Engmann C, Matendo R, Kinoshita R, Ditekemena J, Moore J, Goldenberg RL, et al. Stillbirth and early neonatal mortality in rural Central Africa. International Journal of Gynecology & Obstetrics. 2009;105(2):112–7. 10.1016/j.ijgo.2008.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Engmann C, Walega P, Aborigo RA, Adongo P, Moyer CA, Lavasani L, et al. Stillbirths and early neonatal mortality in rural Northern Ghana. Tropical Medicine & International Health. 2012;17(3):272–82. 10.1111/j.1365-3156.2011.02931.x [DOI] [PubMed] [Google Scholar]
- 58.Welaga P, Moyer CA, Aborigo R, Adongo P, Williams J, Hodgson A, et al. Why are babies dying in the first month after birth? A 7-year study of neonatal mortality in northern Ghana. PloS one. 2013;8(3):e58924 10.1371/journal.pone.0058924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lincetto S-AO, Gomez P, Munjanja S. Antenatal care Opportunities for Africa’s newborns: practical data, policy and programmatic support for newborn care in Africa: World Health Organisation; 2006. [Google Scholar]
- 60.Guevvera Y. World Health Organisation: Neonatal and perinatal mortality: country, regional and global estimates. WHO cebu: sun: 2006. [Google Scholar]
- 61.World Health Organization. Maternal, newborn, child and adolescent health 2020. [cited 2020]. Available from: https://www.who.int/maternal_child_adolescent/topics/maternal/maternal_perinatal/en/. [Google Scholar]
- 62.Liyew EF, Yalew AW, Afework MF, Essén B. Maternal near-miss and the risk of adverse perinatal outcomes: a prospective cohort study in selected public hospitals of Addis Ababa, Ethiopia. BMC pregnancy and childbirth. 2018;18(1):345 10.1186/s12884-018-1983-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.WHO R. Definitions and indicators in family planning and maternal and child health and reproductive health. European Regional Office World Health Organization; 2001. [Google Scholar]
- 64.World Health Organization. Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. 20 Avenue Appia, 1211 Geneva 27, Switzerland: World health organization; 2004. [Google Scholar]
- 65.Kim SY, Park JE, Lee YJ, Seo H-J, Sheen S-S, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. Journal of clinical epidemiology. 2013;66(4):408–14. 10.1016/j.jclinepi.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 66.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7(3):177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 67.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315(7109):629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Desta M, Tadese M, Kassie B, Gedefaw M. Determinants and adverse perinatal outcomes of low birth weight newborns delivered in Hawassa University Comprehensive Specialized Hospital, Ethiopia: a cohort study. BMC research notes. 2019;12(1):118 10.1186/s13104-019-4155-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Haftu A, Hagos H, Mehari M-A. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray Public Health institutions, 2017: cohort study. BMC research notes. 2018;11(1):872 10.1186/s13104-018-3987-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Berhe T, Gebreyesus H, Teklay H. Prevalence and determinants of stillbirth among women attended deliveries in Aksum General Hospital: a facility based cross-sectional study. BMC research notes. 2019;12(1):368 10.1186/s13104-019-4397-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bililign Yimer N, Tenaw Z, Solomon K, Mulatu T. Inadequate prenatal visit and home delivery as determinants of perinatal outcomes: does parity matter? Journal of pregnancy. 2019;2019 10.1155/2019/9024258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Agena AG, Modiba LM. Maternal and foetal medical conditions during pregnancy as determinants of intrapartum stillbirth in public health facilities of Addis Ababa: a case-control study. The Pan African medical journal. 2019;33(21). 10.11604/pamj.2019.33.21.17728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tewabe T, Mehariw Y, Negatie E, Yibeltal B. Neonatal mortality in the case of Felege Hiwot referral hospital, Bahir Dar, Amhara Regional State, North West Ethiopia 2016: a one year retrospective chart review. Italian journal of pediatrics. 2018;44(1):1–5. 10.1186/s13052-017-0437-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Assefa N, Berhane Y, Worku A, Tsui A. The hazard of pregnancy loss and stillbirth among women in Kersa, East Ethiopia: A follow up study. Sexual & Reproductive Healthcare. 2012;3(3):107–12. 10.1016/j.srhc.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 76.Hailemichael HT, Debelew GT, Alema HB, Weldu MG, Misgina KH. Determinants of adverse birth outcome in Tigrai region, North Ethiopia: Hospital-based case-control study. BMC Pediatrics. 2020;20(1):1–9. 10.1186/s12887-019-1898-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Abdo R, Endalemaw T, Tesso F. Prevalence and associated factors of adverse birth outcomes among women attended maternity ward at Negest Elene Mohammed Memorial General Hospital in Hosanna Town, SNNPR, Ethiopia. J Women’s Health Care. 2016;5(4). [Google Scholar]
- 78.Cherie N, Mebratu A. Adverse Birth Out Comes and Associated Factors among Delivered Mothers in Dessie Referral Hospital. North East Ethiopia. 2018:1–6. 10.33805/2573-3877.121. [DOI] [Google Scholar]
- 79.Tsegaye B, Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reproductive health. 2018;15(1):193 10.1186/s12978-018-0631-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sahle-Mariam Y, Berhane Y. Neonatal mortality among hospital delivered babies in Addis Ababa, Ethiopia. The Ethiopian Journal of Health Development (EJHD). 1997;11(3). [Google Scholar]
- 81.Mengesha HG, Wuneh AD, Lerebo WT, Tekle TH. Survival of neonates and predictors of their mortality in Tigray region, Northern Ethiopia: prospective cohort study. BMC pregnancy and childbirth. 2016;16(1):202 10.1186/s12884-016-0994-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shifa GT, Ahmed AA, Yalew AW. Early days of life are crucial for child survival in Gamo Gofa zone, southern Ethiopia: a community based study. BMC Pediatrics. 2016;16(1):30 10.1186/s12887-016-0568-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Asefa D, Akessa G, Araya F, Amenu D, Girma W. Pattern of Perinatal Mortality among Deliveries at Jimma University Teaching Hospital, South-West Ethiopia. J Womens Health, Issues Care 5. 2016;6:2 10.4172/2325-9795.1000252 [DOI] [Google Scholar]
- 84.Woldeamanuel BT, Gelebo KK. Statistical analysis of socioeconomic and demographic correlates of perinatal mortality in Tigray region, Ethiopia: a cross sectional study. BMC Public Health. 2019;19(1):1301 10.1186/s12889-019-7642-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Atnafu H, Belete Z, Kinfu H, Tadesse M, Amin M, Ballard KD. Can a community-based maternal care package in rural Ethiopia increase the use of health facilities for childbirth and reduce the stillbirth rate? International Journal of Women's Health. 2016;8:421 10.2147/IJWH.S104160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yaya Y, Eide KT, Norheim OF, Lindtjørn B. Maternal and neonatal mortality in south-west Ethiopia: estimates and socio-economic inequality. PloS one. 2014;9(4):e96294 10.1371/journal.pone.0096294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sirak B, Mesfin E. Maternal and perinatal outcome of pregnancies with preterm premature rupture of membranes (pprom) at tikur anbessa specialized teaching hospital, addis ababa, ethiopia. Ethiopian medical journal. 2014;52(4):165–72. [PubMed] [Google Scholar]
- 88.Yirgu R, Molla M, Sibley L, Gebremariam A. Perinatal mortality magnitude, determinants and causes in west Gojam: population-based nested case-control study. PloS one. 2016;11(7):e0159390 10.1371/journal.pone.0159390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Andargie G, Berhane Y, Worku A, Kebede Y. Predictors of perinatal mortality in rural population of Northwest Ethiopia: a prospective longitudinal study. BMC Public Health. 2013;13(1):168 http://www.biomedcentral.com/1471-2458/13/168. 10.1186/1471-2458-13-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM. Adverse birth outcomes among deliveries at Gondar University hospital, Northwest Ethiopia. BMC pregnancy and childbirth. 2014;14(1):90 http://www.biomedcentral.com/1471-2393/14/90. 10.1186/1471-2393-14-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Goba GK, Tsegay H, Gebregergs GB, Mitiku M, Kim KA, Alemayehu M. A facility‐based study of factors associated with perinatal mortality in Tigray, northern Ethiopia. International Journal of Gynecology & Obstetrics. 2018;141(1):113–9. 10.1002/ijgo.12438 [DOI] [PubMed] [Google Scholar]
- 92.Roro EM, Sisay MM, Sibley LM. Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Public Health. 2018;18(1):888 10.1186/s12889-018-5757-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Welegebriel TK, Dadi TL, Mihrete KM. Determinants of stillbirth in Bonga General and Mizan Tepi University Teaching Hospitals southwestern Ethiopia, 2016: a case–control study. BMC research notes. 2017;10(1):713 10.1186/s13104-017-3058-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Worede DT, Dagnew GW. Determinants of stillbirth in Felege-Hiwot comprehensive specialized referral hospital, North-west, Ethiopia, 2019. BMC research notes. 2019;12(1):579 10.1186/s13104-019-4621-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Getiye Y, Fantahun M. Factors associated with perinatal mortality among public health deliveries in Addis Ababa, Ethiopia, an unmatched case control study. BMC pregnancy and childbirth. 2017;17(1):245 10.1186/s12884-017-1420-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tilahun D, Assefa T. Incidence and determinants of stillbirth among women who gave birth in Jimma University specialized hospital, Ethiopia. Pan African Medical Journal. 2017;28(1). 10.11604/pamj.2017.28.299.1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Berhie KA, Gebresilassie HG. Logistic regression analysis on the determinants of stillbirth in Ethiopia. Maternal health, neonatology and perinatology. 2016;2(1):10 10.1186/s40748-016-0038-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tilahun S, Gaym A. Past reproductive performance and its correlation with perinatal mortality in the current gestation at teaching hospitals in Addis Ababa, Ethiopia. Ethiopian medical journal. 2008;46(4):313–24. [PubMed] [Google Scholar]
- 99.Ballard K, Belete Z, Kinfu H, Tadesse M, Amin M, Atnafu H. The effect of prenatal and intrapartum care on the stillbirth rate among women in rural Ethiopia. International Journal of Gynecology & Obstetrics. 2016;133(2):164–7. 10.1016/j.ijgo.2015.09.027 [DOI] [PubMed] [Google Scholar]
- 100.Tadesse E, Worku B. Perinatal mortality audit at Tikure Anbessa Teaching Hospital, Addis Ababa, Ethiopia: 1995 to 1996. Malawi medical journal: the journal of Medical Association of Malawi. 2003;15(3):102. [PMC free article] [PubMed] [Google Scholar]
- 101.Lakew D, Tesfaye D, Mekonnen H. Determinants of stillbirth among women deliveries at Amhara region, Ethiopia. BMC pregnancy and childbirth. 2017;17(1):375 10.1186/s12884-017-1573-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Berhan Y. Predictors of perinatal mortality associated with placenta previa and placental abruption: an experience from a low income country. Journal of pregnancy. 2014;2014 10.1155/2014/307043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chekol A. Birth outcome and HIV infection among labouring women in Assosa Hospital, Southwest Ethiopia. Ethiopian Journal of Health Development. 2011;25(1):10–6. 10.4314/ejhd.v25i1.69840 [DOI] [Google Scholar]
- 104.Aragaw Y. Perinatal mortality and associated factor in Jimma university specialized hospital, South West Ethiopia. Gynecol Obstet (Sunnyvale). 2016;6(409):2161–0932. 10.4172/2161-0932.1000409 [DOI] [Google Scholar]
- 105.Mihiretu A, Negash T, Elazar T. Perinatal Death and Associated Factors in Wolaita Sodo Referral Hospital, Southern Ethiopia: a Facility Based Cross-Sectional Study. Primary Health Care: Open Access. 2017;7(2):1–5. 10.4172/2167-1079.1000269 [DOI] [Google Scholar]
- 106.Stephenson P. Focused Antenatal Care: A Better, Cheaper, Faster, Evidence-based Approach. 2005. [Google Scholar]
- 107.Dujardin B, Clarysse G, Criel B, De Brouwere V, Wangata N. The strategy of risk approach in antenatal care: evaluation of the referral compliance. Social Science & Medicine. 1995;40(4):529–35. 10.1016/0277-9536(94)e0095-a [DOI] [PubMed] [Google Scholar]
- 108.Yuster E. Rethinking the role of the risk approach and antenatal care in maternal mortality reduction. International journal of gynecology & obstetrics. 1995;50:S59–S61. 10.1016/0020-7292(95)02488-X [DOI] [PubMed] [Google Scholar]
- 109.Tunçalp Ӧ, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG: an international journal of obstetrics and gynaecology. 2017;124(6):860–2. 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 110.World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience: World Health Organization; 2016. [PubMed] [Google Scholar]
- 111.Gogia S, Sachdev H. Home-based neonatal care by community health workers for preventing mortality in neonates in low-and middle-income countries: a systematic review. Journal of Perinatology. 2016;36(1):S55–S73. 10.1038/jp.2016.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yakoob MY, Ali MA, Ali MU, Imdad A, Lawn JE, Van Den Broek N, et al. The effect of providing skilled birth attendance and emergency obstetric care in preventing stillbirths. BMC Public Health. 2011;11(S3):S7 10.1186/1471-2458-11-S3-S7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? The Lancet. 2014;384(9940):347–70. 10.1016/S0140-6736(14)60792-3. [DOI] [PubMed] [Google Scholar]
- 114.Chinkhumba J, De Allegri M, Muula AS, Robberstad B. Maternal and perinatal mortality by place of delivery in sub-Saharan Africa: a meta-analysis of population-based cohort studies. BMC Public Health. 2014;14(1):1–9. 10.1186/1471-2458-14-1014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gordon A, Raynes-Greenow C, McGeechan K, Morris J, Jeffery H. Risk factors for antepartum stillbirth and the influence of maternal age in New South Wales Australia: a population based study. BMC pregnancy and childbirth. 2013;13(1):12 10.1186/1471-2393-13-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Haider BA, Bhutta ZA. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews. 2017;(4). 10.1002/14651858.CD004905.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rumbold A, Ota E, Nagata C, Shahrook S, Crowther CA. Vitamin C supplementation in pregnancy. Cochrane Database of Systematic Reviews. 2015;(9). 10.1002/14651858.CD004072.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McCauley ME, van den Broek N, Dou L, Othman M. Vitamin A supplementation during pregnancy for maternal and newborn outcomes. Cochrane Database of Systematic Reviews. 2015;(10). 10.1002/14651858.CD008666.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Titaley CR, Dibley MJ. Antenatal iron/folic acid supplements, but not postnatal care, prevents neonatal deaths in Indonesia: analysis of Indonesia Demographic and Health Surveys 2002/2003–2007 (a retrospective cohort study). BMJ Open. 2012;2(6). 10.1136/bmjopen-2012-001399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fekadu GA, Kassa GM, Berhe AK, Muche AA, Katiso NA. The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: a systematic review and meta-analysis. BMC health services research. 2018;18(1):577 10.1186/s12913-018-3370-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lee AC, Cousens S, Wall SN, Niermeyer S, Darmstadt GL, Carlo WA, et al. Neonatal resuscitation and immediate newborn assessment and stimulation for the prevention of neonatal deaths: a systematic review, meta-analysis and Delphi estimation of mortality effect. BMC Public Health. 2011;11(S3):S12 10.1186/1471-2458-11-S3-S12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Patel A, Khatib MN, Kurhe K, Bhargava S, Bang A. Impact of neonatal resuscitation trainings on neonatal and perinatal mortality: a systematic review and meta-analysis. BMJ Paediatrics Open. 2017;1(1). 10.1136/bmjpo-2017-000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. Stillbirths: Where? When? Why? How to make the data count? The Lancet. 2011;377(9775):1448–63. 10.1016/S0140-6736(10)62187-3 [DOI] [PubMed] [Google Scholar]
- 124.Ghosh B, Solomon F, Gobeze AA, Phillips R, East M. Why are pregnant women and newborns still dying in rural Ethiopia? African Journal of Midwifery and Women's Health. 2012;6(3):115–9. 10.12968/ajmw.2012.6.3.115. [DOI] [Google Scholar]
- 125.Vogel J, Souza J, Mori R, Morisaki N, Lumbiganon P, Laopaiboon M, et al. Maternal complications and perinatal mortality: findings of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG: An International Journal of Obstetrics & Gynaecology. 2014;121:76–88. 10.1111/1471-0528.12633 [DOI] [PubMed] [Google Scholar]