Abstract
Introduction
A quarter of all complaints seen in adult primary care and half of all complaints seen in pediatric primary care are otolaryngology related. Even though half of all medical students enter primary care fields, there is no standardized curriculum for otolaryngology during medical school. Due to increasing limitations on specialty teaching during general medical education, computer-assisted instruction has been suggested as a format for increasing exposure to otolaryngology.
Methods
We designed a computer-based learning module for teaching high-yield otolaryngology topics for third- and fourth-year medical students during their primary care clerkship at our institution from 2016–2018. We evaluated students’ prior otolaryngology knowledge with 11 case-based, multiple-choice questions and then evaluated the efficacy of the module by a similar posttest.
Results
Three-hundred and sixty-five students completed the module. The average pre- and posttest scores were 44% (SD = 21%) and 70% (SD = 17%), respectively, showing that the module resulted in significantly increased scores (p < .01).
Discussion
The improvement of test scores indicates that this module was an effective educational intervention at our institution for increasing exposure and improving otolaryngology knowledge in third- and fourth-year medical students. As medical schools shift toward adult learning principles such as independent and self-directed learning, computer-assisted instruction is an alternative to classroom-based didactics. Creating resources for independent study will allow more time for otolaryngology faculty and residents to teach clinical exam skills and interactive case-based discussions, which are less suitable to teach via computer-assisted instruction.
Keywords: Otolaryngology, Primary Care, Computer-Assisted, Self-Regulated Learning
Educational Objectives
By the end of this activity, learners will be able to:
-
1.
Recognize otolaryngology-based clinical cases.
-
2.
Explain common otolaryngology diagnoses.
-
3.
Generate plans for dealing with otolaryngology problems in clinical settings.
Introduction
Almost a quarter of all complaints seen in adult primary care practice and almost half of all complaints seen in pediatric primary care practice are otolaryngology related.1 In 2013, 67% of graduating US medical students entered primary care fields (pediatrics, emergency medicine, internal medicine, family medicine), in which they encountered these complaints.2 Only 34% of medical students in the US are required to participate in an otolaryngology clerkship, and the average exposure to otolaryngology among US medical students ranges from 4 hours to 4 weeks.3 The majority of this exposure occurs during the preclinical years in anatomy and physiology. Currently, there is no standardized otolaryngology curriculum during undergraduate medical education.
Without exposure to otolaryngology during medical school, physicians entering general medical residencies have little confidence in managing otolaryngology conditions commonly seen in primary care, such as otitis media, allergic rhinitis, rhinosinusitis, sudden hearing loss, dysphagia, and tinnitus. In addition, many primary care residents in the US are not aware of the scope of practice for otolaryngology. Of primary care residents in the US polled in a 2012 study, only 47% chose otolaryngologists as experts for thyroid surgery, 32% for sleep apnea, and 3% for facial plastics.4 Furthermore, a 2008 study showed that 50%-60% of general practitioners felt that otolaryngology training during undergraduate medical education was insufficient, and 85% of those practitioners would welcome more otolaryngology education.5
The need for increased otolaryngology training for general practitioners has been well documented in the literature. At our institution, third-year medical students receive at least 2 hours of formal otolaryngology teaching by otolaryngology faculty—a 1-hour lecture during both the primary care and general surgery clerkships. Third- and fourth-year medical students have the opportunity to rotate in otolaryngology for 2 to 4 weeks during the elective time. Other required otolaryngology education, including gross anatomy and clinical exposure, during the pediatric and primary care clerkships are not instructed by otolaryngology faculty. This is a disadvantage to future clinicians who will be referring patients to otolaryngology without sufficient exposure. However, there are barriers to increased specialty teaching during medical school. These barriers include limited faculty time, limited learner time, and decreased perception of relevance to general practice. Due to these limitations, computer-assisted instruction has been suggested as a format for increasing exposure to otolaryngology. The benefits of computer-assisted instruction include availability, repetition, efficiency, and ability for use in self-assessment.6
A literature review was done to evaluate what topics medical students, general practice clinicians, and practicing otolaryngologists deemed important for medical student education. This review focused on topics amenable to computer-assisted instruction and did not include physical exam techniques. A study from 2009 asked medical students, family medicine and emergency medicine physicians, and community otolaryngologists to grade the importance of otolaryngology-related topics and skills for a physician entering a primary care specialty. The highest-ranking topics among all fields were otitis media, rhinitis, sinusitis, angioedema, otitis externa, peritonsillar abscess, sore throat, tonsillar disease, cough, epiglottitis, epistaxis, and hearing loss.7 Community otolaryngologists also ranked hoarseness, gastroesophageal reflux, and dysphagia as highly important.7 Similarly, a 2012 study included the following as essential otolaryngology topics: dizziness/vertigo, ear disease such as otitis externa and media, epistaxis/nasal anatomy, head and neck cancers, hearing loss/tinnitus, neck mass/thyroid disease, pediatric respiratory distress, rhinitis and sinusitis, sore throat, and upper respiratory tract disorder.8 However, a 2015 systematic review by Ishman et al identified knowledge deficits among primary care practitioners in the US to include otitis media, tonsillitis, tracheostomy, and airway obstruction. In the same study, the knowledge considered most important to primary care physicians included understanding hearing loss, interpretation of hearing tests, indications for adenotonsillectomy, and ear and nasal foreign body removal.3 Lastly, a 2012 survey done at our institution, the George Washington University, asked medical students, internal medicine residents, and Children's National Medical Center residents about their confidence in managing various otolaryngology conditions.9 Comfortability increased with year of experience; however, senior residents in both internal medicine and pediatrics only felt completely comfortable with five out of 24 topics. These data functioned as our needs-based assessment and allowed us to select the following topics for inclusion in the module: ear disease, acute sinusitis and its complications, allergic rhinitis, tracheostomy, head and neck masses, hoarseness, epistaxis, hearing loss, and vertigo. These conditions can be emergent, common, and may have a poor outcome if not appropriately recognized.
A search was conducted in MedEdPORTAL to assess whether computer-based learning tools have been implemented in the field of otolaryngology using the following search terms: otolaryngology, computer-based module, computer-assisted instruction, and online module. This search demonstrated limited computer-based teaching in the field of otolaryngology, with most computer-based resources focused on anatomy and quality improvement. However, few of the computer-assisted learning courses found are clinically oriented or case-based, and none of them are specific to otolaryngology. This module is similar to MedEdPORTAL modules in dermatology;10 however, while those present a single case, ours addresses a variety of otolaryngology diagnoses.
Due to the constraints on increased otolaryngology teaching during medical school, we have created an online learning module for undergraduate medical education. The module is a case-based learning tool, which incorporates important and common otolaryngology-related complaints often seen in primary care practice. The purpose of this module is to increase exposure and improve otolaryngology knowledge in third- and fourth-year medical students.
Methods
The development and evaluation of this module followed David Kern's six-step approach for curriculum development in medical education.11 After performing a needs assessment that identified common and important otolaryngology conditions, as well as student comfort levels in treating those conditions in primary care settings, we created an online module (Appendix A). We introduced each topic with a multiple-choice, case-based quiz question, followed by one to five slides on the relevant anatomy, pathophysiology, diagnosis, workup, and management of disease. We created the multiple-choice, case-based questions based on the experience of practicing otolaryngologists at our institution. We obtained information on diagnosis, workup, and management from the American Academy of Otolaryngology-Head and Neck Surgery clinical practice guidelines12 as well as from commonly used otolaryngology references, such as Cummings Otolaryngology13 and Primary Care for Otolaryngology.14
We developed the module slides with Microsoft PowerPoint and formatted them into a screencast video using Camtasia Studio version 8 (TechSmith), which creates an interactive module in which the participant can select answer choices and advance slides. We designed the module with embedded quiz questions to allow the learner to pause at any point. In addition, our module required that the learner respond to each quiz question before proceeding to the subsequent slide. This allowed the facilitator and the learner to evaluate premodule knowledge on each topic. There were 59 slides in the module, including an introductory slide asking about the learner's stage of education (year in medical school) and two free response questions at the end to obtain insight into otolaryngology diagnoses students had previously seen in wards/clinics and on shelf exams, and feedback on the quality of the module. To assess for efficacy of the module, we created a postmodule quiz (Appendix B) that addressed, or expanded upon, the same diagnoses. The quiz consisted of 11 questions in a multiple-choice, case-based, clinical presentation format. Responses were obtained using an online survey tool, Survey Monkey gold version (SurveyMonkey).
The module and postmodule quiz were distributed by email to third- and fourth-year medical students (N = 405) at the George Washington University School of Medicine during their primary care clerkship. The email also included an introduction to the project, explaining the importance of increased exposure to otolaryngology during medical education and was sent 2 weeks prior to the in-person 1-hour otolaryngology lecture. This module was mandatory for students to complete prior to the lecture and upon completion of both assessments, we provided a document with explanations and answers (Appendix B, p. 5-11).
Assessment
We collected data for the module pretest responses using a feature of Camtasia Studio, which provides a detailed report of each respondent's answers, and used a similar feature of Survey Monkey for the posttest data. We collected identifying information only for the purposes of tracking completion. Responses were excluded from the data analysis if completion time was less than 2 minutes for the total of 11 questions, suggesting that these responses were not completed with attention. To eliminate any potential advantage bias, only the students’ first attempt scores were used for analysis. We used an independent-samples t test for a difference in means to analyze the data using SAS version 9.4 (SAS Institute Inc.), with p < .05 considered to be statistically significant. We analyzed the qualitative data by reading through individual survey free-text responses and organizing them based on general categories such as quality of information provided and the quality of software.
The George Washington University Office of Human Research Internal Review Board office deemed this study as exempt.
Results
The results were analyzed after completion of the module (pretest included) and the postmodule quiz, or posttest. The response rate of the posttest was 365 out of 405 students (90%). The average time spent on the pretest and module review was 1 hour and 45 minutes, and the average time spent on the posttest was 46 minutes, for an overall average time spent on this educational tool of 2 hours and 36 minutes.
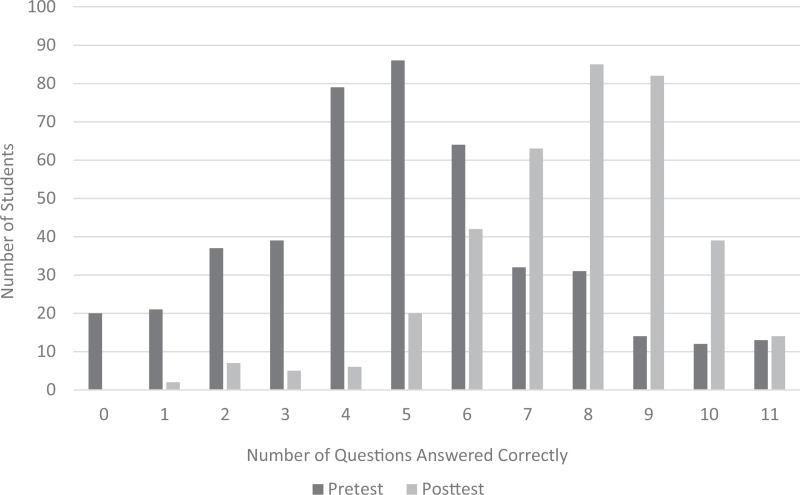
The average score on the pretest was 44% (SD = 24%), with a range of 0% to 100%. The average score on the posttest was 70% (SD = 17%), with a range of 9% to 100% (Figure). Overall posttest scores improved an average of 25% compared to pretest scores. Results from the implemented t test showed a statistically significant increase in posttest scores compared to pretest scores (p < .001). Due to anonymity of the reports, it was not possible to track individual improvement or pair results of pre- and posttest scores.
Figure. Distributions of student scores on pretest and posttest (N = 365).
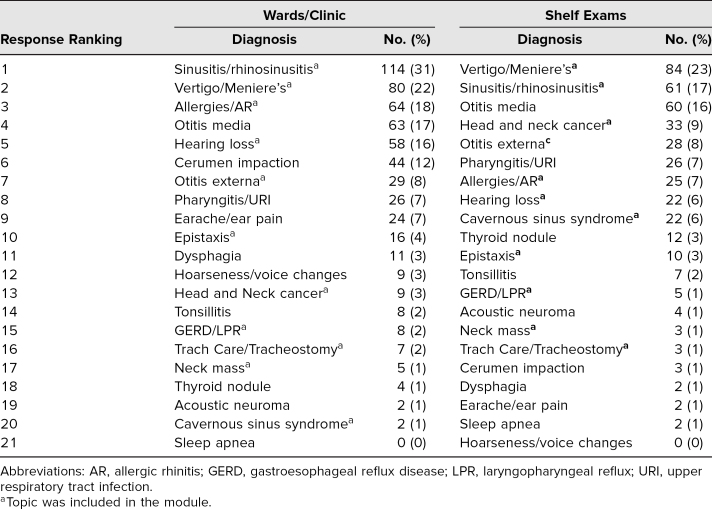
In response to the free-response question on students’ prior clinical exposure and or shelf exam exposure to otolaryngology diagnoses, students mentioned all of the diagnoses presented in the module (Table). Notably, four out of the top five most commonly listed diagnoses in each setting were taught in the module.
Table. Student Free Text Responses of Otolaryngology Diagnoses Seen in Wards/Clinics and on Shelf Exams in Order of Greatest to Least Mentions Compared to Diagnoses Included in the Module.
Overall students responded favorably when asked to comment on module quality and provided few recommendations for improvement. The analysis of student qualitative responses showed that most students appreciated the overall quality of the module, as exhibited by the following responses: “Great module, very short, sweet, and to the point. Very informative and high yield!” and “Loved this module. Very interactive I would recommend it to colleagues.” The module was also found to be appropriate and relevant to students’ clinical experiences, as indicated in the following responses:
-
•
“I liked the information prompted by cases and questions. Slides were helpful, good illustrations chosen. Conditions presented are certainly ones I'd want to be able to know what to do with,”
-
•
“well done and relevant to conditions I've seen […] in primary care clinic.”
-
•
“found the emphasis on current treatment guidelines very helpful.”
Negative responses included comments on audiovisual and software issues that detracted from learning. Many students suggested the addition of audio to the module to improve overall quality and to aid those who are audio learners as opposed to visual leaners. Another student commented that the interface was “clunky and difficult to navigate, [with] no way to go back with a button.”
Other responses included comments on the general lack of otolaryngology teaching during medical school: “More clinical experience with otolaryngology physical exam maneuvers (otoscope, etc.) would be helpful as this is not a part of the first two years.” Another student responded that the module was a “great introduction, [that] got [the student] interested in ENT.” Additionally, one student remarked that this method of learning should “be used more frequently, not only for otolaryngology but for other clerkships/specialties, […] it is very helpful.”
Discussion
We developed an effective educational tool for teaching otolaryngology for the primary care setting during medical school using computer-assisted technology. Significant improvement of posttest scores, when compared with pretest scores, indicates that this module was an effective educational intervention for enhancing otolaryngology education and exposure at our institution.
Student free-text answers regarding which otolaryngology diagnoses they have encountered in the wards/clinic or on shelf exams showed that our module covered 11 out of the 21 mentioned diseases in either setting and contained four out of the five most mentioned diagnoses in each setting. Otitis media was one of the top five diagnoses in both settings and was not covered in our module. The addition of this diagnosis should be considered in future iterations. Additionally, depending on the desired length of the module, instructors could consider adding other diagnoses that they feel are relevant and important. There is no recent literature indicating general trends in otolaryngology topics encountered on medical school exams.
Student free-text feedback indicated the module met students’ needs of being current and relevant to their clinical exposure and an overall positive experience, while also indicating a desire for earlier exposure to otolaryngology, as reflected by comments demonstrating interest in pursuing otolaryngology as a specialty as a result of this exposure. This implies that if not for this module, the student may not have realized his or her interest in the field and may have impacted the decision to pursue an otolaryngology residency. This is important during a time when the field of otolaryngology has seen the number of residency applications fluctuating.15 This is supported by Bhalla and colleagues who concluded that the applicant selection process needs to be modified, and that early introduction to otolaryngology is important for the future of the field.16 In addition, the Otolaryngology Program Directors Organization has taken initiative to inform otolaryngology program directors at medical schools that medical students should have “early exposure to otolaryngology in the curriculum,” in order to counteract the decrease in otolaryngology resident applications that was seen in years prior to the match in 2019.15 For these reasons, the need for increased exposure to otolaryngology in undergraduate medical education in a time efficient manner, makes this computer-assisted instruction ideal. While some comments also indicated there were audiovisual and software issues that may have taken away from learning, further improvements can be made to address all learning styles.
Limitations
While we believe our experience demonstrates an ideal use for computer-assisted instruction, there were limitations to our study. We collected identifying information only for the purposes of tracking completion, and following completion we immediately deidentified the data. For this reason, the pre- and posttest data are not paired with each student, so the most optimal statistical test (paired t test) could not be used. Instead, we used the next most appropriate statistical test (independent-samples t test) to compare the means and variance of the two groups. Future data collection for optimal evaluation of a module such as this one should ideally have paired data for a paired t test. Additionally, student survey responses regarding encountered otolaryngology diagnoses were subject to recall bias.
Another limitation may be the scope of topics covered. Due to limited literature regarding inclusion of otolaryngology during US medical school education, most of the data we presented were based on foreign studies. Investigators of this study are currently working on a needs assessment to identify topics for inclusion in an otolaryngology curriculum for medical students in the US based on input from program directors of internal medicine and otolaryngology residencies. This will further identify appropriate topics for inclusion to optimize students’ educational needs. In addition, the computer-assisted education is limited by the inability to include education regarding clinical skills. Other researchers have investigated the benefit of using computer-assisted instruction to teach physical exam skills and clinical diagnosis. An otoscopy simulator has been used to teach otoscopy and improve diagnostic accuracy with a student-reported average increase in confidence of 93% following intervention.17,18 Simulation could be a method to improve clinical diagnosis when clinical experience may be limited.
Options to improve the module include adding audio narration to accompany the slides, in order to engage both auditory and visual learners. In order to improve the interface of the module and allow students to access the module from a variety of devices including smartphones and computers, we could look into using another software for the module. We also recommend that a PDF version of the module is provided to students for offline studying.
Implications of Computer-Assisted Instruction in Teaching Otolaryngology
Despite these limitations, we believe that computer-assisted instruction requires few resources in regard to classroom and faculty time. It can be completed outside of the classroom and can serve as an introduction to otolaryngology for many students who do not have this opportunity in the early years of the current undergraduate medical school curriculum. Prior research has implicated computer-assisted instruction in teaching otolaryngology during undergraduate medical education.3,6
As medical schools shift toward adult learning principles such as independent and self-directed learning, computer-assisted instruction is a reasonable alternative to classroom-based didactics. However, this should not replace the dedicated curricular time for otolaryngology teaching. This discussion is especially relevant in the present time, given the constraints on preclinical and clinical medical school curriculum in the era of COVID-19. Many medical schools entered the fall 2020 semester entirely virtual with few exceptions for the preclinical curriculum, and many medical schools, including ours, are looking for more online-only electives or online supplementary didactic teaching to offer third- and fourth-year students in their clerkships. We propose that online learning modules will not only be of benefit for the new norm of learning that is being imposed on students due to COVID-19, but also may be more suitable for those that favor self-directed learning. In the field of otolaryngology, when students are not able to visit other programs for away rotations per usual, an online module such as this could be the component of a virtual-acting internship, a concept that many programs have begun to offer in recent months.
Additionally, we propose that creating resources for independent study, such as computer-based modules, will allow for more time for otolaryngology faculty and residents to focus on teaching other educational components, such as clinical exam skills and interactive case-based discussions, which are less suitable to teach via computer-assisted instruction. This type of instruction also applies to the flipped-classroom teaching model, in which students have prework dedicated to a particular topic that is then expanded upon during a didactic session with professors. The American Academy of Otolaryngology-Head and Neck Surgery provides modules to students on their website which include references to resources for learning objectives in otolaryngology and some case-based questions and answers. However, this requires the student to find the references on their own and is not interactive.19 The implementation of a more interactive module with resources presented to students, as is done in our module, could allow for modules such as this one to be used more widely and would provide additional data about the efficacy of this module.
A standardized curriculum for otolaryngology during undergraduate medical education does not currently exist. Our institution dedicates 2 hours of otolaryngology lecturing in two of the required core clerkships. We believe that this module can reduce some of the limitations on specialty training during undergraduate medical education, including perceived irrelevance to general practice, as well as learner and teacher time. The overall goal is to increase exposure to otolaryngology to better prepare future physicians to manage otolaryngology complaints seen in primary care. Today's learners desire more personalized learning, and this format was suitable due to the ability of the student to work at their own pace and in any location.
Appendices
- Student Module and Pretest folder
- Posttest.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Ethical Approval
The George Washington University Office of Human Research Internal Review Board approved this study.
References
- 1.Mace AD, Narula AA. Survey of current undergraduate otolaryngology training in the United Kingdom. J Laryngol Otol. 2004;118(3):217–220. 10.1258/002221504322928008 [DOI] [PubMed] [Google Scholar]
- 2.The Match: National Resident Matching Program—Results and Data: 2018 Main Residency Match. National Resident Matching Program; 2018. https://www.nrmp.org/wp-content/uploads/2018/04/Main-Match-Result-and-Data-2018.pdf [Google Scholar]
- 3.Ishman SL, Stewart CM, Senser E, et al. Qualitative synthesis and systematic review of otolaryngology in undergraduate medical education. Laryngoscope. 2015;125(12):2695–2708. 10.1002/lary.25350 [DOI] [PubMed] [Google Scholar]
- 4.Hu A, Sardesai MG, Meyer TK. A need for otolaryngology education among primary care providers. Med Educ Online. 2012;17:17350 10.3402/meo.v17i0.17350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glicksman JT, Brandt MG, Parr J, Fung K. Needs assessment of undergraduate education in otolaryngology among family medicine residents. J Otolaryngol Head Neck Surg. 2008;37(5):668–675. [PubMed] [Google Scholar]
- 6.Fung K. Otolaryngology—head and neck surgery in undergraduate medical education: advances and innovations. Laryngoscope. 2015;125(suppl 2):S1–S14. 10.1002/lary.24875 [DOI] [PubMed] [Google Scholar]
- 7.Wong A, Fung K. Otolaryngology in undergraduate medical education. J Otolaryngol Head Neck Surg. 2009;38(1):38–48. 10.1016/j.otohns.2009.06.111 [DOI] [PubMed] [Google Scholar]
- 8.Oyewumi M, Isaac K, Schreiber M, Campisi P. Undergraduate otolaryngology education at the University of Toronto: a review using a curriculum mapping system. J Otolaryngol Head Neck Surg. 2012;41(1):71–75. [PubMed] [Google Scholar]
- 9.Wiedermann JP, Zapanta PE. Comfort level managing common head and neck disease. Presented at: American Academy of Otolaryngology-Head and Neck Surgery Foundation; September 9–12, 2012; Washington, DC. [Google Scholar]
- 10.Nguyen L, Mahalingam M, Garg A. Dermatology clinical case modules: 40-year-old woman with a dark mole. MedEdPORTAL. 2010;6:8067 10.15766/mep_2374-8265.8067 [DOI] [Google Scholar]
- 11.Thomas PA, Kern DE, Hughes MT, Chen BY, eds. Curriculum Development for Medical Education: A Six-Step Approach. 3rd ed Johns Hopkins University Press; 2015. [Google Scholar]
- 12.Clinical practice guidelines. American Academy of Otolaryngology-Head and Neck Surgery. Accessed 2020. https://www.entnet.org/content/clinical-practice-guidelines
- 13.Flint PW, Haughey BH, Lund VJ, et al. Cummings Otolaryngology: Head and Neck Surgery Foundation. 6th ed Elsevier; 2015. [Google Scholar]
- 14.Wax MK, ed. Primary Care Otolaryngology. 3rd ed American Academy of Otolaryngology-Head and Neck Surgery Foundation; 2011. [Google Scholar]
- 15.Chang CWD, Gray ST, Malekzadeh S, et al. Cultivating and recruiting future otolaryngology residents: shaping the tributary. Otolaryngol Head Neck Surg. 2019;160(1):8–10. 10.1177/0194599818797091 [DOI] [PubMed] [Google Scholar]
- 16.Bhalla V, Sykes KJ, Kraft SM, Chiu AG. Commentary on Bowe et al, “The state of the otolaryngology match: a review of applicant trends, ‘impossible’ qualifications, and implications.” Otolaryngol Head Neck Surg. 2018;158(2):217–218. 10.1177/0194599817737277 [DOI] [PubMed] [Google Scholar]
- 17.Lee DJ, Fu TS, Carrillo B, Campisi P, Forte V, Chiodo A. Evaluation of an otoscopy simulator to teach otoscopy and normative anatomy to first year medical students. Laryngoscope. 2015;125(9):2159–2162. 10.1002/lary.25135 [DOI] [PubMed] [Google Scholar]
- 18.Davies J, Djelic L, Campisi P, Forte V, Chiodo A. Otoscopy simulation training in a classroom setting: a novel approach to teaching otoscopy to medical students. Laryngoscope. 2014;124(11):2594–2597. 10.1002/lary.24682 [DOI] [PubMed] [Google Scholar]
- 19.Medical student resources. American Academy of Otolaryngology-Head and Neck Surgery; https://www.entnet.org/content/medical-student-resources [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Student Module and Pretest folder
- Posttest.docx
All appendices are peer reviewed as integral parts of the Original Publication.