Abstract
A 53-year-old man, who performed a 44-minute dive to a depth of 21 meters, felt severe abdominal pain with dyspnea after surfacing. An ultrasound study showed a marked snowstorm pattern in the portal vein of the liver and right ventricle, and whole body computed tomography revealed multiple gas bubbles in the right ventricle, inferior vena cava, portal, mesenteric and femoral vein. He was thus diagnosed to have decompression sickness and was therefore transported to another hospital to undergo hyperbaric oxygen therapy. Patients who present with abdominal symptoms after diving should be immediately evaluated by ultrasound and computed tomography.
Keywords: Decompression sickness, Ultrasound, Diagnosis
Introduction
Decompression sickness (DCS) is a disease that results from an ascent profile that does not allow for the orderly elimination of excess gas that was accumulates in tissues during exposure to elevated pressure. DCS can present idiosyncratically, affecting a wide range of systems with a variable degree of insult [1]. One common approach to classification is to describe DCS as type 1 or type 2. Type 1 DCS is usually characterized by musculoskeletal pain and mild cutaneous symptoms [1]. Type 2 symptoms are considered more serious and typically fall into 3 categories: neurological, inner ear, and cardiopulmonary complications [1]. First aid for DCS is high fraction oxygen; the definitive treatment is hyperbaric oxygen therapy. We herein report a rare case of DCS with acute abdomen and usefulness of ultrasound study to diagnose DCS.
Case report
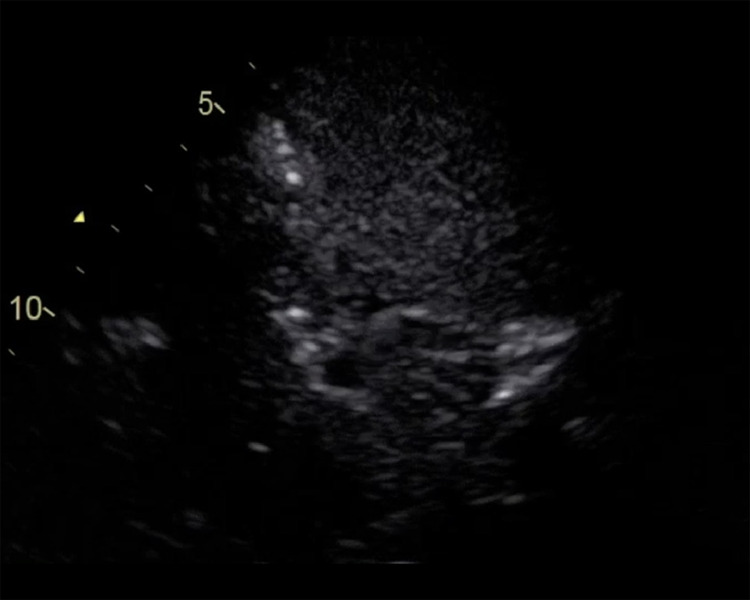
The patient was a 53-year-old man performed 2 sessions of scuba diving even after he felt some chest discomfort after the diving session. The first session was from 08:15 to 08:55, while the second was from 10:30 to 11:15. The maximum depth was 21 meters and the average was 15 meters. After surfacing and being transported to shore by boat, he felt severe abdominal pain with dyspnea. The past history of the patient, who was from Tokyo and who had visited Izu peninsula as a tourist, included hypertension and diabetes mellitus. He had experienced approximately 100 dives. A diving instructor called an ambulance at 11:30 and a physician-staffed helicopter was requested; however, it could not respond due to cloud cover [2]. When an emergency medical physician checked him at 11:40, he showed severe abdominal pain with hyperhidrosis, cyanosis and signs of peritoneal irritation. His vital signs were as follows: Glasgow Coma Scale, E3V4M6; blood pressure, 140/90 mmHg; pulse rate, 104 beats/min; respiratory rate, 24 breaths/min; peripheral oxygen saturation on room air, 84%; and body temperature, 36.1°C. He was transported to our hospital by ambulance. Upon arrival at 12:51, his abdominal pain improved slightly. Cutis marmorata was observed on his abdomen (Fig. 1). His vital signs were as follows: Glasgow Coma Scale, E3V4M6; blood pressure, 130/80 mmHg; pulse rate, 98 beats/min; respiratory rate, 20 breaths/min; peripheral oxygen saturation under 10 L/min by oxygen mask, 94%; body temperature, 36.1°C. Electrocardiography was negative. An ultrasound study performed at 13:00 showed a marked snowstorm pattern in his portal vein in the liver (Fig. 2, Video 1) and right ventricle, and the inferior vena cava was collapsed without ascites while the patient was receiving massive fluid resuscitation. Right-left shunt was not observed. A venous gas analysis revealed the following: pH 7.27; PCO2, 26.2 mm Hg; PO2, 31.6 mm Hg; HCO3−, 20.7 mmol/L; base excess, -6.7 mmol/L; lactate, 3.8 mmol/L and hemoglobin, 20.1 g/dL. A blood analysis on arrival revealed the following findings: white blood cell count, 19,000/mm3; hemoglobin, 20.4 g/dL; platelets, 24.9 × 104/mm3; aspartate aminotransferase, 30 IU/L alanine aminotransferase, 20 IU/L; total bilirubin, 0.8 mg/dL; total protein, 7.4 g/dL; glucose, 183 mg/dL; blood urea nitrogen, 17.4 mg/dL; creatinine, 1.34 mg/dL; amylase, 51 IU/L; creatine phosphokinase, 213 IU/L; sodium, 140 mEq/L; potassium, 3.4 mEq/L; chloride, 100 mEq/L; c-reactive protein, 0.04 mg/dL; prothromboplastin time, 9.9 (control; 11.2) sec; activated partial thromboplastin time, 26.9 (control; 26.9) sec; fibrinogen, 276 mg/dL; fibrin degradation products, 9.2 μg/mL; and troponin T, <0.010 ng/mL. Whole body computed tomography at 13:23 (CT) revealed multiple gas bubbles in right ventricle, inferior vena cava, portal, mesenteric and femoral vein (Fig. 3). Under a diagnosis of DCS, he was transported to another hospital by physician-staffed helicopter (departure, 14:00; arrival 14:27) to receive hyperbaric oxygen therapy. During transportation, he received fluid resuscitation and high-concentration oxygen. After undergoing hyperbaric oxygen therapy (United States Navy Treatment Table 6), magnetic resonance imaging showed multiple cerebral ischemic changes, which were deemed to be compatible with gas embolism (Fig. 4). The air in his body was observed to have diminished on the CT findings obtained on day 2. His condition was complicated with delirium non-convulsive status epilepticus, which was treated with an anticonvulsant. He was finally discharged on foot on day 6 with recent memory disturbance and returned to Tokyo with his wife.
Fig. 1.
The patient on arrival. The chest and abdomen show cuitis marmorata.
Fig. 2.
Ultrasound on arrival. Ultrasound shows a snowstorm pattern in the hepatic portal vein (arrow).
Fig. 3.
Computed tomography (CT) on arrival. CT showed multiple gas bubbles in the heart and vascular system (arrow).
Fig. 4.
Magnetic resonance imaging after undergoing hyperbaric oxygen therapy (upper, diffusion weighted image; lower, apparent diffusion coefficient map). The MRI findings showed multiple cerebral ischemic changes (arrow), which were deemed to be compatible with gas embolism.
Discussion
This is an illustrative case report that indicates the usefulness of ultrasound and subsequent CT in the diagnosis of acute-phase DCS with acute abdomen. Ultrasound shows high sensitivity in the detection of gas in vascular system or heart; thus, even an asymptomatic diver shows gas in their vascular system, immediately after diving [3,4]. Accordingly, if an immediate ultrasound study fails to detect gas in the vascular system or heart of a symptomatic diver immediately after a dive, this may exclude DCS [5,6]. Abdominal pain after diving is a rare symptom. In addition to the general differential diagnosis of abdominal pain, the patient should be assessed for gastric rupture due to barotrauma or abdominal DCS [7], [8], [9], [10], [11]. As ultrasound is a useful and less invasive examination in comparison to other diagnostic methods, the physician should immediately use ultrasound to rule out DCS or to aid in the diagnosis of DCS for a patient whose complains of abdominal pain after diving.
Conclusion
We presented an illustrative case report that indicates usefulness of ultrasound and subsequent CT in the diagnosis of acute-phase DCS with acute abdomen. Patients who present abdominal symptoms after diving should be immediately evaluated by ultrasound.
Footnotes
Acknowledgments: This work was supported in part by a Grant-in-Aid for Special Research in Subsidies for ordinary expenses of private schools from The Promotion and Mutual Aid Corporation for Private Schools of Japan.
Competing Interests: The authors have declared that no competing interests exist.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2021.01.004.
Appendix. Supplementary materials
References
- 1.Pollock NW, Buteau D. Updates in decompression illness. Emerg Med Clin North Am. 2017;35(2):301–319. doi: 10.1016/j.emc.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Yanagawa Y, Onitsuka M, Nozawa Y, Nagasawa H, Ikuto T, Jitsuiki K. The significance of a cooperative medical system for treating decompression illness on the Izu Peninsula in Japan. Wilderness Environ Med. 2019;30(3):268–273. doi: 10.1016/j.wem.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Germonpré P, Balestra C. Preconditioning to reduce decompression stress in Scuba Divers. Aerosp Med Hum Perform. 2017;88(2):114–120. doi: 10.3357/AMHP.4642.2017. [DOI] [PubMed] [Google Scholar]
- 4.Bakovic D, Glavas D, Palada I, Breskovic T, Fabijanic D, Obad A. High-grade bubbles in left and right heart in an asymptomatic diver at rest after surfacing. Aviat Space Environ Med. 2008;79(6):626–628. doi: 10.3357/asem.2244.2008. [DOI] [PubMed] [Google Scholar]
- 5.Yanagawa Y, Omori K, Takeuchi I, Jitsuiki K, Ohsaka H, Ishikawa K. The on-site differential diagnosis of decompression sickness from endogenous cerebral ischaemia in an elderly Ama diver using ultrasound. Diving Hyperb Med. 2018;48(4):262–263. doi: 10.28920/dhm48.4.262-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ohsaka H, Jitsuiki K, Takeuchi I, Yoshizawa T, Omori K, Ishikawa K. Ultrasound for diagnosing inner ear decompression sickness. Sch J Med Case Rep. 2016;4(8):605–606. [Google Scholar]
- 7.Titu LV, Laden G, Purdy GM, Wedgwood KR. Gastric barotrauma in a scuba diver: report of a case. Surg Today. 2003;33(4):299–301. doi: 10.1007/s005950300067. [DOI] [PubMed] [Google Scholar]
- 8.Petri NM, Vranjković-Petri L, Aras N, Druzijanić N. Gastric rupture in a diver due to rapid ascent. Croat Med J. 2002;43(1):42–44. [PubMed] [Google Scholar]
- 9.Kondo A, Nagawasa H, Takeuchi I, Yanagawa Y. Portal venous gas due to decompression sickness. Intern Med. 2018;57(14):2091. doi: 10.2169/internalmedicine.0418-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beale P, Kitchen L, Graf WR, Fenton ME. Abdominal decompression illness following repetitive diving: a case report and review of the literature. Undersea Hyperb Med. 2019;46(2):211–215. [PubMed] [Google Scholar]
- 11.Toyota S, Nagata S, Yoshino S, Kono S, Kawanami S, Maeda S. Mesenteric venous thrombosis as a rare complication of decompression sickness. Surg Case Rep. 2020;6(1):24. doi: 10.1186/s40792-020-0780-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.