Abstract
Objective:
The expansion of Minimally Invasive Surgery (MIS) has been exponential since the introduction of laparoscopic surgery in the late 1980s. This shift in operative technique has led many to believe that surgery residents are not developing the skills needed to adequately perform open operations.
Methods:
We performed a retrospective review of the Accreditation Council for Graduating Medical Education national operative case log database of general surgery residents from January 2003 to December 2019. We compared the open vs. laparoscopic case numbers for six different operations, including cholecystectomy, appendectomy, inguinal hernia repair, colectomy, gastrectomy, and Nissen fundoplication. The Cochran-Armitage test was used to assess the linear trend in the procedures performed.
Results:
Total average residency case volumes for the procedures studied have increased from 270 to 368 (36%) over the 16-year period with MIS steadily representing a greater proportion of these cases. From 2003 to 2018, MIS representation increased in all studied procedures: cholecystectomy (88% to 94%, p = 0.048), inguinal hernia repair (20% to 47%, p ≤ 0.001), appendectomy (38% to 93%, p ≤ 0.001), colectomy (8% to 43%, p ≤ 0.001), gastrectomy (43% to 84%, p = 0.048), and Nissen (71% to 91%, p = 0.21).
Conclusion:
While the overall operative volume has increased nationally for surgical residents, the representation of open cases has steadily declined since the advent of MIS. The experience needed in open surgery during resident training is still to be determined and may be necessary now that laparoscopy is progressively replacing open operations.
Keywords: Minimally invasive surgery, Laparoscopy, Residency, Procedures
INTRODUCTION
Minimally Invasive Surgery (MIS) was pioneered in the 1980s, achieved prominence in the 1990s, and has become the standard of care for many procedures today. However, since its inception, the use of MIS has raised questions about training. The increased predilection for a minimally invasive approach has led to debate on procedural competence, over reliance on technology by today’s surgeons, and the question of whether surgeons remain adequately trained in open techniques.1–3
The role of laparoscopy as a surgical tool has become better defined over the past couple decades, thus, its increase in clinical practice is expected and unsurprising. This move towards a minimally invasive approach can be seen in previous work showing a decline in open surgical techniques in favor of percutaneous, endovascular, and minimally invasive interventions.4–6 Notably, a recent paper published by Bingmer et al. showed a dramatic 462% increase in laparoscopic cases by general surgery residents over the 18-year interval, 2000 to 2018.7
It is not clear how many procedures constitute an adequate experience for surgeons. For instance, using a threshold number of 10 procedures, there was no change in resident experience between 2005 and 2011.8 It also remains unclear what the precise relationship is between procedural volume and procedural competence, but trainees remain tied to defined category minima and volume-based criteria.
In this study, we sought to analyze the procedural volumes of surgical residents in the United States, with a specific emphasis on laparoscopic experience.
METHODS
We performed a retrospective review of the Accreditation Council for Graduating Medical Education (ACGME) national operative case log database of general surgery residents from January 2003 to December 2019. The number of residents who logged cases during the years evaluated were 1017 (252 programs), 1044 (244 programs), 1105 (243 programs), and 1219 (249 programs) during the academic years 2003/04, 2008/09, 2012/14, and 2018/19 respectively. We compared the open and laparoscopic case numbers for six selected operations: cholecystectomy, appendectomy, inguinal hernia repair, colectomy, gastrectomy, and Nissen fundoplication. To account for overall rise in case number, we normalize the data by converting case number to a proportion of total case number. All results were compiled into an Excel database, and the Cochran-Armitage test was used to assess the linear trend in the procedures performed.
RESULTS
The total average residency case volumes for the six procedures studied increased from 270 to 368 (36%) over the 16-year period. Total laparoscopic cases increased from 133 to 280, representing a 111% increase for the six procedures over the study interval. Total case numbers are included in Table 1. From 2003/04 to 2018/19, MIS made up a larger proportion of total case number in all studied procedures (see Figures 1 and 2). This reached statistical significance in five of the six: cholecystectomy (88% to 94%, p = 0.048), inguinal hernia repair (20% to 47%, p ≤ 0.001), appendectomy (38% to 93%, p ≤ 0.001), colectomy (8% to 43%, p ≤ 0.001), gastrectomy (43% to 84%, p = 0.048), and Nissen (71% to 91%, p = 0.21).
Table 1.
Total Case Numbers Reported by General Surgery Residents
| OPEN |
LAPARASCOPY |
|||||||
|---|---|---|---|---|---|---|---|---|
| 2003/04 | 2008/09 | 2013/24 | 2018/19 | 2003/04 | 2008/09 | 2013/24 | 2018/19 | |
| Cholesystectomy | 13 | 9 | NA | 8 | 91 | 112 | NA | 122 |
| Ing Hernia | 48 | 46 | 48 | 46 | 12 | 18 | 30 | 40 |
| Appendectomy | 29 | 19 | 10 | 5 | 18 | 38 | 55 | 66 |
| Colectomy | 48 | 44 | 35 | 35 | 4 | 16 | 22 | 26 |
| Nissen | 2 | 2 | 1 | 1 | 5 | 5 | 7 | 10 |
| Gastrectomy | 4 | 3 | NA | 3 | 3 | 10 | NA | 16 |
Figure 1.
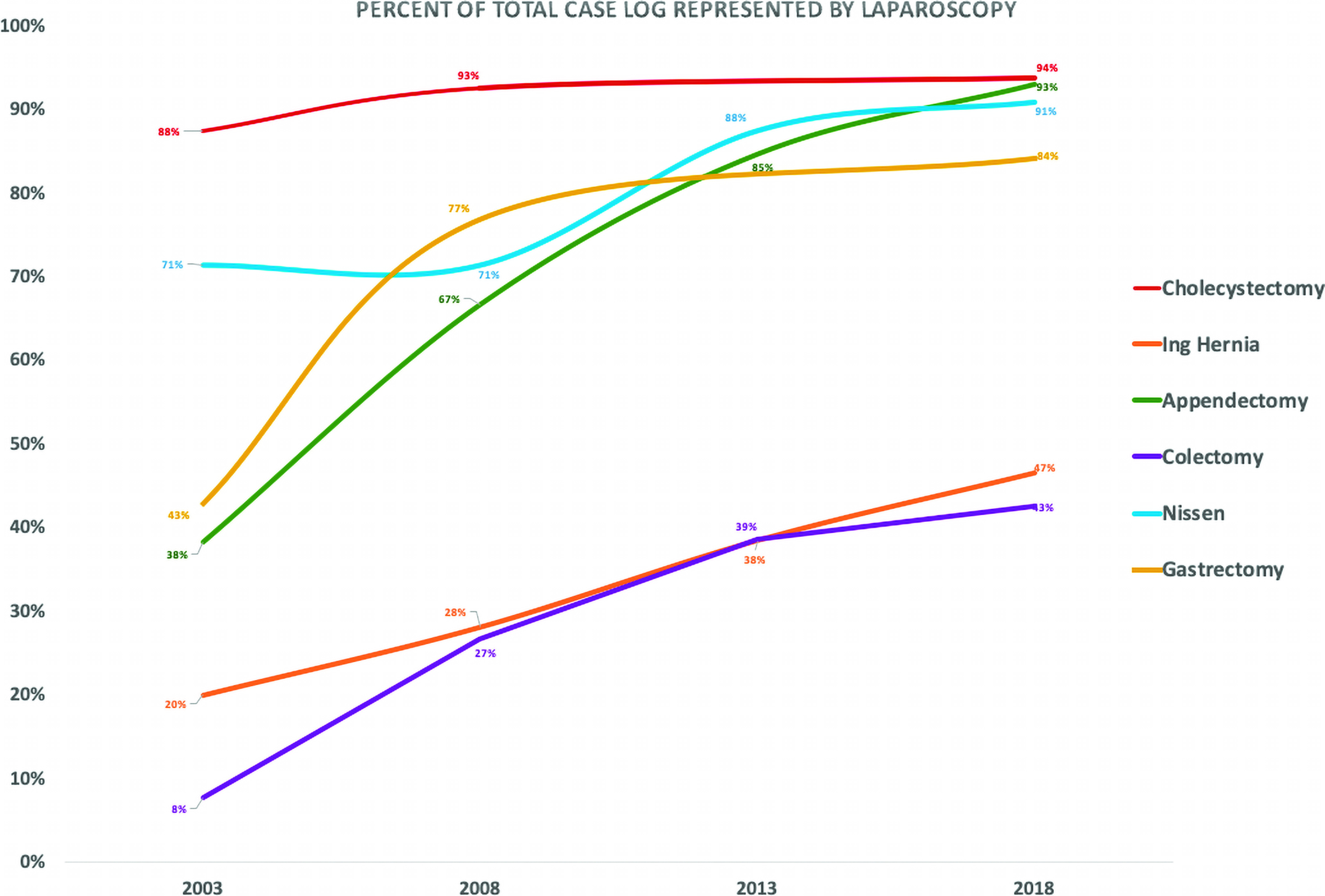
The Rise in Proportion Over the Study Period That is Now Taken Up by Laparoscopic Procedures.
Figure 2.
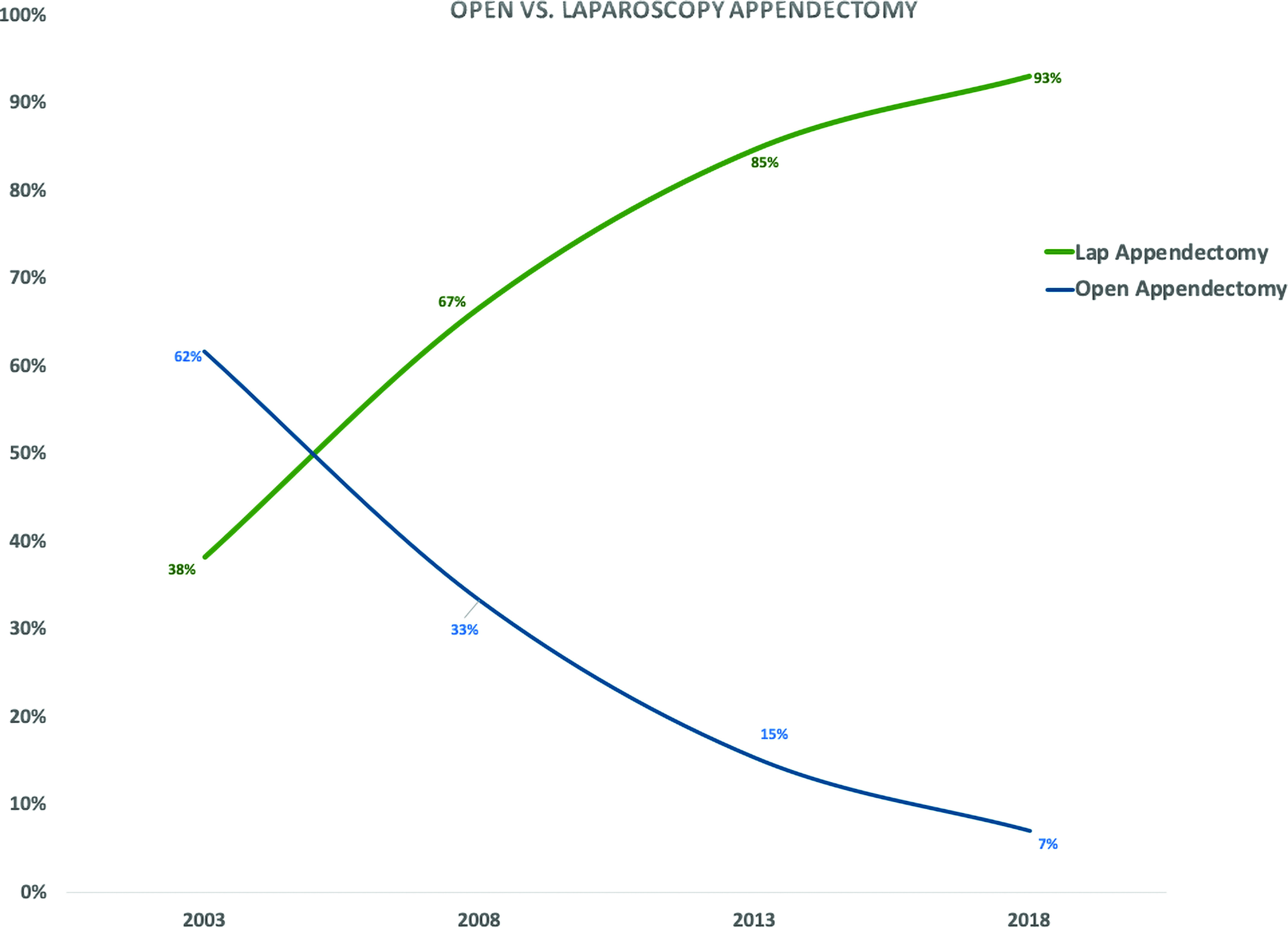
The Explosive Rise of Minimally Invasive Surgery and the Progressive Replacement of Open Procedures.
DISCUSSION
While the overall number of cases that residents are performing is on the rise, there has been a growing concern that the diversity of cases is narrowing.9 Our group did not expect to see this rise in overall case number given reduced hours residents are in the hospital, the increase in case complexity, and a shift towards technology in surgical training. Yet, there was a nearly 40% rise in total case numbers from 2003/04 to 2018/19. We propose that this increase in total case volume can be explained through a couple key elements. First, national case volume is on the rise due to an aging population, shorter hospital stays, reduction in post-surgical mortality, and an increase in ambulatory surgeries.10–13 We postulate that this increase in total case volume has more than made up for the decrease in total hours at the hospital by today’s residents. In addition, there has been an expansion of laparoscopy in surgical practice, along with an increased case minimum in laparoscopy by the ACGME, leading to residents needing to perform more operations with a technique that we are using more often.14
The appendectomy has been a principal case to learn the fundamentals of laparoscopy.15 Our results show an explosive rise in laparoscopic appendectomy and the progressive replacement of the open appendectomy. In just a short time the resident experience with appendectomies is nearly completely represented by a minimally invasive approach (93%). Trainees in 2003 had a much larger experience with open appendectomies, which suggests that today’s surgical graduates are different from surgical graduates from just 16 years ago. This has led to concerns over open surgical training. For example, a recent review of open arterial vascular procedures showed a significant decline in the past decade and a half, leading the authors to question if vascular surgery can remain an essential content area in general surgical training.16
One way to combat deficiencies at the end of a surgical residency is to continue training through a surgical fellowship. It is becoming the standard for general surgery residents to pursue additional specialty training in the form of fellowships after completion of their residency. One study by Borman et al. found that 77% of graduating general surgery chief residents were planning to pursue additional fellowship training.17 A lack of confidence and the need to master an area of clinical practice were noted as major reasons for choosing to do a fellowship.17,18 The striking rise of laparoscopy in the surgical field has led to a focus by the ACGME to ensure that today’s surgical trainees are not deficient in this area.
The ACGME has set minimum procedural volumes for defined categories to be completed by surgical residents. To graduate from a general surgery residency, the ACGME requires a minimum of 75 complex and 100 basic laparoscopic cases, a minimum that has steadily increased over the past 20 years. We can see the effects of this increase through the six procedures included in this study, all of which showed a rise in the representation of laparoscopy, five reaching statistical significance (cholecystectomy, inguinal hernia repair, appendectomy, colectomy, and gastrectomy). The ACGME has not defined a minimum of open cases required by general surgery trainees. We suggest that it is necessary now, more than ever, to define an open case minimum for today’s trainees so that tomorrow’s surgeons are not deficient in this necessary skill.
This study has potential limitations. The ACGME reporting system has been shown to be an imperfect representation of actual resident case experience due to inconsistencies with logging.19 The ACGME case log is a quantitative measure of resident experience where the actual resident level of participation in a given case can be questioned. Resident duty hour restrictions were implemented in 2003, so we did not include data prior to that time point. We also did not include robotic cases to this data, which, if we had, may show an even more drastic representation of MIS.
CONCLUSION
While the overall operative volume has increased nationally for surgical residents, the representation of open cases has steadily declined since the advent of MIS. Laparoscopy has steadily and systematically become a dominant feature of today’s general surgery trainees. The experience needed in open surgery during resident training is still to be determined and may be necessary now that laparoscopy is progressively replacing open operations.
Contributor Information
Ace St. John, University of Maryland Medical Center, Baltimore, Maryland..
Ilaria Caturegli, University of Maryland Medical Center, Baltimore, Maryland..
Natalia S. Kubicki, University of Maryland School of Medicine, Baltimore, Maryland..
Stephen M. Kavic, University of Maryland School of Medicine, Baltimore, Maryland..
References:
- 1.Melmer PD, Chaconas C, Taylor R, et al. Impact of laparoscopy on training: are open appendectomy and cholecystectomy on the brink of extinction? Am Surg. 2019;85:761–763. [PubMed] [Google Scholar]
- 2.Chung RS, Ahmed N. The impact of minimally invasive surgery on residents’ open operative experience: analysis of two decades of national data. Ann Surg. 2010;251:205–212. [DOI] [PubMed] [Google Scholar]
- 3.McCoy A, Gasevic E, Szlabick RE, Sahmoun AE, Sticca RP. Are open abdominal procedures a thing of the past? An analysis of graduating general surgery residents’ case logs from 2000 to 2011. J Surg Ed. 2013;70:683–689. [DOI] [PubMed] [Google Scholar]
- 4.Alkhoury F, Martin JT, Contessa J, Zuckerman R, Nadzam G. The impact of laparoscopy on the volume of open cases in general surgery training. J Surg Ed. 2010;67:316–319. [DOI] [PubMed] [Google Scholar]
- 5.Eckert M, Cuadrado D, Steele S, et al. The changing face of the general surgeon: national and local trends in resident operative experience. Am J Surg. 2010;199:652–656. [DOI] [PubMed] [Google Scholar]
- 6.Quillin III RC, Cortez AR, Garcia MA, et al. Gas off, room lights on: shedding light on the surgical resident’s experience in open and laparoscopic surgery. Surgery. 2019;166:460–468. [DOI] [PubMed] [Google Scholar]
- 7.Bingmer K, Ofshteyn A, Stein SL, Marks JM, Steinhagen E. Decline of open surgical experience for general surgery residents. Surg Endosc. 2020. Feb;34(2):967–972. Epub 2019 Jun 10. PMID: 31183795. [DOI] [PubMed] [Google Scholar]
- 8.Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR. Operative experience of surgery residents: trends and challenges. J Surg Ed. 2013;70:783–788. [DOI] [PubMed] [Google Scholar]
- 9.Cortez AR, Katsaros GD, Dhar VK, et al. Narrowing of the surgical resident operative experience: a 27 year analysis of national ACGME case logs. Surgery. 2018;164:577–582. [DOI] [PubMed] [Google Scholar]
- 10.Etzioni DA, Liu JH, Maggard MA, Ko CY. The aging population and its impact on the surgery workforce. Ann Surg. 2003;238(2):170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Statistical Brief #225. Healthcare Cost and Utilization Project (HCUP). June 2017. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.jsp. [PubMed] [Google Scholar]
- 12.Finks, Osborne, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ambulatory Surgery Center Market Size, Share & Trends Analysis Report By Application (Orthopedics, Plastic Surgery, Ophthalmology, Gastroenterology, Pain Management), By Region, And Segment Forecasts, 2019. – 2026. https://www.grandviewresearch.com/industry-analysis/ambulatory-surgery-center-asc-market.
- 14.Richards MK, McAteer JP, Drake FT, et al. A national review of the frequency of minimally invasive surgery among general surgery residents: assessment of ACGME case logs during two decades of general surgery resident training. JAMA Surg. 2015;150:169–172. [DOI] [PubMed] [Google Scholar]
- 15.Huber T, Paschold M, Bartsch F, Kneist Lang H. W. Appendectomy in surgical residency. What has changed over the past ten years? Chirurg. 2016;87:326–331. [DOI] [PubMed] [Google Scholar]
- 16.Potts III, JR, Valentine RJ. Declining resident experience in open vascular operations threatens the status of vascular surgery as an essential content area of general surgery training. Ann Surg. 2018;268:665–673. [DOI] [PubMed] [Google Scholar]
- 17.Borman KR, Biester TW, Rhodes RS. Motivations to pursue fellowships are gender neutral. Arch Surg. 2010. Jul;145(7):671-678. [DOI] [PubMed] [Google Scholar]
- 18.Viola KV, Bucholz E, Yeo H, Piper CL, Bell RH, Jr, Sosa JA. Impact of family and gender on career goals: results of a national survey of 4586 surgery residents. Arch Surg. 2010. May;145(5):418-424. [DOI] [PubMed] [Google Scholar]
- 19.Nygaard RM, Daly SR, Van Camp JM. General surgery resident case logs: do they accurately reflect resident experience?. J Surg Educ. 2015;72(6):e178–e183. [DOI] [PubMed] [Google Scholar]


