Abstract
Rift Valley fever virus (RVFV) is a mosquito-borne bunyavirus that is pathogenic to ruminants and humans. The virus is endemic to Africa and the Arabian Peninsula where outbreaks are characterized by abortion storms and mortality of newborns, particularly in sheep herds. Vector competence experiments in laboratory settings have suggested that over 50 mosquito species are capable of transmitting RVFV. Transmission of mosquito-borne viruses in the field is however influenced by numerous factors, including population densities, blood feeding behavior, extrinsic incubation period, longevity of vectors, and viremia levels in vertebrate hosts. Animal models to study these important aspects of RVFV transmission are currently lacking. In the present work, RVFV was transmitted to European (Texel-swifter cross-breed) lambs by laboratory-reared Aedes aegypti mosquitoes that were infected either by membrane feeding on a virus-spiked blood meal or by feeding on lambs that developed viremia after intravenous inoculation of RVFV. Feeding of mosquitoes on viremic lambs resulted in strikingly higher infection rates as compared to membrane feeding. Subsequent transmission of RVFV from lamb to lamb by infected mosquitoes was highly efficient in both models. The animal models described here can be used to study mosquito-mediated transmission of RVFV among the major natural target species and to evaluate the efficacy of vaccines against mosquito-mediated RVFV infection.
Subject terms: Biological techniques, Ecology, Microbiology, Diseases, Pathogenesis
Introduction
Rift Valley fever virus (RVFV) is a mosquito-borne RNA virus that causes severe disease in ruminants and humans1. The virus is transmitted via mosquitoes, predominantly of the genera Aedes and Culex2. Sheep are the most susceptible species, with disease being most severe in young lambs. RVFV has a tropism for the liver, with replication in hepatocytes resulting in focal to widespread hepatic necrosis3,4. In severe cases, hepatic necrosis is associated with bleeding tendencies, shock and death. In pregnant ewes, RVFV also targets maternal epithelial cells of the placenta and fetal trophoblasts, resulting in severe placental pathology and abortion5. Heavy mortalities among newborn lambs and abortion storms are key characteristics of RVF outbreaks. Infection of humans generally manifests as a self-resolving febrile illness, whereas a small percentage of patients develop encephalitis or hemorrhagic fever, the latter with high case fatality3. Although the risk of RVFV infection during human pregnancy is yet unclear, RVFV infections have been associated with miscarriage and recent studies have demonstrated that the virus replicates efficiently in human placental explants5,6. The threat that RVFV poses to human health is acknowledged by the World Health Organization that placed RVFV on the Blueprint list of priority diseases likely to cause future epidemics in the face of insufficient or absent countermeasures7.
Since its first description in the 1930s, RVFV has caused severe outbreaks on the African continent and the Arabian Peninsula, where the disease has remained enzootic and continues to cause epizootics and epidemics1,4. Interepizootic maintenance of RVFV is possibly explained by vertical transmission of the virus to the eggs of floodwater Aedes mosquitoes8. These species oviposit near shallow wetlands, known as dambos, which dry out during periods of drought and flood during heavy rains. These dambos provide ideal breeding grounds, as the eggs of floodwater mosquitoes depend on desiccation and rehydration for hatching. In desiccated form, the eggs can remain viable for long periods of time, possibly explaining how RVFV is maintained during periods of low or even apparent absent mosquito activity. Although this hypothesis is plausible, vertical transmission of RVFV to mosquito eggs has been demonstrated only once, and in only one mosquito species, namely Aedes (Neomelaniconion) mcintoshi Huang, a species cited before 1985 as Ae. lineatopennis8. Additionally, evidence is accumulating that RVFV is maintained in mosquito-ruminant-mosquito cycles in the absence of outbreaks9,10.
Apart from re-emergence of RVFV in enzootic areas, climate change, globalization, increasing populations of susceptible animals, and changing ecologies of mosquito vectors may facilitate future incursions into currently unaffected areas. This concern is fueled by data that suggest that over 50 mosquito species, many of which with a global distribution, can potentially act as vectors of RVFV2. These data are based on isolation of RVFV from field-collected mosquitoes and from vector competence experiments in laboratory settings, in which the virus is taken up by mosquitoes by membrane feeding on a RVFV-spiked blood meal2,11,12. However, to more firmly establish the ability of a mosquito species to act as a vector, experiments are required in which the virus is transmitted among susceptible animals via infected mosquitoes. In such experiments, factors such as mosquito population density, blood feeding behavior, and longevity can be taken into account to determine the vectorial capacity of a mosquito vector13. Furthermore, such experiments could address the influence of viremia levels in different vertebrate hosts on mosquito-mediated transmission.
In the present work, Aedes aegypti mosquitoes were infected with RVFV after membrane feeding on a virus-spiked blood meal or after feeding on lambs that developed viremia after intravenous inoculation of RVFV. The virus was subsequently transmitted by these mosquitoes to naive lambs. The presented animal models can be used to study environmental, vector and host factors that contribute to RVFV transmission and to determine the efficacy of vaccines against natural, mosquito-mediated infection.
Results
Infection of lambs via intravenous inoculation of RVFV followed by transmission of the virus between lambs and mosquitoes
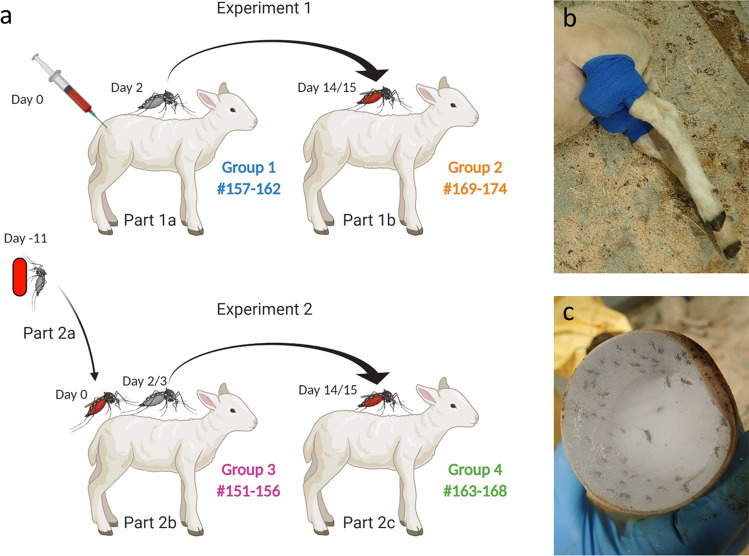
A group of 6 lambs (Group 1, #157–162) was intravenously (IV) inoculated with RVFV on day 0 (Fig. 1a, Experiment 1). Upon onset of pyrexia, previously shown to correspond with peak viremia14, mosquitoes were allowed to take a blood meal. To this end, mosquitoes were placed on sedated lambs in cardboard containers, bound to each of the hind legs with elastic tape (Fig. 1b,c). The average mosquito feeding rate was 85% (± 7%) (Table 1). Fully engorged mosquitoes were collected and maintained in an insect incubator as separate groups per lamb. All IV inoculated lambs developed pyrexia (Fig. 2a), became listless and were disinclined to feed from day 2 onwards. Analysis of daily collected plasma samples with reverse-transcriptase quantitative PCR (RT-qPCR) and virus isolation demonstrated that all lambs developed high viremia, which peaked on day 2 post inoculation (Fig. 2b), confirming that mosquito feeding occurred at peak viremia. One lamb (#159) acutely succumbed to the infection on day 4, one lamb acutely succumbed on day 5 (#157), one lamb had to be euthanized after reaching a humane end-point (HEP) on day 6 (#161) and one on day 7 (#162), resulting in a case fatality rate (CFR) of 67% (Fig. 2c). Necropsies of fatal cases revealed typical pathological manifestations of RVFV infection, with focal to widespread hepatic necrosis (Fig. 3a–c).
Figure 1.
Schematic representation of two experiments performed to study transmission of RVFV between mosquitoes and lambs. (a) In Experiment 1, lambs were inoculated via IV route with RVFV. Two days later, when pyrexia was noted, naive mosquitoes were allowed to take a blood meal from the lambs (Part 1a). Fully engorged mosquitoes were incubated for 12–13 days, after which they were allowed to take a blood meal from lambs of Group 2 (Part 1b). Before start of a parallel experiment (Experiment 2), mosquitoes were allowed to feed on a virus-spiked blood meal using a Hemotek apparatus (Part 2a). Fully engorged mosquitoes were incubated for 11 days, until they were allowed to take a second blood meal on lambs of Group 3 (Part 2b). Two to three days later, when pyrexia was measured, naive mosquitoes were allowed to take a blood meal from the lambs of Group 3 (Part 2b). Fully engorged mosquitoes were incubated for 12–13 days, after which the mosquitoes were allowed to take a second blood meal from naive lambs of Group 4 (Part 2c). The presence of RVFV in mosquito saliva samples was determined retrospectively using forced salivation and virus isolation on Vero cells. (b) Representative picture of a cardboard box containing mosquitoes placed on the hind legs of sedated lambs. (c) Representative picture of a cardboard box after mosquito feeding. Experimental details according to the ARRIVE guidelines30 are presented in Supplementary Table S1 online.
Table 1.
Quantification of transmission parameters.
| Experiment 1, Part 1a | Experiment 1, Part 1b | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1#: | Viremia day 2 (log10) | Naive mosquitoes | Group 2#: | Infected mosquitoes | Viremia Day 17 (log10) | |||||||||
| TCID50/ml | RNA copies | Fed/total (%fed) | Survivors/total (%) | fed/total (% fed) | SP/tested (%SP) | ESP/fed (%ESP) | TCID50/ml | RNA copies/ml | ||||||
| 157 | 5.1 | 8.7 | 70/89 (79) | 63/70 (90) | 169 | 51/63 (81) | 13/44 (30) | 15/51 (30) | 6.2 | 9.8 | ||||
| 158 | 6.5 | 9.2 | 86/97 (89) | 82/86 (95) | 170 | 73/82 (89) | 19/60 (32) | 23/73 (32) | 6.5 | 9.8 | ||||
| 159 | 6.7 | 9.7 | 93/98 (95) | 86/93 (92) | 171 | 59/86 (69) | 23/53 (43) | 26/59 (44) | 6.2 | 9.4 | ||||
| 160 | 5.3 | 8.8 | 80/95 (84) | 72/80 (90) | 172 | 67/72 (93) | 22/57 (39) | 26/67 (39) | 6.9 | 9.3 | ||||
| 161 | 6.2 | 9.6 | 70/92 (76) | 51/70 (73) | 173 | 31/51 (61) | 14/28 (50) | 16/31 (52) | 6.2 | 9.6 | ||||
| 162 | 6.7 | 9.7 | 85/94 (90) | 75/85 (88) | 174 | 47/75 (63) | 13/45 (29) | 14/47 (30) | 6.0 | 8.3 | ||||
| Average | 6.1 ± 0.7 | 9.2 ± 0.5 | 85 ± 7% | 88 ± 8% | Average | 76 ± 14% | 37 ± 9% | 38 ± 9% | 6.3 ± 0.3 | 9.4 ± 0.6 | ||||
| Experiment 2, Part 2a | Experiment 2, Part 2b | Experiment 2, Part 2c | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 3#: | Infected mosquitoes | Group 3#: | Viremia day 2/3 (log10) | Naive mosquitoes | Group 4#: | Infected mosquitoes | Viremia Day 17 (log10) | |||||||
| Fed/total (%fed) | SP/tested (%SP) | ESP/fed (%ESP) | TCID50/ml | RNA copies | fed/total (% fed) | Survivors/total (%) | fed/total (%fed) | SP/tested (%SP) | ESP/fed (%ESP) | TCID50/ml | RNA copies/ml | |||
| 151 | 64/92 (70) | 0/0 (0)a | N.A | 151 | 4.4 | 7.9 | 85/102 (83) | 75/85 (88) | 163 | 64/75 (85) | 21/53 (40) | 25/64 (39) | 6.9 | 9.7 |
| 152 | 35/96 (36) | 1/21 (5) | 2/35 (6) | 152 | 5.1 | 8.6 | 87/100 (87) | 75/87 (86) | 164 | 54/75 (72) | 25/48 (52) | 28/54 (52) | 6.5 | 9.1 |
| 153 | 81/101(80) | 5/54 (9) | 8/81 (10) | 152b | 5.5 | 9.1 | 96/100 (96) | 73/96 (76) | 168 | 55/73 (75) | 6/46 (13) | 7/55 (13) | 6.2 | 8.5 |
| 154 | 73/99 (74) | 3/54 (6) | 4/73 (6) | 153 | 2.5 | 7.0 | 86/94 (91) | 81/86 (94) | 165 | 66/81 (81) | 1/61 (2) | 1/66 (2) | < 1,6 | 4.2 |
| 155 | 45/102(44) | 2/37 (5) | 2/45 (4) | 154 | 6.7 | 9.4 | 96/102 (94) | 88/96 (92) | 166 | 78/88 (89) | 16/65 (25) | 19/78 (24) | 6.7 | 9.6 |
| 156 | 72/90 (80) | 7/41 (17) | 12/72(17) | 155 | 5.8 | 8.4 | 87/100 (87) | 67/87 (77) | 167 | 57/67 (85) | 16/49 (33) | 19/57 (33) | 5.8 | 8.7 |
| Average | 64 ± 19% | 8 ± 5% | 9 ± 5% | Average | 5.0 ± 1.4 | 8.4 ± 0.9 | 90 ± 5% | 86 ± 8% | Average | 81 ± 6% | 27 ± 18% | 27 ± 18% | 6.4 ± 0.4c | 8.3 ± 2 |
In Experiment 1 (Part 1a), lambs from Group 1 (n = 6, blue) were IV-inoculated with RVFV on day 0. When pyrexia was measured on day 2, Ae. aegypti mosquitoes were allowed to take a blood meal. Viremia levels on this day were determined by RT-qPCR and virus isolation using plasma samples. In Experiment 2 (Part 2a), mosquitoes were infected via membrane feeding on a RVFV-spiked blood meal. After 11 days incubation, the mosquitoes were allowed to feed on lambs of Group 3 (day 0), after which the presence of RVFV in mosquito saliva samples was determined. When pyrexia in lambs of Groups 1 and 3 was noted on day 2 or 3, naive mosquitoes were placed on the lambs and viremia levels on this day were determined by RT-qPCR and virus isolation using plasma samples. The total numbers of engorged mosquitoes (fed) and the total numbers of mosquitoes used for feeding (total) are indicated, as well as the percentages fed (%fed). Engorged mosquitoes were maintained in an insect incubator for 12–13 days. After this incubation period, surviving mosquitoes were allowed to feed on naive lambs (Groups 2 and 4). The presence of RVFV in mosquito saliva samples was determined by virus isolation on Vero cells after feeding on the lambs. Arrows indicate the lambs between which RVFV was transmitted. The numbers of saliva-positive mosquitoes are indicated (SP) as well as the numbers of mosquitoes tested (tested) and the percentage of saliva-positive samples (%SP). Because not all mosquitoes survived the incubation period, the expected number of saliva positives (ESP) was extrapolated by multiplying the %SP x fed. Titers of infectious virus and RNA copies in the blood of the lambs from Groups 2 and 4 at peak viremia (experimental day 17) are also indicated. N.A., not applicable.
aThis lamb recovered early from sedation and violently responded to the placement of the cardboard box, resulting in mortality of all blood-fed mosquitoes.
bLamb #156 was not included in Experiment 2, Part b, as this lamb succumbed to the infection before mosquitoes could feed. The corresponding mosquitoes were allowed to feed on lamb #152 on day 3.
cNo infectious virus was detected in plasma of lamb #165. This sample was therefore not included when calculating the average viremia level.
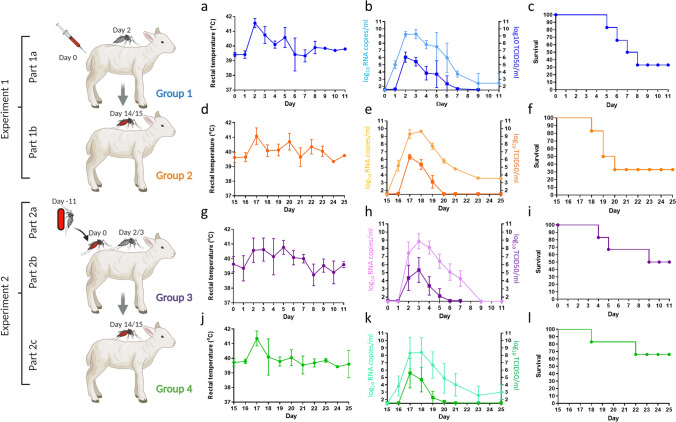
Figure 2.
Analysis of lambs exposed to RVFV via intravenous injection or via infected mosquitoes. Lambs (n = 6/group) were exposed to RVFV either via intravenous inoculation (Group 1) or via infected mosquitoes (Groups 2, 3 and 4), as schematically presented at the left. Mosquitoes that fed on lambs of Group 1 on day 2 were used to transmit the virus to lambs of Group 2 on day 14 or 15. Lambs of Group 3 were exposed to mosquitoes that membrane fed on a RVFV-spiked blood meal 11 days earlier. Naive mosquitoes were allowed to take a blood meal from these lambs on day 2 or 3. After an incubation period, these mosquitoes were used to transmit the virus to lambs of Group 4 on day 14 or 15. Rectal temperatures (a,d,g,j), viral RNA and infectious virus in plasma samples (b,e,h,k) and survival rates (c,f,i,l) are presented. Error bars represent SDs.
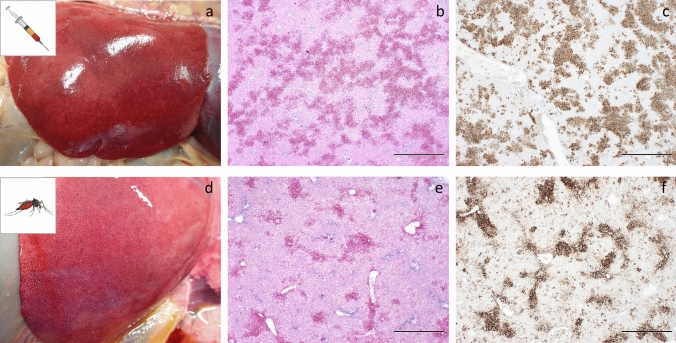
Figure 3.
Representative pathology in lambs exposed to RVFV via IV-inoculation or infected mosquitoes. Panels a–c were obtained from lamb #161 (IV inoculation). Panels d–f were obtained from lamb #154 (mosquito exposure). Both lambs were euthanized after reaching a HEP. Swollen liver with mottled appearance indicative of hepatic degeneration/necrosis (a,d), H&E staining of liver sections showing multifocal to bridging necrosis of hepatocytes with haemorrhages (b,e). IHC staining of a liver section with mAb 4-D4 showing strong immunolabelling for RVF antigen of the areas with degeneration and necrosis of hepatocytes (c,f). Bar = 1,000 μm.
The average survival rate of blood-fed mosquitoes after 13 days of incubation was 88% (± 8%) (Table 1). Following this incubation period, the 6 groups of surviving mosquitoes were each placed on naive lambs (Group 2, #169–174, Fig. 1a) (on average 72 mosquitoes per lamb) and allowed to take a second blood meal as described above. The average feeding rate of these mosquitoes was 76% (± 14%) (Table 1). Two days post feeding (dpf) on the naive lambs (day 17), all lambs developed high fever (Fig. 2d). One lamb (#173) reached a HEP and was euthanized on day 18 (dpf 3), two lambs (#169 and #174) succumbed acutely on day 19 (dpf 4) and one (#170) on day 20 (dpf 5), resulting in a CFR of 67% (Fig. 2f). Similar as observed in Group 1, all lambs that succumbed to the infection revealed typical signs of RVFV infection at necropsy. Analysis of plasma samples by RT-qPCR and virus isolation confirmed that peak viremia occurred on 2 dpf (day 17) (Fig. 2e). As all mosquito-exposed lambs developed viremia, transmission of RVFV by Ae. aegypti mosquitoes from viremic lambs to naive lambs was deemed very efficient.
To retrospectively assess the number of RVFV-positive mosquitoes that had fed on each naive lamb, mosquito saliva samples were collected by forced salivation and assayed for the presence of virus. These analyses demonstrated that 38% (± 9%) of the mosquitoes contained RVFV in saliva and suggested that each of the lambs from Group 2 were exposed to a minimum of 14 and a maximum of 26 saliva-positive mosquitoes (Table 1).
Between group comparisons of the experimental outcomes showed no significant differences (P < 0.05) in onset, viremia levels and peak of viremia between IV-inoculated lambs (Group 1) and lambs exposed to 14–26 RVFV-positive Ae. aegypti mosquitoes (Group 2). Similar morbidity and mortality rates were also observed (Fig. 2c,f and Table 1). In addition, no differences in mean viremia (AUC and peak viremia) were observed, neither in the variance of the measured variables (Fig. 2 and Supplementary Table S2 online). Given these results, mosquito-mediated transmission of RVFV from IV-inoculated lambs to naive lambs was deemed efficient and robust, with all exposed animals developing viremia and clinical signs with low variability observed in measured outcome parameters.
Infection of mosquitoes via membrane feeding on a RVFV-spiked blood meal, followed by transmission of the virus between mosquitoes and lambs
In a parallel experiment, we investigated how efficiently RVFV can be transmitted between mosquitoes and lambs, starting with mosquitoes that ingested the virus via membrane feeding (Fig. 1a, Experiment 2). To this end, mosquitoes were fed on a bovine erythrocyte suspension containing 107.5 TCID50/ml of RVFV, using a Hemotek membrane feeder. After 11 days incubation, the mosquitoes were allowed to feed on lambs from Group 3 (lambs #151–156) (on average 97 mosquitoes per lamb). Feeding was overall successful, although lamb #151 recovered early from its sedation, and violently responded to the cardboard boxes attached to its legs, resulting in death of all (already engorged) mosquitoes. Virtually all other mosquitoes survived the feeding period with an average feeding rate of 64% (± 19%) (Table 1). Retrospectively, forced salivation analysis showed that 9% (± 5%) of the mosquitoes used to infect lambs of Group 3 contained RVFV in saliva, which suggested that each lamb was exposed to 2–12 saliva-positive mosquitoes.
All mosquito-exposed lambs of Group 3 manifested with pyrexia (Fig. 2g) and analysis of plasma samples by RT-qPCR and virus isolation demonstrated that viremia peaked on days 2 or 3 (Fig. 2h and Table 1). All lambs developed clinical signs including lethargy and reduced appetite. One lamb (#156) succumbed acutely to the infection on day 3 and another lamb (#154) had to be euthanized upon reaching a HEP on day 4. Lamb #151 reached a HEP on day 8, resulting in a CFR of 50% (Fig. 2i). Necropsies of euthanized lambs revealed focal to widespread hepatic necrosis associated with RVFV antigen (Fig. 3d–f).
In line with experiment 1, naive mosquitos were placed on lambs of Group 3 when pyrexia was noted. Considering that not all lambs developed pyrexia on day 2, some of the lambs were exposed to mosquitoes on day 3 (Table 1). Of note, lamb #156 succumbed acutely before naive mosquitoes could be allowed to feed on this animal. The mosquitoes that were meant to feed on this lamb were instead allowed to feed on lamb #152 on day 3 (note that another group of mosquitoes fed on the same lamb on day 2). Between 85 and 96 naive mosquitoes were used for feeding and the average feeding rate was 90% (± 5%). Of the fully engorged mosquitoes (fed on Group 3), 86% survived the incubation period of 12–13 days. Surviving mosquitoes were subsequently placed on the naive lambs from Group 4 (lambs #163–168) (average 77 mosquitoes per lamb). Forced salivation analysis showed that 27% (± 18%) of the mosquitoes contained RVFV in saliva, which suggested that lambs of Group 4 were each exposed to 1–28 saliva-positive mosquitoes (Table 1).
All lambs from Group 4 developed pyrexia 2 days post mosquito exposure, corresponding to study day 17 (Fig. 2j). Analysis of plasma samples by RT-qPCR and virus isolation demonstrated that peak viremia occurred on the same day (Fig. 2k). Lamb #163 reached a HEP and was euthanized 3 days post feeding, corresponding to day 18. Lamb #164 reached a HEP 7 days post feeding, corresponding to day 22, resulting in a CFR of 33% (Fig. 2l).
Interestingly, one lamb from Group 3 (#153), revealed relatively low viral RNA levels in plasma samples and titers of infectious virus just above the detection limit of the assay (102.5 TCID50/ml on day 3). Retrospective analysis suggested that this lamb was exposed to 8 membrane-fed RVFV saliva-positive mosquitoes (Table 1). Despite very low level of infectious virus in the blood of lamb #153, RVFV was transmitted successfully to lamb #165 of Group 4. Whereas lamb #165 developed detectable levels of viral RNA, no infectious virus was isolated (Table 1). Analysis of mosquitoes used to transmit virus from lamb #153 to #165 suggested that lamb #165 was exposed to one infected mosquito. Both lambs, #153 and #165 did not develop clinical signs and it was also interesting to find that all lambs, including #153 and #165, developed anti-nucleocapsid antibodies, as determined by ELISA, as well as neutralizing antibodies, which are known to correlate with protection (see Supplementary Fig. S1 online).
No significant differences (P < 0.05) in peak viremia or overall viremia during the course of infection were observed between Groups 3 and 4 . Variances were also similar, however the presence of sheep #153 and #165 in each of these groups led to high variances in the measured variables (Supplementary Table S2 online).
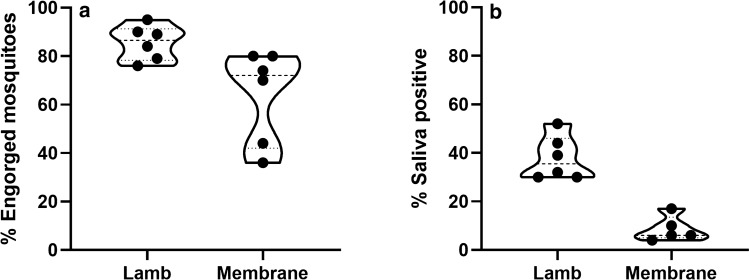
Comparing RVFV transmission to mosquitoes after membrane feeding on a virus-spiked blood meal or on viremic lambs
In the present work, two methods were used to obtain mosquitoes that contained RVFV in saliva. Mosquitoes were fed either on viremic lambs or membrane-fed on a virus-spiked blood meal. The feeding rate (mean ± SD) in mosquitoes fed on needle-inoculated, viremic lambs (85% ± 7) was significantly higher (p = 0.002) than feeding rates of mosquitoes fed on a virus-spiked blood meal (64% ± 19). The percentage of saliva-positive (surviving) mosquitoes was also much higher (p < 0.001) when mosquitoes were fed on viremic lambs (38% ± 9%) as compared to membrane feeding (9% ± 5%) (Fig. 4), whereas the average virus titer during mosquito feeding on the lambs was 30-fold lower.
Figure 4.
Feeding rates depicted as % engorged mosquitoes (a) and percentages of RVFV saliva-positive mosquitoes (b) after feeding on a viremic lamb or after membrane feeding on a virus-spiked blood meal. Mosquitoes were fed on a viremic lamb in Experiment 1, part 1a, or via membrane in Experiment 2, part 2a. Percentages of RVFV saliva-positive mosquitoes were determined after an incubation period of 15–21 days (Experiment 1), or after 14–21 days (Experiment 2). Virus in saliva was demonstrated by incubation on Vero cells, followed by scoring of CPE. Data are presented in violin plots with median and quartiles. Dots represent individual measurements.
Discussion
We here report the reproduction of the complete RVFV transmission cycle under controlled conditions. The established animal models can be used to study transmission of RVFV between laboratory-reared Ae. aegypti mosquitoes and lambs either initiating with IV inoculation of lambs, or with mosquito feeding on a RVFV-spiked blood meal. Although both models result in efficient transmission of the virus among lambs, our results show that feeding on viremic lambs results in much higher percentages of RVFV saliva-positive mosquitoes as compared to membrane feeding. Our results thereby underscore the previous notion that membrane feeding may result in a significant underestimation of vector competence and stress the value of experiments involving vertebrate hosts15,16.
Apart from evaluating the two models individually, our experiments also enabled us to directly compare the outcome of infection following IV inoculation or exposure to infected mosquitoes. Specifically, in Experiment 1, lambs were IV inoculated with a dose of 105 TCID50 (Group 1) whereas in Experiment 2, lambs were exposed to infected mosquitoes (Group 3), which were fed earlier on a RVFV-spiked blood meal. Retrospective analyses of mosquito saliva suggested that these lambs were exposed to an average of 9 RVFV saliva-positive mosquitoes. This resulted (although not statistically significant) in an average lower peak rectal temperature, later onset and lower level of viremia, and a lower mortality rate when compared to the lambs inoculated via IV route with a dose of 105 TCID50. Mosquitoes that were fed on the viremic lambs from both groups were subsequently allowed to feed on naive lambs from Groups 2 and 4. With one notable exception, all lambs developed pyrexia and viremia. The exception was lamb #165 from Group 4, which had an RNA level of 104.2 copies/ml at dpf 2, which is below the limit of detection of our virus isolation assay. Interestingly, this lamb was exposed to mosquitoes that had earlier fed on lamb #153, which was an outlier itself from Group 3, displaying a low viremia level (102.5 TCID50/ml) at the moment of mosquito feeding, possibly explaining the low number of mosquitoes that became infected after feeding on this lamb. Specifically, lamb #165 seemed to be exposed to only one saliva-positive mosquito, developing very low viremia after this exposure. The other lambs in both groups (Groups 2 and 4) were exposed to an average of 20 saliva-positive mosquitoes and the virological and clinical outcomes in these groups were highly similar to those resulting from IV inoculation (Group 1).
Intravenous inoculation of 105 TCID50 of RVFV is currently applied in our laboratory to evaluate efficacy of vaccines which, according to the present study, seems to result in virological and clinical outcomes that mimic those following exposure to ~ 20 RVFV saliva-positive mosquitoes. It is interesting to consider if exposure to 20 RVFV saliva-positive mosquitoes is representative to the field situation. An entomological study performed during the Kenyan outbreak of 2006/2007, revealed an average infection rate below 3 per 1000 mosquitoes17. Although depending on vector densities and attack rates, this finding suggests that animals are unlikely to be exposed to RVFV via more than one mosquito in the field at any given moment, even during outbreaks. It would thus be valuable to evaluate virological and clinical outcome after exposure to a single saliva-positive mosquito in future experiments.
The efficient transmission of RVFV from lamb to lamb in the present work was facilitated by the use of laboratory-reared Ae. aegypti mosquitoes. We selected these mosquitoes for our studies as they are easily reared to very high numbers and as they take multiple bloodmeals in a single gonotrophic cycle18. It must be noted, however, that RVFV was never detected in Ae. aegypti collected from the field. This can be explained by differences in susceptibility between laboratory-reared mosquitoes and field-collected mosquitoes. Alternatively or additionally, the lack of detection of RVFV in field-collected Ae. aegypti mosquitoes may be explained by host preference. Having a preference for human blood, Ae. aegypti is mostly found in urban areas, whereas RVFV is most prevalent in rural areas where ruminants reside19. Nevertheless, the extremely efficient transmission of RVFV as determined in the present work should be considered a warning. Ae. aegypti is the primary vector of four arboviruses with major impact on human health: chikungunya virus, dengue virus, yellow fever virus, and Zika virus and growing populations of humans and livestock will facilitate encounters of Ae. aegypti and RVFV. Therefore, further studies are required to evaluate the risk of human-to-human transmission of RVFV by Ae. aegypti mosquitoes, which could result in urban transmission cycles. Considering this, it is important to determine if viremia levels in infected humans are sufficient to facilitate urban transmission cycles. One study, in which viremia levels approaching 106 TCID50/ml were recorded suggests that humans may not be a dead-end host for RVFV as currently assumed20.
In conclusion, our work has demonstrated that RVFV can be transmitted efficiently from lamb to lamb via laboratory-reared Ae. aegypti mosquitoes and thereby provides novel methods to investigate environmental, vector and vertebrate host factors that affect transmission of RVFV in the field. Importantly, the methods can be used to evaluate efficacy of vaccines against mosquito-mediated exposure.
Methods
Virus and cells
RVFV strain 35/74 was originally isolated from the liver of a sheep that died during a RVFV outbreak in the Free State province of South Africa in 197421. The strain was previously passaged four times in suckling mouse brain and three times in BHK cells. The virus used for IV inoculation of sheep was prepared by a further amplification in BHK-21 cells (ATCC CCL-10) cultured in CO2-independent medium (CIM, Invitrogen), supplemented with 5% FBS (Bodinco) and 1% Pen/Strep (Invitrogen).
To prepare a virus-spiked blood meal for membrane feeding of mosquitoes, the virus was amplified in Aedes albopictus C6/36 cells (ATCC CRL-1660). To this end, C6/36 cells were inoculated with a multiplicity of infection of 0.005 and cultured at 28 °C in absence of CO2 in L-15 medium (Sigma) supplemented with 10% fetal bovine serum (FBS), 2% Tryptose Phosphate Broth (TPB) and 1% MEM nonessential amino acids solution (MEMneaa). At 4 days post infection, culture medium was harvested, cleared by slow-speed centrifugation and titrated using Vero-E6 cells (ATCC CRL-1586), grown in DMEM supplemented with GlutaMAX, 3% FBS, 1% Pen/Strep and 1% Fungizone (DMEM +) at 37 °C and 5% CO2. Titers were determined using the Spearman-Kärber algorithm22,23.
Mosquito rearing and feeding on lambs
Rockefeller strain Ae. aegypti mosquitoes (Bayer AG, Monheim, Germany) were maintained at Wageningen University, Wageningen, the Netherlands, as described24. Briefly, mosquitoes were kept in Bugdorm-1 rearing cages at a temperature of 27 °C with a 12:12 light:dark cycle and a relative humidity of 70% with a 6% glucose solution provided ad libitum. Mosquitoes were subsequently transported to biosafety level three (BSL-3) facilities of Wageningen Bioveterinary Research (Lelystad, the Netherlands), where the mosquitoes were maintained with sugar water (6% sucrose in H2O), provided via soaked cotton pads covered with a lid to prevent evaporation in an insect incubator (KBWF 240, Binder) at 28 °C at a humidity of 70% and a 16:8 light:dark cycle.
Mosquito feeding on lambs was preceded by sedating the lambs with IV administration of medetomidine (Sedator). When fully sedated, cardboard boxes containing 40–50 female mosquitoes were placed on the shaved inner thigh of each hind leg (Fig. 1b,c). After 20 min of feeding, cardboard boxes were removed and atipamezol (Atipam) was administered via intramuscular (IM) route to wake up the animals. Fully engorged mosquitoes were collected using an automated insect aspirator and maintained with sugar water (6% sucrose in H2O), provided via soaked cotton pads covered with a lid to prevent evaporation, in an insect incubator (KBWF 240, Binder) at 28 °C at a humidity of 70% and a 16:8 light:dark cycle.
Feeding of mosquitoes using a Hemotek system
Blood meals to be used for Hemotek membrane feeding were prepared essentially as described before25. Briefly, erythrocytes were harvested from freshly collected bovine EDTA blood by slow-speed centrifugation (650 xg), followed by three wash steps with PBS. Washed erythrocytes were resuspended in L15 complete medium (L15 + 10% FBS, 2% TPB, 1% MEMneaa) to a concentration that is four times higher than found in blood. To prepare a blood meal, one part of the erythrocyte suspension was mixed with two parts of culture medium containing RVFV resulting in a final titer of 107.5 TCID50/ml as determined on Vero-E6 cells.
Mosquitoes were allowed to take a RVFV-spiked blood meal through a Parafilm M membrane using the Hemotek PS5 feeding system (Discovery Workshops, Lancashire, United Kingdom). Feeding was performed in plastic buckets (1 l) covered with mosquito netting. After blood feeding for approximately 1.5–2 h, fully engorged mosquitoes were collected using an automated insect aspirator and maintained with sugar water (6% sucrose in H2O), provided via soaked cotton pads covered with a lid to prevent evaporation in an insect incubator (KBWF 240, Binder) at 28 °C at a humidity of 70% and a 16:8 light:dark cycle.
Virus isolation
Virus isolation from plasma samples was performed using BHK-21 cells, seeded at a density of 20,000 cells/well in 96-wells plates. Serial dilutions of samples were incubated with the cells for 1.5 h before medium replacement. Cytopathic effect was evaluated after 5–7 days post infection. Virus titers (TCID50/ml) were determined using the Spearman-Kärber algorithm22,23.
To check for positive saliva, mosquitoes were sedated on a semi-permeable CO2-pad connected to 100% CO2 and wings and legs were removed. Saliva was collected by forced salivation using 20 µl filter tips containing 7 µl of a 1:1 mixture of FBS and 50% sucrose (capillary tube method). After 1–1.5 h, saliva samples were collected and used to inoculate Vero-E6 cell monolayers. Cytopathic effect (CPE) was scored 5–7 days later.
Serology
Weekly collected serum samples were used to detect RVFV-specific antibodies using the ID Screen Rift Valley Fever Competition Multi-species ELISA (ID-VET). This ELISA measures percentage competition between antibodies present in test sera and a monoclonal antibody. Neutralizing antibodies were detected using the RVFV-4 s-based virus neutralization test as described26.
RT-qPCR
Viral RNA was isolated with the NucliSENS easyMAG system according the manufacturer’s instructions (bioMerieux, France) from 0.5 ml plasma samples. Briefly, 5 µl RNA was used in a RVFV RT-qPCR using the LightCycler one-tube RNA Amplification Kit HybProbe (Roche, Almere, The Netherlands) in combination with a LightCycler 480 real-time PCR system (Roche) and the RVS forward primers (AAAGGAACAATGGACTCTGGTCA), the RVAs (CACTTCTTACTACCATGTCCTCCAAT) reverse primer and a FAM-labelled probe RVP (AAAGCTTTGATATCTCTCAGTGCCCCAA). Primers and probes were earlier described by Drosten et al.27. Virus isolations were performed on RT-qPCR positive samples with a threshold above 105 RNA copies/ml as this was previously shown to be a cut-off point below which no live virus can be isolated.
Pathology and (immuno)histopathology
Liver samples were placed on ice during the necropsies and subsequently stored at − 80 °C until virus isolations and RT-qPCR Tissue samples for histology and IHC were collected, placed in 10% neutral buffered formalin, embedded into paraffin and prepared for H&E staining or IHC staining for RVFV antigen using the RVFV Gn-specific 4-D4 mAb as described5.
Statistics
For statistical analysis, mosquito feeding and mosquito saliva positive rates per group were compared by fitting logistic regression mixed models where lamb or membrane were introduced as random effects. To compare viremia (based on virus isolation results) the area under the curve (AUC) representing the overall viremia during the infected period was calculated for each infected sheep. This AUC and peak of viremia was used for comparison between groups, which was done by fitting linear regression models.
Additionally we also assessed the variability observed between groups on the above mentioned variables (feeding and saliva positive rates, AUC and peak viremia). For these comparisons, data were first assessed for normality using the Shapiro–Wilk test. If data from all groups were normally distributed, the Bartlett's test of homogeneity of variance was used. If the data did not have a normal distribution, the Fligner-Killeen test was applied.
Survival of infected lambs (time to death) was compared between experiment groups using Kaplan–Meier survival analysis and the mortality rates were compared fitting a logistic regression model.
For all comparisons, the threshold for significance was p < 0.05, for analysis involving multiple group comparison a Bonferroni correction was applied. All statistical analysis were performed using the statistical software package R28. The package MESS29 was used to compute the AUC.
Ethics statement
The animal experiment was conducted in accordance with European regulations (EU directive 2010/63/EU) and the Dutch Law on Animal Experiments (Wod, ID number BWBR0003081). Permissions were granted by the Dutch Central Authority for Scientific Procedures on Animals (Permit Number: AVD4010020185564). All experimental protocols were approved by the Animal Ethics Committees of Wageningen Research.
Supplementary Information
Acknowledgements
We thank our animal caretakers for their support during the animal experiment and the insect rearing team of the Laboratory of Entomology for maintenance of the Ae. aegypti colony. We thank Dr. Schmaljohn (USAMRIID, Fort Detrick, MD) for providing the 4-D4 mAb. RVFV strain 35/74 was kindly provided by Prof. Dr. Janusz Paweska (National Institute for Communicable Diseases [NICD], Johannesburg, South Africa). We thank Erick Bermúdez Méndez for critically reviewing the manuscript. Cartoons in this manuscript were created by BioRender.com.
Author contributions
Conceptualization, P.W.S., L.K., and J.K.; methodology, P.W.S., L.K., and J.K.; formal analysis, P.W.S., R.P.M.V., L.K., J.L.G., and J.K.; investigation, R.P.M.V.; resources, T.V., C.J.M.K., C.B.F.V.; writing original draft preparation, P.W.S., J.K.; writing, reviewing and editing, L.K., T.V., J.L.G., C.J.M.K., C.B.F.V.; supervision, J.K.; project administration, P.W.S., J.K.; funding acquisition, J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Netherlands Ministry of Agriculture, Nature and Food Quality project codes: WOT-01-003-083 and KB-21-006-036.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-020-79267-1.
References
- 1.Wright D, Kortekaas J, Bowden TA, Warimwe GM. Rift Valley fever: Biology and epidemiology. J. Gen. Virol. 2019;100:1187–1199. doi: 10.1099/jgv.0.001296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lumley S, et al. Rift Valley fever virus: Strategies for maintenance, survival and vertical transmission in mosquitoes. J. Gen. Virol. 2017;98:875–887. doi: 10.1099/jgv.0.000765. [DOI] [PubMed] [Google Scholar]
- 3.Ikegami T, Makino S. The pathogenesis of Rift Valley fever. Viruses. 2011;3:493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hartman A. Rift Valley fever. Clin. Lab. Med. 2017;37:285–301. doi: 10.1016/j.cll.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oymans J, Wichgers Schreur PJ, van Keulen L, Kant J, Kortekaas J. Rift Valley fever virus targets the maternal-foetal interface in ovine and human placentas. PLoS Negl. Trop. Dis. 2020;14:e0007898. doi: 10.1371/journal.pntd.0007898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMillen CM, et al. Rift Valley fever virus induces fetal demise in Sprague-Dawley rats through direct placental infection. Sci. Adv. 2018;4:9812. doi: 10.1126/sciadv.aau9812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehand MS, Al-Shorbaji F, Millett P, Murgue B. The WHO R&D Blueprint: 2018 review of emerging infectious diseases requiring urgent research and development efforts. Antiviral Res. 2018;159:63–67. doi: 10.1016/j.antiviral.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linthicum KJ, Davies FG, Kairo A, Bailey CL. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J. Hyg. (Lond.) 1985;95:197–209. doi: 10.1017/s0022172400062434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van den Bergh C, Venter EH, Swanepoel R, Thompson PN. High seroconversion rate to Rift Valley fever virus in cattle and goats in far northern KwaZulu-Natal, South Africa, in the absence of reported outbreaks. PLoS Negl. Trop. Dis. 2019;13:e007296. doi: 10.1371/journal.pntd.0007296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lichoti JK, et al. Detection of rift valley fever virus interepidemic activity in some hotspot areas of kenya by sentinel animal surveillance, 2009–2012. Vet. Med. Int. 2014;2014:379010. doi: 10.1155/2014/379010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birnberg L, et al. Field-captured Aedes vexans (Meigen, 1830) is a competent vector for Rift Valley fever phlebovirus in Europe. Parasit. Vec. 2019;12:484. doi: 10.1186/s13071-019-3728-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zakhia R, Mousson L, Vazeille M, Haddad N, Failloux AB. Experimental transmission of West Nile Virus and Rift Valley fever Virus by Culex pipiens from Lebanon. PLoS Negl. Trop. Dis. 2018;12:e0005983. doi: 10.1371/journal.pntd.0005983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kramer LD, Ciota AT. Dissecting vectorial capacity for mosquito-borne viruses. Curr. Opin. Virol. 2015;15:112–118. doi: 10.1016/j.coviro.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wichgers Schreur PJ, Kant J, van Keulen L, Moormann RJ, Kortekaas J. Four-segmented Rift Valley fever virus induces sterile immunity in sheep after a single vaccination. Vaccine. 2015;33:1459–1464. doi: 10.1016/j.vaccine.2015.01.077. [DOI] [PubMed] [Google Scholar]
- 15.Turell MJ. Reduced Rift Valley fever virus infection rates in mosquitoes associated with pledget feedings. Am. J. Trop. Med. Hyg. 1988;39:597–602. doi: 10.4269/ajtmh.1988.39.597. [DOI] [PubMed] [Google Scholar]
- 16.Azar SR, Weaver SC. Vector competence: What has Zika virus taught us? Viruses. 2019 doi: 10.3390/v11090867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sang R, et al. Rift Valley fever virus epidemic in Kenya, 2006/2007: the entomologic investigations. Am. J. Trop. Med. Hyg. 2010;83:28–37. doi: 10.4269/ajtmh.2010.09-0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott TW, et al. Longitudinal studies of Aedes aegypti (Diptera: Culicidae) in Thailand and Puerto Rico: blood feeding frequency. J. Med. Entomol. 2000;37:89–101. doi: 10.1603/0022-2585-37.1.89. [DOI] [PubMed] [Google Scholar]
- 19.Walsh MG, de Willem SA, Mor SM. Wetlands wild Bovidae species richness and sheep density delineate risk of Rift Valley fever outbreaks in the African continent and Arabian Peninsula. PLoS Negl. Trop. Dis. 2017;11:e0005756. doi: 10.1371/journal.pntd.0005756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de St Maurice A, et al. Rift valley fever viral load correlates with the human inflammatory response and coagulation pathway abnormalities in humans with hemorrhagic manifestations. PLoS Negl. Trop. Dis. 2018;12:e0006460. doi: 10.1371/journal.pntd.0006460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnard BJ. Rift Valley fever vaccine–antibody and immune response in cattle to a live and an inactivated vaccine. J. S. Afr. Vet. Assoc. 1979;50:155–157. [PubMed] [Google Scholar]
- 22.Kärber G. Betrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Path. Pharmak. 1931;162:480–483. doi: 10.1007/BF01863914. [DOI] [Google Scholar]
- 23.Spearman C. The method of right and wrong cases (constant stimuli) without Gauss’s formulae. Br. J. Psychol. 1908;2:227–242. [Google Scholar]
- 24.Goertz GP, Vogels CBF, Geertsema C, Koenraadt CJM, Pijlman GP. Mosquito co-infection with Zika and chikungunya virus allows simultaneous transmission without affecting vector competence of Aedes aegypti. PLoS Negl. Trop. Dis. 2017;11:e0005654. doi: 10.1371/journal.pntd.0005654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vloet RPM, et al. Transmission of Rift Valley fever virus from European-breed lambs to Culex pipiens mosquitoes. PLoS Negl. Trop. Dis. 2017;11:e0006145. doi: 10.1371/journal.pntd.0006145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wichgers Schreur PJ, Paweska JT, Kant J, Kortekaas J. A novel highly sensitive, rapid and safe Rift Valley fever virus neutralization test. J. Virol. Methods. 2017;248:26–30. doi: 10.1016/j.jviromet.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Drosten C, et al. Rapid detection and quantification of RNA of Ebola and Marburg viruses, Lassa virus, Crimean-Congo hemorrhagic fever virus, Rift Valley fever virus, dengue virus, and yellow fever virus by real-time reverse transcription-PCR. J. Clin. Microbiol. 2002;40:2323–2330. doi: 10.1128/jcm.40.7.2323-2330.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. (2019).
- 29.Ekstrøm, C. T. MESS: Miscellaneous Esoteric Statistical Scripts. R package version 0.5.6. Claus Thorn Ekstrøm (2019).
- 30.Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. Osteoarthr. Cartil. 2012;20:256–260. doi: 10.1016/j.joca.2012.02.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.