Abstract
Purpose of review
The rise of the pediatric obesity pandemic over the past 40 years has sharpened focus on the management of obesity, hypertension and lipid abnormalities in children. Multiple studies demonstrate that these risk factors track from childhood into adulthood predisposing individuals to premature atherosclerotic cardiovascular disease and putting them at risk for early morbidity and mortality.
Recent findings
Importantly, obesity, hypertension and lipid problems are individual risk factors that can occur independently. Multiple studies have shown that each risk factor causes target organ damage in children. Intensive and focused lifestyle modifications can improve a child’s subclinical disease and decrease the risk for future morbidity.
Summary
Childhood offers a unique opportunity at primordial and primary prevention of atherosclerotic cardiovascular disease. Clinicians must focus on targeting these highly prevalent conditions and applying lifestyle modification and then pharmacologic or surgical therapies as needed.
Keywords: childhood obesity, pediatric hypertension, lipid disorders, review
INTRODUCTION
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of morbidity and mortality in adults. Data from the National Health and Nutrition Examination Survey (NHANES) show the prevalence of ASCVD in adults over 20 years old to be 48% with heart disease being the leading causes of death for adults in the United States. Globally, ~17.6 million deaths were attributed to ASCVD in 2016 alone, a significant increase from the previous decade despite a decreased death rate over the same time period.[1••] A significant proportion of ASCVD risk is due to modifiable risk factors including high systolic blood pressure (SBP), elevated body mass index (BMI), high total cholesterol (TC), high resting blood glucose levels, smoking and low physical activity[2••–6•]. Deaths attributed to ASCVD steadily decreased from ~1980 to 2015 in the United States as well as in all high-income and some middle-income countries.[1••, 2••] Data generated from the IMPACT mortality model attributed 44% of this decrease to improvements in primary prevention including a reduction in TC, SBP, smoking and physical inactivity and 47% to changes in secondary preventative therapies including risk factor modification after an initial event and to a lesser extent catheter and surgical interventions[7].
Risk factors and upstream risk behaviors that contribute to premature ASCVD begin in childhood and track into adulthood. Children with multiple risk factors have been found to have significant target organ damage, also called subclinical atherosclerosis. Subclinical atherosclerosis can be measured using a variety of non-invasive techniques in children. These include carotid intimal medial thickness (cIMT) and computed tomography to evaluate arterial structure, pulse wave velocity (PWV) to measure arterial stiffness, and flow mediated dilation (FMD) to measure endothelial function. [8]
Atherosclerosis in youth was first seen in autopsies performed on Korean and Vietnam War casualties[9, 10]. Since then, the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study, and Bogalusa Heart Study have reproduced these findings on adolescents examined after accidental deaths and more importantly have demonstrated a strong correlation between risk factors and the extent and severity of atherosclerotic plaques.[11, 12] Similarly the Coronary Artery Risk Development in Young Adults (CARDIA) study demonstrated that ASCVD risk factors track from childhood to adulthood and that the progression of atherosclerosis related to the number and severity of risk factors[13]. The accumulation of target organ damage precedes ASCVD events. ASCVD reduction trends are flattening in recent years suggesting that primary and secondary interventions in adults are reaching a limit.[1••] Therefore, childhood offers a unique opportunity at primordial and primary prevention of ASCVD.
Although obesity increases the risk of developing hypertension or dyslipidemia, nearly half of dyslipidemic adolescents are normal weight and similarly a large proportion of obese adolescents have normal lipid profiles[14]. Specific lifestyle modifications can modify dyslipidemia and hypertension with or without initially affecting weight.[15–17] Thus, obesity, dyslipidemia, and hypertension are interrelated but distinct risk factors, with sub-optimal diets and physical activity contributing to each. The 2011 National Heart, Lung, and Blood Institute (NHLBI) Expert Panel guidelines for cardiovascular risk reduction in children encapsulate contemporary recommendations for the diagnosis and management of obesity, dyslipidemia, and hypertension[8] and has subsequently been endorsed by professional societies such as the American Academy of Pediatrics (AAP).
OBESITY
Epidemiology, Life-course Tracking and Temporal Trends
Obesity and overweight are defined as a BMI ≥ 95th percentile, and 85th - 94th percentile for age and sex, respectively. In 2013, the American Heart Association (AHA) added the category of severe obesity, defined as a BMI ≥ 120% of the 95th percentile for age and sex or a BMI ≥ 35, in the effort to better identify this smaller subset of patients at highest risk for complications and reflecting the large increase in that subset over time.[18] According to 2013–2014 NHANES data, 33.4% of children are overweight or worse, 17.2% of children are obese and 5.6% have severe obesity. Notably, in the last decade the prevalence of obesity has plateaued, however this trend masks some important distinctions, especially amongst race and socio-economic status (SES). Obesity amongst those with a higher SES status has decreased, while those with a lower SES status has risen. [19, 20] Racial-ethnic data shows that obesity is more prevalent in Blacks and Hispanics than Whites and Asians. With respect to sex differences, there is a slightly increased prevalence of obesity amongst boys than girls but no difference in the prevalence of severe obesity.[1••]
Like many lifestyle habits, it is now well established that obesity and severe obesity track from childhood into adulthood. A recent meta-analysis showed that obese children were 5 times more likely to be obese as adults than their normal weight peers. About half of obese children become obese adolescents with about 80% of obese adolescents becoming obese adults.[21]
Children with obesity and severe obesity suffer from significant comorbidities in myriad organ systems. Metabolic co-morbidities include major ASCVD risk factors such as hypertension, dyslipidemia, and insulin resistance. In addition, obese children suffer from asthma, non-alcoholic fatty liver disease, sleep apnea, psychological/behavioral disorders, and musculoskeletal complications, amongst many others.[22•] In addition, childhood obesity is associated with target organ damage including changes in cardiac structure and function, arterial structure and function, arterial stiffness, endothelial dysfunction and vascular age.[23] Metabolic syndrome, defined as the clustering of metabolic risk factors centered around insulin resistance, increases linearly in the overweight and obese, and exponentially in the severely obese.[24]
Linking childhood obesity with adult ASCVD events and premature mortality is challenging due to the long follow-up period. A systematic review showed that overweight and obese children had an increased risk of ASCVD morbidity with hazard ratios ranging from 1.1–5.1.[25] A report studying Native Americans found that the rate of ASCVD deaths in the highest BMI quartile of children was more than double that of the lowest BMI quartile. [26] Similarly, data from a Swedish cohort showed that obese children had a 2–3 times increased risk of premature death in early adulthood compared to the general population.[27•]
Diagnosis and Management
Annual screening for overweight and obesity using height and weight to calculate BMI is recommended by most professional societies and US governmental bodies.[28••, 29] Clinicians have historically been poor at diagnosing pediatric obesity due to the perceived lack of time to use BMI calculators and provide prevention counseling, concerns about low parental motivation, problems with billing/reimbursement and the concern about the stigmatization of overweight and obese children.[30–32] In addition, perceived body ideals have significant cultural and racial variation[33].
With respect to treatment, the 2017 US Preventative Task Force (USPTF) stated that only intensive weight loss programs that included at least 26 hours of patient contact led to clinically important weight loss.[34••] These programs aim to improve dietary quality and quantity and to increase physical activity. The cornerstones of an obesity reduction diet include portion control, avoiding calorie-dense, nutrient-poor foods like sugary sweetened beverages (SSB), high-fructose corn syrup, and high-sodium ultra-processed foods while increasing intake of fruits and vegetables. Recent data addresses the weight gain debate between a pure energy balance hypothesis versus diet type/quality hypothesis. In a randomized trial comparing equal caloric foods of “high processed” low quality versus “unprocessed” high quality provided to healthy adults in a closed feeding study laboratory demonstrated that energy intake was higher with an ultra-processed diet in comparison to unprocessed diet even when dietary macronutrients were identical, suggesting “low-quality” has an outsized effect on weight.[35••] In addition to dietary changes, screen time should be limited to < 2 hours per day and physical activity increased to 2–5 hours of vigorous exercise per week.[28••, 29] By incorporating behavioral therapy sessions, these programs have had some success.[36] School-based interventions can also be modestly successful.[37] Most patients can lose 5–10% of their body weight and decrease their BMI by 1–2 units, and maintain it over 5 years with strong commitment.[18, 38] In addition, studies have shown a direct improvement in hypertension and dyslipidemia with each unit of weight loss.[28] Unfortunately, success with these programs is often limited by parental commitment.[39] Also, program attrition is very common in part due to the scale of weight loss needed for severely obese youth who still have substantial linear growth and concomitant weight gain to undergo.[40] As weight decreases so too does resting energy expenditure, making ongoing weight loss increasingly difficult.[41] As a result, early success must be followed by ongoing focus in order to maintain progress. Personal responsibility may need to be complemented with public health policy changes. Indeed prominent editorials have stated that obesity is a natural consequence of “toxic” high calorie density food environments placing the onus of action on individuals and also on collective action.[42•]
Pharmacotherapy for pediatric obesity is limited[43]. Orlistat is the only medication currently FDA approved for weight loss in children if ≥ 12 years old. It has shown modest results for obese but not severely obese adolescents. In one study, orlistat decreased BMI by 0.86 kg/m2 compared to placebo.[44] More efficacious drugs have been developed but were not approved due to adverse effects. Other drugs are under investigation, including for genetic conditions such as for Prader-Willi syndrome.[45] Importantly, there is little data on the long-term use of weight loss drugs.
Over the last decade, bariatric surgery has become more acceptable for select individuals with severe obesity and comorbidities.[46] Several surgical options are available and short-term results are promising. In one study of 81 adolescents, BMI was reduced by 32% at 2 years with corresponding improvements in dyslipidemia and hyperinsulinism. However, 33% suffered adverse effects and 15% needed additional surgeries.[47] Importantly, some bariatric surgeries permanently alter enterohepatic and biliary circulations, the long-term effects of which remain unknown. In addition, the long term safety and success of bariatric surgery is questioned with some data suggesting over 20% of initial responders regain their weight and have recurrence of co-morbidities.[48•] Thus, the appropriateness and availability of surgery will depend on long-term follow-up, which are currently in progress. A summary of a staged approach to weight management is shown in Figure 1[29].
Figure 1.
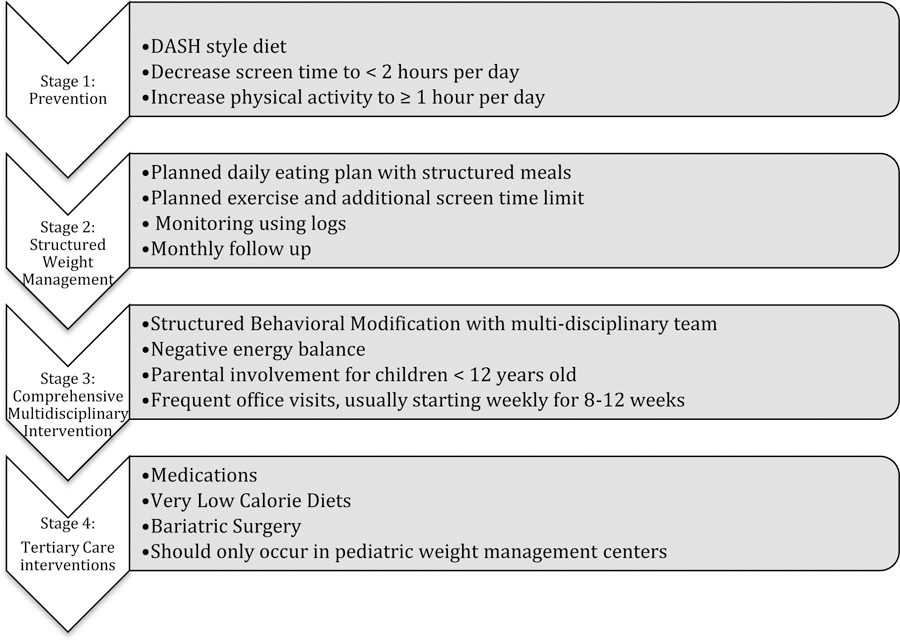
Staged approach to obesity management. This figure summarizes the staged approach to obesity management as outlined by Barlow et. al. [28]
HYPERTENSION
Epidemiology, Life-course Tracking and Temporal Trends
In adults, elevated blood pressure (BP) is the strongest modifiable factor in predicting ASCVD mortality[2••, 4, 49] with one meta-analysis demonstrating that the risk of ASCVD increased in a log-linear fashion with SBP.[50] Widespread attention to pediatric hypertension assessment only started in 1977[51]. Since then multiple studies have been conducted to refine our understanding of pediatric hypertension. The most contemporary evidence-based recommendations for pediatric BP management come from the 2017 AAP BP guidelines and the 2011 NHLBI integrated cardiovascular risk reduction guidelines.[8, 52••]
The prevalence of prehypertension and hypertension in pediatrics has increased over the last half-century despite decreases in the mean SBP during that time.[1••] This is likely due in part to more accurate measurement techniques and growing awareness of hypertension sequelae since the use of BP pharmacotherapy in children remains limited. [53, 54] Another purported contribution on the population level may be reduced lead exposure, which has been linked to declining BP in the U.S. pediatric population[55•]. According to the 2017 AAP BP guidelines, about 14% of early adolescents have an elevated BP.[56••] Several studies have suggested that this increase is related to the obesity epidemic, with evidence showing that BMI exerts strong effects on BP.[57–59] Racial and gender factors are also important. Hypertension is more prevalent amongst Blacks and Hispanics than Whites and Asians. In addition, it is slightly more prevalent in boys than girls.[60•]
According to a systematic meta-analysis of over 50 cohort studies following diverse populations between 1970–2006, there is significant evidence for BP tracking from childhood to adulthood.[61] The strength of BP tracking is greater in adolescents than school age children.[52••] Critically, multiple studies in population based cohorts now show hypertension in adolescence predicts higher all-cause mortality and ASCVD in adulthood.[62, 63] A recent study suggests that with better BP control in children, elevated BP in young adulthood could be averted.[64]
Diagnosis and Classification
The diagnosis and classification of pediatric hypertension has been difficult due to the frequent occurrence of masked hypertension (MH) and white coat, or reactive, hypertension (WCH) in children as well as difficulty ascertaining high BP using age-sex-height dependent normative tables. MH is defined as having a normal in-clinic BP but elevated ambulatory BP. MH occurs in about 7% of children. Pediatric studies have suggested the prevalence of WCH to be around 32%, although WCH prevalence varies significantly across various study populations.[65]
For confirmation of true hypertension, ambulatory blood pressure monitoring (ABPM) is now widely accepted to be superior to office or home BP monitoring in classifying hypertension and in identifying patients as at risk of target organ damage.[52••, 65] Several studies have shown a strong relationship between hypertension diagnosed by ABPM parameters and target organ damage, such as elevated left ventricular (LV) mass[66, 67], thicker cIMT[68, 69], increased PWV[70, 71], and higher carotid artery stiffness[72]. Updated guidelines on the use of ABPM and the interpretation of its results are now available.[52••, 65] Importantly, these guidelines offer a revised classification scheme that addresses previous uncertainty in how to use elevated diastolic blood pressure (DBP), nocturnal BP elevation, and diagnosing prehypertension in children. In addition, ABPM is strongly recommended in obese individuals due to the difficulty in obtaining accurate BP measurements in this population. The cost-effectiveness of ABPM use has been demonstrated in cost effectiveness models in both children and adults with suspected hypertension.[73, 74]
A detailed history and physical is necessary to distinguish between primary and secondary etiologies of hypertension. In one study evaluating the causes of hypertension in a tertiary pediatric hypertension clinic, secondary hypertension was found in 100% patients less than one year old, 80% of patients 1–5 years old and ~50% of patients ≥ 6 years old.[75] A history of prematurity or frequent urinary tract infections or an ABPM with attenuated nighttime dipping[65] may suggest secondary etiologies. A detailed summary of secondary hypertension may be found in the AAP or NHLBI guidelines. In general adolescents with prevalent cardiometabolic risk factors (e.g. elevated BMI and physical inactivity) can be assumed to have essential hypertension until BP improvement does not proceed in an expected fashion.[52••]
Management
Management of pediatric hypertension starts with lifestyle modifications with particular focus on improved dietary quality, increased physical activity and weight management.[5••, 6••, 8, 76] Since publication of the Dietary Approaches to Stop Hypertension (DASH) diet in 1997, multiple studies have consistently shown that its use improves hypertension across various ages and ethnic groups.[77–79•] The DASH diet focuses on increased intake of whole grains, fruits and vegetables high in potassium, magnesium, calcium and fiber, as well as low saturated fat intake through lean meats and fat free dairy and minimal added sugars (Table 1). The DASH diet is a relatively low sodium diet and further reduction in sodium intake has been proven to work synergistically.[80]
Table 1.
Comparison of Hypertension and Dyslipidemia Diets by Macronutrient (referenced to 2000 kcal/day) [8, 75]
| Nutritional Recommendation (per 2000 kcal/day diet) | CHILD-1 | CHILD-2 LDL | CHILD-2 TG | DASH |
|---|---|---|---|---|
| Protein | Lean meats (chicken or turkey without skin, fish, red meat without fat) | |||
| Fats | ||||
| Total | ≤30% of daily kcal (67 grams) | 25–30% of daily kcal (56–67 grams) | 25–30% of daily kcal (56–67 grams) | Limit servings based on age group, fat free milk |
| Saturated | 7–10% daily kcal (16–22 grams) | < 7% daily kcal (<16 grams) | < 7% daily kcal (<16 grams) | |
| Monounsaturated | ≤20% (≤44 grams) | ~10% (22grams) | ~10% (22 grams) | |
| Trans | Avoid | Avoid | Avoid | |
| Cholesterol | < 300 mg/day | <200 mg/day | <200 mg/day | |
| Carbs | Encourage high dietary fiber | Avoid simple carbs, only eat complex carbs | Whole grains (not enriched or bleached), fruits and vegetables | |
| Sugar | Limit added sugars, SSBs | Avoid added sugars, SSBs | Limit servings based on age group | |
While the relationship between physical activity (PA) and BP is well established in adults, data in children and adolescents has been challenging to establish often due to study design or limited participation. One meta-analysis of 1266 subjects showed that exercise reduced SBP and DBP by 1% and 3% respectively, however this did not meet statistical significance.[81] More recent data from the Avon Longitudinal Study of Parents and Children (ALSPAC) followed over 5500 patients and measured exercise using wearable technology. The study confirmed that higher PA was associated with lower BP and suggested that the volume of activity may be more important than the intensity.[82] The strongest evidence for improving PA in children is through school-based intervention strategies.[83, 84]
When 6 months of adequate lifestyle modifications fail to improve BP or if in-clinic or ABPM demonstrates severely elevated BP, initiation of pharmacologic treatment is warranted as outlined by the 2017 AAP guidelines.[52••] In general, calcium channel blockers (CCB), angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor antagonists (ARB) are the preferred first line drugs depending on indications for targeted drug therapy. Of note, thiazide diuretics and beta-blockers can impair glucose metabolism and should be used cautiously in patients at risk for developing diabetes.[85] ASCVD event-based goals for antihypertensive therapy in children are not well established due to the rarity of ASCVD events and paucity of outcome based drug trials in children, so reduction to “normal” levels, either below 90 percentile or below 130/80 are given in the guidelines.[86, 87] Also, causes of secondary hypertension are more common in children and must be addressed if present. Remaining questions include the utility of vascular or cardiac assessments on future ASCVD prediction in pediatric hypertension as well as the role of pharmacological or other interventions for hypertension management in children on future ASCVD risk reduction.
DYSLIPIDEMIA
Epidemiology, Life-course Tracking and Temporal Trends
ASCVD is the end result of a lifelong accumulation of fatty streaks and plaques that begin in utero as evidenced by several autopsy studies.[11–13] While ASCVD events in children are rare, data from the Bogalusa[12, 88], PDAY[11], Muscatine[89, 90] and Cardiovascular Risk in Young Finns[91, 92] studies demonstrate that moderate to severe lipid abnormalities track into adulthood, accelerate the development of atherosclerosis, and lead to earlier ASCVD morbidity and mortality. In particular, familial hypercholesterolemia (FH), a Mendelian-inheritance genetic disorder, links the effects of chronically elevated low-density lipoprotein cholesterol (LDL-c) in childhood to premature ASCVD events in young adulthood. Data from registries and genetic metacohorts show that young and older adults with FH genes have a multifold higher risk for ASCVD than their non-FH peers.[93–95••] Multiple studies have been conducted demonstrating increases in cIMT and PWV and decreases in FMD in children with dyslipidemia.[96]
In the face of the obesity pandemic, lipid profiles have actually slightly improved in children, the reasons for which are unclear.[1••, 97••] According to the most recent NHANES data, the prevalence of adverse levels of TC, triglycerides (TG), high-density lipoprotein cholesterol (HDL-c) and LDL-c are 7.1%, 10.2%, 12.1% and 6.4% respectively[97••]. Elevated LDL-c is slightly more prevalent in girls than boys; however, boys have higher levels of HDL-c and triglycerides (TG) than girls.[1••] In general, Asians have higher TC, LDL-c and TGs than other races. Hispanics have the lowest HDL-c, and Blacks have much lower TG levels than other races.[98] Importantly, while obese individuals have a nearly 3 times higher risk for lipid problems, a substantial proportion of youth with lipid problems are normal weight. Thus, fixating on excess weight in screening will miss a substantial proportion with abnormal lipids and specifically genetic lipid disorders.[99]
Diagnosis and Classification
Generally, there are 4 classes of pediatric lipid disorders: genetic lipid disorders, dyslipidemia related to lifestyle factors, medication-related dyslipidemias, and dyslipidemias secondary to a medical condition. Lifestyle dyslipidemias is defined as the triad of low HDL-c, elevated TG and mildly elevated LDL-c from increased number of small, dense LDL particles. Genetic lipid disorders tend to have more narrow abnormalities in lipid profiles. For example, individuals with FH often have isolated increases in LDL-c.[8]
The primary genetic lipid disorders are FH, familial combined hyperlipidemia (FCH), and familial severe hypertriglyceridemia (HTG). Homozygous FH usually presents with xanthelasmas, xanthomas and ASCVD events in the first two decades of life[100]. Heterozygous FH (HeFH), with prevalence 1/250, and FCH, with prevalence approaching 1/100, both predispose to early ASCVD events in young adulthood and are frequently clinically silent prior to the coronary event. Familial HTG can cause acute pancreatitis at any time and may also predispose to premature ASCVD. A review of secondary lipid disorders is beyond the scope of this review apart from primarily focusing on the underlying condition and any remaining lipid issues thereafter.
Screening
The goal of lipid screening in childhood is the identification of patients with genetic lipid disorders especially HeFH.[101•] Initial screening guidelines published by the National Cholesterol Education Program (NCEP) in 1992 recommended targeted screening by family history which were later revised to include other lifestyle risk factors and medical conditions.[102, 103] However, several studies have shown that screening by family history alone misses 30–60% of children with elevated lipid levels.[104, 105] The 2011 NHLBI guidelines introduced universal screening for lipid disorders in children between 9–11 years old and again between 17–21 years old. The guidelines also recommended focused screening for individuals ≥ 2 years old with elevated risk factors.[8] Universal screening creates the opportunity for reverse cascade screening, i.e. testing parents after a child has been diagnosed. However, universal screening remains controversial due to a lack of data on whether the earlier diagnosis decreases future ASCVD events, the stigmatization following diagnosis, the potential of creating dietary neuroses in children, and the cost of universal screening programs. As a result, the 2016 USPTF review concluded that there was insufficient evidence to recommend for or against universal lipid screening.[106]
Over time, provider screening for children with lipid disorders has not substantially improved. From 2002 to 2012, overall lipid testing declined, however the detection of FH-level LDL-c increased, possibly related to more selective testing of patients at risk of having genetic lipid disorders. Yet the expected proportion were not detected.[107] Barriers to implementation of the 2011 NHLBI guidelines include lack of guideline awareness, a discomfort with managing lipid disorders, and opposition to the use of lipid lowering drugs in children.[107, 108]
Nonetheless, early diagnosis and alteration of risk behaviors is critically important. A recent meta-analysis demonstrated that the use of statin and non-statin drugs were associated with similar relative risk reductions for major ASCVD events per change in LDL-c.[109] Another key study from the Dutch cohort found that offspring with HeFH were essentially completely protected from coronary events before age 40 while their parents were substantially affected before age 40, suggesting the provision of pharmacotherapy during youth altered the natural history.[110••] Another combined meta-analysis compared the effect of lipid lowering agents versus naturally occurring LDL-c lowering genetic polymorphisms on ASCVD events showed that genetic polymorphisms were several times more effective than pharmacological therapy, suggesting life-long exposure to lower LDL-c levels were more protective.[111] In summary, it is the chronic exposure to elevated LDL-c that increases the risk for ASCVD events and this exposure appears modifiable.
Management
The first step in the management of children with dyslipidemias is targeted lifestyle modifications. Importantly, lifestyle modifications can improve lipid levels without affecting weight immediately.[15, 16, 112, 113] Targeting only weight loss instead of an improvement in dietary quality may only further stigmatize the child and lead to failure.[114] The NHBLI Cardiovascular Health Integrated Lifestyle Diet (CHILD-1) is recommended for all patients with dyslipidemia or at risk of developing dyslipidemia due to family history or exposures in the home, which is nearly all children in the USA. With this diet, total fat should be limited to 30% of total calories, saturated fat to 7–10% of calories; trans fat should be avoided, and dietary cholesterol limited to 300mg per day. The diet also stresses the importance of increased fruit and vegetable intake, avoidance of sugar sweetened beverages (SSBs), and limited portion sizes.[8] However, for patients with persistently elevated LDL-c or FH while on the CHILD-1 diet, the CHILD-2 LDL-c diet modification is recommended which further limits saturated fat to < 7% total calories, dietary cholesterol to < 200 mg/day, and endorses incorporation of plant sterols and water-soluble psyllium into the diet. Similarly, for patients with persistently elevated TGs while being on the CHILD-1 diet, the CHILD-2 TG diet modification is recommended which eliminates SSB and added sugars and endorses replacing simple carbohydrates with complex carbohydrates. Table 1 compares the CHILD-1, CHILD-2 and DASH diets. In addition, there is strong evidence that patients should get ~5 hours of moderate to vigorous exercise per week and limit sedentary screen times to less than 2 hours per day across all diets.[8]
Pharmacological therapy is indicated in patients with insufficient lipid improvement despite adequate lifestyle interventions, those with significantly abnormal baseline lipid levels in combination with family history or other ASCVD risk factors, or in those with a diagnosis of FH. While pediatric providers have been slow to initiate statin therapy for lifestyle induced dyslipidemias, the use of statins for FH provides significant experience on the long-term safety of their use in childhood. Several recent publications evaluating pharmacotherapy for HeFH concluded that statin use decreased ASCVD events to close to that of the general population and slowed progression of atherosclerotic plaques.[110••, 115, 116•] Statins decreased LDL-c levels by an average of 32% with 20% of individuals achieving treatment goals. Just as important for children, a Cochrane review of nine randomized placebo control trials of statins in children showed no difference between statin and placebo in liver enzyme levels, incidence of rhabdomyolysis or sexual maturation.[117•] Importantly, there is growing evidence that statin use may be associated with the development of diabetes in children similarly to adults.[118•] As such, statins should be used with caution.
CONCLUSION
With the rise of the obesity epidemic, familiarity with the management of obesity, hypertension and lipid disorders in children has become increasingly necessary. There is ample evidence that these diagnoses track from childhood into adulthood and subsequently significantly increase the risk for ASCVD events earlier in life. In addition, there is a growing body of literature showing the damaging effects that occur in childhood as well. Thus, childhood offers a unique opportunity for primordial and primary prevention of these risk factors and risk behaviors. These risk factors can be improved with lifestyle modification through targeted dietary changes and an increase in physical activity. For hypertension and dyslipidemia, recent data supports focusing on dietary quantity and quality. In certain cases, pharmacological or surgical therapies are indicated. Further work is needed to better understand genetic and phenotypic variation and the effects of public policy in pursuit of healthier behaviors.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of Interest and Sources of Funding: This work was supported by National Heart, Lung, and Blood Institute R01 HL148217 (JPZ). We declare we have no relevant financial conflicts of interest or disclosures. We declare the sponsor had no role in the 1) study design; 2) the collection, analysis, and interpretation of data; 3) the writing of the report; nor 4) the decision to submit the manuscript for publication. This article does not contain any studies with human or animal subjects performed by any of the authors.
REFRENCES AND RECOMMENDED READING
Recent papers of particular importance have been highlighted as:
• Of importance
•• Of major importance
- 1.Benjamin J, Muntner S, Alonso W, et al. (2019) Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 139:e56–e66This article summarizes the most up-to-date statistics regarding heart disease and stroke and the cardiovascular risk factors that contribute to each.
- 2.Roth GA, Johnson CO, Abate KH, et al. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol 3:375–389This article summarizes the national burden of cardiovascular disease in the United States, revealing disparities amongst age, sex, and geography. It also summarizes drivers of change in cardiovascular disease morbidity.
- 3.Fryar CD, Chen T-C, Li X (2012) Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief 1–8 [PubMed]
- 4.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, Ezzati M (2009) The Preventable Causes of Death in the United States: Comparative Risk Assessment of Dietary, Lifestyle, and Metabolic Risk Factors (Mortality Effects of Risk Factors in the US). PLoS Med 6:e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whelton K, Carey M, Aronow S, et al. (2018) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 138:e426–e483This is the most recent clinical practice guideline for the management of high blood pressure in adults.
- 6.Whelton PK, Williams B, Hope K, et al. (2018) The 2018 European Society of Cardiology/European Society of Hypertension and 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines: More Similar Than Different. In: JAMA Totowa, NJ: : Humana Press : Imprint: Humana, pp 1749–7This editorial compares the most recent American and European clinical practice guidelines on the management of high blood pressure in adults.
- 7.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S (2007) Explaining the Decrease in U.S. Deaths from Coronary Disease, 1980–2000. N Engl J Med 356:2388–2398 [DOI] [PubMed] [Google Scholar]
- 8.Expert Panel On Integrated Guidelines FOR Cardiovascular Health And Risk Reduction In Children And Adolescents (2011) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128 Suppl 5:S213–S256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Enos WF, Holmes RH, Beyer J (1953) Coronary disease among United States soldiers killed in action in Korea; preliminary report. J Am Med Assoc 152:1090–1093 [DOI] [PubMed] [Google Scholar]
- 10.McNamara JJ, Molot MA, Stremple JF, Cutting RT (1971) Coronary artery disease in combat casualties in Vietnam. JAMA 216:1185–1187 [PubMed] [Google Scholar]
- 11.Strong JP, Malcom GT, Mcmahan CA, Tracy RE, Newman III WP, Herderick EE, Cornhill JF, for the Pathobiological Determinants of Atherosclerosis in Youth Research Group (1999) Prevalence and Extent of Atherosclerosis in Adolescents and Young Adults: Implications for Prevention From the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA 281:727–735 [DOI] [PubMed] [Google Scholar]
- 12.Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 338:1650–1656 [DOI] [PubMed] [Google Scholar]
- 13.Mcmahan CA, Gidding SS, Malcom GT, Schreiner PJ, Strong JP, Tracy RE, Williams OD, Mcgill HC (2007) Comparison of coronary heart disease risk factors in autopsied young adults from the PDAY Study with living young adults from the CARDIA study. Cardiovasc Pathol 16:151–158 [DOI] [PubMed] [Google Scholar]
- 14.May AL, Kuklina EV, Yoon PW (2012) Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics 129:1035–1041 [DOI] [PubMed] [Google Scholar]
- 15.Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS (2007) Effects of a Low–Glycemic Load vs Low-Fat Diet in Obese Young Adults: A Randomized Trial. JAMA 297:2092–2102 [DOI] [PubMed] [Google Scholar]
- 16.Jacobson MS, Tomopoulos S, Williams CL, Arden MR, Deckelbaum RJ, Starc TJ (1998) Normal Growth in High-Risk Hyperlipidemic Children and Adolescents with Dietary Intervention. Prev Med 27:775–780 [DOI] [PubMed] [Google Scholar]
- 17.Farpour-Lambert NJ, Aggoun Y, Marchand LM, Martin XE, Herrmann FR, Beghetti M (2009) Physical Activity Reduces Systemic Blood Pressure and Improves Early Markers of Atherosclerosis in Pre-Pubertal Obese Children. J Am Coll Cardiol 54:2396–2406 [DOI] [PubMed] [Google Scholar]
- 18.Kelly S, Barlow E, Rao H, Inge L, Hayman M, Steinberger J, Urbina R, Ewing R, Daniels R (2013) Severe Obesity in Children and Adolescents: Identification, Associated Health Risks, and Treatment Approaches: A Scientific Statement From the American Heart Association. Circulation 128:1689–1712 [DOI] [PubMed] [Google Scholar]
- 19.Frederick CB, Snellman K, Putnam RD (2014) Increasing socioeconomic disparities in adolescent obesity. Proc Natl Acad Sci U S A 111:1338–1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogden CL, Lamb MM, Carroll MD, Flegal KM (2010) Obesity and Socioeconomic Status in Children and Adolescents: United States, 2005–2008. NCHS Data Brief Number 51. National Center for Health Statistics; [PubMed] [Google Scholar]
- 21.Simmonds M, Llewellyn A, Owen CG, Woolacott N (2016) Predicting adult obesity from childhood obesity: a systematic review and meta‐analysis. Obes Rev 17:95–107 [DOI] [PubMed] [Google Scholar]
- 22.Sharma V, Coleman S, Nixon J, Sharples L, Hamilton‐Shield J, Rutter H, Bryant M (2019) A systematic review and meta‐analysis estimating the population prevalence of comorbidities in children and adolescents aged 5 to 18 years. Obes Rev 20:1341–1349This systematic review searches 5 databases up to 2018 for the population prevalence of obesity-associated comorbidities in children and adolescents.
- 23.Cote AT, Harris KC, Panagiotopoulos C, Sandor GGS, Devlin AM (2013) Childhood Obesity and Cardiovascular Dysfunction. J Am Coll Cardiol 62:1309–1319 [DOI] [PubMed] [Google Scholar]
- 24.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH (2007) Cardiovascular Risk Factors and Excess Adiposity Among Overweight Children and Adolescents: The Bogalusa Heart Study. J Pediatr 150:12–17.e2 [DOI] [PubMed] [Google Scholar]
- 25.Reilly JJ, Kelly J (2011) Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes 35:891–898 [DOI] [PubMed] [Google Scholar]
- 26.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC (2010) Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N Engl J Med 362:485–493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindberg L, Danielsson P, Persson M, Hagman E, Marcus C (2017) Childhood obesity increases risk of premature death in young adulthood – A prospective cohort studyLouise Lindberg. Eur J Public Health 10.1093/eurpub/ckx189.254This article summarizes the findings of a Swedish cohort showing that obese children had an increased incidence of premature death in early adulthood compared with the general population.
- 28.Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, Yanovski JA (2017) Pediatric Obesity-Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 102:709–757This article summarizes the Endocrine Society’s most recent clinical practice guideline for the assessment, treatment and prevention of childhood obesity.
- 29.Barlow SE (2007) Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 120:S164–S192 [DOI] [PubMed] [Google Scholar]
- 30.Gray JS, Filigno SS, Santos M, Ward WL, Davis AM (2013) The Status of Billing and Reimbursement in Pediatric Obesity Treatment Programs. J Behav Health Serv Res 40:378–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strauss RS, Pollack HA (2003) Social Marginalization of Overweight Children. Arch Pediatr Adolesc Med 157:746–752 [DOI] [PubMed] [Google Scholar]
- 32.Perrin EM, Finkle JP, Benjamin JT (2007) Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr 19:354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, Schwimmer JB (2008) Influence of Race, Ethnicity, and Culture on Childhood Obesity: Implications for Prevention and Treatment. Diabetes Care 31:2211–2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grossman DC, Bibbins-Domingo K, Curry SJ, et al. (2017) Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 317:2417–2426This article from the USPTF recommends that all children 6 years and older be screened for obesity and referred for comprehensive intensive behavioral therapy to improve their weight status.
- 35.Hall KD, Ayuketah A, Brychta R, et al. (2019) Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab 30:67–77.e3In this study, two groups of patients were given either an ultra-processed or unprocessed diet. Even when the diets were matched for calories and macronutrients those eating an ultra-processed diet gained more weight.
- 36.Epstein LH, Roemmich JN, Raynor HA (2001) BEHAVIORAL THERAPY IN THE TREATMENT OF PEDIATRIC OBESITY. Pediatr Clin 48:981–993 [DOI] [PubMed] [Google Scholar]
- 37.Wang Y, Cai L, Wu Y, et al. (2015) What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes Rev Off J Int Assoc Study Obes 16:547–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.August GP, Caprio S, Fennoy I, Freemark M, Kaufman FR, Lustig RH, Silverstein JH, Speiser PW, Styne DM, Montori VM (2008) Prevention and Treatment of Pediatric Obesity: An Endocrine Society Clinical Practice Guideline Based on Expert Opinion. J Clin Endocrinol Metab 93:4576–4599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wrotniak BH, Epstein LH, Paluch RA, Roemmich JN (2005) The Relationship Between Parent and Child Self-Reported Adherence and Weight Loss. Obes Res 13:1089–1096 [DOI] [PubMed] [Google Scholar]
- 40.Dhaliwal J, Nosworthy NMI, Holt NL, Zwaigenbaum L, Avis JLS, Rasquinha A, Ball GDC (2014) Attrition and the management of pediatric obesity: an integrative review. Child Obes Print 10:461–473 [DOI] [PubMed] [Google Scholar]
- 41.Hall KD (2018) The complicated relation between resting energy expenditure and maintenance of lost weight. Am J Clin Nutr 108:652–653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Swinburn BA, Kraak VI, Allender S, et al. (2019) The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. The Lancet 393:791–846This article explains how the obesity epidemic is actually part of a world-wide syndemic and describes how toxic food environments contribute to furthering obesity.
- 43.Sherafat-Kazemzadeh R, Yanovski SZ, Yanovski JA (2013) Pharmacotherapy for childhood obesity: present and future prospects. Int J Obes 37:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chanoine J-P, Hampl S, Jensen C, Boldrin M, Hauptman J (2005) Effect of Orlistat on Weight and Body Composition in Obese Adolescents: A Randomized Controlled Trial. JAMA 293:2873–2883 [DOI] [PubMed] [Google Scholar]
- 45.Crinò A, Fintini D, Bocchini S, Grugni G (2018) Obesity management in Prader-Willi syndrome: current perspectives. Diabetes Metab Syndr Obes Targets Ther 11:579–593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pratt JSA, Lenders CM, Dionne EA, et al. (2009) Best Practice Updates for Pediatric/Adolescent Weight Loss Surgery. Obesity 17:901–910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olbers T, Gronowitz E, Werling M, et al. (2012) Two-year outcome of laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity: results from a Swedish Nationwide Study (AMOS). Int J Obes 36:1388–1395 [DOI] [PubMed] [Google Scholar]
- 48.Heymsfield S, Aronne LJ, Eneli I, Kumar RB, Michalsky M, Walker E, Wolfe BM, Woolford SJ, Yanovski and S (2018) Clinical Perspectives on Obesity Treatment: Challenges, Gaps, and Promising Opportunities. NAM Perspect 10.31478/201809bThis article summarizes the challenges and treatment gaps in the management of obesity including the role of pharmacotherapy, bariatric surgery and policy change.
- 49.World Health Organization (2009) Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks World Health Organization, Albany [Google Scholar]
- 50.Rapsomaniki E, Timmis A, George J, et al. (2014) Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet Lond Engl 383:1899– [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blumenthal S, Epps RP, Heavenrich R, et al. (1977) Report of the task force on blood pressure control in children. Pediatrics 59:I–II, 797–820 [PubMed] [Google Scholar]
- 52.Flynn JT, Kaelber DC, Baker-Smith CM, et al. (2017) Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 10.1542/peds.2017-1904This article summarizes the most recent clinical practice guideline for the management of high blood pressure in children.
- 53.Din-Dzietham R, Liu Y, Bielo M-V, Shamsa F (2007) High Blood Pressure Trends in Children and Adolescents in National Surveys, 1963 to 2002. Circulation 116:1488–1496 [DOI] [PubMed] [Google Scholar]
- 54.Dobson CP, Eide M, Nylund CM (2015) Hypertension Prevalence, Cardiac Complications, and Antihypertensive Medication Use in Children. J Pediatr 167:92–97.e1 [DOI] [PubMed] [Google Scholar]
- 55.Zachariah JP, Wang Y, Penny DJ, Baranowski T (2018) Relation Between Lead Exposure and Trends in Blood Pressure in Children. Am J Cardiol 122:1890–1895This article shows that the recent decline in pediatric blood pressure during the rise of pediatric obesity may be attributable to declining lead exposure.
- 56.Sharma A, Metzger D, Rodd C (2018) Prevalence and Severity of High Blood Pressure Among Children Based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatr 557This article assesses the consequences of the new clinical practice guideline for high blood pressure in children. The article reveals that with the new definitions an additional 5.8% of children would be diagnosed as having high blood pressure.
- 57.Muntner P, He J, Cutler JA, Wildman RP, Whelton PK (2004) Trends in Blood Pressure Among Children and Adolescents. JAMA 291:2107–2113 [DOI] [PubMed] [Google Scholar]
- 58.Shi Y, de Groh M, Morrison H (2012) Increasing blood pressure and its associated factors in Canadian children and adolescents from the Canadian Health Measures Survey. BMC Public Health 12:388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Falkner B, Gidding SS, Portman R, Rosner B (2008) Blood pressure variability and classification of prehypertension and hypertension in adolescence. Pediatrics 122:238–242 [DOI] [PubMed] [Google Scholar]
- 60.Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA (2017) Race and Obesity in Adolescent Hypertension. Pediatrics 10.1542/peds.2016-1433This article shows how the prevalence of adolescent hypertension varies amongst race and ethnicities.
- 61.Chen X, Wang Y (2008) Tracking of Blood Pressure From Childhood to Adulthood: A Systematic Review and Meta–Regression Analysis. Circulation 117:3171–3180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gray L, Lee I-M, Sesso HD, Batty GD (2011) Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study). J Am Coll Cardiol 58:2396–2403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sundström J, Neovius M, Tynelius P, Rasmussen F (2011) Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. The BMJ 10.1136/bmj.d643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kelly RK, Thomson R, Smith KJ, Dwyer T, Venn A, Magnussen CG (2015) Factors Affecting Tracking of Blood Pressure from Childhood to Adulthood: The Childhood Determinants of Adult Health Study. J Pediatr 167:1422–1428.e2 [DOI] [PubMed] [Google Scholar]
- 65.Flynn T, Daniels R, Hayman L, Maahs M, Mccrindle W, Mitsnefes P, Zachariah M, Urbina M (2014) Update: Ambulatory Blood Pressure Monitoring in Children and Adolescents: A Scientific Statement From the American Heart Association. Hypertension 63:1116–1135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stergiou George S, Giovas Periklis P, Kollias Anastasios, Rarra Vayia C, Papagiannis John, Georgakopoulos Dimitris, Vazeou Andriani (2011) Relationship of home blood pressure with target-organ damage in children and adolescents. Hypertens Res 34:640–644 [DOI] [PubMed] [Google Scholar]
- 67.Sorof M, Cardwell J, Franco J, Portman J (2002) Ambulatory Blood Pressure and Left Ventricular Mass Index in Hypertensive Children. Hypertens J Am Heart Assoc 39:903–908 [DOI] [PubMed] [Google Scholar]
- 68.Stabouli S, Kotsis V, Papamichael C, Constantopoulos A, Zakopoulos N (2005) Adolescent Obesity is Associated with High Ambulatory Blood Pressure and Increased Carotid Intimal-Medial Thickness. J Pediatr 147:651–656 [DOI] [PubMed] [Google Scholar]
- 69.Lande B, Carson L, Roy C, Meagher C (2006) Effects of Childhood Primary Hypertension on Carotid Intima Media Thickness: A Matched Controlled Study. Hypertension 48:40–44 [DOI] [PubMed] [Google Scholar]
- 70.Zhu H, Yan W, Ge D, Treiber FA, Harshfield GA, Kapuku G, Snieder H, Dong Y (2007) Cardiovascular Characteristics in American Youth With Prehypertension. Am J Hypertens 20:1051–1057 [DOI] [PubMed] [Google Scholar]
- 71.Kulsum‐Mecci N, Goss C, Kozel BA, Garbutt JM, Schechtman KB, Dharnidharka VR (2017) Effects of Obesity and Hypertension on Pulse Wave Velocity in Children. J Clin Hypertens 19:221–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aggoun Y, Farpour - Lambert NJ, Marchand LM, Golay E, Maggio ABR, Beghetti M (2008) Impaired endothelial and smooth muscle functions and arterial stiffness appear before puberty in obese children and are associated with elevated ambulatory blood pressure. Eur Heart J 29:792–799 [DOI] [PubMed] [Google Scholar]
- 73.Lovibond K, Jowett S, Barton P, et al. (2011) Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet Lond Engl 378:1219–1230 [DOI] [PubMed] [Google Scholar]
- 74.Swartz SJ, Srivaths PR, Croix B, Feig DI (2008) Cost-Effectiveness of Ambulatory Blood Pressure Monitoring in the Initial Evaluation of Hypertension in Children. Pediatrics 122:1177–1181 [DOI] [PubMed] [Google Scholar]
- 75.Gupta-Malhotra M, Banker A, Shete S, Hashmi SS, Tyson JE, Barratt MS, Hecht JT, Milewicz DM, Boerwinkle E (2015) Essential Hypertension vs. Secondary Hypertension Among Children. Am J Hypertens 28:73–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dennison BA (2012) Bright Futures and NHLBI Integrated Pediatric Cardiovascular Health Guidelines. Pediatr Ann 41:e31–e36 [DOI] [PubMed] [Google Scholar]
- 77.Appel LJ, Moore TJ, Obarzanek E, et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336:1117–1124 [DOI] [PubMed] [Google Scholar]
- 78.Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC (2015) Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis 80:1–15This systematic review summarizes the beneficial effect of the DASH diet on blood pressure, overweight and obesity in adolescence.
- 79.Paula Bricarello L, Poltronieri F, Fernandes R, Retondario A, de Moraes Trindade EBS, de Vasconcelos F de AG (2018) Effects of the Dietary Approach to Stop Hypertension (DASH) diet on blood pressure, overweight and obesity in adolescents: A systematic review. Clin Nutr ESPEN 28:1–11 [DOI] [PubMed] [Google Scholar]
- 80.Sacks FM, Svetkey LP, Vollmer WM, et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344:3–10 [DOI] [PubMed] [Google Scholar]
- 81.Kelley GA, Kelley KS, Tran ZV (2003) The Effects of Exercise on Resting Blood Pressure in Children and Adolescents: A Meta-Analysis of Randomized Controlled Trials. Prev Cardiol 6:8–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Leary Sam D, Ness Andy R, Smith George Davey, Mattocks Calum, Deere Kevin, Blair Steven N, Riddoch Chris (2008) Physical Activity and Blood Pressure in Childhood. Hypertension 51:92–98 [DOI] [PubMed] [Google Scholar]
- 83.Steinberger R, Daniels R, Hagberg S, et al. (2016) Cardiovascular Health Promotion in Children: Challenges and Opportunities for 2020 and Beyond: A Scientific Statement From the American Heart Association. Circulation 134:e236–e255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.PAG Midcourse Report: Strategies to Increase Physical Activity Among Youth |. health.gov. https://health.gov/our-work/physical-activity/previous-guidelines/2013-midcourse-report. Accessed 7 Feb 2020.
- 85.Messerli Franz H, Bangalore Sripal, Julius Stevo (2008) Risk/Benefit Assessment of β-Blockers and Diuretics Precludes Their Use for First-Line Therapy in Hypertension. Circulation 117:2706–2715 [DOI] [PubMed] [Google Scholar]
- 86.Ferguson M, Flynn J (2014) Treatment of Pediatric Hypertension: Lessons Learned from Recent Clinical Trials. Curr Cardiovasc Risk Rep 8:1–7 [Google Scholar]
- 87.Ferguson M, Flynn J (2014) Rational use of antihypertensive medications in children. Pediatr Nephrol 29:979–988 [DOI] [PubMed] [Google Scholar]
- 88.Relation of Serum Lipoprotein Levels and Systolic Blood Pressure to Early Atherosclerosis | NEJM https://www.nejm.org/doi/full/10.1056/nejm198601163140302. Accessed 15 Dec 2019 [DOI] [PubMed]
- 89.Schrott HG, Bucher KA, Clarke WR, Lauer RM (1979) The Muscatine hyperlipidemia family study program. Prog Clin Biol Res 32:619–646 [PubMed] [Google Scholar]
- 90.Davis PH, Dawson JD, Riley WA, Lauer RM (2001) Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation 104:2815–2819 [DOI] [PubMed] [Google Scholar]
- 91.Raitakari OT, Juonala M, Kähönen M, et al. (2003) Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 290:2277–2283 [DOI] [PubMed] [Google Scholar]
- 92.Juhola J, Magnussen CG, Viikari JSA, et al. (2011) Tracking of Serum Lipid Levels, Blood Pressure, and Body Mass Index from Childhood to Adulthood: The Cardiovascular Risk in Young Finns Study. J Pediatr 159:584–590 [DOI] [PubMed] [Google Scholar]
- 93.Duell PB, Gidding SS, Andersen RL, et al. (2019) Longitudinal low density lipoprotein cholesterol goal achievement and cardiovascular outcomes among adult patients with familial hypercholesterolemia: The CASCADE FH registry. Atherosclerosis 289:85–93This article reports on an American cohort of patients with FH and shows that with aggressive therapy, the LDL-c in FH patients can be reduced to near normal levels.
- 94.Pérez de Isla L, Alonso R, Mata N, et al. (2017) Predicting Cardiovascular Events in Familial Hypercholesterolemia: The SAFEHEART Registry (Spanish Familial Hypercholesterolemia Cohort Study). Circulation 135:2133–2144This article reports on a Spanish cohort of patients with FH and describes the development of a risk prediction equation for ASCVD events unique to this population.
- 95.Masana L, Zamora A, Plana N, et al. (2019) Incidence of Cardiovascular Disease in Patients with Familial Hypercholesterolemia Phenotype: Analysis of 5 Years Follow-Up of Real-World Data from More than 1.5 Million Patients. J Clin Med 10.3390/jcm8071080This article compares the incidence of ASCVD events in patients with FH to those with normal lipid profiles. The hazard ratio for ASCVD and coronary heart disease in patients with FH were 7.1 and 16.7 respectively.
- 96.Urbina Elaine M, Williams Richard V, Alpert Bruce S, et al. (2009) Noninvasive Assessment of Subclinical Atherosclerosis in Children and Adolescents. Hypertension 54:919–950 [DOI] [PubMed] [Google Scholar]
- 97.Perak AM, Ning H, Kit BK, de Ferranti SD, Van Horn LV, Wilkins JT, Lloyd-Jones DM (2019) Trends in Levels of Lipids and Apolipoprotein B in US Youths Aged 6 to 19 Years, 1999–2016. JAMA 321:1895–1905This article summarizes the most recent NHANES data on the incidence of lipid disorders in children and adolescents.
- 98.Bansal N, Tejtel K (2019) Race/Ethnic differences in dyslipidemia patterns in Youth. J Clin Lipidol 13:e43 [Google Scholar]
- 99.Zachariah J (2016) Lipid Screening in Youth MDText.com, Inc. [Google Scholar]
- 100.Goldberg AC, Hopkins PN, Toth PP, et al. (2011) Familial Hypercholesterolemia: Screening, diagnosis and management of pediatric and adult patients. J Clin Lipidol 5:S1–S8 [DOI] [PubMed] [Google Scholar]
- 101.Akioyamen LE, Genest J, Shan SD, Reel RL, Albaum JM, Chu A, Tu JV (2017) Estimating the prevalence of heterozygous familial hypercholesterolaemia: a systematic review and meta-analysis. BMJ Open This systematic review pooled data from > 2.5 million people to estimate the prevalence of FH to be ~1/250 individuals.
- 102.(1992) National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics 89:495–501 [PubMed] [Google Scholar]
- 103.Daniels SR, Greer FR, Committee on Nutrition (2008) Lipid screening and cardiovascular health in childhood. Pediatrics 122:198–208 [DOI] [PubMed] [Google Scholar]
- 104.Haney EM, Huffman LH, Bougatsos C, Freeman M, Steiner RD, Nelson HD (2007) Screening and treatment for lipid disorders in children and adolescents: systematic evidence review for the US Preventive Services Task Force. Pediatrics 120:e189–e214 [DOI] [PubMed] [Google Scholar]
- 105.Ritchie SK, Murphy EC-S, Ice C, Cottrell LA, Minor V, Elliott E, Neal W (2010) Universal Versus Targeted Blood Cholesterol Screening Among Youth: The CARDIAC Project. Pediatrics 126:260–265 [DOI] [PubMed] [Google Scholar]
- 106.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. (2016) Screening for Lipid Disorders in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 316:625–633 [DOI] [PubMed] [Google Scholar]
- 107.Zachariah JP, Mcneal CJ, Copeland LA, et al. (2015) Temporal trends in lipid screening and therapy among youth from 2002 to 2012. J Clin Lipidol 9:S77–S87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.McNeal C, Zachariah J, Gregory S, Cassidy-Bushrow A, Wilson D, Tom J, VanWormer J, Wright E, Copeland L (2014) Identifying and Reducing Barriers to Improve Lipid Screening in Youth. Curr Cardiovasc Risk Rep 8:1–7 [Google Scholar]
- 109.Silverman MG, Ference BA, Im K, Wiviott SD, Giugliano RP, Grundy SM, Braunwald E, Sabatine MS (2016) Association Between Lowering LDL-C and Cardiovascular Risk Reduction Among Different Therapeutic Interventions: A Systematic Review and Meta-analysis. JAMA 316:1289–1297 [DOI] [PubMed] [Google Scholar]
- 110.Luirink IK, Wiegman A, Kusters DM, Hof MH, Groothoff JW, de Groot E, Kastelein JJP, Hutten BA (2019) 20-Year Follow-up of Statins in Children with Familial Hypercholesterolemia. N Engl J Med 381:1547–1556This article shows that initiation of statin therapy in patients with FH starting in childhood slowed measures of subclinical atherosclerosis and reduced their risk of ASCVD in adulthood.
- 111.Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, Kahn J, Afonso L, Williams KA, Flack JM (2012) Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol 60:2631–2639 [DOI] [PubMed] [Google Scholar]
- 112.Zachariah JP, Chan J, Mendelson MM, Regh T, Griggs S, Johnson PK, Desai N, Gillman M, Graham D, de Ferranti SD (2016) Adolescent Dyslipidemia and Standardized Lifestyle Modification: Benchmarking Real-World Practice. J Am Coll Cardiol 68:2122–2123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Linda Van H, Eva O, Bruce A. B, et al. (2003) A Summary of Results of the Dietary Intervention Study in Children (DISC): Lessons Learned. Prog Cardiovasc Nurs 18:28–41 [DOI] [PubMed] [Google Scholar]
- 114.Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents. :109. doi: 10.1037/amp0000530. [DOI] [PubMed] [Google Scholar]
- 115.Nordestgaard BG, Chapman MJ, Humphries SE, et al. (2013) Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J 34:3478–3490a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.EAS Familial Hypercholesterolaemia Studies Collaboration, Vallejo-Vaz AJ, De Marco M, et al. (2018) Overview of the current status of familial hypercholesterolaemia care in over 60 countries - The EAS Familial Hypercholesterolaemia Studies Collaboration (FHSC). Atherosclerosis 277:234–255This article summarizes the diagnosis and management strategies for FH across nearly 70 countries. Management varies widely with overall suboptimal diagnosis and under-treatment.
- 117.Vuorio A, Kuoppala J, Kovanen PT, Humphries SE, Tonstad S, Wiegman A, Drogari E, Ramaswami U (2017) Statins for children with familial hypercholesterolemia. Cochrane Database Syst Rev 10.1002/14651858.CD006401.pub4This systematic review assesses the effectiveness and safety of statins for the treatment of FH in children. Briefly, statins are effective with no significant safety issues.
- 118.Joyce NR, Zachariah JP, Eaton CB, Trivedi AN, Wellenius GA (2017) Statin Use and the Risk of Type 2 Diabetes Mellitus in Children and Adolescents. Acad Pediatr 17:515–522This article shows how statin use in obese children without a lipid disorder can increase their risk of developing type 2 diabetes.


