Abstract
Objective:
Medication errors are common in community pharmacies. Safety culture is considered a factor for medication safety but has not been measured in this setting. The objective of this study was to describe safety culture measured using the Agency for Healthcare Research and Quality (AHRQ) Community Pharmacy Survey on Patient Safety Culture, and assess predictors of overall patient safety.
Methods:
A cross-sectional survey of community pharmacists practicing in Wisconsin measuring safety culture. Demographic variables collected included pharmacist and pharmacy characteristics. Data were analyzed using descriptive statistics, chi square, and multivariate logistic regression analyses.
Results:
A total of 445 surveys were completed (response rate 82%). Safety culture was positively associated with the following: an independent pharmacy (adjusted odds ratio [AOR] 1.69, 95% Confidence interval [CI] 1.11-2.57), a health maintenance organization or clinic (AOR 2.25, 95% CI 1.34-3.78), being somewhat familiar (AOR 3.35, 95% CI 1.82-6.19) or very/extremely familiar with patients (AOR 8.8, 95% CI 4.68-16.59). Five of the composite scores differed significantly from results of the AHRQ pilot study (response to mistakes, communication openness, organizational learning-continuous improvement, communication about prescriptions across shifts, and overall patient safety). Consistent with the AHRQ pilot study, the composite describing staffing, work pressure and pace had the lowest score (37.6%).
Conclusion:
Understanding the safety culture of community pharmacies can help identify areas of strength and those that require improvement. Improvement efforts that focus on staffing, work pressure, and pace in community pharmacies may lead to better safety culture.
Keywords: safety culture, patient safety, community pharmacy
Background
Patient safety is a key pillar of healthcare quality. The growing interest in the area has stimulated research to measure and report on organizational attributes that are believed to influence patient safety. One such attribute is safety culture, defined as a product of individual and group values, attitudes, perceptions, competencies, and patterns of behavior that determine the commitment to, and the style and proficiency of, an organization’s health and safety management.1 Organizations with a positive safety culture are characterized by communications founded on mutual trust, by shared perceptions of the importance of safety and, by confidence in the efficacy of preventive measures.2 In its 1999 seminal report on patient safety, the U.S. Institute of Medicine made a recommendation that healthcare organizations must develop a culture of safety such that their workforce and processes are focused on improving the safety and reliability of care for patients.3
As an important but underappreciated part of the healthcare system, community pharmacies play a vital role in patient safety by ensuring medications are used safely by patients. However, little is known about patient safety practices and safety culture in these care environments as most of the research and instruments4-7 used to measure safety culture have focused on hospital settings. Nevertheless, understanding the safety culture of community pharmacies can greatly contribute to organizational quality improvement efforts by raising staff awareness about patient safety issues as well as identifying areas of strengths and those that require improvement. Doing so becomes even more important as community pharmacies continue to expand their roles from their traditional functions of dispensing prescriptions8,9 by including other services such as immunization10,11, targeted interventions like smoking cessation programs12, as well as specific disease management programs.13-15
Albeit delayed, a survey instrument developed by the U.S. Agency for Healthcare Research and Quality (AHRQ) to measure safety culture in community pharmacies16, suggests a growing interest to expand safety culture research beyond hospital settings. The survey instrument is designed to measure safety dimensions as they relate to the work environment, communication among pharmacy staff, error mitigation, error documentation, and error handling as well as staff perception about the overall safety rating of the pharmacy. However, except a pilot study conducted by the AHRQ using a convenient sample of pharmacy staff from 55 U.S. pharmacies17, large studies evaluating safety culture in community pharmacies do not exist. Thus, the objective of this study was to quantitatively describe safety culture and assess predictors of overall patient safety rating in a community pharmacy setting.
Methods
Survey Instrument
The AHRQ’s Community Pharmacy Survey on Patient Safety Culture16 was released in October 2012 and contains 36 items that measure the 11 areas of organizational culture to patient safety (Table 1). The survey uses either 5-point agreement scales (“strongly disagree” to “strongly agree”) or frequency scales (“never” to “always”). The survey also included one question that asked participants to rate their pharmacy’s patient safety using a poor to excellent scale. Survey items included a “Does not apply” or “Don’t know” option. Additional demographics questions about the zip code of participants’ pharmacy and familiarity with their patients were added.
Table 1.
AHRQ's Community Pharmacy Patient Safety Culture Composites17
| Patient counseling | Patients are encouraged to talk to the pharmacist; pharmacists spend enough time talking to patients and tell them important information about new prescriptions. |
| Communication openness | Staff freely speak up about patient safety concerns and feel comfortable asking questions, and staff suggestions are valued. |
| Overall perceptions of patient safety | There is a strong focus and emphasis on patient safety, and the pharmacy is good at preventing mistakes. |
| Organizational learning–continuous improvement | The pharmacy tries to figure out what problems in the work process lead to mistakes and makes changes to keep mistakes from happening again. |
| Teamwork | Staff treat each other with respect, work together as an effective team, and understand their roles and responsibilities. |
| Communication about prescriptions across shifts | Information about prescriptions is communicated well across shifts, and there are clear expectations and procedures for doing so. |
| Communication about mistakes | Staff discuss mistakes that happen and talk about ways to prevent mistakes. |
| Response to mistakes | The pharmacy examines why mistakes happen and helps staff learn from mistakes, and staff are treated fairly when they make mistakes. |
| Staff training and skills | Staff get the training they need, new staff receive orientation, and staff have the skills they need to do their jobs well. |
| Physical space and environment | The pharmacy is well organized and free of clutter, and the pharmacy layout supports good workflow. |
| Staffing, work pressure, and pace | There are enough staff to handle the workload, staff do not feel rushed, staff can take breaks, and work can be completed accurately despite distractions. |
The AHRQ survey was selected to evaluate safety culture because the instrument has undergone pilot testing before the final version was released for public use in the U.S. Furthermore, using such a standardized tool facilitates comparisons to be made across pharmacies and regions.
Survey Sample
The survey was administered via mail to a list of registered pharmacists in Wisconsin. A sampling frame that contained a list of 1725 registered pharmacists practicing in Wisconsin was obtained from the Wisconsin Department of Safety and Registration. To be eligible for the study, pharmacists should have practiced in a community/retail pharmacy in the past 12 months. A screening survey was sent to a random sample of 1000 pharmacists in January 2013. Since the return was not adequate, a second set of screener surveys were mailed to the remaining 725 pharmacists. At the end of the screening, 543 eligible sample members were identified to receive the full questionnaire.
The survey design included four attempts to contact eligible participants. In the first wave, participants were sent the survey questionnaire, a cover letter, a $2 bill, and postage-paid return envelope. In the second wave, a postcard reminder was sent to all sampled participants. In the third and fourth waves, those who had not returned their survey were sent the questionnaire and postage-paid return envelopes without the incentive. All mailings of survey questionnaires occurred between April and June of 2013. At the close of data collection, 445 completed surveys were returned yielding overall response rate of 82%.
Analysis of Data
Analyses were conducted using Stata 13 (Stata Corp, College Station, TX). The percentage of missing values was less than 1% for all items except two that had close to 6% (i.e., when the same mistake keeps happening, we change the way we do things; staff feel like their mistakes are held against them). Negatively worded items were reverse coded such that a higher score meant a more positive response to the question. Results are reported as percentage positive scores for each item as well as composites. For positively worded items, percent positive was calculated as the combined percentage of “strongly agree” and “agree” responses, or “Always” and “most of the time” responses depending on the response categories used for the item. For negatively worded items, percent positive was calculated as the total percentage of those who answered negatively. That is, the combined percentage of “Strongly disagree” and “Disagree” responses, or “Never” and “Rarely” responses.
Our results were compared with the AHRQ’s pilot study17 which employed the Community Pharmacy Survey on Patient Safety Culture using a voluntary sample of pharmacists, technicians, and other pharmacy staff from 55 community pharmacies located in wider geographical areas of the U.S. We specifically conducted a Chi-square analysis in order to test the difference of proportions for the 11 patient safety culture composites and that of the overall safety rating between our study and that of the AHRQ pilot study.17 Since the AHRQ pilot study included both pharmacists and technicians, comparison was made only with the pharmacist data. Finally, bivariate and multivariate logistic regression analyses were conducted to examine predictors of overall rating on patient safety using pharmacist and pharmacy characteristics as covariates (pharmacy type, pharmacy work hours, prescription volume, location of pharmacy, gender, age, tenure, pharmacist position, and degree of familiarity with patients). The covariates prescription volume, age, and tenure in the pharmacy were dichotomized using the median values as cutoff points. Bivariate analyses were performed first to identify significant associations with the outcome variable. The final multivariate model included covariates that were only significant during the bivariate analyses.
Results
About half of the participating pharmacies were of the national chain/mass merchandizer/grocer type (51%); independent pharmacies represented 31% and the remaining 18% were affiliated with health maintenance organizations (HMOs) or clinics. The majority of pharmacies did not provide a 24 hour service and 60% of participants reported that they are very or extremely familiar with their patients. Table 2 shows the characteristics of surveyed pharmacies and pharmacists.
TABLE 2.
Characteristics of Surveyed Pharmacies and Pharmacists (n = 445)
| Variables | n (%) |
|---|---|
| Pharmacy type | |
| National chain/mass merchandizer/grocer | 225 (51) |
| Independent | 135 (31) |
| HMO/Clinic | 81 (18) |
| 24-h Pharmacy | |
| Yes | 26 (6) |
| No | 417 (94) |
| Prescription volume per week day | 309 (297)* |
| ≤250 | 241 (54.9) |
| >250 | 198 (45.1) |
| Pharmacy setting | |
| Rural | 139 (34) |
| Urban | 266 (66) |
| Gender | |
| Male | 264 (60) |
| Female | 177 (40) |
| Age, y | 49 (14)* |
| ≤52 | 224 (51) |
| >52 | 211 (49) |
| Tenure in current pharmacy, y | 9 (9)* |
| ≤6 | 234 (54) |
| >6 | 200 (46) |
| Pharmacist position | |
| Managing Pharmacist | 331 (74) |
| Float Pharmacist | 92 (21) |
| Other | 22 (5) |
| Familiarity with patients | |
| Unfamiliar/Slightly familiar | 49 (11) |
| Somewhat familiar | 124 (29) |
| Very familiar/extremely familiar | 260 (60) |
Mean (SD) for continuous variables.
Based on our bivariate and multivariate logistic regression analyses, type of pharmacy and degree of familiarity with patients frequenting the pharmacy were significant predictors of overall rating on patient safety of a pharmacy. Being an independent pharmacy (adjusted odds ratio [AOR] 1.69, 95% Confidence interval [CI] 1.11-2.57), association with an HMO or clinic (AOR 2.25, 95% CI 1.34-3.78), being somewhat familiar (AOR 3.35, 95% CI 1.82-6.19) or very/extremely familiar with patients (AOR 8.8, 95% CI 4.68-16.59) were positively associated with overall rating of a pharmacy on patient safety (Table 3).
TABLE 3.
Predictors of Overall Rating on Patient Safety of a Pharmacy (n = 445)
| Independent variable | AOR | 95% CI |
|---|---|---|
| Pharmacy Type | ||
| National Chain/Mass merchandizer/Grocery | – | |
| Independent | 1.69* | 1.11-2.57 |
| HMO/Clinic | 2.25* | 1.34-3.78 |
| Familiarity with patients | ||
| Unfamiliar/Slightly familiar | – | |
| Somewhat familiar | 3.35* | 1.82-6.19 |
| Very familiar/Extremely familiar | 8.80* | 4.68-16.59 |
| Tenure in this pharmacy, y | ||
| > 6 | – | |
| ≤ 6 | 1.16 | 0.78-1.75 |
| Prescription volume | ||
| > 250/day | – | |
| ≤250/day | 1.15 | 0.79-1.67 |
| 24-h Pharmacy | ||
| Yes | – | |
| No | 1.33 | 0.56-3.17 |
P < 0.05.
Table 4 shows the percentages of positive, neutral and negative responses for each of the survey items under their respective patient safety composites.
Table 4.
Response Types on Survey Item Level
| % Negative | % Neutral | % Positive | |
|---|---|---|---|
| 1. Patient Counseling | |||
| B2. We encourage patients to talk to pharmacists about their medications | 1 | 6 | 93 |
| B7. Our pharmacists spend enough time talking to patients about how to use their medications | 4 | 13 | 83 |
| B11. Our pharmacists tell patients important information about their new prescriptions | 1 | 2 | 97 |
| 2. Communication Openness | |||
| B1. Staff ideas and suggestions are valued in this pharmacy | 7 | 25 | 68 |
| B5. Staff feel comfortable asking questions when they are unsure about something | 1 | 8 | 91 |
| B10. It is easy for staff to speak up to their supervisor/ manager about patient safety concerns in this pharmacy | 11 | 16 | 73 |
| 3. Overall Perceptions of Patient Safety | |||
| C3. This pharmacy places more emphasis on sales than on patient safety** | 16 | 15 | 69 |
| C6. This pharmacy is good at preventing mistakes | 5 | 18 | 77 |
| C9. The way we do things in this pharmacy reflects a strong focus on patient safety | 7 | 16 | 77 |
| 4. Organizational Learning-Continuous Improvement | |||
| C2. When a mistake happens, we try to figure out what problems in the work process led to the mistake | 7 | 11 | 82 |
| C5. When the same mistake keeps happening, we change the way we do things | 7 | 15 | 78 |
| C10. Mistakes have led to positive changes in this pharmacy | 7 | 24 | 69 |
| 5. Teamwork | |||
| A2. Staff treat each other with respect | 6 | 7 | 87 |
| A4. Staff in this pharmacy clearly understand their roles and responsibilities | 7 | 8 | 85 |
| A9. Staff work together as an effective team | 6 | 10 | 84 |
| 6. Communication About Prescriptions Across Shifts | |||
| B4. We have clear expectations about exchanging important prescription information across shifts | 5 | 16 | 79 |
| B6. We have standard procedures for communicating prescription information across shifts | 16 | 20 | 64 |
| B14. The status of problematic prescriptions is well communicated across shifts | 5 | 17 | 78 |
| 7. Communication About Mistakes | |||
| B8. Staff in this pharmacy discuss mistakes | 8 | 19 | 73 |
| B13. When patient safety issues occur in this pharmacy, staff discuss them | 8 | 18 | 74 |
| B15. In this pharmacy, we talk about ways to prevent mistakes from happening again | 9 | 25 | 66 |
| 8. Response to Mistakes | |||
| C1. Staff are treated fairly when they make mistakes | 4 | 9 | 87 |
| C4. This pharmacy helps staff learn from their mistakes rather than punishing them | 7 | 13 | 80 |
| C7. We look at staff actions and the way we do things to understand why mistakes happen in this pharmacy | 8 | 13 | 79 |
| C8. Staff feel like their mistakes are held against them** | 12 | 19 | 69 |
| 9. Staff Training and Skills | |||
| A3. Technicians in this pharmacy receive the training they need to do their jobs | 11 | 11 | 78 |
| A6. Staff in this pharmacy have the skills they need to do their jobs well | 8 | 7 | 85 |
| A8. Staff who are new to this pharmacy receive adequate orientation | 20 | 18 | 62 |
| A10. Staff get enough training from this pharmacy | 16 | 13 | 71 |
| 10. Physical Space and Environment | |||
| A1. This pharmacy is well organized | 6 | 7 | 87 |
| A5. This pharmacy is free of clutter | 21 | 15 | 64 |
| A7. The physical layout of this pharmacy supports good workflow | 19 | 12 | 69 |
| 11. Staffing, Work Pressure, and Pace | |||
| B3. Staff take adequate breaks during their shifts | 24 | 27 | 49 |
| B9. We feel rushed when processing prescriptions** | 31 | 57 | 12 |
| B12. We have enough staff to handle the workload | 12 | 21 | 67 |
| B16. Interruptions/distractions in this pharmacy (from phone calls, faxes, customers, etc.) make it difficult for staff to work accurately** | 19 | 60 | 21 |
Percent negative responses are calculated by combining “strongly disagree” and “disagree” or “never” and “rarely” response categories. Percent neutral responses represent “neither agree nor disagree” or “sometimes” response categories. Percent positive responses are calculated by combining “strongly agree” and “agree” or “always” and “most of the time” response categories.”
Negatively worded questions. For negatively worded items, percent positive response is based on those who responded “strongly disagree” or “disagree” or “never” or “rarely,” depending on the response category used for that particular item.
A1 to A10, B1 to B16, and C1 to C8 correspond to AHRQ survey items.17
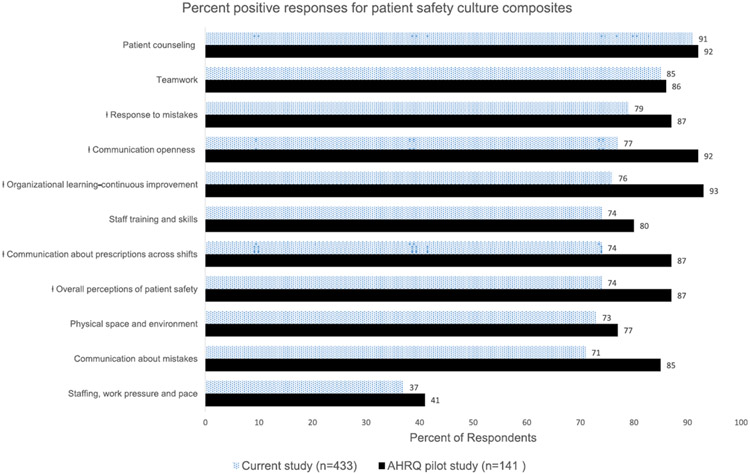
Figure 1 displays the percentage of positive responses for each of the 11 composites. The patient counseling composite had the highest positive response (91%) while staffing, work pressure and pace composite had the lowest (37%). Except for staffing, work pressure and pace, average positive responses for each composite were at least 70%. Figure 1 also includes the percentage of positive responses from the AHRQ pilot study for comparison. There were statistically significant differences in the percentages of positive responses between our study and that of the AHRQ pilot across five of the patient safety culture composites: response to mistakes; communication openness; organizational learning-continuous improvement; communication about prescriptions across shifts; overall perceptions of patient safety.
Figure 1.
Comparison of percent positive responses on patient safety culture composites between the current study and AHRQ's pilot study.
ǂ Results from current study and AHRQ pilot study were significantly different at α=0.05
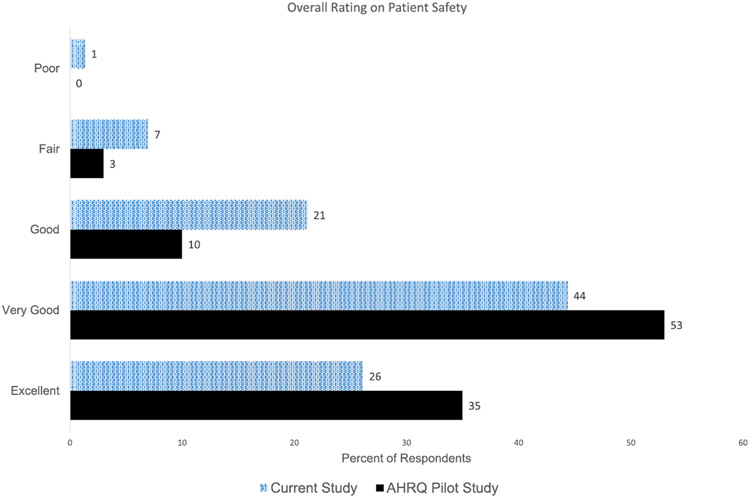
Figure 2 shows the overall rating on patient safety of the current study and the AHRQ’s pilot study. Overall, most respondents favorably rated their pharmacy on patient safety. About 8% of respondents rated their pharmacy as fair or poor on patient safety. Differences in percentage of overall safety ratings between our sample and that of the AHRQ pilot study were not statistically significant.
Figure 2.
Results for overall rating on patient safety.
Discussion
Previous studies of safety culture assessments have largely focused on hospital settings and neglected community pharmacies. Studies have reported that medication errors are common in community pharmacies and many have been linked to the culture of the organization18-20. Thus, safety culture assessments can prove useful for organizational improvement efforts. This study was the first to explore patient safety culture in community pharmacies in the U.S.
Results of this study showed that being affiliated with an HMO or a clinic was a positive predictor of overall rating on patient safety in a community pharmacy. An HMO/clinic pharmacy may be located within a health system, potentially bridging the information gap between inpatient and outpatient settings, and providing prescriptions for patients being discharged from the hospital. Unlike a traditional chain or independent pharmacy, an HMO pharmacy may also have access to a patient’s electronic health record and this may reflect the positive rating on patient safety as pharmacy staff are more likely to obtain complete and accurate information about their patients’ medical conditions. Being an independent pharmacy was also found to be a positive predictor of overall rating on patient safety. This may be due to organizational factors that allow for pharmacists working in the pharmacy to recommend and implement continuous quality improvements without the corporate approval required in national chain pharmacies.
Furthermore, the results showed that, being more familiar with patients receiving care at the pharmacy was a positive predictor of overall safety rating of a pharmacy. This is particularly relevant in light of the fact that multiple pharmacy use is common among the U.S population. In fact, a recent study reported that as much as 41% of the U.S adult, non-institutionalized population uses multiple pharmacies, with young adults (age 18-39), females, and individuals who lack adequate health insurance more likely to use multiple pharmacies.21 Patients can engage in such behavior because they may be incentivized to do so through different marketing strategies such as the use of coupons or other forms of patient assistance programs. But, these practices, while they provide convenience, and possibly cost savings, potentially degrade patient safety because patients cannot develop strong relationships with their pharmacy provider. As a result, the information gap that may result might present as a potential patient safety hazard.
Percent positive responses were calculated for all 11 safety culture composites and this study showed that, except for that of staffing, work pressure and pace, all composites received at least 70% scores. The highest positive score was that of patient counseling (91%). This is not surprising given the evidence that through patient counseling, pharmacists can identify and resolve drug-related problems, recover from errors, and optimize patient quality of care.22-25 There are numerous patient counseling guidelines that have been published by professional organizations,26-28 and patient counseling skills are taught in schools of pharmacy,29,30 emphasizing that it is a key responsibility of pharmacists.
The next highest percent positive score was that of teamwork composite (85%). One plausible explanation for this high score might be the fact that pharmacists operate in environments that have working stations in close proximity to each other. For example, a pharmacist may have another fellow pharmacist, a technician, and a cashier who all work within a distance of few feet. Such “closeness” at the work place may cultivate a good level of team situational awareness through development of “critical language” and better information sharing. Salas et al31 reported that team situational awareness requires unique activities such as coordination and information sharing. Consequently, pharmacists may view their work environment as one that facilitates good teamwork. This percentage was also comparable to that of the pilot result from AHRQ’s survey (86%) with no statistically significant difference.
Staffing, work pressure and pace safety culture composite received the lowest score (37%) and this was comparable to that of the AHRQ’s finding (41%). This suggests pharmacists feel that the workload and pace are not commensurate with the staffing levels of pharmacies. Studies have shown that pharmacist workload in community pharmacies has increased over the years, with greater work pressure cited by pharmacists working in national chain pharmacies.32,33 The perception is that work pressure in community pharmacies, most of which are typically owned and managed by big corporations, results from the need to meet certain targets in such business environments.34 This finding is particularly concerning because inadequate staff can severely limit pharmacists’ ability to safely dispense prescriptions thus increasing risk of patient harm. Gadkari et al35 reported that high workload in community pharmacies was negatively associated with pharmacist-provided drug therapy services. High pharmacist and pharmacy workload were also shown to increase the risk of dispensing drugs with potentially clinically relevant drug-drug interactions.36 A similar study also showed that the task of verifying prescription accuracy in a community pharmacy setting was negatively associated with having enough time to complete the task.37
Response to mistakes, communication openness, organizational learning-continuous improvement, communication about prescriptions across shifts, and overall perceptions of patient safety composites received lower scores in our study compared to findings of AHRQ’s pilot study and these differences were statistically significant. This difference might be explained by the small sample size of pharmacists in the AHRQ’s pilot study (n=141) compared to ours (n=445) which might result in overestimation. In addition, the AHRQ’s pilot study team administered their survey to 141 pharmacists and 234 technicians and other staff, with an average number of surveys administered per pharmacy ranging from 5 to 36.17 As a result, the AHRQ’s pilot study may have had some bias since some pharmacies had greater representation in the aggregate composite scores. And, because participants were recruited from- and surveys may have been completed within the work environment, this could have led to inadvertent group answering of questions and/or socially desirable answers. Our study administered the survey at pharmacists’ home addresses, possibly allowing for more confidential and independent responses. Finally, regional differences in perceptions towards the safety culture dimensions might also account for the differences between our findings and that of the AHRQ’s pilot study.
Most pharmacists rated their current pharmacy at least “good” on overall patient safety (92%) implying a strong sense of appreciation of their pharmacy’s value towards patient safety. However, this rating may not be a true reflection of actual safety in community pharmacies. The emphasis on patient safety found in inpatient settings is still in its infancy in the community pharmacy setting. Community pharmacists are typically not engaged in organizational risk management, or participate in safety evaluations in order to explore potential or actual errors. As a result, pharmacists may not be adequately knowledgeable or skilled in the nuances or characteristics that contribute to safety science. They may not recognize how their current safety infrastructure (i.e., error reporting systems, safety culture, etc.) may be helping or hindering patient safety in their pharmacy.38
A few important limitations need to be discussed. First, our study was conducted in one state of the U.S. and may not reflect the general trend across the country. It would be interesting to confirm our results with a study using a large national sample of pharmacists. Although the AHRQ’s pilot study included pharmacies from the different geographic regions of the U.S., the actual sample size for the pharmacists was small and the study included pharmacists, technicians, and other staff (141 pharmacists and 234 technicians and other staff). Second, our sampling frame included a mailing list of pharmacists who were licensed in the state and opted to receive mail, and therefore may be subject to under-coverage. It is not known if those not in the sampling frame have important differences with those included in our study.
Conclusion
Understanding the safety culture of community pharmacies can help identify areas of strength and those that require improvement. Improvement efforts that target deficient areas such as poor staffing and high work pressure may in turn lead to positive outcomes for pharmacists and their patients. This has important implications for pharmacy practice as pharmacists continue to shoulder the responsibility of dealing with complex drug regimens of patients with chronic conditions which may create multiple opportunities for errors.
Acknowledgments
Funding
The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Competing Interests: None
References
- 1.Nieva VF, Sorra J. Safety culture assessment: a tool for improving patient safety in healthcare organizations. Qual Saf Health Care. 2003;12(suppl 2):ii17–ii23. doi: 10.1136/qhc.12.suppl_2.ii17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AHRQ. User’s Guide: Hospital Survey on Patient Safety Culture. September 2004. http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/hospital/userguide/hospcult1.html. Accessed September 29, 2014.
- 3.Kohn LT, Corrigan JM, Donaldson MS. Institute of Medicine. To err is human: building a safer health system. 2000. [PubMed] [Google Scholar]
- 4.Sexton JB, Helmreich RL, Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6(1):44. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pronovost PJ, Weast B, Holzmueller CG, et al. Evaluation of the culture of safety: survey of clinicians and managers in an academic medical center. Qual Saf Health Care. 2003;12(6):405–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer SJ, Gaba DM, Geppert JJ, Sinaiko AD, Howard SK, Park KC. The culture of safety: results of an organization-wide survey in 15 California hospitals. Qual Saf Health Care. 2003;12(2):112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.AHRQ. Hospital survey on patient safety. 2004. http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/hospital/resources/hospscanform.pdf. Accessed September 25, 2013.
- 8.Christensen DB, Farris KB. Pharmaceutical Care in Community Pharmacies: Practice and Research in the US. Ann Pharmacother. 2006;40(7-8):1400–1406. doi: 10.1345/aph.1G545. [DOI] [PubMed] [Google Scholar]
- 9.WHO. The Role of the Pharmacist in the Health Care System. Report of a WHO Consultative Group. Geneva, Switzerland: World Health Organization; 1994. [Google Scholar]
- 10.Skelton JB, American Pharmacists Association, Academy of Managed Care Pharmacy. Pharmacist-provided immunization compensation and recognition: white paper summarizing APhA/AMCP stakeholder meeting. J Am Pharm Assoc (2003). 2011;51(6):704–712. doi: 10.1331/JAPhA.2011.11544. [DOI] [PubMed] [Google Scholar]
- 11.Hogue MD, Grabenstein JD, Foster SL, Rothholz MC. Pharmacist involvement with immunizations: a decade of professional advancement. J Am Pharm Assoc (2003). 2006;46(2):168–179; quiz 179-182. [DOI] [PubMed] [Google Scholar]
- 12.Sinclair HK, Bond CM, Stead LF. Community pharmacy personnel interventions for smoking cessation. Cochrane Database Syst Rev. 2004;(1):CD003698. doi: 10.1002/14651858.CD003698.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Cranor CW, Christensen DB. The Asheville Project: Short-term outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (2003). 2012;52(6):838–850. doi: 10.1331/JAPhA.2012.12542. [DOI] [PubMed] [Google Scholar]
- 14.Finley PR, Bluml BM, Bunting BA, Kiser SN. Clinical and economic outcomes of a pilot project examining pharmacist-focused collaborative care treatment for depression. J Am Pharm Assoc (2003). 2011;51(1):40–49. doi: 10.1331/JAPhA.2011.09147. [DOI] [PubMed] [Google Scholar]
- 15.Bunting BA, Smith BH, Sutherland SE. The Asheville Project: clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemia. J Am Pharm Assoc (2003). 2008;48(1):23–31. doi: 10.1331/JAPhA.2008.07140. [DOI] [PubMed] [Google Scholar]
- 16.AHRQ. Community Pharmacy Survey on Patient Safety Culture. 2012. http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/pharmacy/index.html. Accessed September 25, 2013.
- 17.AHRQ. Pharmacy Survey on Patient Safety Culture: 2012 Preliminary Comparative Results. September 2012. http://www.ahrq.gov/professionals/quality-patient-safety/patientsafetyculture/pharmacy/2012/index.html. Accessed January 19, 2015.
- 18.Odukoya OK, Stone JA, Chui MA. E-prescribing errors in community pharmacies: exploring consequences and contributing factors. Int J Med Inf. 2014;83(6):427–437. doi: 10.1016/j.ijmedinf.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashcroft DM, Quinlan P, Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Saf. 2005;14(5):327–332. doi: 10.1002/pds.1012. [DOI] [PubMed] [Google Scholar]
- 20.Knudsen P, Herborg H, Mortensen AR, Knudsen M, Hellebek A. Preventing medication errors in community pharmacy: frequency and seriousness of medication errors. Qual Saf Health Care. 2007;16(4):291–296. doi: 10.1136/qshc.2006.018770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Look KA. Patient characteristics associated with multiple pharmacy use in the U.S. population: Findings from the Medical Expenditure Panel Survey. Res Social Adm Pharm. October 2014. doi: 10.1016/j.sapharm.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Wu JYF, Leung WYS, Chang S, et al. Effectiveness of telephone counselling by a pharmacist in reducing mortality in patients receiving polypharmacy: randomised controlled trial. BMJ. 2006;333(7567):522. doi: 10.1136/bmj.38905.447118.2F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rantucci M Pharmacists Talking With Patients: A Guide To Patient Counseling In: A Guide to Patient Counseling. Vol Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 24.Chandra A, Malcolm N, Fetters M. Practicing Health Promotion Through Pharmacy Counseling Activities. Health Promot Pract. 2003;4(1):64–71. doi: 10.1177/1524839902238293. [DOI] [PubMed] [Google Scholar]
- 25.Ebid A, Abdel-Wahab E. Bronchial asthma and COPD: impact of pharmaceutical care on outcomes and quality of life in Egyptian patients. Bull Pharm Sci. 2006;29:167–185. [Google Scholar]
- 26.USP. USP medication counselling behavior guidelines. 1992. www.ipsf.org. Accessed September 4, 2014.
- 27.ASHP. American Society of Health-System Pharmacists. ASHP guidelines on pharmacist-conducted patient education and counseling. Am J Health Syst Pharm. 1997;54(4):431–434. [DOI] [PubMed] [Google Scholar]
- 28.ASCP. American Society of Consultant Pharmacists. Guidelines for pharmacist counseling of geriatric patients. 1998. www.ascp.com. Accessed September 11, 2014.
- 29.Santos AP, Mesquita AR, Oliveira KS, Lyra DP. Assessment of community pharmacists’ counselling skills on headache management by using the simulated patient approach: a pilot study. Pharm Pract. 2013;11(1):3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liekens S, Vandael E, Roter D, et al. Impact of training on pharmacists’ counseling of patients starting antidepressant therapy. Patient Educ Couns. 2014;94(1):110–115. doi: 10.1016/j.pec.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 31.Salas E, Prince C, Baker DP, Shrestha L. Situation Awareness in Team Performance: Implications for Measurement and Training. Human Factors: The Journal of the Human Factors and Ergonomics Society. 1995;37(1):123–136. doi: 10.1518/001872095779049525. [DOI] [Google Scholar]
- 32.McCann L, Hughes CM, Adair CG, Cardwell C. Assessing job satisfaction and stress among pharmacists in Northern Ireland. Pharm World Sci PWS. 2009;31(2):188–194. doi: 10.1007/s11096-008-9277-5. [DOI] [PubMed] [Google Scholar]
- 33.Gidman WK, Hassell K, Day J, Payne K. The impact of increasing workloads and role expansion on female community pharmacists in the United Kingdom. Res Social Adm Pharm. 2007;3(3):285–302. doi: 10.1016/j.sapharm.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Eden M, Schafheutle EI, Hassell K. Workload pressure among recently qualified pharmacists: an exploratory study of intentions to leave the profession. Int J Pharm Pract. 2009;17(3):181–187. [PubMed] [Google Scholar]
- 35.Gadkari AS, Mott DA, Kreling DH, Bonnarens JK. Pharmacy characteristics associated with the provision of drug therapy services in nonmetropolitan community pharmacies. J Rural Health. 2009;25(3):290–295. doi: 10.1111/j.1748-0361.2009.00232.x. [DOI] [PubMed] [Google Scholar]
- 36.Malone DC, Abarca J, Skrepnek GH, et al. Pharmacist Workload and Pharmacy Characteristics Associated With the Dispensing of Potentially Clinically Important Drug-Drug Interactions: Med Care. 2007;45(5):456–462. doi: 10.1097/01.mlr.0000257839.83765.07. [DOI] [PubMed] [Google Scholar]
- 37.Chui MA, Mott DA. Community pharmacists’ subjective workload and perceived task performance: a human factors approach. J Am Pharm Assoc (2003). 2012;52(6):e153–e160. doi: 10.1331/JAPhA.2012.11135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohen MR. Why error reporting systems should be voluntary. BMJ. 2000;320(7237):728–729. [DOI] [PMC free article] [PubMed] [Google Scholar]