Abstract
Background
Psoriasis a chronic inflammatory skin disease manifests with microcirculatory changes within skin which may precede skin manifestations, correlate with their severity, joint involvement and resolve with treatment. Nailfold capillaroscopy (NFC) is used in rheumatology for connective tissue disorder assessment and is assuming significance in psoriasis. The aim was to study the nailfold capillaroscopic findings in patients with psoriasis.
Methods
A cross-sectional observational study was carried out at a skin center of a tertiary care hospital from January 2016 to June 2017. Selected cases underwent NFC using a portable color capillaroscope with an attached computer with software to analyze the nailfold capillaries for morphological parameters and abnormalities. Independent-samples t test and chi-square test was used to analyze the relationships between variables.
Results
Mean capillary loop density in 96% of study population was subnormal (<9 capillaries/mm), mean arterial limb diameter 11.37 ± 2.434μ; mean venous limb diameter 15.89 ± 3.131μ, top of the loop diameter 14.41 ± 4.373μ and length of the loop was 152.51 ± 57.21μ. Only 3 had length of loop >300μ. Bizarre morphology was seen in 15.5% of capillaries (p value < 0.001). Crossed loops/tortuous capillaries were seen in 17.3% of patients (p value < 0.001). Ramified capillaries were seen in 9.1% of patients with psoriasis (p value < 0.001). Other abnormalities observed were hemorrhage, avascular areas and subpapillary plexus. Widespread disease and psoriatic arthritis (18.2%) had irregular and haphazard distribution of capillaries (p value < 0.001). Analysis of Psoriasis Area Severity Index score, age of the patient and NFC did not reveal any statistically significant relationship.
Conclusions
Nailfold capillaroscopy (NFC), a non invasive imaging technique for microcirculation evaluation can serve to prognosticate and follow up patirents with psoriasis as a simple and highly reproducible tool. Nailfold capillaroscopy is a simple and an easy method to study the microvascular abnormalities in psoriasis. Findings correlate with disease severity. It can be used for follow-up as a predictor of disease worsening or response to treatment.
Keywords: Nailfold capillaroscopy, Psoriasis, Psoriatic arthritis
Introduction
Psoriasis is a chronic inflammatory skin disease, with a strong genetic basis characterized by complex alterations in epidermal growth and differentiation. It manifests multiple biochemical, immunologic, and vascular abnormalities. The worldwide prevalence of psoriasis is between 0.09% and 11.4%.1 Nearly two third of people with psoriasis have a mild form of the disease, with less than 3% of skin surface of the body affected, but others have more extensive involvement of the skin.
A significant difference in microcirculation within skin of psoriatic patients is noted when compared with individuals without the disease. The dermal and epidermal papillae become edematous, with dilated and coiled capillary loops,2,3 endothelial pores are more in number in postcapillary venules, resulting in increased excretion of albumin and other blood proteins. Within lesions, the blood flow appears to be increased.4 These vascular changes appear to precede the onset of psoriatic skin lesions though they have also been described in some of the healthy non-lesional skin of patients with psoriasis.5 Levels of angiogenic factors such as transforming growth factor beta, platelet-derived growth factor and vascular endothelial growth factor have also been found to be high.6 Clinical resolution of skin lesions is also associated with reversal of these microvasculature changes to normal.2
Microvasculature of the psoriatic lesions has been studied using magnifying lenses, stereomicroscopes, in vivo microscopes and lately the capillaroscope. Routine microscopic study of the psoriatic plaque gives a frontal view of the capillaries. It is thus difficult to assess whether it is a single capillary or a branch of nearby capillaries which may lead to misinterpretation of the ramifications and tortuosity in them and hence may cause loss of accuracy in estimating capillary density. This artefact is absent in the periungual study. It gives a longitudinal view which allows the viewer to follow the entire course of capillary within the dermal papilla as the nailfold capillaries are arranged parallel to skin surface.7
Nailfold capillaroscopy (NFC) is a technique which allows us to study in vivo morphological and functional characteristics of microcirculation.7 It is quick, non-invasive, and gives an idea about the early changes which occur in periungual circulation. Hence, it is superior to the usual conventional methods which were used in the past to study the microvasculature in the nailfolds. The parameters measured in proximal nailfold include capillary density (normal 8.9–14/mm), capillary width (normal 27–59.5μ), capillary length (normal 92–295μ), arterial limb diameter (normal 7–17μ), and venous limb diameter (normal 11–20.6μ). Abnormalities in patterns may manifest as coiled, ramified, or M-shaped capillaries. These changes carry a poorer prognosis. Tortuosity otherwise considered physiological, may indicate angiogenesis in some diseases.8
Recently, NFC has gained significance for diagnosis of various rheumatic and connective tissue disorders such as systemic sclerosis, dermatomyositis, Sjogren's disease, rheumatoid arthritis, and psoriatic arthritis (PsA). It is also used to identify neovascular changes in cases of diabetes and hypertension.9,10
This study was hence conducted to study the various microvascular changes in the nailfolds of Indian patients with different types of psoriasis using capillaroscope which would enable us to understand the vascular changes associated with the disease. One earlier Indian study on nailfold capillaroscopy using a low cost model USB digital microscope was done, however capillary parameters were not studied.11
Materials and methods
A cross sectional observational study of nailfold capillaries on 110 patients of psoriasis vulgaris (PV) was conducted at our skin center at a tertiary care hospital over a period of 18 months. An independent sample T test and a chi-square test was used to analyze the relationships between variables. With the proposed sample size of 110 determined with an assumed 10% fallout, the study had a power of 90%. P value < 0.05 was used as statistical significance. Patients with psoriasis in the form of PV, palmoplantar psoriasis (PPP), PsA of varying duration and receiving any treatment modality for psoriasis were included. Patients with PsA or conditions known to alter the nailfold capillaries such as pregnancy and lactation, coexistent connective tissue disorders such as systemic lupus erythematosus, systemic sclerosis, dermatomyositis, polymyositis, and rheumatoid disorders, those with psoriasis with coexisting morbidities such as diabetes mellitus, hypertension, cardiovascular risk factors, and or coagulopathy, isolated nail psoriasis, those on vasoactive therapies or anticoagulants, as well as those with primary or secondary Raynaud's phenomenon or acrocyanosis were excluded from the study.
A comprehensive clinical history including the duration of skin and nail changes and area of involvement was recorded followed by a detailed dermatological examination and Psoriasis Area Severity Index (PASI) scoring. Clinical photography of cases was carried out in all. Radio-imaging of hands was performed if indicated.
Standard NFC was carried out using a portable color capillaroscope (Jiangsu Jiahua, JH 1004, China) with inbuilt software to record capillary measurements.
Fifth fingers of both hands were studied at the nailfold by capillaroscope. The nailfold capillaries were visualized and then photographed images were analyzed simultaneously in the computer with the software program installed with the capillaroscope.
The following parameters were recorded: shape, distribution, mean capillary loop density, arterial limb diameter, venous limb diameter, top of loop diameter, length of loop, presence of tortuous loops, presence or absence of ramified capillaries, presence or absence of haemorrhages, visibility of the subpapillary plexus, and presence or absence of avascular areas (Fig. 1, Fig. 2).
Fig. 1.
Clinical presentation (top row) and corresponding capillaroscopy findings (bottom row); (a) Inverse U-shaped capillaries, (b) capillary field count displaying 6, (c) bizarre shaped capillary, (d) regular and parallel arrangement, and (e) Irregular and haphazardly arranged capillaries.
Fig. 2.
Clinical presentation (top row) and corresponding capillaroscopy findings (bottom row); (a) megacapillary, (b) tortuous and ramified capillaries, (c) visible subpapillary plexus, (d) avascular areas, (e) irregular and crossed loops, and (f) ramified/bushy capillaries.
A possible relationship of aforementioned changes to PASI, disease duration, gender, and age of patient was also statistically ascertained.
Results
In this study, patients of different types of psoriasis were studied (Fig. 1, Fig. 2). Diagnosis of psoriasis in most cases was made on clinical grounds. Age group of patients ranged from 14 to 77 years, with 78 (71%) males and 32 (29%) females. A maximum of 73 (66%) patients had PV, 25 (23%) had PPP, 7 (6%) had both PV and PPP, and 5 (4.6%) had PsA (Fig. 3).
Fig. 3.
Capillaroscopy findings observed in accordance with age group.
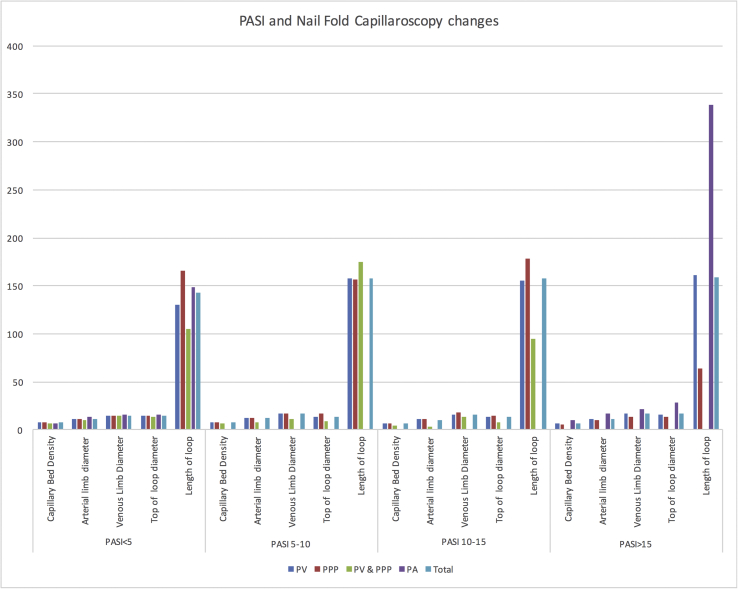
Psoriasis Area Severity Index (PASI) score in 33.6% (37) of patients was <5 suggestive of mild psoriasis, 5 to 10 suggestive of moderate psoriasis was found in 37.3% (41), 21.8% (24) had PASI 10–15, 7.3% (8) patients had PASI score >15 suggestive of severe psoriasis (Fig. 4). Coexistent nail involvement was observed in seven cases and only one of these had involvement of the fifth finger.
Fig. 4.
Psoriasis Area Severity Index (PASI) and nailfold capillaroscopy changes.
Duration of illness ranged from 2 months to 25 yrs (28 less than 1yr, 47 for 1–5yrs, 20 for 5–10 yrs, and 15 patients had disease for more than 10yrs) (Fig. 5).
Fig. 5.
Treatment modality and capillaroscopic findings in accordance with duration of disease.
About 68.2% (75) of patients were on topical medications, whereas 10.9% (12) were on both topical medications and narrow band ultraviolet B (NBUVB), 12.7% (14) patients were on topical medications and methotrexate, and 8.2% (9) patients were on biologics (Fig. 2).
Analysis of various parameters revealed
Inverse U shape of capillaries was seen in 84.5% of total cases. The rest 15.5% had bizarre morphology of capillaries (p value < 0.001) (Table 1).
Table 1.
Distribution of patients based on morphology on nailfold capillaroscopy in different types of psoriasis.
| Types of psoriasis | Morphology of capillaries |
|||
|---|---|---|---|---|
| Inverse ‘U’ |
Bizarre |
|||
| Number | % | Number | % | |
| PV | 62 | 85 | 11 | 15 |
| PP | 21 | 84 | 4 | 16 |
| PV + PP | 7 | 100 | 0 | 0 |
| PsA | 3 | 60 | 2 | 40 |
| Total | 93 | 85 | 17 | 15 |
PV, psoriasis vulgaris; PP, palmoplantar psoriasis; PsA, psoriatic arthritis.
Mean capillary loop density in 76% of patients was between 7 and 9 capillaries/mm, 20% between 4 and 6 capillaries/mm (p value < 0.011) and rest 4% of patients had mean capillary loop density >9 capillaries/mm, whereas none had it less than 4 capillaries/mm. Mean arterial limb diameter in the study population was found to be 11.37 ± 2.434; in 63 it was 11–15. Among these, 42 patients were of PV of which 4 had arterial limb diameter more than 15 microns. Among the patients with PPP, 14 had 11-15, 9 patients had <10. Among the psoriatic patients, 3 had 11-15. Mean venous limb diameter was 15.89 ± 3.131, top of the loop diameter was 14.41 ± 4.373, and length of the loop 152.51 ± 57.21. Only 3 patients had length of loop >300. A majority (83) of patients had loop length between 101 and 200. Seventeen patients had loop length <100 (Table 2, Table 3).
Table 2.
Capillaroscopy findings in different patterns of psoriasis.
| Capillaroscopy findings | Measurement (μm) | PV | PP | PV and PP | PsA |
|---|---|---|---|---|---|
| Mean capillary loop density | <4 | 0 | 0 | 0 | 0 |
| 4–6 | 11 | 7 | 3 | 2 | |
| 7–9 | 60 | 16 | 4 | 3 | |
| >9 | 2 | 2 | 0 | 0 | |
| Arterial limb diameter | <10 | 27 | 9 | 3 | 1 |
| 11–15 | 42 | 14 | 4 | 3 | |
| >15 | 4 | 2 | 0 | 1 | |
| Venous limb diameter | <15 | 36 | 14 | 5 | 4 |
| 16–20 | 31 | 8 | 2 | 1 | |
| >20 | 6 | 3 | 0 | 0 | |
| Top of loop diameter | <10 | 14 | 3 | 2 | 1 |
| 11–20 | 54 | 17 | 5 | 3 | |
| >20 | 5 | 5 | 0 | 1 | |
| Length of loop | <100 | 9 | 3 | 4 | 1 |
| 101–200 | 57 | 19 | 3 | 4 | |
| 201–300 | 6 | 1 | 0 | 0 | |
| >300 | 1 | 2 | 0 | 0 | |
| Crossed loops | 12 | 6 | 0 | 1 | |
| Ramified capillaries | 7 | 2 | 0 | 1 | |
| Hemorrhage | 2 | 0 | 0 | 1 | |
| Avascular area | 2 | 0 | 2 | 0 | |
| Subpapillary plexus | 3 | 0 | 0 | 0 |
PV, psoriasis vulgaris; PP, palmoplantar psoriasis; PsA, psoriatic arthritis.
Table 3.
Distribution of patients based on mean capillary loop density on nailfold capillaroscopy.
| Types of psoriasis | Mean capillary loop density (capillaries/mm) |
Total | |||
|---|---|---|---|---|---|
| <4 | 4–6 | 7–9 | >9 | ||
| PV | 0 | 11 | 60 | 2 | 73 |
| PP | 0 | 7 | 16 | 2 | 25 |
| PV + PP | 0 | 3 | 4 | 0 | 7 |
| PV + PsA | 0 | 2 | 3 | 0 | 5 |
| Total | 110 | ||||
PV, Psoriasis vulgaris; PP, Palmoplantar psoriasis; PsA, psoriatic arthritis.
Crossed loops/tortuous capillaries were seen in 17.3% of patients, whereas it was absent in the remaining 82.7%. This was highly significant (p value < 0.001). Ramified capillaries were seen in 9.1% of patients of psoriasis (p value < 0.001), visible in 20% patients of PsA followed by patients with PV and PPP in 10 and 8%, respectively.
Other abnormalities observed were hemorrhage seen in 2.72%, avascular areas 3.6%, subpapillary plexus in 2.72%; these were found to be not statistically significant (p > 0.05).
Of all patients, 81.8% of patients had regular and parallel distribution of capillaries and the rest 18.2% had irregular and haphazard distribution of capillaries (p value < 0.001).
Analysis of PASI score, age of the patient, and NFC did not reveal any statistically significant relationship.
Discussion
In this study, patients of different types of psoriasis, age groups, and on different treatments were studied. The age and gender distribution and the psoriasis pattern of our patients were consistent with reports in Indian population.12 Duration of illness ranged from 2 months to 25 yrs. All our cases were on treatment with 68.2% of patients on topical medications. Psoriasis with PASI>10 was present in 29% cases.
Abnormal capillary patterns have been reported in association with both PV and PsA. Four patterns on NFC based on the background and presence of abnormal capillaries have been described. Normal or close to normal with pink or pale pink background and few tortuous capillaries (I); Many tortuous coiled, ramified or ‘M’ shaped capillaries (II); Red background, edema and‘plaque-type’ capillaries (III) and Pale background, decreased number of capillaries and/or presence of frail and thin capillaries and well visible subpapillary venular plexus (IV). There was significant correlation between the occurrence of various types of capillaroscopic images and the presence of PsA. Half of the patients with PV had type I capillaroscopic image, one-third had type II, and 13.79% had type III. Type I and II occur in a majority of PV and PsA cases. Type IV was not seen in any of our PsA cases in contrast to their study. Homogeneous red globules have been considered the most significant dermoscopic finding in the psoriasis of darker skin.13
In this study, 84.5% of psoriasis cases had ‘inverse U’ shape of capillaries, whereas the rest manifested abnormal morphology. Bizarre morphology, ramified capillaries, and tortuosity were seen in patients with PV. Ramified/bushy capillaries reflect manifestation of extensive inflammation and increased blood flow leading to neoangiogenesis.14 Avascular areas were seen in both PV and PPP. There was no significant change noted in the patients who had PV with PPP. Megacapillary, decreased capillary density, haemorrhages were noticed in cases of PsA. Reports describe twisted and dilated venular branches or coiled, tortuous and short capillaries characteristic of PV, whereas a reduction in the capillary density, lower mean capillary length, a decreased diameter of afferent limb, and meandering capillaries with tight terminal convolutions, a visible weave,15 drop out,16 and a well visible subpapillary venular plexus were characteristic of PsA. Mean capillary density was subnormal (<9) in 76% of our study population.
Our study included patients on systemic therapy (some PV, PPP, and all PsA cases) in the form of methotrexate and biologicals, as well as on NBUVB. The relatively lesser or reversal of changes in these patients may be because a decrease in the vasoactive amines or endothelial factors responsible for the NFC findings on treatment by the systemic agents. Statistical inference was not significant with respect to individual treatment groups as the number of cases in these were small. A study of nailfold findings at the initial presentation of the disease hence would be required for patients who were on methotrexate or biologics. This would have given a better idea about the prognosis of the disease.
Patients with PV with irregular capillaries, reduced capillary bed density should be followed up to know and identify how many of them proceed to have abnormal NFC findings such as ramified capillaries, hence heralding possible PsA in future. Thereby the NFC can be used to assess prognosis in terms of development of arthritis.
None of these findings were associated with the duration of the disease or with its severity, as measured by the PASI score, or with the presence of arthritis by Vazquez-Lopez et al.14
Our study was limited by a smaller number of cases of clinical psoriasis with nail involvement. Hence an inference that nail involvement in psoriasis affects NFC could not be made. A larger study possibly with healthy controls and follow-up of psoriasis cases over a period of time shall reflect the true prognostic value of our findings and those reported in literature.
Conclusion
Epidermal proliferation and inflammatory changes along with microvascular abnormalities characterize psoriasis. Capillary changes progressing to abnormalities such as ramified/bushy pattern, reduced capillary density, or irregular capillaries amongst others serve to alert a progression to PsA. NFC, a non-invasive imaging technique for microcirculation evaluation can hence serve to prognosticate and follow-up patients with PV to PsA as a highly reproducible tool.17 Earlier institution of appropriate systemic therapy shall hence help reduce morbidity of PsA. NFC lacks specificity but is simple and an easy method to study the microvascular abnormalities in psoriasis.16
Conflicts of interest
The authors have none to declare.
References
- 1.Parisi R., Symmons D.P.M., Griffiths C.E.M., Ashcroft D.M. And the Identification and Management of Psoriasis and Associated Comorbidity (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol. 2013;133:377–385. doi: 10.1038/jid.2012.339. [DOI] [PubMed] [Google Scholar]
- 2.Stinco G., Lautieri S., Valent F., Patrone P. Cutaneous vascular alterations in psoriatic patients treated with cyclosporine. Acta Derm Venereol. 2007;87:152–154. doi: 10.2340/00015555-0216. 7. [DOI] [PubMed] [Google Scholar]
- 3.Riberio C.F., Siqueira E.B., Holler A.P., Fabricio L., Skare T.L. Periungual capillaroscopy in psoriasis. An Bras Dermatol. 2012;87:550–553. doi: 10.1590/s0365-05962012000400005. [DOI] [PubMed] [Google Scholar]
- 4.Hern S., Mortimer O.S. In vivo quantification of micro vessels in clinically uninvolved psoriatic skin and in normal skin. Br J Dermatol. 2007;156:122. doi: 10.1111/j.1365-2133.2007.07889.x. [DOI] [PubMed] [Google Scholar]
- 5.Goodfield M., Hull S.M., Holland D. Investigations of the active edge of plaque psoriasis: vascular proliferations precedes change in epidermal Keratin. Br J Dermatol. 1994;131:808–813. doi: 10.1111/j.1365-2133.1994.tb08582.x. [DOI] [PubMed] [Google Scholar]
- 6.Johann E.G., James T.E. Psoriasis. In: Goldsmith L.A., Katz S.I., Gilchrest B.A., editors. Fitzpatrick's Dermatology in General Medicine. 8th ed. Mc Graw Hill; New York: 2012. pp. 197–216. [Google Scholar]
- 7.Graceffa D., Amorosi B., Maiani E. Capillaroscopy in psoriatic and rheumatoid arthritis: a useful tool for differential diagnosis. Arthritis. 2013 doi: 10.1155/2013/957480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Angelis R., Bugatti L., Del Medico P., Nicolini M., Filosa G. Videocapillaroscopic findings in the microcirculation of the psoriatic plaque. Dermatology. 2002;204:236–239. doi: 10.1159/000057888. [DOI] [PubMed] [Google Scholar]
- 9.Rajaei A., Dehghan P. Farahani, Z. Nailfold capillaroscopy findings in diabetic patients (A pilot cross-sectional study) Open J Pathol. 2015;5:65–72. [Google Scholar]
- 10.Lambova S.N., Müller-Ladner U. The specificity of capillaroscopic pattern in connective autoimmune diseases. A comparison with microvascular changes in diseases of social importance: arterial hypertension and diabetes mellitus. Mod Rheumatol. 2009;19:600–605. doi: 10.1007/s10165-009-0221-x. [DOI] [PubMed] [Google Scholar]
- 11.Vasdev V., Bhakuni D., Bhayana A., Kamboj P. Nailfold capillaroscopy: a cost effective practical technique using digital microscope. Indian J Rheumatol. 2011;6:185–191. [Google Scholar]
- 12.Maldonado G., Guerrero R., Paredes C., Ríos C. Nailfold capillaroscopy in diabetes mellitus. Microvasc Res. 2017;112:41–46. doi: 10.1016/j.mvr.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Kaur I., Kumar B., Sharma V.K., Kaur S. Epidemiology of psoriasis in a clinic from North India. Indian J Dermatol Venereol. 1986;52:208–212. [PubMed] [Google Scholar]
- 14.Vázquez-López Francisco, Manjón-Haces José Antonio, Maldonado-Seral Cayetana, Raya-Aguado Cristina, Pérez-Oliva Narciso, Ashfaq A. Marghoob Dermatology. 2003;207:151–156. doi: 10.1159/000071785. [DOI] [PubMed] [Google Scholar]
- 15.Cutolo M., Sulli A., Pizzorni C., Accardo S. Nailfold videocapilla- roscopy assessment of microvascular damage in systemic sclerosis. J Rheumatol. 2000;27:155–160. [PubMed] [Google Scholar]
- 16.Výbohová D., Adamicová K., Mellová Y., Hešková G. Microvascular changes in relation to inflammation and epidermal hyperplasia in chronic cutaneous lesions of psoriasis vulgaris. Histol Histopathol. 2017:461–470. doi: 10.14670/HH-11-811. [DOI] [PubMed] [Google Scholar]
- 17.Bhusman M., Moore T., Herrick A., Griffiths C.E.M. Nail-fold video capillaroscopy in Psoriasis. Br J Dermatol. 2000;142:1171–1176. doi: 10.1046/j.1365-2133.2000.03544.x. [DOI] [PubMed] [Google Scholar]