Abstract
Background:
Under-reporting and recognition of occupational diseases is a problem in countries with workers’ compensation schemes.
Objective:
To describe the role of a public hospital Occupational Disease Unit (ODU) in Barcelona that resulted in improved reporting and official recognition of occupational diseases from 2010 to 2017.
Methods:
Hospital physicians referred possible cases of work-related disease to the ODU, where in-depth medical evaluations were then performed, and a detailed report addressing causation was generated. Patients with confirmed cases of occupational disease were counselled and followed while pursuing official recognition and benefits claims by the Spanish Social Security System.
Results:
Between 2010 and 2017, 149 cases were referred to the ODU for evaluation. Of these, 80 (53.7%) were confirmed to have an occupational disease, 54 (67.5%) patients pursued official recognition, and to date 26 (48.1%) have been recognized by the Social Security System. The recognition rate varied by diagnosis group (p=0.003), and was highest for skin diseases (71.4%) and cancer (66.7%), and lowest for hearing loss (29.4%) and musculoskeletal disorders (16.7%).
Conclusions:
A hospital ODU can improve reporting and official recognition of occupational diseases that otherwise might not have been recognized. Expanding this experience to other Spanish and European hospitals could improve the efficiency of workers’ compensation schemes and better support preventive policies.
Key words: Occupational medicine, social security, work-related disease, occupational disease
Abstract
«Un’Unità ospedaliera di Medicina del Lavoro: un’esperienza per aumentare il riconoscimento delle malattie professionali».
Introduzione:
La sottostima e il basso riconoscimento delle malattie professionali è un problema comune nei paesi europei che spesso non permette al lavoratore di ottenere il riconoscimento del danno e il risarcimento pur previsto dalla legge. La medicina del lavoro ospedaliera, se presente, può eserciatare un ruolo importante per individuare l’eziologia professionale in casi segnalati dagli specialisti in altre discipline.
Obiettivi:
Descrivere il ruolo dell’Unità di Medicina del Lavoro (UML) di un ospedale pubblico di Barcellona, Spagna, nel migliorare la denuncia e il riconoscimento delle malattie professionali, attraverso iniziative mirate condotte in ospedale nel periodo 2010-2017.
Metodi:
I medici ospedalieri hanno segnalato i possibili casi di malattie lavoro-correlate all’UML, dove sono stati svolti approfonditi accertamenti medici e redatti dettagliati referti sulle cause del disturbo. I pazienti con malattie professionali accertate hanno ricevuto consulenza e sono stati seguiti nel percorso di richiesta di riconoscimento ufficiale e di prestazioni sanitarie, da parte del sistema sociosanitario spagnolo.
Risultati:
Tra il 2010 e il 2017, 149 casi sono stati indirizzati all’UML. Di questi, 80 (53.7%) hanno vista confermata la diagnosi di malattia professionale da parte della medicina del lavoro, 54 (67.5%) pazienti hanno richiesto risarcimento ai sensi della legge e, a oggi, 26 (48.1%) hanno ottenuto il riconoscimento da parte del sistema sociosanitario spagnolo. Il tasso di riconoscimento varia in base alla tipologia della malattia diagnosticata (p=0.003), ed è maggiore per le malattie della pelle (71.4%) e il cancro (66.7%), minore per l’ipoacusia (29.4%) e i disturbi muscoloscheletrici (16.7%).
Conclusioni:
Una UML ospedaliera può rendere più efficace il processo di denuncia e il tasso di riconoscimento ufficiale delle malattie professionali che diversamente potrebbero non essere individuate. Allargare questa esperienza ad altri ospedali spagnoli ed europei potrebbe migliorare l’efficienza dei programmi di compensazione dei lavoratori e meglio supportare politiche di prevenzione.
Introduction
Under-reporting and recognition of occupational disease are longstanding problems that have shown little improvement in most countries with workers’ compensation schemes (16). Lack of awareness of legal obligations and financial incentives are important drivers, together with conflicting interests among stakeholders (insurance companies, employers, workers, and government), leading to complex management issues (2, 4).
To date, most published experience has focused on proposing surveillance systems that include both official occupational and work-related diseases (3, 14, 15). However, an essential challenge of occupational medicine is to identify, report and assure official recognition of occupational disease, so that workers receive just benefits and health care (5).
Certainly, as the EUROGIP report has underscored for Italy, Germany, France, Denmark and Spain (9), under-reporting of occupational diseases that are eligible for recognition of their work-related nature and compensation of the victims is a general problem in all countries. This is especially the case in Spain, where there are no data on the overall number of claims submitted for recognition by the social security system. Furthermore, although in Spain physicians are able to report suspected cases of occupational disease, it is not mandatory and there are no financial incentives to do so, unlike Germany or Denmark.
To deal with the under-reporting of occupational diseases, several initiatives have been developed, mainly focused on general practitioners. A recent systematic review to evaluate the effects of interventions aimed at increasing the reporting of occupational diseases by physicians found that new interventions simplifying the reporting procedure and providing financial incentives are needed (8).
In this study, we describe the role and results of a public hospital Occupational Disease Unit (ODU) in Barcelona (Spain), specifically designed to improve the identification and official recognition of occupational diseases.
Methods
In Spain, where there is an official list of occupational diseases similar to the European list since 2006, any doctor can report the suspicion of an occupational disease. However, a medical committee of the national social security system is the one who officially recognizes it as an occupational disease. Parc de Salut Mar (PSMar) is a public hospital system in Barcelona (Spain), with 1038 beds, over 900 physicians, and more than 30,000 inpatient admissions in 2017. Since 2010, PSMar physicians can refer their patients to the ODU if they suspect an occupational disease. To encourage physician participation, we prepared a finite list of diagnoses for each clinical department, each with broad referral criteria, mostly centered on a history of specific occupational exposures (12). An occupational physician then screened each case referred to the ODU, using the information available in the medical record and/or a brief phone interview with the patient. Those with a suspected occupational disease were then invited for a face-to-face clinical visit with the occupational physician. This initiative was supplemented by periodic talks and seminars to the clinical departments where we provided feedback on the outcomes of the ODU. Most of the cases during the study period came from the otorhinolaryngology (n=50), oncology (n=26), dermatology (n=20), and traumatology (n=19) departments.
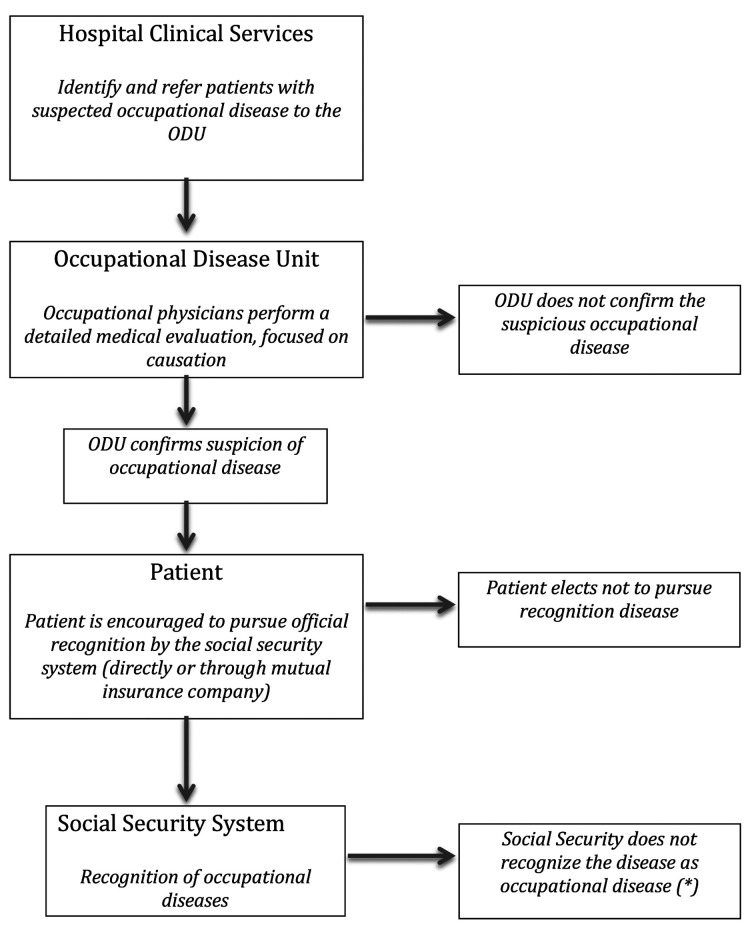
At the ODU, on average one month later, occupational medicine specialists perform an in-depth medical evaluation, focused on a causation analysis (figure 1). In brief, a detailed report is prepared, in which a causal opinion and its rationale are documented, with supporting bibliography from both the scientific literature and official regulations (13). To determine causation, the ODU physicians apply two criteria based on the legal definition of occupational disease in Spain: 1) the disease must be included in the official list of occupational diseases in Spain, and 2) the occupational exposure must also be included as a cause of the disease in the same official list.
Figure 1.
Occupational Diseases Unit (ODU) flow chart. Parc de Salut Mar, Barcelona (Spain)
(*) The patient can appeal to the Court
When an occupational disease is confirmed by the ODU, patients are encouraged to request official recognition from the Social Security System. The Social Security System makes the final determination of work-relatedness, but workers can take the case to court if the claim is denied. When a PSMar patient elects to pursue official recognition, the ODU provides guidance and monitors progress as the worker navigates an oftentimes complex bureaucracy.
We examined the activities of the ODU from 2010 to 2017, estimating the following indicators: 1) confirmation rate (CR) (cases confirmed by the ODU as occupational disease/ suspected cases referred by PSMar physicians); 2) starting reporting process rate (SRPR) (cases that initiated the official recognition process/ cases confirmed by the ODU as an occupational disease); and 3) recognition rate (RR) (cases recognized by the Social Security System/ cases that initiated the official recognition process). These indicators were examined by sex, age (< 55 versus ≥ 55 years) and medical diagnosis groups (musculoskeletal, cancer, skin, ear and others such as asthma and infection diseases). Statistical significance of the differences was estimated by the chi-square test. The study protocol was approved by the PSMar Clinical Research Ethics Committee.
Results
Over the study period, a total of 149 cases were referred by physicians for suspicion of occupational disease. Of these, 12 (8%) cases declined further evaluation for personal reasons, 57 (38.3%) cases were assessed as non occupational diseases, and 80 (53.7%) were confirmed by the ODU physicians as occupational disease. Of the latter, 54 (67.5%) initiated the recognition process, 26 (48.1%) had their claims officially recognized by the Social Security system (24 by the administrative route, and two are in court), and another six (11.1%) remain under review. Of the 26 recognised cases, there were five cases each of mesothelioma, hearing loss, and viral disease (enterovirus, adenovirus and influenza), three were dermatitis, two lung cancers, two cases of asthma, and the remainder were single cases of epicondylitis, nasopharyngeal cancer, latex allergy, and a rotator cuff syndrome. In relation to cancers, various occupational risks were identified. For example, wood dust in case of adenocarcinoma of the ethmoids and paranasal sinuses; asbestos in malignant mesothelioma (pleura and peritoneum); and asbestos, hexavalent chromium, nickel, and crystalline free silica powder in the case of malignant bronchial and lung neoplasm.
The overall CR varied between 40% and 60%, being higher in men (62.5% vs 37.7%; p = 0.004), the older age group (63.3% vs 40.3%; p= 0.006), and also higher for the hearing loss, skin and musculoskeletal than cancer and other groups (78.6%, 52.4%, 51.9%, versus 38.1%, and 35.3%, respectively; p= 0.002). The SRPR was higher in women (90% vs 60%; p= 0.013), but there were no statistically significant differences by age or diagnosis groups. The RR only differed significantly by medical diagnosis groups (p=0.004), being higher for skin diseases (71.4%) and cancer (66.7%) than for musculoskeletal disorders (16.7%) and hearing loss (29.4%).
Discussion
Our results indicate that the addition of the ODU to the PSMar has improved the identification and recognition of occupational diseases in its patient population. These 26 cases, ultimately recognised officially as occupational diseases, would almost certainly not have been officially accepted. However, although we could have expected all ODU confirmed cases to also be officially recognized by the social security, since presumably both use similar scientific and legal criteria, there was a discrepancy in 22 cases. It would be useful to explore the underlying reasons for this discrepancy, but the Spanish social security system does not provide this information to either the worker or the referring physician.
Table 1.
Distribution of cases (n) and rates (%) of identified, confirmed, started recognition process and officially recognized occupational disease by sex, age and medical diagnostic groups. Occupational Disease Unit (ODU). Parc de Salut Mar, 2010-2017
| Table 1-A | ||||||||||
| Sex | Age (years) | |||||||||
| Men | Women | P | Less than 55 | 55 and more | P | |||||
| Cases (n) | Rate (%) | Cases (n) | Rate (%) | Cases (n) | Rate (%) | Cases (n) | Rate (%) | |||
| Identified suspected cases | 96 | 53 | 62 | 87 | ||||||
| ODU confirmed cases | 60 | 20 | 25 | 55 | ||||||
| CR (1) | 62.5 | 37.7 | 0.004 | 40.3 | 63.2 | 0.006 | ||||
| Started Recognition Process Rate | 36 | 18 | 15 | 39 | ||||||
| RPR (2) | 60.0 | 90.0 | 0.013 | 60.0 | 70.9 | 0.334 | ||||
| Recognized cases | 17 | 9 | 10 | 16 | ||||||
| PPV (3) | 47.2 | 50.0 | 0.847 | 66.7 | 41.0 | 0.091 | ||||
| (1) CR: confirmation rate; (2) RPR: recognition process rate; (3) PPV: predictive positive value; p value Chi square test | ||||||||||
| Table 1-B | |||||||||||
| Diagnostic groups | |||||||||||
| MSK | Cancer | Skin | Ear | Others | P | ||||||
| Cases (n) | Rate (%) | Cases (n) | Rate (%) | Cases (n) | Rate (%) | Cases (n) | Rate (%) | Case (%) | Rate (%) | ||
| Identified suspected cases | 27 | 42 | 21 | 42 | 17 | ||||||
| ODU confirmed cases | 14 | 16 | 11 | 33 | 6 | ||||||
| CR (1) | 51.9 | 38.1 | 52.4 | 78.6 | 35.3 | 0.002 | |||||
| Started Recognition Process Rate | 12 | 12 | 7 | 17 | 6 | ||||||
| RPR (2) | 85.7 | 75.0 | 63.6 | 51.5 | 100 | 0.076 | |||||
| Recognized cases | 2 | 8 | 5 | 5 | 6 | ||||||
| PPV (3) | 16.7 | 66.7 | 71.4 | 29.4 | 100 | 0.004 | |||||
| (1) CR: confirmation rate; (2) RPR: recognition process rate; (3) PPV: predictive positive value; p value Chi square test; MSK musculoskeletal disorders | |||||||||||
In any case, the ODU assisted over half of the workers initially identified in navigating a complex process to obtain benefits and medical care. It is likely that, in the absence of the ODU, these cases would have not been reported or officially recognized. To our knowledge, this is the first study in Spain to provide an estimate of the reported to recognized case ratio, one out of three, compared to one out of four described in the EUROGIP report (9) for Italy, Germany, France and Denmark. Although this report included Spain, this ratio was not provided for our country. The higher RR in our paper can be explained in part because all cases came from a hospital, were exhaustively evaluated and, most importantly, were meticulously followed to their conclusion. The lowest values in RR for musculoskeletal and hearing disorders could be due to the fact that these disorders can share both occupational and non-occupational exposures that are often difficult to disentangle. In contrast, the higher RR for cancer cases is likely due to focusing only on those cancers for which occupation has a higher attributable fraction (6).
Clearly, there are opportunities to improve the ODU evaluation and management process. Undoubtedly, not all hospital clinical departments identify all possible cases of suspected occupational disease they manage. Periodic departmental and hospital-wide seminars that review case referral criteria and provide feedback on results could improve clinician awareness and motivation to refer cases to the ODU. Death (especially in cases of cancer) and fear of employer reprisal are among the reasons when, despite being confirmed by the ODU, a case may not progress to recognition. Follow-up during the process, contacting patients periodically to offer information and assistance, and accompanying them to Social Security appointments could be helpful. Special attention is needed for cancer cases (where the patient is often no longer working) and musculoskeletal disorders (where the patient is often still employed). Although the overall numbers are modest, we are now expanding this initiative to 10 other Spanish hospitals.
A limitation of this study is that we could not assess the impact of the ODU on official OD statistics. First, because the number of cases identified by the ODU, and eventually recognised by the Social Security, was small. Second, because official statistics are reported by province, and our hospital is only one of 26 (public and private) in the province. In 2017, there were 2107 accepted occupational diseases in Barcelona province (11), and it is reasonable to assume that at least some of these were recognised thanks to the ODU. In Spain it has been estimated that 83% of occupational and work-related diseases are not recognized as such (10).
There are several implications from this study. Hospitals can play an important role in the identification of suspected cases of occupational disease. Training medical specialists and informing patients properly on how to initiate the process for the recognition of occupational diseases is essential. This effort can significantly increase visibility of the speciality of occupational medicine in hospitals. Lastly, we should not forget that the main beneficiaries of this effort are the workers and their families, who acknowledge the help and support of the ODU. As an example, one family member emailed us, noting: “Although the recognition arrived in his last month of life, my father was grateful to know he left my mother in a better economic situation.”
In conclusion, this initiative stands to contribute to occupational disease surveillance by increasing the number of cases initially not recognized by Social Security. An effort to involve other Spanish and European hospitals in such an initiative could improve occupational disease workers’ compensation schemes and the information to support preventive policies (7).
Key points
Hospitals can play a sentinel role in detecting and reporting cases of occupational disease, as an essential step in securing compensation by social insurance schemes.
A hospital-based occupational disease unit can confirm suspected occupational disease and assist patients in navigating a complex process to secure their right to social benefits.
Expanding this experience to other Spanish and European hospitals could improve the efficiency of workers’ compensation schemes and better support preventive policies.
No potential conflict of interest relevant to this article was reported by the authors
Acknowledgment:
We thank Ana Beltrán, Alonso-Fernando López, Cristina Alvarado for evaluating cases; Álvaro Taus, Ana Giménez, Marta Costey, Montserrat Canton, Rocío Villar, Edurne Arriola, María Gloria Nohales, Pilar Ausín, Gemma Pidemunt, Eva Balcells, Marta Amat, Roser Belmonte, Carles Torrent, Marta Bertolin for referring patients. Olga Martínez, Sandra Garrido for patients contact/follow-up.
Funding:
This work was partly supported by FIS P016/00061 and an agreement between UPF and PSMar. The funders had no role in the study design, data collection, analysis or interpretation of results. The authors have the final responsibility for the paper. GLD was also supported by grant number T42 OH008421 from the U.S. Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health.
References
- 1.Agius R, Lenderink A, Colosio C. Finding ‘new’ occupational diseases and trends in ‘old’ ones. Occup Med (Lond) 2015;65:607–609. doi: 10.1093/occmed/kqv110. [DOI] [PubMed] [Google Scholar]
- 2.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: Conceptual filters explain underreporting. Am J Public Health. 2002;92:1421–1429. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bakusic J, Lenderink A, Lambreghts C, et al. Alert and sentinel approaches for the identification of work-related diseases in the EU. Luxembourg: Publications Office of the European Union, 2018. Available on line in: https://osha.europa.eu/en/tools-and-publications/publications/alert-and-sentinel-approaches-identification-work-related/view . Last accessed 4-7-2019. [Google Scholar]
- 4.Benavides FG, Castejón J, Gimeno D, et al. Certification of occupational diseases as common diseases in a primary health care setting. Am J Ind Med. 2005;47:176–180. doi: 10.1002/ajim.20128. [DOI] [PubMed] [Google Scholar]
- 5.Benavides FG, Boix P, Ramada JM, Serra C. (en nombre les equipo de investigación del proyecto CEPS): Su enfermedad tiene que ver con el trabajo: guía para promover el reconocimiento de una enfermedad profesional. Sevilla: i+3, 2018. Available on line in: https://www.upf.edu/web/cisal/proyecto-ceps . Last accessed 23-6-2019. [Google Scholar]
- 6.Bonzini M, Facchinetti N, Motolese A, et al. Looking for “lost occupational cancers”: a systematic evaluation of occupational exposure in a case series of cutaneous squamous cell carcinomas in Italy. Med Lav. 2013;104:224–235. [PubMed] [Google Scholar]
- 7.Colosio C, Mandic-Rajcevik M, Godderis L, et al. Workers’ health surveillance: implementation of the Directive 89/391/ECC in Europe. Occup Med (Lond) 2017;67:574–578. doi: 10.1093/occmed/kqx113. [DOI] [PubMed] [Google Scholar]
- 8.Curti S, Sauni R, Spreeuwers D, et al. Interventions to increase the reporting of occupational diseases by physicians: a Cochrane systematic review. Occup Environ Med. 2016;73:353–354. doi: 10.1136/oemed-2015-103209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eurogip report-102/E. Reporting of occupational diseases: issues and good practices in five European countries. Available on line at: https://www.eurogip.fr/en/projects/publications-d-eurogip . Last accessed 23-6-2019. [Google Scholar]
- 10.García AM, Gadea R. Incidence and Prevalence of Occupational Diseases in Spain. Aten Primaria. 2008;40:439–446. doi: 10.1157/13126417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministerio de Trabajo, Migraciones y Seguridad Social. Enfermedades profesionales. Available on line at: http://www.seg-social.es/wps/portal/wss/internet/EstadisticasPresupuestosEstudios/Estadisticas/EST231/2082/EST268 . Last accessed 23-6-2019. [Google Scholar]
- 12.Ramada JM, Delclós J, Benavides FG, et al. Evaluación de una unidad de detección de enfermedades profesionales en un hospital de tercer nivel. Arch Prev Riesgos Labor. 2014;17:18–25. doi: 10.12961/aprl.2014.17.1.03. [DOI] [PubMed] [Google Scholar]
- 13.Serra C, Ramada JM, Delclòs J, Benavides FG. en nombre del Grupo Seguimiento UPL-PSMar/CiSAL: Enfermedades profesionales tratadas en el Hospital del Mar de Barcelona [Occupational diseases treated at Parc de Salut Mar (Barcelona, Spain), 2010-2014] Med Clin (Barc) 2016;146:506–510. doi: 10.1016/j.medcli.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Spreeuwers D, De Boer AG, Verbeek JH, van Dijk FJ. Characteristics of national registries for occupational diseases: international development and validation of an audit tool (ODIT) BMC Health Serv Res. 2009;9:194. doi: 10.1186/1472-6963-9-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spreeuwers D, De Boer AG, Verbeek JH, van Dijk FJ. Evaluation of occupational disease surveillance in six EU countries. Occup Med (Lond) 2010;60:509–516. doi: 10.1093/occmed/kqq133. [DOI] [PubMed] [Google Scholar]
- 16.Stocks SJ, McNamee R, van der Molen HF, et al. Trends in incidence of occupational asthma, contact dermatitis, noise-induced hearing loss, carpal tunnel syndrome and upper limb musculoskeletal disorders in European countries from 2000 to 2012. Occup Env Med. 2015;72:294–303. doi: 10.1136/oemed-2014-102534. [DOI] [PubMed] [Google Scholar]