Abstract
The case of a 56-year-old woman with a fibroid uterus who developed utero-cutaneous fistula is presented. The woman was para 0, had an unremarkable medical history, and had no prior diagnosis of a gynecologic pathology, no operative interventions involving the uterine wall or any other risk factor for fistula. Abdominal examination revealed an abdominal mass with overlying deep, purulent ulceration. 18F-FDG PET/CT scan was consistent with uterine leiomyoma, but a differential diagnosis of sarcoma was considered due to the presence of the fistula, patchy increased FDG uptake of the tumor and several mildly enlarged lymph nodes bilaterally in the inguinal and iliac region. Hysterectomy with bilateral salpingo-oophorectomy was performed. Histological diagnosis was of leiomyoma with focal bizarre atypia, degenerative and metaplastic changes and utero-cutaneous fistula. To the best of our knowledge, this is the first case report describing a benign leiomyoma forming a fistula between the uterus and abdominal surface.
Keywords: Leiomyoma, Utero-cutaneous fistula, Case report
Abbreviations: UAE, uterine artery embolization; FDG, fluorodeoxyglucose
Highlights
-
•
Utero-cutaneous fistula is a rare condition.
-
•
We report a case of a 56-year-old woman with benign leiomyoma with a utero-cutaneous fistula.
-
•
Degenerative leiomyoma can mimic malignancy in medical imaging.
-
•
A multidisciplinary team approach is recommended in such unusual cases.
1. Introduction
The most common types of urogenital fistulas are vesico-vaginal and utero-vaginal fistulas. These are almost exclusively related to a difficult childbirth, to operative vaginal delivery, to cesarean section, to gynecologic surgery or to pelvic irradiation [[1], [2], [3], [4], [5], [6]].
In rare cases, development of vesico-vaginal [7], utero-vaginal [8,9], utero-enteric [[10], [11], [12]] and trans-uterine [13] fistulas have been reported in relation with uterine leiomyomas. In all of those cases, fistula formation followed uterine artery embolization (UAE), which is a treatment option for uterine leiomyomas in women who are not candidates for surgery, do not wish undergo a surgical procedure or wish to preserve fertility [[14], [15], [16]].
Utero-cutaneous fistula is a rare condition with only a few reported cases, almost exclusively following surgical intervention such as cesarean delivery [17] or treatment for miscarriage [18]. Based on our literature search, there are no previous reports of the spontaneous development of utero-cutaneous fistula in relation to a benign uterine leiomyoma.
We present a unique case of utero-cutaneous fistula development without the presence of any known risk factors and demonstrate how this benign condition can mimic malignancy on clinical imaging.
2. Case Presentation
A 56-year-old woman, gravida 1 para 0, was referred to the regional department of gynecology and obstetrics from a local diagnostic center, where the patient had been referred due to fatigue, anemia and a recent exuding wound on the right side of the abdomen. The patient had no urinary or gastrointestinal complaints, no symptoms of pelvic pressure and no changes in body weight. During the previous 6 months, the patient had experienced amenorrhea, with prior regular menstruation. She had no previous history of any gynecological disease and other than having undergone one elective abortion approximately 30 years earlier, she had no history of surgical interventions.
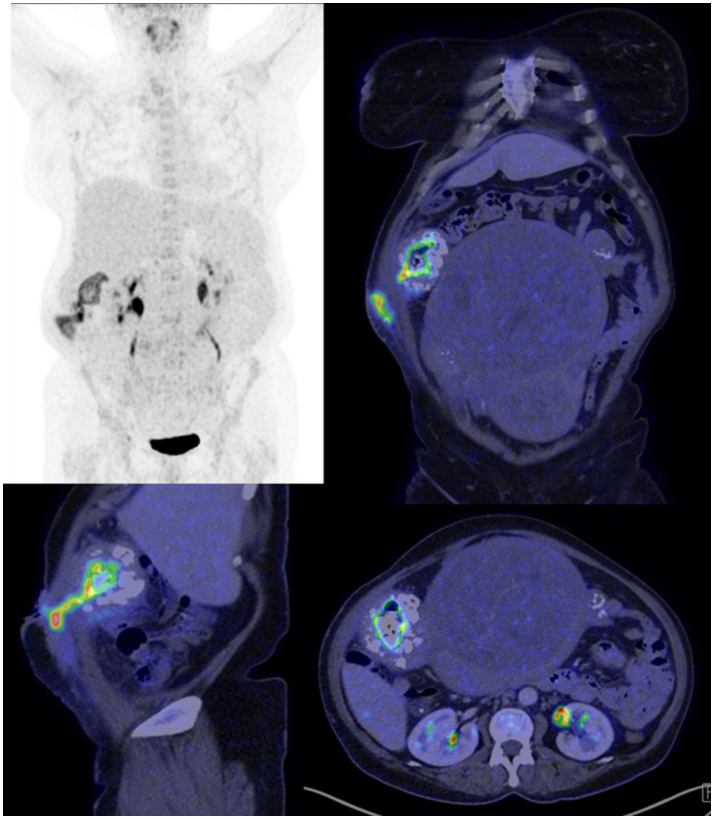
Abdominal examination revealed a large, centrally located firm mass on the right side of the abdomen with deep, foul-smelling and purulent ulceration, raising suspicion of fistula development. A full blood count showed a normal white cell count of 7.9 × 10 g/l, but slightly elevated CRP of 41 mg/l. The patient was mildly anemic, with a hemoglobin level of 6.1 mmol/l with microcytosis. Blood tests for cancer antigen 125, human chorionic gonadotropin and alfa-1-fetoprotein showed normal values. The patient underwent a transvaginal, transabdominal sonogram and 18F-FDG PET/CT scan that visualized a large heterogenic tumor (15 × 25 × 27 cm) with several large calcifications, originating from the uterus. On the right side, the part of the tumor that was adhering to the anterior abdominal wall in the area corresponding to skin ulceration contained calcifications, air and liquid, and intense fluorodeoxyglucose (FDG) uptake, corresponding to the fistulation. The remaining part of the tumor showed faint FDG uptake (Fig. 1).
Fig. 1.
PET and CT scans.
FDG-PET and CT scans visualizing a tumor with adherence to the abdominal wall and intense FDG uptake corresponding fistulation and the inflamed part of the tumor. The remaining part of the tumor showed faint FDG uptake, almost equal to the background.
Findings were consistent with uterine leiomyoma, but a differential diagnosis of sarcoma was considered due to the fistula, patchy increased FDG uptake of the tumor and several mildly enlarged lymph nodes bilaterally in the inguinal and iliac region.
A laparotomy was undertaken via a midline incision. A large fibroid uterus was identified, with marked thickening and inflammation of the surrounding tissues and adhesions to small bowel and omentum. On the right abdominal wall, a fistula with connection to the skin surface was identified. No ascites or peritoneal carcinomatosis were found. Hysterectomy with bilateral salpingo-oophorectomy, debridement of the necrotic tissue and adhesiolysis was performed. No bowel lesions or fistula development between uterus and bowel were identified. No complications occurred during surgery and patient was discharged from the hospital within 48 h. The fistula was left open from the skin side and cleaned regularly. It healed completely within 4 weeks. The patient made an uneventful post-operative recovery and had no sequelae of the treatment or any other complaints at the 4-week post-treatment follow-up.
Examination of the resected specimen revealed a large uterus measuring 30 × 26 × 15 cm and weighing 4800 g, with marked deformation caused by several well demarcated, firm and white-to-grayish intramural tumors (Fig. 2). A calcified subserous lesion measuring 10 × 8 × 8 cm was located at the right fundus. The uterine serosa was intact, except from a defect measuring 5 × 5 cm, on the surface of the calcified lesion that showed signs of ulceration and had attached fatty tissue. This was most likely the site of adhesion to the abdominal wall. After decalcification in formic acid, the calcified lesion was tangentially sectioned. This revealed an irregular, centrally located cavity, with communication to the outer surface.
Fig. 2.
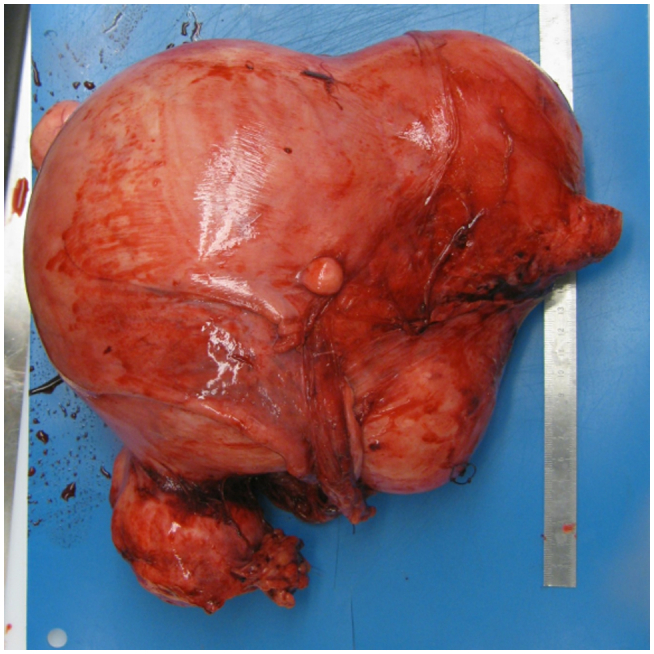
Macroscopy of the specimen.
An enlarged, deformed uterus with several intramural and subserous tumors.
The subserous calcified lesion and the intramural tumors were extensively sampled, with a total sampling of 100 paraffin-embedded tissue blocks.
Microscopic examination of the intramural tumors showed a varied appearance, dominated by fascicles of uniform spindle cells, with abundant eosinophilic cytoplasm, lacking both nuclear atypia and mitotic activity, and areas of degeneration, including hyaline change, myxoid degeneration and focal osseous metaplasia with the presence of osteoid matrix and osteoblasts (Fig. 3A). Focally, an area measuring approximately 4 mm2 showed tumor cells with more size- and shape-varying nuclei (Fig. 3B). The mitotic count was low, and no tumor cell necrosis was observed. Immunohistochemistry showed weak focal immunoreactivity for P53 and P16. Ki-67 proliferation index was low.
Fig. 3.
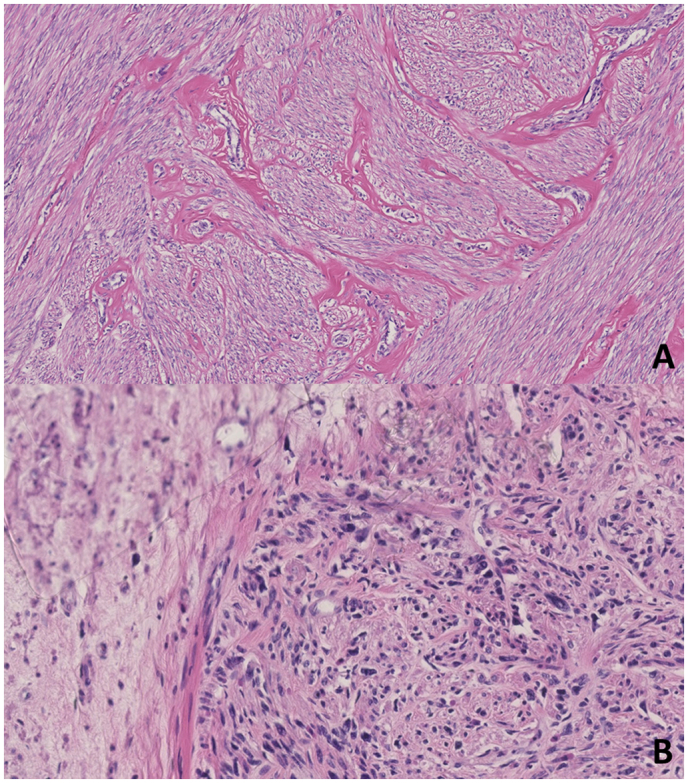
Microscopy of the specimen.
A: Osseous metaplasia with the presence of osteoid matrix and osteoblasts.
B: Focal bizarre atypia.
Histology from the calcified lesion with communication to the skin showed degenerative changes, with extensive osseous metaplasia and central pseudocyst formation, surrounded by granulation tissue with abundant vessels and acute and chronic inflammation. The final diagnosis was leiomyoma with focal bizarre atypia, and extensive degenerative and metaplastic changes with a skin fistula.
3. Discussion
To the best of our knowledge, this is the first case report describing a benign leiomyoma forming a fistula between the uterus and the abdominal surface.
Although little is known about the etiology of urogenital fistula formation, it appears to be multifactorial. According to the literature, one risk factor for fistula formation is surgery, probably by disturbing the integrity of an organ wall and promoting adhesions [17,18]. The other known risk factor is prior UAE, which causes degenerative changes in leiomyomas and an inflammatory response in surrounding tissue [[14], [15], [16]].
The patient had no history of previous abdominal surgery or any other risk factors for adhesion formation. Therefore, our assumption is that the adhesions and the fistula resulted from degenerative ischemic changes in the large leiomyoma. The ischemic changes in a large leiomyoma with inadequate circulation are likely to be similar to those caused by UAE.
UAE causes ischemia and necrosis in uterine leiomyomas, which explains the formation of periuterine adhesions in almost 60% of patients following UAE [[14], [15], [16]]. In a few cases, the presence of adhesions and inflammation causes breakdown of the wall of neighboring structures at the point of contact, which can lead to the development of a fistula.
The spectrum of diagnoses of uterine mesenchymal tumors is continuously evolving [19]. The differential diagnosis of benign uterine leiomyoma includes mesenchymal tumors such as endometrial stromal sarcoma with smooth muscle metaplasia, leiomyosarcoma or smooth muscle tumors of uncertain malignant potential. Thus, a multidisciplinary team approach is required.
Acknowledgments
Contributors
Kristi Bøgh Anderson did the literature search and the following analysis, and participated in writing the paper.
Erik Søgaard-Andersen participated in the examination and treatment of the patient and in writing the paper and obtained the patient's informed consent for publishing the case report.
Ramune Aleksyniene analyzed the radiological images and participated in writing the paper.
Anna Poulsgaard Frandsen participated in the histological examination of the surgery specimen and the histological diagnosis and in writing the paper.
All authors approved the final version of the paper.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
This project did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Patient Consent
Complete informed consent was obtained from the patient for the publication of this study and accompanying images.
Provenance and Peer Review
This case report was peer reviewed.
Contributor Information
Kristi Bøgh Anderson, Email: ander.krist@gmail.com.
Erik Søgaard-Andersen, Email: esa@rn.dk.
Ramune Aleksyniene, Email: raa@rn.dk.
Anna Poulsgaard Frandsen, Email: apf@rn.dk.
References
- 1.Porcaro A.B. Vesicouterine fistulas following cesarean section: report on a case, review and update of the literature. Int. Urol. Nephrol. 2002;34(3):335–344. doi: 10.1023/a:1024443822378. [DOI] [PubMed] [Google Scholar]
- 2.Osman S.A., Al-Badr A.H., Malabarey O.T., Dawood A.M., AlMosaieed B.N., Rizk D.E.E. Causes and management of urogenital fistulas. A retrospective cohort study from a tertiary referral center in Saudi Arabia. Saudi Med. J. Apr. 2018;39(4):373–378. doi: 10.15537/smj.2018.4.21515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reisenauer C. Vesicovaginal fistulas: a gynecological experience in 41 cases at a German pelvic floor center. Arch. Gynecol. Obstet. Aug. 2015;292(2):245–253. doi: 10.1007/s00404-015-3760-8. [DOI] [PubMed] [Google Scholar]
- 4.Prato B. Correlation of recurrence rates and times with posttreatment human papillomavirus status in patients treated with loop electrosurgical excision procedure conization for cervical squamous intraepithelial lesions. Int. J. Gynecol. Cancer. 2008;18(1):90–94. doi: 10.1111/j.1525-1438.2007.00965.x. [DOI] [PubMed] [Google Scholar]
- 5.Deitel M., T. B. To Major intestinal complications of radiotherapy. Arch. Surg. Dec. 1987;122(12):1421. doi: 10.1001/archsurg.1987.01400240069012. [DOI] [PubMed] [Google Scholar]
- 6.Lobo N., Kulkarni M., Hughes S., Nair R., Khan M.S., Thurairaja R. Urologic complications following pelvic radiotherapy. Urology. Dec. 2018;122:1–9. doi: 10.1016/j.urology.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Vural B., Ozkan S., Ciftçi E., Bodur H., Yücesoy I. Spontaneous vaginal expulsion of an infected necrotic cervical fibroid through a cervical fistula after uterine artery embolization: a case report. J. Reprod. Med. Jun. 2007;52(6):563–566. [PubMed] [Google Scholar]
- 8.Price N., Golding S., Slack R.A., Jackson S.R. Delayed presentation of vesicouterine fistula 12 months after uterine artery embolisation for uterine fibroids. J. Obstet. Gynaecol. Feb. 2007;27(2):205–207. doi: 10.1080/01443610601157273. [DOI] [PubMed] [Google Scholar]
- 9.Javali T., Kasaraneni D., Banale K., Babu P.S.M.L., Nagaraj H.K. Vesicouterine fistula and concomitant ureteric necrosis following uterine artery embolization for fibroid uterus. Int. Urogynecol. J. Dec. 2015;26(12):1877–1878. doi: 10.1007/s00192-015-2764-z. [DOI] [PubMed] [Google Scholar]
- 10.Dewdney S.B., Mani N.B., Zuckerman D.A., Thaker P.H. Uteroenteric fistula after uterine artery embolization. Obstet. Gynecol. Aug. 2011;118(2 Pt 2):434–436. doi: 10.1097/AOG.0b013e31821082a3. [DOI] [PubMed] [Google Scholar]
- 11.Pandey B., Sunanda G.V., Crowe P. Enterouterine fistula: a rare and unusual complication of uterine artery embolisation. J. Obstet. Gynaecol. Jan. 2012;32(1):32–33. doi: 10.3109/01443615.2011.615417. [DOI] [PubMed] [Google Scholar]
- 12.Gutierrez L.B., Bansal A.K., Hovsepian D.M. Uteroenteric fistula resulting from fibroid expulsion after uterine fibroid embolization: case report and review of the literature. Cardiovasc. Intervent. Radiol. Oct. 2012;35(5):1231–1236. doi: 10.1007/s00270-011-0318-4. [DOI] [PubMed] [Google Scholar]
- 13.Donnez O., Jadoul P., Squifflet J., Donnez J. Unusual complication after uterine artery embolization and laparoscopic myomectomy in a woman wishing to preserve future fertility. Fertil. Steril. 2007;90(5):e5–e9. doi: 10.1016/j.fertnstert.2008.05.091. Nov. 2008. [DOI] [PubMed] [Google Scholar]
- 14.Ravina J.H. Arterial embolisation to treat uterine myomata. Lancet. Sep. 1995;346(8976):671–672. doi: 10.1016/S0140-6736(95)92282-2. [DOI] [PubMed] [Google Scholar]
- 15.Payne J.F., Haney A.F. Serious complications of uterine artery embolization for conservative treatment of fibroids. Fertil. Steril. Jan. 2003;79(1):128–131. doi: 10.1016/s0015-0282(02)04398-4. [DOI] [PubMed] [Google Scholar]
- 16.Huang J.Y.J., Kafy S., Dugas A., Valenti D., Tulandi T. Failure of uterine fibroid embolization. Fertil. Steril. Jan. 2006;85(1):30–35. doi: 10.1016/j.fertnstert.2005.03.091. [DOI] [PubMed] [Google Scholar]
- 17.Lim P.S., Shafiee M.N., Ahmad S., Hashim Omar M. Utero-cutaneous fistula after caesarean section secondary to red degeneration of intramural fibroid. Sex. Reprod. Healthc. Jun. 2012;3(2):95–96. doi: 10.1016/j.srhc.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Sönmezer M., Sahincioğlu O., Cetinkaya E., Yazici F. Uterocutaneous fistula after surgical treatment of an incomplete abortion: methylene blue test to verify the diagnosis. Arch. Gynecol. Obstet. Feb. 2009;279(2):225–227. doi: 10.1007/s00404-008-0683-7. [DOI] [PubMed] [Google Scholar]
- 19.Ganesan R. Uterine smooth muscle tumour of uncertain malignant potential (STUMP): where are we now? Case Rep. Women’s Health. 30 Jan. 2020;26 doi: 10.1016/j.crwh.2020.e00176. e00176. [DOI] [PMC free article] [PubMed] [Google Scholar]