Abstract
To describe the delivery of care for patients with rheumatic and musculoskeletal diseases (RMDs) from the perspective of rheumatologists in the Netherlands during the first months of the COVID-19 pandemic. A mixed methods design was used with quantitative and qualitative data from a cross-sectional survey sent to all members of the Dutch Rheumatology Society in May 2020. The survey contained questions on demographics, the current way of care delivery, and also on usage, acceptance, facilitators and barriers of telemedicine. Quantitative data were analyzed descriptively. The answers to the open questions were categorized into themes. Seventy-five respondents completed the survey. During the COVID-19 pandemic, continuity of care was guaranteed through telephone and video consultations by 99% and 9% of the respondents, respectively. More than 80% of the total number of outpatient visits were performed exclusively via telephone with in-person visits only on indication. One-quarter of the respondents used patient reported outcomes to guide telephone consultations. The top three facilitators for telemedicine were less travel time for patients, ease of use of the system and shorter waiting period for patients. The top three barriers were impossibility to perform physical examination, difficulty estimating how the patient is doing and difficulty in reaching patients. During the COVID-19 epidemic, care for patients with RMDs in the Netherlands continued uninterrupted by the aid of telemedicine. On average, respondents were content with current solutions, although some felt insecure mainly because of the inability to perform physical examination and missing nonverbal communication with their patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00296-020-04771-6.
Keywords: Telemedicine, COVID-19, Rheumatic and musculoskeletal diseases
Introduction
In March 2020, the emerging COVID-19 pandemic created a compelling reason for in-person care alternatives. Due to lack of a vaccine or effective therapies at that time, social distancing and quarantine regulations were the only widely available interventions [1]. As a result, COVID-19 transformed the delivery of care with breathtaking speed. In particular, telemedicine was applied as a solution to continue care [2].
Telemedicine provides patient health care, public health and health education using telecommunication technologies. It aims to deliver care at a distance and encompasses a broad variety of technologies and methods, both synchronous and asynchronous [3]. Despite that appropriate technology has been available for virtually all modes of its delivery, telemedicine has seen only incremental growth in the past years. For example, in 2019, telemedicine was used by only 8% of people in the United States [4]. Various key barriers for wider adoption have been identified, including lack of knowledge of the possibilities by patients and providers, lack of incentives to change the established practice of in-person care, overall short travel distance to clinics, lack of comfort with telemedicine technologies, patient identification and privacy issues, and limited reimbursement [5, 6]. However, during the COVID-19 lockdown, in some settings telemedicine has seen an increase from 10% of patient contacts to 90% in only 1 week [7, 8].
The emerging literature on the role of telemedicine in response to COVID-19 has focused mainly on health informatics infrastructure aspects [9], primary care visits using mostly audio technologies [8] and the widespread adoption of video consultations among both patients and providers in a large US hospital setting [10]. As yet, there have been few reports specifically on telemedicine for patients with rheumatic and musculoskeletal diseases (RMDs) during the COVID-19 period. Online management of patients with rheumatoid arthritis and assessment of COVID-19 infection in a cohort of patients with systemic lupus erythematodes (SLE) using telemedicine has been shown to be feasible [11, 12]. The question has been posed whether we should be using the current sense of urgency created by the COVID-19 outbreak to prompt us to accelerate the transformation of our rheumatology service delivery into the technology age now [13].
In this report, we describe the results of a survey on the impact of the COVID-19 pandemic on the delivery of care using telemedicine for patients with RMDs from the perspective of rheumatologists in the Netherlands. We were particularly interested in how telemedicine was organized for patients with RMDs during the early months of the pandemic, which forms of telemedicine were used, how rheumatologists experienced this, which barriers arose, how rheumatologists assessed disease activity and what lessons were learned to promote the widespread adoption of telemedicine beyond the COVID-19 pandemic.
Methods
Design and research population
The CHERRIES checklist for reporting the results of Internet surveys was followed [14].
A mixed methods design was used with quantitative and qualitative data from a cross-sectional survey sent to all members of the Dutch Rheumatology Society, almost 2 months after the COVID-19 lockdown was put in place by the Dutch government on the March 12, 2020.
The survey was accessible from 8 to 22 May through an announcement plus link (see supplementary text S1) that was provided in the bi-weekly e-mail newsletter of the Dutch Rheumatology Society. Participation was voluntary. No incentives were used. A convenience sampling strategy was used. Survey items were not randomized. A completeness check was performed automatically before the survey was submitted. A back button was available for review of the responses. Usability and technical functionality were tested by the authors before fielding the survey. Data capture was automated via Google-forms. Completion rate, but not response, view and participation rates were monitored. Preventing multiple entries from the same individual was not monitored.
All participants gave informed consent for the use and publication of the survey data. Participants were aware of the length of the survey, which data were stored where and for how long, who the investigators were and what the purpose of the study was. No personally identifiable information was collected.
The Medical Research involving Human Subjects Act did not apply to this study and therefore did not require review by a medical ethics board.
Data-collection
The open survey was created ad hoc in Google-forms and consisted of two parts of in total 53 questions (see Supplementary Table S1 and S2) divided into 10 sections.
Part one contained questions on demographics of the study population, pre-COVID use of telemedicine, current state and satisfaction with care delivery, current use of telemedicine, how patients were informed about telemedicine, how rheumatologists were informed about the patient’s disease activity during the COVID-19 pandemic and two open questions on positive and negative experiences about care delivery during the COVID-19 pandemic. Usage was self-reported.
Part two contained questions on usage, usability/acceptance and facilitators/barriers of telemedicine. Usage was self-reported. Acceptance was operationalized by nine statements derived and adapted from the technology acceptance model [15] and telehealth usability questionnaire [16] and contained statements on ease of use, satisfaction, time and energy costs, motivation, ease of learning and added value that were scored on a five-point Likert scale (range strongly disagree, strongly agree). Potential facilitators and barriers were derived and adapted from a recent review on barriers and facilitators that influence synchronous telemedicine health services in a variety of medical conditions [17] with the addition of several items that had recently been experienced by the authors. These items were surveyed via a check-box question with multiple possible answers and a free text field for additional comments.
Statistics
All available data were analyzed. All questions excluding the open questions were mandatory. A sample size calculation was not performed. Quantitative data were analyzed descriptively using Excel for Mac version 16.38. The answers to the open questions were categorized into themes by going back and forward between answers and the list of themes. Each time an answer was given that could not be categorized into one of the themes available so far, a new theme was added.
Results
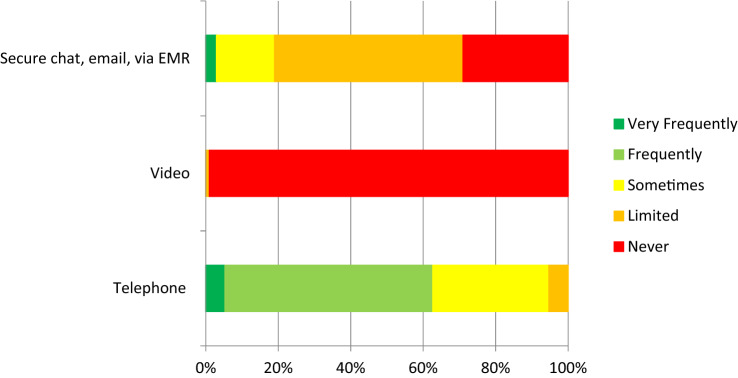
Seventy-five members of the Dutch Rheumatologist Society completed the survey, which corresponds with 17% of all active members. The majority of respondents (76%) was aged between 35 and 54 years, and 52 (69%) were female (Table 1). Nearly all were working as a rheumatologist (90%), mostly in non-academic hospitals (68%). Most respondents had already been using telephone consultations in the pre-COVID-19 era (Fig. 1). Some were also familiar with chat, email or e-consultations using electronic medical records (EMR). Only 1% had previously used video calls for follow-up of their patients. During the lockdown, continuity of care was guaranteed through telephone and video consultations by 74 (99%) and 7 (9%) of the respondents, respectively. More than 80% of all outpatient consultations were performed exclusively via telephone, with in-person visits only for specific indications (for example, arthritis requiring joint aspiration or injection). The use of e-consultation via EMR, chat or email remained limited (Online supplementary Fig. 1).
Table 1.
Baseline characteristics respondents
| Characteristic | Respondents (n = 75) |
|---|---|
| Age categories (years) | |
| < 34 | 7 (9%) |
| 35–44 | 30 (40%) |
| 45–54 | 27 (36%) |
| 55–65 | 10 (13%) |
| > 65 | 1 (1%) |
| Sex | |
| Female | 52 (69%) |
| Male | 23 (31%) |
| Occupation | |
| Rheumatologist | 68 (90%) |
| Fellow in rheumatology | 5 (7%) |
| Specialized rheumatology nurse | 2 (3%) |
| Work setting | |
| Non-academic hospital | 52 (68%) |
| Academic hospital | 14 (19%) |
| Specialized rheumatology clinic | 10 (13%) |
Fig. 1.
Experience with telemedicine consultations in the pre-COVID-19 era (n = 75). *EMR Electronic medical record
During the remote consultations, the care providers were informed about the disease activity of their patients in several ways. Nearly all respondents (74/75, 99%) inquired about this on the phone, 69 (92%) had access to the recent laboratory results, 19 (25%) of the respondents used an electronic patient reported outcome measure (ePROM) before or during telemedicine visits, and 3 (4%) reported inspection of the joints during video consultations.
The respondents (n = 75) rated the quality of their current care delivery on average with 7 (SD 1.0) on a 0–10 scale. Remote consultations were perceived positively in stable patients, who were well known to the rheumatologists respondents (Table 2). Many also liked to use this as a triage tool and it was considered as patient-friendly. On the other hand, several respondents felt insecure about remote consultations, mainly because of being unable to perform physical examination and of missing nonverbal communication with their patients. Both under- and overtreatment was feared. Furthermore, telephone consultations were not considered to be more efficient than physical contacts, due to many questions that patients asked, language barriers, difficulty in rounding off a consultation and several additional administrative tasks that were necessary for payment of the consultation.
Table 2.
Explanations for rating of remote care during the COVID-19 pandemic (n = 63)
| Theme | Positive explanations |
|---|---|
| Delivery of care | Continuity of care is guaranteed, including checking laboratory results, prescribing drugs |
| Good estimation of how a patient is doing | |
| Communication | Good way of reassuring patients |
| Organization | Avoiding creation of a pool of patients waiting for a consultation, reducing waiting list, reducing waiting time |
| Good way of triage (call first, in-person consultation only on indication) | |
| Patient-friendly, no travel time, no need to take a day off from work for patient | |
| Patient characteristics | Easy to do with well-known patients |
| No problem in stable patients, equals physical consultations | |
| Other | Less physical contacts reduce possibility of COVID-19 transmission |
| Sufficient for the time being |
| Theme | Negative explanations |
|---|---|
| Delivery of care | No possibility to do physical examination or interventions (i.e., local injections) |
| Difficult to estimate disease activity | |
| Difficult to estimate whether it is a problem of the joint versus tendon or inflammatory versus degenerative disease | |
| Delay expected in patients avoiding laboratory checks or contacting rheumatologist, fear of coming to hospital | |
| Communication | Lack of nonverbal communication |
| Less effective transfer of information | |
| Difficulty in rounding off consultation | |
| Organization | Time needed (equals in-person consultations) |
| Many additional administrative tasks | |
| Postponement of actual care | |
| Patient characteristics | Difficult with language barrier |
| Not possible for new patients, physical examination is mandatory | |
| Personal feelings | Insecurity, fear of missing diagnosis/fear of missing flares |
| Feeling of suboptimal care delivery | |
| Difficult to check whether patient was satisfied with consultation | |
| Feeling less connected with patient | |
| Fear of under- and overtreatment through remote consultations |
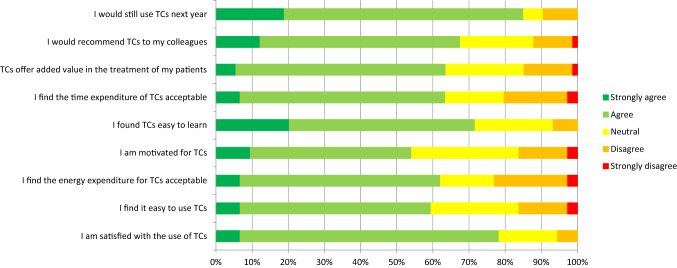
Most respondents (strongly) agreed with the statements on acceptance of the telephone consultations and expect to continue its use next year (Fig. 2). The results for video consultations are not shown due to the low number of respondents that had experience with this mode of delivery (n = 7).
Fig. 2.
Acceptance of telephone consultations (n = 74). TCs Telephone consultations
The respondents (n = 74) experienced several facilitating factors, but also barriers, for the use of telephone consultations during the COVID-19 pandemic. The top three facilitators listed were less travel time for patients, ease of use of the system and shorter waiting time for patients. The top three barriers listed were impossibility to perform physical examination, difficulty in estimating how the patient is doing and difficulty in reaching patients. Facilitators and barriers reported by more than 10 respondents are shown in Table 3. Interestingly, 6 out of 19 (32%) of respondents who used an ePROM reported difficulty estimating how the patient is doing as one of the barriers for telemedicine versus 35 out of 56 (63%) of respondents who did not use an ePROM during telemedicine visits.
Table 3.
Facilitators and barriers for use of telephone consultations during the COVID-19 pandemic
| Respondents (n = 74) | |
|---|---|
| Facilitators | |
| Less travel time for patients | 56 (76%) |
| Ease of use | 36 (49%) |
| Shorter waiting time for patients | 33 (45%) |
| Familiarity with the telephone system | 24 (32%) |
| Facilitative support from organization | 13 (18%) |
| Lower workload | 12 (16%) |
| Barriers | |
| Impossibility to perform physical examination | 53 (72%) |
| Difficulty estimating how the patient is doing | 43 (58%) |
| Difficulty in reaching patients (i.e., phone not being answered) | 42 (57%) |
| Preference for in-person consultation by patients | 33 (45%) |
| Language barrier by patients | 32 (43%) |
| Limited organizational support to convert consultation from in-person to telephone visit | 28 (38%) |
| Less access to care | 27 (37%) |
| Impossibility to conduct additional testing on a short term | 20 (27%) |
| Age of the patients | 17 (23%) |
| Delayed diagnostic or therapeutic trajectory | 15 (20%) |
| Technical issues (i.e., insufficient sound quality) | 12 (16%) |
| Less patient attention for the consultation (distracting factors at home/on the road) | 12 (16%) |
In the open questions, many respondents (n = 67) expressed positive experiences with telemedicine and would recommend continuing its use in the future (Table 4). In particular, when remote consultations were supported by ePROMs, many respondents indicated that only one annual physical visit would suffice for a large group of patients with stable chronic inflammatory diseases. Also, in patients with gout and polymyalgia rheumatica, remote consultations were considered a viable alternative. Remote consultations were also reported to be an eye-opener for patients, i.e., that comparable care could be delivered without traveling to the hospital. Important prerequisites for continued remote care delivery are equal payment and ICT support.
Table 4.
Positive and negative experienceswith remote care
| Positive experiences that should be continued in the post-COVID era (n = 67) |
|---|
| More often use of telephone consultations, replacing physical contacts |
| Continued willingness of organization to speed up ehealth |
| Eye-opener for patients |
| Patient-friendly, no travel time, no need to mobilize family for travels |
| No crowded waiting rooms |
| Combination of telephone consultations and electronic PROM |
| No difference in payment of remote and physical consultations |
| Flexibility in consultations |
| Through apps possible to draw attention to important aspects of disease or treatment |
| Negative experiences that should not be continued in the post-COVID era (n = 64) |
| Full day telephone or video consultations is exhausting |
| Poor availability of patients by phone |
| Many decision moments while insufficient information available |
| No physical examination |
| Difficult to estimate disease activity |
| No personal interaction with patients |
| Not suitable for all patients |
On the other hand, respondents (n = 64) also expressed negative experiences. Respondents experienced a full day of remote consultations as exhausting. Not all patients could easily be reached by phone, giving a feeling of frustration to the care providers respondents. Several decisions need to be made during a consultation, such as whether or not to continue current therapy and when to plan a follow-up visit. The lack of information on disease activity, because physical examination could not be done, patients sometimes refused or were unable to have laboratory tests performed and the absence of ePROMs made some respondents feel insecure. Respondents also missed personal interaction with their patients, as remote consultations frequently had a more formal character. Remote consultations were considered to be unsuitable for new patients, the elderly, those with language barriers, and for patients with only one annual visit.
Discussion
In this study, we report the experience of members of the Dutch Rheumatology Society with telemedicine during the early months of the COVID-19 pandemic. In this period, respondents were acutely forced to change their practice. Coming from a situation with a high density of hospital-based rheumatology practices, with high accessibility for face-to-face consultations for new and regular rheumatic patients and with protocolized high frequency of planned follow-up visits for patients with active disease, now most rheumatologists could continue delivering care to patients through telephone consultations only (99%) and to a lesser extent through video calls (9%). These results are in line with a report from Columbia, reporting continuity of care mostly via telemedicine (92%) [18]. In contrast, surveys done in the Arab world, China and India describe a 65% percent decrease in outpatient clinic visits, cancellation of most outpatient services, and a mere 10% of physicians being able to continue their clinics, respectively [12, 19, 20]. As expected, these results suggest large differences around the world in the continuity of care for patients with RMDs during the COVID pandemic.
Most respondents already had (some) experience with telephone consultations in the pre-COVID-19 era, but not with video consultations, asynchronous forms of communication or electronic PROM use, which did not change much either during the lockdown. On average, the respondents were content with current solutions for remote care, although some felt insecure mainly because of the inability to perform physical examination and missing nonverbal communication with their patients. Interestingly, the sudden experience with telemedicine has led to a change in mind set of respondents, and many of them would now recommend to continue its use of in the future, in particular in patients that are well-known to them, with stable chronic inflammatory disease, and when supported by electronic PROMs.
Our results showed high acceptance of telephone consultations by rheumatologists. This is in line with a two recent Italian reports describing positive experiences with telemedicine (telephone and video) consultations in SLE and psoriatic arthritis during the COVID pandemic [11, 21]. From the pre-COVID period, two 2017 reviews showed that feasibility and satisfaction rates were generally high across various telemedicine intervention types and that telemedicine may provide a well-accepted way to remotely deliver consultations, monitor disease activity and manage treatment in patients with RMDs [3, 22].
On the other hand, our results showed low adoption of video consultations and asynchronous forms of communication. Unfortunately, our survey prohibits any conclusions on the underlying reasons. We can speculate based on personal observations that most organizations in the Netherlands were not ready to deliver video consultations or secure asynchronous communication on a large scale, because the ubiquitous availability of rheumatologists and short travel distance for patients prevented pre-COVID transformation of this type of care delivery. Since the COVID-19 pandemic created a compelling incentive to change the established practice of in-person care, it will be interesting to see whether the adoption of these forms of communication will continue to rise in the coming months.
The most frequently reported barrier of telemedicine was the inability to perform physical examination. Most respondents relied on inquiry or the laboratory results to be informed about disease activity during remote consultations, while 25% used ePROMs. Despite that ePROMs are widely used in clinical trials in patients with RMDs, they have not yet found broad application in routine clinical practice [23]. Nevertheless, ePROMs could facilitate remote care in several ways: They can serve as a proxy for measuring disease activity [24], they can be incorporated in telemonitoring strategies to optimize disease control [25] and in algorithms to improve the number and timing of face-to-face consultations of patients with their rheumatologists [26, 27], and they can facilitate in addressing the concerns that people with RMDs may have [28]. Although not a subject of our study, a patient-derived disease activity score may also be used as a proxy for physical examination [29]. The use of a self-reported tender joint count has shown moderate to marked correlation with those performed by a trained assessor; however, swollen joint counts demonstrated lower levels of correlation [30]. Another interesting option may be assessment of joint involvement during video consultations by systematic virtual examination as was recently published in an orthopedic setting [31], but data for patients with RMDs are lacking.
Our study has several limitations. First, this study was performed in setting of the Dutch healthcare system and may therefore not be generalizable to other parts of the world. We encourage our colleagues from other countries to report their experiences for comparison. Second, selection bias may have occurred, because a convenience sampling strategy was used and only approximately 17% of members of the Dutch Rheumatology Society responded. Third, the survey was created ad hoc and was not validated prior to use in this study. Some of the questions on acceptance were derived from validated questionnaires [15, 16]. Fourth, the survey covered only a short period of a temporary change in the delivery of care. We do not know whether the positive experiences will last in the long term and what the effect of telemedicine on the quality of care delivered in RMDs will be.
Telemedicine may be an efficient way of care delivery, because it can reduce the number of in-person visits. However, we have seen in this survey that the time spend on a teleconsultation equals that of in-person visits. It may also not be as easy as is often assumed. It entails new skills from both patients and care providers, and technical issues also play an important role in conducting a smooth conversation with the patient. Furthermore, there may be issues with payment of this type of care delivery. Fortunately, in response to the COVID-19 lockdown, healthcare insurers across the world, including the Netherlands, have quickly expanded coverage to include all telemedicine visit types [32].
Despite some drawbacks that became clear in this survey, we would recommend to continue experimenting with telemedicine in RMDs, for example by replacing in-person visits with remote monitoring or video consultations. This is in line with current recommendations for the management of patients with RMDs during the ongoing COVID pandemic [33, 34]. The use of ePROMs may facilitate this [28]. We would also recommend incorporating the use and possibilities of telemedicine into the training programs of rheumatology fellows, to better prepare them for future rheumatology practice. Furthermore, it is important that our patients should be actively informed of the availability of this way of care delivery.
In conclusion, the COVID-19 pandemic rapidly changed the delivery of care for patients with RMDs in the Netherlands. Several lessons were learned. Continuity of care for patients with RMDs can be guaranteed through telemedicine. Currently this occurred mainly through telephone consultations, while adoption of other forms of telemedicine (e.g., asynchronous communication and video consultations) was still low. On average, respondents were content with current solutions, although some felt insecure mainly because of the inability to perform physical examination and missing nonverbal communication with their patients. We hope that the future will show that the COVID-19 pandemic was the turning point for the adoption of telemedicine in RMDs, although we realize it will never entirely replace in-person consultations.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank all participating members of the Dutch Rheumatology Society for providing their experiences, Maaike Gerards for her critical review of the survey and Bart Seppen and Jim Wiegel for their useful comments on the first draft of the manuscript.
Author contributions
All authors contributed to the study conception and design. Material preparation and data collection was performed by WB. Analyses were performed by WB and AT. All authors contributed to the interpretation of data for the study. The first draft of the manuscript was written by WB and all authors revised it critically for important intellectual content. All authors read and approved the final version of the manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.’
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Conflict of interest
Dr. Bos reports grants and personal fees from Abbvie, grants and personal fees from Eli Lilly, personal fees from Galapagos, grants and personal fees from Sanofi, grants from Celgene, grants from Pfizer, grants from Roche, grants from UCB, all outside the submitted work; Dr. van Tubergen reports grants from Pfizer, grants from Abbvie, grants from UCB, grants and personal fees from Novartis, grants from Biogen, all outside the submitted work; Dr. Vonkeman reports grants and/or personal fees for lectures and advisory boards and/or travel reimbursement from Abbvie, Amgen, AstraZeneca, BMS, Celgene, Celltrion, Galapagos, Gilead, GSK, Janssen-Cilag, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi-Genzyme, all outside the submitted work.
Ethics approval
The Medical Research involving Human Subjects Act did not apply to this study and therefore did not require review by a medical ethics board.
Consent to participate and publication
All participants gave informed consent for the use and publication of the survey data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wouter H. Bos, Email: w.bos@reade.nl
Astrid van Tubergen, Email: a.van.tubergen@mumc.nl.
Harald E. Vonkeman, Email: h.vonkeman@mst.nl
References
- 1.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19) JAMA. 2020;324(8):782. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 2.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 3.McDougall JA, Ferucci ED, Glover J, Fraenkel L. Telerheumatology: a systematic review. Arthritis Care Res. 2017;69(10):1546–1557. doi: 10.1002/acr.23153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AmericanWell Telehealth Index: 2019 Consumer Survey. (2019). https://static.americanwell.com/app/uploads/2019/07/American-Well-Telehealth-Index-2019-Consumer-Survey-eBook2.pdf. Accessed 29 Jul 2020
- 5.Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018;24(1):4–12. doi: 10.1177/1357633X16674087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med. 2016;375(2):154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 7.Santos-Moreno P, Chavez-Chavez J, Hernández-Zambrano SM, Rivera-Triana DP, Castiblanco-Montañez RA, Aza A, et al. (2020) Experience of telemedicine use in a big cohort of patients with rheumatoid arthritis during COVID-19 pandemic. Ann Rheum Dis. 10.1136/annrheumdis-2020-218193 [DOI] [PubMed]
- 8.Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly Converting to “Virtual Practices”: Outpatient Care in the Era of Covid-19. NEJM Catal. 2020;1(2):1–5. [Google Scholar]
- 9.Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, et al. Rapid response to COVID-19: Health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27(6):853–859. doi: 10.1093/jamia/ocaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mann DM, Chen J, Chunara R, Testa PA, Nov O. (2020) COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Informatics Assoc 1;27(7):1132–5. [DOI] [PMC free article] [PubMed]
- 11.Bozzalla Cassione E, Zanframundo G, Biglia A, Codullo V, Montecucco C, Cavagna L. (2020) COVID-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine. Ann Rheum Dis. 10.1136/annrheumdis-2020-217717 [DOI] [PubMed]
- 12.Zhang Y, Wang J, Zhao L, Xiao J, Shi Z. (2020) Online management of rheumatoid arthritis during COVID-19 pandemic. Ann Rheum Dis. 10.1136/annrheumdis-2020-217548 [DOI] [PubMed]
- 13.Jethwa H, Abraham S. Should we be using the Covid-19 outbreak to prompt us to transform our rheumatology service delivery in the technology age? Rheumatology. 2020;59(7):1469–1471. doi: 10.1093/rheumatology/keaa218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eysenbach G. Improving the quality of web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6(3):1–6. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahimi B, Nadri H, Afshar HL, Timpka T. A systematic review of the technology acceptance model in health informatics. Appl Clin Inform. 2018;9(3):604–634. doi: 10.1055/s-0038-1668091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parmanto B, Lewis AN, Jr, Graham KM, Bertolet MH. Development of the Telehealth Usability Questionnaire (TUQ) Int J Telerehabil. 2016;8(1):3–10. doi: 10.5195/IJT.2016.6196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almathami HKY, Win KT, Vlahu-Gjorgievska E. (2020) Barriers and Facilitators That Influence Telemedicine-Based, Real-Time, Online Consultation at Patients’ Homes: Systematic Literature Review. J Med Internet Res. 2020;22(2):e16407. doi: 10.2196/16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bozzalla Cassione E, Zanframundo G, Biglia A, Codullo V, Montecucco C, Cavagna L (2020) Response to: ‘Experience of telemedicine use in a big cohort of patients with rheumatoid arthritis during COVID-19 pandemic’ by Santos-Moreno et al. Ann Rheum Dis. 10.1136/annrheumdis-2020-218193 [DOI] [PubMed]
- 19.Ziadé N, Hmamouchi I, el Kibbi L, Abdulateef N, Halabi H, Abutiban F, et al. The impact of COVID-19 pandemic on rheumatology practice: a cross-sectional multinational study. Clin Rheumatol. 2020;39(11):3205–3213. doi: 10.1007/s10067-020-05428-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta L, Misra DP, Agarwal V, Balan S, Agarwal V. (2020) Response to: ‘Telerheumatology in COVID-19 era: a study from a psoriatic arthritis cohort’ by Costa et al. Ann Rheum Dis. 10.1136/annrheumdis-2020-218193 [DOI] [PubMed]
- 21.Costa L, Tasso M, Scotti N, Mostacciuolo E, Girolimetto N, Foglia F, et al. Telerheumatology in COVID-19 era: a study from a psoriatic arthritis cohort. (2020) Ann Rheum Dis. 10.1136/annrheumdis-2020-217806 [DOI] [PubMed]
- 22.Piga M, Cangemi I, Mathieu A, Cauli A. Telemedicine for patients with rheumatic diseases: Systematic review and proposal for research agenda. Semin Arthritis Rheum. 2017;47(1):121–128. doi: 10.1016/j.semarthrit.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 23.Fautrel B, Alten R, Kirkham B, de la Torre I, Durand F, Barry J, et al. Call for action: how to improve use of patient-reported outcomes to guide clinical decision making in rheumatoid arthritis. Rheumatol Int. 2018;38(6):935–947. doi: 10.1007/s00296-018-4005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hendrikx J, de Jonge MJ, Fransen J, Kievit W, van Riel PL. Systematic review of patient-reported outcome measures (PROMs) for assessing disease activity in rheumatoid arthritis. RMD Open. 2016;2(2):e000202. doi: 10.1136/rmdopen-2015-000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salaffi F, Carotti M, Ciapetti A, Di Carlo M, Gasparini S, Farah S, et al. Effectiveness of a telemonitoring intensive strategy in early rheumatoid arthritis: Comparison with the conventional management approach. BMC Musculoskelet Disord. 2016;17(1):1–11. doi: 10.1186/s12891-016-1002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hendrikx J, Fransen J, Van Riel PLCM. Monitoring rheumatoid arthritis using an algorithm based on patient-reported outcome measures: A first step towards personalised healthcare. RMD Open. 2015;1(1):e000114. doi: 10.1136/rmdopen-2015-000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Thurah A, Stengaard-Pedersen K, Axelsen M, Fredberg U, Schougaard LMV, Hjollund NHI, et al. Tele-Health Followup Strategy for Tight Control of Disease Activity in Rheumatoid Arthritis: Results of a Randomized Controlled Trial. Arthritis Care Res. 2018;70(3):353–60. doi: 10.1002/acr.23280. [DOI] [PubMed] [Google Scholar]
- 28.Taylor PC. Adopting PROs in virtual and outpatient management of RA. Nat Rev Rheumatol. 2020;16(9):477–8. doi: 10.1038/s41584-020-0449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leung AMH, Farewell D, Lau CS, Choy EHS. Defining criteria for rheumatoid arthritis patient-derived disease activity score that correspond to Disease Activity Score 28 and Clinical Disease Activity Index based disease states and response criteria. Rheumatology. 2016;55(11):1954–8. doi: 10.1093/rheumatology/kew279. [DOI] [PubMed] [Google Scholar]
- 30.Barton JL, Kaiser R, Criswell LA, Chen Y-H, Schillinger D. Systematic review and metaanalysis of patient self-report versus trained assessor joint counts in rheumatoid arthritis. J Rheumatol. 2009;36(12):2635–41. doi: 10.3899/jrheum.090569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the Era of COVID-19. J Bone Jt Surg. 2020;102(12):e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NZA past regelgeving aan vanwege coronavirus (Dutch) (2020) https://www.nza.nl/actueel/nieuws/2020/03/13/nza-past-regelgeving-aan-vanwege-coronavirus. Accessed 29 Jul 2020
- 33.Morales-Torres J, Aceves-Ávila FJ. Rheumatologists in the COVID-19 era: will there be a new role for the rheumatologist in the care of rheumatic patients? Clin Rheumatol. 2020;39(11):3177–3183. doi: 10.1007/s10067-020-05380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Landewé RBM, Landewé RBM, MacHado PM, Kroon F, Bijlsma HWJ, Burmester GR, et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Ann Rheum Dis. 2020;79(7):851–858. doi: 10.1136/annrheumdis-2020-217877. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.