Abstract
Context:
Paget's disease of bone is a common bone disease with a striking variation in its incidence and characteristics in different parts of the world. It is uncommonly reported in African patients.
Aims:
Given the lack of studies describing the characteristics of patients with Paget's disease of bone in North Africa, we aimed to describe demographic, clinical, biochemical, and imaging characteristics, as well as treatment outcomes of Tunisian patients with Paget's disease of bone.
Subjects and Methods:
This bicentric and retrospective study included patients with Paget's disease of bone. Clinical, laboratory, radiological profile, and response to treatment were analyzed.
Results:
Sixty-nine patients were identified. The mean age was 64.9 ± 11.6 years and 52.2% were women. One patient reported a positive family history. Seven patients were asymptomatic. Bone pain was the most common presenting symptom. Eight patients had a history of malignancy. In three patients, Paget's disease of bone was diagnosed as part of a metastatic workup. Monostotic disease was found in half of the cases. The most commonly involved sites were pelvis (43.5%), femur (21.7%), and spine (21.7%). The mean serum alkaline phosphatase level at presentation was 591 U/L (68–8380). Two patients received salmon calcitonin (2.8%) and 47 patients (68.1%) received bisphosphonates. After a mean follow-up of 55 months (2–240 months), bone pain improved in 43.1% of patients and the serum alkaline phosphate levels had normalized in 22 of them (43.1%). During follow-up, there was no malignant transformation.
Conclusions:
In this series of Tunisian patients, Paget's disease of bone had a female predominance and was usually monostotic. The clinical and radiological presentations were similar to the European series.
Keywords: Benign bone disease, bisphosphonate, imaging, Paget's disease of bone, treatment
INTRODUCTION
Paget's disease of bone is the second most common metabolic bone disease after osteoporosis. Genetic factors have been identified in the pathology of this disorder.[1] The risk of developing Paget's disease of bone increases with age. After 50 years, the incidence of Paget's disease of bone appears to double each decade;[2] here is a striking heterogeneity in the incidence of Paget's disease of bone. Individuals of European descent are predominantly affected,[3] while the presence of Paget's disease of bone is rare in Africans and Asians. The highest prevalence of the disease has been reported in Britain (8.3% in Lancashire in 1980) followed by Australia, New Zealand, and the northeastern United States.[4] However, during the last years, there has been an increasing decline in the prevalence and severity of this bone disorder. As demonstrated in Lancashire, from 1994-1995, the prevalence of Paget's disease of bone diminished to 3.7%,[5] and by 2017, the prevalence had further declined to 0.8%.[6]
Currently, the overall prevalence of Paget's disease of bone is approximately 0.3% worldwide.[7]
This benign bone dystrophy is responsible for condensing, hypertrophic, and deforming lesions. However, the majority of cases are incidentally diagnosed on radiographs or bone scans performed for other reasons or during the discovery of elevated serum alkaline phosphatase levels.
This finding helps to explain the underestimated prevalence and diagnostic delay. In symptomatic patients, clinical features vary from bone pain to life-threatening complications.[8] The disease can affect a single bone (monostotic) or two or more bones (polyostotic); common sites include the pelvis, femur, lumbar spine, skull, and tibia. Clinical presentation, distribution of affected bones, and complications vary widely between regions. Given the rarity of Paget's disease of bone in the African continent, data regarding the characteristics of African patients are limited.
In a previous report about the origin of patients with Paget's disease of bone in Israel, 44% were Afro-Asians, with Tunisians representing the largest group.[9] A literature search did not shed light on the characteristics of Paget's disease of bone patients in the Maghreb. Thus, this study aimed to describe demographic, clinical, biochemical, and imaging characteristics, as well as treatment outcomes of Tunisian patients with Paget's disease of bone.
SUBJECTS AND METHODS
Study design
A bicentric retrospective study was conducted in the Department of Rheumatology at two Tunisian university hospitals, from March to December 2019.
Patients
This study included patients diagnosed with Paget's disease of bone between 1994 and 2019. Patients with X-rays of poor quality or small size were excluded. Cases with incomplete data were also excluded. The diagnosis was based on radiological features of Paget's disease of bone, including bony expansion with cortical thickening, loss of distinction between cortex and medulla, osteosclerosis, and osteolytic areas. We recorded demographic data of the patients, the year of presentation, symptoms, complications at presentation and during follow-up, and serum alkaline phosphatase levels at presentation and during follow-up. We also analyzed radiological imaging data, including X-rays for all patients, computed tomography (CT) for nine patients, magnetic resonance imaging (MRI) for ten patients, and radionuclide bone scintigraphy for 23 patients.
The treatment received, the side-effects experienced, and response to treatment were also retrieved. Paget's disease of bone was considered active in case of increased levels of alkaline phosphatase (N: 40–125 U/L) or marked tracer uptake on bone scans. The biochemical remission was defined as reducing and maintaining serum total alkaline phosphatase concentrations within the reference range,[6] and clinical response was defined as the resolution of pagetic pain. Ethical approval for this study was obtained from the Scientific and Ethical Committees of hospitals where this study was conducted. Ethical approval for this study was obtained from the Scientific and Ethical Committees of hospitals where this study was conducted in February 2019.
RESULTS
The diagnosis of Paget's disease of bone was established in 122 patients (0.04%) among the 277,563 patients who presented to the rheumatology outpatient departments between 1994 and 2019. Of the 122 patients, 69 patients with complete data were included [Figure 1]. Among the 69 patients, 36 were female (52.2%). The mean age at diagnosis was 64.9 ± 11.6 years (35–87), with a range of 52 years. The mean diagnostic delay was 38 ± 55 months (1–192), with a range of 191 months.
Figure 1.
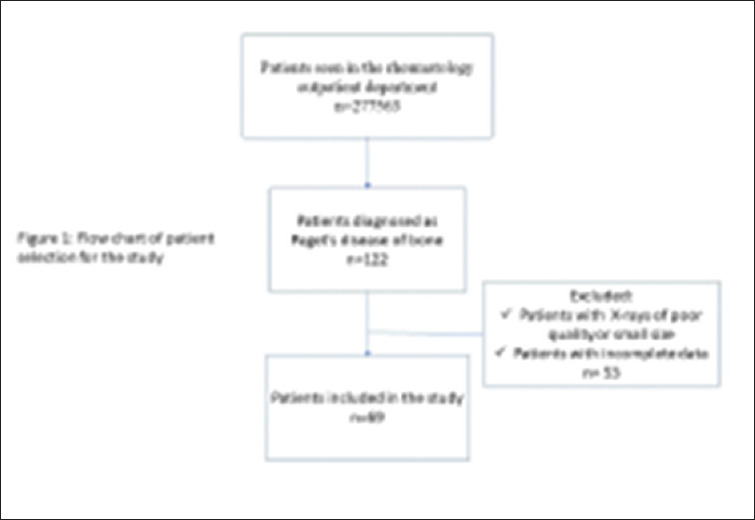
Flow chart of patient selection for the study
The mean follow-up period was 64.9 ± 55 months, ranging from 1 to 156 months. One patient had a family history of Paget's disease of bone. Eight patients had a history of malignancy: prostate adenocarcinoma (two patients), breast carcinoma (two patients), multiple myeloma (one patient), mediastinal tumor (one patient), gastric lymphoma (one patient), and colorectal cancer (one patient). Two patients had concomitant hyperparathyroidism. Seven patients were asymptomatic, and the disease was incidentally discovered on routine X-ray films (four patients) or elevated serum total alkaline phosphatase (three patients). Paget's disease of bone was diagnosed during the staging of known neoplasia in three patients with no Paget's disease of bone-related symptoms.
The mean diagnostic delay in symptomatic patients was 3 years, varying from 1 month to 16 years. The most common presenting symptoms were bone pain (88.7%), skeletal deformities (8%), pathological fractures (15.9%), hearing loss (4.8%), and headache (4.8%). Monostotic Paget's disease of bone was seen in 38 patients (55.1%). Regarding radiologic evaluation and bone scans, the most commonly involved bones included the pelvis, spine, and femur. The skeletal sites involved are cited in Table 1.
Table 1.
Skeletal sites involved in patients with Paget’s bone disease
| Number (%) | |
|---|---|
| Pelvis | 30 (43.5) |
| Spine | 15 (21.7) |
| Femur | 15 (21.7) |
| Skull | 14 (20.2) |
| Tibia | 4 (5.8) |
| Humerus | 3 (4.3) |
| Ribs | 3 (4.3) |
| Inferior maxillary bone | 2 (2.9) |
| Scapula | 2 (2.9) |
Mean serum alkaline phosphatase at the time of diagnosis was 591 U/L (68–8380), with no statistically significant difference in mean serum alkaline phosphatase values between men and women (768 U/L vs. 430 U/L, P = 0.219). Compared to those with monostotic involvement, patients with polyostotic involvement had higher alkaline phosphatase levels. However, this difference was not statistically significant (660 U/L vs. 540 U/L, P = 0.653). Alkaline phosphatase levels were higher in patients who reported bone pain; however, this difference did not reach statistical significance (635 U/L vs. 482 U/L, P = 0.658). Serum calcium and phosphate were normal except for one patient with coexistent hyperparathyroidism who had hypercalcemia (serum calcium 2.8 mmol/L).
Plain radiography showed osteolytic lesions (16.4%), coarsening of trabecular markings (30%), cortical thickening (17.9%), osseous expansion (67.16%), loss of corticomedullary differentiation (42%), increase in density (64.17%), and deformity (7.5%). Radionuclide bone scintigraphy was performed in 23 patients (33.3%); fifteen patients (65.2%) showed increased uptake in multiple sites suggestive of polyostotic disease.
Nineteen patients underwent CT scans. We identified the following features: cortical thickening (21%), expansion of bone (26.3%), loss of corticomedullary differentiation (26.3%), mixed lytic/sclerotic lesions (26.3%), disorganized structure (15.7%), and sclerotic lesions (31.5%). MRI was performed in ten patients (14.5%). Indications for MRI were neurological deficit (four cases) and suspicion of malignant transformation (six cases).
Complications occurred in 51 patients (73.19%) and were present at diagnosis in all cases. Forty patients had one complication. Nine patients had two complications, and two patients had three complications.
The most common complications were hearing loss (n = 18, 26%) and secondary osteoarthritis (n = 16, 23.1%). Other complications included fractures (n = 11, 15.9%), headache (n = 4, 5.8%), and hydrocephalus (n = 1, 1.4%). The fractures affected the femur (n = 6), lumbar vertebra (n = 2), thoracic vertebra (n = 1), humerus (n = 1), and tibia (n = 1). Osteoarthritis was located in the knees in four cases and the hips in 12 cases. No patient had high output cardiac failure or osteosarcoma, and during follow-up, we did not observe any additional complications.
Of the 69 patients, 47 (68.1%) received bisphosphonates and two patients received salmon calcitonin (2.8%). Indications for treatment (regardless of the drug used) were localization at risk of developing complications (74%), metabolically active disease (66.6%), and joint involvement (14.8%). After zoledronate perfusion, two patients reported flu-like symptoms and another patient developed hypophosphatemia and atrial fibrillation. In the other cases, bisphosphonates were well tolerated. Fifty-one patients (73.9%) had been followed up for an average of 55 months (2–240).
Bone pain improved in 43.1% of patients, and according to most recent blood tests, the serum alkaline phosphate level had normalized in 22 patients (43.1%), stabilized in 20 patients (39.2%), and worsened in nine patients (17.6%). Patients in clinical remission achieved biochemical remission as well, except for three patients (P< 0.001) who had a high level of alkaline phosphatase despite the resolution of bone pain. Patients who achieved biochemical remission were of younger age at diagnosis (59 years vs. 66.8 years, P = 0.018). Baseline alkaline phosphatase levels were not correlated with biochemical or clinical remission. Fifteen patients (30.6%) relapsed and required more than one course of treatment because of active disease.
Eleven patients needed to switch to a different agent. Of patients on zoledronate, 80% achieved clinical and biochemical remission. A second treatment course was needed in 22.2% of patients. Patients on pamidronate required more than one course of treatment in 44.4% of cases, and a switch to another agent was indicated for 66.6% of patients. Patients on calcitonin or etidronate had the worst outcomes and needed to switch to another agent in all cases. Table 2 summarizes therapeutic agents used and outcomes following treatment.
Table 2.
Therapeutic agents and treatment outcomes of patients with Paget’s bone disease
| Zoledronate | Risedronate | Pamidronate | Etidronate | Calcitonin | P | |
|---|---|---|---|---|---|---|
| Number of patients | 10 | 20 | 9 | 8 | 2 | - |
| Clinical remission (%) | 80 | 38.8 | 100 | 12.5 | 0% | 0.005 |
| Biochemical remission (%) | 80 | 38.8 | 62.5 | 12.5 | 0 | 0.009 |
| Retreatment (%) | 22.2 | 10 | 44.4 | 0 | 0% | 0.269 |
| Switch (%) | 0 | 35.3 | 66.6 | 100 | 100% | 0.111 |
DISCUSSION
To our knowledge, this case series is the largest reported thus far in North Africa, including 69 patients. Although the prevalence of Paget's disease of bone in Tunisia has yet to be determined by a national multicentric study, Paget's disease of bone was estimated to occur in 0.04% of patients who presented to the rheumatology outpatient department services of two Tunisian university hospitals. The mean age at diagnosis was about 63 years; however, two patients were under 40 years old. There was a female predominance. The majority of cases were monostotic, with the pelvis and the femur being the most commonly affected bones. Complications were frequent; however, malignant transformation was not identified in this series. In contrast to previous studies, only one patient had a positive family history, but the sample size was too small for this observation. Familial aggregation was observed in 26% in an Australian study,[7] 6.3% in a Japanese study,[8] and 0.3% in a recent Chinese study.[9] These findings suggest that genetic factors are important in the development of this disease. Mutations in the SQSTM1 gene were identified in sporadic and familial cases of Caucasian patients.[10]
It has also been hypothesized that environmental factors may play a role in the pathogenesis of Paget's disease of bone. Several pathogens have been implicated as triggers of this disease. Intranuclear inclusion bodies similar to paramyxovirus nucleocapsids were found in pagetic osteoclasts.[11] Based on this hypothesis, the decline in the prevalence of Paget's disease of bone could be related to the increase in vaccination coverage for canine distemper and measles virus.[1]
There are regional variations in the characteristics of Paget's disease of bone worldwide. Table 3 compares clinical and management features of Paget's disease of bone among various countries, based on data from systemic reviews and large studies.[8,9,12,13,14,15] While men were more affected in China[9] and the United Kingdom (UK),[13] this study noted a slight predominance of the female gender. Female preponderance was also reported in Japanese[8] and Brazilian[16] studies. The mean age of Tunisian patients was 64.9 years, similar to Japanese patients[8] and patients from the United States.[14] Notably, two patients were under 40 years (35 and 39 years old). In this regard, 5.7% of the patients were diagnosed before 40 years of age in a Spanish study.[17] It has been suggested that Paget's disease of bone starts in youth but is not diagnosed until later.
Table 3.
Comparison of clinical and management features of Paget’s disease of bone among various countries
| Nb of patient | Age | Gender (M/F) | Family history (%) | Monostotic/Polyostotic (%) | Affected bones (%) | Symptoms (%) | Treatment (%) | |
|---|---|---|---|---|---|---|---|---|
| China[9] | 332 | 55 | 1.46/1 | 0.3 | 54.4/45.6 | Skull (31.2)*, femur (26.2)*, pelvis (15)* | Bone pain (63.5), deformity (51.5), hearing loss (12.6) | Calcitonin (28.1), pamidronate (21.5), zoledronate (18.2) |
| Japan[8] | 169 | 64.7 | 0.86/1 | 6.3 | 51.5/48.5 | Pelvis (55), spine (32), femur (27) | Bone pain (64.4), deformity (18.9), hearing loss (6.3) | Calcitonin (62.1), etidronate (14.8), alendronate (8.9) |
| India[12] | 48 | 60 | 1.82/1 | 4.1 | 13/87 | Pelvis (73.3), spine (62.2), skull (31.1) | Back pain (56), bone pain (44.4), hearing loss (13.3) | Zoledronate (60), alendronate (35.4), risedronate (4.2) |
| UK[13] | 2465 | 75 | 1.04/1 | NR | NR | Pelvis (47.5), femur (25.8), tibia/fibula (21.7) | Bone pain (66.7), deformity (9.2), swelling (9.2) | Bisphosphonate (26.9), calcitonin (7.3) |
| USA[14] | 236 | 69.6 | 1/2.57 | NR | 28/72 | Pelvis (67), spine (41), femur (31) | Bone pain (70.9), deformity (23.1), fracture (4.5) | NR |
| Australia[15] | 531 | 65 | 1.13/1 | NR | 39/61 | Pelvis (65), spine (38), femur (38) | NR | Pamidronate (34), alendronate (30), risedronate (19) |
| Tunisia (our study) | 69 | 64.9 | 0.91/1 | 1.4 | 55.1/44.9 | Pelvis (43.5), femur (21.7), spine (21.7). | Bone pain (88.7), deformity (8), fracture (15.9) | Risedronate (40.8), zoledronate (20.4), pamidronate (18.3) |
NR: No record, M: Male, F; Female. *Data available for monostotic involvement
The distribution of affected bones was also different among various countries. The pelvis was reported to be the most commonly affected bone in this series, a finding replicated in previous studies in the United States,[14] the United Kingdom,[13] and Japan.[8] In this study, only seven patients (10.1%) were asymptomatic, whereas the literature claims that approximately half of the cases present no symptoms and are incidentally diagnosed.[18] These statistics suggest that currently, more patients are routinely screened. Furthermore, among symptomatic patients, the prevalence of bone pain, a typical presenting symptom, ranges between 40% and 70%, but in this study, the prevalence of bone pain was higher than 88%.
Complications may also be a presenting symptom. For instance, the frequency of fracture as a presenting feature varies widely between different regions: from 3% in Brazil[16] to 27% in India.[19] In this study, fracture was the presenting symptom in 15.9% of patients.
Osteosarcoma is a life-threatening but rare complication. It affects 1% of patients with Paget's disease of bone.[20]
This complication was not noted in our series. However, a history of malignancy was reported in eight patients (11.6%). Pagetic bone can be hard to differentiate from metastases,[21] especially since Paget's disease of bone and osseous metastases often coexist.[22] This possibility must be considered to avoid mistaken diagnosis and ensure the correct staging and treatment of patients. The patients in this study demonstrated typical imaging findings: osteolytic areas, cortical thickening, loss of distinction between cortex and medulla, trabecular thickening, osteosclerosis, bone expansion, and bone deformity. The combination of these patterns is highly suggestive of Paget's disease of bone. To assess the extent of disease, patients underwent radionuclide bone scintigraphy, revealing polyostotic involvement in 44.9% of them. This test is also useful to monitor disease activity and treatment response.
High bone turnover is also characteristic of Paget's disease of bone; therefore, treatment options often target osteoclasts. In this series, the main indications for treatment were active disease (high alkaline phosphatase levels) and localization at risk of complications. Calcitonin was the first antiresorptive agent to be used to treat Paget's disease of bone.
While calcitonin has been shown to reduce biochemical markers of bone turnover and produce radiological improvement, complete control of the disease activity is rarely achieved, and relapses are frequent after treatment discontinuation.[23] Calcitonin was the most commonly used specific drug in Japanese[8] and Chinese studies.[9] In this series, two patients received calcitonin and both reported aggravation of symptoms with higher alkaline phosphatase levels following treatment. Given its moderate efficacy, the use of calcitonin is mainly reserved for patients with contraindications to bisphosphonates.
Bisphosphonates are currently the most used antiresorptive agents and include alendronate, risedronate, pamidronate, etidronate, ibandronate, and zoledronic acid. They are effective in reducing bone turnover and bone pain, and they promote the healing of osteolytic lesions.[24] However, their efficacy to prevent complications of Paget's disease of bone is still debated. Bisphosphonates have a long residual half-life. Thus, their effects on bone may persist after therapy cessation for months or even years. Nonetheless, some patients may require more than one course of treatment.
In this series, 30.6% of patients needed more than one course of treatment, whereas Walsh et al. reported a higher frequency (57%).[15] This difference could be related to more severe disease in the latter study. Oral and parenteral bisphosphonates were both highly successful in controlling symptoms and reducing alkaline phosphatase levels. However, intravenous zoledronate is considered to be the most potent bisphosphonate in clinical use,[25] as seen in this study.
In addition to their well-proven effectiveness, bisphosphonates have a good safety profile. The most common adverse effects are esophageal irritation and upper gastrointestinal discomfort, mainly with oral bisphosphonates. One of the striking observations in this study was the occurrence of hypophosphatemia after zoledronic acid perfusion. This adverse event was previously reported following IV zoledronic acid administration for hypercalcemia of malignancy[26] and osteoporosis.[27] Another adverse event was the occurrence of atrial fibrillation, which is supported by prior studies that have reported an association between bisphosphonates and atrial fibrillation/flutter.[28]
Treatment regimens continue to improve with the use of newer therapeutic approaches such as RANK-ligand (RANKL) inhibitor. Denosumab was proven to be partially successful in controlling pain in Paget's disease of bone, but it failed to achieve sustained remission.[29] Besides its high cost, repeated injections are needed and may limit its prescription. However, denosumab should be considered to treat unresectable giant cell tumors complicating Paget's disease of bone since it can reduce the tumor size.[30]
Several limitations should be noted, including the retrospective nature of the study, which resulted in specific information not being systemically available. Moreover, many patients were lost to follow-up, and the follow-up period was variable.
In addition, there was significant heterogeneity in diagnostic and therapeutic measures.
In summary, Paget's disease of bone does occur in the Tunisian population, although its prevalence has yet to be determined by a national multicentric study.
Although Paget's disease of bone is a benign bone disorder, complications are common.
Available treatments have not demonstrated a benefit in reversing complications; thus, we highlight the importance of an early and proper diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Poór G, Donáth J, Fornet B, Cooper C. Epidemiology of Paget's disease in Europe: The prevalence is decreasing. J Bone Miner Res Off J Am Soc Bone Miner Res. 2006;21:1545–9. doi: 10.1359/jbmr.060704. [DOI] [PubMed] [Google Scholar]
- 2.Sofaer JA, Holloway SM, Emery AE. A family study of Paget's disease of bone. J Epidemiol Community Health. 1983;37:226–31. doi: 10.1136/jech.37.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corral-Gudino L, Borao-Cengotita-Bengoa M, Del Pino-Montes J, Ralston S. Epidemiology of Paget's disease of bone: A systematic review and meta-analysis of secular changes. Bone. 2013;55:347–52. doi: 10.1016/j.bone.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 4.Nebot Valenzuela E, Pietschmann P. Epidemiology and pathology of Paget's disease of bone – A review. Wien Med Wochenschr. 2017;167:2–8. doi: 10.1007/s10354-016-0496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magen H, Liel Y, Bearman JE, Lowenthal MN. Demographic aspects of Paget's disease of bone in the Negev of southern Israel. Calcif Tissue Int. 1994;55:353–5. doi: 10.1007/BF00299314. [DOI] [PubMed] [Google Scholar]
- 6.Tan A, Goodman K, Walker A, Hudson J, MacLennan GS, Selby PL, et al. Long-term randomized trial of intensive versus symptomatic management in paget's disease of bone: The PRISM-EZ Study. J Bone Miner Res. 2017;32:1165–73. doi: 10.1002/jbmr.3066. [DOI] [PubMed] [Google Scholar]
- 7.Britton C, Brown S, Ward L, Rea SL, Ratajczak T, Walsh JP. The changing presentation of paget's disease of bone in Australia, a high prevalence region. Calcif Tissue Int. 2017;101:564–9. doi: 10.1007/s00223-017-0312-1. [DOI] [PubMed] [Google Scholar]
- 8.Hashimoto J, Ohno I, Nakatsuka K, Yoshimura N, Takata S, Zamma M, et al. Japanese committee on clinical guidelines of diagnosis and treatment of paget's disease of bone of the Japan osteoporosis society. Prevalence and clinical features of Paget's disease of bone in Japan. J Bone Miner Metab. 2006;24:186–90. doi: 10.1007/s00774-005-0670-z. [DOI] [PubMed] [Google Scholar]
- 9.Wang Q-Y, Fu S-J, Ding N, Liu S-Y, Chen R, Wen Z-X, et al. Clinical features, diagnosis and treatment of Paget's disease of bone in mainland China: A systematic review. Rev Endocr Metab Disord. 2020 doi: 10.1007/s11154-020-09544-x. doi: 101007/s11154-020-09544-x. [DOI] [PubMed] [Google Scholar]
- 10.Hocking LJ, Lucas GJA, Daroszewska A, Mangion J, Olavesen M, Cundy T, et al. Domain-specific mutations in sequestosome 1 (SQSTM1) cause familial and sporadic Paget's disease. Hum Mol Genet. 2002;11:2735–9. doi: 10.1093/hmg/11.22.2735. [DOI] [PubMed] [Google Scholar]
- 11.Singer FR. Paget's disease of bone-genetic and environmental factors. Nat Rev Endocrinol. 2015;11:662–71. doi: 10.1038/nrendo.2015.138. [DOI] [PubMed] [Google Scholar]
- 12.Cherian KE, Kapoor N, Shetty S, Jebasingh FK, Asha HS, Hephzibah J, et al. Paget's disease of bone: An entity still exists in India. Indian J Endocrinol Metab. 2018;22:368–72. doi: 10.4103/ijem.IJEM_19_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Staa TP, Selby P, Leufkens HGM, Lyles K, Sprafka JM, Cooper C. Incidence and natural history of Paget's disease of bone in England and Wales. J Bone Miner Res Off J Am Soc Bone Miner Res. 2002;17:465–71. doi: 10.1359/jbmr.2002.17.3.465. [DOI] [PubMed] [Google Scholar]
- 14.Wermers RA, Tiegs RD, Atkinson EJ, Achenbach SJ, Melton LJ. Morbidity and mortality associated with Paget's disease of bone: A population-based study. J Bone Miner Res Off J Am Soc Bone Miner Res. 2008;23:819–25. doi: 10.1359/JBMR.080215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh JP, Attewell R, Stuckey BGA, Hooper MJ, Wark JD, Fletcher S, et al. Treatment of Paget's disease of bone: A survey of clinical practice in Australia. Bone. 2008;42:1219–25. doi: 10.1016/j.bone.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 16.Werner de Castro GR, Heiden GI, Zimmermann AF, Morato EF, Neves FS, Toscano MA, et al. Paget's disease of bone: Analysis of 134 cases from an island in Southern Brazil: Another cluster of Paget's disease of bone in South America. Rheumatol Int. 2012;32:627–31. doi: 10.1007/s00296-010-1648-2. [DOI] [PubMed] [Google Scholar]
- 17.Holgado S, Rotés D, Gumà M, Monfort J, Olivé A, Carbonell J, et al. Paget's disease of bone in early adult life. Ann Rheum Dis. 2005;64:306–8. doi: 10.1136/ard.2004.021139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan A, Ralston SH. Clinical presentation of Paget's disease: Evaluation of a contemporary cohort and systematic review. Calcif Tissue Int. 2014;95:385–92. doi: 10.1007/s00223-014-9904-1. [DOI] [PubMed] [Google Scholar]
- 19.Anjali, Thomas N, Rajaratnam S, Shanthly N, Oommen R, Seshadri MS. Paget's disease of bone: Experience from a centre in southern India. J Assoc Physicians India. 2006;54:525–9. [PubMed] [Google Scholar]
- 20.Singer FR, Bone HG, Hosking DJ, Lyles KW, Murad MH, Reid IR, et al. Endocrine Society.Paget's disease of bone: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:4408–22. doi: 10.1210/jc.2014-2910. [DOI] [PubMed] [Google Scholar]
- 21.Sá Pinto A, Alves VM, Oliveira A, Castro RH, Pereira JG. Incidental finding of a monostotic form of Paget Disease of the scapula in a lung cancer patient. Radiogr Lond Engl. 1995;2017(23):e72–4. doi: 10.1016/j.radi.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Sonoda LI, Balan KK. Co-existent paget's disease of the bone, prostate carcinoma skeletal metastases and fracture on skeletal scintigraphy-lessons to be learned. Mol Imaging Radionucl Ther. 2013;22:63–5. doi: 10.4274/Mirt.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martint TJ, Jerums G, Melick RA, Xipell JM, Arnott R. Clinical, biochemical and histological observations on the effect of porcine calcitonin in paget's disease of bone*. Aust N Z J Med. 1977;7:36–43. doi: 10.1111/j.1445-5994.1977.tb03354.x. [DOI] [PubMed] [Google Scholar]
- 24.Gennari L, Rendina D, Picchioni T, Bianciardi S, Materozzi M, Nuti R, et al. Paget's disease of bone: An update on epidemiology, pathogenesis and pharmacotherapy. Expert Opin Orphan Drugs. 2018;6:485–96. [Google Scholar]
- 25.Reid IR, Miller P, Lyles K, Fraser W, Brown JP, Saidi Y, et al. Comparison of a single infusion of zoledronic acid with risedronate for Paget's disease. N Engl J Med. 2005;353:898–908. doi: 10.1056/NEJMoa044241. [DOI] [PubMed] [Google Scholar]
- 26.Clark SL, Nystrom EM. A case of severe, prolonged, refractory hypophosphatemia after zoledronic acid administration. J Pharm Pract. 2016;29:172–6. doi: 10.1177/0897190015624050. [DOI] [PubMed] [Google Scholar]
- 27.Chiam P, Chandran M. Profound and protracted hypophosphatemia after a single dose of zoledronic acid infusion for osteoporosis associated with normocalcemic primary hyperparathyroidism. Med Case Rep. 2017;3:3. [Google Scholar]
- 28.Loke YK, Jeevanantham V, Singh S. Bisphosphonates and atrial fibrillation: Systematic review and meta-analysis. Drug Saf. 2009;32:219–28. doi: 10.2165/00002018-200932030-00004. [DOI] [PubMed] [Google Scholar]
- 29.Reid IR, Sharma S, Kalluru R, Eagleton C. Treatment of paget's disease of bone with denosumab: Case report and literature review. Calcif Tissue Int. 2016;99:322–5. doi: 10.1007/s00223-016-0150-6. [DOI] [PubMed] [Google Scholar]
- 30.Ralston SH, Corral-Gudino L, Cooper C, Francis RM, Fraser WD, Gennari L, et al. Diagnosis and management of paget's disease of bone in adults: A clinical guideline. J Bone Miner Res Off J Am Soc Bone Miner Res. 2019;34:579–604. doi: 10.1002/jbmr.3657. [DOI] [PMC free article] [PubMed] [Google Scholar]


