Abstract
Nontyphoidal salmonella (NTS) infection has a high mortality rate. Bowel resections affect gut microbiota and immune function, and the association between bowel resection and NTS infection in human beings has not been addressed. We conducted a nationwide propensity score (PS)-matched cohort study to clarify this association. Data from the Longitudinal Health Insurance Database of Taiwan were used to establish a case-cohort with bowel resections from 2000 to 2013. Informed consent was waived by the Institutional Review Board of China Medical University Hospital (CMUH104-REC2-115) because all personal identifying information used had been de-identified. Each case was matched with one control without any bowel resection according to age, gender, index date, and propensity score (PS). Cumulative incidences of and hazard ratios (HRs) for NTS infection development were analyzed. The incidence of NTS infection was greater in patients with a bowel resection than in the control group (2.97 vs. 1.92 per 10,000 person-years), with an adjusted hazard ratio (aHR) of 1.64 (95% CI = 1.08–2.48). The incidence of NTS infection increased significantly for cases with small bowel resections and right hemicolectomies. Age (31–40 and > 50 years), hypertension, chronic kidney disease, chronic obstructive pulmonary disease, and autoimmune diseases were significant risk factors of NTS infection. Stratification analysis revealed that patients without comorbidities were prone to NTS infection after bowel resections. The increased risk of developing NTS infection could be related to the bowel resection. Specific age groups and comorbidities also contribute to increased risk of NTS infection.
Subject terms: Microbiology, Gastroenterology
Introduction
Nontyphoidal salmonella (NTS) infection is an important issue. The incidence of invasive NTS was 7.5 cases per 100,000 people worldwide in 20171. The main risk factors of hosts include extreme age, immunocompromised status and immunomodulator use2,3. NTS bacteremia usually results in higher rate of mortality in patients with underlying diseases4.
Our gut mucosal immune system can keep pathobionts in check, restrict microbial overgrowth, and react to invading microorganisms that breach the intestinal chemical and physical barriers5. Several bacteria have some controlling effects on S. enterica, such as Bifidobacterium thermophilum and Lactobacillus casei6,7. Argüello et al. discovered that manipulating certain taxa of microbiota could decrease salmonella infection for pigs8.
In human beings, bowel resection strongly influences gut microbiota and intestinal healing9. In the small intestine, the main reported bacterial species included Bacilli (Firmicutes), Streptococcaceae (Firmicutes), Actinobacteria, Clostridium and Bacteroides5. Phyla Bacteroidetes and Firmicutes can dominate the mucosa-associated bacteria from the distal small intestine and the colon5. Specialized bacteria (e.g., Clostridium, Lactobacillus, or Enterococcus) able to adhere to mucus (as a nutrient source) and different species in feces (belonging to Bacteroides, Bifidobacterium, Streptococcus, Enterobacteriaceae, Enterococcus, Clostridium, Lactobacillus, and Ruminococcus) were identified5. Kunz et al. indicated that gastrectomy could lead to S. enteritis. This might result from relative or absolute achlorhydria, decreased hydrogen ion concentration, rapid emptying of food into the small intestine and the colon and altered bacterial flora10.
However, currently the association between bowel resection (except the stomach) and NTS infection was still not clarified. The present nationwide propensity score (PS)-matched cohort study was carried out in Taiwan to evaluate the risk of NTS infection after bowel resection.
Materials and methods
Data source and ethics statement
We extracted the claims-based data from the Longitudinal Health Insurance Database 2000 (LHID), which is a dataset included in Taiwan’s National Health Insurance Research Database (NHIRD). The NHIRD contains patients’ characteristics, medical information, total expenditure, and diagnoses coded in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) format. Taiwan’s National Health Insurance (NHI) programme is administered by the government and covers more than 99% of the 23.4 million population of Taiwan11. Data for the LHID were collected by systematically and randomly sampling from the NHIRD; this database includes the data of one million individuals. Information on demographic data, inpatient and outpatient cares, date of clinic visit or hospitalization, and prescriptions were available in the database for the period from 1997 to 2013. The NHRI reported no significant differences between the patients in the LHID and those in the original NHIRD12. The studies involving human participants were reviewed and approved by the Institutional Review Board of China Medical University Hospital (approval number CMUH104-REC2-115). Written informed consent for participation was not required for this study in accordance with national legislation and institutional requirements. Our research adhered strictly in accordance with relevant guidelines/regulations.
Study subjects and design
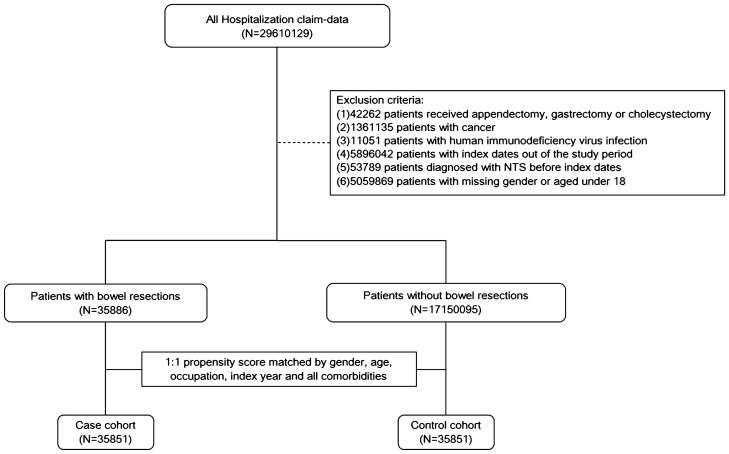
A bowel resection-related case group was established, including patients aged 18 years and over who had received a bowel resection (small bowel, large bowel, or both) from 2000 to 2013. We included the cases identified by the procedure codes of 45.6 (small bowel resection), 45.73 (right hemicolectomy), 45.74 (transverse colon resection), 45.75 (left hemicolectomy), 45.76 (sigmoidectomy), 45.8 (total colectomy), or 45.9 (bowel anastomosis). We defined the index date as the operation date. We excluded patients with appendectomy/gastrectomy/cholecystectomy, any kind of cancer, human immunodeficiency virus infection, index dates out of the study period, diagnosis of NTS, or missing gender or aged under 18 before index dates (Fig. 1). The outcome was the development of NTS (ICD-9-CM codes: 003.xx) after the index date.
Figure 1.
Study flowchart.
Propensity score matching and covariates
A matched control was assigned to each case (Fig. 1). We used the PS-matching method to account for baseline differences13. The observed covariates in the logistic regression model to generate the PS were hypertension (ICD9 codes: 401–405), diabetes (ICD9 code: 250), hyperlipidemia (ICD9 codes: 272), coronary artery disease (ICD9 codes: 410–414), cerebrovascular accident (430–438), chronic kidney disease (ICD9 code: 585), chronic obstructive pulmonary disease (COPD, ICD9 codes: 491, 492, 496), chronic liver disease (ICD9 code: 571.4), autoimmune diseases (including systemic lupus erythematosus, ICD9 code: 710.0; ankylosing spondylitis, ICD9 code: 720.0; rheumatoid arthritis, ICD-9-CM code: 714.0; Sjögren's syndrome, ICD-9-CM code: 710.2), psoriasis (ICD9 code: 696), vasculitis (ICD9 code: 446), and inflammatory bowel disease (IBD, including Crohn’s disease, ICD9 codes: 555.x and ulcerative colitis, ICD9 codes: 556.x).
Statistical analysis
Chi-square test was used to determine the differences of baseline characteristics for categorical variables and Student’s t-test was applied to examine continuous variables between case group (bowel resection) and the control group. Standardized mean difference (SMD) was used to assess the difference between the case group and the control group after PS matching; a value of < 0.1 was considered negligible13. Incidence of NTS infection was estimated for both groups by the end of 2013. We used the Kaplan–Meier method to measure fractions free of NTS infection during the follow-up period in the two groups and used the log-rank test to examine the difference. Incidence rates (IRs) of NTS infection, per 10,000 person-years, were calculated for patients with or without bowel resections, gender, age group, occupation, and comorbidities. Cox proportional-hazards regression analysis was used to calculate the case group to the control group hazard ratio (HR) of NTS infection and 95% confidence interval (CI). Adjusted hazard ratio (aHR) was estimated after controlling for covariates. Gender-, age-, occupation-, and comorbidities-stratified analyses of NTS infection with or without bowel resection were conducted. All statistical analyses were performed using SAS software version 9.4 (SAS Institute INC., Carey, NC, USA). A two-tailed p-value below 0.05 was considered as significant.
Sensitivity analysis
According to Wu et al.14, a temporal association between the use of proton pump inhibitors and increased susceptibility to NTS was demonstrated, which would bias our results. Therefore, we performed the sensitivity analysis by excluding peptic ulcer disease patients (ICD9 codes: 531, 532, 533, and 534) who had a high probability of taking proton pump inhibitors and PS matching.
Results
Demographic characteristics of patients
Our study population includes 35,851 cases and 35,851 controls. Table 1 shows that the male ratio and the mean age were 52% and 56.1 years in the case group, and 51% and 55.6 years in the control group, respectively. There was no significant difference in the baseline occupation and comorbidities. The overall median follow-up time was 4.53 years.
Table 1.
Demographic Characteristics of Patients with and without Bowel Resection.
| Variables | Bowel resection | SMD | |||
|---|---|---|---|---|---|
| No (n = 35,851) | Yes (n = 35,851) | ||||
| n | % | n | % | ||
| Gender | 0.01 | ||||
| Female | 17,522 | 49% | 17,300 | 48% | |
| Male | 18,329 | 51% | 18,551 | 52% | |
| Age, year | |||||
| 18–30 | 3418 | 10% | 3229 | 9% | 0.02 |
| 31–40 | 4788 | 13% | 4659 | 13% | 0.01 |
| 41–50 | 6382 | 18% | 6344 | 18% | 0.003 |
| > 50 | 21,263 | 59% | 21,619 | 60% | 0.02 |
| Mean, (SD) | 55.6 | (18.5) | 56.1 | (18.3) | 0.02 |
| Occupation | |||||
| Officer | 16,360 | 46% | 16,721 | 47% | 0.02 |
| Worker | 8198 | 23% | 7964 | 22% | 0.02 |
| Farmer | 685 | 2% | 602 | 2% | 0.02 |
| Fisher | 6215 | 17% | 6275 | 18% | 0.004 |
| Others | 4393 | 12% | 4289 | 12% | 0.01 |
| Comorbidities | |||||
| Hypertension | 10,584 | 30% | 10,266 | 29% | 0.02 |
| Diabetes | 5733 | 16% | 5529 | 15% | 0.02 |
| Hyperlipidemia | 2900 | 8% | 2401 | 7% | 0.05 |
| Coronary artery disease | 4129 | 12% | 3830 | 11% | 0.03 |
| Cerebrovascular accident | 3798 | 11% | 3255 | 9% | 0.05 |
| Chronic kidney disease | 1211 | 3% | 1207 | 3% | 0.001 |
| COPD | 2455 | 7% | 2226 | 6% | 0.03 |
| Chronic liver disease | 1836 | 5% | 1631 | 5% | 0.03 |
| Autoimmune disease | 451 | 1% | 406 | 1% | 0.01 |
| Psoriasis | 87 | 0.24% | 74 | 0.21% | 0.01 |
| Vasculitis | 27 | 0.08% | 14 | 0.04% | 0.02 |
| IBD | 673 | 2% | 772 | 2% | 0.02 |
SD standard deviation, SMD standardized mean difference, COPD chronic obstructive pulmonary disease, IBD Inflammatory bowel disease.
Cumulative incidence and risk of NTS infection
By the end of follow-up, the Kaplan–Meier analysis showed that the NTS infection was significantly more in the bowel resection group than in the control group (p = 0.03) (Fig. 2). The IR of NTS infection was higher in the bowel resection group than in the control group (2.97 vs. 1.92 per 10,000 person-years), with an aHR of 1.64 (95% CI = 1.08–2.48) for the bowel resection group (Table 2). Considering the location of bowel resection, the IR of NTS infection was higher in the small bowel resection group than in the control group (3.66 vs. 1.92 per 10,000 person-years), with an aHR of 1.96 (95% CI = 1.20–3.19) for the small bowel resection group, and higher in the right hemicolectomy group than in the control group (3.32 vs. 1.92 per 10,000 person-years), with an aHR of 1.96 (95% CI = 1.02–3.77) for the right hemicolectomy group. Besides, age (31–40 years, aHR of 4.71, 95% CI = 1.05–21.1; > 50, aHR of 5.25, 95% CI = 1.27–21.8), hypertension (aHR of 1.61, 95% CI = 1.00–2.58), chronic kidney disease (aHR of 2.35, 95% CI = 1.06–5.21), COPD (aHR of 2.18, 95% CI = 1.18–4.02), and autoimmune disease (aHR of 3.83, 95% CI = 1.4–10.47) also increased the risk of NTS infection significantly. Large bowel resection, left hemicolectomy, sigmoidectomy, total colectomy, and bowel anastomosis did not increase the NTS infection risk prominently.
Figure 2.
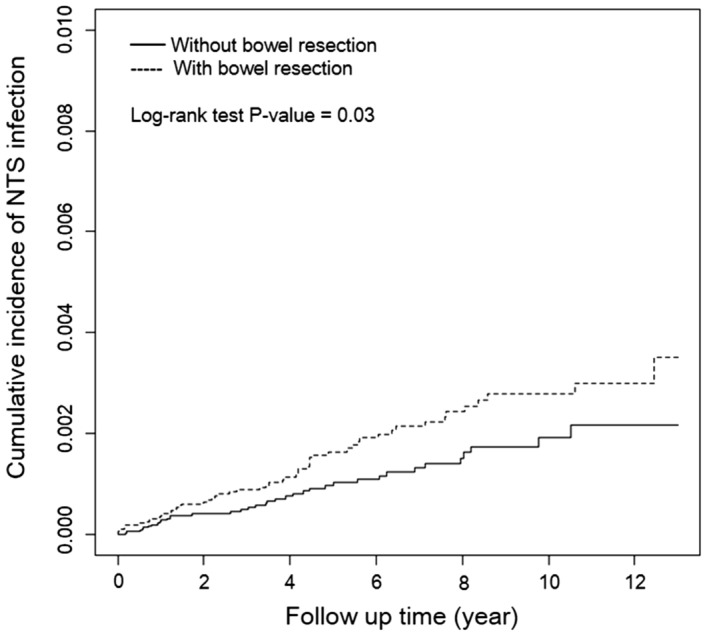
Cumulative incidence curves of nontyphoidal salmonella (NTS) infection among the propensity score–matched Cohort using The Kaplan–Meier method.
Table 2.
Incidence Rate and Hazard Ratio of NTS Infection.
| Variables | NTS infection | cHR | (95% CI) | aHR† | (95% CI) | ||
|---|---|---|---|---|---|---|---|
| n | PY | IR | |||||
| Bowel resection | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 56 | 188,270 | 2.97 | 1.56 | (1.03, 2.37)* | 1.64 | (1.08, 2.48)* |
| Small bowel resection | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 29 | 79,213 | 3.66 | 1.93 | (1.18, 3.14)** | 1.96 | (1.20, 3.19)** |
| Large bowel resection | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 28 | 98,288 | 2.85 | 1.52 | (0.93, 2.48) | 1.59 | (0.97, 2.60) |
| Right hemicolectomy | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 12 | 36,091 | 3.32 | 1.77 | (0.92, 3.39) | 1.96 | (1.02, 3.77)* |
| Transverse colon resection | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | ||
| Yes | 0 | 2847 | 0.00 | 0.00 | |||
| Left hemicolectomy | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 6 | 12,670 | 4.74 | 2.51 | (1.06, 5.95)* | 2.12 | (0.89, 5.04) |
| Sigmoidectomy | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 6 | 16,997 | 3.53 | 1.84 | (0.78, 4.37) | 1.66 | (0.70, 3.96) |
| Total colectomy | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | ||
| Yes | 0 | 3392 | 0.00 | 0.00 | |||
| Bowel anastomosis | |||||||
| No | 37 | 192,902 | 1.92 | 1.00 | – | 1.00 | – |
| Yes | 11 | 57,857 | 1.90 | 1.01 | (0.52, 1.99) | 1.18 | (0.60, 2.33) |
| Gender | |||||||
| Female | 34 | 174,426 | 1.95 | 1.00 | – | ||
| Male | 59 | 206,746 | 2.85 | 1.48 | (0.97, 2.26) | ||
| Age, year | |||||||
| 18–30 | 2 | 43,760 | 0.46 | 1.00 | – | 1.00 | – |
| 31–40 | 12 | 53,443 | 2.25 | 4.86 | (1.09, 21.7)* | 4.71 | (1.05, 21.1)* |
| 41–50 | 6 | 70,720 | 0.85 | 1.83 | (0.37, 9.07) | 1.67 | (0.34, 8.31) |
| > 50 | 73 | 213,249 | 3.42 | 7.36 | (1.81, 30.0)** | 5.25 | (1.27, 21.8)* |
| Occupation | |||||||
| Officer | 38 | 174,857 | 2.17 | 1.00 | – | ||
| Worker | 16 | 88,397 | 1.81 | 0.83 | (0.47, 1.50) | ||
| Farmer | 1 | 7159 | 1.40 | 0.65 | (0.09, 4.70) | ||
| Fisher | 21 | 65,542 | 3.20 | 1.48 | (0.87, 2.51) | ||
| Others | 17 | 45,218 | 3.76 | 1.73 | (0.98, 3.06) | ||
| Comorbidities | |||||||
| Hypertension | |||||||
| No | 53 | 292,983 | 1.81 | 1.00 | – | 1.00 | – |
| Yes | 40 | 88,190 | 4.54 | 2.48 | (1.64, 3.75)*** | 1.61 | (1.00, 2.58)* |
| Diabetes | |||||||
| No | 72 | 332,861 | 2.16 | 1.00 | – | 1.00 | – |
| Yes | 21 | 48,312 | 4.35 | 1.98 | (1.22, 3.23)** | 1.28 | (0.76, 2.14) |
| Hyperlipidemia | |||||||
| No | 84 | 358,349 | 2.34 | 1.00 | – | ||
| Yes | 9 | 22,823 | 3.94 | 1.66 | (0.84, 3.31) | ||
| Coronary artery disease | |||||||
| No | 79 | 347,841 | 2.27 | 1.00 | – | 1.00 | – |
| Yes | 14 | 33,332 | 4.20 | 1.82 | (1.03, 3.21)* | 0.92 | (0.50, 1.70) |
| Cerebrovascular accident | |||||||
| No | 85 | 353,319 | 2.41 | 1.00 | – | ||
| Yes | 8 | 27,854 | 2.87 | 1.16 | (0.56, 2.41) | ||
| Chronic kidney disease | |||||||
| No | 86 | 373,043 | 2.31 | 1.00 | – | 1.00 | – |
| Yes | 7 | 8130 | 8.61 | 3.62 | (1.67, 7.85)** | 2.35 | (1.06, 5.21)* |
| COPD | |||||||
| No | 80 | 362,642 | 2.21 | 1.00 | – | 1.00 | – |
| Yes | 13 | 18,530 | 7.02 | 3.12 | (1.73, 5.61)*** | 2.18 | (1.18, 4.02)* |
| Chronic liver disease | |||||||
| No | 88 | 366,101 | 2.40 | 1.00 | – | ||
| Yes | 5 | 15,071 | 3.32 | 1.35 | (0.55, 3.34) | ||
| Autoimmune disease | |||||||
| No | 89 | 377,224 | 2.36 | 1.00 | – | 1.00 | – |
| Yes | 4 | 3948 | 10.13 | 4.26 | (1.56, 11.59)** | 3.83 | (1.4, 10.47)** |
| Psoriasis | |||||||
| No | 93 | 380,403 | 2.44 | 1.00 | – | ||
| Yes | 0 | 770 | 0.00 | 0.00 | |||
| Vasculitis | |||||||
| No | 93 | 380,965 | 2.44 | 1.00 | – | ||
| Yes | 0 | 207 | 0.00 | 0.00 | |||
| IBD | |||||||
| No | 91 | 372,731 | 2.44 | 1.00 | – | ||
| Yes | 2 | 8442 | 2.37 | 0.98 | (0.24, 3.97) | ||
NTS nontyphoidal salmonella, COPD chronic obstructive pulmonary disease, IBD Inflammatory bowel disease, PY person-year, IR incidence rate per 10,000 person-year, cHR crude hazard ratio, aHR adjusted hazard ratio.
†Adjusted by age, hypertension, diabetes, coronary artery disease, chronic kidney disease, COPD and rheumatoid autoimmune disease.
*p value < 0.05; **p value < 0.01; ***p value < 0.001.
Stratification analysis of nontyphoidal salmonella infection
The stratification analysis (Table 3) revealed that in those without comorbidities, compared with patients without bowel resections, patients who received bowel resections had significantly increased risk of NTS infection for those without hypertension (aHR of 2.34, 95% CI = 1.3–4.22), diabetes (aHR of 2.11, 95% CI = 1.29–3.46), hyperlipidemia (aHR of 1.91, 95% CI = 1.22–2.98), coronary artery disease (aHR of 1.82, 95% CI = 1.15–2.88), cerebrovascular accident (aHR of 1.59, 95% CI = 1.03–2.46), chronic kidney disease (aHR of 1.56, 95% CI = 1.01–2.39), COPD (aHR of 1.85, 95% CI = 1.17–2.93), chronic liver disease (aHR of 1.62, 95% CI = 1.05–2.48), vasculitis (aHR of 1.64, 95% CI = 1.08–2.48), or IBD (aHR of 1.59, 95% CI = 1.04–2.42). The significant association between bowel resection and NTS infection was not found in each age group of all patients, different genders, different occupations, patients without autoimmune disease or psoriasis, and patients with comorbidities.
Table 3.
The Stratification Analysis of NTS Infection.
| Variables | Without bowel resection | With bowel resection | cHR | (95% CI) | aHR† | (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | PY | IR | n | PY | IR | |||||
| Gender | ||||||||||
| Female | 14 | 88,765 | 1.58 | 20 | 85,661 | 2.33 | 1.51 | (0.76, 3.00) | 1.61 | (0.81, 3.19) |
| Male | 23 | 104,137 | 2.21 | 36 | 102,609 | 3.51 | 1.59 | (0.94, 2.68) | 1.63 | (0.96, 2.75) |
| Age, year | ||||||||||
| 18–30 | 1 | 22,053 | 0.45 | 1 | 21,707 | 0.46 | 1.07 | (0.07, 17.1) | 1.71 | (0.10, 30.2) |
| 31–40 | 3 | 27,077 | 1.11 | 9 | 26,366 | 3.41 | 3.19 | (0.86, 11.8) | 3.66 | (0.94, 14.2) |
| 41–50 | 3 | 35,047 | 0.86 | 3 | 35,674 | 0.84 | 0.97 | (0.19, 4.80) | 1.07 | (0.21, 5.34) |
| > 50 | 30 | 108,726 | 2.76 | 43 | 104,523 | 4.11 | 1.49 | (0.93, 2.38) | 1.54 | (0.96, 2.45) |
| Occupation | ||||||||||
| Officer | 14 | 86,403 | 1.62 | 24 | 88,454 | 2.71 | 1.70 | (0.88, 3.28) | 1.77 | (0.92, 3.43) |
| Worker | 8 | 45,223 | 1.77 | 8 | 43,174 | 1.85 | 1.03 | (0.38, 2.75) | 1.07 | (0.40, 2.88) |
| Farmer | 0 | 3893 | 0.00 | 1 | 3266 | 3.06 | ||||
| Fisher | 9 | 33,987 | 2.65 | 12 | 31,554 | 3.80 | 1.44 | (0.60, 3.41) | 1.44 | (0.61, 3.43) |
| Others | 6 | 23,397 | 2.56 | 11 | 21,821 | 5.04 | 2.01 | (0.74, 5.44) | 2.02 | (0.75, 5.47) |
| Comorbidities | ||||||||||
| Hypertension | ||||||||||
| No | 16 | 145,886 | 1.10 | 37 | 147,097 | 2.52 | 2.31 | (1.28, 4.15)** | 2.34 | (1.3, 4.22)** |
| Yes | 21 | 47,017 | 4.47 | 19 | 41,173 | 4.61 | 1.04 | (0.56, 1.93) | 1.07 | (0.58, 2.00) |
| Diabetes | ||||||||||
| No | 24 | 167,344 | 1.43 | 48 | 165,517 | 2.90 | 2.04 | (1.25, 3.33)** | 2.11 | (1.29, 3.46)** |
| Yes | 13 | 25,559 | 5.09 | 8 | 22,753 | 3.52 | 0.70 | (0.29, 1.68) | 0.74 | (0.30, 1.78) |
| Hyperlipidemia | ||||||||||
| No | 30 | 179,471 | 1.67 | 54 | 178,879 | 3.02 | 1.82 | (1.16, 2.84)** | 1.91 | (1.22, 2.98)** |
| Yes | 7 | 13,432 | 5.21 | 2 | 9392 | 2.13 | 0.41 | (0.09, 2.00) | 0.37 | (0.08, 1.78) |
| Coronary artery disease | ||||||||||
| No | 29 | 174,143 | 1.67 | 50 | 173,698 | 2.88 | 1.74 | (1.10, 2.75)* | 1.82 | (1.15, 2.88)* |
| Yes | 8 | 18,759 | 4.26 | 6 | 14,572 | 4.12 | 0.96 | (0.33, 2.76) | 0.90 | (0.31, 2.58) |
| Cerebrovascular accident | ||||||||||
| No | 34 | 176,656 | 1.92 | 51 | 176,663 | 2.89 | 1.51 | (0.98, 2.33) | 1.59 | (1.03, 2.46)* |
| Yes | 3 | 16,247 | 1.85 | 5 | 11,607 | 4.31 | 2.34 | (0.56, 9.79) | 2.21 | (0.53, 9.27) |
| Chronic kidney disease | ||||||||||
| No | 35 | 188,352 | 1.86 | 51 | 184,691 | 2.76 | 1.50 | (0.97, 2.30) | 1.56 | (1.01, 2.39)* |
| Yes | 2 | 4551 | 4.39 | 5 | 3579 | 13.97 | 3.19 | (0.62, 16.5) | 2.63 | (0.50, 13.8) |
| COPD | ||||||||||
| No | 29 | 182,097 | 1.59 | 51 | 180,545 | 2.82 | 1.78 | (1.13, 2.82)* | 1.85 | (1.17, 2.93)** |
| Yes | 8 | 10,806 | 7.40 | 5 | 7725 | 6.47 | 0.86 | (0.28, 2.62) | 0.87 | (0.28, 2.70) |
| Chronic liver disease | ||||||||||
| No | 35 | 184,434 | 1.90 | 53 | 181,667 | 2.92 | 1.55 | (1.01, 2.37)* | 1.62 | (1.05, 2.48)* |
| Yes | 2 | 8468 | 2.36 | 3 | 6603 | 4.54 | 1.95 | (0.33, 11.7) | 1.88 | (0.31, 11.3) |
| Autoimmune disease | ||||||||||
| No | 37 | 190,628 | 1.94 | 52 | 186,596 | 2.79 | 1.45 | (0.95, 2.21) | 1.51 | (0.99, 2.31) |
| Yes | 0 | 2274 | 0.00 | 4 | 1674 | 23.89 | ||||
| Psoriasis | ||||||||||
| No | 37 | 192,392 | 1.92 | 56 | 188,011 | 2.98 | 1.56 | (1.03, 2.37)* | 1.51 | (0.99, 2.31) |
| Yes | 0 | 510 | 0.00 | 0 | 259 | 0.00 | ||||
| Vasculitis | ||||||||||
| No | 37 | 192,762 | 1.92 | 56 | 188,204 | 2.98 | 1.56 | (1.03, 2.37)* | 1.64 | (1.08, 2.48)* |
| Yes | 0 | 141 | 0.00 | 0 | 67 | 0.00 | ||||
| IBD | ||||||||||
| No | 37 | 188,948 | 1.96 | 54 | 183,783 | 2.94 | 1.52 | (1.00, 2.3) | 1.59 | (1.04, 2.42)* |
| Yes | 0 | 3955 | 0.00 | 2 | 4487 | 4.46 | ||||
NTS nontyphoidal salmonella, COPD chronic obstructive pulmonary disease, IBD inflammatory bowel disease, PY person-year, IR incidence rate per 10,000 person-year, cHR crude hazard ratio, aHR adjusted hazard ratio.
†Adjusted by age, hypertension, diabetes, coronary artery disease, chronic kidney disease, COPD and rheumatoid autoimmune disease.
*p value < 0.05, **p value < 0.01, ***p value < 0.001.
Results of sensitivity analysis
Results of our sensitivity analysis were almost consistent with those of our primary analyses (Table 4). The differences are that our sensitivity analysis even indicated that patients would have an increased risk of NTS infection receiving large bowel resection (aHR of 1.69, 95% CI = 1.02–2.80) or left hemicolectomy (aHR of 2.41, 95% CI = 1.01–5.77). The patient baseline characteristics in our sensitivity analysis are shown in Table 5.
Table 4.
Sensitivity Analysis (Excluding Peptic Ulcer Disease Patients).
| Type of bowel resection | NTS infection | cHR | (95% CI) | aHR† | (95% CI) |
|---|---|---|---|---|---|
| n | |||||
| Bowel resection | 52 | 1.58 | (1.02, 2.43)* | 1.66 | (1.07, 2.56)* |
| Small bowel resection | 27 | 1.93 | (1.17, 3.21)* | 1.92 | (1.04, 3.19)* |
| Large bowel resection | 27 | 1.58 | (0.95, 2.62) | 1.69 | (1.02, 2.80)* |
| Right hemicolectomy | 12 | 1.90 | (0.98, 3.68) | 2.27 | (1.17, 4.43)* |
| Transverse colon resection | 0 | ||||
| Left hemicolectomy | 6 | 2.71 | (1.14, 6.46)* | 2.41 | (1.01, 5.77)* |
| Sigmoidectomy | 6 | 2.01 | (0.84, 4.78) | 1.91 | (0.79, 4.57) |
| Total colectomy | 0 | ||||
| Bowel anastomosis | 9 | 0.90 | (0.43, 1.88) | 1.06 | (0.51, 2.23) |
NTS nontyphoidal salmonella, n number of event, cHR crude hazard ratio, aHR adjusted hazard ratio.
†Adjusted by age, hypertension, diabetes, coronary artery disease, chronic kidney disease, COPD and rheumatoid autoimmune disease.
*p value < 0.05, **p value < 0.01, ***p value < 0.001.
Table 5.
Demographic Characteristics of Patients with and without Bowel Resection (Excluding Peptic Ulcer Disease Patients).
| Variables | Bowel resection | SMD | |||
|---|---|---|---|---|---|
| No (n = 35,004) | Yes (n = 35,004) | ||||
| n | % | n | % | ||
| Gender | 0.01 | ||||
| Female | 17,098 | 49% | 16,886 | 48% | |
| Male | 17,906 | 51% | 18,118 | 52% | |
| Age, year | |||||
| 18–30 | 3396 | 10% | 3195 | 9% | 0.02 |
| 31–40 | 4621 | 13% | 4592 | 13% | 0.002 |
| 41–50 | 6345 | 18% | 6217 | 18% | 0.01 |
| > 50 | 20,642 | 59% | 21,000 | 60% | 0.02 |
| Mean, (SD) | 55.4 | (18.4) | 56.0 | (18.3) | 0.03 |
| Occupation | |||||
| Officer | 16,298 | 47% | 16,332 | 47% | 0.002 |
| Worker | 7586 | 22% | 7762 | 22% | 0.01 |
| Farmer | 738 | 2% | 582 | 2% | 0.03 |
| Fisher | 6076 | 17% | 6119 | 17% | 0.00 |
| Others | 4306 | 12% | 4209 | 12% | 0.01 |
| Comorbidities | |||||
| Hypertension | 10,099 | 29% | 9965 | 28% | 0.01 |
| Diabetes | 6247 | 18% | 5371 | 15% | 0.07 |
| Hyperlipidemia | 2683 | 8% | 2329 | 7% | 0.04 |
| Coronary artery disease | 4192 | 12% | 3714 | 11% | 0.04 |
| Cerebrovascular accident | 3674 | 10% | 3159 | 9% | 0.05 |
| Chronic kidney disease | 1111 | 3% | 1176 | 3% | 0.01 |
| COPD | 2449 | 7% | 2153 | 6% | 0.03 |
| Chronic liver disease | 1977 | 6% | 1585 | 5% | 0.05 |
| Autoimmune disease | 400 | 1% | 390 | 1% | 0.003 |
| Psoriasis | 72 | 0.2% | 74 | 0.2% | 0.001 |
| Vasculitis | 166 | 0.5% | 14 | 0.04% | 0.09 |
| IBD | 665 | 2% | 752 | 2% | 0.02 |
SD standard deviation, SMD standardized mean difference, COPD chronic obstructive pulmonary disease, IBD inflammatory bowel disease.
Discussion
Our study first demonstrated that bowel resection was associated with a significantly increased risk of NTS infection. Of note, the HR of NTS infection for patients with small bowel resection or right hemicolectomy was nearly two times greater than for those without small bowel resection or right hemicolectomy.
We hypothesized that based on the bowel resection site, the microbiota composition change would result in NTS infection. As mentioned above, the reported bacterial species in the intestine included Bacilli (Firmicutes), Streptococcaceae (Firmicutes), Actinobacteria, Clostridium, Staphylococcus, Bacteroides, Lactobacillus, Enterococcus, Bifidobacterium, Enterobacteriaceae, and Ruminococcus. Oh et al. demonstrated the potential protective effects of using Bacillus subtilis CSL2, against Salmonella gallinarum infection on laying hens15. Actinomyces might have antimicrobial potency toward NTS 16. Jacobson et al. discovered that in mice, Bacteroides spp. limit intestinal Salmonella typhimurium expansion and fecal shedding17. Lactobacillus has remarkable anti-salmonella activities in vivo and in vitro18,19. Strains of Bifidobacterium were antagonistic to Salmonella20. Bifidobacterium thermophilum RBL67 influences the transcriptome of Salmonella and causes an imbalanced virulence gene expression, but can protect hosts from infection21. Clostridia, including the genera Roseburia and Blautia from the family Lachnospiraceae and the genera Ruminococcus and Anaerovibrio, were more abundant in Salmonella-negative pigs8. A metabolite from bacteria—indole, is probably associated with NTS infection in our gut. Indole can prevent NTS infection because of its effects on decreasing Salmonella invasion in vivo, Salmonella motility, virulence gene expression, and increasing epithelial cells’ resistance to Salmonella invasion22.
Gordon et al. indicated that host risk factors included extremes of age and immunocompromised status such as rheumatologic disease, which corresponded with our results3. We discovered that patients aged 31–40 years had an increased risk of NTS infection, which was first reported by us. Our study demonstrated other risk factors for NTS infection like hypertension, chronic kidney disease, and COPD. Atherosclerosis was demonstrated a risk factor for endovascular Salmonella bacteremia23. Traditional risk factors for atherosclerosis included hypertension, so the hypertension might be associated with NTS infection24. Chronic kidney disease was not identified as a risk factor for NTS infection before. The possible explanation is that chronic kidney disease could result in immunocompromised status so that patients easily got NTS infection. Lisowska’s study showed peripheral CD4 + and CD8 + T cells and B cells in the blood decrease25, and Fernández-Fresnedo et al. indicated an increased incidence of apoptosis in B cells in chronic kidney disease patients26. In end-stage renal disease patients, increased apoptosis and diminished populations of naïve and central memory T cells were found, and their antigen-specific memory CD4 + T cells were impaired27. In smokers with COPD, Knobloch’s research revealed that interferon-γ release from ex vivo generated CD4+ effector cells of the Th1 subtype upon challenge with lipopolysaccharide (LPS) purified from Salmonella minnesota would decrease28.
Our stratification analysis showed patients without hypertension, diabetes, hyperlipidemia, coronary artery disease, cerebrovascular accident, chronic kidney disease, COPD, chronic liver diseases, vasculitis, or IBD would be at higher risk of NTS infection after bowel resection. We might explain this phenomenon by the fact that affected patients usually have underlying diseases, so that NTS poses significant health threats4. If underlying covariates did not exist, bowel resection would play a significant predisposing factor of NTS infection. Our results reaffirm that in patients without underlying diseases, bowel resection should be considered carefully to avoid possible NTS infection in the future.
Our study has the advantage that it is a large-scale nationwide analysis with longitudinal follow-up. However, we admit several limitations to our study. First, we lacked information regarding body mass index, alcohol consumption, betel nut use, smoking, and other immunomodulator prescription. However, we used adjusted covariates, such as autoimmune diseases, psoriasis, and IBD, which could represent immune-related medication use. Second, the potential misclassification in establishing study cohorts might exist. We used bowel resection procedure codes to identify the case group. The policy of patient anonymity within the NHIRD prevented us from confirming patients’ diagnoses. Third, we demonstrated that right hemicolectomy in our primary analyses and left hemicolectomy in our sensitivity analysis increased the risk of NTS infection, but we did not discover any reference which could explain the mechanism.
Conclusions
Bowel resection causes an increased risk of NTS infection. Patients aged 31–40 and > 50 years or those with comorbidities such as hypertension, chronic kidney disease, COPD, and autoimmune disease have an elevated risk of NTS infection. Furthermore, in patients without comorbidities, bowel resection should be considered carefully.
Acknowledgements
The authors expressed their appreciation to the Department of Medical Education and Research and Research Center of Medical Informatics in Kaohsiung Municipal United Hospital for inquiries and assistance in data processing.
Author contributions
Conceptualization: K.-T.Y., S.-E.J., J.C.-C.W., R.C., Y.-M.H. Data curation: K.-T.Y., S.-E.J., J.C.-C.W., H.-T.Y., R.C., Y.-M.H. Formal analysis: J.C.-C.W., H.-T.Y., R.C., Y.-M.H. Investigation: K.-T.Y., R.C. Methodology: S.-E.J., J.C.-C.W., Y.-M.H. Project administration: K.-T.Y., S.-E.J., J.C.-C.W., H.-T.Y., R.C., Y.-M.H. Visualization: J.C.-C.W., H.-T.Y., Y.-M.H. Writing—original draft: K.-T.Y., S.-E.J. Writing—review and editing: R.C, Y.-M.H.
Funding
This study was supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST 109-2321-B-039-002), China Medical University Hospital (DMR-109-231), Tseng-Lien Lin Foundation, Taichung, Taiwan.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.GBD 2017 Non-Typhoidal Salmonella Invasive Disease Collaborators The global burden of non-typhoidal salmonella invasive disease: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis. 2019;19:1312–24. doi: 10.1016/S1473-3099(19)30418-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia-Vidal C, Rodríguez-Fernández S, Teijón S, Esteve M, Rodríguez-Carballeira M, Lacasa JM, et al. Risk factors for opportunistic infections in infliximab-treated patients: the importance of screening in prevention. Eur. J. Clin. Microbiol. Infect. Dis. 2009;28:331–337. doi: 10.1007/s10096-008-0628-x. [DOI] [PubMed] [Google Scholar]
- 3.Gordon MA. Salmonella infections in immunocompromised adults. J Infect. 2008;56:413–422. doi: 10.1016/j.jinf.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 4.Gradel KO, Dethlefsen C, Schønheyder HC, Nielsen H. Magnitude of bacteraemia is associated with increased mortality in non-typhoid salmonellosis: a one-year follow-up study. APMIS. 2008;116:147–153. doi: 10.1111/j.1600-0463.2008.00886.x. [DOI] [PubMed] [Google Scholar]
- 5.Dieterich W, Schink M, Zopf Y. Microbiota in the gastrointestinal tract. Med. Sci. (Basel). 2018;6:116. doi: 10.3390/medsci6040116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanner SA, Chassard C, Zihler Berner A, Lacroix C. Synergistic effects of Bifidobacterium thermophilum RBL67 and selected prebiotics on inhibition of Salmonella colonization in the swine proximal colon PolyFermS model. Gut. Pathog. 2014;6:44. doi: 10.1186/s13099-014-0044-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le Moal VL, Fayol-Messaoudi D, Servin AL. Compound(s) secreted by Lactobacillus casei strain Shirota YIT9029 irreversibly and reversibly impair the swimming motility of Helicobacter pylori and Salmonella enterica serovar Typhimurium, respectively. Microbiology. 2013;159:1956–1971. doi: 10.1099/mic.0.067678-0. [DOI] [PubMed] [Google Scholar]
- 8.Argüello H, Estellé J, Leonard FC, Crispie F, Cotter PD, O'Sullivan O, et al. Influence of the intestinal microbiota on colonization resistance to salmonella and the shedding pattern of naturally exposed pigs. mSystems. 2019;4:e00021–19. doi: 10.1128/mSystems.00021-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bachmann R, Leonard D, Delzenne N, Kartheuser A, Cani PD. Novel insight into the role of microbiota in colorectal surgery. Gut. 2017;66:738–749. doi: 10.1136/gutjnl-2016-312569. [DOI] [PubMed] [Google Scholar]
- 10.Kunz LJ, Waddell WR. Association of Salmonella enteritis with operations on the stomach. N. Engl. J. Med. 1956;255:555–559. doi: 10.1056/NEJM195609202551203. [DOI] [PubMed] [Google Scholar]
- 11.Hsing AW, Ioannidis JP. Nationwide population science: lessons from the Taiwan national health insurance research database. JAMA Intern. Med. 2015;175:1527–1529. doi: 10.1001/jamainternmed.2015.3540. [DOI] [PubMed] [Google Scholar]
- 12.National Health Research Institutes. National Health Insurance Research Database, Taiwan. http://nhird.nhri.org.tw/en/index.htm. Accessed May 30th, 2020.
- 13.Heinze G, Jüni P. An overview of the objectives of and the approaches to propensity score analyses. Eur. Heart J. 2011;32:1704–1708. doi: 10.1093/eurheartj/ehr031. [DOI] [PubMed] [Google Scholar]
- 14.Wu HH, Chen YT, Shih CJ, Lee YT, Kuo SC, Chen TL. Association between recent use of proton pump inhibitors and nontyphoid salmonellosis: a nested case-control study. Clin. Infect. Dis. 2014;59:1554–1558. doi: 10.1093/cid/ciu628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oh JK, Pajarillo EAB, Chae JP, Kim IH, Kang DK. Protective effects of Bacillus subtilis against Salmonella infection in the microbiome of Hy-Line Brown layers. Asian Aust. J. Anim. Sci. 2017;30:1332–1339. doi: 10.5713/ajas.17.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohamed H, Miloud B, Zohra F, García-Arenzana JM, Veloso A, Rodríguez-Couto S. Isolation and characterization of actinobacteria from algerian sahara soils with antimicrobial activities. Int. J. Mol. Cell Med. 2017;6:109–120. doi: 10.22088/acadpub.BUMS.6.2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobson A, Lam L, Rajendram M, Tamburini F, Honeycutt J, Pham T, et al. A gut commensal-produced metabolite mediates colonization resistance to salmonella infection. Cell Host Microbe. 2018;24(296–307):e7. doi: 10.1016/j.chom.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu J, Hu D, Chen Y, Huang H, Zhang H, Zhao J, et al. Strain-specific properties of Lactobacillus plantarum for prevention of Salmonella infection. Food Funct. 2018;9:3673–3682. doi: 10.1039/C8FO00365C. [DOI] [PubMed] [Google Scholar]
- 19.Abatemarco Júnior M, Sandes SHC, Ricci MF, Arantes RME, Nunes ÁC, Nicoli JR, et al. Protective effect of lactobacillus diolivorans 1z, isolated from brazilian kefir, against salmonella enterica serovar typhimurium in experimental murine models. Front Microbiol. 2018;9:2856. doi: 10.3389/fmicb.2018.02856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bielecka M, Biedrzycka E, Biedrzycka E, Smoragiewicz W, Smieszek M. Interaction of Bifidobacterium and Salmonella during associated growth. Int. J. Food Microbiol. 1998;45:151–155. doi: 10.1016/S0168-1605(98)00150-0. [DOI] [PubMed] [Google Scholar]
- 21.Tanner SA, Chassard C, Rigozzi E, Lacroix C, Stevens MJ. Bifidobacterium thermophilum RBL67 impacts on growth and virulence gene expression of Salmonella enterica subsp. enterica serovar Typhimurium. BMC Microbiol. 2016;16:46. doi: 10.1186/s12866-016-0659-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kohli N, Crisp Z, Riordan R, Li M, Alaniz RC, Jayaraman A. The microbiota metabolite indole inhibits Salmonella virulence: involvement of the PhoPQ two-component system. PLoS ONE. 2018;13:e0190613. doi: 10.1371/journal.pone.0190613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu RB, Lin FY. Risk factors for bacteraemia and endovascular infection due to non-typhoid salmonella: a reappraisal. QJM. 2005;98:821–827. doi: 10.1093/qjmed/hci126. [DOI] [PubMed] [Google Scholar]
- 24.Fruchart JC, Nierman MC, Stroes ES, Kastelein JJ, Duriez P. New risk factors for atherosclerosis and patient risk assessment. Circulation. 2004;109:III-15-9. doi: 10.1161/01.CIR.0000131513.33892.5b. [DOI] [PubMed] [Google Scholar]
- 25.Lisowska KA, Dębska-Ślizień A, Jasiulewicz A, Heleniak Z, Bryl E, Witkowski JM. Hemodialysis affects phenotype and proliferation of CD4-positive T lymphocytes. J. Clin. Immunol. 2012;32:189–200. doi: 10.1007/s10875-011-9603-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fernández-Fresnedo G, Ramos MA, González-Pardo MC, de Francisco AL, López-Hoyos M, Arias M. B lymphopenia in uremia is related to an accelerated in vitro apoptosis and dysregulation of Bcl-2. Nephrol. Dial Transpl. 2000;15:502–510. doi: 10.1093/ndt/15.4.502. [DOI] [PubMed] [Google Scholar]
- 27.Litjens NH, Huisman M, van den Dorpel M, Betjes MG. Impaired immune responses and antigen-specific memory CD4+ T cells in hemodialysis patients. J. Am. Soc. Nephrol. 2008;19:1483–1490. doi: 10.1681/ASN.2007090971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knobloch J, Schild K, Jungck D, Urban K, Müller K, Schweda EK, et al. The T-helper cell type 1 immune response to gram-negative bacterial infections is impaired in COPD. Am. J. Respir. Crit. Care Med. 2011;183:204–214. doi: 10.1164/rccm.201002-0199OC. [DOI] [PubMed] [Google Scholar]