Abstract
Context:
There is a growing prevalence of cardiovascular disease (CVD) risk factors in West Africa and among its migrants to industrialized countries. Despite this, no study has reviewed CVD risk factor prevalence among West Africans in Africa and industrialized countries.
Objective:
To appraise studies on the prevalence of two CVD risk factors (hypertension and overweight/obesity) among two major West African populations (Ghanaians and Nigerians) in Africa and industrialized countries.
Methods:
A comprehensive literature search from 1996 to July 2012 was undertaken to identify quantitative studies on hypertension and overweight/obesity among adult Ghanaians and Nigerians in West Africa and industrialized countries.
Results:
Twenty studies were included with 10 conducted in Ghana, six conducted in Nigeria and four in industrialized countries. Studies in Ghana and Nigeria reported a hypertension prevalence of 19.3–54.6% with minimal differences between rural, urban, semi-urban, and mixed populations. Of the hypertensive patients, 14–73% were aware of their condition, 3–86% were on treatment, and 2–13% had controlled blood pressures. Overweight/obesity prevalence in Ghana and Nigeria ranged from 20 to 62% and 4 to 49%, respectively. The four studies in industrialized countries reported a hypertension prevalence of 8.4–55% and overweight/obesity prevalence of 65.7–90%.
Conclusion:
Hypertension and overweight/obesity are highly prevalent conditions in West Africa and in its migrants residing in industrialized countries. Urgent measures are needed to prevent CVD risk factors and halt the clinical sequelae.
Keywords: African immigrants, Ghana, hypertension, immigrants, industrialized countries, migrants, Nigeria, obesity, overweight
INTRODUCTION
Cardiovascular disease (CVD) has become the leading cause of death globally [1,2] with a high prevalence of major risk factors for CVD, including tobacco use, alcohol use, hypertension (HTN), high cholesterol, obesity, physical inactivity, and unhealthy diets. CVD is an emerging public health problem in West Africa and especially in Ghana and Nigeria where rapid epidemiological transitions have occurred [3]. These countries were selected for this systematic review because they are both English-speaking West African countries whose inhabitants exhibit similar sociodemographic characteristics, political/historical backgrounds, and have been relatively well studied.
In West Africa, HTN and overweight/obesity have emerged as important regional risk factors for CVD [4,5]. Among 79 cases of sudden cardiac deaths in Ile-Ife, Nigeria, hypertensive CVD was the cause of death in 83.5%, of which only 30.3% were previously diagnosed [6]. Similarly, a case-fatality rate of 43% was reported in 445 Nigerian hypertensive cases that presented to an urban tertiary hospital, suggesting that HTN is a major cause of morbidity [7]. HTN is also a leading cause of renal failure and heart failure in Ghana [8] and in the Greater Accra Region, HTN became the second leading cause of outpatient morbidity in 2007 [9].
Once considered a problem of wealthy nations, the WHO estimates that overweight and obesity have increased dramatically in sub-Saharan Africa (SSA) [10] and the obesity prevalence is trending upward in West Africa [11]. Obesity is also the most prevalent nutrition-related disorder in developed and developing countries [12]. These trends are worrisome as HTN and overweight/obesity are associated with increased morbidity and mortality, and pose a large disease burden for numerous noncommunicable diseases [13–15]. Further, the concurrent prevalence of obesity and malnutrition in West African countries result in an even greater disease burden and pose unique challenges for these settings [16].
Rates of CVD and risk factors among some ethnic groups increase following migration to countries where CVD rates are high, which indicates a substantial environmental influence [17]. There are growing West African populations in industrialized regions [18]. An estimated two to three million people from SSA reside in the European Union [19] and 1.1 million reside in the United States [20]. Although limited, available data suggest that African immigrants in these regions bear a disproportionate burden of CVD and CVD risk factors [21–25].
The purpose of this systematic review, therefore, was to critically appraise existing studies on the prevalence of two major CVD risk factors: HTN and overweight/obesity in two West African populations (Ghanaians and Nigerians) residing in Africa and in industrialized countries.
METHODS
Search strategy for identification of studies
Searches were undertaken using the PUBMED electronic database to identify population-based quantitative studies on HTN and overweight/obesity in adult Ghanaians and Nigerians in Africa, Europe, and North America using relevant diagnostic criteria [26–28]. Articles were included in this review if they were published in English between 1996 and June 2012. To enhance the comprehensiveness of the search, both subject headings and free text searches were implemented. Subsequently, reference lists of relevant identified articles were examined to retrieve other studies that were not indexed by PUBMED. The keywords and medical subject headings (MeSHs) used in the development of the search strategy included Ghana, Nigeria, African immigrants, HTN, high blood pressure (BP), overweight, obesity, risk factors, prevalence, and BMI. All MeSH words and keywords were truncated and exploded to capture as many articles as possible.
Study selection and data extraction
The titles and abstracts of the articles were screened and retrieved from the multiple sources described above. Articles were included if they reported on original prevalence (crude or adjusted), and contained epidemiological data on HTN and overweight/obesity. The full texts of potentially relevant articles were examined on the inclusion criteria and for methodological soundness. No pooled analysis was performed due to the heterogeneity of study populations. Figure 1 [29] is the flow chart of study selection and extraction.
FIGURE 1.
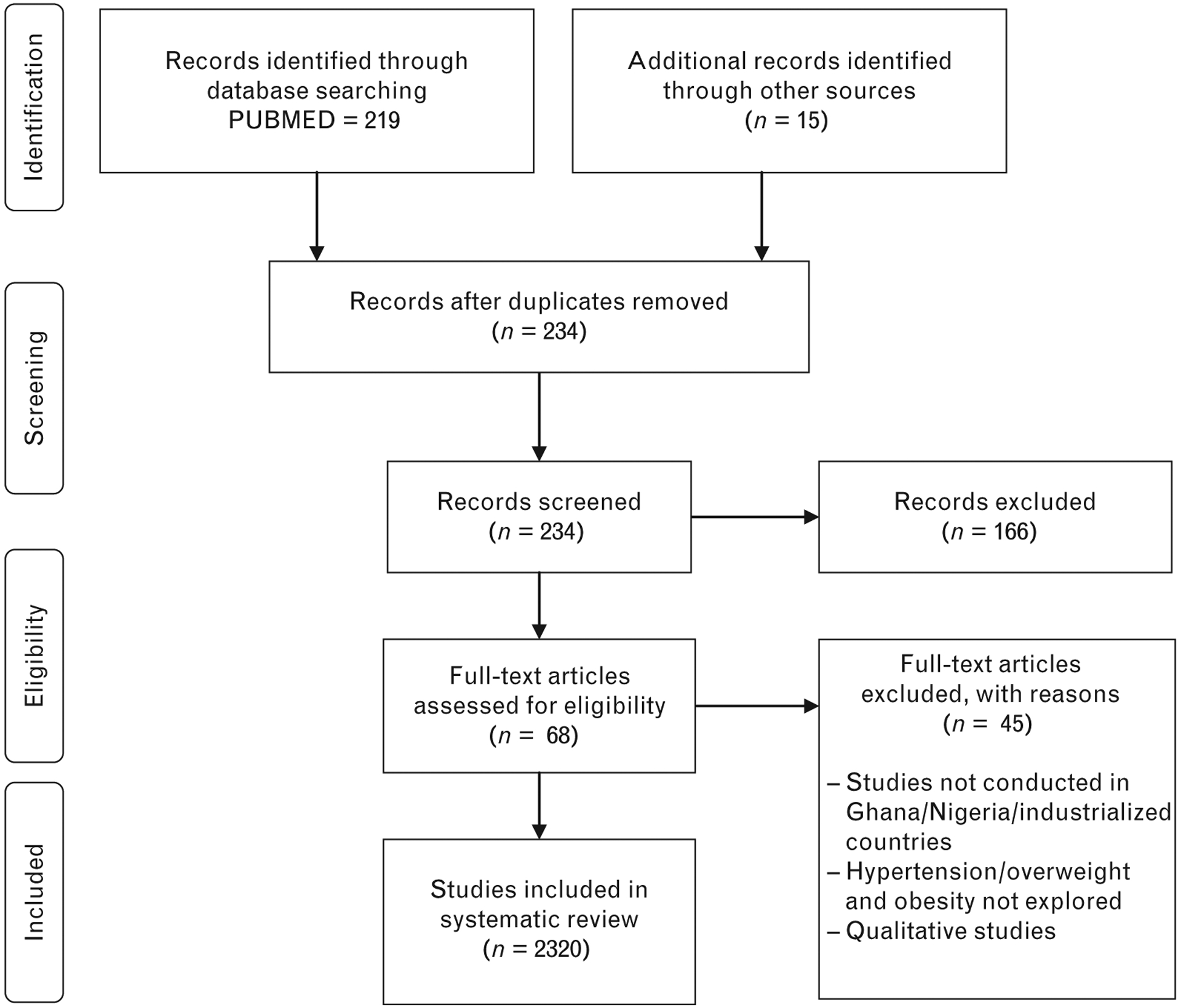
Study selection and data extraction. Adapted from [29].
RESULTS
Description of studies
Twenty (20) independent studies were included in this review, with 10 studies [30–38] conducted in Ghana, six studies [39–44] conducted in Nigeria, and four studies [45–48] conducted in industrialized countries. No epidemiological studies on HTN and overweight/obesity in Ghanaian or Nigerian immigrants in North America were reported. The majority of studies conducted in Africa were population-based and cross-sectional studies. All the four studies conducted in industrialized countries were cross-sectional. Sample sizes of the studies ranged from 85 to 4733 in Africa and 45 to 1471 in industrialized countries.
Hypertension in Ghanaians and Nigerians residing in Africa
HTN was defined using Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC −7) criteria [26] of SBP at least 140 mmHg and/or DBP at least 90 mmHg or as individuals being on antihypertensive medication. Notably, some studies also considered individuals who self-reported a prior diagnosis of HTN as hypertensive participants [30–32]. Three studies [34,36,37] restricted their diagnosis of HTN to only one BP measurement. Mean age of participants ranged from 31.6 to 46.8 years in both countries.
Studies in Ghana and Nigeria reported a crude prevalence of HTN between 19.3 and 54.6% (Table 1) [30–32, 33–43,44,49]. The study by Kunutsor and Powles [37], which reported the lowest crude prevalence rate in a rural Ghanaian population, and the study by Duda et al. [36], which reported the highest crude prevalence among urban Ghanaian women, both only obtained one BP measurement and neither reported adjusted prevalence rates. Notably, only two studies [31,32] adjusted the HTN prevalence rates to the world standard population. Studies in Nigeria reported a crude HTN prevalence between 20.8 [42] and 36.6% [39], whereas their counterparts in Ghana reported a crude prevalence between 19.3 [37] and 54.6% [36]. Minimal differences in HTN prevalence rates were noted between rural, urban, semi-urban, and mixed populations in both countries. In two of the four rural populations, the HTN prevalence was 25% or higher [30,34]. In all six urban populations, the HTN prevalence was 27% or higher. Where reported, there were sex differences in HTN prevalence rates, although no clear pattern was noted (see Table 1). Six [34,35,41–43,49] of the 11 studies that analyzed rates by sex reported a higher HTN prevalence in men compared with women.
TABLE 1.
Cross-sectional studies of hypertension in [A] Ghanaians and [B] Nigerians in Africa
| Author name | Population type, city | (n) | HTN prevalence (Unadjusted, adjusted†) | Hypertension | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sampling method | Study period | Mean age ± SD years | (M) | (F) | (Total) | Awareness % (nA/x)* | Treatment % (nT/x)* | Control % (nc/x)* | Control % (nc/nT)Δ |
|||
| [A] Ghana | ||||||||||||
| Amoah [32] | Urban (Accra) | 4733 | Random cluster | 1998 | 44.3 ± 14.7 | -, 27.6† | -, 29.5† | 28.3 28.4† | 34 (458/1337) | 18 (243/1337) | 3.7 (49/1337) | 20.2 (49/243) |
| Cappuccio et al. [35] | Mixed (Ashanti) | 1013 | Stratified random | 2001–2002 | 54.7 ± 11.3 | 29.9 | 28.0 | 28.7 | 22.0 (64/291) | 11.3 (33/291) | 2.8 (8/291) | 24.2 (8/33) |
| Burket [34] | Rural (Volta region) | 287 | Convenience | 2002 | 41.8 | 39.4 | 30.7 | 32.8 | 18.9 | - | - | |
| Spencer et al. [38] | Semi-urban | 343 | Convenience | 2002–2003 | 48 | 28.7 | 30.7 | 30 | 73 (250/343) | 43 (148/343) | 3.6 (12/343) | - |
| Addo et al. [30] | Rural (Accra) | 362 | Convenience | - | 42.4 ± 18.6 | 24.1 | 25.9 | 25.7 | 32.3 (30/93) | 12.9 (12/93) | 2.2 (2/93) | 16.7 (2/12) |
| Duda et al. [36] | Urban women (Accra) | 1328 | 2-stage Cluster Stratified Random | 2003 | 46.8 ± 18.0 | N/A | 54.6 | 54.6 | 23.7 (309/1328) | 52.4 (162/309) | 2.3 (7/309) | 4.3 (7/162) |
| Agyemang [49] | Mixed (Kumasi) | 1431 | Random | 2004 | 35.9 ± 0.16 | Rural-27 Urban-33.4 |
Rural-27 Urban-28.9 |
29.4 | 34 (486/1431) | 28 (401/1431) | 6.2 (89/1431) | 12.2 (49/401) |
| Addo et al. [31] | Urban (Accra) | 1015 | Random | 2006 | 44.0 ± 10.1 | 31. 7 | 28 | 30.3 27.4† | 54.1 (166/307) | 31.3 (96/166) | 12.7 (39/307) | 40.4 (39/96) |
| Kunutsorand Powles [37] | Rural (North) | 574 | Random | 2007 | 37.75 ± 14.05 | - | - | 19.3 | - | - | - | - |
| [B] Nigeria | ||||||||||||
| Oladapo et al. [42] | Rural (Egbeba) | 2000 | Systematic Random | 2002–2005 | 42.1 ± 21.6 | 21.1 | 20.5 | 20.8 | 14.2 (59/415) | 2.6 (11/415) | - | - |
| Ekore et al. [40] | Urban (Ibadan) | 405 | Convenience | 2007 | 31.6 ± 6.9 | 34.4 | 28.3 | 30.6 | - | - | - | - |
| Adedoyin et al. [39] | Semi-urban (Ile-Ife) | 2097 | Multistage Cluster | - | 44.2 ± 11.6 | 36.8 | 34.7 | 36.6 | - | - | - | - |
| Oghagbon et al. [43] | Urban (Ilorin) | 281 | Convenience | - | 40.34 ±9.58 | 29.0 | 22.9 | 27.1 | - | - | - | - |
| Ulasi et al. [44] | Mixed (Enugu) | 1458 | Stratified random | - | 43.8 ± 13.7 | - | - | 32.8 | - | 18.9 (11.5/59) | - | - |
| Isezuo et al. [41] | Mixed (Sokoto) | 782 | Multistage Cluster | - | 38.9 ± 13.9 | 25.9 | 23.6 | 24.8 | 13.9 (27/194) | 85.7 (23/27) | 12.5 (2.9/23) | - |
‘–’, Results not reported;
, Age-adjusted to world standard population;
, Control rate calculated with the number of hypertensive patients (x) as the denominator, and the numerator (nA) is the number of those participants who were aware of their hypertension; nT is the number treated with antihypertensive medication; nC is the number who had their blood pressure controlled to 140/90mmHg;
, Control rate calculated with the number treated with antihypertensive medication (nT) as the denominator; Mixed, Rural+Urban/Semi-urban+Rural Population.
Detailed analyses of the awareness, treatment, and control of HTN were available for only eight studies conducted in Africa. Of the hypertensive patients, 14–73% were aware of their condition, 3–86% were on treatment, and 2–13% had controlled BPs less than 140/90 mmHg according to the JNC-7 criteria [26]. The highest awareness, treatment, and control rates were observed among urban civil servants in Accra, Ghana [31] and semi-urban participants in Sekondi-Takoradi, Ghana [38] with awareness, treatment, and control rates of 54.1, 31.3, and 12.7 and 73, 59, and 5%, respectively. The worst was observed in a mixed population-based sample of semi-urban and rural participants in the Ashanti region, Ghana where detection, treatment, and control rates were significantly higher in semi-urban (25.7, 14.3, and 3.4%) than in rural villages (16.4, 6.9, and 1.7%) [35]. Generally, women had higher awareness, treatment, and control rates than men [31,35,42,49]. Differences in study populations hinder further analysis of other trends in awareness, treatment, and control.
Overweight/obesity in Ghanaians and Nigerians residing in Africa
All studies except one [43] in this review utilized international criteria for BMI classification [28,50], with normal weight defined as a BMI of 18.5–24.9 kg/m2, overweight 25–29.9, and obesity as at least 30 kg/m2. The study by Oghagbon et al. [43] differed by categorizing normal weight as BMI of 20–24.9 kg/m2.
The overall prevalence of overweight and obesity ranged from 20 to 62% and 4 to 49%, respectively (see Table 2) [30,31,33–37,40–44,49,51]. Although two of the three rural studies had lower rates of overweight and obesity compared with urban and mixed population, Burket’s study [34] was the exception, in which about 44% of the population was found to be overweight or obese. However, a potential selection bias of women (77%) at the market limits the generalizability of the findings. In general, urban studies reported a higher prevalence of overweight or obesity with rates as high as 62%, observed in urban women in the Women’s Health Study of Accra. The lowest rate of overweight or obesity (3.9%) [43] was observed in rural Egbegba, Nigeria; however, 60.9% of this population was underweight. This difference in prevalence of overweight or obesity is also reflected in the average BMIs of urban and rural populations in Table 2. Five studies [31,34,41,49,52] did not report BMI status by sex. In all studies in which BMI status was reported by sex, women had a higher prevalence of overweight or obesity. This sex disparity in prevalence of overweight or obesity corroborates the findings of systematic review by Abubakari and Bhopal [53]. In all urban studies [31,51], obesity was approximately four times higher in women than men with the exception of study by Duda et al. [36], which excluded men. The prevalence of overweight or obesity was higher in Ghanaians (range of 21.1–62.3%), compared with Nigerians (range of 3.9–49%). Given the frequent concurrence of overweight/obesity and HTN, it is no coincidence that the prevalence of overweight/obesity and HTN are high in majority of the studies that addressed both risk factors as illustrated in Fig. 2.
TABLE 2.
Cross-sectional studies on overweight/obesity in Ghanaians and Nigerians residing in Africa
| First author, year | Population type, area | (n) | Sampling method | Study period | Mean age ± SD/mean age (95% Cl) All | BMI (kg/m2) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| %Normal (18.5–24.9) | % Overweight (25.0–29.9) | %Obese ≥30.0 | Mean ±SD | ||||||||||||||
| M | F | All | M | F | All | M | F | All | M | F | All | ||||||
| [A] Ghana | |||||||||||||||||
| Amoah [51] | Urban (Accra) | 4733 | Random cluster | 1998 | 44.3 ± 14.7 | 68.5 | 46.1 | 54.9 | 17.5 | 27.1 | 23.4 | 4.6 | 20.2 | 14.1 13.6† | 22.6 ± 0.1 | 25.6 ± 0.1 | 24.4 ± 0.1 |
| Cappuccio et al. [35] | Mixed (Ashanti) | 1013 | Stratified random | 2001–2002 | 54.7 ± 11.3 | - | - | - | - | - | - | - | - | - | 20.2 ± 3.1 | 21.1 ± 4.6 | 21.1 ± 4.2 |
| Burket [34] | Rural (Volta) | 287 | Convenience | 2002 | 41.8 | - | - | - | - | - | 25.5 | - | - | 9.1 | - | - | 24.0 |
| Biritwum et al. [33] | Mixed | 4231 | Random | 2003 | - | 69 | 60.9 | 64.6 | 13.7 | 17.3 | 15.6 | 2.8 | 7.9 | 5.5 | - | - | - |
| Addo et al. [30] | Rural (Accra) | 362 | Convenience | - | 42.4 ± 18.6 | - | - | 74 | - | - | 15.7 | - | - | 10.2 | 21.5 ± 2.8 | 23.9 ± 5.4 | 23.2 ± 4.9 |
| Duda et al. [36] | Urban | 1328 | 2-stage Cluster Stratified Random | 2003 | 46.8 ± 18.0 | N/A | 29.9 | 29.9 | N/A | 27.7 | 27.7 | - | 34.6 | 34.6 | N/A | - | - |
| Agyemang [49] | Mixed (Kumasi) | 1431 | Random | 2004 | 35.9 ± 0.2 | 85.9 | 75.1 | 79.9 | 12.3 | 13.3 | 12.9 | 1.9 | 11.6 | 7.2 | 22.0 | 24.0 | 23.1 ± 0.04 |
| Addo et al. [31] | Urban (Accra) | 1015 | Random | 2006 | 44.0 ± 10.1 | 52 | 27 | 42.2 | 34 | 34 | 34 | 9.9 | 35.5 | 20 | 24.7 ± 4.3 | 28.2 ± 5.8 | 26.1 ± 5.8 |
| Kunutsorand Powles [37] | Rural (North) | 574 | Random | 2007 | 37.8 ± 14.1 | - | - | - | - | - | - | - | - | - | 21.1 ± 2.3 | 22.2 ± 3.4 | 21.8 ± 3.1 |
| [B] Nigeria | |||||||||||||||||
| Oladapo et al. [42] | Rural (Egbeba) | 2000 | Systematic Random | 2002–2005 | 42.1 ± 21.6 | 32.4 | 37.4 | 35.2 | 1.9 | 1.8 | 1.9 | 1.5 | 2.4 | 2.0 | 22.8 ± 7.9 | 25.6 ± 11.3 | - |
| Ekore et al. [40] | Urban (Ibadan) | 405 | Convenience | 2007 | 31.6 ± 6.9 | - | - | - | - | - | 22.5 | - | - | 8.6 | - | - | 23.7 ±4.3 |
| Oghagbon et al. [43] | Urban (Ilorin) | 281 | Convenience | - | 40.3 ± 9.6 | 71** | 38.6 | 62.9 | 21.9 | 30 | 23.9 | 7.1 | 31.4 | 13.21 | 24.3 ± 4.9 | 24.6 ± 4.5 | 24.4 ± 4.8 |
| Ulasi et al. [44] | Mixed (Enugu) | 1458 | Stratified random | - | 43.8 ± 13.7 | - | - | - | - | - | 31.6 | - | - | 17.3 | - | - | 23.7 ± 4.3 |
| Isezuo et al. [41] | Mixed | 782 | Multistage Cluster | - | 38.9 ± 13.9 | - | - | - | - | - | - | 2.0 | 5.9 | 4.3 | 22.8 ± 3.6 | 23.2 ± 4.0 | 23.0 ± 3.8 |
CI, confidence interval. ‘-’ Results not reported;
, Adjusted to world standard population; N/A, not applicable; -, not reported;
Normal BMI classified as 20–24.9 kg/m2; Mixed, Rural+Urban/Semi-urban+Rural Population.
FIGURE 2.
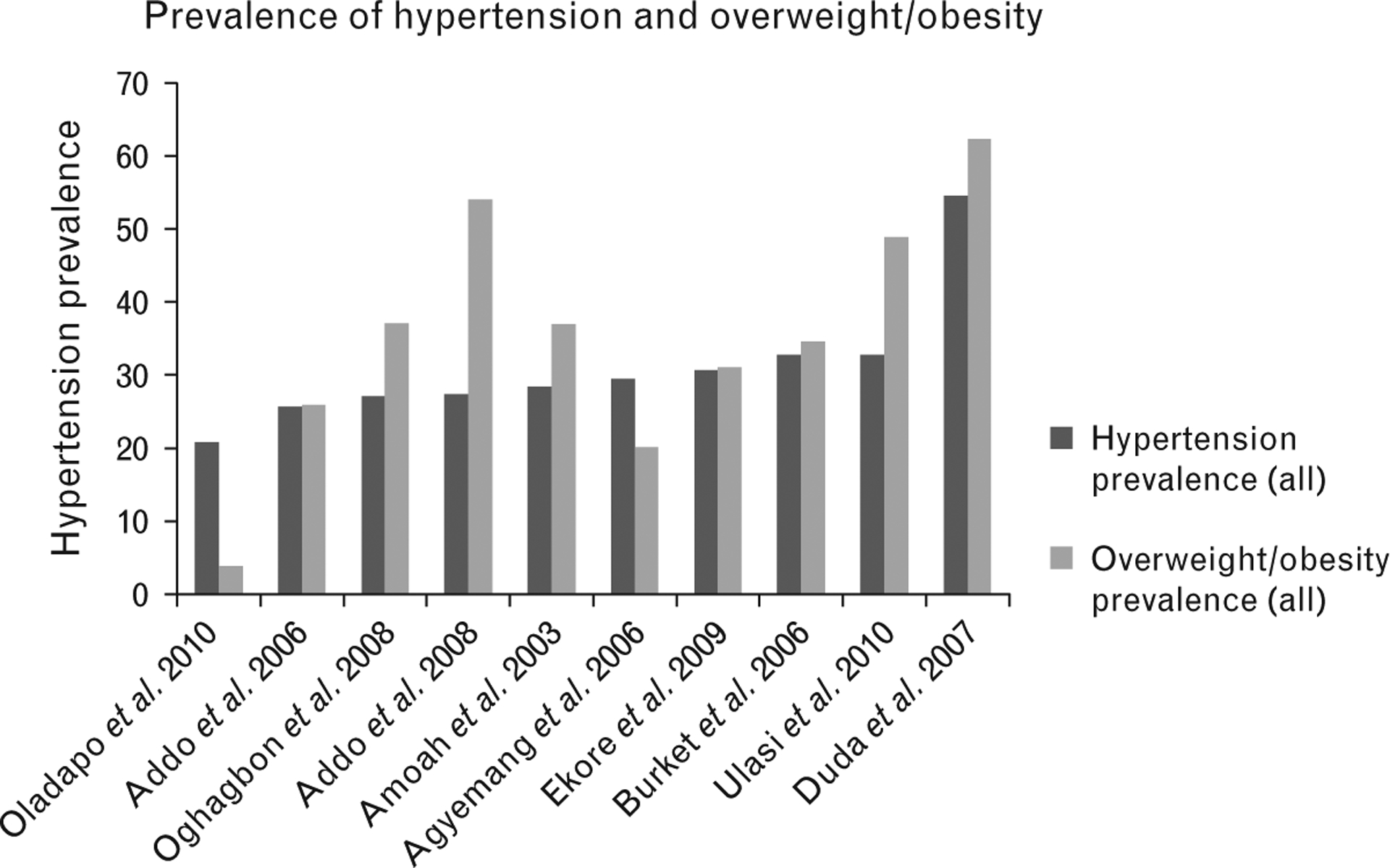
Bar chart of studies that examined the prevalence of hypertension and overweight/obesity.
Hypertension and overweight/obesity in Ghanaians and Nigerians residing in industrialized countries
There were four studies conducted in industrialized countries that addressed HTN and overweight/obesity in Ghanaians and Nigerians with the results presented in Table 3 [45–48]. Two studies were conducted in the Netherlands, whereas the other two were conducted in Italy and Australia. Sample sizes ranged from 45 to 1471. The prevalence of HTN in Ghanaians and Nigerians residing in industrialized countries ranged from 8.4 to 55%. Only study by Agyemang et al. [48] examined the awareness, treatment, and control of HTN and reported rates of 50, 45, and 33%, respectively.
TABLE 3.
Studies addressing hypertension and overweight/obesity in [A] Ghanaians and [B] Nigerians in industrialized countries
| Author name, design | Population type | (n) | Design | CVD risk factor | Results |
|---|---|---|---|---|---|
| Agyemang et al. [45] Netherlands, Ghana | Dutch-Ghanaians, rural & urban Ghanaians | 1471 | Cross-sectional | Overweight/obesity | Overweight/Obesity prevalence: 69.1% (M), 79.5% (F) in Dutch-Ghanaians which was significantly higher than urban Ghanaians: 22.0% (M), 50.0% (F) and rural Ghanaians: 10.3% (M), 19.0% (F) |
| Dominguez et al. [46] Italy | African immigrants (Ghanaians, Nigerians, Ivorians) | 83 | Cross-sectional | HTN, CVD risk profiles | HTN prevalence: 8.4%, HTN treatment: 0%. Obesity prevalence: 2.2% and significant correlations b/n duration in Italy and weight (P <0.001), BMI (P<0.0001), SBP (P<0.01), & DBP (P<0.05) |
| Saleh et al. [47] Australia | Ghanaian immigrants | 45 | Cross-sectional | HTN, overweight/obesity | HTN prevalence: 40% (M), 17% (F), HTN awareness 29%, Overweight/obesity prevalence: 71% (M), 65.7% (F), 63% participants had one or more metabolic risk factors. |
| Agyemang et al. [48] Netherlands | Ghanaian immigrants | 221 | Cross-sectional | HTN, overweight, obesity, diabetes, smoking, physical activity | HTN prevalence: 55%, HTN awareness: 50%, HTN treatment: 45%, HTN control: 33%, overweight/obesity prevalence: 90% |
CVD, cardiovascular disease; HTN, hypertension.
DISCUSSION
Compared with the earliest epidemiological studies in Ghana and Nigeria, which revealed a low prevalence of CVD and associated risk factors [54], this systematic review found a high prevalence of HTN and overweight/obesity in the two countries, as foretold by Pobee et al. [55] in 1979. Also, this review shows that HTN and overweight/obesity are significant problems even in the poorest rural populations [30,34,40,42]. In a relatively young sample with a mean age of 31 years, a crude HTN prevalence of 30.6% [40] was observed. This finding is particularly concerning, considering the fact that an HTN prevalence of 33.5% has been reported in the United States in adults at least 20 years of age [21], but Ghana and Nigeria are more resource-limited settings. Further, rates of HTN in West African samples, regardless of setting and sample, are comparable to, or higher than the estimated global prevalence rate of 26.4% [56]. These findings should dispel the myth that HTN is only a problem for the wealthy and elderly.
Although Ghanaians have the highest prevalence of fruit and vegetable consumption in comparison to 52 other countries internationally [50], the prevalence of overweight/obesity is high in this review. The prevalence of overweight/obesity in urban women across studies is alarming. Although lower than the prevalence of 80% in African–American women [57], it still has profound public health implications in developing countries, where resources are scarce and malnutrition remains a public health concern [16]. This may be attributed to low physical activity, as epidemiological studies have shown that Ghanaians and Nigerians do not engage in regular physical activity [33,42,52], or to other dietary factors, as Ghanaians and Nigerians consume dietary salt exceeding recommended limits [37]. Several clinical trials have established that interventions to increase physical activity and reduce dietary sodium [58–60] lower BP, and may reduce CVD risk. However, to enhance the effectiveness of these interventions in Ghana and Nigeria, tailoring to the specific population social, economic and cultural context must be considered.
Although considerable progress has been made toward HTN control in western countries, this review shows that West Africa is lagging behind. In comparison to the United States, where awareness, treatment, and control rates of 80.7, 72.5, and 50.1%, respectively, were reported in 2008 [61], the highest corresponding rates were 54.1, 31.3, and 12.7% [32] in Ghanaians. Possible reasons for the poor treatment and control rates include the high cost of medications [62], absence of national treatment guidelines [5], and misconceptions about HTN [38]. There is an urgent need to improve awareness, treatment, and control of HTN in these two countries to curb the looming epidemic of CVD.
The high prevalence of overweight/obesity in Dutch-Ghanaians (90%) in study by Agyemang et al. [48] reviewed deserves great attention and is comparatively higher than rates reported in the United States [57]. Saleh et al. [47] reported similar findings in Australian-Ghanaians where 89% of men and 92% of women were overweight or obese. Although the sample size of 45 in the latter study is small, the findings are equally disturbing. These two studies provide the closest estimate of what can be expected in the Ghanaian and Nigerian immigrants in North America. In West Africa, there is a positive social perception about overweight/obesity, as they are taken to mean signs of ‘good living’ and are associated with wealth, feminine beauty, and freedom from HIV/AIDS [63,64]. This perception could reinforce unhealthy lifestyles that lead to overweight/obesity in African immigrants. It is well known that 75% of the incidence of HTN is related directly to obesity [65]. It is, therefore, important to develop effective treatment strategies for the management of overweight/obesity in order to reduce the occurrence of obesity-related HTN.
No US-based studies were included in this review because African immigrants are often lumped into one racial/ethnic category and classified as ‘blacks’ [66,67], which may include African immigrants, and Afro-Caribbean immigrants. The lack of epidemiological data on CVD risk factors such as HTN and obesity in the recently immigrated West African population residing in the United States limits healthcare providers and policy makers’ abilities to address CVD prevention and management of CVD in this rapidly growing population.
Limitations and implications of findings for future research
The small number of high-quality, large-scale and comparable studies made this review difficult. Establishing a clear link between temporal trends and increasing prevalence of HTN and overweight/obesity was not possible, although the data suggest that the prevalence rates of HTN and overweight/obesity are high. The absence of sex and age-specific estimates limited interpretation and comparison of the data. There is an urgent need for cross-sectional studies on CVD risk factors in African immigrants to the USA and other industrialized countries. Studies should report world-standardized prevalence rates to permit comparisons between age groups, sexes, areas, and time points globally. Furthermore, studies should build on strengths of previous studies including the use of representative samples and large sample sizes. Longitudinal studies of Ghanaian and Nigerian immigrants starting from the time of migration to industrialized nations may adequately characterize the environmental factors that may contribute to the development or progression of CVD risk factors.
In conclusion, this review has demonstrated a high prevalence of HTN and overweight/obesity in both urban and rural areas of Ghana and Nigeria. The awareness, treatment, and effective control of HTN in these two countries are unacceptably low. Improving the awareness, treatment, and control of HTN in these two West African countries is critical in reducing and preventing morbidity and mortality from CVD. Overweight and obesity are highly prevalent conditions in Ghanaians and Nigerians residing in West Africa and even greater in their counterparts residing in industrialized countries. The factors that contribute to this phenomenon need to be further explored in future studies. Ghanaians and Nigerians residing in West Africa may have a high risk of CVD due to the high prevalence and poor management of HTN and overweight/obesity and this risk may further deteriorate upon migration to industrialized countries. Future longitudinal studies will improve our understanding of the evolution of CVD risk in persons who migrate from West African countries to industrialized countries.
Abbreviations:
- BP
blood pressure
- CVDs
cardiovascular diseases
- HTN
hypertension
- MeSH
medical subject headings
- Mixed
Rural+Urban/Semi-urban+ Rural Population
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mathers CD, Lopez AD, Murray CJL. The burden of disease and mortality by condition: data, methods, and results for 2001 In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global burden of disease and risk factors. Washington (DC): The International Bank for Reconstruction and Development/The World Bank Group; 2006. [PubMed] [Google Scholar]
- 2.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001; 104:2746–2753. [DOI] [PubMed] [Google Scholar]
- 3.Agyei-Mensah S, de-Graft Aikins A. Epidemiological transition and the double burden of disease in Accra, Ghana. J Urban Health 2010; 87:879–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kadiri S Tackling cardiovascular disease in Africa. BMJ 2005; 331:711–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper RS, Amoah AG, Mensah GA. High blood pressure: the foundation for epidemic cardiovascular disease in African populations. Ethn Dis 2003; 13:S48–S52. [PubMed] [Google Scholar]
- 6.Rotimi O, Fatusi AO, Odesanmi WO. Sudden cardiac death in Nigerians: the Ile-Ife experience. West Afr J Med 2004; 23:27–31. [DOI] [PubMed] [Google Scholar]
- 7.Arodiwe EB, Ike SO, Nwokediuko SC. Case fatality among hypertension-related admissions in Enugu, Nigeria. Niger J Clin Pract 2009; 12:153–156. [PubMed] [Google Scholar]
- 8.Plange-Rhule J, Phillips R, Acheampong JW, Saggar-Malik AK, Cappuccio FP, Eastwood JB. Hypertension and renal failure in Kumasi, Ghana. J Hum Hypertens 1999; 13:37–40. [DOI] [PubMed] [Google Scholar]
- 9.Greater Accra Regional Health Directorate. Greater Accra Regional Health Directorate: Annual Report 2007 In: Ghana Health Service, editor. Accra: Greater Accra Regional Health Directorate; 2007. [Google Scholar]
- 10.Guilbert JJ. The World Health Report 2006: working together for health. Educ Health (Abingdon) 2006; 19:385–387. [DOI] [PubMed] [Google Scholar]
- 11.Abubakari AR, Lauder W, Jones MC, Kirk A, Agyemang C, Bhopal RS. Prevalence and time trends in diabetes and physical inactivity among adult West African populations: the epidemic has arrived. Public Health 2009; 123:602–614. [DOI] [PubMed] [Google Scholar]
- 12.Bray GA. Obesity: a time bomb to be defused. Lancet 1998; 352:160–161. [DOI] [PubMed] [Google Scholar]
- 13.Visscher TL, Seidell JC. The public health impact of obesity. Annu Rev Public Health 2001; 22:355–375. [DOI] [PubMed] [Google Scholar]
- 14.Folsom AR, Burke GL, Byers CL, Hutchinson RG, Heiss G, Flack JM, et al. Implications of obesity for cardiovascular disease in blacks: the CARDIA and ARIC studies. Am J Clin Nutr 1991; 53:1604S–1611S. [DOI] [PubMed] [Google Scholar]
- 15.Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Med Sci Sports Exerc 1999; 31:S646–S662. [DOI] [PubMed] [Google Scholar]
- 16.Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol 2006; 35:93–99. [DOI] [PubMed] [Google Scholar]
- 17.Polednak A Racial and ethnic differences in disease. New York: NY: Oxford University Press; 1989. [Google Scholar]
- 18.Terrazas A African Immigrants in the United States. Migration Information Source; 2009.
- 19.Organization for Economic Cooperation and Development. Table A.1.1. Inflows of Foreign Population into Selected OECD Countries OECD 2006.
- 20.Capps R, McCabe K, Fix M. New streams: black African migration to the United States. Migration Policy Institute; 2011. [Google Scholar]
- 21.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics - 2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu X, Liu M, Tsilimingras D, Schiffrin EL. Racial disparities in cardiovascular risk factors among diagnosed hypertensive subjects. J Am Soc Hypertens 2011; 5:239–248. [DOI] [PubMed] [Google Scholar]
- 23.Cappuccio FP. Ethnicity and cardiovascular risk: variations in people of African ancestry and South Asian origin. J Hum Hypertens 1997; 11: 571–576. [DOI] [PubMed] [Google Scholar]
- 24.Kaufman JS, Owoaje EE, James SA, Rotimi CN, Cooper RS. Determinants of hypertension in West Africa: contribution of anthropometric and dietary factors to urban-rural and socioeconomic gradients. Am J Epidemiol 1996; 143:1203–1218. [DOI] [PubMed] [Google Scholar]
- 25.Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S, et al. The prevalence of hypertension in seven populations of west African origin. Am J Public Health 1997; 87:160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 27.Whitworth JA, World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003; 21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 28.Anonymous Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854:1–452. [PubMed] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, Group PRISMA. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 30.Addo J, Amoah AG, Koram KA. The changing patterns of hypertension in Ghana: a study of four rural communities in the Ga District. Ethn Dis 2006; 16:894–899. [PubMed] [Google Scholar]
- 31.Addo J, Smeeth L, Leon DA. Prevalence, detection, management, and control of hypertension in Ghanaian civil servants. Ethn Dis 2008; 18:505–511. [PubMed] [Google Scholar]
- 32.Amoah AG. Hypertension in Ghana: a cross-sectional community prevalence study in greater Accra. Ethn Dis 2003; 13:310–315. [PubMed] [Google Scholar]
- 33.Biritwum R, Gyapong J, Mensah G. The epidemiology of obesity in Ghana. Ghana Med J 2005; 39:82–85. [PMC free article] [PubMed] [Google Scholar]
- 34.Burket BA. Blood pressure survey in two communities in the Volta region, Ghana, West Africa. Ethn Dis 2006; 16:292–294. [PubMed] [Google Scholar]
- 35.Cappuccio FP, Micah FB, Emmett L, Kerry SM, Antwi S, Martin-Peprah R, et al. Prevalence, detection, management, and control of hypertension in Ashanti, West Africa. Hypertension 2004; 43:1017–1022. [DOI] [PubMed] [Google Scholar]
- 36.Duda RB, Kim MP, Darko R, Adanu RM, Seffah J, Anarfi JK, Hill AG. Results of the Women’s Health Study of Accra: assessment of blood pressure in urban women. Int J Cardiol 2007; 117:115–122. [DOI] [PubMed] [Google Scholar]
- 37.Kunutsor S, Powles J. Descriptive epidemiology of blood pressure in a rural adult population in Northern Ghana. Rural Remote Health 2009; 9:1095. [PubMed] [Google Scholar]
- 38.Spencer J, Phillips E, Ogedegbe G. Knowledge, attitudes, beliefs, and blood pressure control in a community-based sample in Ghana. Ethn Dis 2005; 15:748–752. [PubMed] [Google Scholar]
- 39.Adedoyin RA, Mbada CE, Balogun MO, Martins T, Adebayo RA, Akintomide A, Akinwusi PO. Prevalence and pattern of hypertension in a semiurban community in Nigeria. Eur J Cardiovasc Prev Rehabil 2008; 15:683–687. [DOI] [PubMed] [Google Scholar]
- 40.Ekore RI, Ajayi IO, Arije A. Case finding for hypertension in young adult patients attending a missionary hospital in Nigeria. Afr Health Sci 2009; 9:193–199. [PMC free article] [PubMed] [Google Scholar]
- 41.Isezuo SA, Sabir AA, Ohwovorilole AE, Fasanmade OA. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in northern Nigeria. J Hum Hypertens 2011; 25:224–230. [DOI] [PubMed] [Google Scholar]
- 42.Oladapo OO, Salako L, Sodiq O, Shoyinka K, Adedapo K, Falase AO. A prevalence of cardiometabolic risk factors among a rural Yoruba south-western Nigerian population: a population-based survey. Cardiovasc J Afr 2010; 21:26–31. [PMC free article] [PubMed] [Google Scholar]
- 43.Oghagbon EK, Okesina AB, Biliaminu SA. Prevalence of hypertension and associated variables in paid workers in Ilorin, Nigeria. Niger J Clin Pract 2008; 11:342–346. [PubMed] [Google Scholar]
- 44.Ulasi II, Ijoma CK, Onodugo OD. A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res 2010; 10:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Agyemang C, Owusu-Dabo E, de Jonge A, Martins D, Ogedegbe G, Stronks K. Overweight and obesity among Ghanaian residents in The Netherlands: how do they weigh against their urban and rural counterparts in Ghana? Public Health Nutr 2009; 12:909–916. [DOI] [PubMed] [Google Scholar]
- 46.Dominguez LJ, Galioto A, Pineo A, Ferlisi A, Vernuccio L, Belvedere M, et al. Blood pressure and cardiovascular risk profiles of Africans who migrate to a western country. Ethn Dis 2008; 18:512–518. [PubMed] [Google Scholar]
- 47.Saleh A, Amanatidis S, Samman S. Cross-sectional study of diet and risk factors for metabolic diseases in a Ghanaian population in Sydney, Australia. Asia Pac J Clin Nutr 2002; 11:210–216. [DOI] [PubMed] [Google Scholar]
- 48.Agyemang C, Nicolaou M, Boateng L, Dijkshoorn H, van de Born BJ, Stronks K. Prevalence, awareness, treatment, and control of hypertension among Ghanaian population in Amsterdam, the Netherlands: the GHAIA study. Eur J Prev Cardiol 2012; 20:938–946. [DOI] [PubMed] [Google Scholar]
- 49.Rural Agyemang C. and urban differences in blood pressure and hypertension in Ghana, West Africa. Public Health 2006; 120: 525–533. [DOI] [PubMed] [Google Scholar]
- 50.Hall JN, Moore S, Harper SB, Lynch JW. Global variability in fruit and vegetable consumption. Am J Prev Med 2009; 36:402–409; e5. [DOI] [PubMed] [Google Scholar]
- 51.Amoah AG. Obesity in adult residents of Accra, Ghana. Ethn Dis 2003; 13:S97–S101. [PubMed] [Google Scholar]
- 52.Ike SO, Aniebue PN, Aniebue UU. Knowledge, perceptions and practices of lifestyle-modification measures among adult hypertensives in Nigeria. Trans R Soc Trop Med Hyg 2010; 104:55–60. [DOI] [PubMed] [Google Scholar]
- 53.Abubakari AR, Bhopal RS. Systematic review on the prevalence of diabetes, overweight/obesity and physical inactivity in Ghanaians and Nigerians. Public Health 2008; 122:173–182. [DOI] [PubMed] [Google Scholar]
- 54.Colbourne MJ, Edington GM, Hughes MH, Ward-Brew A. A medical survey in a Gold Coast village. Trans R Soc Trop Med Hyg 1950; 44:271–290. [DOI] [PubMed] [Google Scholar]
- 55.Pobee JO, Larbi EB, Dodu SR, Pisa Z, Strasser T. Is systemic hypertension a problem in Ghana? Trop Doct 1979; 9:89–92. [DOI] [PubMed] [Google Scholar]
- 56.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365:217–223. [DOI] [PubMed] [Google Scholar]
- 57.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012; 307:491–497. [DOI] [PubMed] [Google Scholar]
- 58.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003; 289:2083–2093. [DOI] [PubMed] [Google Scholar]
- 59.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER trial. Circulation 2009; 119:2026–2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Charlton KE, Steyn K, Levitt NS, Peer N, Jonathan D, Gogela T, et al. A food-based dietary strategy lowers blood pressure in a low socioeconomic setting: a randomised study in South Africa. Public Health Nutr 2008; 11:1397–1406. [DOI] [PubMed] [Google Scholar]
- 61.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010; 303: 2043–2050. [DOI] [PubMed] [Google Scholar]
- 62.Ohene Buabeng K, Matowe L, Plange-Rhule J. Unaffordable drug prices: the major cause of non-compliance with hypertension medication in Ghana. J Pharm Pharm Sci 2004; 7:350–352. [PubMed] [Google Scholar]
- 63.Mvo Z, Dick J, Steyn K. Perceptions of overweight African women about acceptable body size of women and children. Curationis 1999; 22:27–31. [DOI] [PubMed] [Google Scholar]
- 64.Beune EJ, Haafkens JA, Agyemang C, Bindels PJ. Inhibitors and enablers of physical activity in multiethnic hypertensive patients: qualitative study. J Hum Hypertens 2010; 24:280–290. [DOI] [PubMed] [Google Scholar]
- 65.American Heart Association. Overweight and obesity statistics – 2009 update; 2009.
- 66.Read JG, Emerson MO, Tarlov A. Implications of black immigrant health for U.S. racial disparities in health. J Immigr Health 2005; 7:205–212. [DOI] [PubMed] [Google Scholar]
- 67.Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, Black African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. J Epidemiol Community Health 2005; 59:1014–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]


