Abstract
Traditional measures of socioeconomic status (SES) are associated with asthma morbidity, but their specific contributions are unclear. Increased exposure to indoor allergens among low SES children is an important consideration. Material hardship, a concept describing poor access to basic goods and services, may explain the relationship between low SES and indoor allergen exposure, and thereby, the increased risk of asthma morbidity. We sought to (i) describe the specific hardships experienced by low-Income, urban, minority children with asthma and indoor allergen sensitization and (ii) determine if material hardship is associated with indoor allergen exposure in this population. We conducted a cross-sectional analysis of children undergoing the baseline assessment for a clinical trial of home environmental modification. Participants were scored in five domains of material hardship. Domain scores were assigned based on caregiver responses to a questionnaire and were summed to generate a total material hardship score. Linear regression was used to examine the relationship between material hardship scores and bedroom floor concentrations of five common indoor allergens. Participants experienced high levels of material hardship in each of the five domains, with 33% not having access to a car, 35% not being able to pay utility bills, and 28% not being able to pay rent in the past year. Each one-point increase in material hardship was associated with an increase in cockroach allergen of 16.2% (95% CI: 9.4%, 24.6%) and an increase in mouse allergen of 9.4% (95% CI: 1.0%, 18.5%). After adjusting for traditional measures of SES, including household income, health insurance type, caregiver education, and caregiver employment status, the association between material hardship and cockroach allergen, but not mouse allergen, remained. These data suggest that a significant proportion of families of low-income, minority children with asthma may experience material hardship, and that they may be at greater risk of cockroach allergen exposure than their peers with similar income, but without material hardship.
Keywords: Material hardship, socioeconomic status, childhood asthma, indoor allergens, basic needs, transportation, housing conditions, monthly payments, medical needs, food insecurity
Introduction
Low socioeconomic status (SES) is a well-known risk factor for asthma morbidity among children,1–3 likely acting through poor health literacy, reduced access to and quality of health care, and increased housing- and neighborhood-related environmental exposures, among other factors.4 However, traditional measures of SES, such as income and education, do not capture many aspects of poverty. Our understanding of the burden of poverty and its effects on the underlying causes of asthma morbidity among low-income and minority children with asthma is therefore incomplete.
In 2004, the United States Department of Health and Human Services (DHHS) published a key report characterizing material hardship as it relates to low-income families with children.5 The report identified eight core indices of material hardship frequently used in research, including the presence of essential durable goods in the household, housing quality, housing insecurity, difficulty affording utility bills, unmet medical needs, food insecurity, housing overcrowding, and the amount of outside assistance available to the household. Several of these and related measures (poor housing quality, crowding, lack of amenities, and no vehicle access) have been associated with increased odds of asthma diagnosis and asthma-related emergency room visits;6 however, the relationship between material hardship and the underlying risk factors for asthma morbidity, particularly indoor allergen exposure, is not well understood. Pest allergens, such as mouse and cockroach allergens, are major contributors to the excess asthma morbidity among low-income and minority populations7–9 and are associated with poor housing quality.10,11 This suggests that material hardship may be a marker of exposure, independent of traditional measures of SES like income and education. Other indoor allergens, including dust mite and pet allergens, are also implicated in asthma morbidity in low-income populations12 and may be related to material hardship as well.
We therefore hypothesized that low-income, urban, minority children with asthma would experience many varieties of material hardship and that material hardship would be associated with indoor allergen exposure, independent of traditional measures of SES. We tested our hypothesis in 124 of the 155 randomized children and adolescents from Baltimore, Maryland with persistent asthma with both bedroom floor allergen data and material hardship data. Our objectives were to characterize material hardship and examine associations between multiple domains of material hardship and indoor allergen exposure among a population of predominately low-income, urban, minority children with persistent asthma.
Methods
Study Design
We conducted a cross-sectional analysis of a predominantly low-income, African American population of 5–17 year old children in Baltimore undergoing a baseline evaluation for the Environmental Control as Add-on Therapy in Childhood Asthma (ECATCh) clinical trial (NCT02251379). The study was approved by the Johns Hopkins Institutional Review Board and informed consent was obtained from the parents or guardians of all participants. The clinical trial sought to determine the effects of home environmental modifications on asthma outcomes and environmental exposures in children with persistent asthma and sensitization to ≥1 indoor allergen. We surveyed the primary caregivers of these children using a material hardship questionnaire developed using the 2004 DHHS Measures of Material Hardship Report. Baseline data for randomized patients in the clinical trial was collected from February 2015 to March 2018; however, data pertinent to our analysis was gathered from March 2015 to November 2017.
Participants
Eligible participants were required to have persistent asthma and sensitization to ≥1 indoor allergen. Persistence was defined as either being on a long-term controller medication for asthma or meeting the National Asthma Education and Prevention Program guideline requirements for persistent disease (symptoms ≥3 days per week over the past 2 weeks or nocturnal asthma symptoms ≥3 times in the past month). Participants also had to meet one of the following criteria within the previous 18 months: (i) one asthma-related unscheduled visit to an emergency department, clinic or urgent care facility (ii) one asthma-related overnight hospitalization or (iii) one or more bursts of oral corticosteroids. Finally, participants had to be sensitized to dust mite, cockroach, mouse, cat, or dog allergen, defined as either a positive skin prick test (net wheal ≥2mm) or a specific IgE ≥0.35 kU/L as quantified using the ImmunoCAP system (ThermoFisher, Uppsala, Sweden). Participants were excluded if they were not sensitized to the above allergens, had significant other cardiovascular or pulmonary comorbidities, were taking beta-blockers, were escalating on allergen immunotherapy, were active smokers, were pregnant or did not sleep in the assessed home for at least 4 nights per week.
Material Hardship Questionnaire
The material hardship questionnaire was organized into five domains that covered six of the eight hardship indices outlined in the 2004 DHHS report. Domains included (i) durable goods or transportation in the household, (ii) housing quality, (iii) housing-related payments (which contained items assessing both housing insecurity and difficulty affording utility bills), (iv) medical needs, and (v) food security. Although the questionnaire asked participants to disclose the number of rooms in their homes, data from the parent study did not quantify the number of individuals living in the household; therefore, we could not assess household crowding. A scoring system was devised for each domain such that a higher score indicated increased hardship in that category.
A deficiency in durable goods or transportation was defined as reporting a lack of a working washing machine, dishwasher, refrigerator, smart phone, internet connection or automobile in the household. Families were assigned a score of 0 for each item owned and a score of 1 for each item they did not own. If they had access to, but did not own, a washing machine or automobile, they were assigned a score of 0.5 for that item. Total scores ranged from 0–6, with 6 being the maximal level of hardship. Poor housing quality was designated by report of a leaking roof or ceiling, windows that were broken or would not shut, exposed electrical wires in the finished areas of the home, non-working plumbing, holes or cracks in the walls wider than the edge of a dime, or holes in the floor big enough to trip over. Families received a score of 1 for each problem present, with a possible range of 0–6.
Inability to afford housing-related payments was defined as reporting an inability to pay rent, telephone, or utility bills within the past twelve months. Families received a 0 in each category if they were able to make timely payments. A score of 1 was assigned if the family was evicted, had telephone service withheld, or had utilities discontinued. If the family could not make payments in one of the categories, but did not face eviction or discontinuation of services, they received a score of 0.5 for that item. Total scores ranged from 0–3, with 3 indicating maximal hardship. The unmet medical needs domain was defined as reporting the inability of a household member to see a doctor or dentist within the past twelve months. Ability to see both of these healthcare providers was assigned a score of 0, whereas the ability to see only one was assigned a score of 1, and being unable to see either was assigned a score of 2. Possible scores range from 0–2, with 2 indicating maximal hardship. Finally, food insecurity within the past four months was measured on a scale of 0–3. Families that indicated they had both the desired amount and variety of food were assigned a score of 0. Those with an adequate amount, but not always the desired variety of food, received a score of 1. Additional points were assigned if the family “sometimes” or “often” did not have enough to eat. Scores from each domain were added to generate a total material hardship score for each participant ranging from 0 (no hardship) to 20 (maximum hardship).
Settled Dust Collection
Settled dust was collected from the bedroom floors of eligible participants and analyzed for the five most common indoor allergens: dust mite (Der f 1), cockroach (Bla g 1), mouse (Mus m 1), cat (Fel d 1), and dog (Can f 1). As expected for this population, dust mite allergen levels were generally very low and well below clinically meaningful concentrations, which are in the microgram/gram range (median 7 ng/g, IQR <LLOD-35.5 ng/g). Dust mite allergen was therefore excluded from the final analysis.
Statistical Analysis
Linear regression was used to examine the relationships between domain-specific and total material hardship scores and log10-concentrations of bedroom floor mouse, cockroach, cat, and dog allergens, adjusted for age and sex. We did not adjust for race since our sample was predominately African American (92%). Models were adjusted for traditional measures of SES, which included household income, caregiver education, caregiver employment, and insurance type. Measures of traditional SES were incorporated into the model as ordinal variables: household income included eleven ascending brackets ranging from $0 to ≥$50,000 in $5,000 increments; caregiver education was ranked 1–7 from ≤8th grade to any post-graduate work; caregiver employment was ranked 1 (disabled or laid off), 2 (homemaker or retired), and 3 (working at a full time job); and insurance type was ranked 1 (public) and 2 (private). Data labeled “unknown” or “prefer not to say” was excluded from the regression analysis; these included 22 caregivers with unknown income and eight caregivers with unknown employment status. Linear regression was also conducted to examine the relationships between each traditional measure of SES and each indoor allergen. Associations between material hardship scores (or traditional measures of SES) and allergen concentrations were expressed as the percent change in allergen concentration with each one-point increase in material hardship score (or traditional measure of SES) by transforming the ß coefficients as follows: (eß-1)*100. Stata/SE 14.0 software (StataCorp, College Station, TX) was used to conduct all analyses.
Results
Study Population Demographics and Bedroom Floor Allergen Measurements
A total of 255 participants were screened, 220 received a home visit for primary data collection, and 155 were randomized. Of these, 124 had bedroom floor allergen sampling and completed a material hardship questionnaire. Table 1 presents the baseline demographic and socioeconomic features of the study population. The sample included primarily African American children (92%) with public health insurance (91.1%). Approximately 94% of children had a primary caregiver with an education level less than a college degree, 46% lived in a household with an annual income <$25,000, and 32% had a primary caregiver who was unemployed or disabled. A summary of bedroom floor allergen measurements and the numbers of individuals who were sensitized (wheal ≥2mm or ImmunoCAP ≥0.35 kU/L) to each allergen is included in Table 2. Two individuals had neither skin prick testing or serum IgE testing for cat or dog allergen; thus, their sensitization to these allergens could not be determined.
Table 1.
Baseline demographics, n = 124.
| Age of child in years, median (range) | 10 (5–17) |
| Sex of child (%) | |
| Male | 72 (58.1) |
| Female | 52 (41.9) |
| Race of child, n (%) | |
| Black/African American | 114 (92.0) |
| Mixed Race | 8 (6.4) |
| White | 2 (1.6) |
| Health insurance of child, n (%) | |
| Public | 113 (91.1) |
| Private | 11 (8.9) |
| Caregiver employment status, n (%) | |
| Working at a Paying Job | 62 (50.0) |
| Unemployed/Disabled | 40 (32.3) |
| Retired/Homemaker | 14 (11.3) |
| Other/Refused | 8 (6.5) |
| Household income, n (%) | |
| <$10,000 | 27 (21.8) |
| $10,000-$24,999 | 30 (24.2) |
| $25,000-$49,999 | 28 (22.6) |
| ≥$50,000 | 17 (13.7) |
| Unknown/refused | 22 (17.7) |
| Highest caregiver education level, n (%) | |
| Less than high school | 19 (15.3) |
| High school diploma | 46 (37.1) |
| Technical diploma/some college | 51 (41.1) |
| College degree/post-graduate work | 8 (6.5) |
Table 2.
Bedroom floor allergen concentrations and number of sensitized children, n=124
| Baseline bedroom floor allergen level, median (IQR) | |
| Cockroach, Bla g 1 (U/g) | 0.4 (<LLOD§-3.4) |
| Mouse, Mus m 1 (ng/g) | 569.5 (165.5–2871.5) |
| Cat, Fel d 1 (ng/g)* | 126 (27–1660) |
| Dog, Can f 1 (ng/g)† | 44.5 (16–437) |
| Number of sensitized children by allergen, n (%) | |
| Cockroach | 70 (56.5) |
| Mouse | 87 (70.2) |
| Cat‡ | 49 (40.2) |
| Dog‡ | 35 (28.7) |
n=123,
n=120,
n=122,
lower limit of detection
The material hardship questionnaire and response data are presented in Table 3. Approximately 73% of caregivers reported having no dishwasher, 33% reported having no automobile or access to an automobile, and 25% reported having no internet. Smart phones and refrigerators were widely available, however, with more than 90% of caregivers citing ownership of these items. Among the poor housing conditions described, holes in the walls or ceiling (38.7%) and leaking roofs (18.6%) were the most prevalent. Regarding housing-related payments, 34.7% of caregivers were unable to pay a utility bill and 28.2% were unable to pay their full rent/mortgage within the past twelve months; 11.3% of families reported disconnected telephone services, 6.4% reported discontinued utilities, and 1.6% reported eviction. Regarding unmet medical needs, 14.5% reported a household member being unable to see a dentist and 13.7% reported a household member being unable to see a doctor when needed within the past twelve months. Nearly one-in-four (23.4%) caregivers cited insufficient food variety within the past four months and nearly one-in-eight (12.1%) reported sometimes or often not having enough to eat. The distributions of total material hardship score and its various domain subscores are depicted in Figure 1. The total material hardship score ranged from 0–9.5 (out of a possible 20 points), with a median value of 3.5.
Table 3.
Material hardship questionnaire and response data, n=124.
| Durable goods and transportation in the household, n (%) | |||
|---|---|---|---|
| Do you currently have the following items in your home, in working condition? | |||
| Do not own or have access | Have access, but do not own | Own | |
| Dishwasher | 91 (73.4) | N/A | 33 (26.6) |
| Automobile | 41 (33.1) | 23 (18.5) | 60 (48.4) |
| Internet access | 31 (25.0) | N/A | 93 (75.0) |
| Washing machine | 16 (12.9) | 9 (7.3) | 99 (79.8) |
| Smart phone | 7 (5.6) | N/A | 117 (94.4) |
| Refrigerator | 2 (1.6) | N/A | 122 (98.4) |
| Housing quality, n (%) | |||
| Are any of the following conditions present in your home (select all that apply)? | |||
| Holes in the walls or ceiling; cracks wider than the edge of a dime | 48 (38.7) | ||
| A leaking roof or ceiling | 23 (18.6) | ||
| Broken window glass or windows that can’t shut | 17 (13.7) | ||
| A toilet, hot water heater, or other plumbing that doesn’t work | 8 (6.5) | ||
| Exposed electrical wires in the finished areas of your home | 6 (4.8) | ||
| Holes in the floor big enough for someone to catch their foot on | 2 (1.6) | ||
| Housing-related payments, n (%) | |||
| Evicted/services discontinued | Not paid, but not evicted/services not discontinued | No | |
| Was there a time in the past 12 mo. when the phone company disconnected service because payments not made? | 14 (11.3) | N/A | 110 (88.7) |
| Was there a time in the past 12 mo. when you did not pay the full amount of gas, oil, or electricity bills and/or the utility company discontinued services? | 8 (6.4) | 43 (34.7) | 73 (58.9) |
| Was there a time in the past 12 mo. when you did not pay the full amount of rent or mortgage and/or were evicted? | 2 (1.6) | 35 (28.2) | 87 (70.2) |
| Medical needs, n (%) | |||
| Yes | No | ||
| Was there a time in the past 12 months you or anyone in your household needed to see a dentist but did not go? | 18 (14.5) | 106 (85.5) | |
| Was there a time in the past 12 months you or anyone in your household needed to see a doctor/go to hospital but did not go? | 17 (13.7) | 107 (86.3) | |
| Food security, n (%) | |||
| Which of these statements best describes the food eaten in your household in the last 4 months? | |||
| Enough of the kinds of food we want | 80 (64.5) | ||
| Enough but not always the kinds of food we want to eat | 29 (23.4) | ||
| Sometimes not enough to eat | 12 (9.7) | ||
| Often not enough to eat | 3 (2.4) | ||
Figure 1.
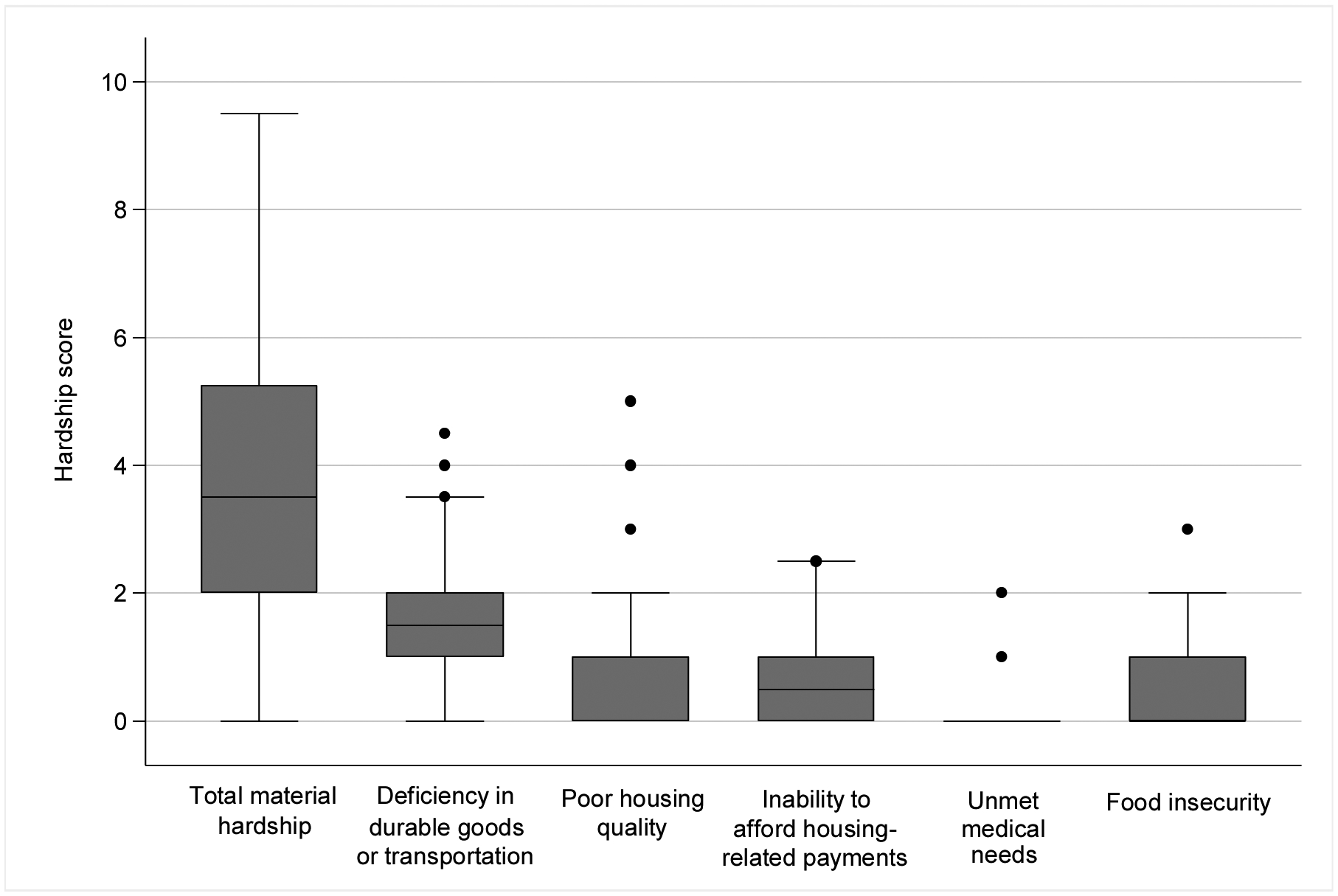
Distributions of total material hardship score and material hardship domain scores. The maximum possible score for deficiency of goods or transportation and poor housing quality is 6; for inability to afford housing-related payments and food insecurity, the maximum possible score was 3, and for unmet medical needs, it was 2.
Association of Bedroom Floor Allergen Concentrations with Material Hardship
The median bedroom floor concentrations of cockroach, mouse, dog and cat allergens among children in the highest quartile of material hardship were 2.9U/g, 1073 ng/g, 36 ng/g and 71 ng/g, respectively, compared to < 0.1 U/g (LLOD), 240 ng/g, 36 ng/g and 61 ng/g for children in the lowest hardship quartile. In analyses adjusted for age and sex only, total material hardship was significantly correlated with cockroach and mouse allergen concentrations, but not with cat or dog allergen concentrations (Table 4). Among the hardship domains, the deficiency of durable goods and transportation, poor housing quality, unmet medical needs and food insecurity were significantly correlated with cockroach allergen concentrations, but not with mouse, cat, or dog. Inability to afford housing-related payments had no correlation with any type of allergen exposure. Following adjustment for age, sex, and traditional measures of SES (household income, health insurance status, caregiver education level, and caregiver employment), material hardship remained associated with cockroach allergen concentrations, but not with mouse. Among the hardship domains, poor housing quality, unmet medical needs and food insecurity remained correlated with cockroach exposure, but the deficiency of durable goods and transportation did not. Inability to afford housing-related payments continued to have no correlation with any type of indoor allergen exposure. Figure 2 depicts the estimated percent changes in allergen levels per unit increase in total material hardship score, both before and after adjustment for traditional measures of socioeconomic status
Table 4.
Percent change in allergen concentration per unit increase in corresponding hardship score.
| Hardship Score | Cockroach (Bla g 1) | Mouse (Mus m 1) | Cat (Fel d 1) | Dog (Can f 1) | ||||
|---|---|---|---|---|---|---|---|---|
| Percent change (95% C.I.) | Percent change (95% C.I.) | Percent change (95% C.I.) | Percent change (95% C.I.) | |||||
| Model 1* | Model 2† | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| n=124 | n=102 | n=124 | n=102 | n=123 | n=101 | n=120 | n=98 | |
| Total Material Hardship | 16.2 (9.4, 24.6) | 16.2 (7.3, 25.9) | 9.4 (1.0, 18.5) | 6.2 (−3.9, 17.4) | 3.0 (−6.8, 12.7) | 2.0 (−8.6, 13.9) | −2.0 (−10.4, 8.3) | −3.9 (−13.9, 7.3) |
| Hardship Subscores | ||||||||
| Deficiency of home appliances | 17.4 (1.0, 36.3) | 4.1 (−13.1, 25.9) | 17.4 (−1.0, 39.1) | 12.7 (−9.5, 39.1) | −2.0 (−19.7, 19.7) | −13.9 (−32.3, 10.5) | −12.2 (−28.1, 6.2) | −12.2 (−30.9, 11.6) |
| Poor housing conditions | 25.9 (8.3, 44.8) | 31.0 (11.6, 52.2) | 13.9 (−3.9, 33.6) | 9.4 (−9.5, 32.3) | −1.0 (−18.9, 20.9) | 2.0 (−18.1, 27.1) | 2.0 (−16.5, 23.4) | −3.0 (−21.3, 20.9) |
| Difficulty affording housing payments | 5.1 (−18.9, 37.7) | 9.4 (−18.1, 47.7) | 2.0 (−23.7, 37.7) | 3.0 (−26.7, 44.8) | 1.0 (−28.8, 44.8) | 13.9 (−22.9, 66.5) | 16.2 (−17.3, 63.2) | 12.7 (−22.9, 64.9) |
| Unmet medical needs | 35.0 (4.1, 75.1) | 40.5 (7.3, 85.9) | 9.4 (−18.1, 47.7) | 5.1 (−24.4, 46.2) | 35.0 (−3.9, 91.6) | 22.1 (−14.8, 76.8) | 11.6 (−20.5, 56.8) | −1.0 (−30.9, 41.9) |
| Food Insecurity | 29.7 (7.3, 58.4) | 29.7 (3.0, 63.2) | 13.9 (−8.6, 41.9) | 2.0 (−22.1, 33.6) | 8.3 (−17.3, 40.5) | 10.5 (−18.9, 50.7) | −4.9 (−26.7, 23.4) | −9.5 (−33.0, 22.1) |
adjusted for age and sex;
adjusted for age, sex, household income, health insurance status, caregiver education level, and caregiver employment. Statistically significant associations are bolded.
Figure 2.
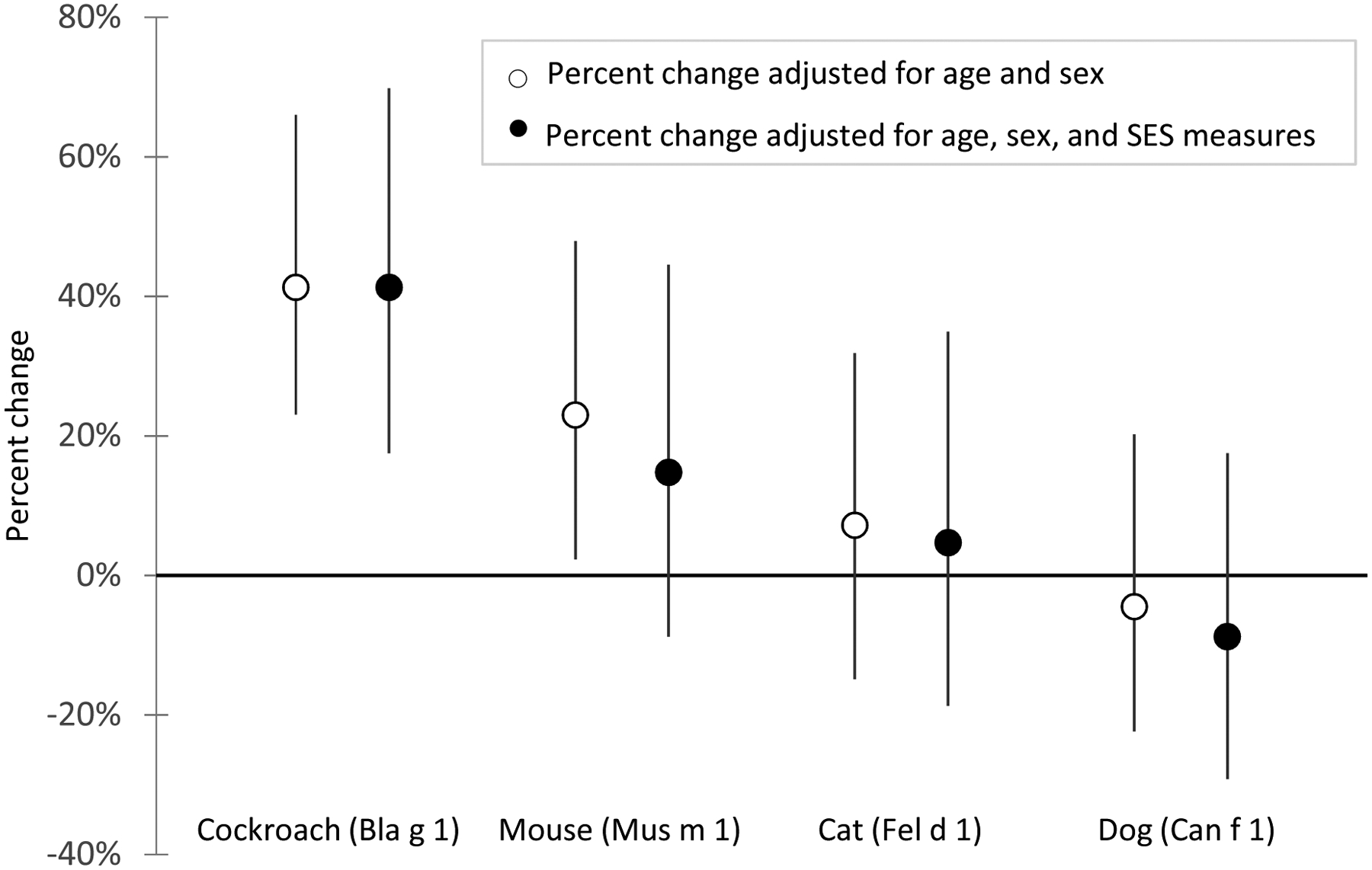
Estimated change in allergen levels per 1-point increase in total material hardship score. Circles represent the estimated percent change and whiskers represent the 95% confidence intervals.
Association of Bedroom Floor Allergen Concentrations with Traditional SES Measures
Table 5 shows the percent change in allergen levels per unit increase in each traditional SES variable. Only cockroach allergen and household income were significantly correlated; cockroach allergen decreased as household income increased. However, this relationship was lost when adjusting for total material hardship.
Table 5.
Percent change in allergen concentration per unit increase in traditional SES hardship variables.
| Traditional SES Variable | Cockroach (Bla g 1) | Mouse (Mus m 1) | Cat (Fel d 1) | Dog(Can f 1) | ||||
|---|---|---|---|---|---|---|---|---|
| Percent change (95% C.I.) | Percent change (95% C.I.) | Percent change (95% C.I.) | Percent change (95% C.I.) | |||||
| Model 1* | Model 2† | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| n=124 | n=102 | n=124 | n=102 | n=123 | n=101 | n=120 | n=98 | |
| Household income | −4.9 (−9.5, −1.0) | −2.0 (−6.8, 2.0) | −3.0 (−8.6, 2.0) | −2.0 (−7.7, 4.1) | −4.9 (−11.3, 1.0) | −4.9 (−11.3, 2.0) | 1.0 (−4.9, 7.3) | 1.0 (−5.8, 7.3) |
| Caregiver education level | −7.7 (−18.9, 4.1) | −3.9 (−14.8, 8.3) | −5.8 (−18.9, 8.3) | −3.9 (−16.5, 11.6) | −13.9 (−27.4, 2.0) | −13.1 (−27.4, 3.0) | 2.0 (−13.1, 20.9) | 2.0 (−13.9, 20.9) |
| Caregiver employment | −9.5 (−24.4, 8.3) | −3.0 (−18.1, 15.0) | 3.0 (−14.8, 24.6) | 7.3 (−12.2, 29.7) | 13.9 (−9.5, 43.3) | 16.2 (−8.6, 46.2) | 4.1 (−17.3, 32.3) | 4.1 (−18.1, 31.0) |
| Health insurance status | −23.7 (−55.1, 31.0) | −9.5 (−45.1, 50.7) | −9.5 (−50.3, 64.9) | 0.0 (−45.1, 82.2) | −11.3 (−56.8, 80.4) | −8.6 (−56.0, 87.8) | −14.8 (−57.3, 69.9) | −16.5 (−58.5, 68.2) |
adjusted for age and sex;
adjusted for age, sex, and total material hardships score. Statistically significant associations are bolded.
Discussion
In this population of predominantly low-income African American children with persistent asthma, material hardship was common, with a significant proportion of families having no access to a car, being unable to pay utility bills or rent, and having food insecurity. Total material hardship was significantly associated with cockroach, but not mouse, allergen exposure, even after adjusting for traditional measures of SES (household income, health insurance status, caregiver education level, and caregiver employment). Furthermore, household income was the only traditional measure of SES that was significantly correlated with reduced cockroach allergen exposure, but this relationship was lost when controlling for material hardship. These findings suggest that many families of urban, low-income, minority children with persistent asthma experience material hardship, and that they may be at greater risk of cockroach allergen exposure than their peers with similar income, education, insurance, and employment status, but without material hardship.
Material hardship was common. Approximately one-in-three families had holes in the walls or ceilings of their home, one-in-three lacked access to an automobile, and one-in-three could not pay utility bills. One-in-four families had housing insecurity and one-in-eight reported food insecurity. Similar rates of hardship are seen in other populations of low SES children,13 indicating that these hardships are not specific to low SES children with asthma only. However, the prevalence of these hardships among low-income minority children with asthma was previously unclear; these estimates provide valuable insight into their pervasiveness and highlight their potential role in asthma morbidity within this population. It is plausible, for example, that lack of access to transportation contributes directly to asthma morbidity by limiting access to health care, while an inability to make ends meet contributes indirectly by increasing stress levels and/or de-prioritizing asthma care. Although an analysis of the contributions of each of these hardships to asthma morbidity is beyond the scope of this study, future studies aimed at identifying the hardship factors that contribute to asthma morbidity may help to inform the development of interventions.
We also observed an association between several domains of material hardship and cockroach allergen exposure, a well-established cause of asthma morbidity,14,15 that was independent of traditional measures of SES. Although the association between poor housing quality and cockroach allergen is well established,10,11,16 the association between unmet medical needs and food insecurity and cockroach allergen has not yet been described to our knowledge. The causative link between poor housing quality and cockroach infestation is intuitive, such that holes in the walls or leaking plumbing create entry points and water sources for these pests to flourish. Unmet medical needs and food insecurity likely serve as markers of other factors that lead to cockroach allergen exposure, such as poor housing conditions that were not captured by the housing quality questions or residence in a neighborhood or multi-family housing structure with endemic infestation. These particular hardships may be indicators of families with the greatest social needs, which may drive asthma morbidity as well as other chronic health conditions.
Total material hardship was also associated with increased exposure to mouse allergen, but the association was not independent of traditional measures of SES. Furthermore, there was no significant correlation between any traditional measure of SES and exposure to mouse allergen, suggesting that mouse allergen may be endemic among Baltimore children with persistent asthma and a recent exacerbation. In fact, mouse allergen was detected in virtually all homes in other studies that enrolled a similar population of Baltimore children and was often present in high concentrations.11,17 Mouse allergen was also virtually ubiquitous among children with asthma living in high poverty neighborhoods in Chicago, New York City, and Boston, but not Seattle, Dallas, or Tucson, highlighting the importance of geography and the built environment in promoting mouse infestation.18–20 Thus, an independent association with material hardship may have been observed had our sample been more socioeconomically or geographically diverse. Not surprisingly, exposure to cat and dog allergens had no significant associations with total material hardship or any of its five domains as pet allergen levels were low overall. This finding likely reflects the urban demographic and intrinsic poverty status of our sample as there is less ownership of cats and dogs in poor, urban environments compared to suburban environments.21
The clinical importance of changes in allergen exposure per unit increase of material hardship is difficult to assess based on data presented in this study alone. However, other published literature suggests that the per-unit changes are generally small. Morgan et al. found that 50% reduction in bedroom cockroach and dust mite allergens one year following home environmental intervention significantly reduced asthma morbidity (maximal number of symptom days per 2-week period, number of unscheduled ED or clinic visits for asthma per 2-month period, and number of hospitalizations for asthma per 2-month period).22 Grant et al. observed that reducing mouse allergen exposure by ≥75% from baseline was associated with greater improvements in spirometry compared to those who did not achieve that reduction metric.23 Finally, Matsui et al. identified that a 50% decrease in bedroom floor mouse allergen was associated with significant reductions in asthma symptoms, short-acting β-agonist use, and healthcare utilization.24 Here, we observed that cockroach and mouse allergen levels changed by 16.2% and 9.4%, respectively, with each unit of total material hardship. Thus, it could be estimated that a minimum three point reduction in total material hardship score would be needed before clinically important outcomes would be seen in this population if material hardship is causally related to pest allergen exposure. However, more investigation regarding the magnitude of material hardship change required to influence clinical outcomes is needed.
There are several limitations to the analyses presented here. First, we focused on describing the burden of material hardship in this population and its relationship to housing-related exposures known to exacerbate asthma; many questions about the role of material hardship in excess of indoor allergen burden among low-income and minority populations remain. Asthma is a complex disease with a variety of contributing factors; thus, increased exposure to indoor allergens should not be considered the sole contributor to asthma morbidity among families living with material hardship. Other environmental exposures (particulate matter, air nicotine) and psychosocial exposures (stress, depression, and poor medication adherence), all of which have been linked to increased asthma morbidity,25 need to be considered as potential effects of material hardship. However, an allergic phenotype is quite prevalent among individuals with asthma,26 and pest allergens are important contributors to morbidity in this population.14,27,28 Second, the study population was almost entirely Black/African American, so we were unable to examine racial differences in material hardship and its relationship to environmental exposures. Given that Black/African American populations are known to have greater material hardship than white populations with the same income, employment, and educational attainment,29 future studies should determine if material hardship explains any differences in environmental exposures among racial and ethnic groups. Last, although the results may not be generalizable to other populations, research questions about material hardship are most relevant to populations that are at risk for these hardships.
Conclusion
Material hardship related to housing quality, housing stability, ability to make ends meet, and food security was common among this population of low-income, predominantly Black/African American children with asthma. These hardships may interfere with their caregiver’s ability to access and prioritize asthma care and increase the risk of environmental exposures that exacerbate asthma. In fact, material hardship was significantly associated with greater exposure to bedroom floor cockroach allergen, even after adjusting for traditional measures of SES. These findings suggest that traditional measures of SES may not fully capture the features of social disadvantage among asthmatic children living in poverty, and that material hardship may be a risk factor for cockroach allergen exposure, independent of traditional measures of SES.
Acknowledgements:
We would like to acknowledge Jean Curtin-Brosnan, MA for her assistance with data collection and statistical analysis and Sarah Louise Poynton, PhD for her constructive critique of this manuscript.
Declaration of Funding:
Funding Source: Dr. Jabre’s time was supported by an NIH fellowship training grant [T32HL072748]. Dr. Matsui’s was supported by grants from the National Institutes of Health (R01 ES026170, K24 AI114769, R01 ES023447). These funding agencies were not directly involved in study design, data collection or analysis, writing of the report, or submission for publication.
Abbreviations:
- SES
socioeconomic status
- LLOD
lower limit of detection
- N/A
not applicable
References:
- 1.Bollinger ME, Butz A, Tsoukleris M, Lewis-Land C, Mudd S, Morphew T. Characteristics of inner-city children with life-threatening asthma. Ann Allergy Asthma Immunol 2019; 122:381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cardet JC, Louisias M, King TS et al. Income is an independent risk factor for worse asthma outcomes. J Allergy Clin Immunol 2018;141(2):754–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Litonjua A, Carey V, Weiss S, Gold D. Race, socioeconomic factors, and area of residence are associated with asthma prevalence. Pedatr Pulmonol 1999;28:394–401. [DOI] [PubMed] [Google Scholar]
- 4.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol 2009;9:154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ouellette T, Burstein N, Long D, Beecroft E. Measures of material hardship: final report. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Office of the Secretary, U. S. Department of Health and Human Services; 2004. Retrieved May 14, 2019, from http://www.aspe.hhs.gov/hsp/material-hardship04/report.pdf. [Google Scholar]
- 6.Hughes HK, Matsui EC, Tschudy MM, Pollack CE, Keet CA. Pediatric asthma health disparities: race, hardship, housing, and asthma in a national survey. Acad Pediatr 2017;17(2):127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelber LE, Seltzer LH, Bouzoukis JK, Pollart SM, Chapman MD, Platts-Mills TAE. Sensitization and exposure to indoor allergens as risk factors for asthma among patients presenting to hospital. Am Rev Respir Dis 1993; 147:573–578. [DOI] [PubMed] [Google Scholar]
- 8.Matsui EC. Environmental exposures and asthma morbidity in children living in urban neighborhoods. Allergy 2014; 69(5):553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C, Abou El-Nour MM, Bennet GW. Survey of pest infestation, asthma, and allergy in low-income housing. J Community Health 2008; 33:31–39. [DOI] [PubMed] [Google Scholar]
- 10.Rauh VA, Chew GR, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ. Health Perspect 2002;.110(Suppl. 2):323–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsui EC, Simons E, Rand C et al. Airborne mouse allergen in the homes of inner-city children with asthma. J Allergy Clin Immunol. 2005; 115:358–63. [DOI] [PubMed] [Google Scholar]
- 12.Perry TT, Rettiganti M, Brown RH, Nick TG, Jones SM. Uncontrolled asthma and factors related to morbidity in an impoverished, rural environment. Ann Allergy Asthma Immunol 2012; 108:254–259. [DOI] [PubMed] [Google Scholar]
- 13.Fuller AE, Brown NM, Grado L, Oyeku SO, Gross RS. Material hardships and health care utilization among low-income children with special health care needs. Acad Pediatr 2019;19:733–739. [DOI] [PubMed] [Google Scholar]
- 14.Rosenstreich DL, Eggleston P, Kattan M et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med 1997; 336:1356–63. [DOI] [PubMed] [Google Scholar]
- 15.Gruchalla RS, Pongracic J, Plaut M et al. Inner city asthma study: relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol 2005;115(3):478–485. [DOI] [PubMed] [Google Scholar]
- 16.Northridge J, Ramirez OF, Stingone JA, Claudio L. The Role of Housing Type and Housing Quality in Urban Children with Asthma. J Urban Health. 2010; 87(2):211–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahluwalia S, Peng RD, Breysse PN, et al. Mouse allergen is the major allergen of public health relevance in Baltimore City. J Allergy Clin Immonol 2013; 132(4):830–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pongracic JA, Visness CM, Gruchalla RS, Evans R 3rd, Mitchell HE. Effect of mouse allergen and rodent environmental intervention on asthma in inner-city children. Ann Allergy Asthma Immunol. 2008; 101(1):35–41. [DOI] [PubMed] [Google Scholar]
- 19.Rosenfeld L, Rudd R, Chew G, Emmons K, Acevedo-Garcia D. Are neighborhood-level characteristics associated with indoor allergens in the household? J Asthma 2010; 47(1):66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bradman A, Chevrier J, Tager I et al. Association of housing disrepair indicators with cockroach and rodent infestations in a cohort of pregnant Latina women and their children. Environ Health Perspect 2005;113(12):1795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsui EC, Hansel NN, McCormack MC, Rusher R, Breysse PN, Diette GB. Asthma in the inner city and the indoor environment. Immunol Allergy Clin North Am 2008; 28(3):665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 2004; 351(11);1068–80. [DOI] [PubMed] [Google Scholar]
- 23.Grant T, Phipatanakul W, Perzanowski M, et al. Reduction in mouse allergen exposure is associated with greater lung function growth. J Allergy Clin Immunol 2020; 145(2):646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matsui EC, Perzanowski M, Peng RD, et al. Effect of integrated pest management intervention on asthma symptoms among mouse-sensitized children and adolescents with asthma: a randomized clinical trial. JAMA 2017;317:1027–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canino G, McQuaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J Allergy Clin Immunol 2009;123(6):1209–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romanet-Manent S, Charpin D, Magnan A, Lanteaume A, Vervloet D, for the EGEA Cooperative Group. Allergic vs. nonallergic asthma: what makes the difference? Allergy 2002;57:607–13. [DOI] [PubMed] [Google Scholar]
- 27.Matsui EC, Eggleston PA, Buckley TJ et al. Household mouse allergen exposure and asthma morbidity in inner-city preschool children. Ann Allergy Asthma Immunol 2006;97:514–520. [DOI] [PubMed] [Google Scholar]
- 28.Gergen PJ, Mitchell HE, Calatroni A, Sever ML, Cohn RD, Salo PM, et al. Sensitization and Exposure to Pets: The Effect on Asthma Morbidity in the US Population. J Allergy Clin Immunol Pract. 2017. July 08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neckerman KM, Garfinkel I, Teitler JO, Waldfogel J, Wimer C. Beyond income poverty: measuring disadvantage in terms of material hardship and health. Acad Pediatr 2016;16(3):S52–S59. [DOI] [PMC free article] [PubMed] [Google Scholar]


