Abstract
Introduction
Independently, trauma and appendicitis are two of the most common conditions in surgical practice. Rarely, both conditions may coexist, which raises the controversy whether it is merely a coincidence or trauma may lead to acute appendicitis. Presentation of Case. We report a case of acute appendicitis after blunt abdominal trauma caused by a camel hoof kick to the abdomen in a young man and discuss the potential underlying pathophysiologic mechanisms with review of the pertinent literature.
Conclusions
Blunt abdominal trauma caused by a camel kick to the abdomen requires a close observation of the patients. A camel kick may increase intra-abdominal pressure and cause internal organ injury including the appendix. Therefore, acute appendicitis should be considered in differential diagnosis in any patient with abdominal pain resembling appendicitis following blunt abdominal trauma.
1. Introduction
Appendicitis is one of the most common surgical conditions affecting about 7% of people during their lifetime [1]. The etiology of acute appendicitis is multifactorial, with luminal obstruction being considered the major cause [1]. Blunt abdominal trauma (BAT) has been infrequently reported as a possible cause for acute appendicitis; however, most of the reported cases were in pediatric age group (Table 1). Herein, we report a rare case of acute appendicitis after blunt abdominal trauma caused by a camel hoof kick to the abdomen.
Table 1.
Summary of the case reports with publication year showing the cases of acute appendicitis secondary to traumatic abdominal injuries.
| Study∗ | Sex | Age | PH | MOI | Presentation | D | Examination | Labs | XR | US | CT | Surgery | Intraop | Histo | HS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current study Qatar |
M | 35 y | UR | Camel kick | RLQ pain few hours after the kick, anorexia, V | 2 d | Vit: Nr, RLQ bruise, tenderness | WBC: 15.5, CRP: 90.5, bilirubin: 29.1 | NR | NR | Ap 16 mm, wall enhancement, periappendiceal fat stranding | L Appy | AA | AA | 12 h |
| Zvizdic 2019 Bosnia & Herzegovina Cc [2] |
M | 7 y | UR | Horse kick | Sudden, progressive pain in RLQ, V | 10 h | BP: 95/55, P: 110, T: 38.3, RR: 18. Abrasions, swelling tenderness and guarding RLQ | WBC: 11.5, Hb: 13.2, Plt: 280 | NR | Pericecal free fluid, extending to pouch of Douglas | Small focus of free peritoneal air, free pelvic fluid | Lap, Appy | Perf AA with localized peritonitis | Perf AA, full thickness inflammation of Ap wall | 6 d postop |
| Cobb 2017 U.S [6] |
M | 17 y | AD | MVC | Diffuse progressive Abd pain 24 h after MVC, V 10 times | NR | Vit: Nr, tender in both LQ's (Lt>Rt) and Lt upper quadrant | WBC: 10.8, Hb: 15.8, Plt: 243 | Abd XR: abnormal bowel loop RLQ | NR | Dilated Ap 1.3 cm surrounding fluid in RLQ and pelvis | L Ex, Lap, Appy | Inflamed Ap, dark fluid in RLQ concerning for viscus injury | AA | 10 d postop |
| Ahmed 2014 India [4] |
M | 12 y | UR | Hit disk's corner | Periumbilical Abd pain 1 d after trauma, fever | 1 d | P: 114, BP: 90/56, minimal Abd movement with resp, bruise RLQ, rigid diffusely tender abdomen | WBC: 17, Hb: 10.5 | Abd XR: air under diaphragm | Pelvic free fluid | NR | Ex Lap, Appy | Pus in pelvis, Perf AA at tip | AA | >4 d |
| Paschos 2012 Greece [7] |
F | 17 y | UR | Bicycle accident | Abd pain 12 h after trauma, discharged and came back with pain, anorexia, N&V | 1 d | Vit: Nr, ecchymosis and tenderness RLQ | WBC: 9.1, on readmission: 12.7, Hb: 1.95 mmol/L | NR | Abd free fluid | NR | Lap, Appy | Free fluid, AA, contusion cecal base | AA | 2 d |
| Torres-Grau 2012 UK [3] |
M | 15 | UR | Fall from bicycle | Abd pain 30 m after fall | 6 h | BP: 105/47, P: 57, T: 36.7, RLQ tenderness | WBC: 16.2, Neu: 13.6, Hb: 14.4, CRP: 1 Amy | NR | Free fluid in the peritoneum | NR | L Ex, Appy | Necrotic, non-Perf Ap | AA | NR |
| Atalla 2010 Australia [8] |
M | 53 y | UR | Fall on edge of car door | Abd pain 7 h after fall | 7 h | P: ↑, BP: ↓, RLQ tenderness and guarding | WBC: ↑ | NR | UR | Thickened Ap (10 mm) with fat stranding | L Ex, Appy | AA | AA | 1 d postop |
| Toumi 2010 UK [1] |
M | 11 y | UR | Injury by elbow to RLQ | Abd pain after trauma, N&V, anorexia, fever | 3 d | T: ↑, P: ↑, RLQ tenderness | UA: trace blood; Inf m: ↑ | NR | NR | AA with adjacent collection | Appy | AA | AA serositis | 4 d postop |
| Etensel 2005 Turkey [9] |
M | 9 y | NR | Fall | Polytrauma | 1 h | BP: 80/50, P: 86, T: 36.7, confused, resp dist, head and Lt chest abrasions, ↓ breath sounds Lt chest | Hb: 11.2, WBC: 17.2 | Chest and Abd XR: Lt lung contusion, free peritoneal air | Free air | Head CT: brain edema, Lt parietal bone fx; Abd CT: free air | Lap, Appy | AA, no bowel Perf | AA | 10 d |
| Houry 2001 Colarado [10]. |
M | 5 y | UR | Fall | Abd pain | 1 h | BP: 114/75, P: 149, RR:32, T: 37.7, Abd tenderness and guarding more in RLQ | N | N | Free fluid in pouch of Douglas | Pelvic free fluid, AA | Ex Lap, Appy | AA, Perf at the base | AA | NR |
| Serour 1996 Israel [11] |
M | 11 y | UR | Punch | RLQ pain, N&V | 18 h | BP: 115/60, P: 100, T: 37, looked ill, RLQ tenderness | Hb: 13.7, WBC: 4.5 | NR | NR | Calcified appendicolith, prerectal fluid | Lap. Appy | Gangrenous Ap | Gangrenous appendicitis with periappendicitis | NR |
| Serour 1996 Israel [11] |
M | 8 y | UR | Fall | Abd pain, N and fever | 3 h | BP: 95/55, P: 96, T: 38.2, ecchymosis over right side of the face, RLQ tenderness, guarding, and rebound | Hb: 12.5, WBC: 20.1 | NR | NR | NR | Appy | AA | Phlegmonous appendicitis with periappendicitis | NR |
| Serour 1996 Israel [11] |
M | 7 y | UR | Fight | Abd pain, fever, V | Few d | T: 40, acute Abd | NR | NR | NR | Abscess in RLQ | Appy, drainage of abscess | Gangrenous Perf Ap | Gangrenous Perf appendicitis | NR |
| Ciftci 1996 Turkey [12] |
M | 8 | NR | MVC | Abd pain | 2 h | NR | NR | NR | NR | NR | Appy | Perf Ap | AA | Average hospital stay 6.4 d |
| Ciftci 1996 Turkey [12] |
F | 5 | NR | Fall | Abd pain | 6 h | NR | NR | NR | NR | NR | Appy | AA | AA | |
| Ciftci 1996 Turkey [12] |
F | 13 | NR | Ball | N | 12 h | NR | NR | NR | NR | NR | Appy | AA | AA | |
| Ciftci 1996 Turkey [12] |
M | 14 | NR | MVC | Abd pain | 4 h | NR | NR | NR | NR | Dilated bowel loops, free fluid | Appy | Perf Ap | AA | |
| Ciftci 1996 Turkey [12] |
M | 7 | NR | Assault | Abd pain | 12 h | NR | NR | NR | NR | Dilated bowel loops, free fluid | Appy | AA | AA |
∗For space considerations, only the first author is cited; AA: acute appendicitis; Abd: abdomen/al; AD: atopic dermatitis; Ap: appendix/appendiceal; Appy: appendectomy; BP: blood pressure in mmHg; CRP: C-reactive protein; D: duration of symptoms; d: days; diaph: diaphragm/atic; Ex: exploratory/ion; fx: fracture; h: hour/s; Hb: hemoglobin g/dL; Hem: hematoma; Histo: histology; HS: hospital stay postoperatively; Intraop: intraoperative findings; Inf m: inflammatory markers; I.O: intestinal obstruction; L: laparoscopic; Lap: laparotomy; LQ: lower quadrant; Lt: left; M: male; m: month/s; min: minute/s; McB: McBurney's point; MOI: mechanism of injury; MVC: motor vehicle collision; N: nausea; Neu: neutrophils; NR: not reported; Nr: normal; P: pulse in beats per minute; Perf: perforation; PH: past history; pneumomed: pneumomediastinum; Plt: platelets K/μL; postop: postoperative; resp: respiration; Retro: retroperitoneal; resp dist: respiratory distress; RLQ: right lower quadrant; RR: respiratory rate; Rt: right; T: temperature °C; UA: urine analysis; UR: unremarkable; V: vomiting; Vit: vital signs; WBC: white blood cell count K/μL; y: year/s; ↑: high; ↓: low.
2. Case Presentation
A 35-year-old Bangladeshi man presented to the emergency department at Hamad Medical Corporation, Doha, Qatar, with two-day history of progressive right lower abdominal pain, associated with four times vomiting and loss of appetite. He was doing completely well but developed these symptoms few hours after a strong direct camel kick on his right abdomen. He did not have any urological symptoms, nor any comorbidities, and his systemic review was unremarkable.
The patient was conscious and had normal vital signs. Generally, was looking well, abdominal examination showed a right lower abdominal bruise, tenderness, rebound tenderness, and involuntary guarding in the right iliac fossa. Head to toe examination showed no other signs of trauma. Laboratory tests showed high inflammatory markers (white blood cell count (WBC) 15.5 K/μL, hemoglobin 15.3 g/dL, platelets 207 K/μL, CRP: 90.5, and bilirubin: 29.1). CT abdomen with IV and oral contrast was done and showed a dilated appendix in the right iliac fossa (16 mm in diameter), with wall enhancement and periappendiceal fat stranding (Figure 1). The patient was diagnosed with acute appendicitis, and an emergency laparoscopic appendectomy was performed. Intraoperative findings showed grossly inflamed appendix with fibrinous exudate with no collection or perforation (Figure 2), and the inspected other intra-abdominal solid and hollow organs were normal. Postoperatively, the patient recovered well and was discharged one day after surgery. On follow-up 2 weeks in the clinic, he was completely healthy, wounds were healed, and histopathology confirmed the diagnosis of acute appendicitis.
Figure 1.
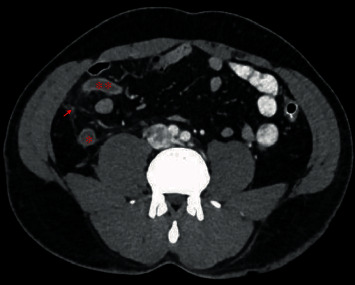
Abdomen CT scan with IV and oral contrast showing dilated appendicular tip (∗∗) and base (∗), with periappendiceal fat stranding (arrow) and enhancing wall.
Figure 2.
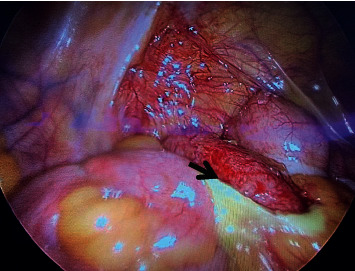
Intraoperative findings showing acutely inflamed appendix with fibrinous exudate.
3. Discussion
The most commonly identified cause of acute appendicitis is the luminal obstruction leading to inflammation and complications of the appendix [2]. One of the earliest well-documented reports that linked blunt abdominal trauma (BAT) with traumatic appendicitis (TA) was the Hungarian stunt performer, Harry Houdini, who used to voluntarily hit his abdomen as a show of strength, subsequently developed peritonitis due to perforated appendix and died [3]. Despite the reports on the possible relationship between BAT and appendicitis are limited (Table 1), however, many theories support this relationship [4]. Some speculated that BAT might cause inflammation by the direct impact and appendiceal injury, and others attributed it to the indirect effect, leading to increased intraluminal pressure followed by burst or intraluminal pressure induced mucosal injury resulting in hematoma/edema that will cause luminal narrowing followed by obstruction and inflammation [4].
Looking at the demographic characteristics of patients who develop TA, most of the reported cases (including ours) showed male predominance, similar to nontraumatic appendicitis; however, in former, more male predominance is expected as blunt trauma is more frequent among males [5], mostly seen in pediatric age group in contrast to our case who was an adult (Table 1). A possible explanation underlying pediatric patients' predominance is the smaller abdominal cavity, softer, and less muscular abdominal wall as compared with adults, where the transmission of energy following trauma is more significant leading to greater increase in intra-abdominal pressure, causing increased appendicular luminal pressure and thus appendicitis. Older children may represent the most sensitive age group due to the fact that they are more independent to participate in risky outdoor activities than their younger counterparts [1].
Patients usually present as the classical picture of acute appendicitis with a difference of preceding trauma, developing abdominal pain within 6-48 hours following the severe blunt abdominal injury. This can be associated with other typical symptoms of acute appendicitis including nausea, vomiting, and anorexia (Table 1). Our patient had abdominal pain that started few hours after the BAT, in agreement with most of other reported cases in literature.
As for investigations, similar to that of nontraumatic appendicitis, blood tests usually show raised inflammatory markers and peculiar clinical signs and imaging, specifically CT scan of the abdomen, if required will confirm the diagnosis (Table 1), as our patient showed leukocytosis and had features of acute appendicitis on abdominal CT scan.
Diagnostic criteria for TA were postulated by Shutkin and Wetzler as follows:
Absolute freedom from abdominal symptoms, including pain, nausea, vomiting, and tenderness, before the trauma
Direct trauma must be severe and forcible, involving the abdominal wall and specially in the right half
Indirect trauma must be violent, acute, and unexpected
Symptoms must appear immediately after the trauma
Symptoms must be persistent and progressive, assuming the symptoms and signs of acute appendicitis
The pathologic findings must indicate a suppurative, destructive, or necrotic process [3]
Our patient fulfilled all the mentioned criteria, so we regarded it as TA.
As for the management, TA does not differ than nontraumatic appendicitis, with mainstay of treatment being surgical appendectomy (Table 1).
In terms of postoperative recovery, we noticed that patients treated for TA have relatively longer hospital stay than those with nontraumatic cause (Table 1). This might be because of the accompanied injuries; in fact, some of these patients presented with polytrauma, and TA was just a part of their multisystem involvement.
4. Conclusions
Blunt abdominal trauma caused by a camel kick to the abdomen requires a close observation of the patients. A camel kick may increase intra-abdominal pressure and cause indirect injury to internal organs including the appendix. Therefore, abdominal pain in these patients should not be regarded as being caused solely by abdominal wall contusion, and acute appendicitis should be considered in the differential diagnosis in any patient with abdominal pain following blunt abdominal trauma.
Data Availability
The data used to support the findings of this study are included in the article.
Ethical Approval
As all the information was given retrospectively from the chart review and the patient was deidentified, this case report was exempted and waiver of consent was obtained and approved by medical research center, Hamad Medical Corporation, reference number (MRC-04-20-811).
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available on request.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
AT contributed to the study concept, data collection, interpretation, and writing the paper; OA participated in the study concept and writing the paper; ZH, SA, MA, and MS contributed to the data interpretation and writing the paper; SMA supervised all the steps and finalized and edited the final manuscript.
References
- 1.Toumi Z., Chan A., Hadfield M. B., Hulton N. R. Systematic review of blunt abdominal trauma as a cause of acute appendicitis. The Annals of The Royal College of Surgeons of England. 2010;92(6):477–482. doi: 10.1308/003588410X12664192075936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zvizdic Z., Pasic-Sefic I., Vranic S. Acute perforated appendicitis after blunt abdominal trauma: a report from a 7-year-old. The American Journal of Emergency Medicine. 2020;38:408.e1–408.e2. doi: 10.1016/j.ajem.2019.158447. [DOI] [PubMed] [Google Scholar]
- 3.Torres G. J., Monkhouse S. Trauma induced appendicitis … a real entity. Emergency Medicine Journal. 2005;3:124–125. doi: 10.1136/emj.2004.018895. [DOI] [Google Scholar]
- 4.Ahmed S. T., Ranjan R., Saha S. B., Singh B. Traumatic appendicitis misdiagnosed as a case of haemoperitoneum. Case Reports. 2014;2014(apr23 1):p. bcr2013202082. doi: 10.1136/bcr-2013-202082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin K.-B., Lai K. R., Yang N.-P., et al. Epidemiology and socioeconomic features of appendicitis in Taiwan: a 12-year population-based study. World Journal of Emergency Surgery. 2015;10(1) doi: 10.1186/s13017-015-0036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cobb T. Appendicitis following blunt abdominal trauma. The American Journal of Emergency Medicine. 2017;35(9):1386.e5–1386.e6. doi: 10.1016/j.ajem.2017.06.051. [DOI] [PubMed] [Google Scholar]
- 7.Paschos K. A., Boulas K., Liapis A., Georgiou E., Vrakas X. Traumatic appendicitis in minor blunt abdominal injury. Emergency Medicine Australasia. 2012;24(3):343–346. doi: 10.1111/j.1742-6723.2012.01557.x. [DOI] [PubMed] [Google Scholar]
- 8.Atalla M. A., Carangan M., Rozen W. M. Re: Acute traumatic appendicitis following blunt abdominal trauma. ANZ Journal of Surgery. 2010;80(7-8):572–573. doi: 10.1111/j.1445-2197.2010.05390.x. [DOI] [PubMed] [Google Scholar]
- 9.Etensel B., Yazici M., Gürsoy H., Özkisacik S., Erkuş M. The effect of blunt abdominal trauma on appendix vermiformis. Emergency Medicine Journal. 2005;22(12):874–877. doi: 10.1136/emj.2004.018895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Houry D., Colwell C. Abdominal pain in a child after blunt abdominal trauma: an unusual injury1. The Journal of Emergency Medicine. 2001;21(3):239–241. doi: 10.1016/S0736-4679(01)00386-9. [DOI] [PubMed] [Google Scholar]
- 11.Serour F., Efrati Y., Klin B., Shikar S., Weinberg M., Vinograd I. Acute appendicitis following abdominal trauma. Archives of Surgery. 1996;131(7):785–786. doi: 10.1001/archsurg.1996.01430190107026. [DOI] [PubMed] [Google Scholar]
- 12.Ciftci A. O., Tanyel F. C., Büyükpamukçu N., Hiçsönmez A. Appendicitis after blunt abdominal trauma: cause or coincidence? European Journal of Pediatric Surgery. 1996;6(6):350–353. doi: 10.1055/s-2008-1071013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included in the article.


