Sir,
Mucous membrane pemphigoid (MMP) is a rare autoimmune disease characterized by subepithelial blisters of mucosal and, seldom, of cutaneous surfaces.[1] MMP lesions usually result in scars affecting oral or ocular mucosae; laryngeal MMP is rare (estimated prevalence of 1/10,000,000 people) but it could become severe enough to require emergency tracheostomy.[2] We observed a unique case of a laryngeal MMP in a patient who was treated with chemoradiotherapy (CT-RT) for an advanced-stage laryngeal carcinoma six years earlier. He began complaining of new-onset odynophagia, so he underwent several biopsies in the operating room in order to exclude a recurrence. Multiple areas of blisters, erosions, and pseudomembranes on the epiglottis and aryepiglottic folds were observed [Figure 1a-d] but final histopathology was suggestive of pemphigoid; therefore, he was referred for a dermatology consultation. Cutaneous examination showed just one erythematous-crusty and itchy lesion on the scalp, in the absence of oral, ocular, or genital mucosal involvement [Figure 2]. Lesional and perilesional tissue biopsies were performed for histology and direct immunofluorescence (DIF) respectively. A sample of blood was taken for indirect immunofluorescence (IIF) and ELISA test and all the results confirmed the diagnosis of MMP because of the positivity of antibodies to only BP-180, with a peculiar low titer. Histology showed a subepidermal blistering with eosinophilic dermal infiltrate [Figure 3a-c] and DIF demonstrated linear deposits of IgG and C3 along the dermal–epidermal junction [Figure 3d]. IIF on monkey esophagus sample revealed the presence of autoantibodies IgG against the basement-membrane antigens and ELISA test confirmed the presence of autoantibodies against only BP-180 at a titer of 23.3 U/ml (normal value < 9 U/ml). Antibodies against BP-230 were negative. The patient was treated with systemic prednisone at a dose of 0.5 mg/kg per day for 3 months and then a maintenance oral dose of 5 mg every other day. Ultimately, he had complete resolution of symptoms without mucosal or cutaneous scars after several months.
Figure 1.
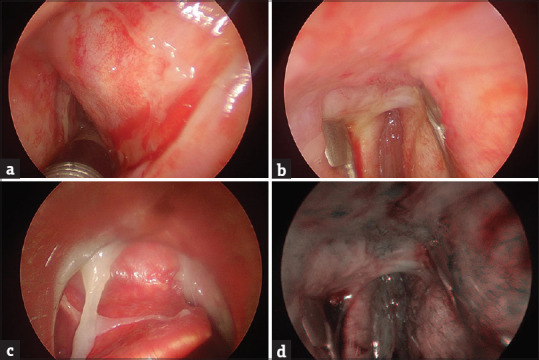
(a) A large portion of mucosa sloughing off in the epiglottic vallecula; (b) a magnified view of mucosal peeling in the anterior commissure region; (c) an endoscopic view of a large erythematous lesion involving the right vestibular fold; (d) view of mucosal peeling in the anterior commissure region with polarized light NBI to visualize the blood vessels
Figure 2.
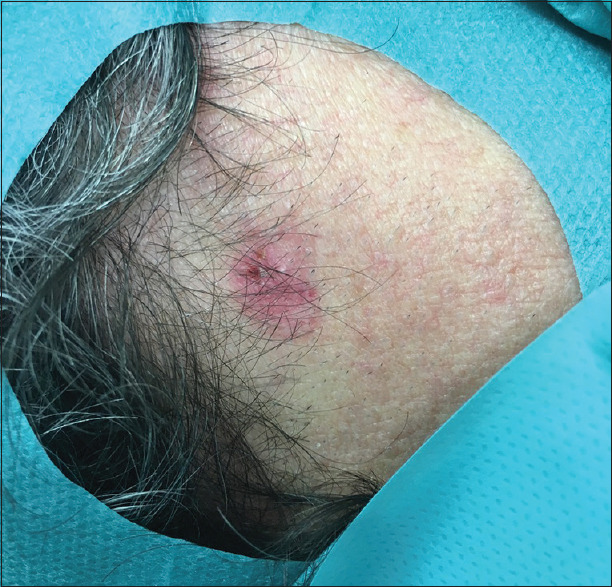
Cutaneous involvement - an erythematous-crusty lesion of the scalp
Figure 3.
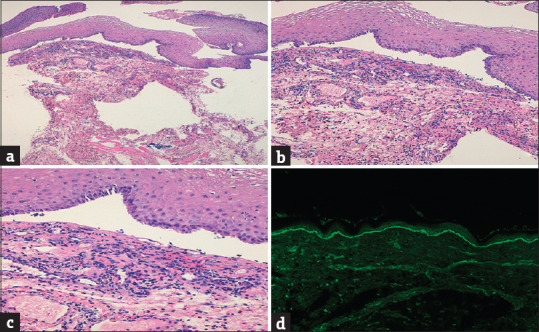
Histopathology of the cutaneous lesion showing subepidermal blistering and eosinophilic dermal infiltrate [H and E, (a) ×50; (b) ×100; (c) ×200]; (d) linear deposit of IgG and C3 along the dermal–epidermal junction at DIF on perilesion skin (×20)
The diagnosis of MMP is clinical but it must be confirmed by the demonstration of IgG and C3 linear deposits on the basement membrane on DIF and identification of subepithelial blistering on histology.[3] IIF shows in only 50% of cases the circulating antibodies (usually against BP-180 or, more rarely, BP-230, α6β4 integrin, and laminin-332) which have typically a low titer and their characterization may be performed by ELISA or immunoblotting.[4] Our case is very intriguing because of the temporal relationship of laryngeal MMP with previous RT exposure. In the literature, RT has been reported to be a trigger factor for localized bullous pemphigoid but not, to the best of our knowledge, for MMP. It can be assumed that RT alters epithelial biology thus exposing the antigens of the basement membrane that in turn can activate an autoimmune reaction.[5] Of course, more cases and further basic and clinical research are needed to confirm this hypothesis. However, the possibility of an autoimmune bullous disease must be taken into consideration in a patient who had undergone RT especially when new symptoms develop after long time.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Benoit S, Scheurlen M, Goebeler M, Stoevesandt J. Structured diagnostic approach and risk assessment in mucous membrane pemphigoid with oesophageal involvement. Acta Derm Venereol. 2018;98:660–6. doi: 10.2340/00015555-2938. [DOI] [PubMed] [Google Scholar]
- 2.Higgins TS, Cohen JC, Sinacori JT. Laryngeal mucous membrane pemphigoid: A systematic review and pooled-data analysis. Laryngoscope. 2010;120:529–36. doi: 10.1002/lary.20763. [DOI] [PubMed] [Google Scholar]
- 3.Lazarova Z, Sitaru C, Zillikens D, Yancey KB. Comparative analysis of methods for detection of anti-laminin 5 autoantibodies in patients with anti-epiligrin cicatricial pemphigoid. J Am Acad Dermatol. 2004;51:886–92. doi: 10.1016/j.jaad.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Jindal A, Rao R, Bhogal BS. Advanced diagnostic techniques in autoimmune bullous diseases. Indian J Dermatol. 2017;62:268–78. doi: 10.4103/ijd.IJD_196_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Low GJ, Keeling JH. Ionizing radiation-induced pemphigus: Case presentations and literature review. Arch Dermatol. 1990;126:1319–23. [PubMed] [Google Scholar]


