Abstract
Acute coronary syndrome (ACS) admissions are common and costly. The association between comprehensive ACS care pathways, outcomes and costs are lacking. From 434,172 low-risk, uncomplicated ACS patients eligible for early discharge (STEMI 35%, UA/NSTEMI 65%) from the Premier database, we identified ACS care pathways, stratified STEMI vs. UA/NSTEMI, that included access site for PCI (trans-radial intervention (TRI) vs. trans-femoral intervention (TFI)) and length of stay (LOS). Associations with costs and outcomes (death, bleeding, acute kidney injury and myocardial infarction at 1-year) were tested using hierarchical, mixed-effects regression and projections of cost-savings with change in care pathways were obtained using modeling. In low-risk uncomplicated STEMI patients, compared with TFI and LOS≥3 days, a strategy of TRI with LOS<3 days and TFI with LOS<3 days were associated with cost-savings of $6,206 and $4,802, respectively. Corresponding cost-savings for UA/NSTEMI patients were $7,475 and $6,169, respectively. These care-pathways did not show an excess risk of adverse outcomes. We estimated that >$300 million could be saved if prevalence of the TRI with LOS<3 days and TFI with LOS<3 days strategies are modestly increased to 20% and 70%, respectively. In conclusion, we demonstrate the potential opportunity of cost-savings by repositioning ACS care pathways in low-risk and uncomplicated ACS patients, towards transradial access and a shorter LOS without an increased risk of adverse outcomes.
Keywords: Acute coronary syndrome, trans radial, radial access, costs, health care costs, percutaneous coronary intervention
INTRODUCTION
The staggering costs of acute coronary syndrome (ACS) hospitalization are unsustainable, and threaten the financial health of Medicare, Medicaid and the broader USA healthcare system.1-5 Approaches to reduce costs of ACS have been attempted but have led to modest, if any, reductions in cost.6,7 Alternative payment models, such as bundled payments, are a mechanism for payers to shift financial risk to hospitals and force them to improve the efficiency of care for patients presenting with AMI.1-5 In the current climate of health care reform,8 improved efficiency and lower costs of care offer the hospitals a competitive advantage to overcome the pressure of reimbursement challenges. For example, we have recently shown that a hospital could save nearly half million US$ by simply improving the efficiency of their care pathways for elective PCI patients.9 A similar economic evaluation of care pathways for ACS patients is lacking. We thus interrogated a large, national database to examine the costs associated with eight care pathways based on vascular access site and length of stay among patients undergoing PCI for low-risk and uncomplicated ACS.
METHODS
This study used the Premier database (https://www.premierinc.com/), representing ~20% of all acute care hospitalizations in the United States for over 15 years. The Premier database contains information on the socio-demographic characteristics, interventional procedures, medications, outcomes at the end of 1-year follow-up from index hospitalization and International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes for diagnoses and procedures as reported by the contributing hospitals.
The dataset used in this study covers a 13-year period from 2004 to 2016 during which 905,411 PCIs were performed for patients hospitalized with ACS. From this set of ACS patients, we excluded patients not eligible for earlier discharge by minimizing confounding due to four sources: i) patients with comorbidities, ii) patients undergoing complex PCI, iii) patients having complications after PCI, and iv) critically ill ACS patients. The set of exclusion criteria used here are based on clinical reasoning that complicated patients with complex procedures would not be eligible for a rapid discharge. These exclusions resulted in a final eligible pool of 434,172 (~48%) ACS patients from 478 US hospitals who represented a low-risk and uncomplicated ACS population potentially eligible for early discharge (Supplementary Figure 1).
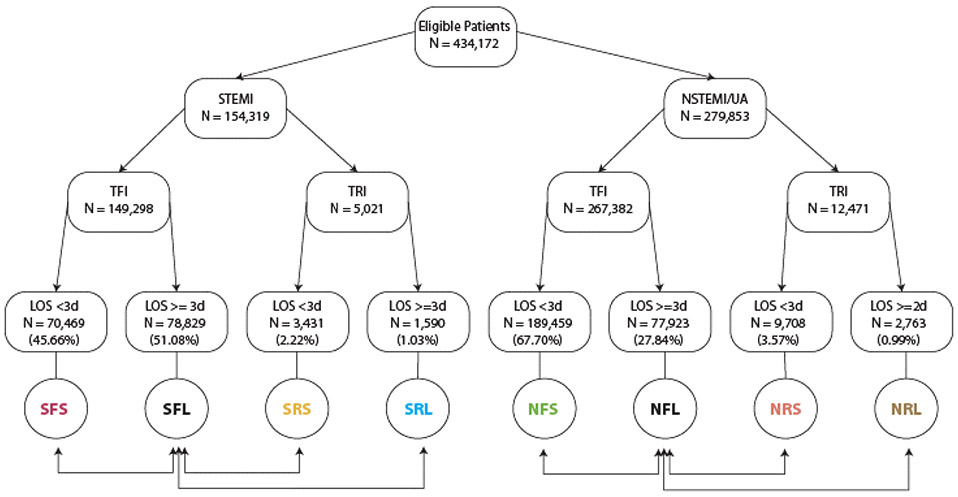
Considering that the standards of care differ across presence or absence of STEMI, we evaluated care pathways separately for STEMI and UA/NSTEMI patients. These ACS care pathways (shown in Figure 1) considered were combinations of three binary sub-divisions based on i) the presence of STEMI or UA/NSTEMI; ii) the use of transfemoral (TFI) or transradial intervention (TRI); and iii) a short or long length of hospital stay during index hospitalization, not explained by comorbidities, complex PCI, critical illness, or complications. Each care pathway was thus identified based on a three-letter acronym – the first letter indicated whether STEMI was present or absent (S or N, respectively); the second letter indicated TFI or TRI (F or R, respectively) and the third letter indicated a short or long length of stay (S or L, respectively). A short length of stay was defined as that shorter than 3 days – a time period considered reasonable for low risk STEMI and NSTEMI patients.10. Within each of these ACS types, we used the subgroup of TFI patients with a long length of stay as the reference group. Thus, there were three competing care pathways in each of the STEMI and UA/NSTEMI patients as indicated by the double headed arrows in Figure 1.
Figure 1. Schematic representation of the competing care pathways considered in this study.
Shown at the bottom of each pathway is an acronym-based and color-coded identification of each pathway. The double headed arrows indicate the comparisons conducted herein. Prevalence of each care pathway within the subgroups of STEMI and UA/NSTEMI patients is shown above each pathway acronym.
The primary endpoint of all the analyses was costs from a hospital perspective. Premier uses a micro-costing approach to report department-wise and total costs related to PCI and hospitalization. Costs were reported as total fixed, total variable and total costs. All the costs were inflation-adjusted to the 2016 US $. Information on death, bleeding events, acute kidney injury (AKI), acute myocardial reinfarction following the index PCI, stroke, repeat PCI and CABG was available at the end of 1-year follow-up from the date of PCI and were the secondary outcomes. The main predictor variable of interest was the eight care pathways defined above. We also included information on the following potential confounders: hospital characteristics – number of beds in the hospital, whether the hospital is a teaching hospital and hospital location; primary payer; socio-demographics of the patient, procedural characteristics and details; prior history of concomitant presence of 17 co-morbidities and medication use. Detailed description of these variables is provided in Table 1.
Table 1.
Characteristics of the patients and procedures
| Characteristic | STEMI (n=154,319) | UA/NSTEMI (n=279,853) | ||
|---|---|---|---|---|
| Hospital characteristics | ||||
| Total number of beds at hospital | ||||
| 000-099 | 1,455 | (0.94 %) | 3,012 | (1.08 %) |
| 100-199 | 11,578 | (7.50 %) | 19,246 | (6.88 %) |
| 200-299 | 21,048 | (13.64 %) | 32,729 | (11.70 %) |
| 300-399 | 34,318 | (22.24 %) | 57,434 | (20.52 %) |
| 400-499 | 26,173 | (16.96 %) | 51,208 | (18.30 %) |
| 500+ | 59,747 | (38.72 %) | 116,224 | (41.53 %) |
| Hospital Teaching | ||||
| No | 81,465 | (52.79 %) | 131,727 | (47.07 %) |
| Yes | 72,854 | (47.21 %) | 148,126 | (52.93 %) |
| Hospital - Urban/Rural | ||||
| Rural | 13,218 | (8.57 %) | 23,593 | (8.43 %) |
| Urban | 141,101 | (91.43 %) | 256,260 | (91.57 %) |
| General patient and hospitalization | ||||
| Age (years)* | 57.17 | (10.61 %) | 60.14 | (10.50 %) |
| Women | 38,495 | (24.95 %) | 87,821 | (31.38 %) |
| Married | 84,594 | (54.82 %) | 159,392 | (56.96 %) |
| Single | 51,534 | (33.39 %) | 86,826 | (31.03 %) |
| Other marital status | 18,191 | (11.79 %) | 33,635 | (12.02 %) |
| White | 112,658 | (73.00 %) | 202,227 | (72.26 %) |
| Black | 10,414 | (6.75 %) | 20,910 | (7.47 %) |
| Hispanic | 3,463 | (2.24 %) | 6,335 | (2.26 %) |
| Other race | 27,308 | (17.70 %) | 49,731 | (17.77 %) |
| Unknown race | 476 | (0.31 %) | 650 | (0.23 %) |
| Insurance Payor | ||||
| Medicare | 42,267 | (27.39 %) | 109,378 | (39.08 %) |
| Medicaid | 12,116 | (7.85 %) | 20,279 | (7.25 %) |
| Managed Care / Commercial | 72,277 | (46.84 %) | 116,811 | (41.74 %) |
| Self Pay | 16,758 | (10.86 %) | 17,893 | (6.39 %) |
| Other | 10,901 | (7.06 %) | 15,492 | (5.54 %) |
| AMI | 154,319 | (100.00 %) | 173,561 | (62.02 %) |
| Unstable angina | 6,749 | (4.37 %) | 126,617 | (45.24 %) |
| NSTEMI | 6,229 | (4.04 %) | 159,167 | (56.88 %) |
| STEMI | 154,319 | (100.00 %) | 8,131 | (2.91 %) |
| Heart failure | 11,495 | (7.45 %) | 24,691 | (8.82 %) |
| Cerebrovascular episode | 1,152 | (0.75 %) | 3,481 | (1.24 %) |
| Acute renal failure | 752 | (0.49 %) | 2,176 | (0.78 %) |
| COPD | 14,770 | (9.57 %) | 36,213 | (12.94 %) |
| Any type of cancer | 9,232 | (5.98 %) | 21,388 | (7.64 %) |
| Diabetes | 36,889 | (23.90 %) | 91,076 | (32.54 %) |
| Dyslipidemia | 106,283 | (68.87 %) | 213,935 | (76.45 %) |
| Hypertension | 95,511 | (61.89 %) | 211,075 | (75.42 %) |
| Smoking | 86,859 | (56.29 %) | 135,914 | (48.57 %) |
| Alcohol abuse | 2,101 | (1.36 %) | 3,341 | (1.19 %) |
| Drug abuse | 1,027 | (0.67 %) | 1,617 | (0.58 %) |
| PCI characteristics | ||||
| DES used | 107,410 | (69.60 %) | 224,352 | (80.17 %) |
| Multi-vessel PCI | 17,617 | (11.42 %) | 53,925 | (19.27 %) |
| Transradial access | 5,021 | (3.25 %) | 12,471 | (4.46 %) |
| Prasugrel used | 23,195 | (15.32 %) | 34,453 | (12.88 %) |
| Ticagrelor used | 14,871 | (9.82 %) | 20,301 | (7.59 %) |
| Outcomes at 1-year | ||||
| Mortality | 513 | (0.33 %) | 1,057 | (0.38 %) |
| Bleeding | 2,541 | (1.65 %) | 5,041 | (1.80 %) |
| Acute kidney injury | 1,927 | (1.25 %) | 4,438 | (1.59 %) |
| Acute myocardial infarction | 10,660 | (6.91 %) | 12,594 | (4.50 %) |
| Repeat PCI | 12,982 | (8.41 %) | 23,842 | (8.52 %) |
| CABG | 2,497 | (1.62 %) | 2,895 | (1.03 %) |
| Stroke | 994 | (0.64 %) | 2,048 | (0.73 %) |
In all analyses, to account for hospital-level clustering we used hierarchical, mixed effects regression models with the contributing hospital as the random effect. These models simultaneously included the three comparisons (within STEMI and UA/NSTEMI groups separately) and the results thus provided cost (or outcome) differential for all the candidate care pathways compared against the same reference pathway (Figure 1). To study the association of the care pathways with hospital costs we used mixed effects linear regression. To test the association of the care pathways with study outcomes we used mixed effects logistic regression models. Finally, to gauge the potential practice implications of the observed cost reductions, we conducted modeling studies 11 based on changing from a higher to a lower cost care pathway. Descriptive statistics included means (SD) for continuous variables and numbers (percentage) for categorical variables. All statistical analyses were conducted using Stata 12.0 (Stata Corp., College Station, TX). Significance was tested at a type 1 error rate of 0.05.
RESULTS
From a total of 905,411 eligible ACS PCI hospitalizations, we included 434,172 (47.9%) PCI hospitalizations from 478 US hospitals, with the number of patients per year ranging from a minimum of 54,329 in 2016 to a maximum of 85,484 in 2015. A total of 154,319 (35.5%) patients presented with STEMI. The characteristics of the study participants are detailed in Table 1. Briefly, the mean age was 59.1 years and most of the patients were males (70.1%) and white (72.5%). There was wide variation in hospitals characteristics, with most (40.5%) having 500 or more beds; 91.5% hospitals were urban and 50.9% were teaching hospitals. Medicare/Medicaid was the insurance payer for 42.4% of admissions. Multivessel PCI was performed in 16.5% of the procedures and as shown in Figure 1, TRI approach was used in 5,021 (3.3%) of STEMI PCIs and 12,471 (4.5%) of the UA/NSTEMI PCIs. TRI increased over time and in 2016 with 7,248 (13.3%) patients underwent TRI PCI. The prevalence of the eight care pathways was: in STEMI patients – SFS: 45.7%, SFL: 51.1%, SRS: 2.2%, SRL: 1.0%; in UA/NSTEMI patients NFS: 67.7%, NFL: 27.8%, NRS: 3.5% and NRL: 1.0%. During 1-year follow-up, as would be expected in this low-risk and uncomplicated ACS population, only 0.4% patients died, 1.8% had bleeding events, 1.5% had AKI events, 5.8% had AMI events and 0.7% had stroke.
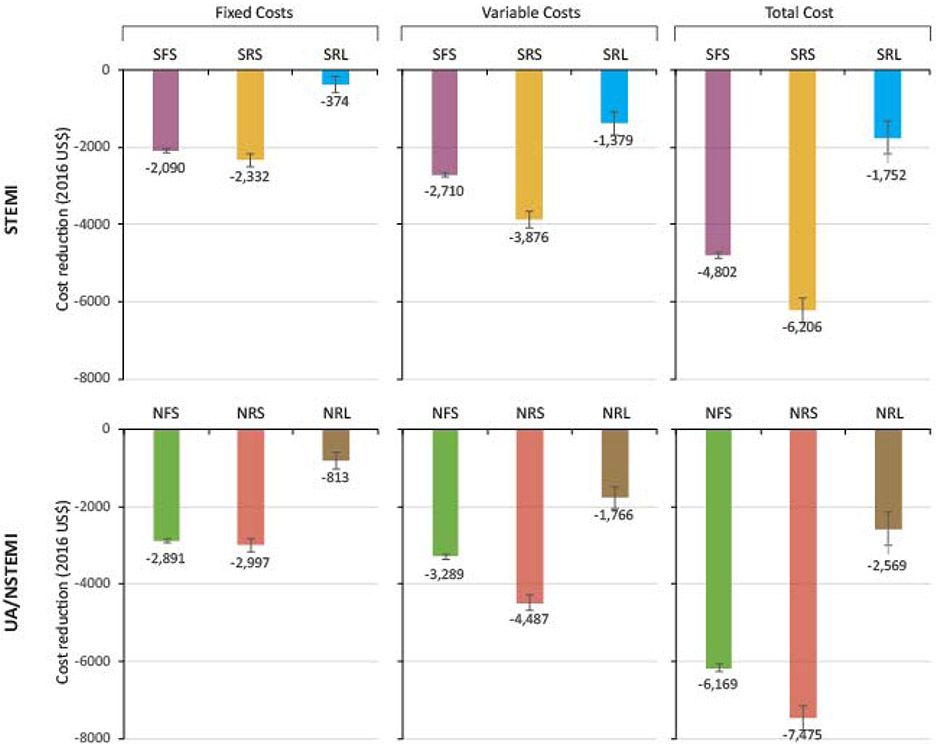
We first determined the costs in the STEMI patients that were associated with the SFS, SRS and SRL pathways as compared to the SFL reference pathway. Figure 2 shows that the SRS pathway (orange bars) was associated with the greatest cost reduction with $2,332 reduction in fixed costs, $3,876 reduction in the variable costs and $6,206 reduction in total hospitalization costs per patient. This group was followed by the SFS group (purple bars) with corresponding cost reductions of $2,090, $2,710 and $4,802, respectively. By comparison, the cost reductions associated with the SRL pathway (cyan bars) were smaller ($374, $1,379 and $1,752, respectively) albeit statistically significant. The detailed estimates of cost reductions along with their 95% confidence intervals for the STEMI patients are provided in Supplementary Table 1.
Figure 2. Cost reduction associated with the care pathways for ACS.
The bars are color-coded and match the color-coded pathways shown in Figure 2. Error bars indicate 95% confidence intervals. All cost reduction estimates were obtained using 2-level hierarchical, mixed effects linear regression models (separate for cost shown in the Figure) that used the contributing hospital as random effects. The model used inflation adjusted (to 2016 US$) cost as the dependent variable and the following predictor variables: the three care pathways simultaneously compared against the reference pathway, age, female gender, history of PCI, history of congestive heart failure, history of chronic obstructive pulmonary disease, history of diabetes, history of hypertension, multiple vessel affliction, use of bare metal stents, Medicare/Medicaid as the primary insurance payer, number of beds In the hospital, teaching hospital and hospital located in an urban area. Models were run separately for STEMI and UA/STEMI groups. Detailed results are provided in Supplementary Tables 1 and 2.
Concordant with the observations in the STEMI patients, those with UA/NSTEMI also demonstrated that the largest gains in cost reductions were associated with the NRS pathway, followed by the NFS group and then by the NRL group (Figure 2, Supplementary Table 2). In general, the corresponding cost reductions were greater for the UA/NSTEMI patients as compared to the STEMI patients (compare the bars in Figure 2 for STEMI to those for UA/NSTEMI patients). Across STEMI as well as UA/NSTEMI groups, the cost reduction was consistently more for the variable costs than for fixed costs (Figure 2). Notably, a comparison of the TRI versus TFI access pathways (when the length of stay was short) demonstrated a substantial cost reduction ($1,404 in STEMI patients and $1,306 in UA/NSTEMI patients).
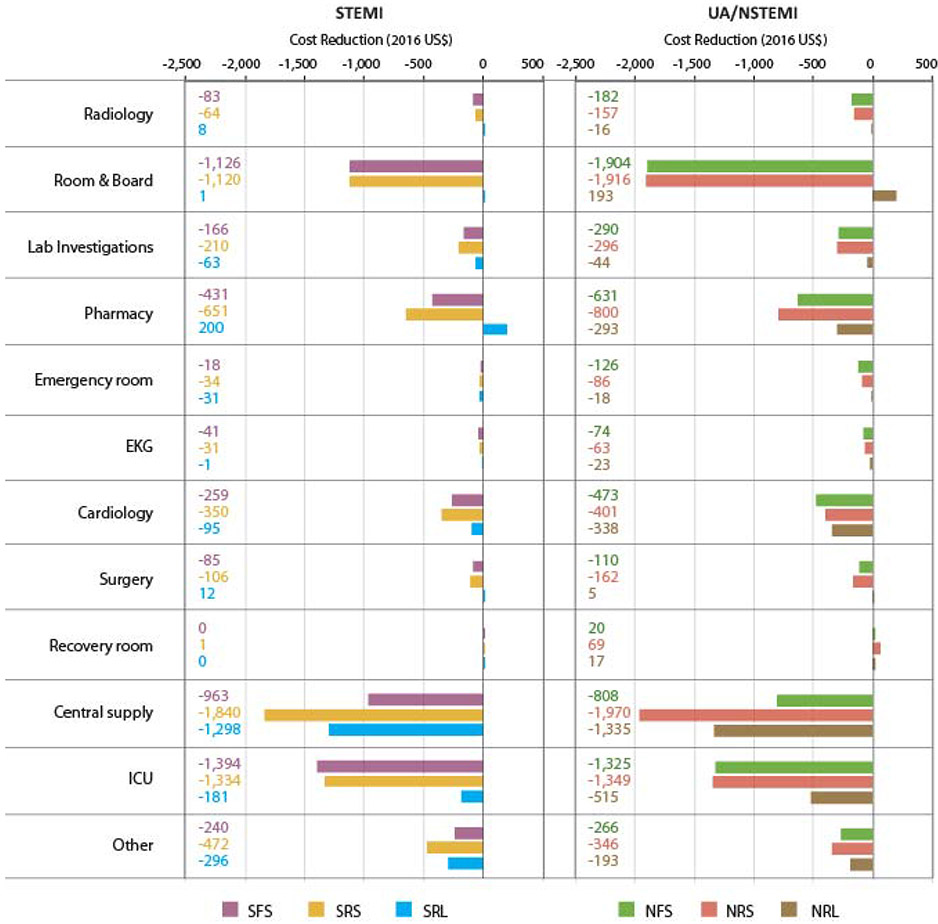
The micro-costing approach used in the Premier dataset permitted us to conduct the cost reduction analyses at the level of the contributing departments within the hospitals. For STEMI patients the cost reductions observed in the SFS and SRS strategies were primarily driven by the central supply, ICU stay and room and board departments (Figure 3, bar graph on left). In comparison, for the UA/NSTEMI patients the major cost reducing department was still central supplies, but the costs reduced via room and board exceeded those reduced through ICU stay. More conservative cost reductions were associated with cardiology, pharmacy and laboratory investigation departments both for STEMI and UA/NSTEMI patients. It is also noteworthy that the SRS and NRS strategies were associated with the largest cost reductions as compared to their respective reference pathways (orange and red bars in Figure 3), especially for the central supplies, ICU and Room and Board departments. Detailed cost reductions (along with their 95% confidence intervals) associated with each care strategy and each department are provided in Supplementary Tables 3 (STEMI) and 4 (UA/NSTEMI).
Figure 3. Department-wise drivers of total cost reduction based on care pathways.
Results are from 2-level, hierarchical, mixed effects models run separately for the STEMI and UA/NSTEMI groups and for each cost component shown. Model specification was the same as that mentioned in legend to Figure 3. Color-coded numbers show the cost reduction in 2016 US$. Detailed results are provided in Supplementary Tables 3 and 4.
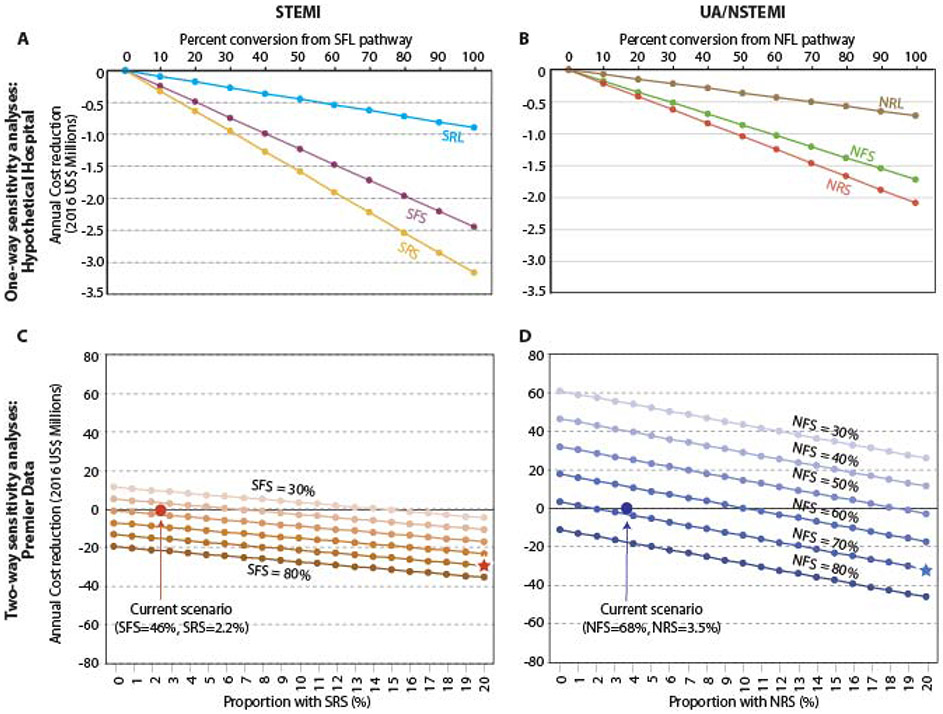
To gauge the potential practice implications of the observed cost reductions, we conducted modeling studies.11 We observed that the average, adjusted (for all the covariates mentioned in Figure 2 legend) per-patient hospitalization costs for STEMI and UA/NSTEMI patients were $14,202 and $13,892, respectively. In this study, the observed proportions of SFS and SRS care strategies were 46% and 2.2% while the proportions of the NFS and NRS strategies were 68% and 3.5%, respectively. We first conducted a set of one-way analyses for the scenario of a hypothetical hospital that conducts 1,000 PCIs annually for each of the STEMI and UA/NSTEMI conditions. By varying the proportion of the patients converting from the SFL (NFL for UA/NSTEMI) pathway to the SFS, SRS or SRL pathways (NFS, NRS and NRL for UA/NSTEMI) and using cost savings from Figure 2, we estimated the hypothetical hospital cost reductions. We observed (Figure 4A-B) that even if 50% of the SFL patients were to be managed by the SRS or SFS pathways then there would be a cost reduction of 1.6 and 1.2 million US$ per 1000 STEMI PCIs for the hypothetical hospital. Corresponding numbers for the UA/NSTEMI group were 1.0 and 0.9 million US$, respectively. The cost reductions associated with the SRL and NRL pathways were substantially smaller.
Figure 4. Results of modeling to predict the potential cost reduction associated with a shift of ACS care pathways.
(A-B) One-way sensitivity analysis for a hypothetical hospital that conducts 1,000 PCIs of each type of ACS. Results show the associated cost reductions when a given percentage of patients from the SFL pathway for STEMI (NFL for UA/NSTEMI) is converted to the candidate pathway. Per-patient hospitalization costs associated with each care pathway and adjusted for covariates mentioned in the legends to Figure 3 were obtained using 2-level hierarchical, mixed effects models. (C-D) Two-way sensitivity analyses. The proportion of the patients belonging to the SFS and SRS pathways for STEMI (NFS and NRS for UA/NSTEMI) was varied over a range of 30 – 70% and 0 – 20%, respectively. The resulting per patient costs were compared to the currently observed proportions (indicated using the colored circles). The results are shown as annual cost reduction in 2016 million US$. Hypothetical target of 70% SFS and 10% SRS groups is shown using color-coded stars.
While SRS and SFS strategies were associated with the most cost savings, we recognized that adopting transradial access in ACS patients, particularly STEMI patients, may be challenging. Therefore, we performed a two-way modeling where we retained a higher proportion of the SFS pathways while simultaneously varying a smaller proportion of SRS pathway to mimic the transradial learning curve.12,13 We found (Figure 4C-D) that the cost reductions were more sensitive (with steeper lines that were more widely spaced) for the UA/NSTEMI patients than for the STEMI patients. Even a small shift in care strategies aimed at increasing use of TRI and a shorter LOS is likely to be associated with substantial cost reductions. For example, in the context of low-risk and uncomplicated STEMI, if one sets a target of SRS=20% and SFS=70%, the cost reductions are likely to be as large as $29.2 million annually within the Premier database. If one were to set the same targets for UA/NSTEMI patients, then the estimated annual cost reduction would be $32.1 million. Considering that Premier data represents ~20% of all US PCIs, the total cost reduction across the nation could be ~$307 million if care pathways were to focus on modestly shorter length of stay and TRI.
Finally, we evaluated the clinical outcomes associated with the SFS/SRS and NFS/NRS care pathways at the end of 1 year of follow-up. The results of these analyses are shown in Supplementary Table 5 and demonstrated that except for the outcome of AMI, all the outcomes were significantly less likely in the SRS and NRS groups as compared to the respective reference groups. The SFS and NFS groups were consistently associated with all improved outcomes (except for repeat PCI for the NFS group, p = 0.7718). Together, the SFS/SRS and NFS/NRS pathways were not only associated with lower costs, but these pathways were also safe and associated with no excess risk of long-term outcomes following PCI.
DISCUSSION
In this first unique analysis of low risk and uncomplicated ACS care patterns across a national, large and real-world dataset from 478 US hospitals we make three key observations. First, there exists a large potential opportunity of cost savings by shifting ACS care approaches towards transradial access and a shorter length of hospital stay in low risk and uncomplicated ACS patients. From a practice stand-point, such a practice shift entails the need to determine pre-procedural risk of adverse outcomes. Tools to risk stratify and screen patients for identification of the low-risk ACS based on the exclusion criteria listed in Supplementary Figure 1 may be necessary. Low-risk and uncomplicated ACS thus identified can then be managed with a goal towards early discharge. In support of the transformative potential of care pathways to reduce healthcare costs, prior studies have shown that in patients undergoing elective PCIs a same-day discharge care pathway may reduce PCI costs by ~$3,000-5,000.9 An elective PCI same-day discharge care pathway implemented at the Barnes Jewish Hospital, St Louis, MO was associated with cost savings that surpassed these estimates.14 Second, patients with these different care strategies did not have an excess risk of adverse clinical outcomes as reflected by low 1-year rates of mortality, bleeding, AKI and stroke. Third, these ACS care strategies may have implications for the US healthcare system in the era of bundle payments or alternative payment models. We demonstrate that across US hospitals there exists a potential to save >$300 million annually providing hospitals the opportunity for sustenance in a challenging payment reform climate.8,15
The cost savings from the ACS care strategies studied here need to be placed in perspective of the total cost of care of ACS hospitalization. The average costs of a low-risk STEMI and UA/NSTEMI hospitalization were US$ 14,202 and 13,892, respectively. The average cost savings from the SRS and NRS pathways as compared to the traditional SFL and NFL pathways were US$ 6,206 and US$ 7,475, respectively. These represent as large as 44% and 54% cost savings, respectively. Furthermore, variable cost savings were greater in magnitude than fixed cost savings (Figure 3). Consistent with this observation, we found that reduction in the costs of room and board, ICU stay, and central supply departments were the major drivers of cast savings (Figure 4). We surmise that a reduction in length of stay would directly lead to a reduction in patient-specific resource costs such as those due to laboratory tests, medications, medical supplies, surgical supplies and nursing expenses thus leading to a greater reduction in variable costs. Considered together, these findings imply that hospitals that can embrace a shift towards these ACS care strategies in low and uncomplicated ACS patients with reliability, are likely to attain cost savings large in magnitude. Moreover, these cost savings are likely to be rapidly evident since they result from variables costs.16
It is noteworthy that the cost-savings attributable to such a practice change did not come with any added risks of adverse clinical outcomes in low-risk and uncomplicated ACS patients. The low incidence of adverse outcomes in this study is not surprising. There are at least two reasons for this. First, we chose a low-risk and uncomplicated ACS population expected to have good outcomes. Second and equally pertinent is that the past decade has seen tremendous advances in the technical and procedural aspects of coronary intervention. In that regard, the low rate of death, bleeding, AKI and AMI over the full year is reassuring.
Our study has following limitations. First, this is an observational study. Therefore, the study only reports associations and does not imply causal inference of cost savings with the care strategies studied. Large, randomized trials are needed to demonstrate direct benefits of ACS care pathways using the strategies discussed above. Second, classification of STEMI and UA/NSTEMI are derived from administrative codes with a possibility of potential misclassification. Third, we did not have angiographic details therefore we were unable to adjust for anatomic complexity. Fourth, long term outcomes have been ascertained via ICD-9 and ICD-10 codes, which could result in misclassification of outcomes. Fifth, although we chose low-risk and uncomplicated ACS population by applying extensive exclusion criteria, the clinical reasoning behind choice of transradial access and earlier discharge in these patients remains unknown. Lastly, there are likely unmeasured confounders in the selection of patients for TRI and short LOS that cannot be adjusted for in the analyses.
In conclusion, our study shows a simple, novel and modifiable repositioning of the existing ACS care strategies in US to achieve cost savings without compromising patient safety. Future prospective studies evaluating costs and outcomes guided by these principles are needed.
Supplementary Material
Acknowledgments
Dr. Amit P. Amin – is funded via a comparative effectiveness research KM1 career development award from the Clinical and Translational Science Award (CTSA) program of the National Center for Advancing Translational Sciences of the National Institutes of Health, Grant Numbers UL1TR000448, KL2TR000450, TL1TR000449 and the National Cancer Institute of the National Institutes of Health, Grant Number 1KM1CA156708-01; an AHRQ R18 grant award (Grant Number R18HS0224181-01A1), and is a consultant to Terumo. No sponsor participated in the design and conduct of the study, collection, analysis, or interpretation of the data, nor in the preparation, review, nor approval of the manuscript. Mr. House and Dr. Kulkarni had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Medicaid CfMa. BPCI Advanced., 2018. [Google Scholar]
- 2.Kuehn BM. Shifting Landscape for Bundled Payments for Heart Conditions. Circulation 2018;137:1740–1741. [DOI] [PubMed] [Google Scholar]
- 3.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Participation and Dropout in the Bundled Payments for Care Improvement Initiative. JAMA 2018;319:191–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jimenez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O'Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 5.King MW. Health Care Efficiencies: Consolidation and Alternative Models vs. Health Care and Antitrust Regulation - Irreconcilable Differences? Am J Law Med 2017;43:426–467. [DOI] [PubMed] [Google Scholar]
- 6.Tsai TC, Joynt KE, Wild RC, Orav EJ, Jha AK. Medicare's Bundled Payment initiative: most hospitals are focused on a few high-volume conditions. Health Aff (Millwood) 2015;34:371–380. [DOI] [PubMed] [Google Scholar]
- 7.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 8.Burns J Bundled payment: hospitals see the advantages, but face big challenges too. Hospitals & Health Networks 2013;87:26–31. [PubMed] [Google Scholar]
- 9.Amin AP, Pinto D, House JA, Rao SV, Spertus JA, Cohen MG, Pancholy S, Salisbury AC, Mamas MA, Frogge N, Singh J, Lasala J, Masoudi FA, Bradley SM, Wasfy JH, Maddox TM, Kulkarni H. Association of Same-Day Discharge After Elective Percutaneous Coronary Intervention in the United States With Costs and Outcomes. JAMA Cardiol 2018;3:1041–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swaminathan RV, Rao SV, McCoy LA, Kim LK, Minutello RM, Wong SC, Yang DC, Saha-Chaudhuri P, Singh HS, Bergman G, Feldman DN. Hospital length of stay and clinical outcomes in older STEMI patients after primary PCI: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol 2015;65:1161–1171. [DOI] [PubMed] [Google Scholar]
- 11.Amin AP, Patterson M, House JA, Giersiefen H, Spertus JA, Baklanov DV, Chhatriwalla AK, Safley DM, Cohen DJ, Rao SV, Marso SP. Costs Associated With Access Site and Same-Day Discharge Among Medicare Beneficiaries Undergoing Percutaneous Coronary Intervention: An Evaluation of the Current Percutaneous Coronary Intervention Care Pathways in the United States. JACC Cardiovasc Interv 2017;10:342–351. [DOI] [PubMed] [Google Scholar]
- 12.Hess CN, Peterson ED, Neely ML, Dai D, Hillegass WB, Krucoff MW, Kutcher MA, Messenger JC, Pancholy S, Piana RN, Rao SV. The learning curve for transradial percutaneous coronary intervention among operators in the United States: a study from the National Cardiovascular Data Registry. Circulation 2014;129:2277–2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ball WT, Sharieff W, Jolly SS, Hong T, Kutryk MJ, Graham JJ, Fam NP, Chisholm RJ, Cheema AN. Characterization of operator learning curve for transradial coronary interventions. Circulation: Cardiovasc Interv 2011;4:336–341. [DOI] [PubMed] [Google Scholar]
- 14.Amin AP, Crimmins-Reda P, Miller S, Rahn B, Caruso M, Pierce A, Dennis B, Pendegraft M, Sorensen K, Kurz HI, Lasala JM, Zajarias A, Bach RG, Kulkarni H, Singh J. Novel Patient-Centered Approach to Facilitate Same-Day Discharge in Patients Undergoing Elective Percutaneous Coronary Intervention. J Am Heart Assoc 2018;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Obama B United States Health Care Reform: Progress to Date and Next Steps. JAMA 2016;316:525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jegers M, Edbrooke DL, Hibbert CL, Chalfin DB, Burchardi H. Definitions and methods of cost assessment: an intensivist's guide. ESICM section on health research and outcome working group on cost effectiveness. Intensive Care Med 2002;28:680–685. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.