Abstract
This study aims to locate the knots of cumulative coronavirus disease 2019 (COVID-19) case number during the first-level response to public health emergency in the provinces of China except Hubei. The provinces were grouped into three regions, namely eastern, central and western provinces, and the trends between adjacent knots were compared among the three regions. COVID-19 case number, migration scale index, Baidu index, demographic, economic and public health resource data were collected from 22 Chinese provinces from 19 January 2020 to 12 March 2020. Spline regression was applied to the data of all included, eastern, central and western provinces. The research period was divided into three stages by two knots. The first stage (from 19 January to around 25 January) was similar among three regions. However, in the second stage, growth of COVID-19 case number was flatter and lasted longer in western provinces (from 25 January to 18 February) than in eastern and central provinces (from 26 February to around 11 February). In the third stage, the growth of COVID-19 case number slowed down in all the three regions. Included covariates were different among the three regions. Overall, spline regression with covariates showed the different change patterns in eastern, central and western provinces, which provided a better insight into regional characteristics of COVID-19 pandemic.
Key words: COVID-19, first-level response, major public health emergency, spline regression
Introduction
On 31 December 2019, the WHO China Country Office was informed that cases of pneumonia of unknown aetiology were found in Wuhan City, Hubei Province of China [1–4]. On 7 January 2020, the Chinese authorities identified a new type of coronavirus. And the coronavirus study group of the International Committee on Taxonomy of Viruses named it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on 11 February 2020 [5]. On the same day, WHO named this new infectious disease as coronavirus disease 2019 (COVID-19) [6].
On 23 January 2020, the Chinese government initiated the first-level response to major public health emergencies. The central and all levels of governments took a combination of measures to prevent and control the outbreak of COVID-19. Until 12 March 2020, the number of daily confirmed cases out of Hubei had reduced to 3. Considering the limited number of active COVID-19 cases, the levels of response to major public health emergency in many regions were adjusted to second- or third level. Until the end of June, only 2750 local cases were newly confirmed out of Hubei, averaging 25 cases per day.
In the meantime, the outbreak of COVID-19 has become a global health threat as more than 200 countries and regions from Africa, America, eastern Mediterranean, Europe, South-East Asia and western Pacific are being influenced by COVID-19. Until 30 June 2020, a total of 10 185 374 cases had been confirmed around the world, including 503 862 deaths [7]. The growing trend of confirmed COVID-19 cases has not been effectively contained globally. Previous studies have reported the aetiological, epidemiological, clinical characteristics and treatment of COVID-19 cases [8–13], but few researchers have analysed the knots of COVID-19 case number with spline regression. After the implementation of controlling measure, the number of COVID-19 cases showed non-linear characteristics and non-trend patterns. Splines allow for smooth transitions and subtle structural shifts by piecing together different polynomial line segments, which is an alternative model to deal with the characteristics of COVID-19 case number. Agiwal's study [14] showed spline function is useful to convert the non-linear trend of newly COVID-19 cases into a linear pattern. Sousa et al. [15] proposed an automatic method based on the minimisation of the sum of squared residuals plus a penalty to estimate the knot number and locations. Demertzis et al. [16] applied regression splines of random knots and complex-network regression splines to fit cumulative COVID-19 infection, death and ICU patient curve of Greece, which performed better than cubic fittings. In these studies, social and medical factors were not considered, which would influence the spread of SARS-CoV-2. And as far as we know, there were no studies analysing the data of COVID-19 cases in China with spline terms.
Therefore, this study was conducted to analyse the cumulative COVID-19 case number during the first-level response in provinces out of Hubei, who experienced importing, spreading and containing stages during this period. Influencing factors at province level were considered, too. The first confirmed cases in the provinces out of Hubei were all imported cases, indicating the influence of transient population from Hubei. Detection, diagnosis, isolation and treatment of COVID-19 cases heavily relied on the public health resources in each province, and population susceptibility might be influenced by demographic characteristics, economic status and access to COVID-19 information. Stepwise procedure was used to select knot numbers, locations and covariates, which were statistically selected [17]. The objectives of this study were: (1) to locate the knots of COVID-19 case number, (2) to describe the change pattern of each segment; (3) to explore the difference of change patterns among eastern, central and western provinces.
Methods
Data collection
The daily numbers of newly confirmed COVID-19 cases between 19 January 2020 and 12 March 2020 for all provinces (except Hubei) were obtained from the websites of Provincial Municipal Health Commission. This 54 day research period was chosen specifically because the first COVID-19 case out of Hubei was confirmed on 19 January 2020 and 26 provinces adjusted emergency response to second- or third level before 12 March 2020. Provinces initiating the first-level response to major public health emergency between 23 January 2020 and 25 January 2020 were included, and provinces with incomplete data or reporting less than 100 cases during the research period were excluded.
Daily transient population size at the province level was obtained from Qianxi Map, an open data platform funded by Baidu [18]. Baidu provides mobile termination service for more than 1.1 billion people and location-based service (LBS) over 120 billion times per day in China. When a customer sends a service request to Baidu, his or her location is included in the request. Therefore, the transient population to any provinces and regions are recognised through the location-based system, no matter what types of transportation they take. Migration scale index, calculated based on LBS data, represents the size of the transient population. It is comparable horizontally among provinces or regions, and one migration scale index is equal to about 56 137 travellers [19]. For each included province, daily migration scale index from Hubei was collected.
Baidu index (BI) of two variances of novel coronavirus and three variances of novel coronavirus pneumonia was used to reflect public attention to COVID-19. This index was calculated based on the number of times that a word appeared in Baidu search engine, which was the largest search engine in China, holding 63.56%–72.72% market share in China from January 2020 to March 2020 [20, 21]. These variances had the highest searching frequency in Baidu search engine among the ones related to COVID-19 during the research period.
Yearly demographic, economic and public health resource data of each province in China were extracted from Chinese Health Statistical Yearbook 2019, published by Chinese National Municipal Health Commission on 1 August 2019 [22]. This book presented Chinese health care and inhabitant's health status in the whole nation and each province in 2018. Provinces were grouped into eastern, central and western, according to the geographic location. Population by age groups (0–14 years old, 15–64 years old and over 65 years old) and sex ratio (male/female) at province level were extracted from this book, since previous studies had reported older age and gender as potential factors affecting the risk of COVID-19 at personal level [23, 24]. Per capita gross domestic product (GDP), per capita health care expenditure, number of registered doctors, nurses, beds in infectious disease department and public health professionals per 1000 population at province level were collected as well, because they probably would reflect economic status related to general health and public health resources related to infectious disease.
Data analysis
Continuous variables were presented as median and inter-quartile range (IQR). Categorical variables were described as frequencies and percentages. Pearson correlation was conducted to explore the correlation among daily-reported variables, and Spearman rank-order correlation was conducted among annually reported variables. Annually or daily reported variables, among which there was no correlation, would be included in multivariate regression. Interaction terms of included variables would be included, if their effects on containing pandemic might be related. Then, multivariable analysis with spline terms was conducted to fit the number of cumulative COVID-19 cases at province level. In order to explore the possibility of different knots in eastern, central and western regions, four models were built based on data of eastern, central, western and all included provinces, respectively. The general model for k knots in an n degree polynomial regression was
 |
where Y was cumulative COVID-19 case number and X represented the number of days since 19 January 2020. The X values of the k knots were designated ti where i = 1,2…k. Since the number and location of spline knots were unknown, a series of dummy variables (Di) were created as follows:
where ti = 1,2,…,53. Linear (n = 1), quadratic (n = 2) and cubic (n = 3) adjustments were applied, respectively. Stepwise regression was used to select the degree of adjustment, knot locations and covariates. Variance inflation factor (VIF) was used to assess co-linearity. Adjusted R-square (R2) and Akaike information criterion (AIC) were used to evaluate the performance of the models. All the analysis was performed with Statistical Analysis System (SAS, version 9.4, SAS Institute).
Results
Characteristics of provinces out of Hubei
Data from 22 provinces in China were analysed in this study. As of 12 March 2020, the median of cumulative COVID-19 case number in the 22 provinces was 459 (IQR: 245–935), while Guangdong, Henan, Zhejiang and Hunan reached over 1000 cases (Fig. 1). Central provinces had a median of 962 cases, when the data for eastern and western provinces were 346 and 252, respectively (Table 1).
Fig. 1.
Cumulative number of COVID-19 cases for 22 provinces from 19 January 2020 to 12 March 2020.
Table 1.
Characteristics of provinces out of Hubei (median, inter-quartile range)
| All provinces (N = 22) | Eastern provinces (N = 11) | Central provinces (N = 6) | Western provinces (N = 5) | |
|---|---|---|---|---|
| COVID-19 case number | 459 (245−935) | 346 (168−760) | 962 (482−1018) | 252 (245−539) |
| Migration scale index from Hubei | 1.37 (0.88−3.45) | 1.20 (0.38,2.41) | 3.86 (0.68−10.09) | 2.35 (1.03−2.45) |
| BI | 1992.38 (1453.74−3348.19) | 2535.6 9(1757.19−4129.42) | 2083.22 (1463.47−2488.15) | 1441.95 (1367.21−1525.24) |
| Population ≤14 years old (thousand) | 814.94 (508.73−1269.42) | 729.09 (23 479−136 008) | 1105.93 (580.01−1269.42) | 766.80 (602.78−1098.50) |
| Population 15–64 years old (thousand) | 3163.50 (2476.80−5304.31) | 3138.48 (1649.96−5845.03) | 3741.26 (2939.17−4787.91) | 2832.31 (2476.80−3349.68) |
| Populaton ≥ 65 years old (thousand) | 456.02 (356.4−873.64) | 374.40 (269.25−891.61) | 639.33 (455.50−841.68) | 443.59 (428.90−477.82) |
| Male/female ratio (%) | 103.95 (101.90−108.30) | 103.50 (102.70−11 110 | 104.70 (103.80−108.30) | 101.90 (99.60−107.20) |
| Registered doctors per 1000 population | 157.05 (135.34−303.10) | 180.92 (154.62−303.10) | 153.02 (116.65−426.20) | 135.37 (135.31−156.85) |
| Registered nurses per 1000 population | 211.85 (196.81−233.15) | 232.75 (196.82−274.15) | 198.67 (184.73−208.97) | 224.97 (216.16−225.74) |
| Beds in infectious disease department per 1000 population | 8.44 (7.26−10.11) | 7.26 (6.53−9.80) | 9.23 (8.54−11.14) | 8.35 (7.38−10.11) |
| Public health professionals per 1000 population | 9.12 (7.61−11.31) | 8.39 (7.32−9.57) | 9.59 (8.55−10.09) | 11.87 (11.31−12.02) |
| Per capita GDP (Yuan) | 55 478.50 (47 712.00−91 197.00) | 91 197.00 (58 008.00−120 711.00) | 47 573.00 (45 328.00−50 152.00) | 48 883.00 (41 489.00−63 477) |
| Per capita health care expenditure (Yuan) | 1410.15 (1135.90−1704.80) | 1510.90 (1319.50−2390.00) | 1289.75 (1135.90−1424.00) | 1320.20 (1075.60−1471.90) |
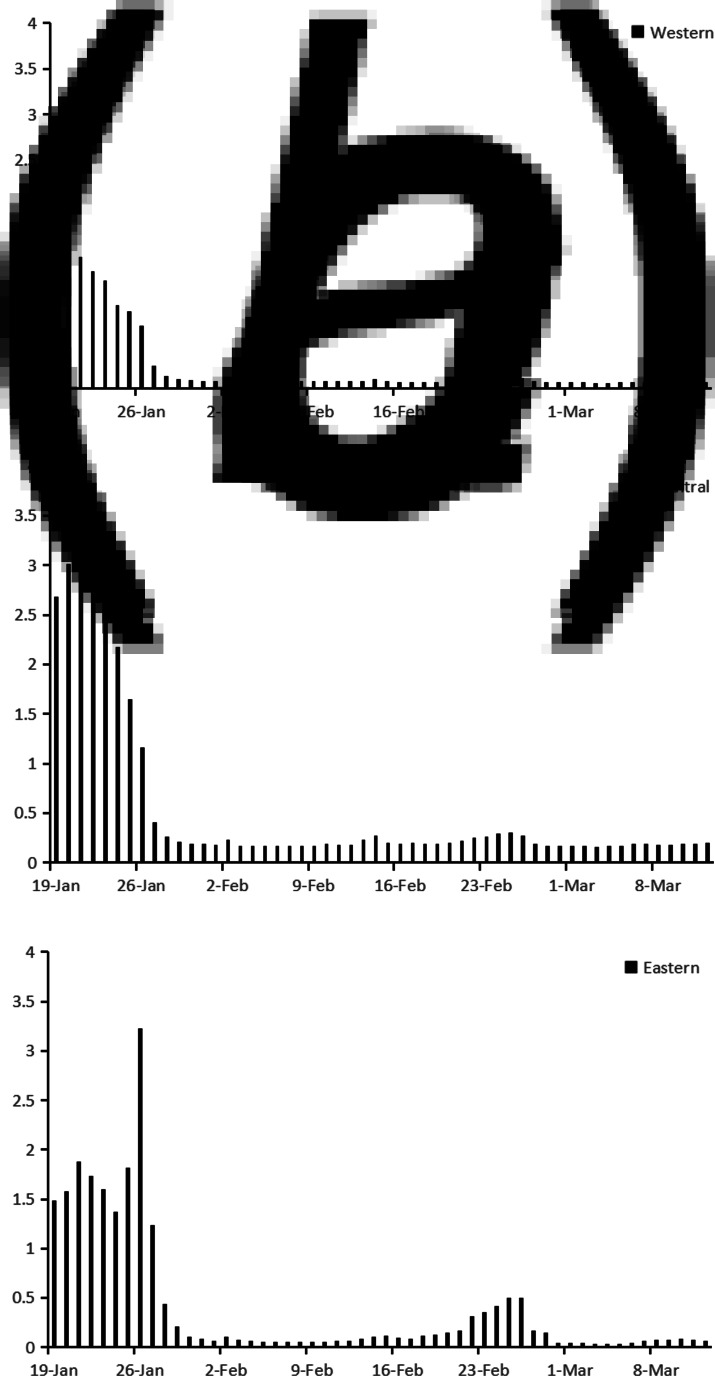
Migration scale index out of Hubei from 19 January to 12 March are shown in Figure 2. Before 23 January 2020, migration scale index out of Hubei was higher than 6, which was similar to that in 2019. On 24 January, the Chinese government locked down 14 cities in Hubei due to the quick spread of COVID-19, when migration scale index dropped to less than 5. In order to contain SARS-CoV-2 spreading further, the whole province was locked down before 27 January. Then, the index plunged to less than 1, but the data were experiencing an upward trend in 2019. Until 12 March, the index stayed at around 0.4, which was much lower than that in 2019. Figure 3 showed the change of migration scale index from Hubei to eastern, central and western provinces. The peak value of migration scale index was much lower in western provinces than that in eastern or central provinces, as well as the total migration scale (Table 1).
Fig. 2.
Migration scale index out of Hubei from 19 January 2019 to 12 March 2019 and from 19 January 2020 to 12 March 2020.
Fig. 3.
Migration scale index from Hubei to eastern, central or western province from 19 January 2020 to 12 March 2020.
BI from 19 January 2020 to 12 March is shown in Figure 4. Before 19 January, BI for COVID-19 was less than 10 000 in China. After that, it surged from 34 506 on 19 January to the top of 2 490 679 on 25 January. Then the index decreased gradually to around 500 000 at the end of February and fluctuated between 400 000 and 500 000 before 12 March. Among the eastern, central and western provinces, change patterns of BI were similar, but in western provinces the value of BI was lower (Fig. 4 and Table 1).
Fig. 4.
BI for COVID-19 from 19 January 2020 to 12 March 2020.
The annually reported data of eastern, central and western provinces were shown in Table 1. Medians of population by age groups were highest in central provinces, when sex ratios were similar among the three regions. With regard to public health resource per 1000 population, the medians of registered doctors and nurses were highest in eastern provinces, while the western provinces owned the highest median of public health professionals. With regard to economic status, eastern provinces had significantly higher per capita GDP and health care expenditure.
Correlation analysis
Pearson's correlation analysis was applied to migration scale index and BI, which showed significant correlation (rx,y = 0.4262, P < 0.0001). Spearman's rank-order correlation was conducted among annually reported variables. The results are shown in Table 2. Population ≤14 years old was significantly correlated with population of other two age groups and per capita health care expenditure. Population of 15–64 years old was significantly correlated with population ≥65 years old. As for variables related to public health resource, the number of registered nurses was significantly correlated with public health professional number. And the correlation between per capita GDP and per capita health care expenditure was significant, too. Therefore, daily and annually reported variables, except cumulative BI, population ≤14 years old, population of 15–64 years old, registered nurse and per capita health care expenditure, were included into multivariate regression. In addition, interaction items among public health professionals, registered doctors and beds in infectious department were included, because their roles and effects were related in preventing and controlling COVID-19 pandemic. Public health professionals and doctors both participated in epidemic investigation and COVID-19 testing, while doctors and beds in infectious disease department reflected the capacity of COVID-19 admissions.
Table 2.
Spearman's rank-order correlation analysis among annually reported variables (rx,y, sig.)
| Population 15−64 years old (thousand) | Population ≥ 65 years old (thousand) | Male/female ratio (%) | Registered doctors (for per thousand people) | Registered nurses (for per thousand people) | Beds in infectious disease department (for per thousand people) | Public health professionals (for per thousand people) | Per capita GDP (Yuan) | Health care per capita expenditure (Yuan) | |
|---|---|---|---|---|---|---|---|---|---|
| Population ≤14 years old (thousand) | 0.92707 <0.0001 |
0.83749 <0.0001 |
0.13920 0.5367 |
0.13721 0.5426 |
−0.39890 0.0659 |
−0.07166 0.7513 |
−0.37225 0.0880 |
−0.33810 0.1238 |
−0.47658 0.0249 |
| Population 15–64 years old (thousand) | 0.90493 <0.0001 |
0.15053 0.5037 |
0.09405 0.6772 |
−0.37894 0.0820 |
−0.05885 0.7948 |
−0.39004 0.0727 |
−0.15470 0.4918 |
−0.32455 0.1406 |
|
| Population ≥ 65 years old (thousand) | −0.12499 0.5794 |
0.11991 0.5950 |
−0.31983 0.1468 |
−0.03186 0.8881 |
−0.34391 0.1171 |
−0.13369 0.5531 |
−0.28436 0.1996 |
||
| Male/female ratio (%) | −0.19218 0.3916 |
−0.34767 0.1129 |
0.12035 0.5937 |
−0.33774 0.1242 |
0.05386 0.8118 |
−0.02515 0.9115 |
|||
| Registered doctors (for per thousand people) | 0.11405 0.6133 |
−0.15095 0.5025 |
0.15081 0.5029 |
−0.12448 0.5810 |
−0.19218 0.3916 |
||||
| Registered nurses (for per thousand people) | −0.23968 0.2827 |
0.97539 <0.0001 |
0.08504 0.7067 |
−0.04659 0.8369 |
|||||
| Beds in infectious disease department (for per thousand people) | −0.20387 0.3628 |
−0.264553 0.2342 |
0.00654 0.9770 |
||||||
| Public health professionals (for per thousand people) | −0.06181 0.7847 |
−0.13869 0.5382 |
|||||||
| Per capita GDP (Yuan) | 0.74027 <0.0001 |
||||||||
Regression splines
Spline regression model was applied to fit cumulative COVID-19 case number in eastern, central, western and all provinces, respectively. The results are shown in Table 3. Models with knots and covariates fitted the data better than the ones with knots only. No quadratic or cubic terms were included. In the model of all provinces, estimated knots were 8th and 24th days, which were similar with knots of eastern and central province models. But in the model of western provinces, knots were located at 7th and 31st days. As for covariates, migration scale index from Hubei was included in each model for eastern, central and western provinces, which was positively correlated with cumulative COVID-19 case number. Other included covariates were different among the three regions.
Table 3.
Spline regression of cumulative COVID-19 case number in eastern, central, western and all provinces
| Model | Variables | Estimates | s.e. | Adjusted R2 | AIC |
|---|---|---|---|---|---|
| Model 1a | D5 | 27.9 | 1.02 | 0.6596 | 13 721.5264 |
| D23 | −25.26 | 2.02 | |||
| Model 2b | D8 | 21.98 | 1.14 | 0.8702 | 12 581.3221 |
| D24 | −21.41 | 1.69 | |||
| Migration scale index from Hubei | 93.7 | 3.04 | |||
| Registered doctors | −0.09 | 0.009 | |||
| Registered nurses | −3.05 | 0.62 | |||
| Beds in infectious disease department | −8.11 | 1.45 | |||
| Populaton ≥ 65 years old | 0.12 | 0.02 | |||
| Model 3c | D4 | 21.65 | 1.09 | 0.6112 | 6897.3392 |
| D28 | −21.53 | 2.87 | |||
| Model 4d | D8 | 18.89 | 1.62 | 0.8537 | 6320.9008 |
| D24 | −17.87 | 2.42 | |||
| Migration scale index from Hubei | 116.29 | 4.61 | |||
| Public health professionals | −3.07 | 0.63 | |||
| Populaton ≥ 65 years old | 0.09 | 0.02 | |||
| Per capita GDP | −0.0004 | 0.0002 | |||
| Model 5e | D5 | 38.45 | 1.71 | 0.8099 | 3725.9779 |
| D25 | −36.69 | 3.71 | |||
| Model 6f | D8 | 37.82 | 1.75 | 0.9461 | 3320.5095 |
| D25 | −39.77 | 2.67 | |||
| Migration scale index from Hubei | 91.84 | 3.44 | |||
| Registered doctors | −0.08 | 0.009 | |||
| Public health professionals | −19.09 | 2.13 | |||
| Model 7g | D4 | 14.29 | 0.65 | 0.8025 | 2665.7809 |
| D29 | −14.67 | 1.80 | |||
| Model 8h | D7 | 8.54 | 0.63 | 0.9400 | 2352.1051 |
| D31 | −9.31 | 1.28 | |||
| Migration scale index from Hubei | 62.53 | 3.25 | |||
| Registered doctors | −0.28 | 0.04 | |||
| Population ≥ 65 years old | 0.1 | 0.01 |
Model with knots fitting cumulative COVID-19 case number in all provinces.
Model with knots and covariates fitting cumulative COVID-19 case number in all provinces.
Model with knots fitting cumulative COVID-19 case number in eastern provinces.
Model with knots and covariates fitting cumulative COVID-19 case number in eastern provinces.
Model with knots fitting cumulative COVID-19 case number in central provinces.
Model with knots and covariates fitting cumulative COVID-19 case number in central provinces.
Model with knots fitting cumulative COVID-19 case number in western provinces.
Model with knots and covariates fitting cumulative COVID-19 case number in western provinces.
Discussion
In this study, COVID-19 case number out of Hubei during first-level response was analysed with spline regression model. A stepwise procedure was used to select the number, location and degree of polynomial, as well as covariates. In order to explore the change patterns of COVID-19 case number in different regions, spline models were used to fit the data of eastern, central and western provinces, respectively. The research period was divided into three stages by two knots in all models, but the locations of knots were different in the three regions (Fig. 5).
Fig. 5.
Timeline of implemented measures in China and the three stages in eastern, central and western provinces.
The first stage was similar among the three regions, lasting from 19 January to around 26 January. In this stage, cumulative COVID-19 case number was associated with covariates, such as migration scale index out of Hubei, public health professionals and registered doctors, but not the number of days since 19 January. The daily situation reports of Guizhou, Tianjin and Shanghai, which released the exposure history of each COVID-19 case, provided an insight into this situation [25–27]. In the first 8 days of outbreak, imported cases mainly contributed to the increase of COVID-19 case number, taking a proportion of 50.0%~88.9%. In order to prevent case spilling over, Hubei province was gradually locked down since 23 January, which decreased the risk of case importation for other provinces. In the second stage, cumulative COVID-19 case number started to increase rapidly with time. Imported case proportion decreased, and indigenous case proportion surged, ranging from 43.7% to 73.5%. In this stage, SARS-CoV-2 spread among inhabitants and secondary infection cases were diagnosed extensively. The Chinese government took a combination of preventing and controlling measures to contain the pandemic. In eastern and central provinces, the growth slowed down since 11 or 12 February. However, in western provinces, it slowed down after 18 February. Cumulative COVID-19 case number of western provinces increased more slowly in the second stage, while eastern and central provinces experienced a sharper increase in a shorter second stage.
Previous studies mostly fitted the data of COVID-19 with regression models at national or global level. Ekum et al. [28] conducted hierarchical polynomial regression with daily cases of COVID-19 globally, which indicated cubic model fitted the data better than linear or quadratic models. Demertzis et al. [16] applied spline model and cubic model to the cumulative number of COVID-19 infections, deaths and ICU patients in Greece. In their study, spline models outperformed cubic ones with each outcome. Sousa et al. [15] and Agiwal et al. [14] fitted the daily reported COVID-19 cases of European, American and Asian countries with linear and cubic spline terms, identifying the knots of each country. However, change patterns might be different among various regions in a country. In this study, models with different knots and parameters were developed for eastern, central and western provinces, which showed the specific change patterns of COVID-19 among the three regions. Therefore, in addition to studies at global and national levels, analysis with province data was needed. The difference might be attributed to regional risk of case importation, local epidemiological features, applicability of preventing and controlling measures and public compliance. To reveal the cause of different change pattern at province level, studies with more detailed data on case characteristics, implementation of controlling measures and public behaviours were required.
Meanwhile, previous studies exploring the knots of COVID-19 case number did not include other explanatory variables. In this study, stepwise procedure was used to select knot number, locations and covariates. There were different systematic methods to estimate the number and locations of knots. Friedman [29] and Silverman et al. [30] discussed stepwise-based method, Osborne et al. [31] proposed an algorithm based on the LASSO estimator and Denison et al. [32] considered the bayesian method. All these methods were successful. Stepwise procedure allowed for any combination of adjustments (linear, quadratic and cubic) in each segment and took into account other explanatory variables at the same time. It provided the added utility of a simple, unconstrained function which can be easily implemented in non-linear trend analysis. This study showed the models with knots and covariates fitted the data better than the models with knots only. In addition to the segments of time, variance of cumulative COVID-19 case number was attributed to transient population from Hubei, population ≥65 years old and variables reflecting health resources at the province level. These findings were consistent with other studies' result. Chen's study showed migration scale index from Hubei was associated with confirmed COVID-19 cases per day in China except Hubei from 20 January to 2 February [33]. Data from seven countries, including Spain, Canada, Netherlands, Italy, Germany and Korean, revealed that older population with low immunity had higher risk of infection, taking 27%–58.1% of the confirmed cases [34–39]. A comparison analysis between COVID-19 and H1N1 outbreaks proved public health professionals and doctors played a crucial role in public health emergency response [40, 41]. These findings supported the assumption; spline regression models with other explanatory variables might provide better insight into the trend pattern of COVID-19 cases.
This study had several potential limitations. Firstly, the cumulative number of COVID-19 cases did not equal to the total number of infections due to unconfirmed cases. Asymptomatic cases might not be recognised due to the lack of symptoms and infected patients could ignore the mild symptoms at early stage resulting in delay to diagnosis. Secondly, the data extracted from the Chinese Health Statistical Year book was based on the latest available national survey finished in 2018, which might not match the medical resources and population characters during outbreak period completely. Thirdly, some covariates related to the spread of SARS-CoV-2, such as testing intensity, were not included in this study, because no corresponding public database were available.
Conclusion
This study analysed cumulative COVID-19 case number during the first-level response with spline regression models at province level out of Hubei. Inclusion of covariates made spline models fit COVID-19 data better. The research period was divided into three stages by two knots. The spline models of eastern, central and western provinces demonstrated different trend patterns in each region. Spline function with covariates would be a practical tool to analyse the non-linear trend of COVID-19 data. Analysis at province level was necessary to explore the change patterns of COVID-19 data in corresponding regions. To reveal more information about the regional characteristics of COVID-19 pandemic, studies with more detailed data at province level were needed. A better understanding of COVID-19 pandemic will help the policy makers to more effectively control the spread of SARS-CoV-2 and lessen the adverse social effect to a greater extent.
Author contributions
Chen Liang and Li Shen contributed equally to this work. They designed the experiment, collected the data, performed the analysis and wrote this paper. All authors read and approved the final paper.
Financial support
This research was not supported by any funding.
Ethical standards
Not applicable.
Conflict of interest
All authors declare no conflicts of interest relevant to this paper.
Data
The datasets used in this study is available from the corresponding author Chen Liang on reasonable request (Email: liangchen_sjtu@163.com).
References
- 1.Lu H, Stratton CW and Tang YW (2020) Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. Journal of Medical Virology 92, 401–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hui DS et al. (2020) The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – the latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases 91, 264–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 395, 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Na Z et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. The New England Journal of Medicine 382, 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Committee on Taxonomy of Viruses, ICTV. Naming the 2019 Coronavirus. Available at https://talk.ictvonline.org/information/w/news/1300/page (Aceessed 19 July 2020).
- 6.WHO. Novel Coronavirus(2019-nCoV) Situation Report-22. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_ Published 11 February 2020 (Accessed 19 July 2020).
- 7.WHO. Novel Coronavirus(2019-nCoV) Situation Report-163. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200701-covid-19-sitrep-163.pdf?sfvrsn=c202f05b_2 (Accessed 19 July 2020).
- 8.Jantien AB et al. (2020) Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travelers from Wuhan, China, 20−28 January 2020. Eurosurveillance 25, 2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qun L et al. (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. The New England Journal of Medicine 382, 1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiaowei X et al. (2020) Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. British Medical Journal 368, m792. Published 2020 Feb 27. [DOI] [PubMed] [Google Scholar]
- 11.WHO. Novel Coronavirus(2019-nCoV) Situation Report-7. Available at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200127-sitrep-7-2019--ncov.pdf?sfvrsn=98ef79f5_2 Published 27 January 2020 (Accessed 19 July 2020).
- 12.Nanshan C et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (London, England) 395, 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dawei W et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. The Journal of the American Medical Association 323, 1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agiwal V et al. (2020) Study the trend pattern in COVID-19 using spline-based time series model: a bayesian paradigm. Preprints 2020, 2020070306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sousa ARDS et al. (2020) Model selection criteria for regression models with splines and the automatic localization of knots. arXiv, 2006.02649. Available at http://arxiv.org/abs/2006.02649 (Accessed 7 September 2020). [Google Scholar]
- 16.Demertzis K et al. (2020) Modeling and forecasting the COVID-19 temporal spread in Greece: an exploratory approach based on complex network defined splines. International Journal of Environmental Research and Public Health 17, 4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marsh LC (1986) Estimating the number and location of knots in spline regressions. Journal of Applied Business Research 2, 60–70. [Google Scholar]
- 18.Xianxi Map. Available at http://qianxi.baidu.com/ Published January 2020 (Accessed 19 July 2020).
- 19.Yuan ZM et al. (2020) A simple model to assess Wuhan lock-down effect and region efforts during COVID-19 epidemic in China Mainland. MedRxiv, 2020.02.29.200229561. doi: 10.1101/2020.02.29.20029561. [DOI] [Google Scholar]
- 20.Baidu Index. Available at http://zhishu.baidu.com (Accessed 19 July 2020).
- 21.Search Engine Market Share China (Jan−Dec 2019). Available at https://gs.statcounter.com/search-engine-market-share/all/china/2019 (Accessed 19 July 2020).
- 22.Chinese National Municipal Health Commission (2019) Chinese Health Statistical Yearbook 2019. Dongdan 3rd, Dongcheng, Beijing, China: Peking Union Medical College Press. [Google Scholar]
- 23.Sun P et al. (2020) Understanding of COVID-19 based on current evidence. Journal of Medical Virology 92, 548–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bulut C and Kato Y (2020) Epidemiology of COVID-19. Turkish Journal of Medical Sciences 50, 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Health Commission of Guizhou. Available at http://www.gzhfpc.gov.cn/xwzx_500663/tzgg/ (Accessed 19 July 2020).
- 26.Health Commission of Tianjin. Available at http://wsjk.tj.gov.cn/col/col87/index.html (Accessed 19 July 2020).
- 27.Health Commission of Shanghai. Available at http://wsjkw.sh.gov.cn/xwfb/index.html (Accessed 19 July 2020).
- 28.Ekum M and Ogunsanya A (2020) Application of hierarchical polynomial regression models to predict transmission of COVID-19 at global level. International Journal of Clinical Biostatistics and Biometrics 6, 027. [Google Scholar]
- 29.Friedman JH (1991) Multivariate adaptive regression splines. Annals of Statistics 19, 1–67. [Google Scholar]
- 30.Friedman JH and Silverman BW (1989) Flexible parsimonious smoothing and additive modeling. Technometrics 31, 3–21. [Google Scholar]
- 31.Osborne MR, Presnell B and Turlach BA (1998) Knot selection for regression splines via the lasso. Computing Science and Statistics 30, 44–49. [Google Scholar]
- 32.Denison DGT, Mallick BK and Smith AFM (1998) Automatic Bayesian curve fitting. Journal of the Royal Statal Society: Series B (Statal Methodology 60, 333–350. [Google Scholar]
- 33.Chen H et al. (2020) Correlation between the migration scale index and the number of new confirmed novel coronavirus pneumonia cases in China. Epidemiology and Infection 148, e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Actualización no 67. Enfermedad por el coronavirus (COVID-19). Available at https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Actualizacion_67_COVID-19.pdf (Accessed 19 July 2020).
- 35.Age distribution of COVID-19 cases (n = 5,261) in Canada. Available at https://www.canada.ca/en/public health/services/diseases/2019-novel-coronavirus-infection/health-professionals/epidemiological-summary-covid-19-cases.html#a3 (Accessed 19 July 2020).
- 36.Epidemiologische situatie COVID-19 in Nederland 3 april 2020. Available at https://www.rivm.nl/documenten/epidemiologische-situatie-covid-19-in-nederland-3-april-2020 (Accessed 19 July 2020).
- 37.Integrated surveillance of COVID-19 in Italy. Available at https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_6aprile%20ENG.pdf (Accessed 19 July 2020).
- 38.Coronavirus disease 2019 (COVID-19) daily situation report of the Robert Koch Institute 06/04/2020-updated status for Germany. Available at https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-06-en.pdf?__blob=publicationFile (Accessed 19 July 2020).
- 39.Korean Society of Infectious Diseases et al. (2020) Report on the epidemiological features of Coronavirus Disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. Journal of Korean Medical Science 35, e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang Q et al. (2020) Characteristics of and public health emergency responses to COVID-19 and H1N1 outbreaks: a case-comparison study. International Journal of Environmental Research and Public Health 17, 4409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murthy BP et al. (2017) Progress in public health emergency preparedness − United States, 2001−2016. American Journal of Public Health 107, S180–S185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used in this study is available from the corresponding author Chen Liang on reasonable request (Email: liangchen_sjtu@163.com).