Highlights
-
•
SEEG is feasible with little to no skull to anchor a bolt.
-
•
To the best of our knowledge, this is the first report describing SEEG electrode placement with no skull bone.
Keywords: Recurrent seizures, SEEG, Anchor bolts, Limited or absent bone
Abstract
Stereo electroencephalogram (SEEG) electrode placement with cranially fixed guide bolts is recognized as one of the most accurate and safest implantation strategies to sample deep and buried cortex during certain clinical scenarios involving epilepsy surgery. Bone thickness of less than 2 mm is a relative contraindication to SEEG. Here, we describe a case drug-resistant focal epilepsy where prior craniotomies, infections and radiation therapy yielded limited skull bone requiring invasive EEG monitoring. Due to the inability to use bolts over areas with limited skull bone, we successfully utilized a combination of the standard and a modified SEEG techniques for implantation and stabilization of intracranial electrodes without complications. This strategy enabled optimal intracranial EEG monitoring and surgical management of the patient’s drug-resistant focal seizures.
Introduction
Bone thickness of less than 2 mm is a relative contraindication to SEEG [1]. However, what happens when there is little to no bone over sites that are crucial to the epileptic network?
Case presentation
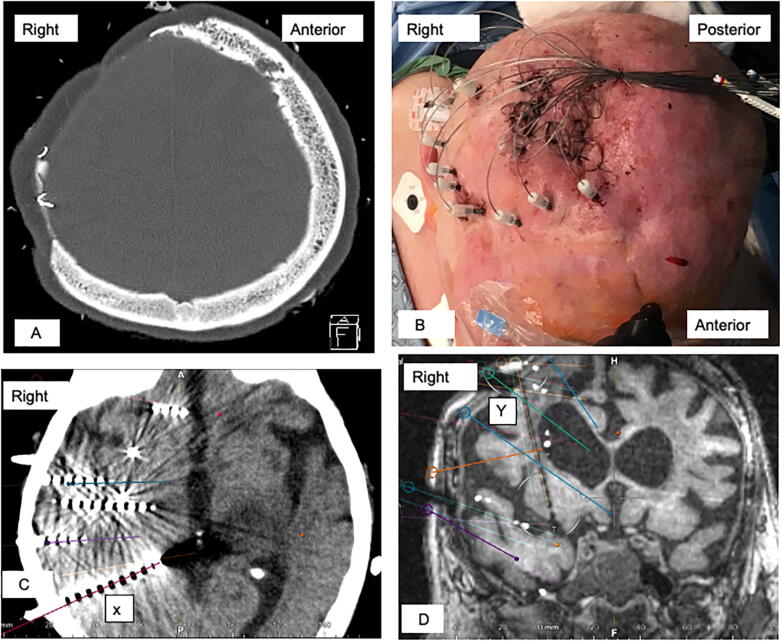
A 72-year-old woman with a 30-year history of epilepsy and a right frontal glioma status post multiple craniotomies, radiation treatment, cranial infections, and reconstruction. As a result, she had incomplete bone coverage of her original craniotomy defect. She had done well with no tumor recurrence on serial brain MRIs or seizures on two antiseizure medications (ASMs) before being admitted following a convulsive seizure that progressed to non-convulsive status epilepticus consisting of left upper extremity movements, aphasia, with impaired awareness. Her EEG showed electroclinical seizures in the right frontocentral regions. A thorough evaluation, showed no toxic, metabolic, infectious, residual or recurrent tumor etiologies, although atrophy with encephalomalacia were seen on brain MRI. Multiple ASMs were used to control her seizures resulting in significant sedation, changes of which resulted in seizure recurrence. Epilepsy surgery with SEEG was recommended with a challenging implantation due to thin or absent bone over regions of interest (Fig. 1A).
Fig. 1.
(A) CT head axial bone window, limited bone over the right frontal regions. (B) OR SEEG placement-lateral view, (C) Post-operative CT head with axial images merged with preplanned trajectories, showing X bolted SEEG leads. (D) Post-opearative merged CT/MRI and pre planning MRI with a coronal view showing Y cannulated sutured SEEG lead (anterior insular).
Methods
Based on the seizure hypothesis, pre-planned SEEG electrode trajectories on the patient's brain MRI using a frameless stereotactic navigation system with intraoperative CT were used. SEEG electrode placement varied depending on bone thickness. For trajectories that traversed areas with sufficient cranial bone, SEEG electrodes placement used a previously described technique [2], [3].
For trajectories that traversed areas with little to no cranial bone, a modified previously described technique was used [2]. A drill was used to penetrate the skin and soft tissue down to the dura, which was punctured with a K-wire. The navigation system was then used to calculate the distance from the trajectory arm to the target, which ranged from 36.3 mm to 72.3 mm. This distance was marked on a slotted cannula and SEEG lead. The slotted cannula was passed to the target. The SEEG lead was passed to the target, at which point the slotted cannula and lead stylet were removed. Since there were no bolts for these leads, they were secured to the scalp using a drain stitch with 4-0 Nurolon. The bundle of electrodes was secured to the scalp with 2-0 Nurolon suture (Fig. 1B) and a tight head wrap applied.
All electrodes were connected to the EEG monitoring system with appropriate recordings. Pre-planned and performed trajectories were compared by visual analysis of postoperative head CT/MRI (Fig. 1C and D).
Results
Eleven SEEG electrodes were placed with bolts using the standard technique, while five additional electrodes were placed with a modified method using cannulas and sutures, with either orthogonal and oblique trajectories. Electrodes placed the with the standard technique had an intracerebral distance ranging from 25.6 mm to 57.1 mm, while those with a modified version ranged from 23.7 mm to 59.6 mm.
All electrodes were within the region of interest, including one lead placed by a modified technique in an orthogonal trajectory length with an intracerebral length of 55.4 mm. Repositioning of electrodes was not required. There was no hemorrhage or cerebral spinal fluid (CSF) leak.
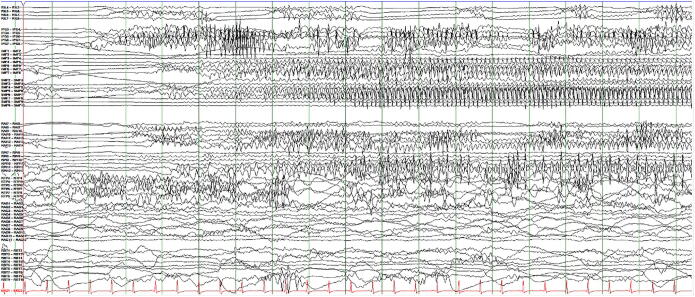
All electrodes remained secured, recording optimally over seven days. Seizures were recorded (Fig. 2), allowing for resection of seizure onset zones whose histology showed focal cortical dysplasia without tumor. After resection, reduction of ASM without ictal recurrence was achieved
Fig. 2.
A 18-second epoch of intracranial EEG demonstrating the early seizure network involving regions sampled by SEEG electrodes bolted (rows 7,2) and cannulated/sutured (rows 3,4,6) LF 0.1 Hz, HF 500 Hz, sensitivity of 50 microvolts.
Discussion
Stereotactic depth electrode placement is a technique used for a variety of neurosurgical procedures. Electrodes can be placed for permanent or temporary use. Permanent lead placement is usually performed when implanting a deep brain stimulation or responsive neurostimulation system. Since these systems are entirely internalized, the leads are typically internally anchored using burr hole covers or other internal anchoring devices. By contrast, temporary depth electrodes are typically used for electrographic monitoring procedures like SEEG and Subdural grids with depth electrodes. Temporary depth electrodes are anchored in such a way that the extracerebral end of the lead is connected to an external monitoring system.
SEEG electrode implantation is aimed at sampling hypothesized epileptic network that might include an anatomical lesion (if present), likely structure(s) and pathway(s) of seizure propagation [3]. SEEG electrodes are predominantly placed with cranial-based guide and anchor bolts that protrude through the scalp [4], [5]. A minimum bone thickness of 2 mm is required to anchor the bolts [1], posing a challenge in cases that might have limited bone over regions of interest.
In a cadaveric study, SEEG implantation with guiding bolts and external stylets was found to be superior to implantation without guiding bolts and external stylets [2]. Generally, the most common complication of SEEG is hemorrhage seen in 1.0%, 95% CI 0.6–1.4% [3], while, the rate of malpositioning which greatly impacts the sucess of the evaluation is 0.6% [3] A significant concern with the “non-bolted” SEEG technique is implantation errors, resulting in displacement especially with orthogonal approach and trajectories greater than 50 mm (from entry to target points) as well as electrode dislodgement. In a hybrid model of intracranial EEG using subdural grid with depth electrodes, the later are generally placed without guide/anchor bolts, although external stylets are used, and electrodes anchored with sutures. Leveraging this information, we placed some SEEG electrodes using the later technique in the areas anchor bolts could not be placed. Using pre-implantation MRI and post operative CT-MRI evalautions, electrodes were generally within the intended regions of analysis. EEG was comparable for “bolted” and “non-bolted” SEEG electrodes allowing for definitive surgical treatment. We did not encounter any complications including CSF leak reported in 12.1% of craniotomies with thin skulls [6], [7]. The risk of electrode dislodgement post-operative was decreased by securing the electrodes with sutures as well as placing a secure head wrap. Electrodes remained secured over the course of the recording, and while no brain imaging was obtained just prior to electrode removal, no dislodgement was visually seen.
Conclusions
SEEG electrode placement with cranially fixed guide bolts in certain clinical contexts, is recognized as the optimal and safest implantation strategy. To the authors' knowledge, this is the first reported case utilizing cranially implanted SEEG electrodes without fixed guide bolts in a living patient. This case might suggest a safe and effective alternative SEEG implantation strategy, especially when bone limitations exist; however, future follow up studies may help clarify these findings and optimize the technique.
Data Statement
The data that supports the findings of this manuscript is available from the corresponding author upon reasonable request due to privacy and ethical restrictions.
Ethical statement
This submission was reviewed by the Office of Human Research Ethics, which has determined that this submission does not constitute human subjects research as defined under federal regulations [45 CFR 46.102 (e or l) and 21 CFR 56.102(c)(e)(l)] and does not require IRB approval.
Funding
The authors received no financial support for the research, authorship, and publication of this article
Conflicts of interest
The authors have no affiliation with or involvement with any organization or entity with any financial or non-financial interest in the subject matter or material discussed in this manuscript.
References
- 1.Minotti L., Montavont A., Scholly J., Tyvaert L., Taussig D. Indications and limits of stereoelectroencephalography (SEEG) Neurophysiol Clin. 2018 doi: 10.1016/j.neucli.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Jones J.C., Alomar S., McGovern R.A., Firl D., Fitzgerald Z., Gale J. Techniques for placement of stereotactic electroencephalographic depth electrodes: Comparison of implantation and tracking accuracies in a cadaveric human study. Epilepsia. 2018 doi: 10.1111/epi.14538. [DOI] [PubMed] [Google Scholar]
- 3.Mullin J.P., Shriver M., Alomar S., Najm I., Bulacio J., Chauvel P. Is SEEG safe? A systematic review and meta-analysis of stereo-electroencephalography-related complications. Epilepsia. 2016 doi: 10.1111/epi.13298. [DOI] [PubMed] [Google Scholar]
- 4.Isnard J., Taussig D., Bartolomei F., Bourdillon P., Catenoix H., Chassoux F. French guidelines on stereoelectroencephalography (SEEG) Neurophysiol Clin. 2018 doi: 10.1016/j.neucli.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Martinez J., Mullin J., Vadera S., Bulacio J., Hughes G., Jones S. Stereotactic placement of depth electrodes in medically intractable epilepsy: Technical note. J Neurosurg. 2014 doi: 10.3171/2013.11.JNS13635. [DOI] [PubMed] [Google Scholar]
- 6.Arya R., Mangano F.T., Horn P.S., Holland K.D., Rose D.F., Glauser T.A. Adverse events related to extraoperative invasive EEG monitoring with subdural grid electrodes: A systematic review and meta-analysis. Epilepsia. 2013 doi: 10.1111/epi.12073. [DOI] [PubMed] [Google Scholar]
- 7.Yang P.F., Zhang H.J., Pei J.S., Tian J., Lin Q., Mei Z. Intracranial electroencephalography with subdural and/or depth electrodes in children with epilepsy: Techniques, complications, and outcomes. Epilepsy Res. 2014 doi: 10.1016/j.eplepsyres.2014.08.011. [DOI] [PubMed] [Google Scholar]