Abstract
Background
The COVID-19 pandemic has resulted in radical changes in the delivery of healthcare worldwide. Our oncology service (at an Irish national cancer centre) rapidly transitioned to the use of telemedicine or virtual clinics (VC) to minimise potential risk of exposure to COVID-19 amongst an immunosuppressed, high-risk population. Our study aimed to evaluate the use of VC in this setting.
Methods
An 18-point questionnaire was designed to investigate the patient experience of VC during the COVID-19 pandemic in Ireland and compliance with guidelines developed in Ireland to conduct VC and the role of VC in the future. Questionnaires were distributed following the receipt of verbal consent from patients during the VC. Descriptive statistics were utilised for data analysis using SPSS®.
Results
One hundred and four patients returned completed surveys (n = 104/164, 63% response rate). Overall satisfaction levels were high with most patients (n = 58/100, 58%; no answer provided (NAP), n = 4) equally satisfied or nearly equally satisfied with VC in comparison to a usual clinic encounter. The majority of patients felt that there should be a role for VC in the future (n = 84/102, 82%; NAP, n = 2). The majority of patients (n = 61/99, 61%; NAP, n = 5) were very relieved to avoid a hospital visit due to perceived risk of potential exposure to COVID-19.
Conclusion
The majority of oncology patients were satisfied with a VC encounter. VC may have a role in the future of medical care in Ireland post the COVID-19 pandemic.
Keywords: COVID-19, Oncology, Virtual clinics
Introduction
The COVID-19 pandemic has placed unprecedented demands on healthcare services worldwide and has necessitated rapid changes in how healthcare is delivered [1, 2]. Clinicians have been asked to balance the risk to benefit ratio of diagnostics, therapeutics and in-person reviews. Balancing these benefits and risks for patients with cancer poses unique challenges. Clinicians need to minimise risk of infection for this vulnerable population while continuing their cancer treatment. National guidelines have been rapidly developed and shared with broad advice on minimising spread of COVID-19, how and when to screen and test for the virus and support for rationalising routine hospital visits where possible [3, 4]. It is evident that stringent infection prevention and control measures will need to be incorporated into the delivery of healthcare for the foreseeable future. In our hospital and others, this includes the provision of adequate physical distancing for our patients and staff wherever possible with ensuing restructuring of clinics. Due to the recent resurgence of COVID-19 in Ireland, healthcare practices need to be flexible to accommodate fluctuating demands and minimise infection risk [5]. Guidelines issued by the National Cancer Control Programme (NCCP) in conjunction with the HSE recommend that VC are conducted with access to patient notes. They also recommend that the doctor confirms at least two details of the patient, that the doctor explains the advantages and disadvantages of VC and that they verbally consent patients for the VC [3, 4].
The Mater Misericordiae University Hospital is a National Cancer Control Programme-designated cancer centre that provides tertiary medical oncology services. In an average week, the hospital accommodates approximately 150 clinic appointments and 300 systemic anti-cancer treatment (SACT) appointments to ambulatory patients. Virtual clinics (VC) or telemedicine have been introduced for medical oncology outpatient clinics in the Mater Hospital since March 2020.
Clinics are prepared in advance of scheduled appointments and patients deemed suitable for virtual review are called in advance of their scheduled outpatient appointment via phone. Video conferencing software has been not utilised widely at our institution to date; efforts are under way both locally and nationally to improve clinician access to video conferencing facilities [5]. If clinical issues arise in the course of the consultation warranting an in-person review, an appointment is arranged. During the period of March to June of 2020, an in-person clinical appointment was provided to a minority (approximately 20-40%) of oncology patients at our hospital where, in the opinion of the supervising physician, such a review is deemed clinically essential. Guidelines have been developed to assist clinicians in conducting safe and clinically useful VC [4, 6, 7]. These include verification of patient with at least two identifiers, patient acknowledgement of the limitations of VC, availability of complete medical record and provision of correspondence to the patient’s general practitioner following the VC.
Virtual clinics may provide certain advantages for patients including the ability to avoid the hospital and associated risks of contamination with infection and reduced travel costs; however, we hypothesized that patients might miss in-person interaction with their physician, in particular if they were receiving difficult or upsetting information.
Traditionally, oncology clinics have been conducted in-person often with family members present. There is limited evidence describing the patient experience of VC in oncology in the pre-COVID era [8]. Furthermore, the patient experience of VC in oncology during the COVID-19 pandemic is unknown. The purpose of this study was to gauge patient experience of VC in oncology conducted during the COVID-19 pandemic, to assess compliance with NCCP guidelines on VC and to explore the potential role for the use of VC beyond the pandemic. We hypothesised that the majority of patients would be equally satisfied or nearly equally satisfied with their VC encounter in comparison to previous experience of a face-to-face visit.
Methods
This study was approved by our local audit/service evaluation committee. A survey was designed to assess the patient experience of VC which included age category of patient, phase in treatment plan (active/follow-up), consent process of doctor, experience of the absence of a physical examination, relief at avoiding a hospital visit, experience of a hospital appointment at home, the use of VC beyond the COVID-19 pandemic and overall patient satisfaction (see Table 1).
Table 1.
Questions and associated objectives
| Objective | Question | |||
|---|---|---|---|---|
| Q1 | Demographic details |
Which of the following categories are you in? Please mark all that apply. < 35, 35-65, > 65, on active treatment, not on active treatment but on follow-up |
||
| Q2 | Compliance with NCCP guidelines | When the doctor called you for the ‘virtual clinic’, did s/he confirm two or more of your personal details? E.g. name, date of birth, address | ||
| Yes, two or more | No, one | No, none at all | ||
| Q3 | Compliance with NCCP guidelines | When the doctor called you for ‘virtual clinic’, did s/he explain the advantages and disadvantages of being reviewed over the phone compared to in person? | ||
| Yes | No | |||
| Q4 | Compliance with NCCP guidelines | When the doctor called you for ‘virtual clinic’, did s/he ask for your permission to review you over the phone? | ||
| Yes | No | |||
| Q5 | Patient experience of VC |
How did you feel about not having a physical examination at the time of your review with the doctor? Please rank on a scale of 1–5, 5 being extremely bothered about not being examined, 1 being not bothered at all. |
||
| Q6 | Patient experience of VC |
Did you miss having eye contact with your doctor? Please rank on a scale of 1–5, 5 being missed it a lot, 1 being did not miss it at all. |
||
| Q7 | Patient experience of VC |
How did you feel about avoiding a hospital visit given the current circumstances in particular the risk of infection with COVID-19? Please rank on a scale of 1-5, 5 being very relieved to avoid the visit and 1 being not relieved at all. |
||
| Q8 | Patient experience of VC |
How did you feel about avoiding a hospital visit to avoid the cost and time savings associated with the travel to hospital? Please rank on a scale of 1-5, 5 being very relieved to avoid the visit and 1 being not relieved at all. |
||
| Q9 | Patient experience of VC |
How did you feel about the doctor not being able to show you your scan results on the computer? Please rank on a scale of 1–5, 5 being extremely bothered by not being able to see the scan, 1 being not bothered at all. |
||
| Q10 | Patient experience of VC | Did you receive good or bad news during your virtual clinic? | ||
| Good | Bad | |||
| Q10b | Patient experience of VC | If you received bad news during your phone/video clinic, were you more comfortable to be in your home rather than hospital? Please rank on a scale of 1-5, 5 being more comfortable and 1 being much less comfortable. | ||
| Q11 | Patient experience of VC | How comfortable did you feel discussing symptoms over the phone? Please rank on a scale of 1-5 how comfortable you were, 5 being very comfortable, 1 being not comfortable at all. | ||
| Q12 | Patient experience of VC | Were you concerned that a family member might hear your conversation with the doctor? Please rank on a scale of 1-5 how concerned you were about the above, 5 being very concerned and 1 being not concerned at all. | ||
| Q13 | Patient experience of VC |
Did you feel in any way rushed by the doctor on the phone? Please rank on a scale of 1-5, 5 meaning feeling very rushed and 1 being not rushed at all. |
||
| Q14 | Patient experience of VC | Have you had any experience being called by a doctor via video call? | ||
| Yes | No | |||
| Q15 | Role of VC in the future | Following the COVID-19 crisis, do you think there should be a role for phone/video clinics? | ||
| Yes | No | |||
| Q15b | Role of VC in the future | If yes to the above, would you like to have the choice of attending in person or having a ‘virtual’ visit? | ||
| Yes – I would like the choice. | No – I would like my doctor to decide if I would be best suited to a phone/video call. | |||
| Q16 | Patient experience of VC |
In contrast to a regular outpatient clinic encounter, how satisfied have you been by the experience of phone/video clinic encounters? Please rank on a scale of 1-5, 5 being equally satisfied to a face-to-face encounter, 1 being not satisfied at all. |
||
The survey was designed with the input of all the practicing medical oncologists at our institution. It included 18 questions with 10 of those questions including a 5-point Likert scale customised for each question [9]. This questionnaire has not been validated. There were no any validated questionnaires designed to address the purposes of this study available at the time of the study design, nor is there now to the best of the authors’ knowledge.
At the time of virtual clinic review, patients were invited to participate in the survey. If patients consented, they chose to participate via e-mail invitation or postal. An electronic or paper survey was distributed with a pre-paid return envelope included. Inclusion criteria were as follows: recent attendance at virtual medical oncology clinic, English as first language and voluntary consent to participation.
Patients were invited to participate over a 7-week period from the 27th of April until the 12th of June 2020. Data cut-off was the 3rd of July 2020. Electronic and paper results were collated. SPSS ® statistics was used for descriptive statistics and significance testing. Descriptive statistics were used to present results. A p value of less than 0.05 was considered significant in formal testing. In a post hoc analysis, a Chi-square test and a Mann-Whitney U test were used to compare results for under and over 65 s
Results
A total of 164 patients declared an interest in participating in the survey and 104 completed surveys were returned representing a response rate of 63%.
Patients were within the following age categories: over 65 (n = 43/103, 42%); 35-65 (n = 40/103, 39%); < 35 (n = 20/103, 20%); and no answer provided (NAP) (n = 1). The majority of patients were on follow-up (n = 61/92, 66%) with a minority of patients on active treatment (n = 31/92, 34%) and the remainder provided no answer (n = 12). Follow-up refers to any patients who is not on active treatment. This may also include patients with advanced disease who are currently under surveillance. Active treatment pertains only to treatments which require day-ward attendance (this was clarified for patients in the questionnaire).
Compliance with NCCP guidelines (questions 2-4, see Table 1)
The vast majority of patients (n = 78/103, 76%, NAP; n = 1) recalled being asked to confirm at least one personal identifier prior to proceeding with the VC. Most consultations (n = 79/103, 77%, NAP, n = 1) involved a discussion of the advantages and disadvantages of a virtual clinic review. Almost all consultations (n = 98/102, 96%, NAP; n = 2) included consent from the patient for the virtual review to be conducted over the phone.
Patient experience of VC (questions 5-14, 16, see Table 1)
The majority of patients were very relieved to avoid a hospital visit due to the perceived risk of contamination with COVID-19 (n = 61/99, 62%, NAP; n = 5) with only a small minority not relieved at all by this (n = 4/99, 4%, NAP; n = 5). Almost one-third of patients (n = 32/103, 31%, NAP; n = 1) were very relieved to avoid a hospital visit due to the cost and time savings; however, some patients (n = 24/103, 23%, NAP; n = 1) were not relieved by this at all. Two-thirds of patients (n = 67, 67%, NAP; n = 4) felt that they were very comfortable discussing symptoms over the phone, and most patients (n = 74, 74%, NAP; n = 4) had no concerns that their family at home may overhear their consultation. Less than half of patients (n = 36/98, 37%, NAP; n = 6) were not bothered at all by not being examined by a doctor. Only a small minority (n = 13/98, 13 %, NAP; n = 6) of patients were extremely bothered by this. Over one-third (n = 36/98, 37%, NAP; n = 6) of patients did not miss eye contact at all and only a few patients (n = 14/98, 14%, NAP; n = 6) were extremely bothered by this. Almost half (n = 45/102, 44%, NAP; n = 2) of patients were not bothered at all by not being able to review their scan results on the computer and with just a small minority (n = 12/102, 12%, NAP; n = 2) of patients were extremely bothered by this. The majority of our patients (n = 88/100, n = 88%, NAP; n = 4) felt in no way rushed by the doctor on the phone. Only a small minority of patients (n = 7/100, n = 7%, NAP; n = 4) experienced bad news in virtual clinic. Even less patients (n = 4/100, 4%, NAP; n = 4) experienced virtual clinic with the assistance of video conferencing software.
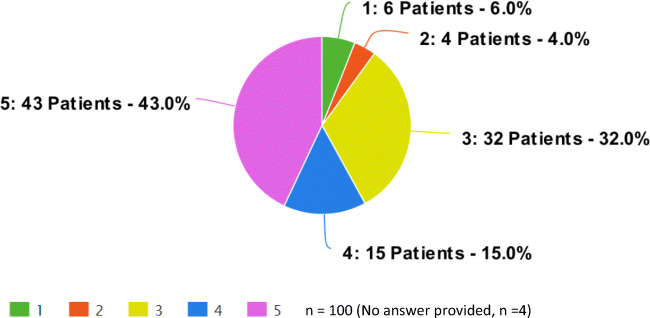
Patients were asked how satisfied they were by the virtual clinic experience in contrast to a regular clinic encounter (see Fig. 1). They were asked to rank their encounter on a scale of 1–5, 5 being equally satisfied to a face-to-face encounter, 1 being not satisfied at all. The results were as follows: rank of 5 (n = 43/100, 43%); rank of 4 (n = 15/100, 15%); rank of 3 (n = 32/100, 32%); rank of 2 (n = 4/100, 4%) and rank of 1 (n = 6/100, 6%); NAP (n = 4). Patients on active treatment were more likely to be equally satisfied; rank of 5 (n = 17/31, 55%); rank of 4 (n = 2/31, 6%); rank of 3 (n = 10/31, 32%); rank of 2 (n = 0) and rank of 1 (n = 2/31, 6%). Amongst patients on follow-up, patients were less likely to be equally satisfied; 5 (n = 26/61, 43%); rank of 4 (n = 13/61, 21%); rank of 3 (n = 22/61, 36%); rank of 2 (n = 4/61, 6%) and rank of 1 (n = 4/61, 6%).
Fig. 1.
Question 16. In contrast to a regular outpatient clinic encounter, how satisfied have you been by the experience of phone/video clinic encounters? Please rank on a scale of 1-5, 5 being equally satisfied to a face-to-face encounter, 1 being not satisfied at all
Role for VC in the future (question 16, see Table 1)
The vast majority of patients (n = 84/102, 82%, NAP; n = 2) felt there should be a role for VC following the COVID-19 pandemic. In that event, over two-thirds of patients (n = 58/83, 70%, NAP/not applicable; n = 21) would like their doctor to decide if their consultation was appropriate to be conducted via phone with the remainder preferring to have the choice themselves (n = 25/83, 30%, NAP/not applicable; n = 21).
Although subgroups were small, there were no significant differences between patients over and under 65 with regard to overall satisfaction (Mann-Whitney U test, p = 0.47), relief at avoiding a hospital visit (Mann-Whitney U test, p = 0.48) and the role of VC in the future of oncology clinics (χ2 = 0.3, p = 0.58) (see Tables 2 and 3).
Table 2.
Questions 5, 7 and 8
| n = 104 | 1 | 2 | 3 | 4 | 5 | No answer provided |
|---|---|---|---|---|---|---|
| Q5 |
How did you feel about not having a physical examination at the time of your review with the doctor? Please rank on a scale of 1–5, 5 being extremely bothered about not being examined, 1 being not bothered at all. |
|||||
| 36 (37%) | 11 (11%) | 33 (33%) | 5 (5%) | 13 (13%) | 6 | |
| Q7 |
How did you feel about avoiding a hospital visit given the current circumstances in particular the risk of infection with COVID-19? Please rank on a scale of 1-5, 5 being very relieved to avoid the visit and 1 being not relieved at all. |
|||||
| 4 (4%) | 9 (9%) | 13 (13%) | 12 (12%) | 61 (62%) | 5 | |
| Q8 |
How did you feel about avoiding a hospital visit to avoid the cost and time savings associated with the travel to hospital? Please rank on a scale of 1-5, 5 being very relieved to avoid the visit and 1 being not relieved at all. |
|||||
| 24 (23%) | 10 (10%) | 25 (24%) | 12 (12%) | 32 (31%) | 1 | |
Table 3.
Under and over 65 s
|
Over 65 s – n = 43 Under 65 s – n = 60 |
||||||
| Q7 |
How did you feel about avoiding a hospital visit given the current circumstances in particular the risk of infection with COVID-19? Please rank on a scale of 1-5, 5 being very relieved to avoid the visit and 1 being not relieved at all. |
|||||
| 1 | 2 | 3 | 4 | 5 | No answer provided | |
| Over 65 s | 1 (2%) | 2 (5%) | 14 (34%) | 5 (12%) | 19 (46%) | 2 |
| Under 65 s | 5 (8%) | 3 (5%) | 17 (29%) | 10 (18%) | 25 (44%) | 3 |
| p = 0.46 (Mann-Whitney U test) | ||||||
| Q8 | Following the COVID-19 crisis, do you think there should be a role for phone/video clinics? | |||||
| Yes | No | No answer provided | ||||
| Over 65 s | 32 (80%) | 8 (20%) | 3 | |||
| Under 65 s | 50 (83%) | 10 (17%) | 0 | |||
| χ2 = 0.3, p = 0.58 | ||||||
| Q16 |
In contrast to a regular outpatient clinic encounter, how satisfied have you been by the experience of phone/video clinic encounters? Please rank on a scale of 1-5, 5 being equally satisfied to a face-to-face encounter, 1 being not satisfied at all. |
|||||
| 1 | 2 | 3 | 4 | 5 | No answer provided | |
| Over 65 s | 2 (5%) | 1 (2%) | 14 (34%) | 4 (10%) | 20 (49%) | 2 |
| Under 65 s | 4 (7%) | 3 (5%) | 16 (28%) | 11 (19%) | 24 (41%) | 2 |
| p = 0.47 (Mann-Whitney U test) | ||||||
Discussion
Our study is the first, to the best of our knowledge, to describe the oncology patient experience of VC during the COVID-19 pandemic. It also provides the first experience of Irish patients of VC during the COVID-19 pandemic. Overall patient satisfaction levels with VC were high.
The majority of our patients were relieved at avoiding a hospital visit (mostly not only due to perceived risk of increased potential exposure to infection, but also due to time and cost savings). Contrary to our expectations, the majority of patients were not concerned at some of the practical difficulties of conducting virtual clinics. These include missing eye contact, the absence of a physical examination, not being able to review scans visually, discussing symptoms over the phone and discussing symptoms in the presence of their family. These results suggest that there may be opportunity to explore the role of VC beyond the pandemic. It is particularly encouraging that many of these disadvantages could be overcome with the use of video conferencing software.
We discovered that the patients over 65 s were equally satisfied with their VC experience and equally likely to recommend the use of VC in the future. Additionally, older patients were also not more likely to be relieved at avoiding a hospital visit compared to younger patients.
The overall high satisfaction level amongst patients is consistent with previous work in tele-oncology. Two early studies from the USA concluded that patient satisfaction levels were high [10–12]. Tele-oncology was initially designed to minimise travel time and costs as opposed to infection risk. This high satisfaction in our study is despite this policy being implemented rapidly without patient consultation, without patient choice in the matter and without access to video conferencing software. With ever-increasing subspecialisation in medicine, telemedicine may allow access to speciality services at significant distances including telegenetics, telepathology, remote chemotherapy supervision and clinical trial enrolment [8, 13–16]. Patient satisfaction may be improved in the future with access to video conferencing software and utilising the above more modern applications of teleoncology. Teleoncology has been demonstrated to be cost-effective [17, 18]. A recent study demonstrated that patients save, on average over $300,000, over the course of their treatment [18]. In Ireland, the travel costs may not be so significant but it does highlight the issue on a global scale. A PubMed search revealed no other studies which investigated patient experience of VC in oncology during the COVID-19 pandemic. However, high patient satisfaction levels (90%) were identified amongst patients who attended orthopaedic outpatient appointments during the COVID-19 pandemic [19].
Our study has several limitations. This was a selected population of patients felt to be suitable for a virtual clinic assessment. No new patients were included and the vast majority of patients receiving challenging results were not included in the study as they were invited by their physician for an in-person review. Significantly, the study questionnaires were distributed and completed during the initial wave of COVID-19 in Ireland and at this time the country was in the early phase of national restrictions which included a policy of ‘cocooning’ for at-risk patient populations (such as all those with active cancer) [20]. It is possible that patient opinion may change over the coming months or at a time of perceived lower risk of exposure to COVID-19. The majority of patients are satisfied with their VC experience. While satisfaction levels are high, patients are divided in their level of satisfaction and how they would ideally like a VC to be conducted.
Our research informs us that we need to tailor our clinical visits to each individual patient. While a majority of patients were satisfied with their encounter, a significant minority were not. Additionally, some patients did miss eye to eye contact and physical examination. Future work could focus on collecting more clinical data to identify patients who may benefit from VC. For example, patients with a history of breast cancer may be more appropriate to attend a face-to-face visit to allow for clinical examination. Clinicians and patients need to work in a collaborative manner to decide on the most appropriate patient, clinician and clinical appointments that are suitable for VC. We also learned that only a very small proportion of patients had experienced video consultations which may enhance the patient experience. Clinicians should work with stakeholders within their organisation to ensure adequate access to IT infrastructure. Future work could focus on evaluating more complex outcomes of care including quality, appropriateness, sustainability and the impact of VC on patient outcomes.
The findings of our study encourage the further development and utilisation of VC for oncology patients during and beyond the COVID-19 crisis. Telehealth solutions should continue to evolve to best accommodate individual patient, clinician and cultural needs. The recent resurgence of COVID-19 infection in Ireland means many services will return to VC, and it is paramount that we continue to optimise the patient experience at this challenging time for our patients.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bai G, Zare H. Hospital cost structure and the implications on cost management during COVID-19. J Gen Intern Med. 2020;35:2807–2809. doi: 10.1007/s11606-020-05996-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anoushiravani AA, O’Connor CM, DiCaprio MR, Iorio R. Economic impacts of the COVID-19 crisis: an orthopaedic perspective. J Bone Joint Surg Am. 2020;102:937–941. doi: 10.2106/JBJS.20.00557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Cancer Control Programme (2020) NCCP advice for Medical Professionals on the management of patients undergoing Systemic Anti-Cancer Therapy (chemotherapy) in response to the current novel coronavirus (COVID-19) pandemic. Dublin
- 4.National Health Service (2020) Clinical guide for the management of remote consultations and remote working in secondary care during the coronavirus pandemic. London
- 5.Health Service Executive (2020) Virtual health. In: April. https://healthservice.hse.ie/staff/coronavirus/working-from-home/virtual-health/virtual-health.html. Accessed 1 Jul 2020
- 6.Scheduled Care Transformation Programme Group H (2020) Procedure for the management of virtual outpatient clinics. Dublin
- 7.State Claims Agency Providing Telehealth:Virtual Sessions. Dublin
- 8.Liu R, Sundaresan T, Reed ME, et al. Telehealth in oncology during the COVID-19 outbreak: bringing the house call back virtually. JCO Oncol Pract. 2020;16:289–293. doi: 10.1200/OP.20.00199. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan GM, Artino AR., Jr Analyzing and interpreting data from likert-type scales. J Grad Med Educ. 2013;5:541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mair F, Whitten P, May C, Doolittle GC. Patients’ perceptions of a telemedicine specialty clinic. J Telemed Telecare. 2000;6:36–40. doi: 10.1258/1357633001933925. [DOI] [PubMed] [Google Scholar]
- 11.Allen A, Hayes J. Patient satisfaction with teleoncology: a pilot study. Telemed J. 1995;1:41–46. doi: 10.1089/tmj.1.1995.1.41. [DOI] [PubMed] [Google Scholar]
- 12.Doolittle GC, Allen A. Practising oncology via telemedicine. J Telemed Telecare. 1997;3:63–70. doi: 10.1258/1357633971930869. [DOI] [PubMed] [Google Scholar]
- 13.Baquet CR, Henderson K, Commiskey P, Morrow JN. Clinical trials: the art of enrollment. Semin Oncol Nurs. 2008;24:262–269. doi: 10.1016/j.soncn.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jhaveri D, Larkins S, Kelly J, Sabesan S. Remote chemotherapy supervision model for rural cancer care: perspectives of health professionals. Eur J Cancer Care (Engl) 2016;25:93–98. doi: 10.1111/ecc.12309. [DOI] [PubMed] [Google Scholar]
- 15.Galsky MD, Shahin M, Jia R, et al. Telemedicine-enabled clinical trial of metformin in patients with prostate cancer. JCO Clin cancer informatics. 2017;1:1–10. doi: 10.1200/CCI.17.00044. [DOI] [PubMed] [Google Scholar]
- 16.Sirintrapun SJ, Lopez AM (2018) Telemedicine in cancer care. Am Soc Clin Oncol Educ B 540–545. 10.1200/EDBK_200141 [DOI] [PubMed]
- 17.Monypenny R, Associate A, Olver I, et al. Cost savings from a telemedicine model of care in northern Queensland. Australia. 2013;199:414–417. doi: 10.5694/mja12.11781. [DOI] [PubMed] [Google Scholar]
- 18.Thota R, Gill DM, Brant JL, et al. Telehealth is a sustainable population health strategy to lower costs and increase quality of health care in rural Utah. JCO Oncol Pract. 2020;16:e557–e562. doi: 10.1200/JOP.19.00764. [DOI] [PubMed] [Google Scholar]
- 19.Gilbert AW, Billany JCT, Adam R, et al. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020;9:e000985. doi: 10.1136/bmjoq-2020-000985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Health IG (2020) Guidance on cocooning to protect people over 70 years and those extremely medically vulnerable from COVID-19 -updated guidance from 29 June. https://www.gov.ie/en/publication/923825-guidance-on-cocooning-to-protect-people-over-70-years-and-those-extr/. Accessed 23 Jul 2020