Abstract
Background/Aims
Previous publications confirmed that after internal urethrotomy success rates in the short-term (less than 6 months) are varied (70-80%) and in the long-term results are generally low. In this study, the efficacy of triamcinolone instillation based on a newly introduced protocol on the rate of recurrence in patients with anterior urethral strictures was evaluated.
Methods
A total of 66 patients were divided into treatment group (n = 33), in which triamcinolone was instilled on urethra after removing of Foley catheter and control group (n = 33) that not received any intervention. Each 40 mg/1 ml of triamcinolone vial was dissolved in 9 ml of distilled water and then a 2 ml of diluted solution was used for each instillation and 8 ml was kept in 4°C. Triamcinolone was instilled based on daily in week 1, every other day for week 2 and then every Monday and Friday for 2 months. Penile clamp was used after instillation for 1 hour. Treatment failure was based on urine flow rate, rate of recurrence and time to appearance of recurrence.
Results
There were not any significant differences regrading to age (p = 0.09), length (p = 0.41) and diameter (p = 0.36) of stricture between 2 groups. Time to appearance of recurrence showed significantly in the treatment group when compared with that in the control group (1,350 ± 900 vs. 124.3 ±112 days; p < 0.01). In the treatment group, 88% had reasonable consequence, while in control 48%. There were 3 patients with a mean length-diameter of stricture around 0.3-5 cm who showed recurrence free with the mean of 720 days after intervention.
Conclusion
Administration of triamcinolone instillation in urethra is associated with a decreased risk of stricture recurrence. Superior outcomes were seen in patients with a stricture length of more than 2 cm and this may in part reflect the increasing efficacy of the instillation method in the management of urethral strictures. These findings help identify patients with aggressive features of strictures in urethra who may benefit from intensified treatment efficacy of triamcinolone instillation.
Key Words: Efficacy, Triamcinolone, Instillation, Recurrence, Urethrotomy, Stricture
Introduction
Narrowing of the urethral lumen that is surrounded by the corpus spongiosum called urethral strictures. Male urethral stricture diseases have always been common [1,2] as the ancient Egyptians treated stricture disease 4,000 years ago [3]. Most patients present with a range of signs such as obstructive lower urinary tract symptoms. In addition, abundant sequelae such as bladder calculi, recurrent infection, fistula, and chronic renal deficiency can be resulted from untreated urethral stricture disease and significantly affect the quality of patients' life. Treatment failure rates were reported significantly as 32% for anterior urethroplasty and 21% for posterior urethroplasty, at a mean follow-up of < 3 years [1,2,3]. Amount of damage to the corpus spongisum could define the severity of damage, in which could develop to spongiofirosis. Fibrosis of the epithelial-lined cavernous tissue could cause consistency of corpus spongiosum with scar formation. Spongiofibrosis is exacerbated by tears and fissures of the metaplastic epithelium, allowing urine to leak into the underlying corpus spongiosum [4,5]. There is no definite consensus on the best study for evaluation of urethral strictures [6]. Location of the obstruction, length of the obstruction, and associated urethral pathology were mentioned as 3 key points for treatment strategy. Management of urethral strictures included catheterization, dilation, endoscopic internal urethrotomy, and urethroplasty [7,8,9]. Regarding to internal urethrotomy, it has the benefits of easiness, straightforwardness, rapidity, and short period of recovery. However, success rates vary and long-term results are generally low. In the short-term (< 6 months), success rates are 70-80%. After 1 year, recurrence rates approach 50-60% and by 5 years, the rates fall significantly and reach to 74-86% [8,10]. As the formation of scar in urethra is a result of the migration of collagens and extracellular matrix [11], and triamcinolone is one of the most important drugs for prevention of recurrence, therefore this study aimed to investigate the efficacy of antifibroblast and anticollagen triamcinolone instillation after internal urethrotomy in the long-term rate of recurrence in patients with urethral strictures.
Materials and Methods
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments. The study was approved by the ethics committee of the Isfahan University of Medical Sciences by the Code No. 396454. This cross-section clinical study was conducted in the urology ward of Alzahra Hospital and kidney transplantation research center. This study included 66 patients, those admitted to hospital and underwent internal urethrotomy (n = 63 + 3). The indication for internal urethrotomy was determined by an experienced urologist, and the decision for urethrotomy was based on retrograde urethrography for each individual, and guidelines and reference sources for urology. The length of the strictures was around 2 cm in 60 and 5 cm in 3 subjects. They did not receive any medical management previously. Exclusion criteria were those who did not have any of inclusion criteria, those not co-operated or those who might have an allergic reaction to triamcinolone. There were 2 groups; treatment (instillated triamcinolone according to a newly introduced protocol) and control group (not received any intervention). The patients in both groups were matched for age, length and diameter of stricture in most cases. The strictures characteristics, including length, diameter and outcome, including rate of recurrence and time to appearance of recurrence were recorded. In all control (n = 33) and treatment groups (n = 30 + 3), internal urethrotomy were performed with Wolf Urethrotom® instrument. In the treatment group, triamcinolone was instilled on urethra after removing of the silicone Foley catheter.
The criteria for triamcinolone dose selection were based on previous publications [12,13,14,15] and time for instillation was based on the protocol associated with previous experience of senior surgeon [12,14,15]. Each 40 mg/1 ml of triamcinolone vial was dissolved in 9 ml of distilled water. The obtained solution was used for 5 instillation occasions based on protocol. On the day of the visit by the senior surgeon, a 2 ml of diluted solution instilled into the urethra, based on daily in week 1, every other day for week 2 and then every Monday and Friday for 2 months. Penile clamp was used after instillation of triamcinolone dilution into the urethra for 1 hour [12]. Planned time for follow-up after being off treatment was, at least for 6 months after internal urethrotomy.
The association of triamcinolone instillation with clinical outcomes were analyzed in the IBM SPSS software version 20.0 (IBM Corp., Armonk, NY, USA). Kolmogorov-Smirnov test, independent t-test and Chi-square tests were used to define variables that affected outcome such as a recurrence. All p < 0.05 were considered as indicating a statistically significant difference.
Results
Patient characteristics of the analytic cohorts are presented in Table 1. One-sample Kolmogorov-Smirnov test confirmed normal distribution of age in the population studied (p = 0.10). With a minimum of 19 and a maximum of 81, the mean ± SD of age was 46.6 ± 17.4 years. There was not any significant difference between age in the treatment group versus the control group (43.6 ± 16.3 vs. 50.2 ± 18.0; p = 0.09, independent t-test) respectively.
Table 1.
Demographic and clinical variables in treatment and control group
| Treatment |
Control |
p | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Max | Mean | SD | Min | Max | Mean | SD | ||
| Age, years | 19 | 81 | 43 | 16.3 | 21 | 82 | 50.2 | 18 | 0.09 |
| Length, cm | 0.5 | 2 (5: n = 3) | 1.9 | 1.3 | 8 | 2 | 1.7 | 0.3 | 0.4 |
| Diameter, cm | 0.1 | 0.7 | 0.3 | 0.16 | 0.1 | 0.8 | 0.35 | 0.17 | 0.36 |
| Time to recurrence, days | 360 | 2,520 | 1,350 | 900 | 30 | 425 | 124.3 | 112 | 0.00 |
| Rate of recurrence, % | 12% | 48% | 0.03 | ||||||
Cause of stricture: traumatic (n = 34), inflammation (n = 13), idiopathic (n = 19).
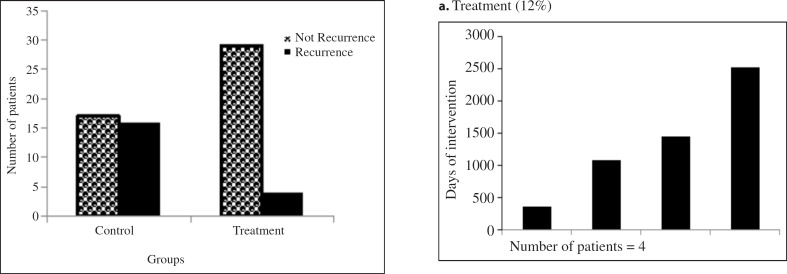
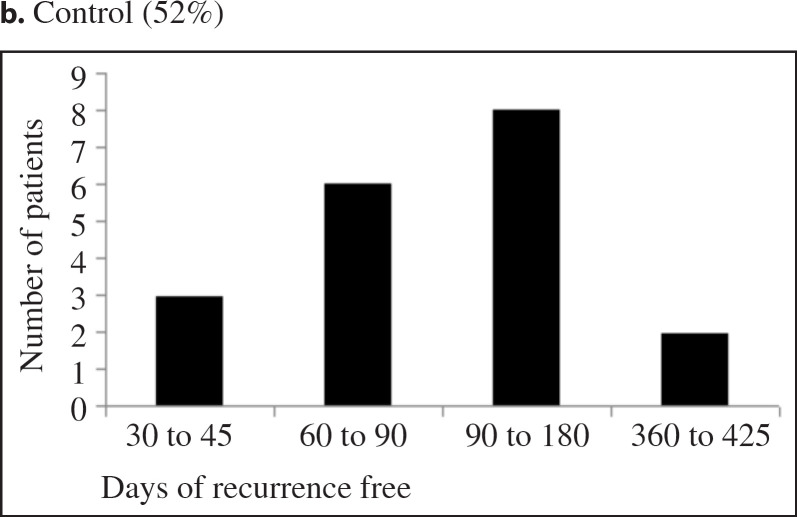
Length of strictures did not follow a normal distribution (p = 0.00). The mean ± SD length of strictures in the treatment group versus control group were 1.9 ± 1.3 versus 1.7 ± 0.3 cm. There was not any significant difference (p = 0.41) between the length of strictures in both control and treatment group. Distribution of data associated to the diameter of strictures followed non-normal pattern (p = 0.02). The mean ± SD diameter of strictures in the treatment group versus the control group were 0.7 ± 0.2 versus 0.35 ± 0.17 cm, that was not significant (p = 0.36). The cause for urethral strictures in the treatment group versus the control group, were traumatic (18 vs. 16; 51%), inflammation (6 vs. 7; 20%) and idiopathic (9 vs. 10; 29%) correspondingly. In treatment group 29 patients (88%) showed no evidence of recurrence whereas in control group 17 patients (52%). Figure 1 shows a comparison of recurrence in treatment and control group. There was not any significant difference in the mean ± SD length of strictures (cm) in population showed recurrence versus those not (1.7 ± 0.3 vs. 1.9 ± 1.1; p = 0.9). In addition, associated to the diameter of strictures there was not significant differences (p = 0.4) in the mean ± SD diameter of strictures (cm), and in population showed recurrence versus those not showed recurrence (0.4 ± 0.14 vs. 0.3 ± 0.2; p = 0.4). Figure 2 shows that there was significant difference (p = 0.00), between the mean ± SD time to recurrence (days after intervention) in the treatment group (1,350 ± 900 days; Fig. 2a) versus control group (124.3 ±112 days; Fig. 2b) correspondingly. In 3 patients with a mean age of 38.3, the mean length-diameter of the stricture was 0.3-5 cm respectively. There were all recurrences free (mean of 720 days) after instillation of triamcinolone. The cause of stricture in 1 patient was inflammation and in 2 cases was idiopathic. There was not any difference in the recurrence associated with the cause of stricture.
Fig. 1.
Comparison of recurrence within 2 groups (treatment and control).
Fig. 2.
Recurrence presented within 2 groups. a treatment; b control.
Discussion
In this study, we demonstrate results of triamcinolone instillation into the stricture's urethra. After internal urethrotomy which performed by same Senior Surgeon Professor Hamid Mazdak and removing of silicone foley catheter, triamcinolone instillation based on protocol showed no evidence of stricture recurrence in treatment 4 (12%) versus control group 17 (48%), respectively. There were lower rate of recurrence and shorter time to appear recurrence in the treatment group when compared to control group (p ≤ 0.01). This is in agreement with previous publication that confirmed injection of triamcinolone significantly reduced stricture recurrence after internal urethrotomy [12].
The stricture is a tightening of the urethraowing to wound tissue, which indicates to disruptive voiding dysfunction with severe consequences for the entire urinary tract. The main signs of urethral stricture are those of blocked and aggravated micturition, with augmented urination time and a feeling of inadequate bladder discharging, jointly with increased micturition frequency and urgency [9].
As there is no standardized treatment algorithm for urethral strictures and management modality often descents to urologist preference [12,14,15,16], our findings demonstrate lower rate of recurrence in urethral stricture of those triamcinolone instilled. This is in agreement with previous publication that confirmed injection of triamcinolone significantly reduced stricture recurrence after internal urethrotomy [12]. In another study, injection of corticosteroid after internal urethrotomy, showed a significant decrease in time to recurrence in the experimental group versus the control group (8.08 ± 5.55 vs. 3.6 ± 1.59 months) (p < 0.05) [17]. Study associated with the use of triamcinolone ointment for clean intermittent self catheterization in the prevention of urethral stricture recurrence after internal urethrotomy showed a 22.2% recurrence rate in the patients of the triamcinolone group against 46.4% in those of the control group after the first internal urethrotomy (p = 0.04) [18].
Submucosal injection of mitomycin C showed a significant reduction in stricture recurrence after internal urethrotomy [14]. The therapeutic impact of instillation method into the urethra is consistent with a recent study of platelet-rich plasma injection, which confirmed a decrease at the rate of stricture recurrence in about a year after the intervention [19].
Internal urethrotomy that is recommended for the treatment of urethral strictures shorter than 1.5 cm, has been associated with high recurrence rates. It is well known that epithelial healing could not be provided completely by internal urethrotomy, as the exact pathology associated with healing process remains unclear and wound contraction narrows the lumen before completion of epithelialization [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. For that reason any drug or procedure that can delay wound contraction may thus decrease the likelihood of stricture procedure.
In our study triamcinolone instillation caused delay in the stricture course, by stopping imitation of fibroblasts and inhibiting collagen synthesis. This is the first prospective clinical study that evaluated triamcinolone instillation into the anterior urethra due to a stricture, after internal urethrotomy based on the newly introduced protocol. This protocol significantly decreased the stricture characteristics by influencing on time to recurrence. The mean ± SD length of the stricture was 1.9 ± 1.3 cm, in which after triamcinolone instillation urine flow increased to 12-15 ml/s. The best urine flow was obtained from 3 patients (aged 31, 24 and 60 years) that were not suitable candidates for internal urethrtomy due to a stricture length of around 5 cm. After instillation of triamcinolone based on protocol, they showed recurrence after 360, 720 and 1,080 days after the intervention.
Finally, the number of patients that studied is small for claiming a strong decision concerning the extended period success rate following internal urethrotomy and instillation triamcinolone based on the newly introduced protocol. In this study, instillation of triamcinolone due to efficacy, ease of application and safety could be recommended as a guideline of treatment option after internal urethrotomy or in those with stricture length of around 5 cm that could not get the criteria for internal urethrotomy.
Conclusion
According to the available data, this study considered the efficacy of triamcinolone instillation into the anterior urethra after internal urethrotomy for up to 2 months based on a newly introduced protocol, and found it significantly reduced rate of recurrence. In addition, 3 patients who were not good candidates for internal urethrotomy due to stricture length of about 5 cm, instillation of triamcinolone significantly improved urine flow. In view of its efficacy, ease of application, and safety, the newly introduced protocol could be used following internal urethrotomy or without urethrotomy in those with long strictures of around 5 cm. Further studies are necessary to authorize its effectiveness and safety in this context.
References
- 1.Benson CR, Goldfarb R, Kirk P, Qin Y, Borza T, Skolarus TA, Brandes S. Population analysis of male urethral stricture management and urethroplasty success in the United States. Urology. 2019;123:258–264. doi: 10.1016/j.urology.2018.06.059. [DOI] [PubMed] [Google Scholar]
- 2.Smith TG., 3rd Current management of urethral stricture disease. Indian J Urol. 2016;32:27–33. doi: 10.4103/0970-1591.173108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mundy AR. Management of urethral strictures. Postgrad Med J. 2006;82:489–493. doi: 10.1136/pgmj.2005.042945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cavalcanti AG, Costa WS, Baskin LS, Mc-Aninch JA, Sampaio FJ. A morphometric analysis of bulbar urethral strictures. BJU Int. 2007;100:397–402. doi: 10.1111/j.1464-410X.2007.06904.x. [DOI] [PubMed] [Google Scholar]
- 5.Mundy AR, Andrich DE. Urethral strictures. BJU Int. 2011;107:6–26. doi: 10.1111/j.1464-410X.2010.09800.x. [DOI] [PubMed] [Google Scholar]
- 6.Angermeier KW, Rourke KF, Dubey D, Forsyth RJ, Gonzalez CM. SIU/CUD consultation on urethral strictures: evaluation and follow-up. Urology. 2014;83((3 Suppl)):S8–17. doi: 10.1016/j.urology.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Dubey D. Management of urethral strictures. Indian J Urol. 2011;27:363. doi: 10.4103/0970-1591.85448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stamatiou K, Papadatou A, Moschouris H, Kornezos I, Pavlis A, Christopoulos G. A simple technique to facilitate treatment of urethral strictures with optical internal urethrotomy. Case Rep Urol. 2014;2014:137605. doi: 10.1155/2014/137605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tritschler S, Roosen A, Füllhase C, Füllhase C, Stief CG, Rübben H. Urethral stricture: etiology, investigation and treatments. Dtsch Arztebl Int. 2013;110:220–226. doi: 10.3238/arztebl.2013.0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong SSW, Aboumarzouk OM, Narahari R, O'Riordan A, Pickard R. Simple urethral dilatation, endoscopic urethrotomy, and urethroplasty for urethral stricture disease in adult men. Cochrane Database Syst Rev. 2012;12:CD006934. doi: 10.1002/14651858.CD006934.pub3. [DOI] [PubMed] [Google Scholar]
- 11.Baskin LS, Constantinescu SC, Howard PS, McAninch JW, Ewalt DH, Duckett JW, Snyder HM, Macarak EJ. Biochemical characterization and quantitation of the collagenous components of urethral stricture tissue. J Urol. 1993;150:642–647. doi: 10.1016/s0022-5347(17)35572-6. [DOI] [PubMed] [Google Scholar]
- 12.Mazdak H, Izadpanahi MH, Ghalamkari A, Kabiri M, Khorrami MH, Nouri-Mahdavi K, Alizadeh F, Zargham M, Tadayyon F, Mohammadi A, Yazdani M. Internal urethrotomy and intraurethral submucosal injection of triamcinolone in short bulbar urethral strictures. Int Urol Nephrol. 2010;42:565–568. doi: 10.1007/s11255-009-9663-5. [DOI] [PubMed] [Google Scholar]
- 13.Ashraf J, Radford AR, Turner A, Subramaniam R. Preliminary experience with instillation of triamcinolone acetonide into the urethra for idiopathic urethritis: a prospective pilot study. J Laparoendosc Adv Surg Tech A. 2017;27:1217–1221. doi: 10.1089/lap.2017.0064. [DOI] [PubMed] [Google Scholar]
- 14.Mazdak H, Meshki I, Ghassami F. Effect of mitomycin C on anterior urethral stricture recurrence after internal urethrotomy. Eur Urol. 2007;51:1089–1092. doi: 10.1016/j.eururo.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 15.Mazdak H, Khorram AK, Tolou-Ghamari Z. A retrospective survey of pediatric urethral strictures in Isfahan, Iran. J Compr Ped. 2019;10:e88802. [Google Scholar]
- 16.Broadwin M, Vanni AJ. Outcomes of a urethroplasty algorithm for fossa navicularis strictures. Can J Urol. 2018;25:9591–9595. [PubMed] [Google Scholar]
- 17.Tavakkoli Tabassi K, Yarmohamadi A, Mohammadi S. Triamcinolone injection following internal urethrotomy for treatment of urethral stricture. Urol J. 2011;8:132–136. [PubMed] [Google Scholar]
- 18.Regmi S, Adhikari SC, Yadav S, Singh RR, Bastakoti R. Efficacy of use of triamcinolone ointment for clean intermittent self catheterization following internal urethrotomy. JNMA J Nepal Med Assoc. 2018;56:745–748. doi: 10.31729/jnma.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rezaei M, Badiei R, Badiei R. The effect of platelet-rich plasma injection on post-internal urethrotomy stricture recurrence. World J Urol. 2019;37:1959–1964. doi: 10.1007/s00345-018-2597-8. [DOI] [PubMed] [Google Scholar]