Acknowledgments
We gratefully acknowledge the contributions to prior editions of this chapter by Drs. Ken Jubb, Peter Kennedy, Nigel Palmer, Julie Yager, Danny Scott, Pamela Ginn, Joanne Mansell, and Pauline Rakich.
General Considerations
The integument serves as the anatomic boundary between the body and the ambient environment. The vast surface area of the skin puts it in constant contact with environmental irritants, pollutants, and pathogens. Unlike diseases in internal viscera, lesions in the skin are readily apparent, and thus skin disease is one of the most common reasons for veterinary consultation. Skin diseases range from minor, esthetic problems to life-threatening conditions. In companion animals, a healthy pelage (haircoat) stands as the interface between the human owner and pet. In addition to causing undo suffering, severe skin disease may interfere with the human-animal bond. In farm animals, skin diseases produce severe economic losses because of damage to wool, hides, and meat or from decreased milk production or growth rates.
The protective barrier of the skin is complex, and much of this function is provided by the stratum corneum (SC), the outermost layer of the epidermis. This innocuous appearing layer of terminally differentiated (dead) keratin squames maintains hydration of the body by restricting water loss. The constant shedding (desquamation) and renewal aids in the removal of surface pathogens. The SC also contains antimicrobial peptides (e.g., β-defensins, cathelicidins) and a variety of lipids that also aid in bacterial and chemical defense. Constant immunosurveillance is provided by the skin immune system that consists of orchestrated interactions between Langerhans cells, keratinocytes, lymphocytes, and dermal dendritic cells. Hair and melanin pigment deliver the bulk of photoprotection as well as provide thermoregulation. The epidermis is also an important site of vitamin D regulation. Sunlight acts on the epidermis to convert provitamin D3 (7-dehydrocholesterol) to vitamin D3 (cholecalciferol). In the liver, vitamin D3 is hydroxylated to 25-hydroxy D3 and in kidneys to the active form 1,25-vitamin D3. Vitamin D3 regulates epidermal differentiation and proliferation. The skin is involved in thermoregulation by virtue of the pelage, blood flow, and, in some species (e.g., equids), sweating. Last, the state of the skin is an indicator or general health and internal disease.
As dermatologic cases are more commonly presented to veterinary clinicians for examination, skin biopsies have become a routine diagnostic tool. An understanding of the pathologic processes in skin, as in any tissue, requires knowledge of normal structure and function. As a general rule, clinicians are more adept at recognizing gross lesions than anatomic pathologists. To interpret skin biopsies, pathologists must have a good understanding of the characteristic gross lesions and patterns manifest by diseases in the species being examined. This fact underscores the importance of the inclusion of the gross findings in the surgical pathology request. Although the architecture of the skin is conserved across most mammalian species, the pathologist must be aware of differences between species and site differences within the same species, to interpret normal versus abnormal. The dermis contributes most to the thickness of the skin. The haired skin is thickest over the dorsal surface of the body and lateral aspect of the limbs and thinnest on the ventral aspect of the trunk and medial limbs. The epidermis is naturally thicker in areas that need enhanced protection because of lack of hair and exposure to surface trauma (e.g., lips, pawpads, and nasal planum). The thinnest epidermis is found in well-protected sites (e.g., ventral abdomen, inguinal area).
The integument is composed of epidermis, dermis, adnexal structures (simple and compound hair follicles, epitrichial apocrine glands, atrichial [eccrine] glands, sebaceous glands, arrector pili muscles), and the subcutis, as well as nails, hooves, and claws.
Epidermis
The epidermis consists of a highly organized, continuously renewing squamous epithelium that is stratified into functionally distinct layers: stratum basale, stratum spinosum, stratum granulosum, and stratum corneum. The keratinocytes of the epidermis undergo a process of differentiation and proliferation that facilitates repair after external trauma and yields a hydrophobic protective barrier, the stratum corneum, which is continuously shed into the environment. The steady state of the epidermis is a balance between cell proliferation, differentiation, and desquamation. The renewal is provided by a small population of slow-cycling stem cells (~10% of cells) in the basal layer that undergo proliferation into transiently amplifying cells. The amplified cells briefly proliferate then exit the cell cycle and undergo terminal differentiation. In doing so, the cells march toward the final product—fully-cornified anucleate keratinocytes (corneocytes) that are shed into the environment. Within keratinocytes as well as other epithelial cells, keratin, an intermediate filament, forms the fibrous cytoskeleton that connects to desmosomes. Type I (acidic) and type II (basic) keratin subunits assemble into heterodimers through disulfide bonds. The type of keratin is differentially expressed in layers of the epidermis as well as body site (e.g., nonhaired skin of the pawpad and hair follicles). Keratin 5 (K5) and keratin 14 (K14) form heterodimers in basal layer keratinocytes. Commitment to differentiation in suprabasal keratinocytes is associated with induction of keratins 1 (K1) and K10. Keratin 2 (K2) is expressed in the stratum granulosum (SG).
The epidermis is a prime example of an adult tissue that undergoes continual and rapid flux. The epidermis maintains homeostasis by constant proliferation of a single inner (basal) layer of rapidly dividing progeny of stem cells. As the basal keratinocytes withdraw from the cell cycle, the transiently amplifying cells commit to terminally differentiate, detaching from the basement membrane and initiating a trek toward the skin surface.
-
•
The stratum basale (basal layer) is the deep germinative layer of the epidermis and is composed of a single layer of cuboidal to low columnar cells resting on the basement membrane zone. The basal cells are attached to the underlying basement membrane by hemidesmosomes and to adjacent and overlying keratinocytes by desmosomes. Desmosomes are anchoring structures that mediate adhesion between cells. They have a complex structure that includes cadherin proteins of 2 types—desmocollins and desmogleins. These proteins have different isoforms, and they are differentially expressed in different layers of the epidermis. Whereas basal cells express a pair of desmogleins and desmocollins of simple epithelia, desmosomes of the spinous layer express more varied isoforms. These adhesion molecules are the immunologic target in several blistering autoimmune diseases.
-
•
The stratum spinosum (prickle cell layer) is characterized by prominent intercellular bridges that are the desmosomal attachments between cells. The spinous appearance is due to shrinkage artifact that occurs during tissue processing. The cells are polyhedral to slightly flattened and are arranged in 1 or 2 layers in haired skin of dogs and cats and up to 4 layers in large animals. This layer is much thicker in nonhaired skin and may be up to 20 cells thick in the footpads and nasal planum.
-
•
The stratum granulosum is variably apparent on light microscopy in haired skin and appears only 1-2 cells thick. In nonhaired skin, this layer is more prominent, averaging 4-8 layers in thickness. The SG is composed of flattened cells with shrunken nuclei and deeply basophilic keratohyaline granules. The granules contain a precursor of filaggrin, a histidine-rich interfibrillary matrix protein that functions as a biological glue that aggregates and aligns keratin filaments.
-
•
The stratum corneum (SC) is composed of >20 overlapping layers of bland, polyhedral, anucleate cells sandwiched between layers of lipid. This inconspicuous layer is an active and tough hydrophobic barrier that regulates water movement into and out of the skin. Much of the content of the SC is lost during biopsy sampling, cutting, and processing. The basket-weave pattern is an artifact resulting from loss of the lipid lamellae during processing. Thickness varies by species and site, but it is generally adapted to the degree of surface trauma or friction. The SC is thickest in nonhaired areas, such as footpads and nasal planum. Cornification (keratinization) is the process by which keratinocytes undergo terminal differentiation from the basal layer to the highly specialized corneocyte. In doing so, keratinocytes must lose a large amount of water volume (from 70% water in nucleated layers to 15% in stratum corneum). Minor injuries to the corneal layer from tape stripping or applications of solvents will result in increased transepidermal water loss.
Several steps must occur for cornification to proceed normally: (1) bundling of keratin to establish the corneocyte core, (2) replacement of the cell membrane with a thick cornified envelope, (3) formation of lipid lamellar bilayers, and (4) active desquamation. Alterations in any step can lead to hyperkeratosis, clinical scaling, and decreased barrier function.
The lipid is derived via lipid-laden organelles, called lamellar bodies (also called Odland bodies, membrane coating granules, lamellar granules, keratinosomes), which are synthesized in the upper stratum spinosum. At the junction of the SG and SC, the lamellar bodies fuse with the cell membrane and expel their contents into the intercellular space. Lamellar bodies contain glucosylceramides (GlcCer), sphingomyelin, glycerophospholipids, and cholesterol sulfate, along with many modifying enzymes. During this release, enzymes modify polar “probarrier” lipids into nonpolar “barrier” lipids. The final product in the lipid bilayers of the SC contains an equimolar ratio of ceramides, cholesterol, and free fatty acids that together create a hydrophobic seal.
The protein core of the corneocyte provides much of the structural integrity of the stratum corneum. Profilaggrin, found in the keratohyaline granules of the SG, undergoes processing (proteolysis, dephosphorylation) to the active enzyme filaggrin, which cross-links the cytoplasmic keratin filaments. Transglutaminases, calcium-containing enzymes, are located within both the epidermis and hair follicles. These proteins (in particular, transglutaminase 1) catalyze the formation of the cornified envelope (CE) by cross-linking small protein molecules (e.g., involucrin, loricrin, cystatin A) that replace the cell membrane. The CE surrounds the protein core and provides a mechanical barrier as well as a scaffold that organizes the extracellular lipids into lamellar membranes. In the mature SC, multiple layers of corneocytes are sandwiched between layers of lipid, producing the so-called “mortar and bricks” analogy. Corneodesmosomes (desmosomes retained in the SC) are enzymatically cleaved, and keratin squames (corneocytes) are shed into the environment.
Epidermal nonkeratinocytes
Melanocytes are located in the basal layer of the epidermis and outer root sheath of hair follicles; and in hematoxylin and eosin (H&E) sections, they appear as clear cells with a small dark-staining nucleus because of shrinkage artifact. There is ~1 melanocyte per 10-20 keratinocytes. The dendritic processes can be seen with silver stains. Derived from the neural crest, melanocytes migrate into the epidermis during early fetal life. Their processes are intertwined between the surrounding keratinocytes to which they transfer melanin pigment. A melanocyte and its surrounding constellation of keratinocytes is termed the “epidermal melanin unit.” Melanogenesis occurs in membrane-bound organelles called melanosomes, which originate from the Golgi apparatus. The melanosomes migrate to the tips of the dendrites and are phagocytosed by adjacent keratinocytes. Most melanin pigment in skin is in the basal layer, but in dark-skinned animals, melanin may be present throughout the epidermis. The epidermis of most dogs and cats is only lightly pigmented. Melanin is photoprotective, and exposure to ultraviolet (UV) light increases melanin production, often resulting in a cap of pigment granules over the nucleus. Skin pigmentation is affected by local inflammation because melanocytes respond to inflammatory mediators by increasing or decreasing melanogenesis and by altering melanin transfer to keratinocytes.
Langerhans cells are bone marrow–derived dendritic cells that are functionally and immunologically related to monocyte-macrophage cells. They appear as clear cells on routine H&E sections and may be distributed from the stratum basale to the stratum spinosum, depending on species and region of the skin. They are usually less numerous than melanocytes, however. Langerhans cells are characterized ultrastructurally by rod- or racket-shaped cytoplasmic granules called Birbeck granules. Birbeck granules have been identified in Langerhans cells of the pig, cat, cattle, sheep, goat, horse, and human, but not in the Langerhans cells of the dog. Langerhans cells express CD1, class II major histocompatibility complex (MHC) antigens, CD45, vimentin, and S-100. The long dendritic processes of Langerhans cells traverse the intercellular space to the granular cell layer, where they function in immunosurveillance as antigen-presenting cells. Langerhans cells trap antigens in the epidermis and migrate via afferent lymphatics to draining lymph nodes, where they present antigen to T cells in paracortical areas, resulting in proliferation of a population of sensitized T cells. Langerhans cells express a high-affinity receptor for immunoglobulin E (IgE) (FcεRI), which allows Fc receptor–mediated uptake of allergens. Exposure to UVB radiation decreases Langerhans cell numbers in the epidermis and interferes with their antigen-presenting capacity. Langerhans cells are involved in development of contact hypersensitivity, and increased numbers of epidermal Langerhans cells have been found in horses with insect hypersensitivity and dogs with atopic dermatitis.
A second type of clear cell in the basal layer is the Merkel cell. There has been a long-standing debate over whether Merkel cells originate from epidermal or neural stem cells, but current studies indicate an epidermal origin. Unlike melanocytes, Merkel cells are connected to adjacent keratinocytes by desmosomes. Merkel cells are also located in the external root sheath of hair follicles. They are identified ultrastructurally by characteristic dense-core cytoplasmic granules. Immunohistochemical markers include cytokeratin, neurofilaments, neuron-specific enolase, and desmosomal proteins. Merkel cells have been identified in the dog, cat, sheep, pig, monkey, various laboratory animals, birds, reptiles, and amphibians. Their density in the epidermis is variable, and they are in highest numbers in areas involved with sensory perception. Merkel cells form Merkel cell–neurite complexes with axons in tylotrich pads and sinus hairs that are thought to function as gentle touch receptors that initiate slow-adapting type 1 responses. Their exact function in these structures is uncertain, but they are thought not to act as sensory cells but rather to function as abutments for deformation of the mechanosensitive nerve endings. Merkel cells are also thought to have various neuroendocrine effects and to be involved in control of the hair cycle.
Basement membrane zone
The basement membrane zone (BMZ) is the structurally and biochemically complex junction between the epidermis and dermis. Both the epidermis and dermis contribute to production of the various components of the BMZ. The area is indistinct in H&E sections but visible as a thin, homogeneous band with periodic acid–Schiff (PAS) stain. It varies in thickness in different sites and is most prominent in nonhaired areas of skin and mucocutaneous junctions. In all animals except swine, the dermal-epidermal junction is straight, and the BMZ parallels the skin surface, whereas in swine and humans, the dermal-epidermal junction is thrown into undulating folds called rete ridges. The BMZ has a crucial role in anchoring the epidermis to the dermis, and abnormalities of the BMZ result in serious and potentially fatal bullous diseases. The BMZ also influences growth and differentiation of keratinocytes and acts as a selective barrier for passage of molecules between the epidermis and dermis.
Ultrastructurally, the BMZ is composed of (1) the plasma membrane of basal keratinocytes with their specialized attachment structures, hemidesmosomes; (2) the electron-lucent lamina lucida; (3) the electron-dense lamina densa; and (4) the subbasal lamina fibrous zone. Hemidesmosomes are located on the basal aspect of basal keratinocytes, and they consist of a cytoplasmic plaque that connects to the cytoskeleton and a transmembrane portion that binds to the underlying basement membrane. The cytoplasmic plaque is composed of a number of proteins, including bullous pemphigoid antigen 230 (bullous pemphigoid antigen 1) and plectin, which connect keratin 5 and 14 intermediate filaments to the plasma membrane. Hemidesmosomes also have a transmembrane portion that includes α684 integrin and bullous pemphigoid antigen 2 (type XVII collagen). The proposed ligand for α684 integrin is laminin 5, which is a component of the anchoring filaments of the lamina lucida, and this binding mediates the stable adhesion of keratinocytes to components of the BMZ. Anchoring filaments are 2-4 nm diameter filaments composed of laminin 5 (also called epiligrin, kalinin, and BM600). They pass from the plasma membrane through the lamina lucida to attach to the lamina densa. The lamina densa is composed of multiple molecules, including type IV collagen, laminin, nidogen, and several glycoproteins. The lamina densa is connected to anchoring plaques of the underlying dermis by anchoring fibrils. The subbasal lamina fibrous zone of the superficial dermis is composed of anchoring fibrils, anchoring plaques, and microfibrils. Anchoring fibrils are composed of type VII collagen and form looping arrays with one or both ends of the fibrils attached to the lamina densa, thereby anchoring the BMZ to the dermis.
Dermis
The dermis is involved in maintenance and repair of the skin and is the major component responsible for the tensile strength and elasticity of the skin. In addition, the thickness of the dermis largely determines the thickness of the skin. The dermis is composed of collagen and elastic fibers embedded in a ground substance, blood and lymphatic vessels, nerves, and low numbers of lymphoid cells. Except for swine, domestic animals have no dermal papillae as occur in human skin. Thus, instead of papillary and reticular dermis, the dermis is divided somewhat arbitrarily into superficial and deep dermis in domestic animals.
The dermal fibers include collagen, reticular fibers (reticulin), and elastic fibers, all of which are synthesized by dermal fibroblasts. Collagen fibers are the most abundant constituent of the dermis, and they confer tensile strength to skin. The majority of dermal collagen is types I and III. The superficial dermis is composed of fine, loosely arranged collagen fibers. The deep dermis consists of thick, densely arranged collagen fibers that roughly parallel the skin surface. Reticular fibers represent a special thin type of collagen III. Elastic fibers are inconspicuous in routine H&E sections. They can be visualized with special stains, such as orcein stain or Verhoeff–van Gieson elastin stain. They are thicker and less numerous in the deep dermis and arranged parallel to the skin surface. The elastic fibers become progressively thinner near the epidermis.
The ground or interstitial substance is an amorphous gel-sol that fills the space between dermal structures but allows electrolytes, nutrients, growth factors, and cells to pass through. It consists of proteoglycans and glycoproteins. Proteoglycans are high-molecular-weight complexes composed of glycosaminoglycans linked to proteins, and those most abundant in the dermis include hyaluronic acid and various chondroitin sulfates. Proteoglycans bind various chemical mediators and thereby function as storage matrix as well as provide lubrication and structural support. Fibronectins are glycoproteins involved in mediating cell-cell and cell-matrix interactions that are required for various cell functions, including cell adhesion, phagocytosis, and cell migration. The ground substance is usually not visible in normal H&E sections; however, a fine granular to fibrillar basophilic material is occasionally evident between collagen fibers. This material is especially abundant in the dermis of Chinese Shar-Pei dogs as a normal variant for this breed.
The dermal vasculature is arranged in 3 intercommunicating plexuses. The deep plexus is located at the junction of the dermis and subcutis, and it supplies branches to the middle plexus, which is located at the level of the sebaceous glands. It, in turn, supplies branches to the superficial plexus. The capillary loops parallel to the skin surface immediately beneath the epidermis arise from the superficial plexus. An unusual vascular arrangement is present in the dermis of the llama. It consists of clusters of capillary-sized, thick-walled vessels lined by plump endothelial cells distributed throughout the superficial and middle dermis. Dermal lymphatic vessels are inconspicuous in normal skin and only become visible when they become dilated because of increased lymphatic drainage. The skin is supplied with sensory and autonomic nerves that are usually associated with blood vessels.
The dermis is normally sparsely cellular. Fibroblasts are distributed in low numbers throughout the dermis. They synthesize most of the fibrillar and ground substance proteins of the dermis as well as various growth factors and cytokines. Melanocytes in the dermis are usually located near superficial dermal vessels. In contrast to melanocytes of the epidermis and hair follicles (“secretory melanocytes”), dermal melanocytes do not transfer their melanin to surrounding cells (“continent melanocytes”). Normal dermis also contains small numbers of perivascular monocytes and lymphocytes, which are indistinguishable from each other. Dermal lymphocytes are primarily T cells of the helper subtype.
Mast cells are tissue-dwelling cells that are most numerous in sites, such as the skin, that interface with the environment. Mast cell numbers in skin vary greatly, depending on body location, with numbers in cats of 4-20 per 400× field around superficial dermal blood vessels, and 4-12 per 400× field in dogs. In dogs, the highest mast cell density is in the pinnae and interdigital skin, whereas the nasal planum has the lowest density. Mast cells are concentrated around blood vessels, especially postcapillary venules. Mast cells are not present in normal epidermis. Although mast cells are evident in routine H&E sections, they are better visualized with Giemsa and toluidine blue, which stain mast cell granules metachromatically.
Mast cells are released from the bone marrow as immature precursors and migrate to tissues, where they differentiate into mature cells. The proliferation and differentiation is regulated by stem cell factor (SCF), a cytokine produced by fibroblasts and keratinocytes, as well as T-cell–derived cytokines (e.g., interleukin-3 [IL-3], IL-4, IL-9, IL-10). SCF is thought to home mast cells to the dermis as well as regulate the synthesis of mast cell mediators and secretory function. The receptor for SCF on mast cells is c-kit. Mast cells exert their effects by synthesizing and releasing a host of inflammatory mediators (e.g., histamine, proteases, cytokines). The release of mast cell granules is triggered by the interaction between allergens and allergen-specific IgE bound to a high-affinity IgE receptor (FcεRI). Degranulation of both canine and human mast cells is thought to involve breakdown of their secretory granules and solubilization of contents during exocytosis. Mast cells have laminin receptors that mediate their adhesion to the extracellular matrix. The perivascular space is rich in laminin, which contributes to the localization of mast cells to this site.
Mast cells are a heterogeneous population based on differences in histochemical, biochemical, and functional characteristics that vary between species and different tissues within a single species. Mast cell heterogeneity has been demonstrated in the skin of cattle, dogs, and sheep. A subpopulation of mast cells that does not exhibit metachromasia following formalin fixation has been demonstrated in the skin of dogs and cattle, and heterogeneity of protein content has been identified in dermal mast cells of sheep.
Mast cell granules contain an array of preformed mediators, but they are also capable of synthesizing mediators such as leukotrienes (LTC4) and prostaglandins (PGD2) following stimulation. Tumor necrosis factor-α (TNF-α), a potent proinflammatory cytokine, is both preformed and newly synthesized upon activation of mast cells. Mast cells have long been known to be the critical effector cell in initiation of acute type I hypersensitivity reactions and in protection against parasitic infections with helminths and ectoparasitic arthropods. Mast cells also function in persistent chronic inflammatory reactions, tissue repair and remodeling, pathologic fibrosis, angiogenesis, hemostasis, hematopoiesis, antibody production, protection against bacterial infections, response to neoplasms, and possibly in control of the hair cycle.
Dermal muscles
Arrector pili muscles are smooth muscles present in all haired skin. They arise in the connective tissue of the superficial dermis and attach to the connective tissue sheath of the hair follicle below the level of the sebaceous gland duct. They are situated on the obtuse angle of the hair follicle, and when the muscles contract, the hair follicles are pulled into a vertical position (piloerection). This results in formation of air pockets in the haircoat, which provides insulation. Contraction of arrector pili muscles may also be involved in emptying of sebaceous glands. These muscles are largest in skin of the dorsal midline from the neck to the tail. They may be vacuolated in normal animals, especially aged dogs.
In addition to arrector pili muscles, pigs also have interfollicular smooth muscles. These muscles span the triad of hair follicles at a level midway between the sebaceous and apocrine glands. Their contraction draws the hair follicles together and rotates the outer follicle of the triad. The functional significance of this muscle is uncertain.
Skeletal muscles may be present in the muzzle, forehead, eyelid, and perianal regions. These muscle fibers originate from cutaneous trunci muscle that penetrates into the dermis to allow voluntary movement of the skin. Skeletal muscle fibers also are associated with the large sinus hairs of the face.
Immunologic function
The skin has been proposed to function as an immunosurveillance organ, and the term skin-associated lymphoid tissue (SALT), analogous to gut-associated and bronchial-associated lymphoid tissues (GALT, BALT), has been suggested to describe those cellular elements of the skin that deal with antigenic challenges at the skin surface. However, this concept has been disputed because of presumed differences in immune function between the common mucosal immune system and normal skin. The alternative name, skin immune system (SIS), has been suggested as a more appropriate term to encompass the skin-specific immune response–associated cells and humoral factors present in normal skin. Key components of this system include keratinocytes, Langerhans cells, the dermal perivascular unit, and skin-homing T cells.
-
•
Keratinocytes produce multiple inflammatory cytokines, adhesion molecules, and chemotactic factors following nonspecific stimulation, and thereby have a nonspecific proinflammatory and upregulating effect.
-
•
Langerhans cells are thought to trap antigens in the epidermis, migrate out to regional lymph nodes via lymphatics, and present the antigen to T cells. Thus induction of the immune response does not normally occur within the skin itself but rather in the skin-draining lymph nodes.
-
•
The dermal perivascular unit consists of the mast cells, monocytes and macrophages, tissue dendritic cells, and T cells situated around postcapillary venules. As a result of cytokines such as IL-1 and TNF-α released by injured keratinocytes, endothelial cells increase their expression of addressins intercellular adhesion molecule-1 (ICAM-1) and E-selectin and vascular cell adhesion molecule-1 (VCAM-1). These vascular endothelial molecules promote adhesion of circulating leukocytes, especially granulocytes and memory T cells.
-
•
E-selectin is thought to act as an adhesion molecule or vascular addressin for a specific subset of skin-homing memory T cells, which have the ligand cutaneous lymphocyte antigen (CLA) on their surface. A circulating pool of such skin-homing T lymphocytes, identified by CLA antigen, represents the cellular basis of immunologic memory of skin.
Thus it appears that the proinflammatory, upregulating effects of keratinocytes prepare the dermis for specific immunologic activity, whereas migrating antigen-presenting Langerhans cells induce expansion of specific lymphocytes in skin-draining lymph nodes. T cells are then recruited to the skin because of binding of skin-specific adhesion molecules to the vascular addressins of dermal endothelial cells.
Hair follicles
Hair serves a number of functions, including protection, thermal insulation, social communication, and sensory perception. Arrangement and type of hair follicles vary with species, breed, individual, and body region. In general, however, hair follicle density is greatest over the dorsolateral aspect of the body and least on the ventral aspect. Hair follicles are classified as primary or secondary, and simple or compound. Primary hairs have a large diameter, are rooted more deeply in the dermis or subcutis, and are associated with sebaceous and epitrichial sweat glands and an arrector pili muscle. Secondary hair follicles are smaller in diameter, are more superficially rooted, and may be accompanied by a sebaceous gland but lack a sweat gland and arrector pili muscle. Follicles in which a single hair emerges from the follicular orifice are termed simple follicles, whereas those in which multiple hairs emerge from a single opening are called compound follicles. Each hair of the compound follicle has its own papilla, but at the level of the sebaceous gland opening, the follicles unite to exit from a single external follicular orifice. Horses and cattle have simple hair follicles that are evenly distributed. Swine have simple follicles that are grouped in clusters of 2-4 surrounded by dense connective tissue. In sheep, the hair-growing areas consist predominantly of simple follicles, whereas the wool-growing areas have many compound follicles and consist of clusters of 3 primary follicles and a number of secondary follicles. Goats have primary follicles in groups of 3, with 3-6 secondary follicles associated with each group. Follicular arrangement in dogs and cats consists of 2-5 large primary hairs surrounded by groups of smaller secondary hairs. The primary hairs tend to be simple, whereas the secondary hairs are compound. As many as 15 hairs may emerge from a single follicular orifice. In cats, secondary hairs far outnumber primary hairs (10-24 secondary hairs per 1 primary hair).
The hair follicle is formed by a downward invasion of the surface ectoderm (primary hair germ) into the underlying mesoderm of the embryo. As they grow down, the epithelial cells envelop a small group of mesenchymal cells in the underlying dermis. These mesodermal cells eventually become the follicular papilla that repeatedly induces and maintains growth of the hair follicle throughout the life of the individual. If the papilla is somehow damaged or destroyed, the hair follicle fails to regrow. The epithelial downgrowth eventually becomes canalized to form the hair follicle. In longitudinal section, the fully developed hair follicle consists of 3 segments:
-
•
The lower or inferior portion, from the base of the follicle to the point of insertion of the arrector pili muscle
-
•
The isthmus, the short section from the attachment of the arrector pili muscle to the entrance of the sebaceous duct
-
•
The infundibulum, extending from the entrance of the sebaceous duct to the follicular orifice
The inferior segment can be considered temporary because it disappears during the involution stage of the hair cycle and reforms again during the active phase. In contrast, the isthmus and infundibular portions of the hair follicle are permanent.
The base of the hair follicle consists of a terminal bulbous expansion of epithelial cells, the hair bulb, with a concavity at its bottom that is occupied by the connective tissue papilla. The bulb is composed of the highly proliferative matrix cells and melanocytes, and they are separated from the papilla by a thin extension of the basement membrane. The matrix cells give rise to 6 different cell types arranged in concentric layers. The 3 innermost layers form the medulla, cortex, and cuticle of the emerging hair. The next 3 layers form the cuticle, Huxley layer, and Henle layer of the inner root sheath. These layers are further surrounded by the outer root sheath, which is an extension of the epidermis and becomes continuous with the epidermis in the upper portion of the follicle. External to the outer root sheath are the glassy membrane, corresponding to the basement membrane of the epidermis, and finally the connective tissue sheath. All 3 layers of the inner root sheath keratinize by means of eosinophilic trichohyaline granules and become fully keratinized and disintegrate at the level of the isthmus. The inner root sheath is responsible for providing the rigid support for the developing hair and its final shape, for instance, twisted hair follicles produce curly hairs. From the base of the hair follicle to the isthmus, the outer root sheath is covered by the inner root sheath, and it does not keratinize. In the isthmus, where the inner root sheath is no longer present, the outer root sheath undergoes trichilemmal cornification that is, without keratohyaline granules. In the infundibulum, the outer root sheath is identical to surface epidermis and undergoes keratinization with formation of keratohyaline granules.
Hair does not grow continuously but rather in cycles consisting of a growth phase, anagen; a transitional or involuting phase, catagen; and a resting phase, telogen. This cyclic activity is thought to be an adaptive response to seasonal variation in ambient temperature. The hair growth cycle varies between different species, breeds, body sites, and hair follicle type. A detailed study of the hair cycle in Beagle dogs revealed that 30% of the follicles were in anagen, 8% in catagen, and 27% in telogen. The hair cycle in the remaining follicles could not be assigned a specific stage.
In domestic animals, neighboring hairs cycle independently of each other and are in different stages of the hair cycle at any one time. Hair shaft length is directly related to the duration of anagen phase, which is preordained according to body region and genetics. At the onset of catagen, mitotic activity of matrix cells and melanin production by melanocytes of the hair bulb cease. The keratinocytes of the inferior segment of the follicle undergo a controlled process of involution via a burst of apoptosis. This results in the upward migration of the hair follicle and the lower follicle becoming a thin cord of epithelial cells surrounded by a fibrous root sheath. Growth of the inner root sheath stops so that the lower end of the hair shaft is surrounded by thick trichilemmal keratin. The thin cord of epithelial cells is surrounded by a thickened, corrugated glassy membrane, and as it retracts upward, it is followed by the shrunken, contracted papilla. In telogen phase, the base of the bulb is located at the level of attachment of the arrector pili muscle and is  of its former length. The base of the hair is encased in trichilemmal keratin and surrounded completely by outer root sheath (club hair). A population of stem cells (secondary hair germ) remains somewhere in the permanent portion of the hair follicle. These cells eventually reform the hair follicle during the next growth cycle. In rodents, the bulge region of the follicle appears to be the site that contains slow-cycling relatively undifferentiated cells from which arise a population of transient amplifying cells that become the matrix keratinocytes of the new hair bulb. The bulge region is an area on the outer root sheath at the base of the permanent portion of the hair follicle to which the arrector pili muscle attaches. Slow-cycling stem cells have been identified in the bulge region of canine hair follicles that share features with human bulge cells.
of its former length. The base of the hair is encased in trichilemmal keratin and surrounded completely by outer root sheath (club hair). A population of stem cells (secondary hair germ) remains somewhere in the permanent portion of the hair follicle. These cells eventually reform the hair follicle during the next growth cycle. In rodents, the bulge region of the follicle appears to be the site that contains slow-cycling relatively undifferentiated cells from which arise a population of transient amplifying cells that become the matrix keratinocytes of the new hair bulb. The bulge region is an area on the outer root sheath at the base of the permanent portion of the hair follicle to which the arrector pili muscle attaches. Slow-cycling stem cells have been identified in the bulge region of canine hair follicles that share features with human bulge cells.
Hair growth in many animals has been shown to be regulated by photoperiod, ambient temperature, various hormones, nutritional status, and general health. However, the exact mechanisms that control the cycle are incompletely understood. Growth and development of hair are influenced by many growth factors; these include fibroblast growth factor (FGF), epidermal growth factor (EGF), insulin-like growth factor-1 (IGF-1), transforming growth factor-β (TGF-β), and keratinocyte growth factor (KGF, same as FGF-7). Both IGF-1 and KGF are produced by the dermal papilla, and their receptors are found in the overlying anagen hair follicle matrix cells. Factors from the papilla mesenchymal cells are thought to act on a stem cell population in the permanent upper portion of the hair follicle. These competent cells respond to the signals from the papilla by growing deep into the dermis to form the full-length anagen hair follicle. Transition between anagen and catagen appears to be regulated by FGF-5.
The histologic appearance of the hair follicle changes considerably during the hair cycle. The hair cycle has been best characterized in the mouse because the follicles cycle together (i.e., synchronous stages of anagen, catagen, and telogen). In contrast, most companion animals have a mosaic cycle (i.e., hair follicles cycle into different stages independently of each other). Hair shafts are only produced in anagen. Anagen follicles have a well-developed, flame-shaped, plump dermal papilla (DP) that is capped completely by the hair bulb. The inner root sheath is fully developed. The bulb is located in the deep dermis or subcutis. A layer of columnar matrix cells lines the papilla, and melanocytes are dispersed among the matrix cells in pigmented hair follicles. Catagen, the intermediate remodeling stage, is short-lived and very difficult to assess on routine histology as it requires a perfectly sectioned follicle in a longitudinal plane. In catagen, the hair bulb is lost, and the follicular papilla devaginates. The inner root sheath is partially replaced by trichilemmal keratin. Catagen follicles have a thick glassy membrane and increased apoptotic cells. In dogs, catagen has been described as having an onion-shaped dermal papilla and a fibrous stalk that trails behind the DP. In telogen, the resting stage, the inner root sheath is replaced completely by trichilemmal cornification that anchors the club hair to the outer root sheath. The dermal papilla is located at the base of the follicle. Telogen may be further described as “haired telogen,” which has retention of the hair shaft, and “hairless telogen” or “kenogen,” in which a telogen follicle rests without a hair shaft.
Sinus hairs (tactile hairs, vibrissae) are highly specialized mechanoreceptors that respond to vibratory stimuli as well as static hair displacements. They are located on the muzzle (whiskers, vibrissae), face, throat, and palmar aspect of the carpus. They are thick, stiff hairs that are tapered distally. Histologically, they are composed of a large simple hair follicle surrounded by an endothelial cell-lined blood-filled sinus situated within the dermal connective tissue sheath. The sinus is supplied with numerous nerves, and skeletal muscles attach to the outer sheath of the follicle to confer some voluntary control of the hairs.
Sebaceous glands
Sebaceous glands are distributed throughout the haired skin of all mammals, with the exception of whales and porpoises, and are essential for maintaining normal skin and hair. The sebaceous glands have a long list of important functions, including production of sebum, photoprotection, thermoregulatory and repelling properties, wound healing, regulating the independent endocrine function of the skin, and the expression of vitamin D receptors and vitamin D–metabolizing enzymes. Sebaceous glands produce sebum, an oily secretion composed of triglycerides, phospholipids, and cholesterol. This material combines with epitrichial gland secretions to form an emulsion that coats the skin to act as a physical barrier to retain moisture and maintain normal hydration, and as a chemical barrier against microbial pathogens. In addition, the oily film coats the hair shafts to give them a glossy sheen; it also acts as a pheromone. Sebum also has proinflammatory and anti-inflammatory properties, antimicrobial activity, and transports anti-oxidants to and from the skin surface. Sebaceous glands also appear to be involved with normal hair development, because, in the absence of sebaceous glands, the hair shaft fails to separate normally from the sheath. For a more thorough discussion on all of the functions of the sebaceous glands, the reader is directed to the reference by Zouboulis et al. in the Further reading section.
Sebaceous glands consist of a solid mass of epithelial cells surrounded by a connective tissue sheath. The periphery of the gland consists of a single layer of cuboidal mitotically active cells resting on a basal lamina, analogous to basal cells of the epidermis. As the cells move inward toward the duct, they enlarge and accumulate lipid that is lost during routine processing. Sebaceous glands are holocrine glands, and their secretion is formed by decomposition of cells. This is brought about by release of lysosomal enzymes in cells nearest the duct, causing them to disintegrate and form sebum, which empties via a squamous epithelium-lined duct into the upper portion of the hair canal. All primary hairs and some secondary hairs have sebaceous glands. They are usually largest in areas with lowest hair follicle density, such as mucocutaneous junctions, interdigital spaces, coronet, and dorsal neck and rump. Sebaceous glands are especially numerous and well developed in the chin of cats (submental organ), dorsal surface of the tail in dogs and cats (tail gland), base of the horn in goats, and infraorbital, inguinal, and interdigital regions of sheep. The footpads and nasal planum are devoid of sebaceous glands, and they are rare in glabrous skin, where they empty directly to the skin surface.
Perianal glands
These are specialized secretory glands in the perianal regions, and they are commonly sites for the development of lesions.
-
•
Anal glands are specialized apocrine glands that open directly onto anal skin via a duct at the rectoanal junction. Similar apocrine glands line the anal sacs. The anal sacs are squamous epithelial-lined cystic cavities containing odoriferous secretions, presumably with some territorial marking function. They are present in many species, including domestic and wild felids, ferrets, raccoons, mink, rodents, pigs, and canids.
-
•
Hepatoid glands (also called circumanal, perianal glands) are presumed to be modified sebaceous glands based on histology, and are composed of small glands and nests of cells without a prominent ductular network. Islands of these glands are concentrated in the subcutis around the anus, but foci are commonly present over lateral and ventral aspects of the base of the tail, the dorsum of the tail, the dorsolumbosacral area, and prepuce. The glands are distinctive, composed of lobules of large eosinophilic epithelial cells (hepatoid cells) surrounded by low numbers of small basal reserve cells. Larger ducts, lined by stratified squamous epithelium, may be evident in neoplasms. These ducts are thought to regress during embryonal development, which leaves the glands largely ductless. Hepatoid glands are best described in the dog, and are most developed in entire males. Their function is uncertain, but they may have a role in steroid metabolism, in production of pheromones, and in territorial marking. Similar glands are also present in cats and in pericloacal glands of reptiles, where they probably have similar roles in territorial marking.
Sweat glands
Two types of sweat glands are present in the skin of mammals; they differ in origin, distribution, and possibly in the mode of secretion. These glands have been called apocrine and eccrine glands, but because of questions concerning the mechanism of the secretory process of these glands, the names epitrichial and atrichial glands have been proposed for apocrine and eccrine glands, respectively. Epitrichial (apocrine) sweat glands develop embryologically from primary hair germ, and they are distributed throughout all haired skin, usually deep to the sebaceous glands. Epitrichial glands are associated with primary hair follicles only, and they tend to be largest in areas with lower hair follicle density, such as mucocutaneous junctions, interdigital spaces, coronet, and dorsal midline. Sweat mixes with sebum to form the protective skin surface film. Epitrichial sweat glands function in thermoregulation only in horses and cattle. In other species, the secretion may contribute to scent that is involved in social communication. Epitrichial secretion may also provide a means of excreting waste products and secreting immunoglobulins that are present on the skin surface. They are simple saccular or tubular glands with a coiled secretory portion and straight duct. The secretory portion is composed of a single row of flat cuboidal to columnar epithelial cells surrounded by a single layer of myoepithelial cells situated between the secretory cells and basal lamina. The duct empties into the pilary canal, usually above the entrance of the sebaceous duct or, rarely, directly to the skin surface. The name apocrine refers to the mode of secretion, which was originally thought to involve pinching off (apo = off) of a portion of the cell. The existence of an apocrine secretory process has been questioned; however, ultrastructural examination of these glands in humans, pigs, horses, and dogs indicates that several modes of secretion are involved, including the apocrine type.
In contrast to epitrichial glands, atrichial (eccrine) sweat glands are derived from the embryonal epidermis rather than from the primary hair germ, and they are located only in specialized areas. They occur in the pawpad of dogs and cats, frog of ungulates, snout of pigs, planum nasolabiale of cattle, and medial surface of the carpus of pigs (carpal glands). The function of eccrine glands is uncertain. The secretion may be involved with scent signaling, and in the footpad of cats, it may improve frictional capacity of the paw. Atrichial glands are histologically similar to apocrine glands, but their ducts open directly to the skin surface. There is no recent detailed examination of eccrine gland secretion to identify the mode of secretion conclusively.
Subcutis
The deepest layer of the skin is the subcutis. It is composed of lipocytes subdivided into lobules by thin bands of collagen and small vessels. The collagenous septa provide structural support by compartmentalizing the subcutis and anchoring the dermis to the fascial planes deep to the subcutis.
Further reading
Al-Bagdadi FK, et al. Histology of the hair cycle in male beagle dogs. Am J Vet Res 1979;40:1734-1741.
Atoji Y, et al. Circumanal glands of the dog: a new classification and cell degeneration. Anat Rec 1998;250:251-267.
Borradori L, Sonnenberg A. Structure and function of hemidesmosomes: more than simple adhesion complexes. J Invest Dermatol 1999;112:411-418.
Bos JD, Kapsenberg ML. The skin immune system: progress in cutaneous biology. Immunol Today 1993;14:75-78.
Danilenko DM, et al. Keratinocyte growth factor is an important endogenous mediator of hair follicle growth, development, and differentiation. Normalization of the nu/nu follicular differentiation defect and amelioration of chemotherapy-induced alopecia. Am J Pathol 1995;147:145-154.
de Mora F, et al. The role of mast cells in atopy: what can we learn from canine models? A thorough review of the biology of mast cells in canine and human systems. Br J Dermatol 2006;155:1109-1123.
Foster AP. A study of the number and distribution of cutaneous mast cells in cats with disease not affecting the skin. Vet Dermatol 2008;5:17-20.
Gargiulo AM, et al. The process of secretion in swine apocrine sweat glands. Anat Histol Embryol 1990;19:264-268.
Hill PB, Martin RJ. A review of mast cell biology. Vet Dermatol 1998;9:145-166.
Iwasaki T. An electron microscopic study on secretory process in canine apocrine sweat gland. Jpn J Vet Sci 1981;43:733-740.
Kobayashi T, et al. Canine follicle stem cell candidates reside in the bulge and share characteristic features with human bulge cells. J Invest Dermatol 2010;130:1988-1995.
Kube P, et al. Distribution, density and heterogeneity of canine mast cells and influence of fixation techniques. Histochem Cell Biol 1998;110:129-135.
Lavker RM, et al. Hair follicle stem cells: their location, role in hair cycle, and involvement in skin tumor formation. J Invest Dermatol 1993;101:16S-26S.
Marinkovich MP. The molecular genetics of basement membrane diseases. Arch Dermatol 1993;129:1557-1565.
Messenger AG. The control of hair growth: an overview. J Invest Dermatol 1993;101:4S-9S.
Meyer W, et al. Cytological and lectin histochemical characterization of secretion production and secretion composition in the tubular glands of the canine anal sacs. Cells Tissues Organs 2001;168:203-219.
Miller WH, et al. Structure and function of the skin. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013.
Müntener T, et al. The canine hair cycle—a guide for the assessment of morphological and immunohistochemical criteria. Vet Dermatol 2011;22:383-395.
Müntener T, et al. Canine noninflammatory alopecia: a comprehensive evaluation of common and distinguishing histological characteristics. Vet Dermatol 2012;23:206-e44.
Nishifuji K, Yoon JS. The stratum corneum: the rampart of the mammalian body. Vet Dermatol 2013;24:60-72.
Paus R, Cotsarelis G. The biology of hair follicles. N Engl J Med 1999;341:491-497.
Robert C, Kupper TS. Inflammatory skin diseases, T cells, and immune surveillance. N Engl J Med 1999;341:1817-1827.
Stenn KS, et al. Hair follicle growth controls. Dermatol Clin 1996;14:543-558.
Sture GH, et al. Ovine mast cell heterogeneity is defined by the distribution of sheep mast cell proteinase. Vet Immunol Immunopathol 1995;48:275-285.
Suter MM, et al. Review article. Keratinocyte biology and pathology. Vet Dermatol 1997;8:67-100.
White SD, Yager JA. Resident dendritic cells in the epidermis: Langerhans cells, Merkel cells and melanocytes. Vet Dermatol 1995;6:1-8.
Zouboulis CC, et al. Frontiers in sebaceous gland biology and pathology. Exp Dermatol 2008;17(6):542-551.
Dermatohistopathology
The pathology of the skin, more than that of any other organ, has a specialized vocabulary. Many gross and histologic changes are unique to the skin. The pathologist must communicate proper terminology of both gross and histologic lesions to interpret lesions.
Glossary: histologic terms
Acantholysis refers to a loss of cohesion between individual keratinocytes resulting from a breakdown of the intercellular bridges (desmosomes). Acantholytic cells are individualized round cells with a central nucleus that is rimmed by condensed eosinophilic cytoplasm (Fig. 6-1 ). Acantholysis is the hallmark of the pemphigus complex. It can also result from proteolytic enzymes released by neutrophils or eosinophils in an inflammatory process. In domestic animals, acantholysis is most commonly manifested within pustules and crusts of pemphigus foliaceus.
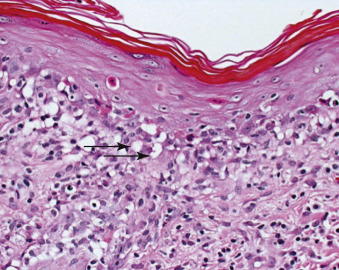
Figure 6-1.
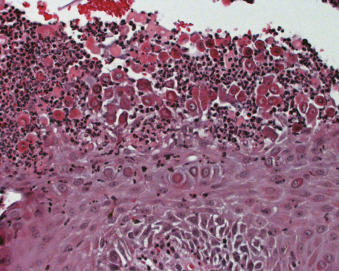
Acantholysis in pemphigus foliaceus. Loss of cohesion between keratinocytes leads to individualization of cells. Note that the acantholytic cells have normal nuclear morphology.
Acanthosis specifically indicates an increased thickness of the stratum spinosum, and is the result of hyperplasia and occasionally hypertrophy of cells of the stratum spinosum. Acanthosis, however, is often used synonymously with hyperplasia when referring to the epidermis.
Apoptosis refers to individual programmed cell death. It is usually seen in the basal layer but can be seen in any layer of the epidermis. Apoptotic keratinocytes are eosinophilic and shrunken. They are sometimes referred to as apoptotic bodies (colloid bodies, hyaline bodies). In general, the term Civatte body refers to an apoptotic keratinocyte in the stratum basale. The term “dyskeratosis” has been previously used to describe premature or abnormal keratinization of individual keratinocytes; however, apoptosis is most likely the underlying process as the histologic features are indistinguishable from each other.
Atrophy, in regard to the epidermis, is assessed by decreased thickness of the nucleated layers. An early sign of epidermal atrophy is the loss of the rete ridges in areas of skin, where they are normally present. Atrophy can be difficult to interpret as the normal epidermis in the haired skin of domestic animals is naturally thin. Atrophy is most commonly seen with hypercortisolemia (topical or systemic) and chronic ischemia. Dermal atrophy is thinning of dermal collagen fibrils resulting in decreased dermal thickness.
Ballooning degeneration of the epidermis is the result of intracellular edema (Fig. 6-2 ). It is characterized by swollen eosinophilic cytoplasm, enlarged or condensed nuclei, and a loss of cohesion, resulting in acantholysis and sometimes vesicle formation. Ballooning degeneration is a characteristic feature of viral infections, particularly of herpesviruses and poxviruses.
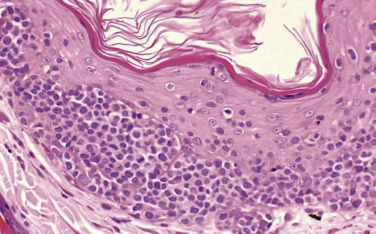
Figure 6-2.
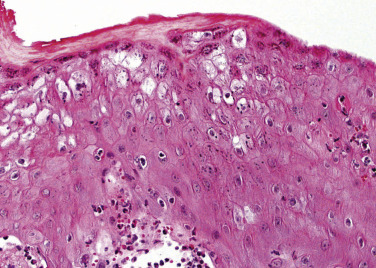
Ballooning degeneration in viral dermatitis. Keratinocytes are enlarged and pale because of marked intracellular edema.
Clefts are slit-like spaces within the epidermis or at the dermoepidermal junction. Clefts may be caused by acantholysis or hydropic degeneration of basal cells. However, clefts may also result from handling artifacts (Fig. 6-3 ).
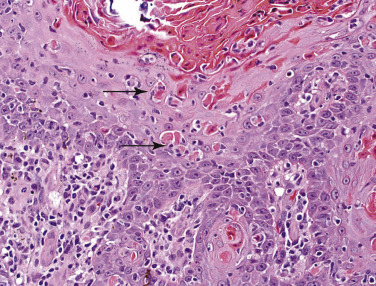
Figure 6-3.
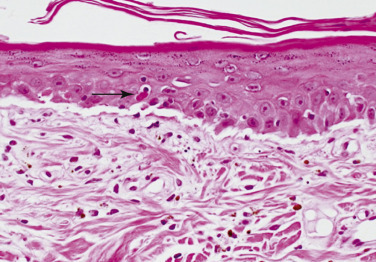
Subepidermal cleft in dermatomyositis. There is separation of the epidermis from the dermis by a clear space. Note the shrunken, darkly staining necrotic (apoptotic) keratinocytes with hypereosinophilic cytoplasm and pyknotic nuclei (arrow).
Collagen degeneration is a term that has been replaced by “collagen flame figure” or “flame figure.” Collagen flame figures are characterized by dermal deposition of amorphous eosinophilic material on collagen fibers with an infiltrate of eosinophils. The collagen fibrils have a frayed appearance. Ultrastructurally, flame figures contain degranulated eosinophils, but the collagen fibrils have a normal (i.e., not degenerate) periodicity. In chronic lesions, the eosinophil content decreases, histiocytes increase in number, and palisading granulomas may be formed. Flame figures may be seen in eosinophilic granuloma, insect-/arthropod-bite reactions, and other eosinophil-rich conditions, such as mast cell tumors.
Crust is a gross and histologic term that refers to consolidated, desiccated surface exudate that contains keratin, serum, cellular debris, and often microorganisms. Crusts are described on the basis of their composition: serous (mostly serum), hemorrhagic (mostly blood), cellular (mostly inflammatory cells), and serocellular (a mixture of serum and inflammatory cells). Crusts should be examined closely for dermatophyte spores and hyphae, Dermatophilus congolensis, and acantholytic keratinocytes, which can be indicators of superficial pemphigus.
Dermal edema is recognized by dilated lymphatics (not visible in normal skin), widened spaces between blood vessels and perivascular collagen (perivascular edema), or widened spaces between dermal collagen fibers (interstitial edema). The dilated lymphatics and widened perivascular and interstitial spaces may or may not contain lightly eosinophilic, homogeneous, proteinaceous fluid. Dermal edema is a common feature of any inflammatory dermatosis. Severe edema of the superficial dermis may result in subepidermal vesicles and bullae, necrosis of the overlying epidermis, and predisposition to artifactual dermoepidermal separation during handling and processing of biopsy specimens. Severe edema of the superficial dermis may result in vertical orientation and stretching of collagen fibers, producing the “gossamer” (web-like) collagen effect seen in severe urticaria.
Desmoplasia usually refers to fibroplasia and collagenous stroma induced by neoplastic processes.
Dyskeratosis is premature or abnormal keratinization of individual keratinocytes in the epidermis or follicular epithelium. Histologically, dyskeratotic cells are eosinophilic and shrunken, with condensed, dark-staining nuclei. Dyskeratosis may be seen in a number of dermatoses, including lupus erythematosus, erythema multiforme, and graft-versus-host disease. It can also occur in neoplastic dermatoses, especially papillomas. Dyskeratosis is a feature of the severe epidermal dysplasia that precedes the development of some squamous cell carcinomas.
Dysplasia refers to faulty or abnormal development of the epidermis, hair follicles, or any component of the skin. It is an abnormal but nonneoplastic change; however, it can accompany or precede neoplastic changes.
Dystrophic mineralization is the deposition of calcium salts as basophilic, amorphous, granular material along collagen fibrils, as in hyperglucocorticism. Dystrophic mineralization of the hair follicle basement membrane can be seen in hyperglucocorticism, in dogs receiving exogenous glucocorticoids, and as a senile change in dogs, especially in Poodles.
Epidermal mast cells are frequently seen in biopsies from cats with inflammatory dermatoses. They are found within the epidermis as well as the hair follicle outer root sheath, and are most commonly found in diseases associated with tissue eosinophilia, such as feline eosinophilic plaque and feline eosinophilic granuloma, and thus are associated with allergic skin disease in cats.
Exocytosis is the migration of inflammatory cells and/or erythrocytes through the intercellular spaces of the epidermis. Exocytosis of inflammatory cells is a common feature of any inflammatory dermatosis. Exocytosis of neutrophils implies an infectious process, whereas exocytosis of eosinophils suggests a hypersensitivity reaction, such as ectoparasitism and feline eosinophilic plaque. Exocytosis of erythrocytes implies purpura, severe vasodilation, or trauma.
Festoons are dermal papillae devoid of attached epidermal cells that project into a vesicle or bulla. Festoons can be seen in mechanobullous disorders, such as epidermolysis bullosa or bullous pemphigoid.
Fibrinoid degeneration or fibrinoid necrosis typically refers to the deposition of amorphous eosinophilic material resembling fibrin in the walls of blood vessels. The fibrinoid change results in loss of structural detail and may be accompanied by necrotic cell debris or leukocytoclasia.
Fibroplasia is a reactive process and is the formation and development of fibrous tissue resulting from an increased number of fibroblasts.
Flame follicles are catagen and telogen follicles with pronounced eosinophilic trichilemmal keratin (Fig. 6-4 ). These can be seen in endocrinopathies, hair cycle arrest, and are also prominent in normal haired skin of plush-coated breeds of dog, such as the Nordic breeds and Pomeranians.
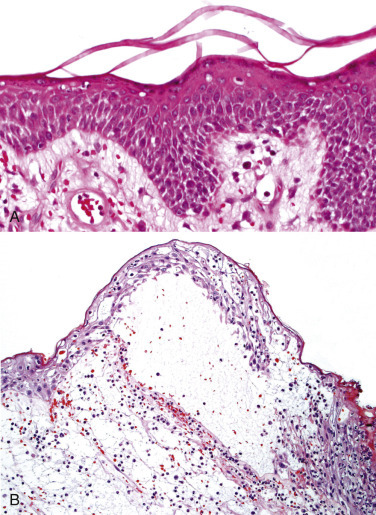
Figure 6-4.
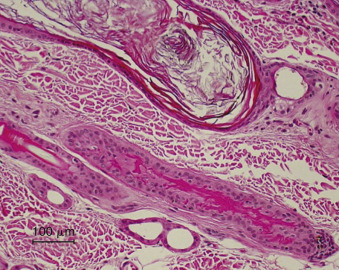
Flame follicle in canine alopecia X. The follicle has pronounced eosinophilic trichilemmal cornification. The keratin has a serrated border resembling a flickering flame.
Follicular atrophy refers to the gradual involution and disappearance of hair follicles characteristic of hormonal dermatoses, follicular dysplasia, and ischemia.
Follicular dysplasia (also known as follicular dystrophy) refers to the inability to produce structurally normal hair follicles and hair shafts. Examples include black hair follicular dysplasia and color-dilution alopecia.
Follicular keratosis refers to the distention of hair follicle infundibula by keratin.
Folliculitis is inflammation of the hair follicle. It can further be divided into mural folliculitis (inflammation of the follicular epithelium) (Fig. 6-5A ), luminal folliculitis (inflammation in the follicular lumen) (Fig. 6-5B), and perifolliculitis (inflammation around but not significantly impinging on the follicle) (Fig. 6-5C).
Figure 6-5.
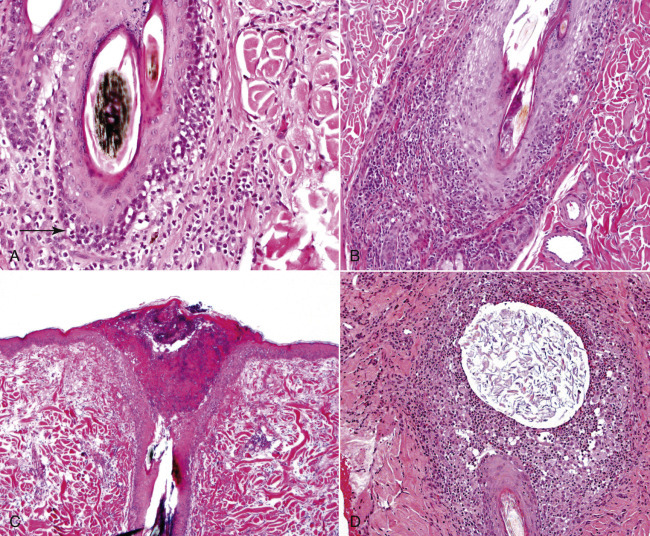
Folliculitis. A. Idiopathic mural folliculitis in a dog. Note the wall of the hair follicle is infiltrated by mononuclear leukocytes (arrow). B. Perifolliculitis and mural folliculitis in demodicosis. Note the periadnexal inflammatory infiltrate. C. Luminal folliculitis in staphylococcal pyoderma. D. Furunculosis in bacterial folliculitis. The wall of the follicle has been perforated, and follicular contents are in the dermis.
Furunculosis is inflammation of the hair follicle that has resulted in destruction of the follicular epithelium and release of the luminal contents into the dermis, causing dermal inflammation (Fig. 6-5D, 6-6 ). This can be seen in any process that is destructive to hair follicles, such as bacterial infection, dermatophytosis, demodicosis, and trauma.
Figure 6-6.
Furunculosis. Higher magnification of Figure 6-5D. Note the abundant free keratin surrounded by pyogranulomatous inflammation.
Granulation tissue is the result of a reparative process characterized by neovascularization and a proliferation of fibroblasts within a proteoglycan rich matrix. It is named for the pink granular appearance of a wound bed. The blood vessels have plump endothelial cells and are oriented perpendicular to the surface of the skin. Fibroblasts and collagen fibrils are oriented parallel to the surface of the skin.
Grenz zone is a zone of relatively normal collagen that separates the epidermis from an underlying dermal alteration. The presence or absence of a grenz zone is a criterion used in the diagnosis of neoplastic conditions (e.g., plasmacytomas often have a prominent grenz zone, whereas histiocytomas abut the dermoepidermal junction).
Hamartoma is a tumor-like malformation composed of an abnormal mixture of normal tissue elements or an abnormal proportion of a single element. Unlike a choristoma, the components of a hamartoma are normal to the location. By definition, hamartomas are congenital lesions; however, they may not be detected until later in life, and the term is often used interchangeably with nevus. The term “nevus” refers to focal malformation of the skin, congenital or tardive in onset, caused by an embryonic failure of normal development. Hamartoma is the term preferred in veterinary dermatopathology; however, there are a few conditions where “nevus” is ingrained in the veterinary literature.
Hidradenitis is inflammation of epitrichial (apocrine) sweat glands. These glands commonly become involved secondarily in suppurative and granulomatous dermatoses. Periglandular accumulation of plasma cells is commonly seen in chronic pyoderma and acral lick dermatitis.
Horn cysts (keratin cysts) are epidermal cysts that contain concentric layers of keratin and are lined by attenuated keratinocytes. Horn cysts are features of some follicular and epithelial tumors. Pseudohorn cysts are keratin-filled, cyst-like structures formed by the irregular invagination of a hyperplastic, hyperkeratotic epidermis, having a cystic appearance because of cross-sectioning. They are seen in numerous hyperplastic or neoplastic epidermal dermatoses.
Keratin pearls (horn pearls, squamous pearls) are focal, circular, concentric layers of squamous cells showing gradual keratinization toward the center, often accompanied by cellular atypia and dyskeratosis. Keratin pearls are commonly seen in squamous cell carcinoma.
Hypergranulosis indicates increased thickness of the stratum granulosum, often accompanied by larger, more intensely stained granules. Hypergranulosis may be seen in any dermatosis in which there is epidermal hyperplasia.
Hyperkeratosis refers to increased thickness of the stratum corneum. It can be either orthokeratotic (without nuclei) (Fig. 6-7A ), or parakeratotic (nuclei retained) (Fig. 6-7B). Hyperkeratosis and orthokeratosis are sometimes used synonymously. Orthokeratosis can be divided into basket weave (the normal pattern in the stratum corneum), compact, and laminated. Basket weave orthokeratosis is the most common form and is seen in many conditions, including hypersensitivities, endocrinopathies, and cornification disorders. Compact orthokeratosis is a feature of long-standing surface trauma. Laminated orthokeratosis characterizes ichthyosis. Orthokeratosis and parakeratosis are not mutually exclusive and are often seen in the same section of hyperkeratotic skin. Diffuse parakeratosis can be seen in many chronic dermatoses, especially zinc-responsive dermatosis, dermatophilosis, superficial necrolytic dermatitis, and thallotoxicosis.
Figure 6-7.
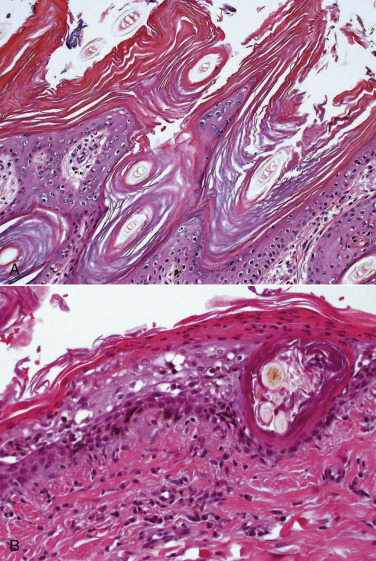
A. Orthokeratotic hyperkeratosis in nonepidermolytic ichthyosis. The stratum corneum is expanded by laminated layers of compact anuclear keratin. B. Parakeratotic hyperkeratosis in superficial necrolytic dermatitis. The corneal layer is expanded by nucleated corneocytes.
Hyperpigmentation refers to increased melanin within the epidermis and, often, concurrently in dermal melanophages. Hyperpigmentation may be focal or diffuse, and confined to the stratum basale or present throughout all epidermal layers. It is a common nondiagnostic finding in chronic inflammatory and hormonal dermatoses, as well as in some developmental and neoplastic disorders. Hyperpigmentation must always be cautiously assessed with regard to the animal's normal pigmentation.
Hyperplasia is an increase in the number of cells. In reference to the epidermis, it refers to an increased number of keratinocytes. Epidermal hyperplasia is a common feature of almost all chronic inflammatory conditions. Acanthosis is a term often used synonymously with epidermal hyperplasia. Epidermal hyperplasia may be further specified as irregular (in which the hyperplastic rete ridges are uneven in shape and height), regular or psoriasiform (in which the hyperplastic rete ridges are of even thickness and length), papillated (digitate projections of the epidermis above the skin surface), and pseudocarcinomatous (extreme, irregular hyperplasia that may demonstrate increased mitotic activity and branched or fused rete pegs) (Fig. 6-8 ). The process may resemble squamous cell carcinoma; however, there is no cellular atypia, and the basement membrane remains intact.
Figure 6-8.
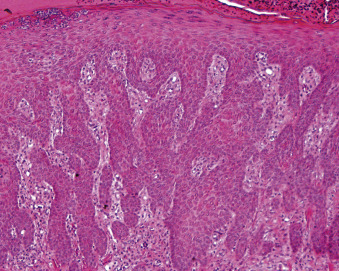
Pseudocarcinomatous epidermal hyperplasia. The epidermis has marked irregular hyperplasia with branched or fused rete pegs. The basement membrane is intact, and there is no cellular atypia.
Hypopigmentation refers to decreased melanin in the epidermis. It may be associated with congenital or acquired idiopathic defects in melanization (leukoderma, vitiligo), toxic effects of certain chemicals on melanocytes (e.g., monobenzylether of dihydroquinone in rubbers and plastics), inflammatory disorders that affect melanization or destroy melanocytes, hormonal disorders, and dermatoses featuring hydropic degeneration of basal cells (e.g., lupus erythematosus).
Intracellular edema of the epidermis is characterized by increased size, cytoplasmic pallor, and, sometimes, displacement of the nucleus to the periphery of the affected cell. Intracellular edema of the epidermis may affect cells in a laminar fashion, leading to horizontal layers of edematous keratinocytes. Severe intracellular edema may result in reticular degeneration and intraepidermal vesicles. Intracellular edema is a common feature of any acute or subacute inflammatory dermatosis. Hydropic degeneration is a specific type of intracellular edema restricted to the basal layer and basal keratinocytes of the outer root sheath of hair follicles. Hydropic degeneration may result in intrabasal clefts or vesicles, or subepidermal clefts or vesicles because of dermoepidermal separation. It is characterized by clear vacuoles within basal keratinocytes, sometimes accompanied by individual keratinocyte necrosis (Fig. 6-9 ). Vacuolar degeneration is sometimes seen in conjunction with hydropic degeneration and refers to vacuoles above and below the basement membrane zone. Hydropic degeneration of basal cells can be seen in lichenoid dermatitides, drug eruptions, lupoid dermatoses, and dermatomyositis. Caution must be exercised not to confuse freezing artifact or delayed fixation artifact with intracellular edema.
Figure 6-9.
Hydropic degeneration. Clear spaces (arrows) are present within and below basal keratinocytes.
Lymphoid nodules are well-circumscribed, rounded, dense, sometimes perivascular accumulations of predominantly mature lymphocytes in the deep dermis and/or subcutis. They are uncommon and seen primarily in the cat. They are seen most frequently in conjunction with immune-mediated dermatoses, dermatoses associated with tissue eosinophilia, and in panniculitis, such as injection-site panniculitis. They can also be seen in insect-bite granuloma (pseudolymphoma).
Mucinosis (myxedema, myxoid degeneration, mucoid degeneration) is an accumulation of dermal ground substance that appears as slightly granular, basophilic material that separates, thins, or replaces dermal collagen fibers and surrounds blood vessels and appendages in H&E-stained sections. Only small amounts of mucin are visible in normal skin. Mucin is more easily demonstrated with stains for glycosaminoglycans, such as Alcian blue and colloidal iron. Mucinous degeneration may be seen as a focal process in numerous inflammatory, neoplastic, and developmental dermatoses. Diffuse mucinosis is a feature of normal skin of the Chinese Shar-Pei dog.
Multinucleated keratinocytes can occasionally be seen in infections by viruses, such as herpesvirus, canine distemper virus, and feline leukemia virus.
Munro's microabscess is a small, desiccated accumulation of neutrophils within the stratum corneum.
Necrosis is the death of cells or tissues. Necrotic keratinocytes are identified by loss of intercellular bridges with resultant rounding up of the cell, and a normal-sized or swollen eosinophilic cytoplasm. The nucleus becomes pyknotic, cytoplasm becomes eosinophilic and homogeneous, and the cell loses its normal shape. Apoptosis is often used synonymously with individual keratinocyte death that may occur from a variety of processes. Individual keratinocyte necrosis can occur in erythema multiforme, graft-versus-host disease, and interface dermatoses. Necrosis of the epidermis or dermis may be more extensive due to physical and chemical injury, or to interference with vascular supply.
Nests (theques) are well-circumscribed clusters or groups of cells within the epidermis and/or the dermis. Epidermal nests are often seen in melanocytic neoplasms.
Panniculitis (steatitis) refers to inflammation of subcutaneous fat. It can occur without significant involvement of the overlying dermis and epidermis (e.g., sterile nodular panniculitis, feline nutritional steatitis), or can be involved by extension of inflammation of the dermis. Fat micropseudocyst formation and lipocytes containing radially arranged needle-shaped clefts can be seen with subcutaneous fat sclerosis and idiopathic sterile panniculitis.
Papillomatosis refers to the projection of dermal papillae and epidermis above the surface of the skin, resulting in an irregular undulating configuration of the epidermis. Papillomatosis is associated with epidermal hyperplasia and is seen with chronic inflammatory and neoplastic dermatoses.
Pautrier's microabscess is a small, focal accumulation of abnormal lymphoid cells in the epidermis or follicular epithelium, typical of epitheliotropic lymphoma (Fig. 6-10 ).
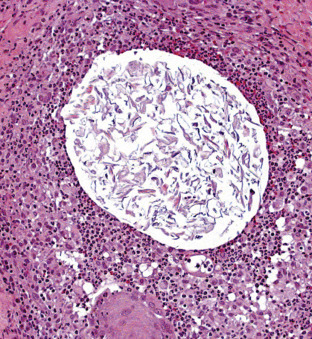
Figure 6-10.
Pautrier's microabscess in epitheliotropic lymphoma. Aggregates of neoplastic lymphocytes reside within the epidermis.
Pigmentary incontinence refers to the presence of melanin granules free within the subepidermal dermis and within dermal macrophages (melanophages). It can result from any process that damages the stratum basale, especially hydropic degeneration of basal cells (lichenoid dermatoses, lupus erythematosus, dermatomyositis, erythema multiforme).
Reticular degeneration is caused by severe intracellular edema of epidermal cells. These cells burst, resulting in multilocular intraepidermal vesicles whose septa are formed by resistant cell walls. It may be seen with any acute or subacute inflammatory dermatosis, such as acute contact dermatitis.
Satellitosis refers to individual necrotic keratinocytes in the epidermis surrounded by lymphoid cells (satellite cells) (Fig. 6-11 ). It is a characteristic finding in erythema multiforme and occasionally is seen in other interface dermatoses.
Figure 6-11.
Satellitosis in erythema multiforme. Lymphocytes (arrows) surround individually necrotic (apoptotic) keratinocytes.
Sclerosis (scar) is the end point of fibrosis. Increased numbers of collagen fibers have a thick, eosinophilic, hyalinized appearance, and the number of fibroblasts is greatly reduced.
Sebaceous gland hyperplasia refers to increased numbers of sebaceous glands and is common in chronic inflammatory conditions. Generalized sebaceous gland hyperplasia is a histologic feature seen in many chronic inflammatory conditions. Nodular aggregates of hyperplastic sebaceous glands form exophytic firm papules. These lesions are common and often multifocal in aged dogs.
Spongiform pustule of Kogoj is a multilocular accumulation of neutrophils within a sponge-like area of the stratum granulosum and stratum spinosum.
Spongiosis (intercellular edema) of the epidermis is characterized by widening of the intercellular spaces with accentuation of the intercellular bridges, giving the epidermis a “spongy” appearance (Fig. 6-12A ). Severe intercellular edema may lead to rupture of the intercellular bridges and the formation of intraepidermal vesicles (Fig. 6-12B). Severe spongiotic vesicle formation may disrupt the basement membrane zone in some areas and form subepidermal vesicles. Intercellular edema is a common feature of acute or subacute inflammatory dermatoses. Diffuse spongiosis, which also involves the hair follicle outer root sheath, may be seen in other inflammatory disorders, including feline eosinophilic plaque or granuloma.
Figure 6-12.
Spongiosis. A. Extracellular edema results in widening of intercellular spaces between keratinocytes. B. Spongiosis with vesicle formation. Marked intercellular edema has led to breakdown of intercellular bridges and vesicle formation.
Squamous eddies are whorl-like patterns of squamous cells with no atypia, dyskeratosis, or central keratinization. Squamous eddies are features of numerous neoplastic and hyperplastic epidermal disorders.
Transepidermal elimination is a mechanism by which foreign or altered constituents can be removed from the dermis. This can be illustrated by the elimination of mineralized collagen across the epidermis and follicular epithelium in calcinosis cutis.
Vesicle is a fluid-filled blister <1.0 cm in diameter. They may be subcorneal, suprabasilar, subepidermal, or immediately below the epidermis. When these lesions contain large numbers of inflammatory cells, they may be referred to as vesicopustules.
Villus is a dermal papilla covered by 1 or 2 layers of epidermal cells that projects into the base of a vesicle or bulla. Villi are seen in pemphigus vulgaris and warty dyskeratoma.
Gross terminology
Bullae are collections of fluid within or below the epidermis >1.0 cm in diameter. They may be caused by severe intercellular or intracellular edema, ballooning degeneration, acantholysis, hydropic degeneration of basal cells, subepidermal edema, or other factors resulting in dermoepidermal separation, such as the autoantibodies in bullous pemphigoid.
Callus is a thickened, often pigmented, and hyperkeratotic plaque that occurs in areas of chronic pressure trauma or friction (e.g., elbow callus in large-breed dogs).
Comedo is a cystically dilated, keratin-filled hair follicle. Comedones are characteristically seen in Schnauzer comedo syndrome, some endocrine dermatopathies, and actinic dermatosis.
Dells are small depressions or hollows in the surface of the epidermis independent of adnexal structures. They are usually associated with focal epidermal atrophy and orthokeratotic hyperkeratosis. This term is not commonly used in veterinary dermatology.
Epidermal collarette is a special type of loose scale that is arranged in a circular pattern around a central area of erythema or hyperpigmentation. Epidermal collarettes most likely represent ruptured pustules or papules from bacterial folliculitis.
Eschar is a thick crust that forms in association with an ulcer and is tightly adherent to the skin because of the incorporation of dermal collagen (e.g., thermal burn).
Lichenification is exaggeration of the normal skin markings resulting from long-standing surface trauma or friction (e.g., axilla in chronic atopic dermatitis). Lichenified areas are often hyperpigmented.
Macules are nonraised lesions of <1.0 cm diameter in which the color differs from that of the surrounding normal skin (e.g., black macules in feline lentigo simplex). A patch is a macule that measures >1 cm.
Papules are solid, circumscribed, elevations in the skin that are <1 cm in diameter. Papules can be follicular (e.g., staphylococcal folliculitis) or nonfollicular (e.g., flea-bite hypersensitivity).
Plaques are solid, slightly raised elevations in the skin that are >1 cm in diameter (e.g., feline eosinophilic plaque).
Pustules can be gross or microscopic accumulations in skin that are filled with inflammatory cells, usually neutrophils or eosinophils. Grossly, pustules, as in papules, can be follicular or nonfollicular (e.g., superficial pemphigus).
Scale refers to a flat plate of stratum corneum (e.g., Golden Retriever ichthyosis). It is important to distinguish scale versus crust on physical examination.
Wheal is a firm, circumscribed, raised elevation in the skin, composed of edema and is often erythematous (e.g., equine urticaria).
Pattern analysis
Used commonly in the diagnoses of neoplasms, a system of pattern analysis is also applied to inflammatory/nonneoplastic dermatoses. Most dermatologic lesions can be grouped into 1 of 10 histologic patterns on low magnification. It is far more efficient for a dermatopathology trainee to use pattern recognition to generate a list of differentials than to learn by memorizing the histologic features of each disease. Unlike “tumor” biopsies, where the name of the neoplasm is given (e.g., squamous cell carcinoma), most skin biopsies generate a morphologic diagnosis and comment that will aid the clinician in making therapeutic choices.
The pathologist must be aware of the normal features of the species and the specific site being examined. The specimen is initially perused at scanning magnification to determine the dermatopathologic pattern. At higher magnification, additional features (e.g., cell type: lymphocytic, histiocytic, neutrophilic, eosinophilic, plasmacytic) will be used to narrow the differential diagnosis. It is not unusual to see more than one pattern of inflammation in a biopsy. For instance, it is quite common to have a hyperplastic perivascular pattern in allergic skin disease along with a superficial pustular pattern of pyoderma. It can be difficult to gauge the importance of each pattern within the biopsy. Some patterns are more specific than others; there are far fewer differentials for interface dermatitis than perivascular dermatitis.
Perivascular dermatitis
Perivascular dermatitis is the least specific pattern of inflammation, and it is necessary to observe the type of leukocyte involved and the epidermal changes to create a differential list. In perivascular dermatitis, the predominant inflammatory reaction is centered on the superficial or deep dermal blood vessels, or both. Most perivascular dermatitides involve predominantly the superficial dermal blood vessels. In the horse and cat, most perivascular dermatitis is both superficial and deep. The primary cause of superficial perivascular dermatitis is a hypersensitivity reaction, although chronic bacterial infections, viral infections, cornification disorders, and metabolic disease can all demonstrate this pattern at some point during evolution of the condition. Perivascular infiltrates containing eosinophils should first be suspected of representing dermatitis, such as ectoparasitism, food allergy, or atopy. Focal areas of eosinophilic exocytosis and necrosis (“epidermal nibbles”) are suggestive of ectoparasitism. Other perivascular dermatitides that may contain eosinophils include zinc-responsive dermatosis, equine multisystemic eosinophilic epitheliotropic disease, and chronic pyoderma. Perivascular dermatitis is subdivided on the basis of accompanying epidermal changes into 4 types:
-
•
In pure perivascular dermatitis, there are few or no epidermal changes. The most common dermatoses in this category include acute hypersensitivity reactions and urticaria (Fig. 6-13 ).
-
•
Perivascular dermatitis with spongiosis is characterized by various degrees of spongiosis and spongiotic vesicle formation. Severe spongiotic vesiculation may disrupt the basement membrane zone, resulting in subepidermal vesicles. The epidermis has variably severe hyperkeratosis and hyperplasia. The most common dermatoses in this category include hypersensitivity reactions, acute contact or irritant dermatitis, ectoparasitism, feline eosinophilic plaque, feline miliary dermatitis, and viral infections. When the hair follicle outer root sheath is also involved, feline allergic dermatitides, such as feline eosinophilic plaque and feline eosinophilic granuloma, are suggested.
-
•
Perivascular dermatitis with epidermal hyperplasia is characterized by various degrees of epidermal hyperplasia and hyperkeratosis with little or no spongiosis. This is a common, nondiagnostic, chronic reaction pattern. The most common dermatoses in this category are chronic hypersensitivity reactions, acral lick dermatitis, and any dermatitis that has undergone chronic irritation and trauma.
-
•
Perivascular dermatitis with hyperkeratosis is characterized by various degrees of either orthokeratosis or parakeratosis. The presence of parakeratosis suggests zinc-responsive dermatosis, chronic ectoparasite hypersensitivity, or Malassezia dermatitis.
Figure 6-13.
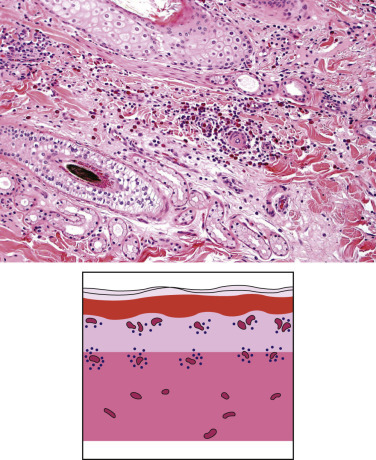
Histologic and schematic appearance of superficial perivascular dermatitis.Culicoides insect-bite hypersensitivity in a horse. Note leukocytes, in this case eosinophils, surrounding dermal vessels.
Interface dermatitis
Interface dermatitis is characterized by damage to the basal layer of keratinocytes, such as basal cell degeneration or necrosis of keratinocytes that obscures the dermoepidermal junction. This pattern can be divided into interface cell poor (interface changes with minimal superficial dermal inflammation) or interface lichenoid (interface changes with a lichenoid band of mononuclear inflammation). Pigmentary incontinence and apoptotic bodies are commonly seen in both types.
-
•
The cell-poor interface pattern can be seen in diseases such as dermatomyositis, ischemic dermatopathy, erythema multiforme, drug eruptions, graft-versus-host reactions, bovine viral diarrhea, and bovine pseudolumpy skin disease.
-
•
The lichenoid interface pattern is seen with discoid lupus erythematosus, cutaneous exfoliative lupus erythematosus, vesicular lupus erythematous, idiopathic lichenoid dermatoses, lichenoid keratoses, Vogt-Koyanagi-Harada (VKH)-like syndrome (uveodermatologic syndrome), lichenoid psoriasiform dermatosis of Springer Spaniels, cyclosporine-associated lichenoid psoriasiform dermatosis, malignant catarrhal fever, and drug eruptions (Fig. 6-14 ). The lichenoid band of inflammation is usually lymphocytic and plasmacytic, except in VKH-like syndrome, where it is primarily composed of lymphocytes and histiocytes that contain fine melanin granules.
Figure 6-14.
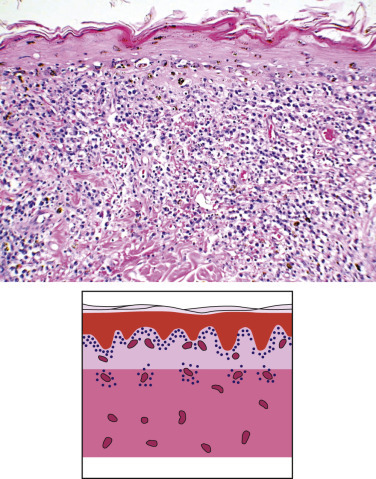
Histologic and schematic appearance of lichenoid interface dermatitis in chronic cutaneous lupus erythematosus. Large numbers of lymphocytes and plasma cells abut the epidermal-dermal junction. The basal layer of the epidermis demonstrates apoptosis and vacuolar degeneration of keratinocytes.
Caution should be exercised in differentiating interface lichenoid inflammation from lichenoid inflammation. There is controversy over these terms in the literature. To date in veterinary dermatopathology, the term “lichenoid” refers to a band of inflammation, commonly plasmacytic, closely apposed to the dermoepidermal junction, which does not necessarily involve damage to the basal cell layer, such as mucocutaneous pyoderma.
Vasculitis
Vasculitis is characterized by inflammation targeting the walls of venules or arterioles, resulting in at least partial destruction of the vessel wall, sometimes with fibrin deposition (Fig. 6-15 ). It can be accompanied by fibrinoid necrosis, thrombosis, hemorrhage, and evidence of ischemia. Vasculitis can be immune mediated or septic. Immune-mediated vasculitis is due to type III hypersensitivity. The deposition of antigen-antibody complexes in vessel walls activates complement, which results in generation of factors chemotactic for neutrophils. Activation of neutrophils with release of reactive oxygen species and lysosomal enzymes then directly damages vessel walls. Septic vasculitis is caused by systemic infection with agents that have a predilection for endothelial cells, resulting in endothelial damage. Vasculitis can also be locally induced by bacterial antigens deposited in vessel walls.
Figure 6-15.
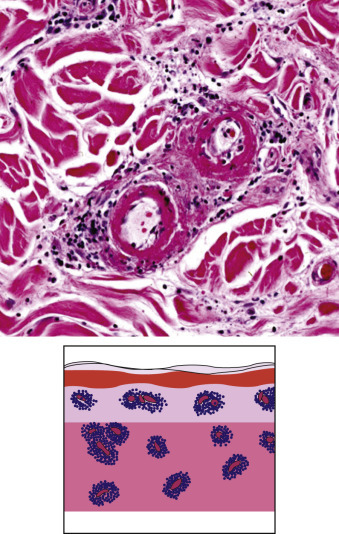
Histologic and schematic appearance of vasculitis. Leukocytes target vessel walls. Fibrin, erythrocytes and leukocytic debris are in the dermis and vessel walls.
Vasculitis can further be classified on the basis of the dominant inflammatory cell within vessel walls. There are neutrophilic, eosinophilic, lymphocytic, and mixed types. It should be noted that the inflammatory cell involved often reflects the stage of the disease rather than characterizing a specific disease.
-
•
Neutrophilic vasculitis is by far the most common type and may be leukocytoclastic (associated with karyorrhexis of neutrophils resulting in “nuclear dust”) or nonleukocytoclastic. It is seen with hypersensitivity reactions, septicemia, connective tissue disorders, equine purpura hemorrhagica, Rocky Mountain spotted fever, classical swine fever, thrombophlebitis, and as an idiopathic disorder.
-
•
Lymphocytic vasculitis may be seen with dermatomyositis, malignant catarrhal fever, vaccine-induced panniculitis, and rarely in cutaneous lymphoma. It can also reflect a chronic stage of a vasculitis that was originally neutrophilic.
-
•
Eosinophilic vasculitis is rare. It is seen most commonly in lesions induced by arthropod insult, drug eruptions, food hypersensitivity, equine axillary nodular necrosis, idiopathic nodular eosinophilic vasculitis in horses, feline eosinophilic granulomas, and rarely in mast cell tumors.
Nodular and diffuse dermatitis
Nodular and diffuse dermatitis is characterized by nodules, or diffuse sheet-like infiltrates of inflammatory cells, in the dermis or subcutis (Fig. 6-16 ). Nodular and diffuse dermatitis may be characterized by the predominant cell type present (neutrophils, macrophages, lymphocytes, eosinophils, or mixed). The inciting antigen may be an infectious agent, noninfectious material, or the inflammation may be idiopathic. Neutrophils predominate in dermal abscesses associated with infectious agents such as bacteria, fungi, algae, and protozoa. They can also be present in sterile lesions, as in foreign-body reactions and the sterile pyogranuloma syndrome. Histiocytes predominate in granulomatous inflammation, which is typically chronic. Granulomatous infiltrates containing large numbers of neutrophils are frequently called pyogranulomas. Although all granulomatous dermatitis is nodular or diffuse in pattern, not all nodular and diffuse dermatitides are granulomatous.
Figure 6-16.

Histologic and schematic appearance of nodular-to-diffuse dermatitis in bacterial dermatitis. Coalescing nodules of lymphocytes, plasma cells, and macrophages obscure the deep dermis.
Granulomas are discrete foci of granulomatous inflammation. They may be subclassified as “tuberculoid” (a central zone of neutrophils and necrosis surrounded by histiocytes, epithelioid macrophages, and giant cells, in turn surrounded by lymphocytes and an outer layer of fibroblasts) or “sarcoidal” (consisting of epithelioid macrophages). Tuberculoid granulomas may be seen in tuberculosis, feline leprosy, atypical mycobacterial infection, and Corynebacterium pseudotuberculosis infections. Sarcoidal granulomas may be seen in sterile sarcoidal granulomas and foreign-body reactions. Palisading granulomas are characterized by the alignment of histiocytes, such as staves around a central focus of collagen degeneration (feline, canine, and equine eosinophilic granuloma; equine mastocytoma); parasite or fungus (habronemiasis, pythiosis, conidiobolomycosis, basidiobolomycosis, demodicosis); lipids (xanthoma); or other foreign material (e.g., calcium as in dystrophic calcinosis cutis and calcinosis circumscripta). Granulomas and pyogranulomas that track hair follicles, resulting in large, vertically oriented (“sausage-shaped”) lesions, are seen in sterile granuloma/pyogranuloma syndrome of dogs and cats, or can be seen together with folliculitis because of the presence of intrafollicular antigens such as dermatophytes.
Nodular and diffuse dermatitis is often associated with certain unusual inflammatory cell types. Foam cells are histiocytes with vacuolated cytoplasm resulting from their contents (lipid, debris, microorganisms). Epithelioid macrophages are histiocytes with elongated or oval vesicular nuclei and abundant finely granular, eosinophilic cytoplasm with ill-defined cell borders. Multinucleated giant cells are histiocytic variants that assume 3 morphologic forms: Langhans (nuclei form a circle or semicircle at the periphery of the cell), foreign body (nuclei are scattered throughout the cytoplasm), and Touton (nuclei form a wreath that surrounds a central, homogeneous, amphophilic core of cytoplasm that is, in turn, surrounded by abundant foamy cytoplasm). In general, these 3 forms of giant cells have little diagnostic specificity, although the Touton variety is strongly indicative of xanthomas, and the Langhans type suggests the need for an acid-fast stain. Eosinophils may predominate in feline, canine, and equine eosinophilic granuloma; in certain parasitic dermatoses (habronemiasis, elaeophoriasis, parafilariasis, dirofilariasis, dracunculiasis); in furunculosis, and in hairy vetch toxicosis. Mixed cellular infiltrates are most commonly neutrophils and macrophages (pyogranuloma), or eosinophils and macrophages (eosinophilic granuloma), or a combination of the 3 cell types. Plasma cells are common components of nodular and diffuse dermatitis in domestic animals and are of no particular diagnostic significance. They may contain eosinophilic, intracytoplasmic inclusions that are called Russell bodies. These accumulations of glycoprotein are largely globulin and may be large enough to displace the cell nucleus. Reactions to ruptured hair follicles are a common cause of nodular and diffuse pyogranulomatous dermatitis in domestic animals, and any such lesion should be examined for keratinous and epithelial debris. All other nodular and diffuse dermatitides should be cultured, examined in polarized light for foreign material, and stained for bacteria and fungi. In general, microorganisms are most likely to be found near areas of suppuration and necrosis.
Intraepidermal vesicular and pustular dermatitis
Intraepidermal vesicles and pustules can be caused by intercellular edema that can be seen in any acute or subacute dermatosis, viral infections, hydropic degeneration of keratinocytes, and by acantholysis (Fig. 6-17 ). It can be useful to subdivide this category on the basis of the site of the vesicle or pustule within the epidermis.
-
•
Subcorneal pustules and vesicles are most commonly seen in pemphigus foliaceus, pustules associated with superficial pyoderma, and eosinophilic pustules resulting from hypersensitivities.
-
•
Pustules and vesicles in the stratum spinosum are most commonly seen in the pemphigus complex, viral diseases, and occasionally in hepatocutaneous syndrome.
-
•
Suprabasilar pustules and vesicles are a feature of pemphigus vulgaris.
-
•
Intrabasilar vesicles can be seen in lupus erythematosus, dermatomyositis, erythema multiforme, graft-versus-host disease, and toxic epidermal necrolysis.
Figure 6-17.

Histologic and schematic appearance of intraepidermal vesicular/pustular dermatitis in pemphigus foliaceus. A collection of neutrophils and acantholytic keratinocytes (arrows) is within a subcorneal pustule.
Subepidermal vesicular and pustular dermatitis
This pattern is characterized by separation of the epidermis from the dermis (Fig. 6-18 ). Subepidermal vesicles and pustules may be formed through hydropic degeneration of basal cells, dermoepidermal separation, severe subepidermal edema and/or cellular infiltration, and severe intercellular edema with disruption of the basement membrane zone. Caution is warranted when examining older lesions, as re-epithelialization may result in subepidermal vesicles and pustules assuming an intraepidermal location as re-epithelialization forms a pseudobase to a vesicle. Such re-epithelialization is usually recognized as a single layer of flattened, elongated basal epidermal cells at the base of the vesicle or pustule.
Figure 6-18.
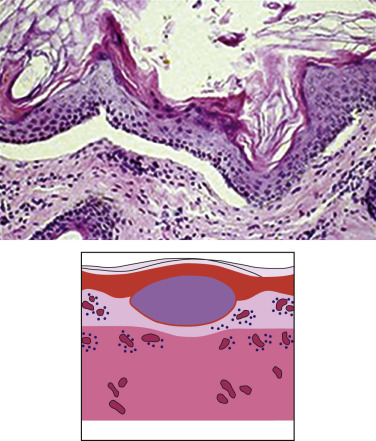
Histologic and schematic appearance of subepidermal vesicular dermatitis in junctional bullosa. The epidermis is separated at the dermal-epidermal junction.
Perifolliculitis, folliculitis, and furunculosis
Perifolliculitis (see Fig. 6-5C) means accumulation of inflammatory cells around a hair follicle in which the inflammation does not significantly impinge on the follicular epithelium. It can be accompanied by mild follicular spongiosis. Mural folliculitis (see Fig. 6-5A) is characterized by inflammation that targets the wall of the follicle. Luminal folliculitis (see Fig. 6-5B) implies the accumulation of inflammatory cells within follicular lumina. Furunculosis (see Fig. 6-6) occurs when the hair follicle ruptures, releasing the contents into the dermis. Perifolliculitis, mural and luminal folliculitis, and furunculosis usually represent a pathologic continuum, and all may be present in the same specimen. Follicular inflammation is a common gross and microscopic finding in dogs, and is less common in other species. It can be caused by bacteria, dermatophytes, and parasites, such as Demodex spp., Pelodera strongyloides, and Stephanofilaria spp.
Furunculosis leads to a foreign-body reaction to free keratin. Aside from granulomatous to pyogranulomatous inflammation, it is not uncommon to find eosinophils, presumably present in reaction to released keratin. Idiopathic sterile eosinophilic folliculitides may be seen in cattle and dogs (sterile eosinophilic pustulosis). Insect stings are postulated as the cause of eosinophilic folliculitides affecting the muzzle of dogs. In cats and horses, sterile eosinophilic folliculitis may be seen in conjunction with hypersensitivity reactions (mosquito-bite hypersensitivity, atopy, food allergy, onchocerciasis, equine eosinophilic granuloma, Culicoides hypersensitivity, flea-bite hypersensitivity). Feline herpesviral dermatitis can also result in eosinophilic folliculitis and furunculosis.
Mural folliculitis can be seen with interface dermatitis as well as demodicosis and dermatophytosis. Less common conditions include feline degenerative mucinotic mural folliculitis and pseudopelade. The hair follicle outer root sheath may be involved in hydropic degeneration and lichenoid cellular infiltrates of lupus erythematosus, drug eruptions, erythema multiforme, and idiopathic lichenoid dermatoses.
Lymphocytic peribulbitis directed at the bulb of anagen hair follicles is characteristic of alopecia areata.
Fibrosing dermatitis
Fibrosis marks the resolving stage of an intense, destructive inflammatory reaction or signifies an ongoing, more insidious, inflammatory process. Fibrosis that is recognizable histologically does not necessarily produce a visible clinical scar. Ulcers limited to the upper portion of the superficial dermis do not usually result in scarring, whereas virtually all ulcers that extend into the deep dermis result in fibrosis and clinical signs of scarring. Fibrosing dermatitis follows many severe insults to the dermis and is often of minimal diagnostic value. Common causes of fibrosing dermatitis include furunculosis, equine exuberant granulation tissue, actinic dermatitis, acral lick dermatitis, scleroderma, and morphea (localized scleroderma).
Panniculitis
Panniculitis is inflammation of subcutaneous fat (Fig. 6-19 ). This inflammation often also secondarily involves the deep dermis. Likewise, the panniculus can be secondarily involved in deep dermal inflammation. Panniculitis may be caused by infectious agents, foreign bodies, vitamin E deficiency, trauma, pancreatic disease, vasculitis, and adverse drug reaction. However, it is often sterile and idiopathic.
Figure 6-19.

Histologic and schematic appearance of panniculitis. Inflammation targets the subcutaneous tissues. Note replacement of the adipose tissue with dense inflammatory cell aggregates.
Panniculitis can be divided into lobular (fat lobules are primarily involved), septal (interlobular connective tissue septa are primarily involved), and diffuse (both anatomic areas involved) types. Septal panniculitis is often associated with vasculitis. However, all 3 patterns may be seen in a single lesion from the same patient. The majority of inflammatory conditions of the panniculus are granulomatous or pyogranulomatous, and the histologic appearance of panniculitis caused by an infectious agent can be very similar to sterile panniculitis.
In dogs, one form occurs in dogs at sites of previous rabies vaccination and is characterized by lobular hyaline degeneration of fat, lymphocytic vasculitis, lymphoid nodules, and sometimes mucinous degeneration.
Atrophic dermatosis
Atrophic dermatosis is usually characterized by atrophic changes in the hair follicles and adnexal structures (Fig. 6-20 ). It can also refer to atrophy of the epidermis or the dermis. Evaluation of atrophy of the epidermis and dermis should always take into account the site from which the biopsy was taken. Epidermis is normally thicker on the dorsum than the ventrum, and hair follicles and shafts are larger and closer together on the dorsum than on the ventral or glabrous skin. In addition, familiarity with the various stages of the hair follicle cycle is essential if atrophy of the follicle is to be evaluated. Atrophic dermatosis is often accompanied by some, or all, of the following features: atrophic hair follicles (telogen follicles are usually predominant), orthokeratotic hyperkeratosis, follicular keratosis, decreased numbers of hair shafts in follicular infundibula, epidermal atrophy, sebaceous gland atrophy, and dermal atrophy (this can be difficult to assess without site-matched controls). Atrophic dermatosis is rarely diagnostic for a specific condition but can suggest a group of diseases such as the endocrine dermatoses, the most common cause of atrophic dermatosis. It will almost always be necessary to confirm the identity of the endocrinopathy with endocrine function tests. Other causes of atrophic dermatoses include ischemia, feline acquired skin fragility, and alopecia X.
Figure 6-20.
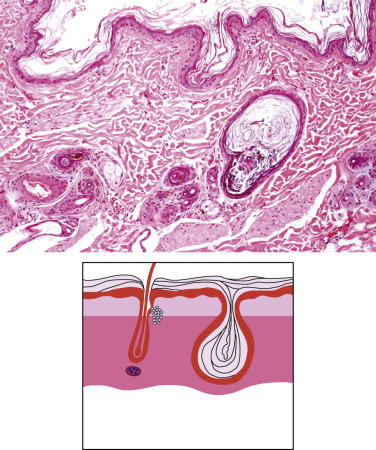
Histologic and schematic appearance of atrophic dermatosis. The epidermis is thinned at 1-2 nucleated cells in this layer, and follicles are reduced to small epithelial cell clusters. Sebaceous glands are inconspicuous. There is outer root sheath thinning with follicular keratosis. In the schematic, note the thin dermis, hyperkeratosis, pilosebaceous atrophy, follicular keratosis, and plugging.
Follicular and adnexal atrophy can also be secondary, rather than the primary disease process. An example is follicular atrophy as a result of a chronic inflammatory process, such as chronic allergic dermatitis, or sebaceous adenitis. In this case, there would be histologic evidence of the chronic inflammation previously present, such as scarring or epidermal hyperplasia/hyperkeratosis and superficial dermal perivascular inflammation.
Further reading
Claudy A. Pathogenesis of leukocytoclastic vasculitis. Eur J Dermatol 1998;8:75-79.
Fitzpatrick JE, et al. Patterns in dermatopathology. In: Farmer ER, Hood AF, editors. Pathology of the Skin. New York: McGraw-Hill; 2000. p. 113-130.
Foster AP. A study of the number and distribution of cutaneous mast cells in cats with disease not affecting the skin. Vet Dermatol 1994;5:17-20.
Gross TL, et al. An anatomical classification of folliculitis. Vet Dermatol 1997;8:147-156.
Gross TL, et al. Diseases of the panniculus. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 537-561.
Miller WH, et al. Structure and function of the skin. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 1-56.
Noli C, et al. Apoptosis in selected skin diseases. Vet Dermatol 1998;9:221-229.
Scott DW. Lymphoid nodules in skin biopsies from dogs, cats, and horses with nonneoplastic dermatoses. Cornell Vet 1989;79:267-272.
Scott DW. Epidermal mast cell in the cat. Vet Dermatol 1990;1:65-69.
Scott DW, et al. Diagnostic methods. In: Scott DW, et al., editors. Muller & Kirk's Small Animal Dermatology. 6th ed. St Louis: Elsevier; 2001. p. 71-206.
Seaman WJ, Chang SH. Dermal perifollicular mineralization of toy poodle bitches. Vet Pathol 1984;21:122-123.
Shiohara T, et al. Induction and control of lichenoid tissue reactions. Springer Semin Immunopathol 1992;13:369-385.
Steffen C. Dyskeratosis and the dyskeratoses. Am J Dermatopathol 1988;10:356-363.
Trump BF, et al. The pathways of cell death: oncosis, apoptosis, and necrosis. Toxicol Pathol 1997;25:82-87.
Weedon D. An approach to the interpretation of skin biopsies. Skin Pathol 1997;3-26.
Yager JA. Introduction to histological interpretation of inflammatory and degenerative lesions of the skin. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat. London: Mosby Year Book; 1994. p. 11-50.
Congenital and Hereditary Diseases of Skin
Congenital diseases are those that are present at birth. They may be hereditary or result from other factors that were present during development in utero. Various environmental influences, such as infectious agents, nutrient imbalances, toxic chemicals and plants, and ambient temperature, present during gestation, can bring about abnormalities in the skin and hair that are present at birth but are not hereditary. Some congenital diseases are incompatible with life and result in death at birth or shortly thereafter. Congenital abnormalities of the skin may be associated with abnormalities of other tissues or organs. In contrast, although they are genetically determined, some hereditary abnormalities of skin (genodermatoses) are not apparent at birth and may instead be manifested later in life, that is, tardive onset. For example, color-dilution alopecia may not be evident until early adulthood. These conditions are covered elsewhere in the chapter under the appropriate section.
As developments in medical science have reduced the incidence of preventable diseases, an increasing awareness of genetic diseases has developed. New genetic disorders are being recognized at an increasing rate as the degree of diagnostic sophistication of veterinary medicine has grown. This is happening, at least in part, because knowledge from genetic disorders in humans often leads to recognition of similar diseases in animals. Once an analogous genetic disease is identified in animals, affected animals may be used to gain new knowledge regarding the genetics, pathogenesis, or treatment of the condition, thereby producing reciprocal benefits for both human and animal health.
Ichthyosis
In veterinary medicine, the term “ichthyosis” is used to describe generalized scaling that arises from congenital and/or hereditary defects in the formation of the stratum corneum (Fig. 6-21 ). Ichthyosis is derived from the Greek word for fish, and reflects the resemblance of clinical lesions to fish scales. In human medicine, “ichthyosis,” is used for both hereditary and acquired (e.g., paraneoplastic ichthyosis) conditions. “Inherited ichthyosis” is the generic term for Mendelian disorders of cornification (MeDOC).
Figure 6-21.

Lamellar ichthyosis in a Dachshund. Marked thickening of the skin by thick adherent brown scale.
The literature on ichthyosiform disorders in human medicine is extensive and complex, and, not unlike veterinary medicine, molecular tests are not available for all disorders. MeDOC are characterized by an abnormal skin barrier; the resulting phenotype is a reflection of the body's response to correct the barrier defect. There have been deliberate attempts to refine the classification system and apply structure- and function-based algorithms to understand and therapeutically address the phenotypic manifestations. Ichthyosis vulgaris, the most common form in humans is an autosomal dominant disease characterized histologically by orthokeratotic hyperkeratosis and a decreased or absent granular layer, and ultrastructurally by retention of corneodesmosomes in the stratum corneum and small or absent keratohyaline granules. It is produced by a defect in synthesis of filaggrin. X-linked ichthyosis, a recessive disorder in which males have more severe disease than female heterozygotes, is caused by an absence of steroid sulfatase activity. Steroid sulfatase acts on cholesteryl sulfate, a product of lamellar bodies, which is discharged into the intercellular space and is involved in cell cohesion in the lower stratum corneum. Failure of the enzyme to inactivate cholesteryl sulfate results in persistent cell cohesion and interferes with the normal process of desquamation. The histologic features of X-linked recessive ichthyosis are orthokeratotic hyperkeratosis with a normal or hyperplastic granular layer. Keratohyaline granules are ultrastructurally normal. Neither ichthyosis vulgaris nor X-linked ichthyosis has been documented in domestic animals.
Autosomal recessive congenital ichthyoses (ARCI) is the umbrella that captures a group of inherited cornification disorders. Most of the reported veterinary disorders fall into this grouping. In humans, ARCI may manifest as 1 of 3 clinical forms: lamellar ichthyosis (LI), nonbullous congenital ichthyosiform erythroderma (CIE), and harlequin ichthyosis (HI). The phenotypes of LI and CIE are often overlapping, and some patients may switch phenotypes with age and treatment. HI is a severe disorder that is characterized by generalized severe plate-like scaling at birth and clinically a high mortality rate (Fig. 6-22 ). HI has been seen in a calf and a greater kudu. LI is characterized by brown plate-like scale in the absence of erythema, whereas the scale in CIE is fine and white with prominent erythema. Although LI is often associated with the transglutaminase 1 (TGM1) gene, it is by no means specific for a TGM1 mutation. To date, 8 genes have been associated with ACRI: TGM1, ABCA12, ABHD5 (CG158), 2 lipoxygenases (ALOXE3 and ALOX12B), a NIPA-like domain containing 4 (NIPAL4 or ICTHYIN), LIPN, CYP4F22, and PNPLA-1.
Figure 6-22.
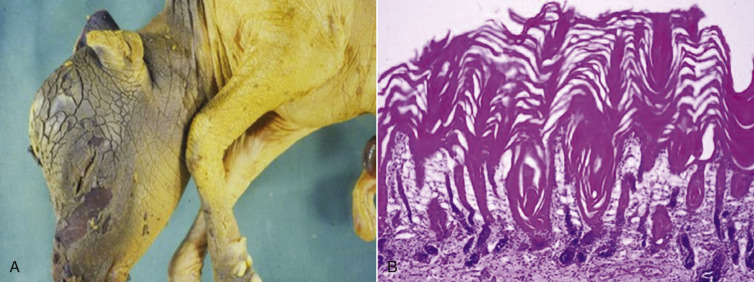
Harlequin ichthyosis in a neonatal calf. A. Generalized plate-like scaling. B. Diffuse and severe orthokeratotic hyperkeratosis
(Courtesy R. Dunstan.)
The diagnosis of ichthyosiform disorders is based on the following: signalment, history, character and distribution of the scale, presence or absence of extracutaneous lesions, and skin biopsy analysis, perhaps including molecular testing. For breeding dogs, molecular testing, if available, may be needed to identify carrier dogs. A pathologist should be able to narrow the mutational causes by determining if the disorder is epidermolytic (rare but uniquely associated with keratin mutations) or nonepidermolytic (more common and less specific).
Epidermolytic ichthyosis is also referred to as epidermolytic hyperkeratosis. The name “epidermolytic” is based on the presence of vacuoles and lysis of keratinocytes within the spinous and granular cell layers, which occur along with hypergranulosis and hyperkeratosis (eFig. 6-1). Unlike nonepidermolytic ichthyosis (see later), this finding uniquely corresponds to a defect in keratin formation (i.e., formation of the corneocyte core). Ultrastructurally, the keratin filaments are clumped and retracted. The biochemical basis is most often associated with a defect in the K1 and K10 genes. Epidermolytic ichthyosis in the Norfolk terrier is autosomal recessive and caused by a mutation in epidermal keratin (KRT10). Epidermolytic ichthyosis has been sporadically described in other dogs (Rhodesian Ridgeback, Labrador cross). The affected dogs have multifocal regions of pigmented scale with alopecia and roughening of the skin.
eFigure 6-1.
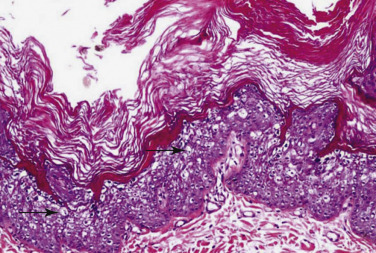
Epidermolytic hyperkeratosis in a dog. Note the marked vacuolation of keratinocytes within the spinous and granular cell layers (arrows), which occur along with hypergranulosis and marked orthokeratotic hyperkeratosis.
(Courtesy D. Shearer.)
Nonepidermolytic ichthyosis
To date, the nonepidermolytic forms of ichthyosis, which have been characterized in dogs, have been documented or presumed to be autosomal recessive traits. Nonepidermolytic ichthyosis (NI) is not necessarily recessive (e.g., X-linked ichthyosis and autosomal dominant ichthyosis vulgaris are also nonepidermolytic); however, these disorders have yet to be documented in domestic animals. Veterinary pathologists currently label these ARCI disorders by their breed predilection, a practice that may change in the future.
Golden Retriever ichthyosis is generally considered a “mild” form of scaling, and affected dogs are otherwise healthy. The clinical presentation consists of large, soft, white-to-gray adherent scale that is prominent on the trunk and may be associated with ventral hyperpigmentation (eFig.6-2). Histologically, affected dogs have diffuse lamellar orthokeratotic hyperkeratosis in the absence of epidermal hyperplasia and dermal inflammation. The granular layer is prominent and contains keratinocytes with distinct perinuclear clear spaces. Golden Retrievers are typically diagnosed at <1 year of age; however, adult-onset cases are not uncommon. Some dogs develop secondary bacterial folliculitis, which may lead to pruritus and clinical confusion with allergic skin disease. The disease may wax and wane with periodic bouts of exacerbation and remission. Golden Retriever ichthyosis is caused by a mutation in PNPLA1 gene. The gene is thought to play a role in lipid organization and metabolism within the outer epidermis.
eFigure 6-2.

Golden Retriever ichthyosis. Pelage with large white scales.
American Bulldogs have a similar but more severe ichthyosiform disorder. Unlike the Golden Retriever, the Bulldogs consistently develop clinical signs before weaning. Young puppies have a scruffy/disheveled haircoat when compared to the smooth coat of normal littermates. The glabrous skin is erythematous with tightly adherent light brown scale, which gives the abdominal skin a “wrinkled” appearance. In the adult dog, the entire abdomen, axilla, and inguinal regions have a red-brown discoloration (eFig. 6-3). Large white to light tan scales are distributed throughout the haircoat. Malassezia yeast overgrowth may be severe. The development of otitis externa, intertrigo, and pododermatitis corresponds with yeast proliferation and the onset of pruritus. The clinical presentation may be misinterpreted as nonseasonal atopic skin disease. Occasional adult dogs may have footpad hyperkeratosis. The disorder has been linked to ICHTHYN, and similar to the PLPLA1 mutation in Golden Retrievers, is likely related to lipid metabolism in the epidermis. The histologic lesions are the similar but more severe than Golden Retriever ichthyosis; furthermore, yeast are often found in the stratum corneum (eFig. 6-4).
eFigure 6-3.

American Bulldog ichthyosis. Erythema and wrinkled appearance to abdomen with thick adherent scale.
eFigure 6-4.
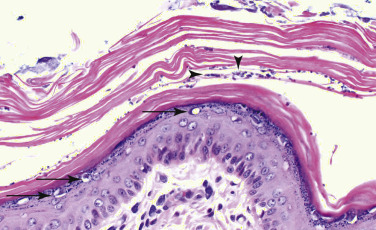
American Bulldog ichthyosis. Note the expansion of the stratum corneum by diffuse lamellar orthokeratotic hyperkeratosis with proliferation of Malassezia (arrowheads). Granular layer keratinocytes have perinuclear clear spaces (arrows).
Nonepidermolytic ichthyosis in Jack Russell Terriers (JRTs) is caused by a loss-of-function mutation in transglutaminase 1 (TGM1). TGM1 mediates calcium-dependent cross-linking of peptides (e.g., involucrin, loricrin) to form the cornified envelope—the strong exterior of the corneocyte. The phenotype in the JRT is characterized by large, thick, adherent parchment paper-like scales. This is generally more severe than the previously described disorders. The dogs develop severe Malassezia infections with corresponding inflammation and pruritus.
A number of other breeds have been diagnosed with NI on light microscopy and clinical examination (Soft-coated Wheaten Terriers, West Highland White Terriers), but further molecular characterizations have not been documented. Many cases are likely confirmed on skin biopsy and do not receive further workup.
A congenital and familial form of keratoconjunctivitis sicca with scaling has been documented in Cavalier King Charles Spaniel dogs. The dogs have a syndrome that includes the following features: keratoconjunctivitis noted from the beginning of eyelid opening, a roughened/curly haircoat, scaling with abdominal hyperpigmentation, footpad hyperkeratosis, and nail dystrophy. A recessive mode of inheritance has been proposed.
Congenital follicular parakeratosis is a cornification disorder reported in Rottweiler and Labrador Retriever dogs. An X-linked dominant mode of inheritance has been suggested in Rottweilers because the 5 reported dogs were female, and no male relatives were affected. The clinical lesions are generalized scaling and hyperkeratotic pigmented plaques. The plaques contain thick waxy and papillated follicular fronds. In Rottweilers, the lesions follow Blasko's lines. Histologically, the epidermis is acanthotic, and hair follicles have marked papillated parakeratotic hyperkeratosis that forms conically shaped projections. Clear (lipid-laden) vacuoles are located in the thick nucleated keratin. Ultrastructural changes in 2 dogs included large keratohyaline granules, tonofilament clumps, and numerous lipid vacuoles in the stratum corneum and granulosum. In Labradors, the condition may be confused with a presumably immune-mediated adult-onset form of mural folliculitis with parakeratosis.
Hereditary footpad hyperkeratosis has been reported in Irish Terriers and in a family of Dogues de Bordeaux. All footpads become progressively hyperkeratotic, fissured, and painful. Both males and females are affected, and lesions are evident by 6 months of age. The mode of inheritance has not been determined. The histologic features are mild to moderate papillated epidermal hyperplasia and diffuse orthokeratotic hyperkeratosis.
Ichthyosis has been reported in many breeds of cattle, and the mode of inheritance appears to be autosomal recessive. Both males and females are affected. Two forms of ichthyosis have been described in cattle, ichthyosis fetalis and ichthyosis congenita. However, the underlying molecular defect(s) is unknown, and it is uncertain whether the forms are distinct diseases or merely represent variations in expression of a single abnormality. Ichthyosis fetalis is the more severe form, and it has been compared to the harlequin fetus form of ichthyosis in humans. Affected calves are stillborn or die shortly after birth. The skin is hairless and covered by thick scales divided into plates by deep fissures that represent normal cleavage planes of the skin. The tight, inelastic skin is everted at the mucocutaneous junctions, and the ears are usually smaller than normal. Ichthyosis congenita is a less severe form compatible with life in which the limbs, abdomen, and muzzle are primarily involved. The skin is dry, hard, and inflexible like old leather, and may be prominently folded. There are flat plates of hyperkeratosis in which dense mats of hairs are entrapped. The keratin plaques are separated by shallow hyperemic fissures. The condition is characterized histologically by prominent laminated orthokeratotic hyperkeratosis of the epidermis and superficial portion of hair follicles. The epidermal surface is wrinkled or folded and acanthosis is variable.
Further reading
Alhaidari Z, et al. Congenital ichthyosis in two cavalier King Charles spaniel littermates. Vet Dermatol 1994;5:117-121.
Ammirati CT, Mallory SB. The major inherited disorders of cornification. New advances in pathogenesis. Dermatol Clinics 1998;16:497-508.
Baker JR, Ward WR. Ichthyosis in domestic animals: a review of the literature and a case report. Br Vet J 1985;141:1-8.
Cadiergues MC, et al. Cornification defect in the golden retriever: clinical, histopathological, ultrastructural and genetic characterization. Vet Dermatol 2008;19:120-129.
Credille K, et al. Transglutaminase 1-deficient recessive lamellar ichthyosis associated with a LINE-1 insertion in Jack Russell terrier dogs. Br J Dermatol 2009;161:265-272.
Credille KM, et al. Mild recessive epidermolytic hyperkeratosis with a novel keratin 10 donor splice-site mutation in a family of Norfolk terrier dogs. Br J Dermatol 2005;153:51-58.
Elias PM, et al. Ichthyoses. Clinical, Biochemical, Pathogenic and Diagnostic Assessment. Current Problems in Dermatology. Basel: Karger; 2010;39. p. 1-29.
Grall S, et al. PNPLA1 mutations cause autosomal recessive congenital ichthyosis in golden retriever dogs and humans. Nat Genet 2012;44:140-147.
Hargis A, et al. Proliferative, lymphocytic, infundibular mural folliculitis and dermatitis with prominent follicular apoptosis and parakeratotic casts in four Labrador retrievers: preliminary description and response to therapy. Vet Dermatol 2013;24:346-354.
Helman RG, et al. Ichthyosiform dermatosis in a soft-coated wheaten terrier. Vet Dermatol 1997;8:53-58.
Julian RJ. Ichthyosis congenita in cattle. Vet Med 1960;55:35-41.
Lewis DT, et al. A hereditary disorder of cornification and multiple congenital defects in five Rottweiler dogs. Vet Dermatol 1998;9:61-72.
Lewis DT, et al. Characterization and management of a Jack Russell terrier with congenital ichthyosis. Vet Dermatol 1998;9:111-118.
Mauldin EA, et al. The clinical and morphologic features of non-epidermolytic ichthyosis in the golden retriever. Vet Pathol 2008;45:174-180.
Mauldin EA. Canine ichthyosis and related disorders of cornification. Vet Clin North Am Small Anim Pract 2013;43:89-97.
Mecklenburg L, et al. Epidermolytic ichthyosis in a dog: clinical, histopathological, immunohistochemical and ultrastructural findings. J Comp Pathol 2000;122:307-311.
Paradis M. Footpad hyperkeratosis in a family of Dogues de Bordeaux. Vet Dermatol 1992;3:75-78.
Wattles
Wattles (tassels), similar to those seen in goats, occur occasionally in swine and rarely in sheep. They occur in many breeds of swine with no apparent sex predilection and are inherited as an autosomal dominant trait. Wattles are asymptomatic, cylindrical, teat-like structures that hang from the ventral mandibular region. They are 5-7 cm long and may be unilateral or bilateral. Histologically, they are composed of a core of fibrocartilage, surrounded by fibrous and adipose connective tissue, and covered by haired skin.
Wattles have also been reported in Dorset Down, Merino, and Karakul sheep. The structures in sheep are smaller than those of pigs, and they lack the fibrocartilaginous core seen in wattles of goats and pigs.
Further reading
Lancaster MJ, Medwell WD. Neck wattles in lambs. Aust Vet J 1991;68:75-76.
Roberts E, Morrill CC. Inheritance and histology of wattles in swine. J Hered 1944;35:149-151.
Hereditary zinc deficiency
Hereditary zinc deficiency occurs in cattle and Bull Terrier dogs and results in multisystemic disease that includes skin lesions. Animals are normal at birth and usually begin developing skin lesions at approximately 1-2 months of age, at which time growth retardation also becomes evident. Skin lesions consist of crusting, which is most prominent on the face and distal extremities, dry flaky skin, and hair color fading. A decrease in serum zinc concentration precedes clinical signs; and alkaline phosphatase, a zinc-dependent enzyme, frequently decreases in parallel with the zinc concentration. Affected animals also commonly have diarrhea. Animals with hereditary zinc deficiency have a hypoplastic thymus, and, consequently, secondary infections are common because of associated immune system dysfunction involving both humoral and cell-mediated immunity. The condition is an autosomal recessive trait in both cattle and dogs, and it is considered analogous to acrodermatitis enteropathica of humans. The characteristic histologic lesion is marked diffuse parakeratotic hyperkeratosis.
Hereditary zinc deficiency (HZD) in cattle is also called lethal trait A46, hereditary parakeratosis, hereditary thymic aplasia, and Adema disease. It affects Friesian cattle and Black Pied Danish cattle of Friesian descent in Europe, and has been reported in Shorthorn cattle in the United States. The condition normally begins with depression, diarrhea, and skin lesions when calves are 4-8 weeks of age. The skin becomes dry and flaky, and the haircoat is rough. Patches of erythema, scaling, oozing, crusting, and alopecia begin on the muzzle and then appear around the eyes, ears, and intermandibular space. Similar lesions develop later on the legs, and the skin around the stifles, fetlocks, and coronary bands becomes particularly crusty, fissured, and painful. The flanks, perianal area, and ventral abdomen may also be affected. The hair may lighten in color, a change that may be especially prominent around the eyes and resemble the spectacle lesion of copper deficiency. Affected calves are lethargic, drool, and may have difficulty suckling. They are smaller than unaffected calves of the same age. Conjunctivitis, rhinitis, bronchopneumonia, and other infections are common because of immune dysfunction. Untreated calves usually die 4-8 weeks after the onset of clinical disease.
This disease is associated with impaired intestinal zinc absorption caused by abnormal function of a protein belonging to a family of zinc-uptake proteins. Acrodermatitis enteropathica and HZD are associated with defects in the gene SLC39A4. Oral zinc supplementation effects a complete reversal of clinical signs and may restore thymic morphology if instituted early enough. Intestinal malabsorption of zinc is the cause of the disorder in cattle. Zinc is absorbed from the intestine by 2 separate pathways, that is, a transporter-dependent active system and passive diffusion, and it is the zinc-binding ligand system that is suspected to be defective. A cysteine-rich intestinal protein (CRIP) has been identified in the ligand-dependent pathway and has been suggested as being defective in this condition.
The most striking and consistent gross abnormality is marked thymic hypoplasia. Histologic abnormalities include depletion of small lymphocytes of the thymus, especially in the cortical region, and hypoplasia of the spleen, lymph nodes, and Peyer's patches. The skin lesions are characterized histologically by perivascular dermatitis, acanthosis, pallor and vacuolation of the upper spinous and granular layers, and marked diffuse parakeratosis. Neutrophilic exocytosis and superficial bacterial cocci may be prominent.
Lethal acrodermatitis of Bull Terrier dogs is also thought to be caused by an abnormality in zinc absorption or metabolism; however, zinc supplementation fails to produce clinical improvement. The concentrations of both serum zinc and copper have been found to be lower in affected Bull Terriers compared with control dogs, raising the question of the role of copper deficiency in the pathogenesis of the canine disease. The condition is characterized by growth retardation, progressive skin lesions, paronychia, diarrhea, abnormal behavior, bronchopneumonia, and death usually by 18 months. Some affected puppies have lighter pigmentation than their normal littermates, and this difference becomes more pronounced with age. By 2 months of age, they are obviously smaller than their normal littermates. Skin lesions usually begin by 6-8 weeks of age and consist of crusty exfoliative lesions involving the distal extremities, footpads, and mucocutaneous junctions, particularly on the muzzle and mouth (eFig. 6-5). Digits are prominently splayed, and footpads develop cracks and frond-like masses of keratin. The skin is erythematous and moist under the crusts. Interdigital pyoderma and paronychia are common. Many affected dogs also have diarrhea and exhibit abnormal behavior consisting of increased aggressiveness initially, and lethargy and decreased responsiveness later in the course of disease. Respiratory tract infections are common, and bronchopneumonia is a common cause of death.
eFigure 6-5.
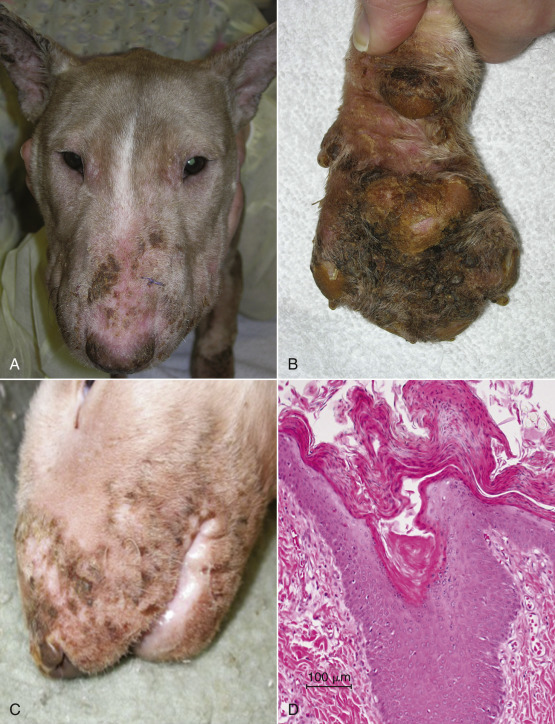
Lethal acrodermatitis of Bull Terrier dogs. A, C. Note the thick coalescing hyperkeratotic plaques on the face. B. The palmer surface of the interdigital paws is massively thickened by yellow-brown plaques. D. Histologically, there is marked acanthosis with diffuse parakeratotic hyperkeratosis.
Extracutaneous postmortem lesions consist of a small or absent thymus and may also include a high, arched palate and brachygnathia inferior. Histologic changes in the skin are mild to moderate perivascular dermatitis, moderate to marked acanthosis that may be accompanied by pallor of the superficial epidermis, and marked diffuse parakeratotic hyperkeratosis (see eFig. 6-5D). There may also be neutrophilic exocytosis, intraepidermal neutrophilic pustules, and serocellular crusts containing bacterial cocci and/or yeasts. Diagnosis is straightforward if signalment and clinical history are known. If this information is not available, differential diagnoses include superficial necrolytic dermatitis, zinc-responsive dermatosis, and generic dog food dermatosis. However, parakeratosis is less severe in these diseases, and superficial epidermal necrolysis is not a feature of lethal acrodermatitis.
Further reading
Ackland ML, Michalczyk A. Zinc deficiency and its inherited disorders—a review. Genes Nutr 2006;1:41-49.
Machen M, et al. Bovine hereditary zinc deficiency: lethal trait A 46. J Vet Diagn Invest 1996;8:219-227.
McEwan NA, et al. Diagnostic features, confirmation and disease progression in 28 cases of lethal acrodermatitis of bull terriers. J Small Anim Pract 2000;41:501-507.
Perafan-Riveros C, et al. Acrodermatitis enteropathica: case report and review of the literature. Pediatr Dermatol 2002;19:426-431.
Perryman LE, et al. Lymphocyte alterations in zinc-deficient calves with lethal trait A46. Vet Immunol Immunopathol 1989;21:239-248.
Smits B, et al. Lethal acrodermatitis in Bull Terriers: a problem of defective zinc metabolism. Vet Dermatol 1991;2:91-96.
Uchida Y, et al. Serum concentrations of zinc and copper in Bull Terriers with lethal acrodermatitis and tail chasing behavior. Am J Vet Res 1997;58:808-810.
Vogt DW, et al. Hereditary parakeratosis in Shorthorn beef calves. Am J Vet Res 1988;49:120-121.
Wang K, et al. A novel member of a zinc transporter family is defective in acrodermatitis enteropathica. Am J Hum Genet 2002;71:66-73.
Yuzbasiyan-Gurkana V, Bartletta E. Identification of a unique splice site variant in SLC39A4 in bovine hereditary zinc deficiency, lethal trait A46: an animal model of acrodermatitis enteropathica. Genes Nutr 2006;88:521-526.
Epidermolysis bullosa
Epidermolysis bullosa (EB) is a heterogeneous group of mechanobullous genodermatoses that are all characterized by skin and mucous membrane blistering and ulceration in response to minor mechanical trauma. EB is caused by mutations in structural proteins that comprise the basement membrane zone and cytoskeleton of basal keratinocytes. In veterinary medicine, advances in molecular techniques have elucidated the mutations in genes that encode structural proteins: plakophilin 1 (PKP1), desmoplakin (DSP), keratins 5 and 14 (KRT5 and KRT14), plectin (PLEC1), αbβ5 integrin (ITGA6), laminin (LAMA3, LAMB3, LAMC2), and collagen types XVII and VII (COL17A1, COL7A).
Much of the older literature uses the term epitheliogenesis imperfecta (EI) to describe congenital mechanobullous conditions in many species; however, many of these conditions would be more appropriately termed epidermolysis bullosa in the current classification. Furthermore, epitheliogenesis imperfecta descriptively encompassed 2 different diseases: epidermolysis bullosa and aplasia cutis congenita. In swine, aplasia cutis congenita (also called epitheliogenesis imperfecta) is very rare and a clinically distinct, recessively inherited trait. The disorder arises predominantly in male piglets. Most piglets have extensive lesions and die shortly after birth. Piglets with small focal lesions may survive but are smaller than normal littermates. At least some affected piglets also have hydroureter and hydronephrosis. The defects are typically located within the caudal half of the body (Fig. 6-23 ), and are characterized by an absence of epidermis and sometimes loss of dermis. Piglets may have fluid-filled subcutaneous bullae. An underlying cause is not known.
Figure 6-23.

Aplasia cutis congenita (epitheliogenesis imperfecta) in a pig.
Epidermolysis bullosa is divided into 3 broad groups based on the ultrastructural level of the skin cleavage: epidermolysis bullosa simplex (EBS; epidermolytic epidermolysis bullosa), junctional epidermolysis bullosa (JEB), and dystrophic epidermolysis bullosa (dermolytic epidermolysis bullosa). JEB may be further classified into Herlitz or non-Herlitz type. Herlitz JEB is a severe (typically lethal) and generalized disease with widespread cutaneous and mucous membrane blistering. EB is further classified into >20 subtypes in humans based on clinical manifestations of skin lesions, mode of inheritance, and presence or absence of extracutaneous abnormalities, as well as ultrastructural features. The clinical presentation may range from minimal localized involvement of hands and feet to severe, life-threatening generalized blistering with extracutaneous involvement. Corneal erosions, tooth, nail, and hair abnormalities, and tracheal, gastrointestinal, genitourinary, and musculoskeletal involvement occur in various subtypes of epidermolysis bullosa in humans. In animals, epidermolysis bullosa has been reported rarely and, in most instances, has led to the death of affected individuals.
-
•
Epidermolysis bullosa simplex is characterized by cytolysis of the basal keratinocytes, which produces intraepidermal clefting. This form of the disease is caused by fragility of the epidermal basal cells because of mutations in basal cell–specific keratins 5 and 14. These mutations result in disruption of the assembly, structure, and/or function of the keratin intermediate filaments that act as the skeleton of basal keratinocytes. Ultrastructurally, cytolysis of the basal cells is seen as intraepidermal clefting. In some forms, cytolysis is preceded by aggregation and clumping of the keratin tonofilaments that are attached to hemidesmosomes.
-
•
In junctional epidermolysis bullosa, clefting occurs within the lamina lucida because of abnormalities of the anchoring filament-hemidesmosome complexes, which may be reduced in number and poorly formed or may be completely absent. Most cases of JEB are the result of a deficiency or abnormality in one of the hemidesmosome-associated proteins laminin-5, collagen XVII (also called BPAG 2 and BP180), or integrin α6β4, or the extracellular protein LAD-1, which is secreted by epidermal cells and localizes to the upper aspect of the anchoring filaments. The Herlitz type of JEB has more severe skin lesions than other types of EB. The lesions are widespread with all hooves affected, and most animals die within the first week of life. Whereas hemidesmosomes may be normal or reduced in size and number in the non-Herlitz type, they are markedly reduced or absent with an absent sub-basal dense plate in the Herlitz type of JEB.
-
•
Dystrophic epidermolysis bullosa is characterized by a split in the superficial dermis below the lamina densa in the region of the anchoring fibrils, which are fewer in number and distorted or completely absent. The molecular cause of dystrophic epidermolysis bullosa is a mutation in the anchoring fibril protein, type VII collagen.
Affected animals usually develop lesions shortly after birth; however, in some cases, the disease is not evident until the animal is several months old. Initial lesions consist of vesicles and bullae, but they quickly rupture, and only ulcers may be evident clinically. Lesions are located in areas of the skin and mucous membranes that are most prone to frictional trauma, such as over bony prominences of the distal extremities, footpads, lips, tongue, palate, and gingiva. Hoof sloughing and nail dystrophy and shedding accompany skin lesions in some forms of the disease. Lesions may be induced accidentally by rough handling of an affected animal or intentionally for diagnostic purposes by gentle frictional trauma.
Histologically, most forms of epidermolysis bullosa are characterized by subepidermal clefts and vesicles with minimal inflammation (see Fig. 6-18), changes that are indistinguishable from other mechanobullous diseases (e.g., bullous pemphigoid [BP], mucous membrane pemphigoid). Even in the epidermolytic form of epidermolysis bullosa, the cleavage is usually so low in the epidermis that the vesicle appears subepidermal in routine sections. PAS staining to visualize the basement membrane zone may be helpful in determining the level of cleavage, but definitive diagnosis requires ultrastructural examination. Basement membrane antigen mapping by immunofluorescence or immunohistochemistry may be a diagnostic adjunct or alternative to electron microscopy to establish the diagnosis. In epidermolysis bullosa simplex, the PAS-positive basement membrane is at the base of the blister as are type IV collagen, laminin, and BP antigen. In JEB, the PAS-positive basement membrane, type IV collagen, and laminin are at the base of the blister, whereas the BP antigen is primarily on the blister roof. The PAS-positive basement membrane as well as all 3 basement membrane proteins, that is, type IV collagen, laminin, and BP antigen, are at the roof of the blister in dystrophic epidermolysis bullosa.
Further reading
Agerholm JS, et al. Investigations on the occurrence of hereditary diseases in the Danish cattle population 1989-1991. Acta Vet Scand 1993;34:245-253.
Benoit-Biancamano MO, et al. Aplasia cutis congenita (epitheliogenesis imperfecta) in swine: observations from a large breeding herd. J Vet Diagn Invest 2006;18:573-579.
Bentinck-Smith J. A congenital epithelial defect in a herd of Berkshire swine. Cornell Vet 1951;41:47-51.
Dalir-Naghadeh B, et al. Congenital bovine epitheliogenesis imperfecta: a report of three cases from Iran. J Vet Med A Physiol Pathol Clin Med 2004;51:409-412.
Dubielzig RR, et al. Dental dysplasia and epitheliogenesis imperfecta in a foal. Vet Pathol 1986;23:325-327.
Frey J, et al. Collagen and lipid biosynthesis in a case of epitheliogenesis imperfecta in cattle. J Invest Dermatol 1989;93:83-86.
Hewitt MP, et al. Epitheliogenesis imperfecta in a black Labrador puppy. Can Vet J 1975;16:371-374.
Lieto LD, Cothran EG. The epitheliogenesis imperfecta locus maps to equine chromosome 8 in American Saddlebred horses. Cytogenet Genome Res 2003;102:207-210.
Munday BL. Epitheliogenesis imperfecta in lambs and kittens. Br Vet J 1970;126:47.
Tontis A, Hofstetter H. Epitheliogenesis imperfecta in lambs. Schweiz Arch Tierheilkd 1991;133:287-289.
Cattle
All 3 forms of epidermolysis bullosa have been described in cattle. In calves, epidermolysis bullosa (termed EI) has been reported in many breeds and appears to be an autosomal recessive trait, and it is seen most often in herds in which there is extensive inbreeding. Both male and female calves are affected. Lesions are usually extensive and involve the extremities most commonly; however, any portion of the body may be affected as well as the squamous epithelium of the muzzle, lips, and oral cavity. Hooves and dewclaws may be missing or incompletely formed. Some affected calves also have deformed teeth and lack pinnae. Brachygnathia and atresia ani have accompanied the cutaneous abnormalities in some calves.
Epidermolysis bullosa simplex (EBS) associated with a mutation in the keratin 5 gene (KRT5) has been identified in the progeny of a 3-year-old Friesian-Jersey crossbred bull. Histologically, the lesions were characterized by dermoepidermal separation; electron microscopy showed that the cleavage occurred above the basement membrane zone and involved basal keratinocyte lysis.
Epidermolysis bullosa simplex has been reported in Simmental cross calves in the United Kingdom. Ultrastructural findings were typical of EBS, but no mutations were found in KRT5 or KRT 14. EBS has also been described in 25 of 72 calves sired by a single Simmental bull. The condition appeared to be inherited as an autosomal dominant trait with high mortality. Lesions were evident in newborn calves and consisted of ulcers of the muzzle, lips, gingiva, dorsum of the tongue, and around joints of distal limbs. Calves were unthrifty, became emaciated after weaning, and developed areas of alopecia, hyperkeratosis, ulcers, and exfoliative dermatitis. Three animals kept under laboratory conditions showed gradual improvement in severity of lesions, but rough handling could still elicit lesions. Histologic changes were typical of EB and consisted of dermal-epidermal separation unassociated with any significant inflammation. PAS-positive basement membrane was evident on the dermal side of the cleft. In thin sections of skin, cytolysis of the basal keratinocytes was seen, but no ultrastructural examination was done to confirm the diagnosis. JEB has been described in a Gir crossbred calf.
A mechanobullous disease suspected to be dystrophic epidermolysis bullosa has been reported in Texas Brangus calves with a common bull in their pedigree. The calves developed ulceration of distal limbs and oral mucosa, nasolabial mucosal sloughing, and sloughing of hooves within the first few days of life. The mode of inheritance was suspected to be recessive because of extensive inbreeding. Histologically, the lesions were dermal-epidermal clefts, with the PAS-positive basement membrane remaining attached to the basal cell layer, that is, forming the roof of the bullae. Ultrastructural examination revealed that the lamina densa was attached to the basal layer of the epidermis; inadequate fixation prevented accurate evaluation of the anchoring fibrils.
A single case report of JEB was reported in a Gir-cross calf. The calf had exungulation of all hooves, oral ulcers, and widespread erosions and crusts on the body.
Sheep
Inherited junctional epidermolysis bullosa (Herlitz type) has been described in 16 German black-headed mutton sheep. The sheep died within the first week of life. Skin lesions, mostly crusted ulcers with a few intact blisters, were most pronounced over the dorsal aspects of the carpal and tarsal regions, coronary bands, hooves, and tongue. Immunohistochemistry with the antibody to laminin-5 showed reduced expression on frozen sections of skin and tongue. A frameshift mutation in LAMC2 was documented.
A congenital bullous disease suggestive of dystrophic epidermolysis bullosa has been described in Suffolk and South Dorset Down lambs in New Zealand, Scottish Blackface lambs, and Weisses Alpenschaf lambs in Switzerland. Blisters that evolved into ulcers were seen at birth or within the first few weeks of life. Lesions occurred in areas with sparse hair and those prone to frictional trauma, such as the muzzle, ears, groin, coronary band, lips, tongue, gums, dental pad, and palate. Lameness and hoof separation and sloughing were common and gave rise to the colloquial name “red foot disease” in Scotland. The lambs grew poorly and were underdeveloped, and there were changes attributed to oral ulceration and reluctance to nurse. Histologic changes were typical of EB and consisted of dermal-epidermal separation with minimal inflammation. The PAS-positive basement membrane zone remained attached to the epithelium and formed the roof of the vesicle, suggestive of dystrophic epidermolysis bullosa. The condition has been characterized only in the Swiss Weisses Alpenschaf breed. Ultrastructural examination of skin from the Swiss lambs indicated that the splitting was below the lamina densa and that anchoring fibrils were absent or rare and rudimentary. Antigen mapping of the lesion identified laminin and type IV collagen at the roof of the cleft, which confirms sublamina densa blistering; and no type VII collagen, the major structural component of anchoring fibrils, could be identified. These findings are consistent with the dystrophic form of epidermolysis bullosa. The disease was found to have a recessive mode of inheritance.
Goats
Dystrophic epidermolysis bullosa (DEB) occurs in goats. The condition was first described in an Anglo-Nubian dairy buck from Brazil. The unaffected twin brother of this buck was bred over 5 consecutive years with the dam and produced 12 kids, 4 of which were affected with DEB, suggesting an autosomal recessive mode of inheritance. Affected kids had a positive Nikolsky sign and developed spontaneous lesions within the first week of life. Alopecia, erosions, and crusts were observed on the pinnae, ventral thorax and abdomen, and dorsal surface of the carpal and tarsal regions. The gums and lips were ulcerated. Erythema and hemorrhage of the coronary bands with detachment of the hooves was observed. Also described in humans with DEB, there was spontaneous healing with scarring of the skin lesions in most of the kids. Malnutrition and growth retardation were also noted.
Horses
The Herlitz form of JEB has been described in both male and female Belgian foals within the first week or 2 of life, in American Saddlebred horses, and in 2 French draft-breed horses. Lesions in foals usually involve the legs and oral cavity. The proximal esophagus may also be affected and hooves may be lacking. In some instances, teeth are malformed. Lesions consist of skin and oral mucosal ulceration, most often of the carpi, stifles, hocks, fetlocks, tongue, gingiva, and hard palate. Hoof separation and sloughing (exungulation) are common features. Extracutaneous lesions are rare, and included ocular lesions in one foal and dental dysplasia in another. The histologic lesions consist of subepidermal clefting with minimal inflammation and PAS-positive basement membrane material evident at the base of the cleft (see Fig. 6-18). Ultrastructurally, the separation is located within the lamina lucida, indicating that hemidesmosomes are underdeveloped. In Belgian foals, the trait is inherited as autosomal recessive. The mutation responsible—a cytosine insertion in exon 10 of the LAMC2 gene—has also been identified in JEB phenotype horses in 2 French draft breeds, the Breton and Comtois. In American Saddlebred horses, the mutation has been identified in LAMA3.
Dogs
All 3 forms of epidermolysis bullosa (EB) have been reported in dogs (Fig. 6-24 ). However, the initial cases reported as epidermolysis bullosa simplex in young Collies are now thought to represent a mild form of dermatomyositis with unrecognized myositis. JEB (Herlitz type) has been described in newborn Toy Poodle and German Shorthaired Pointer puppies via histopathology and electron microscopy. Shortly after birth, the dogs developed vesicles and bullae, and ulcers were present on the pawpads, mucous membranes, and haired skin of frictional sites. Non-Herlitz (nonlethal) JEB has been documented in a 4-year-old mongrel dog. The dog had a history of vesicles, erosions, crusts, and alopecia since birth. Lesions initially occurred on the lips and ventral abdomen and eventually progressed to involve the face, trunk, tail, and acral regions. Cutaneous atrophy and hyperpigmentation, alopecia, and nail dystrophy developed later. In skin sections from the mongrel dog, expression of laminin-5, BPAG2, the α6 subunit of integrin α6β4, and type VII collagen was similar to that of normal canine skin.
Figure 6-24.

Epidermolysis bullosa in a dog. Note that the epidermis of the pawpad is easily detached, leading to extensive ulceration in areas exposed to mechanical trauma.
Junctional EB in German Shorthaired Pointers is autosomal recessive and has been proposed as an animal model. Affected dogs have spontaneous or traumatically induced blisters and ulcers on the footpads, pinnae, tail tip, and on pressure points on the distal limbs. Onychodystrophy or dental enamel dysplasia are not reported. The disease is associated with reduced expression of laminin 5 and is caused by a mutation in the LAMA3 gene for the laminin α3 chain.
Dystrophic epidermolysis bullosa (DEB), associated with mutation in the gene encoding type VII collagen (COL7A1), has been characterized in Golden Retriever dogs. Affected dogs have blisters and ulcers in the oral and esophageal epithelia, together with onychodystrophy and growth retardation. DEB was reported in a 4-year-old female Akita with a lifelong history of trauma-induced ulcers and scars over pressure points of limbs and on footpads. Nail dystrophy was apparent from 1 year of age. The lesions had periodic exacerbations and remissions. The histologic changes were dermal-epidermal clefting with minimal inflammation and PAS-positive basement membrane visible at the roof of the cleft. Ultrastructural examination indicated that the separation was beneath the lamina densa, and anchoring fibrils were in reduced numbers. Expression of type VII collagen, the major structural protein of anchoring fibrils, was normal. A dominant mode of inheritance was speculated in this nonlethal case of EB because the dominant form of DEB in humans is typically relatively mild.
Cats
Epidermolysis bullosa appears to be very rare in cats. JEB has been reported in 2 unrelated domestic shorthaired kittens. Pinnal erosions, oral ulcerations, and severe onychomadesis were described in both. Cat 1 was euthanized because of severe oral and ocular involvement; the second cat had lesions that were relatively mild and was maintained with lifelong conservative management. Immunostaining revealed decreased expression of the γ2 laminin chain in cat 1 and decreased β3 laminin chains in cat 2. Mutations were not documented but proposed to lie in the genes LAMC2 in cat 1 and LAMB in cat 2.
An undetermined type of EB was reported in a 3-year-old male domestic longhaired cat in the United Kingdom. The skin condition had been evident since the cat was 3 months old; a female littermate obtained showed no skin abnormalities. The affected cat had widespread scarring, alopecia, crusting, scaling, blisters, and ulcers. Several nails had been shed, and very few whiskers were present. No lesions were evident in the oral cavity. Histologically, lesions were characterized by dermal-epidermal separation. Ultrastructural examination indicated the cleavage to be above the lamina densa and that hemidesmosomes and anchoring fibrils were fewer and less distinct when compared to skin from a normal cat. EB (termed EI) was reported in a litter of Siamese kittens with linear ulcers on the tongue.
Dystrophic EB has been described in a domestic shorthaired cat and in a Persian cat. The cats had a juvenile onset of ulcers in the oral cavity, haired skin (dorsum), footpads, and onychomadesis. Ultrastructural examination in the Persian cat demonstrated a reduced number of anchoring fibrils, and immunostaining revealed a decreased expression of type VII collagen. Histologic examination of skin biopsies showed dermal-epidermal separation progressing to ulcers. Type IV collagen was shown by immunohistochemistry to be present at the roof of the blisters. Sublamina densa clefting was confirmed by electron microscopic examination, and anchoring fibrils were markedly reduced in number and appeared rudimentary and filamentous in skin sections from the Persian cat. Immunofluorescent staining for collagen VII, the primary component of anchoring fibrils, was markedly reduced. A mutation in the collagen VII encoding gene COL7A1 was suggested as the cause, because this gene is mutated in all subsets of DEB in affected human patients.
Further reading
Alhaidari Z, et al. Junctional epidermolysis bullosa in two domestic shorthair kittens. Vet Dermatol 2005;16:69-73.
Bassett H. A congenital bovine epidermolysis resembling epidermolysis bullosa simplex of man. Vet Rec 1987;121:8-11.
Bruckner-Tuderman L, et al. Animal models of epidermolysis bullosa: update 2010. J Invest Dermatol 2010;130:1485-1488.
Foster AP, et al. Epidermolysis bullosa in calves in the United Kingdom. J Comp Pathol 2010;142:336-340.
Frame SR, et al. Hereditary junctional mechanobullous disease in a foal. J Am Vet Med Assoc 1988;193:1420-1424.
Johnson GC, et al. Ultrastructure of junctional epidermolysis bullosa in Belgian foals. J Comp Pathol 1988;98:329-336.
Jolly RD, et al. Familial acantholysis of Angus calves. Vet Pathol 1973;10:473-483.
McTaggart HS, et al. Red foot disease of lambs. Vet Rec 1974;94:153-159.
Medeiros GX, et al. Dystrophic epidermolysis bullosa in goats. J Comp Pathol 2013;148:354-360.
Medeiros GX, Riet-Correa F. Epidermolysis bullosa in animals: a review. Vet Dermatol 2015;26:3-e2.
Milenkovic D, et al. A mutation in the LAMC2 gene causes the Herlitz junctional epidermolysis bullosa (H-JEB) in two French draft horse breeds. Genet Sel Evol 2003;35:249-256.
Nagata M, et al. Dystrophic form of inherited epidermolysis bullosa in a dog (Akita Inu). Br J Dermatol 1995;133:1000-1003.
Nagata M, et al. Nonlethal junctional epidermolysis bullosa in a dog. Br J Dermatol 1997;137:445-449.
O'Dair HA, Henderson JP. Suspected mechanobullous skin disease in a cat. J Small Anim Pract 1994;35:24-27.
Olivry T, et al. Reduced anchoring fibril formation and collagen VII immunoreactivity in feline dystrophic epidermolysis bullosa. Vet Pathol 1999;36:616-618.
Olivry T, Linder KE. Dermatoses affecting desmosomes in animals: a mechanistic review of acantholytic blistering skin diseases. Vet Dermatol 2009;20:313-326.
Ostmeier M, et al. Inherited junctional epidermolysis bullosa (Herlitz type) in German black-headed mutton sheep. J Comp Pathol 2012;146:338-347.
Palazzi X, et al. Inherited dystrophic epidermolysis bullosa in inbred dogs: a spontaneous animal model for somatic gene therapy. J Invest Dermatol 2000;115:135-137.
Paller AS. Lessons from skin blistering: molecular mechanisms and unusual patterns of inheritance. Am J Pathol 1996;148:1727-1731.
Riet-Correa F, et al. Hereditary suprabasilar acantholytic mechanobullous dermatosis in buffaloes (Bubalus bubals). Vet Pathol 1994;31:450-454.
Spirito F, et al. Animal models for skin blistering conditions: absence of laminin 5 causes hereditary junctional mechanobullous disease in the Belgian horse. J Invest Dermatol 2002;119:684-691.
Thompson KG, et al. A mechanobullous disease with sub-basilar separation in Brangus calves. Vet Pathol 1985;22:283-285.
Weedon D. Epidermolysis bullosa. In: Weedon D, editor. Skin Pathology. Edinburgh: Churchill Livingstone; 1997. p. 124-129.
White SD, et al. Dystrophic (dermolytic) epidermolysis bullosa in a cat. Vet Dermatol 1993;4:91-95.
Genetic acantholytic dermatoses in dogs
A dominantly inherited epidermal acantholytic disease has been described in English Setters. The disease was initially compared to Hailey-Hailey disease (HHD) in humans, but current thought is that the disorder is more likely a form of Darier disease (DD) In humans, autosomal dominant mutations in genes that encode calcium pumps are responsible for both HHD (SPCA1: secretory calcium/magnesium ATPase isoform) and DD (SERCA2: sarcoendoplasmic reticulum calcium ATPase isoform 2).
Hailey-Hailey disease is an autosomal dominant hereditary skin disorder of epidermal keratinocyte cohesion. Lesions in humans consist of vesicles and bullae in flexural regions exposed to chronic frictional trauma. The histologic characteristics include suprabasilar clefting and extensive separation of keratinocytes that remain loosely in place, giving the appearance of a “dilapidated brick wall.” Because of the resemblance to autoimmune pemphigus, HHD is also called benign familial chronic pemphigus. In contrast to HHD, the lesions of DD are papular to verrucous and occur in seborrheic areas. In addition to suprabasilar acantholysis, DD is characterized by dyskeratosis of the keratinocytes with formation of “corps ronds” (cells with small pyknotic nuclei, a perinuclear clear halo, and eosinophilic cytoplasm) and “grains” (compressed cells with elongated nuclei seen in the stratum corneum and granular layer) and columns of parakeratosis. In each disease, ultrastructure shows a retraction of keratin filaments from desmosomal plaques and formation of a ring of keratin around the keratinocyte nucleus.
The condition was seen in a 7-month-old male English Setter and in 2 of his female offspring, at the ages of 1 and 2 months, respectively. Lesions consisted of well-demarcated, alopecic, erythematous, hyperplastic plaques with a rough surface, occasional serous crusting, and peripheral scaling. The lesions occurred on the ventral thorax, head, and stifle. The clinical appearance of the lesions was not typical HHD, but the histologic and ultrastructural features were thought to be similar to benign familial chronic pemphigus. Microscopically, the epidermis was markedly hyperplastic, and suprabasal keratinocytes were much larger than those in the perilesional epidermis. Extensive acantholysis resulted in lacuna formation in the suprabasal and upper epidermis and the follicular epithelium along with parakeratosis and corneocyte separation (eFig. 6-6). Ultrastructurally, the changes included increased intercellular spaces, and intact desmosome-tonofilament complexes and actin filaments in early lesions. Keratin filaments retracted from the desmosomal plaques to form a perinuclear whorl. Immunohistochemical examination of various desmosomal proteins failed to demonstrate any abnormalities, and the molecular defect in these dogs was not identified. Further studies have shown that keratinocytes in lesional and nonlesional skin have depleted SERCA2 stores. Although the precise mechanism is not known, depletion of calcium stores may delay exit from the cell cycle and enhance apoptosis. Thus the clinical appearance, histologic features, and SERCA2 abnormality suggest the disease in dogs is more similar to DD than HHD.
eFigure 6-6.
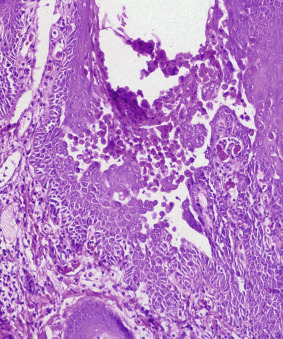
Canine inherited epidermal acantholysis. The histologic characteristics of the condition include suprabasal clefting and extensive separation of keratinocytes that remain loosely in place, giving the appearance of a “dilapidated brick wall.”
(Courtesy M. Goldschmidt.)
A unique autosomal recessive acantholytic dermatosis has been reported in related Chesapeake Bay Retriever dogs. At birth, the dogs showed sloughing of the superficial epidermal layers upon pressure. At 3 months of age, the dogs had recurrent lesions on the mucocutaneous junctions and an abnormal haircoat with multifocal hair loss. Histologically, the puppies had suprabasilar acantholysis, which became less severe with age. The condition is associated with a PKP1 mutation and loss of plakophilin-1 in desmosomal attachments as well as an abnormal arrangement of desmoplakin and keratins 10 and 14.
Genetic acantholytic dermatoses in cattle
A congenital mechanobullous dermatosis of uncertain type has been described in Angus calves in New Zealand and Murrah buffalo (Bubalus bubalis) calves in Brazil. In both reports, skin lesions developed in newborn calves in sites prone to trauma or were induced by trauma. Hoof separation and sloughing were also observed, and in buffalo calves, horns were frequently deformed and partially or completely separated from the underlying corium. Mucous membrane and mucocutaneous involvement was seen in the Angus calves but not in the buffalo calves. The histologic changes seen in the Angus calves were separation of prickle cells and basal cells from each other and sometimes basal cells from the underlying dermis, resulting in suprabasilar to sub-basilar vesicles and subsequent shedding of the epithelium. Many basal and prickle cells contained large eosinophilic cytoplasmic bodies. In the Murrah buffalo calves, the characteristic histologic alteration was suprabasilar clefting with detachment of the stratum spinosum from the underlying basal layer. Ultrastructural changes in affected areas of skin in the buffalo calves consisted of loss of desmosomal adhesion between the basal and prickle cell layers. The basal lamina, hemidesmosomes, anchoring fibrils, and anchoring filaments appeared normal. In the Angus calves, desmosomes were lacking or fewer than normal, and many keratinocytes contained a mass of tonofilaments arranged in whorls. Hemidesmosomes were normal. Although the clinical presentation of these cases was typical of epidermolysis bullosa, the histologic and ultrastructural features were unlike those of the common forms of epidermolysis bullosa. However, some variants of epidermolysis bullosa simplex in humans are characterized by cleft formation with acantholysis in the middle or upper epidermis, and in some instances, cells contain round clumps within their cytoplasm produced by aggregation of tonofilaments. In both reports, the condition in the calves was suspected to be inherited as an autosomal recessive trait.
Further reading
Cooley JE, et al. Hailey-Hailey disease keratinocytes: normal assembly of cell:cell junctions in vitro. J Invest Dermatol 1996;107:877-881.
Haftek M, et al. Internalization of gap junctions in benign familial pemphigus (Hailey-Hailey disease) and keratosis follicularis (Darier's disease). Br J Dermatol 1999;141:224-230.
Müller EJ, et al. Consequences of depleted SERCA2-gated calcium stores in the skin. J Invest Dermatol 2006;126:721-731.
Olivry T, et al. Deficient plakophilin-1 expression due to a mutation in PKP1 causes ectodermal dysplasia-skin fragility syndrome in Chesapeake Bay retriever dogs. PLoS ONE 2012;7:e32072.
Olivry T, Linder KE. Dermatoses affecting desmosomes in animals: a mechanistic review of acantholytic blistering skin diseases. Vet Dermatol 2009;20:313-326.
Sueki H, et al. Dominantly inherited epidermal acantholysis in dogs, simulating human benign familial chronic pemphigus (Hailey-Hailey disease). Br J Dermatol 1997;136:190-196.
Congenital hypotrichosis
Congenital hypotrichosis has been described in all domestic species, but it occurs most frequently in calves. The hairlessness may be associated with congenital anomalies of other systems, such as brachygnathism, dental defects, and thymic or genital abnormalities. Many affected animals are otherwise completely healthy, but some forms of congenital hypotrichosis are associated with ill-thrift and early death. Deliberate propagation of spontaneous mutations producing hairlessness has resulted in development of specific hairless breeds, such as the Chinese Crested dog, Mexican Hairless dog, American Hairless Terrier, Sphinx cat, and Mexican Hairless pig, among others. The haircoat is an important protective barrier for animals, and when it is compromised, as in congenital hypotrichosis, affected animals are predisposed to sunburn, less tolerant to temperature extremes, and more susceptible to bacterial and fungal infection.
Hairlessness varies from partial to complete. Partial hypotrichosis is frequently bilaterally symmetrical, and the hair that is present is frequently abnormal. It is usually sparse, short and fine, or coarse and wiry, brittle, and easily broken or epilated. Histologic changes are variable, likely a reflection of the different mutations responsible for the hypotrichosis. Some affected animals have only follicular disease, whereas others have involvement of other skin appendages, in which case the condition is called ectodermal dysplasia.
Genetic hypotrichosis must be differentiated from various causes of nongenetic hypotrichosis. Iodine deficiency can cause goiter and hypotrichosis in piglets, lambs, and calves. Adenohypophyseal hypoplasia in Guernseys and Jerseys, and maternal ingestion of Veratrum album by Japanese cattle, has been associated with hairlessness in calves. In addition, alopecia of various degrees has been associated with intrauterine infection with bovine viral diarrhea virus in calves and classical swine fever virus in piglets.
Cattle
Various types of inherited hypotrichosis occur in cattle. Many breeds of cattle are affected, and the mode of inheritance varies with the particular form of hypotrichosis. Histologic features are not well characterized for all forms of hypotrichosis in cattle.
A form of lethal hypotrichosis occurs in Holstein-Friesian and Japanese native cattle. Calves are born almost hairless and have only small amounts of hair on the muzzle, eyelids, ears, tail, and pasterns. The condition is inherited as a simple autosomal recessive trait, and homozygous calves die within hours after birth. Histologically the skin contains normal numbers of follicles, but they are shallow, rudimentary in appearance, and do not form hairs. Sebaceous glands and arrector pili muscles appear normal; sweat glands undergo cystic degeneration.
A condition called semihairlessness has been reported in polled and horned Hereford calves. Calves have a thin coat of short fine, curly hair at birth and progressively develop a patchy sparse coat of coarse wiry hair that is thicker and longer on legs than elsewhere. The skin is wrinkled and scaly. Animals may not grow well and may have a wild temperament. The condition is a simple autosomal recessive trait. The histologic changes described are dysplastic hair follicles that do not produce hairs. Similar histologic features have been described in viable hypotrichosis reported in various breeds of cattle, including Guernseys, Jerseys, Holsteins, Ayrshires, and Herefords. Calves are born with various degrees of hairlessness. The condition appears to be inherited as a simple autosomal recessive trait in all breeds affected.
Hypotrichosis and anodontia (hypotrichosis anodontia defect, HAD) has been described in male mixed Maine-Anjou-Normandy cross calves and suspected to be a sex-linked recessive trait. Calves are born hairless and toothless and develop a fine, downy haircoat and partial dentition after several months. Affected calves also have a thick protruding tongue, defective horns, and hypoplastic testicles, and they usually do not survive beyond 6 months of age. Histologic changes include small, inactive hair follicles, deformed dermal papillae lacking a vascular network, and degenerative sweat glands. A HAD syndrome, with hypotrichosis, almost complete lack of teeth, and complete absence of eccrine nasolabial glands, has been observed in a family of German Holsteins; similar anomalies in humans are known as X-linked anhidrotic ectodermal dysplasia (ED1). This Holstein phenotype was inherited as a monogenic X-linked recessive trait and was caused by a deletion in the bovine ED1 gene.
Hypotrichosis and incisor anodontia (hypotrichosis incisor defect, HID) has been described in Holstein-Friesian cross calves, and inheritance is suspected to be an X-linked incompletely dominant gene. Affected calves have variable areas of thin coat of fine short silky hairs usually involving the face, neck, ears, back, and inner thighs. Eyelashes, vibrissae, and tail brush are usually normal. Calves may become normal with age. Histologically, there are numerous small hairs, but large medullated hairs are absent, and only telogen follicles are evident in severely affected HID calves.
Inherited epidermal dysplasia, also called baldy calf syndrome, is a lethal disease of Holstein-Friesian calves that is likely inherited as a single autosomal recessive trait. The disease causes loss of condition and skin, horn, and hoof lesions that can be confused with inherited zinc deficiency. Calves appear normal at birth, but at 1-2 months of age, they begin to lose condition despite normal appetite, and develop generalized hair loss and patchy areas of scaly, wrinkled, thickened skin over the neck, shoulders, flanks, and on pressure points. Hooves are elongated, narrow, and pointed and frequently have horizontal rippling. Horns fail to develop, and ear tips are curled backward. Calves have fine slender limbs and drool. They become emaciated and usually die at 6-8 months of age. Histologic examination indicates variable atrophy of adnexa, remnants of hair follicles and sebaceous glands incorporated into the basal layer, and scattered atrophic remnants of epitrichial sweat glands.
Congenital hypotrichosis of Hereford cattle is thought to be due to a simple autosomal dominant gene. Alopecia is variable and nonprogressive. Calves have thin, pliable skin, extremely curly facial hair, and may have sparse pelage of thin soft curly, easily broken and epilated hairs, or they may be completely hairless. Some calves also have impaired hoof development. The condition is characterized histologically by hypoplastic or degenerate hair follicles with vacuolation and necrosis of Huxley's and Henle's layers and abnormally large trichohyaline granules in Huxley's layer. Most follicles contain fragmented hair shafts. Arrector pili muscles are reduced in number and frequently not associated with hair shafts. Ultrastructural examination indicates that the giant trichohyaline granules lack normal microfilament and macrofilament structures.
A condition consisting of congenital anemia, dyskeratosis, and progressive alopecia has also been described in polled Hereford calves in Canada and the United States. Affected calves are often small at birth and have a prominent forehead. They have a hyperkeratotic muzzle with a dirty faced appearance, and their hair is wiry and kinked or tightly curled and easily epilated. Alopecia is evident initially on the bridge of the nose and ears, and it becomes generalized but is most severe on the head, lateral neck, shoulders, and back. The skin of the face and neck is wrinkled, and hairless skin is hyperkeratotic. Affected calves also have nonregenerative anemia and fail to grow despite a normal appetite. Histologic abnormalities in the skin consist of orthokeratotic hyperkeratosis and hypergranulosis extending into the infundibular portion of hair follicles and prominent dyskeratosis (apoptosis) of individual epidermal and follicular keratinocytes. Hair follicles are normal in number, but many follicles are in telogen phase. There is degeneration of the internal root sheath and atrophy of sebaceous glands. The bone marrow is hyperplastic and characterized by ineffective erythropoiesis with maturation arrest in the late rubricyte stage.
The “rat-tail syndrome” is a form of hereditary congenital hypotrichosis that occurs in a small percentage of calves produced by crossing some Continental cattle breeds, for instance, Simmental with black Angus or Holsteins. The calves have short, curly, malformed, sometimes sparse hair, and a lack of normal tail switch development.
Dogs
X-linked hypohidrotic ectodermal dysplasia (XHED) has been documented in dogs and the inheritance confirmed by breeding studies. XHED is a spontaneous model for the disease in humans. Affected dogs have a triad of lesions: patterned hairlessness, an absence of atrichial sweat glands, and dental abnormalities (conically shaped teeth, anodontia). The lack of hair is apparent on the dorsal head, ventrum, and dorsal tail base (eFig. 6-7). The dogs also have absence of serous and mucinous glands in the trachea, esophagus, and bronchi. The puppies have decreased weight gain and fail to thrive. Hairless areas may have decreased adnexal density as well as partial to complete adnexal loss. XHED is caused by a mutation in ectodysplasin 1 (ED1), which encodes for transmembrane proteins, with a short intracellular domain, a transmembrane domain, and a tumor necrosis factor–ligand motif. This protein is thought to control some epithelial-mesenchymal cell interactions that regulate development of the ectoderm. In humans, this disease causes significant mortality and mortality resulting from hyperthermia and respiratory infections.
eFigure 6-7.

Patterned hairlessness on the dorsum of the head of a dog with X-linked hypohidrotic ectodermal dysplasia.
A semidominant form of ectodermal dysplasia has been documented in congenitally hairless breeds (Mexican and Peruvian hairless dogs, Chinese Crested dog). The disorder has been associated with a member of the forkhead box transcription factor family (FOXI3), which is specifically expressed in developing hair and teeth.
Cats
An autosomal recessive form of congenital hypotrichosis has been described in Siamese and Birman kittens. The Birman kittens were born virtually hairless and had short fragile wrinkled whiskers or lacked whiskers altogether. Both males and females were affected. Although initially healthy, all affected kittens in one report died by 13 weeks of age from various infections. Postmortem examination of some of the affected Birman kittens revealed thymic aplasia and lymphoid depletion of paracortical regions of lymph nodes, spleen, and Peyer's patches, suggesting an immunologic deficiency. Histologic examination of skin indicated reduced numbers of primary hair follicles, which were hypoplastic and devoid of hairs. Sebaceous glands were normal, but sweat glands were hypoplastic and in decreased number, and arrector pili muscles were rare.
Hereditary hypotrichosis is recognized in piglets, and there may be both dominant and recessive forms. The dominant form is thought to be lethal in homozygotes; it is characterized histologically by a decreased number of hair follicles, and most appear atrophic. Congenital hypotrichosis is thought to be a simple autosomal recessive trait in polled Dorset sheep. Alopecia is most pronounced on the face and legs. Histologic abnormalities consist of hypoplastic hair follicles containing keratosebaceous material but no hairs. Congenital hypotrichosis has been described in a Percheron, but is rare in horses. Congenital hypotrichosis is rare in goats.
Further reading
Bracho GA, et al. Further studies of congenital hypotrichosis in Hereford cattle. Zbl Vet Med A 1984;31:72-80.
Casal ML, et al. Congenital hypotrichosis with thymic aplasia in nine Birman kittens. J Am Anim Hosp Assoc 1994;30:600-602.
Casal ML, et al. X-linked ectodermal dysplasia in the dog. J Hered 1997;88:513-517.
Drögemüller C, et al. Congenital hypotrichosis with anodontia in cattle: a genetic, clinical and histological analysis. Vet Dermatol 2002;13:307-313.
Drögemüller C, et al. A mutation in hairless dogs implicates FOXI3 in ectodermal development. Sci 2008;321:1462.
Hanna PE, Ogilvie TH. Congenital hypotrichosis in an Ayrshire calf. Can Vet J 1989;30:249-250.
Hendy-Ibbs PM. Hairless cats in Great Britain. J Hered 1984;75:506-507.
Ihrke PJ, et al. Generalized congenital hypotrichosis in a female Rottweiler. Vet Dermatol 1993;4:65-69.
Jubb TF, et al. Inherited epidermal dysplasia in Holstein-Friesian calves. Aust Vet J 1990;67:16-18.
Mackie JT, McIntyre B. Congenital hypotrichosis in Poll Dorset sheep. Aust Vet J 1992;69:146-147.
Mauldin EA, et al. Neonatal treatment with recombinant ectodysplasin prevents respiratory disease in dogs with X-linked ectodermal dysplasia. Am J Med Gen 2009;149A:2045-2049.
Moura E, Cirio SM. Clinical and genetic aspects of X-linked ectodermal dysplasia in the dog—a review including three new spontaneous cases. Vet Dermatol 2004;15:269-277.
Schalles RR, Cundiff LV. Inheritance of the “rat-tail” syndrome and its effect on calf performance. J Anim Sci 1999;77:1144-1147.
Steffen DJ, et al. Ultrastructural findings in congenital anemia, dyskeratosis, and progressive alopecia in Polled Hereford calves. Vet Pathol 1992;29:203-209.
Valentine BA, et al. Congenital hypotrichosis in a Percheron draught horse. Vet Dermatol 2001;12:215-217.
Hypotrichosis associated with pigmentary alterations
Generalized or regional alopecia attributed to follicular dysplasias that include histologic evidence of pigment abnormalities have been frequently described in dogs and less frequently in other species. They have arbitrarily been divided into 2 categories.
The first of these 2 categories is color dilution alopecia, described in color-dilute animals of breeds such as the Doberman Pinscher, Irish Setter, Dachshund, Chow Chow, Poodle, Whippet, Italian Greyhound, Boston Terrier, Chihuahua, Saluki, Yorkshire Terrier, and mongrels, in which the onset of alopecia can be tardive, generally ranging from 4 months to 3 years. Puppies are born with normal hair, but develop slowly progressive alopecia (Fig. 6-25 ). Pedigree analysis in color-dilute Dachshunds suggests this disorder may be inherited as an autosomal recessive trait. The histologic lesions include misshapen, fragmented anagen hair follicles with pigment clumping in follicular epithelium, hair bulb matrix cells, hair shafts, infundibular keratin, and epidermis (Fig. 6-26). Melanin-containing macrophages are frequently present in the dermis around hair bulbs. There can be some hair follicle atrophy in chronic cases; however, this is a secondary change. A condition similar to color-dilution alopecia in dogs has been described in cattle as cross-related congenital hypotrichosis. This has been reported in crosses involving Simmental, Gelbvieh, and Charolais cattle, most common in the Simmental-Angus and Simmental-Holstein crosses. The condition appears in calves that have color-dilute (gray or chocolate) coats. The affected hair is short, curly, and sparsely haired, leaving the white-haired areas of the coat unaffected. The histologic lesions are virtually identical to canine color-dilution alopecia. Coat-color–linked hair follicle dysplasia has also been described in buckskin Holstein cows (color-dilute tan-and-white Holsteins). These animals have short and clinically abnormal hair in the tan areas of the coat.
Figure 6-25.

Pigmentary follicular dysplasia in 2 dogs. A. In black hair follicular dysplasia, the hair loss is confined to pigmented areas. B. The dog with color-dilution alopecia has generalized thinning hair loss.
Figure 6-26.
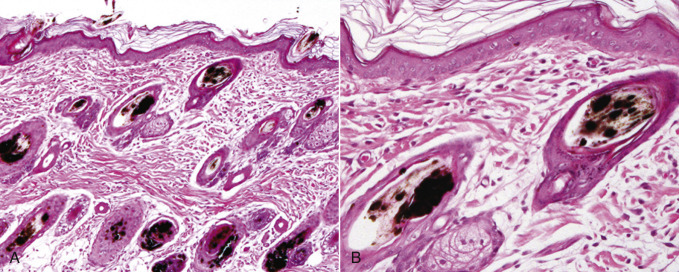
Black hair follicular dysplasia in a 12-week-old puppy. A. Note the clumped melanin in the hair bulbs as well as an accumulation of coarse free melanin within hair follicle infundibula and within misshapen hair shafts. B. Higher magnification.
The second traditional category is black hair follicular dysplasia (see Fig. 6-25), seen in bicolor or tricolor black and white dogs, such as Bassett Hounds, Beagles, Bearded Collies, and mongrels, and in Holstein cattle, in which the alopecia affects only the black-haired areas of the coat, and in which onset is generally in the first few weeks or months of life. Black hair follicular dysplasia is thought to be an autosomal inherited disorder in mongrel puppies, and is thought to have a genetic component in some purebred animals such as Bearded Collies. The histologic lesions in black hair follicular dysplasias are virtually identical to those of color-dilution alopecia. A difference in the appearance of the melanin clumps in whole mounts of hair shafts has been suggested. In Greater Musterlanders, the hair shaft defect appears to be associated with inadequate and disorganized melanosome transfer to keratinocytes, with resultant melanin clumping (see Fig. 6-26 ).
There are other follicular dysplasias associated with pigment abnormalities that do not fall easily into these 2 categories, but have similar histologic changes. These include follicular dysplasia in the Portuguese Water dog that occurs in the black or red color phase of this breed. These are not color-dilute dogs, and the onset can be tardive, generally between 3 months and 5 years. Black-and-red Doberman Pinschers that are not phenotypically color dilute are also reported to have a follicular dysplasia that is generally confined to the caudal dorsum and that has an adult onset. An adult-onset alopecic disorder has been identified in Chesapeake Bay Retrievers (eFig. 6-8). Clinically, the hair loss occurs on the axillae, ventral thorax, flanks, ventrum, dorsum, rump, and/or the caudal part of the thighs in both male and female dogs. Histologically, the lesions resemble cyclic flank alopecia (follicular atrophy with hyperkeratosis), with occasional melanin clumping and hypereosinophilic hair shafts. Follicular dysplasia has been described in Weimaraners, in which affected young adults had progressive alopecia of the trunk with recurrent folliculitis/furunculosis. In cattle, follicular dysplasia has been reported in black Angus and black Angus-Brahman crosses; the histologic changes are similar to those in dogs. These cattle are all black animals that are not phenotypically color dilute; however, there is adult onset of alopecia that is more commonly associated with color-dilution alopecia. In view of the dysplasias in Portuguese Water dogs, black-and-red Doberman Pinschers, and black Angus and their crosses that occur in animals not phenotypically color dilute but that can have adult onset, it is quite possible that separation of follicular dysplasias with pigmentary alteration into color-dilution alopecia and black hair follicular dysplasia is artificial. It is likely that these histologically similar follicular dysplasias are subtypes of a single process; however, until the mechanism underlying follicular dysplasia is characterized, the classification is somewhat arbitrary.
eFigure 6-8.

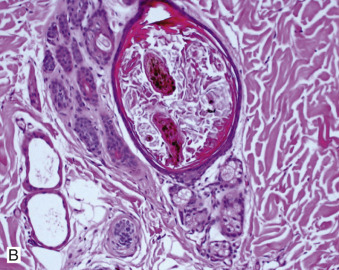
Chesapeake Bay Retriever alopecia. A. The hair loss occurs on the axillae, ventral thorax, flanks, ventrum, dorsum, rump, and/or the caudal part of the thighs in both male and female dogs. B. Histologically, the lesions resemble cyclic flank alopecia (follicular atrophy with hyperkeratosis), with occasional melanin clumping and hypereosinophilic hair shafts.
Further reading
Ayers JR, et al. Pathological studies of cross-related congenital hypotrichosis in cattle. J Vet Med 1989;36:447-456.
Beco L, et al. Color dilution alopecia in seven Dachshunds. A clinical study and the hereditary, microscopical and ultrastructural aspect of the disease. Vet Dermatol 1996;7:91-97.
Cerundolo R, et al. Adult onset hair loss in Chesapeake Bay retrievers. A clinical and histological and study. Vet Dermatol 2005;16:39-46.
Hargis AM, et al. Black hair follicular dysplasia in black and white Saluki dogs: differentiation from color mutant alopecia in the Doberman Pinscher by microscopic examination of hairs. Vet Dermatol 1991;2:69-83.
Ishida Y, et al. A homozygous single-base deletion in MLPH causes the dilute coat color phenotype in the domestic cat. Genomics 2006;88:698-705.
Kim JH, et al. Color-dilution alopecia in dogs. J Vet Sci 2005;6:259-261.
Laffort-Dassot C, et al. Follicular dysplasia in five Weimaraners. Vet Dermatol 2002;13:253-260.
Mansell JL. Follicular dysplasia in two cows. Vet Dermatol 1999;10:143-147.
Miller WH. Follicular dysplasia in adult black and red Doberman Pinschers. Vet Dermatol 1990;1:181-187.
Miller WH. Alopecia associated with coat color dilution in two Yorkshire terriers, one saluki and one mix-breed dog. J Am Anim Hosp Assoc 1991;27:39-43.
Miller WH, Scott DW. Follicular dysplasia of the Portuguese water dog. Vet Dermatol 1995;6:67-74.
Ostrowski S, Evans A. Coat-color-linked hair follicle dysplasia in “buckskin” Holstein cows in central California. Agri Pract 1989;10:12-13.
Rachid MA, et al. Concurrent follicular dysplasia and interface dermatitis in Boxer dogs. Vet Dermatol 2003;14:159-166.
von Bomhard W, et al. Black hair follicular dysplasia in Large Munsterlander dogs: clinical, histological and ultrastructural features. Vet Dermatol 2006;17:182-188.
von Tscharner C, Halliwell REW, editors. Advances in Veterinary Dermatology, vol. 1. London: Baillière Tindall; 1990.
Welle M, et al. MLPH genotype—melanin phenotype correlation in dilute dogs. J Hered 2009;100:75-79.
Hypertrichosis
Congenital hypertrichosis, a condition characterized by an excessive amount of hair, is rare. In some instances, the abnormality involves a change in the character of the hair rather than an absolute increase in amount. Excessively long hair is inherited as an autosomal dominant trait in Friesian cattle in Europe. The condition results in discomfort during hot weather and decreased productivity. High environmental temperature during gestation has been associated with an unusual hairy appearance of newborn lambs. The lambs are small, and most do not survive to weaning; the histologic appearance of this abnormality has not been described. Border disease is a congenital pestiviral infection of sheep in which lambs are born weak and small, have an abnormal haircoat, and exhibit tonic-clonic spasms (hairy shaker disease). Instead of the normal short, fine, closely crimped birthcoat, affected lambs have a long, straight, coarse coat. The coat abnormality is due to aberrant differentiation of hair follicles that develops only when infection occurs prior to 80 days of gestation. The histologic changes include enlargement of primary hair follicles with an increased degree of medullation and a decreased number and retarded development of secondary follicles.
Further reading
Derbyshire MB, Barlow RM. Experiments in Border disease. IX. The pathogenesis of the skin lesion. J Comp Pathol 1976;86:557-570.
Shelton M. Relation of environmental temperature during gestation to birth weight and mortality of lambs. J Anim Sci 1964;23:360-364.
Canine dermatomyositis
Dermatomyositis is an idiopathic inflammatory condition of skin, muscle, and occasionally blood vessels of humans and dogs. A familial pattern of occurrence has been found in Collies, Shetland Sheepdogs (Shelties), and their crosses. It has also been described in Beauceron Shepherd, Belgian Tervuren, and Portuguese Water dogs. A similar disease, referred to as dermatomyositis-like disease, has been described in a number of other breeds. Dermatomyositis in Collies is an autosomal dominant trait with variable expressivity; and it appears to be widespread in Collies in the United States. The disease in Collies has been proposed as a model for a nonfatal form of childhood dermatomyositis, although familial cases are uncommon in humans. The condition in Shelties has been linked to chromosome 35. Dermatomyositis has been identified in Shelties in the United Kingdom. The disease has not been characterized as well in this breed; but it appears that myositis is a less prominent feature of the disease in Shelties.
Dermatomyositis must be distinguished from vaccine-associated ischemic dermatopathy. The latter condition tends to occur in small-breed dogs 1-5 months following rabies immunization. At sites distant from the vaccine injection site, the histologic features are indistinguishable from dermatomyositis. The histologic changes of ischemic dermatopathy can be categorized into 5 subtypes: (1) canine familiar dermatomyositis, (2) juvenile-onset ischemic dermatopathy (similar to canine familial dermatomyositis except for the breed predispositions), (3) focal postrabies vaccination reaction, (4) generalized vaccine-induced ischemic dermatopathy, and (5) adult-onset non–vaccine-induced generalized ischemic dermatopathy.
The cause and pathogenesis of dermatomyositis are unknown. The primary target is thought to be capillary endothelium, although histologic evidence of vessel wall inflammation is often absent. Skin and muscle lesions are a consequence of ischemia leading to atrophy of hair follicles and muscle. Variation in expression of dermatomyositis in dogs suggests that factors other than simple autosomal dominant inheritance are involved in the etiopathogenesis of the disease. Immunologic mechanisms are thought to be involved in this disease in humans, and both cell-mediated and humoral immunity have been implicated in the pathogenesis. In Collies with dermatomyositis, serum levels of circulating immune complexes were found to be increased above normal before clinical disease was evident; the onset and severity of dermatitis and myositis correlated with the serum levels of circulating immune complexes and IgG, and circulating immune complex levels decreased to normal as disease resolved. These findings suggest that the immune complexes initiated inflammation rather than resulted from it. IgG was identified as the immunoglobulin component of the immune complexes, but the identity of the antigen component was not determined. Dermatomyositis has been associated with viral, bacterial, and Toxoplasma infections, but infectious agents are generally not isolated from tissues of affected people. Crystalline structures, suggestive of picornaviruses, have been seen in endothelial cells of muscle from severely affected Collies. Cases in humans have also occurred following immunization, therapy with various drugs, during pregnancy, and in association with neoplasia.
Skin lesions usually develop in juvenile dogs at 7 weeks to 6 months of age. Earliest lesions consist of small pustules, vesicles, papules, and nodules that evolve into erythematous, crusty, ulcerated, alopecic areas with hypopigmentation or hyperpigmentation (Fig. 6-27 ). Lesions are most common on the pinnae, bridge of the nose, lips, periocular skin, over bony prominences of the distal extremities, sternum, and tip of the tail. Mucous membranes and mucocutaneous junctions may be transiently involved early in the course of disease. Pawpad ulceration is rare. The disease exhibits a waxing and waning course over weeks to months, with a variable outcome. In mildly to moderately affected dogs, lesions may resolve spontaneously in 6-12 months, whereas in severely affected dogs, lesions may regress but do not usually resolve completely, and disease may be lifelong and extensive. Lesions heal with no residual scarring in mildly affected dogs; permanent alopecic, hypopigmented, or hyperpigmented disfiguring scars develop, especially on the face, in severely affected dogs. Lesions may be exacerbated by estrus, parturition, or exposure to sunlight. Although cases of adult-onset dermatomyositis have been reported, it is likely that at least some of these dogs had mild transient lesions that were overlooked when they were pups and subsequently developed more obvious disease as adults.
Figure 6-27.

Familial canine dermatomyositis in a Shetland Sheepdog. The muzzle and periocular areas have scarring alopecia with small ulcers and hyperpigmentation and hypopigmentation.
Myositis usually develops several weeks after dermatitis and is proportional in severity to the dermatitis. It is usually first recognized as a bilaterally symmetrical decrease in temporal muscle mass. However, because of the dolichocephalic shape of the Collie head, mild temporal or masseter muscle atrophy may be missed. Myositis principally involves muscles of mastication and extremities below the elbow and stifle, but it is more generalized in more severely affected dogs. Over time, active myositis is succeeded by muscle atrophy and fibrosis. Generalized symmetrical muscle atrophy, weakness, and exercise intolerance may develop in moderately and severely affected dogs. Megaesophagus may develop in some dogs.
Various additional abnormalities may accompany skin and muscle lesions in more severely affected dogs. Peripheral lymph nodes are enlarged because of reactive hyperplasia. Conjunctivitis may develop in dogs with severe periocular skin lesions or because of facial palsy and inability to blink. More severely affected dogs are small and unthrifty compared with normal or mildly affected dogs. Fever and joint swelling are noted in some dogs. Secondary bacterial pyoderma, septicemia, or megaesophagus with secondary aspiration pneumonia may develop in more severely affected dogs. Demodicosis may also be present and complicate diagnosis. Severe secondary amyloidosis with resultant renal failure has been described in one affected Collie.
Affected dogs have variable and usually nonspecific clinicopathologic abnormalities. Moderately and severely affected dogs commonly have inflammatory leukogram changes that include neutrophilia, with or without a left shift, and monocytosis. Nonregenerative anemia typical of chronic inflammation may develop in severely affected dogs. Serum creatine kinase levels in Collies with dermatomyositis were normal or only slightly increased; however, most serum muscle enzyme determinations were done in later stages of disease when active myositis may have been waning. Mild to moderate elevations in serum creatine kinase concentrations were present in several young Shelties with the disease. Occasionally, dogs have positive Coombs tests, and rarely, rheumatoid factor (RF) tests are positive.
The histologic changes in the skin are variable and may be quite subtle or nonspecific. Early lesions consist of scattered individual vacuolated or shrunken, brightly eosinophilic necrotic keratinocytes in the epidermis and infundibular portion of hair follicles. Hydropic degeneration of basal keratinocytes is often present and leads to dermal-epidermal clefts that develop into vesicles that contain proteinaceous fluid, erythrocytes, and inflammatory cells. Diagnostically useful artifactual dermal-epidermal separation may be induced at the margins of the section by the shearing action of the punch biopsy. Ulceration and crusting result from lesions with extensive dermal-epidermal separation. Intraepidermal pustules are uncommon. Hyperkeratosis and acanthosis are variable. In the absence of ulceration, dermal inflammation tends to be mild and consists of mixed cells either surrounding superficial dermal vessels, hair follicles, and glands or distributed in an interface pattern, or in some cases, diffusely distributed. The infiltrate includes mononuclear cells primarily, fewer neutrophils, and occasional eosinophils and mast cells. The most consistently present histologic abnormalities are follicular atrophy and perifollicular inflammation that may be accompanied by perifollicular fibrosis (Fig. 6-28A-C ). Variable dermal fibrosis is usually evident in biopsies from dogs >6 months of age. Muscle lesions include multifocal interstitial and perivascular infiltrations with mixed cells; myofiber degeneration, regeneration, and atrophy; and fibrosis. Vasculitis is an infrequent and subtle finding in the skin, muscle, and occasionally in other tissues.
Figure 6-28.
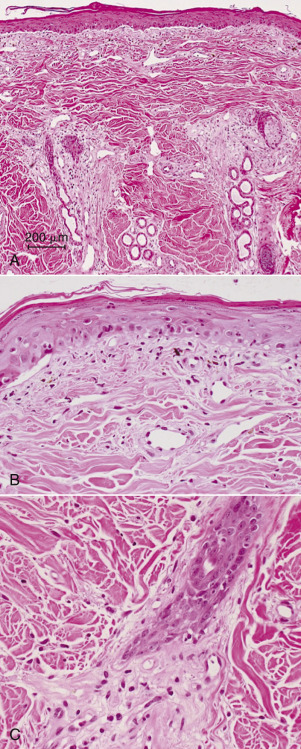
Familial canine dermatomyositis. A. Low magnification showing follicular atrophy, and orphaned adnexal structures. B. Higher magnification showing cell-poor hydropic, interface dermatitis with dermoepidermal clefting. C. An atrophic (faded) follicle is surrounded by prominent connective tissue and scattered lymphocytes and plasma cells.
Further reading
Bresciani F, et al. Dermatomyositis-like disease in a Rottweiler. Vet Dermatol 2014;25:229-232.
Clark LA, et al. Linkage of dermatomyositis in the Shetland sheepdog to chromosome 35. Vet Dermatol 2005;16:392-394.
Ferguson EA, et al. Dermatomyositis in five Shetland sheepdogs in the United Kingdom. Vet Rec 2000;146:214-217.
Hargis AM, et al. Severe secondary amyloidosis in a dog with dermatomyositis. J Comp Pathol 1989;100:427-433.
Hargis AM, Mundell AC. Familial canine dermatomyositis. Compend Contin Educ Pract Vet 1992;14:855-862, 864-865.
Morris DO. Ischemic dermatopathies. Vet Clin North Am Small Anim Pract 2013;43:99-111.
Wahl JM, et al. Analysis of gene transcript profiling and immunobiology in Shetland sheepdogs with dermatomyositis. Vet Dermatol 2008;19:52-58.
White SD, et al. Dermatomyositis in an adult Pembroke Welsh corgi. J Am Anim Hosp Assoc 1992;28:398-401.
Hereditary connective tissue disorders
The connective tissue components of the skin include collagen (primarily types I and III), elastic fibers, and ground substance composed of glycoproteins and proteoglycans. A defect in any one of these skin molecules can result in structural and functional abnormalities of the entire tissue. Inherited connective tissue disorders of skin may consist of abnormalities involving only one of these components, or there may be concurrent alterations in several components. Hereditary collagen dysplasia, the most commonly recognized connective tissue disease, is a complex group of disorders of collagen that results in decreased tensile strength of the skin and may also affect other connective tissues. Alterations in elastic fibers and ground substance may accompany some forms of collagen dysplasia, but there are also diseases in which an abnormality of the elastic fibers or ground substance appears to be primary. Diagnosis of many of these conditions requires ultrastructural examination and biochemical analysis to confirm the presence of structural abnormalities and to identify the molecular defect.
Hereditary collagen dysplasia
Collagen dysplasia (dermatosparaxis, Ehlers-Danlos syndrome, cutaneous asthenia, cutis hyperelastica) has been reported in humans, cattle, sheep, horses, dogs, cats, mink, and rabbits. Collagen is the major structural protein in skin and other connective tissues, and abnormalities in its structure result in skin that is fragile, easily torn, and frequently hyperextensible and loose. In humans, Ehlers-Danlos syndrome (EDS) is divided into at least 10 types based on clinical, biochemical, and molecular genetic studies. The natural history of clinical disease and mode of inheritance vary among the different types of EDS. Joint laxity, vascular abnormalities, bowel or uterine rupture, bone abnormalities, ocular abnormalities, and periodontal disease occur in addition to the fragile skin in the various forms of human EDS. Inheritance may be autosomal dominant, autosomal recessive, or X-linked recessive. In animals, clinical disease has been restricted almost exclusively to skin abnormalities and has been characterized in only a few breeding colonies or herd outbreaks. Most instances of collagen dysplasia occur in single animals, and the molecular defect and mode of inheritance are usually not determined.
Individuals with inherited collagen dysplasia typically have a history of frequent skin lacerations following routine handling, such as shearing or manual restraint; normal activities, such as scratching or playing with littermates; or minor trauma. The skin wounds commonly develop into wide gaping wounds with minimal hemorrhage. Healing usually proceeds normally but results in characteristic thin, pale wrinkled scars resembling tissue paper. Extracutaneous signs, such as joint laxity and ocular abnormalities, have been reported in animals only rarely. The skin is usually soft and velvety, hyperextensible, and may hang in loose folds. In some affected animals, the skin laxity becomes progressively more pronounced with age. Severity of clinical signs is variable, even among animals with the same biochemical abnormality. This variability in clinical severity is most pronounced in sheep. One form of the disease described in sheep exhibits such severe manifestations that all lambs die or require euthanasia within the first day or 2 of life. A second milder form of collagen dysplasia is usually not recognized until later in life when sheep are handled for shearing. In general, the disease tends to be most severe in sheep, less severe in cattle, followed by dogs and cats, and least severe in horses.
Diagnosis of collagen dysplasia is based on typical clinical signs and demonstration of morphologic or biochemical abnormalities of the dermal collagen. In some cases, abnormalities are evident at the light microscopic level, but frequently none are found or the differences are subtle and difficult to determine except by comparison to a breed- and age-matched control. The dermis may be normal, thinner than normal, or thicker than normal because of an increased amount of ground substance. Collagen fibers may be widely separated, finer and paler than normal, and haphazardly arranged. Rarely, increased numbers of elastic fibers are seen with elastic stains. Fibroblasts are in increased numbers in the dermis of some affected animals. Abnormal collagen fibers may stain unevenly with collagen stains such as Masson trichrome. Instead of the uniform blue staining of normal collagen, the abnormal collagen may have a red core. This staining feature is not unique to collagen dysplasia, however, as uneven collagen staining also occurs with degenerative disorders of collagen.
In most cases, ultrastructural examination is required to confirm the collagen abnormality. A variety of alterations of collagen fibrils have been found. In longitudinal sections, collagen fibrils may be loosely wound and flat or helical. In cross-section, they may have several irregular thin projecting arms that give them a “hieroglyphic” appearance. This appearance is typical of dermatosparaxis of sheep and cattle and has also been described in a Himalayan cat and a dog. In other forms of the disease, the collagen fibrils are shaped normally but vary markedly in diameter from the normal range. They may all be uniformly larger or smaller, or there is a mixed population of fibrils that extend beyond the range of normal minimum and maximum diameter sizes. The fibrils frequently are loose and disorganized rather than being arranged in uniform, compact bundles.
The ultrastructural abnormalities are not specific, and biochemical analysis is necessary to determine the particular molecular defect. Collagen synthesis is a multistep process that includes extensive post-translational processing involving multiple intracellular and extracellular enzymes. Abnormalities in several of these enzymes as well as structural mutations involving the collagen chains have been identified in the various forms of collagen dysplasia in humans and animals. For unknown reasons, the same biochemical defect may produce different clinical abnormalities in different individuals and in different species.
Cattle
Collagen dysplasia in cattle is usually referred to as dermatosparaxis, which means “torn skin.” The condition is caused by a mutation in the gene for procollagen I N-proteinase (also called procollagen aminopeptidase), the enzyme that excises the amino-propeptide of type I and type II procollagens. Each of the 3 polypeptide chains making up a collagen molecule have short extensions at the amino and carboxy termini. These additional propeptides make the molecules soluble, to aid in their transport out of the cell. Subsequent extracellular conversion of the procollagen to collagen requires 2 enzymes to cleave the amino- and carboxy-terminal extensions. Following cleavage of the procollagen peptides, the collagen molecules spontaneously assemble into collagen fibrils. The defect in processing of type I procollagen to collagen results in abnormal precursor molecules with peptide extensions that inhibit formation of uniform fibers and fibers capable of producing normal cross-links. They assemble instead into abnormal ribbon-shaped collagen fibrils lacking normal tensile strength. Dermatosparaxis in cattle is recessively inherited as is the biochemically analogous condition in humans, Ehlers-Danlos syndrome type VII C, although clinical signs are not identical.
Most affected calves have thick, wet skin that tears easily and sometimes hangs in loose folds. Associated joint laxity and soft bones have been reported rarely. Light microscopic changes consist of a thicker than normal dermis composed of sparse bundles of fine pale collagen distributed in abundant Alcian blue–positive ground substance (proteoglycans). Individual collagen fibers are smaller in diameter than in normal skin, and their arrangement appears disorganized. There may be an increase in dermal elastin and number of fibroblasts. Ultrastructural examination reveals the collagen to be arranged in loose, twisted flat, or helical ribbons rather than being organized in compact parallel arrays. In cross-section, these fibrils have irregular projecting arms that confer a “hieroglyphic” appearance.
Sheep
At least 2 forms of collagen dysplasia, called dermatosparaxis, have been described in sheep, that is, a severe form in lambs noted shortly after birth, and a milder form not apparent until sheep are handled as adults. The severe form has been described in Norwegian Dala sheep, Border-Leicester-Southdown crossbred sheep in Australia, and white Dorper sheep in South Africa. The condition is inherited as a simple autosomal recessive trait. Only in the Dala breed has the biochemical defect been identified, and it consists of a deficiency in procollagen aminopeptidase activity, as in bovine dermatosparaxis. In Border-Leicester-Southdown crossbred lambs, the biochemical abnormality was not determined, but it did not appear to be a procollagen peptidase deficiency because there was no increase in dermal procollagen detected. Affected lambs develop skin lacerations during birth or shortly thereafter. The skin is soft and edematous. Lambs frequently die within a few days as a consequence of wound infection and septicemia. Gross examination of the skin indicates that the dermis is moist and thicker than normal, with a jelly-like consistency. In some instances, increased friability of internal organs and joint capsules was observed. The histologic and ultrastructural abnormalities are similar to those in cattle with dermatosparaxis.
The less severe form of dermatosparaxis has been found in Merino sheep in Australia when adult sheep were handled for shearing. No skin hyperelasticity or joint hypermobility are associated with the skin fragility. The skin lacerations predispose affected individuals to infections and fly strike. This form is also caused by a deficiency of procollagen aminopeptidase activity. Light microscopic examination reveals a loose, more open appearance to the dermis and a significant increase in the number of dermal fibroblasts in comparison to normal skin. Most collagen fiber bundles are smaller and more lightly stained than those in normal skin. The collagen in some areas is arranged in prominent layers. Transmission electron microscopic examination shows a combination of distorted, hieroglyphic-type fibrils mixed with normal collagen fibrils.
Horses
Hereditary equine regional dermal asthenia (HERDA) is an autosomal recessive skin disorder in Quarter Horses, and predominantly those that originated from elite cutting horse bloodlines. The affected horses have hyperextensible and loose fragile skin that results in poor wound healing and disfiguring scars (eFig. 6-9). Collagen dysplasia has also been reported in a Thoroughbred gelding and an Arabian-cross filly. HERDA is not usually recognized until the animal is 6-12 months of age and develops frequent skin wounds and scarring on the legs, shoulders, and saddle area. Although histology is not diagnostic, the deep dermis contains a horizontal clearing in which the collagen fibers are thinner and shorter than normal.
eFigure 6-9.
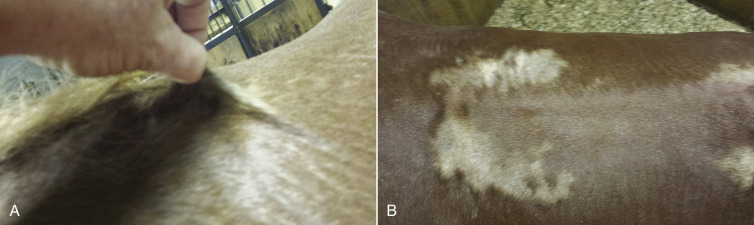
Hereditary regional dermal asthenia in a horse. A. The skin is hyperextensible. B. Large hypopigmented scars are present on the saddle region.
(Courtesy A. Martin.)
Dogs
Collagen dysplasia has been described in many purebred and mixed-breed dogs. Affected dogs typically have soft, easily torn, hyperextensible skin (Fig. 6-29 ). In some cases, the skin hangs in loose pendulous folds, a feature that frequently becomes more prominent with age. Thin, white scars are typically the sequelae to skin wounds. Ocular abnormalities and joint laxity, associated problems commonly seen in humans with Ehlers-Danlos syndrome, have been reported infrequently in dogs, and bone abnormalities are rare. Several breeding studies have shown collagen dysplasia to be inherited in a simple autosomal dominant manner with complete penetrance. The biochemical abnormality has not been identified in any cases of collagen dysplasia in dogs; but the skin of Springer Spaniels with collagen dysplasia has been found to have more uncross-linked α-chains than collagen from normal dogs.
Figure 6-29.

Collagen dysplasia in a dog. Note hyperextensible facial skin.
Histologic changes may be subtle and consist of dermal thinning evident only in comparison to a section from a normal control. In other cases, a decreased amount of dermal collagen, collagen disorganization, variation in collagen staining, increased number of elastic fibers, or increased amount of extracellular matrix may be seen. The abnormal collagen fibers may stain red with trichrome stain. Ultrastructural abnormalities of the collagen consist of variation in the fibril diameter, shape abnormalities, fibril disorganization, and loose fibril packing. A mixture of normal and abnormal collagen fibers may be present.
Cats
Collagen dysplasia in cats is usually referred to as cutaneous asthenia, although in early reports it was called dermatosparaxis. The condition has been reported in a number of breeds; in the majority of the cases, neither the biochemical defect nor the mode of inheritance has been identified. In a single Himalayan cat with collagen dysplasia, the abnormality was determined to be a defect of the amino-terminal procollagen peptidase, as in dermatosparaxis of cattle and sheep. This cat could not be bred, however, and the mode of inheritance was not determined. A breeding study based on an affected male domestic shorthaired cat indicated that the condition is inherited as an autosomal dominant trait, and heterozygous individuals synthesize both normal and abnormal collagen molecules.
Cats with cutaneous asthenia have thin, soft, velvety skin that tears easily but with minimal hemorrhage. Lacerations heal to form typical white, tissue paper–like scars. In some cats, loose folds of skin develop as the cats age. No joint laxity has been described in cats with cutaneous asthenia. Histologic examination of the skin yields variable results. No dermal changes are evident in some cases, whereas in others, the dermis is thinner and collagen fibers are finer and separated by an increased amount of ground substance when compared to skin from an unaffected cat. Normal collagen fibers stain uniformly blue with Masson trichrome stain; abnormal fibers exhibit segmental red staining areas that are birefringent under polarized light. Ultrastructural examination indicates that normal and abnormal collagen fibers may be present in varying proportions. Abnormal fibers are characterized by disorganized, tangled, nonparallel packing of fibrils. Abnormal “hieroglyphic” fibrils were a feature of the affected Himalayan cat.
Skin fragility in cats has also been reported as an acquired condition associated with a number of conditions, including spontaneous and iatrogenic hyperglucocorticism, diabetes mellitus, cholangiohepatitis, hepatic lipidosis, cholangiocarcinoma, multicentric follicular lymphoma, feline infectious peritonitis, disseminated histoplasmosis, and administration of various drugs, including megestrol acetate and other progestational compounds (Fig. 6-30 ). Histologically, cats with acquired skin fragility have profound atrophy of dermal collagen fibers. Collagen fibers are thin and disorganized. Hair follicles are in kenogen and markedly atrophied. The epidermis and other adnexa are also often atrophic. There may be orthokeratotic hyperkeratosis. The exact pathomechanism is unknown; however, it is thought to be related to an effect of glucocorticoids on collagen production. In addition, many of the associated conditions have moderate to severe liver involvement, which suggests that hepatic dysfunction may play a role in pathogenesis.
Figure 6-30.

Feline acquired fragile skin syndrome. Note tearing of fragile skin with minimal hemorrhage.
Abnormalities of elastic fibers
An excess of elastic fibers was reported in several piglets of a litter of Large White X Essex pigs with multiple circular to oval shallow depressed skin lesions. The skin was abnormally elastic in these areas and seemed to be bound less tightly to the underlying subcutis. The increase in thick elastic fibers was present only in those areas in which the skin was hyperextensible, and the condition was termed cutis hyperelastica.
Congenital abnormalities of ground substance
Proteoglycan deficiency.
An abnormality of dermal proteoglycan is a rarely documented cause of fragile skin in humans and animals. Proteoglycan is composed of a core protein and glycosaminoglycan (mucopolysaccharide) side chains, and it is the major component of the extracellular ground substance of the dermis. A 4-month-old female Holstein calf with skin fragility, soft and hyperextensible skin, and poor wound healing typical of dermatosparaxis was found to have normal collagen fibers. However, levels of dermatan sulfate proteoglycan in the dermal connective tissue were undetectable. The defect was identified as a mutation involving the gene that codes for the proteoglycan core protein. The mode of inheritance was not determined.
Cutaneous mucinosis (hyaluronosis) of Chinese Shar-Pei dogs.
Cutaneous mucinosis is a dermal connective tissue disorder in which excessive mucin accumulates in the skin. The mucin deposition is caused by excessive production by dermal fibroblasts of the polysaccharide hyaluronan (HA). The hyaluronan accumulation is related to a higher expression of hyaluronan synthase 2 (HAS2) mRNA and HAS2 protein by dermal fibroblasts. The inherited form of cutaneous mucinosis is considered normal in the Chinese Shar-Pei dog and is responsible for the thick, wrinkled skin characteristic of the breed. The degree of mucin accumulation is variable. In some dogs, large lakes of mucin form nodules or cysts that may rupture and drip clear, stringy fluid.
Histologically, cutaneous mucinosis is characterized by a variable increase in dermal thickness because of excessive mucin separating collagen fibers. Mucin has great water-binding capacity and thus contains a substantial amount of water, the majority of which is removed during processing of the tissue. What remains in H&E-stained tissue sections is fine basophilic granular to fibrillar material separating dermal collagen fibers. Special stains can be used to better visualize the mucin; these include Alcian blue at pH 2.5, which stains mucin blue-green, and mucicarmine, which stains it red. Mucin stains metachromatically with toluidine blue and methylene blue. PAS stain, which stains neutral mucopolysaccharides, does not stain dermal mucin.
Further reading
Barnett KC, Cottrell BD. Ehlers-Danlos syndrome in a dog: ocular, cutaneous and articular abnormalities. J Small Anim Pract 1987;28:941-946.
Bavinton JH, et al. A morphologic study of a mild form of ovine dermatosparaxis. J Invest Dermatol 1985;84:391-395.
Bellini MH, et al. Increased elastic microfibrils and thickening of fibroblastic nuclear lamina in canine cutaneous asthenia. Vet Dermatol 2009;20:139-143.
Benitah N, et al. Diaphragmatic and perineal hernias associated with cutaneous asthenia in a cat. J Am Vet Med Assoc 2004;224:706-709.
Byers PH. Ehlers-Danlos syndrome: recent advances and current understanding of the clinical and genetic heterogeneity. J Invest Dermatol 1994;103:47s-52s.
Colige A, et al. Human Ehlers-Danlos syndrome type VII C and bovine dermatosparaxis are caused by mutations in the procollagen I N-proteinase gene. Am J Hum Genet 1999;65:308-317.
Crosaz O, et al. Skin fragility syndrome in a cat with multicentric follicular lymphoma. J Feline Med Surg 2013;15:953-958.
Daniel AGT, et al. Skin fragility in a cat with cholangiohepatitis and hepatic lipidosis. J Feline Med Surg 2010;12:151-155.
Dillberger JE, Altman NH. Focal mucinosis in dogs: seven cases and review of cutaneous mucinoses of man and animals. Vet Pathol 1986;23:132-139.
Docampo MJ, et al. Increased HAS2-driven hyaluronic acid synthesis in shar-pei dogs with hereditary cutaneous hyaluronosis (mucinosis). Vet Dermatol 2011;22:535-545.
Docampo MJ, Zanna G. Biomechanical and molecular characteristics of hereditary equine regional dermal asthenia in Quarter Horses. Vet Dermatol 2009;20:591-599.
Fernandez CJ, et al. Staining abnormalities of dermal collagen in cats with cutaneous asthenia or acquired skin fragility as demonstrated with Masson's trichrome stain. Vet Dermatol 1998;9:49-54.
Gunson DE, et al. Dermal collagen degradation and phagocytosis. Occurrence in a horse with hyperextensible fragile skin. Arch Dermatol 1984;120:599-604.
Lopez A, et al. Cutaneous mucinosis and mastocytosis in a shar-pei. Can Vet J 1999;40:881-883.
Paciello O, et al. Ehlers-Danlos-like syndrome in 2 dogs: clinical, histologic, and ultrastructural findings. Vet Clin Pathol 2003;32:13-18.
Parish WE, Done JT. Seven apparently congenital noninfectious conditions of the skin of the pig, resembling congenital defects in man. J Comp Pathol 1962;72:286-298.
Rodriguez F, et al. Collagen dysplasia in a litter of Garafiano shepherd dogs. J Vet Med A 1996;43:509-512.
Sequeira JL, et al. Collagen dysplasia (cutaneous asthenia) in a cat. Vet Pathol 1999;36:603-606.
Tajima M, et al. Gene defect of dermatan sulfate proteoglycan of cattle affected with a variant form of Ehlers-Danlos syndrome. J Vet Intern Med 1999;13:202-205.
Tamulevicus AM, et al. Disseminated histoplasmosis accompanied by cutaneous fragility in a cat. J Am Anim Hosp Assoc 2011;47:e36-e41.
van Halderen A, Green JR. Dermatosparaxis in White Dorper sheep. J S Afr Vet Assoc 1988;59:45.
Dermatosis vegetans
Dermatosis vegetans is an inherited disorder of young pigs characterized by vegetating skin lesions, hoof malformation, and giant cell pneumonia. The condition is a simple autosomal recessive trait of Landrace swine in Europe, Canada, and Australia. Clinically affected pigs grow slowly, become emaciated and unkempt, and usually die by 2 months of life. The economic impact of the disease may be considerable because virtually all homozygotes die before reaching slaughter age.
Skin lesions may be present at birth, but more commonly, they develop during the first 3 weeks of life, and in rare cases may not arise until 2-3 months of age. Lesions begin as erythematous papules, 0.5-2.0 cm in diameter, usually on the ventral abdomen and medial aspect of the thighs. They may extend up the sides and back but do not affect the head. The papules enlarge peripherally over the course of 2 or 3 days, and the center becomes depressed. At this stage, the lesions are clinically similar to pityriasis rosea. The papules enlarge to form plaques with a depressed center filled with characteristic gray to brown-black granular brittle material. Over a period of weeks, the lesions continue to expand and develop a dry, horny, papilloma-like appearance. They become dark brown to black, and each crusty plaque is surrounded by a hyperemic raised border that sharply demarcates the lesions from the surrounding normal skin (Fig. 6.31 ). As lesions spread peripherally, they coalesce to form extensive areas covered by black crusts. Affected piglets frequently die when lesions reach the typical papilloma-like appearance at 5-8 weeks of age. Skin lesions then begin to resolve if the pig survives.
Figure 6-31.
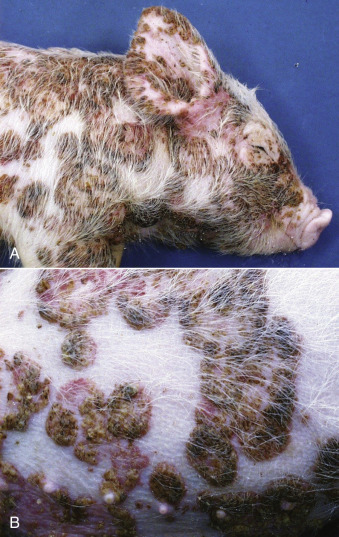
Dermatosis vegetans in a pig. A. Coalesced, red-black crusted plaques on the head, neck, and abdominal wall. B. Close-up view.
(Courtesy P. Habecker.)
When they occur, foot and hoof lesions are always present at birth. Usually more than one limb is affected, and typically all digits, including accessory digits, of an affected foot are involved. The coronary region is markedly swollen and erythematous; and the skin is covered by yellow-brown greasy material. The wall of the hoof is thickened by ridges and furrows parallel to the coronary band. Affected hooves become progressively enlarged, wider, and flatter than normal if pigs survive to 5 or 6 months. Coronary band changes, however, diminish as the pig ages.
At birth, affected piglets seem otherwise normal, but over a period of weeks they gradually decline in growth and vitality. Except for animals that die perinatally, virtually all affected pigs show signs of respiratory dysfunction, typically increased respiratory rate and labored respiration, several days prior to death. Affected pigs commonly develop anemia and secondary infections, especially bacterial pneumonia.
The histologic lesions in the skin vary according to the stage of the condition. Initially, there is superficial dermal edema, vascular congestion, and dermal infiltration with numerous granulocytes, many of which are eosinophils. Fully developed lesions are characterized by marked orthokeratotic and parakeratotic hyperkeratosis, prominent irregular epidermal hyperplasia, intercellular edema, and intraepidermal pustules and microabscesses containing eosinophils and neutrophils. The characteristic histologic lesion in the lung is giant cells in alveoli. The giant cells have been identified immunohistochemically as originating from monocytes/macrophages. In chronic cases, epithelialization and interstitial fibrosis are evident, and multinucleated giant cells may be infrequent when the condition has lasted several months. Typical pulmonary changes may be obscured by secondary infections.
Further reading
Evensen O. An immunohistochemical study on the cytogenetic origin of pulmonary multinucleate giant cells in porcine dermatosis vegetans. Vet Pathol 1993;30:162-170.
Percy DH, Hulland TJ. The histopathological changes in the skin of pigs with dermatosis vegetans. Can J Comp Med 1969;33:48-54.
Dermoid cyst
The dermoid cyst (dermoid sinus) is an uncommon developmental anomaly that has been reported in dogs, cats, horses, and cattle. It is caused by defective epidermal closure along embryonic fissures, which isolates an island of ectoderm in the dermis or subcutis. The majority of dermoid cysts occur on the dorsal midline because of incomplete separation of skin and neural tube during embryonic development; but they also occur in other locations. Although present at birth, dermoid cysts are usually asymptomatic and may not be noticed until they become distended or infected in an older animal. The cyst usually contains hair, keratin, and sebum, and this material may produce progressive enlargement of the structure so that it becomes clinically apparent. Cysts frequently become infected, producing clinical signs such as purulent discharge, local swelling from cellulitis, or neurologic signs secondary to meningomyelitis.
In dogs, dermoid cysts have been reported most commonly in the Rhodesian Ridgeback, a breed in which the lesion appears to be inherited as a simple recessive trait; development of a cyst is predisposed to by a dominant mutation in 3 fibroblast growth factor genes. Dermoid cysts have also been reported in several other breeds. It is unknown whether the lesion is an inherited condition in other breeds of dogs. Dermoid cysts have been associated with multiple vertebral and spinal malformations and hindlimb neurologic deficits in several dogs. The rare condition of nasal dermoid sinus cyst results in a discharging sinus over the external nares in dogs; the cyst may extend into the cranial vault and cause cerebral abscessation or recurrent meningitis. In one survey, all cases in horses were in Thoroughbreds. Several cases reported in cattle all involved Angus. Dermoid cysts are rare in cats, and both cases reported were in domestic shorthairs.
Dermoid cysts may be single or multiple. They consist of a well-circumscribed circular or tubular structure in the skin or subcutis and frequently connect to the skin surface by a small pore. A tuft of hair may protrude through this pore, and it may be surrounded by a whorl of hair. The cyst may end blindly in the subcutis; it may connect to the dorsal spinous process of vertebrae directly or by a fibrous cord; or rarely, it extends down to be continuous with the dura mater of the spinal cord. Microscopically, the dermoid cyst is a circular or tubular structure lined by a wall of well-differentiated, keratinizing squamous epithelium with associated small but well-developed hair follicles, sebaceous glands, and occasional epitrichial sweat glands. The hair shafts project into the cyst cavity that also contains keratin and variable amounts of sebum. Bacterial infection results in neutrophilic infiltration into the cyst. Pyogranulomatous dermatitis or cellulitis ensues when the cyst ruptures because of infection, trauma, or obstruction of the pore.
Further reading
Anderson DM, White RA. Nasal dermoid sinus cysts in the dog. Vet Surg 2002;31:303-308.
Baird AN, et al. Dermoid cyst in a bull. J Am Vet Med Assoc 1993;202:298.
Cornegliani L, Ghibaudo G. A dermoid sinus in a Siberian Husky. Vet Dermatol 1999;10:47-49.
Fatone G, et al. Dermoid sinus and spinal malformations in a Yorkshire terrier: diagnosis and follow-up. J Small Anim Pract 1995;36:178-180.
Fleming JM, et al. Cervical dermoid sinus in a cat: case presentation and review of the literature. J Feline Med Surg 2011;13:992-996.
Hillyer LL, et al. Epidermal (infundibular) and dermoid cysts in the dorsal midline of a three-year-old thoroughbred-cross gelding. Vet Dermatol 2003;14:205-209.
Perazzi A, et al. Multiple dermoid sinuses of type Vb and IIIb on the head of a Saint Bernard dog. Acta Vet Scand 2013;55:62.
Rochat MC, et al. Dermoid cysts in cats: two cases and a review of the literature. J Vet Diagn Invest 1996;8:505-507.
Salmon Hillbertz NH, et al. Duplication of FGF3, FGF4, FGF19 and ORAOV1 causes hair ridge and predisposition to dermoid sinus in Ridgeback dogs. Nat Genet 2007;39:1318-1320.
Tshamala M, Moens Y. True dermoid cyst in a Rhodesian ridgeback. J Small Anim Pract 2000;41:352-353.
Disorders of Epidermal Differentiation
The epidermis is stratified squamous epithelium that forms a continuously regenerating protective sheet around the body. Basal keratinocytes proliferate, then differentiate, become keratinized, and are then sloughed. In normal canine skin, the migration from the basal to the cornified layer requires 22 days, as measured by tritiated thymidine incorporation studies. This turnover rate is shortened in some skin diseases; for example, in seborrheic skin disease, it is 7-8 days. The basement membrane separates the epidermis from the dermis, and basal keratinocytes rest on this membrane anchored by hemidesmosomes and focal adhesions. Basal keratinocytes are the only cells in the epidermis that can undergo mitosis, and once mitosis occurs, the basal cell proceeds to undergo terminal differentiation. These postmitotic cells enter the stratum spinosum, develop intercellular attachments, desmosomes and adherens junctions, and change the keratin composition of the cytoplasmic keratin filaments. In the basal layer, keratins K5 and K14 are expressed, whereas in the suprabasal cells, K1 and K10 are expressed. The intercellular and cell substrate adhesions are complex. Hemidesmosomes and desmosomes are stable junctions that associate with cytoplasmic keratin filaments, whereas focal adhesions and adherens junctions connect to actin filaments and are transitory adhesions. Integrins are receptors that mediate cell-substrate adhesion, whereas cadherins mediate cell-cell adhesion. As the cells are pushed outward, they move into the stratum granulosum and start to make proteins that make up keratohyaline granules. As the cells move into the stratum corneum (SC), the cytoplasmic organelles are lost, and they become metabolically inactive. These flattened inactive keratinocytes are compacted into a keratin layer that eventually exfoliates. In this way, the epidermis is continuously regenerating and degenerating by proliferation, differentiation, and keratinization.
While the cells are moving outward, keratin polypeptides form and polymerize into keratin intermediate filaments that are epithelial specific and the major component of the cytoskeleton of epithelial cells. The keratin intermediate filaments aggregate into tonofilaments that connect with desmosomes, and therefore indirectly with adjacent cells. The molecular structure of keratin is very important, and genetic mutation(s) can affect keratin filament formation. There are at least 30 keratins in epithelium; K9-20 are acidic (type I), and K1-8 are basic (type II). Two different keratins (one acidic and one basic) pair to form heterodimers, for example K1 and K10 in suprabasal cells, and K5 and K14 in basal cells. Hyperproliferative epidermis in skin diseases expresses keratins K6 and K16, not seen in normal skin.
When the cells reach the stratum granulosum, they start to synthesize proteins, stored in keratohyaline granules, necessary to form the mechanically strong macrokeratins in the SC. One of these, profilaggrin, dephosphorylates to form filaggrin, the major molecule responsible for the glue-like aggregation of intermediate filaments. Loricrin is also stored in keratohyaline granules, and this polypeptide contributes to the cell envelope, an insoluble intracytoplasmic barrier. Other proteins involved in cell envelope formation include involucrin, cystatin A, cystine-rich envelope protein (CREP), trichohyaline, small proline-rich proteins (SPRRs), sciellin, and filaggrin. These serve as substrates for the 3 transglutaminases that polymerize and crosslink these proteins in the formation of the cell envelope. The granular layer also contains small lipid-rich granules—submembranous lamellar bodies (Odland bodies, membrane-coating granules)—that contain lipids necessary to form a permeability barrier between cells when they are secreted into the intercellular space. Keratinocytes forming the SC are dead and can be sloughed when desmosomes are broken down. Hydrolytic enzymes, such as cathepsin B–like, carboxypeptidase, and acid phosphatase, are thought to be responsible for this desmosomal degradation and subsequent keratinocyte desquamation.
In various epidermal diseases, this orderly epidermal turnover is altered. For instance, increased proliferation and/or decreased dyshesion of epithelial cells will lead to thickening of the epidermis. Nutritional factors such as amino acids, vitamins A or B, zinc, fatty acids, and copper influence proper differentiation and maintenance of the epidermis. Altered expression of different molecules and keratin mutations, and aberrations in the Notch signaling pathway, are the focus of much research.
Further reading
Borradori L, Sonnenberg A. Structure and function of hemidesmosomes: more than simple adhesion complexes. J Invest Dermatol 1999;112:411-418.
Boyer B, Thiery JP. Epithelial cell adhesion mechanisms. J Membrane Biol 1989;112:97-108.
Eckert RL, et al. The epidermal keratinocyte as a model for the study of gene regulation and cell differentiation. Physiol Rev 1997;77:397-424.
Fuchs E. Epidermal differentiation: the bare essentials. J Cell Biol 1990;111:2807-2814.
Hegde S, Raghavan S. A skin-depth analysis of integrins: role of the integrin network in health and disease. Cell Commun Adhes 2013;20:155-169.
HogenEsch H, et al. Changes in keratin and filaggrin expression in the skin of chronic proliferative dermatitis (cpdm) mutant mice. Pathobiol 1999;67:45-50.
Hohl D. Cornified cell envelope. Dermatologica 1990;180:201-211.
Johnson JL, et al. Desmosomes: regulators of cellular signaling and adhesion in epidermal health and disease. Cold Spring Harb Perspect Med 2014;4:a015297.
Kwochka KW. The structure and function of epidermal lipids. Vet Dermatol 1993;4:151-159.
Mehrel T, et al. Identification of a major keratinocyte cell envelope protein, loricrin. Cell 1990;61:1103-1112.
Nowell C, Radtke F. Cutaneous Notch signaling in health and disease. Cold Spring Harb Perspect Med 2013;3:a017772.
Smack DP, et al. Keratin and keratinization. J Am Acad Dermatol 1994;30:85-102.
Suter MM, et al. Differential expression of cell surface antigens on canine keratinocytes defined by monoclonal antibodies. J Histochem Cytochem 1990;38:541-549.
Suter MM, et al. Keratinocyte biology and pathology. Vet Dermatol 1997;8:67-100.
Thacher SM. Purification of keratinocyte transglutaminase and its expression during squamous differentiation. J Invest Dermatol 1989;92:578-584.
Seborrhea
The term “seborrhea” dates back in the veterinary dermatology literature for more than 5 decades. Seborrheic skin disease is reported most commonly in the dog, but also occurs in horses, cats, goats, sheep, cattle, rodents, and primates. Seborrhea literally means “flow of sebum,” and it has been loosely correlated with abnormal sebaceous gland function. Seborrhea is a clinical, not histologic, term used to describe excessive scaling. Scaling (i.e., seborrhea) is a common reaction of the skin to normalize a damaged skin barrier and can occur with almost any insult. Historically, seborrhea was subdivided into those cases with dry scale (seborrhea sicca) or oily/greasy scale (seborrhea oleosa). The term “seborrheic dermatitis” was used to describe scaling accompanied by inflammation. In older literature, the diagnosis of “seborrhea” was based on gross skin lesions, and in general, histopathology and skin surface cytologic assessments were not included in the dermatologic workup.
Seborrhea has been divided into primary and secondary causes. The term “primary seborrhea” has been reserved for cases in which all known causes of scaling have been ruled out (e.g., ectoparasitism, metabolic diseases and endocrinopathies, allergic disease, etc.). In the 1980s, this designation was potentially useful for treatment purposes, but it antedated the discovery of numerous hyperkeratotic conditions, with sebaceous adenitis and ichthyosis being prime examples. Furthermore, the newer scientific literature has shed light onto the role of Malassezia and staphylococcal infections as promoters of inflammation and epidermal proliferation.
Primary idiopathic seborrheic skin disease is reported in many breeds and has been suggested to have an inherited basis; however, the breed predilections and clinical lesions overlap those of allergic skin disease. Cocker Spaniels and Springer Spaniels with purported idiopathic seborrhea have greasy, inflamed skin with hyperkeratotic plaques, comedones, and follicular casts. Inflammatory ceruminous otitis externa is also a constant finding. In Cocker Spaniels, cell proliferation kinetics indicate that seborrheic individuals have increased epithelial cell proliferation of the epidermis, hair follicle infundibulum, and sebaceous gland. In addition, recombinant grafting studies have shown that the hyperproliferative epidermis from seborrheic Cocker Spaniels remains hyperproliferative. These studies, although showing proliferative response, do not rule out a primary cornification disorder. Other breeds with primary, greasy seborrhea include the Basset Hound, West Highland White Terrier, German Shepherd, Dachshund, and Chinese Shar-Pei. Breeds having a dry form of primary seborrhea include the Irish Setter, Doberman Pinscher, Dachshund, and West Highland White Terrier. Primary seborrhea in German Shepherds, West Highland White Terriers, and Labrador Retrievers is often very inflammatory, lichenified, and pruritic. Seborrheic skin disease is typically more pronounced on the face, pinnae, trunk, pressure points, intertriginous areas, mucocutaneous areas, and paws. In Labrador Retrievers, the distribution is often strikingly ventral (“water-line disease”), which in the current literature would be interpreted as atopic dermatitis. Thus many cases that would have been called “primary seborrhea” in the past would now be classified as pyoderma, Malassezia dermatitis, sebaceous adenitis, allergic dermatitis, and so on. Therefore “seborrhea” should be used only as a clinical descriptive, not an etiologic, term.
The histologic features of primary seborrhea are not specific because they overlap those of allergic skin disease, Malassezia dermatitis, zinc-responsive dermatosis, and superficial pyoderma. Primary seborrhea has been characterized by superficial perivascular dermatitis with epidermal hyperplasia that is mild to moderate and papillated in configuration. The stratum corneum is expanded by alternating vertical tiers of orthokeratotic and parakeratotic hyperkeratosis. The parakeratosis is typically found overlying the shoulders of follicular ostia (parakeratotic “caps”). The underlying dermal papillae are often edematous, leading to spongiosis and leukocytic exocytosis of the overlying epidermis (“papillary squirting”) (Fig. 6-32 ). Spongiform or Munro's microabscesses may be seen in conjunction with the parakeratosis. The perivascular inflammatory cells include variable combinations of lymphocytes, neutrophils, plasma cells, macrophages, and mast cells. The cases may have subordinate patterns of suppurative folliculitis, furunculosis, perifolliculitis, and intraepidermal pustular dermatitis.
Figure 6-32.
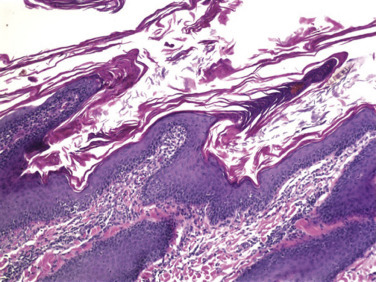
Primary idiopathic seborrhea in a dog. Papillated epidermal hyperplasia with vertical tiers of orthokeratotic and parakeratotic hyperkeratosis.
(Courtesy R. Dunstan.)
Primary seborrhea oleosa, presumably of autosomal recessive inheritance, has been described in Persian cats. Severely affected kittens show lesions at 3-4 days of age, and develop progressively severe, generalized greasiness, matting of the haircoat, rancid odor, comedones, alopecia, and ceruminous otitis externa. Pruritus is absent. A milder form of the disease is recognized in 6-8 week-old kittens, with mild to moderate greasiness of the skin and haircoat. Primary seborrhea in the horse occurs in both dry and greasy forms, and tends to be restricted to the mane and tail. Pruritus is absent. Generalized primary seborrhea is rare in the horse.
Further reading
Jefferies AR, et al. Seborrhoeic dermatitis in pigmy goats. Vet Dermatol 1991;2:109-117.
Kwochka KW, Rademakers AM. Cell proliferation kinetics of epidermis, hair follicles, and sebaceous glands of cocker spaniels with idiopathic seborrhea. Am J Vet Res 1989;50:1918-1922.
Mauldin EA. Canine ichthyosis and related disorders of cornification. Vet Clin North Am Small Anim Pract 2013;43:89-97.
Paradis M, Scott DW. Hereditary primary seborrhea oleosa in Persian cats. Feline Pract 1990;18:17-20.
Pin D. Seborrhoeic dermatitis in a goat due to Malassezia pachydermatis. Vet Dermatol 2004;15:53-56.
Power HT, et al. Use of Etretinate for treatment of primary keratinization disorders (idiopathic seborrhea) in cocker spaniels. West Highland white terriers, and basset hounds. J Am Vet Med Assoc 1992;201:419-429.
Scott DW, Miller WH. Primary seborrhea in English Springer spaniels: a retrospective study of 14 cases. J Small Anim Pract 1996;37:173-178.
Acne
Acne is seen in large short-coated breeds of dogs, especially Boxers, Mastiffs, German Shorthaired Pointers, English Bulldogs, Great Danes, and Doberman Pinschers. It usually occurs at 3-12 months of age with no sex predilection and occasionally persists into adult life. The etiology and pathogenesis are unknown, and aside from an association with puberty, there is little similarity to human acne. The lesions are thought to develop from external hair follicle trauma (rubbing of face) that results in follicular inflammation and traumatic rupture. The lesions consist of follicular papules and pustules on the chin and lips that may ulcerate and ooze suppurative exudate. Histologically, the lesions are characterized by suppurative folliculitis with follicular rupture and pyogranulomatous to suppurative inflammation surrounding free hair shafts. Early lesions may exhibit follicular keratosis, comedones, and variable inflammation.
Acne is common in cats and has no sex or breed predilections. It typically arises in mature cats with a median age of onset at 4 years, and persists for life. Acne is usually asymptomatic, although some cats may develop secondary bacterial folliculitis and furunculosis. The clinical lesions appear on the chin and lips and include comedones, papules, alopecia, crusts, and erythema. Histologically, the lesions consist of dilated sebaceous gland ducts, follicular keratosis with plugging and dilation, chronic periadnexal lymphoplasmacytic inflammation, and less commonly, luminal folliculitis and furunculosis.
Schnauzer comedo syndrome
This condition occurs only in the Miniature Schnauzer breed. Either sex may be affected, and the condition usually develops early in life. The disorder may represent a form of inherited follicular dysplasia or a follicular disorder of cornification. It has some resemblance to a developmental follicular dysplasia in humans termed nevus comedonicus. Clinically, the condition is characterized by multiple asymptomatic comedones over the dorsal midline. Occasionally, secondary bacterial folliculitis and furunculosis may develop. Histologically, there is marked orthokeratotic hyperkeratosis, dilation and plugging of hair follicles (comedones), and variable inflammation.
Tail gland hyperplasia
Many dogs have an oval area of skin on the dorsal surface of the tail above the fifth to seventh coccygeal vertebrae referred to as the tail (supracaudal, preen) gland. Microscopically, large, densely packed perianal (“hepatoid”) and sebaceous glands characterize this area. In some dogs, especially adult to aged males, this area enlarges. The enlargement is usually firm to slightly spongy, and associated with partial alopecia, scaling, and greasiness. At this stage, the lesion is asymptomatic. Occasionally, the lesions become cystic and/or secondarily infected, or neoplastic.
In most instances, canine tail gland hyperplasia is associated with hormonal imbalances, especially elevated levels of blood testosterone. Histologically, the lesions are characterized by marked hyperplasia of the perianal gland component, with a variable inflammatory response.
The entire dorsal surface of the tail in cats is replete with large, densely packed sebaceous glands, which are proposed to be embryonal hepatoid glands. In some cats, especially sexually active males of the Persian, Siamese, and Rex breeds, this area becomes clinically seborrheic, whereupon a brown to black, greasy keratosebaceous material accumulates on the hairs of the skin surface. Unless secondarily infected, the condition is asymptomatic. The cause of feline tail gland hyperplasia is unknown, and the colloquialism “stud tail” is misleading, as the condition is also seen in intact females and neutered males and females. Histologically, the condition is characterized by marked hyperplasia of sebaceous glands, with variable orthokeratotic hyperkeratosis and inflammation.
Further reading
Ruth J. Poor haircoat in a Persian. Feline tail gland hyperplasia (FTGH). Compend Contin Educ Vet 2009;31:208-210.
Scott DW, Reimers TJ. Tail gland and perianal gland hyperplasia associated with testicular neoplasia and hypertestosteronemia in a dog. Canine Pract 1986;13:15-17.
Shabadash SA, Zelinkina TI. Cat caudal gland is hepatoid. Izv Akad Nauk Ser Biol 1997;5:556-570.
Canine nasodigital hyperkeratosis
Canine nasodigital hyperkeratosis is an idiopathic disorder of cornification that is characterized by villous proliferation of keratin on the nasal planum and/or footpads. This disorder occurs in aged dogs and is not associated with inflammation, although the development of fissures may lead to secondary bacterial infections. The clinical presentation is typically diagnostic: thickening of the nose and footpads by fronds of keratin. The footpad lesions typically occur in areas that are not worn (e.g., margins of the footpad). Histologically, the corneal layer is thickened by vertical projections of anucleate (orthokeratotic) keratin.
Digital hyperkeratosis can occur as a congenital and presumed hereditary disorder in the Irish Terrier and Dogue de Bordeaux. The dogs develop severe footpad hyperkeratosis with large fronds of keratin by 5-6 months of age. Fissure formation leads to lameness and secondary bacterial infections. An autosomal mode of inheritance has been shown in the Irish Terrier.
Labrador Retriever nasal parakeratosis
This condition arises in Labradors Retrievers and their crosses at <1 year of age, and is thought to be autosomal recessive. The dogs develop thick, slightly verrucous, brown scale on the nasal planum with variable depigmentation. The disorder has characteristic histologic features: marked parakeratotic hyperkeratosis with serum lake formation with a band of lymphocytes and plasma cells in the superficial dermis. Other histopathologic findings include epidermal hyperplasia, neutrophilic and lymphocytic exocytosis, and pigmentary incontinence. Differentials include canine discoid lupus–like disease, pemphigus erythematosus/foliaceus, and idiopathic (senile) hyperkeratosis.
Keratoses
Keratoses are firm, elevated, circumscribed areas of excessive keratin production. In humans, keratoses are common and of numerous types. Keratoses are uncommonly reported in domestic animals. Actinic keratosis is discussed elsewhere.
Equine linear alopecia (linear keratosis) is a characteristic clinical entity. It occurs in many breeds; however, Quarter Horses seem to be predisposed. The age of onset is usually at 1-5 years. The clinical lesions are characterized by one or more vertically oriented linear areas of alopecia, with variable crusting and scaling. They are usually unilateral and occur most commonly on the neck, shoulder, and lateral thorax (Fig. 6-33A ). The lesions are usually asymptomatic, and may be persistent or permanent. The etiology of the condition is unknown but may involve an immune-mediated attack on the wall of the hair follicle. The reason for the linearity is unknown. Histologically, the lesion is characterized by lymphocytic or lymphohistiocytic mural folliculitis, sometimes with follicular destruction (Fig. 6-33B, C). Multinucleated giant cells and eosinophils are variably present. Sebaceous glands can be secondarily effaced, and there is a variable amount of orthokeratotic or parakeratotic hyperkeratosis, with or without superficial perivascular nonsuppurative inflammation. Linear keratoses with a similar gross and histologic appearance have also been described in cattle.
Figure 6-33.

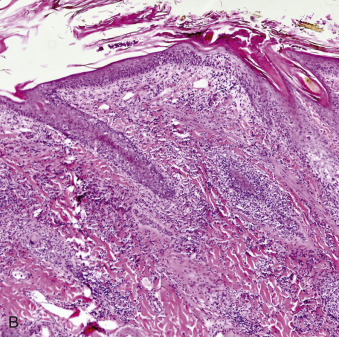
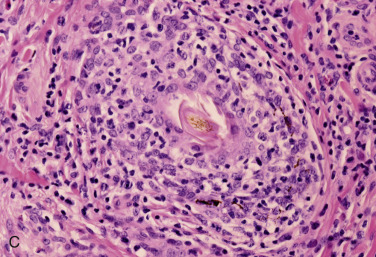
Equine linear alopecia. A. Linear alopecia, with crusting and scaling, on the neck of a horse. B. Low magnification showing a follicular orientation of the inflammatory infiltrate. C. Lymphohistiocytic to granulomatous mural folliculitis disrupts hair follicles.
(Courtesy C. von Tscharner.)
Equine cannon keratosis is a clinically recognizable disease of the horse. It represents a localized form of seborrheic dermatosis, can occur at any age, and has no breed predilection. The colloquial term, “stud crud,” is inappropriate as it also occurs in mares. The lesions consist of vertically oriented, moderately well-demarcated areas of alopecia, scaling, and crusting on the cranial surface of the rear cannon bones. The lesions are usually bilateral and persist for life. Pruritus and pain are absent. Histopathologic findings include orthokeratotic and/or parakeratotic hyperkeratosis, irregular to papillated epidermal hyperplasia, and mild superficial perivascular dermatitis featuring lymphocytes and macrophages.
Seborrheic keratoses have been recognized in dogs. The lesions are considered benign epidermal neoplasms and are very common in humans but rarely diagnosed in middle age to older dogs (mean age 9 years). They are of unknown cause, and have nothing to do with the clinical term seborrhea. The lesions may be single or multiple and have no apparent breed, sex, or site predilections. In both man and dog, the clinical lesion is an irregularly raised, variably pigmented plaque with dry to waxy scale, and a sessile or “stuck-on” appearance. Histologically, the lesions are characterized by papillated exophytic and mildly endophytic acanthosis with orthokeratotic hyperkeratosis (eFig. 6-10). This proliferation of monomorphic basaloid keratinocytes undergoes abrupt cornification and surrounds impacted, hyperkeratotic follicular ostia, which may develop into keratin horn-cysts. The lesions can be confused with viral plaques and are distinguished by the lack of hypergranulosis and papillomavirus cytopathic effect. In humans, the sudden appearance or enlargement of multiple lesions can be associated with an internal malignancy. This association has not been made in domestic animals.
eFigure 6-10.
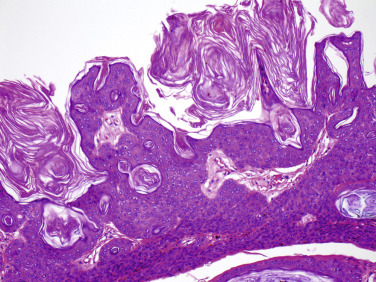
Seborrheic keratosis in a dog. Papillated proliferation of monomorphic basaloid keratinocytes undergoes abrupt cornification and surrounds impacted, hyperkeratotic follicular ostia.
Lichenoid keratoses have been reported as single or occasionally multiple wart-like papules or hyperkeratotic plaques that may be hyperpigmented on the inner surface of the pinna in dogs. Age, breed, and sex predilections have not been noted. Histologically, irregular to papillated epidermal hyperplasia, moderate to marked orthokeratotic and/or parakeratotic hyperkeratosis, and a lichenoid inflammatory infiltrate predominantly consisting of lymphocytes and plasma cells characterizes lichenoid keratosis.
Lichenoid reaction patterns in dogs, and rarely cats, may correspond to specific diseases (e.g., uveodermatologic syndrome, discoid lupus), but an idiopathic lichenoid reaction (lichenoid dermatosis) is occasionally seen in dogs and may represent a poorly characterized form of chronic cutaneous lupus erythematosus. Idiopathic lichenoid dermatosis is characterized by usually asymptomatic, symmetrical, grouped, flat-topped papules and plaques that are variably distributed, and that develop a scaly to markedly hyperkeratotic surface. The lesions have been described as self-limiting, although resolution may take several years. Histologically, these dermatoses are characterized by lichenoid interface dermatitis composed of plasma cells and lymphocytes, marked orthokeratotic hyperkeratosis and follicular keratosis, and moderate epidermal hyperplasia. Apoptotic keratinocytes can be seen primarily, although not exclusively, in the basal layer, and there is often hydropic degeneration of basal keratinocytes. If focal areas of suppurative epidermitis and/or suppurative luminal folliculitis are present, a lichenoid tissue reaction in response to staphylococcal infection should be suspected. A lichenoid psoriasiform dermatosis may occur in dogs on long-standing oral cyclosporine for refractory allergic skin or other conditions.
Cutaneous horns are recognized occasionally in all domestic species. Some are of unknown cause; others originate from papillomas, basal cell tumors, squamous cell carcinomas, or other keratoses. In cattle, sheep, and goats, cutaneous horns may arise in lesions of dermatophilosis. In the cat, multiple cutaneous horns on the footpads have been reported in association with feline leukemia virus (FeLV) infection; FeLV was isolated from the horns, and type C viral particles were seen in the lesions with the electron microscope.
Cutaneous horns may be single or multiple, and have no apparent age, breed, sex, or site predilections. The lesions are firm, well-circumscribed horn-like projections from the skin. They may be small (1-mm diameter × 5-mm length) or quite large (3-cm diameter × 12-cm length). Histologically, cutaneous horns are characterized by extensive, compact, laminated, orthokeratotic, and/or parakeratotic hyperkeratosis. The base of the horn must be inspected for the possible underlying cause.
Linear epidermal nevi are characterized histologically by linear hyperkeratosis with epidermal hyperplasia. They have been reported in several species. These include linear epidermal nevi in Belgian horses, inflammatory linear verrucous epidermal nevus in dogs, and a hereditary disorder of cornification in Rottweiler dogs (see Congenital and hereditary diseases of skin). The term nevus implies a lesion present at birth and composed of mature elements, and therefore, because these linear hyperkeratotic lesions have in common an early age of onset, they may represent linear epidermal nevi that have tardive onset. Equine cannon keratosis is grossly and histologically similar to linear epidermal nevi but differs from the linear epidermal nevi of Belgian horses, as it can occur at any age, and is restricted to the skin of the cannon area.
Further reading
Anderson WI, et al. Idiopathic benign lichenoid keratosis on the pinna of the ear in four dogs. Cornell Vet 1989;79:179-184.
Bradley CW, et al. Clinicopathological findings of canine seborrhoeic keratosis with comparison to pigmented viral plaques. Vet Dermatol 2013;24:432-438.
Clifford C. Neoplastic and non-neoplastic tumors. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013:20. p. 829-831.
Deprez P, et al. A case of bovine linear keratosis. Vet Dermatol 1995;6:45-49.
Gill PA, Purvis-Smith G. Idiopathic lichenoid dermatosis in a Doberman bitch. Aust Vet Pract 1995;25:144-146.
Gross TL, et al. Diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 154-155, 181-183.
Gross TL, et al. Epidermal tumors. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 2564-2565.
Gross TL, et al. Pustular and nodular diseases with adnexal destruction. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 435-440.
Hafner C, et al. Oncogenic PIK3CA mutations occur in epidermal nevi and seborrheic keratoses with a characteristic mutation pattern. Proc Nat Acad Sci 2007;104:13450-13454.
Hafner C, et al. Spectrum of FGFR3 mutations in multiple intraindividual seborrheic keratoses. J Invest Dermatol 2007;127:1883-1885.
Hafner C, Vogt T. Seborrheic keratosis. J Dtsch Dermatol Ges 2008;8:664-677.
Jazic E, et al. An evaluation of the clinical, cytological, infectious and histopathological features of feline acne. Vet Dermatol 2006;17:134-140.
Kawabata A, et al. Seborrheic keratosis in two dogs. Jpn J Vet Dermatol 2008;14:17-19.
Miller WH, et al. Congenital and Hereditary Defects. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 581-582.
Miller WH, et al. Keratinization Defects. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 639-642.
Miller WH, et al. Miscellaneous Skin Diseases. In: Muller & Kirk's Small Anim Dermatol. 7th ed. St Louis: Elsevier; 2013. p. 700-701.
Page N, et al. Hereditary nasal hyperkeratosis in Labrador Retrievers. Proc Am Acad Vet Dermatol Am Coll Vet Dermatol 1999;41-42.
Paradis M, et al. Linear epidermal nevi in a family of Belgian horses. Equine Pract 1993;15:10-14.
Peters J, et al. Hereditary nasal parakeratosis in Labrador retrievers: 11 new cases and a retrospective study on the presence of accumulations of serum (“serum lakes”) in the epidermis of parakeratotic dermatoses and inflamed nasal plana of dogs. Vet Dermatol 2003;14:197-203.
Rees CA, Goldschmidt MH. Cutaneous horn and squamous cell carcinoma in situ (Bowen's disease) in a cat. J Am Anim Hosp Assoc 1998;34:485-486.
von Tscharner C, et al. Disorders of cornification. Vet Dermatol 2000;11:187-189.
Werner AH. Psoriasiform-lichenoid-like dermatosis in three dogs treated with microemulsion cyclosporine A. J Am Vet Med Assoc 2003;223:1013-1016.
White SD, et al. Inflammatory linear verrucous epidermal nevus in four dogs. Vet Dermatol 1993;3:107-114.
Yager JA, Wilcock BP. Interface dermatitis. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat: Dermatopathology and Skin Tumors. London: Wolfe Publishing; 1994. p. 85-105.
Yager JA, Wilcock BP. Perivascular dermatitis. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat: Dermatopathology and Skin Tumors. London: Wolfe Publishing; 1994. p. 69-70.
Sebaceous adenitis
Sebaceous adenitis is an uncommon skin disease of dogs that has also been reported in the cat and rabbit. The condition has been reported in more than 50 breeds of dogs and in mongrels; however, there are breed predilections for the Standard Poodle, Akita, Samoyed, Vizsla, Lhasa Apso, and Havanese. In Standard Poodles and Akitas, an autosomal recessive trait is proposed. Onset of the disorder is usually in young adult to middle-aged animals. There appears to be a slight sex predilection for males in Standard Poodles, Havanese dogs, and Springer Spaniels.
The clinical lesions vary among the breeds of dogs. Longer-coated animals, as typical of the Standard Poodle, initially develop a thin coat because of loss of the undercoat, and then develop symmetrical multifocal to generalized areas of patchy alopecia and brittle to broken hairs encircled by yellow to brown follicular casts. Secondary bacterial infection is common. In short-coated dogs, early lesions consist of patches of scaling and alopecia that tend to appear on the ears and dorsum. These progress to annular areas of alopecia and scaling on the trunk and head. Early histopathologic changes are characterized by granulomatous or pyogranulomatous inflammation targeted on the sebaceous glands and eventually destroying the gland (Fig. 6-34A ). Long-coated dogs tend to have rapid and complete sebaceous gland destruction with little residual inflammation. In short-coated dogs, the lesions are more inflammatory, and sebaceous destruction progresses slowly. Inflammation can occasionally impinge secondarily on the follicular epithelium causing folliculitis. Orthokeratotic and/or parakeratotic hyperkeratosis together with follicular keratosis can be marked. In the chronic stages, both active inflammation and sebaceous glands may be absent, and there may be perifollicular fibrosis (Fig. 6-34B). After the disappearance of the glands, the hair follicles frequently assume a “stretched out” configuration and are keratin filled. Regeneration of sebaceous glands after variable amounts of time has been reported in occasional cases.
Figure 6-34.
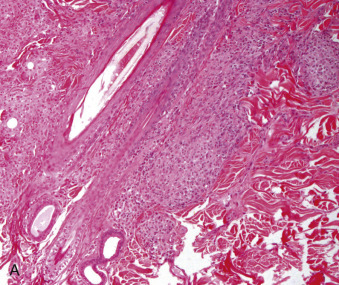
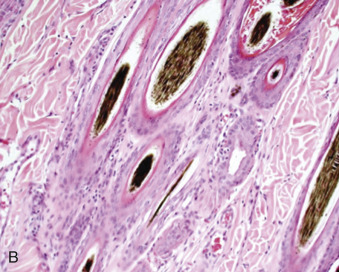
Sebaceous adenitis in a dog. A. Early lesion. Sebaceous glands targeted by pyogranulomatous inflammation. B. Late lesion. Complete sebaceous gland loss with minimal residual inflammation.
The pathogenesis of this disease has not been fully characterized. Several possibilities include (1) destruction of the gland resulting from immune-mediated mechanisms, leading to secondary hyperkeratosis; (2) a primary keratinization defect, resulting in increased amounts of follicular keratin blocking the sebaceous duct and causing inflammation of the gland; or (3) a defect in the structure of the sebaceous duct or gland, resulting in inflammation directed at free sebum. In the predisposed breeds, such as Standard Poodles and Akita, a genetic basis seems probable together with other factors that would explain the variation in onset and progression of the disease.
Further reading
Bardagí M, et al. Histopathological differences between canine idiopathic sebaceous adenitis and canine leishmaniosis with sebaceous adenitis. Vet Dermatol 2010;21:159-165.
Bond R, Brooks H. Transverse sectioning for histological assessment of sebaceous glands in healthy dogs and canine sebaceous adenitis. J Small Anim Pract 2013;54:299-303.
Dunstan RW, Hargis AM. The diagnosis of sebaceous adenitis in standard poodle dogs. In: Bonagura JD, Kirk RW, editors. Kirk's Current Veterinary Therapy XII. Philadelphia: Saunders; 1995. p. 619-622.
Frazer MM, et al. Sebaceous adenitis in Havanese dogs: a retrospective study of the clinical presentation and incidence. Vet Dermatol 2011;22:267-274.
Hernblad Tevell E, et al. Sebaceous adenitis in Swedish dogs, a retrospective study of 104 cases. Acta Vet Scand 2008;50:11.
Reichler IM, et al. Sebaceous adenitis in the Akita: clinical observations, histopathology and heredity. Vet Dermatol 2001;12:243-253.
Scarff DH. Sebaceous adenitis in standard poodles. Vet Rec 2000;146:476.
Spaterna A, et al. Sebaceous adenitis in the dog: three cases. Vet Res Commun 2003;27:441-443.
von Tscharner C, et al. Disorders of cornification. Vet Dermatol 2000;11:187-189.
Wendlberger U. Sebaceous adenitis in a cat. Kleintierpraxis 1999;44:293.
White SD, et al. Sebaceous adenitis in four domestic rabbits (Oryctalagus cuniculus). Vet Dermatol 2000;11:53-60.
Vitamin A–responsive dermatosis
This disorders occurs almost exclusively in adult Cocker Spaniels, but has been reported in a Labrador Retriever and Miniature Schnauzer. True vitamin A deficiency has not been documented. Clinical lesions consist of hyperkeratotic plaques with follicular plugging and follicular casts on the ventral and lateral chest and abdomen. The dogs may have a greasy haircoat with ceruminous otitis. The histologic features are marked follicular orthokeratotic hyperkeratosis, which is more severe than the epidermal surface hyperkeratosis.
Further reading
Gross TL, et al. Diseases with abnormal cornification. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 165-167.
Miller WH, et al. Keratinization defects. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 630-646.
Lichenoid-psoriasiform dermatosis
This is an uncommon dermatosis that affects young English Springer Spaniels of either sex. Asymptomatic, generally symmetrical, hyperkeratotic, erythematous papules usually begin on the pinnae and groin, coalesce to plaques, and progressively involve large areas of the body, especially the ventral abdomen and prepuce. Secondary bacterial infection is common.
Histopathologic findings include lichenoid band of predominantly of plasma cells, with areas of psoriasiform epidermal hyperplasia, occasional apoptotic basal keratinocytes, and intraepidermal microabscesses (containing eosinophils and neutrophils). Although the infiltrate may obscure the dermoepidermal junction, basal cell apoptosis is not a feature. The histologic findings are very similar to lichenoid keratosis and must be differentiated clinically by knowledge of distribution of lesions and knowledge of the breed.
Lichenoid psoriasiform dermatosis can also occur in any dog on long-standing cyclosporine therapy. The lesions respond to decreasing the dose or stopping the drug. An association with staphylococcal infection has been proposed for the condition.
Further reading
Favrot C, et al. Evaluation of papillomaviruses associated with cyclosporine-induced hyperplastic verrucous lesions in dogs. Am J Vet Res 2005;66:1764-1769.
Gross TL, et al. Psoriasiform lichenoid dermatitis in the Springer spaniel. Vet Pathol 1986;23:76-78.
Mason KV, et al. Characterization of lichenoid-psoriasiform dermatosis of Springer spaniels. J Am Vet Med Assoc 1986;189:897-901.
Werner AH. Psoriasiform-lichenoid-like dermatosis in three dogs treated with microemulsified cyclosporine A. J Am Vet Med Assoc 2003;223:1013-1016.
Ear margin dermatosis
This is an idiopathic seborrheic disorder that is localized to the margins of the pinnae. It occurs primarily in the Dachshund, although it can be seen in other breeds with pendulous ears. There is no sex predilection, and the disorder usually begins in young adults. Waxy keratosebaceous accumulations and alopecia follow initial scaling of the ear margins. The disease is symmetrical and asymptomatic. The dermatosis may be complicated by secondary bacterial infection and fissures, at which point ulceration, oozing, crusting, pain, and pruritus may be seen. Histopathologic findings are characterized by marked orthokeratotic and/or parakeratotic hyperkeratosis with follicular keratosis and variable mild superficial perivascular dermatitis.
Further reading
Gross TL, et al. Canine ear margin seborrhea. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 167-169.
Miller WH, et al. Keratinization defects. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 642.
Exfoliative dermatoses (exfoliative erythroderma)
This refers to a cutaneous reaction pattern that can be associated with many diseases. Clinically, it is characterized by scaling and erythema that can be localized or generalized. Most cases of exfoliative dermatosis have been reported in association with thymoma, epitheliotropic lymphoma, visceral malignant neoplasms, drug reactions, or are idiopathic. Histopathologic findings can reflect the underlying condition and can include parakeratosis, epidermal acanthosis, variable psoriasiform epidermal hyperplasia, variable lymphocytic exocytosis, and perivascular to lichenoid dermal inflammation.
Exfoliative dermatosis resembling human large plaque parapsoriasis has been reported in a dog and a cat. The human disease, to which these cases were compared, is frequently a precursor to epitheliotropic lymphoma.
Further reading
Rottenberg S, et al. Thymoma-associated exfoliative dermatitis in cats. Vet Pathol 2004;41:429-433.
Schick RO, et al. Cutaneous lymphosarcoma and leukemia in a cat. J Am Vet Med Assoc 1993;203:1155-1158.
Scott DW. Exfoliative dermatoses in a dog and a cat resembling large plaque parapsoriasis in humans. Compan Anim Pract 1988;2:22-29.
Turek MM. Cutaneous paraneoplastic syndromes in dogs and cats: a review of the literature. Vet Dermatol 2003;14:279-296.
Hyperplastic dermatosis of West Highland White Terriers
West Highland White Terriers develop a severe skin disorder that was previously referred to as “epidermal dysplasia of West Highland White Terriers.” This disorder is now considered an unusually severe manifestation of allergic skin disease and Malassezia and/or staphylococcal infection. Most authors do not believe epidermal disorganization or keratinocyte abnormalities characteristic of dysplasia are present. Clinical signs begin at <1 year to middle age, with severely affected dogs tending to have an earlier age of onset.
Erythema and scaling with pruritus develop on the trunk, especially axillary and inguinal regions, and progress to involve the whole body. In chronic cases, the skin becomes lichenified, alopecic, hyperpigmented, and greasy. This combination of gross lesions has led to this condition being referred to as the “armadillo Westie syndrome.” Histologic epidermal lesions are characterized by irregular epidermal hyperplasia with mild to marked predominantly parakeratotic hyperkeratosis. The base of the hyperplastic epithelium can have a scalloped appearance with crowding of basilar keratinocytes, and there is multifocal spongiosis with lymphocytic exocytosis. Superficial perivascular infiltrates include neutrophils, macrophages, lymphocytes, and plasma cells. Sebaceous glands are often markedly hyperplastic. There is commonly secondary pyoderma and/or infection with Malassezia. The absence of Malassezia organisms in histologic sections does not necessarily exclude their presence as the organisms may be lost in tissue processing. Cytologic evaluation for yeasts is a more reliable indicator of the presence and numbers of yeasts. The lesions of hyperplastic dermatosis of West Highland White Terriers are histologically the same as lesions of chronic allergic dermatitis.
Further reading
Gross TL, et al. Hyperplastic diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 136-160.
Miller WH, et al. Congenital and hereditary diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 573-617.
Nett CS, et al. Epidermal dysplasia and Malassezia infection in two West Highland White Terrier siblings: an inherited skin disorder or reaction to severe Malassezia infection. Vet Dermatol 2001;12:285-290.
Equine coronary band dystrophy
Equine coronary band dystrophy is a condition of unknown etiology and pathogenesis. The condition affects adult horses of any breed, but draft breeds are considered predisposed. Equine coronary band dystrophy is characterized by marked proliferation and hyperkeratosis of the epidermis of the coronary band, and in some cases, the chestnuts and ergots. Usually all 4 limbs are affected; however, the lesion may not encompass the entire coronary band. Clinically, the coronary band is thickened, crusty, and scaly. Cracks and fissures may develop and lead to lameness. The chestnuts and ergots are similarly affected and may be ulcerated. Histologically, the epidermis of affected areas is characterized by marked papillary hyperplasia and marked orthokeratotic to parakeratotic hyperkeratosis. There may be various degrees of neutrophilic and eosinophilic exocytosis with microabscesses, edema, and crust formation. Dermal inflammation is minimal unless secondary infection is present. The diagnosis is made by ruling out other differential diagnoses that include pemphigus foliaceus, the hepatocutaneous syndrome, bacterial or fungal infection, selenium toxicosis, and eosinophilic exfoliative dermatitis. The condition is chronic and treatment is palliative.
Further reading
Menzies-Gow NJ, et al. Coronary band dystrophy in two horses. Vet Rec 2002;150:665-668.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Von Tscharner C, et al. Stannard's illustrated equine dermatology notes—an introduction. Vet Dermatol 2000;11:187-189.
Ichthyosis
The ichthyoses are rare disorders of cornification that result in severe generalized scaling. These disorders are congenital and heritable (see Congenital and hereditary diseases of skin).
Disorders of Pigmentation
Melanin pigments are responsible for the coloration of the hair, skin, and eyes, and also play an important role in photoprotection. Melanin is synthesized by melanocytes, which are dendritic cells originating as melanoblasts in the neural crest. Melanoblasts develop in the neural crest; migrate to peripheral sites such as skin, hair follicles, and dermis; differentiate into melanocytes; and synthesize melanosomes and melanin. Genetic mutations affecting any of these steps can lead to hereditary hypopigmentation. Many such mutations have been characterized in the murine model, but this area has been little studied in domestic animals. Many types of exogenous influences, such as inflammation, ultraviolet (UV) radiation, endocrinopathies, autoimmune diseases, and nutritional status can affect melanocytes in the skin, resulting in acquired hypopigmentation or hyperpigmentation.
Melanin synthesis in melanocytes takes place in melanosomes, which are round or elliptical membrane-bound organelles thought to be derived from endoplasmic reticulum and containing enzymes from the Golgi and lysosomal system. Melanosomes are designated type I through IV, according to their stage of maturation. Type I melanosomes contain no melanin and are electron lucent, whereas type IV are mature melanosomes that are electron dense and migrate to the tips of the dendritic processes to be transferred to adjacent epithelial cells. Melanogenesis in round melanosomes produces eumelanins, the black pigments, and in elliptical melanosomes produces pheomelanins, red and yellow pigments. Pigment types in horses, sheep, goats, and llamas have been analyzed. These melanin pigments arise from the common metabolic pathway of conversion of tyrosine to 3, 4-dihydrophenylalanine (DOPA) and then oxidation to DOPAquinone. Tyrosinase, a copper-containing enzyme, is the critical and rate-limiting enzyme in this pathway, catalyzing tyrosine to DOPA. Many gene products are sequentially important to the melanoblast and melanocyte during their development and maturation. Apart from tyrosinase, the molecular role of these gene products has not been completely characterized, but it appears that platelet-derived growth factor (PDGF), and receptors for fibroblast growth factor-2 (FGF-2), endothelin-B, and the Steel factor (cKIT) are crucial.
Cutaneous pigmentary disorders can be divided into disorders of hyperpigmentation and hypopigmentation.
Further reading
Alhaidari Z, et al. Melanocytogenesis and melanogenesis: genetic regulation and comparative clinical diseases. Vet Dermatol 1999;10:3-16.
Baxter LL, Pavan WJ. The etiology and molecular genetics of human pigmentation disorders. Wiley Interdiscip Rev Dev Biol 2013;2:379-392.
Mort RL, et al. The melanocyte lineage in development and disease. Development 2015;142:620-632.
Sponenberg DP, et al. Pigment types of various color genotypes of horses. Pigm Cell Res 1988;1:410-413.
Sponenberg DP, et al. Pigment types in sheep, goats, and llamas. Pigm Cell Res 1988;1:414-418.
Disorders of hyperpigmentation
Acquired hyperpigmentation
Acquired hyperpigmentation of the skin (melanoderma) is encountered frequently. It is usually postinflammatory, a result of minor or chronic irritation, and may be accompanied by mild hyperkeratosis. Both melanosis and hyperkeratosis are common responses to mild injuries by agents as diverse as mites and irradiation. Hypermelanosis results from an increased rate of melanosome production, an increase in melanosome size, or an increase in the degree of melanization of the melanosome. It is usually associated with an accelerated melanocyte turnover with an increased number of melanosomes, as occurs following trauma and UV exposure. Inflammatory mediators likely play a role in stimulating melanocyte production. Activation of pre-existing immature melanocytes by sunlight, estrogen, and progesterone is thought to occur. Endothelin-1, which is produced and secreted by keratinocytes after UV irradiation, has been shown to accelerate melanogenesis. Basic fibroblast growth factor (bFGF) has been shown to be a mitogen for human melanocytes. Proliferating human epidermal cells in culture produce bFGF, perhaps illustrating the mechanism behind the hyperplastic and hyperpigmented lesions that typify many chronic dermatoses.
Acquired hyperpigmentation may also involve hair (melanotrichia). This is usually seen as a result of inflammatory skin disorders, especially those caused by biting insects in the horse and also has been described in white Merino sheep exposed to UV light.
Further reading
Forrest JW, Fleet MR. Pigmented spots in the wool-bearing skin of white Merino sheep induced by ultraviolet light. Aust J Biol Sci 1986;39:125-136.
Guaguère E, et al. Troubles de la pigmentation mélanique en dermatologie des carnivores. 3. Hypermélanoses. Point Vét 1987;18:699-709.
Halaban R, et al. Basic fibroblast growth factor from human keratinocytes is a natural mitogen for melanocytes. J Cell Biol 1988;107:1611-1619.
Mizoguchi M, et al. Clinical, pathological, and etiologic aspects of acquired dermal melanocytosis. Pigm Cell Res 1997;10:176-183.
Focal macular melanosis
Lentigo simplex has been reported in cats and dogs, and is most common in cats with orange, cream, or tricolored coats. The lesions are flat, or minimally raised, pigmented macules and usually occur on the mucocutaneous junctions of the mouth, eye, and nose, and the footpads. Lesions tend to start at <1 year of age and may increase in size and number with age. The lesions are of no significance, except that they can be confused clinically with melanoma or pigmented hamartoma. Histologically, lentigines are characterized by minimal to mild epidermal hyperplasia with formation of elongated rete ridges. There are increased numbers of melanocytes, particularly in the stratum basale, and usually increased melanin in basal keratinocytes. Low numbers of melanophages may be present in the underlying dermis. Papillated epidermal hyperplasia and hyperkeratosis are not present. Generalized lesions have been reported in a silver cat.
Merino sheep may acquire pigmented macules, particularly after shearing. Lesions are concentrated on the back, suggesting a role for sunlight exposure. Experimental exposure to UV light–induced lesions as early as 10 days postirradiation. Histologically, these lesions are characterized by increased numbers of epidermal melanocytes at the dermoepidermal junction and in the normally nonpigmented outer root sheath epithelium.
Further reading
Ber Rahman S, Bhawan J. Lentigo. Int J Dermatol 1996;35:229-238.
Gross TL, et al. Lentigo. In: Gross TL, et al., editors. Veterinary Dermatopathology. St Louis: Mosby Year Book; 1992. p. 456-458.
Nash S, Paulsen D. Generalized lentigines in a silver cat. J Am Vet Med Assoc 1990;196:1500-1501.
Scott DW. Lentigo simplex in orange cats. Compan Anim Pract 1987;1:23-25.
Canine acanthosis nigricans
Canine acanthosis nigricans is an idiopathic dermatitis, characterized by progressive hyperpigmentation, alopecia, and lichenification. The lesions are roughly bilaterally symmetrical and typically start in the axillae, spreading to involve proximal limbs, ventral abdomen, neck, and inguinal area. Seborrhea, Malassezia infection, and bacterial pyoderma are frequent complications. Histologic examination reveals hyperplastic dermatitis with orthokeratotic and parakeratotic hyperkeratosis, acanthosis, and rete ridge formation. All layers of the epidermis are heavily melanized. Spongiosis, neutrophilic exocytosis, and serous crusts may also be present. The dermal inflammatory reaction is mild, pleomorphic in cell type, and superficial perivascular in location.
The primary or idiopathic form of acanthosis nigricans occurs predominantly in Dachshunds. In view of the early age of onset (usually <1 year of age) and the strong predilection for Dachshunds, it is probable that canine idiopathic acanthosis nigricans is a heritable disorder. In humans, some forms of acanthosis nigricans are associated with internal malignancies, hyperinsulinemia, insulin resistance, drug administration, endocrine dysfunction, and concurrent autoimmune disease; a similar correlation has not been demonstrated in dogs. The histologic lesions of primary acanthosis nigricans are virtually identical to the common histologic changes associated with chronic pruritic dermatitides (sometimes referred to as pseudoacanthosis nigricans or secondary acanthosis nigricans) resulting from several causes, including chronic pyoderma, atopy, seborrheic dermatitis, and some endocrine disorders. The diagnosis of primary acanthosis nigricans requires clinical correlation, together with the histologic findings, to support the diagnosis in a young Dachshund with compatible distribution of lesions.
Further reading
Anderson RK. Canine acanthosis nigricans. Compend Contin Educ Pract Vet 1979;1:466-471.
Yager J, Wilcock B. Color Atlas and Text of Surgical Pathology of the Dog and Cat. St Louis: Mosby; 1994. p. 64.
Acromelanism
Acromelanism is seen in Siamese and Himalayan cats, rabbits, and mice. It is a condition in which coat color can be influenced by external temperature (high temperatures producing light hairs, low temperatures producing dark hairs) and factors affecting heat production and loss (alopecia, inflammation). The coat color changes are usually temporary, and the hair returns to the normal color with the next hair cycle. These phenomena are due to a missense nucleotide substitution in tyrosinase, making the enzyme thermally unstable.
Further reading
Giebel LB, et al. A tyrosinase gene missense mutation in temperature-sensitive type I oculocutaneous albinism. A human homologue to the Siamese cat and Himalayan mouse. J Clin Invest 1991;87:1119-1122.
Iljin NA, Iljin VN. Temperature effects on the color of the Siamese cat. J Hered 1930;21:309-318.
Disorders of hypopigmentation
Leukoderma and leukotrichia
Reduction in pigmentation of the skin is leukoderma, and of the hair is leukotrichia. Leukoderma and leukotrichia may occur independently. They can result from a decrease in melanin (hypomelanosis), a complete absence of melanin (amelanosis), or from a loss of existing melanin (depigmentation). These events result from either an absence of the pigment-synthesizing melanocytes or from a failure of melanocytes to produce normal amounts of melanin or to transfer it to adjacent keratinocytes.
Hereditary hypopigmentation
Hereditary hypopigmentation can be divided into melanocytopenic hypomelanosis, characterized by the absence of melanocytes in affected areas, and melanopenic hypomelanosis, in which melanocytes are present but defective. The condition can be localized, focally extensive, or generalized. Melanocytopenic hypomelanosis can be extensive, as is seen in animals with Waardenburg syndromes and in piebaldism. In these cases, there is failure of melanoblasts to migrate from the neural crest into the skin, or failure to survive in the skin. Melanocytopenic hypomelanosis can also be localized, as in vitiligo, in which there is genetically programmed destruction of melanocytes. Melanopenic hypomelanosis is seen in the various forms of albinism.
Melanocytopenic hypomelanosis.
Syndromes analogous to the human Waardenburg syndrome have been reported in cats, dogs, horses, and rabbits. Affected animals typically have white coats and blue or heterochromatic irides, and are deaf. In cats, this has been shown to be due to an autosomal dominant mutation with complete penetrance for loss of pigmentation and incomplete penetrance for deafness. In dogs, this syndrome has been described in breeds such as the Dalmatian, Bull Terrier, Sealyham Terrier, Collie, and Great Dane. A syndrome analogous to human Waardenburg type 4 (Hirschsprung disease) has been reported in mice with lethal spotting mutation, and in American Paint horses in which white foals from overo mares are born with aganglionic colons. These foals develop colic and die shortly after birth.
Piebaldism is also a form of genetic melanocytopenic hypomelanosis, resulting in multifocal white patches in which there is absence of melanocytes due to a congenital failure of melanoblasts to migrate from the neural crest to the skin, or by their inability to survive and proliferate in the skin. Piebaldism has been seen in many species, including horses, dogs such as the Dalmatian, cats, cattle, and rodents. The defect has been shown to be a mutation in the gene encoding c-kit tyrosine kinase receptor, or a mutation in the gene for stem cell factor, which is the receptor ligand. The c-kit tyrosine kinase receptor is associated with proliferation and survival of melanoblasts.
Literally meaning “blemish,” vitiligo is a melanocytopenic hypomelanosis of humans and animals, which is characterized by gradually expanding pale macules that are often symmetrical or segmental in distribution (Fig. 6-35 ). Vitiligo has been described in the dog, cat, horse, cattle, and the Smyth chicken (DAM chicken), which has been used as an animal model of the human disease. The immediate cause of vitiligo is the destruction of melanocytes. It is considered to be a genetic amelanosis inherited as an autosomal recessive trait in animals. It is thought to be a polygenic disease necessitating simultaneous mutations in several genes, resulting in melanocyte destruction or increased risk of immune-mediated destruction of melanocytes. Theories regarding the pathogenesis of this disease include autoimmune destruction of melanocytes, a neurogenic theory involving release of a neurochemical from peripheral nerves that inhibits melanogenesis, a self-destruction theory that involves failure of protection of melanocytes against the toxic effects of melanin precursors, or a combination of factors. Circulating antimelanocytic antibodies have been detected in some studies, lending support to an immune-mediated pathogenesis.
Figure 6-35.

Vitiligo in a dog. A. Periocular leukotrichia. A, B. Coalescing pale macules on the skin of the lips and nasal planum.
Vitiligo in the dog has been described in Belgian Tervuren, Doberman Pinscher, Newfoundland, Rottweiler, German Shepherd, Dachshund, German Shorthaired Pointer, and Old English Sheepdogs. Vitiligo in a Dachshund developed concurrently with juvenile-onset diabetes mellitus. The condition is best characterized in Belgian Tervurens (eFig. 6-11). The depigmentation in this breed occurs chiefly on the pigmented skin and mucous membranes of the face and mouth in young adult dogs. Histologic examination of affected skin shows an epithelium devoid of both pigment granules and DOPA-positive cells. Electron microscopy confirms the lack of melanocytes in the lesions; their place is taken by Langerhans or indeterminate dendritic cells. Antimelanocytic antibodies have been demonstrated in affected dogs but not in normal animals. Depigmentation restricted to the nasal planum (also called “Dudley nose,” “snow nose”) has been also termed “vitiligo.” This is commonly seen in the Golden Retriever, Nordic breeds (Siberian Husky, Malamute), and yellow Labrador Retrievers. The etiology is not known.
eFigure 6-11.

Vitiligo in a Belgian Malinois dog. Depigmentation of the lips and periocular skin.
(Courtesy K. Shanley.)
Vitiligo has also been described in horses, and is more common in gray horses. In one form, the Arabian fading syndrome, affected animals develop round, depigmented macules on the lips, muzzle, around the eyes, and occasionally the anus, vulva, prepuce, and hooves. The disease can start at any age, but is more common in horses <2 years of age. Circulating antimelanocytic antibodies have been detected in some cases.
In cattle, vitiligo-like lesions have been described in Holstein-Friesians, in black Japanese cattle, and in water buffalo.
Siamese cats may develop vitiligo. Antibodies to an 85-kDa surface antigen of melanocytes were demonstrated in 4 cats with vitiligo. No antibodies were detected in 3 normal Siamese cats tested.
Further reading
Alhaidari Z, et al. Melanocytogenesis and melanogenesis: genetic regulation and comparative clinical diseases. Vet Dermatol 1999;10:3-16.
Boissy RE, Norlund JJ. Molecular basis of congenital hypopigmentary disorders in humans: a review. Pigm Cell Res 1997;10:12-24.
Cerundolo R, et al. Vitiligo in two water buffaloes: histological, histochemical, and ultrastructural investigations. Pigm Cell Res 1993;6:23-28.
Eizirik E, et al. Defining and mapping mammalian coat pattern genes: multiple genomic regions implicated in domestic cat stripes and spots. Genetics 2010;184:267-275.
Gross TL, et al. Perivascular diseases of the dermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 200-237.
Hauswirth R, et al. Novel variants in the KIT and PAX3 genes in horses with white-spotted coat colour phenotypes. Anim Genet 2013;44:763-765.
Kemp EH, et al. Immunological pathomechanisms in vitiligo. Expert Rev Mol Med 2001;2001:1-22.
Lopez R, et al. A clinical, pathological and immunopathological study of vitiligo in a Siamese cat. Vet Dermatol 1994;5:27-32.
Mahaffey MB, et al. Focal loss of pigment in the Belgian tervuren dog. J Am Vet Med Assoc 1978;173:390-396.
Miller WH, et al. Pigmentary abnormalities. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 618-629.
Naughton GK, et al. Antibodies to surface antigens of pigmented cells in animals with vitiligo. Proc Soc Exper Biol Med 1986;181:423-426.
Schmutz SM, Berryere TG. Genes affecting coat colour and pattern in domestic dogs: a review. Anim Genet 2007;38:539-549.
Scott DW, Miller WH. Pigmentary abnormalities. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 389-397.
Spritz RA. Piebaldism, Waardenburg syndrome, and related disorders of melanocyte development. Sem Cutaneous Med Surg 1997;16:15-23.
Sulaimon SS, Kitchell BE. The biology of melanocytes. Vet Dermatol 2003;14:57-65.
Thomas JL, et al. The loss of vacuolar protein sorting 11 (vps11) causes retinal pathogenesis in a vertebrate model of syndromic albinism. Invest Ophthalmol Vis Sci 2011;52:3119-3128.
Melanopenic hypomelanosis.
The various forms of albinism are examples of melanopenic hypomelanosis. In albino animals and people, melanocytes are present and normally distributed but are defective in function and fail to synthesize melanin. The extent of the biochemical defect varies so that albinism covers a spectrum from amelanosis, oculocutaneous albinism (OCA), through graded pigmentary dilution. Oculocutaneous albinisms and pigment dilutions are inherited as autosomal recessive traits. In albino animals with white hair and skin, and translucent irides, there is a mutation in the tyrosinase gene resulting in no residual enzyme activity. A mutation resulting in residual enzyme activity produces animals born with white hair but producing blond or pigmented hair as juveniles. The skin remains white but can develop pigmented nevi. This form has been reported in a gorilla.
Chediak-Higashi syndrome in humans; Hereford, Brangus, and Japanese Black cattle; Persian cats; mink; blue and silver fox; and various other animal species is an example of partial albinism and is inherited as an autosomal recessive trait. Although melanin is produced, there is a mutation of the beige gene, which plays a major role in generating cellular organelles. This results in a membrane defect leading to the formation of giant melanosomes that are passed with difficulty to the keratinocytes. The clumping of these giant melanosomes produces the color-dilution effect. Chediak-Higashi syndrome is discussed in Vol. 3, Hematopoietic system.
Cyclic hematopoiesis (also called Grey Collie syndrome, cyclic neutropenia), a lethal hereditary disease of Collie dogs, is caused by an autosomal recessive gene with a pleiotropic effect on coat color dilution. The mutation in the AP3 gene is responsible for defects in protein sorting processes as well as a silver-gray coat color. The abnormal hair pigmentation results from the diminished formation of melanin from its precursor tyrosine rather than from pigment clumping. The normal Collie coat color is restored in animals receiving bone marrow transplants to correct cyclic hematopoiesis. The hematologic aspects of this disease are considered in Vol. 3, Hematopoietic system.
Coat color dilution and black hair follicular dysplasia has been reported in many species. It occurs in many breeds of dog; in cats, particularly Siamese cats; horses; and cattle. The pale coat coloration is due to clumping of large melanin granules in hair follicles and sometimes in the epidermis. In cats, dilute coat color is thought to be due to an autosomal recessive trait (Maltese dilution). Color-dilution alopecia, a tardive onset hypotrichosis associated with color-dilution traits in the dog, is discussed under Congenital and hereditary diseases of the skin.
Further reading
Adalsteinsson S. Albinism in Icelandic sheep. J Hered 1977;68:347-349.
Benson KF, et al. Mutations associated with neutropenia in dogs and humans disrupt intracellular transport of neutrophil elastase. Nat Genet 2003;35:90-96.
Ogawa H, et al. Clinical, morphologic, and biochemical characteristics of Chediak-Higashi syndrome in fifty-six Japanese Black cattle. Am J Vet Res 1997;58:1221-1226.
Prieur DJ, Collier LL. Maltese dilution of domestic cats. A generalized cutaneous albinism lacking ocular involvement. J Hered 1984;75:41-44.
Schmutz SM, Berryere TG. Genes affecting coat colour and pattern in domestic dogs: a review. Anim Genet 2007;38:539-549.
Schmutz SM, et al. A form of albinism in cattle is caused by a tyrosinase frameshift mutation. Mamm Genome 2004;15:62-67.
Yang TJ. Recovery of hair coat color in gray collie (cyclic neutropenia)—normal bone marrow transplant chimeras. Am J Pathol 1978;91:149-152.
Acquired hypopigmentation
This follows damage to the epidermal melanin unit by various insults, including trauma, inflammation, radiation, contactants, endocrinopathies, infections, and nutritional deficiencies. In general, the severity of the injury determines whether an insult will result in hypopigmentation or hyperpigmentation. Mild injury results in pigmentary incontinence and epidermal hypopigmentation; however, a mild injury allows accelerated keratinocyte turnover and a subsequent increase in production of melanosomes. Severe injury results in the death of melanocytes and no subsequent repigmentation.
Examples of depigmenting diseases in horses include onchocerciasis, Culicoides hypersensitivity, ventral midline dermatitis, and coital vesicular exanthema. Depigmenting lesions in horses may result from contact with equipment, such as rubber bit guards or crupper straps or with feed buckets. Monobenzone (monobenzyl ether of hydroquinone, 4-[benzyloxy]phenol), a common ingredient in rubber, inhibits melanogenesis.
In dogs, hypopigmentation can occur in immune-mediated diseases, such as lupus erythematosus, drug eruptions, bullous pemphigoid, and the various forms of pemphigus. Acquired depigmentation of the lips and/or nose also occurs in dogs as a result of contact with rubber dishes or toys containing monobenzone. Microbial lesions, such as deep pyoderma, may heal with depigmentation. Depigmenting lesions have been noted also in canine leishmaniasis and in dermatophytosis caused by Microsporum persicolor. Epitheliotropic lymphoma often is seen with depigmenting, ulcerative lesions of skin and mucocutaneous junctions. Transient depigmentation has been reported in drug eruptions. Subcutaneous injection of corticosteroid or progesterone hormones may lead to focal hypopigmentation in the dog.
Canine uveodermatologic syndrome (Vogt-Koyanagi-Harada-like syndrome) is a depigmenting condition that partially resembles an extremely rare condition in humans. Arctic breeds such as the Akita, Siberian Husky, Samoyed, and Malamute are predisposed to the condition; however, it has been reported in many breeds. The cause is unknown, although an immune-mediated attack on melanocytes, as in the human disease, is presumed. A recent study demonstrated a loss of dog leukocyte antigen (DLA) genetic diversity and suggested a role for certain DLA class II gene alleles in the pathogenesis of canine uveodermatologic syndrome. The canine lesions comprise bilateral panuveitis (see Vol. 1, Special senses) and bilateral cutaneous depigmentation, chiefly of the lips, nose, and periorbital skin (Fig. 6-36 ). Ocular lesions most often precede onset of cutaneous lesions. The scrotum, vulva, perianal skin, and footpads are less often affected. Leukotrichia is a common finding around the areas of leukoderma. Occasionally, depigmented lesions become ulcerated, erythematous or crusted. Histologically, the lesions are characterized by a lichenoid interface reaction pattern that is composed of histiocytes, often in aggregates, with fewer neutrophils, lymphocytes, and plasma cells (Fig. 6-37 ). There is pigmentary incontinence, and histiocytes often contain fine melanin granules. The basal cell layer does not have a pronounced vacuolar change and apoptotic basal keratinocytes are uncommon. This and the histiocytic nature of the inflammatory infiltrate are major features of differentiation from discoid and systemic lupus.
Figure 6-36.

Uveodermatologic syndrome in a dog. Marked depigmentation of the nose with focal ulcer, regional corneal edema, and anterior uveitis.
Figure 6-37.
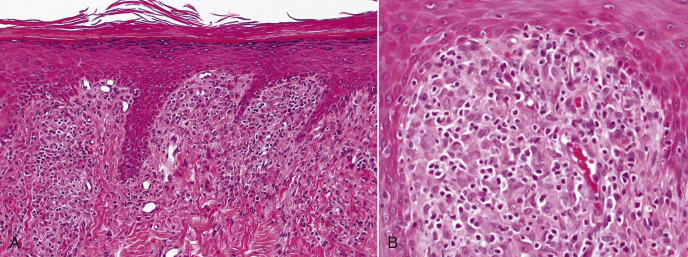
Uveodermatologic syndrome in a dog. A. Low magnification shows a slightly nodular mononuclear cell infiltrate that abuts the dermoepidermal junction. B. The infiltrate is composed predominantly of macrophages and fewer lymphocytes.
Further reading
Angles JM, et al. Uveodermatologic (VKH-like) syndrome in American Akita dogs is associated with an increased frequency of DQA1*00201. Tissue Antigens 2005;66:656-665.
Blackwood SE, et al. Uveodermatologic syndrome in a rat terrier. J Am Anim Hosp Assoc 2011;47:56-63.
Carter WJ, et al. An immunohistochemical study of uveodermatologic syndrome in two Japanese Akita dogs. Vet Ophthalmol 2005;8:17-24.
Laus JL, et al. Uveodermatologic syndrome in a Brazilian Fila dog. Vet Ophthalmol 2004;7:193-196.
Morgan RV. Vogt-Koyanagi-Harada syndrome in humans and dogs. Compend Contin Educ Pract Vet 1989;11:1211-1218.
Sigle KJ, et al. Unilateral uveitis in a dog with uveodermatologic syndrome. J Am Vet Med Assoc 2006;228:543-548.
Warmoes T. Canine model of Vogt-Koyanagi-Harada syndrome. Le Point Veterinaire 1999;30:249-254.
Leukotrichia
Reticulated leukotrichia, colloquially known as “tiger stripe,” is recognized in the Standardbred, Thoroughbred, and Quarter Horse breeds. The lesions occur predominantly in yearlings and comprise linear crusts arranged in a cross-hatch pattern on the dorsal midline from the withers to the tail. Transient alopecia and regrowth of permanently white hair follow crusting. The underlying skin has normal pigmentation. Well-documented precise descriptions of the expected histologic lesions are lacking. Some reports indicate an interface lichenoid dermatitis may be present, whereas others suggest that a mild superficial dermal mononuclear cell infiltrate and pigmentary incontinence are to be expected. The etiology and pathogenesis are unknown. Spotted leukotrichia occurs in the horse as multiple, often somewhat symmetrical, small circular areas of white hair. The spots occur most commonly on the rump and thorax, and Arabians have a predilection. The etiology and pathogenesis are unknown. Hyperesthetic leukotrichia, so-called because the lesions are extremely painful, has been reported only in Californian horses. Single or multiple crusted lesions occur on the dorsal midline and heal leaving permanently white hairs.
Leukotrichia, also termed poliosis, has been reported in dogs in association with Vogt-Koyanagi-Harada–like syndrome, tyrosinase deficiency in Chow Chows, and as an idiopathic, possibly heritable condition in a litter of Labrador Retrievers. In the last example, the condition resolved.
Leukotrichia can be associated with alopecia areata. Alopecia areata and alopecia universalis are discussed in more detail under Other immune-mediated dermatoses.
Further reading
Fadok VA. Update on four unusual equine dermatoses. Vet Clin North Am Equine Pract 1995;11:105-110.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier; 2011. p. 436-467.
Von Tsharner C. Pigmentary disorders. Vet Dermatol 2000;11:205-210.
White SD, Batch S. Leukotrichia in a litter of Labrador retrievers. J Am Anim Hosp Assoc 1990;26:319-321.
Copper deficiency
This pigmentary disorder is seen primarily in cattle and sheep. It has also been reported in moose, and experimentally in dogs. Copper deficiency may be simple or conditioned by other dietary substances, particularly sulfate and molybdenum. Because copper is an essential constituent of tyrosinase, there is depressed tyrosinase activity, and deficient animals show depigmentation of hair or wool. Affected cattle with normally black coats become rusty brown and develop “spectacle” lesions round the eyes. Black sheep develop intermittent bands of light-colored wool corresponding to periods of restricted availability of copper (Fig. 6-38 ). The deficiency of copper also affects the physical nature of the wool or hair. In sheep, the wool has less crimp, prompting the colloquial name of “string” or “steely” wool. The straightness of the wool is due to inadequate keratinization, probably caused by imperfect oxidation of sulfhydryl groups in prekeratin, a process that involves copper (Fig. 6-39 ).
Figure 6-38.
Copper deficiency. Black-wooled sheep with bands of achromotrichia corresponding to periods of molybdenum administration.
(Courtesy W.J. Hartley.)
Figure 6-39.

Staple from sheep that received 1.0 mg of copper per day, then 10 mg per day. Note stringiness and lack of crimp on deficient regime.
(Courtesy W.J. Hartley.)
Physicochemical Diseases of Skin
The integument has a large surface area in direct contact with the environment and is hence extremely vulnerable to chemical and physical injuries. Physical stresses include friction, pressure, vibration, electricity, high and low ambient temperatures, humidity, visible light, and ultraviolet, infrared, and ionizing radiation. Cutaneous reactions to visible light are discussed separately. Chemical toxins may exert their effect directly as in irritant contact dermatitis or envenomation or indirectly, as in thallium poisoning.
Physical injury to skin
Mechanical, frictional, and traumatic injury
The haircoat of most domestic animals protects from “blisters” that so commonly develop in human skin subjected to prolonged pressure or frictional contact with a hard surface. The following examples tend to occur in heavy animals with skin exposed to repeated or constant pressure, such as in animals immobilized by paralysis, or in those exposed to a physically harsh environment.
Dogs.
Calluses occur when continual or repetitive pressure or friction is applied to a localized area of skin and represent a protective response of the integument to the physical injury. They tend to occur over bony prominences, particularly the hocks, elbows, lateral surfaces of the digits, and on the sternum. Callosities can develop in all domestic animal species, but are most common in dogs, particularly the giant breeds, and in pigs housed on concrete floors with inadequate bedding. They are characterized by epidermal proliferation with prominent epidermal and follicular hyperkeratosis. Dilated hair follicles may lead to furunculosis with severe suppurative to pyogranulomatous dermatitis and eventual fibrosis. Grossly, callosities are well-circumscribed, lichenified, raised, alopecic, gray, keratinous plaques. Ulceration may occur. The pig may also develop bursitis.
A hygroma is a false or acquired bursa that develops subcutaneously over bony prominences. Hygromas are most common in the giant breeds of dogs at pressure points such as the lateral aspect of the elbow, the greater trochanter of the femur, and the tuber coxae. Hip dysplasia in dogs can lead to elbow hygromas, as dogs develop an abnormal method of lying down that relies upon dropping to the olecranons to spare the hips. Usually pressure induces a protective callus, but in some animals, persistent decubitus ulcers or recurrent hematoma formation eventually lead to the induction of a hygroma. The gross lesion is a variably sized cystic cavity separated from the skin by loose connective tissue. The wall of the hygroma is dense connective tissue that may have a smooth or a villus inner lining. The contents are mucinous and yellow to red, depending on the degree of hemorrhage. Histologically, the wall is composed of granulation tissue of variable maturity. A flattened layer of fibroblasts may give the appearance of an epithelial lining. The cavity may contain clumps of fibrin. Organization of fibrin deposits at the margin of the cavity gives rise to the grossly apparent villus projections that occasionally undergo cartilaginous metaplasia.
Decubitus ulcers are the result of ischemic necrosis that follows application of constant pressure to a localized area of skin. Studies in Greyhounds suggest that intermittent repeated focal vascular occlusion leads to increased tissue damage from reperfusion injury. Thromboxane A2 and its metabolite, thromboxane B2, are thought to contribute to vasoconstriction and platelet aggregation. Predisposing conditions include prolonged recumbency, lack of proper bedding, improperly applied bandages or casts, poorly fitting tack, atrophy of muscle, loss of fat, malnutrition associated with systemic disease, contusions, irritation from feces or urine, and body types with large bones, thin skin, and low body fat. In large animals, postanesthetic myopathies, laminitis, and neurologic diseases are predisposing conditions. The “downer” cow is particularly prone to decubitus ulcers. Decubitus ulcers are graded from I to IV. In grade I, the lesion consists of focal erythema. In grade II, an ulcer extends into the subcutis. In grade III, the ulcer extends into the deep fascia, and the wound edges may be undermined. Grade IV ulcers extend to bone, have undermined edges, and possibly underlying osteomyelitis and septic arthritis.
Intertrigo refers to localized dermatitis affecting folded areas of skin. The combined effect of friction, heat, maceration, bacterial or yeast proliferation, and irritation by retained secretions leads to superficial inflammation. Examples in dogs include facial, lip, vulvar, and tail fold dermatitis of English Bulldogs and Pugs. Obesity is a predisposing factor. Body fold dermatitis is particularly common in Chinese Shar-Pei puppies. Udder-thigh dermatitis occurs predominantly in first-calf dairy heifers. Udder edema is a predisposing factor. Lesions are erythematous and swollen, sometimes ulcerated, and often have an unpleasant odor. Histologically, the epidermis is hyperplastic, spongiotic, and possibly eroded or ulcerated. Surface pustules, neutrophilic exocytosis, and pigmentary incontinence may be present. The dermis has a dense band of lymphocytes and plasma cells at the dermoepidermal junction. Mucocutaneous pyoderma is the primary differential.
Traumatic injury to the skin is quite common in dogs and is often associated with compound fractures sustained in motor vehicle accidents. Post-traumatic alopecia may occur on the lower back in cats with history of pelvic injury. Dogfight wounds tend to be tears rather than punctures, as occur in cats; consequently, abscesses are a less common sequel. A plethora of foreign bodies may penetrate the canine integument, 2 of the more dramatic examples being foxtails and porcupine quills. The external ear canal and interdigital webs are favored sites for grass awn entry and subsequent migration. Retrievers or other animals wounded with steel shot may develop fistulous tracts or abscesses as steel shot corrodes when embedded in tissues.
Myospherulosis is a rare form of foreign-body reaction in which endogenous erythrocytes interact with an exogenous substance, such as antibiotics or ointments, or with endogenous fat. The lesions are subcutaneous nodules composed of sheets of large macrophages in which the cytoplasm is filled with homogeneous eosinophilic spherules. These structures may resemble fungal organisms but are negative with fungal special stains such as periodic acid–Schiff. The spherules stain for endogenous peroxidase, thus establishing their identity as erythrocytes.
Traction alopecia has been reported in dogs. It results from low-grade local ischemia induced by traction on hairs. The traction force is applied by elastic ties or hair barrettes applied to pull the forelock hair into a topknot. The lesions are focal patches of cutaneous atrophy and alopecia that may become eroded and crusted. Histologically, the lesion is an atrophic dermatosis. The epidermis is thin and may occasionally show single-cell necrosis, erosion, or ulceration. The hair follicles are inactive and atrophic, pale staining, and appear “faded.” Inflammation is minimal and is restricted to areas of surface ulceration.
Pyotraumatic dermatitis or “hot spot” is a common complication of flea-bite hypersensitivity or any pruritic dermatosis that leads to an itch-scratch cycle. It occurs most often in times of warm, humid weather. Breeds with a thick undercoat, such as German Shepherds, Golden Retrievers, Labradors, and Saint Bernards, are particularly prone to develop pyotraumatic dermatitis.. Lesions are extremely painful and occur at sites of self-trauma. Lesions are most often seen on the cheek, neck, and lateral thigh or the dorsal rump in flea-infested dogs. In Rottweilers, lesions typically occur on cheek and neck, whereas the lesions in German Shepherd dogs occur on the rump and thighs. Grossly, the initial lesions are erythematous, exudative, sharply demarcated patches, spreading extensively if not treated. The surface may be colonized by gram-positive cocci. Alopecia and hyperpigmentation are the typical sequelae. Pyotraumatic dermatitis is characterized histologically by epidermal ulceration. A thick serocellular inflammatory crust covers the denuded dermis. The predominantly neutrophilic reaction tends to be restricted to the area beneath the ulcer. Folliculitis and furunculosis are not features of classic pyotraumatic dermatitis but occasionally are concurrent conditions as indicated clinically by scattered papules at the periphery of the lesion. Eosinophils and/or folliculitis were common in one series of cases.
Injection site reactions are relatively common in domestic animals. Subcutaneously administered vaccines and therapeutic drugs may be responsible. The nodules may ulcerate or fistulate and are often suspected to be neoplasms. Histologically, the classic injection site reaction is composed predominantly of nodular aggregates of lymphocytes arranged around a central core of caseous necrosis. Lymphocytes may form follicles. Irregular refractile or faintly basophilic granular material is often embedded in the eosinophilic debris or found within phagocytic cells. Plasma cells, macrophages, and multinucleated giant cells are also present, but in lesser numbers than lymphocytes. The strong antigenic stimulus provided by the exogenous antigen sometimes results in the formation of germinal centers. The heterogeneity of the cell population and the lack of anaplastic characteristics in the lymphoid cells may differentiate these lesions, sometimes termed pseudolymphoma, from genuine lymphoma.
Vaccine administration in cats has been linked to the development of a variety of sarcomas, including fibrosarcomas, osteosarcomas, malignant fibrous histiocytomas, chondrosarcomas, and rhabdomyosarcomas. Vaccine-associated sarcomas have the unique features of a subcutaneous location, concurrent lymphocytic infiltrates, and macrophages that contain blue-gray foreign material. The proposed mechanism involves an overzealous reparative response, followed by malignant transformation of mesenchymal cells. Antigen load and degree of inflammation present at the vaccination site are possible influencing factors. Aluminum adjuvant particles have been identified in tumor-associated macrophages; however, vaccine-associated sarcomas have also been documented to arise from the use of nonadjuvanted vaccines. Injection of killed rabies vaccine in dogs can lead to focal mononuclear vasculitis and ischemic atrophy of surrounding follicles, resulting in a focal area of alopecia and is further discussed under Immune-mediated dermatoses. Injection-site eosinophilic granulomas with necrotic centers developed in some horses within 1-3 days as a response to the use of silicone-coated hypodermic needles. The lesion is suspected to be a form of delayed hypersensitivity.
Cats.
Cats are particularly prone to develop subcutaneous abscesses or cellulitis as a result of fight wounds. The cat bite produces a puncture-type wound that seals over and enables the introduced bacteria (chiefly oral flora) to multiply in the damaged tissue.
Cattle.
Tail tip necrosis of feedlot beef cattle is a disease in which slatted floor housing has been shown to be an important causal factor. The pathogenesis is presumed to be ischemia, secondary to compression of, or blunt trauma to, the more proximal parts of the tail. Clinically, there is alopecia, scaling, and crusting. Ulceration and suppuration are frequent sequelae. In early lesions, histologic examination reveals only perivascular edema and hemorrhage. Fully developed lesions are characterized by dermal scarring, follicular atrophy, vascular wall hypertrophy, and fragmentation of extravasated erythrocytes.
Pigs.
Intensive rearing systems for swine production have increased the occurrence of a variety of traumatic lesions. Those in piglets probably result from contact with concrete floors in farrowing crates. The carpi are the most common site affected, followed by the fetlocks and hocks. The nipples, particularly the cranial pair, are often involved, as is the tail. The lesions occur within a few hours of birth as circumscribed red macules, followed by necrosis, ulceration, and crusting. The ulcers heal over 3-4 weeks, leaving no permanent defect. The supernumerary digits of the hindlegs are subject to trauma in sows housed on concrete slats. Trauma resulting from vices, such as tail biting, ear biting, and flank biting, are common in growing pigs under intensive rearing systems of management. Wounds from a variety of causes, including fight wounds, often develop into subcutaneous abscesses in pigs.
Horses.
Cutaneous wounds are common in horses and can be attributed largely to the flighty temperament of the species. Exuberant granulation tissue—proud flesh—is a relatively frequent and serious sequel to wounds of the distal limbs. Poor circulation, minimal soft tissue, lack of adequate drainage, and a tendency for excessive movement predisposes the distal limbs to the development of excess granulation tissue. Decreased blood flow has been shown in horses with experimentally induced limb wounds as compared with wounds on the body. Furthermore, the limb wounds had lower glucose and higher lactate concentration than body wounds. These findings further support a role for decreased perfusion as well as metabolic disturbances in the development of equine exuberant granulation tissue. The gross lesion, a tumor-like mass of red-brown tissue, must be distinguished from equine sarcoid, cutaneous habronemiasis, mycoses, pythiosis, and squamous cell carcinoma. Histologically, immature capillaries and capillary loops arranged perpendicularly to the elongated fibroblasts and newly synthesized collagen are distinctive features. A superficial layer of granulation tissue may form in association with any of the above-mentioned conditions, and the entire lesion should be examined before a diagnosis is made.
Further reading
Bartels KE, et al. Corrosion potential of steel bird shot in dogs. J Am Vet Med Assoc 1991;199:856-863.
Brennan KE, Ihrke PJ. Grass awn migration in dogs and cats. A retrospective study of 182 cases. J Am Vet Med Assoc 1983;182:1201-1204.
Declercq J. Alopecia and dermatopathy of the lower back following pelvic fractures in three cats. Vet Dermatol 2004;15:42-46.
Gross TL, et al. Atrophic diseases of the hair follicle. A macroscopic and microscopic evaluation of canine and feline skin disease. Vet Dermatol 1992;295-297.
Hargis AM, et al. Myospherulosis in the subcutis of a dog. Vet Pathol 1984;21:248-251.
Hendrick MJ, Dunagan CA. Focal necrotizing granulomatous panniculitis associated with subcutaneous injection of rabies vaccine in cats and dogs: 10 cases (1988-1989). J Am Vet Med Assoc 1991;198:304-305.
Hershey AE, et al. Prognosis for presumed feline vaccine-associated sarcoma after excision: 61 cases (1986-1996). J Am Vet Med Assoc 2000;216:58-61.
Holm BR, et al. A prospective study of the clinical findings, treatment and histopathology of 44 cases of pyotraumatic dermatitis. Vet Dermatol 2004;15:369-376.
Jelinek F. Postinflammatory sarcoma in cats. Exp Toxicol Pathol 2003;55:167-172.
Madsen EB, Nielsen K. A study of tail tip necrosis in young fattening bulls on slatted floors. Nord Vet Med 1985;37:349-357.
Miller WM, et al. Environmental skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 659-684.
O'Dair HA, Foster AP. Focal and generalized alopecia. Vet Clin North Am 1995;25:858-861.
Ordeix L, et al. Traction alopecia with vasculitis in an Old English sheepdog. J Small Anim Pract 2001;42:304-305.
Penny RHC, et al. Clinical observations of necrosis of the skin of suckling piglets. Aust Vet J 1971;47:529-537.
Quist EM, et al. A case series of thermal scald injuries in dogs exposed to hot water from garden hoses (garden hose scalding syndrome). Vet Dermatol 2012;23:162-166.
von Sigmund HM, et al. Udder-thigh dermatitis of cattle: epidemiological, clinical and bacteriological investigations. Bov Pract 1983;18:18-23.
Slovis NM, et al. Injection site eosinophilic granulomas and collagenolysis in 3 horses. J Vet Intern Med 1999;13:606-612.
Sørensen MA, et al. Regional disturbances in blood flow and metabolism in equine limb wound healing with formation of exuberant granulation tissue. Wound Repair Regen 2014;22:647-653.
Swaim SF, et al. Pressure wounds in animals. Compend Contin Educ Pract Vet 1996;18:203-218.
Vitale CB, et al. Vaccine-induced ischemic dermatopathy in the dog. Vet Dermatol 1999;10:131-141.
Psychogenic injury
Several conditions in animals are considered to be similar to obsessive-compulsive disorders in humans. In theory, stress causes an increase in the production of endorphins, creating reinforcement of the stereotypic behavior characterizing each syndrome.
Psychogenic alopecia in cats, a self-induced form of alopecia precipitated or exacerbated by environmental stress, is similar to the obsessive-compulsive disorder of humans, trichotillomania. Although this condition does occur, it is very rare and generally overdiagnosed. A thorough diagnostic workup is needed to rule out allergic skin disease, ectoparasitism, and other medical causes for pruritus. In a study of 18 cats with presumed psychogenic alopecia, 16 cats were identified with medical causes of pruritus, whereas only 2 cats were found to have only psychogenic alopecia, and 3 cats had a combination of psychogenic alopecia and a medical cause of pruritus. The condition can occur in any cat, but is most common in indoor cats and oriental breeds. Affected cats groom excessively, licking, and pulling at the haircoat. Psychogenic alopecia/dermatitis has 2 clinical forms. In one, psychogenic dermatitis, affected cats lick and chew at a single site, creating a well-demarcated erythematous, ulcerated lesion of variable size, which usually is located on an extremity, the abdomen, or flank. The lesion grossly resembles those of eosinophilic plaque. The second, or alopecic form, is characterized by regional alopecia or hypotrichosis or regions of broken (barbered) hairs and normal skin. A trichogram examination of epilated hairs reveals a normal anagen to telogen ratio and fractured tips of hairs rather than tapered ends. Microscopic examination of skin in the alopecic form is usually normal, although wrinkling of the outer root sheath and intrafollicular and perifollicular hemorrhage may reflect the trauma applied to the hairs. Skin biopsies are helpful to identify an allergic reaction pattern in suspected cases; however, a normal biopsy cannot confirm psychogenic alopecia. The inflammatory form has no distinctive histologic features, as it is a nonspecific, ulcerative, hyperplastic, superficial perivascular dermatitis. Differentials for the alopecic form include atopy, flea allergic dermatitis, cheyletiellosis, and Demodex gatoi infestation. As pruritus in the cat is manifested in part by excessive grooming, any degree of perivascular eosinophilic dermatitis should be considered indicative of an underlying hypersensitivity disorder. The condition must also be differentiated from feline acquired hair shaft abnormality, a condition resembling trichorrhexis nodosa in humans. In this condition, cats with an underlying pruritic skin disease, such as flea allergic dermatitis groom excessively. Weakened hair shafts break easily and lead to alopecia. A trichogram reveals white nodes on the hair shafts corresponding to foci of frayed cortical fibers. A biopsy should show evidence of the underlying hypersensitivity condition.
Dogs also develop psychogenic dermatitis, including foot chewing and licking, tail biting, and flank sucking. The gross lesions may be slight, but the superficial excoriations often develop into pyoderma. Acral lick dermatitis, otherwise known as “lick granuloma,” acral pruritic nodule, or neurodermatitis, is a relatively common disorder of large active-breed dogs younger than 5 years. Allergic skin disease may be a predisposing factor. Males are affected twice as frequently as females. The areas traumatized by persistent licking and chewing are most commonly the cranial carpus and metacarpus, followed by the radius, tibia, and metatarsus. Erythema and epidermal excoriations give rise to a single well-circumscribed, eroded or ulcerated, oval plaque. Occasionally, lesions are multiple. Secondary bacterial infection may result. Re-epithelialization of the lesion leaves a well-circumscribed alopecic plaque, often with peripheral hyperpigmentation. Histologically, the lesions have superficial perivascular dermatitis with marked acanthosis and rete ridge formation and compact orthokeratotic and parakeratotic hyperkeratosis (Fig. 6-40 ). The hair follicles are enlarged and elongate. Superficial dermal fibrosis is usually marked, and collagen fibers in dermal papillae are often arranged perpendicular to the surface epithelium (Fig. 6-41 ). This “vertical streaking” of collagen is thought to result from chronic irritation. Perifolliculitis, folliculitis, and sometimes furunculosis are often present. Plasmacytic infiltrates often surround the sweat glands. Sebaceous glands and hair follicles appear hyperplastic.
Figure 6-40.
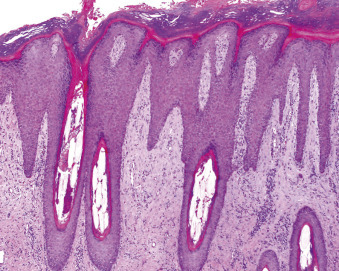
Acral lick dermatitis in a dog. Superficial perivascular dermatitis with marked compact orthokeratotic hyperkeratosis, and acanthosis with rete ridge formation.
Figure 6-41.
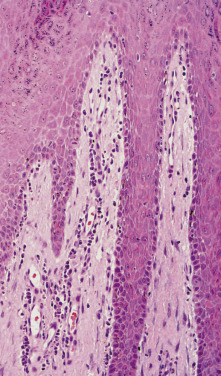
Acral lick dermatitis in a dog. Vertical alignment of collagen.
In horses, the equine self-mutilation syndrome can be misinterpreted as a possible cutaneous disorder as horses bite, kick, or rub the flank or pectoral areas. The behavior is usually accompanied by vocalization, spinning, or rolling and is most common in stallions. The condition is thought to be stress related. There are no primary cutaneous lesions; however, secondary excoriations may be present.
A self-destructive behavioral condition primarily affecting first-calf heifers is characterized by excessive licking of the udder and teats, sometimes leading to teat necrosis and culling. The condition is associated with udder edema and increased levels of histamine in the udder tissue leading to pruritus.
Further reading
Alhaidari Z, et al. Acquired feline hair shaft abnormality resembling trichorrhexis nodosa in humans. Vet Dermatol 1996;7:235-238.
Beale K. Feline demodicosis: a consideration in the itchy or overgrooming cat. J Feline Med Surg 2012;14:209-213.
Dodman NH, et al. Equine self-mutilation syndrome (57 cases). J Am Vet Med Assoc 1994;204:1219-1223.
Sawyer LS, et al. Psychogenic alopecia in cats: 11 cases (1993-1996). J Am Vet Med Assoc 1999;214:71-74.
Shumaker AK, et al. Microbiological and histopathological features of canine acral lick dermatitis. Vet Dermatol 2008;19:288-298.
Virga V. Behavioral dermatology. Vet Clin North Am Small Anim Pract 2003;33:231-251.
Waisglass SE, et al. Underlying medical conditions in cats with presumptive psychogenic alopecia. J Am Vet Med Assoc 2006;228:1705-1709.
Yeruham I, Markusfeld O. Self destructive behavior in dairy cattle. Vet Rec 1996;138:308.
Mineral deposition in cutaneous tissues
Deposition of insoluble calcium salts within cutaneous tissues can occur as a result of injury or degeneration of skin components (dystrophic mineralization or calcification), secondary to calcium/phosphorus metabolic alterations (metastatic mineralization or calcification), as an idiopathic condition, or may occur iatrogenically. Mechanisms leading to calcium salt deposition are complex and involve such factors as the lower pH of injured tissue, mitochondrial concentration of calcium and phosphorus, and the influx of calcium into injured cells in dystrophic forms. In metastatic forms, loss of mineralization inhibitors, changing of ions into a solid phase, and phosphate ion initiation of crystal formation are implicated in salt formation. Mineralization can be localized, as in inflammatory foci (granulomas), in degenerative lesions (follicular cysts), or in neoplasms (pilomatricomas), or may be generalized as in the tissue mineralization associated with chronic renal failure.
Dystrophic mineralization has been associated with hyperadrenocorticism, diabetes mellitus, local inflammation, and tissue degeneration or necrosis. It has also been reported in association with drug injections and severe systemic disease such as leptospirosis. The most well-known form of dystrophic mineralization is calcinosis cutis in dogs with iatrogenic or naturally occurring hyperadrenocorticism, which is discussed in Endocrine diseases of skin.
Metastatic calcinosis is rare. It has been associated with chronic renal failure; congenital renal dysfunction, including renal dysplasia; primary hyperparathyroidism; and hypervitaminosis D. It has also been reported in dogs with systemic blastomycosis and paecilomycosis. Dogs with systemic blastomycosis treated with amphotericin B developed lesions that resolved over time and were indistinguishable from calcinosis cutis of hypercortisolism. Dogs had severe granulomatous cutaneous lesions that may have been predisposed to dystrophic mineralization, but mineralizing lesions were more extensive or separate from primary inflammatory lesions. The dogs had no clinically significant serum calcium/phosphorus abnormalities. Additional factors suspected to contribute to mineralization included mild intermittent serum calcium fluctuations, mononuclear cell production of factors leading to increased osteoclast-mediated bone resorption, and alteration of vitamin D metabolism.
Idiopathic calcinosis cutis occurs in otherwise healthy dogs <1 year of age with no history of glucocorticoid administration. These dogs have widespread lesions that spontaneously regress within 1 year.
Iatrogenic calcinosis cutis occurs secondary to percutaneous absorption of products containing calcium chloride or calcium carbonate. Multifocal, flat-topped, and centrally ulcerated papules and small nodules affect glabrous skin, such as the lips, axilla, and inguinal and interdigital skin. Histologically, granulomas are centered on degenerate, mineralized collagen fibers. Ultrastructural examination of experimental lesions indicated that mineral was deposited within the collagen bundles within 24 hours of initial skin contact. The main differential diagnosis was calcinosis cutis of hyperadrenocorticism, to which the lesions are histologically identical.
A chemically induced, iatrogenic form of calcinosis cutis has been reported in humans and a dog as a consequence of the subcutaneous administration of a 10% calcium gluconate solution for treatment of hypoparathyroidism. In the dog, calcium salts formed on basement membranes, dermal collagen, vessel walls, and adipocyte membranes. Dermoepidermal separation, pyogranulomatous dermatitis, panniculitis, and vasculopathy ensued, leading to marked necrosis and sloughing of the skin. Concurrent hyperphosphatemia was thought to predispose to precipitation of calcium salts.
Calcinosis universalis refers to widespread areas of calcinosis cutis and can be seen with hypercortisolism, percutaneous absorption of calcium-containing products, or from the iatrogenic administration of calcium-containing solutions. Some forms of calcinosis cutis can be indistinguishable histologically from calcinosis cutis associated with hyperadrenocorticism. The clinical presentation, concurrent abnormalities, signalment, and history should allow distinction of the various forms of calcinosis cutis.
Cutaneous lesions include papules, plaques, and nodules that are firm, gritty, and white to yellow. Ulceration and secondary infection are common. Lesions may occur anywhere, but common sites are over the dorsal cervical region, groin, and axillae. Metastatic mineralization may occur more commonly in the pawpads of cats and dogs. Histologically, calcium salts are deposited on collagen and elastin fibers in the dermis and basement membrane zones. The basophilic stippled and fractured material is often surrounded by macrophages, multinucleated giant cells, and fibrosis. The mineralized material is eliminated transepithelially through the epidermis and hair follicles, often leading to ulceration.
Calcinosis circumscripta (tumoral calcinosis) occurs most often in dogs, horses, and occasionally cats (see also Ectopic mineralization and ossification, in Vol. 1, Bones and joints). Lesions in dogs are most often solitary but can be multiple and occur most often in large breeds <2 years of age. German Shepherd dogs are predisposed. The skin over bony prominences of the limbs is most often affected. The tongue and paravertebral soft tissues, pawpads, edges of the pinna in dogs with cropped ears, and cheeks of Boston Terriers are other reported sites. Calcinosis circumscripta of the dorsal thoracolumbar region at a site of previous progestogen injection has been reported in a cat. In horses, young male Standardbred horses appear to be predisposed, and lesions are most common over the lateral stifle.
The gross and histologic features of the lesion evolve over time. Initially, the lesion may be bulging, fluctuant or cystic, variably ulcerated, and contains chalky white material (Fig. 6-42 ). Histologically, subcutaneous to deep dermal lakes of basophilic granular material that stain with von Kossa are surrounded by mild fibrosis and a cellular zone of variable width with giant cells, large macrophages, and fewer lymphocytes and plasma cells (Fig. 6-43 ). Over time, the lesions become firm, progressively more mineralized, and associated with dense fibrous connective tissue bands. Inflammation may subside to some degree over time, and osseous or cartilaginous metaplasia may take place. Epidermal sequestration or transepidermal elimination of mineralized material may lead to ulceration.
Figure 6-42.
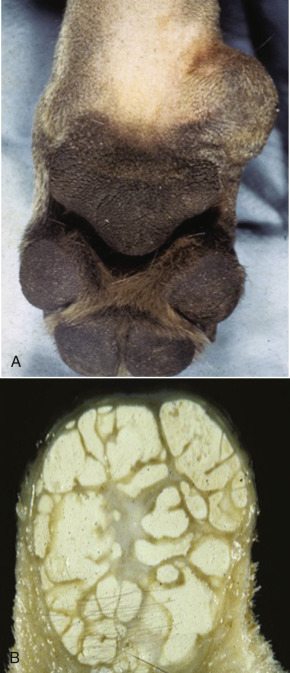
Calcinosis circumscripta in a dog. A. Note the swelling on the medial side of the carpus. B. Subgross shows lakes of chalky material.
(Courtesy M. Goldschmidt.)
Figure 6-43.
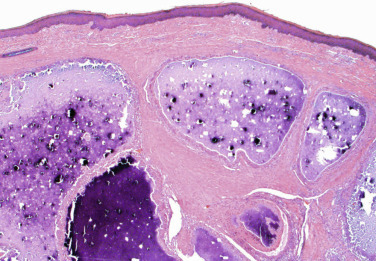
Calcinosis circumscripta in a dog. Dermal lakes of basophilic granular material are surrounded by mild fibrosis and giant cells, macrophages, and fewer lymphocytes and plasma cells.
The pathogenesis of calcinosis circumscripta is not known; it is likely that multiple factors are involved. Dystrophic mineralization secondary to previous tissue trauma has been proposed based on the predilection for skin covering bony prominences. This explanation is not entirely satisfactory as the lesions do not recur after surgical excision, and trauma to these sites in large dogs would be expected to be repetitive. The name “apocrine cystic calcinosis” was previously applied to calcinosis circumscripta because it has been documented to arise from degenerating, cystic apocrine (epitrichial) glands. A relationship to epitrichial glands is not evident in most cases. Lesions have also developed at sites of previous injections, or in association with surgical sites sutured with polydioxanone sutures. Cases of calcinosis circumscripta have also been reported to occur in the pawpads of dogs and cats with chronic renal failure, and in the pawpads of an otherwise healthy German Shepherd dog and in another German Shepherd dog with pododermatitis. Symmetrical cases that resolved spontaneously have been reported in young dogs with underlying skeletal disease, such as hypertrophic osteodystrophy. In humans, the disorder can be inherited as an autosomal recessive trait.
Further reading
Bertazzolo W, et al. Clinicopathological findings in five cats with paw calcification. J Feline Med Surg 2003;5:11-17.
Davidson EB, et al. Calcinosis circumscripta of the thoracic wall in a German shepherd dog. J Am Anim Hosp Assoc 1998;34:153-156.
Declercq J, Bhatti S. Calcinosis involving multiple paws in a cat with chronic renal failure and in a cat with hyperthyroidism. Vet Dermatol 2005;16:74-78.
Doerr KA, et al. Calcinosis cutis in dogs: histopathological and clinical analysis of 46 cases. Vet Dermatol 2013;24:355-361.
Frazier KS, et al. Multiple cutaneous metaplastic ossification associated with iatrogenic hyperglucocorticism. J Vet Diag Invest 1998;10:303-307.
Gortel K, et al. Calcinosis cutis associated with systemic blastomycosis in three dogs. J Am Anim Hosp Assoc 1999;35:368-374.
Gross TL. Calcinosis circumscripta and renal dysplasia in a dog. Vet Dermatol 1997;8:27-32.
Holahan ML, et al. Generalized calcinosis cutis associated with disseminated paecilomycosis in a dog. Vet Dermatol 2008;19:368-372.
Marcos R, et al. Cytochemical detection of calcium in a case of calcinosis circumscripta in a dog. Vet Clin Pathol 2006;35:239-242.
Muller A, et al. Metastatic calcinosis (including calcinosis cutis) in a young dog with multiple urinary tract abnormalities. Vet Dermatol 2011;22:279-283.
O'Brien CR, Wilkie JS. Calcinosis circumscripta following an injection of proligesterone in a Burmese cat. Aust Vet J 2001;79:187-189.
Paradis M, Scott DW. Calcinosis cutis secondary to percutaneous penetration of calcium carbonate in a Dalmatian. Can Vet J 1989;30:57-59.
Schaer M, et al. Severe calcinosis cutis associated with treatment of hypoparathyroidism in a dog. J Am Anim Hosp Assoc 2001;37:364-369.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Stone WC, et al. The pathologic mineralization of soft tissue: calcinosis circumscripta in horses. Compend Contin Educ Pract Vet 1990;12:1643-1648.
Tafti AK, et al. Calcinosis circumscripta in a dog: a retrospective pathological study. J Vet Med A Physiol Pathol Clin Med 2005;52:13-17.
Volk AV, et al. Calcinosis cutis at cytarabine injection site in three dogs receiving prednisolone. Vet Rec 2012;171:327-329.
Cold injury
Most cold-induced cutaneous lesions (frostbite) result not only from direct freezing and disruption of the cells, but more importantly from vascular injury and resultant tissue anoxia. In experimental frostbite lesions in Hanford miniature swine, vacuolation of keratinocytes was the earliest change in the epidermis, followed by spongiosis, epidermal necrosis, and separation of the necrotic epithelium from the dermis. Hyperemia and hemorrhage were also early lesions. Inflammatory changes, comprising neutrophilic infiltration and necrotizing vasculitis, occurred 6-48 hours postinjury. Thrombosis of small arterioles increased in severity up to 1 week postinjury. By 2 weeks, considerable epithelial regeneration had taken place, either as a complete replacement or as crescents beneath the necrotic epidermis.
Cutaneous injury resulting from cold is uncommon in well-nourished, healthy domestic animals. Well-acclimatized longhaired animals can tolerate temperatures of −50° C for indefinite periods. Cold injury occurs most commonly on the tips of the ears and tail of cats, the scrotum of male dogs and bulls, and the tips of the ears, tail, and teats in cattle. The teats are particularly vulnerable if cows are turned out into the cold with wet udders. Affected skin is cool, pale, and hypoesthetic. The gross lesions include alopecia, scaling, and pigmentary alterations of the skin, hair, or both. In severe cases, the ischemic necrosis results in dry gangrene and sloughing of the affected part.
Freeze branding using a branding iron cooled with dry ice or liquid nitrogen—used to identify horses permanently—causes damage to pigment-producing hair cells resulting in leukotrichia.
Further reading
Arvesen A, et al. Early and late functional and histopathological perturbations in the rabbit ear-artery following local cold injury. Vasa 1999;28:85-94.
Barth AD, Waldner CL. Factors affecting breeding soundness classification of beef bulls examined at the Western College of Veterinary Medicine. Can Vet J 2002;43:274-284.
Rothenberger J, et al. Assessment of microcirculatory changes of cold contact injuries in a swine model using laser Doppler flowmetry and tissue spectrophotometry. Burns 2014;40:725-730.
Thermal injury
Heat may be applied to the skin in a variety of forms and, depending on duration and intensity, will produce mild to severe necrotizing lesions. Longer exposure to lower temperatures is more damaging than short exposure to higher temperatures. The lowest temperature at which skin can burn is 44° C (111° F). Dry heat causes desiccation and carbonization, whereas moist heat causes “boiling” or coagulation. Thermal injury in domestic animals may be caused by hot liquids, steam, heating pads, hair dryers, drying cages, hot metals such as wood stoves or car engines, fires, friction from rope “scalds,” electrical burns from chewing electrical wires, improperly grounded electrocautery units, or lightning strikes. Linear burns may occur on the dorsum of dogs exposed to hot water from garden hoses. This typically occurs in the warm summer months when the ambient temperature exceeds 32° C (90° F). Animals struck by lightning may show a jagged line of singed hair running down a shoulder or flank (Fig. 6-44 ). This finding is valuable in establishing an otherwise difficult diagnosis. Rarely, small animals incur microwave burns.
Figure 6-44.

Lightning strike. A linear arrangement of singed hairs in a deer.
(Courtesy J. Czech, Pennsylvania Game Commission.)
Burns are classified into 4 degrees according to depth of injury.
-
•
First-degree burns involve only the epidermis. The heated areas are erythematous and edematous as a result of vascular reaction in the dermis, but vesicles do not form. The epithelial cells show no morphologic sign of injury, although there may be surface desquamation after a few days.
-
•
In second-degree burns, the epidermis and part of the dermis are damaged. The cytoplasm of the epithelial cells is hypereosinophilic, and the nuclei are shrunken or karyorrhectic. Coagulative necrosis of the epidermis (Fig. 6-45 ) can occur in the absence of substantial dermal injury and often “wicks” down to involve the follicular epithelium (Fig. 6-46 ). The vascular changes are more prominent than in lesser burns, with marked dermal edema and spongiosis. Vesicles and bullae form in the epidermis, often at the dermoepidermal junction. The bullae contain serum, granular debris, and leukocytes. Healing can be complete if secondary infection does not lead to deeper injury.
-
•
In third-degree burns, the destructive effect of the heat extends full thickness through the epidermis and dermis, causing coagulative necrosis of connective tissues, blood vessels, and adnexa. Thermal injury causes thrombosis of blood vessels and vascular leakage, leading to the coagulative necrosis of more superficial tissues. Heat of sufficient intensity or duration to penetrate this deeply usually desiccates and chars the outer epidermis. Coagulative necrosis of the dermis produces a swollen amorphous accretion of the connective tissues accompanied by an acute inflammatory reaction. Over time, histiocytes infiltrate the subcutis and fibrosis ensues. Subcutaneous vasculitis may be present. The necrotic tissue sloughs, and the defect is filled in by granulation tissue. Permanent scarring results, with loss of adnexa.
-
•
Fourth-degree burns are similar in character to those of third degree but penetrate below the dermis to and beyond the subcutaneous fascia; their local consequences depend on what lies underneath. Heat in surface tissue is conducted to deeper tissues via the blood and lymph. The degree of injury may not be evident for several days after the insult occurred. Follicular and sweat gland damage continues for 24-48 hours. Once lesions fully develop, the progress of injury should cease, which is helpful in making the diagnosis. Histologically, thermally induced tissue damage is not sharply demarcated and should dissipate gradually with increasing depth of the biopsy. Clinical differentials include toxic epidermal necrolysis, erythema multiforme major, bullous pemphigoid, pemphigus vulgaris, vasculitis, trauma, and other causes of ischemia. Lesions from thermal injury sometimes have an abnormal anatomic distribution or pattern, such as drips, angles, lines, or areas of contact that may be helpful in the differential diagnosis.
Figure 6-45.

Burn on the dorsal head of a dog from the ignition of lighter fluid. A. Acute burn (12 hours old). B. Three weeks later, with scarring.
Figure 6-46.
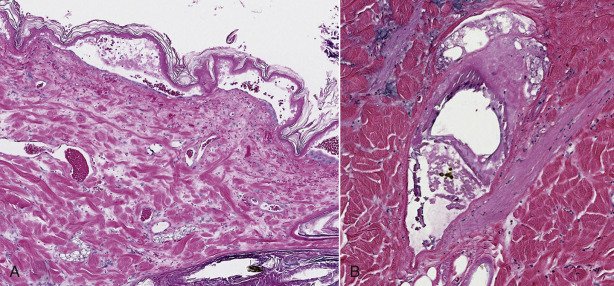
Burn. A. Full-thickness coagulative necrosis of the epidermis with vesiculation and loss of cell detail in the dermis. B. Necrosis in the dermis may be subtle; however, hair follicles and sebaceous glands are often more severely affected because of a “wicking effect.”
(Courtesy K. Credille.)
Microwave burns are unique in that the lesions are sharply delineated histologically without a tapering of the degree of coagulative necrosis in the deeper tissues. The degree of injury is uniform throughout the tissue, and inflammation is minimal. The depth of damage depends on the frequency of the microwaves, with some frequencies sparing the superficial tissues and coagulating the deeper tissues. Pain perception may not occur until the damage is done and lesions may not be evident for up to 6 days. There is no surface charring, blister formation, or edema. There is thrombosis of vessels, and the tissue is mummified. Injury is due to ionizing radiation leading to heat generated from the vibration of molecules in the tissue.
Full-thickness cutaneous burns have been reported to occur in black-haired spots of Dalmatians as a result of solar radiation. Normally, cutaneous injury from solar radiation affects lightly pigmented sparsely haired skin rather than areas protected by pigment. Black skin absorbs approximately 45% more solar radiation than white skin. The absorption of visible light (400-700 nm) can result in the production of thermal energy resulting in a burn. Ultraviolet (UV) light (100-400 nm) does not penetrate into the dermis and does not produce substantial thermal energy, but has other deleterious effects (see Actinic diseases of skin). Pain, prompting moving to the shade, was likely not perceived by the dogs as the burns were multifocal, involving only black-haired areas, and Dalmatians are primarily white.
Another unique type of thermal injury, radiant heat dermatitis, is similar to erythema ab igne in humans. Tissue damage occurs from repeated exposure to moderate heat. Radiant heat dermatitis has been reported as an asymptomatic condition in dogs sleeping next to wood burning stoves or fires, or chronically exposed to heat lamps. The lesions were on the dorsolateral trunk and had a drip-like configuration. Grossly, irregular areas of alopecia were erythematous and hyperpigmented peripherally. Centrally, the lesions are scaly and depigmented. In the acute form, lesions resemble actinic dermatosis with epidermal thinning, basal cell vacuolation, and possible epidermal dysplasia. The dermis has thin fragmented or smudged collagen, increased elastin fibers, and melanin and hemosiderin deposits. There may be eosinophilic, wavy elastin fibrils in the superficial dermis (“red spaghetti of Walder”). Over time, epidermal and infundibular hyperplasia, hyperkeratosis, and dyskeratosis develop with focal spongiosis and cell necrosis. Karyomegaly of basal cells, dermal edema and mucinosis, hyperplastic sebaceous glands, dilated epitrichial glands, and mixed perivascular dermatitis may be present.
Radiation injury
Advances in the treatment of cancer in companion animals have made the possibility of radiation-induced skin injury more likely. Clinicians and pathologists need to be able to recognize these lesions to provide the best management options and accurate prognosis for resolution of the lesions. The varieties of radiation modalities available have variable degrees of tissue penetration and potential for tissue injury. Some forms of radiotherapy penetrate deeper tissues while sparing the skin, and others are more concentrated in the superficial tissues or are preferentially absorbed by specific tissues. The type of radiation therapy, source, dose, intensity, and duration of exposure dictate the range of possible side effects. Ionizing photons disrupt chemical bonds in cells, leading to injury or cell death. Some cells are not lethally damaged but sustain DNA damage to the extent that replication/replacement are not possible. The effects of radiation damage can be divided into acute and chronic forms.
Acute radiation injury to the skin is a result of damage to rapidly dividing cells. Damage is self-limiting and recovery is associated with rapid cell turnover. Clinical lesions of radiation dermatitis appear 2-4 weeks after exposure. Initially, there is erythema, pain, edema, and heat, followed several weeks later by dry or moist desquamation, depending on the degree of injury. Histologically, the lesions resemble a second-degree burn, with suprabasilar or subepidermal bullae formation, dermal edema with fibrin exudation, and a marked leukocytic infiltrate. Re-epithelialization occurs over a period of 10-60 days. The damage sustained to germinal epithelium of hair follicles and sebaceous glands leads to alopecia within 2-4 weeks after exposure. Hair regrowth will follow over the next several months, but damage to sebaceous glands is not reversible and leads to permanent scaling.
The chronic lesions of radiation injury are evident months to years after treatment and are primarily due to damage to the microvasculature. The epidermis is thin, friable, and in some areas hyperplastic, and may become neoplastic. There is hyperpigmentation and hyperkeratosis. Chronic exudative ulcers may develop but granulation tissue does not form. The dermis is fibrotic with atypical fibroblasts, telangiectasia, and possibly deep arteriolar changes. Endothelial swelling, necrosis, and thrombosis lead to occlusion and excessive endothelial proliferation, that when combined with the effects of vascular leakage, leads to vascular collapse. This condition of progressive vessel abnormalities is referred to as obliterative endoarteritis and is known to form a “histohematic” barrier to surrounding tissue, leading to continued anoxia and nutrient shortage.
Further reading
Coyne BE, et al. Thermoelectric burns from improper grounding of electrocautery units: two case reports. J Am Anim Hosp Assoc 1993;29:7-9.
Dernell WS, Wheaton LG. Surgical management of radiation injury-part I. Compend Contin Educ Pract Vet 1995;17:181-190.
Gieser DR, Walker RD. Management of large animal thermal injuries. Compend Contin Educ Pract Vet 1985;7:S69-S78.
Gross TL, et al. Diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 3-193.
Hargis AM, Lewis TP. Full-thickness cutaneous burn in black-haired skin on the dorsum of the body of a Dalmatian puppy. Vet Dermatol 1999;10:39-42.
Holm BR, et al. A prospective study of the clinical findings, treatment and histopathology of 44 cases of pyotraumatic dermatitis. Vet Dermatol 2004;15:369-376.
Miller WM, et al. Environmental skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 659-684.
Quist EM, et al. A case series of thermal scald injuries in dogs exposed to hot water from garden hoses (garden hose scalding syndrome). Vet Dermatol 2012;23:162-166.
Reedy LM, Clubb FJ. Microwave burn in a toy poodle: a case report. J Am Anim Hosp Assoc 1991;27:497-500.
Scarratt WK, et al. Cutaneous thermal injury in a horse. Equine Pract 1984;6:13-17.
Swaim SF, et al. Heating pads and thermal burns in small animals. J Am Anim Hosp Assoc 1989;25:156-162.
Walder EJ, Hargis AM. Chronic moderate heat dermatitis (erythema ab igne) in five dogs, three cats and one silvered langur. Vet Dermatol 2002;13:283-292.
Chemical injury to skin
Primary irritant contact dermatitis
Irritant contact dermatitis is caused by contact with a substance that causes direct toxic damage. An abnormal skin barrier from either physical damage to the stratum corneum (e.g., excessive moisture) or pre-existing inflammatory skin disease may enhance penetration of the offending substance. In small animals, irritant contact dermatitis is relatively uncommon. Irritant substances vary in their potency. Strong acids or alkalis induce immediate and severe tissue damage, whereas mild detergents or soaps may require repeated applications. Agents capable of causing direct cutaneous damage include acids, such as carbolic or sulfuric, alkalis, cresol tars, paints, kerosene, turpentine, antiseptics, and insecticides. An example of the last mentioned is “flea collar dermatitis” of dogs and cats. Feces and urine are also potential irritants.
Primary irritant contact dermatitis must be distinguished from allergic contact dermatitis (discussed under Hypersensitivity dermatoses). Irritant contact dermatitis does not involve prior sensitization. It may occur in any species, but is most frequent in the horse, cow, and dog.
The distribution of gross lesions of contact irritant dermatitis in the dog (Fig. 6-47A, B ) and cat typically involves the glabrous skin of the ventral abdomen, axilla, medial thigh, perianal and perineal areas, footpads, ventral tail, chin, and inner aspect of the pinnae. An irritant reaction can occur in the ear canals of dogs being treated with topical medications for otitis. The concave pinna and vertical canal may develop transient blisters, followed by erosions and a dark red to brown discoloration and fine white scale. The haired skin is only involved if the irritant substance is in an aerosol or liquid form. Flea collar dermatitis lesions occur as a band around the neck corresponding to the position of the offending collar. In horses, lesions occur most commonly on the muzzle, lower limbs, and in areas of contact with the riding tack. Horses with diarrhea may develop severe irritant dermatitis on the soiled perineum.
Figure 6-47.
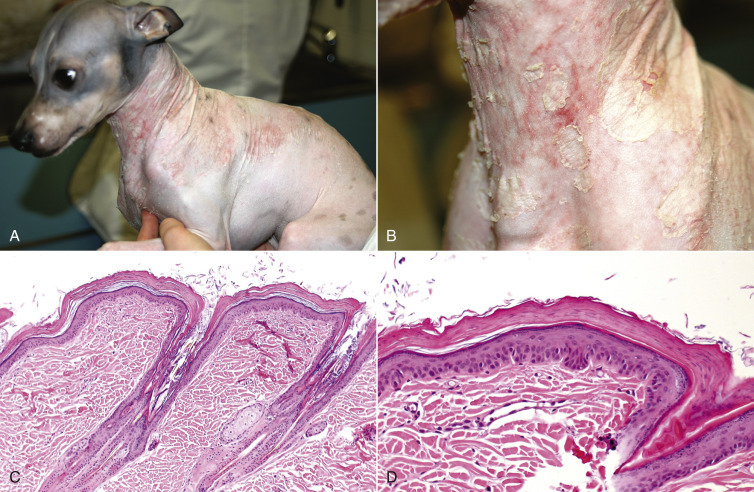
Irritant contact dermatitis in a hairless mixed-breed dog. A, B. Marked erythema and scaling on the neck and thorax caused by a sweater that was washed in irritating laundry soap. C. Diffuse parakeratotic hyperkeratosis with a prominent granular layer. D. Note the inner stratum corneum has normalized to a basketweave pattern.
The gross lesions consist of marked erythema, swelling, and a transient papular-vesicular stage that leads to ulceration and, in severe cases, sloughing of the affected skin. The sequelae include alopecia, scarring, and alteration in skin and hair pigmentation. In dogs, lesions often occur on the glabrous skin of the abdomen and appear erythematous with shiny adherent scale. Hyperpigmentation occurs in most species of domestic animals, but in horses, leukoderma or leukotrichia may be a permanent result of irritant contact dermatitis. Severe lesions can be considered a chemical burn. Differentials include thermal injury and allergic contact dermatitis.
The histologic lesions of irritant contact can be complicated by self-trauma and can be difficult to differentiate from those of allergic contact dermatitis (Fig. 6-47C, D). The histologic lesions vary depending on the caustic nature of the compound. Early lesions consist of epidermal edema with spongiotic vesicles and neutrophils or epidermal necrosis with separation from the dermis. In client-owned animals, lesions that are biopsied are typically in a chronic stage. Histologic suggestions of a chronic irritant reaction include mild acanthosis with compact parakeratotic hyperkeratosis in the presence of a granular layer. The nucleation of the keratin is subtle, which distinguishes the lesion form the robust nuclei in superficial necrolytic dermatitis or zinc-responsive dermatosis. The lesion can mimic ichthyosis, particularly if the reaction occurs in a young dog. The inflammatory infiltrate is variable in nature, probably reflecting such factors as chronicity, self-trauma, and secondary infection. The diagnosis of irritant contact dermatitis depends largely on the history and the clinical signs, particularly the distribution of the lesions.
In swine, cutaneous erythema and pruritus have been observed within 48 hours of tiamulin administration. The most severely affected pigs were recumbent and developed fatal necrolytic dermatitis. The areas most severely affected were those in contact with feces and urine. Histologic lesions included full-thickness epidermal necrosis, intraepidermal pustules, and serocellular crusting. It was hypothesized that the lesions represent a severe form of contact irritant dermatitis to tiamulin or one of its metabolites in the excreta. Skin lesions regressed when the drug was withdrawn.
An eosinophilic dermatitis was observed in pigs following heavy salting of pen floors. Lesions were present on the feet.
Further reading
Andersson P, Petaja E. Profound eosinophilic dermatitis in swine caused by sodium chloride. Nord Vet Med 1968;20:706-707.
Declercq J, De Bosschere H. Diesel oil-induced alopecia in two cats. Vet Dermatol 2009;20:135-138.
Gross TL, et al. Diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 3-193.
Kimura T. Contact dermatitis caused by sunless tanning treatment with dihydroxyacetone in hairless descendants of Mexican hairless dogs. Environ Toxicol 2009;24:506-512.
Kimura T. Contact hypersensitivity to stainless steel cages (chromium metal) in hairless descendants of Mexican hairless dogs. Environ Toxicol 2007;22:176-184.
Murayama N, et al. A case of superficial suppurative necrolytic dermatitis of miniature schnauzers with identification of a causative agent using patch testing. Vet Dermatol 2008;19:395-399.
Nesbitt GH, Schmitz JA. Contact dermatitis in the dog: a review of 35 cases. J Am Anim Hosp Assoc 1977;13:155-163.
Niza ME, et al. Effects of pine processionary caterpillar Thaumetopoea pityocampa contact in dogs: 41 cases (2002-2006). Zoonoses Public Health 2012;59:35-38.
Oberkirchner U, et al. Metaflumizone-amitraz (Promeris)-associated pustular acantholytic dermatitis in 22 dogs: evidence suggests contact drug-triggered pemphigus foliaceus. Vet Dermatol 2011;22:436-448.
Scott DW, et al. Small Animal Dermatology. 5th ed. Philadelphia: WB Saunders; 1995. p. 867-869.
Trenti D, et al. Suspected contact scrotal dermatitis in the dog: a retrospective study of 13 cases (1987 to 2003). J Small Anim Pract 2011;52:295-300.
Turner V, et al. A survey for small animal veterinarians regarding flea and tick control pesticide products. Can Vet J 2011;52:1080-1082.
Envenomation
The venom of insects, spiders, other arthropods and snakes can cause mild or severe skin lesions with or without systemic signs. Effects are dependent upon composition of the venom, individual victim response, anatomic location of the envenomation, and specific characteristics of the offending organism that may be influenced by season of the year, geographic location, time since the last inflicted bite or sting, depth of injury, and so on. Different species of animals respond differently to the same venom.
Stings from Solenopsis invicta, the imported fire ant, are common in humans in South America and in most of the southern United States. The ants swarm by the hundreds, covering objects or parts of victims and simultaneously inflict numerous painful stings. The fire ant venom is primarily composed of an insoluble alkaloid (solenopsin A), shown to be cytotoxic, bactericidal, fungicidal, insecticidal, and hemolytic. Lesions in dogs have been documented and consist of initial swelling progressing to erythematous nodules within 10-20 minutes. Histologically, the sting in dogs produces a vertically oriented zone of coagulative dermal necrosis with variable epidermal necrosis. Necrosis includes the adnexa and may extend into the subcutis. Lesions resolve quickly. Severe type I hypersensitivity (anaphylaxis) reactions are possible.
Stings from hymenopteran insects, such as bees, wasps, and hornets, produce effects of a local (angioedema) or possibly systemic type I hypersensitivity reaction caused by the histamine, serotonin, and kinins in the venom (see Hypersensitivity dermatoses). Multiple-sting dermatoses lead to toxic reactions that can be fatal.
Spider bites are rarely documented definitively in animal or human patients as the initial bite goes unnoticed, and the spider is no longer recoverable by the time lesions develop. Bites occur most often on the face and extremities. Most spider bites produce localized pain, erythema, and swelling and are not of further consequence. Spiders of importance to the study of the integumentary system are those with venoms leading to dermonecrosis and eschar formation, a condition referred to as “necrotic arachnidism.” The brown recluse spider (Loxosceles reclusus) is the spider most well known to induce dermal necrosis, although there are a number of others. Brown recluse venom contains hyaluronidase and sphingomyelinase-D, which degrade tissues. A blister with a surrounding pale halo and more peripheral erythema characterizes initial reactions documented in humans and some experimental animals. Necrosis and eschar formation occur within 5-7 days. Ulceration may be extensive. Histologically, there is hemorrhage and edema, neutrophilic vasculitis, and arterial wall necrosis. The epidermis and dermis undergo necrosis that may extend into the subcutis and underlying muscle. Panniculitis may be present. Eventually, there is dermal scarring and replacement of the subcutis and muscle by hypocellular connective tissue. Brown recluse spider bites in humans can also lead to massive hemolysis. Differentials include other venomous bites, vasculitis, slough caused by iatrogenic injection of irritating substances, thermal burns, necrotizing fasciitis or other cutaneous infection, septic embolization, or trauma. Compatible lesions, environmental history, and ruling out other conditions producing similar lesions can lead to the presumptive diagnosis of a spider bite.
Snakebite envenomation produces local tissue necrosis and variable systemic effects. Snake venom contains various enzymes, proteins, peptides, and kinins. Systemic effects of snake venom include paralysis, coagulation disturbances, shock, increased capillary permeability, myocardial damage, rhabdomyolysis, and renal failure. Of the 5 genera of venomous snakes, crotaline (rattlesnake, copperhead, cottonmouth, and others) venom contains the highest concentration of proteolytic enzymes. Local effects include pain, edema, hemorrhage, bullae formation, necrosis, and sloughing of tissue. Bites inflicted in the head or neck region may lead to swelling that interferes with respiration. Bites of pit vipers also introduce potentially dangerous bacteria, such as Clostridia spp., into the puncture wound. Bites are common in the dog, horse, and, to a lesser degree, cats, and most often are inflicted on the head or legs. The differential diagnoses are similar to those for necrotic arachnidism.
Further reading
Cullimore AM, et al. Tiger snake (Notechis scutatus) envenomation in a horse. Aust Vet J 2013;91:381-384.
da Silva PH, et al. Brown spiders and loxoscelism. Toxicon 2004;44:693-709.
Dickinson CE, et al. Rattlesnake venom poisoning in horses: 32 cases (1973-1993). J Am Vet Med Assoc 1996;208:1866-1871.
Fitzgerald KT, et al. Hymenoptera stings. Clin Tech Small Anim Pract 2006;21:194-204.
Friberg CA, Lewis DT. Insect hypersensitivity in small animals. Compend Contin Educ Pract Vet 1998;20:1121-1131.
Langhorn R, et al. Myocardial injury in dogs with snake envenomation and its relation to systemic inflammation. J Vet Emerg Crit Care (San Antonio) 2014;24:174-181.
Lewis N, et al. Mass envenomation of a mare and foal by bees. Aust Vet J 2014;92:141-148.
Peterson ME. Brown spider envenomation. Clin Tech Small Anim Pract 2006;21:191-193.
Rakich PM, et al. Clinical and histologic characterization of cutaneous reactions to stings of the imported fire ant (Solenopsis invicta) in dogs. Vet Pathol 1993;30:555-559.
Sams HH, et al. Necrotic arachnidism. J Am Acad Dermatol 2001;44:561-573.
Thallotoxicosis
The heavy metal thallium is a potent toxin with pharmacologic actions similar to lead and mercury. Thallium salts are odorless, tasteless, colorless, and water soluble. Thallium was used extensively as a rodenticide and insecticide prior to 1963, when its sale to the general public in the United States and some other countries was banned. It continued to be used by government agencies as a pesticide and in various industries, such as the manufacture of optical lenses, jewelry, and scintillation counters. Thallium remains available from chemical supply companies; it has a restricted use as a rodenticide in Europe, and can be used without restrictions in some developing countries. Currently, thallium is used by the semiconductor industry, in optical lenses, and for cardiac perfusion imaging. A recent case of thallium toxicosis in a dog was associated with ingestion of mycoplasma agar plates in which thallium is used as a growth medium. Thallium, purchased from a chemical supply company, was also used in the malicious poisoning of a dog and human family.
Accidental or malicious thallium poisoning is rare and is due to the use of undestroyed supplies of old, but newly exposed, baits. It occurs chiefly in dogs, less often in cats, and is reported in sheep, cattle, and pigs. The LD50 for the dog is 10-15 mg/kg, and the toxin is cumulative. Absorption occurs rapidly from the gastrointestinal and respiratory tracts and skin. The toxin is disseminated widely in the body and is persistent, being very slowly excreted in bile and urine.
The mechanism of toxicity is not fully understood. There are 2 main hypotheses. The first holds that thallium exerts its toxic effect by combining with sulfhydryl groups, a mechanism common to many heavy metals and leading to disruption of mitochondrial respiratory chain enzymes. The second, which is based on the similarity of ionic radii between thallium and potassium, suggests that thallium may replace potassium in many critical biochemical functions, thus acting as a general cellular poison. The toxic effect may be, in part, the result of thallium interacting adversely with derivatives of riboflavin. Thallium can depolarize nerve cell membranes and antagonize effects of calcium on the heart.
The clinical effects depend on the dose and rapidity of administration. Signs of acute thallotoxicosis are evident within 12 hours of exposure and are characterized by severe gastrointestinal irritation and neurologic signs, including motor paralysis. Glossitis, stomatitis, rhinitis, and bronchitis develop. Death by respiratory failure may occur. Animals may survive the acute episode to develop the chronic syndrome or may bypass the acute disease altogether. Cutaneous, renal and neurologic abnormalities, progressive debilitation, and death characterize the chronic syndrome.
The cutaneous lesions develop 7-10 days after ingestion of thallium and principally affect frictional areas. The pattern of skin involvement in cats and dogs is characteristic, beginning at the commissures of the lips or nasal cleft, occasionally on the ear margins, and expanding over the face and head. The mucous membranes are characteristically “brick-red” and may be ulcerated. Lesions also develop on the interdigital skin, footpads, axillae, inguinal areas, perineum, and lateral extensor surfaces. The lesions are marked erythema, scaling, alopecia, exudation, and crusting. The layers of scale-crust exfoliate with attached hairs to leave a raw, oozing surface. The paws often become very swollen. In more chronic cases, thick scales on the footpads resemble “hard pad” disease conventionally associated with canine distemper. In less severely affected animals, ease of depilation may be the only clinical indication of thallium poisoning. The pathogenesis of the alopecia is not fully understood. Although thallium enters the hair, as do other heavy metals, by binding to sulfhydryl groups in the keratin, this is unlikely to be destructive to the hair follicle. Thallium may interfere with the energy metabolism of the rapidly dividing matrix cells of anagen follicles. In experimental intoxication of rats, a rapid decline in the mitotic rate is followed by necrosis of the matrix cells within 48 hours. The follicle passes into an abnormal catagen phase, followed by complete involution (telogen). However, no club attachment is formed, and the hairs are rapidly shed. If the animal survives, hair growth is resumed. Thallium also severely alters the cornification process, and both the surface and external root sheath epithelium demonstrate marked parakeratotic hyperkeratosis.
The microscopic lesions in the skin are dominated by massive, diffuse parakeratotic hyperkeratosis, which affects both surface and external root sheath epithelia. There is accompanying follicular plugging, hypogranulosis, and epidermal hyperplasia (Fig. 6-48 ). Neutrophil exocytosis and spongiform pustules develop in both surface and follicular epithelia. Partial or full-thickness necrosis of the surface epithelium may also occur. The dermal lesions include marked hyperemia, edema, erythrocytic exocytosis and infiltration of neutrophils and mononuclear cells. There may be focal necrosis of sweat and sebaceous glands. Hair follicles are mostly in catagen or telogen. Degenerative changes are noted in anagen follicles.
Figure 6-48.
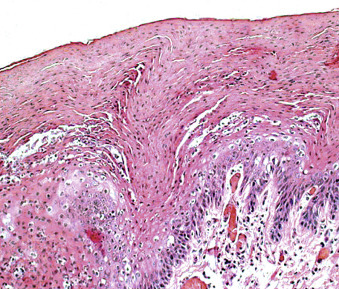
Thallium toxicity in a dog. Marked parakeratosis.
Histologic lesions in other tissues include multifocal necrosis of myocardial and skeletal muscle fibers, nephrosis, pulmonary edema, reticuloendothelial hyperplasia, and lymphoid depletion of spleen and lymph nodes. Secondary bacterial bronchopneumonia may occur as a result of the damage to ciliated epithelia and resultant disturbance of the mucociliary apparatus. Hemorrhagic gastroenteritis occurs in acute thallotoxicosis. Focal suppurative pancreatitis has been described in several animals, but its causal relationship to thallium is not established. Ulcerative esophagitis follows dilation secondary to neuronal damage. Lesions in the central nervous system include neuronal chromatolysis, neuronophagia, and severe edema with little glial reaction. Myelinated peripheral nerves have degenerative lesions, including focal distention of myelin sheaths and swelling and occasional fragmentation of axons.
The differential diagnoses of acute thallium toxicity include other heavy metal toxicoses, infectious and noninfectious causes of hemorrhagic gastroenteritis, and pancreatitis. Differentials for the clinical lesions include superficial necrolytic dermatitis, zinc-responsive dermatosis, generic dog food dermatosis, toxic epidermal necrolysis, mucocutaneous candidiasis, epitheliotropic lymphoma, and autoimmune diseases, such as pemphigus vulgaris and bullous pemphigoid. The microscopic lesions of thallium toxicosis, zinc-responsive dermatosis, and superficial necrolytic dermatitis are similar, and confirmation requires a compatible history and demonstration of thallium in the urine by the Gabriel-Dubin colorimetric assay or in the stomach content, suspected bait, urine, liver, or kidneys by atomic absorption spectroscopy.
Further reading
Arbiser JL, et al. Effects of thallium ion on cellular components of the skin. J Dermatol 1997;24:147-155.
Galvan-Arzate S, Santamaria A. Thallium toxicity. Toxicol Lett 1998;99:1-13.
Mulkey JP, Oehme FW. A review of thallium toxicity. Vet Hum Toxicol 1993;35:445-453.
Puschner B, et al. Thallium toxicosis in a dog consequent to ingestion of mycoplasma agar plates. J Vet Diagn Invest 2012;24:227-230.
Thomas ML, McKeever PJ. Chronic thallium toxicosis in a dog. J Am Anim Hosp Assoc 1993;29:211-215.
Volmer PA, et al. Thallium toxicosis in a Pit Bull Terrier. J Vet Diagn Invest 2006;18:134-137.
Zook BC, et al. Thallium poisoning in cats. J Am Vet Med Assoc 1968;153:285-299.
Arsenic toxicosis
Arsenic is the metal most toxic to the skin and is found as a component of wood preservatives, herbicides, insecticides, insulation materials, paint pigments, feed additives, and some medications, and is a byproduct of some mining activities. It is a water supply contaminant in some parts of Mexico, Argentina, Chile, Taiwan, India, the United Kingdom, and the United States. Safe standards for levels of arsenic in drinking water have not been established. Arsenic is absorbed by the gastrointestinal tract and skin and is excreted in urine, bile, milk, hair, nails, and exfoliated epidermal cells. Its presence in the skin increases the skin's susceptibility to damage by UV light. Chronic arsenic exposure in humans occurs in environmental (water contamination) and industrial settings and is associated with increased incidence of visceral and cutaneous malignancies, Bowen's disease, palmar and solar hyperkeratoses, and cutaneous pigmentary disturbances. The generation of free radicals with resultant nucleic acid damage is suspected to be involved in arsenic-related carcinogenesis. Arsenic may lead to cellular proliferation through increased production of keratinocyte-derived growth factors. Urine, hair, and liver are the tissues of choice for establishing arsenic exposure.
Acute arsenic poisoning is an important toxicosis in domestic animals, particularly cattle and dogs, and is due to sulfhydryl group binding and inhibition of cellular metabolism. Signs and lesions are referable to the gastrointestinal tract, liver, and kidneys. Skin lesions are the result of chronic systemic low-level arsenic exposure or to direct contact. Arsenic is an established low-grade corrosive that produces irritant contact dermatitis. Contact lesions occur in animals sprayed or dipped in a concentrated arsenic solution or in dogs lying on heavily contaminated ground. Lesions include erythema and epidermal necrosis, leading to the formation of nonhealing ulcers. Lesions may affect oral cavity, lips, other mucocutaneous junctions, and the feet. Less is known about the effects of chronic systemic exposure of arsenic on the skin in animals; however, chronic arsenic poisoning in farm animals is associated with ill thrift and a dry, seborrheic, alopecic coat.
Further reading
Ashrafihelan J, et al. Arsenic toxicosis in sheep: the first report from Iran. Interdiscip Toxicol 2013;6:93-98.
Bertin FR, et al. Arsenic toxicosis in cattle: meta-analysis of 156 cases. J Vet Intern Med 2013;27:977-981.
Evinger JV, Blakemore JC. Dermatitis in a dog associated with exposure to an arsenic compound. J Am Vet Med Assoc 1984;184:1281-1282.
Germolec DR, et al. Arsenic enhancement of skin neoplasia by chronic stimulation of growth factors. Am J Pathol 1998;153:1775-1785.
Hughes MF, et al. Arsenic exposure and toxicology: a historical perspective. Toxicol Sci 2011;123:305-332.
Lansdown ABG. Physiological and toxicological changes in the skin resulting from the action and interaction of metal ions. Crit Rev Toxicol 1995;25:397-462.
Pace LW, et al. Acute arsenic toxicosis in five horses. Vet Pathol 1997;34:160-164.
Thomas DJ, et al. The cellular metabolism and systemic toxicity of arsenic. Toxicol Appl Pharmacol 2001;176:127-144.
Mercury toxicosis
Organomercurial toxicosis in domestic animals is associated chiefly with neurologic and renal disorders and is discussed in Vol. 1, Nervous system and Vol. 2, Urinary system, respectively. In chronic poisoning in cattle, skin manifestations, including pustules, ulcers, hyperkeratosis, and alopecia at the tail head are described, but their pathogenesis is poorly understood. Horses ingesting mercury-treated seed grain develop total body alopecia, followed by loss of the long hairs of mane, tail, and forelock. The hooves are not affected, and the cutaneous lesion is mild scaling. Experimental chronic methylmercury intoxication in horses produces exudative dermatitis, but histologic lesions are not described. Local toxic contact dermatitis follows application of mercurial containing counterirritants to the legs in horses.
Further reading
Casteel SW. Metal toxicosis in horses. Vet Clin North Am Equine Pract 2001;17:517-527.
Irving F, Butler DG. Ammoniated mercury toxicity in cattle. Can Vet J 1975;16:260-264.
Seawright AA, et al. Chronic methylmercurialism in a horse. Vet Hum Toxicol 1978;20:6-9.
Cutaneous iodism
Iodides have widespread use as antiseptics, expectorants, intravenous contrast agents, bronchodilators, antithyrotoxicants, and as salt or feed additives. Iodine is readily absorbed from the skin. The majority of reports of adverse effects of iodine occur as hypersensitivity reactions and not toxicoses. Generalized seborrhea sicca is reported in horses and cattle accidentally overdosed with iodine-containing drugs or medicated feed. In experimental toxicosis of calves, the cutaneous lesions were limited to scaly patches without alopecia. Conversely, suspected iodism in a horse produced generalized alopecia, sparing only the face, mane, and tail.
Further reading
Fadok VA, Wild S. Suspected cutaneous iodism in a horse. J Am Vet Med Assoc 1983;10:1104-1106.
Ginn PE, et al. Self-limiting subepidermal bullous disease in a neonatal foal. Vet Dermatol 1998;9:249-256.
Mangkoewidjojo S, et al. Pathologic features of iodide toxicosis in calves. Am J Vet Res 1980;41:1057-1061.
Selenium toxicosis
Selenium is a metalloid that acts as an antioxidant with toxic potential. It has chemical properties similar to sulfur. It is excreted from the body in urine, feces, and sweat and integumentary structures. Experimental studies in rodents suggest that selenium may diminish UV radiation–induced skin damage when applied topically. However, some forms are strong contact irritants and vesiculants. The toxic potential of selenium in the diet varies by the chemical form present, nature of the diet, rate of consumption, and by the species and individual animal. The mechanism by which selenium might exert its effects on the integument is not known, but conceivably, being competitive with sulfur, it modifies the structure of keratin.
Selenium is widely distributed in soils at concentrations ranging from <0.01 parts per million (ppm) to >500 ppm. Areas of high soil concentration are particularly extensive in parts of the United States (Wyoming, Montana, Utah, Colorado, North and South Dakota, Arizona, Kansas, Nebraska) and in western Canada, but also occur in parts of Australia, New Zealand, China, Ireland, Mexico, and Israel, among other countries.
Selenium toxicosis occurs in horses, cattle, sheep, and pigs, chiefly as a result of the ingestion of plants that have accumulated toxic levels of selenium, but occasionally as a result of accidental overdose of selenium supplements. Plants are divisible into seleniferous and nonseleniferous species. Seleniferous plants can selectively concentrate selenium in their foliage and seeds as compared with nonseleniferous species grown under the same conditions. The seleniferous species are subdivided into obligate accumulators, which require high levels of selenium for survival, and facultative accumulators. The former, which include members of the genus Astragalus, Machaeranthera, and Stanleya, may accumulate >1,000 ppm selenium. Because of their high requirement for selenium, they are known as “indicator” species. Facultative or secondary selenium accumulators, such as Aster, Atriplex, Castilleja, and Gutierrezia, take up lesser amounts of selenium. Many nonseleniferous weeds, crop plants, and grasses are capable of passively accumulating selenium if growing on soils with high selenium content. Also, indicator plants increase the availability of selenium to nonseleniferous plants by converting insoluble selenites to soluble selenates and returning these to the soil. Selenium poisoning can occur whenever seleniferous plants are eaten, irrespective of levels of selenium in the soil, and it can occur whenever the levels of water-soluble selenium in the soil are high, irrespective of the botanical composition.
Seleniferous plants are not palatable, and indigenous stock learns to avoid them. Selenium poisoning occurs chiefly in newly introduced or traveling animals and in indigenous animals forced to eat the seleniferous plants in times of scarcity. Clinically, there are acute and chronic syndromes associated with the ingestion of seleniferous plants, such as Astragalus and Oxytropis. Acute toxicity causes severe gastrointestinal and cardiovascular signs, with mortality in some instances approaching 100%. Two different syndromes have been described as chronic selenium poisoning. Blind staggers, characterized by neurologic signs, is probably not due to selenium alone but to other toxic principles in the seleniferous plants. The second syndrome is named alkali disease because it was originally believed that the pH of the selenium-rich soils was a factor in its pathogenesis. Unlike blind staggers, alkali disease is reproducible in ungulates fed sublethal concentrations of selenium. The presence of internal lesions, such as nephrosis, myocardial degeneration, and hepatic fibrosis, in chronically poisoned livestock is not found in experimentally reproduced disease, suggesting that other factors are involved.
Horses and cattle chronically intoxicated with selenium become emaciated and develop partial alopecia and a general roughness of coat. Foals delivered from affected mares may have lesions. Initially, there is loss of the long hairs in the mane, forelock, and tail of horses (leading to the name bobtail disease), and loss of the long tail hairs in cattle. Sheep do not show cutaneous lesions, although, in Australia, fleece shedding has been attributed to selenium toxicity on some properties. Selenium toxicity is also suspected in alopecias of the beard and flanks of goats in the western United States. In all species, lesions commencing at the coronary band may lead to separation and shedding of the hoof or to the formation of dystrophic grooves, cracks, or corrugations that parallel the coronary band, resulting in lameness (Fig. 6-49 ). Lesions take months to develop. Histologic lesions of experimental chronic selenium toxicosis in cattle showed extensive separation of the stratum medium of the hoof with replacement by parakeratotic cellular debris. The germinal epithelium of the hoof wall was disorganized, parakeratotic, and hyperplastic. Hair follicles from the tail were atrophic with dyskeratosis and mild hyperkeratosis.
Figure 6-49.
Selenium toxicosis in a horse. Hoof wall deformed by rings and grooves.
(Courtesy Queensland Department of Agriculture.)
Diagnosis requires the demonstration of compatible clinical signs, progression of lesions, and identification of a dietary source of selenium with a concentration in the air-dried feed sample of >5 ppm selenium. High levels of selenium in the blood (>2 ppm) or integumentary tissues, such as hair, hoofwall, or sole (>10 ppm), should also be present. Individual animals have a variable response to selenium exposure, and some animals with high levels of selenium may not show signs of toxicosis.
Further reading
Davidson-York D, et al. Selenium elimination in pigs after an outbreak of selenium toxicosis. J Vet Diagn Invest 1999;11:352-357.
Davis TZ, et al. Toxicokinetics and pathology of plant-associated acute selenium toxicosis in steers. J Vet Diagn Invest 2012;24:319-327.
Desta B1, et al. Acute selenium toxicosis in polo ponies. J Vet Diagn Invest 2011;23:623-628.
O'Toole D, Raisbeck MF. Pathology of experimentally induced chronic selenosis (alkali disease) in yearling cattle. J Vet Diagn Invest 1995;7:364-373.
Raisbeck MF. Selenosis. Vet Clin North Am Food Anim Pract 2000;16:465-480.
Stowe HD, et al. Selenium toxicosis in feeder pigs. J Am Vet Med Assoc 1992;201:292-295.
Tinggi U. Essentiality and toxicity of selenium and its status in Australia: a review. Toxicol Lett 2003;137:103-110.
Traub-Dargatz JL, Hamar DW. Selenium toxicity in horses. Compend Contin Educ Pract Vet 1986;8:771-776.
Van Kampen KR, James LF. Manifestations of intoxication by selenium accumulating plants. In: Keeler RF, et al., editors. Effects of Poisonous Plants on Livestock. New York: Academic Press; 1978. p. 135-138.
Witte ST, et al. Chronic selenosis in horses fed locally produced alfalfa hay. J Am Vet Med Assoc 1993;202:406-409.
Organochlorine and organobromine toxicoses
Organochlorine and organobromine compounds implicated in toxicities causing, among others, cutaneous lesions, include the highly chlorinated naphthalenes (HCNs), polybrominated biphenyls (PBBs), and dibenzofurans. Polychlorinated biphenyls (PCBs) are the cause of an important industrial dermatitis of humans known as chloracne.
Highly chlorinated naphthalene toxicosis (X-disease, bovine hyperkeratosis), the result of exposure to tetra-, penta-, hexa-, hepta-, or octachloronaphthalenes, is largely of historical interest. HCNs were found to be responsible for high mortality and large economic losses in the cattle industry within the United States, Australia, New Zealand, and Germany during the 1940s and early 1950s. HCN was a common additive in many petroleum products, including those used as lubricants for farm machinery, such as feed pelleting equipment; wood preservatives; roofing paper; and building board. HCNs were a frequent feed contaminant. These chemicals have not been used in lubricants since 1953. Recent reports are the result of animals exposed to dumps with stores of old lubricant or abandoned machinery lubricated years ago with HCN-containing products. Percutaneous exposure produces cutaneous lesions, whereas parenteral exposure results in both cutaneous and visceral lesions. The poison is cumulative, and the disease is chronic. Lesions of HCN toxicity result from interference with the conversion of carotene to vitamin A and resemble the lesions of vitamin A deficiency. The first sign of poisoning is a fall in vitamin A levels in the plasma.
Cattle are the most susceptible species. Initial signs are increased lacrimation and drooling, depression, decreased appetite, and weight loss. Within the first few months, hallmark cutaneous lesions of marked alopecia with nonpruritic, lichenified, deeply fissured plaques of hyperkeratotic scale are evident on the skin of the neck, shoulders and perineum. Lesions gradually generalize, sparing only the legs. Marked involvement of the skin of the medial thighs is characteristic. Horn growth may be delayed. The animal may die before the skin lesions are severe, if exposure is high. Concurrent severe secondary infections with bovine papular stomatitis virus, papilloma virus, or dermatophytes may be present. The histologic lesions are marked hyperkeratosis of surface and follicular epithelia. Internal lesions are the result of hyperplasia and squamous metaplasia of the epithelial lining of ducts and glands of the body, including liver, pancreas, kidneys, and reproductive tract. Bulls may have epididymal enlargement early in the disease process, from hyperplasia and squamous metaplasia of ducts.
Differential diagnoses include other markedly hyperkeratotic dermatopathies, such as zinc or vitamin A deficiency, dermatophilosis, dermatophytosis, or toxicosis caused by other polyhalogenated aromatic compounds. Definitive diagnosis is dependent upon identification of a source of HCN and extraction of the toxin by capillary gas chromatography and mass spectrometry. Vitamin A levels in the plasma and liver are low, but toxicosis cannot be reversed by vitamin A therapy, and the prognosis is poor.
Cutaneous lesions in cats exposed to wood preservatives have been ascribed to chlorinated naphthalene toxicity. The lesions include bilateral alopecia and encrustations on the eyelid and around the nostrils.
Pentachlorophenol (PCP)-contaminated wood shavings used as bedding led to chronic toxicity characterized by a proliferative dermatitis with crusting, scaling, and alopecia accompanied by a multitude of systemic signs, including peripheral edema, bone marrow hypoplasia, liver disease, and wasting in a group of horses. Gross and histologic cutaneous lesions resembled those of HCN toxicity. Wood shavings containing 4 times the maximal allowable levels of PCP/kg were traced to a lumber company using improper processing techniques. Toxicity was attributed to dibenzofuran and chlorinated dibenzo-p-dioxin isomers found as contaminants of the PCP. Contaminants of PCP products include a large group of dioxin isomers with a wide range of toxicity that can vary by species exposed and among animals within the species. PCP compounds are used as antiseptics, disinfectants, herbicides, fungicides, and wood and hide preservatives. The toxicity of the herbicide, Agent Orange, widely sprayed in Vietnam, is attributed to dioxin contaminants. The compounds enter the body via oral, dermal, or respiratory routes. High exposure leads to rapid death because of uncoupling of mitochondrial oxidative phosphorylation. Chronic toxicity is more common. The contaminants in the PCP compounds are thought to bind to aromatic hydrocarbon receptors in the cell nucleus and influence gene expression. The response may be proliferative or suppressive. Elevated levels of the compounds can be demonstrated in the liver and adipose tissue years after exposure, whereas serum levels are cleared quickly. Similar cases of dioxin isomer toxicity have been reported in horses exposed to riding arenas sprayed with contaminated waste oil used for dust control.
Further reading
Carter CD, et al. Tetrachlorodibenzodioxin: an accidental poisoning episode in horse arenas. Science 1975;188:738-740.
Fries GF. The PBB episode in Michigan: an overall appraisal. CRC Crit Rev Toxicol 1985;16:105-156.
Kerkvliet NI, et al. Dioxin intoxication from chronic exposure of horses to pentachlorophenol-contaminated wood shavings. J Am Vet Med Assoc 1992;201:296-302.
Panciera RJ, et al. Bovine hyperkeratosis: historical review and report of an outbreak. Compend Contin Educ Pract Vet 1993;15:1287-1294.
Mimosine toxicosis
Mimosine is a toxic amino acid found as a main constituent in the tropical to subtropical, cultivated leguminous shrubs Mimosa pudica and Leucaena leucocephala (formerly L. glauca). Mimosine and its metabolite, 3-hydroxy-4-(1H)-pyridone (DHP), are toxic. In ruminants, mimosine is a depilatory, whereas DHP is a goitrogen. Poisoning can be acute or chronic and is characterized by alopecia, poor growth, oral ulcerations, and goiter not prevented by iodine supplementation. Toxicity occurs in a number of countries and goes by a variety of local names: jumbey in the West Indies, lamtoro in Indonesia, and koa haole in Hawaii. A variation of animal susceptibility to mimosine toxicity in different parts of the world is due to the geographic distribution of ruminal bacteria capable of degrading DHP. In vitro antemortem assays for detection of DHP-degrading bacteria can be performed on feces or ruminal contents. A group of bacteria, Synergistes jonesii, can be inoculated into the rumen of livestock to prevent toxicity. Mimosine has been shown to reduce DNA synthesis and to block the progression of the cell cycle by chelating iron. DHP prevents iodine binding in the thyroid gland. Mimosine toxicity occurs in horses, cattle, pigs, and sheep and has been experimentally reproduced in cattle and laboratory animals.
Horses appear to be most susceptible and lose their hair, especially the long hair of the mane and tail. In severe cases, there is patchy loss of hair above and below the hocks and knees and on the flanks and neck. Disturbed growth at the coronet and periople may produce dystrophic rings on the hooves. There is loss of condition and weakness that perhaps is attributable to malnutrition rather than to mimosine.
Mimosine has a marked depilatory action on the fleece of sheep. The fleece becomes easily epilated 14 days after a single oral dose of 400-650 mg/kg body weight. DNA synthesis in the wool follicles is reduced. Mimosine toxicity causing depilation in pigs is reported from Indonesia and the Bahamas.
Further reading
Anderson RC. Drought associated poisoning of cattle in South Texas by the high quality forage legume Leucaena leucocephala. Vet Human Toxicol 2001;43:95-96.
Hammond AC. Leucaena toxicosis and its control in ruminants. Review. J Anim Sci 1995;73:1487-1492.
Kulp KS, Vulliet PR. Mimosine blocks cell cycle progression by chelating iron in asynchronous human breast cancer cells. Toxicol Appl Pharmacol 1996;139:356-364.
Mladenov E, Anachkova B. DNA breaks induction by mimosine. Z Naturforsch [C] 2003;58:732-735.
Reis PJ, et al. Fate of mimosine administered orally to sheep and its effectiveness as a defleecing agent. Aust J Biol Sci 1975;28:495-501.
Gangrenous ergotism and fescue toxicosis
These conditions can be considered together because the cutaneous lesions of chronic ergotism caused by Claviceps purpurea and those of poisoning by tall fescue, Festuca arundinacea or F. eliator, are identical.
Ergotism is the oldest known mycotoxicosis. The ergot of Claviceps spp. fungi is a compacted mass of hyphae, the sclerotium, which develops in the seed heads of many species of grasses and cereal grains and completely replaces the ovary. Ergotism is the disease that results from ingestion of toxic alkaloids produced by the fungi. The alkaloids are derivatives of lysergic acid and include ergotamine, ergometrine, and ergotoxine, which is a composite of 3 alkaloids. The quantity and spectrum of alkaloids in the ergots vary considerably with the strain of fungus, type of plant, season of the year, climatic conditions, and other regional factors. The ergots also produce a variety of amines, such as histamine, acetylcholine, and other nitrogenous compounds with physiologic activity.
Of the various pharmacologic effects exerted by the ergot alkaloids, the most important in the pathogenesis of gangrenous ergotism is direct stimulation of adrenergic nerves supplying arteriolar smooth muscle. This produces marked peripheral vasoconstriction. Arteriolar spasm and damage to capillary endothelium leads to thrombosis and ischemic necrosis of tissues.
Gangrenous ergotism caused by C. purpurea is a disease mainly of cattle. It may occur in animals at pasture but is more common in housed animals fed infected grain. Gangrenous ergotism represents the chronic form of intoxication by ergot-producing fungi. Chronic ergotism develops after a week of feeding contaminated grain and begins with acute lameness with redness and swelling of the extremities. The hindlegs are more frequently affected than the forelegs. Lesions seldom extend above the fetlock (Fig. 6-50 ), but ischemic necrosis may extend to the mid-metatarsus. The feet become cold and insensitive, with dry necrosis and a prominent line of separation between viable and dead tissue. The necrotic tissue may slough. Ergotism also causes dry gangrene of the tips of the ears and tail. Gangrenous ergotism has been described in goats feeding on ergot-infected pasture. The toxicosis can be produced experimentally in sheep, but the syndrome is quite different from that in cattle, being characterized by ulceration of the tongue and of the alimentary mucosae. Sows are relatively resistant but may develop agalactia as a result of central inhibition of prolactin secretion.
Figure 6-50.

Ergotism in a bovid. Sharply demarcated ischemic necrosis of digit with foot ready to slough.
(Courtesy C.L. Davis Foundation and National Northeast University.)
Fescue toxicosis has a variable presentation, depending upon the animal species exposed. The most common manifestation, “fescue foot,” is a disease of cattle characterized in the acute form by dry gangrene of the extremities commencing 2 weeks after ingestion of the tall fescue grass, Festuca arundinacea. This perennial grass is the most common pasture plant in the United States and is usually harmless. The endophytic fungus Neotyphodium (Acremonium) coenophialum infects ~75% of fescue pastures and imparts increased resistance of the plant to insects and extreme environmental temperatures. Under certain poorly understood conditions, the endophyte-infected plant is toxic. Fescue foot tends to occur with the onset of colder weather, indicating that low ambient temperatures may contribute to its development. The alkaloids, ergonovine, ergotamine, and N-acetyl loline are responsible for toxicity and act as peripheral vasoconstrictors. The acute syndrome in cattle is virtually identical to ergotism.
A chronic disease in cattle, known as “summer slump,” refers to an increased susceptibility to heat stress seen in certain breeds of cattle in conditions of high environmental temperature combined with intake of endophyte-infected fescue. Cattle have decreased skin temperature and open-mouth breathing, suggesting defective thermoregulation. Experimental intravenous injection of alkaloids found in fescue produced lowered skin temperature, heart rate, and prolactin levels, and elevated blood pressure and respiratory rates in heifers. Ingestion of endophyte-infected fescue in horses does not lead to the visibly evident effects of peripheral vasoconstriction as in cattle, but experimental studies have demonstrated that peripheral vasoconstriction does occur, suggesting exposure could lead to foot or leg problems. The more commonly recognized manifestations of fescue toxicosis in the horse are prolonged gestation, agalactia, thickened placentas, and possible abortion. Abdominal lipomatosis associated with marked necrosis of abdominal fat and severe weight loss occurs in domestic ruminants and some species of wildlife consuming endophyte-infected fescue. A heritable predisposition exists in cattle.
Further reading
Abney KL, et al. Vasoconstrictive effects of tall fescue alkaloids on equine vasculature. J Equine Vet Sci 1993;13:334-340.
Belser-Ehrlich S, et al. Human and cattle ergotism since 1900: symptoms, outbreaks, and regulations. Toxicol Ind Health 2013;29:307-316.
Botha CJ, et al. Gangrenous ergotism in cattle grazing fescue (Festuca elatior L.) in South Africa. J S Afr Vet Assoc 2004;75:45-48.
Browning R, Browning ML. Effect of ergotamine and ergonovine on thermal regulation and cardiovascular function in cattle. J Anim Sci 1997;75:176-181.
Riet-Correa F, et al. Mycotoxicoses of ruminants and horses. J Vet Diagn Invest 2013;25:692-708.
Smith GW, et al. Abdominal fat necrosis in a pygmy goat associated with fescue toxicosis. J Vet Diagn Invest 2004;16:356-359.
Tor-Agbidye J, et al. Correlation of endophyte toxins (ergovaline and lolitrem B) with clinical disease: fescue foot and perennial ryegrass staggers. Vet Hum Toxicol 2001;43:140-146.
Wallace LL, et al. Effects on environmental heat and intake of tall fescue seed infested with Acremonium coenophialum on the acid-base status of young bulls. J Vet Diagn Invest 1996;8:233-237.
Trichothecene toxicoses
Macrocyclic trichothecene toxins produced by the fungus Stachybotrys spp. cause stachybotryotoxicosis. Ulcerative and necrotizing lesions of the skin and mucous membranes have been reported in horses, cattle, sheep, and pigs, chiefly from Russia and Eastern Europe. Initial lesions affect the lips, buccal commissures, and nostrils. Marked edema of the face may follow. Death follows development of hemorrhagic diathesis, enteritis, and septicemia. At autopsy, lesions in addition to the hemorrhagic diathesis include alimentary ulceration, pneumonia, renal infarcts, multifocal hepatic necrosis, and lymphadenitis. In many instances, these lesions may represent secondary mycotic or bacterial involvement.
T-2 toxin is a highly irritant trichothecene mycotoxin from Fusarium molds on grain, and causes cutaneous ulceration when applied locally to the skin of pigs. Experimental feeding of T-2 toxin–contaminated feed, in combination with aflatoxin, induces crusting and ulceration of the lips, snout, buccal commissures, and prepuce. The pathogenesis of the lesion is thought to be contact irritant dermatitis due directly to the T-2 toxin or to a urinary metabolite, HT-2 toxin. In rodent studies, topical T-2 toxin induces a cascade of events that leads to oxidative stress and subsequent apoptosis of keratinocytes, with release of tumor necrosis factor-α and interleukin-1β.
Various other trichothecene mycotoxins are also cutaneous irritants and may cause vomition or feed refusal.
Further reading
Doi K, Uetsuka K. Mechanisms of mycotoxin-induced dermal toxicity and tumorigenesis through oxidative stress-related pathways. J Toxicol Pathol 2014;27:1-10.
Harvey RB. Cutaneous ulceration and necrosis in pigs fed aflatoxin and T-2 toxin containing diets. J Vet Diagn Invest 1990;227-229.
Hintikka EL. Stachybotryotoxicosis in cattle and captive animals: stachybotryotoxicosis in horses: stachybotryotoxicosis in sheep: stachybotryotoxicosis in swine. In: Wyllie TD, Morehouse LG, editors. Mycotoxic Fungi, Mycotoxins and Mycotoxicoses. New York: Dekker.; 1978. p. 152-161, 181-185, 203-207, 268-273.
Le Bars J, Le Bars P. Recent acute and subacute mycotoxicoses recognized in France. Vet Res 1996;27:383-394.
Vetch toxicosis and vetch-like diseases
Hairy vetch (Vicia villosa Roth) is a cultivated legume used as pasture, hay, and silage in most of the United States, and in other countries such as Argentina, Australia, and South Africa. Hairy vetch toxicosis in cattle is seen as 3 unique syndromes: (1) acute neurologic disease and hemolysis, followed by death after consumption of seeds; (2) swelling of the upper body, accompanied by herpetiform eruptions of the oral mucous membranes, respiratory distress, and death after consuming vetch pasture; and (3) a syndrome characterized by dermatitis, conjunctivitis, diarrhea, and granulomatous inflammation of many organs. The third syndrome is the most common form of hairy vetch toxicosis and occurs in cattle and, to a lesser extent, horses after consumption of vetch-containing pastures. The clinical syndrome begins 2 or more weeks after consumption and consists of pruritic dermatitis, diarrhea (possibly bloody), and wasting. Morbidity is low and mortality is high. Holsteins, Angus, and cattle aged 3 years or older are more often affected. Death in cattle occurs approximately 10-20 days after illness begins.
Initial lesions consist of a rough coat with papules and crusts affecting the skin of the udder, teats, escutcheon, and neck, followed by involvement of the trunk, face, and limbs. The skin becomes less pliable, alopecic, and lichenified. Marked pruritus leads to excoriations. At autopsy, yellow nodular infiltrates disrupt the architecture of a wide range of organs, but are most severe in myocardium, kidney, lymph nodes, thyroid, and adrenal glands. The kidney may have radially oriented cortical infiltrates that follow the vasculature. Other affected organs may include the mammary and salivary glands, liver, urinary bladder, meninges, and spleen. Histologically, the infiltrates consist of monocytes, lymphocytes, plasma cells, multinucleated giant cells, and, in the cow, eosinophils. The skin has similar perivascular to diffuse infiltrates, marked hyperkeratosis, and dermal and epidermal edema. This form of the disease has been induced experimentally in an Angus cow that had recovered from vetch toxicosis the previous year. Lesions were evident 11 days after feeding vetch. Death occurred even though vetch was removed from the diet at 12 days. Experimental lesions mirrored those of naturally occurring disease with the additional finding of necrosis of cutaneous apocrine glands.
Other species of Vicia and additional compounds are capable of inducing disease indistinguishable from vetch toxicity.
Pyrexia with dermatitis in dairy cows is a syndrome with similarities to hairy vetch toxicity. It has been reported in the United States, England, Wales, France, and the Netherlands. Friesian dairy cows developed pruritic papular eruptions affecting the head and neck, tail head, and udder. Secondary lesions were the result of self-trauma. In another outbreak, hemorrhages were a prominent clinical sign. The episode in Wales was associated with the introduction of a new silage additive on several farms. The outbreak in the Netherlands was associated with the feeding of di-ureido-isobutane (DUIB) in the seed cake. This condition was reproduced in 2 cows fed a DUIB-containing diet for 1 month. Histologically, the lesions of the Dutch outbreak also resembled those of the putative hairy vetch toxicity. Visceral lesions resembling hairy vetch toxicity occur in dairy cows fed a diet containing citrus pulp; the syndrome resolves after removal of citrus pulp from the diet.
Hairy vetch toxicosis in horses resembles that in cattle, except for the infrequent finding of eosinophils in the infiltrate and lack of heart involvement. Conditions very similar to vetch toxicosis have been reported in horses with no vetch exposure. These cases have been variably referred to as idiopathic granulomatous disease involving the skin, systemic granulomatous disease, generalized granulomatous disease, or equine sarcoidosis. Organ involvement is variable. Skin lesions include scaling, crusting, and alopecia on the face or limbs, and progress to a generalized exfoliative dermatitis. Histologically, the skin has multifocal, sometimes perifollicular to deep dermal nodules of granulomatous inflammation. Sarcoidosis in man has a genetic basis and is thought to represent a hypersensitivity response to a persistent antigen. Equine sarcoidosis is discussed more fully under Miscellaneous skin conditions.
Toxicity from vetch seeds is known to be due to the presence of prussic acid. The cause of the granulomatous diseases listed above remains unclear. Nor is it certain whether they represent one entity or a common tissue reaction to a variety of insults. One proposed pathogenesis is that ingestion of vetch or another substance leads to antigen formation in the form of a hapten or a complete antigen that sensitizes lymphocytes and evokes the cell-mediated response upon repeat exposure. Factors that support this hypothesis are the resemblance of the histologic lesions to a type IV hypersensitivity response, age incidence, low morbidity, genetic influence, and possible need for repeat exposure. Lymphocyte blastogenesis and cutaneous hypersensitivity studies have not substantiated this hypothesis; however, only a few vetch antigens have been studied.
The diagnosis of vetch toxicity or vetch-like disease is a diagnosis by exclusion. It is made after review of the herd history, and character and distribution of the lesions. The combination of lesions is fairly distinctive.
Further reading
Fighera RA, Barros CS. Systemic granulomatous disease in Brazilian cattle grazing pasture containing vetch (Vicia spp). Vet Hum Toxicol 2004;46:62-66.
Green JR, Kleynhans R. Suspected vetch (Vicia benghalensis L) poisoning in a Friesland cow in the Republic of South Africa. J S Afr Vet Assoc 1989;60:109-110.
Iizuka A, et al. An outbreak of systemic granulomatous disease in cows with high milk yields. J Vet Med Sci 2005;67:693-699.
Panciera RJ, et al. Hairy vetch (Vicia villosa Roth) poisoning of cattle, update and experimental induction of disease. J Vet Diagn Invest 1992;4:318-325.
Saunders GK, et al. Suspected citrus pulp toxicosis in dairy cattle. J Vet Diagn Invest 2000;12:269-271.
Wood PR, et al. Granulomatous enteritis and cutaneous arteritis in a horse. J Am Vet Med Assoc 1993;203:1573-1575.
Woods LW, et al. Systemic granulomatous disease in a horse grazing pasture containing vetch (Vicia sp. J Vet Diagn Invest 1992;4:356-360.
Quassinoid toxicosis
Quassinoid compounds, such as neoquassin and quassin found in hardwood trees of the genus Quassia (Simarouba amara) in the family Simaroubaceae, have been reported to be associated with a vesiculobullous dermatitis of the skin around the eyes, nose, ears, anus, and lips of horses. Wood shavings from these plants have been incorporated in bedding, and the outbreaks have occurred in large numbers of exposed horses. Gross lesions develop within the first few days of exposure, and most often resolve within a week. Systemic signs such as anorexia and icterus accompany cutaneous lesions in some cases. Hepatopathy and nephrosis have been reported. Similar symmetrical lesions of the oral mucosa, mucocutaneous junctions, and pressure points have been reported in dogs exposed to Simarouba shavings.
Quassinoids have been shown experimentally to have insecticidal and anthelmintic properties, whereas their derivatives have antitumor, antiulcer, and cytotoxic activity in vitro. The mechanisms leading to toxicity are not known. Definitive diagnosis is dependent upon a compatible history, exclusion of viral diseases such as vesicular stomatitis, and exposure to other toxins, and the positive identification of plants of the Quassia genus in the bedding material.
Further reading
Campagnolo ER, et al. Outbreak of vesicular dermatitis among horses at a Midwestern horse show. J Am Vet Med Assoc 1995;207:211-213.
Declercq J. Suspected wood poisoning caused by Simarouba amara (marupa/caixeta) shavings in two dogs with erosive stomatitis and dermatitis. Vet Dermatol 2004;15:188-193.
Matsumura T. Simarouba poisoning in horses—Japan. Equine Dis Q 2002;10:2.
Actinic Diseases of Skin
The radiant energy of the sun includes components that are potentially harmful to mammalian skin. This radiation is known as actinic radiation, and its acute effect is the well-known sunburn reaction. Photosensitization is essentially an exacerbated form of sunburn, caused by the activation of photodynamic chemicals in the skin by radiation of an appropriate wavelength and is discussed under the heading Photosensitization dermatitis. Photoallergy is distinct from phototoxicity; it occurs when the photoproduct of an exogenous chemical acts as an antigen. Photoallergic reactions require prior sensitization to the drug or chemical and are more clinically diverse. Photoallergies have not been documented conclusively in animals. Skin cancers induced or exacerbated by actinic radiation are considered with Tumors of the epidermis. The terms “actinic” and “solar” are used interchangeably; however, “actinic” is defined as ultraviolet (UV) rays from sunlight and UV lamps, whereas “solar” refers to radiation from the sun.
Direct effect of solar radiation
Solar energy is a form of nonionizing radiation composed of UV light (100-400 nm), visible light (400-700 nm), and infrared light (700 nm to 1 mm) rays. Most of the direct photobiologic reactions in the skin are induced by high-energy light in the ultraviolet radiation UVB range (290-320 nm). Longer wavelengths of 320-400 nm constitute UVA and may augment UVB-mediated damage. The integument is normally protected against the deleterious effects of ultraviolet radiation by the haircoat, the stratum corneum, and melanin pigmentation. The quantity of ozone, smog, altitude, latitude, season of the year, and time of day also strongly influence the amount of UV rays reaching the skin. The greatest potential for solar-induced skin damage occurs at high altitudes and temperate latitudes during mid-summer days, and in thin, lightly pigmented, sparsely haired, sun-exposed skin. An increasing prevalence of sun-induced dermatoses and tumors has been noted in humans, coincident with the depletion of the ozone layer and a consequent increase in the intensity of UV radiation reaching the earth's surface. This trend may also become evident in animals. Potentially, all animals are susceptible to the acute and chronic effects of actinic radiation, but the protection afforded by the haircoat, and, to a lesser extent, stratum corneum and skin pigmentation, is normally sufficient to prevent solar-induced damage. The conditions described below typically affect animals whose anatomic defenses are poor, either by lacking skin pigmentation or hair cover.
UVB radiation stimulates light-absorbing molecules in the skin referred to as chromophores. Chromophores include keratin proteins, melanin, carotene, nucleic acids, peptide bonds, and some amino acids, to name a few. Light absorbed by chromophores results in electron transfers and free radical production. Energy dissipated from electron transfers induces chemical reactions to form altered cell components referred to as photoproducts, which include altered DNA molecules, enzymes, and hydrogen and disulfide bonds within proteins. Nucleoprotein is susceptible to UV radiation damage, resulting in mitotic inhibition and, if extensive enough, cell death. Sublethal damage may promote mutagenesis or carcinogenesis by the formation of thymidine dimers between pyrimidine base pairs of DNA. Pyrimidine dimer repair mechanisms normally correct DNA damage prior to cell replication; however, repeated or extensive damage may lead to failure of repair mechanisms and cell transformation. The “sunburn cell” associated with UV damage is a keratinocyte that has undergone apoptosis. UVB-induced keratinocyte apoptosis is a complex event that involves cytokines such as tumor necrosis factor-α and probable p53-mediated induction of apoptosis in cells sustaining substantial DNA damage. Studies in mice have shown that UVB radiation–induced apoptotic keratinocytes are replaced by hyperproliferative keratinocytes, leading to epidermal hyperplasia, suggesting that apoptosis and hyperplasia are related events. UV light also induces mutations of the p53 tumor suppressor gene in keratinocytes, contributing to a proliferative advantage to mutated cells that is found in solar-induced actinic keratoses and squamous cell carcinomas in humans. These findings indicate that UV radiation can serve as both a tumor initiator and promoter. UV radiation may also alter immunologic reactivity in favor of the growth of the tumor, through the induction of suppressor T cells and possible impairment of natural killer–cell function. UVB radiation exposure reduces the number of Langerhans cells and impairs their antigen-presenting functions. Contact hypersensitivity responses in experimental animals are reduced following UVB irradiation.
Apoptotic keratinocytes, “sunburn cells,” arranged singly or in clusters or bands in the outer stratum spinosum, are a characteristic microscopic feature of acute sun-induced epithelial damage. These may be induced within 30 minutes of sun exposure. Other lesions include spongiosis, vacuolation of keratinocytes, loss of the granular layer, and, in severe burns, vesiculation. Dermal hyperemia and edema are prominent features. In mild lesions, there is a slight increase in mononuclear cells; in severe burns, there is marked vascular damage, erythrocyte extravasation, and neutrophilic exocytosis. The initial lesion of UV irradiation–induced injury consists of transient erythema, probably resulting from a direct heating effect and the photobiologic effects of UVB acting directly on dermal capillaries. The delayed erythema reaction may be due to direct damage to endothelial cells or the release of cytokines from the radiation-damaged keratinocytes. UV radiation has been shown to increase the production of keratinocyte-derived cytokines. UV light also induces adaptive responses in the epidermis, in particular epidermal hyperplasia and alterations in melanin pigmentation. An immediate pigment darkening is due to changes in existing melanin, and the delayed or “tanning” reaction to stimulation of melanogenesis and proliferation of melanocytes. Melanin both absorbs and scatters UV radiation and, being able to trap free radicals, is important in minimizing the deleterious effects of incident photons. Basal keratinocytes with melanin granules forming protective caps over the nucleus have an increased distribution in sun-exposed skin. In chronically sun-damaged skin, pigment distribution can become irregular because of impaired transfer of melanin from melanocytes to keratinocytes, thereby weakening host defenses. Long-term effects of UV irradiation include variable degenerative changes in the dermis (solar elastosis and fibrosis), adnexa (comedones, cysts), and epidermis (solar keratosis). Lesions vary by species and among individuals within the species.
Solar dermatitis, or sunburn, occurs most frequently in cats, dogs, pigs, cows, and goats. The lesions in cats typically affect the tips of the ears, nose, eyelids, and lips of white, blue-eyed animals. The initial lesion is erythema followed by alopecia, scaling, and crusting. The ear tip may curl over. Lesions are exacerbated each summer, often eventuating in malignant transformation into squamous cell carcinoma (Fig. 6-51 ). Primary phototoxicity in swine occurs in white or light-colored pigs. Although any age group may be affected, the condition is most severe in suckling and weaner pigs. Occasionally, severely affected ears may slough. Light-colored goats and cows are also prone to solar dermatitis. The udders are particularly susceptible when does are turned out into strong sunlight after a winter indoors.
Figure 6-51.

Squamous cell carcinoma on the pinna of a white cat, with erythematous, crusted patches, and plaques, likely a progression from solar dermatitis.
Solar dermatitis occurs most often in shorthaired dogs with light pigmentation. Breeds most often affected include Bull Terriers, Whippets, Beagles, and Dalmatians. Lesions are most often present on the ventrolateral abdomen and thorax, lateral flank, hocks, and bridge of nose in nonpigmented skin. Such lesions are probably related to the basking behavior exhibited by the animals. Early lesions of erythema and scaling evolve into thick, lichenified, erythematous, crusted patches and plaques. Hemorrhagic bullae may develop. The most consistent histologic finding in dogs with chronic solar dermatitis is a narrow, hypocellular, pale-staining band of collagen along the dermoepidermal junction. This change may be present prior to clinical signs of actinic dermatitis and may be used as an indicator of solar damage if the history, anatomic site, and breed are supportive. Other changes noted in canine sun-damaged skin include epidermal acanthosis, epitrichial gland ectasia, and follicular keratosis, resulting in follicular cyst formation and possible furunculosis, particularly over pressure points (Fig. 6-52A ). A layer of fibrosis often surrounds cystic follicles. A superficial perivascular mixed infiltrate of lymphocytes, plasma cells, monocytes, neutrophils, and rare eosinophils is usually present. Furunculosis leads to a marked foreign body response. Follicular changes are thought to be due to loss of support of follicles; however, elastin studies in dogs have not demonstrated degeneration of elastin fibers supporting the follicular wall. Advanced lesions may have epidermal dysplasia (Fig. 6-52B) or concurrent UV light–induced neoplasms, such as squamous cell carcinoma, hemangioma, or hemangiosarcoma. It is important to note that UV light–induced neoplasms may arise in skin devoid of other changes suggestive of actinic damage. Actinic comedones may also be present without lesions suggestive of actinic epidermal damage. Differentials are many and include other conditions resulting in comedone formation, acne, various allergies, bacterial or fungal infections, neoplasia, or a primary keratinization disorder. Restriction of lesions to nonpigmented, sparsely haired skin and a history of sun exposure should be helpful in differentiation.
Figure 6-52.
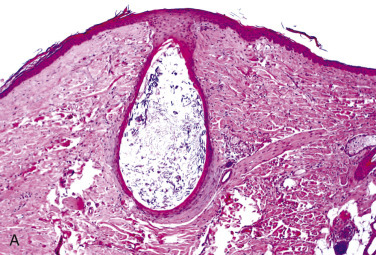
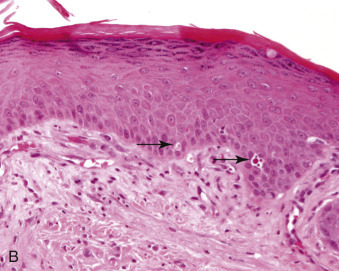
Solar dermatitis. A. Hyperplastic epidermis, superficial layer of pale dermal collagen, and comedone formation. B. A few individually necrotic keratinocytes in the lower epidermis (arrows).
Increased cyclooxygenase-2 (COX-2) expression appears to play an early role in actinic keratosis and squamous cell carcinoma in rodent studies and humans. COX-2 overexpression leads to increased expression of prostaglandin E2 (PGE2). Activation of the COX-2/PGE2 pathway induces cell proliferation, inhibits apoptosis, and promotes angiogenesis and carcinogenesis. COX-2 expression has been shown in feline, canine, and equine cutaneous squamous cell carcinoma (SCC). Furthermore, use of COX-2 inhibitors may have a therapeutic role in the prevention or management of actinic keratosis and SCC.
Solar elastosis, a hallmark of chronic sun exposure in humans, has been described only rarely in dogs, cats, sheep, and horses and essentially represents disorganization of dermal components caused by altered fibroblast function. The lesions usually occur in conjunction with solar radiation–associated neoplasms, particularly SCCs. Solar elastosis appears in H&E-stained sections as scattered or agglomerated, thick, irregular, basophilic degenerate elastic fibers (Fig. 6-53 ). Silver impregnation staining techniques may be needed to demonstrate elastin changes in animals. Solar dermatitis is often present without evidence of elastosis.
Figure 6-53.
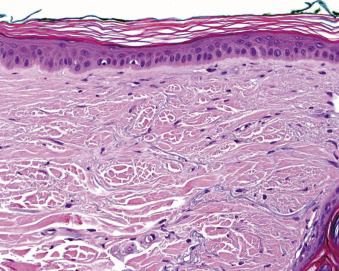
Solar elastosis. The dermis is filled with agglomerated, thick, irregular, basophilic, degenerate elastic fibers.
Solar keratoses, common precancerous skin lesions in humans, occur in cats, dogs, and horses. The conjunctiva of horses with white eyelids is a common site. Histologically, the early lesions have many of the features of sunburn, including epidermal hyperplasia, spongiosis, acute dermal inflammation, and focal necrotic keratinocytes. More chronic lesions show pronounced epidermal hyperplasia with dysplasia, orthokeratotic and parakeratotic hyperkeratosis, perivascular mononuclear cell infiltrates, and dermal scarring, but seldom develop significant solar elastosis, as typifies human solar keratoses. Lesions frequently progress to invasive SCC. Solar keratoses may also develop cutaneous horns.
Further reading
Almeida EM, et al. Photodamage in feline skin: clinical and histomorphometric analysis. Vet Pathol 2008;45:327-335.
Baba T, et al. The study of ultraviolet B-induced apoptosis in cultured mouse keratinocytes and in mouse skin. J Dermatol Sci 1996;12:18-23.
Bardagí M, et al. Immunohistochemical detection of COX-2 in feline and canine actinic keratoses and cutaneous squamous cell carcinoma. J Comp Pathol 2012;146:11-77.
Campbell GA, et al. Solar elastosis with squamous cell carcinoma in two horses. Vet Pathol 1987;24:463-464.
Frank LA, et al. Distribution and appearance of elastic fibers in the dermis of clinically normal dogs and dogs with solar dermatitis and other dermatoses. Am J Vet Res 1996;57:178-181.
Gross TL, et al. Hyperplastic diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 148-151.
Hargis AM. Actinic keratosis and squamous cell carcinoma. J Small Anim Dermatol Pract 2009;2:12-24.
Kimura T, Kunio D. Responses of the skin over the dorsum to sunlight in hairless descendants of Mexican hairless dogs. Am J Vet Res 1994;55:199-203.
Leffell DJ. The scientific basis of skin cancer. J Am Acad Dermatol 2000;42(1 Pt 2):18-22.
Miyauchi-Hashimoto H, et al. Ultraviolet radiation-induced suppression of natural killer cell activity is enhanced in xeroderma pigmentosum group A (XPA) model mice. J Invest Dermatol 1999;12:965-970.
Montagna W, et al. Histology of sun-damaged human skin. J Am Acad Dermatol 1989;21:907-918.
Ouhtit A, et al. Temporal events in skin injury and the early adaptive responses in ultraviolet-irradiated mouse skin. Am J Pathol 2000;156:201-207.
Ziegler A, et al. Sunburn and p53 in the onset of skin cancer. Nature 1994;372:773-776.
Photosensitization dermatitis
Photosensitization dermatitis occurs in animals when photodynamic or fluorescent pigments are deposited in sunlight-exposed skin. Photodynamic pigments absorb UV light or visible light in the action spectrum and convert it to light of a longer wavelength, usually beyond the UVB range. The energy from the absorbed light leads to tissue injury by reacting directly with molecular oxygen, producing reactive oxygen intermediates, such as superoxide anion, singlet oxygen, and hydroxyl radical. Oxygen free radicals may also be formed indirectly, as the result of calcium-dependent, protease-mediated activation of xanthine-oxidase in the skin. Release of reactive oxygen species initiates chain reactions that lead to mast cell degranulation and damage to cell membranes, nucleic acids, proteins and subcellular organelles, particularly lysosomes and mitochondria.
The photodynamic agent usually reaches the skin via the systemic circulation, although percutaneous absorption of some photodynamic agents can cause local contact photosensitization. The agent may originate externally, or it may be an endogenous substance that has accumulated to an abnormal degree as a result of metabolic dysfunction. Sources include plant pigments and drugs or, in the case of metabolic dysfunction, the byproducts of hemoglobin metabolism or chlorophyll degradation products. The 3 categories of photosensitization are classified according to the source of the agents.
-
•
In type I, or primary, photosensitization, the animal ingests plants or drugs containing photoreactive substances that are deposited in the skin. Most exogenous sources of photoreactive pigments are found in plants, and therefore foraging animals, such as horses, sheep, cattle, and goats, are most frequently affected.
-
•
In type II photosensitization, an inherent inability to properly metabolize heme pigments necessary for erythrocyte production leads to the build-up of the photoreactive pigments, hematoporphyrins.
-
•
An abnormal build-up of phylloerythrin, a degradation product of chlorophyll, induces type III photosensitization. This is known also as hepatogenous photosensitization because it depends upon the failure of a damaged or immature liver to eliminate phylloerythrin. Type III photosensitization occurs most often in animals ingesting large amounts of green forage.
-
•
A fourth group contains those examples of photosensitization for which the pathogenesis is presently undetermined.
The gross lesions are similar for all forms of photosensitization. They occur on those areas of the body most exposed to sunlight and that lack protective fleece, haircoat, or skin pigmentation. In cattle, any area of light-colored skin is susceptible. This is best demonstrated in broken-colored animals such as Holsteins, in which the white skin is affected, but the black is spared. The relatively hairless skin of the teats, udder, perineum, and muzzle is also affected. The ventral surface of the tongue is frequently affected in cattle if constantly exposed during licking. In sheep, the susceptible sites are the ears, eyelids, face, muzzle, and coronets, although the back may be affected in animals with an open fleece or that have been shorn closely. The udders and teats of dairy goats are predisposed. In horses, lesions are most common on the face, perineum, and distal extremities but may affect any white skin. Lesions in pigs are uncommon, and have a predilection for the ears, eyelids, udder, and back. Photosensitization is rare in dogs and cats, and causative agents remain obscure.
The initial reaction in photosensitization is erythema, followed by edema, which is more prominent in sheep than in cattle. The very marked edema of the ears in sheep causes them to droop, and swelling of the muzzle may cause dyspnea. The disease in sheep is appropriately known as “bighead” or geeldikkop, a South African term meaning “thick, yellow head”; the equivalent term in New Zealand is “facial eczema.” The lesions are intensely pruritic, causing rubbing, scratching, and kicking at affected parts. Vesicles or bullae may develop. There is marked exudation and extensive necrosis. Affected skin becomes dry and sloughs in desiccated sheets (Fig. 6-54 ). Necrosis is frequently seen on the upper surfaces of the ears of sheep; the tips typically curl upward as a result of mummification or may slough entirely. There is swelling of the eyelids and excessive lacrimation. Among the more obscure manifestations of photosensitization is the convulsive reaction of some sheep and cattle, photosensitized by ingestion of St. John's wort, on contact with cold water. Icterus typically is associated with hepatogenous photosensitization, but hepatogenous photosensitization may occur in its absence. Economic losses in livestock can be severe due to damaged hides, weight loss, fly strikes, secondary infections, and reluctance of animals to let the young nurse damaged udders. In severe episodes of photosensitization, animals may die. This is more often the result of concomitant damage to other organs, particularly the liver, than to cutaneous damage alone. Injury to erythrocytes in cutaneous circulation may produce severe hemolysis.
Figure 6-54.

Photosensitization in a horse. Note necrosis and sloughing of skin from white areas of the face.
Histologic lesions mirror the gross lesions with coagulative necrosis of the epidermis and possibly the follicular epithelium, adnexal glands, and superficial dermis. Subepidermal clefts or vesicles form, and the dermis is edematous. Endothelial cells of the superficial, mid, and occasionally deep dermal vessels are often swollen or necrotic. Fibrinoid degeneration of vessel walls and thrombosis may be present. Initially, inflammation is sparse, but soon the lesions are infiltrated by neutrophils. Secondary bacterial colonization is common.
Differential diagnosis should include other vesicular or necrotizing dermatopathies, including chemical or thermal burns. Establishing the diagnosis is dependent upon anatomic distribution of lesions in nonpigmented, poorly haired, sun-exposed regions. Lesions limited to areas of contact, such as the extremities, ventrum, or muzzle, suggests the presence of a contact photosensitizing agent. Multiple affected animals in a herd suggest exposure to a photosensitizing agent rather than a photoallergic reaction. Types I, II, and III photosensitivities can be differentiated by signalment and concurrent clinical signs, such as evidence of liver disease combined with examination of pastures and feedstuffs, and investigating photodynamic drug or chemical exposure. The Candida albicans inhibition assay is a simple, inexpensive, quantitative, and relatively rapid assay for screening plants and feedstuffs for potential primary contact or systemic photosensitizers. The test does not detect all phototoxins. Thin-layer chromatography techniques may be useful in identifying phototoxic compounds. Analysis of suspect vegetation for the identification and quantification of fungal spores may be needed to establish fungal organisms and associated mycotoxins as contributing factors.
Primary photosensitization (type I photosensitization)
Plants are the most common cause of primary photosensitization; hence herbivores are most commonly affected. Additional sources include mycotoxins, molds, chemicals, and drugs. The majority of photosensitizing plants contain pigments belonging to either the helianthrone or furocoumarin family of pigments.
The helianthrones include the red fluorescent pigments, hypericin, and fagopyrin. Some of the most commonly implicated plants include St. John's wort (Hypericum perforatum) and buckwheat (Fagopyrum spp.), and the resulting diseases are referred to as hypericism and fagopyrism, respectively. Photosensitization induced by St. John's wort affects horses, cattle, sheep, and goats. Hypericin is present at all stages of plant growth but significant amounts are consumed by livestock only when the plant is prolific or other feed is scarce. Other related plants that can lead to hypericism include goatweed, Tipton weed, amber, cammock, and Klamath weed. Photosensitization induced by buckwheat affects sheep, pigs, cattle, goats, and horses.
The furocoumarin family of pigments contains the photodynamic agents, psoralens. Photosensitization occurs in cattle, sheep, white chickens, and ducks as a result of ingestion of plants such as spring parsley (Cymopterus watsonii), bishop's weed (Ammi majus), and Dutchman's breeches (Thamnosma texana). The furocoumarins differ from the helianthrone-photosensitizing pigments by inducing, additionally, corneal edema and keratoconjunctivitis. Primary photodermatitis of pigs in Argentina occurred after consumption of feed contaminated with Ammi majus seeds containing the furocoumarin xanthotoxin. Furocoumarins have also been documented to form phytoallexins in fungus-infected parsnips (Pastinaca sativa) and celery (Apium graveolens), leading to phytophotocontact dermatitis. Psoralens adsorbed onto the skin react with UV light. These have been associated with phytophotocontact dermatitis in pigs in New Zealand. Lesions were vesicular, affecting only the dorsal aspect of the snout. Rubbing the snouts and feet of white pigs with the leaves of the fungus-infected celery and parsnips before exposing the areas to UV light reproduced the lesions. Cymopterus watsoni causes phytophotodermatitis in sheep in Utah and Nevada. Lesions principally affected the nonwooled areas, such as the muzzle, lips, and udder. High lamb mortality may be incurred from mismothering. Contact photodermatitis suspected to be caused by giant hogweed (Heracleum mantegazzianum) occurred in dogs. Giant hogweed contains psoralens and has been documented to cause photodermatitis in man, ducks, and goats.
Texas cattle and deer develop primary photosensitization after consuming moldy leaves of Cooperia pedunculata. In addition to skin lesions, keratitis occurs frequently and may lead to blindness.
Ingestion of alsike clover (Trifolium hybridum), also known as red clover hay, results in a primary photodermatitis referred to as trifoliosis in cattle, sheep, hogs, and some horses. Trifoliosis has been reported in the United States, Canada, Australia, and England. A second syndrome, referred to as alsike clover poisoning, is characterized by hepatic dysfunction and photodermatitis and has only been reported in the horse. The toxic mechanism is not known but is thought to be due to a toxin within the plant itself or to the presence of a mycotoxin. The variable presentations are speculated to be related to seasonal changes, stage of plant growth, and soil and environmental conditions.
A condition clinically and histologically compatible with a primary photodermatitis occurred in 12 of 30 Harrier Hounds in a kennel in New Zealand. Lesions were limited to the nonpigmented, sun-exposed skin of the tricolored hounds and resolved within a short period of time with supportive care. The hounds were fed a diet of horse and cattle meat. Although an ingested compound was suspected as the cause, no phototoxin could be identified. Similar cases have been reported in Foxhounds in England and Border Collie dogs in New Zealand. Photosensitization has been reported in a cat receiving clofazimine for the treatment of feline leprosy.
Phenothiazine photosensitization is characterized by typical cutaneous lesions and in ruminants by the additional lesions of corneal edema and keratoconjunctivitis. The secretion of the ruminal metabolite, phenothiazine sulfoxide, in tears and aqueous humor, has explained the unusual location of the lesions. Phenothiazine photosensitization occurs most commonly in calves but also in sheep, swine, and birds. Pigs develop cutaneous lesions more frequently than sheep or cattle, probably because the activating radiation is more able to penetrate the integument. The greater susceptibility of calves has been ascribed to a relatively inefficient conversion of the photodynamic sulfoxide metabolite back to phenothiazine in the liver. This conversion depends on effective mixed-function oxidase enzyme activity in the liver.
Photosensitization resulting from defective pigment synthesis (type II photosensitization)
Photosensitization resulting from endogenous pigment accumulation occurs because of a congenital enzyme deficiency causing abnormal heme synthesis, with the resultant blood and tissue accumulation of photodynamic agents, such as uroporphyrin I, coproporphyrin I, and protoporphyrin III.
Bovine congenital hematopoietic porphyria is the result of a deficiency in uroporphyrinogen III cosynthetase, a key enzyme in heme biosynthesis. The condition is inherited as a simple recessive trait affecting many breeds, including Shorthorn, Ayrshire, Holstein, and Jamaican cattle. It has also been reported in crossbred cattle. The disease is known as “osteohemochromatosis” and “pink tooth,” both suggested by the red-brown coloration of porphyrin pigments in dentin and bone. The pigment is also deposited in other tissues, but the discoloration may be obvious only in lungs, spleen, and kidney, in which it is deposited in the interstitial tissue and tubular epithelium.
The pigments are excreted in the urine; hence the alternative names “porphyrinuria” and “hematoporphyrinuria.” Affected urine is amber to brown, darkens on exposure to light, and fluoresces bright red on exposure to UV radiation. Affected teeth and bones also fluoresce. The anemia of bovine congenital erythropoietic porphyria is discussed in Vol. 3, Hematopoietic system.
The cutaneous lesions result from the photodynamic properties of the accumulated porphyrins, in particular the uroporphyrins that absorb UVA radiation. Reactive oxygen species directly induced by the porphyrins or, possibly, via activation of xanthine oxidase in the skin are responsible for the cell membrane damage. The gross cutaneous lesions are typical of photosensitization. The microscopic lesions closely resemble those of erythropoietic porphyrias in man. The chief lesions are subepidermal clefts, hyalinization of dermal capillary walls, and a minimal infiltrate of inflammatory cells. The basement membrane zone lines the base of the subepidermal cleft, in some instances covering small projections of dermal papillae (festoons). Festoons are a more prominent feature of the human lesion because dermal papillae are better developed in human skin.
Bovine erythropoietic protoporphyria is inherited as a recessive trait in Limousin cattle in the United States. It differs from bovine congenital porphyria in that photodermatitis is the sole clinical manifestation of the disease. Animals do not have discolored teeth, anemia, or urine porphyrin excretion. The enzyme defect is a deficiency of ferrochelatase, which allows protoporphyrin IX to accumulate in blood and tissues. Heterozygotes have reduced (50%) ferrochelatase activity and are clinically normal.
Porphyria of swine is inherited as a dominant characteristic. Although it mimics certain aspects of bovine erythropoietic porphyria, photosensitization does not occur, even in white-skinned animals. The defect in porcine porphyria is not known.
Photosensitization occurs in Siamese cats with excessive accumulation of uroporphyrinogen I, coproporphyrinogen I, and protoporphyrins in blood, urine, feces, and tissues. The defect is presumably a deficiency of uroporphyrinogen cosynthetase III, as has been established in humans and cattle.
Hepatogenous photosensitization (type III photosensitization)
The most common form of photosensitization in domestic animals occurs in conjunction with primary hepatocellular damage or, less commonly, bile duct obstruction and is due to impaired capacity of the liver to excrete the potent photodynamic agent, phylloerythrin. Phylloerythrin is a chlorophyll catabolite formed by microbial action in the intestinal tract and transported to the liver via the portal circulation. Hepatocytes assimilate the phylloerythrin and excrete it into the bile. One of the earliest signs of liver cell damage is a reduced ability to transport and excrete phylloerythrin. Mild renal tubular damage caused by some toxins may further inhibit the excretion of phylloerythrin. The circulating phylloerythrin accumulates in tissues, including the skin. Photodermatitis occurs provided the animal is on a chlorophyll-rich diet and is exposed to sufficient solar radiation of the appropriate wavelength. High ambient solar radiation and lack of shade are contributing factors. Photosensitization tends to occur most often when the hepatic damage is generalized, even if mild. Severe focal necrotizing lesions of the liver generally do not cause photosensitization because there is enough hepatic reserve to remove the phylloerythrin from the circulation. The cause of hepatic damage may be a plant toxin, mycotoxin, infectious agent, or chemical.
Toxic plants and mycotoxins account for most cases of hepatogenous photosensitization. A few of the many plants implicated in hepatotoxic photosensitization include lantana (Lantana camara), bog asphodel (Narthecium ossifragum), Tribulus terrestris, Agave lecheguilla, Nolina texana, Cymadothea trifolii–infested clover, Trifolium hybridum (“alsike clover poisoning”), and Panicum spp. grasses, such as kleingrass (Panicum coloratum). Kleingrass is a perennial grass forage crop with a toxic principle suspected to be a saponin. Cases of kleingrass induced–photosensitization are sporadic, potentially related to environmental conditions and have been reported in Australia, Africa, and Texas. Some plants work in combination; black sagebrush appears to precondition sheep to photosensitization caused ultimately by Tetradymia spp.
A number of reports of hepatogenous photosensitization in livestock cite a variety of common forage crops, such as alfalfa hay or silage, winter wheat, Bermuda grass pasture, crab grass, oat stubble, or various clover pastures. In the majority of cases, the toxicity was preceded by unusual climatic conditions of drought, increased rainfall, or temperature variations. In many cases, a specific toxic compound cannot be identified. A plausible explanation is the establishment of optimum conditions for the production of mycotoxins, hepatotoxins, or photodynamic agents in the damaged plant material.
Forages containing the mycotoxin sporidesmin, from spores of Pithomyces chartarum, cause facial eczema, an economically important hepatogenous photosensitization of sheep and cattle in Australia, New Zealand, South Africa, and the northwestern United States. Geeldikkop, a disease characterized by hepatogenous photosensitization, is associated with extensive losses among sheep and goats in South Africa. A hepatogenous photosensitization, secondary to a presumed genetic defect in phylloerythrin transport, has been reported in Corriedale lambs.
Hepatic dicrocoeliosis has been identified as a probable cause of photosensitization affecting a group of 14-month-old ewe lambs in Scotland. Hepatogenous photosensitization is discussed in more detail in Vol. 2, Liver and biliary system.
Further reading
Ames T, et al. Secondary photosensitivity in horses eating Cymadothea trifolii infested clover. Proc Am Assoc Vet Lab Diagn 1994;37:45.
Athar M, et al. A novel mechanism for the generation of superoxide anions in hematoporphyrin derivative-mediated cutaneous photosensitization. J Clin Invest 1989;83:1137-1143.
Bennett S. Photosensitization induced by clofazimine in a cat. Aust Vet J 2007;85:375-380.
Betty RC, Trikojus VM. Hypericin and a non-fluorescent photosensitive pigment from St. John's wort (Hypericum perforatum). Aust J Exp Biol Med Sci 1943;21:175-182.
Binns W, et al. Cymopterus watsonii: a photosensitizing plant for sheep. Vet Med Small Anim Clin 1964;59:375-379.
Campbell WM, et al. Photodynamic chlorophyll a metabolites, including phytoporphyrin (phylloerythrin), in the blood of photosensitive livestock: overview and measurement. N Z Vet J 2010;58:146-154.
Casteel SW, et al. Photosensitization outbreak in Shorthorn calves in Missouri. J Vet Diagn Invest 1991;3:180-182.
Colon JL, et al. Hepatic dysfunction and photodermatitis secondary to alsike clover poisoning. Compend Contin Educ Pract Vet 1996;18:1022-1026.
Cornelius CE, et al. Hepatic pigmentation with photosensitivity. A syndrome in Corriedale sheep resembling Dubin-Johnson syndrome in man. J Am Vet Med Assoc 1965;146:709-713.
Cornick JL, et al. Kleingrass-associated hepatotoxicosis in horses. J Am Vet Med Assoc 1988;193:932-935.
De Vries H, et al. Photochemical reactions of quindoxin, olaquindox, carbadox and cyadox with protein, indicating photoallergic properties. Toxicol 1990;63:85-95.
Dickie CW, Berryman JR. Polioencephalomalacia and photosensitization associated with Kochia scoparia consumption in range cattle. J Am Vet Med Assoc 1979;175:463-465.
Dollahite JW, et al. Photosensitization in cattle and sheep caused by feeding Ammi majus (greater Ammi; bishop's weed). Am J Vet Res 1978;39:193-197.
Dolowy WC. Giant hogweed photodermatitis in two dogs in Bellevue, Washington. J Am Vet Med Assoc 1996;209:722.
Enzie FD, Whitmore GE. Photosensitization keratitis in young goats following treatment with phenothiazine. J Am Vet Med Assoc 1953;123:237-238.
Fairley RA, Mackenzie IS. Photosensitivity in a kennel of harrier hounds. Vet Dermatol 1994;5:1-7.
Glastonbury JRW, Boal GK. Geeldikkop in goats. Aust Vet J 1985;62:62.
Hansen DE, et al. Photosensitization associated with exposure to Pithomyces chartarum in lambs. J Am Vet Med Assoc 1994;204:1668-1671.
House JK, et al. Primary photosensitization related to ingestion of alfalfa silage by cattle. J Am Vet Med Assoc 1996;209:1604-1607.
Laksevela B, Dishington IW. Bog asphodel (Northecium ossifragum) as a cause of photosensitization of lambs in Norway. Vet Rec 1983;112:375-378.
Lopez TA, et al. Ergotism and photosensitization in swine produced by the combined ingestion of Claviceps purpurea sclerotia and Ammi majus seeds. J Vet Diagn Invest 1997;9:68-71.
Montgomery JF, et al. A vesiculobullous disease in pigs resembling foot and mouth disease. II. Experimental reproduction of the lesion. N Z Vet J 1987;35:27-30.
Morison WL, et al. Photoimmunology. Arch Dermatol 1979;115:350-355.
Oertli EH, et al. Phototoxic effect of Thamnosma texana (Dutchman's breeches) in sheep. Am J Vet Res 1983;44:1126-1129.
Pearson EG. Photosensitivity in horses. Compend Contin Educ Pract Vet 1996;18:1026-1029.
Quinn JC, et al. Secondary plant products causing photosensitization in grazing herbivores: their structure, activity and regulation. Int J Mol Sci 2014;15:1441-1465.
Riet-Correa F, et al. Mycotoxicoses of ruminants and horses. J Vet Diagn Invest 2013;25:692-708.
Rowe LD. Photosensitization problems in livestock. Vet Clin N Am 1989;5:301-323.
Sargison ND, et al. Hepatogenous photosensitisation in Scottish sheep casued by Dicrocoelium dendriticum. Vet Parasitol 2012;189:233-237.
Sassa S, et al. Accumulation of protoporphyria IX from D-aminolevulinic acid in bovine skin fibroblasts with hereditary erythropoietic protoporphyria. J Exp Med 1981;153:1094-1101.
Scott DW, et al. Dermatohistopathologic changes in bovine congenital porphyria. Cornell Vet 1979;69:145-158.
With TK. A short history of porphyrins and the porphyrias. Int J Biochem 1980;11:189-200.
With TK. Porphyria in animals. Clin Hematol 1980;9:345-370.
Witte ST, Curry SL. Hepatogenous photosensitization in cattle fed a grass hay. J Vet Diagn Invest 1993;5:133-136.
Yamashita C, et al. Congenital porphyria in swine. Nippon Juigaku Zasshi 1980;42:353-359.
Photoaggravated dermatoses
In humans, several autoimmune dermatoses are exacerbated by exposure to UV light. These include pemphigus, lupus erythematosus, and bullous pemphigoid. A similar relationship has been proposed in the analogous canine diseases.
A poorly understood disease in the horse, photoactivated vasculitis affects only the white-haired extremities. The pathogenesis is not currently known. An immune-mediated vasculitis, in which immune complexes may be acting as photodynamic agents has been proposed. Percutaneous absorption of initiating agents has not been ruled out. Affected horses have normal liver function and no known exposure to photosensitizing compounds. In addition, lesions may be restricted to one white extremity, other white areas on the horse are unaffected, and the lesions do not always regress with cessation of exposure to sunlight, all indicating the lesions are not a form of photosensitization. The lesions often affect the heels and must be differentiated from the other manifestations of the “greasy heel” complex. The acute lesions are well demarcated, erythematous, oozing, and crusted in lesional white skin; erosion and ulceration may occur, and the affected limb may be edematous and painful. The lesions tend to occur on the lateral and medial aspects of unpigmented hindlegs. The chronic lesions are hyperkeratotic plaques. Histologically, there is dermal edema, vascular dilation and intramural inflammatory cells, leukocytoclasia with nuclear dust, microhemorrhages, and thickening of the vessel wall of the small superficial, mid, and deep dermal vessels. Thrombi may be seen occasionally. The epidermis may be eroded or ulcerated but undergoes papillary hyperplasia over time.
Further reading
Psalla D, et al. Equine pastern vasculitis: a clinical and histopathological study. Vet J 2013;198:524-530.
Stannard AA. Photoactivated vasculitis. In: Robinson NE, editor. Current Therapy in Equine Medicine II. Philadelphia: WB Saunders; 1987. p. 647.
von Tscharner C, et al. Stannard's illustrated equine dermatology notes. Vet Dermatol 2000;11:161-215.
White SD, et al. Cutaneous vasculitis in equines: a retrospective study of 72 cases. Vet Dermatol 2009;20:600-606.
Nutritional Diseases of Skin
The elasticity of the skin, the orderly maturation of the epidermis, and the quality and luster of the horny appendages are an indication of the state of the health of the animal as a whole. This applies equally to nutritional diseases and to diseases of other causes. Many systemic diseases result in cutaneous changes. The general metabolic transformations that take place in the skin are not qualitatively different from those in other tissues, but there are some quantitative differences, such as the high requirements and turnover of sulfur-containing amino acids in the elaboration of keratin. In most metabolic disturbances and deficiencies of essential nutrients, whether from dietary lack, malabsorption, the action of antimetabolites, or the body's inability to properly absorb or use nutrients, changes will be reflected in the skin. The molecular basis for these skin lesions is, however, poorly understood. There are only a few syndromes that occur naturally and are sufficiently clearly defined to warrant discussion here. A larger number can be produced experimentally. Cutaneous manifestations of systemic disease not known to be a result of a nutritional derangement are discussed in other, more appropriate sections of this chapter, such as Endocrine diseases of skin and Cutaneous paraneoplastic syndromes.
Protein-calorie deficiency
Starvation or protein-calorie malnutrition results in changes in the skin, the first being the disappearance of subcutaneous fat. Even though water intake may not be restricted, there is reduced hydration of the connective tissues of the subcutis and dermis, and the skin wrinkles and loses its elasticity. As hair is 95% protein, hair growth and keratinization can require up to 25-30% of an animal's daily protein requirement. Protein deficiencies are rare but can occur in cats fed primarily food formulated for dogs, in young dogs fed a low-protein diet, or in animals with increased nutrient requirements.
An early sign of starvation is the development of a dull, dry, and often brittle haircoat. Hypotrichosis develops as a thinning of the hair rather than baldness, and seasonal shedding may cease or be prolonged. Lesions may be symmetrical on the head and trunk and spread to the limbs. The skin may atrophy, or hyperkeratosis, hyperpigmentation, and possibly loss of hair pigmentation develop. The histopathologic findings in the skin may mimic an endocrinopathy, with severe epidermal and adnexal atrophy, orthokeratotic hyperkeratosis, and telogenization of hair follicles. In pigs, the skin often becomes hyperkeratotic and assumes a dirty, dry appearance, and the hair becomes long and shaggy. The skin of a malnourished animal has an increased susceptibility to bacterial infection and parasitic infestations and their effects. Under-nutrition of the pregnant ewe, between 115-135 days of gestation, decreases the number of secondary wool follicles in the developing fetus. Most experimental work on the effects of nutrition on hair growth has been performed in sheep, the purpose being either to improve wool production or to investigate chemical methods of shearing. Changing sheep from a low-protein to a high-protein diet led to a 33% increase in fleece production, attributed mostly to an increase in the rate of mitosis in the hair bulb. Specific amino acid deficiencies have been investigated as potential replacements for mechanical shearing as wool production is highly dependent upon levels of certain amino acids, specifically cysteine.
The effects of starvation on other organs such as liver, pancreas, bone, and bone marrow are discussed elsewhere.
Fatty acid deficiency
Fatty acid deficiency may occur in all domestic species in association with general dietary deficiency, malabsorption, or liver disease. Deficiencies may be evident in animals when the fat has either leached from a diet, has become rancid from improper or prolonged storage, or when the diet was formulated with low fat content to save cost. Animals on specially formulated low-fat diets for therapeutic reasons may develop signs of fatty acid deficiency and require specific types of supplementation. Animals on antioxidant-deficient diets may also develop signs of fatty acid deficiency. Cutaneous lesions take months to develop and begin with diffuse scaling, loss of haircoat sheen, and alopecia. The scaliness is initially dry but over months progresses to an oily, often pruritic stage. Otitis externa may be an accompanying lesion, and the skin is susceptible to secondary bacterial and yeast infection. Histologic lesions include epidermal hyperplasia, orthokeratotic or parakeratotic hyperkeratosis, and hypergranulosis. The pathologic mechanisms underlying the epidermal hyperproliferation are not well understood. Experimental studies demonstrated an increase in epidermal DNA synthesis and a decrease in prostaglandin E and F levels in the skin of essential fatty acid–deficient mice. The lower prostaglandin levels likely reflect a lack of precursor arachidonic acid. Deficiency of prostaglandin E2 could influence epidermal cell kinetics through its effect on ratios of cyclic AMP to guanosine monophosphate (GMP). Supplementation of animal diets with balanced omega-6 and omega-3 fatty acids is thought to modulate arachidonic acid metabolism and subsequent production of leukotrienes and prostaglandins that, in turn, may influence epidermal turnover kinetics and the inflammatory response.
A seborrheic dermatosis in cats, characterized by dry scaly skin and alopecia, is responsive to fatty acid supplementation but is not likely to be the result of a true deficiency. Experimental essential fatty acid deprivation in cats produces dry, scaly coats. Diets containing linoleic acid and linolenic acids as the sole source of essential fatty acids also induce a seborrheic dermatosis. Cats are obligate carnivores, as they lack delta-6-desaturase, the enzyme responsible for converting these 18-carbon fatty acids to longer-chain fatty acids. Arachidonic acid is an essential fatty acid for the cat.
Hypovitaminoses and vitamin-responsive dermatoses
Cutaneous lesions may occur as manifestations of deficiencies of vitamins A, C, and E; riboflavin; pantothenic acid; biotin; and niacin. Most of these are described in experimentally induced deficiencies. Many of the naturally occurring hypovitaminoses are probably not the result of a single vitamin deficiency but represent the cumulative effect of several inadequacies of the diet.
Vitamin A deficiency
Vitamin A is a fat-soluble vitamin belonging to a group of compounds referred to as retinoids. Vitamin A is involved in cellular growth and differentiation, as well as in visual processes and reproduction. Vitamin A has a controlling effect on epithelial differentiation. Cutaneous lesions of vitamin A deficiency are squamous epithelial hyperkeratosis and squamous metaplasia of secretory epithelia. Vitamin A oversupplementation is teratogenic and can lead to toxicity if liver storage capacity is exceeded. Signs are manifest primarily in the skeletal system and liver, or as malformations of the fetus in pregnant animals.
Hypovitaminosis A has been reported in all species of domestic animals, although many accounts are anecdotal. It may be secondary to dietary deficiency, decreased intestinal absorption, liver disease, or toxicities such as chlorinated naphthalene toxicity of cattle. Bile and pancreatic enzymes are needed for dietary absorption of vitamin A. The cutaneous lesions of hypovitaminosis A in cattle are a marked scaling and crusting dermatitis; in the pig, follicular hyperkeratosis; and, in cats, scaling, follicular plugging, and alopecia. A report in the dog indicated thickened, hyperpigmented skin with alopecia and follicular hyperkeratosis.
Vitamin A–responsive dermatoses occur in dogs and almost exclusively in the Cocker Spaniel. In one syndrome, Cocker Spaniels are predisposed, probably because of a congenital abnormality of epidermopoiesis and keratinization (see Seborrhea). The condition is characterized by adult-onset hyperkeratotic plaques, follicular plugging, and the formation of keratin fronds. Ventral and lateral chest and abdomen are sites of predilection. There may be accompanying ceruminous otitis externa and pyoderma. Histologically, the predominant lesion is marked follicular orthokeratotic keratosis (Fig. 6-55 ). Vertically oriented keratin casts protrude from the follicular ostia. There is mild to moderate epidermal hyperplasia and surface hyperkeratosis of the basket-weave type. Dermal inflammation is mild, mononuclear, and perivascular, unless secondary bacterial infection intervenes to produce neutrophilic folliculitis and/or furunculosis. There are rare reports of vitamin A–responsive dermatoses in other breeds of dogs. These diseases are not vitamin A deficiencies per se, in that plasma levels of vitamin A are within the normal range. The fact that therapy is effective can be attributed more to the “normalizing” effect of vitamin A (and retinoids) on cellular differentiation in the epidermis. Differentials include primary or secondary seborrhea and late-stage sebaceous adenitis. Oral supplementation with vitamin A may be needed to confirm the diagnosis.
Figure 6-55.
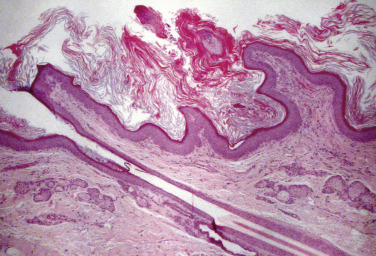
Vitamin A–responsive dermatosis. Note the marked follicular hyperkeratosis.
Vitamin B deficiencies
The B-vitamin complex is essential to the maintenance and proper functioning of many important metabolic pathways. B vitamins are water soluble and not stored within the body, necessitating a constant dietary supply. These vitamins interact with each other, with vitamin C, and with fat-soluble vitamins. Single deficiencies of these vitamins are rare. Deficiencies result in dry, flaky seborrhea with alopecia, anorexia, and weight loss.
Riboflavin (vitamin B2) deficiency is mostly a problem in swine and chickens fed grain rations with borderline concentrations of the vitamin. Ruminants do not become deficient because of rumen synthesis of the B-complex vitamins. Young calves, however, may develop deficiency if deprived of milk or an appropriate replacer. Animals develop hyperemia around the lips, nose, and buccal mucosa; diarrhea; weight loss; and generalized alopecia. Cutaneous lesions described in hyporiboflavinosis include scaling and ulcerative dermatitis in the pig, erythema, scaling, and dry haircoat on the ventral abdomen and hindlegs in the dog, and alopecia in the cat.
Pantothenic acid is a component of coenzyme A, an essential factor for entrance of acetic acid into the Krebs cycle. Deficiency is documented in pigs, but may occur in dogs and calves. Pantothenic acid deficiency in pigs produces progressive alopecia with dermatitis and ulceration, in addition to the general effects of weight loss, diarrhea, and neurologic signs. Young preruminant calves may show dermatologic signs that include alopecia, a roughened coat, and dermatitis. Leukotrichia has been described in dogs.
Biotin deficiency rarely occurs spontaneously, except in intensively reared swine, as the vitamin is widely distributed in feeds. Biotin is essential for proper use of fats, glucose, and amino acids. Feeding raw egg whites that contain avidin, a substance that renders biotin unavailable, may induce deficiencies. Cutaneous lesions reported in biotin-deficient pigs include alopecia, pustular dermatitis, and cracked hooves, causing lameness and significant economic loss. Microscopic lesions include epidermal hyperplasia, orthokeratotic and parakeratotic hyperkeratosis, epidermal necrosis and pustules, and folliculitis. A deficiency attributed, in part, to a lack of vitamin B, probably biotin, was reported in lambs reared artificially on reconstituted cow's milk. Alopecia was largely due to a fleece in which individual fibers were thin, weak, and straight. Histologically and ultrastructurally, the wool fibers had reduced numbers of cortical cells. Histochemical stains showed a delay in the incorporation and oxidation of sulfhydryl groups. Supplementation with B-group vitamins partially restored the fleece. Biotin deficiency reportedly causes a dry, brittle, haircoat, scaling, and leukotrichia in dogs. Dogs deficient in biotin may develop periocular and facial alopecia resembling the clinical lesions of systemic lupus erythematosus, discoid lupus, or other dermatoses affecting the face.
Niacin is a component of the pyridine nucleotides NAD+ and NADP+ needed for the function of a number of enzymes involved in nutrient metabolism. Deficiency occurs spontaneously in animals fed diets low in pyridoxine (vitamin B6) and tryptophan, as all of these components are needed for pyridine nucleotide synthesis. Pigs fed a low animal-protein diet that is also high in corn renders niacin unavailable to the animal because of low tryptophan levels. Cutaneous lesions include alopecia and a crusting dermatitis. Niacin deficiency in dogs induces reddening and ulceration of the oral mucous membranes, resembling human hyponiacinosis, known as pellagra. Reports of canine cases from the first quarter of the 20th century indicate severe necrotizing glossitis and stomatitis, leading to the term black tongue.
Pyridoxine (vitamin B6) serves as coenzyme in amino acid and protein metabolism. Deficiency produced experimentally in cats resulted in a dull, unkempt coat with scaliness and alopecia of the head and extremities. Histologically, hair follicles were in telogen, and there was epidermal and follicular hyperkeratosis. Because pyridoxine may be indirectly involved in zinc transport, through its effect on tryptophan metabolism, these effects might be due to alteration in the levels of zinc. Isoniazid has been reported to inactivate pyridoxine.
Vitamin C deficiency
Vitamin C (ascorbic acid) is required for the proper synthesis and structural maintenance of collagen and as a component of a number of essential enzymes. Almost all mammals synthesize vitamin C with the exception of humans, nonhuman primates, guinea pigs, Indian fruit bats, and Indian pipistrelles. Insects, invertebrates, and fish also cannot synthesize vitamin C. Deficiencies (scurvy or scorbutus) are limited to these species of animals, and signs are related to the inability of fibroblasts to form collagen or osteoid and are discussed in Vol. 1, Bones and joints.
Vitamin C–responsive dermatosis has been described in two10-week-old dairy calves. The condition is characterized by nonpruritic scaling, alopecia, crusts, and easily epilated hair on the head and limbs. There may be erythema, petechiae, and ecchymoses on extremities. Severely affected calves may have systemic signs, such as depression and slow growth. Histologic changes include diffuse orthokeratotic hyperkeratosis, curlicue hairs, periadnexal hemorrhage, and vascular dilation and congestion.
Vitamin E deficiency
Vitamin E deficiency is discussed primarily in Vol. 1, Bones and joints and Vol. 2, Liver and biliary system. Steatitis or “yellow-fat disease” involves subcutaneous fat and may be seen clinically as a skin disease, and can result from consumption of high levels of unsaturated fatty acids and/or insufficient vitamin E. The yellowness of the fat is due to the deposition of ceroid. Vitamin E acts as an antioxidant to prevent lipid peroxidation. Dietary requirements vary by species and individual and with the other components of the diet. Naturally occurring vitamin E deficiency has not been reported in the dog.
Nutritional panniculitis occurs in cats, mink, foals, and swine. The disease is associated the feeding of fishmeal, fish offal, or other products with a high concentration of unsaturated fatty acids. Diets with a high content of oily fish, such as tuna, white fish, and sardines, are most often implicated; however, the condition in cats also has been associated with diets containing primarily pig's brain, liver, diets with only a small fish content, or improperly stored or outdated commercial cat food. The practice of feeding high-fish diets to cats is reported to be common in Greece. Destruction of vitamin E also occurs in food that, through improper processing or storage, becomes rancid. The disease is not, however, the result of a simple deficiency, because cats fed diets deficient in vitamin E but also lacking in unsaturated fatty acids, do not develop panniculitis. In mink and foals, it may be associated with degeneration of muscles, and in swine it may occur alone or be associated with any one or combination of ulceration of the squamous mucosa of the stomach, muscle degeneration, and hepatosis dietetica. The disease has variable mortality in cats after a short clinical course in which there is progressive depression, possible fever, hyperesthesia, reluctance to move, and palpable thickening and increased firmness of the subcutaneous fat, easiest to detect in the inguinal region. The changes are not confined to the subcutaneous tissues but affect all fat depots. Biopsy reveals fat that varies from gray to lemon yellow to orange and is indurated and sometimes edematous. Hematologic changes may include neutrophilic leukocytosis and anemia.
The initial histologic change is deposition of globules of ceroid in the interstitial tissue. This, together with a fishy odor, may be all that is observed in swine in which the fat is soft and gray rather than yellow. In most affected cats, fat necrosis stimulates inflammation, which is initially neutrophilic but becomes granulomatous. Numerous macrophages, and occasionally giant cells, ingest the ceroid pigment. Mineralization may be present. Ceroid may be found also in macrophages of the liver, spleen, and lymph nodes. In cats, the initial differential should include infectious steatitis, sterile nodular panniculitis, lupus panniculitis, or other noncutaneous diseases, such as feline infectious peritonitis, ascites of various causes, and other causes of hyperesthesia. The clinical signs and the demonstration of ceroid, a variant of lipofuscin, which is acid fast and autofluorescent, should establish the diagnosis.
Vitamin E–responsive dermatosis has been described in goats. Kids and adults on a selenium-deficient diet developed periorbital alopecia and generalized seborrhea. The haircoat was dull and brittle. Histologically, the lesions were orthokeratotic hyperkeratosis and mild superficial perivascular dermatitis, in which mononuclear cells predominated.
Alopecia in calves associated with the feeding of milk substitute was attributed, in part, to vitamin E deficiency. The calves had low levels of serum vitamin E, and the hair regrew after vitamin E therapy was initiated for concurrent nutritional myopathy.
Further reading
Blanchard PC, et al. Pathology associated with vitamin B-6 deficiency in growing kittens. J Nutr 1991;121:S77-S78.
Carey CJ, Morris JG. Biotin deficiency in the cat and the effect on hepatic propionyl CoA carboxylase. J Nutr 1977;107:330-334.
Chapman RE, Black JL. Abnormal wool growth and alopecia of artificially reared lambs. Aust J Biol Sci 1981;34:11-26.
Codner EC, Thatcher CD. Nutritional management of skin disease. Compend Contin Educ Pract Vet 1993;15:411-423.
De Jong MF, Sytsema JR. Field experience with d-biotin supplementation to gilt and sowfeeds. Vet Q 1983;5:58-67.
Elias PM, et al. Retinoid effects on epidermal structure, differentiation, and permeability. Lab Invest 1981;44:531-540.
Frigg M, et al. Clinical study on the effect of biotin on skin conditions in dogs. Schweizer Arch Tierheilkunde 1989;131:621-625.
Hensel P. Nutrition and skin diseases in veterinary medicine. Clin Dermatol 2010;28:686-693.
Hutchison G, Mellor DJ. Effects of maternal nutrition on the initiation of secondary wool follicles in foetal sheep. J Comp Pathol 1983;93:577-583.
Hynd PI. Effects of nutrition on wool follicle cell kinetics in sheep differing in efficiency of wool production. Aust J Agric Res 1989;40:409-417.
Ihrke PJ, et al. responsive dermatosis in the dog. J Am Vet Med Assoc 1983;182:687-690.
Miller WM. et al. Nutrition and skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 685-694.
Niza MM, et al. Feline pansteatitis revisited: hazards of unbalanced home-made diets. J Feline Med Surg 2003;5:271-277.
Outerbridge CA. Cutaneous manifestations of internal diseases. Vet Clin North Am Small Anim Pract 2013;43:135-152.
Pritchard GC. Alopecia in calves associated with milk substitute feeding. Vet Rec 1983;112:435-436.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Nutritional skin diseases. In: Scott DW, et al., editors. Small Animal Dermatology. 5th ed. Philadelphia: WB Saunders; 1995. p. 890-901.
Ward KA, et al. The regulation of wool growth in transgenic animals. In: von Tscharner C, Halliwell REW, editors. Advances in Veterinary Dermatology, vol. 1. London: Baillière Tindall; 1990. p. 70-76.
Watson TD. Diet and skin disease in dogs and cats. J Nutr 1998;128(Suppl. 12):2783S-2789S.
Zini E, et al. Pansteatitis and severe hypocalcaemia in a cat. J Feline Med Surg 2007;9:168-171.
Mineral deficiency and mineral-responsive dermatoses
Iodine, cobalt, copper, and zinc deficiencies may lead to integumentary lesions. Iodine deficiency is discussed in Vol. 3, Endocrine glands. The effects of copper deficiency on wool and hair are referred to under Disorders of pigmentation. Cobalt deficiency causes a progressive, wasting disease in ruminants. There are nonspecific changes in the wool or haircoat, including lack of growth and increased fragility.
Zinc deficiency
Zinc is an essential trace element. Naturally occurring true zinc deficiency is rare in dogs, extremely rare in cats, and not reported in horses. Zinc-responsive dermatosis in dogs is discussed in the next section. In the integument, a substantial proportion of zinc is in the wool or the haircoat. Zinc is a component of many important metalloenzymes and is a cofactor for many others. It exerts its primary effect through zinc-dependent enzymes that regulate RNA and DNA metabolism. Zinc thus plays a role in all metabolic processes involved with tissue growth, maturation, and repair, and is involved in vitamin A metabolism and in enzymes needed for free radical scavenging. Zinc also modulates many aspects of the immune and inflammatory responses. The relationship between the changes in particular tissue enzyme activities brought about by zinc deficiency and clinical manifestations of the deficiency syndrome are not, however, well understood. Zinc is known to have an inhibitory effect on apoptotic pathways. The parakeratosis seen in cases of zinc deficiency and zinc-responsive dermatosis may be related to decreased activity of zinc-related lytic enzymes along with increased epidermal cell turnover, which results in failure of nuclear hydrolysis.
Zinc deficiency causes anorexia, alterations in food use, growth retardation, reproductive disorders, depression of the immune response, hematologic abnormalities, depression of central nervous system development, decreased wound healing, and keratinization defects in epidermis, hair, wool, and horny appendages. True zinc deficiency is of most significance in the pig.
Parakeratosis in swine.
Zinc-responsive dermatosis in swine (parakeratosis) became an important clinical entity in the 1950s, coincident with and related to the widespread introduction of dry meal feeding. The cause is not a simple deficiency. The availability of dietary zinc is adversely affected by the presence of phytic acid in plant protein rations, a high concentration of calcium, a low concentration of free fatty acids, alterations in intestinal flora, and the presence of bacterial and viral enteric pathogens, such as transmissible gastroenteritis virus. Zinc deficiency may induce secondary vitamin A deficiency as a result of its effect on appetite and food use. Economic losses are due to depression of growth rate, but, with improved management techniques, parakeratosis is no longer a major problem. Parakeratosis occurs in young, growing pigs, 2-4 months of age. The initial gross lesions are erythematous macules on the ventral abdomen and medial surface of the thigh. The lesions develop into papules, which become covered with a gray-brown, dry, roughened scale-crust that may reach 5-7 mm in thickness. Deep fissures penetrate the crust and are filled with brown-black detritus, which is composed of sebum, sweat, soil, and other debris. These areas are susceptible to secondary bacterial infection, often leading to pyoderma or subcutaneous abscessation. Lesions are roughly symmetrical and have a predilection for the lower limbs, particularly over the joints, around the eyes, ears, snout, scrotum, and tail. In severely affected animals, lesions may become generalized. Pruritus is not a feature of parakeratosis. The dorsal surface of the tongue is “furred,” and the esophageal mucosa loses its normal smooth sheen and becomes dull and white.
The microscopic lesion in the skin is marked hyperplastic dermatitis with diffuse parakeratotic hyperkeratosis (Fig. 6-56A, B ). The oral mucous membranes also demonstrate hyperplastic epithelium. Acanthosis, elongation of rete ridges, and mitotic figures in the basal keratinocytes are regular features of the hyperplastic response of the epidermis. The dermal lesions in uncomplicated parakeratosis include variable vasodilation and a mild to moderate, predominantly mononuclear cell, perivascular infiltrate. With bacterial infection, there may be nodular or diffuse neutrophilic dermatitis, folliculitis, perifolliculitis, or furunculosis.
Figure 6-56.
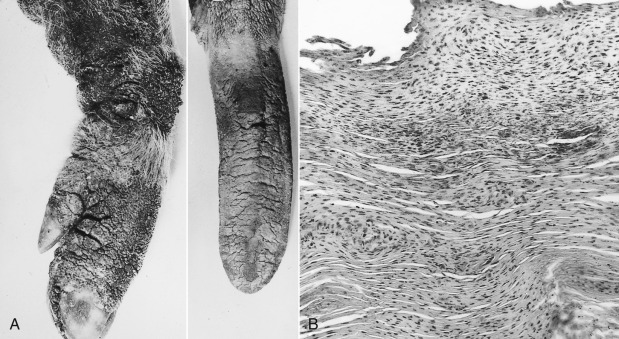
Zinc-responsive dermatosis in a pig. A. Marked hyperkeratosis of the skin of the foreleg and tongue epithelium. B. Marked parakeratotic hyperkeratosis.
Parakeratosis in swine must be differentiated grossly from sarcoptic mange and exudative epidermitis. The former is usually intensely pruritic, and the latter usually occurs in a younger age group, and the scale-crust is greasy rather than dry. Parakeratosis is rarely fatal unless toxemia or septicemia secondary to cutaneous bacterial infection develop or because of exacerbation of intercurrent infections such as pneumonia. Affected pigs recover rapidly upon zinc supplementation.
Zinc deficiency in ruminants and camelids.
Zinc-responsive dermatoses occur in goats, sheep, cattle, alpacas, and llamas. The condition is uncommon to rare. Characteristic dermatitis occurs in true zinc deficiency as well as an idiopathic zinc-responsive condition. Hyperkeratosis also affects the forestomachs of ruminants. Secondary infections in the skin are common. Causes of zinc deficiency include diets deficient in zinc or diets with high calcium, iron, phytates, or other zinc-chelating agents. Drinking water with excessive iron can also be a factor. In true zinc deficiency, multiple animals in a herd may be affected and show clinical signs of decreased appetite and growth, weight loss, decreased milk production, depression, stiff joints, and diarrhea. Those with idiopathic zinc-responsive disease do not have systemic signs, and, in general, only one animal is affected. The hereditary zinc deficiencies of cattle are discussed under Congenital and hereditary diseases of skin.
In ruminants, scaling, crusting, and alopecia occur in a symmetrical pattern over the face, pinnae, mucocutaneous junctions, pressure points, and distal limbs. Dull, rough, brittle haircoat may be seen. Pruritus is variable. In sheep, fleece/wool biting may be seen. Histopathologic changes include irregular to papillated epidermal hyperplasia with spongiosis, superficial perivascular to interstitial lymphoeosinophilic dermatitis, with marked diffuse parakeratotic hyperkeratosis. In goats and sheep, there may be a mix of orthokeratotic and parakeratotic hyperkeratosis.
In alpacas, tightly adherent crusts are seen on the perineum, ventral abdomen, groin, medial thighs, axillae, and medial forelegs. The bridge of the nose, muzzle, and periocular region may also be affected. Pruritus is absent or mild. In alpacas, it is thought that breeding females and those with darker fleeces are more susceptible to zinc-responsive dermatosis because of a higher demand for zinc. Histopathologic findings include papillated epidermal hyperplasia with predominantly orthokeratotic hyperkeratosis, parakeratotic caps, and lymphoeosinophilic superficial perivascular dermatitis.
Zinc deficiency in horses.
Experimental zinc deficiency has been reported in foals fed a zinc-deficient diet. Lesions included alopecia and scaling of the limbs, ventral abdomen, and thorax. Anecdotally, a few horses with scaling and erythema around the eyes, lips, coronets, and other pressure points; with histologic changes of epidermal hyperplasia; diffuse parakeratotic hyperkeratosis; and superficial perivascular lymphoeosinophilic dermatitis responded well to oral zinc supplementation.
Further reading
Krametter-Froetscher R, et al. Zinc-responsive dermatosis in goats suggestive of hereditary malabsorption: two field cases. Vet Dermatol 2005;16:269-275.
Nielsen FH. History of zinc in agriculture. Adv Nutr 2012;3:783-789.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Endocrine, nutritional, and miscellaneous hair coat disorders. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 360-377.
Singer LJ, et al. Zinc responsive dermatopathy in goats: two field cases. Contemp Top Lab Anim Sci 2000;39:32-35.
Suttle NF. Problems in the diagnosis and anticipation of trace element deficiencies in grazing livestock. Vet Rec 1986;119:148-152.
White CL, et al. The effect of zinc deficiency on wool growth and skin and wool follicle histology of male Merino lambs. Br J Nutr 1994;71:425-435.
Canine zinc-responsive dermatoses
Naturally occurring zinc-responsive dermatoses in the dog fall under 2 syndromes:
-
•
Syndrome 1 affects primarily Siberian Huskies and Alaskan Malamutes, and rarely other breeds not of Arctic origin, such as Great Danes. The cutaneous lesions usually become manifest before the dogs are 1 year of age. Older dogs may develop lesions during times of stress, such as pregnancy, lactation, or intercurrent disease. Lesions comprise scaling and crusting dermatitis with a predilection for the face, particularly around the eyes, lips and nose, pressure points, and footpads (Fig. 6-57A ). Lesions may be unilateral initially and progress to a bilateral distribution. Pruritus may be present. Secondary pyoderma is not uncommon. The pathogenesis of the syndrome is not well established. Alaskan Malamutes with chondrodysplasia have zinc-responsive spermatozoal defects and reduced zinc absorption from the intestinal tract; malabsorption may be responsible for the dermatologic disease. Lifetime supplementation of zinc is necessary to alleviate signs. A severe form of zinc-responsive dermatosis has been documented in a litter of Pharaoh Hounds. A role for oxidative stress has been shown in cases of canine zinc-responsive dermatosis. Dogs with zinc-responsive dermatosis have decreased epidermal immunoreactivity for metallothioneins, which are sulfhydryl-rich proteins that store zinc and act as free radical scavengers. The change may be indicative of low epidermal zinc levels. The epidermis of affected dogs also shows high expression levels of heat shock proteins, increased ki-67, as well an absence of caspase 3 activation.
-
•
Syndrome 2 occurs in puppies of any breed and is associated with a relative deficiency of zinc, probably secondary to excessively high levels of calcium and/or phytates in the diet in rapidly growing animals. Excessive iron in the drinking water may also contribute. In the United States, this disease has been associated with the feeding of generic dog food, in Britain and Sweden with the feeding of soy- and/or cereal-based diets. Recovery quickly follows restoration of a diet meeting the National Research Council standards for canine nutrition or zinc supplementation of cereal diets. Now that dog food manufacturers are aware of the problem, the disease is less common. The gross lesions are multiple, scaling, and crusted plaques, particularly affecting the muzzle, pressure points, distal extremities, and trunk. There is extreme thickening and fissuring of the footpads and, sometimes, the planum nasale. Secondary pyoderma may develop, and puppies often show a local lymphadenopathy.
Figure 6-57.

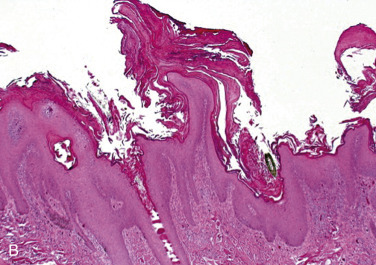
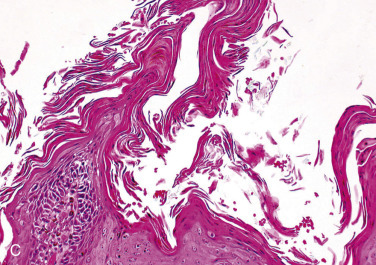
Zinc-responsive dermatosis in a dog. A. Hyperkeratotic plaques on muzzle and around the eyes. B. Papillary epidermal hyperplasia with prominent parakeratotic follicular spires. C. Higher magnification for parakeratotic projections from hair follicle ostia.
The histologic lesions of both syndromes are usually typical of zinc deficiency, with papillary epidermal hyperplasia, marked spongiotic parakeratotic hyperkeratosis affecting the epidermis and follicular ostia, and multifocal neutrophilic crusts (Fig. 6-57B, C). Mild to moderate superficial perivascular mononuclear or eosinophil-rich dermatitis is present. Some reports indicate that the keratinization defect was sufficiently severe to induce dyskeratotic changes at all levels of the epidermis, whereas in others, orthokeratotic hyperkeratosis alone was found.
Differential diagnoses include superficial necrolytic dermatitis, lethal acrodermatitis, thallium toxicity, and chronic hypersensitivity dermatitis that may look very similar histologically. Dermatophytosis, pemphigus foliaceus, and pyoderma should be considered based upon gross lesions. The signalment, history, lesion distribution, and pathologic changes should help to establish the diagnosis. In some cases, response to dietary changes and/or zinc supplementation may be needed for confirmation of the suspected diagnosis. Serum and plasma zinc levels are not an accurate method of assessing zinc status. Values, even in a normal animal, are subject to marked variation according to sex, age, stress, concurrent disease, and collection methods. It is possible that dietary factors other than zinc are involved in some of these diseases, particularly those responding to dietary changes and not just to zinc supplementation.
Further reading
Campbell GA, Crow D. Severe zinc responsive dermatosis in a litter of Pharaoh Hounds. J Vet Diagn Invest 2010;22:663-666.
Colombini S. Canine zinc-responsive dermatosis. Vet Clin North Am Small Anim Pract 1999;29:1373-1383.
Romanucci M, et al. Oxidative stress in the pathogenesis of canine zinc-responsive dermatosis. Vet Dermatol 2011;22:31-38.
White SD, et al. Zinc-responsive dermatosis in dogs: 41 cases and literature review. Vet Dermatol 2001;12:101-109.
Superficial necrolytic dermatitis (hepatocutaneous syndrome)
A histologically distinct cutaneous reaction pattern characterized by the so called “red, white, and blue” epidermal changes of parakeratosis, epidermal necrolysis or laminar intraepidermal edema, and basilar hyperplasia has been recognized most often in the dog, and occasionally in the cat. The condition resembles necrolytic migratory erythema, a human paraneoplastic syndrome most often associated with α-cell neoplasms of the pancreas. The pathogenesis of superficial necrolytic dermatitis (SND) is unknown, but hepatic dysfunction and derangement of glucose and amino acid metabolism are clearly involved. Elevated glucagon levels alone are unlikely to be directly responsible for the skin lesions, as both dogs and humans may develop the disease in their absence, and dermatitis is not an inevitable result of the hyperglucagonemic state. Hypoaminoacidemia, the result of sustained gluconeogenesis and increased hepatic catabolism, is documented in both canine and human patients, and it has been postulated that it may deplete epidermal proteins and induce epidermal necrosis. Zinc and fatty acid metabolism may also be deranged. The most likely pathogenesis of abnormal or impaired ability to properly use nutrients and the clinical and histologic similarities of this entity to zinc-responsive dermatoses warrant discussion of SND in this section.
In dogs, SND has been reported to occur in association with a variety of systemic diseases, including glucagon-secreting tumors of the pancreas, hyperglucagonemia, diabetes mellitus, and liver disease. Severe hepatopathy is reported in >90% of the canine cases. The variety of concurrent diseases and the histologic appearance have led to terms for the characteristic cutaneous reaction pattern in dogs. These include superficial necrolytic dermatitis, hepatocutaneous syndrome, diabetic dermatopathy, metabolic epidermal necrosis, and necrolytic migratory erythema. Diabetes and hyperglucagonemia in some cases could be secondary to hepatic degeneration. Some dogs have a history of long-term phenobarbital administration. Rare reports in cats include a pancreatic carcinoma presumably of endocrine origin and a glucagon-producing primary hepatic neuroendocrine carcinoma.
Lesions have a roughly bilaterally symmetrical distribution. The muzzle, lips, periocular skin, edges of the pinnae, distal extremities, ventrum, and points of pressure or friction, such as the hocks, and the external genitalia are typically affected. Oral and mucocutaneous lesions are occasionally reported. Lesions are erythematous, erosive, ulcerative, and crusted. The footpads are markedly hyperkeratotic (Fig. 6-58A ). Footpad lesions were not a feature of SND in the cat. The histologic lesions of the “red, white, and blue” epidermis are virtually pathognomonic; the distinctive feature is a band of hydropic, pale-staining keratinocytes in the upper half of a usually acanthotic stratum spinosum (Fig. 6-58B). Both intracellular and intercellular edema contribute to the epidermal pallor. As these cells degenerate, clefts and vesicles may form in the outer stratum spinosum. Neutrophils may accumulate to form subcorneal pustules. The stratum corneum is diffusely and markedly parakeratotic and appears hypereosinophilic in comparison to the subjacent pale-staining stratum spinosum of the epidermis. The epithelium of the follicular infundibulum can also be affected. The basal cell layer is basophilic and hyperplastic, forming small rete ridges. Individual necrotic keratinocytes may be located randomly in the epidermis and make distinction from erythema multiforme difficult in some cases. In SND, the necrotic keratinocytes lack satellitosis. Dermal inflammation is minimal, and predominantly mononuclear and perivascular. In eroded lesions, neutrophilic exocytosis is prominent, and inflammatory crust covers the surface.
Figure 6-58.
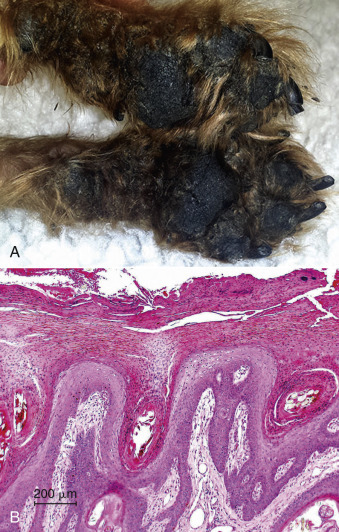
Superficial necrolytic dermatitis in a dog. A. Marked hyperkeratosis and crusting around the margins of the footpads and adjacent haired skin. B. The histologic changes of the epidermis make a characteristic “red (parakeratosis), white (intracellular edema in the spinous layer), and blue (basal layer hyperplasia)” pattern.
In cases associated with liver disease, the most commonly associated gross lesion is a nodular liver with intervening firm, collapsed parenchyma. Histologically, there is loss of parenchyma and minimal inflammation. Hepatocytes are markedly vacuolated by a mix of lipid and glycogen. The nodules have been interpreted in some cases to represent regeneration and in others to be composed of nodular remnants of atrophic hepatic parenchyma.
The diagnosis is based on typical histologic findings. However, the pathognomonic epidermal edema may not be present in every biopsy. Differential diagnoses include other parakeratotic, hyperplastic dermatitides, such as the zinc-responsive dermatoses, lethal acrodermatitis of Bull Terriers, and thallium toxicity. The clinical differential is the same as listed for zinc-responsive dermatoses. The prognosis is generally considered poor because most cases have advanced liver disease. Cases associated with a pancreatic neoplasm may have resolution of skin lesions following tumor excision.
A similar syndrome has been described in horses with erosive, ulcerative, and exudative coronitis and concurrent liver pathology. The histopathologic changes in the skin are as described above, and may lead to necrosis and sloughing of the hoof wall.
Further reading
Allenspach K, et al. Glucagon-producing neuroendocrine tumour associated with hypoaminoacidaemia and skin lesions. J Small Anim Pract 2000;41:402-406.
Asakawa MG, et al. Necrolytic migratory erythema associated with a glucagon-producing primary hepatic neuroendocrine carcinoma in a cat. Vet Dermatol 2013;24:466-469.
Byrne KP. Metabolic epidermal necrosis-hepatocutaneous syndrome. Vet Clin North Am Small Anim Pract 1999;29:1337-1355.
Hill PB, et al. Resolution of skin lesions and long-term survival in a dog with superficial necrolytic dermatitis and liver cirrhosis. J Small Anim Pract 2000;41:519-523.
Kimmel SE, et al. Clinicopathological, ultrasonographic, and histopathological findings of superficial necrolytic dermatitis with hepatopathy in a cat. J Am Anim Hosp Assoc 2003;39:23-27.
March PA, et al. Superficial necrolytic dermatitis in 11 dogs with a history of phenobarbital administration (1995-2002). J Vet Intern Med 2004;18:65-74.
Mizuno T, et al. Superficial necrolytic dermatitis associated with extrapancreatic glucagonoma in a dog. Vet Dermatol 2009;20:72-79.
Outerbridge CA, et al. Plasma amino acid concentrations in 36 dogs with histologically confirmed superficial necrolytic dermatitis. Vet Dermatol 2002;13:177-186.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Turek MM. Cutaneous paraneoplastic syndromes in dogs and cats: a review of the literature. Vet Dermatol 2003;14:279-296.
Endocrine Diseases of Skin
Endocrine disorders frequently manifest clinically as skin disease, but these dermatoses are rarely specific for any one endocrinopathy. Although these dermatopathies are more common in dogs, they can occur in any species. Clinical features of many endocrine dermatoses include a dry, coarse, brittle, dull, easily epilated haircoat that fails to regrow after clipping; hypotrichosis and hyperpigmentation; and alopecia that is frequently bilaterally symmetrical. Secondary pyoderma and scaling are common. In addition, endocrine dermatoses share many histologic features, including orthokeratotic hyperkeratosis, follicular dilation and keratosis, hair follicle atrophy, absence of hair shafts in follicles, increased numbers of telogen follicles, variably increased trichilemmal cornification (flame follicles) of follicles, and epidermal hyperpigmentation. These histologic changes suggest an endocrine dermatosis but frequently are not pathognomonic for a specific endocrinopathy. A combination of clinical and histologic features, together with clinical testing to demonstrate hormonal deficiency or excess, is required for confirmation.
Hypothyroidism
Hypothyroidism, almost always primary hypothyroidism, is the most common endocrine dermatopathy in dogs. Histologically, the thyroid gland may have lymphoplasmacytic inflammation (lymphocytic thyroiditis) or atrophy without inflammation (idiopathic atrophy). Lymphocytic thyroiditis has been likened to Hashimoto's thyroiditis, a similar immune-mediated condition in humans. Idiopathic thyroid atrophy may represent the end stage of lymphocytic thyroiditis. In addition, hypothyroidism may be caused by developmental defects of the thyroid gland and rarely iodine deficiency. Congenital hypothyroidism with goiter has been reported in Tenterfield Terriers, as well as Toy Fox and Rat Terriers. The cause, so-called dyshormonogenesis, is caused by failure of the thyroid gland to produce sufficient hormone to inhibit pituitary release of thyroid-stimulating hormone (TSH). Pituitary neoplasia, or hypopituitarism, resulting in decreased secretion of TSH can lead to secondary hypothyroidism. It is a disease of middle-aged dogs, and there is no sex predilection, although the incidence is increased in neutered males and ovariohysterectomized females. Breeds that are predisposed include the Doberman Pinscher, Golden Retriever, Chow Chow, Great Dane, Irish Wolfhound, Boxer, English Bulldog, Dachshund, Afghan Hound, Newfoundland, Alaskan Malamute, Brittany Spaniel, Poodle, Irish Setter, and Miniature Schnauzer.
Clinical cutaneous changes include seborrhea, dry, coarse, brittle hair; hair that does not regrow after clipping; and hyperpigmentation and hypotrichosis with fine retained hairs that give the appearance of a “puppy coat.” Alopecia typically develops on frictional areas, such as the elbows and hips, around the neck (from the collar), as well as the entire length of the tail (eFig. 6-12) (“rat tail”), and bridge of the nose. Pruritus is not a feature unless there is secondary pyoderma. Some cases may be presented with refractory pyoderma or chronic otitis externa. Hypothyroidism is thought to alter the skin barrier function; animal models suggest impaired lymphocyte and neutrophil function. Myxedema occurs in severe cases and may result in “tragic facial expression” see eFig. 6-12). Histologic changes can be nonspecific and simply suggest an endocrinopathy. The most common changes are orthokeratotic hyperkeratosis with follicular keratosis; normal to mildly hyperplastic epidermis; sebaceous glands are atrophied, normal, or slightly hyperplastic; and most hair follicles in hairless telogen (kenogen). Myxedema is a more specific but less common finding. Occasionally, dysplastic follicles, flame follicles, vacuolated arrector pili muscles, and epidermal melanosis may occur.
eFigure 6-12.

Hypothyroidism in a dog. A. Marked facial myxedema. B. Scaling and hair loss on the tail.
Hypothyroidism occurs less frequently in other domestic animals, and usually in association with iodine deficiency and goiter. In Merino sheep and Afrikander cattle, a hereditary defect in the biosynthesis of thyroid hormone produces symmetrical hypotrichosis and thick, myxedematous, wrinkled skin. In goats, hypothyroidism occurs in a mixed strain of Saanen and dwarf goats in association with hereditary congenital thyroglobulin deficiency. Gross cutaneous changes include bilaterally symmetrical hypotrichosis and thick, myxedematous, scaly skin. Histologic findings include orthokeratotic hyperkeratosis, follicular keratosis, diffuse dermal mucinous degeneration (myxedema), and dermal thickening.
Hyperadrenocorticism
Hyperadrenocorticism is common in dogs and can be caused by bilateral adrenocortical hyperplasia resulting from a pituitary tumor (pituitary-dependent hyperadrenocorticism), a neoplasm of the adrenal cortex (usually unilateral), or exogenously administered glucocorticoids resulting in iatrogenic hyperglucocorticism. Of the naturally occurring forms, the pituitary-dependent form is considerably more common. The disease is seen most commonly in middle-aged or older dogs, and the Boxer, Boston Terrier, Dachshund, and Poodle are predisposed. Occasionally, skin lesions will be the only clinical sign of hyperadrenocorticism. Cutaneous changes can include bilaterally symmetrical hypotrichosis or alopecia affecting primarily skin of the trunk, pendulous abdomen, thin skin that has decreased elasticity, slow wound healing, hyperpigmentation, telangiectasia, scaling, comedones, and calcinosis cutis (Figs. 6-59 , 6-60A ). Lesions of calcinosis cutis occur most commonly in the dorsal neck region or axilla and groin. The lesions appear as firm erythematous papules or plaques that frequently ulcerate. Calcinosis cutis is most commonly the result of iatrogenic hyperadrenocorticism. Other causes of mineral deposits in the skin are discussed under Physical injury to skin.
Figure 6-59.

Hyperadrenocorticism in a dog. Note pendulous abdomen, truncal alopecia, and redistribution of adipose tissue. The dog has a decubital ulcer on the right elbow.
Figure 6-60.

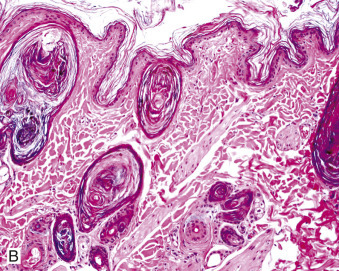
Hyperadrenocorticism in a dog. A. Comedones in a dog. Note gross appearance of distended follicles. B. Note thin epidermis and hair follicles distended with keratin.
Histologically, canine hyperadrenocorticism is characterized by thin epidermal and follicular epithelium, which can be 1-3 nucleated cell layers thick (Fig. 6-60B). If calcinosis cutis is present, the epidermis is frequently hyperplastic and can be ulcerated. Other changes can include orthokeratotic hyperkeratosis; marked follicular keratosis, sometimes with comedone formation; thin dermis; hair follicles that are frequently in telogen or kenogen; sebaceous gland atrophy; sebaceous melanosis; dysplastic follicles; and variable hyperpigmentation. The presence of calcinosis cutis (Fig. 6-61 ), which can occasionally result in osseous metaplasia, is virtually pathognomonic for hyperadrenocorticism, bearing in mind that mineralization of the external root sheath can be seen in normal old dogs and in Poodles. Cutaneous histologic lesions of hyperadrenocorticism can occur focally at the site of topical glucocorticoid application.
Figure 6-61.
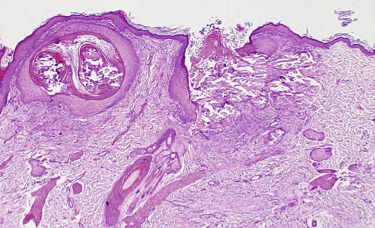
Calcinosis cutis in hyperadrenocorticism in a dog. The epidermis is hyperplastic. A large area of mineralized dermal collagen accompanied by granulomatous inflammation is undergoing transepidermal elimination.
Hyperadrenocorticism is considerably less common in cats. As in dogs, the condition is more commonly pituitary dependent than adrenal dependent or iatrogenic. The clinical presentation in cats is similar to that in the dog; however, in addition, there is often concurrent diabetes mellitus, and marked skin fragility in which dermal collagen is reduced. This can result in tearing and lacerations of the skin (feline skin fragility syndrome). Histologic lesions in the cat are similar to those in the dog; however, calcinosis cutis, and telangiectasia have not been reported.
Hyperadrenocorticism (referred to as pituitary dependent pars intermedia dysfunction) occurs in horses and is almost always seen in association with hypertrophy, adenomatous hyperplasia, or functional neoplasms of the pars intermedia of the pituitary. The disease affects primarily aged horses and has no breed or sex predilection. Gross cutaneous changes may include a coarse, brittle, long, shaggy haircoat (hirsutism), an abnormal shedding pattern, episodic hyperhidrosis, poor wound healing, decreased muscle tone, weight loss, and susceptibility to secondary skin infections.
Hyposomatotropism and hypersomatotropism
Hyposomatotropism, decreased production of growth hormone, occurs in young dogs with congenital pituitary dwarfism. The cause is a failure of the pharyngeal ectoderm to differentiate into hormone-secreting cell populations. Undifferentiated cells produce fluid, which causes large cysts in the sella turcica. The clinical signs are predominantly related to growth hormone deficiency, which may occur along with reduced levels of thyroid, adrenal, and sex hormones. In the German Shepherd dog and Karelian Bear dog, pituitary dwarfism is thought to be inherited as a simple autosomal recessive condition and is usually associated with a cystic Rathke's cleft. Clinically, the dogs are normal at birth, but show growth retardation and small stature. The most striking change is retention of the puppy haircoat.
Hypersomatotropism refers to the production of excess growth hormone, whereas acromegaly is the name of the syndrome that results from that state of excess growth hormone production. Acromegaly is very rare in dogs. Excessive somatotropin (growth hormone) production is associated with administration of progestins or with the metestrus (luteal) phase of the estrous cycle in intact female dogs. Cutaneous changes include thick, folded, myxedematous skin, especially on the head, neck, and distal extremities. The haircoat may be long and thick, and the nails may exhibit rapid overgrowth. Histologic findings in canine hypersomatotropism include thickened dermis resulting from increased production of glycosaminoglycans and collagen by dermal fibroblasts. Myxedema is present in about a third of cases. In cats, hypersomatotropism or acromegaly is caused by excess endogenous growth hormone secretion from a pituitary acidophil adenoma. Clinical signs include insulin-resistant diabetes mellitus, weight gain, broad facial features, inferior prognathia, heart murmur, organomegaly, and respiratory stridor.
Hyperestrogenism
Hyperestrogenism can occur in male or female dogs. In middle-aged to older intact male dogs, it is associated with functional testicular neoplasms, primarily Sertoli cell neoplasms, and occasionally functional interstitial cell tumors and seminomas. The Boxer, Shetland Sheepdog, Cairn Terrier, Pekingese, Collie, and Weimaraners are predisposed. Hyperestrogenism is also seen in middle-aged to older intact female dogs with polycystic ovaries or functional ovarian neoplasms. It can also occur in male or female dogs following estrogen administration. Rare cases can arise from physical contact with humans wearing topical estradiol compounds.
The clinical lesions of hyperestrogenism include symmetrical hypotrichosis or alopecia, which typically originates at the perineum and genital region and progresses cranially on the trunk. The hair is dry and dull, is easily epilated, can fail to regrow after clipping, and can be accompanied by hyperpigmentation, especially macular pigmentation. Male dogs may develop a pendulous prepuce, gynecomastia, or prostatomegaly with squamous metaplasia of the prostatic ducts. Females may develop an enlarged vulva. Histologic changes include hair follicles that are primarily in telogen, orthokeratotic hyperkeratosis, and follicular keratosis.
Alopecia X
Growth hormone/castration-responsive dermatosis has many synonyms, including hyposomatotropism of the adult dog, sex hormone alopecia, pseudo-Cushing's syndrome, testosterone-responsive dermatosis, estrogen-responsive dermatosis, congenital adrenal hyperplasia–like syndrome, and hair cycle arrest. This diversity in nomenclature reflects the differences in endocrine values and responses to various treatments and the fact that the pathogenesis of these conditions has not been fully characterized. To simplify the nomenclature, the condition is now being referred to as alopecia X. These dogs have normal thyroid function and adrenal function. Theories include genetics and hair follicle receptors, and most theories involve a deficiency or imbalance in sex hormones, such as a partial deficiency of 21-hydroxylase or other adrenocortical enzymes necessary for adrenal steroidogenesis and/or a growth hormone deficiency.
Alopecia X occurs most often in plush-coated Nordic breeds, such as the Pomeranian, Keeshond, Chow Chow, Samoyed, Siberian Husky, Alaskan Malamute, Norwegian Elkhound, American Eskimo Dog, and occasionally in other breeds. Affected dogs have a dull dry coat with loss of primary hairs. There is symmetrical alopecia of the trunk, perineum, caudal thighs, and neck, sparing the head and distal extremities (Fig. 6-62 ). Hyperpigmentation of exposed skin is common. Dark haircoats may fade. Coat changes can occur between 1 and 10 years of age, and either sex can be affected. These dogs tend to regrow tufts of hair at sites damaged by biopsy or surgery. Initial histologic changes are characterized by follicular atrophy; trichilemmal cornification in primary hairs can be quite prominent. Caution is warranted in making the diagnosis of alopecia X based exclusively on this feature because normal primary hair follicles of Nordic breeds can have increased trichilemmal cornification. The histologic features must be interpreted in light of clinical findings.
Figure 6-62.

Alopecia X in a dog.
Canine recurrent flank alopecia
Canine recurrent flank alopecia (seasonal flank alopecia, cyclical flank alopecia) is a condition seen most commonly in the Boxer, English Bulldog, Airedale Terrier, Schnauzer, and Griffon Korthal, but can occur in many, typically short-coated, breeds. It is characterized by alopecia of the skin of the flank that is usually bilaterally symmetrical, rarely unilateral, and occurs recurrently or seasonally. The first episode occurs at approximately 4 years of age but can be variable. In the Northern Hemisphere, the onset of alopecia is usually between November and March. There is spontaneous hair regrowth after 3-8 months; however, occasional dogs have progressively less hair regrowth after each episode. Rare dogs fail to regrow hair after the first episode; and some dogs have one episode of alopecia that never recurs.
Clinically, the bilaterally symmetrical lesions are usually confined to the thoracolumbar regions, have well-demarcated margins with abrupt transition from affected to unaffected skin, and are usually hyperpigmented (Fig. 6-63A ). Histologic changes are those of noninflammatory, nonscarring follicular atrophy. Follicular infundibula are dilated and filled with keratin that can extend into the openings of the primary and secondary atrophic follicles, giving the appearance of an inverted footprint over the remnants of the follicular epithelium (Fig. 6-63B). Sebaceous melanosis may be seen. Rarely, canine recurrent flank alopecia is associated with an interface dermatitis in Boxer dogs (eFig. 6-13). The interface reaction is manifest by annular areas of scaling localized within the areas of alopecia.
Figure 6-63.

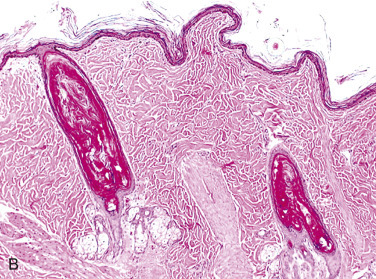
Recurrent flank alopecia. A. Large geographic area of hyperpigmentation and alopecia in the lateral thorax/flank area of an English Bulldog. B. Follicular infundibula are dilated and filled with keratin that extends into the openings of the primary and secondary atrophic follicles, giving the appearance of an inverted footprint.
eFigure 6-13.

Canine recurrent flank alopecia with interface dermatitis. Annular foci of scaling are located within the areas of alopecia.
(Courtesy W.M. Miller.)
Further reading
Barsanti JA, et al. Diethylstilbestrol-induced alopecia in a dog. J Am Vet Med Assoc 1983;182:63-64.
Credille KM, et al. The effects of thyroid hormones on the skin of beagle dogs. J Vet Intern Med 2001;15:539-546.
Daminet S, Paradis M. Evaluation of thyroid function in dogs suffering from recurrent flank alopecia. Can Vet J 2000;41:699-703.
Doliger S, et al. Histochemical study of cutaneous mucins in hypothyroid dogs. Vet Pathol 1995;32:628-634.
Frank LA, et al. Adrenal steroid hormone concentrations in dogs with hair cycle arrest (alopecia X) before and during treatment with melatonin and mitotane. Vet Dermatol 2004;15:278-284.
Frank LA. Comparative dermatology—canine endocrine dermatoses. Clin Dermatol 2006;24:317-325.
Frank LA. Endocrine and metabolic diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 501-553.
Frazier KS, et al. Multiple cutaneous ossification associated with iatrogenic hyperglucocorticism. J Vet Diagn Invest 1998;10:303-307.
Gross TL, Ihrke PJ. The histologic analysis of endocrine-related alopecia in the dog. In: von Tscharner C, Halliwell REW, editors. Advances in Veterinary Dermatology. London: Baillière Tindall; 1990. p. 75-88.
Helton-Rhodes K, et al. Cutaneous manifestations of feline hyperadrenocorticism. In: Ihrke PJ, et al., editors. Advances in Veterinary Dermatology. Oxford, UK: Pergamon Press; 1993: 2. p. 391-396.
Levy M, et al. Diagnosis and treatment of equine Cushing's disease. Compend Contin Educ Pract Vet 1999;21:766-769.
Miller MA, Dunstan RW. Seasonal flank alopecia in Boxers and Airedale Terriers: 24 cases (1985-1992). J Am Vet Med Assoc 1993;203:1567-1572.
Müntener T, et al. Canine noninflammatory alopecia: a comprehensive evaluation of common and distinguishing histological characteristics. Vet Dermatol 2012;23:206-e44.
Niessen SJ, et al. Hypersomatotropism, acromegaly, and hyperadrenocorticism and feline diabetes mellitus. Vet Clin North Am Small Anim Pract 2013;43:319-350.
Panciera DL. Hypothyroidism in dogs—66 cases (1987-1992). J Am Vet Med Assoc 1994;204:761-767.
Rac R, et al. Congenital goitre in Merino sheep due to an inherited defect in the biosynthesis of thyroid hormone. Res Vet Sci 1968;9:209-223.
Ris-Stalpers C, Bikker H. Genetics and phenomics of hypothyroidism and goiter due to TPO mutations. Mol Cell Endocrinol 2010;322:38-43.
Rosser EJ. Castration responsive dermatosis in the dog. In: von Tscharner C, Halliwell REW, editors. Advances in Veterinary Dermatology. London: Baillière Tindall; 1990. p. 75-88.
Rosychuk RAW. Dermatologic manifestations of canine hypothyroidism and the usefulness of dermatohistopathology in establishing a diagnosis. Canine Pract 1997;22:25-26.
Scott DW, Concannon PW. Gross and microscopic changes in the skin of dogs with progestogen-induced acromegaly and elevated growth hormone levels. J Am Anim Hosp Assoc 1983;19:523-527.
Scott DW. Cutaneous phlebectasias in cushingoid dogs. J Am Anim Hosp Assoc 1985;21:35-354.
Scott-Moncrieff JC. Clinical signs and concurrent diseases of hypothyroidism in dogs and cats. Vet Clin North Am Small Anim Pract 2007;37:709-722.
Seaman WJ, Chang SH. Dermal perifollicular mineralization of toy poodle bitches. Vet Pathol 1984;21:122-123.
Watson PJ, Herrtage ME. Hyperadrenocorticism in six cats. J Small Anim Pract 1998;39:175-184.
Zur G, White SD. Hyperadrenocorticism in 10 dogs with skin lesions as the only presenting clinical signs. J Am Anim Hosp Assoc 2011;47:419-427.
Immune-Mediated Dermatoses
Hypersensitivity dermatoses
In the context of infection or vaccination, contact with exogenous antigens usually leads to induction of a protective response, but when the immune response causes damage to tissues, it is called hypersensitivity or allergy. Compounds such as pollens, food, drugs, insect components, various chemicals, and agents such as dust mites, Staphylococcus, and Malassezia spp. contain antigens that are normally innocuous but may induce allergic reactions in predisposed individuals. Most cutaneous hypersensitivity reactions are mediated by type I (immediate) hypersensitivity, type IV (cell-mediated or delayed) hypersensitivity, or by a combination of the 2 types. Hypersensitivity reactions cause a variety of dermatoses that range from annoying and uncomfortable (Fig. 6-64 ) to severely debilitating or life threatening. Allergic dermatoses are common and important in dogs, cats, and horses, but are rarely reported in food animals. Most of the research in allergy of domestic animals has focused on canine atopic dermatitis.
Figure 6-64.

Urticaria in a horse. Discrete, well-circumscribed, serpiginous plaques with a flat top and steep sides.
(Courtesy J. Greek.)
Atopic dermatitis
Atopy is a defined as an inherited tendency to produce IgE antibodies and develop clinical allergy to pollens and other environmental antigens. Atopy is a general term and when used as an adjective, “atopic,” it describes a disease process in an organ system (e.g., atopic rhinitis, atopic asthma, atopic dermatitis [AD]).
A surge of investigations into pathogenesis atopic disorders has dramatically changed the understanding of AD. There are bodies of evidence that stress the “outside in” theory that begins with an abnormal skin barrier that results in a pathologic immune response, as opposed to the “inside out” theory that focuses on immunologic aberrations that result in skin disease. The strong link between an abnormal skin barrier and AD is corroborated by investigations into the genetics of ichthyosis vulgaris (IV). Individuals with IV are homozygous for mutations in the filaggrin gene. Heterozygous relatives are clinically normal but predisposed to AD and atopic asthma. Although filaggrin is not the only predisposing cause of atopic disease, loss of function mutations are present in about 10% of the population in Western Europe. During cornification, profilaggrin, located within keratohyaline granules of the stratum granulosum, is dephosphorylated to filaggrin. Filaggrin serves to anneal keratin intermediate filaments to form the strong central corneocyte core. Degradation products of filaggrin (e.g., urcanic acid) act as a natural moisturizing factor for the stratum corneum (SC). Even subtle defects in the organization or composition of the SC enable transepidermal allergen penetration and sensitization. Humans with AD have xerosis (dry skin), which is a result of increased transepidermal water loss (TEWL) and impairment of the water-holding capacity of the skin. In dogs, there is only limited evidence of an association between filaggrin and canine atopic dermatitis (CAD). Mutations in the filaggrin gene FLG do not appear to play a role in the development of CAD, although altered filaggrin expression may be present. There is reasonable evidence that dogs with CAD have an altered skin barrier: deranged lipid profiles in the SC (e.g., decreased free ceramides), ultrastructural changes in the SC of atopic dogs, and increased TEWL in both normal and abnormal skin.
Canine atopic dermatitis.
Canine atopic dermatitis has been defined as a genetically predisposed inflammatory and pruritic allergic skin disease with characteristic clinical features most commonly associated with IgE antibodies to environmental allergens. It is a common condition that is estimated to affect 10% of the canine population, and runs second only to flea-bite hypersensitivity in geographic areas where fleas are endemic.
CAD is a multifactorial disease that involves immune dysregulation, allergen sensitization, skin barrier defects, environmental conditions, and altered microbial flora.
CAD has a strong genetic component, but the precise genetic basis remains unclear. Numerous studies (quantitative PCR, microarrays, single nucleotide polymorphism [SNP], genome-wide linkage, and genome-wide association) have implicated many genes that are differentially expressed in CAD; however, there is little concordance between studies both within and among breeds. In the United States, predisposed breeds include Labrador Retriever, Golden Retriever, West Highland White Terrier, Chinese Shar-Pei, Bull Terrier, Bichon Frise, and Tibetan Terrier; however, the predilection can vary geographically. In Britain, guide dogs (mainly Golden Retriever and Labrador Retriever guide dogs) are at high risk of developing CAD. Other breeds considered predisposed include the French Bulldog, Cairn Terrier, Basset Hound, Scottish Terrier, Lhasa Apso, Shih Tzu, Wirehaired Fox Terrier, Dalmatian, Pug, Irish Setter, Boston Terrier, Boxer, English Setter, Miniature Schnauzer, Belgian Tervuren, and Beauceron.
Caution is urged when attempting to differentiate causes of allergic skin disease based on histopathology. Although there may be histologic features that support CAD, the diagnosis of CAD is based on a combination of historical findings, gross lesions, and exclusion of other allergic conditions (e.g., sarcoptic mange, flea-bite hypersensitivity, food hypersensitivity). When interpreting skin biopsies, pathologists should be aware of the clinical presentation and characteristic clinical lesions. The primary clinical sign is pruritus, which frequently begins seasonally but eventually becomes perennial. Pruritus and erythema most commonly affect the face (Fig. 6-65 ), paws, distal extremities, and ventrum and is often manifested as face rubbing and foot chewing and licking. Skin lesions are usually due to self-trauma, secondary pyoderma, and Malassezia dermatitis. Secondary skin changes include alopecia and salivary staining of the hair, excoriations, scale, hyperpigmentation, lichenification, and pyotraumatic dermatitis (eFig. 6-14). Atopic dogs characteristically have an unpleasant odor that results from a combination of scaling, secondary bacterial or yeast infection, and hyperhidrosis. Atopic otitis externa is common. Noncutaneous clinical signs are rare and may include conjunctivitis, rhinitis, asthma, and gastrointestinal disorders.
Figure 6-65.

Acute atopic dermatitis in a dog. Note the perioral, periocular, and aural erythema.
eFigure 6-14.

Atopic dermatitis in a dog. Note the flexural fold lesions with marked hyperpigmentation, lichenification, and alopecia. A. Chest. B. Thorax. C. Inguinal area.
The following criteria are significantly correlated with CAD: onset before 3 years of age, indoor living, pruritus prior to lesion onset, lesions on the forepaws, and concave pinnae. Lesions on the ear margins (sarcoptic mange) and dorsolumbosacral region (flea-bite hypersensitivity) do not support CAD. The presentation varies among different dog breeds. For example, West Highland White Terriers have lesions on the feet, flexural surfaces, dorsolumbosacral skin, and face, and often with generalized involvement. Boxers are more likely to have urticaria and otitis.
CAD was once considered a strictly Th2 cell–mediated disease; however, newer evidence shows that CAD reflects a slow progression from Th2 humoral inflammation (associated with high IgE) in the early phase to a Th1 cell–mediated response in the chronic phase. One hypothesis to explain the etiology of CAD begins with a defective skin barrier. For decades, allergic inhalant dermatitis was ingrained prominently in the veterinary literature as the consequence of an allergic reaction triggered by inhaled aeroallergens. There is strong evidence that transdermal exposure is more important, which predisposes to allergen penetration and sensitization. In dogs, transdermal exposure correlates with the distribution of lesions on sparsely haired areas (i.e., paws, ventrum, flexural folds). Allergens are captured by high-affinity receptors for IgE (FcεR1) receptors on Langerhans cells that process and present antigen to T lymphocytes. Atopic dogs and cats have increased and often aggregated Langerhans cells within the epidermis. Moreover, there are increased T cells in the epidermis, and the dermis contains clusters of perivascular dendritic cells. Functionally, these findings correlate with antigen capture by Langerhans cells (dendritic cells in the epidermis) and enhanced antigen presentation by dendritic cells to lymphocytes. The cytokine thymic stromal lymphopoietin (TSLP) is innately released by activated keratinocytes and serves as a potent activator of dermal dendritic cells. Dendritic cells activate allergen-specific T cells and drive the Th2 response.
Th2 cytokines (particularly interleukin-4 [IL-4], IL-5, IL-13) enhance eosinophilic inflammation and overproduction of allergen-specific IgE. IL-4 is a critical cytokine in the development of allergic diseases. It signals T cells to become Th2 cells, which are the major source of IL-4 production, thereby initiating a self-amplifying process. IL-4 induces expression of IgE receptors on Langerhans cells, resulting in enhanced antigen presentation capability. IL-4 and IL-13 induce the antibody isotype switch from IgM to IgE. They also upregulate expression of vascular cell adhesion molecule-1 (VCAM-1), an adhesion molecule expressed by cutaneous endothelial cells and involved in migration of eosinophils and mononuclear cells into sites of allergic inflammation. IL-5 promotes differentiation, vascular endothelial adhesion, and survival of eosinophils.
IgE appears to have a multifunctional role in the pathogenesis of atopic dermatitis (AD). An immediate type of hypersensitivity reaction develops within minutes of allergen exposure when mast cells bearing allergen-specific IgE bind allergen and release a variety of preformed mediators, most notably histamine. The skin histamine content has been found to be increased in humans and dogs with AD. Activated mast cells also release cytokines, such as IL-4, IL-5, IL-6, tumor necrosis factor-α, and platelet-activating factor (PAF), that further promote inflammation. An IgE-dependent late-phase reaction develops subsequently when expression of leukocyte adhesion molecules on postcapillary venule endothelium promotes influx of eosinophils, neutrophils, and mononuclear cells into the skin. Eosinophils release various mediators, including PAF, eosinophil major basic protein (MBP), eosinophil cationic protein (ECP), and cytokines that promote inflammation and cause tissue damage. Antigen-specific IgE antibodies also appear to be involved in a nonclassic role in antigen uptake and processing. IgE-bearing antigen-presenting cells (APCs), particularly Langerhans cells and dermal dendritic cells, bind, process, and present specific antigen locally to allergen-specific indeterminate T cells (Th0), thereby directing them to the Th2-cell phenotype. Moreover, IgE-mediated antigen presentation increases the presenting capacity of these APCs up to 100-fold, a mechanism known as “facilitated antigen presentation.” Ultimately, B cells are stimulated to produce more allergen-specific IgE, which is bound to antigen-presenting cells, and a vicious cycle of facilitated antigen presentation is perpetuated.
In lesional skin of atopic dogs, superficial perivascular eosinophils, subcorneal eosinophilic micropustules, eosinophil degranulation, and increased CD4+ and CD8+ T cells are present. Tissue-selective homing of T cells is thought to be regulated at the level of T-cell recognition of vascular endothelial cells via interaction of differentially expressed T lymphocyte homing receptors, such as cutaneous lymphocyte antigen (CLA), and their endothelial cell ligands. Therefore it seems likely that the elevated expression of adhesion molecules by endothelial cells promotes migration of increased numbers of CLA+ T cells into the skin. The tendency to develop AD, as opposed to asthma or allergic rhinitis, may depend on differences in the memory/effector T cells that are specialized to home to the skin versus lung. Furthermore, cytokines released by Th2 cells (e.g., IL-31) appear to incite pruritus. IL-31 activates Janus kinase/signal transducer and activator of transcription (Jak/STAT) pathways in a broad range of immune cells, and receptors for IL-31 are also found on keratinocytes. As pruritus persists, self-trauma further compromises the skin barrier and facilitates additional allergen exposure.
With chronicity, the inflammation becomes Th1 polarized. Dendritic cells release IL-12, and a Th1 cytokine milieu (interferon-γ [IFN-γ], IL-2) ensues. In contrast to the Th2 response, Th1 cells produce IFN-γ, which inhibits IgE synthesis and differentiation of Th2 cells. The balance between Th1 and Th2 cells may be modulated by biochemical defects in monocytes. Peripheral blood mononuclear cells of individuals with AD have been shown to have increased activity of phosphodiesterase, which results in increased monocyte prostaglandin E2 (PGE2) production. PGE2 tends to inhibit Th1 production of IFN-γ and accentuate secretion by Th2 cells. Histologically, the progression to a Th1-mediated immune response corresponds with a greater abundance of superficial perivascular lymphocytes and plasma cells, with eosinophils becoming a less prominent component of the inflammatory infiltrate.
Dogs and humans with AD are predisposed to superficial infections with Malassezia and Staphylococcus. Although Staphylococcus pseudintermedius is part of the normal canine flora, it is the most frequent cause of pyoderma in dogs with AD. Dogs with AD have higher levels of anti-staphylococcal IgE than non-atopic dogs. Multidrug resistance to S. pseudintermedius is not uncommon in dogs that have received multiple antibiotic courses. Staphylococcus aureus in humans is believed to augment allergen-induced skin inflammation in AD by secreting exotoxins that act as superantigens. Superantigens have the capacity to activate large numbers of T cells nonspecifically by virtue of their ability to bridge the linkage between the class II major histocompatibility complex molecule on the antigen-presenting cell (APC) and certain classes of the T-cell receptor without having to be processed and presented by the APC. IgE antibodies directed against these exotoxins have been identified in individuals with AD, and the severity of disease correlates with these IgE antibody titers, presumably because the locally produced exotoxins are absorbed through the skin surface and cause IgE-dependent mast cell degranulation within the dermis.
As in the dog, the diagnosis of AD in cats is made clinically by a combination of historical findings, gross lesions, and specifically by exclusion of other allergic conditions (e.g., flea-bite hypersensitivity; ectoparasites such as Cheyletiella, Demodex gatoi, Notoedres; and adverse food reaction). Devon Rex and Abyssinian breeds may be predisposed. Clinical signs usually develop at 6-24 months of age; however, AD can arise in older cats. The pruritus associated with AD in cats is often nonseasonal and severe. Clinical lesions of AD cannot distinguish causes of non–flea-induced hypersensitivity. Reaction patterns include self-induced alopecia, eosinophilic granuloma complex lesions, miliary dermatitis, recurrent swelling or ulceration of the lower lip, otitis externa, and pruritus of the face, pinnae, and neck, as well as the abdomen/axillae, dorsal trunk, and distal limbs and paws. In some cases, pruritus might not be obvious because of the secretive nature of cats. Instead, hair loss, secondary to covert licking and chewing, may be the only abnormality, and the skin may appear normal. Miliary dermatitis is a clinical reaction pattern of cats that consists of numerous small erythematous crust-covered papules. It is not specific for AD and may also occur in ectoparasite, food, and drug hypersensitivities. Noncutaneous signs associated with atopy in cats include sneezing, conjunctivitis, coughing, and asthma. Lymphadenopathy may be present in cats with miliary dermatitis or eosinophilic granulomas.
Pruritus is the primary clinical sign in horses with atopy. Some cases are manifested as recurrent pruritic urticaria. Onset is usually between 1.5 and 4 years of age. Skin lesions usually develop secondarily in response to self-trauma and include alopecia, excoriations, lichenification, and hyperpigmentation. The face, ears, ventrum, and legs are most commonly affected. Arabians and Thoroughbreds may be predisposed. A seasonal pruritic dermatosis typical of AD has been described in 2 Suffolk ewes.
Microscopic changes associated with AD have been considered nonspecific and usually consist of perivascular to interstitial dermatitis. In dogs, the epidermis is variably hyperplastic and may have mild, patchy intercellular edema; focal parakeratosis; and crusting. Erosion and ulceration may be present from self-trauma. Exocytosis of lymphocytes or eosinophils and small subcorneal accumulations of eosinophils may be seen. Dermal inflammation is superficial perivascular to interstitial, and consists of lymphocytes and macrophages primarily. Mast cells are in increased numbers and may be numerous. Eosinophils and neutrophils are usually in low numbers, but eosinophils may be missed because of degranulation. Sebaceous glands are hyperplastic, and apocrine sweat glands may be dilated in chronic lesions. Superficial dermal blood vessels may be congested, and the superficial dermis may be mildly edematous.
Histologic changes in the skin of cats with AD vary according to the lesions biopsied. The epidermis varies from normal to variably hyperplastic. Serocellular crusts, foci of intercellular edema and epidermal necrosis, and exocytosis of small numbers of eosinophils are usually present in lesions of miliary dermatitis. The dermis contains a superficial perivascular to interstitial infiltrate of mixed cells. Mast cells, eosinophils, lymphocytes, and neutrophils are typically present but vary in their proportions. Neutrophils are most numerous in areas of erosion or ulceration. In some cases, the lesions are those of an eosinophilic plaque. The microscopic lesion in atopic horses and sheep is hyperplastic perivascular dermatitis with a predominance of eosinophils.
Diagnosis of AD is based on compatible history and physical examination findings coupled with demonstration of allergen-specific IgE antibodies. In dogs, measurement of total serum IgE has not been found to be useful because there is no significant difference in IgE concentrations between atopic and clinically normal dogs. Intradermal skin testing (IDST) has been considered to be the most reliable method of identifying clinically relevant allergens. In vitro tests that measure concentrations of allergen-specific IgE are commercially available but generally have been found to correlate poorly with IDST results. However, newer procedures (radioallergosorbent test, ELISA, and liquid-phase immunoenzymatic assay) for measurement of allergen-specific IgE may be more accurate in identifying clinically relevant allergens in dogs and cats. Diagnosis may be complicated by the presence of concurrent hypersensitivity conditions; such as flea-bite allergy or food allergy, and solely histologic findings in these conditions are indistinguishable.
Further reading
DeBoer DJ. Canine atopic dermatitis: new targets, new therapies. J Nutr 2004;134:2056S-2061S.
DeBoer DJ, Hillier A. The ACVD task force on canine atopic dermatitis (XVI): laboratory evaluation of dogs with atopic dermatitis with serum-based “allergy” tests. Vet Immunol Immunopathol 2001;81:277-287.
Favrot C. Feline non-flea induced hypersensitivity dermatitis: clinical features, diagnosis and treatment. J Feline Med Surg 2013;15:778-784.
Gonzales AJ, et al. Interleukin-31: its role in canine pruritus and naturally occurring canine atopic dermatitis. Vet Dermatol 2013;24:48-53.
Gross TL, et al. Correlation of histologic and immunologic findings in cats with miliary dermatitis. J Am Vet Med Assoc 1986;189:1322-1325.
Halliwell REW. Efficacy of hyposensitization in feline allergic diseases based upon results of in vitro testing for allergen-specific immunoglobulin E. J Am Anim Hosp Assoc 1997;33:282-288.
Hämmerling R, DeWeck AL. Comparison of two diagnostic tests for canine atopy using monoclonal anti-IgE antibodies. Vet Dermatol 1998;9:191-199.
Hanifin JM, Chan SC. Monocyte phosphodiesterase abnormalities and dysregulation of lymphocyte function in atopic dermatitis. J Invest Dermatol 1995;105:84S-88S.
Hill PB, et al. Concentrations of total serum IgE, IgA, and IgG in atopic and parasitized dogs. Vet Immunol Immunopathol 1995;44:105-113.
Kanda S, et al. Characterization of canine filaggrin: gene structure and protein expression in dog skin. Vet Dermatol 2013;24:25-31.
Klukowska-Rötzler J, et al. Expression of thymic stromal lymphopoietin in canine atopic dermatitis. Vet Dermatol 2013;24:54-59.
Leung DYM. Pathogenesis of atopic dermatitis. J Allergy Clin Immunol 1999;104:S99-S108.
Marsella R, et al. International Task Force on Canine Atopic Dermatitis. Current evidence of skin barrier dysfunction in human and canine atopic dermatitis. Vet Dermatol 2011;22:239-248.
Marsella R, et al. Current understanding of the pathophysiologic mechanisms of canine atopic dermatitis. J Am Vet Med Assoc 2012;241:194-207.
Nimmo-Wilkie JS, et al. Morphometric analyses of the skin of dogs with atopic dermatitis and correlations with cutaneous and plasma histamine and total serum IgE. Vet Pathol 1990;27:179-186.
Nuttall T, et al. Canine atopic dermatitis—what have we learned? Vet Rec 2013;172:201-207.
O'Dair HA, et al. An open prospective investigation into aetiology in a group of cats with suspected allergic skin disease. Vet Dermatol 1996;7:193-202.
Olivry T, Hill PB. The ACVD task force on canine atopic dermatitis (XVIII): histopathology of skin lesions. Vet Immunol Immunopathol 2001;81:305-309.
Olivry T. Is the skin barrier abnormal in dogs with atopic dermatitis? Vet Immunol Immunopathol 2011;144:11-16.
Ravens PA, et al. Feline atopic dermatitis: a retrospective study of 45 cases (2001-2012). Vet Dermatol 2014;25:95-102.
Rees CA. Canine and feline atopic dermatitis: a review of the diagnostic options. Clin Tech Small Anim Pract 2001;16:230-232.
Roosje PJ, et al. Increased numbers of CD4+ and CD8+ T cells in lesional skin of cats with allergic dermatitis. Vet Pathol 1998;35:268-273.
Sinke JD, et al. Immunophenotyping of skin-infiltrating T-cell subsets in dogs with atopic dermatitis. Vet Immunol Immunopathol 1997;57:13-23.
Voie KL, et al. Drug hypersensitivity reactions targeting the skin in dogs and cats. J Vet Intern Med 2012;26:863-874.
Zunic M. Comparison between IMMUNODOT tests and the intradermal skin test in atopic dogs. Vet Dermatol 1998;9:201-205.
Urticaria and angioedema
Urticaria (hives, heat bumps) and angioedema (angioneurotic edema) are variably pruritic, edematous skin lesions produced by mediators released by basophils and dermal mast cells. Urticaria is most common in horses, uncommon in dogs, and rare in ruminants, pigs, and cats. Angioedema is rare. A wide variety of immunologic and nonimmunologic causes have been implicated, but frequently the specific causative agent cannot be determined for a particular individual. Immunologic causes of urticaria/angioedema are thought to involve type I hypersensitivity reactions primarily; type III hypersensitivity is involved occasionally. Recognized initiators in all species include foods and food additives, drugs, biological agents, stinging and biting arthropods, intestinal parasites, inhalant and contact allergens, and bacterial, fungal, and viral infections. Nonimmunologic factors associated with urticaria/angioedema include physical factors such as heat, cold, or pressure; mast cell degranulating agents such as radiocontrast media; and agents that result in perturbation of arachidonic acid metabolism. Deficiency of C1 esterase inhibitor is a genetic cause of chronic urticaria in humans. Aspirin and other nonsteroidal anti-inflammatory drugs, psychologic stress, and concurrent febrile illness may be exacerbating factors, if not causative ones, in humans with chronic urticaria. Another cause of chronic urticaria identified in humans is IgG autoantibody directed against the IgE receptor of cutaneous mast cells and circulating basophils. Binding of the autoantibody to this receptor induces release of histamine. T-helper 2 cytokines, eosinophils, mast cells, and macrophages have been suggested to play a role in the pathogenesis of equine recurrent urticaria. Regardless of cause, the final common pathway is increased vascular permeability and resultant edema produced by histamine, the major mediator, and possibly also by kinins, eicosanoids, and neuropeptides.
Drugs are probably the most frequent cause of urticaria in horses. A wide variety of systemic drugs and biological products have been implicated in initiating urticaria. Wheals frequently develop in minutes to hours after exposure to the offending drug and usually subside within several hours. Cholinergic or heat-reflex urticaria, induced by exercise or a hot bath, has been reported in a horse; pruritus in this horse appeared to be exacerbated by pelleted feed. An unusual form of urticaria called dermatographism, which is induced by blunt pressure to the skin, has also been described in the horse. In some instances, urticaria is thought to be caused by overfeeding of grains, especially those high in protein content (“protein bumps,” “feed bumps”). Lesions occur anywhere on the body but are most common on the face, neck, and thorax. In cattle, a unique form of urticaria has been described in high-producing dairy cows, especially Jerseys and Guernseys, that become sensitized to casein in their own milk (milk allergy). Foods, drugs, biological agents, and venomous stings are reported most frequently as causes of urticaria and angioedema in dogs and cats.
Urticaria is characterized by wheals (hives), which are discrete, well-circumscribed, erythematous, edematous plaques with a flat-top and steep sides (see Fig. 6-64). They are cool and pit upon digital pressure. They vary in size and may coalesce to measure many centimeters in diameter. Wheals are usually round; but in some instances, they assume bizarre and irregular serpentine shapes. The overlying hair may stand erect, giving the impression of a follicular disease. The lesions may be localized to a single body region, for instance, lateral neck, head, or thorax, or they may involve the entire body. The individual lesions usually last <12-24 hours and disappear, leaving no residual skin changes unless pruritus results in self-mutilation. Although individual lesions are transient, new ones may erupt over a period of days or weeks. The occurrence in horses of one of the multiple hypersensitivities of recurrent airway obstruction, insect-bite hypersensitivity, and urticaria may predispose the horse to the other hypersensitivities.
Angioedema consists of larger, less well-demarcated swellings that originate subcutaneously. With time, the swellings may gravitate ventrally. Angioedema is a potentially serious condition because involvement of perilaryngeal tissues may cause asphyxiation. Approximately 50% of affected humans develop both lesions concurrently, but development of both wheals and angioedema does not seem to be as common in animals.
Microscopic lesions are variable and nonspecific. The epidermis is usually normal in nontraumatized lesions. Urticaria is characterized by dermal edema, which is visualized as widening of spaces between collagen fibers in the superficial and middle dermis. The change may be very subtle and can be missed. Edema is typically more severe and involves the deep dermis and subcutaneous tissue in angioedema. Small vessels are congested, and lymphatics are dilated. Inflammation is inconsistent. When present, it usually consists of perivascular granulocytes, mast cells, and fewer lymphocytes and macrophages. The reaction involves the upper and middle dermis in urticaria and the deep dermis and subcutis in angioedema. Vasculitis is not a typical feature of urticaria and angioedema.
Diagnosis is usually based on the history and appearance and transitory nature of the clinical lesions. Biopsy is performed to rule out other conditions when the lesions are recurrent or chronic, and the diagnosis is uncertain. Identification of a particular inciting cause relies on history and a combination of elimination trials, environmental alterations, intradermal skin testing, and insect control measures.
Further reading
Dibbern DA Jr, Dreskin SC. Urticaria and angioedema: an overview. Immunol Allergy Clin North Am 2004;24:141-162.
Evans AG. Urticaria in horses. Compend Contin Educ Pract Vet 1993;15:626-632.
Fadok VA. Update on equine allergies. Vet Clin North Am Equine Pract 2013;29:541-550.
Hinden S, et al. Characterization of the inflammatory infiltrate and cytokine expression in the skin of horses with recurrent urticaria. Vet Dermatol 2012;23:503-e99.
Jose-Cunilleras E, et al. Intradermal testing in healthy horses and horses with chronic obstructive pulmonary disease, recurrent urticaria, or allergic dermatitis. J Am Vet Med Assoc 2001;219:1115-1121.
Kehrli D, et al. Multiple hypersensitivities including recurrent airway obstruction, insect bite hypersensitivity, and urticaria in 2 Warmblood horse populations. J Vet Intern Med 2015;29:320-326.
Logas D, et al. Cholinergic pruritus in a horse. J Am Vet Med Assoc 1992;201:90-91.
Matthews NS, et al. Urticarial response during anesthesia in a horse. Equine Vet J 1994;25:555-556.
Cutaneous adverse food reaction
The term “adverse food reaction” is a broad term that has replaced “food allergy” and “food hypersensitivity” in veterinary medicine. It is often unclear if the pathologic mechanisms represent a specific immune-mediated response (e.g., type I hypersensitivity) to food antigens or if the mechanism is related to nonimmune-mediated intolerance to a component in the food. When an adverse food reaction is manifested by dermatologic signs, it is termed cutaneous adverse reaction to food (CARF); however, affected animals can have concurrent gastrointestinal signs. The skin may represent the second most frequent target organ, after the gastrointestinal tract, in adverse food reactions. The clinical distribution and histologic lesions are largely indistinguishable from atopic dermatitis (AD).
Food allergy in humans is thought to develop as a consequence of physiologic and immunologic immaturity, resulting in increased absorption of food antigens during early life in association with the inherited tendency for increased production of IgE antibody. Absorption of intact food proteins is limited by the intestinal mucosal barrier and by combination of the proteins with food allergen–specific IgA secreted into the gut. However, adult levels of IgA are not generally produced until puberty, and this relative IgA deficiency may contribute to increased permeability of the gastrointestinal barrier during childhood. Gastrointestinal infections and parasitism may also contribute to disruption of the mucosal barrier to increase absorption of food antigens. The majority of food allergens are glycoproteins molecular weight 10,000-80,000 Da, which tend to be resistant to proteolysis and are heat stable and water soluble. Even in the mature intestine, ~2% of ingested food antigens are absorbed into the circulation in an immunologic form. However, these immunologically recognizable proteins do not normally cause adverse reactions despite being transported throughout the body because tolerance develops in most individuals. Tolerance is thought to involve activation of CD8+ T suppressor cells in gut-associated lymphoid tissue (GALT) to suppress an immune response. The development of tolerance to food appears to have little effect on B cells, given that antibody production to food proteins is a universal phenomenon; although low concentrations of serum IgG, IgM, and IgA food-specific antibodies are found in normal individuals, they are of no clinical consequence. In genetically predisposed infants, however, ingested antigens result in excessive production of IgE antibodies. These food-specific antibodies bind high-affinity receptors on mast cells, dendritic cells, and macrophages in tissues and basophils in circulation. When food allergens penetrate mucosal barriers and reach the IgE bound to mast cells and basophils, mediators are released that induce the signs of immediate hypersensitivity. Activated mast cells also generate various mediators (such as IL-4, tumor necrosis factor-α (TNF-α), and platelet-activating factor) that may induce an IgE-mediated late-phase response in which eosinophils, lymphocytes, and monocytes are attracted to the site of reaction and release additional inflammatory mediators and cytokines that drive a Th2-mediated response. The development of dermatitis rather than respiratory signs in individuals with food allergy may be related to homing of allergen-specific T cells to the skin by way of cutaneous lymphocyte-associated antigen (CLA), a homing molecule that directs these cells to the skin.
In companion animal species, the pathogenesis of adverse food reactions is poorly understood and does not correlate with food hypersensitivity in humans. In humans, the disorder is seen most commonly in infants and young children; and in many cases, a loss of clinical sensitivity develops after 1-3 years of an appropriate food elimination diet. Although signs may initially develop in young animals, CARF is typically a disease of adult animals, and no loss of clinical sensitivity has been observed in affected animals. Because gastrointestinal parasitism and viral enteritides are relatively common in animals, disruption of the intestinal mucosal barrier may be an important factor in the development of CARF. Furthermore, laboratory tests that measure food-specific IgE or IgG antibodies in dogs are notoriously inaccurate.
In dogs, CAFR does not show breed or sex predilections. CARF may affect up to 8% of dogs and accounts for 7-25% of allergic skin disorders in dogs. A minor population of dogs with CARF shows gastrointestinal signs (10-15%). In dogs, cutaneous adverse food reactions arise before 1 year of age in 33-48% of cases, and 51-85% are manifested between 1-3 years. Fewer cases (16%) arise in dogs aged 4-11 years; 23-45% of dogs with CARF have concurrent hypersensitivity conditions, such as AD, flea-bite allergy, or both. Adverse food reactions may be provoked by more than one dog food ingredient. The most common allergens identified in dogs are beef, soy, chicken, milk, corn, wheat, and eggs.
The most consistent sign is nonseasonal pruritus affecting the ears, feet, face, ventrum, limbs, or perineal regions. CARF may mimic sarcoptic mange, flea allergy dermatitis, or AD. The pruritus may be unresponsive or poorly responsive to glucocorticoid therapy. Primary skin lesions may include erythema, papules, or pruritic urticaria-angioedema, but they are frequently obscured by self-trauma as a consequence of chronic pruritus. More commonly, only secondary lesions are seen, and these typically include excoriation, alopecia, hyperpigmentation, lichenification, scales, and crusts. In a small number of cases, pruritic otitis externa or recurrent superficial pyoderma may occur in the absence of any other clinical signs of food allergy. Bacterial pyoderma and Malassezia infection are common secondary complications. Some dogs also exhibit concurrent gastrointestinal signs, which include increased frequency of defecation most commonly, and mucus and/or blood in feces, tenesmus, flatulence, vomiting, and diarrhea. Neurologic signs, such as malaise and seizures, and respiratory signs have been reported rarely in conjunction with skin lesions in dogs with food allergy.
The prevalence of CARF in cats is estimated to be 1-6% of all feline dermatoses. Furthermore, CARF may affect 12-16% of cats with pruritus and 10% of cats with military dermatitis. No breed or sex predilection is apparent. Most cases are recognized in young adult cats. The major complaint is severe pruritus that is usually nonseasonal and frequently poorly responsive to glucocorticoid therapy. The face, ears, and neck are most commonly involved, but pruritus may be generalized (Fig. 6-66 ). Allergens identified include fish, lamb, milk, whale meat, beef, chicken, rabbit, eggs, and pork. Food-allergic cats may also have other hypersensitivity conditions, such as AD or flea-bite allergy. Skin lesions are extremely variable and include erythema, angioedema-urticaria, self-induced alopecia and excoriations, crusting, seborrhea, or miliary dermatitis. They may be localized to the face and head or generalized in distribution. Eosinophilic granuloma complex lesions may be a manifestation of food allergy. Concurrent gastrointestinal or respiratory signs are uncommon.
Figure 6-66.

Food allergy in a cat with marked self-trauma. Note the preauricular and periocular crusting, and erythema.
Cutaneous adverse food reaction has been reported rarely in horses, cattle, and pigs. Substances that have been incriminated include wheat, barley, bran, oats, concentrates, and tonics in horses; wheat, bran, corn, clover hay, rice bran, and soybeans in cattle; and clover pasture in pigs. Clinical signs in horses and cattle are pruritic papular eruptions, pruritic urticaria, and tail rubbing. A condition described as food allergy in white hogs on new clover pasture consisted of generalized erythema and skin pain, depression, and reluctance to move. However, the description of this condition is more suggestive of an adverse food reaction, such as photosensitization, than of food hypersensitivity.
The microscopic lesions associated with food allergy are variable and are not diagnostic. The epidermis is variably acanthotic and may be multifocally spongiotic. Crusting, erosion, and ulceration may be present. The superficial dermis is mildly to moderately edematous, and inflammation is variable. In dogs, inflammation may be perivascular, interstitial, or diffuse. The cells are mixed and include lymphocytes, macrophages, eosinophils, and mast cells. Neutrophils and plasma cells are present in numbers proportional to the degree of self-trauma. Sebaceous and epitrichial glands may be hyperplastic in chronic lesions. Rarely, eosinophilic vasculitis has been described in dogs with CARF. In cats, dermal inflammation may be a superficial perivascular mononuclear dermatitis but more commonly is characterized by eosinophilic inflammation that is perivascular to diffuse and extends into the subcutis. Mast cell numbers are commonly moderately to markedly increased throughout the dermis. Collagen flame figures may occur in areas of intense eosinophilic inflammation. Eosinophilic folliculitis and furunculosis and lesions of eosinophilic plaque are present in some cases of food allergy in cats. The microscopic lesion ascribed to food allergy in large animals is superficial perivascular dermatitis, with eosinophils comprising a significant proportion of the inflammatory cells.
The diagnosis of food allergy is made by a combination of appropriate clinical history, exclusion of other pruritic conditions, and resolution of pruritus with feeding of a novel protein diet. Intradermal skin testing and measurement of serum allergen-specific IgE levels have been found to be unreliable for diagnosis of food allergy in animals.
Further reading
Chesney CJ. Food sensitivity in the dog: a quantitative study. J Small Anim Pract 2002;43:203-207.
Guilford WG, et al. Food sensitivity in cats with chronic idiopathic gastrointestinal problems. J Vet Intern Med 2001;15:7-13.
Hardy JI, et al. Food-specific serum IgE and IgG reactivity in dogs with and without skin disease: lack of correlation between laboratories. Vet Dermatol 2014;25:447-e70.
Ishida R, et al. Antigen-specific histamine release in dogs with food hypersensitivity. J Vet Med Sci 2003;65:435-438.
Jackson HA. Diagnostic techniques in dermatology: the investigation and diagnosis of adverse food reactions in dogs and cats. Clin Tech Small Anim Pract 2001;16:233-235.
Marsella R. Hypersensitivity disorders. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 363-431.
Mueller R, Tsohalis J. Evaluation of serum allergen-specific IgE for the diagnosis of food adverse reactions in the dog. Vet Dermatol 1998;9:167-171.
Paterson S. Food hypersensitivity in 20 dogs with skin and gastrointestinal signs. J Small Anim Pract 1995;36:529-534.
Sampson HA. Food allergy. Part I: Immunopathogenesis and clinical disorders. J Allergy Clin Immunol 1999;103:717-728.
Scott DW, Miller WH. Skin immune system and allergic skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 263-313.
Sicherer SH, Sampson HA. Food hypersensitivity and atopic dermatitis: pathophysiology, epidemiology, diagnosis, and management. J Allergy Clin Immunol 1999;104:S114-S122.
Verlinden A, et al. Food allergy in dogs and cats: a review. Crit Rev Food Sci Nutr 2006;46:259-273.
Vogelnest LJ, Cheng KY. Cutaneous adverse food reactions in cats: retrospective evaluation of 17 cases in a dermatology referral population (2001-2011). Aust Vet J 2013;91:443-451.
Allergic contact dermatitis
Allergic contact dermatitis is an uncommon hypersensitivity condition in domestic animals. Although considered a typical delayed (type IV) hypersensitivity reaction, there is considerable overlap in pathogenesis between allergic contact dermatitis and primary irritant dermatitis, and the rigid distinction between the 2 conditions is becoming blurred. It has been estimated to account for 1-10% of dermatoses in dogs. The low incidence, as compared to that in humans, is thought to be due to the natural protection afforded by the haircoat of most animals and by the decreased exposure to potential allergens in cosmetics and industrial chemicals.
Allergic contact dermatitis is caused by contact with a nonirritating concentration of a substance to which an individual has previously become sensitized. The compounds involved are usually lipid-soluble haptens (low-molecular-weight substances) that become immunogenic only after penetrating the epidermis and binding covalently to an autologous structural or cell surface protein to form a complete antigen. This antigen is subsequently internalized and processed by Langerhans cells and presented to CD4+ T cells. Langerhans cells are crucial to development of allergic contact dermatitis, as depletion of these cells results in a decreased ability to induce contact sensitization. During the induction phase of the reaction, Langerhans cells present antigen to CD4+ cells in the paracortical region of regional lymph nodes, where the specifically sensitized T cells undergo clonal expansion and then circulate as memory cells in blood and home to skin by virtue of adhesion molecules that bind to addressins on endothelial cells. Development of allergic contact dermatitis depends on the nature of the allergen, frequency of contact, and state of the skin. Factors that damage the integrity of the protective barrier of the skin predispose to development of allergic contact dermatitis. The induction phase is typically a prolonged process, estimated to require 6-24 months to develop. Although strong immunogens can elicit sensitivity after as short a period of contact as 7-21 days, most contact allergens are weaker immunogens and require chronic repeated exposure for sensitization to develop. Upon subsequent exposure to the contact allergen, specifically sensitized T cells in skin and circulation are presented the antigen by Langerhans cells (elicitation phase), become activated, and elaborate various cytokines that attract and activate other inflammatory cells and stimulate proliferation of the epidermis. Only a very small fraction (<1%) of the infiltrating T cells are specific for a relevant antigen. Thus various amplification and recruitment mechanisms are involved in induction of the reactions. The activated T cells secrete a Th1 profile of cytokines, including interferon-γ (IFN-γ) and TNF-β, which recruit and activate a wide variety of inflammatory cells, affect keratinocyte function and differentiation, and induce expression of adhesion molecules on endothelial cells and keratinocytes. TNF-β and IFN-γ induce expression of intercellular adhesion molecule-1 (ICAM-1) on keratinocytes and endothelium, which promotes homing of T cells to the dermis and epidermis. Unlike the delayed-type hypersensitivity reaction that develops in response to antigen injected into the dermis, which primarily involves CD4+ cells, the response to hapten painted on the epidermis involves both CD4+ and CD8+ T cells. Local production of cytokines induces arrival of more T cells and further amplification of proinflammatory mechanisms. Irritated keratinocytes also release a variety of cytokines that induce or augment the inflammatory response.
Allergic contact dermatitis has been reported most frequently in dogs and horses, although most cases have not been confirmed by patch testing. Numerous plants and chemicals have been suspected or shown to cause allergic contact dermatitis in animals. In dogs, wandering Jew (Tradescantia fluminensis), spreading dayflower (Cornelina diffusa), doveweed (Murdannia nudiflora), leaves and bulbs of plants in the family Amaryllidaceae, dandelion leaves, cedar wood, and Asian jasmine have been implicated in cases of allergic contact dermatitis. Cobalt and nickel ions, pine oil resin found in cleaning products, topical medications such as neomycin, rubber, cement, and various fragrances such as those in shampoos and carpet deodorizers are a few of the chemical causes of allergic contact dermatitis in dogs and cats. Hairless dogs may have an increased frequency of allergic contact dermatitis. Contact hypersensitivity has been document in Mexican hairless dogs housed in stainless steel cages (chromium metal). In horses, pasture plants, insecticides, various dyes and preservatives of tack items, soaps, and bedding materials have been suggested as causes of allergic contact dermatitis.
The clinical course is typically prolonged, and lesions in dogs are usually confined to sparsely haired areas of the body, such as the lips, chin, ventral cervical and thoracic areas, abdomen, scrotum, perineum, and ventral interdigital skin. Footpads are usually protected by the thick stratum corneum; however, cracking of footpads of all 4 feet was a feature described in a cat with suspected allergic contact dermatitis to carpet deodorizer. Lesion distribution is also dependent on the contactant involved. Primary lesions include erythema, papules, plaques, and vesicles, but these are very transient and thus rarely seen. Pruritus is variable, ranging from mild to severe. Chronic secondary lesions are more commonly seen and include alopecia, lichenification, scaling, crusting, excoriations, and pigmentary changes. Secondary bacterial or fungal infection may complicate lesions.
Microscopic changes described in various reports of allergic contact dermatitis in animals have been conflicting. Differences in histologic lesions no doubt reflect, at least in part, differences in stage of the reaction. Whereas neutrophils have been the predominant cell type seen in some cases, lymphocytes or eosinophils predominated in others. The epidermis may be variably spongiotic and may develop vesicles in some areas. In allergic contact dermatitis produced experimentally in dogs by topical application of 1-chloro-2,4-dinitrochlorobenzene (DNCB), histologic changes at 48 and 72 hours postchallenge included mild acanthosis, mild dermal edema, and perivascular and perifollicular infiltrations of lymphocytes and macrophages. Mild and focal to widespread and marked epidermal necrosis may occur, both in patch test reaction sites as well as in spontaneous lesions. Exocytosis of inflammatory cells is a common feature, but the cells vary and may be neutrophils, lymphocytes, eosinophils, or a combination thereof. The superficial dermis may be edematous, and the predominant inflammatory cells may be lymphocytes, neutrophils, or eosinophils. Inflammation may be perivascular, diffuse interstitial, or lichenoid and frequently perifollicular. The histologic changes of allergic contact dermatitis are frequently indistinguishable from those caused by irritant contact dermatitis.
The list of differential diagnoses is extensive and includes a wide variety of allergic and parasitic conditions, bacterial and fungal infections, and irritant contact dermatitis. When a single animal of a group is affected, allergic contact dermatitis is considered more likely than irritant dermatitis. Diagnosis is based on history, physical examination findings, exclusion of other dermatoses, and is confirmed by restriction followed by provocative exposure to the suspected allergen or patch testing.
Further reading
Jörundsson E, et al. Prominence of γδ T cells in the elicitation phase of dinitrochlorobenzene-induced contact hypersensitivity in lambs. Vet Pathol 1999;36:42-50.
Kimura T. Contact hypersensitivity to stainless steel cages (chromium metal) in hairless descendants of Mexican hairless dogs. Environ Toxicol 2007;22:176-184.
Leung DYM, et al. Allergic and immunologic skin disorders. J Am Med Assoc 1997;278:1914-1923.
Marchal IS-A, et al. Feline Langerhans cells migrate from skin and vaginal mucosa to regional lymph nodes during experimental contact sensitization with fluorescein isothiocyanate. Vet Dermatol 1998;9:9-17.
Marsella R, et al. Use of pentoxifylline in the treatment of allergic contact reactions to plants of the Commelinceae family in dogs. Vet Dermatol 1997;8:121-126.
Thomsen MK, Thomsen HK. Histopathological changes in canine allergic contact dermatitis patch test reactions. A study on spontaneously hypersensitive dogs. Acta Vet Scand 1989;30:379-384.
Walder EJ, Conroy JD. Contact dermatitis in dogs and cats: pathogenesis, histopathology, experimental induction and case reports. Vet Dermatol 1994;5:149-162.
Insect hypersensitivity
Insects are cosmopolitan in their distribution, and virtually all animals are exposed to them. Many insects are capable of inducing allergic reactions, including various dermatoses. Antigens of insect origin that produce hypersensitivity are usually proteins, and sources include venom, saliva, whole bodies, shed skins, egg capsules, feces, and insect hemoglobin. These antigens can be introduced via the bite or sting of insects or by inhalation, ingestion, or percutaneous absorption. In general, lesions associated with insect hypersensitivity are seasonal or seasonally more severe and involve short- or sparsely haired regions, such as the nose, muzzle, pinnae, inguinal area, and distal extremities. Lesions typically consist of pruritic crusted papules and are characterized histologically by eosinophilic inflammation.
The most well-known insect hypersensitivities of veterinary significance are those caused by an allergic reaction to salivary antigens, and these are flea-bite hypersensitivity of dogs and cats and Culicoides hypersensitivity of horses. Hypersensitivity to mosquito bites has been recognized in cats, and an eosinophilic furunculosis of the face of dogs is suspected to be a hypersensitivity response to the sting or bite of various insects. The first 3 of these conditions will be discussed in this section. Canine eosinophilic furunculosis of the face is discussed under Eosinophilic dermatitides.
Flea-bite hypersensitivity is a pruritic dermatitis caused by hypersensitivity to allergens in the saliva of fleas. It is the most common allergic dermatosis of dogs and cats in flea-endemic regions. The cat flea, Ctenocephalides felis felis, is the major initiator of the condition. Because many animals harbor large numbers of fleas without any apparent skin abnormalities, it is likely that animals develop skin disease as a result of flea infestation only if they are allergic to fleas.
Both type I and type IV hypersensitivity reactions are believed to be involved in the pathogenesis of flea-bite hypersensitivity. Participation of immediate hypersensitivity is supported by the fact that clinically allergic animals develop immediate skin reactions in response to intradermal injection of flea antigen and that IgE antibodies to flea antigen are demonstrable in sera from allergic animals. Histologic evidence also supports a role for immediate hypersensitivity and suggests that cell-mediated/delayed hypersensitivity is involved in the pathogenesis of flea allergy as well. Many flea-allergic animals also have delayed skin test reactions—further support for a type IV hypersensitivity component. Upregulation of mast cell proteases has been demonstrated during sensitization, with selective release of mast cell tryptase after exposure to flea antigen.
No breed or sex predilections have been reported in flea-bite hypersensitivity, and in cats, no age predilection has been recognized. In dogs, disease occurs most commonly between 3 and 5 years of age, unless naive dogs are moved to a flea-endemic area at a later age. Disease is rare prior to 6 months. Signs tend to be more severe in summer and fall in animals living in areas with cold winters but are year-round in those living in warm regions or where indoor infestation persists. Affected individuals may have other hypersensitivity conditions, such as atopic dermatitis (AD) or food allergy.
Flea-bite hypersensitivity in dogs is characterized by pruritus, erythema, wheals, and papules that may become crusted. Primary lesions are usually obscured by secondary lesions that develop in response to chronic pruritus. These may include hyperkeratosis, lichenification, hyperpigmentation, alopecia, excoriations, redundant skin folds on the rump and caudal thighs, and seborrhea. Lesions typically involve the dorsal lumbosacral area, flanks, caudal and medial aspect of the thighs, and ventral abdomen. In severely hypersensitive dogs, lesions may become generalized. Pyotraumatic dermatitis (“hot spots”) and bacterial pyoderma are common secondary complications. Firm alopecic nodules (“fibropruritic nodules”) may develop on the dorsal lumbosacral region secondary to self-trauma in chronically affected dogs. Differential diagnoses include other hypersensitivity conditions (AD, food allergy), sarcoptic mange, cheyletiellosis, and bacterial or yeast infection.
The lesions of flea-bite hypersensitivity in cats are extremely variable. The most common manifestation is multiple erythematous pruritic papules covered by brown crust (“miliary dermatitis”) on the dorsal lumbosacral area, flanks, caudal and medial aspect of the thighs, ventral abdomen, and neck. In some cats, the condition may be manifested as overzealous grooming rather than scratching, producing alopecia that may be ventral abdominal, bilaterally symmetrical along the lateral aspect of the trunk, or dorsal lumbosacral. The skin may appear completely normal grossly, or excoriations, crusts, scales, and hyperpigmented macules may be seen. Fleas or flea dirt may not be evident because of the fastidious grooming behavior typical of most cats. Eosinophilic granuloma complex lesions have also been associated with flea-bite hypersensitivity in cats. Secondary bacterial pyoderma is uncommon. Differential diagnosis is extensive because the manifestations of flea allergy are so varied in cats. The most common differentials for miliary dermatitis include other hypersensitivity conditions (AD, food hypersensitivity), dermatophytosis, and cheyletiellosis. Cases characterized by self-induced alopecia with normal-appearing skin may resemble an endocrinopathy.
Histopathology is useful in confirming the suspected diagnosis of a hypersensitivity condition, but the microscopic changes associated with flea-bite hypersensitivity are similar to those seen in other hypersensitivities, and the specific diagnosis cannot be made histologically. The epidermis is variably acanthotic, and foci of spongiosis and serocellular crusting are commonly seen. Mixed orthokeratotic and parakeratotic hyperkeratosis and self-induced erosion or ulceration may be present. Foci of epidermal necrosis and intraepidermal eosinophilic pustules may be evident. The superficial dermis is mildly to moderately edematous, and perivascular to interstitial infiltration of eosinophils, lymphocytes, fewer macrophages, and mast cells is present in the superficial to mid-dermis in dogs and may extend into the subcutis in cats. The proportion of eosinophils in relation to mononuclear cells varies, with eosinophils being most numerous in early lesions and mononuclear cells predominating in more chronic reactions. Melanophages are in variable numbers and may be numerous in chronic cases with prominent lichenification. Sebaceous and epitrichial glands may be hyperplastic in chronic lesions. Neutrophils are numerous in association with ulceration or bacterial infection. In cats, eosinophilic mural folliculitis and furunculosis have been seen in flea bites as have histologic lesions of eosinophilic granuloma complex.
Culicoides (insect) hypersensitivity is the most common allergic dermatosis of horses. It occurs worldwide, and Culicoides spp. gnats are the most common cause. The condition is known by a variety of colloquial names worldwide, including Queensland itch, kasen, dhobie itch, sweet itch, muck itch, summer itch, and summer eczema. It is a major annoyance to horse and owner, and substantial economic losses can be incurred from treatment, prevention, and damage caused by scratching horses. Culicoides hypersensitivity is an intensely pruritic dermatosis that can render affected animals too restless and anxious to perform.
The insects are also called biting midges, punkies, and “no-see-ums.” Hundreds of different species exist throughout the world, and they vary in their favored feeding sites and time of activity. They are most active when the ambient temperature is >10° C (50° F), when humidity is high, and when there is no breeze because they are weak fliers. The insects are in highest numbers in wetlands and swampy areas.
The hypersensitivity to salivary antigens of Culicoides gnats is thought to be mediated by both type I and type IV hypersensitivity reactions. Support for immediate hypersensitivity is provided by immediate skin test reactivity to Culicoides antigens, presence of specific IgE in affected horses, and peripheral eosinophilia and increased blood histamine concentrations during periods of insect activity. The presence of increased numbers of primarily CD4+ T lymphocytes and eosinophils in skin test reactions is also consistent with immediate hypersensitivity. Also, sulfidoleukotriene generation from peripheral blood leukocytes in response to Culicoides extract was increased in horses with insect hypersensitivity, indicating involvement of IgE-mediated hypersensitivity in the pathogenesis of Culicoides hypersensitivity. Delayed reactions (up to 48 hours) to intradermal skin tests suggest that type IV hypersensitivity may also be involved in the pathogenesis of the condition.
Culicoides hypersensitivity is typically a seasonal disease, but in warm climates it may be a problem virtually year-round. Horses of any breed and either sex are affected; pedigree studies suggest there may be a genetic basis. Lesions are uncommon in horses <2 years of age; however, in tropical and subtropical climates with a long insect season, sensitization and mild clinical disease may develop within the first year of exposure. The favored feeding sites vary with the species of Culicoides endemic to a particular environment, accounting for the varied distribution of skin lesions. Distribution may be dorsal and involve the head, ears, neck, withers, back, and tailhead, or it may be primarily ventral and involve the intermandibular space, legs, and ventral midline. In some areas, such as Florida in the United States, multiple species of Culicoides are active at different times and have different favored feeding sites, such that disease may be generalized. The primary lesions are pruritic papules that may be recognized initially by clusters of erect hairs and commonly become encrusted. Because of severe pruritus, however, self-mutilation obscures the primary lesions and results in more commonly observed secondary lesions, such as excoriations, crusts, lichenification, pigmentary changes, broken hairs, alopecia, and a short stubbled tail (“rat tail”) (Fig. 6-67 ). The mane may be rubbed off, and the skin over the neck and withers may become thickened and rugose. Lesions typically heal during winter and recur in spring or summer and commonly worsen with age. Affected horses may scratch and bite themselves and rub objects in their environment, thereby causing damage to themselves, their riders, and environmental objects. Constant anxiety and restlessness may prevent severely affected animals from performing as riding or show animals. Also, because sweating exacerbates pruritus, affected horses cannot be worked vigorously. The differential diagnoses include ectoparasitism and other hypersensitivity dermatoses. The diagnosis is based on seasonality of the condition, location and appearance of lesions, sporadic occurrence of the condition in a group, eliminating other diseases, and response to therapy.
Figure 6-67.

Culicoides hypersensitivity in a horse. Alopecia at the tail head caused by self-trauma (“rat tail”).
(Courtesy N. Radwanski.)
The histologic lesions of Culicoides hypersensitivity are typically superficial or superficial and deep perivascular dermatitis consisting of eosinophils and lymphocytes primarily. The epidermis is variably acanthotic, spongiotic, and hyperkeratotic with foci of parakeratosis, and may be focally necrotic. Increased numbers of T lymphocytes and Langerhans cells are present in the basal portion of the epidermis. Erosions and ulceration may be present as a result of self-trauma and are associated with neutrophilic inflammation. The dermis is variably edematous and increased numbers of mast cells, which may be degranulated, are present. In some cases, eosinophilic inflammation is diffuse, and collagen flame figures or eosinophilic folliculitis may also be seen.
A seasonal pruritic dermatosis attributed to Culicoides hypersensitivity has also been described in cattle, sheep, and donkeys. Affected sheep were 2-5 years of age and had an intensely pruritic, exudative dermatitis with loss of wool and marked skin thickening of the abdomen, udder, teats, and legs. Lesions in adult dairy cattle consisted of marked thickening and folding of the skin of the head, ears, and neck. Donkeys developed exudative dermatitis, alopecia, crusting, and skin thickening of the legs and head. Affected animals were restless and often bit at themselves, suggesting that they were intensely pruritic. Histologic examination of biopsies from affected sheep and cows showed primarily an eosinophilic dermal infiltrate.
Mosquito-bite hypersensitivity dermatitis is documented in the Mosquito-bite dermatitis section.
Further reading
Benarafa C, et al. Role of the chemokine eotaxin in the pathogenesis of equine sweet itch. Vet Rec 2002;151:691-693.
Bevier DE. Insect and arachnid hypersensitivity. Vet Clin North Am Small Anim Pract 1999;29:1385-1405.
Fadok VA. Update on equine allergies. Vet Clin North Am Equine Pract 2013;29:541-550.
Friberg CA, Lewis DT. Insect hypersensitivity in small animals. Compend Contin Educ Pract Vet 1998;20:1121-1131.
Greiner EC. Entomologic evaluation of insect hypersensitivity in horses. Vet Clin North Am Equine Pract 1995;11:29-41.
Hobi S, et al. Clinical characteristics and causes of pruritus in cats: a multicentre study on feline hypersensitivity-associated dermatoses. Vet Dermatol 2011;22:406-413.
Kunkle GA, et al. Pilot study to assess the effects of early flea exposure on the development of flea hypersensitivity in cats. J Feline Med Surg 2003;5:287-294.
Kurotaki T, et al. Immunopathological study on equine insect hypersensitivity (“Kasen”) in Japan. J Comp Pathol 1994;110:145-152.
Lam A1, Yu A. Overview of flea allergy dermatitis. Compend Contin Educ Vet 2009;31:E1-E10.
Lee SE, et al. Putative salivary allergens of the cat flea, Ctenocephalides felis felis. Vet Immunol Immunopathol 1999;69:229-237.
Lewis DT, et al. Clinical and histological evaluation of immediate and delayed flea antigen intradermal skin test and flea bite sites in normal and flea-allergic cats. Vet Dermatol 1999;10:29-37.
Marti E, et al. On the genetic basis of equine allergic diseases: II. Insect bite dermal hypersensitivity. Equine Vet J 1992;24:113-117.
Marti E, et al. Sulfidoleukotriene generation from peripheral blood leukocytes of horses affected with insect bite dermal hypersensitivity. Vet Immunol Immunopathol 1999;71:307-320.
McKelvie J, et al. Characterisation of lymphocyte subpopulations in the skin and circulation of horses with sweet itch (Culicoides hypersensitivity). Equine Vet J 1999;31:466-472.
von Ruedorffer U, et al. Flea bite hypersensitivity: new aspects on the involvement of mast cells. Vet J 2003;165:149-156.
Wilson AD, et al. Detection of IgG and IgE serum antibodies to Culicoides salivary gland antigens in horses with insect dermal hypersensitivity (sweet itch). Equine Vet J 2001;33:707-713.
Yeruham I, et al. Field observations in Israel on hypersensitivity in cattle, sheep and donkeys caused by Culicoides. Aust Vet J 1993;70:348-352.
Hormonal hypersensitivity
Pruritic dermatitis resulting from hypersensitivity to endogenous sex hormones is recognized in women (“autoimmune progesterone dermatitis”) and is very rare in dogs. Results of intradermal skin tests with aqueous progesterone in women indicate that type I and/or type IV hypersensitivity are involved. Most canine cases are in intact females, frequently with a history of irregular estrus or recurrent pseudopregnancy. The condition is characterized by intense pruritus that develops or is exacerbated near the time of estrus or pseudopregnancy but tends to become more severe and protracted with each episode; pruritus is generally perennial in male dogs. Bilaterally symmetrical erythema and crusted papules typically begin in the dorsal lumbosacral, perineal, genital, and caudomedial thigh areas and progress cranially. In chronic cases, the condition is generalized, and the skin becomes alopecic and lichenified. Pruritus is usually unresponsive to glucocorticoid treatment. Differential diagnoses include other allergic conditions and sarcoptic mange. The microscopic lesion is a hyperplastic superficial perivascular dermatitis in which neutrophils, mononuclear cells, or eosinophils may predominate. Diagnostic clues include poor response to glucocorticoid therapy and development or exacerbation of cutaneous signs coincident with estrus or pseudopregnancy. Gonadectomy is curative.
Further reading
Scott DW, Miller WH. Probable hormonal hypersensitivity in two male dogs. Canine Pract 1999;17:14-17, 20.
Intestinal parasite hypersensitivity
Hypersensitivity to intestinal parasites has been suspected of causing pruritic dermatoses in dogs, cats, horses, and humans. The pathomechanism is unknown, but a type I hypersensitivity reaction has been proposed. Ascarids, coccidia, hookworms, tapeworms, and whipworms have rarely been associated with pruritic dermatoses that resolve with elimination of the intestinal parasites. Lesions that have been attributed to intestinal parasite hypersensitivity include multifocal or generalized papulocrustous eruptions, pruritic seborrheic disease, pruritic urticaria, and pruritus without skin lesions. The histologic changes described are superficial perivascular dermatitis with variable numbers of eosinophils, ranging from few to many. Diagnosis is based on fecal examination and resolution of the skin lesions following appropriate parasiticidal therapy.
Further reading
Cooper PJ. Intestinal worms and human allergy. Parasite Immunol 2004;26:455-467.
Marsella R, et al. Hypersensitivity disorders. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 417.
Autoimmune dermatoses
The autoimmune skin diseases are uncommon to rare but merit detailed consideration as many are debilitating to life threatening and require specific therapy. Their characteristic microscopic lesions, combined with clinical information and careful interpretation of ancillary studies, often enable a specific diagnosis to be made. In the vast majority of cases, the stimulus triggering the aberrant T- or B-cell responses against self-antigens is unknown. Drug therapy, underlying neoplasia (see Paraneoplastic pemphigus), tissue injury, infectious diseases, other autoimmune diseases, and genetic makeup are all factors known to be associated with the occurrence of autoimmune diseases. Penicillinamine, for example, may precipitate clinically, histologically, and immunologically classic cases of pemphigus in humans, which regress when the drug is withdrawn. Drug-induced forms of pemphigus are thought to be the result of haptenization of keratinocyte antigens, rendering them immunogenic. One theory suggests environmental agents, such as drugs, influence T cells by causing DNA methylation abnormalities that, in turn, alter gene expression. Exposure to ultraviolet light is known to exacerbate cutaneous autoimmune disease, perhaps by inducing keratinocyte intercellular adhesion molecule-1 (ICAM-1) expression and keratinocyte production of proinflammatory cytokines. Still another theory suggests that the structural similarities of peptide fragments of some infectious agents to host proteins may trigger postinfectious autosensitization.
The recognition that one autoimmune disease, tissue injury, inflammatory or neoplastic process in an individual may precede the onset of cutaneous autoimmune disease led to investigation of the phenomenon termed epitope spreading. Epitope spreading refers to the process by which the targets of the autoimmune response do not remain fixed but drift to include other epitopes on the same protein or nearby proteins of the same tissue. This may account for regional variations in pemphigus antigen expression and the clinical variation of cutaneous autoimmune diseases. Epitope spreading may also account for aberrant immune responses developing to tissue antigens after the tissue has been injured, possibly leading to the release or exposure of a previously sequestered antigen.
Selection of fully-developed lesions is crucial to diagnosis. Demonstration of tissue-bound or circulating autoantibody using appropriate immunologic tests may be helpful in confirming the diagnosis of an autoimmune skin disease. However, such tests (e.g., direct and indirect immunofluorescence testing, immunohistochemistry) are fraught with interpretation pitfalls (false-positive or false-negative test results) and should never be interpreted in the absence of histologic examination. Demonstration of autoantibodies does not necessarily confirm causative roles for these antibodies, just as negative results do not necessarily exclude the diagnosis of a cutaneous autoimmune disease. For example, the various entities of the pemphigus complex are characterized by the deposition of immunoglobulin, with or without complement, on the surface of keratinocytes or at the basement membrane zone using the techniques of direct immunofluorescence (IF) testing or immunohistochemistry (IHC). Unfortunately, false-negative (poor lesion selection, prior glucocorticoid therapy) and false-positive (any dermatosis in which spongiosis or numerous lymphocytes and plasma cells are present) reactions are frequent. In addition, normal epithelium of the canine nasal planum and footpad often label nonspecifically. Hence these immunopathology tests can only be interpreted in the light of clinical and histopathologic findings. Indirect immunofluorescence testing has variable usefulness in domestic animals with pemphigus as results may be falsely negative, or “pemphigus-like” antibodies can be occasionally found in nonpemphigus diseases. Indirect IF testing for canine PF can be useful provided the appropriate substrate (bovine esophagus) is used. In many of the putative cases of autoimmune skin disease in animals, the criteria for autoimmunity have not been met fully.
Further reading
Bradley GA, Calderwood Mays MB. Immunoperoxidase staining for the detection of autoantibodies in canine autoimmune skin disease: comparison to immunofluorescence results. Vet Immunol Immunopathol 1990;26:105-113.
Chan LS, et al. Epitope spreading: lessons from autoimmune skin diseases. J Invest Dermatol 1998;110:103-109.
Day MJ, et al. Immune-mediated skin disease in the dog and cat. J Comp Pathol 1993;109:395-407.
Iwasaki T, et al. Effect of substrate on indirect immunofluorescence tests for canine pemphigus foliaceus. Vet Pathol 1996;33:332-336.
Kalaher KM, et al. Direct immunofluorescence testing of normal feline nasal planum and footpad. Cornell Vet 1990;80:105-109.
Rose NR. The role of infection in the pathogenesis of autoimmune diseases. Semin Immunol 1998;10:5-13.
Rubin RL. Etiology and mechanisms of drug-induced lupus. Curr Opin Rheumatol 1999;11:357-363.
White SD, et al. Putative drug-related pemphigus foliaceus in four dogs. Vet Dermatol 2002;13:195-202.
Zipfel W, et al. Demonstration of immunoglobulins and complement in canine and feline autoimmune and non-autoimmune skin diseases with the direct immunofluorescence and indirect immunoperoxidase method. J Vet Med 1992;39:494-501.
Autoimmune diseases characterized by vesicles, pustules, or bullae as the primary lesion
The pemphigus complex.
Pemphigus refers to a group of autoimmune skin diseases characterized clinically by pustules, vesicles, bullae, erosions, and ulcers and histologically by loss of adhesion between cells (acantholysis). Autoantibodies directed against antigens within stratified squamous epithelia, including haired skin, mucocutaneous junctions, oral and genital mucosa, and esophagus, develop and can be detected via immunologic assays. Classic pemphigus in humans is divided into pemphigus vulgaris and pemphigus foliaceus. The clinical phenotypes correlate with the autoantibody profile in the skin. Autoantibodies are directed against components of keratinocyte transmembrane glycoproteins (i.e., extracellular domains of desmoglein 1 or desmoglein 3) that are responsible for keratinocyte cell-to-cell adherence. The autoantibodies cause loss of cohesion between keratinocytes (acantholysis) and blister formation. In pemphigus vulgaris, blisters occur in the lower layers of the epidermis (suprabasilar), where the antibody targets desmoglein-3, the predominant antigen at this location on mucous membranes. Pemphigus foliaceus lesions occur only on haired skin, and the antibody targets desmoglein-1, which resides in upper layers of the epidermis. Pemphigus vulgaris can have both mucous membrane and haired skin involvement if there is concurrent autoantibody formation to desmoglein-1. IgG autoantibodies can also occur in humans with paraneoplastic pemphigus.
The mechanisms leading to acantholysis are not completely understood. Antigen-antibody binding may result in a type II immune reaction or promote proinflammatory cytokine release from keratinocytes. The binding of pemphigus autoantibodies to keratinocyte antigens is associated with the synthesis and secretion of urokinase-type plasminogen activator (uPA), a serine protease that activates plasminogen. Activation of plasminogen may indirectly induce the cleaving of intercellular contacts. Anti-uPA antibodies or the specific inhibitor of uPA, plasminogen activator inhibitor type-2, inhibit lesion formation in vitro. Another hypothesis proposes that the binding of autoantibodies to keratinocyte antigens may disrupt the structural integrity of the adhesion molecule. Experimental studies in mice have demonstrated that acantholysis in pemphigus foliaceus (PF) can occur with passive transfer of PF IgG autoantibody as well as with transfer of Fab fragments and F (ab′)2 fragments in both complement-sufficient and complement-deficient mice.
Pemphigus foliaceus is the most common form of pemphigus in domestic animals and has been reported in the dog, cat, horse, goat, and a Barbary sheep. In humans, PF autoantibodies recognize the desmosomal protein, desmoglein 1. In contrast to humans, desmoglein 1 is only a minor autoantigen in dogs; the major autoantigen is desmocollin-1. Desmocollin-1 is a transmembrane calcium-dependent desmosomal glycoprotein involved in intercellular adhesions. Desmocollin-1 is found primarily in the upper layers of the epidermis, where PF pustules typically arise. Pemphigus foliaceus often arises spontaneously; however, cases have been triggered by adverse drug reactions as well as topical flea and tick preventatives. PF has no sex predilection in dogs, but Akitas, Chow Chows, Bearded Collies, Collies, Chinese Shar-Peis, Dachshunds, Newfoundlands, Doberman Pinschers, Schipperkes, English Springer Spaniels, and Appaloosa horses appear predisposed. In dogs, most cases occur before 5 years of age. In all species, the clinical lesions are nonpruritic to mildly pruritic pustules that rupture and form thick crusts with scaling. On the face, the skin lesions are often bilaterally symmetrical (Fig. 6-68 ). Dogs and cats may have pawpad hyperkeratosis and crusting with involvement of the claw fold (paronychia). In cats, thick crusts are often bilaterally symmetrical on the face and ears (particularly pinnal margins) (Fig. 6-69 ). PF is the most common autoimmune skin disease in horses; lesions often begin on the face or distal extremities, or may be localized to coronets. In any species, the lesions may become generalized (Fig. 6-70A, B ). Foals may also be affected with a benign form of PF that responds rapidly to treatment or may resolve spontaneously. Pain and pruritus may be present.
Figure 6-68.

Pemphigus foliaceus in a Chow Chow. Note the thick pustules and crusts on the muzzle, nose, periocular area, and apical pinnae.
Figure 6-69.

Pemphigus foliaceus in a cat. Note the thick crusts in the haired skin of the nasal area.
Figure 6-70.


Pemphigus foliaceus in a horse. A. Generalized exfoliative dermatitis and alopecia. B. Detail of skin showing massive build-up of scales and crusts.
(Courtesy K. Moriello.)
The histologic pattern of pemphigus foliaceus is a superficial intraepidermal pustular dermatitis that typically involves the corneal layer and granular cell layer (see Figs. 6-1 and 6-17). Either neutrophils or eosinophils may predominate. At the base of the pustule, acantholytic keratinocytes continue to detach and enter the pustule. Ruptured pustules form a thick inflammatory crust in which acantholytic cells are prominent. The external root sheath of the hair follicle undergoes a similar acantholytic process. Dermal infiltrates consist of mild perivascular to interstitial neutrophils or eosinophils. There is dermal edema, vascular congestion, and occasionally hemorrhage. Rarely, a lichenoid inflammatory infiltrate is seen. Deposition of IgG at intercellular bridges in all layers of the suprabasilar epidermis or in the superficial epidermis demonstrated by IF or IHC is characteristic, but not specific, for PF. Secondary bacterial infection may complicate lesions. The primary differential for PF is superficial bacterial folliculitis. Acantholytic cells are more numerous and can more often be found in rafts in PF than in superficial folliculitis. The “cling-on” stratum granulosum cells are only present in PF. In PF, pustules also span the interfollicular epidermis encompassing multiple follicles, whereas in superficial folliculitis pustules are more likely to be centered on single follicles. Evidence of recornification and reformation of pustules is often prominent in PF. Dermatophytosis and superficial pyoderma (impetigo) can also have similar gross and histologic lesions. Careful examination of skin sections with fungal and bacterial stains and possibly cultures may be needed for differentiation. Impetigo does not involve hair follicles, whereas PF may.
Pemphigus erythematosus (PE) and pemphigus vegetans are terms that have been loosely applied to veterinary diseases based on human comparisons. Further studies suggest the conditions are not directly comparable. Criteria for diagnosis and differentiation from PF were dependent upon the immunologic demonstration of both a diffuse cell surface IF or IHC pattern typical of the pemphigus group and a linear band of immunoglobulin, with or without complement, deposited at the basement membrane zone. For reasons stated previously, IF and IHC are not dependable. Pemphigus erythematosus is a poorly characterized facially oriented PF in dogs and cats. It is unclear if PE is indeed different from PF, a localized variant of PF, or if the disease is a crossover between discoid lupus and PF. Reported cases of pemphigus vegetans in veterinary patients are very limited and originally thought to be benign variants of pemphigus vulgaris. A documented case of pemphigus vegetans has been reported in a Greater Swiss Mountain dog. The dog had verrucous superficial PF pustules/crust and deep epidermal pemphigus vulgaris lesions. Panepidermal pustular pemphigus (PPP) is a term previously used to describe a deep epidermal form of pemphigus in the dog that encompassed some of the features of pemphigus foliaceus, pemphigus vegetans, and pemphigus erythematosus. PPP is now thought to be a histologic variant of PF.
Pemphigus vulgaris (PV) is the most severe and rare form of pemphigus in animals. This life-threatening disease has been reported in the dog, cat, horse, goat, monkey, and llama. There is no apparent breed or sex predilection. Middle-aged dogs are most commonly affected. In humans and dogs, PV autoantibodies recognize the desmosomal protein desmoglein 3. Desmoglein 3 also belongs to the cadherin family of cell-adhesion molecules and is most prominent in the area of the basal layer of keratinocytes of the epidermis and mucosal epithelium, hence lesions occur deeper in the epidermis and in the oral mucosa. The fragile vesicles or bullae in the epidermis are extremely transient and readily rupture to leave the more common presenting lesion of a roughly circular, shallow, flat-based erosion or ulcer. Firm sliding pressure to adjacent unaffected skin may induce fresh vesicle formation or dislodge the skin (the Nikolsky sign). Lesions involve mucous membranes (Fig. 6-71A ), mucocutaneous junctions and skin in the mechanically stressed areas, such as the inguinal and axillary regions. Oral involvement is present in 90% of cases, and in 50% of cases, the lesions commence in the mouth. Involvement of the nailbeds occurs also, and corneal ulceration may be present. Animals may be febrile, depressed, and anorectic and have leukocytosis. Drooling is often a presenting complaint.
Figure 6-71.

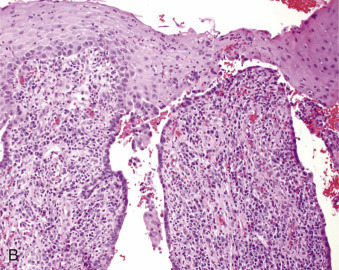
Pemphigus vulgaris in a Rottweiler. A. The nasal planum and lips are markedly ulcerated. B. Separation of the epidermis occurs between the stratum spinosum and stratum basale. Basal keratinocytes also lose intercellular contact, leaving the basal layer arranged to resemble a “row of tombstones.”
Microscopically, the earliest lesions consist of spongiosis and vacuolation of the suprabasilar epidermis progressing to suprabasilar acantholysis with intraepidermal clefts, vesicles, or bullae between the stratum basale and the stratum spinosum (Fig. 6-71B). The basal keratinocytes, although separated from each other following disruption of intercellular contacts, are anchored to the basal lamina resembling a “row of tombstones.” The outer layers of the epidermis form the roof of the vesicle that may contain a few acantholytic keratinocytes, singly or in clumps, but few or no inflammatory cells. The process may extend into the hair follicle epithelium. The dermal reaction in haired skin varies from a mild superficial perivascular to interstitial accumulation of mononuclear cells and eosinophils. A moderately intense lymphocytic-plasmacytic interface infiltrate may be present in mucosal lesions.
Clinical differentials include mucous membrane pemphigoid, erythema multiforme, bullous pemphigoid, toxic epidermal necrolysis, vesicular lupus erythematosus of Collies and Shetland Sheepdogs, mycosis fungoides, and other diseases resulting in oral ulcers. Histopathologic findings of primary lesions in PV are diagnostic.
Further reading
Bizikova P, et al. Cloning and establishment of canine desmocollin-1 as a major autoantigen in canine pemphigus foliaceus. Vet Immunol Immunopathol 2012;149:197-207.
Bizikova P, et al. Serum autoantibody profiles of IgA, IgE and IgM in canine pemphigus foliaceus. Vet Dermatol 2014;25:471-e75.
Brenner DJ, et al. Pemphigus foliaceus in a barbary sheep (Ammotragus lervia). Vet Rec 2009;165:509-510.
Eversole LR. Immunopathology of oral mucosal ulcerative, desquamative, and bullous diseases. Oral Surg Oral Med Oral Pathol 1994;77:555-571.
Gross TL, et al. Bullous and acantholytic diseases of the epidermis and the dermal-epidermal junction. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 27-38.
Gross TL, et al. Pustular diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 3-26.
Halliwell REW. Autoimmune and immune-mediated dermatoses. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 432-500.
Kuhl KA, et al. Comparative histopathology of pemphigus foliaceus and superficial folliculitis in the dog. Vet Pathol 1994;31:19-27.
Mattise AW. Canine pemphigus vegetans: a report of 16 cases. Proc Ann Meeting Am Acad Vet Dermatol Am Coll Vet Dermatol 1991;7:28.
Oberkirchner U, et al. Metaflumizone-amitraz (Promeris)-associated pustular acantholytic dermatitis in 22 dogs: evidence suggests contact drug-triggered pemphigus foliaceus. Vet Dermatol 2011;22:436-448.
Olivry T, et al. Desmoglein-3 is a target autoantigen in spontaneous canine pemphigus vulgaris. Exp Dermatol 2003;12:198-203.
Olivry T, Linder KE. Dermatoses affecting desmosomes in animals: a mechanistic review of acantholytic blistering skin diseases. Vet Dermatol 2009;20:313-326.
Preziosi DE, et al. Feline pemphigus foliaceus: a retrospective analysis of 57 cases. Vet Dermatol 2003;14:313-321.
Scott DW, Miller WH. Immune-mediated disorders. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 314-359.
Suter MM, et al. Ultrastructural localization of pemphigus vulgaris antigen on canine keratinocytes in vivo and in vitro. Am J Vet Res 1990;51:507-511.
Valdez RA, et al. Use of corticosteroids and aurothioglucose in a pygmy goat with pemphigus foliaceus. J Am Vet Med Assoc 1995;207:761-765.
Vandenabeele SI, et al. Pemphigus foliaceus in the horse: a retrospective study of 20 cases. Vet Dermatol 2004;15:381-388.
Winfield LD, et al. Pemphigus vulgaris in a Welsh pony stallion: case report and demonstration of antidesmoglein autoantibodies. Vet Dermatol 2013;24:269-e60.
Wurm S, et al. Comparative pathology of pemphigus in dogs and humans. Clin Dermatol 1994;12:515-524.
Paraneoplastic pemphigus.
Paraneoplastic pemphigus (PNP) is an aggressive form of pemphigus most often associated with solid or hematopoietic neoplasia. PNP has been documented in humans, 2 dogs, and a single putative case in a cat with thymic lymphoma and a horse with a sarcoma on the neck. Of the 2 cases reported in dogs, one had thymic lymphoma and the other an undifferentiated sarcoma in the spleen. Cutaneous lesions may precede detection of the neoplastic process. The condition is resistant to treatment. Lesions consist of severe mucosal and mucocutaneous blistering and erosions. Histologically, lesions have a combined pattern of erythema multiforme and suprabasilar acantholysis characteristic of pemphigus vulgaris. Lymphohistiocytic, lichenoid interface dermatitis, and apoptosis of keratinocytes with lymphocytic satellitosis throughout the epidermis are characteristic. Immunologically, labeling of intercellular bridges and/or basement membrane is detected by IHC or IFA staining. Direct immunofluorescence studies implicate autoantibodies to a 190-kDa protein, the 210- and 250-kDa desmoplakin proteins, and to the 230-kDa BPAGI, one of the bullous pemphigoid antigens. Antidesmoglein IgG was recently documented in the serum of canine PNP. Not all cases with the above-described lesions and autoantibodies have underlying neoplasia. Histologic differentials include panepidermal pustular pemphigus and those listed for PV and mucous membrane pemphigoid.
Further reading
Elmore SA, et al. Paraneoplastic pemphigus in a dog with splenic sarcoma. Vet Pathol 2005;42:88-91.
Halliwell REW. Autoimmune and immune-mediated dermatoses. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 432-500.
Hill PB, et al. Putative paraneoplastic pemphigus and myasthenia gravis in a cat with a lymphocytic thymoma. Vet Dermatol 2013;24:646-649.
Lemmens P, et al. Paraneoplastic pemphigus in a dog. Vet Dermatol 1998;9:127-134.
Nishifuji K, et al. IgG autoantibodies directed against desmoglein 3 cause dissociation of keratinocytes in canine pemphigus vulgaris and paraneoplastic pemphigus. Vet Immunol Immunopathol 2007;117:209-221.
Turek MM. Cutaneous paraneoplastic syndromes in dogs and cats: a review of the literature. Vet Dermatol 2003;14:279-296.
Mucous membrane pemphigoid.
Mucous membrane pemphigoid (MMP), also called cicatricial pemphigoid, is an autoimmune blistering disorder with a distinct clinical presentation of lesions localized to mucous membranes and mucocutaneous junctions. In dogs and cats, MMP is the diagnosis given to half of the patients with autoimmune subepidermal blistering diseases. The lesions typically appear as vesicles that ulcerate and then heal with scar tissue. In dogs, lesions typically arise on the nasal planum (Fig. 6-72A ), medial canthus, oral cavity, ear canals, and genitalia. The lesions arise in adult dogs and cats. German Shepherd dogs account for about 30% of canine cases. Despite the unique clinical presentation, autoantibodies may be found toward various components of the basement membrane proteins, including BPAG2 and laminin V. Histologically, the cases have subepidermal clefting with various degrees of inflammation (Fig. 6-72B).
Figure 6-72.

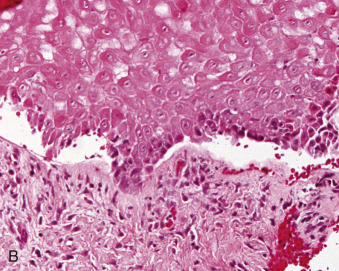
Mucous membrane pemphigoid in a dog. A. Ulcers on the nasal planum and dorsal muzzle. B. Subepidermal vesiculation. The basement membrane zone forms the floor of the vesicle. Note the lack of acantholysis.
Further reading
Olivry T, et al. A spontaneous canine model of mucous membrane (cicatricial) pemphigoid, an autoimmune blistering disease affecting mucosae and mucocutaneous junctions. J Autoimmun 2001;16:411-412.
Olivry T, et al. Laminin-5 is targeted by autoantibodies in feline mucous membrane (cicatricial) pemphigoid. Vet Immunol Immunopathol 2002;88:123-129.
Bullous pemphigoid.
Bullous pemphigoid (BP) is a chronic, autoimmune skin disease characterized clinically by vesicles, bullae, and ulcers, and histologically by subepidermal vesicles/bullae containing eosinophils or other leukocytes. In humans, the autoantibodies are directed against BP antigen 1 (BPAG1, a 230-kDa intercellular antigen) and BP antigen 2 (BPAG2, also called type XVII collagen, a 180-kDa hemidesmosomal transmembrane molecule). In animals, only BPAG2 has been identified. The mechanism of dermoepidermal separation is thought to be the result of the release of proinflammatory cytokines IL-1, IL-5, IL-6, IL-8, and others by keratinocytes altered by antigen-antibody interactions. Cytokines recruit neutrophils and eosinophils, leading to the release of damaging proteases. Separation of basal cells from the underlying dermis may also be the direct result of disorganization or internalization of components of the hemidesmosomes. In almost all cases, the stimulus triggering the immune response is unknown, although drugs may precipitate clinically, histologically, and immunopathologically classic cases of pemphigoid that regress when the drug is withdrawn. Exposure to ultraviolet light is known to exacerbate BP.
The diagnosis of BP in dogs and cats has come under intense scrutiny in recent literature. Many cases that have been reported as BP were cited before techniques were available to identify the target protein. Although Collies are supposedly predisposed to BP, the disease process would currently be classified as cutaneous vesicular lupus erythematosus. Furthermore, additional cases in dogs and cats would now be classified as mucous membrane pemphigoid. One confirmed BP case was documented in 3-year-old dog with vesicles and erosions on the prepuce, trunk, face, and paws. The dogs was documented with IgG autoantibodies that targeted BPAG2 (XVII collagen). BP has been documented in horses and Yucatan minipigs. In horses, the lesions are often generalized with marked sloughing of the oral mucosa and signs of systemic illness. Lesions on the rump and back characterize the disease in Yucatan minipigs. Mucosal lesions have not been described in pigs.
Histologically, there is a subepidermal bulla filled with fibrin and variable numbers of neutrophils, eosinophils, and mononuclear cells. Eosinophils are not always present as they are in lesions of humans. Acantholytic keratinocytes are not present. The basal cells that line the roof of the bulla are not initially degenerate. The basement membrane zone lines the floor of the bulla as separation occurs within the lamina lucida. There is often marked subepidermal vacuolar alteration. The dermis is usually markedly edematous, capillaries are dilated and lined with swollen endothelial cells, and there is perivascular accumulation of neutrophils, eosinophils, and mononuclear cells. Mild to moderate lichenoid interface dermatitis may be present, particularly in mucocutaneous regions. Histologic differential diagnoses include pemphigus vulgaris, vesicular lupus erythematosus, mucous membrane pemphigoid, epidermolysis bullosa acquisita, toxic epidermal necrolysis (TEN), and thermal burns.
Classically, BP is characterized by the presence of immunoglobulin (IgG, IgM, or IgA) and/or complement deposited at the basement membrane zone within skin lesions. The BP180 antigen extends to the lateral and apical aspects of basal keratinocytes, and labeling may extend to these areas. Serum autoantibodies may be detected in some cases.
Further reading
Iwasaki T, et al. Canine bullous pemphigoid (BP): identification of the 180-kD canine BP antigen by circulating autoantibodies. Vet Pathol 1995;32:387-393.
Olivry T. An autoimmune subepidermal blistering skin disease in a dog? The odds are that it is not bullous pemphigoid. Vet Dermatol 2014;25:316-318.
Olivry T, et al. A spontaneously arising porcine model of bullous pemphigoid. Arch Dermatol Res 2000;292:37-45.
Olivry T, et al. Equine bullous pemphigoid IgG autoantibodies target linear epitopes in the NC16A ectodomain of collagen XVII (BP180, BPAG2). Vet Immunol Immunopathol 2000;73:45-52.
Olivry T, Jackson HA. Diagnosing new autoimmune blistering skin diseases of dogs and cats. Clin Tech Small Anim Pract 2001;16:225-229.
Tanaka T, et al. cDNA cloning of bullous pemphigoid (BP) antigen reveals structural and sequence homology with desmoplakin (DP) I. J Invest Dermatol 1990;94:583.
Linear immunoglobulin A disease in dogs.
Linear IgA disease (LAD) is an acquired autoimmune subepidermal blistering disease occurring in humans and dogs. IgG and/or IgA autoantibodies against LAD-1, defined as the processed extracellular domain of type XVII collagen, are demonstrable at the basement membrane zone of lesional skin and in the serum of affected dogs and humans. It is interesting to note the BP antigen is also type XVII collagen; however, in BP, antibodies recognize the transmembrane form of type XVII collagen. Clinically, LAD is characterized by erosions, ulcers, and crusts on the face, extremities, and in the oral cavity. Histologically, dermoepidermal clefting with little or no neutrophilic infiltration is present. Differential diagnoses are similar to those listed for BP and TEN. Differentiation of LAD from other subepidermal blistering diseases requires demonstration of linear IgA deposits at the basement membrane zone of skin lesions as well as identification of circulating autoantibodies against the target antigen, LAD-1. Too few cases have been documented in the dog to define the prognosis.
Further reading
Olivry T, et al. Autoantibodies against the processed ectodomain of collagen XVII (BPAG2, BP180) define a canine homologue of linear IgA disease of humans. Vet Pathol 2000;37:302-309.
Epidermolysis bullosa acquisita in the dog.
Epidermolysis bullosa acquisita (EBA) is a subepidermal blistering disease characterized by vesicle formation in areas of concurrent neutrophilic superficial dermatitis. The condition has been reported in dogs and humans. Circulating and tissue-bound autoantibodies targeting the distal end of anchoring fibrils in the sub-lamina densa of the lower basement membrane zone have been demonstrated using immunofluorescence and immunoelectron microscopy. The actual target antigen has been shown to be the amino-terminal globular noncollagenous domain of type VII collagen. Clinical lesions in the dog are characterized by erythematous and urticarial eruption with vesicles, bullae, or ulcerations arising in areas subject to friction, including oral ulcerations. Histologically, dermoepidermal separation is present in association with marked neutrophilic inflammation in the superficial dermis and within vesicles and bullae. Too few cases have been documented to provide information regarding triggering events or clinical outcome. Differentials include those listed for BP.
Further reading
Olivry T, Dunston SM. Usefulness of collagen IV immunostaining for diagnosis of canine epidermolysis bullosa acquisita. Vet Pathol 2010;47:565-568.
Olivry T, et al. Canine epidermolysis bullosa acquisita: circulating autoantibodies target the aminoterminal non-collagenous (NC1) domain of collagen VII in anchoring fibrils. Vet Dermatol 1998;9:19-31.
Olivry T, et al. Novel localized variant of canine epidermolysis bullosa acquisita. Vet Rec 2000;146:193-194.
Lupus erythematosus
Lupus erythematosus (LE) represents a spectrum of inflammatory disorders that varies from mild skin-limited conditions to life-threatening systemic disease (systemic lupus erythematosus, SLE). Cutaneous lupus erythematosus (CLE) refers to the skin-specific effects of LE, regardless of whether or not there is systemic involvement (i.e., polyarthritis, glomerulonephritis, thrombocytopenia, etc.). In human medicine, CLE is subdivided into 3 major categories: chronic CLE (localized and generalized discoid lupus), subacute CLE, and acute CLE. The subsets serve as prognosticators and are based on the morphology of skin lesions, variations in the histologic reaction, and clinicopathologic findings. For example, chronic CLE is more likely to remain skin localized than acute or subacute CLE. However, patients with chronic CLE who have generalized skin involvement (i.e., disseminated discoid LE) have increased risk of developing systemic manifestations of LE. Acute CLE is the typical malar “butterfly” rash associated with flare-ups of SLE. Subacute CLE is characteristically provoked by solar exposure. The feature common to the lupus subsets is a distinct constellation of histopathologic changes affecting the basal layer and basement membrane zone: basal cell vacuolar degeneration, basement membrane thickening, mononuclear cell infiltration of the dermoepidermal junction and dermis and dermal edema/mucin deposition. It is important to note that lupus patients may develop a variety of skin lesions that are not histologically distinct for lupus (lupus nonspecific), and may be seen with another disease processes.
In veterinary and human medicine, the diagnosis of SLE is based on fulfillment of 4 of 11 criteria established by the American College of Rheumatology, with virtually all cases having a positive antinuclear antibody (ANA) titer. CLE and SLE are thought to have similar pathogenic mechanisms whether or not the disorder remains skin localized. The pathogenesis of CLE involves genetic predisposition (e.g., major histocompatibility complex [MHC] subtype) and generation of autoreactive antibodies that may be triggered by solar exposure, drugs, and tobacco smoke.
Veterinary medicine has historically classified LE into discoid lupus erythematosus (DLE) and SLE. Discoid lupus, the prototype in dogs, has a classic presentation on the nasal planum and/or lips and vulva or prepuce. Although having some features of DLE in humans, the overall disease is not comparable, and veterinarians/owners should be discouraged from applying generalizations from the human literature. The nosology of this disorder remains questionable. Furthermore, 2 diseases (lupoid dermatosis of German Shorthaired Pointers and idiopathic ulcerative dermatosis of Shetland Sheepdogs and Collies) have since been reclassified as variants of cutaneous lupus. Recently, case reports have documented disseminated forms of discoid lupus in dogs, which are more comparable to the disease in humans. It is likely that many unclassified “interface diseases” will fall into CLE as the dermatopathology expertise evolves in veterinary medicine.
Aside from a few exceptions in case reports, the following generalizations hold true for most cases of CLE in veterinary medicine.
-
•
Cutaneous lupus in domestic animals generally does not precede the onset of systemic lupus.
-
•
The frequency of SLE related skin disease is controversial. Although “skin disease” is considered a major sign of SLE, the precise lesions are often not defined, and inclusion may erroneously fulfill criteria for the diagnosis of SLE. “Dermatitis” associated with some cases of SLE may reflect “lupus nonspecific” skin lesions.
-
•
Well-characterized CLE disorders in dogs are often breed specific and presumed hereditary.
Systemic lupus erythematosus.
Dogs, cats, and horses have been documented with skin manifestations of SLE. Aside from one recent report in a dog, the cutaneous lesions do not herald the onset of SLE. SLE is reported to occur in middle-aged animals without age or sex predilections. German Shepherd dogs appear to be predisposed. SLE is a chronic condition that may wax and wane. Drug administration, pregnancy, extreme heat or cold, and ultraviolet (UV) radiation have been known to trigger onset of SLE. Polyarthritis, thrombocytopenia, fever of unknown origin, anemia, stomatitis, and glomerulonephritis are common manifestations. Although “dermatitis,” is cited as a common manifestation, (i.e., occurring in  of affected dogs) the type of skin lesion (i.e., “lupus specific” vs. lupus nonspecific) is generally not indicated. Contrary to citations in textbooks and reviews, true cutaneous manifestations of SLE are probably rare. The gross lesions that have been described are extremely variable, and range from a mucocutaneous, ulcerative dermatitis resembling pemphigus vulgaris and bullous pemphigoid to erythema, scaling, and alopecia. Lesions may occur in sun-exposed regions (i.e., face, ears, nose, lips) and sparsely haired, lightly pigmented, thin skin of other body regions.
of affected dogs) the type of skin lesion (i.e., “lupus specific” vs. lupus nonspecific) is generally not indicated. Contrary to citations in textbooks and reviews, true cutaneous manifestations of SLE are probably rare. The gross lesions that have been described are extremely variable, and range from a mucocutaneous, ulcerative dermatitis resembling pemphigus vulgaris and bullous pemphigoid to erythema, scaling, and alopecia. Lesions may occur in sun-exposed regions (i.e., face, ears, nose, lips) and sparsely haired, lightly pigmented, thin skin of other body regions.
The histopathology consists of a cell-poor to lichenoid interface dermatitis with hydropic degeneration of basal cells and a lymphohistiocytic infiltrate at the dermoepidermal junction. Lymphocytes predominate; however, plasma cells are intermixed at mucocutaneous sites. Apoptosis of basal keratinocytes and pigmentary incontinence, a consequence of the basal cell degeneration, are key histologic lesions, as is subepidermal vacuolar change. One well-documented case of SLE (bullous form) with IgG autoantibody against collagen VII has been reported in the dog and found to be similar to the condition in humans. Histologically, subepidermal bullae were associated with circulating IgG autoantibodies to type VII collagen as well as IgG deposits at the basement membrane zone. In the acute cutaneous lesions of SLE, there is dermal edema, capillary dilation, extravasation of leukocytes and erythrocytes, and variable lymphohistiocytic infiltrates around vessels of superficial and deep capillary plexuses. Mucinous degeneration may be prominent. With chronicity, a few cases may show thickening of the basement membrane caused by accumulation of antigen-antibody complexes. Fibrinoid deposits may also occur around superficial blood vessels. Leukocytoclastic vasculitis develops occasionally. Immunoglobulin and complement deposition at the basement membrane zone may be detectable by IF or IHC staining. An antinuclear antibody (ANA) titer of >256 is present in 97-100% of dogs with SLE but is not entirely specific for the disease. Differential diagnoses vary with the type of lesions present but may include other autoimmune skin diseases, drug eruption, vasculitis, ischemic dermatopathy, and dermatomyositis.
There are anecdotal cases of SLE with cutaneous manifestations in the horse and a documented case in a 2-year-old Standardbred filly. The horse developed weight loss, bilateral symmetrical alopecia with scaling oral ulcers, and lymphadenopathy. Abnormal findings included a Coombs test–positive hemolytic anemia and a positive ANA test result. An autopsy revealed membranous glomerulonephritis and fibrinous synovitis. Skin biopsies had an interface reaction with IgG deposition at the basement membrane zone.
SLE-like disease occurs in the cat, but with only a few case reports and case series, a cohesive dermatologic manifestation has not been revealed. Approximately 50% of SLE cases in cats are reported to have skin lesions (seborrhea, exfoliative erythroderma, symmetrical erythematous scaling and crusting); however, it is unclear how many cases with dermatitis had a lupus-specific reaction pattern. Glomerulonephritis, thrombocytopenia, and hemolytic anemia and neurologic disease have been cited. One case report documents a cat with LE-specific histologic lesions and criteria for the diagnosis of SLE (symmetrical facial dermatitis, thrombocytopenia, positive ANAs, oral ulceration).
Cutaneous lupus erythematosus.
In dogs, localized forms of lupus include nasal planum discoid lupus, and disseminated discoid lupus, as well as breed-specific cutaneous vesicular lupus and exfoliative cutaneous lupus. Nasal DLE, a distinct entity in dogs and very rarely seen in cats, is currently under close scrutiny. The terminology for this clinicopathologic condition is likely to change, as the pathogenesis becomes understood. There does not appear to be a relationship between nasal planum DLE and SLE. The clinical findings are distinct on the nasal planum: loss of cobblestone architecture, depigmentation, erosions/ulcers, hyperkeratosis, and crusting. The condition affects the entire nasal planum, and may be exacerbated or triggered by solar exposure, which is the reason for a proposed name change (photosensitive nasal dermatitis). Some dogs may have similar lesions around the eyes, lips, vulva, and prepuce. Biopsies are often complicated by surface bacterial infection. Histologic features consist of lichenoid lymphoplasmacytic interface dermatitis with pigmentary incontinence, mild vacuolar change in the basal cell layer, and a few individually necrotic basal keratinocytes. The epidermis may have elongated rete ridges, which are generally thin, as is the epidermis between the ridges. Many pathologists have been frustrated by these biopsies, as the features found in routine cases often represent a “blurred line” that cannot distinguish DLE from mucocutaneous pyoderma. This clinical distribution can be helpful because mucocutaneous pyoderma generally affects the junctions of the alar folds and haired skin rather than the entire nasal planum. Mucocutaneous pyoderma also lacks evidence of basal cell damage and is predominantly plasmacytic. Both conditions may be present simultaneously. Other differential diagnoses include parasympathetic nasal dermatitis, Labrador Retriever nasal parakeratosis, superficial dermatophytosis, adverse drug reaction, and uveodermatologic syndrome. The biopsy is most helpful to rule out other conditions (e.g., cutaneous lymphoma, pemphigus foliaceus, vitiligo). A final diagnosis is achieved with both histologic and clinical evaluation.
Cutaneous (discoid) lupus erythematosus is rarely described in horses. There are no age, breed, or sex predilections. Lesions commonly begin on the face, especially around mucocutaneous junctions, leading to annular and oval symmetrical areas of erythema, scaling, alopecia, and variable degrees of leukoderma and leukotrichia. Lesions may also occur on the pinna, neck, shoulders, perianal, perineal, and genital areas. As in other species, the disease is exacerbated by UV radiation.
Disseminated discoid lupus erythematosus has been documented in a 9-year-old Chinese Crested dog and a 3-year-old, female Spitz. Both dogs had generalized lesions affecting the haired skin without mucous membrane involvement. The Chinese Crested dog had annular and polycyclic hyperpigmented and scaly skin lesions with central erosions, hypopigmentation. Skin biopsies showed a lymphocyte-rich interface dermatitis with epidermal atrophy and dermoepidermal deposition of immunoglobulins and activated complement. The Spitz had diffuse erythema and scaling on the dorsal trunk with an interface dermatitis characterized by hydropic degeneration of the basal layer, plasmacytic perivascular dermatitis, and a plasma cell–rich interface mural folliculitis.
Exfoliative cutaneous lupus erythematosus (ECLE) in the German Shorthaired Pointer is a severe heritable variant form of CLE. Early in life, these dogs develop widespread skin lesions (scaling, erythema, erosions/ulcers, pigment loss) as well as variable lethargy and lameness. The inheritance is autosomal recessive and maps to canine chromosome 18. All dogs generally develop lesions by 6 months of age. The clinical and histologic features are diagnostic. The lesions are not solar associated. This first manifestation is adherent scale on the dorsal muzzle (Fig. 6-73 ). This is followed by erythema, with progression to hair loss, pigment alterations, erosions, and ulcers. As the lesions change, the distribution becomes truncal and involves the scrotum (often severe), limbs, and ears. The collar area is generally spared. The dogs are generally nonpruritic. Biopsies of peripheral lymph nodes reveal reactive lymphoid hyperplasia; nodes are often palpably enlarged before the onset of severe skin lesions. The dogs have consistent mild lymphopenia and hyperproteinemia, with some dogs having minimal to mild thrombocytopenia. ANA titers are negative. With time, the dogs develop progressive shifting leg lameness and a hunched “tucked up” stance. Joint aspirates, detailed radiographic studies, and postmortem examinations have failed to find a source for the apparent arthralgia. Both males and females are infertile. The males have oligospermia, and the females have delayed or absent estrus cycles.
Figure 6-73.

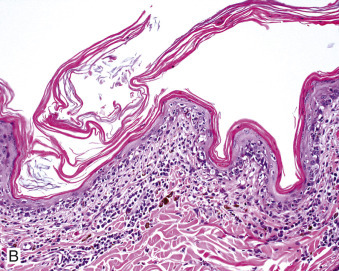
Exfoliative cutaneous lupus erythematosus in a German Shorthaired Pointer. A. Scaling, alopecia, and hypopigmentation on the muzzle and medial pinna. B. Lymphocytic interface dermatitis with basal layer vacuolar change, pigmentary incontinence, and marked orthokeratotic hyperkeratosis.
The histologic changes are lupus specific and characteristic of ECLE. A subtle interface change can be detected as early as 6 weeks of age but typically is not fully developed until 4-6 months. The interface reaction is characterized by a sparse to mild lymphocytic superficial dermal inflammatory infiltrate, basal keratinocyte vacuolar change with individual basal keratinocyte necrosis, dermoepidermal clefting, and pigmentary incontinence. Some individually necrotic keratinocytes can be found in the spinous layer as in human CLE. The interface reaction affects outer root sheaths, and may be associated with patchy (not complete) sebaceous gland loss. With time, hair follicles undergo atrophy. The stratum corneum has marked orthokeratotic hyperkeratosis. Although the disease may wax and wane for several years, most dogs are eventually euthanized because of intractable skin disease. The main differential diagnosis is erythema multiforme.
Vesicular cutaneous lupus erythematosus is a disorder, formerly known as idiopathic ulcerative dermatosis, that is seen in Rough-coated Collies, Shetland Sheepdogs, and Border Collies. This condition was originally thought to be an adult-onset variant of dermatomyositis, but recent immunologic studies indicate the presence of autoantibodies that target nuclear antigens similar to that seen in CLE. Antinuclear antibody testing is negative. Lesions develop in middle-aged to older dogs. Clinical lesions consist of vesicles and bullae that evolve into erosions and ulcers. The inguinal and axillary regions are most commonly involved, but lesions may also occur on mucocutaneous junctions. Histologic changes consist of interface lymphocytic dermatitis with hydropic degeneration of basal cells, keratinocyte apoptosis, and extensive vesicles and bullae at the dermoepidermal junction.
Lupus panniculitis (lupus profundus) is characterized by well-circumscribed subcutaneous nodules over the trunk and proximal extremities. It is reported rarely in dogs, and because the features are identical to rabies vaccine–associated panniculitis, the “lupus” association is questionable. Histologically, it is initially a septal panniculitis with dense nodular infiltrates of lymphocytes and plasma cells and fewer macrophages. The fat lobules may undergo necrosis, often represented by hyalinization without mineralization. Usually the dermis and epidermis show the typical microscopic features of lupus, including hydropic degeneration of basal cells, pigmentary incontinence, thickened basement membrane zone, and sclerosis of the dermis. Abundant mucinous degeneration is usually prominent. Leukocytoclastic vasculitis may be present in the interlobular septa.
Further reading
Bennion SD, et al. In three patterns of interface dermatitis, different patterns of expression of intercellular adhesion molecule-1 (ICAM-1) indicate different triggers of disease. J Invest Dermatol 1995;105:71S-79S.
Chabanne L, et al. Canine systemic lupus erythematosus. Part I. Clinical and biologic aspects. Compend Contin Educ Pract Vet 1999;21:135-141.
Fournel C, et al. Canine systemic lupus erythematosus. I. A study of 75 cases. Lupus 1992;1:133-139.
Geor RJ, et al. Systemic lupus erythematosus in a filly. J Am Vet Med Assoc 1990;197:1489-1492.
Gibson I, Barnes J. Vesicular cutaneous lupus erythematosus in a border collie in New Zealand. N Z Vet J 2011;59:153.
Goldman M. Cytokines in the pathophysiology of systemic lupus erythematosus. Autoimmunity 1990;8:175-179.
Goo MJ, et al. Discoid lupus erythematosus (DLE) in a Spitz dog. J Vet Med Sci 2008;70:633-635.
Jackson HA. Eleven cases of vesicular cutaneous lupus erythematosus in Shetland sheepdogs and rough collies: clinical management and prognosis. Vet Dermatol 2004;15:37-41.
Jackson HA, Olivry T. Ulcerative dermatosis of the Shetland sheepdog and rough collie may represent a novel vesicular variant of cutaneous lupus erythematosus. Vet Dermatol 2001;12:19-27.
Linker-Israeli M, et al. Elevated levels of endogenous IL-6 in systemic lupus erythematosus. A putative role in pathogenesis. J Immunol 1991;147:117-123.
Mauldin EA, et al. Exfoliative cutaneous lupus erythematosus in German shorthaired pointers: disease development, progression and evaluation of three immunomodulatory drugs (ciclosporin, hydroxychloroquine, and adalimumab) in a controlled environment. Vet Dermatol 2010;21:373-382.
Oberkirchner U, et al. Successful treatment of a novel generalized variant of canine discoid lupus erythematosus with oral hydroxychloroquine. Vet Dermatol 2012;23:65-70.
Olivry T, et al. Bullous systemic lupus erythematosus (type 1) in a dog. Vet Rec 1999;145:165-169.
Olivry T, Linder KE. Bilaterally symmetrical alopecia with reticulated hyperpigmentation: a manifestation of cutaneous lupus erythematosus in a dog with systemic lupus erythematosus. Vet Pathol 2013;50:682-685.
Pericard P, Plasslart G. Suspicion of systemic lupus erythematosus in a female cat. Prat Vet 2004;2:7.
Smee NM, et al. Measurement of serum antinuclear antibody titer in dogs with and without systemic lupus erythematosus: 120 cases (1997-2005). J Am Vet Med Assoc 2007;230:1180-1183.
Sontheimer RD. The lexicon of cutaneous lupus erythematosus—a review and personal perspective on the nomenclature and classification of the cutaneous manifestations of lupus erythematosus. Lupus 1997;6:84-95.
Soulard M, et al. Autoimmune antibodies to hnRNPG protein in dogs with systemic lupus erythematosus: epitope mapping of the antigen. J Autoimmun 2002;18:221-229.
Vitale CB, et al. Systemic lupus erythematosus in a cat: fulfillment of the American Rheumatism Association criteria with supportive skin histopathology. Vet Dermatol 1997;8:133-138.
vonTscharner C, et al. Stannard's illustrated equine dermatology notes. Vet Dermatol 2000;11:163-178.
Wiemelt SP, et al. A retrospective study comparing the histopathological features and response to treatment in two canine nasal dermatoses, discoid lupus erythematosus and mucocutaneous pyoderma. Vet Dermatol 2004;15:341-348.
Wilbe M, Andersson G. MHC class II is an important genetic risk factor for canine systemic lupus erythematosus (SLE)-related disease: implications for reproductive success. Reprod Domest Anim 2012;47(Suppl. 1):27-30.
Wilhelm S. Two cases of feline exfoliative dermatitis and folliculitis with histological features of cutaneous lupus erythematosus. Tierärztliche Praxis Ausgabe 2005;33:364.
Yager JA, Wilcock BP. Part II.5: Interface dermatitis. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat: Dermatopathology and Skin Tumors. London: Mosby Year Book; 1994. p. 93-96.
Other immune-mediated dermatoses
Drug eruptions
Drug eruptions are occasionally reported in dogs, cats, and horses and rarely in other domestic animals. Drugs responsible for skin eruptions may be administered orally, topically, or by injection or inhalation. Any drug may cause an eruption, and any one drug consistently produces no specific type of reaction. Thus drug eruption can mimic virtually any dermatosis. Erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis (TEN), and vasculitis are well-recognized dermatoses that can be manifestations of cutaneous drug eruptions and are described individually later in this section. Criteria for establishing a cutaneous reaction as a confirmed drug eruption include (1) elimination of other causes of the skin lesions, (2) timing of onset of reaction with administration of a suspect drug, (3) improvement upon drug withdrawal, (4) recognition that the suspect drug has been associated with similar reactions in other animals or species in the past, and (5) recurrence of lesions upon rechallenge of the patient with the drug. Understandably, all 5 of these criteria are not often met, particularly rechallenge as this can be associated with high morbidity or mortality. The time period between drug administration and onset of an adverse reaction varies widely from hours to months, and lesions can result from a single or repeated administration. Drug-induced gross and histologic lesions are not pathognomonic for an adverse cutaneous drug eruption, although histopathologic changes may often point to a limited list of differentials. Histologic patterns that have been recognized as forms of adverse drug reactions include urticaria, perivascular dermatitis (allergy-like), hydropic and/or lichenoid interface dermatitis (erythema multiforme, TEN, lupus erythematosus-like), perforating folliculitis, vasculitis, intraepidermal vesiculopustular dermatitis (pemphigus-like), and subepidermal bullous reactions (pemphigoid-like). The pathogenesis of lesion formation in many types of drug eruptions is not known with certainty. Drug hypersensitivities are believed to involve all 4 types of hypersensitivity reactions, and in some cases are not thought to be immunologically mediated.
The most common drugs recognized to produce hypersensitivity reactions in domestic animals are the sulfonamides (especially trimethoprim-potentiated) and penicillins. Erythema multiforme, Stevens Johnson syndrome, and TEN (discussed later in this section) have been seen most commonly with trimethoprim-potentiated sulfonamides, cephalosporins, and levamisole. Diethylcarbamazine and 5-fluorocytosine have been associated with fixed-drug eruption on the scrotum of dogs. The ulcerative lesions healed with hyperpigmentation when the drug was withdrawn but recrudescence at the same site, with vesiculation, occurred when the dog was rechallenged. The mechanism underlying fixed-drug eruption is unknown. In humans, the epidermal invasion of T cells in fixed-drug eruptions is associated with the expression of the intercellular adhesion molecule-1 (ICAM-1) on the surface of lesional keratinocytes. In dogs, cyclosporine has been reported to cause a lichenoid lymphoplasmacytic dermatitis as well as cutaneous papillomas and viral plaques. These changes are likely attributed to long-term immune suppression rather than an immune-mediated adverse drug reaction. Urticaria and angioedema have been associated with levamisole, barbiturates, and some antibiotics. Drug eruptions manifesting as exfoliative erythroderma have been seen in dogs treated with levamisole and lincomycin. Acute maculopapular eruptions with erythroderma are reported in dogs being treated for gastrointestinal illness, so-called Wells-like syndrome, but specific drugs have not been implicated.
Drug eruptions resembling bullous pemphigoid clinically, histologically, and immunohistochemically have been associated with triamcinolone. It is quite possible that some cases described as bullous pemphigoid actually represent drug eruptions. Pemphigus foliaceus–like drug eruptions have been described in cats treated with ampicillin or cimetidine and dogs receiving trimethoprim-sulfonamide. Lesions consisted of classic subcorneal pustules with acantholytic cells, with an additional feature of vasculitis in some cases. Systemic lupus–like drug reactions have been reported in dogs and in cats. Cutaneous vasculitis caused by immune complex deposition may be initiated by drug administration. Sulfadiazine administration in Doberman Pinschers causes a poorly defined skin rash as well as ocular, joint, kidney, and hematologic abnormalities suggestive of systemic vasculitis.
Further reading
Affolter VK, von Tscharner C. Cutaneous drug reactions: a retrospective study of histopathological changes and their correlation with the clinical disease. Vet Dermatol 1993;4:79-86.
Evans AG, Stannard AA. Idiopathic multiple cutaneous seromas in a horse: a possible manifestation of drug eruption. Equine Pract 1990;12:27-34.
Favrot C, et al. Evaluation of papillomaviruses associated with cyclosporine-induced hyperplastic verrucous lesions in dogs. Am J Vet Res 2005;66:1764-1769.
Ginn PE, et al. Self-limiting subepidermal bullous disease in a neonatal foal. Vet Dermatol 1998;9:249-256.
Ihrke PJ. Cutaneous adverse drug reactions. Compend Contin Educ Pract Vet 1997;19:87-92.
Mason KV. Blistering drug eruptions in animals. Clin Dermatol 1993;11:567-574.
Mauldin EA, et al. Clinical associations with severe eosinophilic dermatitis in dogs: a retrospective study. Vet Dermatol 2006;17:338-347.
McKenna JK, Leiferman KM. Dermatologic drug reactions. Immunol Allergy Clin North Am 2004;24:399-423.
Noli C, et al. A retrospective evaluation of adverse reactions to trimethoprim-sulphonamide combinations in dogs and cats. Vet Q 1995;17:123-128.
Ruocco V, Sacerdoti G. Pemphigus and bullous pemphigoid due to drugs. Int J Dermatol 1991;30:307-312.
Scott DW, Miller WH. Idiosyncratic cutaneous adverse drug reactions in the cat: literature review and report of 14 cases (1990-1996). Feline Pract 1998;26:10-15.
Shiohara T, et al. Fixed drug eruption. Expression of epidermal keratinocyte adhesion molecule-1 (ICAM-1). Arch Dermatol 1989;125:1371-1376.
Werner AH. Psoriasiform-lichenoid-like dermatosis in three dogs treated with microemulsified cyclosporine A. J Am Vet Med Assoc 2003;223:1013-1016.
Cryopathies
Cryopathies are cold-related hypersensitivity syndromes that include cold agglutinin disease, a condition in which erythrocyte autoantibodies react at lower temperatures to produce microvascular thrombosis in superficial dermal vessels. Other cryopathies are small vessel vasculopathies associated with abnormal serum proteins (paraproteins) that precipitate out of the serum at cooler temperatures and redissolve upon warming. Paraproteins include cryofibrinogens, cryoglobulins, macroglobulins, and γ heavy chains. Cryoglobulins may be monoclonal IgG or IgM (type I cryoglobulinemia), or mixed monoclonal and polyclonal, with one antibody directed against the other, in which case, immune complexes are in the circulation (type II cryoglobulinemia). In type III cryoglobulinemia, the immunoglobulins are polyclonal. Type I cryoglobulinemia is often associated with underlying disease, such as multiple myeloma, leukemia, or lymphoma, whereas in type II or III, connective tissue disease, such as SLE, or a systemic infection is present. Type II and III may also be idiopathic. Most cases reported in dogs and cats are the result of cold-reacting anti-erythrocyte antibodies. Cold agglutinin disease has been reported rarely to cause skin disease in dogs and cats. Cold agglutinin disease as a postinfectious event has been reported in sheep, horses, and pigs. One report in Birman cats occurred in association with neonatal isoerythrolysis and suggested that group B blood group cats may be predisposed. A monoclonal cryoglobulinemia associated with multiple myeloma has been reported in a cat. Lead exposure and hemobartonellosis (Mycoplasma haemofelis) have also been implicated as predisposing factors in dogs and cats. Cryopathy caused by cryofibrinogens and cryoglobulins has also been reported in the dog.
Cutaneous signs associated with cryopathies result from vascular insufficiency (obstruction, stasis, spasm, and thrombosis). Lesions include erythema, purpura, cyanosis, necrosis, ulceration, and occasionally sloughing of extremities, and are precipitated or exacerbated by exposure to cold. The paws, pinnae, nose, and tip of the tail are typically involved. Skin biopsy usually reveals necrosis, ulceration, and often secondary suppurative changes. Microvascular thrombosis may be evident in cold agglutinin disease. In other types of cryopathies, paraproteins are precipitated and deposited throughout vessel walls and within vascular lumens. The proteins stain pink with H&E and bright red with PAS. Hemorrhage may be present. In type I cryopathies, inflammation is usually absent, whereas a leukocytoclastic vasculitis is often present in types II and III.
Diagnosis requires a test for cryoprecipitates and analysis of serum proteins. Erythrocyte agglutination on a cooled slide that reverses upon warming and a positive Coombs test at 4° C should be present in cases of cold agglutinating anti-erythrocyte antibodies. Differential diagnoses include frostbite, disseminated intravascular coagulation, SLE, dermatomyositis, and other causes of vasculitis.
Further reading
Barnhill RL, Busam KJ. Vascular diseases. In: Elder D, et al., editors. Lever's Histopathology of the Skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p. 196-197.
Bridle KH, Littlewood JD. Tail tip necrosis in two litters of Birman kittens. J Small Anim Pract 1998;39:88-89.
Dickson NJ. Cold agglutinin disease in a puppy associated with lead intoxication. J Small Anim Pract 1990;31:105-108.
Godfrey DR, Anderson M. Cold agglutinin disease in a cat. J Small Anim Pract 1994;35:267-270.
Hickford FH, et al. Monoclonal immunoglobulin G cryoglobulinemia and multiple myeloma in a domestic shorthair. J Am Vet Med Assoc 2000;217:1029-1033.
Maede Y, et al. Cryoglobulinemia in a horse. J Vet Med Sci 1991;53:379-383.
Nagata M, et al. Cryoglobulinaemia and cryfibrinogenaemia: a comparison of canine and human cases. Vet Dermatol 1998;9:277-281.
Zulty JC, Kociba GJ. Cold agglutinins in cats with haemobartonellosis. J Am Vet Med Assoc 1990;196:907-910.
Graft-versus-host disease
Graft-versus-host disease (GVHD) occurs as a complication of bone marrow transplantation. It has been recorded in humans, dogs, cats, and horses. The disease results from donor T-lymphocyte responses to recipient histocompatibility antigens in the acute phase, and from immunocompetent recipient lymphocyte responses to transplantation antigens in the chronic phase. Principal target organs are the skin, liver, and intestinal tract. GVHD is considered the classic example of cell-mediated attack upon the epidermis. Proposed target cells in the skin include basal keratinocytes, follicular stem cells, and/or Langerhans cells. Studies indicate both CD8+ and CD4+ lymphocytes are active in the disease process, with CD8+ T cells found more often in the epidermis and CD4+ T cells in the dermal infiltrate. Natural killer (NK) cells may also play a role. T-cell production of interferon-γ (IFN-γ) results in keratinocyte expression of ICAM-1, the binding molecule for lymphocyte function-associated antigen 1 (LFA-1) found on infiltrating T cells. Tumor necrosis factor-α (TNF-α) production by activated keratinocytes and Langerhans cells and IFN-γ lead to keratinocyte production of IL-8 attracting more lymphocytes.
Skin lesions in the acute phase include generalized erythematous macules, multifocal alopecia, and ulcerative dermatitis. Oral lesions, epidermal detachment, and follicular papules may be present. In the chronic phase, erythema, irregular hyperpigmentation, dermal fibrosis, cutaneous atrophy, and cicatricial alopecia from chronic ulceration may occur. Histologic findings include various degrees of hydropic and/or lichenoid interface dermatitis with marked lymphocytic satellitosis of necrotic keratinocytes in all layers of the epidermis and the follicular epithelium. There are lymphocytic exocytosis and spongiosis. Dermal lymphocytic infiltrate is variable. Dermal-epidermal cleft or ulceration may also be present. Over time, epidermal atrophy and dermal sclerosis with loss of adnexa may occur. Basal layer vacuolation and inflammation persist. Differential diagnoses include erythema multiforme, toxic epidermal necrolysis (TEN) or other drug eruption, alopecia areata, and radiation dermatitis. The history and the triad of cutaneous, hepatic, and intestinal signs should lead to the proper diagnosis of GVHD.
Erythema multiforme/Stevens-Johnson syndrome/toxic epidermal necrolysis
Historically, erythema multiforme (EM) has represented one end of the spectrum of diseases that includes Stevens-Johnson syndrome (also called erythema multiforme major) and TEN, based on comparison of veterinary diseases to the human literature. EM is considered the “mild” disease form (i.e., EM minor), with TEN being the most severe. In human medicine, it is now accepted that EM and Stevens-Johnson syndrome (SJS)/TEN are different entities and not a spectrum of disease. SJS and TEN are likely triggered by an adverse drug reaction. EM minor in human is associated with herpes simplex infection, and the name has now changed to “herpesvirus-associated EM.” Only rare cases of EM minor are due to adverse drug reactions (“drug-associated EM”).
In veterinary medicine, EM has been reported in dogs, cats, horses, cattle, swine, a ferret, and anecdotally in the goat. Adverse drug reaction has been firmly entrenched in the literature; however, this association has come under intense scrutiny. Two cases series have reported adverse drug reactions as the cause of EM at 19 and 59%, respectively. Many cases are idiopathic, and old dogs are more likely to have idiopathic EM rather than drug-induced EM. A number of drugs have been reported to trigger EM in animals (e.g., D-limonene–based dips, levamisole, cephalexin, trimethoprim-sulfa, gentamicin, penicillin). Many of cases in earlier literature would be putative, at best, if strict criteria or drug provocation testing was applied. A multicenter study reclassified cases of EM based on aspects of the human classification system. The study found that SJS/TEN in dogs was likely to be triggered by drugs, whereas EM was not. The study also showed that skilled pathologists were unable to distinguish EM from SJS or TEN on light microscopy.
To date, there is no consensus on the classification of these disorders in veterinary medicine. Although the diagnosis of EM/SJS/TEN requires histopathology, the diseases are separated by clinical features and not by microscopic differences. For example, SJS involves >50% of the skin with <10% epidermal detachment and involvement of more than one mucosal surface; whereas TEN has similar criteria, but there is >30% epidermal detachment. In humans, the specific type of clinical lesion is paramount to distinguishing the reactions: EM is raised and palpable, whereas SJS/TEN lesions are flat. A recent review of 3 dogs with TEN reports the clinical lesions as flat purpuric macules.
SJS in humans may also be associated with infectious disease, with the most common agent being Mycoplasma pneumoniae. Interestingly, TEN has been associated with Mycoplasma bovis infection in calves. There are also reports of parvovirus-associated EM in dogs. Unlike herpesvirus-associated EM in people, the lesions in dogs have parvoviral inclusions, indicating active virus replication and likely represent systemic viral infection with unusual skin involvement. Equid herpesvirus-5–associated dermatitis resembling herpes-associated erythema multiforme was described in a 9-year-old Holsteiner stallion. Skin lesions consisted of nonpruritic, multifocal, pustular dermatitis around the eyes, nostrils, and muzzle. Histopathologically, there was interface dermatitis with apoptotic keratinocytes and intranuclear inclusions within the stratum spinosum and stratum granulosum.
There are also anecdotal reports of EM in cats triggered by feline herpesvirus infections. The lesion of thymoma-associated dermatosis in cats has also been likened to erythema multiforme.
The pathogenesis of EM/SJS/TEN is poorly understood in animals. The histologic lesions, cellular infiltrates and types of lymphocytes present mirror that of GVHD, lending further support for a cell-mediated immune response. One study of GVHD and EM in dogs revealed similar populations of CD4 and CD8+ cells. In humans, the pathogenesis of herpesvirus-associated EM (HAEM) is thought to be markedly different from SJS/TEN. In HAEM, viral proteins on the surface of keratinocytes provoke a Th1 CD4+ αβ response. Activated T cells secrete IFN-γ profile, which leads to a cascade of cytokines. Effector CD8+ cytotoxic T cells and NK cells target keratinocytes expressing herpesvirus protein. Apoptosis is mediated by granzyme that enters keratinocytes via transient pores induced by perforin. In drug-induced SJS/TEN, it remains unclear how the drug causes sensitization and why only rare individuals are affected. The hapten model proposes that small drug moieties bind to host proteins and are recognized as immunogenic. Keratinocyte death is similarly mediated by CD8+ T cell and NK cells; however, the apoptosis in TEN/SJS is often confluent. Soluble mediators such as TNF-α, FAS- ligand, and granulysin may play a role. The reader is referred to the reference by Yager (2014) for a detailed review of EM.
A wide range of clinical lesions (maculopapular to vesiculobullous and ulcerative and hyperkeratotic) has been reported in animals. Many of the clinical lesions of EM are likely confused with SJS/TEN. EM is often manifest as erythematous macules, papules, and plaques with central clearing (Fig. 6-74A, B ). Dogs may have very thick hyperkeratotic crusted plaques that ulcerate. For SJS/TEN, epidermal detachment with resultant ulcers is the hallmark lesion (Fig. 6-74C). Clinical lesions of SJS/TEN include urticarial plaques and vesiculobullous lesions. In SJS/TEN, the animals have widespread painful lesions with systemic signs (fever, lethargy, inappetance). Some cases may have a positive pseudo-Nikolsky sign (i.e., digital pressure causes separation of the inflamed skin). Dogs and cats often have ulcers involving mucocutaneous junctions; footpads may also be involved (Figs. 6-74D, 6-75 ). SJS/TEN cases are clinical emergencies, which require intense critical care. The mortality rate for TEN is high.
Figure 6-74.




Erythema multiforme and Stevens-Johnson syndrome. A, B. Bilaterally symmetrical hyperkeratotic and ulcerative plaques in a dog with erythema multiforme. C. Bright red erythematous macules progressing to serpiginous erosions and ulcers in a dog with Stevens-Johnson syndrome. D. Ulcers and erosions on the lips and gums in a dog with Stevens-Johnson syndrome.
Figure 6-75.

Toxic epidermal necrolysis in a cat. Severe epidermal sloughing and ulcers.
(Courtesy T. Grieshaber.)
Histologically, the lesions of EM show the characteristic cytotoxic (interface) dermatitis. Necrotic keratinocytes, often with lymphocytic satellitosis, are scattered throughout the epidermis and the adnexal epithelia (see Fig. 6-11). A sparse lymphohistiocytic infiltrate occurs at the dermoepidermal junction and around superficial blood vessels. Vasculitis is not a feature. Although full-thickness coagulative necrosis of the epidermis may be present, it is not always present and most likely represents a continuum of disease. It is very important to note that the dermis is not necrotic. This feature enables distinction of TEN/EM from a thermal burn or cutaneous infarct.
Clinical differentials for SJS/TEN include thermal or caustic burns, vesicular cutaneous lupus erythematosus, urticaria, vasculitis, other immune-mediated dermatoses, epitheliotropic lymphoma, superficial necrolytic dermatitis, and necrotic arachnidism. Occasionally, lesions of EM may histologically resemble epitheliotropic T-cell lymphoma (CTCL). Important distinguishing features are atypical lymphocytes (CTCL), and apoptosis accompanied by lymphocytic satellitosis in all levels of the epidermis (EM). Chronic EM in old dogs is often idiopathic and is characterized by the additional changes of a proliferative epidermis with marked parakeratosis and extensive lymphocytic exocytosis.
Further reading
Banovic F, et al. Clinical and microscopic characteristics of canine toxic epidermal necrolysis. Vet Pathol 2015;52:321-330.
Bennion SD, et al. In three different types of interface dermatitis, different patterns of expression of intercellular adhesion molecule-1 (ICAM-1) indicate different triggers of disease. J Invest Dermatol 1995;105(Suppl. 7):1S-79S.
Cohen LM, et al. Noninfectious vesiculobullous and vesiculopustular diseases. In: Elder D, et al., editors. Lever's Histopathology of the Skin. 8th ed. Philadelphia: Lippincott-Raven; 1997. p. 239-244.
Favrot C, et al. Parvovirus infection of keratinocytes as a cause of canine erythema multiforme. Vet Pathol 2000;37:647-649.
Foedinger D, et al. Autoantibodies to desmoplakin I and II in patients with erythema multiforme. J Exp Med 1995;181:169-179.
Gross TL, et al. Necrotizing diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005. p. 75-104.
Herder V, et al. Equid herpesvirus 5-associated dermatitis in a horse resembling herpes-associated erythema multiforme. Vet Micro 2012;155:420-424.
Hinn AC, et al. Erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis in the dog: clinical classification, drug exposure, and histopathological correlations. J Vet Allergy Clin Immunol 1998;6:13-20.
March PA, et al. Superficial necrolytic dermatitis in 11 dogs with a history of phenobarbital administration (1995-2002). J Vet Intern Med 2004;18:65-74.
Nuttall TJ, Malham T. Successful intravenous human immunoglobulin treatment of drug-induced Stevens-Johnson syndrome in a dog. J Small Anim Pract 2004;45:357-361.
Paquet P, Pierard GE. Erythema multiforme and toxic epidermal necrolysis: a comparative study. Am J Dermatopathol 1997;19:127-132.
Rosenbaum MR, Kerlin RL. Erythema multiforme major and disseminated intravascular coagulation in a dog following application of d-limonene-based insecticidal dip. J Amer Vet Med Assoc 1995;207:1315-1319.
Senturk S1, et al. Toxic epidermal necrolysis associated with Mycoplasma bovis in calves. Vet Rec 2012;170:566.
Woldemeskel M, et al. Canine parvovirus-2b associated erythema multiforme in a litter of English Setter dogs. J Vet Diagn Invest 2011;23:576-580.
Yager JA, Wilcock BP. Part II.5: Interface dermatitis. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat: Dermatopathology and Skin Tumors. London: Mosby Year Book; 1994. p. 86-89.
Yager JA. Erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis: a comparative review. Vet Dermatol 2014;25:406-e64.
Vasculitis
Cutaneous vasculitis is characterized as an aberrant immune response directed toward dermal blood vessels. The pathophysiology is complex, often poorly understood, and involves a variety of mechanisms that lead to loss of vascular integrity, dermal edema, hemorrhage, and sometimes necrosis. The clinical presentation correlates with degree of vascular damage, type of vessels involved, and chronicity. Pathogenic mechanisms are diverse and may be associated with hypersensitivity reactions (type I, II, or III) infectious agents, malignancy, toxins, and many cases are idiopathic. Classic examples include infection with an endotheliotropic organism (Rickettsia rickettsii) and septicemia (Erysipelothrix rhusiopathiae). In textbooks, systemic lupus erythematosus (SLE) is considered the classic example of immune complex (type III hypersensitivity)–induced cutaneous vasculitis; however, cases of true cutaneous involvement in domestic animals are exceedingly rare and poorly documented. Clinical signs of immune-complex cutaneous vasculitis have been documented in healthy and critically ill dogs given intravenous human albumin. Cutaneous vasculitis may be a secondary event associated with cutaneous diseases, such as staphylococcal infections. In veterinary medicine, drug-induced vasculitis is probably under-diagnosed. Dose-dependent vasculitis has been seen in dogs receiving itraconazole for cutaneous fungal disease. The mechanism is thought to be the result of haptenization of host proteins, direct drug toxicity against vessel walls, autoantibodies against endothelial cells, or possibly cell-mediated cytotoxic reactions against vessels.
Cutaneous vasculitis is seen most often in the dog and horse and is considered to be rare in cats, pigs, and cattle; ~50% of cases of vasculitis in dogs and horses are idiopathic. Gross lesions suggestive of vasculitis include erythematous plaques or macules, palpable purpura, hemorrhagic bullae, edema, necrosis, and well-demarcated ulcers (Fig. 6-76 ). Ischemic necrosis may occur leading to eschar formation and sloughing of the skin or distal extremities. Paws, pinnae, lips, tail, and oral mucosa are most commonly affected. Ischemic atrophy of folliculosebaceous units may lead to areas of alopecia and scaling in long-standing lesions of more subtle vasculitis.
Figure 6-76.

Typical punched-out ulcers on the margins of the ears caused by vasculitis in a dog.
(Courtesy M.S. Canfield.)
Small arterioles, capillaries, and postcapillary venules are most often affected in cutaneous vasculitis. Histologic lesions in the classic case feature evidence of damage to the vessel wall, such as necrotic cell debris and fibrinoid necrosis within the vessel wall, mural infiltrates of either neutrophils or lymphocytes, and intramural or perivascular edema, hemorrhage, or fibrin exudation (see Fig. 6-15). Subtle cases of vasculitis may be characterized by edema, rare necrotic cells in the vicinity of vessels, and a mild interstitial mononuclear cell infiltrate. Microscopic evidence of vasculitis in the dog is often subtle and may lead to under-diagnosis of the condition. Some pathologists prefer to refer to very cell-poor cases of vasculitis as a vasculopathy rather than true vasculitis when degenerative lesions of vessel wall and evidence of ischemia are detected in the absence of inflammation of vessel walls. Edema, hemorrhage, and evidence of ischemia and homogenization of dermal collagen are helpful changes. A preponderance of leukocytes in vessels walls rather than in the dermis suggests that vessels are the primary target of inflammation and not just serving to deliver leukocytes. Vessels will stand out in the section because of the attraction of leukocytes to vessel walls.
Some generalizations regarding the pathogenesis of the vasculitis can be made from types of leukocytes present within vessel walls; however, the types of leukocytes present do not necessarily point to a particular etiology and may simply reflect the stage of the disease process.
-
•
Neutrophilic vasculitis is most suggestive of a type III immune-complex hypersensitivity reaction and is often referred to as leukocytoclastic vasculitis if neutrophil degeneration and nuclear karyorrhexis are evident. Examples include the vasculitis associated with staphylococcal dermatitis in dogs, immune-mediated vasculitis as in SLE, some drug eruptions, and septicemia. In the case of septicemia, the vasculitis tends to be non-leukocytoclastic.
-
•
Lymphocytic vasculitis may suggest a cell-mediated immune basis, such as rabies vaccine–induced cutaneous vasculitis and some drug eruptions.
-
•
Eosinophilic vascular infiltrates are most suggestive of a type I hypersensitivity reaction. Eosinophils may be the predominant cells in some cases of equine vasculitis and in association with the markedly eosinophilic dermatitis seen in some arthropod bite lesions, mast cell tumors, or in lesions of the eosinophilic granuloma complex in the cat. Eosinophilic vasculitis has been documented in cases of drug reaction and in some dogs with food hypersensitivity.
-
•
Involvement of deep dermal blood vessels in all cases may suggest systemic disease.
-
•
In dogs, cutaneous vasculitis has been associated with drugs, systemic or localized infections (Rocky Mountain spotted fever, Babesia, staphylococcal pyoderma), malignancies, and connective tissue diseases. Three cases of cutaneous vasculitis have been reported in dogs seropositive for Bartonella vinsonii; all dogs responded to antimicrobial treatment.
Familial or inherited forms of vasculitis have also been recognized.
-
•
A syndrome of cutaneous ulceration in conjunction with limb edema and/or acute renal failure, referred to as cutaneous and renal glomerular vasculopathy (CRGV) of Greyhounds, or in layman's terms “Alabama rot,” has been reported sporadically in young Greyhounds throughout the United States. Multifocal cutaneous ulcers, renal afferent arteriolar and dermal arterial thrombosis, azotemia, microangiopathic hemolytic anemia, and thrombocytopenia with normal coagulation times characterize CRGV. Cutaneous lesions may occur in the absence of renal or other systemic disease. The syndrome has many features in common with the hemolytic-uremic syndrome in people caused by a Shiga-like toxin–induced endothelial cell necrosis. Studies have failed to identify infectious agents, toxins, or evidence of an immune-mediated reaction in CRGV. Exposure to Shiga-like toxin–producing Escherichia coli has not been completely ruled out. Affected dogs may be genetically predisposed to develop CRGV as outbreaks have occurred in related groups of dogs. Hemorrhage, fibrinoid arteritis, thrombosis with infarction, and ulceration characterize the skin lesions that are most often found on the limbs. Renal glomerular necrosis and tubular necrosis are present in the kidneys.
-
•
An arteritis affecting the nasal philtrum has been documented in adult Saint Bernards, one Giant Schnauzer, and one Basset Hound. It has been reported anecdotally in several other breeds. The dogs develop deep deforming ulcers on the philtrum and may have episodes of arterial bleeding. Deep dermal arteries and arterioles have a subendothelial spindle cell proliferation with fibrosis and deposition of mucinous (Alcian blue–positive) matrix.
-
•
A genodermatosis affecting German Shepherd dog puppies characterized by swelling, depigmentation; frequent ulceration of footpads, pinnae, and tail tips; and nasal planum depigmentation has been reported in Canada. A neutrophilic to mononuclear nodular dermatitis, dermal collagenolysis, and subtle vasculitis are present histologically. Nasal lesions correspond to a hydropic interface dermatitis. The cause is unknown but presumed to be immunologically mediated as lesions are temporally related to vaccination dates. Dogs recover by 5-6 months of age. The condition may also be related to an underlying collagen disorder, as musculoskeletal abnormalities are also present.
-
•
Familial vasculitis has been reported in a litter of Scottish Terriers. Lesions were limited to the nasal epithelium and mucosa and were characterized by leukocytoclastic vasculitis and pyogranulomatous inflammation, leading to ulceration and destruction of the nasal planum.
-
•
Cutaneous vasculitis has been reported in Jack Russell Terriers, leading to alopecia and ulcerative lesions of the extremities and bony prominences with histologic lesions virtually indistinguishable from dermatomyositis of Collies and Shetland Sheepdogs (see Congenital and hereditary diseases of skin).
In horses, cutaneous vasculitis has been seen with or following numerous infections, such as with Streptococcus, influenza A virus, equine arteritis virus, equine infectious anemia virus, Ehrlichia, Rhodococcus equi, and Corynebacterium pseudotuberculosis.
-
•
Equine purpura hemorrhagica is an acute, usually streptococcal infection (strangles)-associated, leukocytoclastic vasculitis characterized clinically by urticaria and extensive edema of the distal limbs, ventrum, and head. These swellings may progress to exudation and sloughing.
-
•
Pastern leukocytoclastic vasculitis is a syndrome unique to the horse that affects the unpigmented, sun-exposed skin of distal extremities and sometimes muzzle; hence ultraviolet radiation is thought to play a role in pathogenesis. Adult horses are most often affected. There is no evidence of liver disease or exposure to photosensitizing compounds. Interestingly, a single limb may be affected, although other limbs lack pigment as well. Lesions are crusty, eroded or ulcerated, sharply demarcated, and may be associated with extensive edema and pain. Histologically, leukocytoclastic vasculitis of the superficial dermal vessels is present. Chronic cases develop papillary hyperplasia of the epidermis, giving the lesion a verrucous appearance.
-
•
Nodular eosinophilic vasculitis is seen as firm, painful, nodular to linear lesions on one or more legs. Lesions may ulcerate, bleed, and crust.
Cutaneous vasculitis in pigs is most commonly associated with Erysipelothrix rhusiopathiae infection. Systemic vasculitis affecting primarily the skin and kidneys occurs in pigs and has been called the porcine dermatitis and nephropathy syndrome. Skin lesions consist of irregularly enlarging hemorrhagic macules and papules on the ears, limbs, abdomen, thorax, and perineum. Leukocytoclastic vasculitis is present in the dermis, panniculus, synovium, and renal pelvis. Pigs have concurrent pneumonia and pathogenesis studies indicate that porcine circovirus 2 is associated with the condition.
Direct immunofluorescence testing or immunohistochemistry may demonstrate immunoglobulin and/or complement in vessel walls and occasionally at the basement membrane zone in suspected cases of vasculitis. Positive tests are most likely in lesions <24 hours old. False positives occur also. Adverse drug reactions, infection, familial vasculopathies, cryopathies, and systemic autoimmune diseases, such as SLE, should be ruled as possible causes. In many cases, a specific cause cannot be determined.
Further reading
Affolter VK, von Tscharner C. Cutaneous drug reactions: a retrospective study of histopathological changes and their correlation with the clinical disease. Vet Dermatol 1992;3:157-163.
Breitschwerdt EB, et al. Clinicopathological abnormalities and treatment response in 24 dogs seroreactive to Bartonella vinsonii (berkhoffi) antigens. J Am Anim Hosp Assoc 2004;40:92-101.
Cowan LA, et al. Clinical and clinicopathologic abnormalities in greyhounds with cutaneous and renal glomerular vasculopathy: 18 cases (1992-1994). J Am Vet Med Assoc 1997;210:789-793.
Francis AH, et al. Adverse reactions suggestive of type III hypersensitivity in six healthy dogs given human albumin. J Am Vet Med Assoc 2007;230:873-879.
Ihrke PJ. Cutaneous adverse drug reactions. Compend Contin Educ Pract Vet 1997;(Suppl. 19):87-92.
Innerå M. Cutaneous vasculitis in small animals. Vet Clin North Am Small Anim Pract 2013;43:113-134.
Jasani S, et al. Systemic vasculitis with severe cutaneous manifestation as a suspected idiosyncratic hypersensitivity reaction to fenbendazole in a cat. J Vet Intern Med 2008;22:666-670.
Malik R, et al. Acute febrile neutrophilic vasculitis of the skin of young Shar-Pei dogs. Aust Vet J 2002;80:200-206.
Mellor PJ, et al. Neutrophilic dermatitis and immune-mediated haematological disorders in a dog: suspected adverse reaction to carprofen. J Small Anim Pract 2005;46:237-242.
Morris DD. Cutaneous vasculitis in horses: 19 cases (1978-1985). J Am Vet Med Assoc 1987;191:460-464.
Nichols PR, et al. A retrospective study of canine and feline cutaneous vasculitis. Vet Dermatol 2001;12:255-264.
Niza MM, et al. Cutaneous and ocular adverse reactions in a dog following meloxicam administration. Vet Dermatol 2007;18:45-49.
Opriessnig T, Langohr I. Current state of knowledge on porcine circovirus type 2-associated lesions. Vet Pathol 2013;50:23-38.
Parker WM, Foster RA. Cutaneous vasculitis in five Jack Russell Terriers. Vet Dermatol 1996;7:109-115.
Pedersen K, Scott DW. Idiopathic pyogranulomatous inflammation and leukoclastic vasculitis of the nasal planum, nostrils, and nasal mucosa in Scottish Terriers in Denmark. Vet Dermatol 1991;2:85-89.
Powell C, et al. Type III hypersensitivity reaction with immune complex deposition in 2 critically ill dogs administered human serum albumin. J Vet Emerg Crit Care (San Antonio) 2013;23:598-604.
Pratschke KM, Hill PB. Dermal arteritis of the nasal philtrum: surgery as an alternative to long-term medical therapy in two dogs. J Small Anim Pract 2009;50:99-103.
Psalla D, et al. Equine pastern vasculitis: a clinical and histopathologic study. Vet J 2013;198:524-530.
Scott DW, Miller WH. Immune-mediated disorders. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 314-359.
Segales J, et al. Porcine dermatitis and nephropathy syndrome in Spain. Vet Rec 1998;142:483-486.
Tasaki Y, et al. Generalized alopecia with vasculitis-like changes in a dog with babesiosis. J Vet Med Sci 2013;75:1367-1369.
Thibault S, et al. Cutaneous and systemic necrotizing vasculitis in swine. Vet Pathol 1998;35:108-116.
Torres SM, et al. Dermal arteritis of the nasal philtrum in a Giant Schnauzer and three Saint Bernard dogs. Vet Dermatol 2002;13:275-281.
von Tscharner C, et al. Stannard's illustrated equine dermatology notes. Vet Dermatol 2000;11:163-178.
Weir JAM, et al. Familial cutaneous vasculopathy of German shepherds: clinical, genetic, and preliminary pathological and immunological studies. Can Vet J 1994;35:763-769.
White SD, et al. Cutaneous vasculitis in equines: a retrospective study of 72 cases. Vet Dermatol 2009;20:600-606.
Yager JA, Wilcock BP. Vasculitis. In: Yager JA, Wilcock BP, editors. Color Atlas and Text of Surgical Pathology of the Dog and Cat: Dermatopathology and Skin Tumors. London: Mosby Year Book; 1994. p. 107-118.
Rabies vaccine–induced vasculitis and alopecia in dogs
This disease is characterized by a localized inflammatory and ischemic reaction to subcutaneously administered rabies vaccine in the dog. Although any breed can be affected, the disorder typically affects small-breed dogs such as Poodles, Yorkshire Terriers, and Silky Terriers. The pathogenesis remains unknown, but formation of antigen-antibody complexes that become lodged in vessel walls (a type III hypersensitivity response) has been proposed.
There are 2 clinical presentations: a localized form where the lesion arises at the site of vaccination and a generalized form that mimics canine familial dermatomyositis. The localized form is common and develops several months after vaccination. The gross lesion is a focal, typically depressed, alopecic, and hyperpigmented patch (Fig. 6-77A ). The histologic features are characteristic and involve combination of changes in the subcutis, dermis, adnexa, and basement membrane zone/epidermis. Panniculitis is only present at the site of vaccination. The vascular lesions are subtle and not seen in all cases. Venules, arterioles, and small arteries develop a very mild chronic lymphocytic vasculitis, characterized by thickening of the vessel wall, a few intramural mononuclear inflammatory cells, scattered nuclear debris, and variable perivascular mononuclear infiltrates (Fig. 6-77B). Occasionally, a more florid leukocytoclastic vasculitis is seen. A cell-poor interface dermatitis with vacuolar change in the basal epithelial layer and pigmentary incontinence and mural folliculitis may be present in some cases. The dermis is atrophic and hyalinized, sometimes mucinous. Hair follicles are markedly atrophied and pale staining (“faded”) (Fig. 6-77C). At the site of vaccination, the subcutis contains lymphocytic panniculitis, and some cases may have blue-grey material (vaccine product) extracellularly and within the cytoplasm of macrophages. The additional lesions of erosions and ulcers of the oral mucosa and skin of the extremities and bony prominences and ischemic myopathy in subjacent musculature have been reported in cases with multicentric involvement. Immunofluorescence staining has identified rabies antigen in the vessels and epithelium of the hair follicles. A low-grade immune-mediated vasculitis with resultant tissue anoxia, leading to the atrophic changes in the overlying skin has been suggested as the pathogenesis. Lesions may remain for months to years. Differential diagnoses include dermatomyositis, traction alopecia, idiopathic vasculopathy, and lupus profundus.
Figure 6-77.


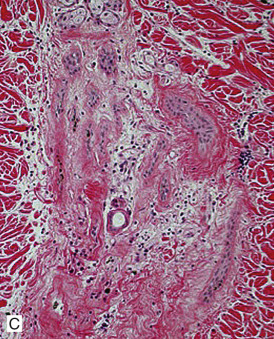
Rabies vaccine–associated vasculitis. A. Focal area of alopecia on the dorsum in a Yorkshire Terrier. B. Marked atrophy of follicles with smudged dermal collagen and lymphocytic panniculitis. C. Higher magnification showing marked follicular atrophy (faded follicles).
Further reading
Morris DO. Ischemic dermatopathies. Vet Clin North Am Small Anim Pract 2013;43:99-111.
Nichols PR, et al. A retrospective study of canine and feline cutaneous vasculitis. Vet Dermatol 2001;12:255-264.
Vitale CB, et al. Vaccine-induced ischemic dermatopathy in the dog. Vet Dermatol 1999;10:131-142.
Wilcock BP, Yager JA. Focal cutaneous vasculitis and alopecia at sites of rabies vaccination in dogs. J Am Vet Med Assoc 1986;188:1174-1177.
Canine uveodermatologic syndrome (Vogt-Koyanagi-Harada [VKH] syndrome)
This syndrome, seen only in dogs and humans, is characterized by the concurrent acute onset of bilateral uveitis and depigmentation of the nose, lips, eyelids, and occasionally the footpads and anus. Although the cause of the disorder is unknown, a cell-mediated hypersensitivity to melanin has been hypothesized. VKH is discussed further under Disorders of pigmentation.
Plasma cell pododermatitis
This is a rare disorder of cats of all breeds, ages, and sex. A possible link to feline immunodeficiency virus (FIV) has been suggested, and one study demonstrated 50% of plasma cell pododermatitis cases tested positive for FIV. Although the pathogenesis is unknown, an immune-mediated basis is suggested by the tissue plasmacytosis, hypergammaglobulinemia, and beneficial response to immunosuppressive and immunomodulating drugs (e.g., doxycycline monohydrate). In addition, occasional cats have other abnormalities, such as renal amyloidosis, plasmacytic stomatitis, positive antinuclear antibody tests, Coombs-positive anemia, polyclonal gammopathy, or glomerulonephritis with positive direct immunofluorescence testing (immunoglobulin deposited at the basement membrane zone). PCR testing of tissue digests has been performed to assess for infectious agents, and particularly those that may respond to the antimicrobial properties of doxycycline (e.g., Bartonella spp., Ehrlichia spp., Anaplasma phagocytophilum, Chlamydophila, Mycoplasma spp.). DNA of those pathogens was not amplified from tissue.
Clinically, plasma cell pododermatitis begins as soft, nonpainful swelling of multiple footpads on multiple paws. The central metacarpal or metatarsal pads are usually most severely affected. Affected pads feel soft resulting from collapse of the underlying fatpad. Footpad surfaces are crosshatched with white scaly striae but may become ulcerated or develop fleshy granulomatous proliferations that may hemorrhage. Lameness develops with progression of the lesions. Some cases spontaneously resolve or may recur seasonally.
Histologically, early lesions are characterized by superficial and deep perivascular dermatitis with plasma cells predominating. Later, there is a diffuse plasmacytic dermatitis. Russell bodies can be numerous. Leukocytoclastic vasculitis is rarely seen. Ulcerated or proliferative lesions show various degrees of superimposed suppurative-to-pyogranulomatous inflammation. The gross and histologic features are diagnostic.
Further reading
Bettenay SV, et al. Feline plasmacytic pododermatitis: a prospective study of a novel treatment using systemic doxycycline. Vet Rec 2003;152:564-566.
Bettenay SV, et al. An immunohistochemical and polymerase chain reaction evaluation of feline plasmacytic pododermatitis. Vet Pathol 2007;44:80-83.
Dias Pereira P, Faustino AM. Feline plasma cell pododermatitis: a study of 8 cases. Vet Dermatol 2003;14:333-337.
Guaguere E, et al. Feline plasma cell pododermatitis: a retrospective study of 26 cases. Vet Dermatol 2004;15(Suppl. 1):27.
Cutaneous amyloidosis
The physical structure of amyloid gives it special properties, such as apple-green birefringence when Congo red–stained sections are polarized. Primary cutaneous amyloidosis is thought to share a common pathway with other amyloid diseases. The amyloid fibrils (AL amyloid) are derived from monoclonal immunoglobulin light chains. Cutaneous amyloidosis occurs rarely in horses, dogs, and cats. The cutaneous lesion in dogs has been associated with monoclonal gammopathy, dermatomyositis, and is seen occasionally in the stroma of plasmacytomas of skin and oral cavity (see Cutaneous plasmacytoma). In dogs with monoclonal gammopathy, purpuric lesions are seen, and cutaneous hemorrhage is easily induced by minor external trauma. The superficial dermis contains an amorphous, homogeneous, eosinophilic substance, and the walls of blood vessels in the involved area are thickened by deposits of the same substance. There may be a familial tendency in Abyssinian and Siamese cats. Cutaneous amyloidosis is usually associated with chronic inflammation, neoplasia, and accumulations of plasma cells.
The pathogenesis of amyloidosis in horses is unclear. The lesions are multiple, asymptomatic papules, nodules, and plaques that are seen most commonly on the head, neck, shoulders, and pectoral region. There is no established breed, age, or sex predisposition. The lesions are firm, well circumscribed, and 0.5-10 cm in diameter. The overlying skin and haircoat are normal. The initial lesions may be urticarial in type. The cutaneous lesions may be accompanied by similar nodules in the respiratory mucosa and regional lymph nodes but are seldom associated with systemic amyloidosis. Lesions may regress, become recurrent or progressively enlarge. Histologic findings include nodular-to-diffuse granulomatous dermatitis and panniculitis. Large extracellular deposits of amyloid appear as variably sized areas of homogeneous, amorphous, hyaline, eosinophilic material, which may contain clefts or fractures. Multinucleated histiocytic giant cells are usually numerous. Clinical differentials include infectious and noninfectious granulomas, cutaneous neoplasms, and eosinophilic granulomas.
Further reading
Borowicz J, et al. Nodular cutaneous amyloidosis. Skinmed 2011;9:316-318.
Gliatto JM, Alroy J. Cutaneous amyloidosis in a horse with lymphoma. Vet Rec 1995;137:68-69.
Gross TL, Ihrke PJ. Cutaneous amyloidosis. In: Gross TL, et al., editors. Veterinary Dermatopathology: A Macroscopic and Microscopic Evaluation of Canine and Feline Skin Disease. St Louis: Mosby Year Book; 1992. p. 229-232.
Mathison PT. Eosinophilic nodular dermatoses. Vet Clin North Am Equine Pract 1995;11:81-83.
Woldemeskel M. Primary localized nodular cutaneous amyloidosis in a male neutered Golden Retriever. Dtsch Tierarztl Wochenschr 2007;114:473-475.
Alopecia areata
Alopecia areata (AA) is a nonscarring, presumably autoimmune, alopecic inflammatory disorder directed against hair follicles in humans, nonhuman primates, dogs, cats, horses, and cattle. Alopecia areata may be focal, multifocal, or generalized (alopecia universalis). Lesions occur most commonly on the face, neck, and trunk (Fig. 6-78A ). Some horses may have hair loss on the mane and tail. Areas of alopecia are usually hyperpigmented and may exhibit sparse short and dystrophic hairs Leukotrichia may be seen in some animals initially. Lesions may be bilaterally symmetrical. There is no apparent age, breed, or sex predilection. Rodent models are available to study the condition—the C3H/HeJ mouse and the Dundee experimental bald rat.
Figure 6-78.

Alopecia areata in a dog. A. Note discrete area of non-inflamed, hyperpigmented alopecic skin.
(Courtesy M.S. Canfield.)
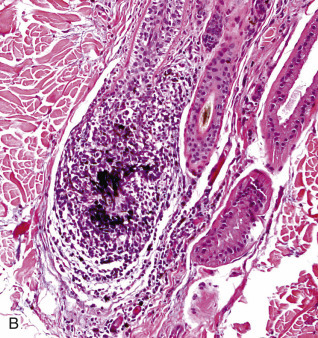
B. Peribulbar lymphocytic folliculitis. Lymphocytes are in and around the hair bulb.
Early, clinically active lesions are characterized histologically by an accumulation of lymphocytes (“swarm of bees”) in and around the inferior segment of anagen hair follicles—the classic example of peribulbar lymphocytic folliculitis (Fig. 6-78B). Unfortunately, the classic lesion is not always evident, and more subtle bulbar inflammation is the rule. Bulbar keratinocytes are frequently vacuolated, apoptotic, or karyorrhectic. Pigmentary incontinence and melanophagia in the peribulbar region are also typical findings. Telogen follicles are unaffected, and dystrophic hair follicles may be present. Demonstration of the lymphocytic peribulbitis may be difficult and require examination of multiple sections from different levels of the paraffin-embedded biopsy specimen. Immunostaining to detect CD3+ lymphocytes may be helpful in some cases. Biopsies from the periphery of early, expanding lesions are most rewarding. Histologic findings in chronic, clinically static lesions are nondiagnostic, revealing a predominance of telogen hair follicles and follicular atrophy that may be misdiagnosed as an endocrine skin disorder. Immunologic studies in dogs and horses have indicated that the intrabulbar lymphocytes are primarily cytotoxic CD8+ lymphocytes. CD1+ dendritic antigen-presenting cells and both CD8+ and CD4+ lymphocytes are found in the peribulbar infiltrate. In addition, various autoantibodies targeting trichohyaline, hair keratins, and other components of the hair follicle have been demonstrated in various species, indicating a role for humoral immunity. In dogs and horses, AA frequently reverses spontaneously; however, sometimes the hair regrowth is white.
Clinical differentials include telogen effluvium and many other causes of lymphocytic mural folliculitis, such as erythema multiforme (EM), systemic lupus erythematosus (SLE), graft-versus-host disease (GVHD), ischemia, and demodicosis, to name a few. The distinguishing feature of AA is the fact that the hair bulb and inferior segment of anagen hairs are the primary targets of inflammation rather than the infundibulum or the isthmus, although the isthmus has been reported to be affected in a horse.
Further reading
Colombo S, et al. Alopecia areata with lymphocytic mural folliculitis affecting the isthmus in a thoroughbred mare. Vet Dermatol 2004;15:260-265.
De Jonghe SR, et al. Trachyonychia associated with alopecia areata in a Rhodesian Ridgeback. Vet Dermatol 1999;10:123-126.
Gross TL, et al. Anatomical classification of folliculitis. Vet Dermatol 1997;8:147-156.
McElwee KJ, et al. Comparison of alopecia areata in humans and nonhuman mammalian species. Pathobiol 1998;66:368-376.
Olivry T, et al. Antifollicular cell-mediated and humoral immunity in canine alopecia areata. Vet Dermatol 1996;7:67-79.
Rosychuk RA. Noninflammatory, nonpruritic alopecia of horses. Vet Clin North Am Equine Pract 2013;29:629-641.
Timm K, et al. Alopecia areata in Eringer cows. Vet Dermatol 2010;21:545-553.
Tobin DJ, et al. A natural canine homologue of alopecia areata in humans. Br J Dermatol 2003;149:938-950.
Valentine BA, et al. Alopecia areata in two black Angus cows. J Vet Diagn Invest 2012;24:405-407.
Viral Diseases of Skin
Cutaneous lesions occur in the course of a number of viral diseases in domestic animals. Viruses may induce skin lesions upon local infection, but the intact integument is resistant to viral penetration; injection via an arthropod bite or introduction through a cutaneous wound is a prerequisite for infection. Examples of local viral infection include papillomas induced by the papillomaviruses, bovine mammillitis induced by a herpesvirus, and the so-called milker's nodule in humans caused by a parapoxvirus. More often, viruses localize in the skin during the viremic phase of a systemic infection. Examples include some poxvirus infections, malignant catarrhal fever, and the vesicular diseases, such as vesicular stomatitis and foot-and-mouth disease. Pantropic viruses, such as canine distemper virus and classical swine fever virus, may cause cutaneous lesions; but most viruses causing cutaneous lesions are epitheliotropic. Some epitheliotropic viruses, in particular the poxviruses, have a predilection for the epithelium of the skin. Others, including the viruses associated with the mucosal diseases, cause primary lesions in the alimentary tract with lesser involvement of the skin.
A “rash,” comprising erythematous macules caused by long-lasting dilation of dermal blood vessels, is often associated with systemic viral disease in humans. Such lesions are uncommon in animals, but may be hidden by the haircoat. Exceptions are the cutaneous erythema occurring in classical swine fever and African swine fever, and hemorrhagic diathesis of skin occurring with disseminated porcine adenovirus infection. In addition, a condition known as dermatitis/nephropathy syndrome of pigs, seen clinically as erythematous macules, papules, and plaques, caused by cutaneous and systemic necrotizing vasculitis, is associated with porcine circovirus 2 (PCV-2) infection.
Cutaneous viral diseases are more common in food-producing animals than in pets. Some of these diseases, notably sheeppox, cause significant mortality. Others have an economic impact because of their deleterious effect on production. Herpes mammillitis and pseudocowpox, for example, reduce milk yield in dairy cattle; contagious pustular dermatitis affects the growth rate of lambs by interfering with their ability to suckle. A few of the large animal viral dermatoses are extremely mild, for example, molluscum contagiosum in the horse.
Systemic viral diseases with cutaneous manifestations are rare in dogs and cats. Canine distemper virus is associated with nasodigital hyperkeratosis, so-called “hard pad” disease, and pustular dermatitis. In cats, rare occurrences of cutaneous disease occur with feline calicivirus infection. Cutaneous lesions caused by felid herpesvirus 1 can occur in the absence of respiratory disease, a presumed recrudescence of a latent herpesvirus infection.
Traditionally, viral diseases have been diagnosed by light and electron microscopy, serology, and viral culture. However, the development of monoclonal antibodies to specific viruses for use with immunofluorescence and immunoperoxidase techniques is increasingly being used for specific and rapid diagnosis. PCR testing can be used to detect virus-encoded DNA and RNA and identify many different viruses. In addition, viral genome DNA sequencing has led to the detection and understanding of the relationships among many different viruses.
Further reading
Fenner F, et al. Veterinary Virology. 2nd ed. San Diego: Academic Press; 1993.
Koutinas AF, et al. Histopathology and immunohistochemistry of canine distemper virus-induced footpad hyperkeratosis (hard pad disease) in dogs with natural canine distemper. Vet Pathol 2004;41:2-9.
Segales J. Porcine circovirus type 2 (PCV2) infections: clinical signs, pathology and laboratory diagnosis. Vir Res 2012;164:10-19.
Tang KN, et al. Disseminated adenovirus infection associated with cutaneous and visceral hemorrhages in a nursing piglet. Vet Pathol 1995;32:433-437.
Thibault S, et al. Cutaneous and systemic necrotizing vasculitis in swine. Vet Pathol 1998;35:108-116.
Timoney JF, et al. Hagan and Bruner's Microbiology and Infectious Diseases of Domestic Animals. 8th ed. Ithaca, NY: Comstock Publishing; 1988.
Poxviral infections
The Poxviridae is a large family of complex DNA viruses. Highly epitheliotropic, they cause cutaneous and systemic disease in birds, wild and domestic mammals, and humans. Some species of the Poxviridae, including Sheeppox virus, Ectromelia virus, Monkeypox virus, and the now eradicated Variola virus (human smallpox), cause severe systemic disease. Others cause mild, localized disease, for example, pseudocowpox, which chiefly affects the teats of milking cows. A few poxviruses are associated with hyperplastic or neoplastic conditions, such as molluscum contagiosum in horses and Shope fibroma of rabbits.
The Poxviridae share group-specific nucleoprotein antigens. Animal poxviruses are in the subfamily Chordopoxvirinae. The genera (species names italicized) include
-
•
Parapoxvirus: Orf virus (contagious pustular dermatitis virus, contagious ecthyma virus), Pseudocowpox virus (milker's nodule virus), Bovine papular stomatitis virus, and Parapox virus of red deer. Unassigned members in the genus are Auzduk disease virus (camel contagious ecthyma virus), chamois contagious ecthyma virus, sealpox virus, and a virus that causes papillomatous dermatitis and pododermatitis in cattle.
-
•
Orthopoxvirus: Cowpox virus, Vaccinia virus (buffalopox virus, rabbitpox virus), Horsepox virus, Camelpox virus, Ectromelia virus (mousepox virus), and Monkeypox virus; unassigned member of the genus is Uasin Gishu disease virus
-
•
Molluscipoxvirus: Molluscum contagiosum virus
-
•
Capripoxvirus: Sheeppox virus, Goatpox virus, Lumpy skin disease virus
-
•
Suipoxvirus: Swinepox virus
-
•
Avipoxvirus: Fowlpox virus, Pigeonpox virus, and many other avian poxviruses.
-
•
Leporipoxvirus: Myxoma virus; Rabbit fibroma virus (Shope fibroma virus).
-
•
Yatapoxvirus: Tanapox virus, Yaba monkey tumor virus
Many of the poxviruses are host specific; but the orthopoxviruses, such as Cowpox virus and Vaccinia virus, affect a wide range of species. Some poxviruses, for example Pseudocowpox virus, are zoonotic. Infection is usually achieved by cutaneous or respiratory routes. Poxviruses, whether acquired by the subcutaneous or respiratory routes, usually gain access to the systemic circulation via the lymphatic system, although multiplication at the site of injection in the skin may lead to direct entry into the blood and primary viremia. Secondary viremia disseminates the virus back to the skin and to other target organs.
Poxviruses induce lesions by a variety of mechanisms. Degenerative changes in the epithelium are caused by virus replication and induce vesicular lesions typical of many poxvirus infections. Degenerative lesions in the dermal or submucosal tissues sometimes result from ischemia secondary to vascular damage caused by viral multiplication in endothelial cells. Poxvirus infections also induce proliferative lesions. Poxviruses, such as Orf virus, replicating in the epidermis typically induce hyperplasia along with degenerative changes. Host cell DNA synthesis is stimulated before the onset of cytoplasmic virus-related DNA replication. Proliferative changes may be explained by a gene, present in several poxviruses, including Molluscum contagiosum virus, whose product has significant homology with epidermal growth factor. Poxviruses also encode for functions that may counteract host defenses. These include genes related to those encoding the serine protease inhibitors (SERPINs), a superfamily of related proteins important in regulating serine protease enzymes that mediate kinin, complement, fibrinolytic and coagulation pathways, and genes encoding anti-interferon activities.
Pox lesions have a typical developmental sequence. They commence as erythematous macules, become papular, and then vesicular. The vesicular stage is well developed in some pox infections, such as sheeppox, and is transient or non-existent in others, such as contagious pustular dermatitis. Vesicles develop into umbilicated pustules with a depressed center and a raised, often erythematous border. This lesion is the so-called “pock.” The pustules rupture, and a crust forms on the surface. This crust may become very thick, as in lesions of contagious pustular dermatitis. Lesions heal and often leave a residual scar. The mucosal lesions are briefly vesicular and develop into ulcers rather than pustules.
Histologically, pox lesions begin as epidermal cytoplasmic swelling and vacuolation, usually first affecting the cells of the outer stratum spinosum. There is evidence, from experimental studies with the virus of contagious pustular dermatitis, that postinjury proliferating keratinocytes are the target for viral replication. Rupture of the damaged keratinocytes produces multiloculated vesicles, so-called reticular degeneration. The early dermal lesions include edema, vascular dilation, a perivascular mononuclear cell infiltrate, and a variable neutrophilic infiltrate. Neutrophils migrate into the epidermis and aggregate in vesicles to form microabscesses. Large intraepidermal pustules may form and sometimes extend into the superficial dermis. There is usually marked epithelial hyperplasia and sometimes pseudocarcinomatous hyperplasia of the adjacent epithelium. This contributes to the raised border of the umbilicated pustule. Rupture of the pustule produces an inflammatory crust, often colonized on its surface by bacteria.
Poxvirus lesions often contain characteristic intracytoplasmic inclusion bodies. These are single or multiple and of variable size and duration. The more prominent inclusions are designated type A. They are eosinophilic, reflecting their high protein content, and weakly Feulgen positive. Smaller, basophilic, Feulgen-positive, type B bodies also occur and represent the site of virus replication.
Diagnosis of poxvirus infections is usually based on typical clinical appearance and may be supported by characteristic histologic lesions. Parapoxviruses are ultrastructurally distinct from the other poxviruses that are morphologically similar to each other when viewed by electron microscopy.
Further reading
Buller RM, Palumbo GJ. Poxvirus pathogenesis. Microbiol Rev 1991;55:80-122.
Fenner F, et al. The Orthopoxviruses. New York: Academic Press; 1989.
Lewis-Jones S. Zoonotic poxvirus infections in humans. Curr Opin Infect Dis 2004;17:81-89.
Mercer A, et al., editors. Poxviruses. Birkhauser Advances in Infectious Diseases. Basel: Birkhauser Biosciences; 2007.
Parapoxviral diseases
Contagious pustular dermatitis.
Contagious pustular dermatitis is a highly contagious zoonotic poxviral disease of sheep and goats, with incidental infections occurring in humans, camelids, cattle, and many wild ruminants, and very rarely dogs. Dogs may acquire infection by eating infected lamb carcasses. The disease is caused by species Orf virus (ORFV), a Parapoxvirus closely related to Pseudocowpox virus and Bovine papular stomatitis virus. Synonyms for contagious pustular dermatitis include contagious ecthyma, orf, infectious labial dermatitis, soremouth, and scabby mouth.
The disease is geographically widespread and occurs wherever sheep or goats are raised. The virus can repeatedly infect sheep and goats, and although live-virus vaccines control the disease and decrease the severity of the disease, they also ensure its continuance by perpetuating infection in the environment. The economic significance of contagious pustular dermatitis results chiefly from loss of condition, because affected animals neither suckle nor graze. Morbidity in a susceptible population may reach 90%, but mortality rarely exceeds 1% unless secondary infection intervenes, or unless the animals are immunosuppressed or stressed, in which case mortality can be high. Mortality often results from the invasion of primary lesions by the larvae of the screwworm fly (Cochliomyia hominivorax) or by bacteria such as Fusobacterium necrophorum and occasionally Dermatophilus congolensis. Cellulitis may complicate pedal lesions, mastitis may complicate mammary lesions, and necrotizing stomatitis and aspiration pneumonia may complicate oral lesions.
Contagious pustular dermatitis affects sheep and goats of all breeds. It is predominantly a disease of lambs and kids. Infection is established through cutaneous abrasions, particularly those associated with dry and prickly pasture or forage. Clinically affected lambs may transmit the virus to the udder of the ewe. The virus is hardy and probably persists in a dry environment indefinitely in crust material shed from affected animals. Chronically infected, reinfected, or possibly, latently infected carrier animals may allow the virus to persist in a flock for several years.
Viral vascular endothelial growth factor (VEGF) is an important virulence gene in the pathogenesis of orf. Epidermal hyperplasia and capillary growth with increased vascular permeability allows increased virus replication and formation of crusts. Crusts rich in virus particles favor the chances of virus survivability in the environment for extended periods. Via the CD95 pathway, ORFV can induce apoptosis of antigen-presenting cells. By inhibiting Bcl-2 (B-cell lymphoma 2), the virus is also able to inhibit apoptosis of virally infected cells.
Gross lesions usually commence at the commissures of the lips and spread around the lip margins to the muzzle and sometimes on the face and around the eyes (Fig. 6-79A ). In severe cases, lesions may develop on the gingiva, dental pad, palate, and tongue. Lesions mainly confined to the tongue must be differentiated from those of foot-and-mouth disease. The buccal lesions are raised, red, or gray foci with a surrounding zone of hyperemia. Very rarely, lesions extend to the esophagus, rumen, and omasum in the lower alimentary canal, causing ulcerative gastroenteritis, and in lungs and heart. Lesions on the limbs are less common than on the lips and tend to involve the coronet, interdigital cleft, and bulb of the heels. They may extend, in severe cases, to the knee or hock on the caudal aspect of the leg. Lesions of the mammary gland affect the teats and adjacent skin of the udder. Lesions may develop in other areas of sparsely wooled skin, such as the inner thigh, axilla, and the edge of wounds in recently earmarked lambs, or tail-dock sites. Proliferative lesions affecting predominantly the head, neck, and body have been described in Nubian goats.
Figure 6-79.

Contagious pustular dermatitis (orf). A. Crusted lesions around the eyes and at the margins of the lips in a goat.
(Courtesy W.H. Miller).
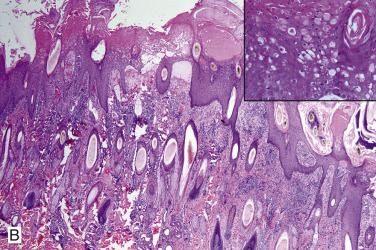
B. Epidermal hyperplasia with marked intracellular edema of keratinocytes, reticular degeneration, and intracytoplasmic eosinophilic inclusion bodies (see inset). Marked edema and perivascular dermatitis.
The lesions develop through the typical pox phases but are much more proliferative. The vesicular stage is transient and pustules are flat rather than umbilicated. The most significant feature of the gross lesion is the layer of thick brown-gray crust that may be elevated 2-4 mm above the skin surface. Depending on the degree of secondary infection, regression is usually complete by 4 weeks. Papillomatous growths, resulting from continued epidermal proliferation, sometimes occur.
A severe persistent and generalized form of the disease has been described in Boer goats and crosses. All affected animals have had multifocal severe proliferative dermatitis and peripheral lymphadenopathy that persisted for several months. A genetic defect or immune deficiency has been proposed. Premature thymic involution, suppurative arthritis, and pneumonia have been detected in many of these goats.
The microscopic lesions of contagious pustular dermatitis are characterized by vacuolation and swelling of keratinocytes in the stratum spinosum, reticular degeneration, marked epidermal proliferation, intraepidermal microabscesses, and accumulation of scale-crust (Fig. 6-79B). In experimentally abraded sheep skin, the active site of viral replication was found to be the newly proliferative keratinocyte population, growing up under the superficial necrotic layer. By ~30 hours postinfection, keratinocyte swelling and vacuolation commences in the outer stratum spinosum. It is accompanied by cytoplasmic basophilia, which corresponds ultrastructurally to an increased number of polyribosomes, presumably active in viral protein synthesis. Basophilic intracytoplasmic inclusion bodies are reported as early as 31 hours postinfection. By 72 hours postinfection, the keratinocytes show nuclear pyknosis and marked intracytoplasmic edema, leading to reticular degeneration. The term ballooning degeneration is often used, but the keratinocytes do not have the homogeneous eosinophilic cytoplasm typical of this condition. At this time, intracytoplasmic eosinophilic inclusion bodies appear (see Fig. 6-79B inset). The inclusion bodies persist for 3-4 days. The proliferative reaction in the epidermis is underway by 55 hours postinfection, with mitotic figures numerous in the stratum basale. By 3 days postinfection, the epithelium is 3-4 times normal thickness, and rete ridges are markedly elongated. Pseudocarcinomatous hyperplasia is common.
Dermal lesions include superficial edema, marked capillary dilation, and an early influx of neutrophils, followed by a marked accumulation of major histocompatibility complex class II dendritic cells, with CD4+ T cells, CD8+ T cells, and B cells. A thick layer of scale-crust is built up, composed of orthokeratotic and parakeratotic hyperkeratosis, proteinaceous fluid, degenerating neutrophils, cellular debris, and bacterial colonies. The subsequent microscopic appearance of the lesions depends on the degree of secondary bacterial infection.
Further reading
de la Concha-Bermejillo A, et al. Severe persistent orf in young goats. J Vet Diagn Invest 2003;15:423-431.
Gumbrell RC, McGregor DA. Outbreak of severe fatal orf in lambs. Vet Rec 1997;141:150-151.
Haig DM, Mercer AA. Ovine diseases. Orf Vet Res 1998;311-326.
Hosamani M, et al. Orf: an update on current research and future perspectives. Expert Rev Anti Infect Ther 2009;7:879-893.
Mercer A, et al. Molecular genetic analyses of parapox pathogenic for humans. Arch Virol Suppl 1997;13:25-34.
Ulcerative dermatosis of sheep.
Ulcerative dermatosis is a disease of the epidermis of sheep that has been reported in the literature as being caused by an unclassified poxvirus, which is similar to Orf virus, but the viruses do not cross-protect. The disease has been reported in South Africa, where it is known as “pisgoed” or “pisgras”; in the United Kingdom as a contagious venereal infection; and in the United States, where it is known as “lip and leg ulceration,” “anovulvitis,” “infectious balanoposthitis,” and “ulcerative vulvitis.” The various names indicate the essential features of the disease, which are ulcerative papules on the lips, face, legs, feet, vulva, prepuce, and occasionally, the glans penis. The genital lesions are transmissible by coitus.
Presumably, infection results from viral contact with damaged skin. The pathologic process is primarily ulcerative, with ulcers of up to 4-5 cm in diameter and 3-5 mm deep. Pus covers the granulation tissue at the base of the ulcer and underlies a scab that is thin, brown and bloody, and unlike the thick parakeratotic crusts that develop in contagious pustular dermatitis. The underlying dermis is diffusely swollen, especially in distensible parts, such as the vulva and prepuce. The lesions on the hairy parts of the face tend to be fairly well circumscribed, but those of the feet tend to spread, especially on the interdigital skin. The vulval lesions usually begin on the tip and spread around the margins of the lips. An ulcerative ring tends to form around the preputial orifice, but the preputial mucosa is spared. Lesions on the glans penis remain moist. The urethral process may become necrotic. The labial and pedal lesions must be distinguished from those of contagious pustular dermatitis and foot-and-mouth disease, and the preputial lesions must be distinguished from noncontagious forms of balanoposthitis. Detailed descriptions of the histopathology of ulcerative dermatitis are lacking; the lesions are supposedly distinguishable from those of contagious pustular dermatitis by the lack of epithelial hyperplasia.
Further reading
Steyn DG. Pisgoed or pisgras (ulcerative dermatosis). 16th Rep Direct Vet Services Anim Indust Union S Afr 1930;417-420.
Trueblood MS. Relationship of ovine contagious ecthyma and ulcerative dermatosis. Cornell Vet 1966;56:521-526.
Vestweber JG, Milleret RJ. Ulcerative dermatosis in sheep (a case report). Vet Med Small Anim Clin 1972;67:672-674.
Pseudocowpox.
Pseudocowpox is caused by species Pseudocowpox virus, genus Parapoxvirus. The virus is closely related to Bovine papular stomatitis virus and Orf virus. It is a common endemic infection in cattle throughout most of the world. Transmission occurs via contamination of skin abrasions. It affects chiefly milking herds and occasionally beef herds. Morbidity in a herd approaches 100%, but only 5-15% of cows are affected at any one time. The economic significance lies in the effect on milk production, either as a result of sore teats or because of secondary bacterial mastitis. Lesions typically affect the teats and udder and occasionally the perineum, medial thighs, and scrotum. Lesions usually start as erythematous macules and papules, and do not form the umbilicated pustules seen in cowpox and vaccinia infections. Instead, a characteristic ring or horseshoe-shaped crust forms that may become umbilicated as it expands, but infrequently ulcerates (Fig. 6-80 ). The histologic appearance of lesions is typical of other poxviral infections. The lesions usually heal within 6 weeks. Occasionally, lesions develop in the mouth and on the muzzle of suckling calves, and the infection can be spread by cross-suckling as well as poor hygiene in milking sheds. Transmission to people induces “milker's nodule.” The lesion in humans starts as an erythematous papule that becomes a nodule with a target-like appearance, red center surrounded by a white ring and then red peripheral margin. There is a red oozing center that forms a crust.
Figure 6-80.

Pseudocowpox in a cow. Note the horseshoe-shaped red crust on the teat.
(Courtesy E. Pichon.)
Bovine papular stomatitis.
Species Bovine papular stomatitis virus is distributed worldwide, and although it causes disease more commonly in cattle <1 year of age, it can occur at any age and in any breed. Like pseudocowpox, transmission occurs via contamination of skin abrasions. Lesions occur on the muzzle, nostrils, lips, and mouth, although they can become more widespread (see Vol. 2, Alimentary system and peritoneum), and cows with suckling calves can develop teat and udder lesions. The appearance of initial lesions is similar to pseudocowpox; however, lesions may become papillomatous or undergo central necrosis and become crusted. Resolution of lesions occurs in days to weeks. A chronic and fatal form has been described in calves and is characterized by exudative necrotic dermatitis, proliferative and necrotizing stomatitis, and marked hyperkeratosis around the mouth, anus, and ventral tail. A necrotic dermatitis of the tail of feedlot cattle (“rat-tail syndrome”) has been associated with bovine papular stomatitis. Affected cattle lose the tail switch, leaving an ulcerated area. Transmission to humans induces lesions identical to “milker's nodule” caused by Pseudocowpox virus infection. The histologic appearance of lesions is typical of other poxviral infections.
Further reading
Bowman KF, et al. Cutaneous form of bovine papular stomatitis in man. J Am Med Assoc 1981;246:2813-2818.
Gibbs EPJ. Viral diseases of the skin of the bovine teat and udder. Vet Clin North Am 1984;6:187-202.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Yeruham I, et al. Clinical and pathological description of a chronic form of bovine papular stomatitis. J Comp Pathol 1994;111:279-286.
Parapox of red deer.
A new addition to the genus Parapoxvirus is species Parapox virus of red deer, first noted in 1986 in farmed red deer in New Zealand. Morbidity is high, but mortality is low unless secondary infections are present. The virus causes crusty lesions on the lips, muzzle, face, ears, and neck, and on the antler velvet in stags. Removal of the crusts leaves a red raw ulcer. A more severe form of the disease was recently reported in red deer in Italy. These animals had proliferative lesions, erosion and ulcers on the lips and hard palate, and died as a result of starvation. Histologic lesions are characterized by epithelial hyperplasia with marked intracellular edema, dyskeratosis, and eosinophilic cytoplasmic viral inclusions. Like some of the other members of genus Parapoxvirus, viral VEGF is thought to contribute to the proliferative and highly vascular nature of the lesions.
Further reading
Horner GW, et al. Parapox infections in New Zealand farmed red deer (Cervus elaphus). N Z Vet J 1987;35:41-45.
Robinson AJ, Mercer AA. Parapoxvirus of red deer: evidence for its inclusion as a new member in the genus parapoxvirus. Virology 1995;208:812-815.
Scagliarini A, et al. Parapoxvirus infections of red deer, Italy. Emerg Infect Dis 2011;17:684-687.
Ueda N, et al. Parapoxvirus of red deer in New Zealand encodes a variant of viral vascular endothelial growth factor. Vir Res 2007;124:50-58.
Orthopoxviral diseases
Cowpox.
Species Cowpox virus is a zoonotic virus belonging to the genus Orthopoxvirus. Cowpox affects a range of species, including wild and domestic felids, cattle, dogs, rodents, humans, nonhuman primates, horses, and several zoo and circus animals, including elephants and rhinoceros. Cowpox is enzootic in Europe and in some western states of the former Soviet Union, and in adjacent areas of Northern and Central Asia. The natural reservoirs are wild rodents, with the highest seroprevalence in bank voles (Clethrionomys glareolus). In cattle, poxvirus lesions most commonly develop on the teats and udder. A thick red crust, 1-2 cm in diameter is characteristic. In severe cases, lesions occur on the medial thighs, perineum, vulva, scrotum, and mouth of nursing calves. Human cowpox infection is rare, and most have been associated with infected cats.
Domestic cats develop cutaneous and, occasionally, respiratory lesions. Transmission is probably through rodent bites or feeding on rodents carrying the virus. Most cats have a single primary cutaneous lesion, usually on the head, neck, forelimbs, or paws (Fig. 6-81A ). A secondary bacterial infection may develop, resulting in an abscess or cellulitis. A viremic period occurs 1-3 weeks following the initial infection, and affected cats may be febrile, inappetent, and depressed. Secondary skin lesions develop during this viremic phase and consist of multiple papules that enlarge to small nodules over 3-5 days and ulcerate, forming craters and crusts. Lesions are rarely vesicular except on the oral mucosa and inner aspect of the pinna. The ulcers heal with thick gray crusts over 2-3 weeks. Mucocutaneous junctions, oral mucosa, and the tongue may also be involved. Most cats recover within 4-5 weeks, and permanent scarring can occur. However, some cats develop more severe and sometimes fatal disease. Rarely, domestic cats can develop a fatal necrotizing pneumonia without typical skin lesions. Exotic felids, especially cheetahs, are at high risk of developing a rapidly fatal necrotizing pneumonia during the viremic period. More severe disease is rare in domestic cats and is often associated with severe secondary bacterial infection or immune suppression caused by concurrent infection with feline leukemia virus, feline immunodeficiency virus, feline panleukopenia virus, feline herpesvirus, or from glucocorticoid therapy.
Figure 6-81.

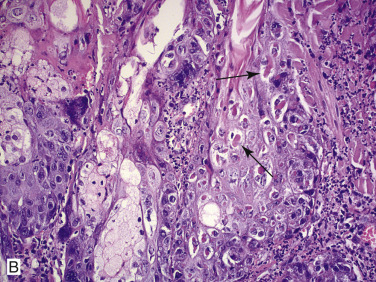
Cowpox in a cat. A. Ulcerative lesion on the paw. B. Necrotizing dermatitis with eosinophilic intracytoplasmic inclusions (arrows) within hair follicle epithelium and sebocytes at the edge of an ulcer.
(Courtesy W. von Bomhard.)
A few cats exhibit clinical signs of upper respiratory tract disease. Lower respiratory tract lesions, which are rare in domestic cats, include pleural effusion and localized areas of cream-colored consolidation in the ventral lung lobes. They are thought to develop from systemic spread rather than from primary respiratory infection.
The microscopic lesions in naturally infected cats are focal, sharply demarcated ulcers covered by fibrinonecrotic exudate. The ulcers may extend to the deep dermis, subcutis, or even muscle. An intense dermal inflammatory cell infiltrate of neutrophils and mononuclear cells may be associated with the base of the ulcers. Eosinophilic, homogeneous, intracytoplasmic inclusion bodies, 3-7 µm in diameter, occur in keratinocytes in the hyperplastic epithelium at the margin of the ulcers and in the epithelium of the external root sheath and sebaceous gland (Fig. 6-81B). Epidermal lesions typical of poxvirus infections develop in cats experimentally infected intravenously or by skin scarification. These lesions include focal hyperplasia, with reticular degeneration and multilocular vesiculation. Epidermal cells bordering the vesicles contain eosinophilic intracytoplasmic inclusion bodies. Viral inclusions also occur in macrophages, fibroblasts, and endothelial cells. The extensive necrosis is probably ischemic in origin following viral damage to endothelial cells. The pulmonary lesion is necrotizing alveolitis in which eosinophilic inclusion bodies are present in the degenerating cells.
Electron microscopic examination of scabs reveals typical orthopox virions. Cowpox virus infection may be confirmed by immunohistochemical staining of lesions, PCR, or virus isolation. Serologic tests may be helpful in establishing retrospective diagnoses, as virus neutralizing antibodies persist for several years.
There have been outbreaks of severe orthopoxviral infections in several species of nondomestic felids in English and Russian zoos. Lions, cheetahs, pumas, jaguars, and ocelots have been affected. Rats were implicated as the source of infection in the Russian outbreaks. Two forms of the disease are recognized. The cutaneous form is rarely fatal. The lesions are ulcerative and crusted as described for domestic cats. The respiratory form is uniformly fatal and consists of severe fibrinous and necrotizing bronchopneumonia and pleuritis. A virus closely resembling Cowpox virus is responsible.
Cowpox has been described in 3 dogs, 2 of which were <1 year of age, and all had a solitary raised ulcerated nodule, clinically mimicking a canine cutaneous histiocytoma. None of the dogs showed signs of dissemination or systemic spread.
Raccoonpox virus, also belonging to the genus Orthopoxvirus, was reported to cause a localized ulcerative and exudative lesion on the forepaw of a 2-year-old cat in Canada.
Further reading
Baxby D, Bennett M. Cowpox: a re-evaluation of the risks of human cowpox based on new epidemiological information. Arch Virol Suppl 1997;13:1-12.
Baxby D, et al. An outbreak of cowpox in captive cheetahs: virological and epidemiological studies. J Hyg (Camb) 1982;89:365-372.
Chantrey J, et al. Cowpox: reservoir hosts and geographical range. Epidemiol Infect 1999;122:455-460.
Godfrey DR, et al. Unusual presentations of cowpox infection in cats. J Small Anim Pract 2004;45:202-205.
Herder V, et al. Poxvirus infection in a cat with presumptive human transmission. Vet Dermatol 2011;22:220-224.
Miller WH, et al. Viral rickettsial and protozoal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 343-362.
Von Bomhard W, et al. Localized cowpox infection in a 5 month old Rottweiler. Vet Dermatol 2012;22:111-114.
Vaccinia.
Species Vaccinia virus (VACV), and vaccinia-like viruses in genus Orthopoxvirus, infects horses, cattle, swine, and humans. This virus was used for the immunization of humans during the smallpox eradication campaign. The origin of the virus is controversial. One theory is that it represents the laboratory survival of horsepoxvirus, which is now considered extinct in nature, and that horse-derived material was the source of vaccine material used by Edward Jenner in 1817 to protect against variola or smallpox. It may have arisen from buffalopox virus, which is antigenically almost identical to VACV. Another theory is that VACV was derived from cowpox virus by repeated passage on the skin of cows, sheep, and other animals, and that “horsepox” was caused by the infection of horses with cowpox virus. Incidental infections in cattle, horses, and pigs were transferred from vaccinated people. The lesions in cattle are indistinguishable from those of cowpox, and in swine are indistinguishable from those of swinepox. When vaccinia is inoculated onto scarified skin of horses, papular lesions resembling a naturally occurring poxvirus infection described in horses in the United States results. Furthermore, inoculation of the skin of the flexor surface of the pastern produces lesions resembling the classic “grease heel” form of horsepox. Although most clinical descriptions of VACV are associated with vaccination, over the past decade, a number of outbreaks of VACV affecting dairy cattle and humans in Brazil have been reported. Coinfection by VACV and orf virus–like parapoxvirus has also been reported in dairy cattle in Brazil. An outbreak of orthopoxvirus involving 14 horses in Brazil had gross findings similar to those of the buccal form of horsepox, but molecular analysis showed a high nucleotide sequence homology (95-100%) with Brazilian VACV isolates.
Further reading
Baxby D. Edward Jenner's inquiry: a bicentenary analysis. Vaccine 1999;17:301-307.
Brum MCV, et al. An outbreak of orthopoxvirus-associated disease in horses in southern Brazil. J Vet Diagn Invest 2010;22:143-147.
Chapman JL, et al. Animal models of Orthopoxvirus infection. Vet Pathol 2010;47:852-870.
de Sant'Ana FJF, et al. Coinfection by Vaccinia virus and an Orf virus-like parapoxvirus in an outbreak of vesicular disease in dairy cows in midwestern Brazil. J Vet Diag Invest 2013;25:267-272.
Lewis-Jones S. Zoonotic poxvirus infection in humans. Curr Opin Infect Dis 2004;17:81-89.
Patel DD, et al. Isolation of cowpoxvirus A-type inclusions and characterization of their major protein component. Virology 1986;149:174-189.
Taylor CED. Did vaccinia virus come from a horse. Equine Vet J 1993;25:8-10.
Buffalopox.
Buffalopox virus, an Orthopoxvirus closely related to Vaccinia virus, is the cause of buffalopox, an economically important disease of domestic buffaloes. It is thought that buffalopox virus is a subspecies of Vaccinia virus resident in the water buffalo population. First reported in India in 1967, it has subsequently been reported in Pakistan, Indonesia, Egypt, Italy, and Russia. In India, it is considered to be an emerging enzootic virus and can occur in epidemic form, with significant economic impact. Zebu cattle are apparently refractory to infection. Pox lesions predominantly affect the teats and udder and can lead to mastitis. Lesions can also occur on the medial aspects of the thighs, lips, and muzzle and may be generalized, especially in calves. Buffalopox virus is zoonotic, causing lesions primarily on the hands. Human-to-human transmission has been postulated following the occurrence of disease in children who had had no contact with infected animals. Experimentally, the virus can be transmitted to cattle, rabbits, guinea pigs, and mice.
Further reading
Anand Kumar P, Butchaiah G. Partial antigenic characterization of buffalopox virus. Vet Res Commun 2004;28:543-552.
Essbauer S, et al. Zoonotic poxviruses. Vet Microbiol 2010;140:229-236.
Kolhapure RM, et al. Investigation of buffalopox outbreaks in Maharashtra state during 1992-1996. Indian J Med Res 1997;106:441-446.
Singh M, et al. Biological transmissibility of buffalopoxvirus. J Appl An Res 1996;9:79-88.
Camelpox.
Camelpox virus, a distinct species of genus Orthopoxvirus, causes severe disease in Old World camelids (Camelus dromedarius and Camelus bactrianus). First reported in Russia and later India, the disease is known to occur throughout the camel breeding areas of Northern Africa, the Middle East, and Asia, but has not been reported in wild camels in Australia. It is characterized by high morbidity and a relatively high mortality rate in young animals. A major effect is a fall in milk production and loss of condition. The disease is characterized by fever, lymphadenopathy, and skin lesions. Lesions affect both skin and mucous membranes and follow the usual pattern of pox lesions. Lesions tend to be most concentrated around the face, including eyelids, nostrils, and margins of the pinnae. In severe cases, the whole head may be swollen. Intense pruritus may be seen in acute cases. Later, skin lesions may extend to the neck, limbs, genitalia, mammary glands, and perineum. Generalized skin lesions occur more typically in calves. Skin lesions may take 4-6 weeks to heal. Rarely, the infection can become systemic and involve the mucous membranes of the mouth, respiratory, and digestive tract. Fatalities are usually associated with secondary bacterial infection leading to septicemia, a phenomenon more prevalent in the rainy season. The lesions can be identical to parapox (camel contagious ecthyma), and laboratory tests such as ELISA, PCR, and immunohistochemistry, as well as electron microscopy, can be used to differentiate the infections. Histologic lesions are similar to those caused by other orthopoxviruses.
Further reading
Afonso CL, et al. The genome of camelpox virus. Virology 2002;295:1-9.
Bhanuprakash V, et al. Camelpox: epidemiology, diagnosis and control measures. Expert Rev Anti Infect Ther 2010;8:1187-1201.
Kinne J, et al. Pathological studies on camelpox lesions of the respiratory system in the United Arab Emirates (UAE). J Comp Pathol 1998;118:257-266.
Pfeffer M, et al. Diagnostic procedures for poxvirus infections in camelids. J Camel Pract Res 1998;5:189-195.
Pfeffer M, et al. Fatal form of camelpox virus infection. Vet J 1998;155:107-109.
“Horsepox” and Uasin Gishu disease.
Species Horsepox virus (HSPV), genus Orthopoxvirus, is the cause of horsepox. Horsepox was a common disease of horses in Europe before the 20th century. It is rare today, and some consider it extinct. It is thought that Jenner, in his “cowpox” vaccination experiments to protect humans from smallpox, was actually using horse-derived material as a source of the vaccine, and that Vaccinia virus may be the long-lost agent of horsepox. Experimental infection of horses with Vaccinia virus reproduces the “grease heel” lesions of Jenner's horsepox and the more generalized form known as equine papular dermatitis. Although there is a close genetic relationship between HSPV and known VACV-like viruses, HSPV is considered a unique virus.
Poxviral lesions in the horse take several clinical forms. Jenner originally described an exudative dermatitis of the flexor aspects of the hind pasterns. The condition is colloquially named “grease heel” because thick, yellow, grease-like exudate mats the hair. Unfortunately, poxvirus infection is only one manifestation of this clinical entity, sparking considerable controversy as to the true nature of equine pox.
A second form has a predilection for the muzzle and buccal cavity (contagious pustular stomatitis). The lesions, which develop in the typical sequence of a pock, affect the inner surface of the lips and cheeks, the gums, and the ventral surface of the tongue. Following the development of the buccal eruptions, crops of pocks may appear in the rostral nares, on the face, and on other parts of the body. It is a benign infection, sometimes seriously complicated by bacterial contamination.
Equine papular dermatitis or viral papular dermatitis, may be a variant of horsepox. It has been described as a highly contagious disease of horses in the United States, Australia, and New Zealand. The disease is characterized by a papular reaction and is reported to spread by direct contact and through infected harness, bedding, and grooming tools. The lesions are firm papules, up to 0.5 cm diameter, which tend to develop on the lateral neck and shoulder and thorax but become generalized. The papules become crusted, and the crusts slough to leave circular alopecic patches. Resolution may take 6 weeks.
There is one case report of a donkey from Kansas (United States) with horsepox-like lesions over the face, nares, lips, cheeks, and gingiva. Histologic lesions resembled those of other orthopoxviruses and pox virions were noted with electron microscopy, but the virus was not further characterized. The donkey was euthanized because of a femoral fracture.
Uasin Gishu disease in Kenya, caused by an Orthopoxvirus, is also characterized by generalized skin lesions, but the disease differs clinically from equine papular dermatitis. Lesions begin similarly as small papules but develop into crusted papillomatous proliferations, up to 2 cm diameter. Lesions eventually resolve, but the disease may continue for 2 years. The histologic lesions of Uasin Gishu disease are identical to molluscum contagiosum.
Further reading
Baxby D. Edward Jenner's inquiry; a bicentenary analysis. Vaccine 1999;17:301-307.
Eby CH. A note on the history of horsepox. J Am Vet Med Assoc 1958;132:420-422.
Jayo MJ, et al. Poxvirus infection in a donkey. Vet Pathol 1986;23:635-637.
Kaminjolo JS, Winqvist G. Histopathology of skin lesions in Uasin Gishu skin disease of horses. J Comp Pathol 1975;85:391-395.
Tulmas ER, et al. Genome of horsepox virus. J Virol 2006;80:9244-9258.
Molluscipoxviral disease
Equine molluscum contagiosum.
Species Molluscum contagiosum virus (MCV), genus Molluscipoxvirus, is most commonly reported in humans, with a few reports in the veterinary literature that include predominantly horses, with rare reports of macropods (kangaroos and quokkas), chimpanzees, donkeys, and anecdotal reports in dogs.
In situ hybridization experiments indicate there is very close homology between the equine and human MCV. It has been suggested that the disease may actually be transmitted from humans to horses. Attempts to grow both the human and equine MCV in culture have failed, and this can help differentiate the virus from the orthopoxvirus of Uasin Gishu, which produces histologically and clinically similar lesions, but which can be grown in culture. Molluscipoxvirus can also be identified with PCR.
Molluscum contagiosum virus can be found worldwide, with a higher distribution in tropical areas. In horses, it is a benign cutaneous infection characterized clinically by multiple, slightly raised, smooth to slightly roughened, white and shiny, 2-8 mm papules that may occur anywhere on the body but seem to occur more frequently on the neck, chest, shoulders, limbs, and inguinal region. Lesions may remain localized to one body region, such as the muzzle, prepuce, or scrotum, or they may become widespread with hundreds of lesions. As the lesions enlarge, papules become umbilicated and may bleed or have a central white to brown crust or horn projecting from the surface. Lesions may remain for months to years without regression.
The microscopic lesions of molluscum contagiosum are highly characteristic. Well-demarcated foci of epidermal hyperplasia and hypertrophy form pear-shaped lobules. The individual keratinocytes are markedly swollen and contain large intracytoplasmic inclusions known as “molluscum bodies” (Fig. 6-82 ). These occur initially as eosinophilic, floccular aggregates in the cells of the inner stratum spinosum. As the keratinocytes move toward the surface, the inclusions grow in size and density, compressing the nucleus against the cytoplasmic membrane until it is a thin crescent. The inclusion becomes increasingly basophilic so that cells of the stratum corneum contain deep-purple molluscum bodies. These exfoliate through a pore that forms in the stratum corneum and enlarges into a central crater. There is usually no dermal reaction. Molluscum bodies are easily identified in cytologic preparations.
Figure 6-82.
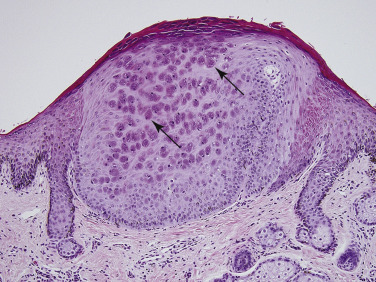
Molluscum contagiosum in a horse. Focal epidermal hyperplasia. Note large intracytoplasmic inclusion bodies referred to as “molluscum bodies” (arrows).
Further reading
Fox R, et al. Molluscum contagiosum in two donkeys. Vet Rec 2012;170:649-651.
Lange L, et al. Molluscum contagiosum in three horses. J S Afr Vet Assoc 1991;62:68-71.
Scott DW, Miller WH. Viral and protozoal skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 251-262.
Thompson CH, Yager JA. Close relationship between equine and human molluscum contagiosum virus demonstrated by in situ hybridization. Res Vet Sci 1998;64:157-161.
Capripoxviral diseases
Sheeppox, goatpox, and lumpy skin disease of cattle are caused by viruses of the genus Capripoxvirus and cause significant economic losses in countries where they are endemic. The exact relationship between these viruses has been controversial. It is believed that they represent strains of a single virus. The evidence includes antigenic and biochemical similarity, a high degree of nucleotide sequence homology, lack of absolute host specificity in most strains, evidence of recombination in the field, and demonstration of cross-infection and cross-protection. The viruses are indistinguishable by conventional serology; nevertheless, the geographic distributions of the three are different, indicating the viruses are distinct. Most strains of Capripoxvirus show definite host preferences; however, some isolates can infect both species, and the disease caused by the same isolate can vary dramatically between sheep and goats. There is one report from China of an outbreak of sheeppox associated with goatpox virus in which 6 of 26 affected sheep died. PCR methods of identification of capripoxvirus have been developed so that classic virology methods based on live virus need not be used in areas of the world where the virus is exotic.
Further reading
Embury-Hyatt C, et al. Pathology and viral antigen distribution following experimental infection of sheep and goats with capripoxvirus. J Comp Pathol 2012;146:106-115.
Gerson PD, Black DN. A comparison of the genomes of capripoxvirus isolates from sheep, goats and cattle. Virology 1988;164:341-349.
Heine HG, et al. A capripoxvirus detection PCR and antibody ELISA based on the major antigen p32, the homologue of the vaccinia virus H3L gene. J Immunol Methods 1999;227:187-196.
Yan X, et al. An outbreak of sheep pox associated with goat poxvirus in Gansu province of China. Vet Microbiol 2012;156:425-428.
Sheeppox.
Sheeppox is the most serious of the pox diseases of domestic animals. It exists in Africa, Asia, and the Middle East where, despite attempts at vaccination, it is responsible for cycles of epidemic disease, followed by periods of endemic maintenance with low morbidity. The disease is exotic to the Americas, Australia, and New Zealand. Eradication measures eliminated the disease from Britain in the mid-19th century but have only recently been successful in Eastern European countries. Sheeppox causes extensive economic loss through high mortality; reduced meat, milk, or wool yields; commercial inhibitions from quarantine requirements; and the cost of disease prevention programs.
Transmission of infection is by direct contact with diseased sheep or indirect contact via contaminated environment. Insect transmission has been demonstrated experimentally. Species Sheeppox virus is resistant to desiccation and remains viable for up to 2 months on wool or 6 months in dried crust. There are breed differences in disease susceptibility. Fine-wooled Merino sheep are particularly sensitive, whereas breeds native to endemic areas, such as Algerian sheep, are comparatively resistant. Sheeppox occurs in all ages of sheep with high morbidity, and mortality as high as 50%, but the disease is most severe in lambs, with mortality reaching 80-100%. A high level of background immunity, such as occurs in endemic areas of Kenya, is associated with low mortality, even in the young.
Sheeppox is a systemic disease. Infection is usually by the respiratory route but may occur through skin abrasions. The incubation period is 4-7 days and is followed by a leukocyte-associated viremia. The virus localizes in many organs, including the skin, where the virus concentration is highest 10-14 days postinfection. The initial clinical signs are fever, lacrimation, drooling, serous nasal discharge, and hyperesthesia. Skin lesions, which develop 1-2 days later, have a predilection for the sparsely wooled areas and typically involve eyelids, cheeks, nostrils, vulva, udder, scrotum, prepuce, ventral surface of the tail, and medial thigh.
The macroscopic lesions follow the typical pattern for pox infections. Sheeppox lesions have a prominent vesicular stage (Fig. 6-83A
). The vesicles are umbilicated and, being multilocular, yield only a small amount of fluid if punctured. Occasionally a large vesicle forms as a result of cleavage of necrotic epidermis from underlying dermis. The pustule stage is characterized by the formation of a thin crust. In severely affected animals, the lesions coalesce. There may be marked, gelatinous dermal edema. Highly susceptible animals often develop hemorrhagic papules early in the course of the disease and, later, ulcerative lesions in the gastrointestinal and respiratory tracts. Approximately  of animals develop multiple foci of pulmonary consolidation. There may be multiple fleshy nodules throughout the renal cortices.
of animals develop multiple foci of pulmonary consolidation. There may be multiple fleshy nodules throughout the renal cortices.
Figure 6-83.

Sheeppox in a sheep. A. Vesicle (arrow) on teat.
(Courtesy A. Alcaraz.)

B. Erythematous papules, nodules, and plaques around the mouth, nose, and eyes.
(Courtesy J.M. Gourreau.)
Healing of the skin lesions is slow, taking up to 6 weeks, and a scar may remain. In the milder form of the disease, seen in endemic areas, the full range of pox lesions does not develop. Instead, epidermal proliferation produces papules covered by scale-crust, which heal with desquamation in a few days (Fig. 6-83B). Such lesions often occur on the ventral surface of the tail.
Sheeppox lesions have the epithelial changes typical for the group, including marked vacuolar degeneration of stratum spinosum keratinocytes, microvesiculation, eosinophilic intracytoplasmic inclusion bodies, and epidermal hyperplasia. The lesions affect both surface epithelium and that of the hair follicles. There are, in addition, marked dermal lesions reflecting the systemic route of cutaneous involvement and possibly implicating immune-mediated lesions in addition to those caused by direct viral damage. The initial dermal lesions, corresponding to the macroscopic erythematous macule, are marked edema, hyperemia, and neutrophilic exocytosis. During the papular stage, large numbers of mononuclear cells accumulate in the increasingly edematous dermis. These cells are called “cellules claveleuses” or “sheeppox cells” and are characteristic of the disease. The nuclei of sheeppox cells are vacuolated and have marginated chromatin. The vacuolated cytoplasm contains single, occasionally multiple, eosinophilic intracytoplasmic inclusion bodies. Sheeppox cells are virus-infected monocytes, macrophages, and fibroblasts, but not endothelial cells. Sheep experimentally infected with capripoxvirus may develop large spindle-shaped syncytial cells with intracytoplasmic inclusions within the dermis. Approximately 10 days postinfection and corresponding with the most prominent epithelial lesions and peak of skin infectivity, severe necrotizing vasculitis develops in arterioles and postcapillary venules. Virus particles have not been identified in endothelial cells, and the vasculitis may be due to immune-complex deposition. Ischemic necrosis of the dermis and overlying epidermis follows.
The pulmonary lesions are proliferative alveolitis and bronchiolitis with focal areas of caseous necrosis. Alveolar septal cells contain intracytoplasmic inclusion bodies. Additional histologic lesions, characterized by the accumulation of sheeppox cells, may involve heart, kidney, liver, adrenals, thyroid, and pancreas.
The course and outcome of sheeppox depend not only on the usual host-virus relationship but also on the nature and location of secondary infections. The virus itself may cause death during the febrile, eruptive phase of the disease. Of great importance, however, are the secondary bacterial infections that rapidly develop in the necrotic tissue of the pocks. Death is often due to bacterial septicemia or pneumonia.
Goatpox.
Goatpox, caused by species Goatpox virus, occurs in North Africa and the Middle East. A benign form of goatpox occurs in California and Sweden. The clinical signs of goatpox vary in different geographic areas. The disease has many parallels with sheeppox, but is generally milder with a low mortality rate (5%), although generalized eruption with mortality rates approaching 100% may occur. The cutaneous lesions have a predilection for the same areas as for sheeppox. In nursing kids, lesions may appear on the buccal mucosa or rostral nares. In animals with higher levels of resistance, the lesions may be confined to the udder, teats, inner aspects of thighs, or ventral surface of the tail. Occasionally, only nodular lesions are seen (“stone pox”), resembling lumpy skin disease of cattle.
Further reading
Embury-Hyatt C, et al. Pathology and viral antigen distribution following experimental infection of sheep and goats with capripoxvirus. J Comp Pathol 2012;146:106-115.
Garner MG, et al. The extent and impact of sheep pox and goat pox in the state of Maharashtra, India. Trop Anim Health Prod 2000;32:205-223.
Rao TV, Bandyopadhyay SK. A comprehensive review of goat pox and sheep pox and their diagnosis. Anim Health Res Rev 2000;1:127-136.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Lumpy skin disease.
Lumpy skin disease, caused by species Lumpy skin disease virus of the genus Capripoxvirus, is a disease of cattle, buffalo, and occasionally other wild species of hoofstock, characterized by the eruption of multiple, well-circumscribed skin nodules, accompanied by fever, ventral edema, and generalized lymphadenopathy. Lumpy-skin disease is found throughout the African continent and Madagascar, with sporadic reports from the Middle East and Israel.
Cattle of all ages, sex and breeds are affected, although the disease is more severe in Channel Island breeds. Both Bos indicus and Bos taurus cattle are susceptible; however, the disease can be less severe in Zebu breeds. The disease occurs in epidemics; a notable one in 1944 affected 8 million cattle. Transmission is believed to occur mainly by blood-feeding arthropods. Epidemics tend to follow periods of prolonged rainfall, which favor population increases in vector species. A forest maintenance cycle, probably involving Cape buffalo, is thought to be the reservoir of infection in the interepidemic periods. No reservoir host apart from cattle has been identified.
The morbidity is extremely variable, and inapparent infection is common. Mortality is usually low; around 1% but may be >50%. Economic losses are due to debilitation, loss of milk and meat production, damage to hides, and reproductive wastage resulting from fever-associated abortions and temporary sterility in bulls.
The natural incubation period of lumpy skin disease is 2-4 weeks, but this may be halved in experimental infection. In severely affected animals, the development of large numbers of cutaneous lesions over most of the body is preceded by fever, marked weight loss, profuse drooling, oculonasal discharge, ventral edema, and generalized lymphadenopathy. In the mild disease, there may be few isolated nodules and no prodromal fever. The cutaneous lesions are firm, circumscribed, flat-topped papules and nodules, 0.5-5.0 cm in diameter. They may coalesce. The nodules have a creamy gray color on cut section and involve the full width of the cutis, extending into the subcutis and occasionally adjacent muscles. Nodules affecting the scrotum, perineum, udder, vulva, glans penis, eyelids, and conjunctiva are usually flatter, and in nonpigmented tissue are surrounded by a zone of intense hyperemia. The fate of the nodules varies. Typically, they undergo central necrosis and sequestration, but some may resolve rapidly and completely, and others may fail to separate but, instead, become indurated and persist as hard intradermal lumps for many months. Sequestration is preceded by central necrosis in the nodule and occurs rapidly. Separation of the epidermis around the margin of the nodule exposes a rim of dermal granulation tissue. As the process of separation extends into the dermis, the nodule comes to contain a core or sequestrum of necrotic material (“sit-fast”), which is cone shaped and flat topped (Fig. 6-84 ). When the sequestrum is removed, a deep ulcer remains that is slowly filled with granulation tissue. Secondary bacterial infections develop in the necrotic cores of the nodules and contribute very significantly to the seriousness of the disease. Large craterous ulcers develop, which lead to lymphangitis and lymphadenitis. Local extension of lesions causes blindness, tenosynovitis, arthritis, or mastitis.
Figure 6-84.
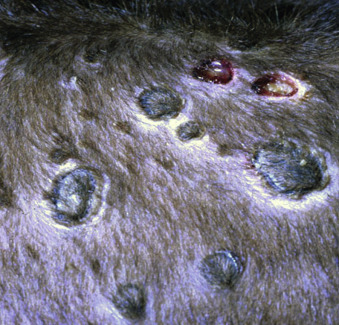
Lumpy skin disease in a calf. Circumscribed necrotic tissue (“sit-fasts”) and deep ulcers.
(Courtesy I. Yeruham.)
The mucous membranes of the upper respiratory and upper alimentary tracts often develop multiple, discrete ulcerative lesions, irrespective of the number of cutaneous nodules. Those in the respiratory tract may cause swelling sufficient to result in severe dyspnea and asphyxia. Aspiration may lead to pneumonia or, if the animal recovers, scarring may cause stenosis of the cranial portion of the trachea. Nodules occasionally occur in parenchymal organs, including kidneys, lungs, and testes.
Although the virus is introduced percutaneously, the infection is systemic. A leukocyte-associated viremia disseminates the virus to various tissues, including the skin, where greatest virus concentration occurs 9-12 days postinfection. The virus infects a wide range of cells, including keratinocytes, mucous and serous glandular epithelium, fibrocytes, skeletal muscle, macrophages, pericytes, and endothelial cells. Damage to endothelial cells causes vasculitis that is central to the pathogenesis of the lumpy skin disease lesions.
Acute lesions consist of vasculitis, lymphangitis, thrombosis, marked dermal edema that sometimes induces dermoepidermal separation, and infarction. The epidermis shows the typical vacuolar changes associated with poxvirus infection. Intracytoplasmic, eosinophilic, homogeneous, and occasionally granular inclusion bodies occur in endothelial cells, pericytes, keratinocytes, macrophages, and fibroblasts. Virions in various stages of development are present in these inclusion-containing cells and in peripheral nerves. Neutrophils, macrophages and occasionally eosinophils migrate into the dermis in the acute lesions, to be replaced as the lesion ages by a predominantly mononuclear cell population. The infarcted tissue is sequestered and surrounded by granulation tissue. Inclusion bodies are absent from the resolving lesions but may be present in adjacent skin or sebaceous glands. Lymph nodes are edematous and hyperplastic.
The chief differential diagnosis is pseudo–lumpy skin disease caused by a herpesvirus identical to the bovine herpes mammillitis virus but originally known as the Allerton virus. Pseudo–lumpy skin disease is a milder condition clinically, and the nodules are superficial, resembling only the early stage of lumpy skin disease. Confirmation of the latter is best achieved by demonstration of poxvirus particles in fresh or formalin-fixed tissue.
Further reading
Hunter P, Wallace D. Lumpy skin disease in southern Africa: a review of the disease and aspects of control. J S Afr Vet Assoc 2001;72:68-71.
Tulman ER, et al. Genome of lumpy skin disease virus. J Virol 2001;75:7122-7130.
Tuppurainen ESM, Oura CAL. Review: lumpy skin disease: an emerging threat to Europe, the Middle East and Asia. Transbound Emerg Dis 2012;59:40-48.
Suipoxviral disease
Swinepox.
The host-specific Swinepox virus (SWPV), the sole species in genus Suipoxvirus, is the chief cause of pox lesions in swine. In the past, Vaccinia virus was also responsible. The disease occurs worldwide and is endemic in areas of intensive swine production. The disease has received relatively little attention as it is usually mild and mortality is negligible. It chiefly affects young, growing piglets but occurs in neonates, promoting speculation that transplacental infection may be possible. Normally, SWPV is transmitted by contact. The virus is resistant and persists in dried crust from infected animals. The sucking louse Haematopinus suis often acts as a mechanical vector and also assists infection by causing skin trauma. The gross lesions typically affect the ventral and lateral abdomen, lateral thorax, and medial foreleg and thigh. Occasionally, lesions on the dorsum predominate (Fig. 6-85 ). In severe infection, lesions may be generalized and rarely involve the oral cavity, pharynx, esophagus, stomach, trachea, and bronchi. The morphology of the gross lesions follows the typical pattern of pox infection. The erythematous papules usually transform into umbilicated pustules without a significant vesicular stage. The inflammatory crust eventually sheds to leave a white macule.
Figure 6-85.

Swinepox in a piglet. Multifocal to coalescing erythematous macules and plaques, some with central necrosis.
(Courtesy B. Sansot.)
The histologic lesions also follow the pattern for pox infections. The eosinophilic, intracytoplasmic inclusion bodies are quite transient and are not found in older lesions. Vacuoles develop in the nuclei of infected stratum spinosum keratinocytes early in the course of swinepox infection.
Further reading
Afonso CL, et al. The genome of swinepox virus. J Virol 2002;76:783-790.
Massung RF, Moyer RW. The molecular biology of swinepox. II. The infectious cycle. Virology 1991;180:355-364.
Medaglia ML, et al. Swinepox virus outbreak, Brazil, 2011. Emerg Infect Dis 2011;17:1976-1978.
Thibault S, et al. Congenital swinepox: a sporadic skin disorder in nursing piglets. Swine Health Prod 1998;6:276-278.
Herpesviral infections
The Herpesviridae is a large family of enveloped DNA viruses responsible for important animal diseases, of which relatively few are primary skin diseases. Bovine herpesvirus 2 (BoHV-2) causes primary cutaneous infections and is widespread in many parts of the world. It is responsible for 2 distinct clinical forms of skin disease: bovine mammillitis of cattle, which is the major cutaneous infection, and pseudo—lumpy skin disease. Skin lesions occur in systemic herpesvirus infections such as malignant catarrhal fever, and infectious bovine rhinotracheitis in cattle, and pseudorabies in pigs.
A unique form of alopecia and mural folliculitis has been described in sika deer with Caprine herpesvirus 2 infection and in one goat with Ovine herpesvirus 2 infection. Skin lesions consisted of nonpruritic scaling and crusting of the pinna, nares, and peribuccal skin in addition to papules, erythema, and scaling of the distal limbs. Microscopically, there was irregular epidermal hyperplasia with compact orthokeratotic and parakeratotic hyperkeratosis layered with inflammatory cells. The main feature was mural folliculitis with large numbers of macrophages, fewer lymphocytes, plasma cells, eosinophils, and occasional multinucleated giant cells.
Skin lesions associated with Felid herpesvirus 1 infection are also recognized, usually in the absence of respiratory lesions. Vesicles, pustules, ulcers, and depigmentation are seen on the genital organs and occasionally the lips and nostrils of horses with Equid herpesvirus 3 infection (equine coital exanthema), and in Bovine herpesvirus 1 infection (infectious vulvovaginitis and balanoposthitis).
Further reading
Crawford TB, et al. Mural folliculitis and alopecia caused by infection with goat-associated malignant catarrhal fever virus in two sika deer. J Am Vet Med Assoc 2002;221:843-847.
Ezura K. Gastrointestinal and skin lesions in piglets naturally infected with pseudorabies virus. J Vet Diagn Invest 1995;7:451-455.
Fenner F, et al. Veterinary Virology. 2nd ed. San Diego: Academic Press; 1993.
Foster AP, et al. Diagnostic exercise: generalized alopecia and mural folliculitis in a goat. Vet Pathol 2010;47:760-763.
Bovine herpesvirus 2 diseases
Pseudo—lumpy skin disease.
Species Bovine herpesvirus 2 (BoHV-2) is a member of the Alphaherpesvirinae subfamily and is antigenically related to human herpes simplex virus 1. First isolated in Africa in 1957 from lesions resembling lumpy skin disease, it was named the Allerton virus. The associated disease was subsequently named “pseudo—lumpy skin disease” to differentiate it from the more serious disease caused by Lumpy skin disease virus. Pseudo—lumpy skin disease is widespread in southern Africa, with sporadic reports from Australia, the United Kingdom, the United States, and Israel. It is characterized by a generalized eruption of superficial cutaneous nodules that develop a central depression but that heal without scar formation and do not produce the deep necrotic sequestra of true lumpy skin disease. The natural mode of transmission is not clear but is thought to be spread by inoculation into the dermis by biting flies.
Bovine herpes mammillitis.
Bovine herpes mammillitis, or ulcerative mammillitis, is a localized form of BoHV-2 infection seen sporadically in the United States, Canada, Great Britain, Europe, Africa, and Australia. Serologic surveys indicate that infection is much more common than disease. In Africa, Asia, and Hungary, several species of wild animals have antibody titers or PCR detection of the virus, although clinical disease is not seen.
Herpes mammillitis is chiefly a disease of lactating dairy cows but occurs in heifers about to calve and in beef animals. The incidence is usually sporadic with occasional local epidemics in fully susceptible herds. In previously exposed herds, the disease affects only the recently introduced nonimmune, first-calf heifers. There is no mortality. The economic significance of teat lesions lies in the effect on milk production or secondary bacterial mastitis, which complicate ~20% of cases.
Intact teat skin is refractory to virus penetration, indicating that some form of teat trauma precedes infection. Transmission of the virus is presumed to involve mechanical vectors, particularly the milking machine, but biting flies, such as Stomoxys calcitrans, have also been implicated. In the latter instance, it is difficult to explain the localization of lesions to the teat and mammary gland. Local tissue temperature has, however, been shown to be critical in the pathogenesis, and environmental conditions have been associated with the occurrence of outbreaks. Experimental cutaneous inoculation of BoHV-2 results in higher virus titers and larger and more persistent lesions when the site is kept cold. The increased prevalence of disease in the autumn months may also be related to the temperature sensitivity of the virus. The source of infection within a herd is not known, but latency, a characteristic of herpesviruses, is likely important. Latency has been demonstrated in experimental BoHV-2 infections.
The macroscopic lesions affect the teats, less frequently the udder, and occasionally the perineum of lactating cows. Transmission of infection to nursing calves may result in ulcerative lesions of the muzzle, chin, lips, and occasionally the oral cavity. Teat lesions develop after a 3- to 7-day incubation period. The teat becomes very swollen and painful and develops 1- to 2-cm diameter plaques. Vesicles are rare. The epidermis in the center of the plaque becomes necrotic and sloughs to expose an erythematous, irregularly shaped ulcer. Exuded serum mixed with blood forms a thin brown crust, which is easily displaced by the teat cups. The lesions heal beneath the crust, and there is no residual scar. Lesions on the udder are often diffuse, giving rise to the term “gangrene of the udder.” Regional lymph nodes are swollen in the early stages.
The microscopic lesions are characterized by the formation of epithelial syncytia containing prominent intranuclear eosinophilic inclusion bodies. The inclusion bodies are typical Cowdry type A. The nuclear chromatin is marginated, and the eosinophilic inclusions are surrounded by a clear halo. The inclusions are numerous from the time of the first macroscopic lesion until the fifth day. Thereafter, they are very difficult to find. Syncytial cell formation commences early in groups of cells in the stratum basale and inner stratum spinosum. The process extends to involve the full thickness of the epidermis, the outer root sheath of the hair follicle infundibulum, and the sebaceous gland. By day 5, after macroscopic lesions develop, the epidermis is necrotic, although the outlines of syncytial cells are apparent. The inclusion bodies lose their sharp outline and fill the entire nucleus. Some are free in the necrotic epidermis, released from fragmenting nuclei. The necrotic epidermis and adnexa are infiltrated with large numbers of neutrophils. Loss of the necrotic epithelium leaves an ulcer, which is covered by hemorrhagic and fibrinous exudate and a band of degenerating neutrophils. Deeper, there is dermal edema and a predominantly mononuclear cell infiltrate. In the healed lesion, the epithelium is re-established; there is superficial dermal fibrosis and a perivascular infiltrate of predominantly mononuclear cells.
The diagnosis of herpes mammillitis is confirmed by isolation of the virus. A rapid provisional diagnosis may be made by examining clinical material by electron microscopy. Biopsy is diagnostic if lesions are collected before the fifth day. Cytology smears prepared from an early lesion are diagnostic if syncytial cells containing eosinophilic intranuclear inclusion bodies are found. Serologic tests allow a retrospective diagnosis, provided paired samples are collected and a rising titer identified.
Experimental intravenous inoculation of sheep with BoHV-2 results in lesions resembling those of similarly inoculated cattle. Naturally occurring outbreaks of dermatitis of the pasterns caused by BoHV-2 have been described in captive Dahl sheep. Goats will only develop skin lesions following intravenous inoculation.
Further reading
Bhat MN, et al. Serological evidence of bovine herpesvirus 1 and 2 in Asian elephants. J Wildl Dis 1997;33:919-920.
Brenner J, et al. Herpesvirus type 2 in biopsy of a cow with possible pseudo-lumpy skin disease. Vet Rec 2009;165:539-540.
d'Offay JM, et al. Use of a polymerase chain reaction assay to detect bovine herpesvirus type 2 DNA in skin lesions from cattle suspected to have pseudo-lumpy skin disease. J Am Vet Med Assoc 2003;222:1404-1407.
Janett F, et al. Bovine herpes mammillitis: clinical symptoms and serologic course. Schweiz Arch Tierheilkd 2000;142:375-380.
Kalman D, Egyed L. PCR detection of bovine herpesvirus from nonbovine ruminants in Hungary. J Wild Dis 2005;41:482-488.
Letchworth GJ, Carmichael LE. Local tissue temperature: a critical factor in the pathogenesis of bovine herpesvirus 2. Infect Immun 1984;43:1072-1079.
O'Connor M. Meteorological features associated with outbreaks of bovine herpes mammillitis in Ireland. Irish Vet J 1995;48:71-80.
Torres FD, et al. Distribution of latent bovine herpesvirus 2 DNA in tissues of experimentally infected sheep. Res Vet Sci 2009;87:161-166.
Woods JA, et al. Isolation of bovine herpesvirus-2 (BHV-2) from a case of pseudo-lumpy skin disease in the United Kingdom. Vet Rec 1996;138:113-114.
Bovine herpesvirus 4 diseases
A strain of species Bovine herpesvirus 4 (BoHV-4) can cause udder lesions on dairy cows (mammary pustular dermatitis); the teats are not involved. The macroscopic lesions are vesicles, pustules, ulcers, and crusts, originally 2-4 mm in diameter, becoming larger with coalescence. The microscopic lesion is intraepidermal pustular dermatitis. The etiologic association between BoHV-4 and the cutaneous disease is controversial, however, because the virus is a ubiquitous herpesvirus of cattle that can produce no disease when experimentally inoculated into susceptible cattle and can be isolated from cell cultures prepared from clinically normal cattle. Although not a primary mastitis pathogen, BoHV-4 may prolong cases of bacterial mastitis. BoHV-4 infection is considered a risk factor for abortion in cows, and is reported as a cause of endometritis in postparturient dairy cows.
Further reading
Frazier K, et al. Endometritis in postparturient cattle associated with bovine herpesvirus-4 infection: 15 cases. J Vet Diagn Invest 2001;13:502-508.
Kalman D, et al. Role of bovine herpesvirus 4 in bacterial bovine mastitis. Microb Pathog 2004;37:125-129.
Osorio FA, Reed DE. Experimental inoculation of cattle with bovine herpesvirus-4: evidence for a lymphoid-associated persistent infection. Am J Vet Res 1983;44:975-980.
Thiry E, et al. The biology of bovine herpesvirus-4. Ann Med Vet 1992;136:617-624.
Equine herpesvirus
Equine herpes coital exanthema is caused by species Equid herpesvirus 3 (EHV-3) and is found in most parts of the world. Lesions include papules, vesicles, or pustules that may enlarge to plaques and bullae on the penis, prepuce, and scrotum of stallions, and on the vagina, vulva, and perineum of mares. Lesions may also occur on the muzzles of foals in contact with infected mares. Lesions heal over 2-5 weeks, and depigmentation may occur where lesions have healed. Microscopically, there is ballooning degeneration of keratinocytes with eosinophilic intranuclear inclusion bodies. Species Equid herpesvirus 2 (EHV-2) occurs worldwide and is isolated from normal horses and foals with respiratory disease. One horse was reported to have multiple plaques over the neck and chest. Microscopically, the lesions were composed of deep dermal infiltrates of neutrophils, lymphocytes, plasma cells, macrophages, and multinucleated giant cells, and thrombosed blood vessels with necrosis. Eosinophilic intranuclear inclusions were present within the macrophages and multinucleated giant cells. Species Equid herpesvirus 5 (EHV-5)–associated dermatitis resembling herpes-associated erythema multiforme was described in a 9-year-old Holsteiner stallion. Skin lesions consisted of nonpruritic, multifocal, pustular dermatitis around the eyes, nostrils, and muzzle. Histologically, there was interface dermatitis with apoptotic keratinocytes and intranuclear inclusions within the stratum spinosum and stratum granulosum.
Further reading
Herder V, et al. Equid herpesvirus 5-associated dermatitis in a horse resembling herpes-associated erythema multiforme. Vet Microbiol 2012;155:420-424.
Scott DW, Miller WH. Viral and protozoal skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 251-262.
Felid herpesvirus 1
Species Felid herpesvirus 1 (FeHV-1, Feline viral rhinotracheitis virus), a well-recognized pathogen of the upper respiratory tract, is commonly associated with oral ulceration. It can also be associated with focal ulcerative lesions, primarily on the haired skin of the face or on the nasal planum, with rare reports of lesions on the feet and trunk. The lesions generally occur in the absence of clinical respiratory signs. In common with other herpesviruses, FeHV-1 can establish latency in the trigeminal ganglion. As affected cats often have a history of previous respiratory disease or recent stress, recrudescence of a latent herpesvirus infection is likely. The macroscopic lesions consist of crusts, ulcers, and vesicles, frequently on the face or nasal planum, which can be persistent or recurrent (Fig. 6-86A ). Microscopically, the lesions are ulcerative and necrotizing, and the mixed dermal inflammation frequently includes numerous eosinophils. There may be foci of degranulating eosinophils around collagen fibers (flame figures). Large amphophilic or glassy intranuclear inclusions are present in the surface and adnexal epithelium (Fig. 6-86B). They are variable in number and sometimes hard to find in small rafts of epithelial cells surrounded by necrotic debris. The similarity of the inflammatory component in this condition with that of the feline hypersensitivity conditions, such as mosquito- bite hypersensitivity or feline eosinophilic granuloma complex, warrants close scrutiny of eosinophilic necrotizing cutaneous lesions for intranuclear inclusions or examination by molecular techniques.
Figure 6-86.

Feline herpesviral dermatitis. A. Ulceration and crusting around eyes and nose.
(Courtesy W.H. Miller.)
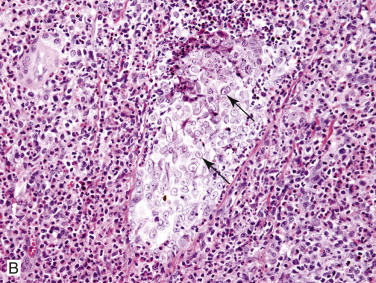
B. Eosinophilic intranuclear inclusion bodies (arrows) within hair follicle epithelium surrounded by eosinophilic dermatitis.
A similar FeHV-1 associated eosinophilic dermatitis, although reportedly more severe and widespread, occurs in captive cheetahs.
Further reading
Hargis AM, et al. Ulcerative facial and nasal dermatitis and stomatitis in cats associated with feline herpesvirus 1. Vet Dermatol 1999;10:267-274.
Munson L, et al. Chronic eosinophilic dermatitis associated with persistent feline herpes virus infection in cheetahs (Acinonyx jubatus). Vet Pathol 2004;41:170-176.
Persico P, et al. Detection of feline herpes virus 1 via polymerase chain reaction and immunohistochemistry in cats with ulcerative facial dermatitis, eosinophilic granuloma complex reaction patterns and mosquito-bite hypersensitivity. Vet Dermatol 2011;22:521-527.
Retroviral infections
Several skin disorders have been associated with retroviral infections caused by species Feline leukemia virus (FeLV) and Feline immunodeficiency virus (FIV) in cats. Because both viruses are immunosuppressive, most dermatologic conditions are considered secondary. However, primary viral infection of keratinocytes has been reported. Scaling, crusting, and alopecic lesions affecting primarily the head and face, with occasional involvement of trunk and extremities is seen rarely in FeLV-infected cats. Histologically, syncytial keratinocytes are seen in the epidermis and superficial follicular epithelium, accompanied by individual cell necrosis (apoptosis), pustules, and ulcers. Immunohistochemical staining demonstrates FeLV antigen in epithelial cells and giant cells. In addition, cutaneous keratin horns seen in FeLV-infected cats have been reported as a primary effect of viral infection of keratinocytes. Recurrent pyoderma and paronychia have been attributed to the immunosuppressive effects of FeLV. Dermatologic diseases associated with naturally occurring chronic FIV infection include generalized demodectic mange, notoedric mange, dermatophytosis, Malassezia dermatitis, cowpoxvirus infections, bowenoid in situ lesions, atypical mycobacteriosis, and abscesses. Cats that are FIV positive are more frequently diagnosed as having subcutaneous abscesses and cellulitis than are noninfected cats. Because the virus is shed in high titer in the saliva, and bite wounds are thought to be an important mode of transmission, this finding may simply reflect a greater tendency for cats that fight to become FIV positive. Many of the associations made between retroviral infection and specific diseases are anecdotal. A nonpruritic generalized skin disorder characterized by a papulocrustous eruption with alopecia and scaling most severe on the head and limbs has been described in 3 FIV-positive cats. Microscopically, there was hydropic interface dermatitis with occasional giant cells and pale basal epidermal cells. Degenerative mucinotic mural folliculitis is described rarely in cats infected with FIV (see Miscellaneous skin conditions).
Further reading
Fleming EJ, et al. Clinical, hematologic, and survival data from cats infected with feline immunodeficiency virus (1983-1988). J Am Vet Med Assoc 1991;199:913-916.
Gross TL, et al. Giant cell dermatosis in FeLV-positive cats. Vet Dermatol 1993;4:117-122.
Gross TL, et al. Degenerative mucinotic mural folliculitis in cats. Vet Dermatol 2001;12:279-283.
Merchant SR, Taboada J. Systemic diseases with cutaneous manifestations. Vet Clin North Am Small Anim Pract 1995;25:945-959.
Miller WH, et al. Viral, rickettsial and protozoal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 343-362.
Parvoviral infections
More typically associated with reproductive problems, species Porcine parvovirus (PPV) has been implicated in outbreaks of vesicular and ulcerative dermatitis and glossitis in 1-4 week-old piglets in the midwestern United States. Various clinical signs, including diarrhea and sneezing, accompanied the skin lesions. Small slit-like erosions, ruptured vesicles, and extensive ulceration were seen on the tongue, lips, snout, coronary band, and interdigital spaces. Severe lesions sometimes led to separation and sloughing of the hoof wall. Intact vesicles were seen rarely. Sporadic cases have been reported in which the lesions were exudative rather than ulcerative. They were grossly indistinguishable from those of exudative epidermitis. PPV has been cultured from skin and internal organs of affected piglets, and PPV antigen has been detected in hair follicles of lesional skin. Skin lesions were reproduced with tissue culture–origin PPV, but were not as severe as those induced with crude suspensions prepared from the skin lesions. In the sporadic cases, Staphylococcus spp. and swinepox virus were also recovered. It is likely that the severe clinical disease results from dual bacterial and viral infection.
Further reading
Lager KM, Mengeling WL. Porcine parvovirus associated with cutaneous lesions in piglets. J Vet Diagn Invest 1994;6:357-359.
Whitaker HK, et al. Parvovirus infection in pigs with exudative skin disease. J Vet Diagn Invest 1990;2:244-246.
Caliciviral infection
Species Feline calicivirus belongs to the genus Vesivirus. Many different strains exist. The most common clinical signs associated with infection are oral vesicles, ulcers, depression, pyrexia, sneezing, and conjunctivitis with ocular and nasal discharge. An unusual pustular dermatitis of the shaved ventral abdomen was described in 2 cats following routine ovariectomy. The histopathology showed panepidermal pustulosis and necrotizing dermatitis. Virulent systemic calicivirus has been associated with facial and paw edema and with ulcers and crusting of the skin of the nose, lips, pinnae, periocular region, and distal limbs. Cutaneous vasculitis is seen in some of these cats.
Further reading
Declercq J. Pustular calicivirus dermatitis on the abdomen of two cats following routine ovariectomy. Vet Dermatol 2005;16:395-400.
Pesavento PA, et al. Pathologic, immunohistochemical, and electron microscopic findings in naturally occurring virulent systemic feline calicivirus infection in cats. Vet Pathol 2004;41:257-263.
Papillomaviral infections
Papillomaviruses are associated with a variety of proliferative skin lesions, typically benign epithelial neoplasms, although they have also been shown to be associated with proliferative cutaneous plaques and papules. Although these lesions are almost always benign and often self-limiting, there is evidence that, in some cases, both in humans and animals, the virus can be a factor in the development of malignant tumors. Papillomaviruses tend to be species-specific viruses that affect stratified squamous epithelium in all domestic and numerous wildlife species. Papillomavirus-associated lesions are discussed under Tumors of the epidermis.
Miscellaneous viral infections of the skin
Foot-and-mouth disease, vesicular stomatitis, vesicular exanthema of swine, swine vesicular disease, bovine viral diarrhea, and bluetongue are discussed in Vol. 2, Alimentary system and peritoneum.
Feline infectious peritonitis (FIP), caused by a mutated feline coronavirus, is a systemic viral disease with rare cutaneous manifestations. Multiple papular to nodular, nonpruritic lesions over the head, neck, trunk, and limbs have been described. Histologically, these lesions have been characterized by pyogranulomatous perivascular to nodular dermatitis, pyogranulomatous vasculitis, and folliculitis. Immunohistochemistry for the detection of intracellular feline coronavirus (FCoV) antigen in macrophages is required to confirm the diagnosis. Ulcerative lesions around the head and neck associated with superficial dermal vasculitis have been described in experimentally infected cats.
Further reading
Bauer BS, et al. Positive immunostaining for feline infectious peritonitis (FIP) in a Sphinx cat with cutaneous lesions and bilateral panuveitis. Vet Ophthalmol 2013;16(Suppl. 1):160-163.
Declercq J, et al. Papular cutaneous lesions in a cat associated with feline infectious peritonitis. Vet Dermatol 2008;19:255-258.
Miller WH, et al. Viral rickettsial and protozoal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 343-362.
Bacterial Diseases of Skin
Normal skin of healthy individuals is highly resistant to invasion by bacteria because of natural defense mechanisms, consisting of physical, chemical, immunologic, and microbial components. The stratum corneum is composed of tightly packed keratinized cells and intercellular substance derived from lamellar granules that form an impermeable physical barrier. Furthermore, this layer continually desquamates, and any adherent bacteria are lost as the outer cells are shed. The sebum-sweat emulsion, which spreads along the skin surface, contains a variety of antibacterial substances, including fatty acids, inorganic salts, and proteins such as complement components, transferrin, and immunoglobulins. Finally, the normal skin microflora prevents pathogenic bacteria from multiplying and becoming established on the skin. These normal resident bacteria are a mixture of organisms that live in symbiosis and maintain static, consistent populations restricted to the superficial layers of the stratum corneum and hair follicle infundibula. They inhibit colonization of invading organisms by competition for limited nutrients and production of antibacterial substances. The protective effect of bacterial interference is well documented. For example, the development of exudative epidermitis has been prevented by exposing piglets to avirulent strains of Staphylococcus hyicus.
The normal skin flora is established shortly after birth, and it is difficult subsequently to introduce other bacteria. The normal resident flora of skin has been investigated most extensively in dogs. Coagulase-negative staphylococci, Micrococcus spp., some aerobic gram-negative species, and Clostridium spp. are most numerous and are probably residents of canine skin. Although Staphylococcus pseudintermedius is the most frequent bacterial pathogen isolated from canine clinical specimens, it is also a part of the normal cutaneous microflora and colonizes the skin, hair follicles/coat, and in particular, mucocutaneous sites, such as the nose, mouth, and anus. It is thought to be part of the resident biota of these regions, and these sites can be spread to other regions of the body. S. pseudintermedius constitutes about 90% of staphylococci isolated from canine healthy carriers and from dogs with underlying skin disease. In all species, skin surface humidity and temperature are important factors in determining the composition and density of skin microflora, with hot humid conditions being associated with increased numbers of skin bacteria. Regional variation in numbers and types of bacteria occurs, and moist intertriginous areas and oily skin have the highest numbers of bacteria.
Cutaneous bacterial infections are typically pyogenic and are thus commonly called pyodermas. They can be categorized as primary and secondary or superficial and deep. Primary pyodermas are those for which no underlying cause can be found. However, it is now thought that the vast majority of pyodermas are secondary to underlying cutaneous, endocrine, or immunologic abnormalities. Localized disruption of normal host defenses may be produced by maceration, biting ectoparasites, scratching, abrasions and other skin wounds, or introduction of foreign bodies, such as plant thorns or awns; such disruption promotes development of clinical infection. Allergic, seborrheic, and follicular disorders are the most common predisposing causes of bacterial skin infection in dogs. Hypothyroidism and spontaneous and iatrogenic hyperadrenocorticism are common metabolic conditions associated with pyoderma. Primary immunologic abnormalities are uncommon to rare predisposing factors.
Bacterial skin disease is seen much more frequently in dogs than in any other mammalian species, and pyoderma is one of the most common skin diseases in dogs. This apparent increased susceptibility of dogs to pyoderma has been attributed to the relatively thin compact stratum corneum, the small amount of intercellular lipids in the stratum corneum, lack of a protective lipid seal at the entrance of canine hair follicles, and the relatively high pH of canine skin. S. pseudintermedius is the predominant bacterial isolate from canine pyodermas. It is also frequently isolated from canine ear and wound infections and can be a complicating factor in immunomodulatory-responsive lymphocytic-plasmacytic pododermatitis. The pathogenesis of S. pseudintermedius infection is poorly understood. It is an opportunistic pathogen and does not cause disease unless the resistance of the host is lowered or the skin barrier is altered by atopic dermatitis, medical and surgical procedures, and/or immunosuppressive disorders. Similar to Staphylococcus aureus, S. pseudintermedius produces a variety of virulence factors, including enzymes such as coagulase, thermonuclease, and proteases; surface proteins such as clumping factor and protein A; and toxins such as cytotoxins, exfoliative toxin, and enterotoxin. It has also been shown to form biofilms. A major rapidly emerging problem with this organism has been multidrug resistance generally characterized by methicillin resistance and the presence of the mecA gene. The mecA gene encodes an altered, surplus cell wall penicillin-binding protein 2a (PBP2a), which has a low affinity to virtually the entire class of β-lactam antibiotics.
Coagulase-positive staphylococci are also the most common bacteria isolated from pyoderma in horses (S. aureus, S. delphini) and in cattle, goats, and sheep (S. aureus). S. hyicus causes exudative epidermitis in piglets and has been associated with superficial pyoderma in several other species. Many other bacteria cause skin infections. Dermatophilus congolensis is responsible for superficial pyoderma in many species. Many gram-negative bacteria are opportunistic pathogens that can invade already diseased or compromised skin. Organisms that are typically associated with infections of other organ systems occasionally cause skin disease. Listeria monocytogenes has been found to be the cause of pyoderma in a small number of humans and a dog with multiple nodules over the back. Although bacterial infections are typically associated with neutrophilic inflammation, certain bacteria, such as mycobacteria, Actinomyces, and Nocardia, typically produce pyogranulomatous dermatitis or panniculitis.
Further reading
Bannoehr J, Guardabassi L. Staphylococcus pseudintermedius in the dog: taxonomy, diagnostics, ecology, epidemiology and pathogenicity. Vet Dermatol 2012;23:253-266.
Foster AP. Staphylococcal skin disease in livestock. Vet Dermatol 2012;23:342-351.
Harvey RG, Lloyd DH. The distribution of bacteria (other than staphylococci and Propionibacterium acnes) on the hair, at the skin surface and within hair follicles of dogs. Vet Dermatol 1995;6:79-84.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Lloyd D. Ecology of the skin: balance and disruption. Compend Contin Educ Pract Vet 1997;19(Suppl. ):97-100.
Loncarevic S, et al. A case of canine cutaneous listeriosis. Vet Dermatol 1999;10:69-71.
Mason IS, et al. A review of the biology of canine skin with respect to the commensals Staphylococcus intermedius, Demodex canis and Malassezia pachydermatis. Vet Dermatol 1996;7:119-132.
Superficial bacterial pyoderma
Superficial pyodermas involve the epidermis and/or superficial portion of hair follicles. They occur more commonly than deep pyodermas. Superficial pyodermas usually are of short duration, heal without scarring, and are not usually associated with systemic illness. Gross lesions are extremely variable and include papules, pustules, crusts, circular scaling areas of alopecia with epidermal collarettes (Fig. 6-87 ), hyperpigmented or erythematous macules, a moth-eaten appearance to the haircoat, diffuse erythroderma, and hyperpigmented lichenified plaques. Microscopic lesions consist of subcorneal or loosely organized, spongiotic superficial epidermal pustules, superficial folliculitis, and crusts. Neutrophils are the predominant inflammatory cell. Bacteria are not always visible histologically, and culture may be necessary to confirm the etiology.
Figure 6-87.

Pustule (arrow) and annular erythematous lesion with central hyperpigmentation and epidermal collarette.
(Courtesy M.S. Canfield).
Impetigo
Impetigo is a superficial pustular dermatitis that does not involve hair follicles. It is most common in dogs but also occurs in kittens, piglets, cows, sheep, and goats. Impetigo is usually caused by coagulase-positive staphylococci. In puppies, it tends to occur before or at the time of puberty for no apparent reason. In other animals, it is usually seen in association with predisposing causes, such as moist and dirty environments, cutaneous abrasions, parasitism, stress, and poor nutrition. Lesions develop in young kittens as a result of excessive wetting of the skin by the queen as she transports the kittens. Bullous impetigo is more often seen in adult dogs and is usually associated with diabetes mellitus, hypothyroidism, and natural or iatrogenic hyperglucocorticism. In these cases, other bacteria such as Escherichia coli and Pseudomonas spp. may be present.
The lesions begin as small erythematous papules that develop into superficial pustules. They are fragile and rupture easily, leaving a honey-colored crust adherent to a shallow erosion. A bullous form of impetigo consists of large flaccid pustules. In puppies, the lesions are most common on the glabrous skin of the inguinal and axillary areas. In kittens, the lesions are usually confined to sites that are most commonly in contact with the queen's mouth; these include the back of the neck, head, and shoulder areas. Lesions in cows and does are usually on the udder, especially at the base of the teats and the intermammary sulcus. Occasionally, the infection extends to involve the teats, ventral abdomen, medial thighs, perineum, and ventral surface of the tail. In general, these lesions are nonpruritic, nonpainful, and heal spontaneously. Spread of infection by the milker to other cows or does and to the hands of milkers has been suggested. One outbreak of contagious impetigo in a herd of dairy cattle was associated with crowding and intensive showering of the cows to decrease heat stress during the heat of summer.
The microscopic lesion of impetigo is a subcorneal pustule composed primarily of neutrophils. The pustules usually extend above the skin surface and are located between hair follicles. Bullous impetigo consists of larger pustules that span several hair follicles (Fig. 6-88 ). Acantholysis may be mild. Gram-positive cocci are present within intact pustules (see Fig. 6-88 inset). The epidermis is mildly to moderately acanthotic, and variable intercellular edema is common beneath pustules. The superficial dermis is edematous, and superficial perivascular to interstitial inflammation is composed predominantly of neutrophils. The principal differential diagnosis is pemphigus foliaceus. However, in contrast to pemphigus, acantholysis is absent or minimal in impetigo, and bacteria are present in intact pustules of impetigo.
Figure 6-88.
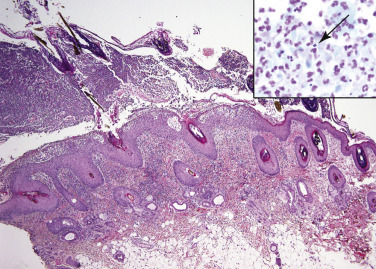
Bullous impetigo in a dog. Large subcorneal pustule spans multiple follicles and contains degenerate neutrophils and gram-positive bacterial cocci (arrow, see inset).
Mucocutaneous pyoderma primarily affects the lips and perioral skin of dogs and rarely horses. German Shepherd dogs and their crosses are at increased risk. Lesions are symmetrical and include erythema, swelling, crusting, erosions, and depigmentation of the lips. Histologically, this condition has features similar to discoid lupus erythematosus. There is epidermal hyperplasia with a lichenoid infiltrate of lymphocytes and plasma cells and pigmentary incontinence. In addition, there are moderate to large numbers of neutrophils in the epidermis and superficial dermis, and the basement membrane is not obscured. Hydropic degeneration and apoptosis of the stratum basale are usually not present. The etiology is unknown; however, the condition responds to antibiotic therapy.
Exudative epidermitis of pigs
Exudative epidermitis is an acute, exudative, superficial pyoderma of young pigs most commonly caused by Staphylococcus hyicus subsp. hyicus. There may be other staphylococcal bacteria involved, such as S. chromogenes and S. sciuri. The disease has also been called greasy-pig disease, impetigo contagiosa suis, and seborrhea oleosa. The infection is common and occurs worldwide. It is most common in piglets 5-35 days of age, but mild cases occur in older pigs also. The morbidity ranges from 10-90% and mortality from 5-90%. Mortality is higher in young pigs with lower resistance. Usually, when a litter is affected, all piglets develop the disease. The infection may cause significant economic loss. Autogenous vaccines prepared from toxigenic strains of bacteria have been used to prevent infection in some situations.
The pathogenesis of exudative epidermitis is incompletely understood. Both virulent and nonvirulent strains of S. hyicus are part of the normal skin flora of healthy pigs; it is carried on the conjunctiva, snout, ear skin, and vagina. The highest rates of carriage of the organism are found in the youngest piglets, suggesting that the organisms are acquired at birth. It is thought that infection develops as a result of trauma that breaches the skin barrier. Other factors that may predispose piglets to developing clinical disease include agalactia of the sow, concurrent infections, and nutritional deficiencies. The presence of porcine circovirus 2 and porcine parvovirus have been suggested as predisposing factors. The most important factor in the pathogenesis of this skin disease is considered to be the presence of bacterial strains that express exfoliative toxins known as ExhA, ExhB, ExhC, ExhD, SHETA, and SHETB. The Exh toxins have been shown to digest desmoglein-1 in the epidermis of porcine skin. This disease process is considered to involve the same mechanisms as staphylococcal scalded skin syndrome and bullous impetigo in humans.
The disease can be divided into acute, subacute, and chronic forms:
-
•
In the acute form, most common in piglets only a few days old, there is abrupt onset of lesions around the eyes, snout, chin, and on the ears, with extension to the medial aspect of the legs. Lesions then rapidly spread to the thorax, abdomen, entire legs, and coronets. Lesions begin as peeling of small areas of the stratum corneum, leaving red, glistening, moist areas. These areas are quickly covered by greasy, dark brown exudate. Lesions become generalized in 24-48 hours, and the entire body is erythematous and covered with brown, greasy, malodorous exudate. Erosions of the coronary bands and heels commonly develop. Conjunctivitis also occurs frequently and typically causes matting together of the eyelids and results in an inability to see. Death occurs within 3-5 days as a result of dehydration, electrolyte imbalance, negative energy balance, and septicemia.
-
•
In the subacute form, the course is more protracted. The skin becomes thick and wrinkled, and the exudate covering the entire body becomes dry, hard, and cracked, producing a generalized furrowed appearance. The underlying skin visible in the furrows is red (Fig 6-89 ).
-
•
The chronic form occurs in older piglets, and skin lesions are milder and usually confined to the head and ears and consist of erythema and waxy brown crusts. Older piglets with less severe forms of disease frequently survive; however, recovery is slow, and the piglets are severely stunted. Lesions that may also occur in affected piglets are subcutaneous abscesses, necrosis of the ears and tail, and polyarthritis.
Figure 6-89.

Exudative epidermitis in a piglet. Parallel rows of matted hair (“furrows”) separated by erythematous waxy skin.
The earliest microscopic lesion is subcorneal vesicular to pustular dermatitis. Extension of infection to hair follicles results in a superficial purulent luminal folliculitis. In fully developed lesions, the skin is covered with a thick crust composed of orthokeratotic and parakeratotic keratin, lakes of serum, accumulations of neutrophils, necrotic debris, and microcolonies of gram-positive cocci. The epidermis is variably acanthotic and rete ridges are elongated. Cells in the outer stratum spinosum exhibit variable intracellular edema. Neutrophilic exocytosis, intercellular edema, and spongiotic pustules may be seen in the epidermis and infundibular portion of hair follicles. The dermis is edematous, dermal vessels are congested, and there is a perivascular to interstitial neutrophilic infiltrate. Dermal inflammation is more intense and diffuse in areas of ulceration. In chronic cases, exudation is less severe, and there is more marked epidermal hyperplasia and hyperkeratosis. Inflammation in the dermis becomes primarily mononuclear.
Microscopic lesions may also be seen in other tissues. Lymph nodes draining severely affected areas of skin contain foci of hemorrhage, purulent inflammation, and occasional microcolonies of bacterial cocci. Renal lesions are common, and bacteremia is not required for them to be present. The lesions are distinctive, with early vacuolation of the epithelium of collecting ducts and renal pelvis progressing to epithelial degeneration and exfoliation. Intratubular casts of desquamated epithelium may be sufficiently severe to be evident macroscopically, leading to linear striations of the renal pelvis, and accumulation of cellular sediment in the pelvis and ureters. The process may be sufficiently severe to occlude the ureters. In cases in which bacteremia is present, purulent pyelonephritis is common. Animals with greasy pig disease may also have lesions in the oral cavity and conjunctiva, and the causative organism has been associated with abortion in sows.
S. hyicus has been associated with skin lesions in other species. The organism is common in cattle and has been associated with concurrent psoroptic mange. The organism was isolated from skin lesions of a young pygmy goat with chronic generalized seborrheic dermatitis and alopecia. The microscopic lesion was a purulent exudative epidermitis similar to that in pigs. S. hyicus has been cultured from a number of horses with exudative crusty alopecic skin lesions on the distal limbs that resembled “grease heel” clinically.
Further reading
Devriese LA, et al. Staphylococcus hyicus in skin lesions of horses. Equine Vet J 1983;15:263-265.
Foster AP. Staphylococcal skin disease in livestock. Vet Dermatol 2012;23:342-351.
Fudaba Y, et al. Staphylococcus hyicus exfoliative toxins selectively digest porcine desmoglein 1. Micro Pathogen 2005;39:171-176.
Iyori K, et al. Identification of a novel Staphylococcus pseudintermedius exfoliative toxin gene and its prevalence in isolates from canines with pyoderma and healthy dogs. FEMS Microbiol Lett 2010;312:169-175.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Yeruham I, et al. Contagious impetigo in a dairy cattle herd. Vet Dermatol 1996;7:239-242.
Dermatophilosis
Dermatophilosis (cutaneous streptothricosis, mycotic dermatitis, cutaneous actinomycosis, lumpy wool, strawberry foot rot, rain scald, rain rot, Kirchi, Gasin-Gishu, Senkobo disease, Drodo-Boka, Savi, Ambarr-Madow) is an acute, subacute, or chronic superficial exudative dermatitis caused by the actinomycete Dermatophilus congolensis. The disease occurs worldwide and has a wide host range, but it is most common in the hot humid tropics and subtropics and in areas with heavy prolonged rains. In hot monsoon climates, cattle are the primary animals affected, and the disease is endemic in some portions of Africa. In more temperate climates, sheep and goats are involved primarily. The disease is occasional in horses and camels; it is rare in dogs, cats, pigs, and humans. Anecdotal reports exist for alpacas. Cases of dermatophilosis have also been reported in a wide variety of wild and captive mammals and reptiles. There is no apparent sex or age predilection, and congenital infections have been reported in calves and lambs.
In cattle and sheep, dermatophilosis causes important economic losses by virtue of decreased meat and milk production, damaged hides, wool loss, infertility, and early culling. Severe udder and teat lesions may interfere with suckling by calves and result in decreased growth rate. Affected animals are predisposed to secondary infections and cutaneous myiasis. Severely affected animals of any species may become emaciated and die.
Dermatophilus congolensis is a gram-positive facultative anaerobic bacterium whose natural habitat is unknown. Attempts to culture it from soil have been unsuccessful. Studies have shown that the organism's survival in soil is dependent on the type of soil and the water content but not the pH. Clinically normal carrier animals and crusts from infected animals probably serve as sources of infection. Zoospores can remain viable in crusts at a temperature of 28-31° C for up to 42 months. D. congolensis has a distinctive life cycle in which coccoid bodies germinate to produce branching filaments. These filaments undergo transverse and longitudinal septation to form parallel rows of coccoid bodies. The cocci are resistant to unfavorable conditions and are reproductively dormant until the appropriate wet conditions occur and they are activated to become motile zoospores.
Dermatophilosis cannot be reproduced experimentally to resemble natural disease, even with large doses of the organism. Multiple factors appear to be involved in pathogenesis of the natural disease. Two factors that appear to be most important are trauma to the skin and prolonged wetting. Zoospores are unable to overcome the protective barriers of the hair, surface lipid film, and stratum corneum, and their entry is facilitated by breaks in the skin surface. Trauma from ectoparasites, shearing, dipping, barbed wire injuries, sharp stones, and scratches from sharp vegetation can act as portals of entry for the zoospores. Besides producing skin trauma, external parasites such as flies, mites, lice, ticks, and mosquitoes also act as mechanical vectors. In addition to skin trauma, prolonged moisture is needed for the activation, proliferation, and spread of the zoospores. Wetting may also act to breach skin barriers by dissolving the surface lipid film and softening the stratum corneum. Outbreaks of dermatophilosis are frequently associated with periods of unusually heavy rainfall, housing in pastures or paddocks with standing water or mud, or after intensive high-pressure washing of animals.
Other factors involved in development of disease are less well understood. Genetic factors may be involved, because some breeds of cattle appear to be more resistant to disease than are others. Skin color appears to have an effect because some light-skinned breeds or light-skinned areas may be more susceptible to infection. A definite association between infestation with the tick Amblyomma variegatum and occurrence of dermatophilosis in cattle has been found. In herds with effective tick prevention, there is a much lower incidence or diminished severity of the disease. Because the lesions of dermatophilosis do not correspond to sites of tick attachment, a systemic effect on the animal's immune system has been suspected. In addition, concurrent diseases or stresses, including intestinal parasitism, nutritional deficiencies, stress of pregnancy or migration, and viral infections may contribute to the development of dermatophilosis by compromising the host's immune system.
Once the normal skin surface has been disrupted and activated zoospores gain access to the epidermis, infection can develop. The zoospores are apparently attracted to the low carbon dioxide concentration of the normal epidermis, and there they germinate to form filaments that invade the viable epidermis and outer root sheaths of hair follicles. Only rarely do the bacteria proliferate in the dermis or deeper tissues. The means by which D. congolensis invades the epidermis is unknown, but it is thought that the bacteria produces exoenzymes. As the filaments invade the epidermis, keratinocytes at sites of penetration begin to cornify, and numerous neutrophils accumulate beneath and migrate into the epidermis, which subsequently separates from the underlying dermis. The neutrophils inhibit further invasion by the organism, and the epidermis re-forms from cells in adjacent external hair follicle sheaths. This new epidermis is again invaded by organisms arising from the hair follicles to initiate another cycle of epidermal penetration, neutrophilic exocytosis, and epidermal detachment. These repeated sequences of bacterial invasion, inflammation, and epidermal regeneration produce the thick laminar and parakeratotic crusts characteristic of dermatophilosis.
The earliest lesions of dermatophilosis consist of patches of slight erythema that are visible only in unpigmented areas. Very small papules and pustules develop next and are more evident by palpation than by visual inspection. As the lesions become covered by exudate and hairs become entrapped within the developing crust, they form small tufts that resemble paintbrushes (Fig. 6-90A ). As these small lesions coalesce, they form the typical large oval to circular domed yellow-brown adherent scabs that when removed leave a moist hyperemic base that may bleed. The lesions are painful and nonpruritic. In chronic cases, lesions progress to form thick layers of dry spongy material involving extensive areas of long hair or hard wart-like crusts that protrude above the hair surface, usually in areas with a short haircoat.
Figure 6-90.

Dermatophilosis. A. Tufted papules and annular areas of alopecia over the rump and sides of a horse.
(Courtesy D.W. Scott.)

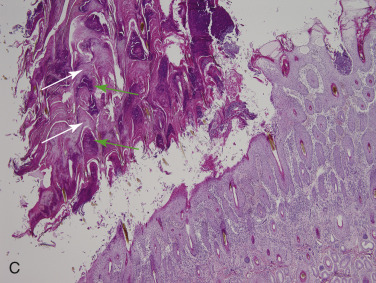
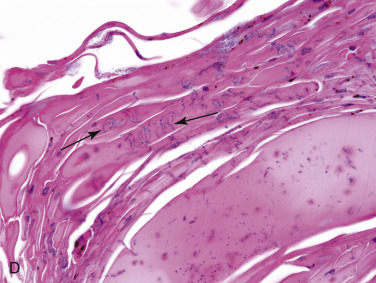
B. Crusted papules and erythema on the muzzle of a horse. C. Skin biopsy from a calf shows large surface crust composed of thick alternating layers of hyperkeratosis (white arrows) and degenerate neutrophils (green arrows) parallel to the skin surface. D. Coccoid organisms forming branching filaments (“railroad tracks”) (arrows) within the surface keratin.
The distribution of lesions in cattle is variable. Lesions confined to the face and ears are most often seen in young suckling calves. In other forms of the disease, lesions occur on the brisket, axillae, and inguinal areas, or on the udder and teats of cows, and scrotum and prepuce of bulls. Cattle standing in deep water or mud develop lesions on the legs. Lesions located in the perineum and tail are assumed to result from trauma caused by mounting by other animals. In many cases, lesions are diffusely distributed over the head, topline of the neck and body to the tail, and dorsal sides. Animals with >50% of body involvement often show weight loss, dehydration, and death. Rare instances of subcutaneous abscesses, lymphadenitis, and oral lesions have been reported.
In sheep, infection of the wooled areas is frequently missed in early stages, and some animals recover spontaneously during the acute stage of infection. If the disease continues to progress, the wool of the neck, back, and flank becomes matted with exudate to form dense pyramidal masses (lumpy wool, mycotic dermatitis) that may last for months to years in some individuals. “Strawberry foot rot” is an infection that begins at the coronet regions and may progress to involve the skin to the carpi and/or tarsi. In some cases, crusts may be confined to the ears, nose, and face, a clinical form common in lambs. Concurrent infection with contagious ecthyma and pox has been reported.
Dermatophilosis in goats frequently consists of 2-3 mm crusty lesions on the pinnae and tail of kids and large pyramidal crusts on the dorsal midline, sides, caudal thighs, and scrotum of adults. Lesions involving the distal limbs resemble strawberry footrot of sheep. Concurrent infection with contagious ecthyma and pox may occur, and secondary infections with staphylococci, streptococci, or corynebacteria may develop. In addition, as with cattle, tick infestations (Amblyomma variegatum and Boophilus decoloratus) are a risk factor for clinical dermatophilosis.
In horses, lesions of dermatophilosis are frequently located on the dorsal aspect of the body and look as if large drops of liquid have scalded the skin (“rain scald”). Horses kept in wet, marshy, or muddy enclosures, and undergoing trauma to the legs, develop lesions of the distal extremities primarily (grease heel, scratches, mud fever). Lesions on the legs may be associated with swelling, pain, and lameness. In some instances, only the head is affected. Unpigmented skin may be more susceptible to infection, and lesions on these areas are typically very erythematous (Fig. 6-90B). These lesions may represent a type of photodermatitis caused by D. congolensis (“dew poisoning”). Outbreaks in show horses have been associated with frequent high-pressure washing.
Dermatophilosis cases reported in cats are notable in that they have all been subcutaneous or extracutaneous infections. The lesions consisted of draining nodules involving, or in the area of, the popliteal lymph nodes or the subcutaneous tissue of a paw and masses on the tongue and serosal surface of the urinary bladder. In at least one of the cats with subcutaneous infection, superficial wounds suggestive of a recent cat fight were seen, prompting speculation that the infection was traumatically introduced.
Dermatophilosis lesions in camels are present, especially on the rump, neck, flanks, and lower abdomen. The legs are generally spared. In one study, infected camels were often infested with Hyalomma spp. ticks, suggesting that ticks may have an important role in the pathogenesis of dermatophilosis in camels.
The earliest histologic lesions of dermatophilosis are superficial dermal congestion, edema, and neutrophil infiltration of the superficial dermis. Exocytosis of neutrophils becomes more pronounced as lesions progress, and intraepidermal or subcorneal pustules may develop. Eventually, repeated cycles of bacterial invasion and inflammation result in thick crusts composed of alternating layers of parakeratotic and orthokeratotic keratin, serous fluid, degenerate inflammatory cells, and bacterial filaments composed of multiple parallel rows of cocci “palisading crust” (Fig. 6-90C, D). The epidermis is acanthotic, with orthokeratotic and parakeratotic hyperkeratosis. Purulent luminal folliculitis with intralesional bacterial filaments is also usually present. Dermal inflammation is usually mild and superficial perivascular. In cases of dermatophilosis in cats and rare instances of subcutaneous and lymph node infection in cattle, the lesions consist of granulomas or pyogranulomas with scattered necrotic foci that contain typical D. congolensis filaments. In one 3-year-old pony, the infection was seen as only granulomatous lymphadenitis.
Ovine fleece rot
So-called “fleece rot” in sheep is caused by excessive moisture (6 days of continual wet wool and skin) and subsequent proliferation of Pseudomonas spp. The bacterial proliferation causes acute inflammation with serum exudation and matting of the wool. The wool becomes discolored by chromogenes produced by the bacteria and has a rotten odor. Histologically, there are epidermal pustules and superficial suppurative luminal folliculitis. Affected sheep are predisposed to myiasis.
Further reading
Ambrose N, et al. Immune responses to Dermatophilus congolensis infections. Parasitol Today 1999;15:295-300.
Ambrose NC, et al. Preliminary characterization of extracellular serine proteases of Dermatophilus congolensis isolates from cattle, sheep and horses. Vet Microbiol 1998;62:321-335.
Byrne BA, et al. Atypical Dermatophilus congolensis infection in a three-year-old pony. J Vet Diagn Invest 2012;22:141-143.
Chatikobo P, et al. Bovine dermatophilosis, a re-emerging pandemic disease in Zimbabwe. Trop Anim Health Prod 2009;41:1289-1297.
Hargis AM, Ginn PE. The integument. In: Zachary JF, McGavin MD, editors. Pathologic Basis of Veterinary Disease. 5th ed. St Louis: Elsevier Mosby; 2012. p. 972-1084.
Hermoso de Mendoza J, et al. Enzymatic activities of Dermatophilus congolensis measured by APIZYM. Vet Microbiol 1993;37:175-179.
Kaya O, et al. Isolation of Dermatophilus congolensis from a cat. J Vet Med B Infect Dis Vet Public Health 2000;47:155-157.
Khodakaram-Tafti A, et al. Prevalence and pathology of dermatophilosis in camels (Camelus dromedarius) in Iran. Trop Anim Health Prod 2012;44:145-148.
Msami HM, et al. Dermatophilus congolensis infection in goats in Tanzania. Trop Anim Health Prod 2001;33:367-377.
Norris BJ, et al. Fleece rot and dermatophilosis in sheep. Vet Micro 2008;128:217-230.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Bacterial skin disease. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Woldemeskel M, Gashaw M. Study on caprine and ovine dermatophilosis in Wollo, Northeast Ethiopia. Trop Anim Health Prod 2010;42:41-44.
Yeruham I, et al. Outbreak of dermatophilosis in a horse herd in Israel. J Vet Med 1996;43:393-398.
Deep bacterial pyoderma
Deep pyodermas are serious bacterial infections that involve the hair follicle, dermis, and/or subcutis. They are often chronic or recurrent, heal with scarring, and are commonly associated with regional or generalized lymphadenopathy and systemic signs. The clinical appearance of deep pyoderma is tremendously diverse. Lesions commonly seen in deep pyodermas include dark red or violaceous raised nodules, poorly demarcated areas of tissue swelling, hemorrhagic bullae, draining tracts, abscesses, purulent or serosanguineous exudate that dries to form crusts, and necrotic or ulcerated skin covered by crusts. Pain may be severe. Microscopic changes associated with deep pyodermas include folliculitis, furunculosis, nodular-to-diffuse dermatitis or panniculitis, and variable fibrosis. Bacteria may not be seen microscopically even with special stains.
Staphylococcal folliculitis and furunculosis
Staphylococcus spp. are the most common cause of folliculitis in domestic animals. Other organisms less frequently or rarely associated with folliculitis include Streptococcus spp., Corynebacterium spp., Pseudomonas spp., Bacillus spp., and Pasteurella multocida. Inflammation of the deep portion of hair follicles frequently results in rupture of the follicular wall (furunculosis) and extension of infection to the surrounding dermis and panniculus. Staphylococcal folliculitis and furunculosis are very common in the dog; common in horses, goats, and sheep; and uncommon in cats, cattle, and pigs. Skin lesions associated with folliculitis and furunculosis are extremely variable. The earliest skin lesion is a follicular papule with one or several hairs protruding from the center. The papule develops into a pustule, but these are very fragile, break easily, and are thus very transient. Consequently, crusted papules are seen more commonly than are pustules. In shorthaired dogs, horses, and cattle, the earliest clinical sign is a dishevelment of the haircoat produced by small groups of hairs tufting together above the skin surface, an appearance that can be confused with urticaria. As the hairs fall out of infected follicles, multiple small foci of alopecia and scaling develop. The haircoat develops a moth-eaten appearance as the areas of alopecia become progressively larger. Lesions often enlarge and develop a central ulcer that discharges purulent or serosanguineous exudate that dries to form a crust. When furunculosis occurs, dark red to violaceous nodules, draining fistulae, ulcers, and extensive tissue swelling develop (Fig. 6-91A ). Hemorrhagic bullae may be prominent in some cases (Fig. 6-91B). Scarring, alterations in pigmentation of the hair and skin, and lichenification may result. Regional and generalized lymphadenopathy are common. Constitutional signs, such as fever and anorexia, may occur when infection is severe or extensive.
Figure 6-91.


Deep bacterial folliculitis and furunculosis. A. Draining tracts in the distal limb of a horse. B. Hemorrhagic bullae on the ventrum of a dog.
(Courtesy W.H. Miller.)
The microscopic changes of staphylococcal folliculitis and furunculosis are as varied as the gross lesions. The epidermis is variably acanthotic and may be ulcerated. Serocellular crusting is common. Staphylococcal folliculitis is characterized by neutrophilic inflammation, but the relative number of neutrophils is extremely variable, depending on the duration of the infection and presence of furunculosis. Pustules composed of neutrophils may be seen within the infundibulum or ostium of hair follicles. Small numbers of eosinophils may be seen and in some cases may indicate a concurrent allergy or ectoparasite. Neutrophils accumulate within the lumen of hair follicles, distending the lumen and frequently causing rupture of the hair follicle wall (see Fig. 6-5B). Neutrophils, eosinophils, macrophages, and plasma cells form dense sheets in the dermis and may extend to the panniculus. Hemorrhagic bullae consist of large pustules with hemorrhage in the interfollicular dermis. Large dermal pustules may form cavitary lesions. Release of hair and keratin into the dermis or panniculus induces an intense foreign-body reaction that may completely efface the follicle (see Fig. 6-6). Fragments of hair or keratin may be surrounded by discrete granulomas (trichogranuloma) composed of multinucleated giant cells, epithelioid macrophages, and neutrophils. Eosinophils may be numerous around the fragments of hair and keratin. Inflammation may become diffuse as adjacent furuncles coalesce and completely replace normal dermal structures. Hemorrhage and fibroplasia are variable. Bacteria may not be evident even with special stains, such as tissue Gram stain or Giemsa stain.
Deep pyoderma is not as common as superficial pyoderma but is still a relatively common disease in dogs. Staphylococcus pseudintermedius is usually the primary pathogen in bacterial folliculitis and furunculosis in dogs. However, gram-negative bacteria, such as Proteus, Pseudomonas, and Escherichia coli are common secondary invaders. Rarely, acute deep pyoderma presenting with dorsal truncal pain has been associated with a pure culture of Pseudomonas aeruginosa in dogs. In some cases, this condition may be associated with self-service dog-grooming facilities or aggressive grooming, such as back-clipping and back-combing. Deep pyoderma may be localized or widespread. Localized forms of staphylococcal deep pyoderma commonly involve the bridge of the nose, the chin (“canine acne”), paws (interdigital “pedal” folliculitis-furunculosis), and pressure points. A particularly refractory form of staphylococcal pyoderma has been recognized in German Shepherd dogs. German Shepherd pyoderma is a genetically inherited characteristic clinical syndrome that can be triggered by a variety of other diseases in susceptible individuals. This condition affects middle-aged German Shepherd dogs and their crosses. Rump, back, ventral abdomen, and thighs are the typical distribution. In some cases, lesions are more generalized. These dogs have a disproportionately severe form of pyoderma. Typical lesions include papules, pustules, erosions, and crusts, followed by ulcers, draining tracts, furunculosis, alopecia, and hyperpigmentation. Lesions are pruritic and may be painful. An immunologic abnormality is suspected because most affected dogs have a relative increase in the CD8+ T lymphocytes and relative decrease in the CD4+ and CD21+ lymphocytes in peripheral blood. Whether these changes are a cause or effect of the disease is unknown, and in addition, some believe that in general normal German Shepherd dogs have lower lymphocyte subpopulations with a relative increase of CD8+ T lymphocytes. Examination of T and B lymphocytes in histologic sections found a marked paucity of T lymphocytes in lesions of deep pyoderma of German Shepherd dogs as compared to similar lesions from dogs of other breeds. Although not always apparent, there is generally thought to be another factor that triggers the condition (e.g., flea-bite hypersensitivity, atopic dermatitis, adverse food reactions, ehrlichiosis, or hypothyroidism).
Staphylococcal folliculitis and furunculosis in horses are usually secondary to trauma and various physiologic stresses. Lesions most often involve the harness, saddle (saddle scab, saddle boils), neck, and dorsal lumbosacral regions. Friction from tack is considered an important initiating factor. It is most common in the summer, coincident with excessive sweating, higher environmental temperature and humidity, and increased numbers of biting insects. Lesions are usually painful rather than pruritic. Staphylococcal pyoderma may be one of many causes of pastern dermatitis (grease heel, scratches) in which lesions involve the caudal aspect of the pastern and fetlock areas of one or more legs. In tail pyoderma, the dorsal surface of the tail is particularly affected, and infection is usually secondary to skin abrasions caused by tail rubbing associated with insect bites, mange, biting lice, pinworms, yeast dermatitis, herpes coital exanthema, or vice. Although much less common, Corynebacterium pseudotuberculosis can cause folliculitis and clinical lesions (“contagious acne”) similar to those with staphylococcal folliculitis.
Staphylococcal folliculitis and furunculosis are common in goats and sheep, frequently are secondary to trauma or moisture, and Staphylococcus aureus is most commonly isolated. Lesions include papules, pustules, crusting, and alopecia. Common locations in goats are periocular areas, pinnae, distal limbs, dorsal trunk, neck, ventral abdomen, and medial thighs. Severe infections, particularly those with secondary mastitis, may produce pyrexia, anorexia, depression, and septicemia. In sheep, lesion distribution is muzzle, tail, and perineum of otherwise healthy 3-4 week-old lambs that usually regresses spontaneously within 3 weeks. A generalized skin infection with septicemia similar to porcine exudative epidermitis has been described in neonatal lambs. Staphylococcus xylosus, a coagulase-negative staphylococcus, was isolated from the skin and various tissues. In adult sheep, lesions of bacterial folliculitis and furunculosis usually occur on the poorly wooled areas of the face (periocular, pinna, base of the horn, nasal bones, maxillary ridge) and include pustules, crusts, erosions, and ulcerations. These lesions are commonly associated with crowded feeding in troughs, with head rubbing and fighting (facial eczema, eye scab), particularly of adult ewes just prior to lambing. In both goats and sheep, lesions are generally nonpruritic, but furunculosis can be painful.
Staphylococcal folliculitis and furunculosis occur occasionally in cattle, pigs, cats, and alpacas. Infection in cattle is seen most commonly in young bulls on the tail, perineum, scrotum, and face, and S. aureus is most commonly isolated. Trauma and poor hygiene may be initiating factors. Staphylococcal folliculitis in pigs usually occurs on the hindquarters, abdomen, and chest of piglets <8 weeks of age and spontaneously regresses. Pustules covering much of the body rupture, forming brown crusts that are neither painful nor pruritic. Bacterial folliculitis and furunculosis is uncommon in cats and is usually secondary to other underlying conditions, such as feline acne and hypersensitivity conditions. Lesions may consist of a crusted papular eruption on the face, head, or over the dorsum that clinically resembles miliary dermatitis. Bacterial folliculitis in alpacas may be associated with insect-bite hypersensitivity, contact dermatitis, or idiopathic. Lesions consist of erythematous papules, pustules, brown-to-yellow crusts, epidermal collarettes and annular areas of alopecia and scaling, and are most common over the muzzle, back, ventrum, and distal hindlegs. Pruritus is more likely with an underlying hypersensitivity.
Further reading
Bannoehr J, Guardabassi L. Staphylococcus pseudintermedius in the dog: taxonomy, diagnostics, ecology, epidemiology and pathogenicity. Vet Dermatol 2012;23:253-266.
Chabanne L, et al. Lymphocyte subset abnormalities in German shepherd dog pyoderma (GSP). Vet Immunol Immunopathol 1995;49:189-198.
Day MJ. An immunopathological study of deep pyoderma in the dog. Res Vet Sci 1994;56:18-23.
Denerolle P, et al. German shepherd dog pyoderma: a prospective study of 23 cases. Vet Dermatol 1998;9:243-248.
Foster AP. Staphylococcal skin disease in livestock. Vet Dermatol 2012;23:342-351.
Hillier A, et al. Pyoderma caused by Pseudomonas aeruginosa infection in dogs: 20 cases. Vet Dermatol 2006;17:432-439.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Rosser EJ. German shepherd dog pyoderma. Vet Clin North Am Small Anim Pract 2006;36:203-211.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Feline dermatology at Cornell University: 1407 cases (1988-2003). J Fel Med Surg 2012;15:307-316.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Abscesses and cellulitis
Abscesses are well-circumscribed accumulations of pus. Cellulitis is a severe, deep, suppurative infection that is poorly defined and tends to dissect through tissue planes. The lesions are usually painful, often warm, and overlying skin is often friable, dark, devitalized, and may be sloughed. The wounds frequently have a putrid smell and may be emphysematous if the organism is a gas producer (Clostridium spp., Bacteroides spp.). Pyrexia and regional lymphadenopathy may be present. Abscesses and cellulitis are fairly common in large animals and are one of the most common disorders in cats, where they are a frequent sequel to fight wounds. Other predisposing causes include traumatic puncture wounds, foreign bodies, injections, and shearing and clipping wounds. Microscopically, abscesses consist of central accumulations of neutrophils and/or necrotic debris, frequently surrounded by a wall of granulation tissue or dense collagenous connective tissue, depending on duration. In contrast, cellulitis is poorly circumscribed and consists of extensive purulent to pyogranulomatous dermal and subcutaneous inflammation that may be accompanied by hemorrhage, necrosis, and thrombosis. Bacteria may or may not be visible histologically.
A wide variety of aerobic and anaerobic bacteria have been associated with abscesses and cellulitis. The most common organisms include Staphylococcus spp. (dogs, horses, cattle, goats, pigs), Clostridium spp. (malignant edema, gas gangrene, and big head in horses, cattle, sheep, goats, pigs, and dogs), Pasteurella multocida (cats), and Corynebacterium pseudotuberculosis (abscesses in horses, goats, cattle, alpacas, and sheep; ulcerative lymphangitis in horses, cattle, sheep, and goats; caseous lymphadenitis in sheep and goats; pyogranulomas in cats), and Trueperella pyogenes (abscesses in cattle, goats, sheep, pigs, horses; ulcerative lymphangitis in cattle and goats). Rhodococcus equi, most commonly associated with pneumonia in young horses, has been isolated from cutaneous abscesses and cellulitis in young horses and rarely in cats. Pasteurella granulomatis has been associated with a disease in southern Brazil called lechiguana, which is characterized by large subcutaneous fibrosing eosinophilic abscesses. Lesions are most commonly located in the scapular region, and the condition is frequently fatal if untreated. Various mycoplasmas and mycoplasma-like organisms have been recovered from abscesses in cats and from decubital abscesses in calves.
Streptococcus canis, Lancefield group G, has been isolated in most cases of necrotizing fasciitis. This is a rare condition that has been described most commonly in dogs, very rarely in cats, and one 2-year-old bull. Staphylococcus pseudintermedius and E. coli have been isolated from a few affected dogs. Arcanobacterium haemolyticum was isolated from the bull. Necrotizing fasciitis is a severe life-threatening disease that usually starts as a localized infection but spreads rapidly and aggressively within hours. The condition is characterized grossly by extensive exudation along fascial planes and necrosis of subcutaneous fat and fascia, resulting in extensive sloughing of necrotic skin. The microscopic lesions of necrotizing fasciitis include severe necrosis, suppuration, fibrinous exudation, and hemorrhage of the dermis and subcutaneous fat, fascia, and muscle. In some instances, the epidermis and superficial dermis are infarcted as a result of thrombosis of dermal and subcutaneous blood vessels. Colonies of bacterial cocci may be evident in the inflamed subcutaneous tissue.
A condition histologically identical to toxic shock syndrome (TSS) in humans has been described in dogs. TSS in humans is associated with S. aureus and group C streptococci infections. Bacterial toxins, including toxic shock syndrome toxin-1 (TSST-1), are thought to induce massive cytokine release (including tumor necrosis factor-α and interleukin-1), increased sensitivity to cytokines, and endothelial damage. In dogs, TSS has been associated with S. pseudintermedius infection. Lesions include macular erythema and edema of the trunk and limbs initially with vesicles, ulcers, and variable crusting seen later. Fever, depression, anorexia and hypoalbuminemia are common. Disseminated intravascular coagulation is a consistent finding in dogs that succumb to infection. Histologically, there is epidermal and follicular epithelial spongiosis, with individual keratinocyte necrosis (apoptosis) associated with neutrophils and occasionally eosinophils surrounding the necrotic cells. There may also be suppurative epidermitis, crusts, and confluent epidermal necrosis. In the dermis, there is edema, extravasation of erythrocytes, and variable perivascular neutrophils and fewer eosinophils.
In dogs, Streptococcus canis and S. pseudintermedius have also been associated with a toxic shock–like syndrome where infected dogs rapidly develop sepsis. Acinetobacter baumannii was isolated from a cat with necrotizing fasciitis and toxic shock. Toxic shock–like syndrome was reported in a 3-year-old Thoroughbred gelding with S. aureus pneumonia.
L-form infections are described in dogs and cats. L-forms are bacterial variants that lack a cell wall and divide by a variety of processes. Lesions occur as one or more draining abscesses, usually over joints. Some animals may be febrile or depressed. L-forms cannot be cultured by routine techniques.
Melioidosis, caused by the gram-negative, intracellular bacterium Burkholderia pseudomallei, produces abscesses in multiple organs. This organism is a soil saprophyte, and infection may occur through inhalation, arthropod-bite and wound contamination. Skin lesions include multiple small nodules that tend to rupture and drain. In addition, horses may develop papulocrustous dermatitis and lymphangitis of the limbs. Glanders, like melioidosis, can have systemic involvement, and both infections are commonly fatal. Glanders is caused by Burkholderia mallei. The cutaneous form of this disease is called farcy. Horses are highly susceptible and are considered the natural reservoir. In the acute form, clinical signs include fever, respiratory signs, painful and enlarged submaxillary lymph nodes, skin nodules on the legs and abdomen, and death caused by septicemia. The chronic form is more common, and skin lesions include nodules forming chains along lymphatics, ulceration, and exudation. Both of these organisms have been eradicated from many parts of the world.
Further reading
Brachelente C, et al. A case of necrotizing fasciitis with septic shock in a cat caused by Acinobacter baumanni. Vet Dermatol 2007;18:432-438.
DeWinter LM, et al. Virulence of Streptococcus canis from canine streptococcal toxic shock syndrome and necrotizing fasciitis. Vet Microbiol 1999;70:95-110.
Fairley RA, Fairley NM. Rhodococcus equi infection of cats. Vet Dermatol 1999;10:43-46.
Gross TL, et al. Necrotizing diseases of the epidermis. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 75-104.
Holbrook TC, et al. Toxic shock syndrome in a horse with Staphylococcus aureus pneumonia. J Am Vet Med Assoc 2003;222:620-623.
Kinde H, et al. Mycoplasma bovis associated with decubital abscesses in Holstein calves. J Vet Diagn Invest 1993;5:194-197.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Miller CW, et al. Streptococcal toxic shock syndrome in dogs. J Am Vet Med Assoc 1996;209:1421-1426.
Nguhiu-Mwangi JA, et al. Necrosis and sloughing of skin associated with limb cellulitis in four cows and a calf: predisposing causes, treatment and prognosis. Vet Rec 1991;129:192-195.
Riet-Correa F, et al. Lechiguana (focal proliferative fibrogranulomatous panniculitis) in cattle. Vet Res Commun 2000;24:557-572.
Scott DW, Miller WH. Bacterial skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Slovak JE, et al. Toxic shock syndrome in two dogs. J Am Anim Hosp Assoc 2012;48:434-438.
Walker RD, et al. Recovery of two mycoplasma species from abscesses in a cat following bite wounds from a dog. J Vet Diagn Invest 1995;7:154-156.
Yager JA, et al. Streptococcal necrotizing fasciitis and toxic shock syndrome in dogs. Proc 13th Am Acad Vet Dermatol / Am Coll Vet Dermatol Mtg 1997;122-123.
Cutaneous bacterial granulomas
A wide variety of bacteria are capable of producing granulomatous inflammation of the skin. The organisms are frequently of low virulence and are introduced by traumatic implantation. These infections are typically slowly progressive and produce cutaneous or subcutaneous nodules. Inflammation is nodular or diffuse, granulomatous, or pyogranulomatous, and involves the dermis, panniculus, or both. Diagnosis commonly requires special stains, such as tissue Gram stain and routine acid-fast (Ziehl-Neelsen) or modified acid-fast (Fite-Faraco) stains. Staining frozen sections of formalin-fixed tissue may be necessary to demonstrate the bacteria in some atypical mycobacterial infections. Organisms are so infrequent in some cases that confirmation of the bacterial etiology cannot be made histologically and depends instead on cultural isolation of the agent or PCR testing.
Actinomycosis and nocardiosis
Actinomycosis and nocardiosis are uncommon subacute-to-chronic opportunistic cutaneous, pulmonary, and disseminated infections that develop secondary to wound contamination, inhalation, or ingestion. The diseases are discussed together because of their clinical and histologic similarities. Actinomyces and Nocardia are the most common actinomycetes, so-called higher bacteria, which cause disease, but occasional reports of infections in animals by other actinomycetes include Streptomyces and Actinomadura. The infections occur sporadically and are worldwide in distribution. They are not considered of public health significance.
Actinomyces spp. are gram-positive, non–acid-fast, filamentous anaerobic or microaerophilic rods that are commensal inhabitants of the oral cavity, intestine, and upper respiratory tract. Infection is usually secondary to penetrating wounds of the oral mucosa and skin. Cutaneous actinomycosis occurs in cattle, dogs, horses, camelids, goats, pigs, and cats. In cattle, lesions are most commonly on the mandible and maxilla (lumpy jaw) and are most commonly caused by A. bovis. These are firm, variably painful, swellings due to osteomyelitis, with extension into the skin resulting in nodules, abscesses, and draining tracts (Fig. 6-92A ). Osteomyelitis caused by actinomycosis has also been described in dogs, camelids, goats, and a horse. Actinomycosis is rare in horses but has been associated with mandibular lymphadenitis and abscesses, fistulous withers, and poll evil. Hunting or field dogs in warm climates are most commonly affected. It can take months to years for signs to develop after injury. Lesions in dogs and cats are usually tender, subcutaneous, may or may not have draining tracts, and are most common on the head or neck, thoracic, paralumbar, or abdominal regions. In pigs, nodules are most common in the udder and ventral abdomen. In goats, they have been described in the leg and shoulder.
Figure 6-92.

Actinomyces bovis. A. Firm swelling with alopecia and crusting over the mandible in a cow (lumpy jaw).
(Courtesy J.M. Nicol.)
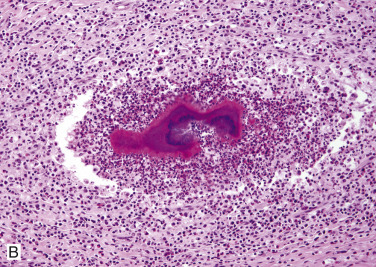
B. Clusters of filamentous organisms surrounded by eosinophilic Splendore-Hoeppli material forming a “sulfur granule.”
Nocardia spp. are ubiquitous saprophytes occurring in soil, straw, grasses, decaying vegetable matter, and water. Unlike Actinomyces spp., they are not part of the normal flora of mammals. They are opportunistic pathogens that cause infection by wound contamination, inhalation, or ingestion, particularly in immunocompromised animals. Several cases have been reported in dogs receiving immunomodulatory therapy for atopic dermatitis. Nocardia spp. are aerobic, gram-positive, branching filamentous organisms that are variably acid fast. Pathogenic Nocardia spp. are facultative intracellular bacteria. Major virulence factors are the complex cell wall lipids and resistance to phagocytosis. Nocardia spp. also have the ability to invade blood vessels, leading to vascular necrosis and ischemia. Cutaneous nocardiosis is reported most frequently in cats, dogs, horses, and cattle, with very rare occurrence in goats. In cattle, Nocardia spp. are more commonly associated with mastitis. There are >30 named Nocardia spp., and different species are correlated with differences in disease features and pathogenicity. The most commonly isolated organisms are Nocardia asteroides complex types I-VI, which include N. nova, N. farcinica, N. brasiliensis, and N. otitidis-caviarum.
The gross lesions of actinomycosis and nocardiosis are usually indistinguishable. In cats, nocardia panniculitis is clinically indistinguishable from panniculitis caused by rapidly growing mycobacteria. Lesions consist of abscesses, cellulitis, ulcerated nodules, draining tracts, and dense fibrous masses. When the triad of clinical signs consisting of tumefaction, draining tracts, and tissue grains is present, the lesion can be termed an actinomycotic mycetoma. Lesions progress slowly by local extension. They occur most commonly on the head, neck, and extremities. Pleural and retroperitoneal infections may extend to involve the subcutaneous tissues of the lateral thoracic wall and flank area, respectively. The exudate is variable and ranges from thin serosanguineous to thick purulohemorrhagic. It may be odorless or foul smelling and contain white, yellow, tan, or gray “sulfur granules.” Sulfur granules are more common in actinomycosis than in nocardiosis. Regional lymphadenopathy frequently accompanies skin lesions. Mandibular and maxillary osteomyelitis may occur in dogs and cats.
Microscopically, actinomycosis and nocardiosis are characterized by pyogranulomatous dermatitis and panniculitis. The epidermis is variably acanthotic and may be ulcerated. The dermis and subcutis contain central accumulations of neutrophils surrounded by a wall of epithelioid macrophages and variable numbers of multinucleated giant cells. Necrosis may be prominent within the central abscess. The pyogranulomas are separated by granulation tissue or dense fibrous connective tissue containing lymphocytes and plasma cells. Fibrosis tends to be more common and severe in actinomycosis than in nocardiosis. Organized masses, measuring 30-3,000 µm or more in diameter, of basophilic- or amphophilic-staining organisms, may be seen in the centers of the abscesses (Fig. 6-92B). They are commonly bordered by a clubbed corona of brightly eosinophilic Splendore-Hoeppli material. These structures correspond to the sulfur granules seen grossly in the exudate. Although granule formation is a more common feature of actinomycosis, Nocardia spp. may form granules in cutaneous lesions that are morphologically indistinguishable from those of Actinomyces. In nocardiosis, the bacteria tend to be distributed singly and are more difficult to identify in H&E-stained sections. With Gram stain, the bacteria are evident as delicate, branched, and beaded filaments, from 10-30 µm or more long and 0.5-1.0 µm wide. The beaded appearance is due to alternating gram-positive and gram-negative regions within the filament and is less prominent with Actinomyces than with Nocardia spp. Most Nocardia spp. are at least partially acid fast when using a modified acid-fast stain such as Fite-Faraco stain in tissue sections (Fig. 6-93 ), whereas Actinomyces spp. and other anaerobic actinomycetes are not acid fast. Definitive diagnosis can be made with anaerobic culture for Actinomyces and aerobic culture for Nocardia spp. Diagnosis of specific Nocardia spp. can be made by molecular sequencing of 16S rRNA.
Figure 6-93.
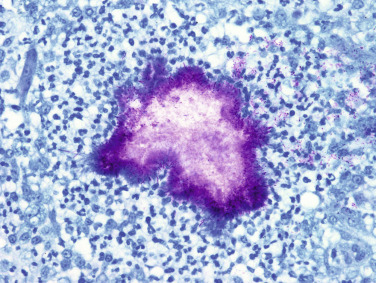
Nocardiosis in a cat. Filamentous organisms are acid fast with Fite-Faraco stain.
Further reading
Fielding CL, et al. Actinomyces species as a cause of abscesses in nine horses. Vet Rec 2008;162:18-20.
Kilic N, Kirkan S. Actinomycosis in a one-humped camel (Camelus dromedarius). J Vet Med 2004;51:363-364.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Malik R. Nocardia infections in cats: a retrospective multi-institutional study of 17 cases. Aust Vet J 2006;84:235-245.
Rodrigues de Farias M, et al. Uncommon mandibular osteomyelitis in a cat caused by Nocardia africana. BMC Vet Res 2012;8:239-243.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Bacterial skin disease. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Siak MK, Burrows AK. Cutaneous nocardiosis in two dogs receiving ciclosporin therapy for the management of canine atopic dermatitis. Vet Dermatol 2013;24:453-456, e102-e103.
Vos NJ. Actinomycosis of the mandible, mimicking a malignancy in a horse. Can Vet J 2007;48:1261-1263.
Mycobacterial infections
Mycobacterial infections are caused by bacteria that belong to the family Mycobacteriaceae, order Actinomycetales. Mycobacterium is a genus comprising morphologically similar, aerobic, gram-positive, acid-fast, non–spore-forming, nonmotile, pleomorphic bacilli with wide variations in host affinity and pathogenic potential. Cutaneous mycobacterial infections are caused by obligate pathogens, such as the tuberculosis groups (Mycobacterium tuberculosis, M. bovis, M. microti,) the leprosy group (M. lepraemurium, M. visibilis), and the opportunistic group considered to be saprophytes or facultative pathogens (subdivided based on growth rate and pigment production). Rapid-growing opportunistic organisms (M. fortuitum, M. smegmatis, M. chelonae, M. abscessus, M. thermoresistible) and slow-growing opportunistic organisms (M. avium-intracellulare complex, M. kansasii, M. ulcerans) are inhabitants of soil, water, and decomposing vegetation, and cutaneous infections are usually acquired via wound contamination or traumatic implantation. Most mycobacteria are intracellular pathogens that are able to persist in tissue by entering macrophages. They survive and replicate in macrophages by inhibiting fusion with lysosomes. Tissue destruction results from persistence of antigen in the tissue and a cell-mediated inflammatory response. Mycobacterial organisms produce granulomatous to pyogranulomatous dermatitis and panniculitis with variable necrosis in many domestic animal species, particularly cats, less frequently dogs and cattle, and rarely in horses and other species. The number of organisms within lesions may be rare to numerous and are best visualized with acid-fast (Ziehl-Neelsen) or modified acid-fast (Fite-Faraco) stains. Because many of these organisms are fastidious and difficult to culture, diagnosis is often made by molecular techniques such as PCR.
Cutaneous infections caused by slow-growing mycobacteria
Tuberculosis.
Cutaneous infections caused by M. tuberculosis and M. bovis (the “bovine bacillus”) are rare but can occur in cattle, dogs, cats, and possibly horses. M. tuberculosis causes tuberculosis in humans. M. bovis, which infects many animals, historically spread to humans when they began drinking milk following cattle domestication. These facultative or obligate intracellular parasites grow best in tissue with high oxygen concentrations, such as lungs. Pulmonary and alimentary infections are more common in cattle, horses, and dogs, but skin infections can develop alone or in combination with disseminated infection. Most cases of tuberculosis in cats are cutaneous, with alimentary and respiratory forms less frequent. M. microti (the “vole bacillus”) causes cutaneous tuberculosis in cats, llamas, and rarely dogs. M. microti infection is believed to be transmitted via direct contact with wild rodents and other small mammals. In cats, most cases of M. microti involve submandibular lymphadenopathy and/or cutaneous lesions that typically affect the “fight and bite” sites: face, legs, and tail base. In some cases, the infection can become disseminated with spread to the lungs. Tuberculous mycobacteria possess mycolate-containing molecules in their cell walls, including the original cord factor trehalose 6,6′-dimycolate. These substances are associated with virulence and the production of characteristic tubercles. To be maintained in nature, they require infection of reservoir mammalian hosts because environmental survival is limited to a maximum of a few weeks on infected fomites.
Cutaneous lesions are single or multiple ulcers, plaques, nodules, or abscesses that exude thick yellow to green fluid. Lesions are most common on the head, neck, and limbs. Patients usually have systemic signs, such as anorexia, weight loss, fever, and localized or generalized lymphadenopathy. Histology of skin lesions shows a nodular-to-diffuse granulomatous to pyogranulomatous dermatitis and panniculitis with central caseous necrosis. There may be small numbers of multinucleated giant cells and mineralization with few to many acid-fast bacteria.
Nontuberculous mycobacteria.
The Mycobacterium avium-intracellulare complex (MAC) includes M. avium subspp. avium, hominissus, and paratuberculosis. These are slow-growing opportunistic organisms that are associated with 2 forms of disease: localized infections of the skin and subcutis in immunocompetent hosts and disseminated disease in immunocompromised animals. Clustering of cases within breeds (Bassett Hounds, Siamese cats, Somali cats, and Abyssinian cats) suggests a genetic predisposition. Affected animals have signs of respiratory and/or gastrointestinal disease, generalized lymphadenopathy, or nodular skin disease with regional lymphadenopathy. Failure to regrow hair after clipping is a unique feature of disseminated MAC infection in Abyssinian cats. Although mycobacteriosis is rare in horses, the most common isolate is M. avium subsp. avium. Lesions in horses range from fairly localized granulomatous dermatitis and panniculitis to exfoliative dermatitis with ulcers, to swollen painful limbs with areas of necrosis, to severe systemic disease. Histologically, there is granulomatous dermatitis and panniculitis without formation of tubercles. Lesions tend to have numerous organisms, and therefore they may be visible in aspirates of masses and various tissues.
Opportunistic cutaneous mycobacterial infections occur in cattle (bovine cutaneous opportunistic mycobacteriosis). Mycobacterium kansasii has been isolated from some of these lesions. Lesions occur as single or multiple nodules 1-8 cm in diameter in the dermis and subcutis. Lesions in cattle are usually unilateral and affect the distal leg. They may spread to the thigh, shoulder, or abdomen. Papules and nodules may be single or multiple, hard or fluctuant, and often occur in chains with intralesional large and palpable (“corded”) lymphatics. Lesions may rupture and discharge thick, yellow to gray pus. Regional lymph nodes are normal, animals are otherwise healthy, and pruritus and pain are absent. Histologically, there is nodular-to-diffuse granulomatous dermatitis and panniculitis with intracellular acid-fast bacilli and variable fibrosis and mineralization. Small lesions may spontaneously resolve, but larger lesions persist.
Mycobacterium ulcerans is the causative agent of Buruli ulcer, a chronic localized infection of the skin and subcutis of humans typically associated with necrotizing skin ulcers with undermined edges. The extensive tissue destruction is associated with mycolactone, a necrotizing cytotoxin and immunosuppressant. The disease is most prevalent in West Africa but also occurs in coastal Victoria and Queensland, Australia. The infection is most commonly reported in marsupial species of Australia but has also been diagnosed in dogs, horses, alpacas, and a cat.
Cutaneous infections caused by rapidly growing mycobacteria (atypical mycobacteriosis).
Rapidly growing mycobacteria (RGM) (formerly Runyon Group IV or atypical mycobacteria) are by definition characterized by the ability to form colonies on solid media within 7 days of incubation. These bacteria are ubiquitous free-living organisms that are usually harmless and commonly found in water, soil, and decaying vegetation. RGM cause opportunistic disease in both healthy and immunocompromised individuals. These organisms are opportunistic environmental saprophytes. Infections are most common in cats, less frequent in dogs and rare in cattle, horses, and other species. Infection has been reported in Australia, the United States, Canada, New Zealand, France, Finland, the Netherlands, Italy, and Switzerland. Three syndromes are recognized: mycobacterial panniculitis involving chronic infection of the subcutis and skin, pyogranulomatous lobar pneumonia, and disseminated systemic disease in immunocompromised individuals. Panniculitis is the most common clinical presentation, especially in Australian cats. Rapidly growing mycobacteria reported to cause cutaneous granulomas in dogs and cats are the Mycobacterium fortuitum group (including M. fortuitum, M. perigrinum, and the third biovariant complex), the Mycobacterium chelonae/abscessus group (including M. chelonae and M. abscessus), the M. smegmatis group (including M. smegmatis sensu stricto, M. goodii, M. wolinskyi), and a variety of other species, including M. phlei and M. thermoresistibile. M. smegmatis is the most commonly isolated organism in Australia; M. fortuitum is most common in the United States. M. smegmatis was isolated from a firm, painful, subcutaneous abscess in the stifle region of a horse.
Lesions can occur anywhere but are most common in the cat in the caudal abdomen, inguinal region, or lumbar region. The causative organisms thrive in fatty tissues. The bacterial cell wall contains glycolipids. It is thought that the lipid may provide nutrients for the organisms to grow and protect them from the immune response. A lipid-rich environment activates virulent mycolic acids in the bacterial cell walls, resulting in granulomatous inflammation. Lesions may or may not be painful, and the regional lymph nodes may not be enlarged. With solitary lesions, systemic illness is rarely observed. In immunocompromised animals, lesions may be widespread, and anorexia, fever, and inappetence may be observed. Lesions generally develop slowly over a period of weeks to months after a history of a penetrating wound or cat fight. Lesions include single or multiple cutaneous and subcutaneous nodules, plaques, purpuric macules, or diffuse swellings. Multiple punctate ulcers or large draining tracts frequently develop and discharge serous, serosanguineous, or purulent exudate that is not usually malodorous (Fig. 6-94 ).
Figure 6-94.

Multiple draining tracts on the ventral abdomen of a cat caused by atypical mycobacteriosis.
(Courtesy M.S. Canfield.)
The microscopic lesions of atypical cutaneous mycobacteriosis are usually multinodular-to-diffuse pyogranulomatous dermatitis and panniculitis, often with circular clear vacuoles surrounded by a rim of neutrophils and a wider outer zone of epithelioid macrophages and variable numbers of neutrophils among more diffuse inflammation composed of macrophages, neutrophils, and lymphoid cells. Multinucleated giant cells are infrequent. Organisms are characteristically rare and difficult to find but are usually located in small clumps within the clear vacuoles. Small numbers of organisms may also be found within macrophages. The bacilli may stain more intensely with modified acid-fast stain than with routine acid-fast stain. In some instances, staining frozen sections of formalin-fixed tissue may result in enhanced acid-fast staining. The organisms are long rods to short filamentous bacilli. Intracellular bacteria tend to be shorter rods. The organisms stain unevenly positive with tissue Gram stains, resulting in a beaded appearance to the bacilli. Because of the scarcity of organisms, any single section may lack organisms, and the diagnosis will be missed. In rare instances, fibroplasia may be marked, and the lesion may be confused for a spindle cell tumor. The specific diagnosis of opportunistic mycobacterial infection requires identification by culture or molecular-based techniques. Because of the scarcity of organisms in some lesions, diagnosis may require multiple attempts at biopsy, culture, and PCR.
Feline leprosy.
Feline leprosy is a rare localized cutaneous infection caused by mycobacteria that are not culturable by standard mycobacteriologic methods. Cases occur worldwide, although certain mycobacterial species have strong geographic predilections. Mycobacterium spp. associated with feline leprosy include M. lepraemurium, M. visibile, M. spp. strain Tarwin, and a novel species found in New Zealand and the East Coast of Australia. M. lepraemurium infections have been reported from the United Kingdom, the Netherlands, France, Greece, Australia, New Zealand, Canada, and the United States. Feline leprosy has no zoonotic potential; however, lesions can be clinically and microscopically indistinguishable from lesions caused by tuberculosis bacteria (M. bovis and M. microti) and members of M. avium complex (MAC).
Young male cats with access to the outdoors are over-represented, and lesions are most common over the head, neck, and limbs. Cats may present with single or multiple cutaneous papules and nodules 2-40 mm in diameter often accompanied by lymphadenopathy. The nodules are generally firm, well circumscribed, alopecic, and some may ulcerate. The location of lesions on cats suggests inoculation of organisms through insect bites, rodent bites, or fight wounds. The development of the disease is due to a complex and incompletely understood interaction between the organism and the immune response of the host. Some organisms (M. spp. strain Tarwin) are associated with localized disease in an immunocompetent host, whereas others (M. visible and the novel Australian East Coast species) are associated with hematogenously disseminated (usually limited to the skin) in the immunodeficient host. Feline leprosy syndrome has a progressive and occasionally aggressive clinical course, depending on the causal species, the size of the infective inoculum, and the immunologic response of the host. In some cases, widespread lesions can develop, and large tuberculoid lesions may ulcerate.
Histologically there are 2 distinct morphologic patterns of inflammation. In lepromatous leprosy, there is nodular-to-diffuse dermal to subcutaneous granulomatous inflammation without necrosis and with large numbers of intracellular acid-fast bacilli. These large granulomas are composed of solid sheets of large, pale, foamy epithelioid macrophages with smaller numbers of multinucleated histiocytic giant cells often containing bacilli. Variable numbers of lymphocytes and plasma cells surround vessels. In some cases, there are scattered neutrophils resembling pyogranulomas. This lepromatous reaction pattern is generally indicative of a poor host immune response. Differential diagnoses for the lepromatous form includes cutaneous xanthoma/xanthogranuloma. Xanthomas are sterile granulomatous lesions composed of foamy macrophages. In tuberculoid leprosy, there are dermal to subcutaneous granulomas with central caseous necrosis surrounded by a zone of lymphocytes. Few to moderate numbers of acid-fast bacilli are generally limited to the areas of necrosis. Variable numbers of lymphocytes surround blood vessels.
In most mycobacterial infections, bacilli are not visible in routine H&E-stained sections. However, M. visible and the novel Australian East Coast species can be seen in H&E-stained sections because they weakly take up the hematoxylin. Regional lymph nodes are characterized by variable architectural disruption by infiltrates of macrophages. Acid-fast bacteria are rare within lymph nodes.
Canine leproid granuloma.
Canine leproid granuloma is a cutaneous to subcutaneous localized nodular granulomatous skin disease that is usually confined to the head, especially pinna, but can occur anywhere. This condition is thought to be caused by a single novel mycobacterium that has not been fully characterized. The condition can be seen worldwide but is most common in Australia and Brazil. Affected dogs are otherwise healthy and generally short-coated breeds, particularly Boxers and their crosses, Doberman Pinschers, and Bullmastiffs. Lesions consist of one or more asymptomatic nodules, 2-5 cm in diameter, confined to the skin and subcutis. Larger lesions may ulcerate (Fig. 6-95 ). Regional lymph nodes are generally not enlarged. The route of infection is unknown, but it is speculated, based on the propensity for pinnal lesions in short-coated breeds, that biting insects or arthropods may introduce the mycobacteria directly into the skin. Lesions within the dermis and subcutis are characterized by nodular-to-diffuse pyogranulomatous inflammation composed of epithelioid macrophages, Langerhans-type giant cells with scattered neutrophils, plasma cells, and small numbers of lymphocytes. The number and morphology of the acid-fast bacilli is highly variable. Bacteria range from long slender filaments in parallel sheaves to short variably beaded bacilli or highly beaded to coccoid forms. Lesions can be disfiguring and cause irritation, especially when they are secondarily infected with bacteria. Lesions may spontaneously resolve over the course of several months, but some persist.
Figure 6-95.

Canine leproid granuloma. Large ulcerated nodule on the pinna of a dog.
(Courtesy M.S. Canfield.)
Miscellaneous mycobacterial infections.
Farcy is a common pyogranulomatous disease of the skin and lymphatics that occurs in cattle in tropical and subtropical climates of Africa, Asia, Latin America, and the Caribbean. Historically it was thought to be caused by Nocardia farcinica, but is now known to be caused by Mycobacterium senegalense and M. farcinogenes. The mycobacterial organisms gain entry via skin wounds, particularly those caused by tick bites. Skin lesions are most common on the head, neck, shoulder, and legs. Firm, painless, slow-growing subcutaneous nodules may ulcerate and discharge thick, stringy, odorless, gray or yellow material. Enlarged “corded” lymphatics and regional lymphadenopathy are present. Histopathology shows nodular-to-diffuse pyogranulomatous dermatitis and panniculitis with intracellular gram-positive acid-fast bacilli. Farcy has a prolonged course and may have widespread organ involvement, emaciation, and death. Economic losses are high in endemic areas.
Further reading
Aranaz A, et al. Use of polymerase chain reaction in the diagnosis of tuberculosis in cats and dogs. Vet Rec 1996;138:276-280.
Couto SS, Artacho CA. Mycobacterium fortuitum pneumonia in a cat and the role of lipid in the pathogenesis of atypical mycobacterial infections. Vet Pathol 2007;44:543-546.
Davies JL, et al. Histological and genotypical characterization of feline cutaneous mycobacteriosis: a retrospective study of formalin-fixed paraffin-embedded tissue. Vet Dermatol 2006;17:155-162.
Foley JE, et al. Clinical, microscopic, and molecular aspects of canine leproid granuloma in the United States. Vet Pathol 2002;39:234-239.
Foster ES, et al. Cutaneous lesion caused by Mycobacterium tuberculosis in a dog. J Am Vet Med Assoc 1986;188:1188-1190.
Fox LE, et al. Disseminated subcutaneous Mycobacterium fortuitum infection in a dog. J Am Vet Med Assoc 1995;206:53-55.
Greene CE, Gunn-Moore DA. Mycobacterial infections. In: Greene CE, editor. Infectious Diseases of the Dog and Cat. 4th ed. St Louis: Elsevier Saunders; 2012. p. 495-521.
Hamid ME. Epidemiology, pathology, immunology and diagnosis of bovine farcy: a review. Prev Vet Med 2012;105:1-9.
Hargis AM, Ginn PE. The integument. In: Zachary JF, McGavin MD, editors. Pathologic Basis of Veterinary Disease. 5th ed. St Louis: Elsevier Mosby; 2012. p. 972-1084.
Hughes MS, et al. Determination of the etiology of presumptive feline leprosy by 16S rRNA gene analysis. J Clin Microbiol 1997;35:2464-2471.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Malik R, et al. Ulcerated and nonulcerated nontuberculous cutaneous mycobacterial granulomas in cats and dogs. Vet Dermatol 2013;24:146-e33.
Miller MA, et al. Inflammatory pseudotumor in a cat with cutaneous mycobacteriosis. Vet Pathol 1999;36:161-163.
Rufenacht S, et al. Mycobacterium microti infection in the cat: a case report, literature review and recent clinical experience. J Fel Med Surg 2011;13:195-204.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Bacterial skin disease. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Stevenson K, et al. Feline skin granuloma associated with Mycobacterium avium. Vet Rec 1998;143:109-110.
Wilson VB, et al. Pathology in practice. J Am Vet Med Assoc 2011;238:171-173.
Bacterial pseudomycetoma
Bacterial pseudomycetoma (botryomycosis, bacterial pseudomycosis, bacterial granuloma) is a chronic infection caused by nonfilamentous bacteria that form colonies visible as tissue grains or granules within lesions. Clinically and histologically, the condition resembles actinomycotic and eumycotic mycetomas. The disease occurs in humans and all domestic animals, including alpacas. Although reported rarely, the condition is probably not uncommon. Lesions are usually localized in the skin and subcutis but may extend deep to involve underlying bone and muscle. Disseminated infection with visceral involvement is rare. Coagulase-positive staphylococci are involved most commonly, but Streptococcus, Pseudomonas, Actinobacillus, Pasteurella, Proteus, Escherichia, Trueperella, and Bibersteinia have also been isolated from lesions. Infection is thought to develop as a result of wound contamination or trauma, such as bites, lacerations, or puncture wounds with foreign bodies.
Lesions typically consist of firm, nonpruritic single or multiple nodules that ulcerate and develop draining tracts. They discharge purulent material that frequently contains white to yellow sand-like grains. The most common lesion sites in horses are limbs, lips, chin, and scrotum. The microscopic lesion is characterized by the presence of basophilic granules within the center of neutrophilic abscesses or pyogranulomas in the dermis or subcutis. These granules correspond to the grains seen grossly in the discharge. They are surrounded and separated by fibrous tissue that may be quite extensive. Plant debris or other foreign material may also be seen in the lesions and indicate the means of infection. The granules consist of compact bacterial colonies that are usually surrounded by amorphous, deeply eosinophilic, radially arranged Splendore-Hoeppli material (Fig. 6-96A ). This material is thought to be antigen-antibody complexes. The bacteria are not well delineated in H&E-stained sections; thus special stains are usually necessary to distinguish the organisms from actinomycotic bacteria and fungi. Individual cocci or bacilli within the granules are seen most clearly in sections stained with tissue Gram or Brown-Brenn stains (Fig. 6-96B). The granulomatous reaction is thought to develop as a result of a delicate balance between the virulence of the organism and the response of the host. The host is able to isolate the infection but is unable to eradicate it. It is speculated that this may be associated with a polysaccharide slime coating produced by the bacteria.
Figure 6-96.
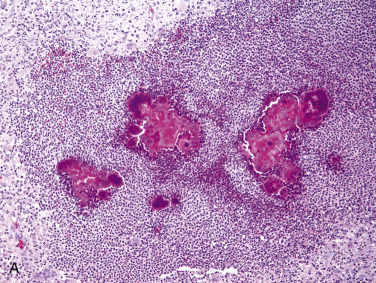
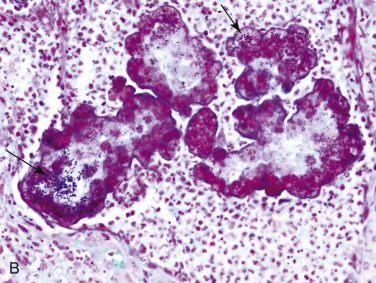
Bacterial pseudomycetoma (botryomycosis). A. Pyogranulomatous dermatitis surrounding multiple angular eosinophilic tissue grains. B. Gram stain reveals gram-positive cocci (arrows).
Further reading
Donovan GA, Gross TL. Cutaneous botryomycosis (bacterial granulomas) in dairy cows caused by Pseudomonas aeruginosa. J Am Vet Med Assoc 1984;184:197-199.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Bacterial skin disease. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Spagnoli S, et al. Subcutaneous botryomycosis due to Bibersteinia trehalosi in a Texas Longhorn steer. Vet Pathol 2012;49:775-778.
Bacterial pododermatitis of horses and ruminants
Proliferative pododermatitis (equine canker)
Equine hoof canker is a destructive painful chronic hypertrophic pododermatitis of the frog, sole, and hoof wall in equids. The condition can affect one or more feet and occur in all breeds, although it is more common in draft breeds. A moist and softer hoof horn may account for the higher occurrence of the disease in these breeds. The cause is unknown; however, the condition has been associated with the presence of a variety of gram-positive and gram-negative bacteria, including Bacteroides spp. and Fusobacterium necrophorum. Spirochetes identified as Treponema spp. have been isolated in some cases. Recent research suggests that bovine papillomavirus 1 and 2 may be involved in the pathogenesis of this condition. Humid environment and poor sanitation and hoof care may be contributing factors; however, the condition also occurs in well-cared-for horses.
Grossly, early lesions consist of focal pink raised tissue on the frog, resembling granulation tissue. This is surrounded by a gray to brown zone that will progress to excessive soft white filiform papillomatous proliferations associated with foul-smelling caseous white exudate. Histologically, the lesions are characterized by marked papillary epidermal hyperplasia with hyperkeratosis and radiating bands of neutrophilic inflammation in the epidermis. There may be marked intracellular edema of the stratum spinosum. There often is superficial interstitial neutrophilic and lymphoplasmacytic dermatitis.
Necrotizing pododermatitis (equine thrush)
Necrotizing pododermatitis is a painful necrotizing condition of the frog and central and lateral sulci of the hoof caused by Fusobacterium necrophorum. The condition can affect all hooves but is most common in the hindfeet. Wet humid conditions allow for softening of the frog and bacterial colonization. F. necrophorum produces leukotoxin as the major virulence factor. Grossly, lesions consist of softening of the frog with black discoloration and a very foul odor. Over time deeper tissues become involved, and there is foul-smelling black exudate with loss of frog tissue. Histologically, the lesions are characterized by necrosis and suppurative inflammation of the frog epithelium and sometimes deeper tissues.
Necrobacillosis of cattle
Necrobacillosis of cattle has a similar etiology and pathogenesis as equine thrush. Trauma to the interdigital skin leads to invasion and colonization by F. necrophorum and Prevotella melaninogenica, and subsequent lameness. Grossly, lesions are characterized by interdigital dermatitis and cellulitis with fissures and necrosis. In severe cases, necrosis and inflammation can extend to deeper structures, such as tendons, bones, and joints. Cutaneous infection with F. necrophorum can occur in other body sites of cattle (especially axillae, groin, and udder). Infection is associated with necrosis, ulceration, crusting, foul odor, and variable systemic signs.
Necrobacillosis of pigs
In pigs, cutaneous infections with F. necrophorum occur especially on the lips, cheeks, legs, and teats.
Necrobacillosis of sheep
In sheep, necrobacillosis includes both interdigital dermatitis and foot abscesses. F. necrophorum and Trueperella pyogenes may be isolated. Foot abscesses occur more in heavy adult sheep during the wet season and include heel and toe abscesses.
Contagious footrot
Footrot is a highly contagious bacterial infection of the digits of sheep, cattle, and goats with worldwide distribution. It has also been reported in pigs. The multistrain, gram-negative, slow-growing obligate anaerobe Dichelobacter nodosus is the essential causal pathogen, with F. necrophorum playing an important synergistic role in infection.
The pathogenesis of footrot is complex and has been studied most extensively in sheep. The disease is initiated by maceration of the interdigital skin brought about by wet conditions along with minor wounds and abrasions. The damaged epidermis then becomes colonized by F. necrophorum, aerobic diphtheroids, coliforms, and other common bacteria originating from the soil, skin, and feces. Footrot develops if the dermatitis is subsequently complicated by infection with D. nodosus. The bacterium is an obligate parasite of the ruminant hoof, and carrier animals serve as the source for uninfected stock. Transmission of infection requires adequate moisture and a mean ambient temperature >10° C. Direct contact between susceptible and infected sheep is not required for transmission of infection. Contact with contaminated substrate for <1 hour has been shown to be adequate for transmission, and outbreaks have been associated with contact with environment contaminated by affected animals as long as 4 days previously. D. nodosus produces a variety of extracellular proteases (the major one is AprV5) that are thought to digest the horn and allow bacterial invasion of the epidermal matrix of the horn. It also produces a heat-stable soluble factor (AprV2) that enhances the growth and invasiveness of F. necrophorum. Type IV fimbriae promote close contact between D. nodosus and host cells and allow the bacteria to translocate to a more anaerobic environment that is necessary for bacterial growth and protease production. F. necrophorum produces a leukocidal exotoxin that reduces phagocytosis. The separation of horn is caused by lysis of the epidermal matrix as a result of the local inflammatory response rather than from direct bacterial attack. T. pyogenes and other aerobic bacteria are usually located superficially in the lesion, where they remove oxygen, destroy hydrogen peroxide, and create the anaerobic environment necessary for the growth of the 2 anaerobic pathogens.
The severity of ovine footrot can vary from benign to a virulent form. Benign footrot, also called foot-scald, is a milder, less persistent form of the condition. It is typically characterized by moderate interdigital dermatitis that causes mild lameness and minimal production loss. The benign form has a greater propensity for self-cure. Virulence of D. nodosus varies widely from strain to strain. Virulent strains of the bacterium produce more extracellular proteases, including elastase, and proteases from virulent strains tend to be more thermostable than those from benign strains. The virulent form of footrot in sheep is the serious, persistent form of the disease characterized by severe necrotic damage to the hoof and extensive separation of hoof horn in more than one foot in a high percentage of the sheep. The infection may persist for more than 1 year if not treated, and chronically infected sheep may die of emaciation as a result of severe pain and lameness. Affected animals are also predisposed to fly strike.
Footrot in sheep develops ~10-20 days after exposure and begins as interdigital dermatitis in the axial bulbar notch. At this early stage, the interdigital skin is pale, swollen, and moist. Inflammation progressively extends forward and caudad around the bulb of the heel. Separation of the horn usually occurs 7 days later, beginning at the skin-horn junction and spreading to the bulb and sole. The animal is severely lame at this stage. From the sole, the process spreads to the hoof wall to involve the axial and abaxial surfaces of the digits. Exudation is minimal and consists of a small amount of gray, greasy malodorous material in the cleft beneath the horn. Because the infection does not destroy the germinative layers of the horn, new horn is continually being regenerated but is rapidly destroyed as long as the infection continues. Chronically infected hooves become long and misshapen.
Benign footrot is indistinguishable from the early stages of virulent footrot. However, in benign footrot, the erosions usually remain confined to the caudal aspect of the interdigital cleft. Occasionally, there is separation of the soft horn of the heel and caudal portion of the sole, but there is no separation of the hard horn. Affected sheep may appear normal or exhibit mild, temporary lameness. The effect of benign footrot on production is minimal.
Diagnosis of footrot in sheep is based on clinical signs, demonstration of D. nodosus in smears from lesional material, and culture and biochemical characterization of isolates to identify antigenic and virulence variants. Because the organism is slow to grow, culture and biochemical testing is time consuming and may require 10-14 days.
Footrot of cattle and goats is typically a less severe disease and resembles the benign form of footrot of sheep. Infection with D. nodosus is more common than is clinical disease. Direct transmission can occur between sheep and goats in the same environment, but this is less common in goats. The lesions in goats tend to stay confined to the interdigital skin. Under-running lesions are not common in goats and are usually restricted to a portion of the soft horn. D. nodosus isolates from cattle with footrot tend to be relatively benign strains. Footrot in cattle usually begins at the caudal aspect of the interdigital space, spreads laterally on the bulbs of the heels, and eventually involves the entire interdigital space. Lesions usually remain confined to the interdigital skin, which may be eroded, ulcerated, or become deeply fissured. The fissures are covered with necrotic material with a characteristic fetid odor. Lesions may extend to the heels, and mild separation of the soft horn may develop. Extensive undermining of the horn, as occurs in sheep, does not typically occur in cattle. Affected animals stand on their toes. In rare severe cases, fever, anorexia, recumbency, and decreased milk production may develop.
Contagious ovine digital dermatitis
Contagious ovine digital dermatitis (CODD) is a condition of the ovine hoof reported in the United Kingdom and Ireland. Initially, this condition was thought to be a severe form of virulent footrot (VFR). Features that distinguish this condition from VFR are the acute severe nature, lesion distribution, and poor response to conventional therapy and vaccination. The cause of this condition is unknown; however, several studies have implicated Treponema as likely playing a role in the pathogenesis. Affected sheep have acute severe lameness. Grossly, lesions are characterized by coronary band ulceration with progression to the abaxial wall lining the hoof, with hoof wall loss in severe cases. Interdigital lesions are not reported, whereas lesions of VFR affect the heel and interdigital region.
Papillomatous digital dermatitis
Papillomatous digital dermatitis (PDD) is a painful, contagious dermatitis of the feet of cattle that occurs worldwide. The condition is also called footwarts and hairy heelwarts, and clinically and histologically, it appears to be the same disease as digital dermatitis, interdigital papillomatosis, verrucose dermatitis, and digital papillomatosis. Papillomatous digital dermatitis is economically important because it frequently causes moderate to severe lameness that results in weight loss, decreased milk production, and poor reproductive performance.
The vast majority of cases are in dairy cows, but it has also been reported in beef cattle. Although the disease occurs in all ages, the highest incidence appears to be in replacement heifers. The pathogenesis of papillomatous digital dermatitis is unknown; however, it is speculated that noninfectious skin lesions lead to a keratinization defect allowing for a suitable growth medium for bacteria. Because Dichelobacter nodosus has been isolated in many cases, some believe that this bacterium may be a first invader, and proteolytic enzymes of D. nodosus allow secondary invasion by various phylotypes of Treponema spp. Proliferation of various treponemes then leads to the proliferative lesions of PDD. It is generally thought that more than one treponemal species is involved in this multifactorial disease. The condition has been compared to chronic periodontitis in humans because both are tissue-destructive diseases with multibacterial etiology in which spirochetes appear to be predominant. The condition is also usually associated with management conditions in which the feet of cattle remain wet for prolonged periods. Some research has indicated that there is upregulation of interleukin-8 (IL-8) by keratinocytes. This may explain the epidermal hyperplasia in these lesions because IL-8 is known to have a stimulatory effect on the migration and proliferation of keratinocytes. IL-8 also plays a key role in the recruitment of neutrophils, which are common in the epidermis of these lesions.
Papillomatous digital dermatitis most commonly affects the skin proximal and adjacent to the interdigital space at the back of the hindfeet (Fig. 6-97 ). The front feet are less frequently involved, and usually only one foot is affected. The cranial aspect of the foot and the interdigital skin are rarely involved. Lesions are painful, forcing the animal to shift its weight to the toe of the foot and resulting in clubbing of the affected foot and atrophy of the bulbs of the heels. Early lesions are well circumscribed, round to oval, red plaques up to 6 cm in diameter with a moist granular surface prone to bleeding and with a very strong, pungent odor. They are partially to completely alopecic and may be bordered by hypertrophied hairs 2-3 times longer than normal. The lesions become progressively more proliferative and less painful with time. Mature lesions are irregular wart-like growths or filamentous papillae that measure 0.5-1.0 mm in diameter, 1 mm to 3 cm in length, and are pale yellow, gray, or brown.
Figure 6-97.

Papillomatous digital dermatitis. Interdigital wart-like growth in a cow.
(Courtesy V. Serre.)
The early microscopic changes of papillomatous digital dermatitis consist of mild epidermal hyperplasia with foci of erosion, necrosis, marked intracellular edema, and microabscesses. The basal layer exhibits an increased mitotic index. The dermis contains minimal perivascular inflammation. Mixed bacteria may be present in the outer necrotic debris, but only spirochetes are present in the deeper viable epidermis. Two morphologically distinct spirochetes have been demonstrated to be in large numbers in early lesions. One is a long thin type with few twists, and the other is a short, thick spirochete with many twists. The spirochetes are oriented perpendicular to the epidermis and appear to invade the keratinocytes. The older lesions are composed of frond-like projections or plaques of markedly hyperplastic epidermis with parakeratotic hyperkeratosis. Foci of necrosis and hemorrhage, marked intracellular edema, and aggregates of neutrophils are scattered throughout the hyperplastic epidermis. At this later stage, inflammation is more intense in the dermis, and plasma cells may be numerous.
Further reading
Bennett G, et al. Dichelobacter nodosus, Fusobacterium necrophorum and the epidemiology of footrot. Anaerobe 2009;15:173-176.
Brandt S, et al. Consistent detection of bovine papillomavirus in lesions, intact skin and peripheral blood mononuclear cells of horses affected by hoof canker. Equine Vet J 2011;43:202-209.
Ghimire SC, et al. Transmission of virulent footrot between sheep and goats. Aust Vet J 1999;77:450-453.
Hargis AM, Ginn PE. The integument. In: Zachary JF, McGavin MD, editors. Pathologic Basis of Veterinary Disease. 5th ed. St Louis: Elsevier Mosby; 2012. p. 972-1084.
Kennan RM, et al. The pathogenesis of ovine footrot. Vet Microbiol 2011;153:59-66.
Moe KK, et al. Detection of treponemes in canker lesions of horses by 16S rRNA clonal sequencing analysis. J Vet Med Sci 2010;72:235-239.
Nagamine CM, et al. Proliferative pododermatitis (canker) with intralesional spirochetes in three horses. J Vet Diagn Invest 2005;17:269-271.
Naylor RD, et al. Isolation of spirochaetes from an incident of severe virulent ovine footrot. Vet Rec 1998;143:690-691.
Petrov KK, Dicks LM. Fusobacterium necrophorum, and not Dichelobacter nodosus, is associated with equine thrush. Vet Microbiol 2013;161:350-352.
Piriz S, et al. Bacteriological study of footrot in pigs: a preliminary note. Vet Rec 1996;139:17-19.
Rasmussen M, et al. Bovine digital dermatitis: possible pathogenic consortium consisting of Dichelobacter nodosus and multiple Treponema species. Vet Microbiol 2012;160:151-161.
Read DH, Walker RL. Papillomatous digital dermatitis (footwarts) in California dairy cattle: clinical and gross pathologic findings. J Vet Diagn Invest 1998;10:67-76.
Refaai W, et al. Digital dermatitis in cattle is associated with an excessive innate immune response triggered by the keratinocytes. BMC Vet Res 2013;9:193-199.
Rogdo T, et al. Possible cross-infection of Dichelobacter nodosus between co-grazing sheep and cattle. Acta Vet Scand 2012;54:19-26.
Sayers G, et al. Identification of spirochetes associated with contagious ovine digital dermatitis. J Clin Microbiol 2009;47:1199-1201.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Sullivan LE, et al. Digital dermatitis in beef cattle. Vet Rec 2013;173:582.
Trott DJ, et al. Characterization of Treponema phagedenis-like spirochetes isolated from papillomatous digital dermatitis lesions in dairy cattle. J Clin Microbiol 2003;41:2522-2529.
Zhou H, et al. Variation in Fusobacterium necrophorum strains present on the hooves of footrot infected sheep, goats and cattle. Vet Microbiol 2009;135:363-367.
Porcine ear necrosis syndrome
Porcine ear necrosis syndrome (PENS, ulcerative spirochetosis of the ear) is a condition of 8-9 week-old pigs (weaners). The pathogenesis is uncertain, but spirochetes are often isolated from these lesions. In one study, some isolates were identified as Treponema spp. Staphylococcus hyicus, β-hemolytic streptococci, and Trueperella pyogenes have also been isolated from these lesions but are thought to be secondary invaders. In another study, in addition to many cases with Staphylococcus and Streptococcus isolated, 7 piglets were positive for porcine reproductive and respiratory syndrome virus, one was positive for Mycoplasma, one had antibodies to Sarcoptes scabiei var. suis, and in 15 samples, no infectious agents were detected. Mycotoxins were detected in some of the feed samples. These results suggest that PENS is multifactorial with no one triggering factor.
Grossly, lesions begin as bilateral small erythematous areas at the base of the pinnae that progress to necrosis and can involve the entire length of the margin of the pinna. The pinnae are bilaterally thickened and may be discolored gray, red, or black. The lesions are covered by thick flat crusts. Histologically, there is vasculitis of the arterioles and venules characterized by hyaline degeneration, medial hypertrophy, and thrombosis, with suppurative dermatitis, epidermal hyperplasia, hyperkeratosis, ulcerations, and crusts. Some lesions may be granulomatous. Spirochetes can be seen with silver stains (modified Steiner) at the junction of granulation tissue and necrosis in some cases. Coccoid or coccobacilli bacteria are frequently seen on the surface in early lesions and in the dermis in chronic lesions. Differential diagnoses for pinnal necrosis in pigs are ear biting, erysipelas, and septicemia.
Further reading
Pringle M, et al. Isolation of spirochetes of genus Treponema from pigs with ear necrosis. Vet Microbiol 2009;139:279-283.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Weissenbacher-Lang C, et al. Porcine ear necrosis syndrome: a preliminary investigation of putative infectious agents in piglets and mycotoxins in feed. Vet J 2012;194:392-397.
Skin lesions in systemic bacterial disease
Skin lesions may develop during the course of systemic bacterial infection. They frequently arise as a result of vasculitis and/or thrombosis. This occurs most commonly in pigs. Swine erysipelas is caused by Erysipelothrix rhusiopathiae, a facultative, non–spore-forming, small, gram-positive bacillus. Pigs 3 months to 3 years of age are most commonly affected. Swine erysipelas is seen in 3 forms: acute, subacute, and chronic.
-
•
Acute erysipelas is characterized by general signs of septicemia and sudden death. There is depression, anorexia, lameness, and blue-to-purple discoloration of the skin, especially the abdomen, pinnae, and legs. Pink to red macules and papules may be seen.
-
•
In the subacute form, animals do not appear sick and have erythematous papules and wheals that enlarge to form square, rectangular, or rhomboid plaques (“diamond skin disease”) (Fig. 6-98 ).
-
•
In the chronic form, there is necrosis and sloughing of the plaques, resulting in black, dry, firm areas of skin that peel away to reveal ulcers. Distal extremities may slough.
Figure 6-98.

Linear, round, and diamond skin lesions in Erysipelothrix rhusiopathiae infection in a pig.
(Courtesy L.L. Pittman.)
Microscopic findings include marked dermal congestion, neutrophilic vasculitis, cutaneous necrosis, and suppurative hydradenitis. Erysipelas is a zoonosis and is of great economic importance in the swine industry because multiple animals are usually affected. Various gram-negative septicemias, in particular septicemic salmonellosis caused by S. choleraesuis, may produce blue-purple discoloration of the skin of the ears, ventral abdomen, snout, and tail, primarily as a result of endotoxin-induced venous thrombosis. Pasteurella multocida may cause similar skin lesions in pigs. Edema disease, caused by a hemolytic Escherichia coli, may be associated with subcutaneous edema secondary to vascular hyaline degeneration, fibrinoid necrosis, and mural edema. Shiga toxin 2e (verotoxin 2e) damages the endothelium and tunica media of vessels.
Skin lesions occur less commonly in other domestic species with systemic bacterial infection. Salmonella enterica ser. Dublin infections in cattle may produce gangrene of distal extremities, tail, and pinnae as a consequence of vascular thrombosis. Cutaneous salmonellosis secondary to septicemia has also been described in horses.
Cutaneous lesions are uncommon in dogs with systemic infections. Rocky Mountain spotted fever, caused by Rickettsia rickettsii, is most often associated with skin lesions. This organism is transmitted by ticks, Dermacentor andersoni and Dermacentor variabilis. Cutaneous lesions consist of petechiae, edema, necrosis, and ulceration as a result of direct endothelial cell damage and vasculitis. Acral dermal necrosis occurs rarely. Dogs may also have ocular, genital, and oral lesions.
Bartonella
Bartonella spp. are highly fastidious gram-negative intracellular bacterial pathogens that infect erythrocytes, endothelial cells, and macrophages. There are at least 22 species and subspecies, and each is highly adapted to preferential mammalian reservoir hosts in which they cause a long-lasting intraerythrocytic bacteremia. Infection is transmitted via various blood-sucking arthropods. Bartonella infection has been described in humans, dogs, and cattle, and endocarditis is most common. Various cutaneous manifestations have been rarely reported in dogs. Three dogs were reported to have pyogranulomatous meningoradiculoneuritis and multiple pyogranulomatous nodular dermatitis or panniculitis in association with Bartonella vinsonii subsp. berkhoffi infection. All 3 dogs responded to surgical decompression and appropriate antibiotic therapy. Another dog with α1-proteinase inhibitor deficiency developed multiple subcutaneous nodules consistent with granulomatous panniculitis, polyarthritis, and meningitis in association with Bartonella spp. bacteremia. In these cases, DNA of the organism was found by PCR within the blood but not in the skin lesions.
Several species of Bartonella, including B. vinsonii subsp. berkhoffii and B. henselae, have been shown to cause proliferative vascular diseases in animals. B. vinsonii subsp. berkhoffii induces activation of hypoxia-inducible factor-1 and production of vascular endothelial growth factor. A dog undergoing immunosuppressive therapy for pancytopenia was diagnosed with bacillary angiomatosis caused by B. vinsonii subsp. berkhoffii. This dog developed multiple erythematous, raised round, variably alopecic, papular to nodular lesions, 5-13 mm in diameter, in the skin of the trunk, limbs, face, and footpads. Histologically, the lesions were located in the subcutis and composed of multifocal proliferations of capillaries lined by plump endothelium with areas of fibrinoid degeneration. Capillary clusters were separated by edematous connective tissue and lightly infiltrated by degenerate inflammatory cells, including neutrophils and macrophages. Warthin-Starry silver stain showed large numbers of bacilli consistent with Bartonella. Bacillary angiomatosis has also been described in immunocompromised humans, and in those cases, like this one, bacteria can be seen with silver stains.
Borreliosis
Borreliosis (Lyme disease) is caused by Borrelia burgdorferi, a gram-negative spirochete that is transmitted from small rodents to mammals by Ixodes spp. ticks. The predominant clinical sign in all species is polyarthritis. Borrelia-associated cutaneous pseudolymphoma has been reported in humans and a horse. Cutaneous pseudolymphoma is a benign self-limiting lymphoproliferative condition in the skin causing papular to nodular asymptomatic lesions. The reported horse was a 10-year-old Belgian-Warmblood mare with multiple, 2-7 mm, dermal papules over the right masseter. The lesions were not alopecic, ulcerated, or painful. The lymphatics around the lesions and the right mandibular lymph node were enlarged. Microscopically, there was a dermal infiltrate composed of small mature CD3+ T cells, CD79a+ B cells, and small numbers of eosinophils with aggregates of CD79a+ B cells and clusters of larger blastic CD3+ T cells around capillaries with hyperplastic endothelial cells (postcapillary high-endothelial venule). B. burgdorferi was detected in the horse's serum by ELISA and Western blot and in the skin biopsy by PCR.
In humans, a characteristic expanding ring-like macule or papule (erythema chronicum migrans) is the most common cutaneous lesion associated with Lyme borreliosis and develops 1-2 weeks post–tick bite. This lesion has been reported in dogs, although no histologic studies were performed, and this lesion has not been experimentally reproduced in dogs. Rarely, seropositive dogs are described to have urticaria, rash, or moist dermatitis. Tetracycline-responsive pyotraumatic dermatitis has been described in seropositive dogs.
Further reading
Beerlage C, et al. Bartonella vinsonii subsp. berkhoffii and Bartonella henselae as potential causes of proliferative vascular diseases in animals. Med Microbiol Immunol 2012;201:319-326.
Cross JR, et al. Bartonella-associated meningoradiculoneuritis and dermatitis or panniculitis in 3 dogs. J Vet Intern Med 2008;22:674-678.
Hargis AM, Ginn PE. The integument. In: Zachary JF, McGavin MD, editors. Pathologic Basis of Veterinary Disease. 5th ed. St Louis: Elsevier Mosby; 2012. p. 972-1084.
Lloyd D. Bacterial skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Mellor PJ, et al. Alpha 1-proteinase inhibitor deficiency and Bartonella infection in association with panniculitis, polyarthritis, and meningitis in a dog. J Vet Intern Med 2006;20:1023-1028.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Bacterial skin disease. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 130-170.
Sears KP, et al. A case of Borrelia-associated cutaneous pseudolymphoma in a horse. Vet Dermatol 2011;23:153-156.
Wang Q, et al. Erysipelothrix rhusiopathiae. Vet Microbiol 2010;140:405-417.
Yager JA, et al. Bacillary angiomatosis in an immunosuppressed dog. Vet Dermatol 2010;21:420-428.
Fungal Diseases of Skin
Fungi are ubiquitous in the environment, but of the thousands present, only a few are capable of causing infection in animals. The vast majority of fungi in nature are incapable of causing infection because they are unable to breach 2 major physiologic barriers to fungal growth in tissue: temperature and oxidation-reduction potential. Many fungi have an optimal growth range considerably below the temperature of the body and cannot survive the relatively high temperature of the body. Other fungi are thermotolerant. The propensity of fungi to cause infection is dependent not only on their ability to adapt to the tissue environment and temperature, but also to withstand the lytic activity of the host's cellular defenses. Some fungi are true pathogens with the ability to cause disease in normal individuals, whereas many more organisms are opportunistic pathogens that infect individuals who have become immunologically or otherwise compromised and are unable to resist and suppress the fungal invasion. Immunocompromise by various infectious agents, as well as pharmacologic immunosuppression, are important predisposing factors in development of some fungal infections. However, many mycotic infections occur in individuals without any clinically overt immune impairment. These infections are likely a consequence of an overwhelming exposure to the infectious propagules or mild immunologic defects that are not readily apparent. Mycotic infections are commonly divided into 3 categories: cutaneous, subcutaneous, and systemic.
-
•
Cutaneous mycoses are the most common fungal diseases in veterinary medicine. The infections are generally confined to the nonliving cornified layers of the skin, hair, and claws.
-
•
Subcutaneous mycoses are fungal infections that involve the skin and subcutaneous tissues. They are caused by a wide variety of saprophytic fungi that gain entry by traumatic implantation. Infection is a very indolent process and usually remains localized to the site of entry with slow spread to surrounding tissue.
-
•
Systemic mycoses are infections of the internal organs. Cutaneous involvement usually occurs as a result of hematogenous dissemination. Skin lesions from direct cutaneous inoculation in systemic mycoses are rare. These infections include blastomycosis, cryptococcosis, coccidioidomycosis, and histoplasmosis. Occasionally, the diagnosis of a systemic fungal infection/mycosis, particularly blastomycosis in dogs and cryptococcosis in cats, is made by biopsy of skin lesions.
Histopathology is an important diagnostic tool for fungal infections. It is a relatively rapid and inexpensive means to make a definitive or presumptive diagnosis of mycotic infection. In many cases, fungal infections are mistaken for neoplasms, and the entire lesion is fixed and submitted for histologic examination. Consequently, only fixed tissue is available, and the pathologist has the responsibility for the final diagnosis because the organism cannot be cultured. Some fungal organisms have distinctive enough morphologic features that, if present in sufficient numbers, they can be identified with a high degree of certainty, for instance, Blastomyces, Cryptococcus, and Coccidioides. Other mycotic infections are caused by a variety of fungi that are similar in appearance in tissues and cannot be specifically identified, although the disease can be named, for instance, dermatophytosis, phaeohyphomycosis, and eumycotic mycetoma. In some cases, fungi may be detectable in tissues but may be impossible to identify, and only the conclusion that mycotic infection exists can be made. Although immunofluorescence and immunohistochemical methods for identification of fungi in formalin-fixed, paraffin-embedded tissue sections have been developed, the specific antisera are not readily available, and culture remains the mainstay for identification of fungal pathogens. Some fungi stain with H&E, but many fungi do not stain or stain very poorly with H&E. However, even in these cases, fungal infection can be suspected because of the presence of clear circular or linear structures, representing unstained fungal hyphae, within the lesion. Special fungal stains, such as Gomori methenamine silver (GMS), which stains fungi black, PAS, which stains fungi pink-red, delineate the fungi so that their morphology can be examined. In general, GMS is better for screening tissue because some fungal-like organisms (e.g., Pythium) stain poorly with PAS. Fungal stains may mask the natural color of fungi, however. To determine whether a fungus is pigmented, it can be examined in unstained cleared and mounted sections, or a melanin stain, such as Fontana-Masson, can be applied to the tissue.
Further reading
Chandler FW, et al. A Color Atlas and Text of the Histopathology of Mycotic Diseases. London: Wolfe Medical Publications; 1989.
Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev 2011;24:247-280.
Matsumoto T, et al. Developments in hyalohyphomycosis and phaeohyphomycosis. J Med Vet Mycol 1994;32(Suppl. 1):329-349.
Rippon JW. Medical Mycology. The Pathogenic Fungi and the Pathogenic Actinomycetes. 3rd ed. Philadelphia: WB Saunders; 1988.
Cutaneous fungal infections
Cutaneous mycoses are infections in which the fungal organisms are generally confined to the nonliving keratinized tissues, that is, stratum corneum, hair, claw, and horn. Pathologic changes, which occur in response to the infectious agent and its metabolic products, involve the epidermis and dermis and may vary from minimal to severe and extensive. These infections include candidiasis, Malassezia dermatitis, and dermatophytosis.
Candidiasis
Candidiasis (candidosis, moniliasis, thrush) is a rare opportunistic infection of skin, mucocutaneous junctions, external ear canal, and the claw bed. Candida spp. yeasts are normal inhabitants of the upper respiratory, alimentary, and genital tracts but are not normally present on the skin except at mucocutaneous junctions of body orifices. Factors that alter the superficial keratin barrier (such as maceration, chronic trauma, or burns), upset normal flora (such as prolonged broad spectrum antibiotic therapy), or produce immunosuppression (such as diabetes mellitus, hyperadrenocorticism, neoplasia, viral infections, cytotoxic chemotherapy, or prolonged glucocorticoid treatment) predispose to infection with the organism. Because neutrophils are a major defense mechanism against Candida, prolonged neutropenia renders an individual more susceptible to candidiasis. The other major mechanism for eliminating Candida from the skin surface is T-cell–mediated immunity.
Cutaneous infections have been described in dogs, cats, pigs, horses, goats, and a llama. Lesions are variable and may begin as erythematous papules, pustules, and vesicles, which evolve into crusts and characteristic sharply delineated ulcers with erythematous borders and a malodorous surface with moist gray-white exudate. Chronic lesions consist of thickened alopecic hyperkeratotic skin with prominent folds. Histologic changes include hyperkeratosis, parakeratosis, serocellular crusts, subcorneal or superficial epidermal neutrophilic pustules, and spongiosis. The dermis is edematous and contains a superficial perivascular to interstitial mixed infiltrate. Yeasts, pseudohyphae, and hyphae may be numerous but are best visualized with PAS or GMS stains. Generally, yeasts are most numerous on the surface of the lesions, whereas hyphae and pseudohyphae extend into the epidermis.
Infection with Candida guilliermondii is reported in a horse with multiple firm painful cutaneous nodules. Histologically, there was nodular granulomatous dermatitis with numerous budding 2-6 µm blastoconidia within macrophages and multinucleated histiocytic giant cells.
Further reading
Lamm CG, et al. Pathology in practice. J Am Vet Med Assoc 2009;234:1013-1015.
Lloyd D. Ecology of skin: Balance and disruption. Compend Contin Educ Pract Vet Suppl 1997;19:97-100.
Mueller RS, et al. Cutaneous candidiasis in a dog caused by Candida guilliermondii. Vet Rec 2002;150:728-730.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Fungal skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 171-211.
Malassezia dermatitis
The genus Malassezia consists of at least 13 species of lipophilic yeasts, which are components of the cutaneous microflora of many mammals, including humans. Malassezia pachydermatis is the only species that does not require lipid supplementation during culture in vitro and is thus characterized as lipophilic, non–lipid dependent. All other species are lipid dependent. Of all the species, M. pachydermatis is most commonly associated with skin disease in dogs and cats. It is also the species most commonly isolated from the skin, mucosa, and ear canals of healthy dogs and cats. When associated with skin disease, it is currently believed that Malassezia infection is due to overgrowth of normal flora resulting from disturbances of the normal physical, chemical, or immunologic mechanisms controlling the skin surface microenvironment and host defenses. Virulence factors associated with M. pachydermatis include the production of various hydrolases, including lipases, phospholipases, aspartyl proteases, and acid sphingomyelinases. Isolates of M. pachydermatis have also been shown to form biofilms on surfaces of various materials.
Malassezia dermatitis is most common in dogs. Greater than 70% of dogs have concurrent dermatoses, including allergies, keratinization defects, endocrinopathies, and bacterial pyoderma. Predisposed breeds include West Highland White Terrier, Bassett Hound, American Cocker Spaniel, Shih Tzu, English Setter, Toy and Miniature Poodle, Boxer, Cavalier King Charles Spaniel, Australian and Silky Terriers, German Shepherd dog, and Dachshund. Excessive surface lipid or cerumen, high humidity, or failure of host defense mechanisms to control overgrowth of the yeast may predispose an animal to develop clinical disease. Dogs with Malassezia dermatitis develop high serum titers of specific IgG antibody and exhibit significantly greater skin test reactions in response to intradermal injection of M. pachydermatis extracts than dogs without evidence of Malassezia dermatitis, suggesting that hypersensitivity may be involved in the pathogenesis of clinical disease. Lesions associated with Malassezia dermatitis include erythema, alopecia, greasiness, yellow-gray scaly plaques, lichenification, and hyperpigmentation (Fig. 6-99A ). A rancid offensive odor is typical, and moderate to severe pruritus is a common feature. Lesions may be localized or generalized, and the most common sites include lips, ear canals, axillae, groin, ventral neck, inguinal area, interdigital skin, perianal area, and intertriginous regions. Malassezia paronychia and/or claw infections produce red-brown discoloration of paronychial hairs or claws (Fig. 6-99B). Involvement of one or several of these areas is more common than generalized disease.
Figure 6-99.

Malassezia dermatitis in a dog. A. The skin is erythematous, alopecic, lichenified, hyperpigmented, and covered with some scale.
(Courtesy W.H. Miller.)

B. Red-brown discoloration of claw.
(Courtesy W.H. Miller.)
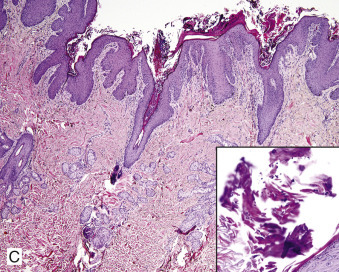
C. Skin biopsy shows irregular epidermal hyperplasia with parakeratotic hyperkeratosis, superficial interstitial dermatitis, and hyperplastic sebaceous glands in disarray. Malassezia spp. yeast can be seen within the surface keratin (see inset).
Malassezia dermatitis in cats is less common and is generally associated with black ceruminous otitis externa, chronic chin acne, facial dermatitis with large dark brown to black scales and follicular casts, with refractory paronychia, or generalized erythematous scaly to waxy dermatitis. Devon Rex and Sphynx cats have been shown to have a higher Malassezia spp. colonization compared to other breeds of cats. Devon Rex cats may be predisposed to greasy seborrheic dermatitis associated with increased Malassezia colonization and paronychia. In cats, Malassezia dermatitis is an opportunistic infection, and it has been associated with localized exfoliative dermatitis, chin acne, idiopathic facial dermatitis of Persian cats, allergic dermatitis, thymoma-associated dermatitis, paraneoplastic alopecia, and in cats with feline leukemia virus and feline immunodeficiency virus infections.
Malassezia dermatitis is uncommon in goats. Poor nutrition and debilitating underlying disease appear to be predisposing factors. Lesions are nonpruritic to mildly pruritic and nonpainful, and are characterized by erythema, hyperpigmentation, scale, greasiness, yellow waxy crusts, and lichenification. Lesions are multifocal, often over the back and trunk, and typically become generalized but tend to spare the head and legs.
Malassezia dermatitis is rarely reported in horses. As in dogs and cats, it is associated with pruritic, greasy to waxy, occasionally foul-smelling dermatitis in intertriginous areas, including axillae, groin, udder, and prepuce. Predisposing conditions include humidity, hormonal alterations, keratinization defects, hypersensitivity disorders, immunosuppressive disease, and immunosuppressive therapy. One horse diagnosed with Malassezia dermatitis had concurrent alopecia areata.
Malassezia otitis externa is common in cattle in South America. There is a ceruminous to suppurative otitis externa caused by predominantly thermotolerant M. sympodialis in the summer and a predominantly less thermotolerant species, M. globosa in the winter.
Histologic features of Malassezia dermatitis of dogs consist of multifocal parakeratotic hyperkeratosis, irregular epidermal hyperplasia, intercellular edema (spongiosis), and lymphocytic and eosinophilic exocytosis (Fig. 6-99C). In dogs, intraepidermal eosinophilic microabscesses, pigmentary incontinence, and subepidermal linear accumulation of mast cells may be seen. There is variable edema and perivascular to interstitial infiltration of mixed cells (lymphocytes, plasma cells, histiocytes, eosinophils) in the superficial dermis. Malassezia organisms are oval to footprint- or peanut-shaped 2 × 4–µm yeasts located in the stratum corneum or in crusts (see Fig. 6-99C inset). They are usually seen in focal aggregates rather than diffusely distributed, and they can best be visualized with PAS or GMS stains. The organism will be missed if the skin surface was scrubbed prior to obtaining the biopsy or if the surface debris is lost during processing. Histologic findings in cats and horses are probably similar, but reports are few. In goats, there tends to be marked surface and follicular orthokeratotic hyperkeratosis and mild lymphocytic perivascular dermatitis. Numerous budding yeasts are seen, which is in contrast to few or none seen in biopsy samples from other species.
Further reading
Ahman SE, et al. Cutaneous carriage of Malassezia species in healthy and seborrhoeic Sphynx cats and a comparison to carriage in Devon Rex cats. J Fel Med Surg 2009;11:970-976.
Bond R, et al. Humoral and cell-mediated responses to Malassezia pachydermatis in healthy dogs and dogs with Malassezia dermatitis. Vet Rec 1998;143:381-384.
Bond R, Lloyd DG. Skin and mucosal populations of Malassezia pachydermatis in healthy and seborrhoeic Basset Hounds. Vet Dermatol 1997;8:101-106.
Cabanes FJ, et al. Two new lipid-dependent Malassezia species from domestic animals. FEMS Yeast Res 2007;7:1064-1076.
Cannizzo FT, et al. Biofilm development by clinical isolates of Malassezia pachydermatis. Med Mycol 2007;45:357-361.
Eguchi-Coe Y, et al. Putative Malassezia dermatitis in six goats. Vet Dermatol 2011;22:497-501.
Forster-Van Hufte MA, et al. Resolution of exfoliative dermatitis and Malassezia pachydermatis overgrowth in a cat after surgical thymoma resection. J Small Anim Pract 1997;38:451-454.
Godfrey DR. A case of feline paraneoplastic alopecia with secondary Malassezia associated dermatitis. J Small Anim Pract 1998;39:394-396.
Kim DY, et al. Diagnostic exercise: severe bilaterally symmetric alopecia in a horse. Vet Pathol 2011;48:1216-1220.
Mauldin EA, et al. Malassezia dermatitis in the dog: a retrospective histopathological and immunopathological study of 86 cases (1990-95). Vet Dermatol 1997;8:191-202.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Morris DO, et al. Type-1 hypersensitivity reactions to Malassezia pachydermatis extracts in atopic dogs. Am J Vet Res 1998;59:836-841.
Nardoni S, et al. Occurrence, distribution and population size of Malassezia pachydermatis on skin and mucosae of atopic dogs. Vet Microbiol 2007;122:172-177.
Ordeix L, et al. Malassezia spp. overgrowth in allergic cats. Vet Dermatol 2007;18:316-323.
Pin D. Seborrhoeic dermatitis in a goat due to Malassezia pachydermatis. Vet Dermatol 2004;15:53-56.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Fungal skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 171-211.
Uzal FA, et al. Malassezia slooffiae-associated dermatitis in a goat. Vet Dermatol 2007;18:348-352.
Volk AV, et al. Malassezia pachydermatis and M. nana predominate amongst the cutaneous mycobiota of Sphynx cats. J Fel Med Surg 2010;12:917-922.
White SD, et al. Malassezia species isolated from the intermammary and preputial fossa area of horses. J Vet Intern Med 2006;20:395-398.
Dermatophytosis
Dermatophytosis (“ringworm”) is a highly contagious, zoonotic, superficial fungal infection generally confined to the keratin layers of the skin, hair, and claws, affecting cats, cattle, horses, dogs, goats, pigs, sheep, and rarely alpacas. In rare instances, deeper tissues are involved. The infection is caused by fungi of the genera Microsporum, Trichophyton, and Epidermophyton, which are cosmopolitan in distribution. They are commonly divided according to the host preference and natural habitat of the fungus.
-
•
Geophilic dermatophytes are normal soil inhabitants. The most common species to infect dogs and cats is Microsporum gypseum.
-
•
Zoophilic dermatophytes (e.g., M. canis, M. equinum, T. equinum) are adapted to living on animals and are rarely found in the soil. They occasionally infect humans.
-
•
Sylvatic dermatophytes (e.g., T. mentagrophytes, M. persicolor) are zoophilic dermatophytes adapted to living on rodents or hedgehogs.
-
•
Anthropophilic dermatophytes (e.g., T. tonsurans, T. rubrum) are primarily adapted to humans and do not survive in the soil. Animals occasionally develop infections with these organisms as a reverse zoonosis from infected humans.
Incidence and prevalence of dermatophytosis vary with individual host factors, health status, climate, season, natural reservoirs, and local environment. Predisposing host factors for dermatophyte infection include young age, stress, poor nutrition, debilitating disease, compromised immune status, and areas of chronically warm moist skin. Environmental factors include hot, humid weather, with wet, poorly ventilated unsanitary conditions, and decreased exposure to sunlight. Transmission of dermatophytes occurs by direct contact with infected animals or indirectly by exposure to infective hair and scales in the environment (contaminated grooming equipment, bedding, saddles, cages, etc.). Hair fragments containing infectious arthrospores are the most effective means of transmission. They can remain infectious for more than 18 months if protected from the deleterious effects of ultraviolet light. This material is the major source of persistent environmental contamination. Certain dermatophytes are associated with specific sources. M. canis, despite its name, is most commonly associated with cats, and the cat is considered the reservoir for this dermatophyte. T. mentagrophytes dermatophytosis is typically acquired from small rodents; infection with M. gypseum is assumed to be acquired from digging or rooting in contaminated soil.
Normal skin is relatively inhospitable to fungal growth because of low moisture conditions, antifungal substances in the surface film, and normal resident flora. Sebum contains fatty acids that are fungistatic and play an important role in resistance to infection. The process by which the stratum corneum (SC) is continually renewed may also present a form of defense against organisms because the process results in continuous shedding of the SC and thus removes infecting organisms with the sloughed keratin. Disruption of the SC, either by microabrasions or maceration, appears to be important in facilitating invasion by the fungus. Fungal cells adhere to keratinocytes and migrate to the follicular orifice. Dermatophytes produce keratinolytic enzymes, endoproteases, and exoproteases, which hydrolyze keratin and enable them to penetrate and invade the hair shaft. They grow downward within the hair shaft toward the hair bulb until they reach the keratogenous zone (Adamson's fringe), where they stop because they cannot grow in viable tissue. Infection continues as long as the downward growth of the fungus is in equilibrium with keratin production; if not, the fungus is sloughed and the hair is cleared of infection. When the hair enters telogen phase, keratin production stops and fungal growth ceases. Hair shafts are weakened as a result of penetration by the fungi, and they become brittle and easily broken.
Dermatophytosis in healthy individuals is usually self-limiting, with lesions resolving in several weeks to 2-3 months. Chronic dermatophyte infections have been reported in dogs. Trichophyton spp. and M. persicolor dermatophyte infections, lasting up to 5 years in some cases, have been described in dogs without any other evidence of immunodeficiency, suggesting that these organisms may produce inhibitory substances that prevent development of an effective immune response and elimination of the organism.
The clinical signs of dermatophytosis are highly variable and depend on the host-fungus interaction. Pruritus varies from absent to severe. Well-adapted species, such as M. canis infection in cats, produce minimal inflammation, whereas less-adapted species, such as the zoophilic dermatophyte M. gypseum, produce more significant inflammation and more prominent lesions. Expanding circular patches of scaling and alopecia or stubbled hairs are considered the classic lesion of dermatophytosis. Follicular papules and pustules, more extensive inflammation caused by furunculosis, and crusting are prominent in some cases. Lesions are typically nonpruritic, but occasionally pruritus is intense. Infection of claws is called onychomycosis and is characterized by misshapen, crumbly or easily broken, and split claws that may be sloughed. Kerions are rapidly developing tender erythematous alopecic nodules that may ulcerate and develop draining tracts. They are usually solitary and most common on the face and forelimbs of dogs that dig in the dirt (Fig. 6-100A ). These lesions result from severe furunculosis producing locally extensive inflammation that may be confused for a tumor. A rare form, the dermatophytic pseudomycetoma seen almost exclusively in Persian cats, occurs as subcutaneous nodules.
Figure 6-100.

Dermatophytosis. A. Kerion on the muzzle of a dog.
(Courtesy W.H. Miller.)
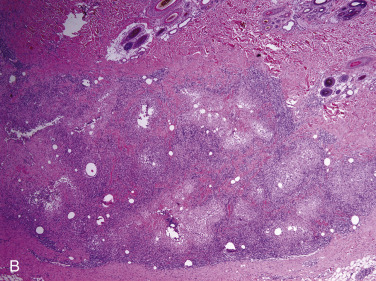
B. Multifocal furunculosis grouped together forming a pyogranulomatous nodular dermatitis.
The microscopic lesions of dermatophytosis are as variable as the clinical lesions. Histopathology is not considered as sensitive as culture for diagnosis, but it can be used to confirm infection when the significance of a cultured organism is in question. It is most useful in the nodular forms, such as kerion and pseudomycetoma, which are frequently negative when superficial material is cultured. Biopsies should be taken within the outer border of expanding alopecia as this is the most active site of infection, and organisms are most likely to be present. In most cases, fungal organisms are evident in H&E-stained sections, but in some instances, fungal stains (PAS, GMS) are necessary to demonstrate infection. Dermatophytes occur as septate hyphae that break up into chains of round to oval arthrospores in the surface and follicular keratin. Hyphae are also usually present in the hair shafts, and arthrospores are formed on the outside of the hairs (ectothrix) or within the hairs (endothrix). In some cases, fungal organisms are present only in the surface keratin (T. mentagrophytes and M. persicolor in dogs); if this material was removed in preparing the skin for obtaining the biopsy or is lost during tissue processing, the diagnosis will be missed. Orthokeratotic and parakeratotic hyperkeratosis is a typical feature of dermatophytosis, and acanthosis is variable, ranging from mild to marked (Fig. 6-101A ). Inflammation may be very mild and consist of low numbers of perivascular and perifollicular lymphocytes and macrophages (Fig. 6-101B). This is the case when infection is caused by a species of dermatophyte that is well adapted to its host. Neutrophilic luminal folliculitis is a common lesion in dermatophytosis and may result in follicular rupture and development of discrete granulomas surrounding fragments of hair at the base of the follicles (Fig. 6-101C). Eosinophils may be numerous in these trichogranulomas. Kerions consist of diffuse pyogranulomatous inflammation in the deep dermis produced by extensive furunculosis (see Fig. 6-100B). This form of inflammation is most commonly caused by poorly adapted organisms, such as the geophilic dermatophyte M. gypseum. Hair fragments containing hyphae and arthrospores are frequently present among the inflammatory cells but may be destroyed by the intense inflammatory reaction. In some cases, the pattern of inflammation may be confused with autoimmune diseases. Lymphocytic lichenoid interface dermatitis, lymphocytic mural folliculitis, and subcorneal pustules containing neutrophils and acantholytic cells have been reported in several cases of dermatophytosis in dogs and horses; however, organisms were evident with fungal stains. The dermatophytic pseudomycetoma is characterized by masses of fungal elements surrounded by granulomatous or pyogranulomatous inflammation in the deep dermis and subcutis.
Figure 6-101.
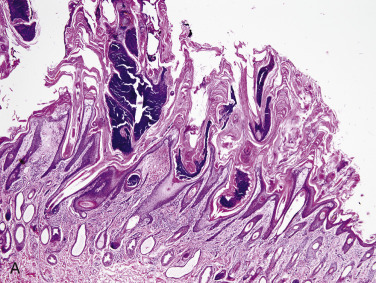
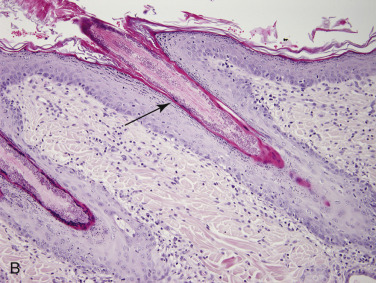
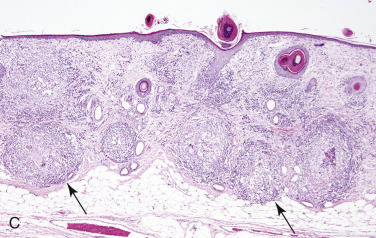
Dermatophytosis histopathology. A. Marked orthokeratotic and parakeratotic hyperkeratosis with suppurative luminal folliculitis in a calf. B. Mild lymphocytic mural folliculitis with intraluminal dermatophytes (arrow) in a dog. C. Multiple trichogranulomas (arrows) in a dog.
Cattle.
Dermatophytosis is common in cattle and is most prevalent in calves. T. verrucosum is the most frequent isolate; others include T. mentagrophytes, T. equinum, M. gypseum, M. nanum, and M. canis. Outbreaks are associated with crowding and confinement indoors during fall and winter. Lesions occur on the neck, head, pinnae, and pelvic area most commonly. The intermandibular space and dewlap are common sites for lesions in bulls. Lesions vary from tufted papules to circular areas of alopecia with variable crusting or scaling (Fig. 6-102 ). In calves, the entire neck may become alopecic, crusty, thickened, and corrugated. Pruritus is rare. The disease may be of some economic significance because of damage to hides or restrictions on showing or marketing of infected animals. In very severe cases, loss of condition and weight loss or decreased milk production may result.
Figure 6-102.
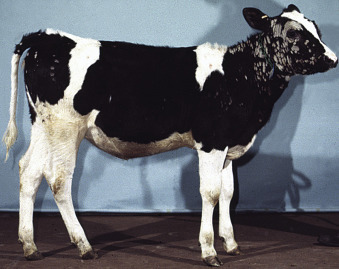
Dermatophytosis in a calf. Annular, thick, gray crusts predominantly on the face and neck.
(Courtesy D.W. Scott.)
Sheep and goats.
Dermatophytosis is common in goats but uncommon in sheep and is most commonly caused by T. verrucosum. Lesions of annular areas of alopecia, scaling, erythema, and yellow crusts are usually on the head, face, pinnae, neck, and limbs in goats. In sheep, T. verrucosum typically affects the haired areas of the head, face, and pinnae, whereas M. canis and M. gypseum are more likely to affect the wooled areas, with lesions characterized by matted wool with brown crusts and exudates. Infection in show lambs in the United States has been most commonly associated with M. gypseum. Pruritus and pain are uncommon.
Pigs.
Dermatophytosis is uncommon in pigs and most commonly caused by M. nanum. T. verrucosum occurs in pigs housed in premises previously occupied by cattle. Infections also are also caused by T. mentagrophytes, M. canis, and M. gypseum. The lesions of M. nanum are especially common on the face, behind the pinnae, and on the trunk, and consist of irregular dark patches with fine brown scales or crusts. Alopecia and pruritus are rare. Lesions may resolve spontaneously or spread slowly to involve extensive areas.
Horses.
Dermatophytosis is common in the horse (girth itch, tinea) and is caused by a variety of organisms but most frequently by T. equinum. Infections with T. mentagrophytes and M. gypseum are also common; T. verrucosum and M. canis infections are less frequent. Outbreaks of dermatophytosis caused by M. gypseum have been associated with periods of humid weather and a high prevalence of mosquitoes and stable flies. In some training establishments, >30% of the horses have ringworm, and the causative agent is M. gypseum. Lesions occur most often in areas in contact with the saddle and tack: face, neck, dorsolateral thorax, and girth. In some cases, the caudal aspect of the pastern may be the only site affected and resembles “grease heel” or “scratches.” The mane and tail areas are not usually affected. Initial lesions may be tufted papules and resemble fly bites or urticaria, but within several days, they become the more typical scaly or crusty circular alopecic foci. Pruritus varies from severe to absent. Lesions may continue to expand for 1-2 months and then regress as an immune response develops. Several horses with T. equinum dermatophytosis that resembled pemphigus foliaceus have been described. Two adult horses developed rapidly progressive painful widespread dermatitis consisting of papules, pustules, crusting, scaling, and erosions. Microscopically, lesions were characterized by prominent acantholysis. However, fungal arthrospores and hyphae were also evident and lesions resolved with antifungal therapy.
Dogs.
M. canis is considered the most common cause of dermatophytosis in dogs, but in some areas, infections caused by M. gypseum predominate. T. mentagrophytes infection is less frequent. Infections with anthropophilic species Epidermophyton floccosum and T. rubrum have been reported and suspected to have been acquired from infected humans. Dermatophyte infections are most often localized, with lesions occurring most commonly on the face, pinnae, paws, and tail. Most cases are seen in dogs <1 year of age. However, sylvatic ringworm is more common in adults. Most cases of dermatophytosis in dogs are follicular, and thus lesions are most commonly one or more peripherally expanding circular patches of alopecia with variable papules, pustules, scaling, and crust.
The lesions of dermatophytosis are grossly indistinguishable from demodicosis or bacterial folliculitis. Trichophyton infection may result in folliculitis or furunculosis affecting one leg or paw. Infection by M. persicolor may produce lesions characterized by prominent scaling but minimal alopecia. This dermatophyte does not invade hair, and thus fungal organisms are seen only in the surface keratin. In some cases, dermatophytosis can occur as generalized greasy scaling resembling seborrhea. Pruritus is usually absent but may be severe in some cases. Cases of dermatophytosis caused by T. mentagrophytes, T. terrestre, and M. persicolor with a very long duration (1-5 years) have been reported. These infections suggest that there is little tendency for spontaneous resolution in some infections, a situation analogous to chronic dermatophytosis in humans. Kerions are often associated with M. gypseum or T. mentagrophytes infections. Onychomycosis is rare and may consist of chronic inflammation of the ungual fold or infection of the claw alone, producing deformity or fragility of the claw.
Several cases of Trichophyton dermatophytosis with clinical and histologic features resembling pemphigus erythematosus or foliaceus have been reported. These dogs had symmetrical nasal or facial to periocular folliculitis and furunculosis with alopecia and crusting. Rarely lesions are generalized. Microscopically, lesions included lymphoplasmacytic lichenoid to interface dermatitis with mural folliculitis, with or without intraepidermal pustules with acantholytic keratinocytes, suggestive of an immune-mediated disease. However, fungal elements were demonstrable with fungal stains. T. mentagrophytes has been isolated in most cases, and M. persicolor, less frequently. These organisms tend to colonize the stratum corneum preferentially over the hair, and thus the lesions are not follicularly oriented. Acantholysis may be due to complement-mediated transepidermal neutrophilic chemotaxis as well as dermatophyte-produced proteolytic enzymes. Some cases lack intraepidermal pustules and acantholysis but have striking interface dermatitis with spreading facial scaling and hair loss (Fig. 6-103A-C ).
Figure 6-103.

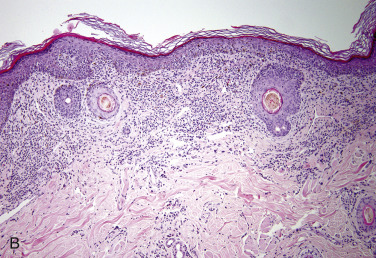
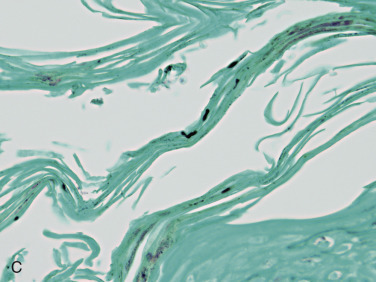
Trichophyton mentagrophytes in a dog. A. Spreading facial alopecia and scaling. B. Skin biopsy shows a lichenoid infiltrate with pigmentary incontinence. C. Small numbers of fungal hyphae are seen in the surface keratin with a silver stain.
Certain breeds of dogs may be predisposed to dermatophytosis. In Europe, dermatophyte infections are more common in the Parson Russell Terrier (especially T. mentagrophytes), Yorkshire Terrier (especially M. canis), and Pekingese (especially M. canis). Severe dermatophytosis and dermatophytic pseudomycetoma with lymph node involvement has been reported in Yorkshire Terriers with M. canis and T. mentagrophytes infections.
Cats.
Dermatophytosis is a common disease in cats. It is more common in cats than dogs, and longhaired and pedigree cats are at particular risk. Persian and Himalayan cats are predisposed to M. canis dermatophytosis. Infection may be endemic in large catteries, with up to 35% of cats culture positive. The vast majority of cases (>90%) are caused by M. canis, which is of considerable public health significance because of its zoonotic potential. Despite the name, this dermatophyte is well adapted to the cat and induces minimal host response. Geographic differences may influence the prevalence of various dermatophytes. A survey of dermatophytes isolated from cats in shelters in the United States found M. canis to predominate in the southeastern United States; whereas in cats from the northern United States, anthropophilic organisms were cultured, and M. canis was not isolated from any cat.
Lesions are extremely variable. They are most common on the face, pinnae, and paws, and may become generalized. As with dogs, dermatophytosis is more common in cats <1 year of age, but sylvatic ringworm is more common in adults. Pruritus is uncommon but may be moderate. Classic circular foci of alopecia and crusting or scaling are more common in kittens. In adult cats, lesions may be extremely subtle and consist of patchy mild alopecia or broken hairs with little skin change. This is especially true of longhaired cats that may have a poor haircoat and excessive shedding. Scaling and crusting may be absent or severe. Lesions may be hyperpigmented. Recurring chin folliculitis resembling feline acne or dermatitis of the dorsal tail resembling “stud tail” may occur. Focal pruritic lesions that resemble eosinophilic plaques can occur. Kerions are uncommon in cats, but longhaired cats, especially Persian cats, can develop dermatophytic pseudomycetomas, usually over the dorsal trunk or tail base, and tissue grains may be seen.
Widespread, pruritic papulocrustous miliary dermatitis is an uncommon manifestation of M. canis infection. Other uncommon clinical presentations associated with M. canis are widespread pruritic exfoliative erythroderma, recurrent otitis externa, asymmetrical paronychia or onychodysplasia, generalized seborrhea-like eruptions, and clinical signs suggestive of pemphigus foliaceus with crusting over the bridge of the nose, pinnae, and paronychia.
Microscopic findings are variable. In some cases, organisms are infrequent, and only a single infected hair may be found in a biopsy, whereas in other cases, organisms may be numerous. Pseudomycetomas are subcutaneous nodules. They are an atypical form of dermatophytosis caused by M. canis in which the deep dermis and subcutis are involved. There is frequently also a history of previous or concurrent superficial dermatophyte infection. Lesions are usually focal and measure 2-3 cm in diameter; but in some instances, they are multiple and may even have systemic lesions. They consist of discrete masses of bizarre, distorted, septate fungal hyphae; larger thick-walled fungal cells resembling chlamydospores; and chains of round structures surrounded by a hyaline eosinophilic Splendore-Hoeppli reaction. These granules are surrounded by granulomatous or pyogranulomatous inflammation. Fungal organisms are not necessarily present in the hair and keratin of the overlying skin. In contrast to pseudomycetoma, true mycetomas contain more abundant organisms and have a less pronounced Splendore-Hoeppli reaction.
Further reading
Bagcigil AF, et al. Recovery of dermatophytes in pet grooming tools from veterinary clinics and pet grooming salons. J Small Anim Pract 2010;51:39-42.
Baldo A, et al. Mechanisms of skin adherence and invasion by dermatophytes. Mycoses 2012;55:218-223.
Bond R. Superficial veterinary mycoses. Clin Dermatol 2010;28:226-236.
Carlotti DN, Bensignor E. Dermatophytosis due to Microsporum persicolor (13 cases) or Microsporum gypseum (20 cases) in dogs. Vet Dermatol 1999;10:17-27.
Chah KF, et al. Dermatophytes from skin lesions of domestic animals in Nsukka, Enuga state, Nigeria. Vet Dermatol 2012;23:522-e104.
DeBoer DJ, Moriello KA. Humoral and cellular immune responses to Microsporum canis in naturally occurring feline dermatophytosis. J Med Vet Mycol 1993;31:121-132.
De Oliveira Nobre M, et al. Disease progression of dermatophyte pseudomycetoma in a Persian cat. Rev Iberoam Micol 2010;27:98-100.
García-Sánchez A, et al. Outbreak of ringworm in a traditional Iberian pig farm in Spain. Mycoses 2011;54:179-181.
González Cabo JF, et al. An outbreak of dermatophytosis in pigs caused by Microsporum canis. Mycopathologia 1995;129:79-80.
Hullinger GA, et al. Dermatophytosis in show lambs in the United States. Vet Dermatol 1999;10:73-76.
Kano R, et al. Confirmed case of feline mycetoma due to Microsporum canis. Mycoses 2008;52:80-83.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Moriello KA, et al. Isolation of dermatophytes from the haircoats of stray cats from selected animal shelters in two different geographic regions in the United States. Vet Dermatol 1994;5:57-62.
Parker WM, Yager JA. Trichophyton dermatophytosis—a disease easily confused with pemphigus erythematosus. Can Vet J 1997;38:502-505.
Peters J, et al. Comparative analysis of canine dermatophytosis and superficial pemphigus for the prevalence of dermatophytes and acantholytic keratinocytes: a histopathological and clinical retrospective study. Vet Dermatol 2007;18:234-240.
Pittman JS, Roberts JD. Ringworm in lactating sows. J Swine Health Prod 2005;13:86-90.
Prado MR, et al. Frequency of yeasts and dermatophytes from healthy and diseased dogs. J Vet Diagn Invest 2008;20:197-202.
Scott DW. Marked acantholysis associated with dermatophytosis due to Trichophyton equinum in two horses. Vet Dermatol 1994;5:105-110.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Fungal skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 171-211.
Sharp MW, et al. Microsporum canis infection in sheep. Vet Rec 1993;132:388.
Sparkes AH, et al. Microsporum canis: Inapparent carriage by cats and the viability of arthrospores. J Small Anim Pract 1994;35:397-401.
Sparkes AH, et al. Experimental Microsporum canis infection in cats: correlation between immunological and clinical observations. J Med Vet Mycol 1995;33:177-184.
Vermout S, et al. Pathogenesis of dermatophytosis. Mycopathologia 2008;166:267-275.
Wagner DK, Sohnle PG. Cutaneous defenses against dermatophytes and yeasts. Clin Microbiol Rev 1995;8:317-335.
Subcutaneous fungal infections
Subcutaneous mycoses are fungal infections that have invaded beyond the skin and hair follicles. These infections produce granulomatous to pyogranulomatous inflammation and can be destructive. These are a heterogeneous group of infections caused by a wide variety of saprophytic fungi that normally exist in soil or vegetation. Infection generally requires mechanical introduction into tissue. The ability of the organism to adapt to the tissue environment and elicit disease is variable. The clinical course is usually insidiously progressive over a period of months to years. Infection usually remains localized to the site of entry and surrounding tissues. Slow extension by way of lymphatics occurs in some diseases, but widespread dissemination is rare.
-
•Mycetoma: The organism has mycelial morphology in tissue and is surrounded by eosinophilic hyaline material (Splendore-Hoeppli reaction: antigen-antibody complexes) resulting in a macroscopic granule or grain.
-
•Eumycotic: The cause is fungal.
-
•Actinomycotic: The cause is a member of the order Actinomycetales, such as Actinomyces and Nocardia.
-
•Chromomycosis: A subcutaneous and systemic disease caused by pigmented (dematiaceous) fungi.
-
•Chromoblastomycosis: The fungus is present in tissue as large (4-15 µm diameter) rounded, dark-walled cells (sclerotic bodies, chromo bodies, Medlar bodies).
-
•Phaeohyphomycosis: Organisms are pigmented and have mycelial and yeast morphology in tissue.
-
•
-
•
-
•
Hyalohyphomycosis: It is a subcutaneous and systemic disease caused by nondematiaceous (nonpigmented, hyaline) fungi. Organisms have septate branching or nonbranching hyphal (mycelial) tissue morphology.
-
•
Pseudomycetoma: The organism is present in tissue as granules or grains, but the formation of the granule is different from that of true mycetomas. Pseudomycetomas are formed by dermatophytes (dermatophytic pseudomycetoma) or bacteria (bacterial pseudomycetoma).
Eumycotic mycetoma
Mycetomas are characterized clinically by the triad of tumefaction (swelling), draining tracts, and grains in the discharge. Eumycotic mycetomas have been reported worldwide but are most frequent near the Tropic of Cancer. They occur in humans, occasionally in dogs and horses, and rarely in cattle and cats. A wide variety of fungi that exist as saprophytes in the soil or on plants have been associated with mycetomas. The organisms involved may also cause other clinical diseases, for instance, phaeohyphomycosis and mycotic granulomas, when all 3 criteria are not present for a diagnosis of a mycetoma. Mycetomas usually involve skin and subcutaneous tissues and sometimes extend to involve underlying bone. Curvularia spp. and the Scedosporium/Pseudallescheria complex are most commonly involved in mycetomas in animals.
Lesions in animals most frequently occur on the extremities and face. Lesions are usually solitary, but rarely, disseminated infections occur. Lesions begin as small dermal or subcutaneous papules that gradually enlarge to form nodules over a period of months to years. As the lesion slowly enlarges, they can become alopecic, hyperpigmented, firm, ulcerated, and develop draining tracks. The discharge is serous, purulent, or hemorrhagic and contains tissue grains. The grains or granules are composed of aggregates of fungal organisms and vary in size from 0.1 mm to several millimeters in size and may be white, yellow, pink-red, brown, or black. The color, size, shape, and texture of the grains may be sufficiently characteristic to suggest the etiologic agent, but definitive identification of the fungus requires culture. Curvularia spp. and Madurella spp. have been associated with black-grained mycetomas, whereas the Scedosporium/Pseudallescheria complex is usually associated with white grains.
The salient histologic feature is the presence of granules in a tumor-like mass of chronically inflamed tissue. Microscopically, the lesions are characterized by nodular infiltrates of pyogranulomatous to granulomatous inflammation in the subcutis and/or dermis surrounding tissue grains (Fig. 6-104 ). The grains (0.2-6 mm) are irregularly shaped (spherical, lobular, or scroll-shaped) masses and consist of densely tangled hyphae in the center with an outer rim of chlamydoconidia (terminal cystic dilations, 5-20 µm in diameter). The fungal hyphae may be embedded in an amorphous eosinophilic “cement-like” substance (see Fig. 6-104 inset). The granules of some mycetomas are surrounded by an amorphous eosinophilic radially arranged or smoothly contoured Splendore-Hoeppli reaction. Fragments of plant material may be seen within the lesion adjacent to the granules and are suspected to be the vehicle of infection. Nodules are surrounded by a chronic inflammatory reaction consisting of epithelioid macrophages, multinucleated histiocytic giant cells, and fewer plasma cells and lymphocytes. Fibrous connective tissue of variable maturity separates the inflammatory foci. In some cases, special stains may be needed to determine if the grains are composed of bacteria or fungi. Culture is the usual means of identification for definitive diagnosis.
Figure 6-104.
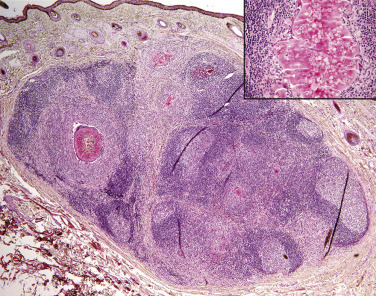
Eumycotic mycetoma in a horse. Nodular pyogranulomatous dermatitis with multifocal intralesional tangles of fungal hyphae embedded in amorphous eosinophilic material forming white tissue grains (see inset).
Further reading
Elad D, et al. Eumycetoma caused by Curvularia lunata in a dog. Mycopathologia 1991;116:113-118.
Elad D, et al. Disseminated pseudallescheriosis in a dog. Med Mycol 2010;48:635-638.
Elad D, et al. Eumycetoma caused by Madurella mycetomatis in a mare. Med Mycol 2010;48:639-642.
Elad D. Infections caused by fungi of the Scedosporium/Pseudallescheria complex in veterinary species. Vet J 2011;187:33-41.
Guillot J, et al. Eumycetoma caused by Cladophialophora bantiana in a dog. J Clin Microbiol 2004;42:4901-4903.
Lambrechts N, et al. Black grain eumycetoma (Madurella mycetomatis) in the abdominal cavity of a dog. J Med Vet Mycol 1991;29:211-214.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Chromomycosis (phaeohyphomycosis and chromoblastomycosis)
Phaeohyphomycosis (chromomycosis) is an uncommon opportunistic subcutaneous, cerebral, or systemic infection caused by a wide variety of fungi that are all characterized by formation of dematiaceous, or pigmented, hyphae and/or yeast in tissue. The pigmentation is due to the presence of melanin, which may act as a virulence factor in the development of infection. The organisms responsible for these infections are numerous and include Alternaria spp., Bipolaris spp., Cladosporium spp., Curvularia spp., Exophiala spp., Phialophora spp., and Wangiella spp. These organisms are worldwide in distribution and are widespread in the soil, on wood, and in vegetation. Some of the organisms can also be cultured from the skin of healthy people and animals. Subcutaneous infection is thought to result from wound contamination or traumatic implantation of wood slivers, thorns, sticks, and the like.
Phaeohyphomycosis has been reported most frequently in cats and occasionally in horses, dogs, cattle, and goats. The disease also occurs in humans. No underlying immune deficiency is apparent in most cases of subcutaneous phaeohyphomycosis, whereas disseminated infections have been associated with immunologic compromise or debilitating disease. German Shepherd dogs may be predisposed. Subcutaneous infection with Staphylotrichum coccosporum, a fungus previously thought to be nonpathogenic, was described in a cat positive for feline leukemia virus. Subcutaneous infection is insidiously progressive and evolves over months to years.
Lesions of phaeohyphomycosis consist of single or multiple subcutaneous nodules. The fungal pigmentation may be grossly visible in the tissue and, in some cases, the nodule is so dark it may be mistaken for a melanoma. In cats, lesions are usually single and occur most commonly on the face (nose and pinnae) and paws. Firm to fluctuant subcutaneous nodules grow slowly and may be ulcerated or have draining tracts. Multiple recurrences following surgical excision are common. The clinical course in some reported cases has been several years. Lesions in horses are frequently multiple and located on several different parts of the body. Occasionally, nodules may be generalized. Multiple ulcerated cutaneous nodules are the usual form of the infection described in cattle, and lesions may also be present in the nasal mucosa. Lesions in dogs are also frequently multiple and may be extensive. They consist of poorly circumscribed ulcerated or draining nodules or plaques on the paws and legs. In one affected dog, lesions consisted of multiple nodules in the area of ascending lymphatics of a leg and an enlarged regional lymph node, a clinical appearance similar to the cutaneous-lymphatic form of sporotrichosis.
The histologic diagnosis of phaeohyphomycosis is made by demonstrating pigmented hyphae within the tissue. The lesions consist of nodular-to-diffuse pyogranulomatous dermatitis and panniculitis (Fig. 6-105A ). The overlying epidermis is acanthotic or multifocally to diffusely ulcerated. Microabscesses with foci of necrosis are frequently prominent. Necrosis may be extensive. Fungi are distributed throughout the lesion as scattered small aggregates and individual hyphae. The hyphae are septate, 2-6 µm wide, and branched or unbranched. They are often constricted at their prominent thick septations and may contain single or chains of thick-walled vesicular swellings, 25 µm or more in diameter, that resemble chlamydospores (Fig. 6-105B). The innate brown pigment may not be readily apparent in tissue sections, especially in cases of Alternaria spp. Melanin stains, such as Fontana-Masson, can be used to confirm the presence of melanin in the hyphae. Fungal stains demonstrate the organisms well but can mask the natural color. The etiologic agents are so similar in appearance within tissues that they cannot be identified on the basis of their morphology. Culture is always needed for specific identification of the fungi. Phaeohyphomycosis has been confused with eumycotic mycetomas caused by dematiaceous fungi. The fungi in mycetomas form discrete organized granules, whereas those of phaeohyphomycosis appear as individual hyphae and small aggregates scattered throughout the lesion. The aggregates of hyphae in phaeohyphomycosis may be surrounded by Splendore-Hoeppli material, but this does not constitute a granule. The fungal elements of phaeohyphomycosis are frequently intracellular within epithelioid macrophages and multinucleated histiocytic giant cells; granules of mycetomas are nearly always extracellular.
Figure 6-105.
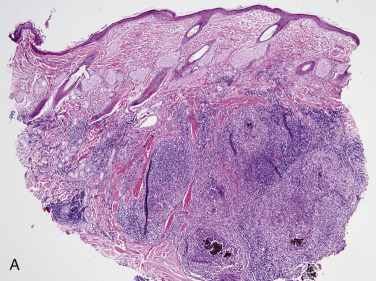
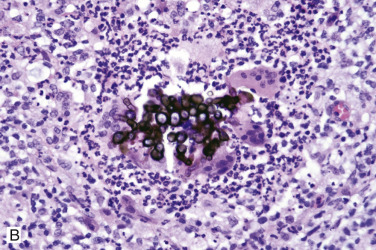
Phaeohyphomycosis in a horse. A. Nodular pyogranulomatous dermatitis with intralesional dematiaceous fungi. B. Dematiaceous fungal hyphae surrounded by multinucleated giant cells, neutrophils, and macrophages.
Hyalohyphomycosis
Hyalohyphomycosis (adiaspiromycosis) are opportunistic infections by nonpigmented saprophytic fungi normally found in soil and water. Numerous fungi have been implicated as a cause of hyalohyphomycosis, including Acremonium spp., Fusarium spp., Geotrichium spp., Paecilomyces spp., and the Scedosporium/Pseudallescheria complex. Aspergillus spp. are not included. Some organisms such as Geotrichium may be part of the normal flora of the host, oral cavity, gastrointestinal tract, and integument. Infections occur via wound contamination or invasion through mucosal surfaces. Common cutaneous sites of infection in dogs and cats are clawbeds, face, head, eyes, and joints. As with phaeohyphomycosis, German Shepherd dogs may be predisposed, and disseminated infection may occur in immunocompromised individuals. Gross lesions vary from well-circumscribed ulcers covered by exudate to nonulcerated nodular masses with variable alopecia and desquamation. Infection may be pruritic in horses. Microscopic findings are similar to phaeohyphomycosis with the important exception that the fungal elements are nonpigmented.
Further reading
Abramo F, et al. Feline cutaneous phaeohyphomycosis due to Cladophyalophora bantiana. J Feline Med Surg 2002;4:157-163.
Chermette R, et al. Exophiala spinifera nasal infection in a cat and a literature review of feline phaeohyphomycosis. J Mycol Med 1997;7:149-158.
Dye C, et al. Alternaria species infection in nine domestic cats. J Fel Med Surg 2009;11:332-336.
Foley JE, et al. Paecilomycosis in dogs and horses and a review of the literature. J Vet Intern Med 2002;16:238-243.
Fondati A, et al. A case of feline phaeohyphomycosis due to Fonsecaea pedrosoi. Vet Dermatol 2001;12:297-301.
Fuchs A, et al. Subcutaneous mycosis in a cat due to Staphylotrichum coccosporum. Mycoses 1996;39:381-385.
Genovese LM, et al. Cutaneous nodular phaeohyphomycosis in five horses associated with Alternaria alternata infection. Vet Rec 2001;148:55-56.
Herraez P, et al. Invasive phaeohyphomycosis caused by Curvularia species in a dog. Vet Pathol 2001;38:456-459.
Hirofumi M, et al. Feline digital phaeohyphomycosis due to Exophiala jeanselmei. J Vet Med Sci 2008;70:1395-1397.
Kimura M, McGinnis MR. Fontana-Masson-stained tissue from culture-proven mycoses. Arch Pathol Lab Med 1998;122:1107-1111.
Knights CB, et al. Phaeohyphomycosis caused by Ulocladium species in a cat. Vet Rec 2008;162:415-417.
Matsumoto T, et al. Developments in hyalohyphomycosis and phaeohyphomycosis. J Med Vet Mycol 1994;32(Suppl. 1):329-349.
McKay JS, et al. Cutaneous alternariosis in a cat. J Small Anim Pract 2001;42:75-78.
Miller RI. Nodular granulomatous fungal skin diseases of cats in the United Kingdom: a retrospective review. Vet Dermatol 2009;21:130-135.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Reppas GP, Snoeck TD. Cutaneous geotrichosis in a dog. Aust Vet J 1999;77:567-569.
Seyedmousavi E, et al. Phaeohyphomycosis, emerging opportunistic diseases in animals. Clin Microbiol Rev 2013;26:19-35.
Whitford HW, et al. Exserohilum dermal granulomas in a bovine. J Vet Diagn Invest 1989;1:78-81.
Sporotrichosis
Sporotrichosis is an uncommon chronic infection usually limited to skin and subcutaneous tissue caused by the opportunist fungal pathogen Sporothrix schenckii. The organism is a dimorphic fungus, growing as hyphae at environmental temperatures and in yeast form in tissue. S. schenckii exists as a saprophyte distributed worldwide in the soil, on plants, and on various plant materials. It is more common in tropical, subtropical, and temperate zones and is endemic in Central and South America and Africa. Since 1998, there has been an ongoing epidemic affecting cats, dogs, and humans in Rio de Janeiro and Southern Brazil. Sporotrichosis has been reported in cats, dogs, horses, mules, donkeys, cattle, goats, swine, camels, humans, and a variety of other animal species. The infection has been reported most often in cats, horses, and dogs. Infection is usually acquired by wound contamination or inoculation of the organism into tissue by puncture wounds caused by thorns, wood splinters, or contaminated claws. Pulmonary infection is occasionally acquired by inhalation of spores. In humans, the disease is considered an occupational hazard for those who work with the soil, plants, or plant materials.
Sporotrichosis is considered a zoonotic disease. Transmission of the infection from cats to humans has been reported many times, and infected cats pose a significant public health danger. Veterinarians, other veterinary professionals and students, and owners exposed to ulcerated wounds or exudates from infected cats have developed infections. The organism may be able to penetrate intact skin because not all patients who develop lesions can recall having wounds or being bitten or scratched by infected cats. The large number of organisms typically present in lesions from cats is thought to be the reason for the transmission of disease from cats to humans. However, even when the lesions in cats had few organisms, transmission to humans has occurred. In contrast, infection was not transmitted from a dog with multiple cutaneous lesions containing relatively numerous organisms to several adults and children with whom the dog had had frequent contact for the 2-year duration of infection. These cases suggest that factors in addition to absolute numbers of yeasts are involved in the apparent ease of cat-to-human transmission.
Sporotrichosis is subdivided into 3 clinical forms.
-
•
The primary cutaneous form consists of multiple scattered raised alopecic, ulcerated, crusted nodules or plaques that remain confined to the point(s) of entry of the organism. It is thought that this form results from a high degree of host immunity, preventing spread of infection. Nodules may become ulcerated and associated with seropurulent exudate and crust formation. The normal grooming behavior of cats may result in autoinoculation and spread of lesions to distant sites. The cutaneous form may have a very chronic course. An unusual case of sporotrichosis in a dog consisted of otitis externa characterized by multiple cutaneous nodules that persisted for >5 years. A donkey with sporotrichosis had multiple slowly progressive facial lesions for 2 years before the disease was diagnosed.
-
•
The cutaneous-lymphatic form involves the skin, subcutaneous tissue, and associated lymphatics. Lesions begin as firm round nodules at the site of entry, usually on an extremity, and spread proximally along lymphatics. Lymphatic vessels become thick and corded, and a series of secondary nodules forms as the infection progresses. The nodules may break open and discharge seropurulent material. Lesions may cavitate and expose extensive areas of underlying muscle and bone. Regional lymphadenopathy is common. This is the most common form in horses and humans. Lesions generally involve the proximal forelimbs, chest, and thigh, but usually no regional lymph node involvement is evident. Dogs usually have the cutaneous or cutaneous-lymphatic form. The head, pinnae, and trunk are involved most frequently. In cats, lesions are usually located on the head, distal limbs, and base of the tail (Fig. 6-106A ). The initial draining puncture wounds may be indistinguishable from cat-inflicted fight wound infections.
-
•
The extracutaneous/disseminated form may involve a single extracutaneous tissue, such as osteoarticular sporotrichosis, or multiple internal organs. It develops as a sequela to cutaneous-lymphatic infection or following inhalation of the fungus. The disseminated form of sporotrichosis occurs most frequently in cats, and no immunosuppressive factors are usually identified. In experimentally induced sporotrichosis in cats, organisms were shown by culture to have disseminated to viscera in 50% of the cases. Cats with disseminated sporotrichosis are often febrile, depressed, and anorexic. This is a rare presentation in dogs.
Figure 6-106.

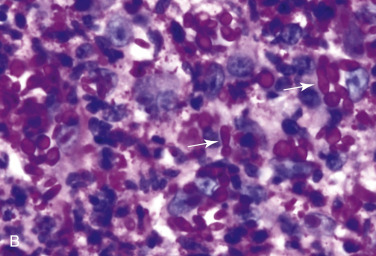
Sporotrichosis in a cat. A. Multiple ulcerated nodules over the face and pinnae. B. Diffuse pyogranulomatous dermatitis with numerous periodic acid–Schiff–positive intralesional round and “cigar-shaped” yeast (arrows).
Microscopically, sporotrichosis is usually a nodular-to-diffuse pyogranulomatous or granulomatous inflammatory reaction involving the dermis and subcutaneous fat. The epidermis is acanthotic or ulcerated. Neutrophils, epithelioid macrophages, multinucleated histiocytic giant cells, and fewer lymphocytes and plasma cells form discrete granulomas or extensive sheets of inflammation replacing dermal and subcutaneous tissues. Fibrosis is variable; and necrosis may be extensive. Yeast(s) surrounded by a stellate radial corona of brightly eosinophilic material (asteroid body/Splendore-Hoeppli reaction) are seen in some cases. The yeasts appear as round, oval, or elongated (“cigar”-shaped) single or budding cells that measure 2-6 µm or more in diameter for the round and oval forms and 2 × 3 to 3 µ 10 µm for the cigar form (Fig. 6-106B). The cigar forms are considered characteristic of Sporothrix, but they may not be regularly found. In general, organisms are numerous in lesions from cats and rare in tissues from dogs and horses. However, some reports indicate that visible organisms may be few or absent in some cats. In immunosuppressed dogs, yeasts may be numerous. The yeasts may be extracellular or within neutrophils and macrophages. The yeasts have a refractile cell wall from which the cytoplasm may shrink during processing and give the appearance of a capsule. In such instances and when no cigar forms are evident, the organism may be mistaken for Cryptococcus neoformans or Histoplasma capsulatum. Yeasts stand out clearly with fungal stains, but serial sections may be needed to demonstrate even a single organism. Without a significant number of cigar-shaped forms, identification may not be possible. Tissue culture, immunohistochemistry, or fluorescent antibody staining may be necessary for definitive identification of the organism. The yeast can usually be cultured from tissue obtained from areas of active inflammation even in dogs and horses, which typically have very few organisms in tissue. In cats, cytologic examination of exudates and material obtained by fine-needle aspiration of nodules is frequently diagnostic because sufficient numbers of yeasts are usually present to identify the organism.
In certain geographic regions, for instance, southern Brazil, a main differential diagnosis for canine sporotrichosis is American tegumentary leishmaniosis. These 2 diseases are clinically similar, are both endemic to this region, and present cross-reactivity in serologic tests. Organisms can be difficult to identify microscopically in both conditions. Although these 2 infections are histopathologically similar, in one study, well-formed granulomas with marked neutrophilic infiltration were more commonly associated with sporotrichosis.
Further reading
Barros MB, et al. Cat-transmitted sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis 2004;38:529-535.
Crothers SL, et al. Sporotrichosis: a retrospective evaluation of 23 cases seen in northern California (1987-2007). Vet Dermatol 2009;20:249-259.
Irizarry-Rovira AR, et al. Diagnosis of sporotrichosis in a donkey using direct fluorescein-labeled antibody testing. J Vet Diagn Invest 2000;12:180-183.
Madrid IM, et al. Feline sporotrichosis in the Southern region of Rio Grande do Sul, Brazil: clinical, zoonotic and therapeutic aspects. Zoonoses Public Health 2010;57:151-154.
Miranda LHM, et al. Comparative histopathological study of sporotrichosis and American tegumentary leishmaniosis in dogs from Rio de Janeiro. J Comp Path 2010;143:1-7.
Miranda LHM, et al. Evaluation of immunohistochemistry for the diagnosis of sporotrichosis in dogs. Vet J 2011;190:408-411.
Schubach TM, et al. Evaluation of an epidemic of sporotrichosis in cats: 347 cases (1998-2001). J Am Vet Med Assoc 2004;224:1623-1629.
Schubach TMP, et al. Canine sporotrichosis in Rio de Janeiro, Brazil: clinical presentation, laboratory diagnosis and therapeutic response in 44 cases (1998-2003). Med Mycol 2006;44:87-92.
Shany M. A mixed fungal infection in a dog: sporotrichosis and cryptococcosis. Can Vet J 2000;41:799-800.
Welsh RD. Sporotrichosis. J Am Vet Med Assoc 2003;223:1123-1126.
Cutaneous oomycosis (pythiosis and lagenidiosis)
Oomycosis refers to infection by Pythium insidiosum and Lagenidium spp. organisms, both of which are aquatic dimorphic water molds and members of the Oomycetes in the kingdom Stramenopila (Chromista). These opportunistic pathogens live in warm stagnant water and are most often reported in regions with tropical to subtropical environments. The organisms are thought to enter the skin through cutaneous wounds, and infection may involve the dermis, subcutis, or distant tissue. These organisms are often associated with devastating and often fatal infections.
Pythiosis (leeches, kunkers, swamp cancer, bursattee) is a chronic cutaneous-subcutaneous, gastrointestinal, or multisystemic infection of horses, dogs, humans, cattle, cats, and sheep, with rare reports in camels and other species. The infection is most common in tropical, subtropical, and temperate regions throughout the world, especially Thailand, Australia, India, Indonesia, and Costa Rica. In North America, infections are most common in the Gulf Coast region but have been reported as far north as New Jersey and as far west as Arizona and California. Pythium spp. are aquatic organisms. Pythium insidiosum is the etiologic agent of pythiosis in mammals. Microscopically, P. insidiosum develops mycelium-like fungi, but it is not a true fungus because its cell walls do not contain chitin but are composed of cellulose and β-glucan, its cytoplasmic membrane lacks ergosterol, the sexual process is oogamy, and the organism develops biflagellate zoospores in wet environments. The infective stage of the organism is a biflagellate aquatic zoospore that is released seasonally in association with warm weather and moisture. Most infections occur in late summer and fall. Infection is thought to be acquired from prolonged contact with stagnant fresh water containing the newly emerged zoospores that are motile and are attracted chemotactically to animal hair, damaged skin, and intestinal mucosa. Once the zoospores are in contact, they encyst on the surface of injured tissue. The encysted zoospores secrete a sticky amorphous glycoprotein that mediates the adhesion of zoospores to tissue. The body temperature of the host stimulates the encysted zoospores to develop a germ tube (hypha) that extends into the infected tissue and can later infiltrate blood vessels. These organisms also produce proteases that weaken host tissue, enhancing the ability of the hyphae to invade tissue. The zoospore stage is not known to form in tissue, and the infection is thus not considered to have zoonotic potential. Not all animals with pythiosis have a history of contact with permanent bodies of water, suggesting that the organism may proliferate in temporary stands of water or even on wet grasses.
Cutaneous pythiosis has been reported most frequently in horses. No age, breed, or sex predilection is recognized. Lesions occur most commonly on the limbs, distal to the carpus and hock, and on the ventral aspect of the thorax and abdomen, sites that are most likely to be in contact with stagnant water and would be traumatized by aquatic plants or vegetation. Affected horses frequently have a history of prolonged contact with water in lakes, ponds, swamps, or flooded areas. Lesions are usually single, but occasional horses develop lesions in several separate sites. Lesions begin as nodules that enlarge very rapidly to become circular masses of granulation tissue. The masses ulcerate or develop multiple draining tracts that discharge thick purulohemorrhagic material. The tracts also contain characteristic gray-white to pale yellow coral-like concretions (called leeches or kunkers) that may be extruded at the skin surface (Fig. 6-107A ). The colloquial name leeches is based on the initial misidentification of the masses. These structures are unique to the horse and are not seen in other animals with pythiosis. Lesions are frequently extremely pruritic, and biting or rubbing the lesion contributes to tissue damage. The largest lesions usually develop on the thorax and abdomen and may attain a size of 45 cm or more in diameter. In chronic cases, underlying bone may be invaded. Regional lymph nodes may be involved, but visceral spread is rare. The clinical appearance of the lesions may resemble basidiobolomycosis, cutaneous habronemiasis, excessive granulation tissue, and neoplasia (particularly sarcoid and squamous cell carcinoma).
Figure 6-107.
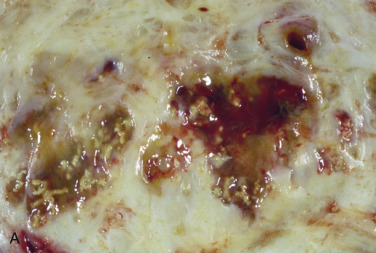
Pythiosis. A. Cut surface reveals multiple foci of necrosis with pale yellow linear concretions (“kunkers”) in a horse.
(Courtesy R. Miller.)

B. Alopecic nodular lesion with draining tracts on the limb of a dog.
(Courtesy M.S. Canfield.)
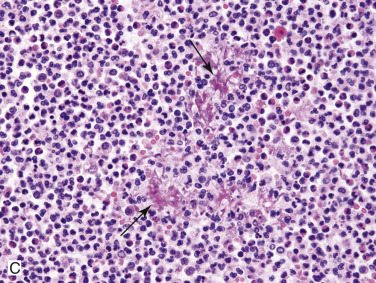
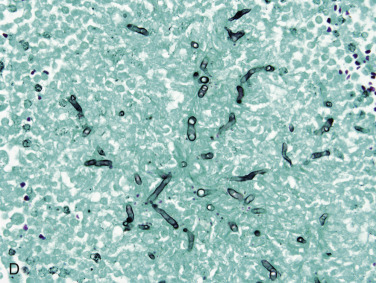
C. Negatively staining hyphae (arrows) surrounded by a small amount of eosinophilic Splendore-Hoeppli material and large numbers of eosinophils, neutrophils, and macrophages. D. Fungal hyphae are Gomori methenamine silver positive.
In dogs, cutaneous pythiosis has been reported less frequently than the gastrointestinal form. The disease occurs most often in young adult, large-breed dogs, and German Shepherd dogs and Labrador Retrievers may be predisposed. Most lesions are on the extremities, face, and tailhead. In most cases, a single body region is involved. The initial lesion is a poorly circumscribed dermal nodule that rapidly expands peripherally and extends into the subcutis to form multiple secondary nodules (Fig. 6-107B). The nodules develop into spongy masses that ulcerate, become necrotic, and develop multiple draining tracts that discharge purulohemorrhagic exudate. Early lesions on the legs may resemble acral lick dermatitis. Pruritus is not as constant a feature in dogs as it is in horses with pythiosis. A common clinicopathologic abnormality is absolute eosinophilia.
Pythiosis has been reported infrequently in cattle and sheep. There are a few reports of epizootic outbreaks in these species. Most reported cases of pythiosis in cattle have been in beef calves <12 months of age. In sheep, the condition appears to have no age, breed, or sex predisposition. In cattle, most lesions are located on the distal extremities, and in sheep lesions are most common on the limbs, ventral abdomen, and prescapular region. Lesions consist of irregular swellings that may or may not be ulcerated with multiple draining tracts. Although no concretions have been present, the tissue contains numerous yellow punctate foci. Secondary bacterial contamination with anaerobes and other bacteria is common in cattle. The lesions may be very painful and lead to recumbency, starvation, and death in calves. However, there have also been reports of spontaneous resolution. Internal spread, especially to lungs, may be more common in sheep than other species. Spontaneous resolution has not been reported in sheep.
Reports of pythiosis in cats are rare. As in other species, lesions usually are located on the extremities. In at least 2 cats, the lesions progressed very slowly, and the clinical course was much more protracted than is typical of the disease in dogs and horses. Ulceration is uncommon. Nodules usually remained confined to the subcutaneous tissues.
Microscopically, the lesions vary depending on the infected host species. In horses, skin lesions are usually extensively ulcerated with surface fibrin, neutrophils, and bacterial colonies. There is abundant fibrous connective tissue extending from the dermis to the subcutis. There are coalescing foci of granulation tissue with scattered macrophages surrounding eosinophilic material (“kunkers”). The kunkers are composed of necrotic tissue containing dense collections of eosinophils. A moderate to large number of negatively stained hyphae are present at the periphery of the kunkers and may be surrounded by many eosinophils and smaller numbers of lymphocytes, plasma cells, and mast cells. The hyphae are broad, sparsely septate, and have smooth, almost parallel walls with inconspicuous dilations. Deeply eosinophilic granular material (Splendore-Hoeppli material) is present around many hyphae. Degenerate or thrombosed arteries may be seen.
Two inflammatory patterns are seen in canine cutaneous pythiosis. The first pattern (necro-eosinophilic) is characterized by broad zones of eosinophilic necrosis, cell debris, and variable numbers of eosinophils. Some areas of necrosis are similar to equine kunkers. The second pattern (granulomatous) consists of epithelioid macrophages and Langerhans giant cells and may be surrounded by connective tissue. Both patterns may be seen in a single lesion. Negatively stained hyphae are more commonly seen in the necroeosinophilic lesions (Fig. 6-107C). Fibrinoid necrosis of arterial walls and small arterial thrombi may be seen. Angioinvasion is noted rarely. Angioinvasion has also been reported in one cat with gastrointestinal pythiosis but did not result in distant spread.
In cattle and sheep, there are multifocal necrotic areas within the dermis and subcutis, with numerous multinucleated histiocytic giant cells, eosinophils, neutrophils, macrophages, and plasma cells. Short poorly stained hyphal elements are observed within giant cells and necrotic areas. There is prominent eosinophilic material around hyphae (Splendore-Hoeppli phenomenon).
Because Pythium does not produce chitin, it stains poorly or not at all with PAS. It is readily stained with Gomori methenamine silver (GMS) and appears as thick-walled, sparsely septate hyphae, 2-7 µm in diameter, with occasional branching (Fig. 6-107D). Organisms are usually most numerous in necrotic foci and may also be seen in walls of small arterioles in some species. They are rare in areas of granulomatous inflammation, and they are not usually present in intervening connective tissue. The hyphae are similar to those of the zygomycetes Basidiobolus and Conidiobolus. The hyphae of these organisms tend to be broader, ranging from 5-20 µm in diameter; however, the differentiation of Pythium spp. from the zygomycetes in tissue is frequently impossible.
Diagnosis of pythiosis is based on the appearance of the gross lesions, microscopic lesions, and culture of the organism. Pythium is readily cultured in most instances, but it cannot be grown in some cases. PCR assays, immunohistochemistry, and immunoblot analyses have been developed for identification and differentiation of Pythium insidiosum, Lagenidium, and the zygomycetes. Not all assays are available for each organism, but a combination of assays and evaluation of the clinical information and laboratory results can lead to a definitive diagnosis.
Cutaneous lagenidiosis is remarkably similar to cutaneous pythiosis in geographic occurrence and clinical and histologic lesions. Lagenidiosis has been reported only in dogs, and most have been young to middle-aged living in the southeastern United States. Gross lesions consist of firm dermal or subcutaneous nodules of the limbs, mammary and inguinal regions, perineum, or trunk. Lesions may be ulcerated with areas of necrosis and draining tracts. Regional lymphadenopathy consisting of granulomatous to pyogranulomatous lymphadenitis is common and may precede skin lesions. The disease can be very aggressive, and affected dogs frequently develop lesions of the great vessels, mediastinum, lungs, and esophagus. Sudden death caused by great vessel rupture has been reported. Gastrointestinal lesions have not been observed. In some dogs, lesions may be slowly progressive, chronic, and limited to cutaneous and subcutaneous tissues. Microscopically, there is severe eosinophilic and granulomatous inflammation with numerous multinucleated histiocytic giant cells centered around broad 7-25 µm infrequently septate hyphae. Pyogranulomatous vasculitis may occur. Again, clinical presentation, PCR assays, immunohistochemistry and immunoblot analyses are needed to differentiate these infections.
Further reading
Dykstra MJ, et al. A description of cutaneous-subcutaneous pythiosis in fifteen dogs. Med Mycol 1999;37:427-433.
Gaastra W, et al. Pythium insidiosum: an overview. Vet Microbiol 2010;146:1-16.
Grooters AM, et al. Clinicopathologic findings associated with Lagenidium sp. Infection in 6 dogs: initial description of an emerging oomycosis. J Vet Intern Med 2003;17:637-646.
Grooters AM. Pythiosis, lagenidiosis, and zygomycosis in small animals. Vet Clin North Am Small Anim Pract 2003;33:695-720.
Martins TB, et al. A comparative study of the histopathology and immunohistochemistry of pythiosis in horses, dogs, and cattle. J Comp Pathol 2012;146:122-131.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Moriello KA, DeBoer DJ. Cutaneous fungal infections. In: Greene CE, editor. Infectious Diseases of the Dog and Cat. 4th ed. St Louis: Elsevier Saunders; 2012. p. 588-709.
Neto RT, et al. Cutaneous pythiosis in a dog from Brazil. Vet Dermatol 2009;21:202-204.
Perez RC, et al. Epizootic cutaneous pythiosis in beef calves. Vet Microbiol 2005;109:121-128.
Reis JL, et al. Disseminated pythiosis in three horses. Vet Microbiol 2003;96:289-295.
Schurko AM, et al. Development of a species-specific probe for Pythium insidiosum and the diagnosis of pythiosis. J Clin Microbiol 2004;42:241-2418.
Tabosa IM, et al. Outbreaks of pythiosis in two flocks of sheep in northeastern Brazil. Vet Pathol 2004;41:412-415.
White SD, et al. Cutaneous pythiosis in a nontravelled California horse. Vet Dermatol 2008;19:391-394.
Zygomycosis
Zygomycosis refers to subcutaneous, systemic, or rhinocerebral infections caused by a wide variety of zygomycete fungi. The class Zygomycetes is composed of 2 orders that cause disease in animals. The order Mucorales includes Rhizopus, Mucor, Lichtheimia (Absidia), Saksenaea, among other genera, and diseases caused by these organisms have been called mucormycosis. The order Entomophthorales contains the genera Basidiobolus (B. ranarum) and Conidiobolus (C. coronatus, C. incongruous, and C. lamprauges), and disease caused by these fungi is called entomophthoromycosis. In humans and animals, Mucorales organisms tend to cause acute, rapidly progressive disease in immunocompromised individuals, whereas Entomophthorales organisms typically cause localized infections in the subcutaneous tissues or nasal submucosa of immunocompetent individuals. Reports of mucormycosis are very uncommon in veterinary species, especially small animals. Zygomycetes are widespread in nature and occur as soil saprophytes, agents of decay, insect pathogens, or as components of normal skin and hair flora. They are common laboratory contaminants and are thus sometimes ignored when cultured from clinical specimens. The portal of entry may be cutaneous (via traumatic implantation or biting insects), gastrointestinal, or respiratory. Zygomycosis is not a contagious disease; the environment is the source of all infections. Infections are typically nonseasonal.
Zygomycosis is a rare disease of humans and animals, including dogs, cats, horses, llamas, sheep, and pigs. It occurs most commonly in tropical and subtropical areas, including the southeastern United States, South America, Australia, and India.
In humans, horses, sheep, and other mammalian species, conidiobolomycosis occurs most often in the nasopharyngeal region with or without extension into the tissues of the face, retropharyngeal region, and retrobulbar space. In horses, most lesions are found on the external nares or nasal passages. Lesions may be unilateral or bilateral, single or multifocal. Within the nasal passages, there are usually multifocal to coalescing firm nodules (1-5 cm) with either a cobblestone appearance or ulceration. Small (0.5 mm) foci of yellow friable material (leeches) may be present. Rhinopharyngeal conidiobolomycosis is an important disease of sheep in Brazil. Unlike the protracted clinical course typical of most cases of zygomycosis, nasal zygomycosis in sheep caused by C. incongruus results in loss of condition and death within a period of 7-10 days after initial clinical signs. This infection produces prominent asymmetrical swelling of the face, extending from the nostrils to the eyes, and marked thickening of the skin and subcutaneous tissue. In advanced cases, the nasal skin is alopecic and necrotic.
Lesions may be associated with exophthalmos and appear as white to yellow firm masses. Nasal conidiobolomycosis has been reported in several dogs and one llama. The llama and one dog had ulcerative dermatitis of the nasal planum. Two dogs also had ulcerative lesions of the hard palate. Subcutaneous zygomycosis caused by Conidiobolus of unknown species has been reported in a young adult dog. Lesions involved the skin of a hind leg and the thoracic wall but not the nasal mucosa or skin surrounding the nose. The lesions on the leg began as an ulcerated mass that progressed to circumferential swelling and induration with numerous coalescing ulcers draining serosanguineous fluid. The condition exhibited some waxing and waning, but new lesions continued to develop. No immunologic compromise or predisposing factors were apparent.
In horses, basidiobolomycosis is usually caused by B. ranarum. Most lesions are found on the trunk, head, and neck. They are characterized by large (up to 50 cm) circular, ulcerative granulomas with serosanguineous discharge. Small irregular gritty masses of yellow-white material (kunkers, leeches) may discharge to the surface. Lesions are usually solitary with moderate to severe pruritus. A discontinuous undulating band of yellow-white material that sharply demarcates the superficial hemorrhagic, edematous tissue from the underlying fibrogranulation tissue characterizes the cut surface of granulomas. The clinical lesions are similar to those of pythiosis but may sometimes be differentiated in the horse by differences in anatomic location, number and appearance of kunkers, and epidemiology. Basidiobolomycosis is a rare cause of pulmonary disease and ulcerative draining skin lesions in dogs. Disseminated infection involving the gastrointestinal tract and other abdominal organs has been described in 2 dogs.
Microscopically, zygomycosis is characterized by multifocal-to-diffuse eosinophilic and granulomatous dermatitis and panniculitis with multifocal necrosis. Necrotic foci consist of eosinophilic coagulated material corresponding to the kunkers seen grossly. Eosinophils, neutrophils, epithelioid macrophages, and multinucleated histiocytic giant cells surround the eosinophilic coagula and are separated by fibrovascular connective tissue. Fungi are usually located in necrotic foci and may be seen as clear linear or circular hyphal “ghosts” often surrounded by a thick (2.5-25 µm) eosinophilic sleeve (Splendore-Hoeppli phenomenon). This finding helps differentiate zygomycosis from pythiosis and lagenidiosis, in which eosinophilic sleeves tend to be thin or absent. In addition, the hyphal diameter (as measured in tissue) tends to be significantly larger for Basidiobolus spp. (5-20 µm). Conidiobolus spp. are 5-13 µm wide, and P. insidiosum are 2-7 µm wide. Basophilic granular protoplasm may be visible with H&E stain, but the organisms are usually better visualized with GMS stain. They frequently stain poorly with PAS. Hyphae are thin walled and have occasional septations and uncommon branching. Folded, twisted, or compressed hyphae may be seen. The lesions of nasal zygomycosis caused by C. incongruus in sheep are characterized by segmental necrosis and thrombosis of subcutaneous blood vessels. Many fungal hyphae are visible in necrotic foci, in thrombi, and within vessel walls. This propensity to invade blood vessels is common with Mucorales but is an unusual feature for the Entomophthorales.
The microscopic lesions of basidiobolomycosis and conidiobolomycosis are similar to those of pythiosis, and the diseases may be histologically indistinguishable, especially when the width of hyphae is at the narrow end of the range. All members of the zygomycetes are morphologically similar in tissue, and consequently culture, PCR, or immunohistochemistry are necessary for specific identification.
Further reading
de Paula DAJ, et al. Molecular characterization of ovine zygomycosis in central western Brazil. J Vet Diagn Invest 2010;22:274-277.
French RA, Ashworth CD. Zygomycosis caused by Conidiobolus coronatus in a llama (Lama glama). Vet Pathol 1994;31:120-122.
Greene CE, et al. Infection with Basidiobolus ranarum in two dogs. J Am Vet Med Assoc 2002;221:528-532.
Grooters AM. Pythiosis, lagenidiosis, and zygomycosis in small animals. Vet Clin North Am Small Anim Pract 2003;33:695-720.
Hillier A, et al. Canine subcutaneous zygomycosis caused by Conidiobolus sp.: a case report and review of Conidiobolus infections in other species. Vet Dermatol 1994;5:205-213.
Jensen HE, et al. Immunohistochemical diagnosis of systemic bovine zygomycosis by murine monoclonal antibodies. Vet Pathol 1996;33:176-183.
Tan RM, et al. Severe chronic diffuse pyogranulomatous, necrohemorrhagic and eosinophilic rhinitis caused by Conidiobolus. J Am Vet Med Assoc 2010;236:831-833.
Ubiali DG, et al. Pathology of nasal infection caused by Conidiobolus lamprauges and Pythium insidiosum in sheep. J Comp Pathol 2013;149:137-145.
Miscellaneous fungal infections of skin
Infections with various opportunist fungi are reported sporadically in animals. These organisms are ubiquitous in the environment, common contaminants of laboratory cultures, and frequently also a component of skin and hair flora of normal animals. Thus diagnosis of infection is difficult to make by culture alone and requires histologic demonstration of tissue invasion by morphologically compatible organisms. In humans, these infections are usually associated with immunosuppression and neutropenia, but predisposing factors are only occasionally identified in animals.
Aspergillus spp. are distributed widely in nature and are found in soil, dust, and decaying vegetation. Aspergillus spp. are not commonly associated with skin infections. Subcutaneous infection with Aspergillus versicolor producing a nodular mass on the upper lip was reported in an adult Saddlebred mare. The lesion recurred once following surgical excision but had not recurred 1 year after the second surgical excision. A. terreus has been associated with subcutaneous granulomas in an adult Holstein cow without any lesions elsewhere. Dogs with disseminated aspergillosis may rarely develop cutaneous lesions secondarily. Nasal and cutaneous aspergillosis caused by A. niger was reported in a goat from Brazil. Lesions included a large mass in the nasal cavity and several raised nodules over the nares (2-3 cm) and pinnae (0.3-1 cm). Microscopically, there was pyogranulomatous rhinitis and dermatitis with central necrosis and intralesional fungal hyphae. Hyphae are septate, branching, 5-7 µm in diameter, have thick walls, and occasionally have bulbous apical dilations.
Piedra is a fungal infection of the extrafollicular portion of the hair shaft caused by Piedraia hortae (“black piedra”) and Trichosporon beigelii (“white piedra”). These organisms are ubiquitous saprophytic yeast-like fungi. Piedra is an opportunistic infection and has been associated with cutaneous infections, urinary tract infections, systemic infections, pneumonitis, valvular endocarditis, fatal mastitis, and abortions. In humans, disseminated systemic infections usually occur in immunocompromised patients with granulocytopenia. Cutaneous white piedra has been described in humans, monkeys, horses, dogs, and cats. The infection is more common in temperate climates of South America, Europe, Asia, Japan, and the southern United States. The infection is characterized by firm, irregular white or pale brown nodules on hair shafts. In horses, the long hairs of the mane, tail, and forelock are affected. The nodules consist of tightly packed septate hyphae that are held together by a cement-like substance. Trichosporon spp. has rarely been reported to cause nasal granulomas in cats and in one cat was reported to cause an ulcerated mass on the distal leg at the site of a previous cat-bite wound. Microscopically, the organisms consist of spherical to oval, 3-8 µm, narrow-based, budding yeast cells and septate, nonpigmented, branching hyphae with nonparallel sides.
Rhodotorula spp. are normal inhabitants of the skin, ear canal, and alimentary tract. These yeast-like fungi are opportunistic pathogens in immunosuppressed patients. Cutaneous infection has been reported in one cat with feline immunodeficiency virus and feline leukemia virus infections. This cat had adherent brown-red crusts over the nasal planum, nostrils, bridge of nose, periocular region, and one digit.
Further reading
do Carmo PM, et al. Nasal and cutaneous aspergillosis in a goat. J Comp Pathol 2014;150:4-7.
Fleming RV, et al. Emerging and less common fungal pathogens. Infect Dis Clin North Am 2002;16:915-933.
Gonzales RN, et al. Outbreaks of clinical mastitis caused by Trichosporon beigelii in dairy herds. J Am Vet Med Assoc 2001;218:238-242.
Keegan KG, et al. Subcutaneous mycetoma-like granuloma in a horse caused by Aspergillus versicolor. J Vet Diagn Invest 1995;7:564-567.
Keller M, et al. Keratinopathogenic mould fungi and dermatophytes in healthy and diseased hooves of horses. Vet Rec 2000;147:619-622.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Sharman MJ, et al. Clinical resolution of a nasal granuloma caused by Trichosporon loubieri. J Fel Med Surg 2010;12:345-350.
Protozoal Diseases of Skin
Cutaneous lesions occur in several systemic or localized protozoal infections. Differentials for protozoal dermatitis should include Besnoitia spp., Leishmania spp., Caryospora spp., Neospora spp., Toxoplasma spp., Sarcocystis spp., and Babesia spp. Cutaneous lesions have also been associated with Theileria infection (see Vol. 3, Hematopoietic system). Trypanosoma equiperdum and dourine are discussed in Vol. 3, Female genital system.
Besnoitiosis
Besnoitia is an apicomplexan protozoal parasite in the family Sarcocystidae. It is closely related to Toxoplasma and Neospora. Besnoitiosis has a worldwide distribution and affects both wild and domestic animals. Infections are reported in cattle, donkeys, horses, goats, sheep, and a number of wild animals, including reindeer, caribou, zebras, rodents, rabbits, the Virginia opossum, and lizards. Currently, there are 10 known species of Besnoitia, but the life cycle of only 4 of those is understood. A feline definitive host has been identified for B. oryctofelis, B. darling, B. neotomofelis, and B. wallacei, which affects rabbits, opossums, southern plains woodrat, and rodents, respectively. The pathogenesis, life cycle, and route of infection are poorly understood for the 4 Besnoitia spp. that affect ungulates: B. besnoiti (cattle), B. bennetti (equids), B. caprae (goats, sheep), and B. tarandi (reindeer, caribou).
In the 4 species in which the definitive host is known to be a felid, sexual reproduction is thought to occur in the intestinal tract of the definitive host, and the sporulated oocysts are passed in the feces. The exact mode of infection of the intermediate hosts is not known, but mechanical transmission by blood-sucking insects is regarded as an important natural mode of transmission. Some studies suggest that direct transmission from intermediate host to intermediate host is possible, such as through mating. Tachyzoites in the intermediate host proliferate in endothelial cells, monocytes, and neutrophils. In the later phases of infection, tissue cysts occur. Infection, however, may be generalized and is typically so in some infections in rodents and wild animals. The tissue cysts represent parasitized host cells, for instance, fibroblasts, myofibroblasts, endothelial cells, or smooth muscle cells. The bradyzoites multiply in cellular vacuoles and induce hyperplastic and hypertrophic changes in the host cells. These often divide to form multinucleated cells. The enlarging mass of crescent-shaped bradyzoites compresses the cell cytoplasm and nuclei into a thin rim forming an inner coat to the cyst. A hyalinized collagenous cyst wall is laid down around the parasitized cell. The cysts, which measure up to 500 µm with a 10- to 50-µm thick wall, are visible to the naked eye. Ingesting parasitized tissue from the intermediate host infects the definitive host.
Besnoitiosis is an emerging disease of cattle in Europe and donkeys in the United States. Bovine besnoitiosis caused by B. besnoiti is enzootic in Africa and Asia, and both enzootic and epizootic in parts of Europe. It has been reported in France, Spain, Portugal, Italy, and Germany. The disease also occurs in Israel, Russia, South Korea, and Venezuela. The disease is of high economic importance in Africa, causing mortality in up to 10% and morbidity in >80%. In Europe, mortality is <1%, and although many animals in an endemic area may be seropositive, most are subclinically infected. Predilections for age, breed, and sex appear to vary between geographic regions. In the enzootic regions of France, bovine besnoitiosis occurs preferentially from spring to autumn. Two- to 4-year-old males are more susceptible than females and have more acute signs with higher mortality rates. In the French Alps, where the disease is epizootic, females are more susceptible. Infection appear to be rare in calves <6 months of age. In clinically affected animals, there is an acute and a chronic stage. The acute stage can be confused with bluetongue or malignant catarrhal fever and is characterized by fever, generalized edema, weakness, anorexia, and lymphadenopathy. During this stage, tachyzoites proliferate in macrophages, fibroblasts, and endothelial cells, resulting in vasculitis and thrombosis, especially in small vessels of the dermis, subcutis, fascia, testes, and upper respiratory mucosa. Pregnant cows may abort, and bulls may develop orchitis and sterility. Besnoitiosis is usually recognized as a chronic disease characterized by alopecia; marked thickening and folding of the skin, especially around the neck, shoulders, and rump; scaling; exudation; and fissuring. Animals lose condition, have decreased milk production, have permanent sterility in some bulls, have significant hide damage, and up to 10% mortality may occur during the chronic stage. Lesions may be painful. During the chronic stage of besnoitiosis, only tissue cysts are found. Tissue cysts are most concentrated around mucous membranes (nares, conjunctiva, vulva, perineum) and sclera (“scleral pearls”) but also occur commonly in the dermis; subcutis; fascia; muscle; epididymis; testes; in the mucosa of the pharynx, larynx, and trachea; and less commonly in the spleen, liver, lung, lymph nodes, periosteum, endosteum, and heart muscle. It is not certain if new tissue cysts are formed during the chronic stage and how long the cysts persist in cattle. Although some tissue cysts do degenerate and cause inflammation, there is no evidence that besnoitiosis can be reactivated from the chronic to acute stage. This is unlike the biology of rodent Besnoitia spp., where it has been shown that chronic B. jellisoni infection in rodents can be reactivated by experimentally induced immunosuppression.
Equid besnoitiosis is caused by B. bennetti and was first described in isolated cases of horses and donkeys in Africa. Besnoitiosis has become an emerging disease of donkeys in the United States, with outbreaks occurring in Michigan, Pennsylvania, and Oregon. No cases have been reported in horses outside of Africa. The disease is also reported in mules and a zebra in Africa. Clinical disease is characterized by tens to hundreds of nonpruritic, white, pinpoint papular lesions in the skin and mucous membranes, especially over the nares, conjunctiva, sclera, pinnae, limbs, and perineum (Fig. 6-108A ). As with bovine besnoitiosis, the presence of scleral pearls is a valuable diagnostic feature. Tissue cysts also occur in the dermis, subcutis, fascia, muscle, epididymis, testes, and in the mucosa of the pharynx, larynx, and trachea. There is variable hair loss and lichenification. For unknown reasons, some infected donkeys remain healthy, whereas others become cachectic and debilitated. Internal dissemination of tissue cysts has not been reported in equid besnoitiosis. Risk factors for infection in donkeys have been suggested to be young age (most affected donkeys have been <3 years of age) and stressful, crowded, or unhygienic conditions.
Figure 6-108.

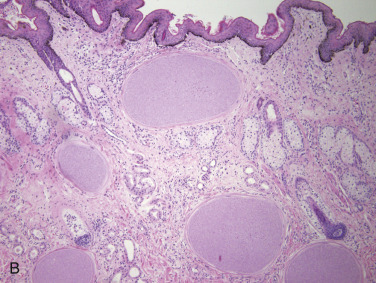
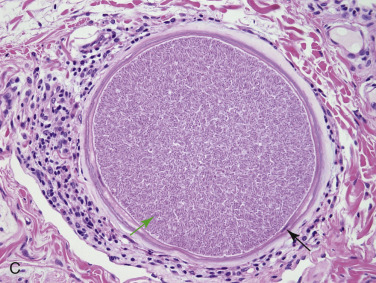
Besnoitiosis in a donkey. A. Multiple periocular pinpoint pale tan to white papules representing encysted protozoa (arrows). B. Five protozoal cysts in the dermis. C. Note the compressed host cell nucleus (black arrow) in the cyst wall and the intraluminal bradyzoites (green arrow).
Caprine besnoitiosis caused by B. caprae is clinically and pathologically similar to bovine besnoitiosis but has only been reported in Iran and Kenya. The prevalence of disease is higher in older goats and rare in goats <1 year of age. In an outbreak affecting >500 domestic goats in Kenya, ocular cysts were the most common finding, but cysts were found in many body systems. Dorper sheep were also affected in that outbreak. A disease resembling besnoitiosis was reported in New Zealand lambs.
Histologically, protozoal cysts are 150-500 µm in diameter with 10-50 µm thick 3-layered walls (Fig. 6-108B, C). The mature cyst wall has 4 distinct layers. Outermost is a condensed, hyalinized, laminated, eosinophilic to amphophilic birefringent layer of collagen fibers. Next is a very thin homogeneous intermediate zone. The third layer is the cytoplasm of the host cell, and in this layer lie several giant, vesicular but compressed host cell nuclei. A thin inner membrane forms the parasitophorous vacuole containing a myriad of tightly packed 7 × 2 µm basophilic crescentic bradyzoites. These may be separated from the wall by an artifactual shrinkage space. Some cysts have no tissue reaction, and some are surrounded by small to moderate numbers of lymphocytes, plasma cells, eosinophils, and histiocytes. Ruptured or degenerate cysts are often surrounded by inflammation (as noted previously) and multinucleated giant cells. Other histopathologic features in donkeys include epidermal hyperplasia, mild orthokeratotic to parakeratotic hyperkeratosis with occasional cellular crusts, intercellular edema in the epidermis, lymphocytic exocytosis, mild lymphocytic mural folliculitis, and mild to moderate diffuse superficial to mid-dermal perivascular infiltrates composed of mixed mononuclear cells, and variable numbers of eosinophils. In cattle in the acute phases, there is epidermal hyperplasia with dermal edema and perivascular accumulations of lymphocytes, plasma cells, and large histiocytes. Crescent-shaped trophozoites occur in arterioles and lymphatics and free in tissue spaces. Occasionally, they may be detected in macrophages. In some cases, there is vasculitis, thrombosis, and extensive dermal and epidermal necrosis. As the parasites become encysted, inflammation and edema diminish (chronic stage). In cattle and goats, cysts are sometimes present within blood vessels.
Diagnosis of besnoitiosis is based on clinical findings and skin biopsies. Serologic tests can be used to detect subclinical infections; however, these tests have a low level of specificity, it takes several weeks for antibodies to be formed in the animal after infection, and some infected animals have low antibody titers. PCR testing has superior sensitivity compared with serology in acutely affected animals.
Further reading
Alvarez-Garcia G, et al. A century of bovine besnoitiosis: an unknown disease re-emerging in Europe. Trends Parasitol 2013;29:407-415.
Cortes H, et al. Besnoitiosis in bulls in Portugal. Vet Rec 2005;157:262-264.
Dubey JP, et al. Ultrastructure of Besnoitia besnoiti tissue cysts and bradyzoites. J Eukaryot Microbiol 2003;50:240-244.
Dubey JP, et al. Redescription of Besnoitia bennetti (Protozoa: Apicomplexa) from the donkey (Equus asinus). Int J Parasitol 2005;35:659-672.
Dubey JP, et al. Development of early tissue cysts and associated pathology of Besnoitia besnoiti in a naturally infected bull (Bos taurus) from South Africa. J Parasitol 2013;99:459-466.
Ellis JT, et al. Molecular phylogeny of Besnoitia and the genetic relationships among Besnoitia of cattle, wildebeest and goats. Protist 2000;151:329-336.
Elsheikha HM, et al. An outbreak of besnoitiosis in miniature donkeys. J Parasitol 2005;91:877-881.
Gentile A, et al. Evidence for bovine besnoitiosis being endemic in Italy—first in vitro isolation of Besnoitia besnoiti from cattle born in Italy. Vet Parasitol 2012;184:108-115.
Jacquiet P, et al. Bovine besnoitiosis: epidemiological and clinical aspects. Vet Parasitol 2010;174:30-36.
Ness SL, et al. Investigation of an outbreak of besnoitiosis in donkeys in northeastern Pennsylvania. J Am Vet Med Assoc 2012;240:1329-1337.
Njagi ON, et al. An epidemic of besnoitiosis in cattle in Kenya. Onderstepoort J Vet Res 1998;65:133-136.
Oryan A, Azizi S. Ultrastructure and pathology of Besnoitia caprae in the naturally infected goats of Kerman, East of Iran. Parastol Res 2008;102:1171-1176.
Oryan A, et al. Histopathologic and ultrastructural studies on experimental caprine besnoitiosis. Vet Pathol 2011;48:1094-1100.
Oryan A, Sadeghi MJ. An epizootic of besnoitiosis in goats in Fars province of Iran. Vet Res Commun 1997;21:559-570.
Rostaher A, et al. Bovine besnoitiosis in Germany. Vet Dermatol 2010;21:329-334.
Leishmaniasis
Leishmaniasis is a zoonotic infection caused by an intracellular, diphasic protozoan of the genus Leishmania. More than 30 Leishmania spp. have been identified. Species vary by geographic region, but Leishmania infantum is the most commonly reported cause of visceral disease in the endemic regions of Europe. The disease is most commonly reported in humans and dogs but occurs in a wide variety of domestic mammals and wildlife. Three forms of clinical leishmaniasis are recognized: cutaneous, mucocutaneous, and visceral. Cutaneous leishmaniasis occurs worldwide in dogs, cats, horses, and cattle. It is endemic in Mediterranean countries, Portugal, and in parts of Africa, India, and Central and South America. Endemic foci have also been reported in the United States and include regions of Texas, Oklahoma, Ohio, Michigan, and Alabama. Leishmaniasis is also endemic in Foxhound populations in the United States.
The most common mode of transmission is through the bite of a female blood-sucking sandfly of the genera Phlebotomus and Lutzomyia. The biting sandfly injects promastigotes and saliva into the skin of the host. The sandfly saliva has potent vasodilating, anticoagulant, anesthetic, and immunomodulatory properties. Other modes of transmission have been suggested, such as blood transfusions and vertical transmission. Domestic and wild dogs, cats, rodents, and other wild mammals act as reservoirs. The parasite's life cycle and manifestations of visceral disease are discussed in Vol. 3, Hematopoietic system.
Leishmaniasis can manifest as a subclinical infection, self-limiting disease, or severe systemic illness. A variety of host and parasite factors are likely important in determining whether the host is resistant or susceptible. Leishmaniasis is a chronic disease with an incubation period that varies from weeks to years. The disease can occur at any age but is more common in young adults. Studies in mice and dogs indicate that resistance to infection is dependent upon a Th1-type of immune response, whereas susceptibility is associated with a Th2-type of immune response. The alopecic form of the cutaneous disease in the dog has been shown to be associated with fewer organisms and a more appropriate cellular immune response in terms of number of antigen-presenting Langerhans cells, major histocompatibility complex II–positive keratinocytes, and infiltrating T cells. In contrast, dogs with the nodular form lacked antigen-presenting cells and had more numerous macrophages containing large numbers of organisms. It has been suggested that the clinical and histologic lesions may be useful in establishing a prognosis for remission in that the character of the lesions that develops reflects epidermal immunocompetence. For example, papular dermatitis caused by Leishmania spp. in dogs has been associated with good response to treatment and reduced antibody titers, which are suggestive of immunocompetence and a favorable prognosis.
Skin lesions occur in >80% of dogs with visceral involvement. The most common presentation is exfoliative dermatitis with silvery white scales. Lesions are most pronounced on the head, pinnae, and extremities but may be generalized. Involved skin may be hypotrichotic to alopecic, and nasodigital hyperkeratosis may also occur. Periocular alopecia “lunettes” is common. Ulcerative dermatitis is the next most common presentation. Other gross lesions include onychogryphosis, paronychia, sterile pustular dermatitis, nasal depigmentation with ulceration, and papular to nodular dermatitis. Papular and nodular lesions are generally nonpainful and nonpruritic and are most common on the ventral abdomen, inner aspect of the pinnae, eyelids, and face but can be anywhere on the body. Nodular mucosal leishmaniasis affecting the oral cavity, tongue, nose, and penis has been reported in the dog.
Histologically, 9 inflammatory patterns have been recognized. The 3 most common patterns are granulomatous perifolliculitis, superficial and deep perivascular dermatitis, and interstitial dermatitis. Other patterns reported include lichenoid interface dermatitis, nodular dermatitis, lobular panniculitis, suppurative folliculitis, and intraepidermal pustular epidermitis. Dogs commonly have more than one pattern. Orthokeratotic and parakeratotic hyperkeratosis are usually prominent, and the inflammatory infiltrate typically is composed of macrophages with fewer lymphocytes and plasma cells. Multinucleated histiocytic giant cells may be present. The infiltrate in areas of ulceration includes neutrophils. Sebaceous adenitis with total obliteration of the sebaceous glands occurs in ~45% of cases. Leishmania amastigotes are found intracellularly (macrophages, leukocytes, endothelial cells, or fibroblasts) or extracellularly in 50% of the cases. Organisms are often contained within round, clear, intracellular parasitophorous vacuoles, many of which contain more than a dozen amastigotes at their periphery. Amastigotes are round to oval, 2-4 µm in diameter, and contain a round basophilic nucleus and a small rod-like kinetoplast. Leishmania organisms can often be seen with routine H&E stains; however, they are best visualized with Giemsa stain. Some animals have infiltrates consisting primarily of large, foamy macrophages with numerous organisms and fewer plasma cells and lymphocytes, whereas other animals have larger numbers of lymphocytes and plasma cells, indicating a more effective cellular immune response. Histologically, the perifollicular pattern with granulomatous inflammation and sebaceous gland destruction may need to be differentiated from sebaceous adenitis and sterile granuloma syndrome.
Feline leishmaniasis is rare and generally occurs as a cutaneous disease without visceral involvement, although visceral involvement can occur. It has been reported in the Mediterranean region and South America, where the disease is endemic, as well as Switzerland, Iran, and the United States. Leishmania mexicana is endemic in Texas, where it is the confirmed cause of cutaneous leishmaniasis in cats. Clinically, cats most commonly have one to multiple variably smooth, ulcerated or scaly papules and nodules on the pinnae and muzzle (Fig. 6-109A ). Histologically, a nodular-to-diffuse pattern of granulomatous dermatitis with numerous intrahistiocytic amastigotes and a variable number of lymphocytes and plasma cells is the most common inflammatory reaction pattern seen in cats (Fig. 6-109B).
Figure 6-109.

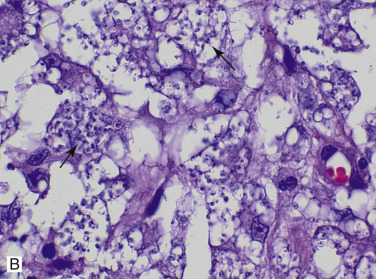
Leishmaniasis in a cat. A. Ulcerated nodule at the base of the pinna. B. Numerous intrahistiocytic amastigotes (arrows) in the dermis.
(Courtesy B.F. Porter.)
Cutaneous leishmaniasis has been reported in horses, mules, and donkeys in Europe, South America, North America, and Puerto Rico. Reports in cattle are rare: one cow from Switzerland with L. siamensis and one suspected case from Zimbabwe. Lesions in equids consist of single to multiple crusted or ulcerated papules and nodules on the pinnae, head, and neck, or less commonly, the legs, scrotum, and penis. In cattle, lesions have been described on the muzzle, pinnae, udder, and legs. Histologically, the dermis contains nodular-to-diffuse infiltrates of macrophages and lymphocytes or distinct granulomas with organisms identified in macrophages or free within the interstitium. Numerous eosinophils and foamy macrophages were described in a case of a 7-year-old Brown Swiss cow from Switzerland. Cutaneous lesions may not be associated with systemic infection.
Diagnosis can be made through finding the organism on cytologic or histologic evaluation of tissues, PCR, immunohistochemistry, in situ hybridization, serology demonstrating anti-Leishmania antibodies, or a positive skin test reaction.
Further reading
Barnes JC, et al. Diffuse cutaneous leishmaniasis in a cat. J Am Vet Med Assoc 1993;202:416-418.
Bourdoiseau G, et al. Immunohistochemical detection of Leishmania infantum in formalin-fixed, paraffin-embedded sections of canine skin and lymph nodes. J Vet Diagn Invest 1997;9:439-440.
Bourdoiseau G, et al. Lymphocyte subset abnormalities in canine leishmaniasis. Vet Immunol Immunopathol 1997;56:345-351.
Ciaramella P, et al. A retrospective clinical study of canine leishmaniasis in 150 dogs naturally infected by Leishmania infantum. Vet Rec 1997;141:539-543.
Cornegliani L, et al. PCR technique detection of Leishmania spp. but not Mycobacterium spp. in canine cutaneous ‘sterile’ pyogranuloma/granuloma syndrome. Vet Dermatol 2005;16:233-238.
Fondevila D, et al. Epidermal immunocompetence in canine leishmaniasis. Vet Immunol Immunopathol 1997;56:319-327.
Font A, et al. Canine mucosal leishmaniasis. J Am Anim Hosp Assoc 1996;32:131-137.
Hervas J, et al. Two cases of feline visceral and cutaneous leishmaniosis in Spain. J Feline Med Surg 1999;1:101-105.
Koutinas AF, et al. Clinical considerations on canine visceral leishmaniasis in Greece: a retrospective study of 158 cases (1989-1996). J Am Anim Hosp Assoc 1999;35:376-383.
Lobsiger L, et al. An autochthonous case of cutaneous bovine leishmaniasis in Switzerland. Vet Parasitol 2010;169:408-414.
Menezes RC, et al. Sensitivity and specificity of in situ hybridization for diagnosis of cutaneous infection by Leishmania infantum in dogs. J Clin Microbiol 2013;51:206-211.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Mozos E, et al. Leishmaniasis and generalized demodicosis in three dogs: a clinicopathological and immunohistochemical study. J Comp Pathol 1999;120:257-268.
Muller N, et al. Occurrence of Leishmania sp. in cutaneous lesions of horses in Central Europe. Vet Parasitol 2009;166:346-351.
Navarro JA, et al. Histopathological lesions in 15 cats with leishmaniosis. J Comp Pathol 2010;143:297-302.
Ordeix L, et al. Papular dermatitis due to Leishmania spp. infection in dogs with parasite-specific cellular immune responses. Vet Dermatol 2005;16:187-191.
Petersen CA. Leishmaniasis, an emerging disease found in companion animals in the United States. Top Companion Anim Med 2009;24:182-188.
Ramos-Vara JA, et al. Cutaneous leishmaniasis in two horses. Vet Pathol 1996;33:731-743.
Reuss SM, et al. Autochthonous Leishmania siamensis in horse, Florida, USA. Emerg Infect Dis 2012;18:1545-1547.
Roura X, et al. Detection of Leishmania infection in paraffin-embedded skin biopsies of dogs using polymerase chain reaction. J Vet Diagn Invest 1999;11:385-387.
Saridomichelakis MN. Advances in the pathogenesis of canine leishmaniosis: epidemiologic and diagnostic implications. Vet Dermatol 2009;20:471-489.
Schubach TM, et al. American cutaneous leishmaniasis in two cats from Rio de Janeiro, Brazil: first report of natural infection with Leishmania (Viannia) braziliensis. Trans R Soc Trop Med Hyg 2004;98:165-167.
Solano-Gallego L, et al. Cutaneous leishmaniosis in three horses in Spain. Equine Vet J 2003;35:320-323.
Trainor KE, et al. Eight cases of feline cutaneous leishmaniasis in Texas. Vet Pathol 2010;47:1076-1081.
Miscellaneous coccidian parasites
Toxoplasma gondii, an apicomplexan intracellular coccidian parasite, has been reported rarely as a cause of cutaneous lesions in humans, cats, and dogs. This parasite has worldwide distribution and is most commonly associated with disseminated and often fatal infections in immunocompromised hosts. Necrotizing hepatitis and pneumonia are most common and are discussed elsewhere in this book. The cat is the definitive host, and most mammals can serve as an intermediate host. Most reports of cutaneous toxoplasmosis have been associated with systemic fatal infections. All 3 dogs described in the literature were on immunosuppressive therapy. Skin lesions are described as single to multiple ulcerated and nonulcerated nodules. One dog was described to have generalized cutaneous pruritic pustules. Histologically, there is severe pyogranulomatous dermatitis and panniculitis with vasculitis, vascular thrombosis, edema, and necrosis. The tachyzoites are 2 × 6 µm and have a crescent shape with pale basophilic cytoplasm and a dark nucleus. They can be single or arranged in clusters, some of which are extracellular or within the cytoplasm of follicular, epidermal, and glandular epithelial cells, and within macrophages, fibroblasts, and endothelial cells.
Caryospora spp., apicomplexan parasites whose primary hosts are reptiles and raptors, rarely cause pyogranulomatous dermatitis in puppies. Immunosuppression and concurrent disease, such as canine distemper, likely play a facilitatory role. Lesions involve skin and draining lymph nodes and comprise diffuse pyogranulomatous dermatitis. Macrophages contain large numbers of intracellular organisms, including schizonts, gamonts, oocysts, and caryocysts. Caryocysts have a thin cyst wall enclosing the host cell nucleus and contain up to 3 sporozoites. Not all stages of the life cycle may be present in tissue sections, precluding a microscopic diagnosis in some cases. Immunohistochemical studies identified the agent in one case as Caryospora bigenetica. Experimental oral infection of immunosuppressed puppies infected with C. bigenetica induced typical skin lesions affecting the muzzle, periocular skin, footpads, ears, and abdomen within 10 days of inoculation.
Neospora caninum is a cyst-forming apicomplexan protozoal parasite. The definitive hosts are domestic and wild dogs, and intermediate hosts include dogs, cattle, sheep, goats, horses, and deer. It is best known as a cause of bovine abortion capable of transplacental transmission. This parasite is a primary pathogen in dogs and has been associated with progressive ascending paralysis, polymyositis, multifocal central nervous system disease, myocarditis, pneumonia, and hepatitis. Cutaneous lesions occur rarely in adult dogs, often with underlying immunosuppression from drug therapy or concurrent disease. It is not known whether the disease in adult dogs results from a reactivated congenital infection or from a recently acquired infection. Lesions have been described as multifocal-to-generalized, ulcerative papulonodular dermatitis. Histologically, there is pyogranulomatous and sometimes eosinophilic, to necrotizing and hemorrhagic, dermatitis. Numerous tachyzoites, 4-7 µm × 1.5-5 µm, may be seen in macrophages, keratinocytes, and neutrophils, and rarely in endothelial cells and fibroblasts. Tissue cysts are not present in the cutaneous lesions. Cutaneous infection with both N. caninum and L. infantum was reported in one dog from Italy. To differentiate neosporosis from toxoplasmosis, immunohistochemistry, electron microscopy, or PCR is necessary.
An unidentified Sarcocystis-like protozoan was associated with multiple cutaneous abscesses and disseminated visceral lesions in a dog. The skin lesions were diffuse, necrotizing, hemorrhagic, and suppurative. Large numbers of protozoa were present, primarily in macrophages and neutrophils, and occasionally in fibroblasts and endothelial cells. Some vessels contained thrombi, and there was associated dermal and epidermal infarction. The organism did not stain with antisera to the other apicomplexan parasites, so far identified as causing dermatitis in dogs, namely, N. caninum, T. gondii, and Caryospora spp.
Infection with Babesia canis and B. gibsoni have been reported to rarely cause cutaneous lesions in dogs. Babesia is a hemoprotozoal parasite that is transmitted through the bite of a tick or through saliva in fighting dogs. Skin lesions include petechiae, ecchymoses, edema, ulceration, and necrosis of extremities, pressure points, and frictional areas—most commonly pinnae, axillae, groin, limbs, and scrotum. In one dog, generalized alopecia was reported. Histologically, there is leukocytoclastic vasculitis with or without vascular necrosis.
Further reading
Anfray P, et al. Feline cutaneous toxoplasmosis: a case report. Vet Dermatol 2005;16:131-136.
Dubey JP, et al. Caryospora-associated dermatitis in dogs. J Parasitol 1990;76:552-556.
Dubey JP, et al. Fatal cutaneous and visceral infection in a Rottweiler dog associated with a Sarcocystis-like protozoon. J Vet Diagn Invest 1991;3:72-75.
Hoffmann AR, et al. Cutaneous toxoplasmosis in two dogs. J Vet Diagn Invest 2012;24:636-640.
Kul O, et al. Clinicopathologic diagnosis of cutaneous toxoplasmosis in an Angora cat. Berl Munch Tierarztl Wochenschr 2011;124:386-389.
La Perle KMD, et al. Cutaneous neosporosis in two adult dogs on chronic immunosuppressive therapy. J Vet Diagn Invest 2001;13:252-255.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Ordeix L, et al. Cutaneous neosporosis during treatment of pemphigus foliaceus in a dog. J Am Anim Hosp Assoc 2002;38:415-419.
Park CH, et al. Cutaneous toxoplasmosis in a female Japanese cat. Vet Pathol 2007;44:683-687.
Tarantino C, et al. Leishmania infantum and Neospora caninum simultaneous skin infection in a young dog in Italy. Vet Parasitol 2001;102:77-83.
Tasaki Y, et al. Generalized alopecia with vasculitis-like changes in a dog with babesiosis. J Vet Med Sci 2013;75:1367-1369.
Webb JA, et al. Cutaneous manifestations of disseminated toxoplasmosis in an immunosuppressed dog. J Am Anim Hosp Assoc 2005;41:198-202.
Algal Diseases of Skin
Protothecosis is an uncommon disease caused by Prototheca spp. organisms, achlorophyllic algae-like unicellular organisms belonging to the family Chlorellaceae. The organism is ubiquitous in organic matter and in fresh and marine waters. Reports of infection in humans and domestic and wild animals are worldwide, but the majority of cases are from the southeastern United States. The 2 most common species associated with infection are Prototheca wickerhamii and P. zopfii. Mastitis in cows and disseminated disease in dogs are more common than cutaneous-subcutaneous infection. In humans, the cutaneous form is the most common and is thought to be initiated by traumatic implantation, resulting in a protracted and indolent clinical course. Cutaneous protothecosis has been reported in dogs and cats in the United States, Australia, England, and Spain, and a goat in Brazil. In those cases in which the organism was speciated, P. zopfii is most often associated with disseminated disease, whereas the cutaneous form has been caused by P. wickerhamii.
Despite widespread distribution of Prototheca spp., the prevalence of infection is very low, and attempts to reproduce infection experimentally have met with mixed success. This has led to speculation that the organism is an opportunist with low pathogenicity that requires an underlying immunologic dysfunction for the development of disease. Most humans with cutaneous protothecosis have a concurrent disease condition that may alter the immune response to the organism; however, immunocompromise has not been documented in most affected animals.
Dermatologic lesions include single to multiple papules and nodules, often over pressure points or nodules and ulcerations involving mucocutaneous junctions (especially nostrils), scrotum, and pawpads (Fig. 6-110A ). Nasal planum depigmentation may be striking. Histologically, there is pyogranulomatous to granulomatous dermatitis and panniculitis with epithelioid macrophages, multinucleated histiocytic giant cells, neutrophils, and lymphoid cells are in variable numbers, and foci of necrosis may be present. Organisms are typically numerous, but they are only lightly stained with H&E and therefore are poorly visualized. The cell wall and internal contents are readily stained with fungal stains, for instance, Gridley (GF), Gomori methenamine silver (GMS), and periodic acid–Schiff (PAS). The organisms vary from 3–30 µm in diameter and consist of cells called sporangia that divide by internal cleavage to form multiple endospores (Fig. 6-110B). Identification of Prototheca can be made reliably by examination of tissue sections, but species identification usually requires culture or immunofluorescence methods because differences in the 2 species are subtle. P. wickerhamii sporangia are smaller (3-15 µm) and round in comparison to the larger (7-30 µm) and oval or cylindrical shape of most P. zopfii. Prototheca must be differentiated from Chlorella algae, whose natural green pigmentation is removed in fixation and routine tissue processing. In contrast to Prototheca cells, Chlorella sporangia contain many large starch granules that are stained by GF, GMS, and PAS.
Figure 6-110.

Prototheca spp. infection in a dog. A. Multiple ulcerations of the pawpad.
(Courtesy R. Last, D. Miller.)
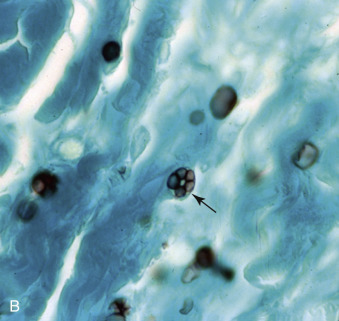
B.Prototheca spp. sporangium (arrow) stained with Gomori methenamine silver.
(Courtesy D.W. Scott.)
Further reading
Dillberger JE, et al. Protothecosis in two cats. J Am Vet Med Assoc 1988;192:1557-1559.
Ginel PJ, et al. Cutaneous protothecosis in a dog. Vet Rec 1997;140:651-653.
Hollingsworth SR. Canine protothecosis. Vet Clin North Am Small Anim Pract 2000;30:1091-1101.
Macedo JTSA, et al. Cutaneous and nasal protothecosis in a goat. Vet Pathol 2008;45:352-354.
Miller WH, et al. Fungal and algal skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 184-222.
Perez J, et al. Canine cutaneous protothecosis: an immunohistochemical analysis of the inflammatory cellular infiltrate. J Comp Pathol 1997;117:83-89.
Arthropod Ectoparasites
Of the parasitic arthropods, very few are parasites of domestic animals, but the harmfulness of these is quite out of proportion to their number. Some, such as the mites, are pathogens in their own right, but most owe their immense importance to their ability to act as mechanical or biological transmitters for many pathogenic viruses, bacteria, protozoa, and helminths. Their role as vectors is discussed in relation to the specific diseases throughout these volumes.
The parasites of concern to us here belong to the 2 large classes, Insecta and Arachnida. The class Insecta contains 4 important orders: Diptera (flies), Siphonaptera (fleas), Mallophaga (chewing lice), and Siphunculata (sucking lice). The class Arachnida contains the order Acarina, in which ticks and mites are classified. For information on biological characters and classification, reference should be made to texts on entomology.
Many arthropod bites or stings go unreported and are of minimal consequence. The type and number of arthropods inflicting the bite or sting and the individual host response determine the severity of the injury. In general, most arthropod bites initially appear as circular, erythematous lesions, 0.5-2.0 cm in diameter. Lesions may progress to focal areas of necrosis with ulceration, alopecia, and crust formation. Histologically, the area of necrosis and inflammation may have a triangular outline with one point of the triangle in the deep dermis or panniculus. In early lesions, the inflammation is perivascular to diffuse and includes variable numbers of eosinophils, neutrophils, lymphocytes, and macrophages. Edema and hemorrhage may be present. As the lesion ages, the area may become nodular to form “arthropod-bite granuloma“ composed of macrophages, lymphocytes, mast cells, eosinophils, and plasma cells. Lymphoid nodules with follicle formation may develop. More specific details concerning injury inflicted by various arthropods, if known, are discussed in the following sections.
Further reading
Bowman DD. Arthropods. In: Bowman DD, editor. Georgi's Parasitology for Veterinarians. 7th ed. Philadelphia: WB Saunders; 1999. p. 1-78.
Gross TL, et al. Nodular and diffuse diseases of the dermis with prominent eosinophils, neutrophils or plasma cells. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 342-372.
Steen CJ, et al. Arthropods in dermatology. J Am Acad Dermatol 2004;50:819-842.
Wall R, Shearer D. Veterinary Entomology, Arthropod Ectoparasites of Veterinary Importance. London: Chapman and Hall; 1997.
Flies
Flies belong to the insect order Diptera. Different species have various degrees of adaptation to a parasitic existence. Adult flies feed on blood, sweat, tears, saliva, feces, urine, and other body secretions. Nonbiting, nuisance flies accomplish this by feeding only at the body surface on wounds or natural body orifices, whereas biting flies puncture the skin to feed. Musca are facultative feeders. Some, such as the Simuliidae and parasitic species of Culicidae and Ceratopogonidae, are obligate blood-suckers, although usually only the females draw blood. At the other end of the spectrum are the Oestridae, whose larvae are obligate parasites, and some members of the Hippoboscidae that are obligate parasites in the adult stage.
Because of the variety of parasitic modes, it is not possible to generalize on the effects of flies on domestic animals, nor, with the exception of a few obligate parasites, is it possible to be specific because there is little information available on primary pathogenicity. Flies adversely affect domestic animals by causing annoyance, by direct toxicity that may be fatal following massive insect attack, by indirect toxicity resulting from the deposition of larva into damaged skin (myiasis), by local irritant effects causing dermatitis that may predispose to secondary bacterial infection or to myiasis, by injection of antigens that induce hypersensitivity reactions, by blood-feeding activities that cause anemia, and by the biological or mechanical transmission of other pathogens. It has been estimated that tabanid flies could transmit 35 pathogens, including equine infectious anemia virus and trypanosomes. Musca spp. have been implicated in the mechanical transmission of anthrax, mastitis, Habronema spp., and conjunctivitis in animals. Stomoxys calcitrans, the stable fly, is thought to be the primary transmitter of habronemiasis in horses.
Animal annoyance, so-called fly-worry, is an important source of economic loss to the cattle, sheep and, to a lesser extent, swine industries. Fly worry refers to the behavioral disturbances in animals brought about by the attempted feeding of flies. Biting flies inflict pain, whereas nonbiting flies cause annoyance by clustering around the eyes and nostrils, where they feed on lacrimal or nasal secretions (Musca autumnalis and Hydrotaea irritans) or by other means, such as simulating the sound of a bumble bee (Hypoderma spp.). Fly-worry occasionally induces such apprehension that the animals run aimlessly (“gadding”), and severe injury or death may result from misadventure. Deaths are usually sporadic, but high levels of mortality have been reported. Of much greater economic importance is the loss of production associated with fly-worry. When the insects are numerous, they cause considerable annoyance to livestock, interfere with feeding and resting, and cause reduced milk production and reduced weight gain. Fly-worry has been attributed to biting flies such as the horn fly (Haematobia [Lyperosia] irritans), the stable fly (Stomoxys calcitrans), and horse flies (several genera in the family Tabanidae), and to nonbiting species such as house flies (Musca spp.), Hypoderma spp., and the sheep-head fly (Hydrotaea irritans). Culicoides spp. biting midges can cause pruritus and restlessness in horses. Horses that develop a hypersensitivity response to Culicoides spp. bites may suffer weight loss as a result of severe pruritus and irritation (see Immune-mediated dermatoses). Louse flies (Hippobosca spp.) parasitize large animals in many parts of the world. They suck blood and tend to cluster in the perineal and inguinal region. Once the fly lands on its host, it sheds its wings and burrows into the skin to feed. They remain on their host for long periods and are a source of irritation and fly-worry.
Mortality may arise from direct toxic effect as well as from misadventure. Death may be the result of urticarial swelling of the head and neck or shock. Many flies are attracted to exhaled carbon dioxide and can occasionally cause death by suffocation of cattle, horses, or other animals when large numbers of flies are inhaled. Mosquitoes, especially aggressive species, such as Aedes vigilex, may cause significant mortality among piglets and puppies. The Simuliidae (black flies or buffalo gnats) are responsible for massive animal mortalities, particularly in temperate latitudes and river valleys following extensive flooding, when the insect population expands. They feed on cattle, horses, sheep, goats, poultry, wild mammals, and birds. Simuliid flies exert systemic effects through inoculation of a heat-stable toxin, which causes increased vascular permeability and abnormalities in cardiorespiratory function, which may cause death.
The hematophagous flies seldom cause serious loss of blood; however, anemia may result from heavy infestations by Haematobia irritans, mosquitoes, the sheep ked Melophagus ovinus, and Stomoxys calcitrans, which may ingest as much as 16 mg of blood per feeding.
In dogs, 3 forms of fly-bite dermatitis have been described. The first form is characterized by annular, macular targetoid lesions with a central puncture surrounded by an edematous zone with a peripheral erythematous rim on the abdomen, axillae, and lateral surfaces of the pinnae (Fig. 6-111 ). These lesions are associated with black fly (Simulium spp.) bites. The second form occurs as erythematous crusted papules that are dark red to black and hemorrhagic on the abdomen and lateral surfaces of the pinnae. The third form has ulcers covered with red to black crusts on the tips and folds of the pinnae. Only the third type is associated with clinical signs of variable pruritus. Both the second and third forms are thought to be associated with bites of stable flies (Stomoxys calcitrans) or deer flies (Chrysops spp.).
Figure 6-111.

Fly-bite dermatitis caused by black flies in a dog.
(Courtesy W.H. Miller.)
In horses, simulids tend to bite thinly haired, areas such as the face, pinnae, neck, ventrum, and legs. Lesions may be localized to the intermandibular region. Lesions are painful papules, wheals, ulcers, or circumscribed areas of necrosis. Simulid bites may be involved in the pathogenesis of ear papillomas and insect-bite hypersensitivity in horses.
Local irritant effect results from injection of salivary fluids into the host. Very little is known of the nature of the cutaneous lesions produced in animals by these insects. The character and severity of the local lesions vary. Pruritus is often intense, resulting in secondary traumatic lesions. The primary lesions are usually erythematous papules or wheals often surrounding a central bleeding point (mosquitoes) or small puncture wounds (biting flies). The wheals are usually transient but may persist for several weeks. The puncture wounds often develop an exudative crust. Some flies (Simuliidae) feed by lacerating the skin until a pool of blood forms on the surface from which they feed.
Histologically, there may be intraepithelial eosinophilic spongiform pustules or focal areas of epidermal necrosis indicating the penetration point. The dermal reaction is superficial perivascular to interstitial in pattern and contains predominantly eosinophils, lymphocytes, and plasma cells. Occasionally, there is acute necrosis of the surface of the papules, including both dermis and epidermis.
The injected salivary substances are irritant, and many are allergenic; hypersensitivity reactions probably contribute to the severity of the local lesions caused by a variety of biting flies. Hypersensitivity reactions to S. calcitrans are recognized in cattle; affected animals develop coalescing blisters on the forelimbs. An important allergic dermatitis of horses is caused by hypersensitivity to Culicoides spp. Black flies have also been associated with insect-bite hypersensitivity in horses.
Rather more important than the blood-sucking or biting flies are those species whose larvae are highly destructive facultative or obligate parasites. Infestations with such larvae cause myiasis, which is discussed later.
Further reading
Foil LD, et al. The role of horn fly feeding and the management of seasonal equine ventral midline dermatitis. Equine Pract 1990;12:6-14.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Scott DW, Miller WH. Fly-bite dermatitis in dogs: a retrospective study of 35 cases (1988-1998). Jpn J Vet Dermatol 2012;18:239-243.
Yeruham I, et al. Skin lesions in dogs, horses and calves caused by the stable fly Stomoxys calcitrans (L.) (Diptera: Muscidae). Rev Elev Med Vet Pays Trop 1995;48:347-349.
Myiasis
Myiasis is the infestation of the tissue of living animals with the larvae of dipterous flies. The larvae are referred to as maggots or grubs and may be facultative or obligate parasites. The important families are Cuterebridae, Sarcophagidae (Wohlfahrtia spp.), Gasterophilidae (stomach bots of horses), Oestridae (nasal bots, warbles), and Calliphoridae (blowflies). Calliphorids feed only on dead tissue. Only those flies whose larvae cause cutaneous or subcutaneous lesions are discussed here. Nasal and stomach bots are described elsewhere. Agents of facultative myiasis affecting the skin live in decaying organic matter, and the females oviposit in wounded, infected, or heavily soiled skin of warm-blooded vertebrate hosts. The larvae feed on host tissues and eventually drop to the ground to pupate. Cochliomyia hominivorax, the screwworm fly, has a widespread geographic distribution, feed only on living tissue and has been eliminated from North America. They produce larvae that are obligatory parasites and are discussed separately.
Cuterebra.
The larvae of Cuterebra spp. (order Diptera; family Oestridae; subfamily Cuterebrinae) are obligate parasites of rodents and rabbits, but occasionally aberrant infestations occur in cats and rarely in dogs, pigs, and humans. Larvae attach to the host's fur and either enter via ingestion through grooming, direct skin penetration, or through natural orifices to migrate to the subcutaneous tissues to produce an initially firm, then fluctuant, cyst-like subcutaneous abscess in which the larvae mature. The larvae breathe through a draining tract in the skin through which they are visible, and feed off tissue debris. Wounds heal slowly after larvae are removed or released, and secondary bacterial infection may occur. The majority of infections occur in late summer or fall. In cats, the larvae have a predilection for the neck area (Fig. 6-112 ), often over the submandibular salivary gland, but swellings also occur in the scrotal region. Larvae may locate in aberrant locations, such as the pharynx, nasal cavity, eye, and brain.
Figure 6-112.

Cuterebra infestation with draining lesion in a cat.
(Courtesy W.H. Miller.)
In South and Central America, Dermatobia hominis (furuncular myiasis) (order Diptera; family Oestridae; subfamily Cuterebrinae) affects horses, cattle, sheep, goats, pigs, rabbits, and people, and rarely dogs and cats. It is also known as the human bot fly. The adult fly captures another carrier insect to which it attaches its eggs. The eggs hatch when the carrier insect visits a host. The larvae then attach to the host and penetrate the skin to form local subcutaneous nodules that can be pruritic. The mature larvae exit the nodule through holes that leave the host susceptible to fly strike. A case report of an infected dog from the Netherlands described lesions as painful, erythematous, exudative nodules with a central pore.
Wohlfahrtia magnifica (order Diptera; superfamily Oestoidea; family Sarcophagidae) is an obligate larval parasite of warm-blooded vertebrates in the Mediterranean basin, Eastern and Central Europe, and Asia Minor. The female fly deposits larvae on the host near body orifices or in wounds. Larvae mature and drop to the ground to pupate in 5-7 days. W. magnifica causes myiasis in sheep, camels, poultry, and to a lesser extent in cattle, horses, pigs, and dogs. Fecal soiling in sheep is a predisposing condition. W. vigil is a parasite of mink, foxes, rabbits, and occasionally dogs and cats in North America. The larvae can penetrate the tender skin of young animals, hence the young are most often affected. W. nubia is a secondary facultative invader of wounds in camels in North Africa and the Middle East.
Further reading
Farkas R, Kepes G. Traumatic myiasis of horses caused by Wohlfahrtia magnifica. Acta Vet Hung 2001;49:311-318.
Glass EN, et al. Clinical and clinicopathologic features in 11 cats with Cuterebra larvae myiasis of the central nervous system. J Vet Intern Med 1998;12:365-368.
Orfanou DC, et al. Myiasis in a dog shelter in Greece: epidemiological and clinical features and therapeutic considerations. Vet Parasitol 2011;181:374-378.
Rodriguez JM, Perez M. Cutaneous myiasis in three obese cats. Vet Q 1996;18:102-103.
Roosje PJ, et al. A case of a Dermatobia hominis infection in a dog in the Netherlands. Vet Dermatol 1992;3:183-185.
Verocai GG, et al. Furuncular myiasis caused by the human bot-fly Dermatobia hominis in a domestic cat from Brazil. J Fel Med Surg 2010;12:491-493.
Williams KJ, et al. Cerebrospinal cuterebriasis in cats and its association with feline ischemic encephalopathy. Vet Pathol 1998;35:330-343.
Warbles.
Warbles (hypodermiasis, grubs) is caused by the larval stages of Hypoderma spp. (H. bovis and H. lineatum) (order Diptera; family Oestridae; subfamily Hypodermatinae). It is common in cattle and seen occasionally in horses, sheep, and goats in the Northern Hemisphere. H. bovis, H. lineatum, and H. sinense are present in Europe and Asia. Intensive eradication programs have eliminated Hypoderma spp. from some northern European countries and have greatly reduced their populations in much of the United States and Canada. Przhevalskiana silenus affects sheep and goats in Asia and Eastern Europe. H. diana, a parasite of roe deer in Europe, has been identified in horses and sheep.
Warble flies are also called heel flies because the eggs are deposited predominantly on the hair of the legs. Larvae emerge 4-6 days later and burrow directly into the skin or into hair follicles, causing minimal irritation. Larvae migrate along fascial planes leaving tracks of green gelatinous material known as “butcher's jelly.” The first instar larvae of H. bovis overwinter in the epidural fat, whereas those of H. lineatum develop in the esophageal submucosa. In the esophageal lesions, collagen bundles around the first instar larvae of H. lineatum appear fragmented, as if undergoing enzymatic digestion. A collagenase has been isolated from H. lineatum. In the epidural lesions of H. bovis, it is the fat tissue that appears necrotic. In the spring, the larvae migrate dorsally to the subcutaneous tissue of the back to form subcutaneous nodules ~3 cm in diameter with a central pore for respiration. The lesions, known as “warbles,” may be painful and last for 4-6 weeks, during which the larvae undergo 2 molts. The mature third-instar larvae emerge from the breathing hole and pupate in the soil. In horses, the lesions are commonly seen over the withers and are often “blind” in that the larvae do not complete their development. Fatalities resulting from aberrant migration into the central nervous system are reported in horses.
Histologically, the cellular reaction is composed of neutrophils and eosinophils, but may be pyogranulomatous to granulomatous. It is the eosinophilic infiltrate that gives “butcher's jelly” its green coloration. However, the most intense inflammatory reactions occur at sites of previous migration rather than around the viable larvae, suggesting that in naive hosts the parasites depress any effective host responses. Proteinases with the capacity to cleave bovine complement C3 have been isolated from the first-instar larvae of H. lineatum. Such enzymes could well ablate the host's inflammatory responses. The actual “warble” is lined by a wall of granulation tissue that matures to form a connective tissue capsule in which lie islands of eosinophils. The cystic cavity between the cuticle of the parasite and the granulation tissue fills with fibrin and a few inflammatory cells, chiefly eosinophils. Cuticle sloughed during ecdysis, or remnants of dead larva, incite a marked foreign-body giant cell reaction. Once the larvae emerge, the cavity is repaired by fibrosis, but small foreign-body granulomas may persist for months.
Warbles are economically important. The buzzing of the adult H. bovis (H. lineatum is silent) disturbs cattle, causing considerable loss in milk and meat production. Larval tracks in the tissues decrease carcass value, and the larval-induced holes markedly depreciate the value of the hide. Larval rupture, either accidental or deliberate, may induce a fatal anaphylactic reaction. This may result from systemic effects of the warble toxin, from type I hypersensitivity reactions or a combination of both.
Further reading
Baron RW. Cleavage of purified bovine complement component C3 in larval Hypoderma lineatum (Diptera: Oestridae) hypodermins. J Med Entomol 1990;27:899-904.
Guo RM, Fu GZ. Report on the infestation of Hypoderma lineatum infestation in sheep. Chin J Vet Med 1986;12:16-17.
Oryan A, Bahrami S. Pathology of natural Przhevalskiana silenus infection in goats. Trop Biomed 2012;29:524-531.
Otranto D, et al. A third species of Hypoderma (Diptera: Oestridae) affecting cattle and yaks in China: molecular and morphological evidence. J Parasitol 2004;90:958-965.
Panciera RJ, et al. Eosinophilic mediastinitis, myositis, pleuritis, and pneumonia of cattle associated with migration of first-instar larvae of Hypoderma lineatum. J Vet Diagn Invest 1993;5:226-231.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Calliphorine myiasis.
Calliphorine myiasis (blowfly strike) is a common disorder of large animals in most areas of the world. It is most common in sheep and can be of major economic importance. The flies involved are members of the subfamily Calliphoridae (blowflies). Important blowfly genera are Lucilia, Calliphora, Condylobia, Protophormia, Phormia, and Chrysomia. The larvae (maggots) adopt a facultative parasitic mode, which is an adaptation of their beneficial and important role in the breakdown of carrion. Adult flies lay eggs on moist, warm skin of weakened or debilitated animals, in wounds or areas of heavy soiling with feces, urine, or other body fluids. Hence any species of animal can be susceptible.
Moisture, whether provided by rain, dew, urine, sweat, or inflammatory exudate, predisposes to bacterial proliferation. The odor induced by the bacterial proliferation and resultant inflammatory exudate attracts the primary flies, which deposit batches of 50-200 ova. The larvae of primary flies emerge within 12-24 hours and grow rapidly, feeding on inflammatory exudates. The primary larvae secrete proteolytic enzymes, including collagenases, which liquefy the host tissues and provide predigested nutrients. The cutaneous necrosis that results attracts the secondary flies to oviposit. The resulting larvae tunnel into the adjacent viable tissue and markedly expand the lesion. The putrefactive odor attracts more flies, and the process is further exacerbated. The lesions of fly strike are often extensive and leave large areas of undermined skin with punched-out holes. The subcutaneous tissues may become cavitated. Muscle may be destroyed and body cavities invaded. Lesions may result in death from shock, debilitation, toxemia, or bacterial septicemia.
The species of fly involved in fly strike differs with geographic location: Lucilia cuprina is the most important primary fly in Australia, Phormia regina in the United States and Canada, and Lucilia sericata in Great Britain. Several different species of flies are involved in the development of the lesion of cutaneous myiasis. Primary flies, such as L. cuprina, are capable of initiating a strike on living animals. Secondary flies, such as Chrysomia rufifaces, are not able to initiate a strike, but greatly exacerbate the lesions initiated by the primary fly. They may also displace the maggots developing from the eggs laid by the primary fly. Tertiary flies, such as the housefly Musca domestica, attack at a later stage and do not contribute significantly to the skin damage.
The development of fly strike depends upon abundance of primary flies, susceptible animals, and moisture. The prevalence of the disease tends to follow the rise and fall in the population of primary flies. In general, the flies require warm and moist but not hot conditions. Thus there is usually a double wave of primary flies, peaking in the spring and autumn. In sheep, the lesions are most common in the perineum (breech strike), particularly in sheep with a narrow conformation and/or marked skin wrinkling, which favor urine or fecal soiling. Lesions may affect the preputial orifice (pizzle strike), particularly in animals with narrow urethral orifices, which predispose to urine soiling. Rams with deep head folds may develop poll strike, possibly predisposed to by fight wounds. Wound strike occasionally follows castration or tail docking, and body strike follows prolonged wetting, which in turn predisposes to fleece rot or dermatophilosis.
Gross lesions consist of “honeycombed” foul-smelling ulcers with scalloped margins that are filled with larvae (maggots). The lesions are irritating and pruritic. Occasionally, the maggots migrate deeper into the muscle.
Further reading
Colditz IG, et al. Production of antibodies to recombinant antigens from Lucilia cuprina following cutaneous immunisation of sheep. Vet Parasitol 2002;104:345-350.
Hall MJ. Traumatic myiasis of sheep in Europe: a review. Parasitologia 1997;39:409-413.
Hendrix CM. Facultative myiasis in dogs and cats. Compend Contin Educ Pract Vet 1991;13:86-93.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Screwworm myiasis.
Screwworm flies differ from blowflies in that screwworm fly larvae are obligate parasites, invading edges of fresh, uncontaminated wounds on live animals. Cochliomyia hominivorax and C. macellaria occur in North, Central, and South America. The African and Asian screwworm fly is Chrysomyia bezziana. Eradication programs have led to a significant reduction in this condition in North and Central America.
Screwworm myiasis affects all domestic animals and humans and is an important cause of mortality in wildlife. The flies oviposit in cutaneous wounds, such as those caused by castration, dehorning, branding, or accidental injuries. The navel of neonatal calves, the perineum of recently calved cows, and tick bites are also favorable sites for oviposition. The larvae feed in groups, to penetrate and liquefy fresh, live host tissue with the aid of proteolytic enzymes. Blood-stained fluid, often containing incompletely digested shreds of tissue, oozes from the wound, which contains clusters of voraciously feeding larvae. A distinctive and particularly foul odor emanates from the lesion. The lesions are extremely painful and pruritic and may expand rapidly, leading to death from toxemia and septicemia in untreated animals. Screwworm infestation is a reportable condition in many countries.
Further reading
Hendrix CM. Facultative myiasis in dogs and cats. Compend Contin Educ Pract Vet 1991;13:86-93.
Litjens P, et al. Characterization of the screwworm flies Cochliomyia hominivorax and Cochliomyia macellaria by PCR-RFLP of mitochondrial DNA. Med Vet Entomol 2001;15:183-188.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Wyss JH. Screwworm eradication in the Americas. Ann N Y Acad Sci 2000;916:186-193.
Sheep ked infestation
Melophagus ovinus (Diptera: Hippoboscidae) is a wingless fly that causes chronic, pruritic dermatitis of sheep. Goats are also affected. Of worldwide distribution, the disease's chief economic importance is the associated loss of wool production.
Melophagus ovinus is an obligate ectoparasite. The eggs develop into larvae within the female until they are ready to pupate. The female attaches its larva to wool fibers with the aid of a sticky substance. The immotile larva transforms into a chestnut-brown pupa ~3-4 mm long. The pupal stage lasts 3-5 weeks, and the adult keds live 4-5 months. The adults are 4-7 mm and red-brown. They prefer the sides of the neck and body and are difficult to detect in fully fleeced animals. Severe pruritus leads to broken wool, alopecia, and excoriations. Heavy infestations can lead to anemia and stained wool from fly excrement. Wool loss and vertical ridging of the skin leads to a condition referred to as “cockle.” The irritation induced by the bites also affects weight gain. Sheep keds can transmit several important infectious agents such as bluetongue virus.
Histologic lesions reported are superficial and deep perivascular dermatitis, with eosinophils and lymphocytes predominating. Fibrinoid necrosis of small arterioles is also described.
Further reading
Arundel JH, Sutherland AK. Animal Health in Australia. Ectoparasitic Diseases of Sheep, Cattle, Goats and Horses, vol. 10. Australian Government Publishing Service; 1988. p. 69-72.
Mehlhorn H, et al. In vivo and in vitro effects of imidacloprid on sheep keds (Melophagus ovinus): a light and electron microscopic study. Parasitol Res 2001;87:331-336.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Horn fly dermatitis
Although mainly an obligate parasite of cattle, the horn fly (Haematobia irritans) is one cause of seasonal ventral midline dermatitis in the horse. In cattle, the flies feed in groups primarily on the back, withers, and head. They leave the animal only briefly to mate and lay eggs. Horn flies require fresh bovine feces to lay eggs. Large numbers of horn flies in cattle can result in significant loss of blood, wounds that attract other flies, and in loss of production. H. irritans is also thought to transmit the skin parasitic nematode of cattle, Stephanofilaria stilesi.
Haematobia irritans was associated with teat atresia in a herd of Limousin cattle in Texas. Only first-calf heifers were affected. A cord of firm tissue was palpated in the area of the teat canal in the majority of teats of the affected calves. Histologically, the papillary duct was replaced by mature fibrous connective tissue. The teat and mammary skin of all glands had fibrosis and superficial and deep, perivascular and interstitial dermatitis with perivascular mast cells and fewer eosinophils. Institution of a horn fly control program eliminated the problem in this herd.
In horses, horn flies cluster on the ventral abdomen (and occasionally on the neck or periocular region), producing bites marked by tiny drops of dried blood. A few days later pruritic, scaling, alopecic patches develop. These become lichenified and heal with either leukoderma or melanosis. The lesions are often single, usually well circumscribed, and occur near the umbilicus. Pruritus is variable. Histologically, lesions are perivascular and eosinophilic, typical of many insect-bite–induced dermatopathies. If ulcerated, lesions predispose to infection by Habronema spp. nematodes. Lesions of Culicoides hypersensitivity (see Immune-mediated dermatoses) and onchocerciasis may also occur on the ventrum, but these are diffuse, often extending from the axillae to the groin. Both Culicoides hypersensitivity and onchocerciasis are sporadic diseases, whereas up to 80% of horses in a group may be affected with horn fly–bite dermatitis.
Further reading
Barros AT. Dynamics of Haematobia irritans irritans (Diptera: Muscidae) infestation on Nelore cattle in the Pantanal, Brazil. Mem Inst Oswaldo Cruz 2001;96:445-450.
Edwards JF, et al. Bovine teat atresia associated with horn fly (Haemotobia irritans irritans [L.])–induced dermatitis. Vet Pathol 2000;37:360-364.
Perris EE. Parasitic dermatoses that cause pruritus in horses. Vet Clin N Am Equine Pract 1995;11:14-15.
Mosquito-bite dermatitis
Mosquito bites in animals are common, and the bite itself is of little consequence most of the time. Mosquitoes serve as vectors for a number of important diseases, including malaria in humans, canine and feline heartworm disease, equine viral encephalitis and equine infectious anemia, and rabbit myxomatosis. In cats, mosquito bites can induce a severe papular, crusting dermatitis characterized by dense eosinophilic infiltrates. Experimental studies in cats, by using intradermal skin tests and Prausnitz-Kustner tests, indicate that these lesions develop only in cats hypersensitive to mosquito-bite antigens and are initiated by a type I hypersensitivity reaction. The disease is seasonal and often pruritic. Clinically, cats initially develop wheals progressing to erythematous papules and plaques that eventuate into crusted, ulcerated, and sometimes hypopigmented lesions (Fig. 6-113A, B ). Sparsely haired regions of the body are most often affected, such as the bridge of the nose, the pinnae, and pawpad margins. The pinnae may develop symmetrical lesions of miliary dermatitis. The severity of lesions varies by individual, leading to scar formation in the more severe cases.
Figure 6-113.

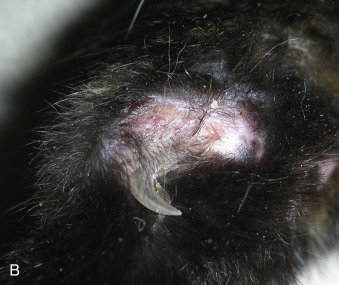
Mosquito-bite dermatitis in a cat. A. Ulcerative and depigmented lesions on the bridge of the nose and nasal planum. B. Similar lesions on the pawpad margin.
(Courtesy M.S. Canfield.)
Histologic lesions include intraepidermal eosinophilic microabscessation and perivascular to diffuse interstitial infiltrates of eosinophils, mast cells, macrophages, and lymphocytes. The epidermis is often spongiotic and hyperplastic. Nodular eosinophilic granulomas with collagen flame figures may be present. Infiltrative and necrotizing eosinophilic and mural folliculitis with mucinosis are common findings. Cats may have regional lymphadenopathy and peripheral eosinophilia.
Miscellaneous insects
Fire ants have a venomous bite. The venom is composed of solenopsin A, which is cytotoxic and hemolytic. Skin lesions include erythematous variably pruritic swellings to a pustular rash, with each pustule surrounded by an erythematous halo. Lesions usually resolve within 48 hours. Histopathologic findings vary. The pustular lesions are neutrophilic intraepidermal pustules with interstitial neutrophilic dermatitis. The swellings tend to be vertically oriented bands of full thickness dermal necrosis surrounded by edema and eosinophils.
Certain caterpillar larvae can cause cutaneous reactions most commonly in dogs. Pine and oak caterpillars (Thaumetopoea spp.) have bristles that contain thaumetopoein, which causes mast cell degranulation and histamine release. Skin lesions are most common on the lips and muzzle and include urticaria, facial pruritus, angioedema, or necrosis. The tongue may also be involved.
Further reading
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Nagata M, Ishida T. Cutaneous reactivity to mosquito bites and its antigens in cats. Vet Dermatol 1997;8:19-26.
Power HT, Ihrke PJ. Selected feline eosinophilic skin diseases. Vet Clin N Am: Small Anim Pract 1995;25:838-840.
Lice
Lice are host-specific obligate parasites of the class Insecta. They are dorsoventrally flattened wingless insects that are common ectoparasites in most parts of the world. Two orders of lice are recognized. The Mallophaga are chewing lice that have mouth parts specially adapted for feeding on the epithelial scales, feathers, and sebaceous secretions of birds and mammals. The Anoplura have piercing mouth parts and are the sucking lice of mammals. Lice spend their complete life cycle on the host and cannot live away from their hosts for more than a few days. Nits (1-2 mm–long operculated eggs) are attached to hairs by a clear adhesive secretion by female lice (3-6 mm). Spread of infection occurs most commonly via direct contact, but transmission via indirect contact also occurs. Because various species of lice have adapted to different microenvironments within the host pelage, it is possible for an animal to carry several species at once.
Infestation with lice is called pediculosis. It tends to be a seasonal problem, being worse in winter. Lice do not breed at temperatures above 30° C and die at temperatures around 50° C. The signs associated with pediculosis are extremely variable. In most instances, lice do not pose a significant threat to the host. Heavy infestations signal an underlying contributing condition, such as poor sanitation, overcrowding, ill thrift, or poor nutrition. In some cases, animals are asymptomatic carriers or only have scaling with variable pruritus. Most lesions result from skin irritation and pruritus, which ranges from mild to severe. Lesions include scaling, crusting, erythema, papules, excoriations, hair loss, and damage to wool or hide caused by rubbing or biting. Sucking lice may induce anemia, especially in young animals, that is occasionally fatal in heavy infestations. Weight loss and decreased milk production are associated with the constant irritation seen in some lice infestations.
Lice are usually host specific, but Heterodoxus longitarsus, normally parasitic on kangaroos, has become an important ectoparasite of Australian dogs. Phthirus pubis, the human crab louse, has been reported to infest dogs living with infested humans. The dog louse, Heterodoxus spiniger has been detected on cats in several countries. Poultry lice feed on horses, dogs, and cats.
Louse infestation occurs in cattle more often than in other domestic species. Haematopinus eurysternus, the short-nosed louse; H. quadripertusus, the tail-switch louse; H. tuberculatis, the buffalo louse; Linognathus vituli, the long-nosed louse; and Solenoptes capillatus, the little blue cattle louse are sucking lice of cattle. Damalinia (Bovicola) bovis is the one chewing species. The various species have preferred habitats. Damalinia bovis tend to cluster about the neck, withers, and tail head. Sucking lice are commonly found on the poll, pinnae, muzzle, periocular region, neck, brisket, withers, tail, axillae, and groin. Heavy periorbital infestation of heifers by H. quadripertusus has caused keratoconjunctivitis and periorbital papillomatosis. Bovine pediculosis usually has little deleterious effect on weight gain and other production parameters. Economic consequences are due to deterioration of hide quality, damage to fences, and costs of treatment. One exception is H. eurysternus infestation, which may cause anemia and death in some uniquely susceptible cattle. L. vituli has been associated with severe anemia and mortality in young buffaloes. Sucking lice can serve as vectors of severe diseases, including anaplasmosis, theileriosis, and dermatomycosis.
The species of sucking lice affecting sheep include Linognathus ovillus (the face or blue louse), L. africanus (also called the blue louse), and L. pedalis (the foot louse). Damalinia ovis is a chewing louse and is most common over the dorsum. L. ovillus affects the face, and L. pedalis the legs and scrotum. Although goat and sheep lice are considered host specific, there are reports of naturally occurring transmission of the goat louse Damalinia caprae to sheep and experimental transmission of D. ovis to goats.
In goats, the sucking lice are Linognathus stenopsis and L. africanus. The chewing lice are Damalinia caprae, D. limbata, and D. crassipes. Lice are most commonly seen on the head, neck, dorsum, and groin. The haircoat of Angora goats may be seriously damaged by the irritation induced by pediculosis.
Two species of lice occur on horses. Haematopinus asini, a sucking louse, prefers the head, neck, back, thighs, and fetlocks. Werneckiella (Damalinia) equi, a chewing louse, favors the head, mane, and base of the tail. The populations of lice fluctuate considerably, being highest when the hair is long as in winter or in debilitated animals that have not shed their hair. In warm weather, the populations decline but some lice persist in the long hair of the mane and tail.
One species, Haematopinus suis, a sucking louse is parasitic on pigs. Preferential sites include the ears and skin folds of the neck, axillae, flanks, and inguinal areas. The lice are vectors for swinepox virus, African swine fever virus, and Eperythrozoon suis.
Pediculosis in alpacas is caused by 2 species of lice: Bovicola (Lepikentron) breviceps, a chewing louse and Microthoracius mazzi (praelongiceps), a sucking louse. B. breviceps is also known to affect llamas. Chewing lice may be more numerous on the rump, dorsal trunk, and neck, and sucking lice on the head, neck, and shoulder.
Linognathus setosus is a sucking louse, and Trichodectes canis and Heterodoxus spiniger are chewing lice of dogs. Trichodectes canis may serve as an intermediate host for the tapeworm, Dipylidium caninum. Pediculosis is a rare disease in pet dogs. Breeds with moderately long, fine hair may provide a more favorable environment for lice, and the disease is more prevalent in the cooler winter months. Lice accumulate under mats of hair and around the ears and body openings. Pediculosis may resemble flea-bite hypersensitivity in dogs. Infestation in the absence of pruritus may be an incidental finding.
Only one species, the chewing louse, Felicola subrostratus, occurs on cats. Infestation may be an incidental finding, or it may be associated with severe pruritus with dermatitis and hair loss over the back. Pediculosis may resemble miliary dermatitis in cats.
Further reading
Arther RG. Mites and lice: biology and control. Vet Clin North Am Small Anim Pract 2009;39:1159-1171.
Cortinas R, Jones CJ. Ectoparasites of cattle and small ruminants. Vet Clin North Am Food Anim Pract 2006;22:673-693.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Norhidayu S, et al. The dog louse Heterodoxus spiniger from stray cats in Penang, Malaysia. Trop Biomed 2012;29:301-303.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Twomey DF, et al. Confirmation of the chewing louse, Bovicola breviceps, in a British llama (Lama glama) herd. Vet Rec 2010;166:790-791.
Yeruham I, et al. Keratoconjunctivitis and periorbital papillomatosis associated with heavy periorbital infestation by the tail louse Haematopinus quadripertusus in heifers. J Vet Med B Infect Dis Vet Public Health 2001;48:133-136.
Fleas
Fleas are ubiquitous and obligate parasites, and their survival depends upon temporary episodes of feeding and a habitat where the host is periodically available. Fleas are wingless and have a laterally compressed body. They primarily parasitize hosts that return on a regular basis to a nest, burrow, bedding, or lair. Hence animals such as ungulates rarely have fleas, and carnivores, rabbits, rodents, and bats often do. Most fleas can parasitize a range of hosts. An exception to this general rule is the more recent finding that cat fleas spend more of their lifetime on the cat than fleas infesting other species. Fleas are chiefly a problem in cats, dogs, pigs, and humans. Flea bites damage the host by irritation, pruritus, blood loss, and possible transmission of infectious agents. Ctenocephalides felis felis, the cat flea; Ctenocephalides canis, the dog flea; and Pulex irritans, the human flea are intermediate hosts for the dog tapeworm Dipylidium caninum and the filarid nematode Acanthocheilonema (Dipetalonema) reconditum. Fleas are also vectors for Rickettsia spp., Bartonella spp., Haemoplasma (Mycoplasma) spp., the promastigotes of Leishmania spp., Francisella tularensis, Yersinia pestis, and rabbit myxomatosis. Flea saliva is injected into the host as the flea feeds, leading to hypersensitivity reactions in some animals.
Fleas are the most common ectoparasites of cats and dogs. The most important species are Ctenocephalides felis felis, the cat flea, and C. canis, the dog flea. However, infestations also occur with P. irritans (human flea), Leptopsylla segnis (rat flea), Echidnophaga gallinacea (chicken stick-tight flea), Spilopsyllus cuniculi (European rabbit flea), and Ceratophyllus spp. (bird and hedgehog fleas). C. felis felis is the most common flea found on both dogs and cats in North America and northern Europe.
The clinical manifestations of flea infestation are highly variable. Most species of fleas move freely around their host's body and can be found virtually anywhere. In general, C. felis felis prefers the rump and inguinal areas. E. gallinacea has a preference for the face. S. cuniculi, the rabbit flea, has a preference for the pinnae and periauricular region. Typically, hunting cats, primarily in parts of Europe and Australia, acquire the infestation from their prey. Macroscopic lesions are crusted, alopecic papules on both aspects of the pinnae and periauricular areas. Histologically, there are perivascular to interstitial eosinophils. Tunga penetrans, most common in South America and Africa, burrows into the skin and produces significant damage at the site of attachment. Some animals, despite heavy infestations, remain asymptomatic carriers. Some animals may develop flea-bite dermatitis, which is a reaction to the many irritant substances in the flea's saliva, but the vast majority of animals that develop lesions do so because of hypersensitivity reactions to allergenic components of the flea saliva. Flea-allergy dermatitis is an extremely common and very important disease of the dog and cat; it is discussed in detail under Immune-mediated dermatoses. Finally, the blood-sucking activities of fleas may induce blood loss, iron deficiency anemia in heavily infested animals, particularly in kittens, puppies, or debilitated adults.
The 2 fleas most commonly associated with swine are the human flea (P. irritans) and the chicken stick-tight flea (E. gallinacea). Infestation with C. felis felis and C. canis have also been reported. In Africa, Tunga penetrans, the chigoe flea or jigger, has been associated with swine infestations, although it is chiefly a human parasite. The female flea burrows into the skin, causing ulcerative lesions. Favored sites are the skin around the coronary band, on the scrotum, and on the snout. Infestations of the teat canal have been associated with agalactia in sows. Fleas may act as vectors for swinepox virus. Heavy infestations with Ctenocephalides spp. in Africa lead to anemia, reduced weight gain, and even death in sheep and goats, particularly in the young. Fleas may also trigger allergic dermatitis in sheep. C. felis felis has been rarely reported in cattle. Heavy infestation with C. felis felis was reported to cause mortality in calves, lambs, and kids in Israel. Rarely, horses may become infested with C. felis felis, E. gallinacea, or T. penetrans. Dermatologic signs include various degrees of rubbing, scratching, chewing, alopecia, excoriations, nonfollicular papules, and crusts. The face, distal limbs, and trunk are typical sites. Heavily infested animals can become anemic.
Further reading
Dobler G, Pfeffer M. Fleas as parasites of the family Canidae. Parasit Vectors 2011;4:139-151.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Studdert VP, Arundel JH. Dermatitis of the pinnae of cats in Australia associated with the European rabbit flea (Spilopsyllus cuniculi). Vet Rec 1988;123:624-625.
Traversa D. Fleas infesting pets in the era of emerging extra-intestinal nematodes. Parasit Vectors 2013;6:59-74.
Visser M, et al. Species of flea (Siphonaptera) infesting pets and hedgehogs in Germany. J Vet Med B Infect Dis Vet Public Health 2001;48:197-202.
Yeruham I, et al. Mortality in calves, lambs and kids caused by severe infestation with the cat flea Ctenocephalides felis (Bouché, 1835) in Israel. Vet Parasitol 1989;30:351-356.
Yeruham I, et al. Seasonal allergic dermatitis in sheep associated with Ctenocephalides and Culicoides bites. Vet Dermatol 2004;15:377-380.
Mites
Sarcoptic mange
Sarcoptes scabiei (Acarina: Sarcoptidae) is responsible for scabies (sarcoptic mange) in humans and many species of mammals worldwide. It is known to cause severe disease in a number of wildlife species. This species of mite has been divided into morphologically indistinguishable host-adapted varieties that rarely cross-infect between species of animals. Most can parasitize people but will not complete their life cycle on a human. People in contact with infected animals often develop lesions, most commonly pruritic erythematous papules. Sarcoptic mange is common in pigs, dogs, and goats and is uncommon to rare in cattle, sheep, horses, and cats. It is the most important ectoparasite of swine. In regions where ivermectin is used regularly in large animal species, this condition is much less common. It is a reportable disease in some countries.
In the normal host, the parasite completes its life cycle in tunnels burrowed into and under the stratum corneum. After mating in a “molting pocket” close to the surface, the female burrows through the stratum corneum to feed on cells of the stratum granulosum and stratum spinosum and lasy ~1-4 eggs per day for ~6 weeks before dying. The eggs develop through the larval and nymphal stages in the same tunnel or in new ones, to reach maturity in 10-15 days, depending on the host species. The entire cycle takes 2-3 weeks. In general, both parasites and ova have poor viability in the external environment; however, low temperature and high humidity may allow some mites and nymphs to persist in the environment up to 21 days. The disease, which is highly contagious, is transmitted largely by direct contact, but may occur following indirect contact with contaminated objects such as bedding. The adult female mite is 200-400 µm in diameter, oval and white with 2 pairs of short legs anteriorly that bear long unjointed stalks with suckers. Two pairs of posterior legs are rudimentary but carry long bristles, and there is a terminal anus.
The pathogenesis of lesions in S. scabiei infestation is due to direct damage inflicted by the parasite mechanically, by the irritant effects of its secretions and excreta, and by an allergic reaction developed against mite antigens, including proteins in the cuticle, saliva, and feces. Scabies is a complex hypersensitivity reaction involving both humoral and cell-mediated components and circulating immune complexes. In an otherwise normal infected individual, a cell-mediated immune response is mounted against mite antigens, and this acquired immunity limits the spread of mites, preventing overwhelming infestation. In undernourished or immuno-compromised individuals, there may be widespread lesions and large numbers of mites.
In most animal hosts, sarcoptic mange is an intensely pruritic disease, and typically multiple animals are affected. In a herd situation, there may be decreased feed intake, weight loss, decreased milk production, hide and fiber damage, difficulty in breeding, and secondary bacterial infections and myiasis. In some wildlife species, sarcoptic mange is very severe and can lead to death. The cause for this is not completely understood but may be related to scarcity of food and animals spending much less time feeding because of intense pruritus. In addition, severe skin lesions can lead to ulceration, myiasis, secondary bacterial infections, toxemia, and sepsis.
The primary parasite-related lesions of sarcoptic mange are erythematous, crusted, nonfollicular papules that progress to scaling, oozing, larger crusts, and alopecia. Peripheral lymphadenopathy may be marked. In animals with heavy mite infestations, the lesions are characterized by alopecia, marked lichenification, accumulation of thick gray scale-crust, and fissuring. Chronic hypersensitivity lesions include excoriations, marked alopecia, scaling, and lichenification.
The distribution of the lesions is characteristic in the various species. In pigs, sarcoptic mange is caused by S. scabiei var. suis, and 2 clinical syndromes exist. The most common (hypersensitivity) form is seen mostly in young growing pigs, with intense pruritus. Lesions include papules, crusts, and excoriations on and in the ears. Aural hematomas sometimes develop. Subsequently, a widespread maculopapular eruption appears over the rump, flanks, and abdomen. In chronic cases, there is lichenification with crusts. The second (hyperkeratotic, chronic) form is seen in multiparous sows or debilitated animals. Lesions include thick asbestos-like crusts on the pinnae, head, neck, and legs. Pruritus is moderate to severe.
In dogs, the condition is caused by S. scabiei var. canis, and the preferred sites are the lateral elbows, hocks, ventral thorax and abdomen, and lateral margin of the pinna. The vast majority of dogs have widespread lesions, but some dogs have localized lesions limited to one area of their body. Localization to the face or pinnae is most common. In most cases, the dorsum is spared. Asymptomatic carriers exist, and some dogs are minimally pruritic. Dogs with compromised immune systems, resulting from coexistent immunosuppressive disease or therapy with corticosteroids or cytotoxic drugs, may be infested by much larger populations of mites.
Infestation with S. scabiei can occur rarely in cats. The primary lesions are crusting on the pinnae, bridge of the nose, paws, and tail. In contrast to most other animal hosts, affected cats are often nonpruritic and mites are easily found with deep skin scrapings. In some cases, the condition in cats has been likened to “crusted scabies” or “Norwegian scabies” in humans. Crusted scabies tends to occur in patients with impaired cell-mediated immunity, and mites multiply unchecked and reach extremely large numbers in skin and scale. The skin reacts to the infestation by increasing keratinocyte turnover, which leads to thick adherent crusts. In humans with Norwegian scabies, pruritus is absent in up to 50% of cases.
In cattle, scabies is caused by S. scabiei var. bovis (“head mange”), the lesions chiefly affect the face, pinnae, neck, shoulders, and rump but may become generalized. The disease in goats, caused by S. scabiei var. caprae, causes lesions most commonly on the face, pinnae, neck, and legs but may become generalized (Fig. 6-114A ). Scabies in sheep is caused by Sarcoptes scabiei var. ovis. Lesions are most common on the nonwooled regions, such as the face, in particular the lips, nostrils, external surface of the pinna, and occasionally the legs. Generalized lesions occur in the more hairy desert sheep of the Sudan. Sarcoptic mange, caused by S. scabiei var. equi, is rare in horses. Lesions begin on the head, pinnae, and neck and may spread caudally.
Figure 6-114.

Sarcoptic mange. A. Alopecia and thick crusts over the pinna, face, and neck of a goat.
(Courtesy I. Yeruham.)
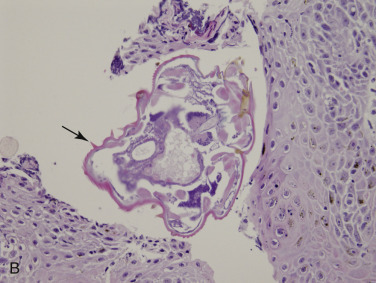
B. Note the dorsal spines (arrow) on the mite burrowing into the epidermis of a dog.
In alpacas, sarcoptic mange, caused by S. scabiei var. auchinae, is a significant cause of weight loss and decreased fiber production in alpacas. The disease often begins on the ventral abdomen and chest, axillae, and groin, with gradual extension to the medial thighs, prepuce, perineum, legs, interdigital spaces, face, and pinnae.
Histologically, lesions vary with the balance between allergic reaction and parasitic infestation and chronicity. Definitive diagnosis requires demonstration of the parasite. Rarely, sections of mites or ova may be present within the epidermis or surface crusts (Fig. 6-114B). Lesions consist of a mild to severely hyperplastic epidermis with variable orthokeratotic to patchy parakeratotic hyperkeratosis. In fully developed lesions, there is marked spongiosis, mixed leukocytic exocytosis, serocellular crusts, and possibly intraepidermal eosinophilic pustules. Vasodilation, endothelial swelling, and edema may also be present. Immunosuppressed animals with large numbers of adult mites in epidermal burrows often have a markedly parakeratotic stratum corneum. Dermal lesions consist of a mild to moderate superficial to mid-level perivascular to interstitial infiltrate with a variable ratio of lymphohistiocytic cells and eosinophils. The chronic allergic lesions reflect continued trauma, with dermal fibrosis, epidermal hyperplasia with prominent rete ridge formation, hyperpigmentation, and a predominantly mononuclear cell perivascular infiltrate.
Diagnosis of the typical allergic form of the disease depends chiefly on the clinical signs of extreme pruritus and the nature and distribution of the cutaneous lesions. Mites are characteristically difficult to demonstrate, either in skin scrapings or in microscopic section. Approximately 50-80% of affected dogs fail to yield parasites even when multiple scrapings are performed. Mites are more commonly recovered from puppies than adult dogs. The microscopic lesions are not diagnostic, being indistinguishable from other allergic and parasitic dermatoses that feature eosinophils. Fifty to 100% of dogs with scabies that have pinnal lesions will have a positive pinnal-pedal reflex. The most useful diagnostic procedure is response to appropriate therapy. In the chronic form of sarcoptic mange associated with poorly developed hypersensitivity reactions, mites are plentiful in scrapings and in tissue section.
Further reading
Dagleish MP, et al. Fatal Sarcoptes scabiei infection of blue sheep (Pseudois nayaur) in Pakistan. J Wildl Dis 2007;43:512-517.
Elbers AR, et al. Production performance and pruritic behaviour of pigs naturally infected by Sarcoptes scabiei var. suis in a contact transmission experiment. Vet Q 2000;22:145-149.
Fthenakis GC, et al. Effects of sarcoptic mange on the reproductive performance of ewes and transmission of Sarcoptes scabiei to newborn lambs. Vet Parasitol 2001;95:63-71.
Hollanders W, Vercruysse J. Sarcoptic mite hypersensitivity: a cause of dermatitis in fattening pigs at slaughter. Vet Rec 1990;126:308-310.
Huang H, Lien Y. Feline sarcoptic mange in Taiwan: a case series of five cats. Vet Dermatol 2013;24:457-459.
Little SE, et al. Responses of red foxes to first and second infection with Sarcoptes scabiei. J Wildl Dis 1998;34:600-611.
Malik R, et al. Crusted scabies (sarcoptic mange) in four cats due to Sarcoptes scabiei infestation. J Fel Med Surg 2006;8:327-339.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Morris DO, Dunstan RW. A histomorphological study of sarcoptic acariasis in the dog: 19 cases. J Am Anim Hosp Assoc 1996;32:119-124.
Pin D, et al. Localised sarcoptic mange in dogs: a retrospective study of 10 cases. J Small Anim Pract 2006;47:611-614.
Rahbari S, et al. Some observation on sheep sarcoptic mange in Tehran province, Iran. Trop Anim Health Prod 2009;41:397-401.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. A retrospective study of 350 dogs suspected of having scabies (1988-1998). Jpn J Vet Dermatol 2013;19:3-9.
Notoedric mange
Notoedres cati (Acarina: Sarcoptidae) is the cause of feline scabies and is also a parasite of the rabbit, and occasionally foxes, dogs, and humans. The disease in cats is uncommon to rare, although there are some endemic areas of higher prevalence. The mite has a life cycle similar to that of S. scabiei. The infestation is highly contagious, with transmission chiefly by direct contact. The major clinical sign is pruritus. The lesions in cats commence on the head and ears, particularly on the margin of the pinna but may extend to the neck, paw, or become generalized (Fig. 6-115A, B ). Female mites burrow into the horny layer of the epidermis between hair follicles. These burrows appear on the skin surface in the center of minute papules. Lesions include partial alopecia, thickening and wrinkling of the skin, and in chronic cases, the formation of tightly adherent yellow-gray crusts. There may be accompanying regional lymphadenopathy. Lesions in dogs are indistinguishable from sarcoptic mange. Histologically, the epidermis is hyperplastic to spongiotic, and there is eosinophil-rich, superficial perivascular to interstitial dermatitis with marked focal parakeratosis. Mite segments may be found within the superficial epidermis. The diagnosis is based on history, clinical signs, and demonstration of typical mites in section or skin scrapings. Notoedres spp. mites are readily found in skin scrapings from infected cats. These mites are smaller than S. canis and have medium-length unjointed sucker-bearing stalks on their legs, more body striations, and a dorsal anus, whereas Sarcoptes has a terminal anus.
Figure 6-115.
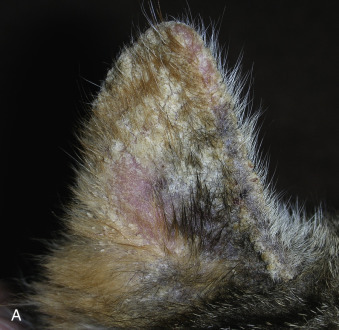

Notoedric mange in a kitten. A. Alopecia and thick adherent crust on the pinna. B. Alopecia, erythema and crusting on all paws and distal limbs.
(Courtesy M.S. Canfield.)
Further reading
Leone F. Canine notoedric mange: a case report. Vet Dermatol 2007;18:127-129.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Psoroptic mange
Psoroptic mange caused by Psoroptes mites (Acarina: Psoroptidae) is highly contagious and infests sheep, cattle, horses, rabbits, and goats as well as other nondomestic species. Humans are not susceptible. There are actually fewer species of psoroptic mites than originally thought, as mites from one host can often infect another host, and morphologic distinctions overlap. Based on critical literature review and molecular genetic analyses, the Psoroptes mites are conspecific, and, by rule of priority, belong to the one genus P. equi (Hering, 1838). Valid species include P. cervinus, P, cuniculi, P. natalensis, and P. ovis, and they are synonyms of P. equi. P. ovis infests sheep, cattle, goats, rabbits, and horses. P. cuniculi is an ear mite of several species, including rabbit, horse, donkey, mule, goat, and sheep, and is a body mite in horses. P. natalensis infests cattle, zebu, water buffaloes, and horses in South Africa, South America, and Europe. P. cervinus occurs as an ear mite in bighorn sheep and as a body mite in wapitis in the western part of the United States. Transmission occurs via direct and indirect contact.
Psoroptic mange is a serious disease in cattle and sheep and is a reportable disease in several countries. Bovine psoroptic mange showed a recrudescence in North America during the 1970s and early 1980s but has been brought under control by the effective use of ivermectin. Ovine psoroptic mange has been eradicated from many countries, including New Zealand, the United States, and Canada. The economic importance in sheep and cattle results from a marked decrease in weight gain, reduced milk production, reduced fleece weight and quality, occasional mortality, and costs related to prevention and eradication campaigns.
Psoroptic mites do not burrow into the outer epidermis, as do the sarcoptic mites, but instead complete their life cycle on the skin surface. Lipids from the stratum corneum provide a major source of nutrients in the early stages of infestation, probably supplemented by serous and hemorrhagic inflammatory exudates in the later stages.
Psoroptic mange is characterized by intensely pruritic dermatitis. The pathogenicity of the mite has been attributed to its local irritant effect on the epidermis, but this does not readily explain the marked loss of condition induced by Psoroptes infestation in some species, particularly cattle. The detrimental systemic effects may derive directly or indirectly from a chronic hypersensitivity reaction rather than from local dermatitis. The histologic lesions, in which the predominant inflammatory cells in the superficial dermis are eosinophils, mast cells, and lymphocytes, are consistent with an allergic pathogenesis. Constant pruritus resulting from allergy markedly reduces feed intake, and secondary bacterial infection or myiasis may further contribute to loss of condition. There is little evidence to support the hypothesis that the mites inoculate a toxic compound along with their saliva.
Histologically, lesions are similar in all species. The pattern of inflammation is superficial perivascular to interstitial dermatitis with predominantly spongiotic, exudative, or hyperplastic reactions, depending on chronicity. The eosinophil is the most numerous of the infiltrating leukocytes, followed by lymphocytes, other mononuclear cells, and mast cells. Eosinophilic microabscesses and focal areas of epidermal edema, leukocytic exocytosis, and necrosis may be found. Dermal edema may be marked. Mites are rarely seen but if present are both on top of and under the surface scale-crust. Sebaceous gland hyperplasia has been described in lesions in sheep and cattle.
Psoroptic mange in sheep, also called sheep scab, is common to uncommon in most parts of the world and is caused by Psoroptes ovis. Psoroptic mange may occur as a latent infection in which mites persist in the ears, infraorbital fossae, inguinal and perineal folds, and at the base of the horns. In rams, mites may be found on the scrotum or prepuce in small, dry lesions. Latency occurs in the summer months, when the fleece microclimate is less favorable to parasite proliferation. In autumn and winter or with debilitation of the host, the parasitic population explodes and lesions are induced. The withers and sides are particularly affected. The initial lesions are vesicles and yellow-green pustules that rupture, ooze, and develop into yellow crusts. The individual lesions expand at the periphery and may coalesce to become diffuse over most of the body surface. Fleece overlying the skin lesions becomes stained, moist, soiled, and matted. Tufts and clumps of matted wool may be shed or pulled out by self-trauma because of the intense pruritus. Affected sheep scratch, kick, rub, and tear out the fleece with their teeth.
Excoriations, ulcerations, and secondary myiasis and bacterial infections occur. In addition, P. cuniculi is an occasional cause of “ear mites” in sheep, and in some cases, clinical signs are limited to the ears and may be due to P. cuniculi or P. ovis. Aural hematomas may result from head shaking, rubbing, and scratching at the pinnae.
In cattle, psoroptic mange is sometimes referred to as body mange. It is uncommon to common in most parts of the world. Mite populations are usually higher during cold weather, and thus clinical signs are more severe in the winter. Lesions in naturally affected cattle usually commence about the poll, withers, or at the base of the tail, and chiefly result from persistent licking, rubbing, and scratching induced by intense pruritus. Early lesions include papules, pustules, exudation, and excoriations. Infested areas are fairly well defined as areas of alopecia. Alopecic areas become lichenified and covered by dry gray crusts and scales. Severely affected calves may develop mild anemia, lymphopenia, and marked neutropenia.
Psoroptic mange is uncommon in goats and is caused by P. cuniculi (the ear canker mite) and P. ovis (previously P. caprae). P. cuniculi is found in the ear canal, and clinically, signs range from absent to head shaking, ear scratching, and variable degree of excessive cerumen, crusted lesions on the inner surface, and alopecia on the outer surface of the pinna. Otitis media and otitis interna are possible if the tympanic membrane ruptures. In debilitated or stressed animals, thick brown-yellow, dry scale-crust accumulates on the inner aspect of the pinna and, rarely, spreads to involve the poll, body, and the legs. Concurrent Mycoplasma and P. cuniculi infections have been described in the ears of goats; however, Mycoplasma may be cultured from the ears of clinically normal animals, placing some doubt on the significance of the finding. P. ovis has been reported to cause otitis externa, crusts, scales, and alopecia of the pinnae, head, face, pasterns, and interdigital areas. Pruritus is variable.
In horses, P. cuniculi is found quite frequently in the ear. Clinical signs are variable, but when present, the main distribution is the topline affecting the ears, mane, and tail and, less commonly, the dorsal trunk. Infested horses may be asymptomatic. Signs of ear disease include head shaking, ear scratching, head shyness, or a lop-eared appearance. Pruritus is variable but can be intense. In mildly pruritic horses, there may be mane and tail seborrhea. In the more pruritic horses, there are commonly nonfollicular papules, crusts, excoriations, and alopecia. P. ovis (P. equi) infestations are rare; lesions are crusted papules with alopecia, and the preferred sites are at the base of the mane, forelock, and tail.
The mite responsible for psoroptic mange in alpacas has been referred to as P. communis var. auchinae. The varieties P. auchinae, P. cuniculi, and P. ovis, however, have not been officially named. The condition is usually pruritic, and lesions are most commonly present on the head, neck, and pinnae but can become more widespread, involving the shoulders, back, rump, sides, and perineum. In some cases, clinical signs are limited to the ears and include head shaking, ear twitching, scaling in the ear canals, and occasionally purulent exudate caused by secondary bacterial infections. Skin lesions include papules, crusts, exudation, and alopecia.
Further reading
Abu-Samra MT, et al. Five cases of psoroptic mange in the domestic donkey (Equus asinus asinus) and treatment with ivermectin. Equine Vet J 1987;19:143-144.
Corke MJ, Broom DM. The behaviour of sheep with sheep scab, Psoroptes ovis infestation. Vet Parasitol 1999;83:291-300.
Fourie LJ, et al. The growth of sheep scab lesions in relation to sheep breed and time of the year. Exp Appl Acarol 2002;27:277-281.
Losson BJ. Sheep psoroptic mange: an update. Vet Parasitol 2012;189:39-43.
Lusat J, et al. Mange in alpacas, llamas and goats in the UK: incidence and risk. Vet Parasitol 2009;163:179-184.
Perris EE. Parasitic dermatoses that cause pruritus in horses. Vet Clin North Am Equine Pract 1995;11:11-28.
Ramey RR, et al. Phylogeny and host specificity of psoroptic mange mites (Acarina: Psoroptidae) as indicated by ITS sequence data. J Med Entomol 2000;37:791-796.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Stromberg PC, Guillot FS. Pathogenesis of psoroptic scabies in Hereford heifer calves. Am J Vet Res 1989;50:594-601.
Zahler M, et al. Species of the genus Psoroptes (Acari: Psoroptidae): a taxonomic consideration. Exp Appl Acarol 2000;24:213-225.
Chorioptic mange
Chorioptic mange, most commonly caused by Chorioptes bovis (Acarina: Psoroptidae), affects horses, cattle, sheep, and goats. C. texanus has also been reported to affect cattle, goats, elk, and reindeer. Not host specific, C. bovis is an obligate parasite that lives on the surface of the skin. The mite populations tend to fluctuate considerably as a result of host and environmental factors. As with Sarcoptes spp. and Psoroptes spp. infestations, mite numbers and thus severity of clinical signs are more prominent in the winter. Mites do not survive, and numbers decline when the environment is hot and dry. Inapparent infections allow persistence in the population. Pruritus is variable. It is absent to intense in the horse, goat, and cattle; tends to be intense in sheep; and tends to be absent to mild in alpacas. Lesions usually occur as erythema and papules progressing to scaling, oozing, crusts, and alopecia. In some cases, lesions may become lichenified, depending upon the duration of the disease and the degree of self-trauma inflicted. The condition is contagious and transmission occurs via direct and indirect contact.
Chorioptic mange (foot mange, tail mange) is uncommon in cattle in most parts of the world. It predominantly affects housed dairy cows and is most prevalent in winter. Subclinical infections are probably quite common. The major clinical sign is pruritus, but this is not as severe as in sarcoptic or psoroptic mange. Chorioptic mange is, in general, a less serious condition than psoroptic mange in cattle, although a syndrome of highly pruritic coronitis was associated with falling milk production. The typical distribution of lesions is perineum, tail, scrotum, udder, and caudal areas of thigh, hindlimbs, and rump. Lesions are predominantly alopecia, erythema, lichenification, and wrinkling of the skin.
The disease in horses is common. As indicated by the colloquial name “leg mange,” lesions occur preferentially on the lower limb around the fetlock but may extend proximally to the thigh and ventral abdomen and rarely become widespread. Draft horses, with thick-feathered fetlocks, are affected more often.
Chorioptic mange is common in goats. Lesions are most common on the feet and hindlegs, although lesions can also be on the forelegs, perineum, tail, udder, teats, scrotum, ventrum, and may spread to the lateral trunk, neck, and face.
In sheep, chorioptic mange (foot mange, scrotal mange) is uncommon in most parts of the world. Lesions are more common in the nonwooled regions, particularly lower hindlimbs (including pastern and interdigital skin) and scrotum. The scrotum may be affected, and the resultant scrotal dermatitis may lead to infertility in rams. Lesions may also be present on the forelegs, udder, teats, and rump. Severe infestations can reduce growth rates and milk and meat yields. Chorioptic mange has been eradicated from the sheep population in the United States. It is a reportable disease in some countries.
Chorioptes bovis is the most common mite infestation of alpacas. Lesions include scale, crust, and alopecia on the ventral tail, perineal region, ventral abdomen, and medial thighs (Fig. 6-116A ). Lesions can spread to the axillae, tips and lateral surface of the pinnae, face, neck, dorsum, and feet. In severe cases, erosions, ulcers and lichenification can be seen. Interestingly, heavily infested alpacas can be clinically normal, and alpacas with extensive lesions can have low numbers of mites.
Figure 6-116.

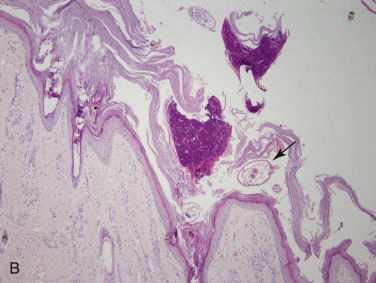
Chorioptic mange in an alpaca. A. Alopecia, crusting, and lichenification of the distal hindlimbs. B. Mild perivascular dermatitis with marked hyperkeratosis. Note the cross-sections of mites (arrow) within the surface keratin.
Definitive diagnosis is based on history, physical examination, and demonstration of mites by scraping, brushing, or combing affected areas and examining those samples microscopically. Mites are active, fast moving, and usually easy to demonstrate during cool weather. Histopathology reveals variable degrees of superficial perivascular to interstitial dermatitis with numerous eosinophils. Eosinophilic epidermal microabscesses and focal epidermal edema, exocytosis, and necrosis (“epidermal nibbles”) may be seen. Mites are not usually seen in skin biopsy specimens (Fig. 6-116B).
Further reading
Sargison ND, et al. Chorioptic mange in British Suffolk rams. Vet Rec 2000;147:135-136.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Skin diseases in the alpaca (Vicugna pacos): a literature review and retrospective analysis of 68 cases (Cornell University 1997-2006). Vet Dermatol 2010;22:2-16.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Suh G, et al. The first outbreak of Chorioptes texanus (Acari: Psoroptidae) infestation in a cattle farm in Korea. Korean J Parasitol 2008;46:273-278.
Otodectic mange
Otodectes cynotis (Acarina: Psoroptidae) is an obligate parasite of the external skin surface of dogs, cats, and ferrets. Although the mite may be found at several body sites, its preferred habitat is the external ear canal. The major lesion is thus otitis externa (see Vol. 1, Special senses). Focal, erythematous, alopecic, or excoriated lesions occur occasionally on the face, paws, neck, or tailhead. Self-trauma and head shaking can lead to aural hematomas. The mites are contagious, particularly in young animals, and can live off the host for extended periods of time. Diagnosis is by direct visualization; however, mites may be difficult to demonstrate in some cases. Mites can cause a transient papular dermatitis in humans or rarely otitis externa.
Cheyletiellosis
Members of the genus Cheyletiella (Acarina: Cheyletidae) affect dogs, cats, rabbits, wild animal species, and, incidentally, humans. Three species are involved: C. parasitivorax is chiefly a parasite of rabbits, although formerly considered as a canine pathogen; C. yasguri is the major canine cheyletid; and, the species most commonly associated with feline infestation is C. blakei. Host specificity is weak, and cross-infestations are common. The mites are large, ovoid, 400 µm, obligate parasites with curved palpal claws. The mites live in the keratin layer of the epidermis; they do not burrow, but they pierce the skin with stylet-like chelicerae to feed on lymph. Ova are non-operculated, smaller than louse nits, and are attached to hairs by fine fibrillar strands. Fully developed nymphs emerge from eggs. The entire life cycle is completed on one host and is about 21 days. Adult female mites can live up to 10 and possibly 30 days off their host without feeding, and thus transmission can be both indirect and direct. The mites are highly contagious.
Pruritus is variable, ranging from absent to intense, and some animals have nonlesional pruritus. The gross lesions in both the dog and cat reflect the mite's predilection for the dorsal midline. Lesions often commence over the caudal back and progress cranially but may become generalized. The typical lesion is a moderate to marked exfoliation of small, dry, white scales (seborrhea sicca). The mites crawl in “pseudotunnels” in the loose keratin debris, and their movement has produced the colloquial name walking dandruff for cheyletiellosis. Hair loss may occur because of scratching and overgrooming, and pruritus tends to increase. The intensity of the pruritus may outweigh the number of mites, suggesting a hypersensitivity reaction. Some animals may develop exfoliative erythroderma or a scabies-like condition with similar distribution of lesions and intensity of pruritus. Cats may develop, in addition, focal, multifocal, or generalized erythematous papules or crusted lesions (miliary dermatitis). Other cats may develop self-induced dorsal hypotrichosis with few or no skin lesions. Free-living cheyletids (Cheyletus eruditus) can also infest dogs and cats. These mites do not induce clinical signs.
Diagnosis depends upon demonstration of the mites via direct examination of the animal, skin scraping, acetate tape, vacuum cleaning, or flea-combing techniques. Cheyletiella eggs and occasionally mites can often be found in feces, especially in grooming cats. Histopathology shows a spongiotic hyperplastic superficial perivascular dermatitis with variable numbers of eosinophils. In some cases, an interface lichenoid lymphoplasmacytic dermatitis is seen. Mite segments are occasionally found within the stratum corneum. Humans in contact with affected animals often develop a pruritic maculopapular rash on the arms and trunk. Individual human cases of a bullous eruption with systemic lupus erythematosus, bullous pemphigoid, and peripheral eosinophilia with elevated immune complexes and joint pain with decreased mobility and numbing of fingertips associated with C. blakei have been reported. As the mites do not complete their life cycle on humans, skin lesions usually regress once the animal is treated.
Further reading
Dobrosavljevic DD, et al. Systemic manifestations of Cheyletiella infestation in man. Int J Dermatol 2007;46:397-399.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Saevik BK, et al. Cheyletiella infestation in the dog: observations on diagnostic methods and clinical signs. J Small Anim Pract 2004;45:495-500.
Sotiraki ST. Factors affecting the frequency of ear canal and face infestation by Otodectes cynotis in the cat. Vet Parasitol 2001;96:309-315.
Wagner R, Stallmeister N. Cheyletiella dermatitis in humans, dogs and cats. Br J Dermatol 2000;143:1110-1112.
Psorergatic mange
Psorergates (Psorobia) ovis (Acarina: Cheyletidae) is a parasite of the integument of sheep. The disease is uncommon and occurs in Australia, New Zealand, South Africa, and South America. It is thought to have been eradicated from the United States and has not been reported in Europe. The mite (100-200 µm), which is much smaller than sarcoptid mites, is an obligate parasite and goes through its life cycle on the skin surface in the loose keratin debris. The mite does not penetrate deeper than the stratum corneum. Infestations occur predominantly in the winter and spring. Sheep experience intense pruritus with rubbing, chewing, and kicking at fleece. There may be scaling and matted, chewed, broken, and absent wool over the lateral thorax, flanks, and thighs. In affected areas, the wool resembles bleached, twisted tufts that give the fleece a ragged, tasseled appearance. Fleece damage is more severe in the fine-wooled Merino.
Psorergates (Psorobia) bos is the cause of psorergatic mange in cattle. The disease is uncommon and has been reported in North America, Africa, Australia, and Europe. Clinical signs vary from absent to severe alopecia, scaling, and pruritus over the dorsal head, neck, shoulders, rump, and back.
Further reading
Cortinas R, Jones CJ. Ectoparasites of cattle and small ruminants. Vet Clin North Am Food Anim Pract 2006;22:673-693.
Johnson PW. The effect of host nutrition on itch mite, Psorergates ovis, populations and fleece derangement in sheep. Med Vet Entomol 1996;10:121-128.
Oberem PT, Malan FS. A new cause of cattle mange in South Africa: Psorergates bos Johnston. J S Afr Vet Assoc 1984;55:121-122.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Sinclair A. The epidermal location and possible feeding site of Psorergates ovis, the sheep itch mite. Aust Vet J 1990;67:59-62.
Demodectic mange
More than 140 Demodex (Acarina: Demodicidae) species or subspecies have been identified in hair follicles, sebaceous glands, Meibomian glands, and ceruminous glands of numerous mammals, including dogs, cats, cattle, goats, horses, sheep, pigs, deer, and hamsters. Demodex gatoi in cats lives in the superficial stratum corneum rather than in the follicles. In small numbers, Demodex spp. are normal inhabitants of the hair follicles and sebaceous glands in dogs, humans, and probably most mammals, and their position is invariably head-down. Transmission of follicular mites usually occurs from mother to young during the first 3 days of life through close physical contact while nursing. Demodex spp. are obligate parasites completing their life cycle on the host. Mites feed on cells, sebum, and epidermal debris. They are rapidly killed by desiccation on the surface of the skin, but mites move from follicle to follicle, and it is probably at this time that transmission to another host takes place. Two or more Demodex spp. can simultaneously parasitize the same mammalian host. Demodicosis or demodectic mange refers to a proliferation of mites associated with clinical signs and is often, but not always, associated with immunocompromise in the host.
Canine demodicosis.
Canine demodicosis (demodectic mange, follicular mange, red mange) is one of the most common skin disorders of dogs in North America. Two species of Demodex have been identified: D. canis (300 µm) and D. injai (the long-bodied mite, 334-368 µm). Recent genetic studies have demonstrated that D. cornei (the short-tailed mite, 90-148 µm) should be considered a morphologic variant of D. canis rather than a separate species. Two types of demodicosis are generally recognized in dogs with D. canis infestations: localized and generalized. Localized demodicosis occurs as one to several, small, well-circumscribed, erythematous, scaly, nonpruritic to occasionally pruritic areas of alopecia, most commonly on the face (periocular and around lips) and forelegs (Fig. 6-117A ). Most cases resolve spontaneously. In some cases, the condition is limited to the external ear canal, and these dogs have pruritic ceruminous otitis externa. Generalized demodecosis is defined as involvement of an entire body region, multiple localized regions or complete involvement of 2 paws or more. Generalized demodecosis usually starts between 3 and 18 months of age. Over time, lesions, as described above, enlarge and may coalesce to form patches. Follicular casts may be pronounced. Peripheral lymphadenopathy may be marked. Lesions that become secondarily infected with bacteria display edema, exudation, and crusting (Fig. 6-117B). In some cases, lesions are nodular, especially in English Bulldogs. Spontaneous resolution occurs in >50% of cases; however, if lesions do not spontaneously resolve and if the dog does not receive adequate treatment, lesions will likely continue into adulthood. This condition can be very severe and even fatal. Dogs that first develop the disease at 4 years of age or older are considered to have adult-onset generalized demodicosis. Disorders associated with adult-onset demodicosis include hypothyroidism, hyperglucocorticism, leishmaniasis, malignant neoplasia, and immunosuppressive therapy. In >50% of cases, no underlying disease can be documented at the time of demodicosis diagnosis but may become evident weeks to months into therapy.
Figure 6-117.

Demodex canis in a dog. A. Localized demodecosis.
(Courtesy E. Smith.)

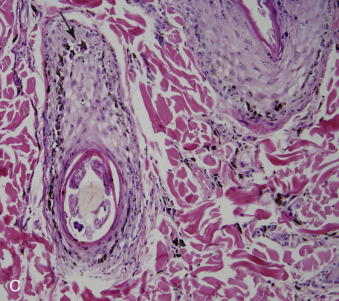
B. Generalized demodecosis. C. Mural interface folliculitis with vacuolar degeneration and apoptosis (arrow) of the outer root sheath, intraluminal mites, and perifollicular pigmentary incontinence.
The pathogenesis of juvenile-onset generalized demodecosis appears to be multifactorial and not completely understood. The disease is thought to be a genetically mediated specific immunodeficiency that allows the proliferation of Demodex mites. The condition is more common in purebred dogs, and breeds at risk include American Staffordshire Terrier, Staffordshire Bull Terrier, and Shar Pei. Although some studies have suggested a decrease in T lymphocytes or premature apoptosis of peripheral blood leukocytes, most dogs are not lymphopenic, and rather, the problem is depressed T-cell function, not decreased numbers. It also appears that immune suppression is worse in those with secondary bacterial pyoderma. One study concluded that dogs with reoccurring demodicosis have higher interleukin-10 (IL-10) levels than healthy dogs and those suffering the disease for the first time. IL-10 can inhibit cytokine secretion by Th1 cells, including IL-1, interferon-γ (IFN-γ) and tumor necrosis factor-β. IL-10 has anti-inflammatory and suppressive effects on most hematopoietic cells, and it indirectly suppresses cytokine production and proliferation of antigen-specific CD4+ T effector cells by inhibiting the antigen-presenting capacity of antigen-presenting cells.
Dogs with infestations with D. injai generally have a different clinical presentation than those with D. canis. Terriers, especially the West Highland White Terrier, Shih Tzu, and Wirehaired Fox Terrier are predisposed. Most dogs are middle-aged to older dogs with generalized disease that is characterized by mild to intense pruritus and greasy seborrhea, especially of the face and topline (Fig. 6-118A). Erythema, hyperpigmentation, and comedones have been described, but hypotrichosis, alopecia, and secondary bacterial skin infections are rare. Many affected dogs have had prior histories of allergic dermatitis, immunosuppression, or immunomodulatory drug use. One 12-year-old spayed female Beagle undergoing immunomodulatory therapy for immune-mediated polyarthritis was reported to have bilateral ceruminous otitis externa associated with D. injai.
Figure 6-118.

Demodex injai in a dog. A. Erythema and greasy haircoat over the dorsal trunk.
(Courtesy W.H. Miller.)
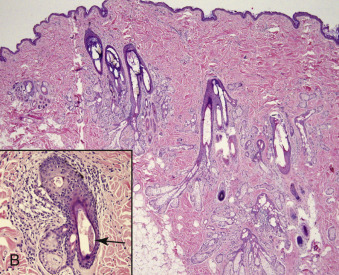
B. Sebaceous gland hyperplasia with perifollicular inflammation and lymphocytic mural folliculitis. Rare intraluminal mites (arrow) are detected (see inset).
Histologically, demodicosis has a variable appearance, depending on the stage of the disease and presence of secondary bacterial infection. Early, uncomplicated lesions are characterized by a predominantly lymphocytic mural interface folliculitis. Lymphocytic infiltration of the isthmus and infundibulum, accompanied by various degrees of vacuolar degeneration and apoptosis of keratinocytes of the outer root sheath; follicular melanosis or pigment clumping in the outer root sheath; and perifollicular pigmentary incontinence, are present (Fig. 6-117C). Immunophenotyping has identified infiltrating lymphocytes as CD8+ cytotoxic T cells, whereas the perifollicular infiltrates were found to be composed of approximately equal numbers of CD4+ and CD8+ lymphocytes. The external root sheath may be hyperplastic. Current research suggests lymphocyte-mediated follicular wall injury may be directed against keratinocytes expressing either altered self-antigens or Demodex antigens. It is not known whether or not the presence of cytotoxic T lymphocytes indicates an appropriate host reaction to eliminate the parasite or if it represents an inappropriate and self-damaging host response.
Perifolliculitis is also a consistent feature with infiltrates of plasma cells, macrophages, and lymphocytes in periadnexal regions. Mast cells and eosinophils may be present in smaller numbers. Marked follicular hyperkeratosis is associated with variable numbers of mites in the upper third of the follicle. Mural folliculitis is also consistently present at later stages and in cases with secondary bacterial infection, but may not be the predominant pattern. In some cases, follicles may contain numerous mites but have no evidence of folliculitis, possibly indicating a poor immune response. Typically, large numbers of mites occupy the hair follicles at all levels and also occlude the opening of the sebaceous gland into the pilar canal. Marked follicular hyperkeratosis and build-up of mite products causes follicular plugging. Bacterial proliferation, chiefly Staphylococcus spp., within the plugged follicle often induces suppurative luminal folliculitis. The combined effects of follicular keratosis, mite proliferation, and folliculitis lead to follicular rupture and release of mites, bacteria, keratin, sebum, and other irritant products into the dermis. The keratin and other irritant substances stimulate a pyogranulomatous reaction, chiefly of neutrophils; epithelioid macrophages; and fewer multinucleated histiocytic giant cells. Epidermal lesions include hyperplasia, orthokeratotic and parakeratotic hyperkeratosis, and variable spongiosis, neutrophilic exocytosis, ulceration, and inflammatory crusting. Longer-standing lesions consist of perifollicular mid to deep dermal or occasionally subcuticular granulomas, sometimes containing remnants of mites. Chronic lesions also have marked dermal fibrosis, often with obliteration of adnexa. Mites or fragments of mites are found in the subcapsular zone of regional lymph nodes associated with a local granulomatous inflammatory response. These do not indicate active invasion but rather passive transport to the node, via lymphatic channels. Through blood and lymph drainage, dead and degenerate mites in all stages can also be found in the spleen, lung, intestinal wall, liver, kidney, urinary bladder, thyroid gland, blood, urine, and feces.
Histopathologic changes in the skin of dogs with D. injai are somewhat different. Usually, there is marked sebaceous gland hyperplasia, especially in the skin of the dorsal trunk (Fig. 6-118B ). In general, very few, if any, mites are detected within the hair follicles of biopsy specimens (see Fig. 6-118B inset). In one study, pyogranulomatous sebaceous adenitis was observed in 2 of 5 cases biopsied. Lymphoplasmacytic periadnexal dermatitis is a typical feature.
Three species of Demodex mites are associated with feline demodecosis. D. gatoi appears to be the most common, and it is the shortest, measuring 91-108 µm. It is a broad mite that inhabits the stratum corneum. D. cati is a long (182-291 µm) slender mite with similar morphology to D. canis. Like D. canis, this mite resides within hair follicles, sebaceous glands, and their ducts. The third unnamed species has rounded edges and measures 139 ± 4.5 µm. It has been found along hair shafts of plucked hairs and therefore is thought to reside within hair follicles; however, this mite has not been demonstrated in biopsy samples.
Demodex gatoi is a contagious mite that is most commonly associated with pruritus and overgrooming; however, some cats are asymptomatic carriers. Affected cats generally have self-induced alopecia over the ventral abdomen, thorax, and medial aspects of the limbs. The skin may be erythematous, scaly, or hyperpigmented, depending on the chronicity and severity of the pruritus. The mite may be difficult to find in cats that groom excessively. Histologically, minimal inflammation is observed. The epidermis may be irregularly hyperplastic, and hyperkeratotic and mites can sometimes be observed within the stratum corneum. In severely pruritic cases, there may be erosions, ulcerations, and crusts with mild to moderate perivascular to diffuse infiltrates of lymphocytes, histiocytes, eosinophils, and mast cells. Neutrophils are prominent in ulcerated areas.
Demodex cati infestation results in a localized or generalized dermatitis as with D. canis in dogs. Localized disease is rare and can involve the eyelids, periocular area, head, or neck. It can occur as ceruminous otitis externa. Skin lesions are variably pruritic with patchy alopecia, papules, comedones, erythema, scaling, and crusting. Generalized feline demodicosis is rare and not usually as severe as the canine form. Lesions are primarily on the face and head, but may be on the neck, trunk, and limbs. Generalized demodicosis caused by D. cati is usually associated with underlying disease, such as diabetes mellitus, hyperglucocorticism, feline immunodeficiency virus, or feline leukemia virus, which presumably suppresses normal cell-mediated immune responses.
Histologic lesions include mild to moderate epidermal hyperplasia with follicular keratosis and mild crusting. There tends to be mild perifollicular inflammation with lymphocytes, macrophages, and neutrophils. There is variable mural follicular inflammation, spongiosis, and mucinosis. In feline viral plaques and bowenoid in situ carcinoma, mites have been found within lesional follicles; adjacent skin is normal.
Cats infested with the third unnamed species generally have concurrent illness or have recently recovered from a systemic illness. Pruritus is variable. Hair is generally easily epilated, and mites have been found on skin scrapings or hair trichograms. Histopathologic findings are described as moderate nonsuppurative and mastocytic dermatitis with moderate superficial orthokeratotic hyperkeratosis. Mites have not been noted on biopsy specimens.
Demodectic mange is uncommon in cattle but occurs worldwide. Three species exist in cattle: D. bovis, D. ghanensis, and D. tauri. Only D. bovis is known to cause clinical disease. It is assumed that all animals experiencing disease resulting from the excessive replication of this normal mite resident are in some way immunocompromised because of concurrent disease, poor nutrition, stress, or genetic predisposition. Economic significance lies largely in the damage that mite infestation produces in hides. In some parts of Africa and Madagascar, demodectic mange in cattle may become generalized and fatal, with this outcome contributed to by other debilitating conditions, such as malnutrition, tick-worry, and tropical heat. There is one report of a 2-year-old heifer from Africa with severe granulomatous nodular dermatitis with marked hyperkeratosis and thick nodular folds over the head, neck, and shoulder caused by concurrent infection with D. bovis and Sarcoptes scabiei. This animal died despite antiparasitic treatment.
Typical gross lesions are multiple cutaneous papules or nodules varying in number from a few to several hundred (Fig. 6-119A ). The nodules are visible in smooth-coated cattle, often indicated by overlying tufts of erect hairs. In rough-coated cattle, such as Herefords, detection usually requires palpation. The preferred sites are the shoulders, neck, dewlap, and muzzle, but in heavy infestations, nodules may be present over most of the body. The content of the nodules is thick, waxy, or caseous material, sometimes stained with blood. The contents may liquefy and discharge to the surface, forming a thick crust, or rupture of the nodule into the dermis may generate a pyogranulomatous reaction. Lesions are neither painful nor pruritic, and there may be a seasonal increase in the number of lesions in the spring and summer.
Figure 6-119.

Demodecosis. A. Multiple crusted papular to nodular lesions in a cow.
(Courtesy D.W. Scott.)
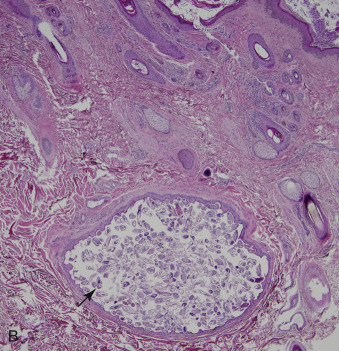
B. Dilated hair follicle in a goat filled with numerous mites (arrow).
Histologically, the nodules are follicular cysts lined by flattened squamous epithelium and filled with keratin squames and large numbers of demodicid mites (Fig. 6-119B). Adult parasites occur occasionally in sebaceous glands and rarely in epitrichial sweat glands. A mild mononuclear cell infiltrate may occur around the epithelial lining. Rupture of a follicular cyst induces a marked nodular granulomatous reaction in which degenerating and occasionally mineralized segments of parasites and keratin debris are surrounded by epithelioid macrophages, multinucleated histiocytic giant cells, lymphocytes, plasma cells, and eosinophils.
Demodectic mange is common in goats. The lesions in goats, caused by D. caprae, are similar to those described for cattle in both distribution and morphology. Some affected goats are mildly depressed, inappetent, and have decreased milk production. Generally, the chief economic significance of caprine demodicosis lies in damage to the hides.
Demodectic mange, caused by D. ovis and D. aries, is rare in sheep. Lesions occur as asymptomatic papules and nodules on especially the face, chin, and pinnae. Widespread lesions and secondary bacterial infections may be seen in debilitated sheep. D. ovis infestation occurs in the medium to coarse-wooled sheep, affecting the Meibomian glands of the eyelid and the sebaceous glands of the primary follicles on the body, particularly the neck, flank, and shoulders. D. aries infests the large sebaceous glands of the vulva, prepuce, and nostrils. D. ovis infestation has been associated with matted fleece (“stringy wool”). Histologically, the mites are present in sebaceous glands or the pilar canal, occasionally inciting folliculitis or furunculosis.
Although Demodex spp. are found commonly in the Meibomian glands of the horse, demodectic mange is a very rare disease. As in other species, follicular demodecosis probably only occurs in horses that are immunocompromised. In horses, demodecosis has been reported in association with chronic treatment with systemic glucocorticoids and in horses with pituitary pars intermedia dysfunction. D. caballi (264-453 µm) parasitizes the pilosebaceous units of the eyelids and muzzle, whereas D. equi (179-236 µm) infestation occurs over the body. Lesions occur on the head, neck, and shoulder but may become generalized. They include asymptomatic hypotrichosis, alopecia, scaling, and crusting. Histologically, hair follicles are distended to various degrees with keratin and demodectic mites. Inflammation may be minimal up to various degrees of perifolliculitis, folliculitis, furunculosis, and foreign-body granuloma formation.
Demodex phylloides of pigs is uncommon and is relatively unimportant in comparison to sarcoptic mange. The principal economic loss results from damage to the hide. The mites reside in the pilosebaceous units. Proliferation of mites is thought to be due to concurrent immunocompromise. The lesions typically involve the ventral abdomen, ventral neck, eyelids, and snout and they are neither painful nor pruritic. They commence as small red macules, developing into cutaneous nodules covered by surface scale. Follicular hyperkeratosis with comedo formation may develop. Incision of the nodules releases thick, white, caseous debris that is full of mites. The histologic lesions are as described in cattle.
Rarely, demodicosis has been described in alpacas and one llama. In the reported llama, lesions were described as multiple pruritic papules with erythema, alopecia, hyperkeratosis, lichenification, and hyperpigmentation on the medial thigh, axilla, inguinal region, and dorsal skin of the lower limb. Demodex spp. (200-280 µm) were identified via skin scraping and microscopy but were not seen in biopsy specimens. Histologically, there was folliculitis, hyperkeratosis of the epidermis, and infiltration of mainly eosinophils and mononuclear cells in the dermis. A nodular pyogranulomatous reaction was occasionally observed in the dermis.
Definitive diagnosis can be made by history, physical examination, and identification of the Demodex mite. In dogs, cats, horses, and llamas with follicular demodecosis, manually squeezing the skin lesions with deep skin scrapings may be necessary to recover the mite. In dogs with D. injai, multiple deep scrapes may need to be performed because mite numbers are generally low. In cats with D. gatoi, multiple surface scrapings should be performed. Mites may also be recovered on fecal flotation. In highly pruritic cats, mites may be difficult to recover, and therefore a treatment trial may help make the diagnosis. In those species with nodular demodicosis (cattle, goats, sheep, pigs), nodules can be incised or manually expressed to reveal multiple mites. Skin scrapings may reveal cigar-shaped larvae, nymphs, and adult mites or elongated ovoid eggs. Adults and nymphs have 4 pairs of legs, whereas larvae have 3 pairs. In dogs, PCR techniques can be used to make a definitive diagnosis regarding mite species.
Further reading
Arther RG. Mites and lice: biology and control. Vet Clin North Am Small Anim Pract 2009;39:1159-1171.
Barriga OO, et al. Evidence of immunosuppression by Demodex canis. Vet Immunol Immunopathol 1992;32:37-46.
Beale K, et al. Feline demodecosis a consideration in the itchy or overgrooming cat. J Fel Med Surg 2012;14:209-213.
Bukva V. Demodex tauri sp. n. (Acari: Demodicidae), a new parasite of cattle. Folia Parasitol (Praha) 1986;33:363-369.
Bukva V. Three species of the hair follicle mites (Acari: Demodicidae) parasitizing the sheep, Ovis aries L. Folia Parasitol (Praha) 1990;37:81-91.
Burrows AK. Generalised demodicosis in the dog: the unresponsive or recurrent case. Aust Vet J 2000;78:244-246.
Caswell JL, et al. A prospective study of the immunophenotype and temporal changes in the histologic lesions of canine demodicosis. Vet Pathol 1997;34:279-287.
Chanie M, et al. Ectoparasites are the major causes of various types of skin lesions in small ruminants in Ethiopia. Trop Anim Health Prod 2010;42:1103-1109.
Chesney CJ. Short form of Demodex species mite in the dog: occurrence and measurements. J Small Anim Pract 1999;40:58-61.
Day MJ. An immunohistochemical study of the lesions of demodicosis in the dog. J Comp Pathol 1997;116:203-216.
Desch CE, Stewart TB. Demodex gatoi: new species of hair follicle mite (Acari: Demodecidae) from the domestic cat (Carnivora: Felidae). J Med Entomol 1999;36:167.
Eo K, et al. Skin lesions associated with Demodex sp. in a llama (Lama peruana). J Zoo Wildl Med 2010;41:178-180.
Felix AOC, et al. Comparison of systemic interleukin 10 concentrations in healthy dogs and those suffering from recurring and first time Demodex canis infestations. Vet Parasitol 2013;193:312-315.
Fondati A, et al. Prevalence of Demodex canis-positive healthy dogs at trichoscopic examination. Vet Dermatol 2009;21:146-151.
Guaguère E, et al. Demodex cati infection in association with feline cutaneous squamous cell carcinoma in situ: a report of five cases. Vet Dermatol 1999;10:61-67.
Hamid ME, et al. Unusual manifestation of a concurrent demodectic and sarcoptic mange in a Zebu-Friesian cross-bred heifer. JS Afr Vet Assoc 2006;77:90-91.
Hill FI, et al. Demodex spp. infestation and suspected demodicosis of alpacas (Vicugna pacos) in New Zealand. NZ Vet J 2008;56:148-149.
Hillier A, Desch CE. Large-bodied Demodex mite infestation in 4 dogs. J Am Vet Med Assoc 2002;220:623-627.
Kano R, et al. Feline demodecosis caused by an unnamed species. Res Vet Sci 2012;92:257-258.
Matthes HF. Investigations of pathogenesis of cattle demodicosis: sites of predilection, habitat and dynamics of demodectic nodules. Vet Parasitol 1994;53:283-291.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Milosevic MA, et al. PCR amplification and DNA sequencing of Demodex injai from otic secretions of a dog. Vet Dermatol 2013;24:286-e66.
Moriello KA, et al. Five observations of a third morphologically distinct feline Demodex mite. Vet Dermatol 2013;24:460-462, e106.
Ordeix L, et al. Demodex injai infestation and dorsal greasy skin and hair in eight wirehaired fox terrier dogs. Vet Dermatol 2009;20:267-272.
Ravera I, et al. Small Demodex populations colonize most parts of the skin of healthy dogs. Vet Dermatol 2013;24:168-172, e37.
Saari SAM, et al. Demodex gatoi-associated contagious pruritic dermatosis in cats—a report from six households in Finland. Acta Vet Scand 2009;51:40-47.
Sadtre N, et al. Phylogenetic relationships in three species of canine Demodex mite based on partial sequences of mitochondrial 16S rDNA. Vet Dermatol 2012;23:509-e101.
Santarem VA, et al. Demodectic mange in fattening pigs in São Paulo, Brazil. Vet Parasitol 2005;131:169-171.
Saridomichelakis M, et al. Adult-onset demodicosis in two dogs due to Demodex canis and a short-tailed demodectic mite. J Small Anim Pract 1999;40:529-532.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW. Untreated generalized demodecosis in young dogs. Vet Dermatol 2012;23:174-176.
Singh SK, et al. The role of apoptosis in immunosuppression of dogs with demodecosis. Vet Immunol Immunopathol 2011;144:487-492.
Trombiculiasis
The nymphs and adults of trombiculid mites are free living or parasitize plants or other arthropods; the larvae are parasitic and are known as “harvest mites,” “chiggers,” or “red bugs.” The parasitic larvae are 6-legged, red to orange to yellow, and 0.2-0.4 mm in length, just visible to the naked eye. The mites attach themselves to the skin and make a channel into the epidermis, called a stylostome, through which salivary enzymes are injected and digested tissue fluids are withdrawn. The mites engorge to twice their original size over a period of 3-5 days, after which they drop off and complete their life cycle in the soil. Intensely pruritic dermatitis develops at the sites of attachment, probably as a result of an allergic reaction to the salivary secretions delivered through the stylostome; the allergic reaction caused by larval trombiculid mites is known as trombidiosis.
Wild vertebrates are the usual hosts for the trombiculid mite larvae, but food-producing domestic animals, pets, and humans may be accidentally infested. The disease tends to have a seasonal incidence, occurring in the late summer and autumn when climatic conditions favor an expansion of the mite population. Factors such as soil type also influence the prevalence of trombiculiasis in different geographic regions. Animals exposed to fields and woodlands are more often infested.
Trombicula (Neotrombicula) autumnalis, the European harvest mite, attacks most domestic species. T. sarcina, an Australian species known as the leg-itch mite, is an important parasite of sheep, although its principal host is the gray kangaroo. T. (Eutrombicula) alfreddugesi (North American chigger) and T. splendens are some of the species implicated in trombiculiasis in cats, dogs, and horses. Straelensia cynotis, normally residing on foxes, has been reported to infest dogs and cats in France, Spain, and Portugal. S. cynotis has a different clinical presentation, histopathologic features, and response to treatment compared to the other trombiculids.
Lesions caused by most trombiculids tend to occur in areas close to ground contact in animals exposed to wild or semi-wild areas. Pruritus is variable but can be intense. Different responses to the infestations may be due to individual hypersensitivity reactions to the mites. In cattle and sheep, the legs, face, pinnae, axillae, and groin are the most commonly affected sites. In goats, legs, face, and ventrum are most commonly affected. The mite in horses is known as the “heel-bug” because of its tendency to parasitize the feathered area of the pastern. Lesions may also occur on the muzzle, nares, face, ears, and neck. Horses may sneeze or head-shake. In cats, lesions affect the paws, head, ears, and ventrum, but an atypical generalized form of the disease may occur in association with Walchia americana infestation. The interdigital web, concave surface of the pinnae, face, and ventral abdomen are the predilection sites in the dog infested with species other than S. cynotis. In a massive infestation reported in 2 dogs, temporary hindlimb paresis developed.
The gross lesions caused by all species, with the exception of S. cynotis, are erythematous crusted papules on which are clustered tiny (0.2-0.4 mm) bright red, orange, or yellow mites. The mites leave a small, shallow ulceration that oozes a serous discharge and becomes crusted. Pruritus induces marked self-trauma, which may incite secondary bacterial infection. Histologically, the mite may be present in tunnels within the stratum spinosum or in the stratum corneum. The presence of the mites induces both hyperplastic and degenerative changes in the epidermis. The stylostome appears as a pale staining, hyalinized tube with undulating margins oriented vertical to the skin's surface and extending into the dermis. A large zone of necrotic cellular debris usually surrounds the stylostome. The surrounding dermis has a superficial perivascular infiltrate, with eosinophils and mast cells predominating.
Dogs infested with S. cynotis (straelensiosis) have multiple alopecic erythematous papules and nodules over the head, neck, dorsum, extremities, and lumbar regions. The ventral thorax and abdomen are rarely involved. Pustules, purulent exudate, crusts, and ulcerations are sometimes very extensive. Uncomplicated lesions are generally nonpruritic. Histologically, hair follicles are dilated, and most contain an intrafollicular larval mite. Marked pseudoepitheliomatous hyperplasia and perifollicular mucinosis are considered pathognomonic. Eosinophilic, sometimes mineralized, dense and amorphous material often surrounds larvae. Dermal inflammation is generally mild, consisting of lymphocytes, plasma cells, and a few mast cells. Eosinophils are rare. There is a striking proliferation of vascular channels surrounding some lesions and occasionally replacing hyperplastic follicular epithelium. The epidermis is hyperplastic with hyperkeratosis, focal spongiosis, and serocellular crusts.
Diagnosis of trombiculosis is confirmed by isolation and identification of mites through visual inspection of the infested animal in most species and histopathology in the case of straelensiosis.
Further reading
Flemming EJ, Chastain CB. Miliary dermatitis associated with Eutrombicula infestation in a cat. J Am Vet Med Assoc 1991;27:529-531.
Goff ML, McKown RD. The genus Hexidionis (Acari:Trombiculidae) with the description of a new species from Texas. J Med Entomol 1997;34:438-440.
Le Net JL, et al. Straelensiosis in dogs: a newly described nodular dermatitis induced by Straelensia cynotis. Vet Rec 2002;150:205-209.
Mair TS. Headshaking associated with Trombicula autumnalis larval infestation in two horses. Equine Vet J 1994;26:244-245.
Prosl H, et al. Neotrombicula autumnalis (harvest mite) in veterinary medicine. Nervous symptoms in dogs following massive infestation. Tierarztl Prax 1985;13:57-64.
Ramirez GA, et al. Clinical, histopathological and epidemiological study of canine straelensiosis in the Iberian Peninsula (2003-2007). Vet Dermatol 2008;20:35-41.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Seixas F, et al. Dermatitis in a dog induced by Straelensia cynotis: a case report and review of the literature. Vet Dermatol 2006;17:81-84.
White B. Early Trombicula autumnalis infection. Vet Rec 2001;148:188.
Other mite-induced dermatoses
The cat fur mite, Lynxacarus radovsky, infests cats and is widely distributed worldwide. The mite attaches to the hair shafts rather than to the skin surface. Mites are usually located along the topline, including the tail tip, tail head, and perineum. The mite infestation mimics seborrhea sicca, giving the coat a characteristic “salt and pepper” appearance. The infestation is not usually associated with lesions, although crusted, exudative, and pruritic lesions and alopecia have been described.
The straw-itch mite (Pyemotes tritici) is normally found in straw or grain, where it parasitizes the larvae of soft-bodied grain insects. The parasite may occasionally infest mammals, causing pruritic dermatitis. Mildly pruritic lesions may develop in horses fed infested hay. Multiple papules and wheals may occur on the muzzle, neck, withers, legs, and ventral thorax and abdomen. Acarus (Tyroglyphus) farinae and A. (Tyroglyphus) longior may cause a pruritic, exudative, crusting, and alopecic dermatosis in horses exposed to contaminated grain or hay.
Horses, cattle, goats, cats, and dogs may be infested on rare occasions with the poultry mite, Dermanyssus gallinae. Adult mites are 0.6 to 1 mm and suck blood. They live and lay eggs in cracks and crevices in the walls of poultry houses or in bird nests. Lesions consist of pruritic papules and crusts. In dogs and cats, the lesions are usually over the back and extremities and in horses lesions tend to be on muzzle, limbs and ventrum, and sometimes the topline, especially if birds are nesting above the horse's stall. Predilection sites in cattle and goats include legs and ventrum.
Ornithonyssus syviarum, the northern fowl mite, is another blood-sucking parasite that can parasitize horses. Adult mites can live off the host for 1-3 weeks. Lesions tend to begin as topline dermatitis because infestations are most commonly due to birds nesting above the horse's stall. Pruritus is variable.
House-dust mites, Dermatophagoides farinae and D. pteronyssinus, are associated with allergic dermatitis in dogs and cats.
Sheep may, on rare occasions, become infested with the stored-product mite, Sancassania berlesei. These mites cannot infest dry skin; infestations are secondary to other conditions such as myiasis.
Further reading
Barton NJ, et al. Infestation of sheep with the stored product mite Sancassania berlesei (Acaridae). Aust Vet J 1988;65:140-143.
Craig TM, et al. Lynxacarus radovskyi infection in a cat. J Am Vet Med Assoc 1993;202:613-614.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Norhidayu JJ, et al. The cat fur mite, Lynxacarus radovskyi Tenorio, 1974 (Acarina: Astigmata: Listrophoridae) from cat, Felis catus in peninsular Malaysia. Trop Biomed 2012;29:308-310.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Ticks
Ticks belong to the class Arachnida, subclass Acari. Ticks are divided into 2 families, the Argasidae (soft ticks) and the Ixodidae (hard ticks). Ticks harm their host most importantly by transmitting various bacterial, viral, protozoal, and rickettsial infections. Ticks are small, attach firmly to their hosts, use multiple hosts, live for prolonged periods of time, and can often survive without feeding for long periods of time. These factors make ticks important in the possible transport and transmission of diseases from one host to another and between countries or continents. Importation of animals harboring ticks can pose a threat to animals in areas free of certain diseases. Babesiosis, Rocky Mountain spotted fever, ehrlichiosis, tularemia, Lyme borreliosis, heartwater disease, Q fever, louping ill, and anaplasmosis are a few examples of tick-transmitted diseases.
If infestation is heavy, fatalities may result. The local injury may predispose to myiasis and secondary bacterial infection, particularly to staphylococcal cutaneous abscesses or septicemia in lambs. Heavy infestations are also capable of causing anemia as a result of the blood-sucking activities of the ticks, but ixodid ticks, which engorge only once at each instar, are much less important in this respect than are argasid ticks, which as adults engorge repeatedly. Tick bites may also induce hypersensitivity reactions. Severe hypersensitivity reactions to the larvae of Boophilus microplus have been described in horses in Australia. Within 30 minutes of reinfestation, sensitized horses develop intensely pruritic papules and wheals, chiefly on the lower legs and muzzle. As tick-bite lesions progress, they are often typified by the “arthropod-bite granuloma” described earlier in this section. Twelve ixodid species have been associated with tick paralysis, and they include Ixodes rubicundus and Rhipicephalus evertsi of South Africa, I. holocyclus of Australia, and R. sanguineus, Dermacentor andersoni and D. variabilis in North America. These ticks have neurotoxins in salivary secretions that can cause paralysis of the host. It may be secreted by the ovaries because it is associated with egg production.
The Argasidae are the so-called soft ticks, lacking the scutum that characterizes the Ixodidae. This group of ticks is more common in warm climates. Adults lay eggs in sheltered spots in the environment, and larvae and nymphs suck blood and lymph and drop off the host to become adults. Included in this group is Otobius megnini and Ornithodoros spp. Otobius megnini, known as the “spinose ear-tick,” is parasitic to all domestic animals causing severe blood and lymph loss, parasitic otitis externa, vigorous head-shaking and scratching, and secondary bacterial infections or myiasis. In some cases, the ear canal becomes packed with immature ticks. Ornithodoros coriaceus, occurring along the Pacific coast of the United States, has a painful bite, and is a vector of epizootic bovine abortion.
Most of the pathogenic species of tick are found in the Ixodidae. Ixodid ticks, such as Dermacentor spp., Rhipicephalus spp., and Amblyomma spp., lay their eggs in sheltered areas. Larvae climb onto grass and shrubbery and wait for a suitable host to come by. Infestations of larval and nymphal Ixodes spp. have been described in dogs and cats. Most cases occur in late summer and autumn. Clinical signs include asymptomatic clusters of tick larvae on the neck, back, and scrotum to multiple variably pruritic erythematous papules on the trunk and thighs. In North America, “seed tick infestation” has been associated with Amblyomma americanum larvae, and in Australia “scrub itch” has been associated with I. holocyclus and Haemaphysalis longicornis larvae. Histologic features of “seed and scrub itch” are as follows: Ticks are attached in well-demarcated deep invaginations (“tick craters”) of the epidermis, variable epidermal hyperplasia and necrosis, and mild to marked diffuse perivascular to interstitial eosinophilic and neutrophilic dermal inflammation.
The local reaction to adult ticks is variable, depending on properties of the tick, for example, its ability to secrete prostaglandins, and on host factors such as the level of tick resistance. Primary tick bite lesions are papules, wheals, and nodules. Crusts, erosions, ulcerations, and alopecia may develop. Pain and pruritus are variable. In horses, tick bites are most common on the face, ears, neck, mane, axillae, groin, distal limbs, and tail. In cattle, goats, sheep, and pigs, tick bites are most common on the ears, face, neck, axillae, groin, and legs.
Histologically, the primary lesions are characterized by focal epidermal edema and necrosis with adjacent dermal edema and infiltration of neutrophils, eosinophils, and mononuclear cells. Reactions in previously infested hosts are characterized by marked spongiosis with eosinophilic and basophilic microabscesses, subepidermal edema, and marked dermal infiltration with basophils, eosinophils, and mononuclear cells. In some cases, especially horses, there may be persistent nodular lesions. These are characterized by diffuse dermatitis composed of lymphocytes, histiocytes, and fewer eosinophils and plasma cells. Lymphoid nodules with developing follicles, resembling pseudolymphoma, may occur.
Further reading
Atwell RB, et al. Prospective survey of tick paralysis in dogs. Aust Vet J 2001;79:412-418.
Baxter CG, et al. Dermatoses caused by infestations of immature Ixodes spp. on dogs and cats in Sydney, Australia. Aust Vet J 2009;87:182-187.
Burridge MJ. Ticks (Acari: Ixodidae) spread by the international trade in reptiles and their potential roles in dissemination of diseases. Bull Entomol Res 2001;91:3-23.
Cortinas R, Jones CJ. Ectoparasites of cattle and small ruminants. Vet Clin North Am Food Anim Pract 2006;22:673-693.
Falcone FH, et al. Do basophils play a role in immunity against parasites? Trends Parasitol 2001;17:126-129.
Madigan JE, et al. Muscle spasms associated with ear tick (Otobius megnini) infestations in five horses. J Am Vet Med Assoc 1995;207:74-76.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Shaw SE, et al. Tick-borne infectious diseases of dogs. Trends Parasitol 2001;17:74-80.
Helminth Diseases of Skin
The skin is the natural portal of entry of a number of metazoal parasites that have their final habitat in the gastrointestinal tract or elsewhere. As a rule, those infective larvae that can invade percutaneously are not host specific, thus infection of aberrant hosts occurs. Such parasites are quite varied in their nature and include infective larvae of trematodes, such as Schistosoma, and of the nematodes of various genera, including Strongyloides, Gnathostoma, Ancylostoma, Bunostomum, Uncinaria, and others. Infective larvae of the filariids, such as Dirofilaria and Setaria, are deposited in the skin by the biting insects that are their vectors. The first percutaneous invasion of one of these parasites in its natural hosts takes place very quickly (for example, the larvae of Strongyloides and Bunostomum reach the dermis in 15 minutes) and provokes little reaction. Repeated invasions in a natural host or single invasion in an unnatural host are met with some resistance that is manifested as acute dermatitis limited to the invaded area. The cutaneous lesions are, except under experimental circumstances, seldom observed in animals. It is on the glabrous nonpigmented skin of people that they are easily observed and well recognized as the so-called “creeping eruption.” There the larvae produce acutely inflamed, serpiginous, vesicular to papular tracts that may advance several centimeters a day. Usually, aberrant larvae die in the skin, but some enter the vessels and become lodged in the lungs or other tissues. Nematode larvae most often incriminated are Ancylostoma braziliense, A. caninum, and Uncinaria stenocephala, the canine hookworm larvae. Bunostomum phlebotomum, Gnathostoma spinigerum, Dirofilaria sp., Strongyloides procyonis, and S. westeri are nematode parasites of other domestic and wild animals that have also been reported to cause cutaneous larval migration in humans.
Hookworm dermatitis, caused by aberrant migration of Ancylostoma spp. and U. stenocephala, occurs in dogs kept on grass or dirt and subjected to poor sanitation. A. caninum can complete its life cycle via skin penetration. Although U. stenocephala rarely completes its life cycle via this route, it can produce marked dermatitis as a result of skin penetration. Third-stage larvae enter the dog's skin on areas of the body that frequently contact the ground. Larvae enter the skin via pressure, leaving no visible penetrating point. Other species of hookworm larvae cause loss of epidermal integrity. Lesions consist of pruritic red papules on parts of the body exposed to the ground. Lesions become erythematous, thickened, and alopecic. Distal limbs and feet are especially affected. The footpads and interdigital regions of the feet may be edematous and painful. Claw deformities may occur. Pruritus varies from mild to severe. Histologically, hyperplastic spongiotic perivascular dermatitis with eosinophils and neutrophils is present. Larval tracts may be present in the epidermis or dermis lined by degenerating leukocytes. Inflammation is thought to be due to a hypersensitivity reaction to migrating larvae. B. phlebotomum cases pruritic dermatitis of feet, legs, and ventrum in cattle. B. trigonocephalum can cause a similar syndrome in sheep.
The cutaneous lesions produced by the blood flukes, and those nematodes that pass through the skin on the way to the gut are discussed elsewhere with the mature parasites (see Vol. 2, Alimentary system and peritoneum). The dermatitis produced by the larvae of Elaeophora is discussed in Vol. 3, Cardiovascular system. To be discussed in more detail here are those helminthic infestations that remain more or less localized to the dermis.
Cutaneous habronemiasis
The aberrant deposition of the larvae of the spirurid nematodes Habronema majus (microstoma), H. muscae, and Draschia megastoma by transmitting flies at cutaneous or mucocutaneous sites causes this common disease of equids (horses, donkeys, mules). The adult worms normally develop in the stomach of horses following the ingestion of infective larva (see Vol. 2, Alimentary system and peritoneum). The cutaneous disease occurs sporadically in horse populations in temperate or tropical climates during the summer when the transmitting flies, Musca spp. and Stomoxys calcitrans, are active. Horses with a hypersensitivity response to the larvae are affected, and the condition is recurrent each summer, hence the term “summer sores.” Lesions are consistently pruritic.
The location of the lesions is in the moist exposed areas of the body that attract flies. The most common sites are the medial canthus of the eye (Fig. 6-120A ), the glans penis and prepuce, and any cutaneous wound. Because lacerations are more common on the distal extremities, these too are predilection sites for habronemiasis. Fly bites alone are sufficient to initiate an infestation. Ulcerative diseases initiated by other causes can be complicated by habronemiasis.
Figure 6-120.

Cutaneous habronemiasis in a horse. A. Crusted papular lesion below medial canthus.
(Courtesy D.W. Scott.)

B. Longitudinal section of Habronema spp. larva surrounded by a palisading eosinophilic granuloma.
The gross lesions are rapidly progressive and proliferative in nature, comprising ulcerated, tumorous masses of red-brown granulation tissue. The surface is friable and bleeds readily. Lesions may be single or multiple and range in size from 5-15 cm in diameter and from 0.5-1.5 cm in depth. They are often irregular in shape in the early stages but become circular as they enlarge. On cut section, multiple small (1-5 mm) yellow-white, caseous, and occasionally gritty foci are scattered through the granulation tissue. These are often confused with the “kunkers” of pythiosis, but lack the characteristic branching pattern of the true kunker. In the deeper parts of the lesion, the more mature connective tissue has a dense, white appearance. The lesions on the conjunctiva and eyelids do not usually exceed 2 cm. Commencing with a serous conjunctivitis, small ulcerated, proliferative nodular lesions develop on the mucous membrane of the third eyelid and at the medial canthus. Lacrimal duct involvement characteristically produces a lesion 2-3 cm below the medial canthus. The entire conjunctiva may be affected, resulting in profuse lacrimation, photophobia, chemosis, and inflammation of the eyelid. On cut section, the nodular lesions of brown-red granulation tissue contain the typical caseous or mineralized foci. Involvement of the penis and prepuce may cause prolapse of the urethral process and dysuria. On rare occasions, Habronema granulomas are found in the lung. Gross lesions of cutaneous habronemiasis may resemble those of exuberant granulation tissue, bacterial pseudomycetoma, pythiosis, equine sarcoid, and squamous cell carcinoma. Habronemiasis may complicate a pre-existing lesion; secondary Habronema infestations occur with pythiosis, Corynebacterium pseudotuberculosis infection, and in skin tumors, particularly squamous cell carcinoma of the penis.
Histologically, there is nodular-to-diffuse dermatitis with numerous eosinophils and mast cells. Multifocal coagulative necrosis with dense aggregates of degranulating eosinophils is a characteristic feature. In 50% of cases, nematode larvae are found within the necrotic foci. Palisading granulomas containing epithelioid macrophages and multinucleated histiocytic giant cells may develop around these foci. (Fig. 6-120B). Larvae are usually degenerate and sometimes mineralized. The fibrous connective tissue is heavily and diffusely infiltrated with eosinophils and with fewer numbers of mast cells, lymphocytes, and plasma cells. The surface of the lesion is usually covered with fibrinonecrotic exudate overlying highly vascular granulation tissue infiltrated with neutrophils.
In addition to equids, cutaneous habronemiasis has been reported in a dog and a dromedary camel. Lesions in the dog developed on the face but, unlike the equine disease, were not characterized by rapid proliferation of granulation tissue. The dog was housed under unsanitary conditions in the company of several heavily parasitized ponies. The camel had a nonhealing, severely pruritic, ulcerative fibrotic plaque at the medial canthus. Histologic findings were similar to those for equids.
Definitive diagnosis is based on history, physical examination, direct smears, and biopsy. PCR may help confirm the diagnosis if larvae are not visible within cytology or biopsy specimens.
Further reading
Hendrix CM, et al. Cutaneous larva migrans and enteric hookworm infections. J Am Vet Med Assoc 1996;209:1763-1767.
Mathison PT. Eosinophilic nodular dermatoses. Vet Clin North Am Equine Pract 1995;11:83-85.
Myers DA, et al. Cutaneous periocular Habronema infection in a dromedary camel (Camelus dromedarius). Vet Dermatol 2010;21:527-530.
Pusterla N, et al. Cutaneous and ocular habronemiasis in horses: 63 cases (1988-2002). J Am Vet Med Assoc 2003;222:978-982.
Sanderson TP, Niyo Y. Cutaneous habronemiasis in a dog. Vet Pathol 1990;27:208-209.
Stephanofilariasis
Members of the genus Stephanofilaria (Spirurida: Setariidae) are parasites of cattle. Stephanofilariasis is uncommon. All stephanofilarid parasites cause similar cutaneous lesions, but the species are geographically separated, and the lesions occur on different parts of the host's body. Stephanofilaria stilesi occurs in North America (especially the west and southwest), affecting the abdominal skin near the midline (including udder, teats, scrotum, and flanks); in Australian cattle, initial lesions develop at the medial canthus of the eye; S. dedoesi in Indonesia causes dermatitis, known locally as “cascado,” on the sides of the neck, dewlap, withers, and around the eyes; S. assamensis causes “hump-sore” of Zebu cattle in India and the Soviet Union; S. kaeli causes dermatitis of the legs of cattle from the Malay Peninsula; S. dinniki affects the shoulder of black rhinoceros; S. boomkeri causes severe dermatitis in pigs in Zaire; S. zaheeri causes dermatitis of the ears of buffalo, and S. okinawaensis causes lesions on the teats and muzzle of cattle in Japan. There is one report of scrotal dermatitis caused by S. stilesi in France. Stephanofilaria kaeli, S. assamensis, and S. dedoesi cause crusting dermatitis of the face, neck, shoulders, and feet in goats.
Flies transmit stephanofilariasis. The horn fly, Haematobia irritans, is the vector of S. stilesi in North America, and the buffalo fly, Haematobia irritans exigua, is the major vector for stephanofilariasis in Australia. Musca conducens transmits S. assamensis and S. kaeli. The flies ingest microfilariae when feeding on cutaneous lesions. After a period of development in the fly, the infective larva is deposited on the skin by the biting species of fly or onto cutaneous wounds in the case of the nonbiting vectors such as M. conducens. The adults of S. stilesi live in cystic diverticula off the base of the hair follicles. The parasites are very small, with males reaching 3 mm and females 8 mm in length.
The initial macroscopic lesions in S. stilesi infections are circular patches 1 cm or less in diameter in the skin of the ventral midline, in which the hairs are moist and erect, and the underlying epidermis is spotted with small hemorrhages and droplets of serum. These initial foci enlarge and coalesce, sometimes to produce a lesion 25 cm or more in diameter. As the foci enlarge, new spots of hemorrhage and exudation develop at the periphery, whereas, in the central areas, the hair is shed and the exudate builds up into scabs or rough dry crusts through which the few remaining hairs penetrate. The lesions are mildly pruritic, and rubbing may aggravate them. In the healing stage, the affected areas remain as alopecic, lichenified plaques (Fig. 6-121A ).
Figure 6-121.

Stephanofilariasis in a bull. A. Chronic alopecic lichenified plaque on the ventrum.
(Courtesy R.J. Ossiboff.)
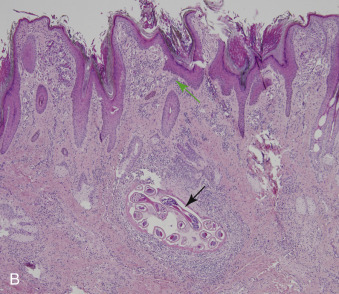
B. Multiple cross sections of nematodes (black arrow) within a dilated hair follicle and numerous microfilariae (green arrow), each surrounded by a vitelline membrane in the superficial dermis.
Histologically, sections of adult parasites may be seen in the cystic diverticula from hair follicles or lying free in the adjacent dermis (Fig. 6-121B). They may be identified as Stephanofilaria spp. with some confidence if microfilariae are seen in the uteri of females because this parasite is viviparous; if ova rather than larvae are found, it is more likely for the parasite to be of the genus Rhabditis. Microfilariae occur free in the dermis or in dermal lymphatics, enclosed within their own vitelline membranes (S. stilesi), or may be found free or unhatched in surface exudate (S. kaeli). In general, there is little dermal reaction to the microfilariae or to the adults enclosed in cystic hair follicles, but the presence of adults in the dermis stimulates a mononuclear inflammatory reaction. There is accompanying superficial and deep perivascular dermatitis characterized by accumulations of eosinophils and mononuclear cells, chiefly lymphocytes. The epidermis is hyperplastic, spongiotic, and often covered by orthokeratotic and parakeratotic hyperkeratosis and inflammatory crust. Spongiform microabscesses containing eosinophils and mononuclear cells are also described; such lesions are more typically associated with the bites of arthropod ectoparasites. It is difficult to assess the relative contributions made to the lesion by the stephanofilarial parasite and by the bites of the fly that acts as the vector.
Diagnosis is usually made on the basis of the typical gross lesions, by histologic examination of biopsy specimens, or by demonstration of microfilariae by deep scrapings.
Further reading
Bain O, et al. Stephanofilaria boomkeri n. sp., as a cause of severe skin disease in pigs in Zaire. Parasite 1996;3:377-381.
Johnson SJ. Stephanofilariasis—a review. Helminthol Abst 1987;56:287-289.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Watrelot-Virieux D, et al. Chronic eosinophilic dermatitis in the scrotal area associated with stephanofilariasis infestation of Charolais bull in France. J Vet Med 2006;53:150-152.
Onchocerciasis
Cutaneous onchocerciasis caused by Onchocerca spp. (Spirurida: Onchocercidae) affects horses, cattle, people, and some wild mammals, including deer and moose. Historically, the prevalence of infection was very high in cattle and horses, ranging up to 100% in some studies. However, the widespread use of avermectins has dramatically reduced the incidence, and in some areas, cutaneous onchocerciasis is quite rare. Onchocerca microfilariae cause cutaneous lesions in some horses; in cattle, the adults cause the cutaneous lesions.
In dogs, onchocerciasis has been associated with nodular lesions of the palpebral conjunctiva, third eyelid, sclera, cornea, and retrobulbar space. Degenerating or mineralized adult Onchocerca spp. parasites were found in the center of pyogranulomas comprising the masses.
Equine cutaneous onchocerciasis
Onchocerca cervicalis, O. reticulata, and O. gutturosa microfilariae are associated with cutaneous lesions in horses in different parts of the world. Culicoides spp. serve as intermediate hosts for all three, Simulium spp. may also be an intermediate host for O. gutturosa, and mosquitoes may serve as intermediate hosts for O. cervicalis. O. gutturosa infests horses in North America, Africa, Australia, and Europe. Adult worms can measure up to 60 cm long and inhabit the lamellar part of the ligamentum nuchae. Microfilariae (200-230 µm) can be found in the dermis of the face, neck, back, and ventral midline. O. reticulata infests horses in Europe and Asia. Adults live in the connective tissue of the flexor tendons and suspensory ligament of the fetlock. Microfilariae (310-395 µm) are found in the dermis of the ventral midline and legs. O. cervicalis infests horses worldwide, and adult worms, measuring up to 30 cm, live in the funicular portion of the ligamentum nuchae. Microfilariae (200-240 µm) are found in the dermis of the ventral midline, face, and neck.
Cutaneous onchocerciasis is thought to represent a hypersensitivity reaction to microfilarial antigens, and most cases are associated with O. cervicalis. Dead and dying microfilariae provoke the most intense inflammation. O. cervicalis can invade ocular tissues, and these lesions are discussed in Vol. 1, Special senses. Affected horses are usually 4 years of age or older. Clinical signs are rare in horses <2 years of age. Lesions are most common on the face and neck, especially around the mane, and ventral chest and abdomen. The ventral lesions are indistinguishable grossly from those of Culicoides hypersensitivity, but onchocerciasis does not cause lesions at the base of the tail. It is likely that onchocerciasis and Culicoides hypersensitivity can exist simultaneously.
Lesion morphology ranges from focal annular areas of alopecia, scaling, crusting, and inflammatory plaques to widespread areas of alopecia, erythema, ulceration, oozing, crusting, and lichenification. An annular lesion in the center of the forehead is very characteristic of onchocerciasis. Pruritus is variable. Cutaneous lesions include partial or complete alopecia, scaling, crusting, and leukoderma. Secondary excoriations or ulcerative dermatitis are induced by self-trauma in pruritic animals. Horses infested with adult worms of O. reticulata may have extensive swelling and lameness.
The microscopic lesions reveal various degrees of superficial and deep perivascular to interstitial to diffuse dermatitis with numerous eosinophils. Microfilariae may be present in large numbers or may be very sparse (Fig. 6-122 ). Other reported histopathologic findings are eosinophilic mural and necrotizing folliculitis, palisaded eosinophilic granulomas, and deep dermal to subcutaneous lymphoid nodules. It is important to note that microfilariae can be seen in skin of normal horses, and thus histopathologic findings should be correlated with historical and physical examination findings. Microfilariae are best recovered from unfixed biopsies that are minced and incubated in saline at 37° C.
Figure 6-122.
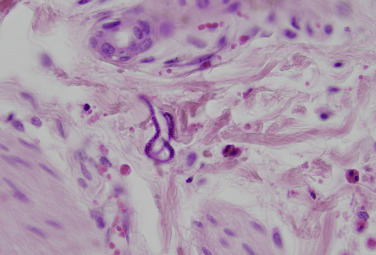
Skin biopsy from a horse with cutaneous onchocerciasis reveals microfilariae in the dermis, accompanied by small numbers of perivascular to interstitial eosinophils.
Viable adult parasites in the nuchal ligament are not associated with significant lesions. In older horses, there is an increased frequency of caseated, mineralized, and granulomatous lesions associated with death of the parasite. Histologic examination shows that this parasite does not penetrate the elastic tissue of the ligament, and the inflammatory reaction is localized around the worm. They are usually encased in a chronic, fibrosing, and pyogranulomatous to granulomatous mass that may also have dystrophic mineralization. Adult O. gutturosa may also be associated with a similar inflammatory response. Mineralization is the fate of degenerate Onchocerca gutturosa worms, in contrast to caseation with O. cervicalis.
Bovine cutaneous onchocerciasis
Cattle can be infected by 3 species of Onchocerca. Cattle infested with O. gibsoni (Africa, Asia, Australia) develop multiple asymptomatic subcutaneous nodules, 2-9 cm in diameter. Lesions may be hard or soft, depending on the degree of mineralization and fibrosis or the degree of caseation and suppuration. Lesions predominantly affect the brisket but also the stifle and hip. Histologic assessment of O. gibsoni nodules revealed dead worms and associated degenerative changes, such as mineralization in 30% of nodules. Eosinophilic infiltration is more marked around viable worms, with eosinophils apparently adherent to the cuticle. In O. gutturosa infestations (North America, Europe, Africa, Australia), the worm is found in the nuchal ligament and connective tissue around tendons and ligaments of the shoulder, hip, and stifle. It may not form nodules and thus is sometimes overlooked. In O. ochengi (Africa) infestations, asymptomatic firm dermal and subcutaneous papules and nodules form on the scrotum, udder, flanks, lateral thorax, and head. Onchocerca spp. microfilariae may be associated with papules, plaques, and ulcers over the teats.
Further reading
Abraham D, et al. Immunity to Onchocerca spp. in animal hosts. Trends Parasitol 2002;18:164-171.
Achukwi MD, et al. Onchocerca ochengi transmission dynamics and the correlation of O. ochengi microfilaria density in cattle with the transmission potential. Vet Res 2000;31:611-621.
Collobert C, et al. Prevalence of Onchocerca species and Thelazia lacrimalis in horses examined post mortem in Normandy. Vet Rec 1995;136:463-465.
Eberhard ML, et al. Ocular Onchocerca infections in two dogs in western United States. Vet Parasitol 2000;90:333-338.
Folkard SG, et al. Eosinophils are the major effector cells of immunity to microfilariae in a mouse model of onchocerciasis. Parasitol 1996;112(Pt 3):323-329.
Lyons ET, et al. Prevalence of selected species of internal parasites in equids at necropsy in central Kentucky (1995-1999). Vet Parasitol 2000;92:51-62.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Parasitic diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 212-250.
Szell Z, et al. Ocular onchocercosis in dogs: aberrant infection in an accidental host or lupi onchocercosis? Vet Parasitol 2001;101:115-125.
Wahl G, et al. Bovine onchocercosis in north Cameroon. Vet Parasitol 1994;52:297-311.
Wildenburg G, et al. Distribution of mast cells and their correlation with inflammatory cells around Onchocerca gutturosa, O. tarsicola, O. ochengi, and O. flexuosa. Parasitol Res 1997;83:109-120.
Pinworms
Oxyuris equi infection of the equine cecum and colon can be associated with pruritic dermatitis of the perineal region, leading to self-induced excoriations and alopecia of the tail known as “rat tail.” The adult female parasite crawls out of the anus to deposit eggs on the hair and skin using a gelatinous material that can induce pruritus. Diagnosis is made by using the tape method in the perianal region for identification of characteristic operculated eggs. Oxyuriasis affects horses in most parts of the world.
Further reading
Perris EE. Parasitic dermatoses that cause pruritus in horses. Vet Clin North Am Equine Pract 1995;11:11-28.
Parafilariasis
Parafilaria multipapillosa occurs in horses in Eastern Europe and Great Britain. Parafilaria bovicola is endemic in cattle in Africa, India, and parts of Europe. Parafilaria bassoni has been reported in African buffalo and springbok in Namibia. The parasites are thin, thread-like worms, 2-7 cm long. The adults inhabit subcutaneous and intermuscular connective tissues producing nodules 1-2 cm in diameter. Lesions are most common over the neck, shoulders, and trunk, and pain and pruritus are variable. In the spring and summer, the nodules rapidly enlarge, burst open, hemorrhage, and heal. This coincides with the migration of the fully gravid female into the more superficial dermis to oviposit and to release infective microfilariae. The vectors, flies such as Haematobia atripalpis in Russia and Musca spp., are infected when they feed from these bleeding points, known as “blood nodules.” Secondary subcutaneous abscesses may occur.
Further reading
Chambers PG. Prevalence of Parafilaria lesions in slaughter cattle in Zimbabwe. Vet Rec 1991;129:431-432.
Chirico J. Prehibernating Musca autumnalis (Diptera: Muscidae)—an overwintering host for parasitic nematodes. Vet Parasitol 1994;52:279-284.
Gibbons LM, et al. Redescription of Parafilaria bovicola Tubangui, 1934 (Nematoda: Filarioidea) from Swedish cattle. Acta Vet Scand 2000;41:85-91.
Keet DF, et al. Parafilariosis in African buffaloes (Syncerus caffer). Onderstepoort J Vet Res 1997;64:217-225.
Van Wuijckhuise L, et al. Parafilariasis: a new parasitic disease of cattle in The Netherlands. Tijdschr Diergeneeskd 2007;132:820-824.
Pelodera dermatitis
Some of the biological characteristics of the Rhabditidae have been discussed with the principal parasitic genus, Strongyloides, in Vol. 2, Alimentary system and peritoneum. Here it is necessary only to describe the cutaneous lesions produced occasionally by the small free-living worms of this family. Those worms that are found in the lesions are usually classified as Pelodera (Rhabditis) strongyloides.
Pelodera dermatitis occurs most commonly in dogs, occasionally in cattle, and rarely in horses, sheep, and humans. Although most reported cases are sporadic, outbreaks involving multiple animals have been described in cattle and sheep. These worms live as saprophytes in warm moist soil that is rich in organic matter, and significant infestations probably require that the host's skin should be continually moist and filthy. Affected dogs often have a history of being bedded on straw. Pruritus is moderate to marked in most species, but is variable and can be absent in cattle. The lesions develop on contact areas (feet, legs, perineum, ventral trunk, tail), particularly at the margins of areas caked with dirt. The gross lesions include erythema, papules, excoriations, scaling, exudation, and crusting, with partial to complete alopecia (Fig. 6-123A ). Pustules may occur, particularly in dogs. In sheep and cattle, lesions become lichenified. Affected sheep may have complete loss of wool.
Figure 6-123.

Pelodera strongyloides in a dog. A. Alopecia and lichenification along the ventral abdomen.
(Courtesy D.W. Scott.)
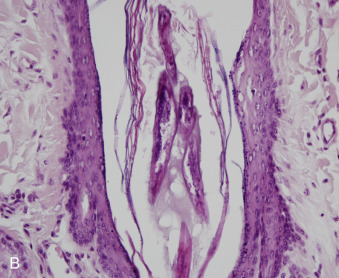
B. Adult rhabditiform parasites within hair follicle.
Histologically, the worms (0.6 mm long) are in the lumina of the hair follicles (Fig. 6-123B) or in the dermis surrounded by eosinophilic and pyogranulomatous inflammation. There is perivascular and perifollicular eosinophilic and lymphoplasmacytic dermatitis and perifolliculitis. Definitive diagnosis is based upon environmental history and deep skin scrapings or biopsy. The infestation is self-limiting once the animal is removed from the source of contamination.
Nematodes of the genus Rhabditis are associated with otitis externa in cattle living in tropical environments. Lesions are painful with brown to yellow purulent foul-smelling discharge.
Further reading
Ramos JJ, et al. Pelodera dermatitis in sheep. Vet Rec 1996;138:474-475.
Rashmir-Raven AM, et al. Papillomatous pastern dermatitis with spirochetes and Pelodera strongyloides in a Tennessee Walking Horse. J Vet Diagn Invest 2000;12:287-291.
Saari SAM, Nikander SE. Pelodera (syn. Rhabditis) strongyloides as a cause of dermatitis—a report of 11 dogs from Finland. Acta Vet Scand 2006;48:18-24.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Yeruham I, et al. Dermatitis in a dairy herd caused by Peloderma strongyloides (Nematoda: Rhabditidae). J Vet Med 2005;52:197-198.
Miscellaneous helminths
Dracunculus medinensis (Spirurida: Dracunculidae) is the “guinea worm” of humans in Asia and Africa. It has been introduced into America, the West Indies, and Fiji. The parasite has been reported in dogs, cats, horses, and cattle as well as other species in endemic areas. Dracunculus insignis is the species of the nematode that occurs in dogs, cats, and wild carnivores in North America. Infection is particularly prevalent in raccoons and mink that appear to be the natural definitive species. The intermediate host is a crustacean copepod, but frogs may act as paratenic hosts. The definitive host ingests the intermediate host, and the larvae are released during digestion and proceed to migrate through the body. The adult worms mature in the connective tissue of the host in ~1 year. The parasite occurs typically in the subcutaneous tissues of the limbs. The mature female may measure up to 70 cm in length, resulting in the formation of a 2-4 cm nodule. Lesions are usually solitary occurring on the limbs and abdomen. The gravid female produces an intraepidermal bulla with her anterior end by means of toxin secretion. Rupture of the bulla forms a shallow ulcer from which a milky exudate drains. When these lesions contact water, the worm is stimulated to release very large numbers of larvae that are ingested by copepods in the water. Fine-needle aspiration of the cutaneous nodules reveals rhabditiform Dracunculus larvae, ~500 µm long and covered by a striated cuticle. The adults lie in a pseudocyst lined by fibrous connective tissue and infiltrated with eosinophils, lymphocytes, and multinucleated giant cells. Ulcerated lesions are seen as draining tracts that may be painful or pruritic. The parasite can be identified by morphologic features.
Parelaphostrongylus tenuis, a common parasite of white-tailed deer, is an occasional cause of neurologic disease in several domestic species, including goats, sheep, llamas, and alpacas. Some affected goats also develop an unusual dermatitis, often restricted to one side of the body. Lesions are vertically oriented, alopecic, ulcerated, crusted, or scarred linear tracks on the shoulder, thorax, or flanks. The lesions have been explained tentatively on the basis of ganglioneuritis, leading to irritation of dermatomes. Histologically, the lesion is a fibrosing dermatitis with focal areas of basal keratinocyte hydropic degeneration.
Strongyloides papillosus can cause pruritic dermatitis of the feet, legs, and ventrum of cattle, goats, and sheep. Strongyloides spp. have been reported to cause a rough, dull, dry haircoat, hemorrhagic pododermatitis, and crusted lesions on the tail, limbs, and ventrum in puppies.
Larval migrans caused by Anatrichosoma spp. has been reported in 2 cats. Clinical signs included lameness with necrosis, ulceration, and sloughing of multiple pawpads on all paws. This same parasite was reported to produce an erythematous scaling nodular lesion on a dog.
Dirofilaria immitis microfilariae can occasionally lead to cutaneous lesions in dogs harboring the adult parasite. A series of 5 cases document a scabies-like, papular to nodular, variably ulcerated, pruritic dermatitis of the skin of the head, trunk, and extremities in dogs infected with D. immitis. Histologic examination of affected skin revealed angiocentric and pyogranulomatous dermatitis with intralesional microfilariae. The numbers of eosinophils is variable. A type II hypersensitivity response was proposed as a pathogenic mechanism based on positive immunoreaction of microfilariae with anti-IgG serum. Lesions resolved with antiparasitic treatment. Ectopic adult D. immitis have been recovered from cutaneous abscesses and interdigital cysts in parasitized dogs and cats. In addition, a generalized cutaneous syndrome characterized by a pruritic papular and crusting dermatitis without intralesional microfilariae has been apparently associated with infection with D. immitis and was thought to be a manifestation of an unusual hypersensitivity reaction. Parasites are not present in the cutaneous tissues. Lesions also resolved with antiparasitic treatment. Dirofilaria repens can cause subcutaneous dirofilariasis in dogs, cats, and wild carnivores in Europe and parts of Africa and Asia. Like D. immitis, mosquitoes are the intermediate host. During a mosquito's blood meal, L3 larvae penetrate into the subcutaneous tissues of a dog, where they molt to L4 and remain for 6-7 months before developing into adults. Adults are 5-17 cm in length. Adult nematodes are rarely found but are occasionally recovered from skin nodules. Other clinical signs include various degrees of erythema, papules, alopecia, scaling, and crusting. Acanthocheilonema (Dipetalonema) reconditum affects dogs in Europe, America, and Asia. Generally, it is not associated with clinical signs; however, there is one report of 10 dogs with an Acanthocheilonema-like parasite showing single to multiple pruritic papules and plaques with alopecia, scarring, erythema, ulceration, and crusting over the head, neck, and shoulders. Histologic changes included ulceration and perivascular, periglandular, or interstitial mixed inflammatory cell infiltrates with variable eosinophils and plasma cells. Microfilariae were free within the dermis or subcutis and within microgranulomas. No microfilariae were present within vessels. One adult nematode was also present in the cutaneous tissues and was determined to be a Acanthocheilonema sp. Microfilariae are much thinner (4-5 µm wide) than D. immitis (5-7.5 µm wide) and D. repens (7-8 µm wide) and have a hook-shaped tail.
Various Cercopithifilaria spp. are transmitted by ticks to dogs and cats. This organism has been reported in southern and eastern Europe, Australia, Brazil, Malaysia, and South Africa. The lesion described in the dermis of dogs is erythematous papular and pruritic dermatitis with perivascular to interstitial inflammatory infiltrates of neutrophils, eosinophils, and lymphocytes surrounding microfilaria. Adult nematodes occur subcutaneously.
Suifilaria suis occurs in pigs in South Africa. The worms are 2-4 cm long and live in the subcutaneous and intermuscular connective tissues, sometimes producing small white nodules. The female is oviparous, and the eggs are released to the surface via small vesicular eruptions in the epidermis. The remainder of the life cycle is unknown.
Subcutaneous abscesses have been reported in dogs with a number of trematodes, cestodes, and nematodes, including Paragonimus kellicotti, Habronema spp., Gnathostoma spinigerum, Lagochilascaris major, and in cats with L. major and Gordius robustus. The larval cestode of Sparganum proliferum was reported to cause painful erythematous to violaceous nodules in the axillary region of a dog with spread to internal organs. Schistosoma cercariae can penetrate the skin of many warm-blooded abnormal hosts and produce dermatitis. Skin lesions are intensely pruritic and include macules and wheals that develop into papules and vesicles.
Further reading
Cornegliani L, et al. Two cases of cutaneous nodular dirofilariasis in the cat. J Small Anim Pract 2003;44:316-318.
Cortes HC, et al. Diversity of Cercopithifilaria species in dogs from Portugal. Parasit Vectors 2014;7:261.
Elkins AD, Berkenblit M. Interdigital cyst in the dog caused by an adult Dirofilaria immitis. J Am Anim Hosp Assoc 1990;26:71-72.
Gabrielli S, et al. Chronic polyarthritis associated to Cercopthifilaria bainae infection in a dog. Vet Parasitol 2014;205:401-404.
Giudice E, et al. Adult of Dirofilaria repens in a dog with recurrent multiple subcutaneous nodular lesions. Parasitol Res 2014;113:711-716.
Hargis AM, et al. Dermatitis associated with microfilariae (Filarioidea) in 10 dogs. Vet Dermatol 1999;10:95-107.
Langlais L. Dracunculosis in a German shepherd dog. Can Vet J 2003;44:682.
Lucio-Forster A, et al. First report of Dracunculus insignis in two naturally infected cats from the northeastern USA. J Fel Med Surg 2013;16:194-197.
Miller WH, et al. Parasitic skin disease. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 284-342.
Moisan PG. Incidental subcutaneous gordiid parasitism in a cat. J Vet Diag Invest 1996;8:270-272.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Seavers A. Cutaneous syndrome possibly caused by heartworm infestation in a dog. Aust Vet J 1997;76:18-20.
Tarello W. Clinical aspects of dermatitis associated with Dirofilaria repens in pets: a review of 100 canine and 31 feline cases (1990-2010) and a report of a new clinic case imported from Italy to Dubai. J Parasitol Res 2011;2011:578385.
Miscellaneous Skin Conditions
Canine juvenile cellulitis
Canine juvenile cellulitis (juvenile sterile granulomatous dermatitis, puppy strangles, juvenile pyoderma) is an idiopathic disease typically affecting puppies <4 months of age. The cause and pathogenesis are unknown; however, heritability is supported by the fact that the condition is seen more commonly in certain breeds, such as the Golden Retriever, Dachshund, Gordon Setter, Labrador Retriever, and Lhasa Apso, and the condition is sometimes seen in more than one puppy from a litter. An underlying immune dysfunction is strongly suspected because the lesions are sterile when cultured, nontransmissible, and respond to corticosteroids and cyclosporine. Special stains and electron microscopy have also failed to identify intralesional infectious agents. Given the young age of onset, some have suggested vaccine reaction as a possible cause; however, reproduction of the disease with subsequent vaccinations does not occur. Depressed in vitro lymphocyte blastogenesis responses have been reported but likely represent the result not the cause of the disease. A condition clinically and histopathologically identical to juvenile cellulitis has also been reported in adult dogs; however, this is controversial.
Cutaneous lesions comprise papules, pustules, crusts, alopecia, and very marked edema (Fig. 6-124A ). Skin of the muzzle, face, ears, and occasionally the feet, abdomen, vulva, prepuce, and anus are affected. Otitis externa is common, and the pinnae are frequently thickened and edematous. Lymphadenopathy of the mandibular nodes is common and may precede the onset of the skin lesions. Lymphadenitis may also occur in nodes distant to the skin lesions and may occur in the absence of skin lesions. The cutaneous lesions are bilaterally symmetrical, painful, but not pruritic. Some puppies develop concurrent sterile pyogranulomatous panniculitis with firm to fluctuant subcutaneous nodules that may develop draining tracts. Anorexia, fever, malaise, and arthritis affecting multiple joints are common. Lameness and paresis can be seen. One dog was reported to develop juvenile cellulitis 2 weeks after hypertrophic osteodystrophy was diagnosed.
Figure 6-124.

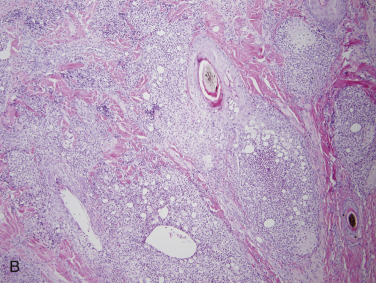
Canine juvenile cellulitis in a puppy. A. Facial edema with alopecia, papules, and crusts around the eyes and muzzle. B. Nodular pyogranulomatous perifollicular dermatitis.
Histologically, the lesions are pyogranulomatous nodular-to-diffuse dermatitis with furunculosis and pyogranulomatous lymphadenitis (Fig 6-124B). Sebaceous glands and epitrichial sweat glands may be obliterated. Inflammation often extends into the panniculus. In some dogs, the condition is self-limiting, resolving in 1-3 months and rarely recurs.
Further reading
Miller WH, et al. Miscellaneous skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 695-723.
Neuber AE, et al. Dermatitis and lymphadenitis resembling juvenile cellulitis in a four-year-old dog. J Small Anim Pract 2004;45:254-258.
Park C, et al. Combination of cyclosporin A and prednisolone for juvenile cellulitis concurrent with hindlimb paresis in 3 English cocker spaniel puppies. Can Vet J 2010;51:1265-1268.
Cutaneous paraneoplastic syndromes
Cutaneous paraneoplastic syndromes are dermatoses associated with internal neoplasms. The neoplasms may be malignant or benign but are most often malignant. In keeping with the definition of a paraneoplastic syndrome, these conditions cannot be directly attributed to the anatomic location of the neoplasm. The skin or mucosal lesions may precede, concur with, or follow the diagnosis of the underlying neoplasm. Removal or elimination of the tumor should alleviate the cutaneous lesions; relapse of the dermatosis signals recurrence of the underlying neoplasm. The majority of cutaneous paraneoplastic syndromes in animals do not have a defined pathogenesis and often have only been reported a limited number of times. These syndromes are better documented in humans, but the increased recognition and clinical significance in domestic animals warrants mention in this chapter. The well-recognized cutaneous lesions seen with functional pituitary, adrenal, or testicular tumors are discussed elsewhere (see Endocrine diseases of skin). Cutaneous lesions associated with the cryoglobulinemia associated with multiple myelomas have been discussed elsewhere (see Other immune-mediated dermatoses).
A unique dermatosis reported in aged cats is characterized by symmetrical ventrally distributed alopecia affecting the trunk and limbs (Fig. 6-125A ) and has been reported to be associated with a concurrent pancreatic carcinoma or bile duct carcinoma. Crusting and brown-black waxy debris tends to be associated with a secondary Malassezia dermatitis. Pawpads may have concentric circular scales and fissures. The alopecia is due to marked follicular atrophy (Fig. 6-125B). Hair follicles are diffusely in telogen and appear miniaturized. Surrounding sebaceous glands are usually normal but may be atrophic in some cases. The epidermis is mildly hyperplastic and often lacks a stratum corneum, giving the regions of affected skin the characteristic “glistening” or moist appearance. The lack of the stratum corneum may be due to licking by the cat. In some areas, there may be parakeratotic hyperkeratosis. Inflammation is not a feature unless complicated by secondary infection. Pawpads may be softened and hyperkeratotic. The pancreatic carcinoma is usually in an advanced stage, often with hepatic metastasis at the time of diagnosis, and the prognosis is grave. The condition must be differentiated from hyperadrenocorticism and feline psychogenic alopecia.
Figure 6-125.

Feline paraneoplastic alopecia. A. Extensive alopecia of the entire ventrum, medial limbs, paws, periocular, and muzzle region in a bilaterally symmetrical distribution. Note the glistening appearance to the skin that is a striking feature of this disease
(Courtesy M.S. Canfield.)
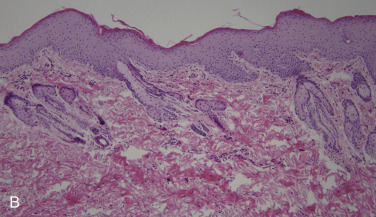
B. Epidermal hyperplasia and marked follicular atrophy.
Thymoma and concurrent exfoliative dermatitis has been reported in cats. Cats are usually aged and may have signs such as dyspnea and coughing referable to an intrathoracic mass. Cutaneous lesions may be well developed prior to onset of respiratory signs. The cutaneous lesions consist of dry exfoliative dermatitis with large scales over the head, neck, and pinnae that may become generalized. Brown, waxy material often accumulates at mucocutaneous junctions and in interdigital spaces and clawbeds. Some lesions may have erythema, thickened skin, and marked crusting with alopecia. The condition is generally nonpruritic unless there is a secondary pyoderma or Malassezia dermatitis. Histologically, there is a cell-poor to cell-rich predominantly lymphocytic interface dermatitis with mild transepidermal and follicular apoptosis and marked orthokeratotic hyperkeratosis, with patchy parakeratotic hyperkeratosis. The interface changes include Civatte bodies, hydropic degeneration, and pigmentary incontinence with a band-like lymphocytic infiltrate with fewer plasma cells and mast cells. Lymphocytic interface to infiltrative mural folliculitis is a consistent feature, and sebaceous glands are frequently reduced to absent. Some cases have been reported to also have an overgrowth of Malassezia pachydermatis and bacteria. It has been speculated that the presence of a thymoma initiates abnormal immunologic responses responsible for the dermatitis, which at times can resemble erythema multiforme or graft-versus-host dermatitis histologically. This condition has been reported in a rabbit and anecdotally in dogs.
Necrolytic migratory erythema (hepatocutaneous syndrome, superficial necrolytic dermatitis) has been reported in dogs and occasionally the cat. The condition is sometimes associated with endocrine tumors of the pancreas (see Nutritional diseases of skin).
Multiple collagenous hamartomas (nodular dermatofibrosis) of the distal limbs, head, and pinnae have been reported in middle-aged German Shepherd dogs and occasionally other breeds (Golden Retriever, Boxer, Belgian Shepherd, mixed breed) in association with renal cysts, renal cystadenocarcinomas, and/or uterine leiomyomas. Both kidneys are often affected. The cutaneous lesions range from 2-40 mm. The overlying skin may be normal, thickened, hyperpigmented, alopecic, or ulcerated. Histologically, the skin lesions are nodules composed of increased numbers of slightly thickened collagen bundles within the subcutis or occasionally the dermis. Animals are usually presented for examination of the cutaneous lesions prior to signs referable to the internal neoplasms. Death occurs most often because of complications of the renal lesions. Multiple collagenous hamartomas are suspected to be inherited in an autosomal dominant manner in German Shepherd dogs.
Severe generalized pruritus without primary gross or histologic cutaneous lesions or other identifiable cause for pruritus has been reported in the dog and horse in association with underlying malignant lymphoma. Self-trauma can lead to extensive excoriations and secondary infection. This condition is also reported in humans with lymphoma and a variety of other internal malignancies. The mechanism of the development of pruritus is not understood but is speculated to be related to tumor-induced release of chemical mediators. Pruritus can only be relieved by successful treatment of the malignancy.
Paroxysmal cutaneous flushing of extensive areas of the skin without pruritus has been reported in a German Shepherd dog with an intrathoracic mast cell tumor and pulmonary adenocarcinoma. Functional pheochromocytomas upon rare occasion can lead to cutaneous flushing in the dog. Flushing is due to vasodilation and is usually caused by vasoactive mediators.
Occasionally, vesicular, pustular, or bullous dermatoses virtually identical to idiopathic autoimmune skin diseases may be associated with an underlying malignancy. The tumor is suspected to trigger the production of autoantibodies. These types of paraneoplastic dermatoses must be differentiated from true autoimmune skin diseases as the prognosis may vary. Differentiation is based on ruling out the presence of an underlying neoplasm and resolution of the skin lesions with tumor removal. A subepidermal bullous stomatitis microscopically identical to bullous pemphigoid has been reported in a horse in association with a hemangiosarcoma. Immunoprecipitation studies indicated the horse had antibodies to desmoplakin I and II, the bullous pemphigoid 230 antigen, and a 190-kDa antigen. This immunoprecipitation profile was consistent with that reported for paraneoplastic pemphigus as reported in humans and the dog. Paraneoplastic pemphigus is a form of pemphigus that is sometimes associated with an underlying malignancy and has been previously discussed (see Immune-mediated dermatoses).
Further reading
Anderson RK, Carpenter JL. Severe pruritus associated with lymphoma in a dog. J Am Vet Med Assoc 1995;207:455-456.
Brooks DG, et al. Pancreatic paraneoplastic alopecia in three cats. J Am Anim Hosp Assoc 1994;30:557-563.
Castellano MC, et al. Generalized nodular dermatofibrosis and cystic renal disease in five German Shepherd dogs. Canine Pract 2000;25:18-21.
Day MJ. Review of thymic pathology in 30 cats and 36 dogs. J Small Anim Pract 1997;38:393-403.
Finley MR, et al. Paraneoplastic pruritus and alopecia in a horse with diffuse lymphoma. J Am Vet Med Assoc 1998;213:102-104.
Forster-van Hufte MA, et al. Resolution of exfoliative dermatitis and Malassezia pachydermatis overgrowth in a cat after surgical thymoma resection. J Small Anim Pract 1997;38:451-454.
Godfrey DR. A case of feline paraneoplastic alopecia with secondary Malassezia-associated dermatitis. J Small Anim Pract 1998;39:394-396.
Lemmens P, et al. Paraneoplastic pemphigus in a dog. Vet Dermatol 1998;9:127-134.
Miller WH, et al. Pigmentary abnormalities. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 618-629.
Pascal-Tenoria A, et al. Paraneoplastic alopecia associated with internal malignancies in the cat. Vet Dermatol 1997;7:221-226.
Rottenberg S, et al. Thymoma-associated exfoliative dermatitis in cats. Vet Pathol 2004;41:429-433.
Turek MM. Cutaneous paraneoplastic syndromes in dogs and cats: a review of the literature. Vet Dermatol 2003;14:279-296.
White SD, et al. Nodular dermatofibrosis and cystic renal disease in three mixed-breed dogs and a boxer dog. Vet Dermatol 1998;9:119-126.
Williams AA, et al. Paraneoplastic bullous stomatitis in a horse. J Am Vet Med Assoc 1995;207:331-334.
Eosinophilic dermatitides
Eosinophilic dermatitis is not a disease but rather a cutaneous reaction pattern to a variety of stimuli, including environmental allergens, food, insects, parasites, drugs, endogenous (e.g., free keratin in the dermis) and exogenous (embedded insect parts) foreign material, and even some viral infections, such as feline herpesvirus 1 in cats. Eosinophils are one of the major sources of inflammatory mediators associated with type I hypersensitivity reactions. Eosinophils can phagocytize small antigens, and they can kill large parasites by releasing toxic substances via degranulation. Eosinophils have 4 major granules containing a wide variety of proteins and enzymes: primary granules, secondary granules, small granules, and lipid bodies. Secondary granules contain major basic protein, eosinophilic cationic protein, eosinophilic peroxidase, and eosinophil-derived neurotoxin. Small granules contain arylsulfatase and acid phosphatase. Lipid bodies are responsible for eicosanoid formation. Eosinophils also produce transforming growth factor-β that is associated with chronic inflammation and fibrosis. Taken as a whole, the contents within eosinophil granules are responsible for inflammation and tissue destruction. They have profound vasoactive and neurogenic properties that manifest clinically as erythema, wheals, and pruritus. Eosinophilic inflammation in the horse and cat is a common tissue reaction, and it seems that the chemotactic stimuli that attract neutrophils in most species attract both eosinophils and neutrophils in these 2 species.
Feline eosinophilic granuloma complex
The eosinophilic granuloma complex (EGC) includes a group of lesions (feline eosinophilic granuloma, eosinophilic plaque, indolent ulcer) that affect the skin, mucocutaneous junctions, and oral cavity of cats. These lesions can occur separately or together and, rather than a specific disease, are considered a mucocutaneous reaction pattern. In most cases, an underlying allergic etiology, particularly to environmental allergens, food, and insect bites (fleas and mosquitoes), are suspected. In human patients with severe atopic dermatitis (AD), there is some evidence to suggest that although the disease is initiated by environmental allergens, some patients may form IgE antibodies directed against human proteins (self-antigens) generated through self-trauma from scratching. Felis domesticus allergen I (Feld I) could be an autoallergen responsible for chronic inflammatory reaction in cats with EGC. And in other cases, the lesions spontaneously resolve and do not recur, making allergy an unlikely trigger in those cases. Bacterial involvement may be a significant factor, especially with indolent ulcers and eosinophilic plaques, and in some cases, lesions resolve with antibiotic therapy alone. In some cases, the oral and lip lesions are thought to be due to embedded foreign material such as insects or plants. Because this condition has been reported in several groups of related cats, there is some evidence to suggest heritable eosinophil dysregulation. Clinically and histologically, these 3 conditions have distinct features, although histologically the features can overlap.
Feline eosinophilic plaque is a common cutaneous lesion in cats. Lesions are pruritic, and affected cats lick them constantly, resulting in well-demarcated, singular to multiple, raised, erythematous, alopecic, eroded to ulcerated to oozing plaques that can develop peracutely (Fig. 6-126 ). Lesions occur most commonly on the ventral abdomen, perineum, and medial thigh. Secondary bacterial infection is common. Peripheral lymphadenopathy may be present. Histologically, the lesions are characterized by epidermal hyperplasia and moderate to marked spongiosis with exocytosis of eosinophils. In some cases, there is epidermal and follicular epithelial mucinosis characterized by pale basophilic or gray mucin between keratinocytes. Inflammation in the dermis is perivascular to interstitial and sometimes diffuse, containing numerous eosinophils, and may extend into the subcutis. Mast cells, lymphocytes, and macrophages are present in smaller numbers.
Figure 6-126.

Eosinophilic plaque on the ventral abdomen of a cat.
(Courtesy W.H. Miller.)
Feline eosinophilic granuloma (linear granuloma) is a common cutaneous, mucocutaneous, and oral lesion in cats. This lesion is the most variable in its clinical presentation and, of the 3 lesions in the EGC, is the most likely to be considered idiopathic. It is often nonpruritic. It can occur at any age; however, it is more common in young cats. Spontaneous regression can occur, especially in cats <1 year of age. A genetic predisposition has been documented in some cases. The lesions can be papular, nodular, or linear, and occur on the skin, pawpads, mucocutaneous junctions, and in the oral cavity. Linear lesions are more common on the caudal or medial thigh, and nodular lesions are more common on the lips, chin, oral cavity, and face (Fig. 6-127 ). The lesions are raised, pink to orange-yellow, and frequently alopecic. Some, especially oral lesions, may be ulcerated with multifocal pinpoint yellow to white foci over the surface. Histologically, the lesions are characterized by diffuse dermal inflammation composed primarily of eosinophils, with fewer mast cells, macrophages, and occasional lymphocytes. Within the inflammation are large irregular foci of collagen fibers and degranulated and degenerating eosinophils (flame figures). These foci may be surrounded by macrophages and multinucleated histiocytic giant cells. Older lesions tend to have palisading granulomas around flame figures with fewer eosinophils. Mucinosis of the epidermis and hair follicle outer root sheath, focal infiltrative to necrotizing mural eosinophilic folliculitis or furunculosis, and focal eosinophilic panniculitis may be present. The epidermis may be acanthotic or ulcerated.
Figure 6-127.

Eosinophilic granuloma on the chin of a cat.
(Courtesy of W.H. Miller.)
Indolent ulcer (rodent ulcer) is a common and clinically distinct condition in cats. Clinically, the condition is characterized by an ulcerated lesion on the upper lip adjacent to the philtrum, which can be unilateral or bilateral (Fig. 6-128 ). The ulcers are not pruritic or painful. Peripheral lymphadenopathy may be present. Histologically, the acute lesions are characterized by diffuse infiltrates of neutrophils with variable numbers of eosinophils, mast cells, and macrophages; however, the lesions are more often biopsied in the chronic phase when the inflammation is composed almost entirely of lymphocytes, plasma cells, macrophages, and neutrophils, together with fibrosis. The numbers of neutrophils vary according to the degree of ulceration. Concurrent bacterial infection is common, and some lesions resolve with antibiotic therapy alone.
Figure 6-128.

Indolent ulcer in a cat.
(Courtesy of W.H. Miller.)
Further reading
Bardagi M, et al. Ultrastructural study of cutaneous lesions in feline eosinophilic granuloma complex. Vet Dermatol 2003;14:297-303.
Bloom PB. Canine and feline eosinophilic skin diseases. Vet Clin North Am Small Anim Pract 2006;36:141-160.
Buckley L, Nuttall T. Feline eosinophilic granuloma complex(ities) some clinical clarification. J Fel Med Surg 2012;14:471-481.
Gross TL, et al. Skin Diseases of the Dog and Cat: Clinical and Histopathologic Diagnosis. 2nd ed. Ames, Iowa: Blackwell; 2005.
Miller WH, et al. Miscellaneous skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 695-723.
Scott DW, Miller WH. Idiopathic eosinophilic granuloma in cats: a retrospective study of 55 cases (1988-2003). Jpn J Vet Dermatol 2012;18:13-18.
Canine eosinophilic granuloma
This is a rare condition in dogs that has many histologic similarities to feline eosinophilic granuloma. Any breed and age can be affected; however, the condition appears to be more common in Siberian Huskies, in dogs <3 years of age, and males. There may be a genetic basis for the disease in Siberian Huskies and Cavalier King Charles Spaniels. The etiology is unknown, although a hypersensitivity has been proposed, because of the fact that the lesions are corticosteroid responsive, the eosinophilic nature of the lesions, and that there is occasionally circulating eosinophilia. The lesions can be nodules or plaques, and occur most commonly in the mouth and on the tongue. Skin lesions are less frequent, although singular to multiple papules, nodules, or plaques have been described on the ventral abdomen, prepuce, digits, flanks, muzzle, external ear canal, nasal planum, and eyelid. Histologically, the lesions are composed of diffuse dermal eosinophilic inflammation within which are foci of degranulating eosinophils sometimes surrounded by epithelioid macrophages. The overlying epithelium or epidermis may be acanthotic or ulcerated.
Further reading
Bredal WP, et al. Oral eosinophilic granuloma in three Cavalier King Charles spaniels. J Small Anim Pract 1996;37:499-504.
Poulet FM, et al. Focal proliferative eosinophilic dermatitis of the external ear canal in four dogs. Vet Pathol 1991;28:171-173.
Vercelli A, et al. Eyelid eosinophilic granuloma in a Siberian husky. J Small Anim Pract 2005;46:31-33.
Equine eosinophilic nodular diseases
Eosinophilic inflammation is a common reaction pattern in the horse, and cutaneous nodules, either single or multiple, are common skin lesions in the horse. Nodular conditions of unknown etiology and pathogenesis include eosinophilic granuloma, axillary nodular necrosis, and unilateral papular dermatosis. Other eosinophilic nodular conditions with known etiologies, such as cutaneous habronemiasis, can look histologically similar (see Helminth diseases of skin). Cutaneous mast cell tumors in the horse can also be seen clinically as cutaneous nodular lesions, and, as histologically, they may contain significant numbers of eosinophils and areas of necrosis, care should be taken to differentiate this tumor from an inflammatory eosinophilic lesion.
Eosinophilic granuloma is the most common of the equine cutaneous eosinophilic nodular diseases and is the most common inflammatory nodular skin disease of the horse. The condition is seen most often in the spring and summer, but can occur at any time of year. The etiology is unknown but probably multifactorial. Proposed causes include insect-bite hypersensitivity, atopic dermatitis, food allergy, localized trauma, injections from silicone-coated needles, and close-clipping with free hair shafts embedded in the dermis provoking the inflammatory response. The lesions occur as single or multiple, firm, raised, well-circumscribed, round papules or nodules measuring 0.5-10 cm in diameter, most commonly on the withers, neck, and back, but can occur anywhere on the body and can be generalized. The lesions are neither painful nor pruritic, and the overlying skin and haircoat are typically normal. Histologically, there are nodular-to-diffuse infiltrates of eosinophils and granulomatous inflammation in the dermis and panniculus. There may be multiple collagen flame figures surrounded by palisading granulomas (Fig. 6-129 ). Other histologic features include eosinophilic folliculitis and furunculosis, lymphoid nodules, and dystrophic mineralization. The granulomatous process is fairly linear in silicone-needle injection reactions. Free hair shafts within the lesion suggest previous close-clipping.
Figure 6-129.
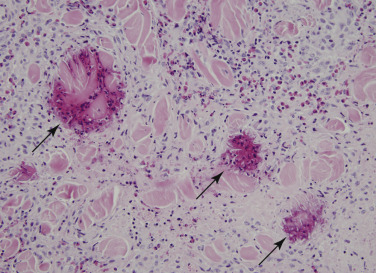
Multiple “flame figures” (arrows) in an equine eosinophilic granuloma.
Axillary nodular necrosis (girth galls) is a rare dermatosis of the horse. The cause and pathogenesis are unknown. The cutaneous and subcutaneous nodules are firm, round, well circumscribed, 1-10 cm in diameter, and can be single or multiple, usually not more than 10. They are usually unilateral and occur on the trunk behind the axilla, Lesions may also be seen caudal to the shoulder and on the proximal medial aspect of the forelimb. The overlying skin and haircoat are usually normal, and lesions are neither pruritic nor painful. Lesions are sometimes arranged in a linear pattern. Histologically, the lesions are characterized by interstitial to nodular-to-diffuse eosinophilic granulomatous dermatitis and panniculitis with foci of coagulative necrosis, collagen flame figures, dystrophic mineralization, palisaded granulomas, and lymphoid nodules. Eosinophilic arteritis is characterized by intimal mucinosis and karyorrhectic nuclear debris in the tunica media. Necrotizing arteritis may be seen.
Unilateral papular dermatosis is an uncommon condition in horses, seen worldwide but reported primarily in the United States, and is more common in spring and summer. It has been seen in many breeds, although Quarter Horses appear to be over-represented. The etiology is unknown; however, the seasonality of the lesions together with the eosinophilic nature of the histologic findings suggests ectoparasite hypersensitivity. It has further been suggested that the unilateral distribution may indicate direct contact hypersensitivity to an ectoparasite inhabiting bedding. Clinically, the lesions are multiple cutaneous papules and nodules measuring 2-10 mm, which occur in a unilateral distribution, usually on the trunk but sometimes on the neck, shoulders, or abdomen. There is neither pruritus nor pain; however, some lesions become crusted and alopecic. The histologic lesions are characterized by eosinophilic folliculitis and furunculosis. Eosinophilic granulomas and collagen flame figures may be present in the surrounding dermis.
Further reading
Rothwell TL, Birch CB. Unilateral papular dermatitis in a horse. Aust Vet J 1991;68:122-123.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Slovis NM, et al. Injection site eosinophilic granulomas and collagenolysis in 3 horses. J Vet Intern Med 1999;13:606-612.
von Tscharner C, et al. Stannard's illustrated equine dermatology notes. Nodular diseases. Vet Dermatol 2000;11:179-186.
Multisystemic, eosinophilic, epitheliotropic disease in the horse
This rare disease typically occurs in young horses (mean 3-4 years of age) and is characterized by eosinophilic infiltration of many organs, including skin. The cause of multisystemic, eosinophilic, epitheliotropic disease is unknown. A genetic basis has been proposed; Standardbreds and Thoroughbreds are over-represented. Recurrent episodes of type I hypersensitivity caused by dietary, inhaled, or parasitic antigens has been suggested in several reports. There is one report of this condition occurring concurrently with intestinal lymphoma, and several other unpublished cases that appear identical to the case described; the authors suggest that the clonal proliferation of T lymphocytes triggers proliferation of eosinophils by secretion of cytokines such as interleukin-5. This mechanism has also been proposed in humans who have concurrent abnormal T-lymphocyte proliferations and hypereosinophilic syndrome.
Affected horses often display severe weight loss, pitting edema, and exudative, exfoliative dermatitis that usually originates at the coronary bands or head and becomes generalized. Chronically, there is scaling, crusting, and alopecia. Early findings include well-demarcated ulcers on the coronary bands, muzzle, mucocutaneous junctions, and mouth. Vesicles, bullae, and wheals are rarely noted. Pruritus is variable, and peripheral lymph nodes may be enlarged. Approximately 50% of horses have diarrhea and fever. Peripheral eosinophilia is only present in ~14% of cases. Histologically, the condition is characterized by eosinophilic and lymphoplasmacytic infiltration of multiple organs, sometimes with eosinophilic granuloma formation. Organs most commonly affected include skin, pancreas, liver, common bile duct, gastrointestinal tract, and lungs. In the skin, the inflammatory pattern is variable, including perivascular, lichenoid interface, interstitial, diffuse, and granulomatous. Eosinophils, lymphocytes, and plasma cells predominate. There is marked epidermal hyperplasia with hyperkeratosis that is orthokeratotic and parakeratotic. An epitheliotropic infiltrate of eosinophils and lymphocytes is common, and apoptotic keratinocytes may be prominent. Eosinophilic folliculitis, furunculosis, and eosinophilic microabscesses may be seen. Collagen flame figures and lymphoid nodules are seen occasionally. Most horses suffer a chronic course of progressive weight loss and dermatitis and die or are euthanized within 8 months of diagnosis.
Further reading
Bosseler L, et al. Equine multisystemic eosinophilic epitheliotropic disease: a case report and review of literature. N Z Vet J 2013;61:177-182.
La Perle KMD, et al. Multisystemic, eosinophilic, epitheliotropic disease with intestinal lymphosarcoma in a horse. Vet Pathol 1998;35:144-146.
Schumacher J, et al. Chronic idiopathic inflammatory bowel diseases of the horse. J Vet Intern Med 2000;14:258-265.
Sterile eosinophilic folliculitis and furunculosis
In dogs, eosinophilic folliculitis and furunculosis is a condition that typically affects the face. The etiology of this condition has not been fully characterized, but a hypersensitivity reaction to insect stings and arthropod bites is strongly suspected. The condition is most common in young, large-breed dogs, and lesions are seen primarily on the dorsal muzzle, around the eyes, ears, and less commonly in the axillae, inguinal areas, and ventrum. Lesions are characterized by sudden onset of vesicles, papules, nodules, crusts, erosions, and ulcers. Pruritus is variable but can be intense. Lesions are painful in some dogs.
In horses, sterile eosinophilic folliculitis and furunculosis can be seen in horses with atopic dermatitis, insect-bite hypersensitivity, food allergy, unilateral papular dermatosis, and onchocerciasis. Lesions are characterized by tufted papules that become alopecic and crusted in a generally symmetrical and multifocal distribution anywhere on the body; however, the neck, shoulders, chest, and dorsolateral thorax are most commonly affected. Pruritus is variable but is commonly moderate to marked.
Sterile eosinophilic folliculitis has been reported in cattle and is characterized by nonpainful, nonpruritic, symmetrically distributed, multiple crusting, or alopecic papules and plaques primarily on the head, neck, and trunk. The condition in nonseasonal, and the cause is unknown. In cats, sterile eosinophilic folliculitis and furunculosis may be seen as a bystander lesion in any allergic dermatitis; however, it is more commonly seen in mosquito-bite hypersensitivity and feline herpesvirus dermatitis, both of which are most commonly located on the face and head.
Histologically, sterile eosinophilic folliculitis and furunculosis are characterized by infiltrative eosinophilic mural folliculitis, luminal eosinophilic folliculitis, and eosinophilic furunculosis. Within the dermis, there is marked edema and mucin accumulation along with variable numbers of eosinophils, neutrophils, and mononuclear cells. Dermal hemorrhage may be prominent in dogs. Collagen flame figures may be present. There is moderate to severe epidermal hyperplasia, spongiosis, and serocellular crusts. There may also be erosions and ulcerations.
Canine sterile eosinophilic pinnal folliculitis is an uncommon, nonseasonal, bilaterally symmetrical dermatosis with variable pruritus and an unknown cause and pathogenesis. Erythematous papules and crusts are present on the concave surface of the pinnae. Eosinophilic folliculitis and furunculosis are seen with histopathology.
Sterile eosinophilic pustulosis
This is a rare idiopathic dermatosis of dogs characterized by peripheral eosinophilia, sterile tissue eosinophilia, and responsiveness to systemic glucocorticoids. Skin lesions include multifocal to generalized pruritic, erythematous, follicular, and nonfollicular papules and pustules that evolve into annular targetoid lesions with erosions, epidermal collarettes, and hyperpigmentation. Histopathology is characterized by subcorneal pustules containing eosinophils and fewer neutrophils. There may be various degrees of flame figures and eosinophilic folliculitis and furunculosis.
Further reading
Gross TL, et al. Pustular and nodular diseases with adnexal destruction. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 406-459.
Guaguere E, et al. Eosinophilic furunculosis. A study of 12 dogs. Prat Med Chirurg Anim Cie 1996;31:413-419.
Hargis AM, et al. Ulcerative facial and nasal dermatitis and stomatitis in cats associated with feline herpesvirus 1. Vet Dermatol 1999;10:267-274.
Miller WH, et al. Miscellaneous skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 695-723.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, et al. Diseases of eyelids, claws, anal sacs, and ears. In: Scott DW, et al., editors. Muller & Kirk's Small Animal Dermatology. 6th ed. Philadelphia: WB Saunders; 2001. p. 1185-1235.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Eosinophilic dermatitis with edema
This is a unique condition in dogs characterized by severe erythema and erythematous to hemorrhagic macules or plaques most pronounced on the ventral abdomen and limbs. Some dogs have lesions with central clearing (targetoid macules), wheals, facial swelling, or generalized edema. The cause is unknown; however, about  of the reported cases have been dogs treated for vomiting and diarrhea; thus drug association has been suspected in many cases. The histologic lesions are marked perivascular to diffuse eosinophilic dermatitis with edema. Collagen flame figures are seen in some cases. Eosinophilic intraepidermal pustules may be present.
of the reported cases have been dogs treated for vomiting and diarrhea; thus drug association has been suspected in many cases. The histologic lesions are marked perivascular to diffuse eosinophilic dermatitis with edema. Collagen flame figures are seen in some cases. Eosinophilic intraepidermal pustules may be present.
Further reading
Holm KS, et al. Eosinophilic dermatitis with edema in nine dogs, compared with eosinophilic cellulitis in humans. J Am Vet Med Assoc 1999;215:649-653.
Mauldin EA, et al. Comparison of clinical history and dermatologic findings in 29 dogs with severe eosinophilic dermatitis: a retrospective analysis. Vet Dermatol 2006;17:338-347.
Sterile neutrophilic dermatoses
Sterile neutrophilic dermatosis is a very rare condition, described in dogs, with marked similarities to the human disease known as acute febrile neutrophilic dermatosis (Sweet's syndrome). Reported lesions include painful red papules, nodules, and plaques with variable degrees of edema and ulceration. Other clinical signs include fever, arthritis, pneumonia, and circulating neutrophilia. The pathogenesis is unknown; however, it is believed to be an antigen-induced T-cell–mediated immune reaction. Possible triggers include drugs, respiratory and gastrointestinal infections, and neoplasia. Three cases have been associated with carprofen. Histologically, there is moderate to severe interstitial neutrophilic dermatitis with variable eosinophils and neutrophilic infiltration into the epidermis forming small pustules.
Subcorneal pustular dermatosis is a very rare, sterile, superficial, pustular condition of dogs with an unknown cause and pathogenesis. Miniature Schnauzers are over-represented. Lesions are multifocal to generalized, symmetrical, and commonly affect the head and trunk. They include intact nonfollicular transient green to yellow pustules that evolve into areas of alopecia, epidermal collarettes, and hyperpigmentation. Lesions may spread peripherally into annular and serpiginous formations. Pruritus is variable and may be extreme. Pawpads are rarely affected.
Further reading
Gross TL, et al. Pustular and nodular diseases without adnexal destruction. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 406-459.
Miller WH, et al. Miscellaneous skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 695-723.
Auricular chondritis
Auricular chondritis (relapsing polychondritis) is a rare condition in the cat and dog characterized by inflammation and destruction of the auricular cartilage. The condition was named after a similar human condition thought to be an immune-mediated attack directed against type II collagen and known to affect other cartilaginous sites, such as the nose, trachea, and cardiac valves. The cause is unknown in cats and dogs, in most cases only affects the pinnae, is generally not reported to relapse, and an autoimmune or immune-mediated pathogenesis has not been supported. In one case, cartilaginous lesions were also noted in the costae, larynx, trachea, and limbs, and the cat had multicentric lymphoma. Trauma or damage to the pinnal cartilage has been proposed as a possible initiator. In a few cases, chronic otitis externa has preceded the development of the disease. Clinically, the condition occurs in young to middle-aged cats and dogs; one or both pinnae are swollen, erythematous, deformed, and often painful. Histologically, the auricular cartilage may be thinned, curled, or wrinkled, with loss of basophilic staining. Lymphoplasmacytic infiltrates and variable numbers of neutrophils surround areas of necrosis of the auricular cartilage. Variable amounts of granulation tissue and fibrosis may be seen.
Nodular auricular chondropathy has been described rarely in horses. The condition occurs as nonprogressive, single to multiple, unilateral to bilateral, firm, raised, nonmoveable, nonpainful papules and nodules along the pinnal margins and tips. Affected cartilage is disorganized, necrotic, or mineralized.
Further reading
Baba T, et al. Auricular chondritis associated with systemic joint and cartilage inflammation in a cat. J Vet Med Sci 2009;71:79-82.
Gerber B, et al. Feline relapsing polychondritis: two cases and a review of the literature. J Feline Med Surg 2002;4:189-194.
Miller WH, et al. Autoimmune and immune-mediated dermatoses. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 432-500.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Follicular lipidosis
Follicular lipidosis is characterized by regional alopecia of areas of mahogany-colored points of the hair of the paws and face of Rottweiler puppies. Histologically, the lesions are characterized by marked swelling, caused by lipid accumulation, of the hair matrix cells of primary anagen hair follicles. Matrix cells of the bulb are most severely affected, whereas cells of the internal and external root sheath are affected to a lesser degree. Scattered hair shafts may contain vacuoles and have irregular, thickened, or frayed cuticles. This condition may represent yet another type of color-associated follicular dysplasia. Too few cases have been recognized to clearly predict the clinical course of the alopecia, or to identify associated abnormalities or the mode of inheritance, if any.
Further reading
Gross TL, et al. Follicular lipidosis in three Rottweilers. Vet Dermatol 2001;8:33-40.
Follicular mucinosis (alopecia mucinosa)
Follicular mucinosis is characterized by collections of mucin in the outer root sheath of the follicular epithelium and of sebaceous glands. Intraepithelial cysts filled with mucin may form. Grossly, the lesions consist of progressive alopecia and scaling that may become generalized. A disease resembling follicular mucinosis in humans has been described in the cat and dog. The condition described in 2 cats chiefly affected the head, neck, and shoulders. Histologically, there was mucinous degeneration of the outer root sheath of the follicular infundibulum. Both cats had swollen facial skin and developed epitheliotropic lymphoma within several months of the initial biopsy. Follicular mucinosis has been reported in 2 older dogs. The skin of the head, limbs, and some areas of the trunk was affected. In addition to the histologic lesions described above, there was a perivascular and perifollicular lymphocytic to plasmacytic infiltrate. The epidermis was mildly acanthotic with compact orthokeratotic hyperkeratosis and multifocal spongiosis with lymphocytic exocytosis. The basal cell layer demonstrated hydropic degeneration, mild apoptosis, and prominent pigmentary incontinence. No follow-up information was available. In humans, follicular mucinosis can resolve spontaneously or become a chronic relapsing condition. Many cases are thought to progress to epitheliotropic lymphoma. It should be noted that epidermal and epithelial mucinosis can be seen in various allergic dermatitides of the cat.
A condition in cats described as degenerative mucinotic mural folliculitis has many similarities to follicular mucinosis. Seven cats have been described, and they all had a several-month to 2-year history of progressive hair loss that started on the face or neck and led to generalized alopecia. The skin of the face, particularly the muzzle, of all the cats was thickened and swollen. There was variable scaling, crusting, and hyperpigmentation. Most of the cats were lethargic, 4 were pruritic, 3 had concurrent feline immunodeficiency virus, and 2 had weight loss. Six of the cats were euthanized because of progressive disease. Histologically, there was moderate to severe mucin accumulation in the superficial outer root sheath. Most cases had follicular atrophy with infiltrative mural folliculitis consisting of lymphocytes, plasma cells, macrophages, and neutrophils focused primarily on the isthmus with extension to the perifollicular dermis. In some cases, pyogranulomas effaced the isthmus of some follicles. In addition, there was moderate epidermal hyperplasia, compact hyperkeratosis, and neutrophilic crusts. In contrast to alopecia mucinosa, interface changes were not described, and none of these cats developed epitheliotropic lymphoma.
Feline scleromyxedema
Scleromyxedema is the generalized form of lichen myxedematosus, a primary dermal mucinosis. This condition is very rare and is characterized by dermal mucin deposits on the head and legs, increased numbers of fibroblasts, variable fibrosis, absence of thyroid disease, and a monoclonal gammopathy. Mucin deposits are also detected on thoracic and abdominal organs.
Further reading
Bell A, Oliver F. Alopecia mucinosa (follicular mucinosis) in a dog. Vet Dermatol 1995;6:221-226.
Gross TL, et al. Degenerative mucinotic mural folliculitis in cats. Vet Dermatol 2001;12:279-283.
Gross Tl, et al. Mural diseases of the hair follicle. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 460-479.
Ishida M, et al. Adult T-cell leukemia/lymphoma accompanying follicular mucinosis: a case report with review of the literature. Int J Clin Exp Pathol 2013;6:3014-3018.
Müntener T, et al. Scleromyxedema-like syndrome with systemic involvement in a cat. Vet Pathol 2010;47:346-350.
Scott DW. Feline dermatology 1983-1985: “The secret sits.” J Am Anim Hosp Assoc 1987;23:255-274.
Localized scleroderma (morphea) and cicatricial alopecia
Localized scleroderma (morphea) is a rare disease described in humans, dogs, cats, and a horse. The cause is unknown; but in humans, vascular injury, abnormal collagen metabolism, and an immune-mediated pathogenesis, such as drug reaction, have all been proposed. Asymptomatic, well-demarcated, sclerotic plaques that are alopecic, smooth, and shiny characterize the condition. Hypopigmentation may occur. Lesions tend to be oval to linear and occur on the trunk, limbs, and head. Histologically, the epidermis is normal, and the dermis is replaced by collagenous connective tissue. Pilosebaceous units are essentially absent. A very mild superficial and deep perivascular accumulation of lymphohistiocytic cells is present. Spontaneous resolution has been reported.
Cicatricial alopecia is grossly and microscopically very similar; however, in this condition, lesions are permanent. Causes include a variety of insults that result in fibrous tissue deposition: injection-site reactions, furunculosis, vasculitis, dermatomyositis, post-traumatic scarring, and so on. Histologically, there is laminar arrangement of collagen replacing the dermis, and the epidermis is hyperplastic. Scattered orphaned sweat glands may be seen.
Generalized scleroderma is a rare multisystemic disorder that results in progressive fibrosis of the skin, lungs, gastrointestinal tract, kidneys, and heart. It has been described in humans and a horse.
Further reading
Frank LA, et al. Diffuse systemic sclerosis in a Paso Fino mare. Comp Cont Educ Pract Vet 2000;22:274.
Gross TL, et al. Degenerative, dysplastic, and depositional diseases of dermal connective tissue. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 373-403.
Miller WH, et al. Miscellaneous skin diseases. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 695-723.
Scott DW, Miller WH. Miscellaneous skin diseases. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 436-467.
Psoriasiform dermatitis of goats
This is a rare condition described in pygmy goats and alpine goats most commonly. Affected animals range from 3 months to young adults. Lesions are nonpruritic and begin on the face and pinnae and may also affect the neck, ventrum, and distal limbs. There is erythema, scaling, and variable degrees of crusting, thickened skin, and alopecia. Lesions wax and wane. Psoriasiform epidermal hyperplasia, neutrophilic intraepidermal microabscesses with neutrophilic perivascular dermatitis, and marked orthokeratotic and parakeratotic hyperkeratosis are described histologically.
Porcine juvenile pustular psoriasiform dermatitis
This disease of weanling pigs was originally named pityriasis rosea. Because the clinical signs and gross lesions bear little relationship to those of the human disease for which it was originally named, the new designation, porcine juvenile pustular psoriasiform dermatitis, has been suggested. The disease is of no significance, except esthetic. The cause is not known. A hereditary predisposition has been suggested but not proved, particularly in Landrace pigs. Lesions develop most often in weaned pigs 3-14 weeks of age. Entire litters or just a few piglets may be affected.
The disease begins with symmetrical, nonpruritic, scaly, erythematous papules on the skin of the abdomen and inner thighs. The papules expand centrifugally to produce, at first, scaly plaques and later, when the central areas return to normal, ring-shaped, erythematous lesions (Fig. 6-130 ). As the rings expand, they coalesce to produce mosaic patterns and may extend to the sides and perineum. The acute histologic lesion is superficial and comprises deep perivascular dermatitis with eosinophils, neutrophils, and mononuclear cells. There may be epidermal spongiosis with intraepidermal eosinophilic and neutrophilic pustules. Superficial epidermal necrosis may extend into the ostia of the hair follicles. As the lesions heal, marked psoriasiform hyperplasia and parakeratotic scale-crusts predominate. The condition spontaneously resolves within about 4 weeks.
Figure 6-130.
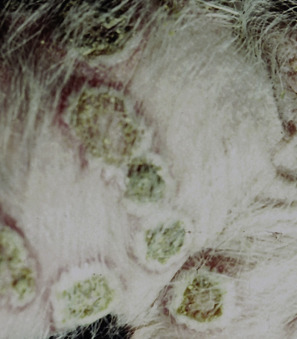
Porcine juvenile pustular psoriasiform dermatitis. Multifocal to coalescing crusted annular lesions with central depressions.
(Courtesy D.W. Scott.)
Miscellaneous porcine dermatoses
Idiopathic hyperkeratosis is commonly described in intensively housed sows and boars. Brown, waxy material accumulates on the dorsal neck and shoulders, dorsum, or flanks. The underlying skin is normal, and the condition is nonpruritic.
Porcine ulcerative dermatitis syndrome is uncommon and mostly described in adult sows. Annular to polycyclic chronic ulcers with thickened margins and crusts are present on the perineum, lateral thorax, abdomen and thighs, mammae, and convex surface of the pinnae. Lesions may resolve during lactation but recur with weaning. Variable features and patterns have been reported histologically. They include epidermal necrosis, hyperkeratosis, dermal perivascular eosinophils with fewer neutrophils and plasma cells, as well as cell-poor lymphoplasmacytic and histiocytic interface dermatitis and folliculitis with hydropic degeneration, apoptotic keratinocytes, and vesicle formation at the dermal-epidermal junction. The latter pattern suggests that this condition may be a form of vesicular cutaneous lupus erythematosus.
Recurrent dermatosis of sows is a rare idiopathic condition characterized by nonpruritic, erythematous macules and patches that enlarge and become scaly, especially on the trunk and only in white skin. Hairs within the lesion become discolored brown. Lesions tend to occur while farrowing and resolve when out of the farrowing house.
Further reading
Dunstan RW, Rosser EJ. Does a condition like human pityriasis rosea occur in pigs? Am J Dermatopathol 1986;8:86-89.
Kimura T, Doi K. Clinical and histopathological findings in pustular psoriasiform dermatitis (pityriasis rosea) in pigs. J Vet Med Sci 2004;66:1147-1150.
Lopez A, et al. Porcine ulcerative dermatitis syndrome in sows: a form of vesicular cutaneous lupus erythematosus? Vet Rec 2009;165:501-506.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Straw BE, et al. eds Skin. In: Straw BE, et al., editors. Diseases of Swine. 8th ed. Ames, Iowa: Iowa State University Press; 1999. p. 955.
Spiculosis
Spiculosis is a dysplastic and dyskeratotic condition of the hair follicle that results in 1-2 mm diameter and 0.5-2.0 cm long brittle spicules (hair shafts) protruding from hair follicles. The condition has been reported in humans and intact male Kerry Blue Terriers. Clinically, the condition is characterized by multiple hard, brittle, follicular spicules on various areas of the body but are most common on the lateral hocks. Affected dogs may chew or lick at the spicules. Histologically, hair follicles have enlarged hair bulbs that may have 2 dermal papillae. Enlargement of the hair bulb results from collections of heavily pigmented matrix cells that keratinize prematurely to form hyperpigmented keratinized amorphous masses or columns of unpigmented keratin in place of normal hairs.
Further reading
McKeever PJ, et al. Spiculosis. J Am Anim Hosp Assoc 1992;28:257-261.
Sebaceous gland dysplasia
Abnormal sebaceous gland differentiation (sebaceous gland dysplasia) is a rare dermatosis in cats and dogs. The lesion develops at a young age, usually <1 year, as variable degrees of scaling, poor-quality haircoat, follicular casting, and hair loss. In kittens, it is characterized by hypotrichosis with scaling that is apparent as early as 4 weeks of age (eFig. 6-15). Lesions tend to start on the face and, whereas hair loss is the main clinical sign in kittens, scaling and follicular cast formation is the most common lesion in dogs. The cause is unknown; however, the juvenile onset suggests a genetic defect leading to abnormal sebaceous gland development.
eFigure 6-15.

Sebaceous gland dysplasia in a kitten. Generalized hypotrichosis and scaling.
(Courtesy K. Kuhl.)
Histologically, sebaceous glands are markedly reduced in size with irregular profiles and composed of haphazardly arranged basaloid epithelial cells and sebocytes. Scattered shrunken sebocytes with hypereosinophilic cytoplasm and pyknotic nuclei are often observed. Sebaceous glands lack the normal differentiation from reserve (basal) cells to mature sebocytes. The lobules have irregularly sized sebocytes intermixed with vacuolated immature basaloid cells (eFig. 6-16).
eFigure 6-16.
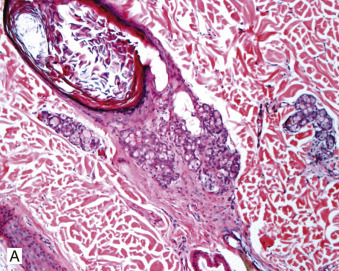
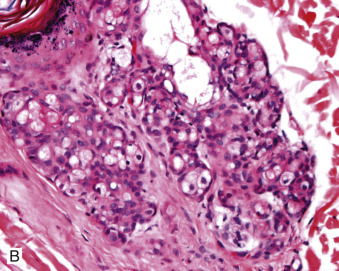
Sebaceous gland dysplasia. A, B. The sebaceous glands lack the normal differentiation from reserve (basal) cells to mature sebocytes. The lobules have irregularly sized sebocytes intermixed with vacuolated immature basaloid cells.
Further reading
Peters-Kennedy J, et al. Scaling dermatosis in three dogs associated with abnormal sebaceous gland differentiation. Vet Dermatol 2014;25:23-e8.
Yager JA, et al. Abnormal sebaceous gland differentiation in 10 kittens (“sebaceous gland dysplasia”) associated with generalized hypotrichosis and scaling. Vet Dermatol 2012;23:136-144.
Perforating dermatitis
Perforating dermatitis is a rare, distinctive reaction pattern in cats and humans. Clinically, there are multiple, conical, brown, firm horn-like papules and plaques. Lesions have been reported on the shoulder, neck, axilla, flank, hip, trunk, legs, and nose. The lesions may be arranged in a linear configuration. Histologically, this is a very distinctive lesion with a large conical crust containing a large number of degenerate inflammatory cells and numerous vertically oriented degenerate collagen fibers protruding into it (Fig. 6-131 ). The superficial to deep dermis contains moderate to marked infiltrates of eosinophils, mast cells, neutrophils, and fewer mononuclear cells. There may be subepidermal fibrosis. Pruritus is variable, ranging from absent to severe. The cause is unknown, although some cases may occur secondary to self-trauma from allergic skin disease. It has been proposed that this condition is the result of abnormal wound healing possibly caused by abnormal collagenesis. There is no age, sex, or breed predisposition. Masson trichrome staining of affected collagen fibers demonstrates segmental red cores; however, this finding is not specific for this condition.
Figure 6-131.
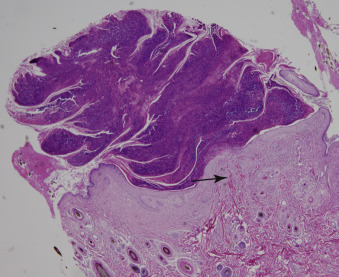
Perforating dermatitis in a cat. Vertically oriented collagen fibers (arrow) extending down from a conical shaped crust.
Further reading
Albanese F, et al. Feline perforating dermatitis resembling human reactive perforating collagenosis: clinicopathological findings and outcome in four cases. Vet Dermatol 2009;20:273-280.
Gross TL, et al. Degenerative, dysplastic, and depositional diseases of dermal connective tissue. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 373-403.
Olivry T. Is feline acquired reactive perforating collagenosis a wound healing defect? Treatment with topical betamethasone and halofuginone appears beneficial. Vet Dermatol 2010;21:434-436.
Sterile granulomas and pyogranulomas
Sterile granulomatous or pyogranulomatous dermatoses have been reported in dogs and less commonly in cats and horses.
Sterile pyogranuloma syndrome
The sterile granuloma/pyogranuloma syndrome (SPGS) is uncommon in dogs and rare in cats and horses. The cause is unknown; however, negative tissue cultures, negative special stains for microbial agents, absence of foreign material with polarization, and good response to immunomodulatory therapy have suggested an immune-mediated pathogenesis. It has been hypothesized by some that SPGS may be caused by an immune response against persistent endogenous or exogenous antigens, such as Leishmania spp. and/or Mycobacterium spp. These agents have been identified by PCR in some cases. Lesions are solitary or multiple, and localized or generalized firm, hair-covered to partially alopecic, erythematous papules, nodules, and plaques (Fig. 6-132A ). Lesions may become ulcerated and secondarily infected. Affected animals are otherwise healthy. Histologic findings include large perifollicular granulomas or pyogranulomas that are elongated and vertically oriented and that track hair follicles but do not invade them (Fig. 6-132B). Older lesions may become diffuse, obliterating adnexal structures and extending into the subcutis. Histiocytes, lymphocytes, and neutrophils predominate, with occasional plasma cells or multinucleated histiocytic giant cells. In horses and some cats, multinucleated histiocytic giant cells may be numerous. There are no age or sex predispositions.
Figure 6-132.

Sterile granuloma syndrome in a dog. A. Alopecic nodule under the lower eyelid.
(Courtesy Cornell University Hospital for Animals, Clinical Dermatology Service.)
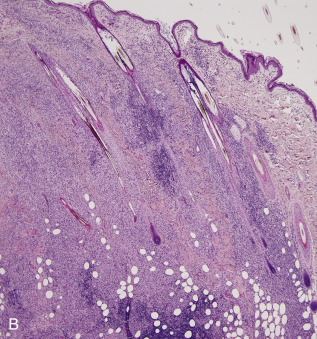
B. Note the vertically oriented perifollicular lymphohistiocytic infiltrates.
In dogs, Collies, Boxers, Great Danes, Weimaraners, English Bulldogs, Doberman Pinschers, Dachshunds, and Golden Retrievers appear to be predisposed. In most dogs, the lesions are multiple, nonpainful, nonpruritic, and can occur anywhere on the body; however, the face and distal extremities are the most common sites. Lymphadenopathy occurs in some cases, and rarely, there can be pyogranulomatous lymphadenitis. The condition may spontaneously resolve or wax and wane. In horses, as in dogs, lesions are generally asymptomatic. They are usually single on the lip, eyelid, or pastern, or multiple and scattered over the body.
In cats, lesions tend to be symmetrical and pruritic. Common sites are periauricular, pinna, and head, less commonly on the paws and trunk. Lesions are violaceus or orange-yellow and may become red to purple when palpated.
Cutaneous xanthoma
Xanthomas (xanthogranulomas) are single to multiple nodular lesions occurring rarely in the cat and very rarely in the dog and horse. Disorders of metabolism, such as hyperlipidemia in cats, diabetes mellitus, or high-fat diets, lead to the formation of xanthogranulomas in most cases; other cases, particularly solitary xanthomas, are idiopathic. In horses, xanthomas have been described in conjunction with equine pituitary pars intermedia dysfunction. Clinically, the lesions are yellow to white papules, plaques, or nodules with erythematous margins. They can be painful or pruritic. The head, distal extremities, paws, and bony prominences are typical sites. Histologically, there are nodular-to-diffuse infiltrates of foamy macrophages in the dermis, with variable numbers of multinucleated histiocytic giant cells and lipid lakes.
Sarcoidosis
Sarcoidosis in humans is a systemic granulomatous disease of undetermined etiology. The granulomas are characteristic, being composed predominantly of epithelioid macrophages with few lymphocytes (“naked” granulomas).
A sterile “sarcoidal” granulomatous dermatitis has been described in dogs and horses. Dogs develop multiple erythematous papules, nodules, and plaques that were neither pruritic nor painful. The lesions most commonly affected the neck, trunk, face, and pinnae. Nodular-to-diffuse sarcoidal granulomatous inflammation was present histologically. This condition is suspected to be part of SPGS.
Equine sarcoidosis (idiopathic generalized or systemic granulomatous disease) is rare and may be seen as a generalized or localized exfoliative dermatitis and/or as granulomatous inflammation in multiple organs. The cause is unknown; however, an immune-mediated pathogenesis, Mycobacterium spp., and hairy vetch toxicosis have been implicated. Sarcoidosis has been categorized into 3 clinical presentations: generalized, partially generalized, and localized. Peripheral lymphadenopathy may occur in the former two. The localized form is defined as localized areas of nonpruritic exfoliative dermatitis on 1 or 2 lower limbs with variable pain, edema, and lameness. The partially generalized form is characterized by exfoliative dermatitis on 1 or 2 limb(s) and/or (sub)cutaneous nodular lesions on a limited body region. The generalized form shows nonpruritic cutaneous signs and or (sub)cutaneous nodules all over the body with one or more of the following signs: low-grade fever, exercise intolerance, pain when touched, respiratory distress, weight loss, and/or peripheral lymphadenopathy. The onset may be insidious or rapid. There are no age, breed, or sex predilections, although most horses are >3 years of age. The skin lesions are characterized by well-demarcated, focal, multifocal, or generalized scaling and crusting, with various degrees of alopecia and increased local skin temperature. Lesions are most common on the lower limbs. Internal nodules may be found in the lung, lymph nodes, liver, gastrointestinal tract, spleen, kidneys, bones, and central nervous system. In some generalized cases, skin lesions may not be present. Histopathology shows multifocal nodular-to-diffuse, lymphogranulomatous dermatitis with multinucleated histiocytic giant cells. Vasculitis may be present, particularly in the localized form. The prognosis is poor for the generalized and partially generalized forms, with most horses being euthanized within months of diagnosis. Prognosis for survival is good for the localized form but guarded for the localized skin disease. Spontaneous resolution has been reported in the generalized and localized form.
Further reading
Cornegliani L, et al. PCR technique detection of Leishmania spp. but not Mycobacterium spp. in canine cutaneous “sterile” pyogranuloma/granuloma syndrome. Vet Dermatol 2005;16:233-238.
Oliveira-Filho JP, et al. Mycobacterium DNA detection in liver and skin of a horse with generalized sarcoidosis. J Vet Diagn Invest 2012;24:596-600.
Panich R, et al. Canine cutaneous sterile pyogranuloma/granuloma syndrome: a retrospective analysis of 29 cases (1976 to 1988). J Am Anim Hosp Assoc 1991;27:519-528.
Santoro D, et al. Cutaneous sterile granuloma/pyogranulomas, leishmaniasis and mycobacterial infections. J Small Anim Pract 2008;49:552-561.
Santoro D, et al. Cutaneous sterile pyogranuloma/granuloma syndrome in a dog. Can Vet J 2008;49:1204-1207.
Scott DW, et al. Idiopathic sterile granulomatous and pyogranulomatous dermatitis in cats. Vet Dermatol 1991;1:129-137.
Scott DW, Noxon JO. Sterile sarcoidal granulomatous skin disease in three dogs. Canine Pract 1990;15:11-18.
Sloet van Oldruitenborgh-Oosterbaan MM, Grinwis GCM. Equine sarcoidosis. Vet Clin North Am Equine Pract 2013;29:615-627.
Sloet van Oldruitenborgh-Oosterbaan MM, Grinwis GCM. Equine sarcoidosis: clinical signs, diagnosis, treatment and outcome of 22 cases. Vet Dermatol 2013;24:218-e48.
Sterile nodular panniculitis
Panniculitis refers to inflammation of the subcutaneous adipose tissue. Panniculitis has many causes, most of which have been discussed in previous sections (bacteria, fungi, immune-mediated disease, trauma, injection of irritant substances, foreign bodies, nutritional disorders, adverse reactions to vaccines or other injections, pancreatic disease). The syndrome of sterile nodular panniculitis (SNP) currently is considered to be idiopathic and either primary in origin or associated with a variety of other illnesses, including pancreatic nodular hyperplasia, pancreatic neoplasia, pancreatitis, or immune-mediated disease, such as rheumatoid arthritis and systemic lupus erythematosus. Concurrent inflammation of the fat in the abdomen, epidural space, and bone (steatitis) can occur in dogs with SNP.
It is a rare condition affecting dogs, cats, horses, and cattle.
The gross lesions are single to multiple, firm or soft, well-delineated or ill-defined, subcutaneous papules to nodules that may become cystic, ulcerate, or develop draining tracts. The exudate may be oily, serosanguineous, or hemorrhagic. Lesions may be grouped or distributed widely (Fig. 6-133 ). Affected animals with single lesions may be asymptomatic; animals with multiple lesions often have pyrexia, lethargy, and anorexia. Pain is variable. A normochromic, normocytic nonregenerative anemia is seen in chronically affected animals with multiple extensive lesions. Some cases spontaneously regress. Most lesions in dogs and cats respond to immunosuppressive doses of glucocorticoids. The condition can be recurrent. There is a tendency for the canine lesions to affect the trunk, and Dachshunds and Poodles are over-represented. Lesions in the horse are most often found on the neck, thorax, abdomen, and proximal limbs, and may elicit pain upon palpation. Shetland ponies may be predisposed. In cats, most lesions are solitary and occur most commonly over the ventral abdomen and ventral thorax. Lesions in cattle have been described over the neck, trunk, and proximal limbs.
Figure 6-133.

Sterile nodular panniculitis in a dog. Note multiple grouped ulcerative draining lesions on the trunk.
(Courtesy M.S. Canfield.)
The microscopic lesion is a lobular to diffuse infiltrate in the subcutis and deep dermis composed predominantly of neutrophils and macrophages and lesser numbers of lymphocytes and plasma cells. Discrete granulomas and pyogranulomas may be present. Adipocytes may appear necrotic or infiltrated with foamy macrophages. Lipid released from damaged lipocytes hydrolyzes to glycerol and fatty acids. Fatty acids incite further inflammation that perpetuates the lesions. Sterile panniculitis may be indistinguishable histologically from the panniculitides of infectious cause, and thus tissue culture and special stains for microbial agents are necessary for a definitive diagnosis.
The presence of saponification of fat and fat necrosis, along with diffuse infiltrates of pyogranulomatous inflammation, is associated with pancreatic disease and vitamin E deficiency in cats. The latter is also associated with ceroid deposits. Septal panniculitis is often associated with vasculitis. Sterile panniculitis resulting from trauma often occurs as a single lesion of lobular fat necrosis surrounded by fibrosis. Panniculitis resulting from repositol injection is usually characterized by fat necrosis and large numbers of degenerate neutrophils. Postinjection panniculitis also occurs with focal necrosis in the subcutis, but this area is surrounded by predominantly foamy macrophages and multinucleated histiocytic giant cells. Rabies vaccine–induced panniculitis is discussed under Immune-mediated dermatoses.
Further reading
Bassage LH, et al. Sterile nodular panniculitis associated with lameness in a horse. J Am Vet Med Assoc 1996;209:1242-1244.
Dagleish MP, et al. Serum alpha-1-proteinase inhibitor concentration in 2 Quarter Horse foals with idiopathic pyogranulomatous panniculitis. Equine Vet J 2000;32:449-452.
German AJ, et al. Sterile nodular panniculitis and pansteatitis in three weimaraners. J Small Anim Pract 2003;44:449-455.
Gross TL, et al. Diseases of the panniculus. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 538-558.
Hughes D, et al. Serum alpha1-antitrypsin concentration in dogs with panniculitis. J Am Vet Med Assoc 1996;209:1582-1584.
Mason KV. Disseminated necrotizing panniculitis associated with pancreatic carcinoma in a dog. Proc Am Acad Vet Dermatol 1989;61.
Menzies-Gow NJ, et al. Chronic nodular panniculitis in a three-year-old mare. Vet Rec 2002;151:416-419.
O'Kell AL, et al. Canine sterile nodular panniculitis: a retrospective study of 14 cases. J Vet Intern Med 2010;24:278-284.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Waitt LH, et al. Panniculitis in a horse with peripancreatic and pancreatic fibrosis. J Vet Diagn Invest 2006;18:405-408.
Symmetrical lupoid onychitis
Symmetrical lupoid onychitis or onychodystrophy (SLO) is a disease of young to middle-aged dogs characterized by onychalgia, onycholysis, and onychomadesis of multiple claws on multiple paws. The cause is unknown, but studies showing that dog leukocyte antigen class II is significantly associated with SLO support an immune-mediated pathogenesis. A genetic predisposition has been established in certain breeds. The condition occurs in many breeds, but German Shepherds, Rottweilers, and Gordon Setters are predisposed. The condition is painful and often leads to lameness. Amputation of the third phalanx of affected digits to include clawbed epithelium is often needed to establish the diagnosis. Histologic lesions are most pronounced on the dorsal aspect of the claw. The most common changes are a lichenoid interface onychitis with lymphocytic exocytosis and spongiosis and multifocal hydropic degeneration of the basal epidermis. Pigmentary incontinence may be severe, and there may be dermal hemorrhage or fibrosis and mucinosis of the deep dermis. Claws regrow but are misshapen, dry, soft or brittle, and discolored. Secondary bacterial infection may occur. The pathogenesis of SLO is not known and, in fact, the possibility that SLO is not a specific disease entity but merely an inflammatory reaction typical for the clawbed is possible. Similar clinical and histopathologic changes have been described in cases of leishmaniasis, systemic lupus erythematosus, food allergy, drug reaction, and idiopathic and antibiotic-responsive disease.
Further reading
Miller WH, et al. Diseases of eyelids, claws, anal sacs and ears. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 724-773.
Ovrebo Bohnhorst J, et al. Antinuclear antibodies (ANA) in Gordon setters with symmetrical lupoid onychodystrophy and black hair follicular dysplasia. Acta Vet Scand 2001;42:323-329.
Scott DW, et al. Symmetrical lupoid onychodystrophy in dogs: a retrospective analysis of 18 cases (1989-1993). J Am Anim Hosp Assoc 1995;31:194-201.
Wilbe M, et al. DLA class II alleles are associated with risk for canine symmetrical lupoid onychodystrophy (SLO). PLoS ONE 2010;5:1-6.
Laminitis
The hoof wall is a complex structure composed of an epidermis and dermis that attaches to the underlying distal phalanx. The distal phalanx is held in place by interdigitation of the epidermal lamina of the inner hoof wall and the dermal lamina of the corium that is attached to the third phalanx. When these laminae fail, the forces of body weight, motion, and tendons lead to sinking and rotation of P3, shearing of vessels that supply these tissues, and damage to the corium of the sole and coronet. The separation of the distal phalanx (coffin bone, P3) from the inner hoof wall is responsible for the severe clinical signs in laminitis, rather than a primary inflammatory process. Laminitis occurs in all hoofed species, but particularly affects horses and cattle. Laminitis is one of the most devastating of equine diseases, often leading to chronic debilitation or euthanasia.
Traditionally, it has been thought that laminitis is caused by one common pathophysiologic pathway. Currently, it is thought that there are 3 phases and 3 distinct forms of laminitis. The 3 phases are developmental, acute, and chronic. Laminitis is a cutaneous manifestation of a systemic problem, and thus there are many risk factors and potential causes that can be categorized into 3 forms.
-
•
The first form is inflammatory laminitis, which includes starch/grain overload; black walnut–induced laminitis, sepsis, and systemic inflammation caused by gastrointestinal disease; pneumonia; and septic metritis. Following release of inflammatory toxins, there is degradation of the lamellar basement membrane and dyshesion of the epithelial cells from the basement membrane. There is matrix metalloproteinase activation and leukocyte infiltration as well as profound hemodynamic changes.
-
•
Endocrinopathic laminitis/laminopathy is the second form and includes horses with insulin resistance, obesity, pituitary pars intermedia dysfunction, and possibly corticosteroid-induced laminitis. This form is characterized by little if any inflammation and stretching of the secondary epidermal lamellae as opposed to early separation from the basement membrane. This will still lead to eventual basement membrane separation at the tips of the secondary epidermal lamellae.
-
•
The third form, contralateral limb laminitis/laminopathy, is thought to be initiated by poor blood flow and ischemia and likely involves subsequent enzyme activation and degradation of the lamellar basement membrane in conjunction with the effects of tension and stretch on the lamellar tissues.
These different forms of laminitis are not entirely exclusive. Laminitis is a syndrome with many contributing factors, and although there may be different pathways, the common lesion in all forms of the disease is dermal-epidermal separation at the interface of the lamellar basal epithelial cells and the underlying basement membrane and dermis.
The earliest changes evident in the laminar tissue anatomy during acute laminitis are elongation and disorganization of basal and parabasal keratinocytes and attenuation of the tips of the secondary epidermal laminae. The basement membrane of the secondary laminae detaches first in the region of parabasal cell attachment and subsequently in the region of the basal cells, leaving aggregates of degenerating basement membrane components within the connective tissue space between the laminae. Loss of the basement membrane leads to separation of the dermal and epidermal laminae of the hoof wall and is crucial in loss of structural integrity of the P3/hoof wall attachment. Collapse of secondary laminae leads to loss of capillaries normally present within the connective tissue between the epidermal laminae. The loss of capillaries leads to increased resistance to blood flow, arteriovenous shunting, and eventual ischemic damage. This early stage is characterized clinically by a bounding digital pulse.
Acute laminitis is seen as sudden lameness and severe pain affecting most commonly the forefeet but may affect all feet, or just the hind feet. An increase in the hoof wall temperature and a bounding digital pulse indicate marked vascular engorgement in the hoof tissues. In horses, pain is often severe enough to provoke systemic disturbances. A section through an acutely affected hoof reveals little gross alteration beyond congestion of the laminar dermis and occasionally hemorrhage. There is no hoof deformity, although the skin above the coronary band may be swollen. Horses with diffuse swelling and depression along the coronary band are often found to have acute separation and displacement of P3 and are referred to as “sinkers,” a manifestation of acute laminitis. Microscopic changes are as described above. In addition, the dermis may be congested, edematous, and have mild hemorrhage and mild infiltrates of mononuclear cells. In time, coagulative necrosis of the secondary laminae may be evident.
Chronic laminitis (founder) refers to the stage of laminitis associated with radiographic or physical evidence of rotational or vertical displacement of the third phalanx relative to the hoof wall. The rotation has been attributed to loss of the interlocking force normally supplied by the epidermal laminae. In chronic cases, the ventral deviation is caused also by irregular hyperplasia of epidermal laminae placing a wedge of epidermis between the phalanx and the immovable hoof wall. The weight of the animal, the leverage forces placed on the toe, and the pulling forces of the deep digital flexor tendon contribute mechanically to the rotation. In severely affected animals, the third phalanx may penetrate the sole, which becomes convex. A mid-sagittal section through the hoof wall at this point will show obvious separation of P3 from the dorsal hoof wall, sinking, and various degrees of rotation of P3. The corium at the coronary band and sole may be edematous or hemorrhagic. In long-standing cases, the space between the dorsal hoof wall and P3 is filled with firm white tissue (proliferative epidermis). The toe usually turns up, and the cranial aspect of the hoof becomes concave and wrinkled by encircling horizontal ridges.
Laminitis occurs sporadically in dairy cows, heifers, fattening cattle, and young bulls. In cattle, carbohydrate overload is also an important predisposing cause of laminitis. Others include metritis, mastitis, and ketosis. A heritable form has been reported in Jersey cattle in South Africa, the United States, and the United Kingdom. Laminitis, not related to traumatic and metabolic episodes, occurs in all species but is important only in ungulates. Erysipelas in lambs; the various causative types of footrot in pigs, sheep, and cattle; and bluetongue in sheep are examples of diseases in which degenerative and inflammatory changes occur in the laminae of the hoof.
The chief microscopic lesion in chronic equine laminitis is marked irregular hyperplasia of the epidermal laminae. The regenerating secondary laminae may not regain their orderly arrangement and instead form irregular and anastomosing epidermal cords. The epidermal laminae, both primary and secondary, become markedly hyperkeratotic. The reason for the hyperkeratosis is not known. Both physical and physiologic influences on keratogenesis are likely altered in chronic laminitis. There is also osteoclastic resorption, boney remodeling, and medullary fibromyxoid proliferation in P3. Similar epidermal lesions occur in chronic bovine laminitis, although parakeratotic hyperkeratosis develops in addition to the orthokeratotic hyperkeratosis. Alterations in the dermal vasculature are most prominent in cattle. Moderate to marked arteriolosclerosis occurs in chronic bovine laminitis, especially in the solar dermis. Other changes in laminitis in cattle include chronic dermal granulation tissue, organized and recanalized vascular thrombi, perineural fibrosis, and perivascular accumulations of macrophages, often containing hemosiderin.
Further reading
Bailey SR, et al. Current research and theories on the pathogenesis of acute laminitis in the horse. Vet J 2004;167:129-142.
Eades SC. Overview of current laminitis research. Vet Clin Equine 2010;26:51-63.
Engiles JB. Pathology of the distal phalynx in equine laminitis: more than just skin deep. Vet Clin North Am Equine Pract 2010;26:155-165.
Katz LM, Bailey SR. A review of recent advances and current hypotheses on the pathogenesis of acute laminitis. Equine Vet J 2012;44:752-761.
Mungall BA, et al. In vitro evidence for a bacterial pathogenesis of equine laminitis. Vet Microbiol 2001;79:209-223.
Neoplastic and Reactive Diseases of the Skin
Epithelial tumors of the skin
Epithelial tumors of the skin are classified according to the predominant pattern of differentiation and the biological behavior. Most of the following tumors are named according to the World Health Organization International Histological Classification of Tumors of Domestic Animals, second series (1998), and Skin Disease of the Dog and Cat: Clinical and Histopathological Diagnosis, 2nd ed. (2005). The decision to classify a given tumor as one or another of the epidermal or adnexal tumors is often quite arbitrary. A neoplasm of the multipotential germinal cells of the epidermis may differentiate into a number of types of epithelial cells characteristic of mature cells of the various components of the epidermis or adnexa. Sometimes the differentiation results in a distinctive group of tumor cells, making precise identification unequivocal. At other times, the tumor cells may differentiate toward several skin structures forming squamous cells, sebaceous cells, or components of the hair follicle. The tumor can then be named according to the most aggressive or dominant cell type within the tumor. Other than squamous cell carcinomas, the majority of tumors derived from the epidermis or adnexa exhibit benign behavior.
-
•
Tumors of the epidermis include squamous papilloma, squamous cell carcinoma, and basal cell tumors.
-
•
Adnexal tumors of follicular origin include infundibular keratinizing acanthoma (intracutaneous cornifying epithelioma, keratoacanthoma), tricholemmoma, trichofolliculoma, trichoblastoma, trichoepithelioma, and pilomatricoma.
-
•
Adnexal tumors arising from glandular structures include sebaceous gland tumors, epitrichial (apocrine) gland tumors, and atrichial (eccrine) gland tumors.
Also included in this section are varieties of tumor-like or keratin-filled cystic lesions that can be confused with true neoplasms. Mention will be made also of tumors that metastasize to the skin.
Cysts, hamartomas, and tumor-like lesions
Cysts
A cyst is a non-neoplastic, simple sac-like structure with an epithelial lining. Classification of cysts depends on identification of the lining epithelium or structure from which the cyst arose. Follicular cysts are classified according to the level of the hair follicle from which they develop. Infundibular, isthmus, matrical, and hybrid are named based on their epithelial lining and type of keratinization. Epithelial and follicular cysts occur in multiple species of animals, including cats, horses, cattle, sheep, alpacas, and camels. They are most common in dogs. In long-standing lesions, the epithelial wall may become very thin, and rupture may release entrapped keratin to stimulate pyogranulomatous dermal inflammation.
Infundibular cysts (epidermoid cyst, epidermal cyst, epidermal inclusion cyst) arise from the infundibular portion of the hair follicle, are lined by squamous epithelium with an obvious granular layer, and filled with laminated concentrically arranged keratin. They may be single or multiple, smooth, most often unilocular, spherical dermal papules or nodules seldom larger than 1 cm in diameter. The keratin may appear as loose flakes. Infundibular cysts may arise from dilation of the infundibulum of occluded hair follicles, and indeed, occasionally one can detect superficial dermal scarring that may support this hypothesis. As well, such cysts may contain fragments of mature hair shafts. One report in the dog documents multiple squamous cell carcinomas arising from multiple infundibular cysts. Some cysts are thought to arise from traumatic, developmental, or surgical implantation of epidermal fragments into dermis or subcutis. Penetrating grass seeds cause implantation of epidermal fragments in sheep. One dog was reported to have >100 infundibular cysts in the perianal area, possibly resulting from chronic external trauma to the perianal area as a response to anal sacculitis. Occasionally, an infundibular cyst can be found within the bone of the third phalanx of the dog (subungual epidermal inclusion cyst).
Isthmus cyst (trichilemmal cyst) is lined by keratinizing epithelium that lacks a granular layer. The inner layers of the epidermis lining the cyst have large amounts of pale eosinophilic cytoplasm and inconspicuous intercellular bridges resembling the outer root sheath of the middle segment of an anagen follicle and the mid to lower portion of a catagen follicle. There is trichilemmal cornification and the cyst contents are paler and more homogeneous than in the infundibular cyst.
Matrical cyst (pilar cyst) is derived from the inferior segment of the anagen hair follicles and is lined by small basaloid epithelial cells with scant cytoplasm and hyperchromatic nuclei. The epithelium keratinizes abruptly forming “ghost” cells.
Hybrid cyst (trichoepitheliomatous cyst, panfollicular cyst) is lined by 2 or all 3 types of follicular epithelium. The presence of 2 or 3 types of keratin may help support this diagnosis (Fig. 6-134 ).
Figure 6-134.
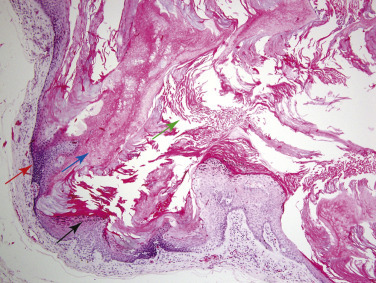
Hybrid follicular cyst in a dog. The cyst wall is lined by stratified squamous epithelium with a prominent granular cell layer (black arrow) and lamellar flaky keratin (green arrow) resembling an infundibular cyst. The cyst wall is also lined by small basaloid epithelium (red arrow) resembling a matrical cyst with abrupt keratinization into ghost cells (blue arrow).
Dilated pore of Winer is a flask-shaped epidermal cyst on the head or neck of middle-aged or old cats and rarely dogs and horses. It is connected to the skin surface by a pore. It is a variant of the infundibular cyst. The stratified keratinizing epithelium of the cyst wall near its base is hyperplastic with very regular rete ridges in parallel columns (Fig. 6-135 ). Keratin may protrude through the pore, forming a cutaneous horn.
Figure 6-135.
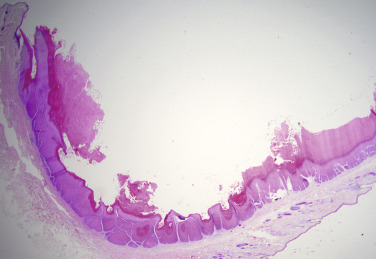
Dilated pore of Winer in a cat. Cystically dilated follicular infundibulum communicates with the skin surface, produces trichilemmal cornification and is lined by thickened squamous epithelium with psoriasiform hyperplasia.
Keratoma (horn cyst, horn tumor, keratin cyst) is a keratin-filled cyst that develops between the hoof wall and the distal phalanx. They are thought to originate from the epidermal horn-producing cells of either the coronary or solar corium. They are rare but do occur in both simple- and cloven-hoofed animals. Most are reported in horses. The cysts are usually solitary, 1-5 cm in diameter, and often exert pressure on P3, leaving an area of bone resorption that can be seen radiographically. There are rare reports of horses with multiple keratomas. Keratomas are painful, causing lameness and bulging of the affected area of the hoof wall. Histologically, the cyst is lined by squamous epithelium of the primary epidermal lamellae and filled with laminated keratin that in some cases may mineralize. Trauma to the hoof wall and infection have been suggested, although not proven, causes of keratomas.
Dermoid cysts (dermoid sinus) are congenital lesions found in young animals, often along the dorsal midline. They arise by developmental failure of epidermal closure along embryonic fissures that maroons an island of multipotential ectoderm within the dermis or subcutis. Some dermoid cysts may extend deep into the tissue and be connected to the dura mater of the spinal cord. Some, such as those occurring in Rhodesian Ridgeback dogs, actually retain a sinus pore to the skin surface (see Congenital and hereditary diseases of skin). Dermoid cysts are common in some families of Boxer dogs, and affected animals have multiple cysts along the midline of the skin over the forehead. In the horse, dermoid cysts occur most often on the midline between the withers and the rump. Dermoid cysts contain keratin and hair fragments and sometimes sebaceous secretions. The dermis abutting the cyst wall has numerous hair follicles, sebaceous glands, and occasionally epitrichial sweat glands. Hair follicles are attached to and radiate from the cyst wall. Specimens with only hair follicle differentiation may be confused with unilocular trichoepitheliomas, but the dermoid cyst has gradual keratinization rather than abrupt trichilemmal cornification.
Epitrichial (apocrine) cysts may be single or multiple and are filled with clear secretions and lined by a single layer of cuboidal to columnar epithelial cells. Multiple cysts at multiple sites are referred to as epitrichial (apocrine) cystomatosis. This is an uncommon lesion that occurs in middle-aged to older dogs for unknown reasons.
Sebaceous duct cysts are extremely rare. They are usually solitary and may occur in Meibomian glands. They are lined by a thin layer of stratified squamous epithelium that has a sparse granular cell layer. Atrophic sebaceous gland lobules surround the cyst.
Hamartomas
Hamartomas are benign tumor-like nodules composed of disorganized and excessive amounts, or enlarged components, of mature tissue elements indigenous to the site in which they arise. Nevus refers to any congenital malformation of the skin. Thus the term hamartoma is more inclusive than nevus and is the preferred nomenclature for most lesions that are regarded as malformations, either congenital or acquired.
-
•
Epidermal hamartomas (pigmented epidermal nevus, linear epidermal hamartoma, verrucous epidermal nevus) grossly appear as focal hyperkeratotic plaques or papules forming one or more linear arrays on the trunk or legs. Some lesions are hyperpigmented. Histologically, there is abrupt irregular epidermal papillary hyperplasia with marked laminated hyperkeratosis. The stratum granulosum may have enlarged keratohyaline granules. In the dog, an association with papilloma virus infection has been documented in some cases. Linear epidermal hamartomas are thought to be a genetically inherited lesion in Belgian horses. Lesions develop at <1 year of age and are seen as bilateral linear vertically oriented bands of hyperkeratosis and alopecia on the caudal aspect of the rear cannon bones.
-
•
Follicular hamartomas have been reported in the dog and consist of one or more clusters of very large anagen hair follicles that extend more deeply than adjacent normal follicles. Associated glands surround the follicles and sebaceous glands may be enlarged. There is normal orientation of follicles and adnexal glands. Clinically, there are single to multiple grouped plaques or small nodules ranging from 0.3 to several centimeters in diameter, and the skin is irregularly thickened. In some cases, locally extensive areas are affected.
-
•
Fibroadnexal hamartoma (adnexal nevus, focal adnexal dysplasia, folliculosebaceous hamartoma) is a common lesion in dogs and consists of aggregates of markedly distorted and variably inflamed folliculosebaceous units surrounded by dense collagen and lacking a connection to the skin surface. Hair bulbs are not present. These lesions are typically solitary, raised, well circumscribed, and 1-4 cm in diameter. They are most common on the distal limbs, pressure points, and interdigital areas. Some pathologists believe this type of lesion is a result of trauma and is not a true hamartoma.
-
•
Sebaceous hamartoma is an uncommon variant of fibroadnexal hamartoma and thus is clinically similar. Histologically, it is composed predominantly of large sebaceous lobules with random distribution. Hair follicles are small and malformed.
-
•
Sweat gland hamartomas are rare in domestic animals but have been described in cats and dogs. Histologically, there are proliferating sweat glands in the superficial dermis. The ductal and secretory epithelia are cytokeratin 8 positive.
-
•
Trichofolliculoma is also thought to be a hamartoma. It is uncommon in dogs and rare in cats. It is a well-circumscribed, nonencapsulated dermal mass composed of one or more large dilated primary follicles that open to the surface, forming a pore seen clinically. Secondary follicles radiate out from the primary follicles, and associated adnexal glands are present. Tumors with large sebaceous glands are called sebaceous trichofolliculomas.
Tumor-like lesions
Idiopathic squamous papillomas (warts) are 1-5 mm papillary masses composed of hyperplastic stratified squamous epithelium supported by dermal projections. The maturation of the epidermis is orderly and does not show viral-induced cytopathic effects as seen in viral papillomas. These lesions are most often seen on the eyelids, face, conjunctiva, or pawpads of older dogs and occasionally cats, and they may be traumatic in origin. One report describes 11 dogs with idiopathic squamous papillomas of the penile mucosa. Congenital papillomas, which may actually represent epidermal hamartomas, have been reported in newborn foals and fetuses. Two cases of nonviral congenital fibropapilloma have been reported in piglets.
Cutaneous horns are rare exophytic cylindrical formations of compact keratin a few millimeters in diameter and 1-2 cm in length, formed by an underlying markedly hyperplastic epithelium. Orthokeratotic hyperkeratosis predominates. Cutaneous horns may arise from viral papillomas, actinic keratosis, squamous cell carcinoma (bowenoid in situ or invasive), infundibular keratinizing acanthomas, or dilated pores of Winer. Cutaneous horns of the pawpad of cats have been associated with feline leukemia virus infection.
Warty dyskeratoma is a rare a cystic cup-shaped dermal mass lined by stratified squamous epithelium resembling the follicular infundibulum. The base of the structure has many filiform projections. There is extensive acantholysis, individual dyskeratosis, and apoptosis of keratinocytes. The lumen is filled with orthokeratotic and parakeratotic debris.
Further reading
Callan MB, et al. Multiple papillomavirus-associated epidermal hamartomas and squamous cell carcinomas in situ in a dog following chronic treatment with prednisone and cyclosporine. Vet Dermatol 2005;16:338-345.
Cornegliani L, et al. Idiopathic mucosal penile squamous papillomas in dogs. Vet Dermatol 2007;18:439-443.
Fadok VA. Overview of equine papular and nodular dermatoses. Vet Clin North Am Equine Pract 1995;11:69-70.
Goldschmidt MH, et al. Histological Classification of Epithelial and Melanocytic Tumors of the Skin of Domestic Animals. Washington, DC: Armed Forces Institute of Pathology; 1998.
Gross TL, et al. Section 2: Neoplasms and Other Tumors. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005.
Nishiyama S, et al. Congenital cutaneous fibropapillomatosis with no evidence of papillomavirus infection in a piglet. J Vet Med Sci 2011;73:283-285.
Park J, et al. Multiple perianal infundibular follicular cysts in a dog. Vet Dermatol 2010;21:303-306.
Redding WR, O'Grady SE. Nonseptic diseases associated with the hoof complex: keratoma, white line disease, canker and neoplasia. Vet Clin North Am Equine Pract 2012;28:407-421.
Scott DW, Miller WH. Neoplasms, cysts, hamartomas, and keratoses. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 468-516.
Scott DW, Teixeira EAC. Multiple squamous cell carcinomas arising from multiple cutaneous follicular cysts in a dog. Vet Dermatol 1995;6:27-31.
Vilafranca M, et al. Generalized apocrine gland cystomatosis in an Old English sheepdog. Vet Dermatol 1994;3:83-87.
White KS, et al. Equine congenital papilloma: pathological findings and results of papillomavirus immunohistochemistry in five cases. Vet Dermatol 2004;15:240-244.
Tumors of the epidermis
Papillomas and papillomavirus-induced lesions
Cutaneous papillomas are benign proliferative epithelial neoplasms that have a complex etiology and pathogenesis. The differences in site preference, clinical course, and histology of such lesions have been made more understandable by the discovery that most papillomas are caused by infection with a host- and often site-specific papillomavirus of the family Papillomaviridae. Not all papillomas are caused by or contain viruses. The nonviral lesion is considered to be an idiopathic squamous papilloma and is described under Tumor-like lesions.
Many papillomaviruses (PVs) have been identified using in situ hybridization, PCR, and DNA sequencing, and they exist in most domestic and nondomestic mammals. Papillomaviruses are double-stranded DNA viruses that reproduce in keratinocyte nuclei. They gain access through defects in the epithelium and infect cells of the stratum basale. However, for viral replication to occur, infected cells must become terminally differentiated, and therefore PVs attempt to increase both proliferation of basal cells and terminal keratinocyte differentiation. PV types are grouped into genera. Most of the >100 human PVs (HPVs) are classified as alpha or beta PVs. Alpha-PV genus includes the oncogenic mucosal types. The beta-PV genus contains cutaneous PVs that are usually associated with immunosuppression. The delta-PV type is important in nonhuman mammals because it is associated with benign fibropapillomas in both ungulates and cats. Although most papillomaviruses are species specific, delta-PVs have the unique ability to infect multiple species.
Immunocompromised animals have increased susceptibility to papillomavirus infection. Papillomaviruses induce and/or are associated with several types of cutaneous lesions, including squamous papilloma, inverted papilloma, feline viral plaques, canine pigmented viral plaques, bowenoid in situ carcinoma (BISC), invasive squamous cell carcinoma (ISCC), and fibropapillomas, including equine and feline sarcoids.
Viral papillomas may regress as a result of cell-mediated immune attack, may persist, or may progress to squamous cell carcinomas. Although some viral and host factors are known to influence the behavior of viral-induced papillomas and fibropapillomas, many other factors are not yet defined.
The typical papilloma is a 1-2 cm wart-like, filiform, exophytic, and hyperkeratotic mass composed of hyperplastic epidermis supported by thin, inconspicuous dermal stalks with dilated capillaries (Fig. 6-136A ). Lesions can be anatomically extensive and multiple. The stratum corneum exhibits variable degrees of orthokeratotic to parakeratotic hyperkeratosis. Most of the hyperplasia is due to marked expansion of stratum spinosum cells, which have pale basophilic cytoplasm. Cells of the spinous and/or granular layer have swollen eosinophilic to lightly basophilic cytoplasm (ballooning degeneration) and enlarged, condensed, or multiple nuclei (koilocytes) (Fig. 6-136B). Degenerating keratinocytes may have condensed eosinophilic cytoplasmic inclusions that represent aggregates of keratin, a result of the viral cytopathic effect. These inclusions should not be confused with the cytoplasmic inclusions associated with poxvirus infections. The stratum granulosum has large, variably sized and shaped basophilic keratohyaline granules. Cells of the stratum spinosum and granulosum may have vesicular nuclei with intranuclear pale basophilic viral inclusions that contain virus particles visible with electron microscopy and viral antigen detectable by immunohistochemistry, but these may not be numerous.
Figure 6-136.

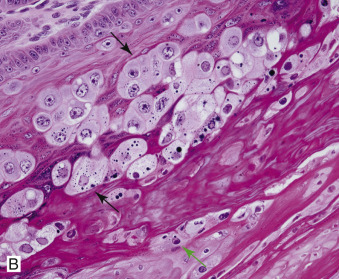
Papillomavirus in a cow. A. Marked papillated epidermal hyperplasia, hypergranulosis, and hyperkeratosis. B. Multiple koilocytes (black arrows) in the stratum granulosum and a few intranuclear inclusion bodies in the stratum corneum (green arrow).
Fibropapillomas appear as nodules or plaques covered by a variably hyperplastic and hyperkeratotic epidermis. Classic examples of fibropapillomas are bovine fibropapilloma, equine sarcoid, and feline sarcoid (feline fibropapilloma). Microscopic lesions typical of fibropapillomas include the features of acanthosis, hyperkeratosis, and downgrowth of rete ridges, but dermal proliferation predominates (Fig. 6-137A ). The proliferating cell is a large, plump fibroblast. The cells are arranged in haphazard whorls and fascicles rather than in perpendicular sheets, as in granulation tissue. In some, the epidermal proliferation is minimal and is seen only as slight acanthosis and accentuation of rete pegs, whereas, in others, the hyperplasia resembles full-fledged papillomas.
Figure 6-137.
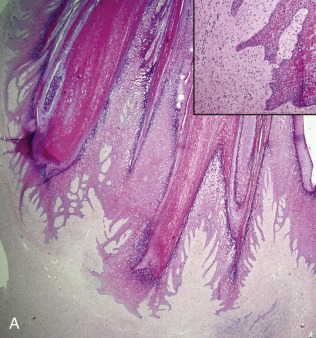

Fibropapilloma in a cow. A. Marked papillated epidermal hyperplasia, koilocytes with rete pegs, and dermal fibroblast proliferation (see inset). B. “Teat fronds” caused by infection with bovine papilloma virus-1 (BPV-1), BPV-2, and BPV-5.
(Courtesy J.M. Gourreau.)
Cattle.
Thirteen bovine papillomaviruses (BPVs) have been described (BPV 1-13) (Table 6-1 ). Bovine papillomatosis may be a herd problem in that the virus is easily transmitted by animal-to-animal contact and by fomites. Depending on the anatomic site and papillomavirus type, both morphologic and biological features of lesions may differ. BPV-1 causes typical fibropapillomas on the teats and penis. BPV-2 causes typical fibropapillomas on the head, neck, dewlap, shoulder, and occasionally the legs and teats. Both of these viruses tend to produce multiple lesions in animals <2 years of age, and the lesions often spontaneously regress within 1 year. BPV-3 causes “atypical warts” in cattle of all ages. The lesions are low, flat, circular, and nonpedunculated and have delicate to thick frond-like projections on their surfaces. These rarely spontaneously regress and can occur anywhere on the body, including the teats. “Teat frond” warts caused by BPV-5 (Fig. 6-137B) are small, white, elongated hyperkeratotic, and do not spontaneous regress. BPV-6 causes nonpedunculated, conical to branch-like, hyperkeratotic, frond-like papillomas on the teats in cattle of all ages. These lesions sometimes break off, leaving ulcers that commonly become secondarily infected with bacteria.
Table • 6-1.
Bovine papillomaviruses
| Virus | PV genus | Lesion |
|---|---|---|
| BPV-1 | Delta | Cutaneous, teat, rumen, and genital fibropapilloma; rumen papilloma; urinary bladder neoplasia; equine sarcoid |
| BPV-2 | Delta | Cutaneous, teat, rumen, and genital fibropapilloma; rumen papilloma; urinary bladder neoplasia; equine sarcoid |
| BPV-3 | Xi | Cutaneous papilloma |
| BPV-4 | Xi | Oral/esophageal/rumen papilloma, urinary bladder neoplasia |
| BPV-5 | Epsilon | Teat and rumen fibropapilloma, cutaneous and rumen papilloma |
| BPV-6 | Xi | Teat papilloma |
| BPV-7 | Dyoxi | Teat papilloma, healthy skin |
| BPV-8 | Epsilon | Cutaneous papilloma, fibropapilloma |
| BPV-9 | Xi | Teat papilloma |
| BPV-10 | Xi | Teat papilloma, tongue papilloma |
| BPV-11 | Xi | Cutaneous papilloma |
| BPV-12 | Xi | Tongue papilloma |
| BPV-13 | Delta | Ear papilloma, equine sarcoid |
BPV, bovine papillomavirus.
Some BPVs are associated with neoplastic transformation in the skin, alimentary tract, and urinary bladder. An angiokeratomatous papilloma has been described in association with PV in an 8-month-old Simmental calf. Many factors are involved, including viral proteins that promote cell dysregulation and immune evasion. BPVs are composed of early (E) and late (L) genes. E5, E6, and E7 are the transforming proteins. E5 is the major BPV transforming oncoprotein. It is believed to be critical in driving cell transformation, especially by activating platelet-derived growth factor receptor β (PDGFRβ). The binding of BPV-1 E5 to PDGFRβ results in activation of the phosphatidylinositol-3-kinase (PI3K)-AKT-cyclin D pathway, leading to cell cycle deregulation. BPV-1 can also down-regulate the expression of toll-like receptor 4 (TLR-4) through the E2 and E7 oncoproteins. TLR-4 downregulation is expected to contribute to immune evasion and viral persistence. In conjunction with several BPVs (BPV-1, BPV-2, and BPV-4), the ingestion of bracken fern (Pteridium aquilinum) has been associated with various epithelial and mesenchymal urinary bladder neoplasms. This plant is known to promote genomic instability, resistance to apoptosis, and cell cycle deregulation by inactivating p53 and activating ras and preventing the immune system from clearing viral papillomas.
Congenital papillomatosis was described in a Holstein heifer, and although BPV-3 was suspected, a viral etiology was not proved, and thus these lesions may be hamartomas.
Horses.
Currently, there are 3 distinct clinical syndromes in the horse caused by Equus caballus papillomaviruses (EcPV 1-7) (Table 6-2 ). Classic equine viral papillomatosis caused by Equus caballus papillomavirus-1 (EcPV-1) is a contagious disease and most commonly causes exophytic viral papillomas on the muzzle and lips of horses <3 years of age (Fig. 6-138 ). Lesions begin as 1-mm diameter raised, round, white to gray smooth papules and develop into broad-based to pedunculated gray to white plaques and nodules with a hyperkeratotic frond-like surface. Spontaneous remission occurs in ~2-3 months. Equine genital papillomas caused by EcPV-2 usually occur on older horses and are not known to spontaneously resolve. This virus has been associated with malignant transformation of penile and vulvar lesions to squamous cell carcinoma (SCC) in situ and invasive squamous cell carcinoma (ISCC). Equine ear papillomas (aural plaques) occur in horses of all ages, rarely spontaneously resolve, and are associated with EcPV 3-6. Early lesions are grossly similar to viral papillomatosis, with the exception of generally being confined to the pinnae. Fully developed lesions are usually bilaterally symmetrical and appear as 1-3 cm white hyperkeratotic plaques. Blackfly bites may be important in the transmission. Aural plaques are similar histologically to exophytic papillomas; however, the epidermis is less papillated, and hypomelanosis may be striking. EcPV-4 has also been isolated from vulvar and inguinal plaques, and EcPV-7 was isolated from an undiagnosed penile mass in a horse. Congenital papillomas have been reported in foals (see the section Hamartomas).
Table • 6-2.
Equine papillomaviruses
| Virus | PV genus | Lesion |
|---|---|---|
| EcPV1 | Zeta | Equine viral papillomatosis |
| EcPV2 | Dyoiota | Genital papilloma, in situ and invasive SCC |
| EcPV3 | Dyorho | Ear papilloma |
| EcPV4 | Dyoiota | Ear papilloma, vulvar and inguinal plaques |
| EcPV5 | Dyoiota | Ear papilloma |
| EcPV6 | Dyorho | Ear papilloma |
| EcPV7 | Dyorho | Undiagnosed penile mass |
EcPV, Equus cabalus papillomavirus; SCC, squamous cell carcinoma.
Figure 6-138.

Viral papillomatosis on the muzzle of a young horse.
(Courtesy D.W. Scott.)
The most important papillomavirus-induced lesion in the horse is the sarcoid, known to be associated with BPV-1, BPV-2, and most recently BPV-13. Sarcoids are locally aggressive, nonmetastatic fibroblastic skin tumors of horses, mules, donkeys, and zebras. They are the most common skin tumor of horses, accounting for up to 90% of tumors. A combination of factors appears to be involved in development of the tumors, including exposure to a viral agent, cutaneous trauma, and a genetic predilection. Viral etiology has been deduced based on reports of epizootics of cases, transmission studies, detection of viral particles in cultured tumor cells, and demonstration of DNA sequences very similar or identical to that of BPV-1 or BPV-2 genome in tumor cells of horses and donkeys. BPV DNA has been demonstrated in normal skin of healthy horses and horses with inflammatory conditions, suggesting that there are more factors involved in sarcoid development than simply viral infection. Sarcoids frequently develop in areas subjected to trauma or at sites of wounds 6-8 months after wound healing. In horses, there is a breed predilection for Appaloosas, Quarter Horses, Arabians, and Thoroughbreds and a lower incidence in Standardbreds and Lipizzaners. In Thoroughbreds and Warmbloods, the increased risk has been associated with major histocompatibility complex (MHC)-1 A3 and W13 alleles, whereas, in Standardbreds and Lipizzaners, a decreased risk is associated with decreased W13 allele and a lack of W13, respectively.
Sarcoids develop anywhere but are most common on the head, legs, and ventral trunk. They may be single or multiple. Young horses 1-7 years of age are at increased risk, with rare reports in older horses. The tumors are classified according to their gross appearance as occult, verrucous, nodular, fibroblastic, mixed, and malignant (malevolent). Many horses have multiple tumors, and all types of sarcoids can be present in the same horse. Occult sarcoids are focal areas with alopecia, scaling, hyperkeratosis, and hyperpigmentation (Fig. 6-139A ). Common locations are neck, face, sheath, medial thigh, and shoulder. The verrucous sarcoid is a small wart-like growth, usually measuring <6 cm in diameter, with a dry, rough surface and variable alopecia (Fig. 6-139B). This type is usually found in the head, neck, axilla, and groin. Nodular sarcoids are spherical dermal to subcutaneous masses. The overlying skin may be normal but can become alopecic and ulcerated. This type is common on the eyelid, groin, and prepuce. The fibroblastic sarcoid is more variable in appearance and may range from a well-circumscribed firm nodule with intact surface to large masses, >25 cm in diameter, with an ulcerated surface prone to hemorrhage and resembling exuberant granulation tissue. Common locations are axilla, groin, legs, and periocular. Malignant/malevolent sarcoids are aggressive and locally invasive. These tumors extend widely into the adjacent skin and subcutis and infiltrate lymphatic vessels. The occult and verrucous and, to a lesser extent, the nodular sarcoid can remain static for years if not traumatized. Any type of sarcoid lesion can develop into an aggressive fibroblastic or malignant/malevolent tumor if traumatized. Spontaneous remission is rare. The tumors are characterized by a high rate of recurrence, up to 50%, following surgical excision.
Figure 6-139.


Equine sarcoid. A. Occult (flat) sarcoid on the medial thigh. B. Multiple verrucous (black arrow) and nodular (green arrow) sarcoids on the groin of the same horse.
(Courtesy D.W. Scott.)
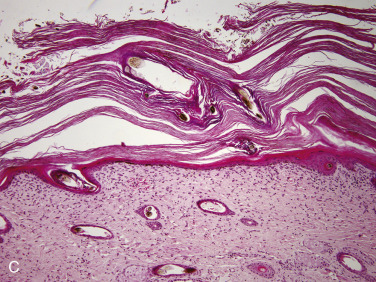
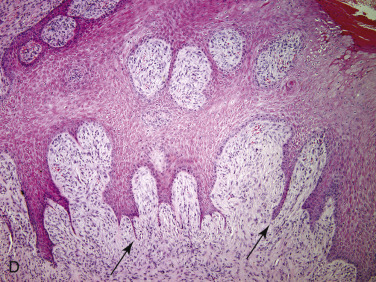
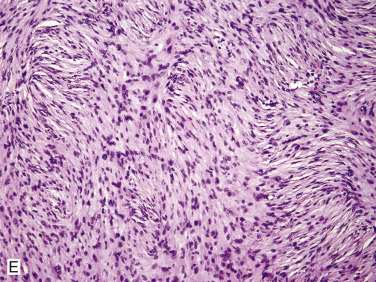
C. Note the subtle fibroblast proliferation in the superficial dermis, marked orthokeratotic hyperkeratosis, and lack of an epidermal response in this early occult sarcoid. D. Prominent fibroblast proliferation and multiple thin rete pegs (arrows). E. The neoplastic fibroblasts of this nodular sarcoid are arranged in whorls and interlacing bundles resembling a peripheral nerve sheath tumor.
Histopathology is necessary for definitive diagnosis of a sarcoid. Sarcoids are typically biphasic tumors composed of both epidermal and dermal components. The epidermal component may be minimal or absent in some tumors, especially nodular and early occult sarcoids (Fig. 6-139C). When the epidermis is intact, hyperkeratosis and irregular epidermal hyperplasia with thin rete pegs extending deep into the dermis are common features (Fig. 6-139D). The dermal component consists of fibroblasts and collagen in various proportions. The fibroblasts have plump nuclei, and nucleoli may be prominent. The mitotic index is usually low. Fibroblasts at the dermal-epidermal junction are frequently oriented perpendicular to the basement membrane in a “picket fence” pattern, which is a distinctive histologic feature seen in most sarcoids. The cells are arranged in whorls, interlacing bundles, or haphazard arrays of variable density (Fig. 6-139E). Tumor margins are typically indistinct, and adequacy of excision is frequently difficult to determine. When the tumor is ulcerated, it may not be possible to differentiate a sarcoid from granulation tissue, fibroma, well-differentiated fibrosarcoma, and peripheral nerve sheath tumor. Immunohistochemical staining for S-100 protein may be useful in confirming a peripheral nerve sheath tumor. Additional biopsies to include intact epidermis may be required to make a diagnosis. BPV infection of equine fibroblasts appears to be mainly nonproductive with respect to producing complete viruses, and therefore there is no histologic or immunohistochemical evidence of PV infection.
Sheep and goats.
Papillomas are uncommon in sheep and goats. Three papillomaviruses have been described in sheep. Ovis aries papillomavirus 1 and 2 (OaPV-1, OaPV-2) are delta-PVs and are associated with fibropapillomas. OaPV-3 (dyolambda-PV) has been associated with SCC. SCC is the most common skin neoplasm of sheep. Filiform squamous papillomas occur in young sheep, especially on the fetlock area of the lower legs. Lesions are 1-3 cm in diameter, raised, and frond-like. Similar lesions may occur on the scrotum of rams. Fibropapillomas occur on the face, pinnae, legs, and teats of adult sheep. Lesions are 0.5-1 cm, raised, hyperkeratotic, and pedunculated. Two clinical entities involving cutaneous papillomas have been described in goats. In one, papillomas occur on the face, pinnae, neck, shoulder, and forelegs, and spontaneous regression occurs in 1-12 months. In the second form, papillomas occur on the udder and teats of white goats especially; cutaneous horns may develop. There is no spontaneous regression, and malignant transformation to SCC can occur. In both forms, lesions are multiple, hyperkeratotic, and verrucous. PV DNA sequenes have only been detected in some goats with mammary lesions. Capra hircus papillomavirus 1, a phi-PV, has been isolated from healthy goat skin.
Dogs.
Cutaneous papillomas are common in the dog, and at least 5 different clinical syndromes are recognized. Fifteen Canis familiaris papillomaviruses (CfPVs) or Canine papillomaviruses (CPVs) have been described (Table 6-3 ). Canine oral papillomatosis has been associated with CPV-1 (Canine oral papillomavirus, COPV) and CPV-13. This is usually a self-limiting disease confined to the mucosa of the oral cavity or lips of young dogs (Fig. 6-140 ). It occasionally affects the conjunctiva and external nares. Lesions are commonly multiple and are characterized by white to gray pedunculated or cauliflower-like hyperkeratotic masses up to 3 cm in diameter. Oral papillomatosis is occasionally associated with immunosuppression. It has been described in Beagles with IgA deficiency, in dogs undergoing immunosuppressive therapy with cyclosporine, and in a Chinese Shar-Pei in association with glucocorticoid therapy.
Table • 6-3.
Canine papillomaviruses
| Virus | PV genus | Lesion |
|---|---|---|
| CPV-1 | Lambda | Oral/cutaneous papilloma, inverted papilloma, invasive SCC |
| CPV-2 | Tau | Cutaneous papilloma, inverted papilloma, invasive SCC |
| CPV-3 | Chi | Pigmented plaque, in situ SCC, invasive SCC |
| CPV-4 | Chi | Pigmented plaque |
| CPV-5 | Chi | Pigmented plaque |
| CPV-6 | Lambda | Cutaneous inverted papilloma |
| CPV-7 | Tau | Cutaneous papilloma, in situ SCC |
| CPV-8 | Chi | Pigmented plaque |
| CPV-9 | Chi | Pigmented plaque |
| CPV-10 | Chi | Pigmented plaque |
| CPV-11 | Chi | Pigmented plaque |
| CPV-12 | Chi | NR |
| CPV-13 | Tau | Oral papilloma |
| CPV-14 | Chi | Pigmented plaque |
| CPV-15 | Chi | NR |
CPV, canine papilloma virus; NR, not reported; SCC, squamous cell carcinoma.
Figure 6-140.

Canine oral papillomatosis. Multiple white to gray pedunculated frond-like masses in the mouth and nasal philtrum of a dog.
Cutaneous (exophytic) papillomas occur in dogs of any age, but they are usually young or elderly. They are associated with CPV-1, CPV-2, and CPV-7. They may be single to multiple, occurring mainly on the head, eyelids, and paws. These lesions are usually smaller than 0.5 cm, pedunculated to cauliflower-like, soft to firm, well circumscribed, alopecic, and smooth to hyperkeratotic. These lesions usually spontaneously regress.
Cutaneous inverted papillomas are usually seen in young adult dogs <3 years of age and have been associated with CPV-1, CPV-2, and CPV-6. Lesions are single to multiple, 1-2 cm in diameter, raised, firm, and contain a central pore filled with keratin (Fig. 6-141A ). They occur most commonly on the ventral abdomen and groin, can occur on limbs and digits and most do not regress spontaneously. Histologically, these lesions are cup shaped with a central core of keratin that may be parakeratotic (Fig. 6-141B). The cup is lined by hyperplastic squamous epithelium with centripetal papillary projections. The cells may exhibit koilocytes or blue-gray cytoplasm. Large keratohyaline granules and intranuclear inclusions may be present. Malignant transformation has been associated with CPV-2 infection in immunosuppressed dogs.
Figure 6-141.

Inverted papilloma in a dog. A. Cup-shaped inverted papilloma.
(Courtesy A. Alcaraz, M. Heil.)
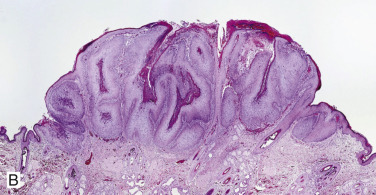
B. Papillated epidermal hyperplasia with hypergranulosis and koilocytes projects from a cup-shaped wall, and the center is filled with keratin.
(Courtesy J. Tran.)
Canine pigmented plaques may be heritable because they are most commonly reported in certain breeds: Miniature Schnauzers and Pugs. Affected dogs are usually young adults. Plaques in other breeds tend to be restricted to immunocompromised dogs. Lesions are most common on the ventral abdomen and groin and are characterized by melanotic macules, papules, and plaques that often have a scaly surface (Fig. 6-142A ). Histologically, there is well-demarcated, moderate epidermal hyperplasia with a scalloped configuration, hyperpigmentation of the lower layers of the epidermis, and clumped keratohyaline granules in the stratum spinosum (Fig. 6-142B). Koilocytes and viral inclusions are rare to absent. The potential for transformation to bowenoid in situ carcinoma (BISC), and ISCC has been reported in lesions infected with CPV-3.
Figure 6-142.

Pigmented viral plaques in a pug. A. Melanotic macules, papules, and plaques on the ventral abdomen.
(Courtesy M.S. Canfield.)
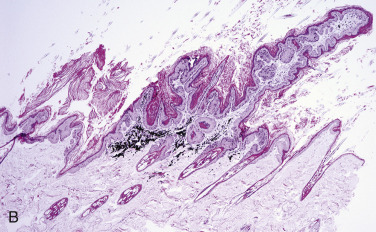
B. Well-demarcated epidermal hyperplasia, hyperpigmentation, hyperkeratosis, scalloped configuration, and pigmentary incontinence.
Canine pigmented papules have been rarely associated with long-term glucocorticoid therapy. Lesions are single to multiple, black papules up to 2 mm in diameter. Histologically, there are well-demarcated, cup-shaped foci of epidermal hyperplasia with marked parakeratotic hyperkeratosis. These lesions may resolve after cessation of glucocorticoid therapy.
Like other PVs, some CPVs have been associated with ISCC and some with BISC. Anecdotally, the author has seen 2 young dogs with generalized demodecosis associated with CPV. One dog had multiple oral and cutaneous papillomas, oral SCC associated with CPV-1, and was thought to have T-cell dysfunction. The other dog had numerous viral plaques that were positive by IHC for canine papillomavirus.
Cats.
Papillomavirus infection has been associated with cutaneous papillomas, feline viral plaques, feline sarcoid (feline fibropapilloma), BISC, and ISCC in cats. PV-induced exophytic cutaneous papillomas are rare in domestic cats, with only 2 cases reported. One developed on the eyelid of a previous surgical site, and the other developed on the nasal planum of an older cat with actinic keratosis. Interestingly, human papillomavirus 9 was isolated from the latter. Feline viral plaques are uncommon and occur as multiple scaly, flat, variably pigmented lesions that can develop anywhere on the body. Felis catus papillomavirus 1 (FcaPV-1), also called Felis domesticus PV-1 (FdPV-1), a lambda-PV, and FcaPV-2, a dyotheta-PV, have been isolated from these lesions; however, FcaPV-2 has also been isolated from many cats with no skin lesions. Viral plaques may spontaneously resolve; however, some have been known to progress to BISC. In fact, FcaPV-2 DNA has been detected in many feline BISC lesions and up to 50% of ISCC lesions and is thought to play a role in the pathogenesis of these lesions. Feline viral plaques have been associated with immunosuppression in some cats but have also been noted in healthy cats. Histologically, they are well-demarcated foci of epidermal hyperplasia and hyperkeratosis. The granular layer is thickened and irregular, and keratohyaline granules are frequently enlarged. Small numbers of koilocytes may be present in the stratum granulosum.
Feline BISC (a multicentric squamous cell carcinoma in situ) usually appears as multiple crusting, hyperpigmented, roughly circular plaques in middle-aged to older cats. Solitary lesions may occur. The face, neck, and limbs may be predisposed. It is uncommon to rare. Lesions may be more severe in hairless breeds. FcaPV-2 and FcaPV-3 (tau-PV) have been detected from many of these lesions. Rarely, intrafollicular Demodex cati can be found in these lesions, sometimes in association with feline immunodeficiency virus infection. Microscopically, there is abrupt hyperplasia and dysplasia of the epidermis and follicular outer root sheath that remain confined to the basement membrane (Fig. 6-143 ). The basal and spinous layers are most affected. Mitotic activity is present in all layers of the epidermis, and keratin pearl formation may be present. Tumor cells often have large hyperchromatic nuclei and may have vacuolated cytoplasm, cytoplasmic pallor, or occasionally are multinucleated. Groups of dysplastic cells have elongated nuclei that tend to orient in one direction (“wind-blown”) appearance. The tumors are often pigmented and may have papillomatous epidermal projections with marked hyperkeratosis, occasionally forming a cutaneous horn. These lesions may progress to ISCC. Distant metastasis is very rare but was reported in a 7-year-old Devon Rex cat.
Figure 6-143.
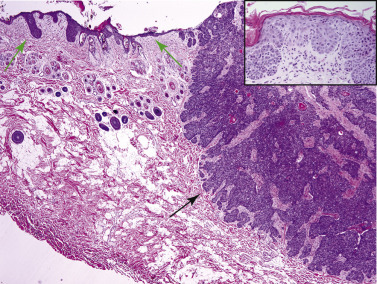
Feline bowenoid in situ carcinoma and invasive squamous cell carcinoma. In situ carcinoma is characterized by abrupt hyperplasia and dysplasia of the epidermis and outer root sheath (green arrows; also see inset). Squamous cell carcinoma is characterized by invasive anastomosing islands and trabeculae of neoplastic epithelial cells (black arrow) with multiple keratin pearls.
Invasive squamous cell carcinomas are the most common malignant cutaneous neoplasms of cats. They are discussed later under Squamous cell carcinoma.
Papillomaviruses have also been associated with feline sarcoids. These are rare cutaneous neoplasms that tend to occur on the nose, lips, or digits of young to middle-aged cats from rural areas (Fig. 6-144 ). Feline sarcoids are firm, smooth, exophytic, and can become ulcerated. Recurrence is common, but metastasis has not been documented. Histologic features virtually identical to the equine sarcoid have been described and found to be associated with papillomavirus DNA via PCR. The implicated virus feline sarcoid-associated PV (FeSarPV) is thought to be a novel bovine papillomavirus (BPV), given the similarity in its DNA sequences to BPV-1, BPV-2, and ovis aries papillomavirus 2 (OaPV-2).
Figure 6-144.

Feline sarcoid on the nose of a cat.
(Courtesy C.G. Knight.)
Camelids.
Fibropapillomas associated with papillomaviruses have been described in both llamas and alpacas. Lesions were located on the nose, lips, and cheeks and histologically resembled equine sarcoids. Of 6 reported cases, all lesions were cured by surgical excision, with the exception of one that recurred and spread. One viral squamous papilloma was reported on the cornea of a dromedary camel. The specific PV was not identified in that case. Camelus dromedarius papillomavirus 1 (delta-PV) has been associated with fibropapillomas in Arabian camels.
Rabbits.
Domestic rabbits develop oral papillomatosis caused by infection with Rabbit oral papillomavirus. Papillomas, which are multiple and found most often under the tongue, are grossly and histologically typical of viral-induced squamous papillomas.
Further reading
Bergvall KE. Sarcoids. Vet Clin North Am Equine Pract 2013;29:657-671.
De Lorimier L, Garrett LD. Neoplastic and non-neoplastic tumors. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 774-843.
Desrochers A, et al. Congenital cutaneous papillomatosis in a one-year-old Holstein. Can Vet J 1994;35:646-647.
Gil da Costa RM, Medeiros R. Bovine papillomavirus: opening new trends for comparative pathology. Arch Virol 2014;159:191-198.
Gorino AC, et al. Use of PCR to estimate the prevalence of Equus caballus papillomavirus in aural plaques in horses. Vet J 2013;197:903-904.
Guaguere E, et al. Demodex cati infestation in association with feline cutaneous squamous cell carcinoma in situ: a report of five cases. Vet Dermatol 1999;10:61-67.
Gulbahar MY, et al. Angiokeratomatous papilloma associated with papillomavirus in a calf. Vet Pathol 2003;40:582-586.
Kilic N, et al. Corneal papilloma associated with papillomavirus in a one-humped camel (Camelus dromedarius). Vet Ophthalmol 2010;13(Suppl. 1):100-102.
Knight CG, et al. Equine penile squamous cell carcinomas are associated with the presence of equine papillomavirus type 2 DNA sequences. Vet Pathol 2011;48:1190-1194.
Kumar P, et al. Detection of bovine papilloma viruses in wart-like lesions of upper gastrointestinal tract of cattle and buffaloes. Transbound Emerg Dis 2013;doi:10.1111/tbed.12127; [Epub ahead of print].
Lange CE, et al. Four novel papillomavirus sequences support a broad diversity among equine papillomaviruses. J Gen Virol 2013;94:1365-1372.
Lange CE, Favrot C. Canine papillomaviruses. Vet Clin Small Anim 2011;41:1183-1195.
Le Net JL, et al. Multiple pigmented cutaneous papules associated with a novel canine papillomavirus in an immunosuppressed dog. Vet Pathol 1997;34:8-14.
Lucroy MD, et al. Cutaneous papillomatosis in a dog with malignant lymphoma following long-term chemotherapy. J Vet Diagn Invest 1998;10:369-371.
Lunardi M, et al. Bovine papillomavirus type 13 DNA in equine sarcoids. J Clin Microbiol 2013;51:2167-2171.
Munday JS. Bovine and human papillomaviruses: a comparative review. Vet Pathol 2014;51:1063-1075.
Munday JS. Papillomaviruses in felids. Vet J 2014;199:340-347.
Munday JS, et al. Feline cutaneous viral papilloma associated with human papillomavirus Type 9. Vet Pathol 2007;44:924-927.
Munday JS, et al. Genomic characterization of Felis catus papillomavirus-3: a novel papillomavirus detected in a feline Bowenoid in situ carcinoma. Vet Microbiol 2013;165:319-325.
Munday JS, Kiupel M. Papillomavirus-associated cutaneous neoplasia in mammals. Vet Pathol 2010;47:254-264.
Nagata M, Rosenkrantz W. Cutaneous viral dermatoses in dogs and cats. Compend Contin Educ Vet 2013;35:E1-E10.
Nasir L, Campo MS. Bovine papillomaviruses: their role in the aetiology of cutaneous tumours of bovids and equids. Vet Dermatol 2008;19:243-254.
Ravens PA, et al. Papillomavirus-associated multicentric squamous cell carcinoma in situ in a cat: an unusually extensive and progressive case with subsequent metastasis. Vet Dermatol 2013;24:642-645, e161-e162.
Rector A, Van Ranst M. Animal papillomaviruses. Virol 2013;445:213-223.
Schulman FY, et al. Feline cutaneous fibropapillomas: clinicopathologic findings and association with papillomavirus infection. Vet Pathol 2001;38:291-296.
Schulman FY, et al. Camelid mucocutaneous fibropapillomas: clinicopathologic findings and association with papillomavirus. Vet Pathol 2003;40:103-107.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Scott DW, Miller WH. Neoplasms, cysts, hamartomas, and keratoses. In: Scott DW, Miller WH, editors. Equine Dermatology. 2nd ed. St Louis: Elsevier Saunders; 2011. p. 468-516.
Torres SMF, Koch SN. Papillomavirus-associated diseases. Vet Clin North Am Equine Pract 2013;29:643-655.
Zhu W, et al. Bovine papillomavirus type 10 with a deletion associated with a lingual papilloma in a cow. Vet J 2014;199:303-305.
Squamous cell carcinoma
Squamous cell carcinoma (SCC) is a relatively common, locally invasive, and occasionally metastatic neoplasm of most domestic species. The behavior of squamous cell carcinoma (SCC) of the skin is usually that of locally destructive spread. Its metastatic potential is low, with certain qualifications depending on location. Those initiated by sunlight are slow to metastasize, and usually only to local lymph nodes. In contrast, those originating on the canine digit may be more prone to metastasize, but even these are cured by amputation in virtually all but the most neglected cases.
Development of SCC has been associated with papillomaviruses in multiple species, including dogs, cats, horses, and sheep (see cutaneous papillomas). Sunlight is probably the most important carcinogenic stimulus for these tumors. The action of sunlight may be related to overexpression of p53 protein as a result of ultraviolet (UV)-induced mutations of the p53 tumor suppressor gene. Chronic sun exposure, lack of pigment, and thin haircoat in the area of tumor development are predisposing factors. In these cases, SCC is usually preceded by actinic keratosis and is seen more frequently in geographic regions exposed to long periods of intense sunlight (see Actinic diseases of skin). Affected animals are usually middle aged to older. In cats, predilection sites for UV-induced SCC are eyelids, pinnae, and nasal planum (Fig. 6-145 ). In dogs, the ventral trunk, digits, limbs, scrotum, and lips are the most common sites. The nasal planum is rarely affected, and when it is affected, it is usually secondary to depigmentation from a chronic inflammatory condition, such as discoid lupus erythematosus. Subungual squamous cell carcinomas in dogs may be multiple and are seen most often in black dogs, particularly large breeds such as Labrador Retrievers and Standard Poodles. Although papillomaviruses have been a suspected etiology, one study did not support a viral pathogenesis. In horses, the periocular region, penis, and perianal regions are predilection sites, and Appaloosas, American Paint horses, Quarter Horses, and males are predisposed. In cattle, Herefords and Ayrshires are at increased risk, and lesions are most common on the face, eyelids, pinnae, back, vulva, and distal legs. In goats, Angoras and Boers may be at increased risk, and lesions are most common in sparsely haired skin of the udder, perianal region, horn base, pinnae, vulva, and eyelid. In sheep, cutaneous SCC is most common on the muzzle, lips, eyelids, pinnae, perineum, and vulva, and Merinos may be at risk. SCC in llamas and alpacas has been reported in ocular tissue, perineum, and haired skin. SCCs are rare in pigs but usually occur in white skin.
Figure 6-145.

Ultraviolet light–induced squamous cell carcinoma in a white cat. Erythematous, ulcerative, crusted lesions on the tips of the pinna, nasal planum, and eyelids.
Rarely, SCC has been reported to arise from burn scars, nonhealing wounds, and chronic inflammation. Brand keratomas in cattle have been reported to undergo malignant transformation to SCC. SCC with regional metastasis was reported in a 12-year-old llama with an 18-month history of a nonhealing wound. SCC have been reported to arise from follicular cysts in both dogs and sheep. Equine smegma has been implicated in the development of preputial SCC.
Squamous cell carcinoma in situ refers to a malignant tumor of cells with squamous differentiation that is confined by the basement membrane. Multicentric SCC in situ in cats (bowenoid in situ carcinoma) is discussed under Papillomas and papillomavirus-induced lesions.
Invasive squamous cell carcinomas (ISCC) are plaque-like, crateriform, or papillary masses that vary from a few millimeters to several centimeters in diameter. Alopecia, erythema, ulceration, and crusting are usually present. Lesions may be single to multiple. On cut section, they are firm and white. In some locations (eye, penis), they are raised and papillary, even though the surface is ulcerated.
Histologically, several subtypes have been described and they include well-differentiated, poorly differentiated, acantholytic, spindle cell, and verrucous variants. The well-differentiated SCC is a plaque-like lesion composed of islands, cords, and trabeculae of squamous cells that originate from the epidermis or rarely hair follicles or follicular cysts, breach the basement membrane, and extend into the dermis. Intercellular bridges between keratinocytes may be prominent, and there is often formation of central accumulations of compact laminated keratin (keratin pearls) within islands of invasive neoplastic epithelial cells. There is a fairly orderly progression from polyhedral, nonkeratinized basal cells at the periphery of the neoplastic epithelial structures to large polygonal keratinized cells at the centers. Neoplastic cells have vesicular nuclei with one or multiple very prominent nucleoli. Cytoplasm is usually abundant and eosinophilic. There is often a desmoplastic reaction in the surrounding dermis. There may be marked crusting and hyperkeratosis. Poorly differentiated SCCs tend to be composed of mostly cords and nests of neoplastic epithelial cells. Neoplastic cells have amphophilic cytoplasm with hyperchromatic nuclei and prominent nucleoli. There is moderate to high mitotic activity and frequent mitotic atypia. Keratin pearls are not observed, and instead, there are individual dyskeratotic cells or clusters of partially keratinized cells.
Acantholytic squamous cell carcinoma is an uncommon variant. Pseudoglandular to pseudocystic structures are formed by drop-out of partially keratinized cells from the centers of epithelial islands and trabeculae resulting from loss of intercellular junctions. This type of tumor must be carefully distinguished from an adenocarcinoma by identifying tumor cell keratinization. Spindle cell squamous cell carcinoma is a rare variant of poorly differentiated SCC and is composed of large pleomorphic spindle and polygonal cells that have abundant pale or amphophilic cytoplasm. Nuclei are large and vesicular with prominent nucleoli. The mitotic index is high. Rare foci of individual cell keratinization will help distinguish this neoplasm from a sarcoma. Verrucous squamous cell carcinoma is a rare variant of SCC only described in dogs. It is a low-grade malignancy. It is both exophytic and endophytic, and the broad trabeculae have smooth rounded margins. There may be large tubular invaginations with sloughed keratinocytes. Keratin pearls are absent. There is mild cellular pleomorphism and low mitotic activity.
Carcinoma of the horn of cattle is almost exclusive to castrated male adult cattle in India and neighboring countries. The tumor gradually infiltrates and destroys the horn core and may invade adjacent sinuses and cranial bone. The histology is of well-differentiated squamous cell carcinoma, but neither the site of origin nor the reason for its peculiar site and sex preference is understood.
Basal cell carcinoma
Basal cell carcinomas (BCCs) are uncommon in cats and dogs and rare in other domestic species. These tumors are thought to arise from epithelial cells of the basal layer of the epidermis and adnexa. They are the most common malignant neoplasms in humans, and chronic exposure to UV radiation is a key factor in the development of these tumors. In cats, chronic UV exposure may also play a role. However, in some cats, BCC arises from BISC, and therefore papillomaviruses may also play a role in pathogenesis. The pathogenesis is unknown in dogs. BCC usually occur as single to occasionally multiple, alopecic and crusted, ulcerated plaques or umbilicated nodules measuring a few millimeters to several centimeters in diameter. The skin may have a black or blue tint because of melanin pigment in the neoplasm. BCC in cats occurs most commonly on the face, nose, and pinnae. BCC in dogs are usually on the trunk. They generally occur in middle-aged to older animals. They are generally considered a low-grade malignancy. Rates of recurrence and metastasis are very low.
There are 3 histopathologic variants: solid, keratinizing, and clear cell. BCC have a horizontal plaque-like configuration extending multifocally from the epidermis. The neoplastic cells of solid basal cell carcinoma resemble basal cells of the epidermis or hair follicles. Each has an oval, deeply basophilic nucleus, a single nucleolus, and scant eosinophilic cytoplasm with indistinct cell boundaries. In contrast to normal stratum basale, there are no intercellular bridges. The cells extend into the dermis as islands, trabeculae, or grow expansively as solid sheets embedded in a moderately cellular stroma of fibrous or fibromyxoid tissue. Caseation necrosis, sometimes with cystic degeneration, is often present in the centers of large epithelial islands. Solid BCCs may have small foci of squamous differentiation. Mitotic figures and nuclear pleomorphism are variable. Tumor cells may contain melanin, and melanophages may be present in the intervening stroma. Keratinizing basal cell carcinomas have similar features to the solid type; however, melanin and cystic degeneration are uncommon. Angular islands and trabeculae of neoplastic epithelium predominate. Mitotic activity is moderate to high, and mitotic atypia can usually be detected. Many of the epithelial islands contain central or peripheral foci of abrupt squamous differentiation that is cytologically benign and may or may not have keratinization. Clear cell basal cell carcinomas are rare. The epithelial cells are larger and have clear to finely granular cytoplasm. Nuclei lack pleomorphism, nucleoli are small, and mitotic activity is variable. Necrosis is common.
Basosquamous carcinoma
This rare tumor has features of both SCC and BCC and has been described in the cat and dog. It is clinically indistinguishable, and histologically it has a similar silhouette. Basosquamous carcinomas are composed primarily of dermal lobules of basaloid cells with centralized foci of atypical abruptly keratinized cells. The squamous component has histologic features of malignancy and lacks differentiation of the follicular isthmus or bulb. These 2 features help differentiate it from a keratinizing BCC. The basaloid population may have foci of dyskeratosis or melanization. Tumor lobules may or may not be connected with the epidermis.
Further reading
De Lorimier L, Garrett LD. Neoplastic and non-neoplastic tumors. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 774-843.
Goldschmidt MH, et al. Histological Classification of Epithelial and Melanocytic Tumors of the Skin of Domestic Animals. Washington, DC: Armed Forces Institute of Pathology; 1998.
Gross TL, et al. Epithelial tumors. In: Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 562-603.
Lascelles BD, et al. Squamous cell carcinoma of the nasal planum in 17 dogs. Vet Rec 2000;147:473-476.
Lohr CV. One hundred two tumors in 100 goats (1987-2011). Vet Pathol 2012;50:668-675.
Munday JS, et al. Papillomaviral DNA sequences are not amplifiable from canine subungual squamous cell carcinomas. N Z Vet J 2013;61:234-236.
Nikula KJ, et al. Ultraviolet radiation, solar dermatosis, and cutaneous neoplasia in beagle dogs. Radiat Res 1992;129:11-18.
O'Brien MG, et al. Treatment by digital amputation of subungual squamous cell carcinoma in dogs: 21 cases (1987-1988). J Am Vet Med Assoc 1992;201:759-761.
Schaffer PA, et al. Cutaneous neoplastic lesions of equids in the central United States and Canada: 3,351 biopsy specimens from 3,272 equids (2000-2010). J Am Vet Med Assoc 2013;242:99-104.
Scott DW. Color Atlas of Farm Animal Dermatology. Ames, Iowa: Blackwell; 2007.
Sironi G, et al. p53 protein expression in conjunctival squamous cell carcinomas of domestic animals. Vet Ophthalmol 1999;2:227-231.
Valentine BA. Survey of equine cutaneous neoplasia in the Pacific Northwest. J Vet Diagn Invest 2006;18:123-126.
Valentine BA, Martin JM. Prevalence of neoplasia in llamas and alpacas (Oregon State University, 2001-2006). J Vet Diagn Invest 2007;19:202-204.
Tumors with adnexal differentiation
Tumors arising from hair follicles
Hair follicle (pilar) neoplasms occur in most domestic species but are most commonly encountered in the dog and cat. Their classification is rather complex; however, the majority of tumors arising in animals share a benign biological behavior. Exceptions exist as follows:
Infundibular keratinizing acanthoma (intracutaneous cornifying epithelioma) is a benign cystic tumor of the skin of dogs. Tumors are 0.5-4 cm in diameter and classically have a central pore with a hard keratinized plug. Common sites are the dorsum of the neck and back. Subungual lesions also occur. Usually, there is only a single tumor, but Norwegian Elkhounds and Keeshonds are predisposed to developing a generalized form affecting the entire body.
The histologic lesion is a well-demarcated cup-shaped dermal mass oriented around a central cyst filled with concentric laminated to amorphous keratin (Fig. 6-146 ). With fortuitous sectioning, a central pore opening to the surface will be seen. The epithelium surrounding the cyst consists of large polygonal cells with abundant pale-pink glassy cytoplasm. There is a sparse granular layer. The periphery of the cyst wall consists of orderly basal cells. Extending into the deeper dermis from the cyst wall are small secondary horn cysts resembling keratin pearls interconnected by narrow cords of basal epithelium. The stroma is poorly cellular and often mucinous. Cartilaginous and osseous metaplasia are occasionally seen. Focal rupture is common, inciting a granulomatous or pyogranulomatous reaction in surrounding dermis.
Figure 6-146.
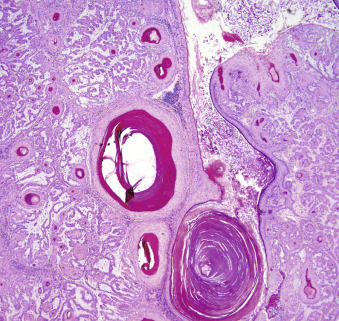
Infundibular keratinizing acanthoma. Cup-shaped mass oriented around a central cyst. Cords of epithelium and secondary horn cysts in mucinous stroma extend out from the cyst wall.
Trichoepitheliomas are common in dogs, uncommon in cats, and reported in horses, cattle, and an alpaca. However, in this author's opinion, the report in the alpaca was probably a hybrid follicular cyst. Trichoepithelioma is a tumor of primitive hair germ that exhibits rudimentary differentiation toward all 3 segments of the follicle: the infundibulum, isthmus, and the inferior segment. Trichoepitheliomas are single or multiple alopecic skin tumors occurring anywhere on the body, with a slight preference for the back in dogs and tail in cats. Persian cats are predisposed. Tumors are usually <2 cm in diameter but on occasion can be very large and ulcerated. Multiple tumors occur most frequently in Basset Hounds. Histologically, the tumor is well circumscribed, unencapsulated, and composed of multiple variably sized epithelial islands and cystic structures. These structures are partially or fully lined by squamous epithelium with or without a granular layer or basaloid epithelial cells resembling matrical epithelium surrounded by a thickened basement membrane. The cystic structures are filled with infundibular, trichilemmal, or keratinized “ghost cells,” depending upon the lining epithelium (Fig. 6-147A, B ).
Figure 6-147.
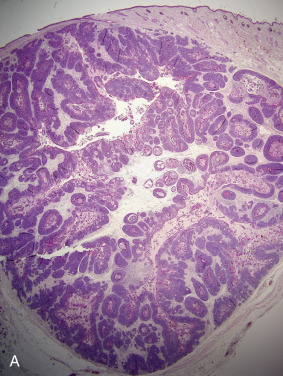
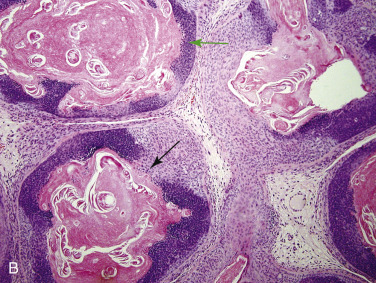
Trichoepithelioma. A. Well-demarcated dermal mass composed of numerous small cystic epithelial structures with a fibromyxoid stroma. B. Note the abrupt keratinization and differentiation toward the isthmus (black arrow) and inferior segment (green arrow) of the follicle.
The outer layer of basal cells usually shows peripheral palisading and may abut the fibrous stroma or send out basal cell ribbons into a mucinous stroma. Some trichoepitheliomas have several large primary cystic areas surrounded by many smaller cysts. Rupture of some of the keratinaceous cysts stimulates pyogranulomatous inflammation within the stroma and even within the cyst, sometimes accompanied by mineralization and foreign body giant cells. Mineralization and inflammation are more typical of the closely related pilomatricoma.
Malignant trichoepitheliomas have only been described in dogs. They are generally larger, asymmetrical, and poorly circumscribed compared to their benign counterpart. Other features include atypical mitotic figures, central caseous necrosis within the islands of matrical cells, minimal squamous component, and invasion of subcutis sometimes accompanied by desmoplasia. Lymphatic invasion is considered an essential finding to confirm malignancy by some pathologists. Regional and pulmonary metastasis is possible. Trichoepitheliomas are distinguished from all other epidermal or appendage tumors by the abrupt (matrical) keratinization and the follicle-like basal cell nests that surround it. Other tumors or cysts simulating trichoepithelioma lack one or both of these features.
Tricholemmoma is a rare, benign, and nonrecurring pilar tumor of the outer root sheath recognized in dogs and cats. There are 2 types: one in which the tumor cells differentiate into cells characteristic of the inferior segment of the hair follicle (inferior tricholemmoma) external root sheath or the second type, the isthmus (isthmic tricholemmoma) section of the external root sheath. Inferior tricholemmomas are very rare, only recognized in dogs, 1-7 cm diameter firm nodules on the head and neck. Tumor cells form nests separated by a fine collagenous stroma. The tumor cells have abundant eosinophilic cytoplasm that is pale (clear cells) peripherally and more intensely eosinophilic toward the center of the nests. Pallor of the outermost layer of cells is due to marked cytoplasmic glycogen storage, seen in histologic section as cytoplasmic clearing. These are thought to represent differentiation toward outer root sheath cells. Each tumor follicle is surrounded by a thick, homogeneous basal lamina resembling the vitreous sheath of the normal follicle. Isthmic tricholemmomas are very rare, raised, alopecic papules and nodules <2 cm in diameter, recognized in cats and dogs. The epithelial cells are arranged as islands, and radiating cords that may intersect or be associated with the epidermis. The tumor cells show central trichilemmal cornification. The granular layer is absent.
Trichoblastoma (basal cell tumor) is a benign tumor derived from the primitive hair germ of embryonic follicular development. There are ribbon, trabecular, granular, spindle cell (with outer root sheath differentiation) variants. These are common in dogs and cats, seen occasionally in horses, and rare in cattle and sheep. Lesions are generally solitary, firm, raised alopecic nodules 1-2 cm in diameter, although they can sometimes be much larger and ulcerated. The head, neck, and base of the ear are common locations, especially in dogs and cats.
-
•
The ribbon (garland, medusa-head) trichoblastoma is a well-demarcated dermal to subcutaneous tumor formed by long, narrow (2-cells thick), branching or winding cords of small basaloid epithelial cells (Fig. 6-148 ) that may join or radiate from a large central aggregate (medusoid pattern). A mucinous stroma is frequently associated with the medusoid pattern. Nuclei in tumors arranged in cords often palisade perpendicular to the long axis of the cord. Mitotic figures may be numerous. Abundant collagen that may appear hyalinized is more common in dog tumors. This pattern is common in dogs and rare in cats and other species.
-
•
Trabecular trichoblastomas are well-demarcated dermal masses composed of islands and broad trabeculae of basal keratinocytes with prominent peripheral palisading. The cells that are centrally located have more abundant cytoplasm. Connection to the overlying epidermis is minimal. Stroma is sparse and may be collagenous to mucinous and is of low cellularity. Keratin microcysts may be present. This is the most common variant of cats.
-
•
Granular trichoblastoma is a rare variant with the same architecture as a ribbon trichoblastoma, but the neoplastic epithelial cells are larger and contain abundant, finely granular or vacuolated cytoplasm. Nuclei are small, angular, and eccentric.
-
•
Spindle cell trichoblastomas are most often seen in cats. They are well-demarcated dermal masses composed of trabeculae and lobules of elongated, streaming, basaloid epithelial cells within a poorly cellular collagenous stroma. Peripheral palisading in not a prominent feature. There is often a broad zone of connection to the epidermis. Tumor cells have scant cytoplasm, oval nuclei with inconspicuous nucleoli, and rare mitoses. Melanin may be present in the tumor cells and accompanying melanophages. Keratinization is rare.
-
•
Trichoblastomas with outer root sheath differentiation are recognized by some pathologists. These are rare, well-demarcated masses in the dermis to subcutis composed of multiple lobules and trabeculae and areas of cystic degeneration. Small epithelial cells form anastomosing cords similar to the ribbon type, and these merge into islands of cells with markedly vacuolated cytoplasm resembling anagen suprabulbar outer root sheath or pale pink isthmus-type keratinocytes that line the cystic zones.
Figure 6-148.
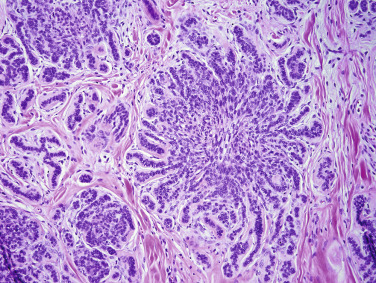
Trichoblastoma, ribbon type. Double rows of small basaloid epithelial cells arranged in branching and winding patterns.
Pilomatricoma (pilomatrixoma, epithelioma of Malherbe, necrotizing and calcifying epithelioma) is an uncommon benign tumor of dogs and is believed to be derived from primitive hair matrix and thus shows incomplete differentiation towards hair cortex. This tumor macroscopically resembles trichoepithelioma but is often more heavily mineralized and consists of fewer, larger cysts than does trichoepithelioma. They usually occur as single, firm to hard, raised, 1-10 cm diameter nodules most commonly on the proximal legs and dorsal trunk over the rump and shoulders. Poodles, Kerry Blue Terriers, and Old English Sheepdogs and other breeds with continuously growing coats, and thus a higher proportion of anagen follicles, are predisposed. The typical microscopic morphology is of one or more large, thick-walled cysts partially filled with so-called shadow or ghost cells (Fig. 6-149 ) typical of matrical differentiation. These cells are flattened eosinophilic epithelial cells with a central empty halo in place of the lysed nucleus. The cyst wall is composed of multiple layers of basal cells, resembling matrical epithelium of the hair bulb, and showing a sudden zonal degeneration to form the central laminations of shadow cells. Small zones of squamous epithelium may be seen. Small foci resembling rounded dermal papilla-like structures may be present in the cyst wall. These tumors are not connected to the overlying epidermis. There is sparse collagenous to mucinous stroma. Mitotic activity may be high. Mineralization of shadow cells is very common, and cyst rupture results in the pyogranulomatous inflammation that is very typical of these tumors. Foci of necrosis within the tumor are frequently seen, and mineralization or even ossification within the stroma occurs occasionally. Melanocytic matricoma, reported in one dog, is similar to pilomatricoma with the additional feature of neoplastic melanocyte proliferation.
Figure 6-149.
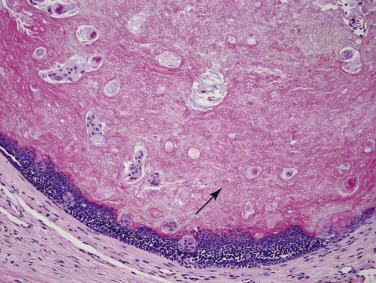
Pilomatricoma. Cystic mass lined by matrical epithelium with abrupt keratinization into the lumen. Note the numerous evenly spaced vacuoles (arrow) within the keratin (keratin ghost cells).
Malignant pilomatricomas (matrical carcinoma, pilomatrix carcinoma) are rare in dogs and not reported in other domestic species. They are locally aggressive and may invade bone, and have been reported to metastasize to multiple distant sites, including lung, central nervous system, and bone. This malignant variant is poorly circumscribed and may extend into the subcutis. Compared to its benign counterpart, there is usually an increased ratio of basaloid cells to keratinized ghost cells, infiltrative borders, increased mitotic activity, and mitotic atypia. Ulcerations and necrosis are common, and some neoplasms are connected to the epidermis. Additional features include desmoplastic stroma, and mineralization or ossification of keratin. Lymphatic invasion is the most important feature to support malignancy.
Tumors arising from sebaceous or modified sebaceous glands
Tumors of sebaceous glands include nodular sebaceous hyperplasia, sebaceous adenoma, sebaceous epithelioma, and sebaceous carcinoma. Modified sebaceous glands include the Meibomian glands of the eyelid and perianal (hepatoid, circumanal) glands. Tumors of the Meibomian gland include Meibomian gland adenomas, epitheliomas, and carcinomas that are histologically identical to the corresponding sebaceous gland lesion and will not be described separately. Perianal glands are only present in canids and are located in the perianal skin as well as around the proximal third of the tail, dorsal lumbosacral area, lateral to the prepuce, and along the ventral midline as far cranial as the neck. Tumors of perianal glands include perianal gland hyperplasia, perianal gland adenomas, epitheliomas, and carcinomas. Epitheliomas are considered to be low-grade malignancies. Sebaceous gland tumors are common in dogs, uncommon in cats and rare in other species.
Nodular sebaceous hyperplasia is common and accounts for 50% of the sebaceous gland tumors in dogs. Lesions are single or multiple, raised, yellow-orange, multilobulated, wart-like, waxy to hyperkeratotic masses. They are most common in Cocker Spaniels and Poodles on the head, eyelids, limbs, and trunk. Size varies but most are <1 cm in diameter. Many are ulcerated by continued tumor growth or by trauma. Histologically, there are multiple, enlarged sebaceous lobules clustered around one or more dilated sebaceous duct(s) and hair follicle(s). Secondary erosion and inflammation are common. The sebaceous cells (sebocytes) are fully mature, and the peripheral rim of basal (reserve) cell population is inconspicuous. There is no increase in basal reserve cells. Occasionally, some sebaceous lobules exhibit a metaplastic transformation to perianal gland cells.
Sebaceous adenomas are grossly similar to nodular sebaceous hyperplasia. Sebaceous adenomas differ from hyperplasia in that there are more basal (reserve) cells than in hyperplasia, and the lobular proliferation is greater and less symmetrical. Lesions are uncommon in cats, with the exception of Persian cats. Histologically, they are divided into simple and compound. Compound adenomas are more common. In the simple variant, ducts are not a prominent feature. Lesions are composed of multiple large lobules of sebocytes that show normal maturation. The compound variant (ductal adenoma) contains glandular lobules and ducts in various proportions. The sebaceous lobules are grouped in radiating clusters around ductal structures. As in nodular hyperplasia, perianal gland metaplasia is rarely observed. There may be compression of adjacent structures. Melanization in reserve cells is common in eyelid tumors.
Sebaceous epitheliomas are grossly similar to sebaceous adenomas. They are common in dogs, occurring most commonly in Shih Tzus and Lhasa Apsos. Histologically, these masses are composed of multiple large irregular lobules of epithelial reserve cells with multiple small foci of distinct sebaceous differentiation (Fig. 6-150 ). Mitotic activity may be high in the basal reserve cells, but mature sebocytes are not mitotically active. Small ducts lined by mature squamous epithelium are usually present. These lesions, especially Meibomian epitheliomas, are variably pigmented. This tumor is considered to be a low-grade malignancy. Sebaceous and Meibomian epitheliomas may recur if incompletely excised; rarely, sebaceous epitheliomas have been reported to invade lymphatics and metastasize to regional lymph nodes and, in one case, lung and central nervous system.
Figure 6-150.
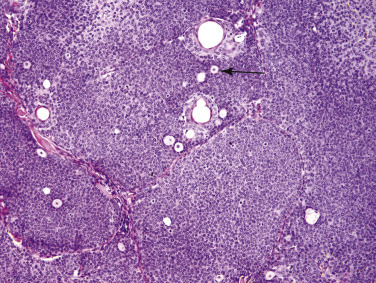
Sebaceous epithelioma in a dog. Lobules of basaloid epithelium with a few scattered mature sebocytes (arrow).
Sebaceous carcinomas are rare malignant neoplasms in dogs and cats. Cocker Spaniels may be predisposed. These lesions are usually solitary, firm nodules, up to 7 cm in diameter and most common on the head. Ulceration and alopecia are common. Histologically, some pathologists divide these tumors into 2 variants: sebocytic and epitheliomatous. Sebocytic carcinomas are multilobular dermal masses that are irregular in shape but well circumscribed and may extend into the subcutis. Neoplastic cells are polygonal and larger than basal reserve cells. Orderly progression from basaloid reserve cells to mature sebocytes is markedly distorted or absent. Neoplastic cells are pleomorphic with eosinophilic cytoplasm that is variably vacuolated. Nuclei are large with prominent nucleoli, and mitotic activity is moderate to high. There may be atypical mitotic figures. Other possible features include ulceration, necrosis, cystic degeneration, squamous differentiation, keratinization, or occasional glandular structures. Epitheliomatous sebaceous carcinomas are composed predominantly of slightly larger and more pleomorphic than normal basaloid reserve cells in islands, cords, and trabeculae. There are scattered foci of mature sebocytes. There may be multifocal connections to the epidermis. They are commonly ulcerated, and margins may be infiltrative and can extend into the subcutis. Distinction between epitheliomatous carcinoma and sebaceous epithelioma includes the following proposed criteria: Carcinomas have an increased nuclear size, a higher mitotic rate, atypical mitotic figures, and mitotic figures in the mature sebocytes. They may be locally aggressive but reports of distant metastasis are rare.
The cause of perianal gland tumors is unknown; however, they are known to be modulated by sex hormones and contain both androgen and estrogen receptors. Nodular perianal gland hyperplasia may occur as either discrete nodules of variable size or as a diffuse bulging ring around the anus. Histologically, there are multiple enlarged lobules of well-differentiated perianal gland cells with a single peripheral layer of basaloid reserve cells. Lobules are organized around small ducts. Mitotic activity is low.
Perianal (hepatoid) gland adenomas are common and occur only in dogs. Males are predisposed. The gross appearance of perianal gland adenomas is of one or more raised rubbery masses that may grow to 10 cm or more in diameter, most commonly around the anus but can occur anywhere perianal glands exist. Adenomas are well-circumscribed nodular or multinodular masses composed of broad, anastomosing trabeculae or islands of well-differentiated perianal gland cells surrounded by a single layer of basal reserve cells (Fig. 6-151 ). There is low mitotic activity, delicate fibrovascular to collagenous stroma, and compression of adjacent glands and structures. Ulceration is common in large tumors. Distinguishing adenomas from hyperplasia can be difficult, but the main difference is that the lobular architecture is maintained in hyperplastic lesions, and adenomas may be highly vascular. Local excision and castration is usually curative and prevents the development of new benign perianal gland tumors.
Figure 6-151.
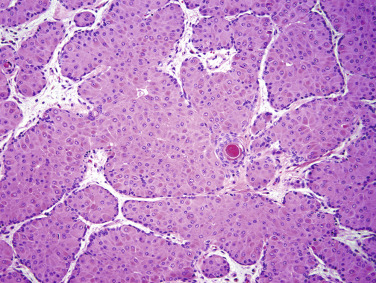
Perianal (hepatoid) gland adenoma in a dog. Anastomosing islands and trabeculae of well-differentiated perianal (hepatoid) gland cells surrounded by a single layer of basaloid reserve cells embedded in a delicate fibrovascular stroma. There is a small focus of squamous metaplasia.
Perianal (hepatoid) gland epitheliomas are rare tumors and may be benign or of low-grade malignancy. They are composed of predominantly (>90%) basal reserve cells with small scattered foci of mature perianal gland cells. Neoplastic cells are arranged in sheets, islands, and anastomosing trabeculae. The tumor margin is irregular and mildly infiltrative. Small ducts may be present. Mitotic activity is increased in comparison to the adenomas, but nuclear atypia is not present, and mitotic figures are not observed within mature perianal gland cells.
Perianal (hepatoid) gland carcinomas are uncommon, and when they occur, they are usually perianal in location. They are grossly similar to adenomas, and most are 2 cm or greater diameter. Histologically, they vary from well differentiated to poorly differentiated. Well-differentiated tumors have similar architecture to adenomas but have variable infiltrative growth at the margins. Mature and basal reserve cells are disorganized and scattered haphazardly within neoplastic islands and trabeculae. Nuclei are larger than those in benign lesions, slightly pleomorphic, and may have multiple prominent nucleoli. Mitotic activity is low to moderate with mitotic atypia and mitoses of mature cells. There may be small scattered foci of squamous metaplasia. Ulceration, hemorrhage, and necrosis are common. Poorly differentiated tumors are rare. They are poorly circumscribed and infiltrative, composed of cords and trabeculae of pleomorphic polygonal cells. Neoplastic cells have eosinophilic to amphophilic cytoplasm that is variably vacuolated. Nuclei are large and vesicular with prominent nucleoli. Mitotic activity is high, and atypia is common. Lymphatic invasion must be diagnosed with caution because compression of reserve cells by lobular expansion may simulate a tumor embolus surrounded by lymphatic endothelium. Carcinomas tend to grow more rapidly and ulcerate more than adenomas. Metastasis to regional lymph nodes occurs in 30% of cases. Direct extension into the pelvic canal can occur. Castration is generally not effective treatment for carcinomas.
Tumors arising from sweat glands
Epitrichial (apocrine) gland tumors can be benign or malignant. Adenomas are more common and occur in cats, dogs, and rarely in horses, cattle, and pigs. They are usually solitary, 0.5-10 cm in diameter, and ulcerated. Cystic tumors may be blue to purple. In dogs, adenomas are more common on the head, neck, dorsal trunk, and limbs. Similar sites are affected in cats, with the addition of pinnae and tail. Pinnae and vulva are common sites in horses. Carcinomas more commonly occur on the legs and may be poorly circumscribed and infiltrative. Adenoma variants include cystadenoma, simple and complex secretory adenoma, and ductular adenomas, which are divided into canine, feline, and solid-cystic ductular adenomas. Epitrichial cystadenomas (apocrine hidrocystoma) are well-circumscribed, dermal masses composed of one or more cystic structures generally lined by a single layer of cuboidal to columnar epithelium. Some cysts contain simple or branching papillary aggregates, and if this is a dominant feature, then the term papillary cystadenoma is appropriate. Small glandular structures may be present. In cats, the majority of these tumors are on the head, including ear canal and eyelid (glands of Moll), and lesions may be multiple in Himalayan and Persian cats. Simple secretory epitrichial adenomas are well-circumscribed dermal neoplasms with acinar, tubular, or papillary patterns. Cystic cavities and glandular lumens may contain pale eosinophilic homogeneous secretory material.
Complex (mixed) secretory epitrichial adenomas are analogous to complex and benign mixed mammary adenomas. Stroma may be myxoid or have chondroid differentiation. Osseous metaplasia is uncommon. Canine epitrichial ductular adenomas are circumscribed, multinodular, and located in the deep dermis to subcutis. Lobules are composed of tightly packed tubular structures lined by a double layer of cuboidal epithelium that resemble basal cells. There are multiple small foci of squamous metaplasia. There is moderate collagenous stroma, moderate mitotic activity, and no secretory activity. Feline epitrichial ductular adenomas are similar to those of dogs (Fig. 6-152 ). The centers of the lobules may be irregularly cystic and partially lined by cuboidal epithelium. Mitotic activity is low and stroma is sparse. Solid-cystic epitrichial adenomas are multinodular, circumscribed, and often vertically oriented in the dermis. There is cystic degeneration of larger lobules. These neoplasms are formed of 2 distinct cell types: a small basaloid cuboidal cell and slightly larger polygonal cells. The smaller cells form occasional short, double rows with or without an obvious, often sharp, angular lumen (ductal structures). Melanization is common in this variant.
Figure 6-152.
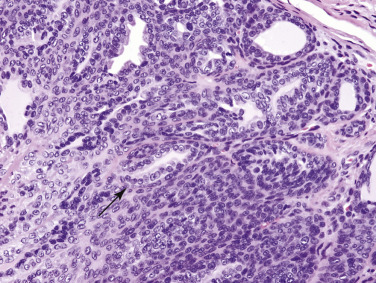
Feline epitrichial ductal adenoma. Multiple tubular structures are lined by a double layer of cuboidal epithelium (arrow).
Epitrichial (apocrine) carcinomas have similar histologic variants to the adenomas: cystadenocarcinoma; simple and complex (mixed) adenocarcinoma; and ductal, solid-cystic ductal, and clear cell ductal carcinoma. Lesions are generally solitary, frequently alopecic, and may be ulcerated. They occur most commonly on the legs in dogs, and on head, legs, and abdomen in cats. In general, these lesions are histologically similar to their benign counterparts, although they tend to be larger and less well circumscribed and have cytologic features of malignancy. Nuclei are larger and more pleomorphic; there may be loss of nuclear polarity, and nucleoli may be prominent. Mitotic activity varies. Atypical mitotic figures may be seen. Well-differentiated lesions do not produce a desmoplastic response, and lymphatic invasion is rare. Poorly differentiated variants are infiltrative, have ill-defined borders, more desmoplasia, and are often ulcerated. The myoepithelial component of the complex adenocarcinoma usually has a benign histologic appearance. However, in some cases, it predominates over the epithelial component. On rare occasions, both glandular and myoepithelial components demonstrate features of malignancy, and the tumor is referred to as an epitrichial gland carcinosarcoma or mixed malignant epitrichial gland tumor.
Ductal epitrichial carcinomas tend to have more desmoplasia, lymphatic invasion, and higher mitotic activity with mitotic atypia than secretory adenocarcinomas. In contrast to ductal adenomas, ductal carcinomas have more irregular infiltrative borders, larger nuclei, prominent nucleoli, larger areas of squamous metaplasia, and zones of necrosis. Solid-cystic epitrichial carcinomas only occur in cats and have a horizontal rather than vertical orientation. Clear cell epitrichial carcinomas (follicular stem cell carcinoma, clear cell hidradenocarcinoma, clear cell adnexal carcinoma) are composed of large polygonal cells in lobules and nests with zones of cystic degeneration. The neoplastic cells have moderate to abundant pale eosinophilic to finely vacuolated cytoplasm. Multinucleated cells are usually seen. Subtle tubules lined by 1-3 layers of cells are present. There is sparse to moderate stroma, and chondroid metaplasia may occur. Occasional nests of small mesenchymal cells consistent with follicular papillary bodies are identified in the stroma. Immunohistochemistry using specific cytokeratin such as CAM5.2, CK7/8, and CK13 may be necessary to support this diagnosis. Lymphatic invasion, regional lymph node, and pulmonary metastasis are reported.
Tumors of atrichial (eccrine) glands are extremely rare and occur only on the footpads of dogs and cats. These tumors are usually malignant, although a few adenomas are described. Lesions are usually poorly circumscribed, ulcerated, and may be seen as swollen pawpad(s) or digit(s). These are aggressive neoplasms that often recur locally and may metastasize rapidly to local lymph nodes. Pulmonary metastasis has been reported. Histologically, they are infiltrative, have desmoplastic stroma, and may invade bone and cause bone lysis. Neoplastic cells form tubular, acinar, cribriform, or papillary structures. Tumor cells are polygonal, have pale amphophilic or eosinophilic cytoplasm, large hyperchromatic nuclei, prominent nucleoli, high mitotic activity, and atypical mitotic figures.
Ceruminous glands can give rise to cysts, cystomatosis, adenomas, complex and mixed adenomas, and the malignant versions of these tumors (Fig. 6-153 ). Morphologic features are very similar to those described for the epitrichial (apocrine) gland counterpart, with the additional distinguishing feature of brown luminal secretions on H&E-stained sections. In addition, foci of tumor cells may be found within the overlying epithelium, and secondary inflammation is more common.
Figure 6-153.

Ceruminous (apocrine) cysts (black arrow) and cystadenoma (green arrow) on the pinna and ear canal of a cat.
Carcinoma of the apocrine glands of the anal sac is a rare neoplasm of dogs. These tumors occur as unilateral or bilateral masses ventrolateral to the anus. Paraneoplastic hypercalcemia occurs in 25-90% of cases and is associated with a shorter survival. Metastasis is primarily to regional lymph nodes but is also reported to occur in the lung, spleen, liver, and bone in 50-80% of cases. The tumor varies histologically from solid, rosette, to tubular types. The solid form consists of sheets of relatively monomorphic polygonal cells with scant eosinophilic cytoplasm and round to oval hyperchromatic nuclei. In the rosette form, tumor cells with peripheral nuclei are arranged radially, sometimes surrounding small amounts of eosinophilic secretory material (Fig. 6-154 ). The tubular arrangement has larger cells with abundant eosinophilic cytoplasm and hyperchromatic nuclei. Tubules are filled with eosinophilic secretions. These tumors are invasive and induce a desmoplastic response. Tumor growth is often directed inward through the pelvic canal so that a grossly visible perianal mass is seen in only ~50% of cases.
Figure 6-154.
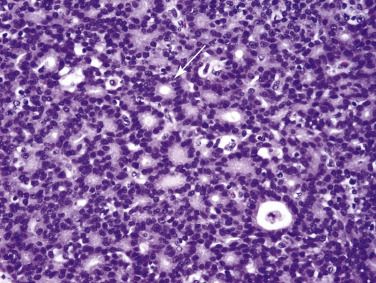
Carcinoma of the apocrine glands of the anal sac. Multifocally, neoplastic cells palisade around a central point or clear central lumen (rosettes) (arrow).
Further reading
Bettini G, et al. Central nervous system and lung metastasis of sebaceous epithelioma in a dog. Vet Dermatol 2009;20:289-294.
Carroll EE, et al. Malignant pilomatricoma in 3 dogs. Vet Pathol 2010;47:937-943.
De Lorimier L, Garrett LD. Neoplastic and non-neoplastic tumors. In: Miller WH, et al., editors. Muller & Kirk's Small Animal Dermatology. 7th ed. St Louis: Elsevier; 2013. p. 774-843.
Goldschmidt MH, et al. Histological Classification of Epithelial and Melanocytic Tumors of the Skin of Domestic Animals. Washington, DC: Armed Forces Institute of Pathology; 1998.
Gross TL, et al. Gross TL, et al., editors. Skin Diseases of the Dog and Cat: Clinical and Histopathological Diagnosis. 2nd ed. Oxford, UK: Blackwell; 2005. p. 562-603.
Gulbahar MY, et al. Mixed apocrine sweat gland tumor of the tail in a cow. Vet Pathol 2002;39:281-285.
Keyerleber MA, et al. Three-dimensional conformal versus non-graphic radiation treatment planning for apocrine gland adenocarcinoma of the anal sac in 18 dogs (2002-2007). Vet Comp Oncol 2012;10:237-245.
Marino DJ, et al. Evaluation of dogs with digit masses: 117 cases (1981-1991). J Am Vet Med Assoc 1995;207:726-728.
Saito S, et al. Melanocytic matricoma in a dog. Vet Pathol 2005;42:499-502.
Schulman FY, et al. Canine cutaneous clear cell adnexal carcinoma: histopathology, immunohistochemistry, and biologic behavior of 26 cases. J Vet Diagn Invest 2005;17:403-411.
Scott DW, Anderson WI. Canine hair follicle neoplasms: a retrospective analysis of 80 cases (1986-1987). Vet Dermatol 1991;2:143-150.
Melanocytic tumors
Tumors derived from melanocytes or melanoblasts are of neuroectodermal origin. They have been reported in most species of domestic animals and many wildlife species, although they are most common in dogs, horses, and some breeds of swine. There are some species differences in melanocytic tumors. In dogs, melanomas in the oral cavity and nonhaired skin of the lip have been historically cited as “almost invariably malignant”; however, newer studies have shown a subpopulation of oral and lip melanocytic neoplasms with a favorable prognosis. Tumors of the nailbeds also are frequently malignant, whereas cutaneous tumors are more commonly benign. In horses, melanomas occasionally occur as congenital tumors; however, they are most common in older gray horses, with a site predilection for the perineum, genital area, and distal limbs (Fig. 6-155 ). The behavior of melanomas in horses is difficult to predict based on histologic features. They can be clinically malignant and aggressive from the outset, or they may demonstrate slow growth for years with a sudden onset of malignant behavior, or growth can be slow for many years without evidence of metastasis. In some breeds of swine, such as Sinclair miniature swine and Hormel crosses (MeLiM strain, melanoma-bearing Libechov minipigs), melanomas can occur as congenital tumors, and these breeds have been extensively used in biomedical research. Melanomas are uncommon in cats and are often amelanotic. Melanomas in cattle may occur as a congenital lesion, or they may occur at any age. Most are benign in cattle, although occasional tumors are malignant. Melanocytic tumors are uncommon in goats and sheep and are generally pigmented.
Figure 6-155.

Melanoma on the prepuce of a horse.
(Courtesy P. Habecker.)
The histologic diagnosis of melanocytic tumors is complicated by the fact that they can display various degrees of pigmentation, from heavily pigmented to amelanotic. In addition, neoplastic melanocytes can be pleomorphic, and melanocytic tumors can display a variety of cell shapes, including spindle cell, balloon cell (clear cell), epithelioid cell, and signet-ring cell, thus making them difficult to distinguish from poorly differentiated sarcomas and carcinomas. Junctional activity can be helpful in identification (Fig. 6-156 ), because the only other tumors to display this activity are epitheliotropic lymphoma, and rarely, cutaneous histiocytomas and mast cell tumors. The advances in development of immunohistochemical detection of melanocytic markers has aided greatly in diagnosis of these tumors, particularly in the diagnosis of amelanotic melanomas. Although antibodies against vimentin, S-100, and neuron-specific enolase are sensitive for tumors of melanocytic origin, they are not specific for these tumors and react with many other tumors. For tumor cell specificity and sensitivity, the current recommendation is to perform immunohistochemical labeling with Melan-A, PNL2, TRP-1, and TRP-2 as single antibodies, or as a cocktail.
Figure 6-156.
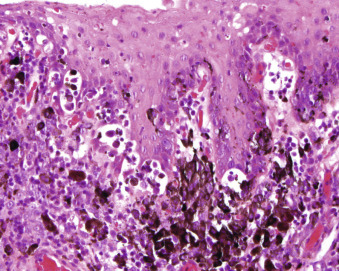
Junctional activity in a malignant melanoma.
The mitotic index (MI) is a key prognostic indicator for clinical behavior of canine melanocytic neoplasms, and it should be determined on all melanocytic tumors. The MI is determined by counting the number of mitotic figures in 10 consecutive high-power (400×) fields (HPFs), commencing in the area of highest mitotic activity for oral and lip neoplasms and in random fields for cutaneous neoplasms. Ulcerated regions should be avoided. Oral and lip tumors that are heavily pigmented and composed of well-differentiated melanocytes with a low mitotic index (<4/10 HPFs) have a favorable prognosis. Currently, Melan A is the most specific immunohistochemical marker for melanomas, albeit not 100% sensitive, and has been shown to be useful in many species, including the dog, cat, and horse. Dogs with cutaneous melanocytic neoplasms that have an MI of >3/10 HPFs are expected to have shorter survival times. Nuclear atypia, presence of ulceration, and deep infiltration beyond the dermis are also associated with a poor outcome, and readers are referred to the publication by Smedley (2011) for more detailed information and a thorough review of prognostic features.
Benign melanocytic tumors
Lentigo (lentigo simplex).
A lentigo is a proliferation of melanocytes that is usually confined to the epidermis, resulting clinically in a pigmented circumscribed macule. This lesion is considered to be a hyperplastic melanocytic lesion rather than neoplastic (see Disorders of pigmentation).
Melanocytoma (benign melanoma, melanocytic nevus).
Cutaneous melanocytomas are usually solitary, black, brown, or gray cutaneous nodules. Histologically, melanocytomas can be junctional (confined to the epidermis and dermoepidermal junction), compound (involving both epidermis and dermis), or dermal. Of these, the most common in domestic animals are compound and dermal melanocytomas. They are moderately circumscribed but not encapsulated and may be composed of any melanocytic cell type, that is, spindle, epithelioid, balloon cell (clear cell), or signet ring. Most commonly, they are composed of spindle cells, epithelioid cells, or a mixture of these cell types. The epithelioid cells often occur in nests in the dermis or in the epidermis and along the dermoepidermal junction, or in follicular epithelium. The spindle cell component may form whorls and fingerprint patterns in the dermis. The degree of pigmentation can vary, with the epithelioid cells commonly being darkly pigmented, and the spindle cells lightly pigmented or amelanotic. Mitotic figures are rare, and in the dog, a mitotic index of <3 is reported to predict benign behavior.
Balloon cell melanocytoma is a well-recognized variant in which the circumscribed dermal mass is composed of large epithelioid to polygonal cells with plentiful pale amphophilic to eosinophilic cytoplasm that has a faintly granular appearance. Fine melanin granules can sometimes be detected in low numbers of tumor cells. The nuclei are small, hyperchromatic, and uniform.
Melanocytoma-acanthoma (melanoacanthoma).
This tumor is composed of both melanocytic and epithelial cells. It is well described in humans but is rare in domestic animals and has been reported only in dogs. The tumors are seen as solitary pigmented nodules, generally ≤1 cm in diameter. Histologically, the tumor is a combination of a junctional melanocytoma with a benign epithelial tumor. The epithelial population forms a mass in the dermis composed of cords and nests with occasional small cystic structures containing keratin. Melanocytic cells form nests in the epidermis and sometimes in the cords of epithelial cells within the dermal mass; melanocytic spindle cells can form whorls and bundles between the epithelial cords and nests.
Malignant melanoma
Malignant melanomas are generally tumors of older animals; however, they have been reported in juvenile animals of many species. Criteria for malignancy and prognosis are described in the introduction to this section; in the dog, a mitotic index of 3 or greater appears to be the most accurate predictor of a poor prognosis. In addition, several studies have indicated that the degree of pigmentation and the histologic pattern are not correlated with prognosis. Malignant melanomas can be composed of a variety of cell morphologies, including spindle cells, epithelioid cells, a mixture of spindle cells and epithelioid cells, signet-ring cells, or balloon cells (clear cells). In addition, the cells can be heavily pigmented or amelanotic and form bundles, sheets, nests, and whorled patterns. Focal areas of chondroid or osseous metaplasia within the tumor may be seen on rare occasion. The most common types of malignant melanoma are composed of epithelioid cells, a mixture of epithelioid and spindle cells, or spindle cells alone, forming an unencapsulated mass in the dermis or subcutis. Various degrees of junctional activity may be present in the epithelioid cell form and in the mixed epithelioid-spindle cell form. The epithelioid cells tend to form clusters and nests, and the spindle cells tend to form sheets, bundles, or whorls. The neoplastic cells have variable nuclear pleomorphism, usually single prominent basophilic nucleoli, 3 or more mitotic figures per 10 HPFs (400×), and mitotic atypia (Fig. 6-157 ). Cytoplasm is generally moderate to abundant, and the degree of pigmentation is highly variable, from darkly pigmented to amelanotic. An infrequent form of spindle cell melanoma, composed entirely of amelanotic spindle cells, can be impossible to distinguish from fibrosarcoma or neurofibrosarcoma without the aid of immunohistochemistry. Although the epithelioid and spindle cell forms of melanoma are usually pigmented to some degree, the uncommon balloon cell form and signet-ring cell form are usually unpigmented or poorly pigmented.
Figure 6-157.
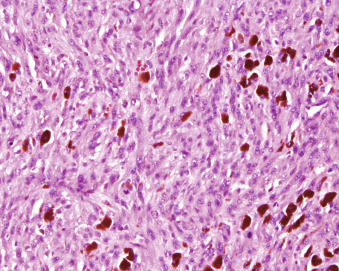
Malignant melanoma on the haired skin of a dog with prominent nuclei and mitotic figures.
Balloon cell malignant melanomas are dermal masses that are sometimes multilobulated, and exhibit no junctional activity. The cells are large, with large vesicular nuclei, prominent nucleoli, a relatively low mitotic index, and plentiful clear cytoplasm without visible melanin. Rare cells may have fine pale cytoplasmic dust-like granules. Occasional multinucleated cells can be present.
Signet-ring malignant melanomas are composed of round to polygonal cells that have eccentric nuclei compressed by abundant faintly eosinophilic or amphophilic cytoplasm that is not visibly pigmented. Occasional cells have fine pale brown granules. Nucleoli are prominent. Occasional multinucleated cells can be present.
Further reading
Aronsohn MG, Carpenter JL. Distal extremity melanocytic nevi and malignant melanomas in dogs. J Am Anim Hosp Assoc 1990;26:605-612.
Bolon B, et al. Characteristics of canine melanomas and comparison of histology and DNA ploidy to their biologic behavior. Vet Pathol 1990;27:96-102.
Campagne C, et al. Canine melanoma diagnosis: RACK1 as a potential biological marker. Vet Pathol 2013;50:1083-1090.
Chenier S, Dore M. Oral malignant melanoma with osteoid formation in a dog. Vet Pathol 1999;36:74-76.
Espinosa de Los Monteros A, et al. Immunohistopathologic characterization of a dermal melanocytoma-acanthoma in a German Shepherd dog. Vet Pathol 2000;37:268-271.
Fleury C, et al. The study of cutaneous melanomas in Camargue-type grayskinned horses (1): clinical-pathological characterization. Pigment Cell Res 2000;13:39-46.
Horak V, et al. Hereditary melanoblastoma in miniature pigs and its successful therapy by devitalization technique. Cell Mol Biol 1999;45:1119-1129.
Jiang L, et al. Constitutive activation of the ERK pathway in melanoma and skin melanocytes in Grey horses. BMC Cancer 2014;14:857.
Löhr CV. One hundred two tumors in 100 goats (1987-2011). Vet Pathol 2013, 50:668-675.
Miller MA, et al. Cutaneous melanocytomas in 10 young cattle. Vet Pathol 1995;32:479-484.
Miller WH, et al. Feline cutaneous melanocytic neoplasms: a retrospective analysis of 43 cases (1979-1991). Vet Dermatol 1993;4:19-26.
Munday JS, et al. Cutaneous malignant melanoma in an 11-month-old Russian blue cat. N Z Vet J 2011;59:143-146.
Okomo-Adhiambo M, et al. Gene expression in Sinclair swine with malignant melanoma. Animal 2012;6:179-192.
Oliveira FN, et al. Cutaneous mast cell tumor with epitheliotropism in 3 dogs. Vet Pathol 2013;50:234-237.
Patnaik AK, Mooney S. Feline melanoma: a comparative study of ocular, oral, and dermal neoplasms. Vet Pathol 1988;25:105-112.
Phillips JC, Lembcke LM. Equine melanocytic tumors. Vet Clin North Am Equine Pract 2013;29:673-687.
Ramos-Vara JA, et al. Retrospective study of 338 canine oral melanomas with clinical, histologic, and immunohistochemical review of 129 cases. Vet Pathol 2000;37:597-608.
Roels S, et al. PCNA and Ki67 proliferation markers as criteria for prediction of clinical behaviour of melanocytic tumours in cats and dogs. J Comp Pathol 1999;121:13-24.
Roels S, et al. Proliferation, DNA ploidy, p53 overexpression and nuclear DNA fragmentation in six equine melanocytic tumours. J Vet Med 2000;47:439-448.
Smedley RC, et al. Prognostic markers for canine melanocytic neoplasms: a comparative review of the literature and goals for future investigation. Vet Pathol 2011;48:54-72.
Smith SH, et al. A comparative review of melanocytic neoplasms. Vet Pathol 2002;39:651-678.
Trappler MC, et al. Scrotal tumors in dogs: a retrospective study of 676 cases (1986-2010). Can Vet J 2014;55:1229-1233.
Tuohy JL, et al. Outcome following curative-intent surgery for oral melanoma in dogs: 70 cases (1998-2011). J Am Vet Med Assoc 2014;245:1266-1273.
Valentine BA. Equine melanocytic tumors: a retrospective study of 53 horses (1988 to 1991). J Vet Intern Med 1995;9:291-297.
van der Linde-Sipman JS, et al. Cutaneous malignant melanomas in 57 cats: identification of (amelanotic) signet-ring and balloon cell types and verification of their origin by immunohistochemistry, electron microscopy, and in situ hybridisation. Vet Pathol 1997;34:31-38.
Yeruham I, et al. Congenital skin neoplasia in cattle. Vet Dermatol 1999;10:149-156.
Spindle cell tumors
Tumors arising from spindle-shaped cells of the skin are common in dogs and cats, sporadic in horses, and uncommon to rare in other domestic species. Classification of these tumors may be difficult, and the nomenclature is inconsistent and controversial. The tumors are classified according to the mature tissue they resemble, but histologic differences are frequently subtle, and morphologic appearance may not be specific enough to reflect histogenesis, particularly for malignant spindle cell tumors. Consequently, accurate diagnosis by morphologic features alone may not be possible for many tumors. An immunohistochemical study of canine cutaneous fibrosarcoma, hemangiopericytoma, and schwannoma found poor correlation between morphologic diagnosis and tumor cell differentiation. Although electron microscopy and immunohistochemistry may be helpful in determining the line of differentiation exhibited by tumor cells, some tumors defy identification because of conflicting results because of loss or alteration in antigens normally present or acquisition of novel antigens. Classification of spindle cell neoplasms is considered important because of the expectation that it will provide a prediction of the biological behavior of the tumor. Exact identification of spindle cell sarcomas of the skin may not be essential, however, because most soft tissue spindle cell tumors exhibit similar behavior and prognosis. The tumors are typically locally invasive, recur frequently after surgical excision, but metastasize infrequently. On gross examination, soft tissue sarcomas can appear well circumscribed or even encapsulated; however, finger-like microextensions of tumor may commonly infiltrate into the surrounding tissue to give rise to satellite lesions that are not visible grossly. The apparent tumor circumscription commonly results in incomplete excision, leaving microscopic foci of tumor tissue that result in recurrence. Wide surgical excision may be curative, however. Because determination of adequacy of excision is prognostic, surgical margins should be marked.
The proposed grading system for soft tissue sarcomas is based on the combination of 3 morphologic features: differentiation score (i.e., how well the sarcoma resembles normal tissue (1-3 with the higher number being poorly differentiated), mitotic index (scores 1-3), and tumor necrosis (0-2). A grade of I, II, or III is assigned by the total score of each category (i.e., ≤3 for grade 1; 4-5 for grade II; ≥6 for grade III). The grading system is useful for predicting which neoplasms are likely to recur and metastasize. For any grade, tumors with complete margins are unlikely to recur. Grade III tumors with close surgical margins are likely to recur, whereas grade I tumors infrequently recur, and grade II have an intermediate risk of recurrence. Metastasis is very rare for grade 1 tumors, rare to infrequent for grade II, and grade III tumors have an increased risk. The reader is referred to the Dennis, et al., 2011 reference for more information.
The mitotic index is more important than the tumor type in predicting the biologic behavior of most soft tissue sarcomas in dogs.
Benign spindle cell tumors
Skin tags (fibrovascular papilloma, acrochordon, skin polyp) are benign, fibrovascular lesions of middle-aged and older dogs that may be a proliferative response to trauma or inflammation rather than actual neoplasms. They are solitary or multiple; soft, polypoid, or filiform; hairless masses up to 1 cm in diameter and 2-3 cm long that occur most commonly on the trunk, sternum, and bony prominences of the limbs. Microscopically, skin tags are composed of mature collagenous tissue that is more highly vascular than normal dermis and covered by an irregularly hyperplastic, hyperkeratotic, and hyperpigmented epidermis. Adnexal structures are absent, and mononuclear inflammatory cells may be present in low numbers. Ulceration and neutrophilic inflammation are common sequelae to trauma.
Collagenous hamartomas (collagen nevi) are focal nodular accumulations of excessive dermal collagen that are relatively common in middle-aged and older dogs. They are typically solitary, alopecic, firm, dome-shaped nodules up to 1 cm in diameter. Microscopically, they are composed of haphazardly arranged bundles of collagen and low numbers of mature fibroblasts that entrap adnexal structures and result in their distortion or atrophy. Collagenous hamartomas are usually located in the dermis, but large masses may extend into the subcutis. The primary differential is fibroma, which tends to be larger and located deeper in the dermis, displaces and compresses adjacent structures, and is more cellular than a collagenous hamartoma. Some veterinary pathologists believe that collagen hamartomas are actually fibromas of low cellularity.
A syndrome called nodular dermatofibrosis, characterized by multiple cutaneous collagenous hamartomas, has been reported as a marker of renal epithelial neoplasia in German Shepherd dogs (see also the previous section Cutaneous paraneoplastic syndromes).The condition is thought to be inherited in an autosomal dominant manner. Affected dogs are adults, and most have bilateral renal cystadenocarcinomas. Nodules may number in the hundreds and are located anywhere on the body. Individual cases in several other breeds have also been reported. Histologically, the lesions are similar to collagen hamartomas and are differentiated primarily on the basis of the large number of lesions present and the breed affected.
Fibromas are uncommon benign tumors of fibroblasts and collagen that occur in adult and aged animals of all species. Fibromas are usually solitary, soft to firm, well-circumscribed, round, dome-shaped, or pedunculated masses that vary from 1-50 cm in diameter. They are usually alopecic and may be hyperpigmented. Large tumors may be ulcerated secondary to trauma. Microscopically, fibromas are well-circumscribed, nonencapsulated, dermal or subcutaneous nodules composed of fibroblasts and abundant collagen. The fibroblasts have uniform, oval to elongate, bland nuclei that may be slightly larger than fibroblasts in the normal dermis and have fine chromatin, inconspicuous nucleoli, and rare mitotic figures. The cytoplasm merges imperceptibly with collagen that is arranged in whorls and interwoven bundles that are thicker and more dense than those in the normal dermis. Adnexal structures are usually displaced and compressed peripherally. Some tumors contain substantial amounts of mucinous or myxomatous matrix material in addition to the collagen, in which case the term fibromyxoma may be used. In contrast to collagenous hamartomas, fibromas are typically larger, more highly cellular, and displace rather than incorporate adnexal structures.
Myxomas (myxofibromas) are rare cutaneous neoplasms arising from fibroblasts or multipotential mesenchymal cells and containing abundant glycosaminoglycan stroma. They usually occur in adult or aged animals as solitary, infiltrative, soft masses that are poorly circumscribed and may extend along fascial planes. The tissue is pale and exudes clear viscous fluid on cut surface. A report of a myxoma developing at the site of a subcutaneously implanted pacemaker in a dog raised the question of whether the implant may have induced the tumor. Microscopically, myxomas are nonencapsulated dermal or subcutaneous masses composed of small stellate to spindle cells randomly distributed within abundant basophilic mucinous stroma with scant, fine collagen fibers. Cellularity is typically low, and the cells have small hyperchromatic nuclei and rare mitotic figures. Recurrence is common because of the infiltrative growth pattern. Myxomas are difficult to differentiate from myxosarcomas because both are poorly circumscribed, locally infiltrative, and have low mitotic activity. However, nuclear and cellular pleomorphism is more apparent, and atypical mitotic figures may be seen in myxosarcomas.
Locally infiltrative and malignant spindle cell tumors
Canine perivascular wall tumors (PWTs) are mesenchymal neoplasms that were previously referred to as hemangiopericytomas. The tumors are relatively common, histologically distinctive spindle cell tumors of dogs. The nomenclature was changed to reflect the origin of the tumor (i.e., derived from components of the vascular wall but not the endothelium). The category of PWT includes the following: glomus tumor, true hemangiopericytoma, angioleiomyoma/sarcoma, angiomyofibroblastoma, and angiofibroma. A large battery of immunohistochemical stains is necessary to differentiate the subtypes, but is generally not needed. All PWTs have similar biological behaviors, and are infiltrative, often invading along fascial planes, and are commonly recurrent; metastasis is uncommon. Increased cellular pleomorphism is seen with each subsequent recurrence. Occasional tumors with similar microscopic features are seen in horses and cats The tumors usually occur on the limbs of older dogs of either sex and any breed but are most common in large-breed (>30 kg) dogs. They are usually solitary, slow-growing, multinodular masses that appear grossly well circumscribed and measure up to 25 cm in diameter. The tissue is usually pale, and the consistency varies from soft to very firm. The tumors frequently recur following excision because of the difficulty in identifying tumor margins and inability to perform wide surgical excision because of anatomic constraints. Metastasis is uncommon, however.
Perivascular wall tumors are usually located in the dermis and subcutis and are primarily composed of uniform plump spindle cells with oval nuclei, fine chromatin, and small central nucleoli. The characteristic microscopic feature of PWTs is plump spindle cells arranged in concentric layers to form whorls, sometimes with small vessels within the centers (Fig. 6-158 ). Sheets and interlacing bundles of similar spindle cells, occasional polygonal cells and multinucleated cells, and variable amounts of collagen also comprise most tumors. Densely cellular areas alternate with loose, myxomatous-appearing areas. Aggregates of lymphocytes may be scattered within some tumors and are usually most prominent along the periphery. At the margins of the tumor, finger-like microextensions of tumor cells commonly infiltrate along fascial planes and are the reason many tumors are incompletely excised despite the clinical impression that they are well circumscribed.
Figure 6-158.
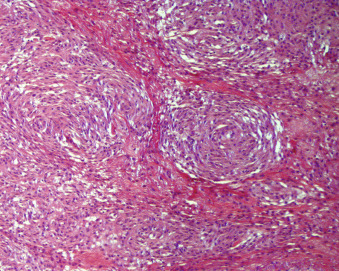
Perivascular wall tumor (“hemangiopericytoma”) in a dog. Note the plump spindle cells arranged in concentric layers to form whorls, sometimes with small vessels within the centers.
Recent investigations in the prognosis of perivascular wall tumors has aided the ability to predict behavior. The tumors fall into 1 of 3 prognostic profiles. Profile 1 are tumors on the limbs that exhibit expansile growth in the subcutis. Limb tumors with incomplete or close surgical margins have an intermediate risk of recurrence. Profile 2 includes tumors that not located on extremities that exhibit infiltrative growth or satellite nodules that extend to skeletal muscle. Profile 2 tumors with incomplete or close margins have a high risk of recurrence. Profile 3 tumors are similar to profile 2, except that the tumor depth reaches only to the subcutis and not to the depth of skeletal muscle. Profile 3 tumors have a low risk of recurrence with any margins (complete, incomplete, close). The size of the tumors has been associated with increased relapse probability. Dogs with tumors >5 cm were about 6 times greater to relapse than dogs with tumors <5 cm. Fortunately, cases in any profile with complete surgical margins typically do not recur. For more information, see Avallone et al., 2014. PWTs should be differentiated from fibrosarcomas, rhabdomyosarcomas, and hemangiosarcomas.
Cutaneous tumors of neural origin are uncommon in domestic animals but are likely under-diagnosed because of their histologic similarity to other more common tumors of the skin. They can be composed of one or more elements of a nerve, that is, axon, Schwann cell, and perineurial fibroblast. Consequently, these tumors are histologically heterogeneous, and the histogenesis is frequently uncertain, resulting in various and confusing classifications and terminologies in the literature. They have been called neurofibromas/neurofibrosarcomas, neurilemmomas, neurinomas, and schwannomas/malignant schwannomas. The name peripheral nerve sheath tumor is a broad term proposed to include all tumors arising from peripheral nerves; however, because most tumors are composed of Schwann cells, the term schwannoma is appropriate for the majority of the tumors. Both benign and malignant forms occur; however, tumors that appear histologically benign commonly recur. Schwannomas are common in cattle but occur primarily in the heart and rarely involve the skin. A condition termed neurofibromatosis has been observed in cattle of all ages and may occur congenitally. It is characterized by multiple neural tumors that usually involve deep nerves and viscera but sometimes also the skin.
Cutaneous peripheral nerve sheath tumors are usually solitary, well-circumscribed, slow-growing, soft to firm nodules in middle-aged to aged animals. In cats, the head and distal limbs may be involved most frequently. Schwannomas are usually subcutaneous in dogs; in cats, they may be confined to the dermis. Microscopically, schwannomas are most commonly composed of small spindle cells characterized by oval, spindle-shaped, or wavy nuclei; fine chromatin; small inconspicuous nucleoli; and pale indistinct cytoplasm. The spindle cells form whorls, interlacing fascicles, and palisades reminiscent of nerve (Fig. 6-159 ). A delicate collagenous stroma is moderately abundant, and a mucinous matrix may be prominent in some tumors. Delicate finger-like projections of tumor cells commonly extend into adjacent tissues and between fascial planes, accounting for frequent recurrences. Cellularity is increased, cellular pleomorphism is more prominent, and there is a decreased tendency to form whorls and palisades in malignant tumors. Mitotic figures are uncommon in benign tumors but may be moderately numerous in malignant peripheral nerve sheath tumors. Histologically and behaviorally, peripheral nerve sheath tumors may be difficult to differentiate from fibromas, well-differentiated fibrosarcomas, and PWTs. However, neural tumors express S-100 protein, myelin basic protein, neuron-specific enolase, and glial fibrillary acidic protein, whereas the other more common cutaneous tumors do not. In dogs, malignant peripheral nerve sheath tumors may arise within the peripheral nervous system (PNS) or within non-PNS soft tissue. It is important to distinguish those tumors arising within peripheral nerves from non-PNS nerve sheath tumors, as the former have a poor prognosis. Tumors arising within peripheral nerves have been shown to have higher S-100 and Olig 2 expression than peripheral nerve sheaths tumors arising in soft tissue. Immunohistochemical staining of granular cell tumors (granular cell myoblastomas) has demonstrated S-100 protein, myelin basic protein, and neuron-specific enolase within tumor cells, suggesting that they also represent a form of peripheral nerve sheath tumor.
Figure 6-159.
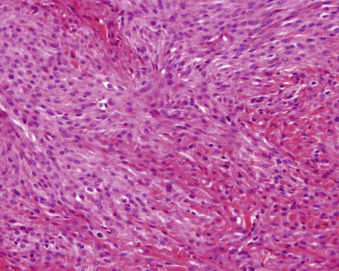
Peripheral nerve sheath tumor taken from the ear of a cat.
Traumatic neuroma (tail dock neuroma, amputation neuroma) is considered an exuberant but non-neoplastic proliferation of the proximal nerve stump occurring in response to injury or surgery. In veterinary medicine, this lesion is rare and occurs most frequently as a result of tail docking in dogs. The tumors develop in young dogs, usually within 1 year after caudectomy. They are typically painful, self-traumatized, alopecic, hyperpigmented, lichenified lesions adherent to the underlying deep tissues at the tip of the tail. Microscopically, traumatic neuromas are well-circumscribed nodules composed of haphazardly arranged myelinated nerve bundles of variable size randomly distributed within a relatively abundant connective tissue stroma.
Fibrosarcomas are malignant tumors of fibroblasts that show no other evidence of cell differentiation. They commonly recur and may metastasize. Fibrosarcomas are undoubtedly over-diagnosed, as virtually any anaplastic highly cellular spindle cell sarcoma containing collagen is diagnosed as a fibrosarcoma when more specific histogenesis is not apparent. However, as immunohistochemistry has become a routine technique in most diagnostic laboratories, fibrosarcoma can be separated from other spindle cell tumors, such as peripheral nerve sheath tumor, leiomyosarcoma, rhabdomyosarcoma, amelanotic malignant melanoma, spindle cell carcinoma, and others.
Fibrosarcomas are common in dogs and cats and uncommon in other domestic species. In dogs, they usually occur in older animals and are most common on the trunk and limbs. They usually arise in the subcutis and are poorly circumscribed masses of variable size that may be soft to firm in consistency. Large tumors are often ulcerated and alopecic. Most canine fibrosarcomas are low-grade malignancies that commonly recur locally and metastasize infrequently. Similarities have been noted between canine fibrosarcomas from presumed injection sites and feline postvaccinal fibrosarcomas, suggesting that postinjection sarcomas may also occur in dogs.
Fibrosarcoma is the most common malignant mesenchymal tumor of cats, and 3 forms of fibrosarcoma have been recognized: virus-induced, solitary in older cats, and postvaccinal.
Virus-induced fibrosarcoma is rare. Feline sarcoma virus (FeSV) is the cause of multicentric fibrosarcoma in cats usually <5 years of age. FeSV is a replication-defective retrovirus that requires Feline leukemia virus (FeLV) as a helper virus. The genetic recombination of the 2 viruses produces an acutely transforming virus that induces multiple simultaneous rapidly growing fibrosarcomas after a short incubation period. FeSV-induced fibrosarcomas are typically locally invasive and metastasize to lung and other sites.
Solitary fibrosarcomas in older cats are much more common than virus-induced multicentric tumors. These may arise in the dermis or subcutis. Subcutaneous tumors are usually on the trunk and limbs; dermal tumors primarily involve the digits and pinnae. The clinical appearance and behavior of this type of fibrosarcoma are similar to those in dogs.
Epidemiologic evidence supports a relationship between vaccine administration in cats and the development of postvaccinal fibrosarcomas and, to a lesser extent, other sarcomas in injection sites. Vaccination site fibrosarcomas have also been reported in ferrets and putatively in dogs. The interval between vaccination and tumor development is 3 months to 3.5 years. The mechanism of tumor development is unknown, but persistent injection-site–induced inflammation leading to deranged fibrous connective tissue repair response and eventual neoplastic transformation in genetically predisposed cats has been postulated. Alterations in oncogene and growth factor expression may be involved in the pathogenesis. Postvaccinal fibrosarcomas typically develop in the subcutis of the dorsal cervical and interscapular area, dorsal and lateral thorax, flank, and musculature of the thigh, locations that are all common vaccination sites. These tumors arise in cats that are younger (median age 8 years) than those with fibrosarcomas at nonvaccination sites (median age 10.5 years) and are larger than nonvaccination site fibrosarcomas. The masses frequently have cystic centers, firm attachments to dorsal spinous processes or other deep structures, and ill-defined margins. They are biologically aggressive and commonly recur multiple times within a period of weeks to months when removed. The metastatic rate is not well characterized, but was found to be as high as 24% in one study. The lungs and regional lymph nodes are the most common sites of metastasis. Wide surgical excision prolongs the interval to recurrence but often fails to remove the tumor completely. Radiation therapy and chemotherapy are under evaluation as adjunctive treatment to prevent local recurrence and systemic spread, respectively.
Microscopically, fibrosarcomas consist of interlacing and intersecting bundles of immature fibroblastic cells. The tumors show a great deal of variation with respect to cellular pleomorphism and density, mitotic activity, and amount and maturity of collagen. Multinucleated giant cells are seen in many fibrosarcomas but are not numerous. The tumors are dermal, subcutaneous, or both. They are usually nonencapsulated, and local invasion is evident as finger-like projections of tumor cells extending along fascial planes and into surrounding tissues. These microscopic extensions of the tumor account for the difficulty in excising the tumor completely and resultant recurrences. Although collagen is the primary stromal element, mucin may also be produced in small amounts. Immunohistochemical staining is positive for vimentin only. Retrospective studies have found only the mitotic index (total number of mitotic figures in 10 [400×] HPFs) to be significant in predicting tumor behavior. In dogs, a mitotic index <9 was associated with greater survival than a mitotic index of 9 or greater. Likewise, cats with solitary fibrosarcomas with a mitotic index of 5 or less had significantly greater survival time than cats with tumors with mitotic index of 6 or greater. Poorly differentiated fibrosarcomas may be difficult to differentiate from a number of other mesenchymal and nonmesenchymal tumors, including malignant schwannoma, malignant fibrous histiocytoma, leiomyosarcoma, and spindle cell forms of amelanotic melanoma and squamous cell carcinoma. In such cases, immunohistochemical staining is necessary to exclude other tumors by showing lack of immunoreactivity to antigens typical of other cell types. In small biopsies with a limited amount of tissue to evaluate, it may be difficult to differentiate fibrosarcoma from reactive granulation tissue.
Postvaccinal fibrosarcomas are typically subcutaneous and have large cavitated centers as a result of extensive necrosis. An inflammatory reaction, consisting of lymphocytes and macrophages that sometimes contain gray-brown or blue globular material typical of a vaccine reaction, is commonly present at the periphery of the tumor. Mitotic activity and cellular pleomorphism tend to be high. Tumor cells of vaccination-site fibrosarcomas have been reported to be consistently strongly immunoreactive for platelet-derived growth factor and its receptor, epidermal growth factor and its receptor, and transforming growth factor-β, whereas non–vaccine-associated fibrosarcomas are negative or only slightly positive.
Undifferentiated pleomorphic sarcoma (malignant fibrous histiocytoma, giant cell tumor of soft parts, extraskeletal giant cell tumor) is an uncommon tumor of controversial histogenesis. It was originally believed to be derived from malignant cells of monocyte-macrophage origin capable of acting as “facultative” fibroblasts. Ultrastructural and immunohistochemical findings, however, indicate that malignant fibrous histiocytoma may not be a distinct entity but rather a collection of anaplastic mesenchymal and nonmesenchymal tumors. Historically, the diagnosis of malignant fibrous histiocytoma was made for those neoplasms characterized histologically by the combination of fibroblast-like spindle cells, vacuolated histiocyte-like cells, and variable numbers of pleomorphic multinucleated giant cells, along with a collagenous stroma. The tumors may now be classified into specific soft tissue tumors (e.g., histiocytic sarcoma) or pleomorphic undifferentiated sarcoma.
Other mesenchymal tumors
Tumors arising from subcutaneous lipocytes occur in all species. Lipomas are most common in dogs and may be multiple. In all species, they usually occur in adult and aged animals and are most commonly located on the trunk and proximal limbs. Lipomas are masses of well-differentiated lipocytes indistinguishable from normal fat, except for a compressed boundary of delicate stroma that normally serves to delineate the margin between tumor and adjacent normal adipose tissue. Some lipomas contain cartilage, bone, collagen, or blood vessels. In addition, some mesenchymal tumors contain roughly equal proportions of adipose tissue mixed with other mesenchymal components. These form distinctive variants, such as angiolipomas, fibrolipomas, and leiomyolipomas. Occasionally, hemangiosarcomas and mast cell tumors may be found arising within lipomatous masses, suggesting that lipomas may sometimes provide a local environment suitable for the emergence of these more sinister neoplasms. Necrosis, hemorrhage, fibrosis, and mild macrophage inflammation may occur as a result of trauma to lipomas.
Infiltrative lipomas are uncommon tumors of dogs. They are usually large, poorly delineated, deep subcutaneous masses composed of well-differentiated lipocytes that infiltrate subcutaneous muscle and fascia. They may cause pain or interfere with limb function and may invade through the body wall.
Liposarcomas are malignant tumors of lipocytes and are uncommon in all species. Liposarcomas in cats have been associated with retrovirus infection and with vaccination sites; a liposarcoma in a dog was associated with a glass foreign body. Liposarcomas may recur but rarely metastasize. They are usually well-circumscribed, nonencapsulated, highly cellular masses of round to polyhedral cells primarily and fewer stellate, spindle, and multinucleated cells. Lipocyte origin is recognized by the presence of cytoplasmic vacuolation that may be numerous fine vacuoles or a single large clear vacuole that displaces the nucleus peripherally. Mitotic figures are generally infrequent. Myxoid liposarcomas have prominent mucinous ground substance. Liposarcomas may be difficult to differentiate from anaplastic sebaceous carcinomas and balloon cell or clear cell melanomas. The tumor cells of liposarcoma are usually arranged in solid sheets of vacuolated cells, whereas in sebaceous carcinoma, the cells tend to be subdivided into nests and lobules. The presence of rare cells with cytoplasmic dusting of very fine brown granules can differentiate melanoma from the other 2 tumors; however, immunohistochemical staining for cytokeratin, vimentin, and a melanocytic marker (such as Melan A) may be needed to differentiate the tumors.
Tumors originating from muscle are rare in the skin of animals. Smooth muscle tumors, leiomyomas and leiomyosarcomas, can arise from arrector pili muscles (piloleiomyomas), cutaneous blood vessels (angioleiomyomas), and specialized muscles of genital skin. These tumors are usually solitary, firm, and well-circumscribed in animals. In humans, piloleiomyomas are commonly multiple; and multiple piloleiomyomas have been reported in an old cat. Microscopically, leiomyomas are small, well-circumscribed dermal masses adjacent to and surrounding hair follicles. They are composed of uniform long spindle cells in whorling and interlacing bundles. The cells have bland elongate nuclei with blunt ends (“cigar-shaped”) and moderately abundant pale eosinophilic cytoplasm. Mitotic figures are rare. Leiomyosarcomas exhibit nuclear pleomorphism and low to moderate mitotic activity. Angioleiomyomas consist of interlacing bundles of smooth muscle cells between numerous vascular channels. Smooth muscle tumors may be confused with fibromas, fibrosarcomas, or malignant schwannomas. In such cases, immunohistochemical staining for actin and desmin can confirm muscle origin.
Cutaneous tumors of skeletal muscle, rhabdomyomas and rhabdomyosarcomas, are extremely rare. Rhabdomyomas of the ear pinna have been reported in 4 white-eared cats. The tumors were thinly haired, red-purple, nonulcerated discoid nodules 1-2 cm in diameter on the convex surface of the pinna. Histologically, they were well-circumscribed masses composed of whorls and bundles of long spindle cells with cross-striations evident in a few tumor cells. Mitotic figures were rare. Surgical excision was curative.
Further reading
Avallone G, et al. Canine perivascular wall tumors: high prognostic impact of site, depth, and completeness of margins. Vet Pathol 2014;51:713-721.
Avallone G, et al. The spectrum of canine cutaneous perivascular wall tumors: morphologic, phenotypic and clinical characterization. Vet Pathol 2007;44:607-620.
Bostock DE, Dye MT. Prognosis after surgical excision of canine fibrous connective tissue sarcomas. Vet Pathol 1980;17:581-588.
Choi H, et al. Undifferentiated pleomorphic sarcoma (malignant fibrous histiocytoma) of the head in a dog. J Vet Med Sci 2011;73:235-239.
Dennis MM, et al. Prognostic factors for cutaneous and subcutaneous soft tissue sarcomas in dogs. Vet Pathol 2011;48:73-84.
Esplin DG, et al. Metastasizing liposarcoma associated with a vaccination site in a cat. Fel Pract 1996;24:20-23.
Finnie JW, et al. Multiple piloleiomyomas in a cat. J Comp Pathol 1995;113:201-204.
Hendrick MJ. Feline vaccine-associated sarcomas. Cancer Invest 1999;17:273-277.
Jones BR, et al. Nerve sheath tumours in the dog and cat. N Z Vet J 1995;43:190-196.
Kim DY, et al. Malignant peripheral nerve sheath tumor with divergent mesenchymal differentiations in a dog. J Vet Diagn Invest 2003;15:174-178.
Kuntz CA, et al. Prognostic factors for surgical treatment of soft-tissue sarcomas in dogs: 75 cases (1986-1996). J Am Vet Med Assoc 1997;211:1147-1151.
Kuwamura M, et al. Canine peripheral nerve sheath tumor with eosinophilic cytoplasmic globules. Vet Pathol 1998;35:223-226.
McCarthy PE, et al. Liposarcoma associated with a glass foreign body in a dog. J Am Vet Med Assoc 1996;209:612-614.
Miller MA, et al. Cutaneous neoplasia in 340 cats. Vet Pathol 1991;28:389-395.
Morris JS, et al. Immunohistochemical and histopathologic features of 14 malignant fibrous histiocytomas from Flat-Coated Retrievers. Vet Pathol 2002;39:473-479.
Munday JS, et al. Histology and immunohistochemistry of seven ferret vaccination-site fibrosarcomas. Vet Pathol 2003;40:288-293.
Pace LW, et al. Immunohistochemical staining of feline malignant fibrous histiocytomas. Vet Pathol 1994;31:168-172.
Pérez J, et al. Immunohistochemical characterization of hemangiopericytomas and other spindle cell tumors in the dog. Vet Pathol 1996;33:391-397.
Roth L. Rhabdomyoma of the ear pinna in four cats. J Comp Pathol 1990;103:237-240.
Rowland PH, et al. Myxoma at the site of a subcutaneous pacemaker in a dog. J Am Anim Hosp Assoc 1991;27:649-651.
Sartin EA, et al. Invasive malignant fibrous histiocytoma in a cow. J Am Vet Med Assoc 1996;208:1709-1710.
Schulman FY, et al. Feline cutaneous fibropapillomas: clinicopathologic findings and association with papillomavirus infection. Vet Pathol 2001;38:291-296.
Stefanello D, et al. Canine cutaneous perivascular wall tumors at first presentation: clinical behavior and prognostic factors in 55 cases. J Vet Intern Med 2011;25:1398-1405.
Vascellari M, et al. Fibrosarcomas at presumed sites of injection in dogs: characteristics and comparison with non-vaccination site fibrosarcomas and feline post-vaccinal fibrosarcomas. J Vet Med A Physiol Pathol Clin Med 2003;50:286-291.
Waters CB, et al. Giant cell variant of malignant fibrous histiocytoma in dogs: 10 cases (1986-1993). J Am Vet Med Assoc 1994;205:1420-1424.
Williamson MM, Middleton DJ. Cutaneous soft tissue tumours in dogs: classification, differentiation, and histogenesis. Vet Dermatol 1998;9:43-48.
Vascular tumors
Cutaneous vasoformative tumors are common in dogs, occasional in cats and horses, and uncommon in other species. The majority are benign in dogs and horses, whereas malignant tumors are more common in cats. Vascular tumors may be associated with thrombocytopenia, disseminated intravascular coagulation, and other hemostatic abnormalities.
Hemangioma is a benign neoplasm of blood vessel endothelium that can originate in the dermis or subcutis. The tumor is usually a solitary, well-circumscribed, fluctuant to firm, blue to red-black, slow-growing mass. Cutaneous hemangioma in dogs usually occurs in older animals (mean, 9-10 years) without apparent sex predilection. The tumor can occur anywhere, but lightly pigmented, sparsely haired, ventral abdominal, and inguinal skin may be predisposed. Chronic solar damage has been suggested as a cause of dermal hemangiomas in this location, and they may be multiple. Surgical excision is curative.
Benign cutaneous vascular lesions in horses frequently occur in animals <1 year of age, and some are congenital, raising the question of whether the lesions are true neoplasms or vascular malformations (hamartoma or nevus). The confusion in categorizing these vascular lesions in young horses has resulted in inconsistent nomenclature, and they have been referred to as lobular capillary hemangioma and vascular nevus in the literature. The lesions are most commonly located on the limbs and occur as a cauliflower or nodular mass or diffuse skin thickening that may become alopecic and ulcerated. The lesions may recur following excision. In some instances, they are too extensive to be excised, necessitating euthanasia of the affected animal. Cutaneous hemangiomas usually occur in adult and aged cattle; congenital hemangiomas have been reported also, and these are frequently multiple.
Microscopically, hemangiomas consist of nonencapsulated dermal or subcutaneous masses composed of blood-filled channels lined by a single layer of flattened, mature endothelium (Fig. 6-160 ). Mitotic figures are rare. Subcutaneous tumors are usually well circumscribed, whereas those in the dermis may not be as well defined and may incorporate adnexal structures within the mass. The tumors are classified as capillary or cavernous, depending on the size of the vascular spaces. The cavernous type is more common in dogs. The vascular channels are usually separated by collagenous septa that contain variable numbers of mast cells, lymphoid cells, and hemosiderin-laden macrophages. Occasional vascular channels contain fibrin thrombi. Solar-induced dermal hemangiomas of glabrous skin are located in the superficial dermis and may be associated with solar elastosis.
Figure 6-160.
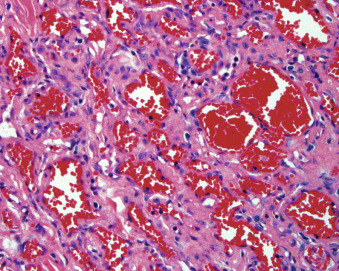
Cutaneous hemangioma in a dog.
A variant of hemangioma, called angiokeratoma, is a raised superficial dermal hemangioma with prominent, irregular hyperplasia of the epidermis that extends down to separate and partially surround the vascular channels. The lobular capillary hemangioma/vascular nevus of young horses consists of multiple discrete dermal lobules of closely packed, haphazardly arranged vascular structures of small caliber. The vessels are lined by endothelial cells with plump oval nuclei and low-mitotic activity.
Cutaneous angiomatosis is a vascular endothelial proliferative disorder, characterized by irregular blood-filled capillaries in the dermis and subcutis. Lesions can appear as red to purple macules, papules, nodules, or plaques. It occurs in cattle and horses most commonly and also is reported in dogs, cats, llamas, and goats. Bacillary angiomatosis caused by infection with Bartonella spp. has been described in an immunocompromised dog. Multisystem progressive angiomatosis affecting the skin, gastrointestinal tract, and visceral surface of the abdominal organs, a syndrome resembling blue rubber bleb nevus syndrome, has been described in one dog. Further, there is a report of cutaneous angiomatosis causing sepsis in one dog.
Hemangiosarcoma, the malignant form of a tumor of blood vessel endothelium, can occur in the skin as a primary site or as a result of metastatic disease from a primary visceral tumor. These tumors usually occur in adult and aged animals. In one study of cutaneous vascular tumors of cats, hemangiosarcomas occurred most frequently in white-haired sites and most commonly involved the pinnae and head. Cutaneous hemangiosarcoma commonly recurs following excision and has the potential for widespread local invasion and metastasis; but in general, it appears to be less aggressive, has a longer clinical course, and prolonged survival when compared to visceral hemangiosarcomas. In contrast to the subcutaneous form, dermal hemangiosarcoma may be cured by wide surgical excision alone.
The degree of differentiation is extremely variable, ranging from well-differentiated tumors with well-defined vascular channels to poorly differentiated tumors with minimal lumen formation. Usually hemangiosarcomas consist of plump pleomorphic endothelial cells arranged in single or multiple layers along trabeculae of collagen or pre-existing dermal collagen fibers to form a poorly circumscribed meshwork of blood-filled spaces. Collagenous trabeculae lined by endothelial cells commonly protrude blindly into the vascular spaces. Mitotic activity may be high. Frequently, portions or entire tumors are composed entirely of sheets or intersecting and anastomosing bundles of pleomorphic spindle cells, and they may be indistinguishable from fibrosarcoma or other poorly differentiated spindle cell sarcomas. The presence of slit-like spaces containing erythrocytes between tumor cells may be the only clue to the diagnosis. Immunohistochemical staining may be required to identify the cells in anaplastic tumors. Endothelial cells express vimentin, factor VIII–related antigen (von Willebrand factor), and CD31 (platelet-endothelial cell adhesion molecule/PECAM). However, immunostaining must be interpreted with knowledge of limitations of the procedure; in poorly differentiated tumors, very anaplastic cells may not express typical antigens, and immature reactive stromal endothelial cells may be mistaken for tumor cells.
Tumors arising from endothelium of lymphatic vessels are rare in domestic animals. Both the benign, lymphangioma, and malignant, lymphangiosarcoma, forms occur in young animals, and it has been suggested that they represent lymphatic malformations resulting from a failure of connection between lymph vessels and the venous system rather than being true neoplasms. The skin and subcutis appear to be the most common site of tumors of lymphatic endothelium, and the caudal ventral abdomen and inguinal areas appear to be predisposed. They typically occur as poorly defined fluctuant or edematous masses that are present for many months and drain clear serous to milky fluid. Rarely, they occur as multiple clear turgid vesicles or bullae. It may be difficult to distinguish between lymphangioma and lymphangiosarcoma histologically because the histologic appearance may not correlate well with the biologic behavior of the tumor. Tumors that appear histologically benign commonly recur and may be locally invasive. Lymphangiosarcomas commonly invade local tissues extensively and metastasize to distant sites. They are poorly defined and difficult to remove completely, resulting in poor wound healing and recurrence. In contrast to tumors of vascular endothelium, lymphangiomas/lymphangiosarcomas are composed of spaces largely devoid of material. They may contain only small amounts of proteinaceous fluid and low numbers of erythrocytes and/or lymphoid cells. The connective tissue stroma separating the vascular spaces is loose or edematous and may contain aggregates of lymphoid cells. These tumors have been reported to be immunoreactive for factor VIII–related antigen (von Willebrand factor); CD31 reactivity is variable. Ulceration, hemorrhage, granulation tissue proliferation, and inflammation are frequently present because of the chronic clinical course and may result in misdiagnosis when a small biopsy is taken. It may not be possible to differentiate a poorly differentiated lymphangiosarcoma from hemangiosarcoma. Further complicating diagnosis is a condition called lymphangiomatosis, which is considered a developmental disorder composed of bland dilated lymph channels involving skin, soft tissue, bone, and parenchymal organs.
Feline ventral abdominal lymphangiosarcoma is a tumor that causes marked swelling on the abdominal skin, with erythema and ulcers that ooze serous fluid. The abdomen often has a bruised appearance. These neoplasms were previously termed “angiosarcomas,” but a detailed case series confirmed a lymphatic origin via a positive-staining marker for lymphatic vessels ((LYVE-1, lymphatic vessel endothelial receptor 1), and ultrastructural findings. The tumors are markedly infiltrative, difficult to completely excise, and commonly recur. Metastasis is rare.
Further reading
Asa SA, et al. Expression of platelet-derived growth factor and its receptors in spontaneous canine hemangiosarcoma and cutaneous hemangioma. Histol Histopathol 2012;27:601-607.
Belanger MC, et al. Invasive multiple lymphangiomas in a young dog. J Am Anim Hosp Assoc 1999;35:507-509.
Berry WL, et al. Lymphangiomatosis of the pelvic limb in a Maltese dog. J Small Anim Pract 1996;37:340-343.
Curran KM, et al. Lymphangiosarcoma in 12 dogs: a case series (1998-2013). Vet Comp Oncol 2014;doi:10.1111/vco.12087; [Epub ahead of print].
Diessler ME, et al. Cutaneous lymphangiosarcoma in a young dog: clinical, anatomopathological and lectinhistochemical description. J Vet Med A Physiol Pathol Clin Med 2003;50:452-456.
Ferrer L, et al. Immunohistochemical detection of CD31 antigen in normal and neoplastic canine endothelial cells. J Comp Pathol 1995;112:319-326.
Galeotti F, et al. Feline lymphangiosarcoma—definitive identification using a lymphatic vascular marker. Vet Dermatol 2004;15:13-18.
Hargis AM, et al. A retrospective clinicopathologic study of 212 dogs with cutaneous hemangiomas and hemangiosarcomas. Vet Pathol 1992;29:316-328.
Hinrichs U, et al. Lymphangiosarcomas in cats: a retrospective study of 12 cases. Vet Pathol 1999;36:164-167.
Ide K, et al. Multi-system progressive angiomatosis in a dog resembling blue rubber bleb nevus syndrome in humans. J Small Anim Pract 2013;54:201-204.
Johnson GC, et al. Histologic and immunohistochemical characterization of hemangiomas in the skin of seven young horses. Vet Pathol 1996;33:142-149.
Miller MA, et al. Cutaneous vascular neoplasia in 15 cats: clinical, morphologic, and immunohistochemical studies. Vet Pathol 1992;29:329-336.
Sluiter KL, et al. Bacterial sepsis resulting in severe systemic illness and euthanasia in a dog with cutaneous angiomatosis. Can Vet J 2013;54:397-402.
Ward H, et al. Cutaneous hemangiosarcoma in 25 dogs: a retrospective study. J Vet Intern Med 1994;8:345-348.
Woldemeskel M, Rajeev S. Mast cells in canine cutaneous hemangioma, hemangiosarcoma and mammary tumors. Vet Res Commun 2010;34:153-160.
Histiocytic proliferative disorders
Histiocytic proliferative disorders are commonly observed in dogs, less often in cats, and rarely in piglets. There is a case report of malignant histiocytosis in an Arabian filly and a case report of a histiocytic sarcoma in the nasal cavity of a Dutch Warmblood horse. Histiocytic proliferative diseases recognized in dogs include histiocytoma, cutaneous Langerhans cell (LC) histiocytosis, cutaneous histiocytosis, systemic histiocytosis, and histiocytic sarcoma (localized and disseminated). In cats, feline progressive histiocytosis, feline pulmonary LC histiocytosis, and histiocytic sarcoma have been described. Congenital cutaneous histiocytosis has been described in piglets.
Histiocytes differentiate from CD34+ stem cell precursors found in the bone marrow into macrophages and several dendritic cell (DC) lineages, such as LCs and interstitial DCs. DCs and macrophages have overlapping functions in that both can function as antigen-presenting cells and can act as effector cells. Macrophages are primarily effector cells and act as elements of the innate immune system, whereas dendritic cells function primarily in antigen presentation and hence provide a strong influence on the adaptive immune system. The morphologic features of neoplastic or abnormally reactive histiocytes are similar and can mimic tumor cells of different histogenic origin or be confused with granulomatous inflammation. Differentiation often requires immunophenotyping and sometimes ultrastructural characterization.
Canine cutaneous histiocytoma
Canine cutaneous histiocytomas (CCH) are tumors arising from proliferations of the intraepidermal dendritic cell, the Langerhans cell. Canine cutaneous histiocytomas are most often solitary, benign tumors that usually undergo spontaneous regression in 1-2 months. More than 70% of CCH occur in dogs <4 years of age and are most often found on the head (pinna), but can occur anywhere on the body at any age. There is no sex predilection. Boxers and Dachshunds are predisposed. Grossly, the tumors are raised, red, frequently ulcerated and alopecic, 0.5-4 cm, papular to nodular lesions that grow rapidly. Metastasis of a solitary histiocytoma to a local lymph node has been reported, and in all reported cases with follow-up, there was spontaneous regression. The tumors are well demarcated but unencapsulated and located primarily in the dermis, with the base of the tumor smaller in configuration than the more superficial aspect (“top heavy”). Microscopically, tumor cells form diffuse sheets that displace adnexal structures and dermal collagen, and extend from the epidermis and superficial dermis into the dermis. Care must be taken to differentiate the lesion from epitheliotropic lymphoma. The epidermis is often attenuated or ulcerated, and associated edema may lead to vertical rowing of tumor cells near the surface. Ulceration is associated with infiltrates of neutrophils. The intact epidermis may be hyperplastic. Individual tumor cells are round to oval with moderate to abundant eosinophilic, slightly foamy cytoplasm. Nuclei are centrally located, round to oval, indented or convoluted with vesicular chromatin, and most often have a single nucleolus that may be inconspicuous. Mitotic figures are variable but most often numerous, with up to 10-15/HPF. The base of the tumor may have infiltrates of CD8+ cytotoxic T lymphocytes, a sign of host-mediated spontaneous tumor regression. Infiltrates of lymphocytes may also be found in perivascular or periadnexal regions. In older lesions, the lymphocytic infiltrates may be more extensive than the remaining tumor cell infiltrates, leading to a misinterpretation of primary inflammatory process or inflamed nonepitheliotropic T-cell lymphoma. Tumor cell apoptosis and zones of necrosis are common findings, particularly in regressing lesions but are not present in all CCH. As the function of LCs is to capture antigen and migrate to regional lymph nodes, regional lymph nodes may be enlarged but are not painful and should regress to normal size after tumor removal.
Tumor histiocytes in CCH consistently express vimentin, CD1a, CD11a/CD18, CD11c/CD18, CD44, CD45, and MHC II. They do not express CD90 (Thy-1) or CD45RA. They may also express E-cadherin, lysozyme, CD11d/CD18, and CD54.
Canine cutaneous Langerhans cell histiocytosis
Affected dogs may have hundreds of raised, red, alopecic, and ulcerated cutaneous papules and nodules that are histologically similar to CCH. Lesions may involve mucocutaneous junctions and the oral cavity. Lesions are generally limited to skin and draining lymph nodes initially, but spread to internal organs can also occur rarely. The condition occurs in many breeds, although Shar Peis are over-represented. Delayed regression of lesions is common, with some lesions persisting for 10 months. About 50% of affected dogs are euthanized because of complications such as ulceration and secondary bacterial infections. Those with metastasis to lymph nodes or widespread metastasis have a worse prognosis. Metastasis to lungs and other viscera has been observed. Histologically, lesions are similar to those of CCH; however, individual lesions may be larger extending into the subcutis and muscle. Also there may be a high degree of cellular atypia with more anisocytosis and multinucleated cells and a lack of T-cell infiltration. Lymphatic invasion may occur.
Cutaneous and systemic reactive histiocytosis
Cutaneous reactive histiocytosis (CRH) is an inflammatory lymphohistiocytic proliferative disorder involving the skin, subcutis, and sometimes the local lymph nodes. Lesions are often multiple and occur as cutaneous to subcutaneous nodules up to 4 cm in diameter, often with overlying ulceration (eFig. 6-17). Common sites are face, nose, neck, trunk, extremities, including pawpads, perineum, and scrotum. Lesions may wax and wane, disappear and reappear in other locations, or spontaneously regress.
eFigure 6-17.

Cutaneous reactive histiocytosis in a dog. Multiple erythematous, alopecic, and ulcerated papules and nodules over the nose.
Systemic reactive histiocytosis (SRH) is the term used to designate a similar condition that affects not only the skin, but also lymph nodes and other body organs. Cutaneous reactive histiocytosis does not necessarily lead to systemic reactive histiocytosis, and not all cases of systemic histiocytosis have cutaneous lesions. SRH has a tendency to involve the skin, ocular and nasal mucosae, and peripheral lymph nodes. It generally affects young to middle-aged dogs, and although it was first described in Bernese Mountain dogs, it has been described in many breeds. Lesions are often multiple, and common sites are nasal planum, eyelids, and scrotum. Clinical signs may include anorexia, weight loss, conjunctivitis, chemosis, and stertorous respiration. Lesions and signs may wax and wane. Widespread metastasis to lung, liver, bone marrow, spleen, peripheral and visceral lymph nodes, kidneys, testes, orbital tissues, and nasal mucosa have been described.
Histologically cutaneous lesions are “bottom-heavy,” extending from the mid-dermis into the subcutis. Dermal interstitial DC and T cells infiltrate blood vessel walls in the mid-dermis, leading to lymphohistiocytic vasculitis, which may cause vascular compromise and infarction (eFig. 6-18). Lymphocytes may comprise 50% of the infiltrate. Smaller numbers of neutrophils, plasma cells, and eosinophils may also be present. Discrete perivascular lesions in the mid-dermis, seen initially, coalesce and form nodular infiltrates extending into the deep dermis and subcutis. Older lesions extend into the more superficial dermis and may have a periadnexal distribution. Epitheliotropism is not a feature. Infiltrates of other tissues and organs in SRH are morphologically similar to the cutaneous infiltrates. Histiocytes express CD1a, C11c/CD18, MHC II, CD4, and Thy-1 (CD90). Histiocytes lack expression of E-cadherin.
eFigure 6-18.
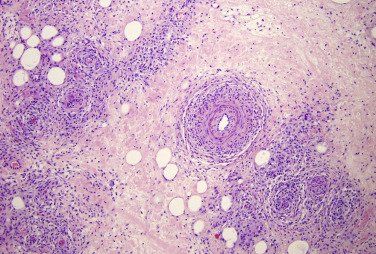
Systemic reactive histiocytosis in a dog. Dendritic cells and lymphocytes infiltrate blood vessel walls in the mid to deep dermis, leading to vascular compromise and necrosis.
The histologic differential diagnoses include a response to infectious agents; other causes of periadnexal granulomas, such as idiopathic sterile pyogranulomas; drug reactions; cutaneous histiocytoma; and lymphomatoid granulomatosis.
The prognosis for CRH is good for survival but guarded for cure without long-term therapy. The prognosis for SRH is guarded. Lesions may wax and wane, and the minority of cases of CRH spontaneously regress. Many times, the lesions are slowly progressive and require long-term management with immunomodulatory therapy and often lead to death, particularly if there is systemic involvement.
Histiocytic sarcoma complex
Histiocytic sarcoma (HS) complex includes a number of distinct syndromes: hemophagocytic HS, articular/periarticular HS, central nervous system HS, dendritic cell leukemia, and feline progressive histiocytosis. Here we will focus only on those conditions with cutaneous involvement: localized HS and feline progressive histiocytosis.
Histiocytic sarcomas can be localized, affecting one site, or disseminated (malignant histiocytosis). Once the lesion spreads beyond the draining lymph node, it is considered disseminated. HSs are usually derived from interstitial dendritic cells. The condition occurs in dogs and is rare in cats. Animals are generally middle-aged to older. Bernese Mountain dogs, Rottweilers, Golden Retrievers, and Flat-coated Retrievers are predisposed. Bernese Mountain dogs and Flat-coated Retrievers have abnormalities in tumor suppressor gene loci (CDKN2A/B, RB1, and PTEN). Clinical signs depend on the organ involved and often include anorexia, weight loss, and lethargy. Mild nonregenerative anemia and hypercalcemia may be seen. In the hemophagocytic form, there are no skin lesions, but there is marked, regenerative, hemolytic anemia and thrombocytopenia.
Localized histiocytic sarcomas (LHS) are rapidly growing malignant neoplasms occurring most often in the skin, subcutis, and associated soft tissues of the extremities. The tumors are often found in periarticular regions and invade the joint capsule, tendons, and muscles of the region. Other reported primary sites for LHS include the spleen, lymph node, lung, bone marrow, and central nervous system. Grossly, masses are infiltrative and destructive and have a uniform smooth cut surface and are pale tan. Articular HS has a distinctive tan multinodular appearance under the synovial lining.
Disseminated histiocytic sarcoma is the term now used to refer to the previously described condition of malignant histiocytosis. Histologically and immunophenotypically, the lesions are identical. It is unclear whether the disseminated histiocytic sarcoma represents metastasis of a primary lesion or multicentric malignant transformation of histiocytes. Secondary sites can be widespread but consistently include liver and lung with primary lung disease and hilar lymph nodes with primary lung disease. Cutaneous involvement is rare with this form. The prognosis is extremely poor, and the condition is rapidly progressive.
Histologically, histiocytic sarcomas consist of a mixture of pleomorphic, anaplastic, plump, round histiocytic cells, and multinucleated histiocytic giant cells. There is marked cytologic atypia with numerous bizarre mitotic figures. Tumor cells have abundant eosinophilic cytoplasm and large oval to indented or twisted vesicular nuclei. Some lesions contain pleomorphic spindle-shaped cells. Mitotic activity is high, and phagocytosis may be evident, although it is much more profound in hemophagocytic HS.
Immunophenotypically, the histiocytic cells comprising these lesions are variable but most consistent with a dendritic cell origin or occasionally macrophage origin. Tumors of interstitial dendritic cell origin express CD1a, MDCII, and CD11c/CD18. Expression of CD4 in not observed. In contrast, expression of CD4 in canine reactive histiocytosis indicates an activation phenotype. In hemophagocytic HS, histiocytes express markers most consistent with macrophage differentiation (CD11d/CD18).
Feline progressive histiocytosis
Feline progressive histiocytosis (FPH) originates in the skin from interstitial DCs in middle-aged to older cats. Cutaneous lesions occur as solitary or more commonly multiple firm, nonpruritic, nonpainful, alopecic and ulcerated papules, nodules, and plaques. Head, trunk, and lower extremities are common sites. Lesions may wax and wane, but there is a poor long-term prognosis. Some cats develop invasive, expansile masses in the lymph nodes, lungs, kidneys, spleen, and/or liver. Histologically, lesions consist of a diffuse dermal infiltrate of morphologically normal histiocytes that may extend into the subcutis. The epidermis may be ulcerated. About 40% of lesions have epitheliotropism characterized by intraepidermal accumulations of one to multiple clusters of histiocytes. Mitotic activity varies. Late-stage lesions resemble HS. Neoplastic cells express CD1a, CD18, and MHC-II. They lack expression of E-cadherin and about half express CD5.
Congenital histiocytosis is a very rare condition of neonatal piglets. Multiple cutaneous macules, papules, and plaques may be widely distributed. On cut surface, they are mottled gray to tan. Histologically, there is a dense infiltrate of spindle cells in short bundles and storiform arrangement in the dermis, extending into the subcutis with variable numbers of histiocytoid cells. A few lymphocytes, plasma cells, and eosinophils may be scattered. There is no epidermotropism, and mitotic activity is low. In one case, expression of lysozyme, CD204, and CD163 within the neoplastic cells supported a histiocytic origin.
Further reading
Affolter VK, Moore PF. Localized and disseminated histiocytic sarcoma of dendritic cell origin in dogs. Vet Pathol 2002;39:74-83.
Affolter VK, Moore PF. Feline progressive histiocytosis. Vet Pathol 2006;43:646-655.
Helie P, et al. Congenital cutaneous histiocytosis in a piglet. Vet Pathol 2013;51:812-815.
Lester GD, et al. Malignant histiocytosis in an Arabian filly. Equine Vet J 1993;25:471-473.
Moore PF. A review of histiocytic disease of dogs and cats. Vet Pathol 2014;51:167-184.
Nagata M, et al. Progressive Langerhans' cell histiocytosis in a puppy. Vet Dermatol 2000;11:241-246.
Paciello O, et al. Histiocytic sarcoma of the nasal cavity in a horse. Res Vet Sci 2013;94:648-650.
Mast cell tumors
Single or multiple nodular dermal proliferations of mast cells occur in all domestic species but are most common in dogs (Fig. 6-161 ). When the mast cells are present in large numbers and as an essentially pure population, a diagnosis of mast cell tumor is usually made. Some, more cautiously, consider such growths as cutaneous mastocytosis until invasive growth or morphologic evidence of anaplasia confirms their neoplastic nature. As heavy accumulations of mast cells may occur in a variety of parasitic, mycotic, allergic, and idiopathic inflammatory syndromes, caution is warranted; however, sheets of mast cells are not present in these other conditions. Multiple spontaneously regressing mast cell tumors have been reported in young dogs, cats, pigs, calves, foals, and humans, suggesting the underlying process may have been mast cell hyperplasia rather than true neoplasia. Diffuse dermal and subcutaneous infiltrates of well-differentiated mast cells occurring over large areas of the body have been reported in cats, dogs, and a foal. The condition has been compared to urticaria pigmentosa in humans.
Figure 6-161.
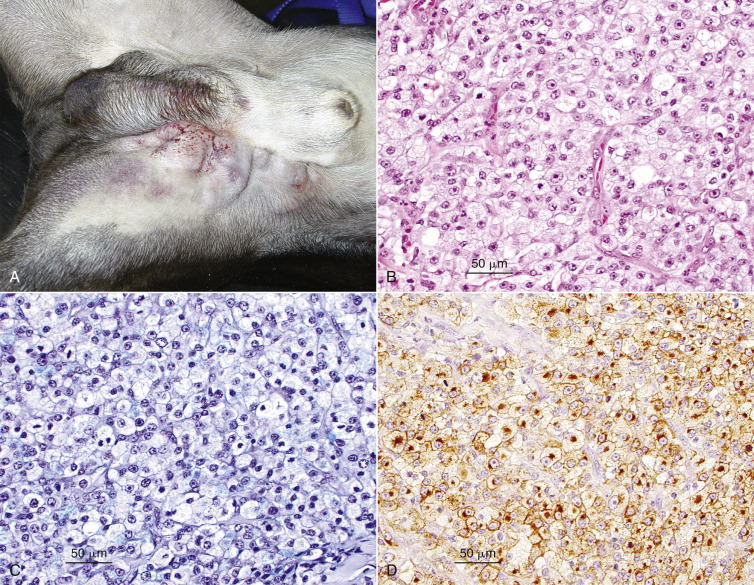
Gross photo of mast cell tumor in a dog. A. Large mast cell tumor located in the inguinal region of a dog, with numerous satellite nodules. B. High-grade mast cell tumor. Note the mitoses and karyomegaly. C. Toluidine blue stain from the tumor in B showing faint metachromatic granules in the cytoplasm of neoplastic cells. D. Cytoplasmic staining with c-Kit in a high-grade mast cell tumor.
The histologic lesion is seldom a diagnostic challenge, except in the very poorly differentiated tumors. The mast cells form diffuse loose sheets or densely packed cords of round cells with a central round nucleus, abundant granular basophilic cytoplasm, and distinct cell membrane (see Fig. 6-161B). Scattered diffusely among the tumor cells are mature eosinophils. Even solid tumors tend to have some areas composed of cords of tumor cells alternating with collagen bundles, particularly at the infiltrative border of the tumor. They are never encapsulated or even well demarcated, except at their superficial edge. A Grenz zone typically separates them from an intact epidermis. Ulceration in large or traumatized tumors may bring the skin surface in contact with the tumor. Eosinophils are few to numerous. Edema may be very severe, giving the tumor an appearance that macroscopically and microscopically resembles acute inflammation. Foci of tumor necrosis, eosinophilic or mononuclear leukocytic vasculitis, vascular necrosis, mineralization, mucinous extracellular matrix, collagen degeneration, or tumor cells with giant or multiple nuclei are all occasionally encountered. Degenerating collagen may incite granulomatous inflammation. Collagen flame figures may be found in some tumors.
In dogs, mast cell tumors (MCTs) account for 15-20% of skin tumors and are the most frequent malignant or potentially malignant tumor of the skin. The mean age of affected dogs is ~9 years, with a range of 3 weeks to 19 years. Boxers, Terriers, Boston Terriers, Labrador Retrievers, Beagles, and Schnauzers are reportedly predisposed. Shar-Peis are also predisposed and, in this breed, mast cell tumors often occur at an earlier age than in other breeds. The macroscopic appearance of canine mast cell tumors varies widely with their stage of progression and degree of histologic differentiation. Well-differentiated tumors most often appear as a rubbery, nodular nonencapsulated variably alopecic dermal mass 1-4 cm in diameter that clinically resembles a lipoma. Poorly differentiated tumors tend to achieve a large size more quickly, are less circumscribed, and often associated with inflammation and edema of the surrounding dermis and possible satellite lesions. Tumors of intermediate grade have a gross appearance that varies between those described previously.
Other clinical signs may occasionally result from the release of histamine or other vasoactive products from the mast cells. Gastroduodenal ulceration is relatively frequent in dogs with disseminated disease, occurring in 35-83% of cases. Histamine release stimulates the specific H2 gastric parietal cell receptors, resulting in increased acid secretion and perhaps local mucosal ischemia. Ulceration follows and may lead to fatal exsanguination. Hypotensive shock from massive synchronous degranulation, as may occur with cryosurgery, is a rarely reported complication.
Several grading systems have been used for MCTs; until recently the Patnaik system was the most widely used. This system designated grade 1 MCTs as well-differentiated tumors with good prognosis, whereas grade 3 MCTs were poorly differentiated tumors with poor prognosis. Grade 2 MCTs were of intermediate differentiation with intermediate prognosis. The histologic features of each grade are as follows: grade 1 (well-differentiated cells, confined to the dermis, no mitoses or necrosis), grade 2 (moderately to highly cellular, extends into the lower dermis/subcutis, 0-2 mitoses/HPF, necrosis/edema/hyalinized collagen), and grade 3 (densely cellular, pleomorphic cells with vesicular nuclei and prominent nucleoli, 3-6/HPF, subcutis involvement, hemorrhage/necrosis/hyalinized collagen). This system left a large gray zone for the prognostication of grade 2 tumors and discordance among pathologists who were grading the tumors.
A newer and more reliable approach is a 2-tiered grading system that divides MCTs into high grade (see Fig. 6-161B) and low grade. The mitotic index (MI) appears to be a distinct indicator of clinical behavior. The MI is defined as the number of mitotic figures/10 consecutive HPFs (400×), and within the region of the tumor with the highest overall mitotic activity. In the 2-tier system, the designation of high grade is based on any one of the following criteria: 7 or greater mitotic index, 3 or more multinucleated (3 or more nuclei) cells in 10 HPFs; 3 or more bizarre nuclei in 10 HPFs; karyomegaly (i.e., nuclear diameters of at least 10% of neoplastic cells vary by at least 2-fold). The designation of low-grade MCT is based on the lack of any high-grade criteria. In this system, high-grade tumors had a shorter time to metastasis or new tumor development and shorter survival time. The median survival time was <4 months for high-grade MCTs but >2 years for low-grade MCTs. Additional studies have corroborated the importance of a MI in grading MCTs.
For many MCTs, additional tests are needed to better define the prognosis, and are often requested by veterinary oncologists. High proliferation indices (Ki-67, AgNOR) have been associated with a worse prognosis and poor survival times. The mast/stem cell growth factor receptor (proto-oncogene c-kit, CD117) appears to be involved in MCT tumorigenesis. The KIT gene encodes the receptor tyrosine kinase that has an extracellular ligand-binding domain (exons 8 and 9), a transmembrane domain (exon 10), a negative regulatory juxtamembrane domain (exons 11 and 12), and a split cytoplasmic kinase. The ligand for KIT is stem cell factor (KIT ligand, mast cell growth factor). Activating mutations in KIT as well as aberrant c-kit expression has been demonstrated in canine MCTs. Approximately 15-40% of MCTs show c-kit mutations, including internal tandem duplications (ITDs) in the juxtamembrane domain, resulting in constitutive activation of KIT in the absence of ligand binding and activating point mutations in c-kit extracellular domains. Canine mast cell tumors that are positive for the activating duplication mutation in exon 11 have a shorter disease-free interval and shorter survival times than tumors without the c-kit mutation. Tumors with mutations in exon 8 or 11 have an increased likelihood of therapeutic success with tyrosine kinase inhibitors. The Kit staining pattern and protein location also has prognostic significance. The staining is defined as follows: pattern 1 (perimembrane), pattern II (focal or stippled cytoplasmic staining), and pattern III (diffuse cytoplasmic staining). Increased cytoplasmic staining is associated with increased rate of local recurrence and decreased survival time (see Fig. 6-161D).
Mast cell tumor margin evaluation is routinely performed on all tumors submitted for histopathology. The surgical guidelines for MCTs suggest that these tumors be resected with surgical margins of 2-3 cm laterally and one tissue plane in depth to minimize recurrence. Wide margins are probably not needed for low-grade MCTs, In one study, 29% (15/51) of low-grade tumors had a histologic margin of 3 mm or less, and only 4% (2/51) recurred locally; 36% of high-grade tumors with complete surgical margins recurred locally.
Mast cell tumors in cats occur as primary cutaneous mast cell tumors and as visceral mastocytosis; these are separate diseases. MCTs are the second most common cutaneous neoplasm in the cat, and account for 20% of skin tumors of cats in the United States. The metastatic potential of feline cutaneous MCTs is very low (~5%), and those destined for behavioral malignancy are easily detected by anisocytosis, hyperchromasia, and mitotic activity. An MI of >5 has been shown to negatively affect survival time. Apparent recurrence at the surgical site or elsewhere in the skin is seen in 25-50% of cases, but most of these probably represent multicentric origin. Cats with multiple MCTs are often feline immunodeficiency virus–positive. Cats with >5 cutaneous MCTs have a more guarded prognosis. There is no widely accepted grading system for feline MCTs.
Mast cell tumors in cats appear as one or several firm, raised pink, alopecic papules ranging in size from millimeters to several centimeters. Less commonly, the tumor appears as a poorly defined area of swelling resulting from an infiltrative rather than nodular lesion. The head and neck are preferred sites. There are 2 histologic subtypes: the mastocytic type and the histiocytic (atypical) type. Histologically, the cells are usually extraordinarily uniform, polygonal to round, and grow in a diffuse sheet interrupted only by small clusters of lymphocytes and rare eosinophils. The cytoplasm is clear, eosinophilic, or only faintly basophilic. Obvious granularity is infrequent. The nucleus is round, central, and relatively hyperchromatic compared with that of canine mast cells. Even with metachromatic stains, such as Giemsa or toluidine blue, cytoplasmic granules may stain poorly, yet ultrastructurally they are abundant. Occasionally, binucleated, multinucleated, or cells with giant nuclei measuring up to 25 µm may be seen. Eosinophils are seen in only a small number of feline MCTs. The tumor is not encapsulated and is most often confined to the dermis. Collagen degeneration and stromal proliferation are rare. Much less frequent is the histologic type (atypical, histiocytic), seen most often in young cats as multiple, simultaneous, or sequential tumors located at the junction of the dermis and subcutis. Siamese cats are predisposed. The tumor mast cells resemble histiocytes, and the lesion may be mistaken for granulomatous inflammation. Toluidine blue or Giemsa staining may be equivocal. The cells are confirmed as mast cells on electron microscopic examination. Eosinophils, lymphoid aggregates, well-circumscribed growth habit, and benign behavior are similar to the more usual MCT of cats described previously.
Mast cell tumors in horses have been cautiously termed cutaneous mastocytosis, but the growths are comparable to the cutaneous tumors of other species. They most commonly occur as solitary nodules on the head, trunk, neck, and limbs. The tumors may be hyperpigmented, alopecic, or ulcerated. Collagen degeneration, large aggregates of eosinophils, necrosis, and focal mineralization are more prominent. Although in some respects resembling such lesions as cutaneous onchocerciasis, habronemiasis, or eosinophilic granulomas, none of these 3 is characterized by sheets of mast cells. Multiple congenital MCTs that spontaneously regress have been reported. There are no reports of metastasis of MCTs in the horse.
Mast cell tumors in ferrets resemble the well-differentiated feline MCT grossly, histologically, and in terms of biological behavior.
In pigs, mast cell nodules have been described as tumors and as multifocal inflammatory aggregates, perhaps in response to Eperythrozoon. Their morphology resembles that of well-differentiated feline tumors. In pigs with multiple skin lesions, visceral aggregates were also found.
In cattle, scant data suggest that the cutaneous tumors are usually multiple and are associated with visceral mast cell aggregates, although purely cutaneous tumors have been reported. Congenital cutaneous MCTs consisting of well-circumscribed 1-7 cm nodules randomly distributed all over the body have also been reported. Histologically, the tumors had features of well-differentiated MCTs. There are more reports of cutaneous metastases of multicentric visceral tumors than there are of primary skin disease. Cattle of any age, including calves, may be affected. There is one report of a calf with congenital diffuse cutaneous mastocytosis. The skin was described as diffusely thickened and wrinkled, with particularly prominent folds on the head, ventrum, and legs. Histologically, there was diffuse dermal infiltration by neoplastic mast cells.
Further reading
Ayl RD, et al. Correlation of DNA ploidy to tumor histologic grade, clinical variables, and survival in dogs with mast cell tumors. Vet Pathol 1992;29:386-390.
Bundza A, Dukes TW. Cutaneous and systemic porcine mastocytosis. Vet Pathol 1982;19:453-455.
Donnelly L, et al. Evaluation of histological grade and histologically tumour-free margins as predictors of local recurrence in completely excised canine mast cell tumours. Vet Comp Oncol 2015;13:70-76.
Ginn PE, et al. Immunohistochemical detection of p53 tumor-suppressor protein is a poor indicator of prognosis for canine cutaneous mast cell tumors. Vet Pathol 2000;37:33-39.
Goldschmidt MH, Shofer FS. Mast cell tumors. In: Goldschmidt MH, editor. Skin Tumors of the Dog and Cat. New York: Pergamon Press; 1992. p. 231-251.
Hendrick MJ, et al. Histological Classification of Mesenchymal Tumors of Skin and Soft Tissues of Domestic Animals. Armed Forces Institute of Pathology; 1998; 2. p. 28-29.
Hill JE, et al. Prevalence and location of mast cell tumors in slaughter cattle. Vet Pathol 1991;28:449-450.
Jaffe MH, et al. Immunohistochemical and clinical evaluation of p53 in canine mast cell tumors. Vet Pathol 2000;37:40-46.
Jeromin AM, et al. Urticaria pigmentosa-like disease in the dog. J Am Anim Hosp Assoc 1993;29:508-513.
Kiupel M, et al. Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Vet Pathol 2011;48:147-155.
Leibman NF, et al. Identification of matrix metalloproteinases in canine cutaneous mast cell tumors. J Vet Intern Med 2000;14:583-586.
Litster AL, Sorenmo U. Characterization of the signalment, clinical and survival characteristics of 41 cats with mast cell neoplasia. J Fel Med Surg 2006;8:177-183.
Lopez A. Cutaneous mucinosis and mastocytosis in a Shar-pei. Can Vet J 1999;40:881-883.
Mathison PT. Eosinophilic nodular dermatoses. Vet Clin North Am Equine Pract 1995;11:75-89.
McManus PM. Frequency and severity of mastocytemia in dogs with and without mast cell tumors: 120 cases (1995-1997). J Am Vet Med Assoc 1999;215:355-357.
Molander-McCrary H, et al. Cutaneous mast cell tumors in cats: 32 cases (1991-1994). J Am Anim Hosp Assoc 1998;34:281-284.
Palyada KS, et al. Diffuse cutaneous mastocytosis in a newborn calf. Vet Dermatol 2008;19:184-186.
Patnaik AK, et al. Canine cutaneous mast cell tumor: morphologic grading and survival time in 83 dogs. Vet Pathol 1984;21:469-474.
Reguera MJ, et al. Canine mast cell tumors express stem cell factor receptor. Am J Dermatopathol 2000;22:49-54.
Romansik EM, et al. Mitotic index is predictive for survival for canine cutaneous mast cell tumors. Vet Pathol 2007;44:335-341.
Sabattini S, et al. Prognostic significance of Kit receptor tyrosine kinase dysregulations in feline cutaneous mast cell tumors. Vet Pathol 2013;50:797-805.
Shaw DP, et al. Multicentric mast cell tumor in a cow. Vet Pathol 1991;28:450-452.
Simoes JPC, et al. Prognosis of canine mast cell tumors: a comparison of three methods. Vet Pathol 1994;31:637-647.
Simoes PC, Shoning P. Canine mast cell tumors: a comparison of staining techniques. J Vet Diagn Invest 1994;6:458-465.
Thompson JJ, et al. Canine subcutaneous mast cell tumor: characterization and prognostic indices. Vet Pathol 2011;48:156-168.
Vail DM. Mast cell tumors. In: Withrow SJ, MacEwen EG, editors. Small Animal Clinical Oncology. 2nd ed. Philadelphia: WB Saunders; 1996. p. 192-210.
Vascellari M, et al. Expression of Ki67, BCL-2, and COX-2 in canine cutaneous mast cell tumors: Association with grading and prognosis. Vet Pathol 2012;50:110-121.
Vitale CB, et al. Feline urticaria pigmentosa in three related Sphinx cats. Vet Dermatol 1996;7:227-233.
Webster JD, et al. Cellular proliferation in canine cutaneous mast cell tumors: associations with c-KIT and its role in prognostication. Vet Pathol 2007;44:298-308.
Webster JD, et al. The role of c-KIT in tumorigenesis: evaluation in canine cutaneous mast cell tumors. Neoplasia 2006;8:104-111.
Whitler WA, et al. Equine mast cell tumor. Equine Pract 1994;16:16-21.
Wilcock BP, et al. The morphology and behavior of feline cutaneous mastocytomas. Vet Pathol 1986;23:320-324.
Yeruham I, et al. Congenital skin neoplasia in cattle. Vet Dermatol 1999;10:149-156.
Cutaneous lymphoma
Lymphomas in the skin can be a primary cutaneous neoplasm or can be part of a multicentric lymphocytic neoplasm. Cutaneous lymphomas have been reported in most domestic animals and in many wildlife species; however, the tumor has been most closely studied in the dog, cat, horse, and in cattle. The body of information about cutaneous lymphomas in veterinary dermatopathology has expanded rapidly in recent years, and is still a subject under close study.
Cutaneous lymphomas in domestic animals are usually divided into 2 groups: epitheliotropic cutaneous lymphomas, in which the neoplastic lymphocytes invade the epidermis and/or adnexal epithelium, and nonepitheliotropic lymphomas, which involve the dermis and subcutis.
Cutaneous epitheliotropic T-cell lymphoma (CTCL) has been reported in the dog, cat, horse, rabbit, and cattle. The misnomer “mycosis fungoides” is an accepted synonym in the human and veterinary literature. CTCL must be differentiated from non-epitheliotropic lymphoma (NEL) or dermal lymphoma. CTCL is classically divided into a localized form pagetoid reticulosis (Woringer-Kolopp disease), classic mycosis fungoides, and Sézary syndrome; however, it is unclear if this classification has any clinical relevance in veterinary medicine. CTCL is a disease of older animals. The clinical presentation varies from an erythematous, exfoliative dermatitis, to multiple plaques and nodules, and mucous membrane/mucocutaneous junction depigmentation (Fig. 6-162 ). Histologically, the neoplastic lymphoid infiltrate involves epidermis and the epithelium of adnexal structures (Fig. 6-163 ). The lymphoid infiltrate in the epithelium can be diffuse, scattered, or form aggregates (Pautrier's microabscesses) (see Fig. 6-163A). Dermal involvement varies from a mixed perivascular cellular component that contains low numbers of neoplastic lymphocytes to a more fulminating diffuse monomorphic neoplastic infiltrate. CTCL frequently causes ulcers, and verification of the epitheliotropic nature of the neoplasm can be difficult; however, a neoplastic lymphocytic component that abuts the ulcerated epidermis suggests epidermotropism. The neoplastic lymphocytes can vary from a small cell type, with a low mitotic index, hyperchromatic nucleus, and scant cytoplasm, to a large cell type, with moderate mitotic index together with moderate amounts of pale basophilic to clear cytoplasm. Although less well characterized than the human form of mycosis fungoides, epitheliotropic lymphomas in domestic animals also express T-cell surface antigens such as CD3. In contrast to human epitheliotropic lymphomas, which are reported to express CD4 in ~90% of cases as well as αβ T-cell receptor, 80% of epitheliotropic lymphomas in domestic animals express CD8 and the γδ T-cell receptor. CTCL with a leukemic blood component (Sézary syndrome) has been reported in the dog, cat, horse, and cow. Canine pagetoid reticulosis (Woringer-Kolopp disease) is a localized solitary plaque form of epitheliotropic lymphoma that is well recognized in humans and has been reported rarely in the dog. In this form, the neoplastic lymphocytes are confined primarily to the epidermis and the dermal component is a mixture of mature lymphocytes and macrophages. This may represent an early form of CTCL, as it is unclear if there is a true difference in clinical behavior in the dog.
Figure 6-162.

Dog with cutaneous epitheliotropic T-cell lymphoma. Note the swelling and depigmentation of the lips, nasal planum, rostral muzzle, and periocular skin.
Figure 6-163.
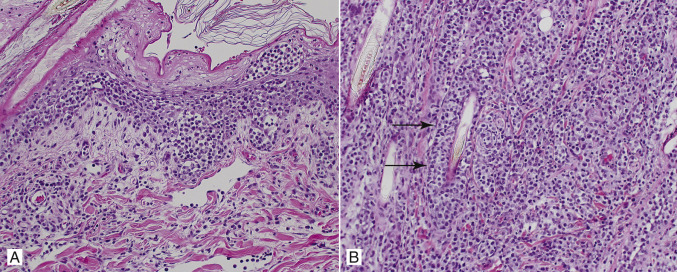
Cutaneous T-cell epitheliotropic lymphoma in a dog. A. Large aggregates of neoplastic cells (Pautrier's microabscesses) infiltrate the epidermis. B. Neoplastic cells infiltrate and efface outer root sheaths of hair follicles (arrows).
In cats, cutaneous epitheliotropic lymphoma is very rare and tends to be a more challenging clinical diagnosis. Affected cast have erythematous to scaly plaques and patches or ulcerated nodules and plaques. Adnexal involvement may be less common than in the dog.
An indolent form of cutaneous nonepitheliotropic T-cell lymphoma that resembles or arises from cutaneous lymphocytosis has been reported in dogs and cats. In cats, the disease occurs at a mean age of 12 years, with no breed predilection. The majority of the lesions appear as solitary areas of alopecia with scaling, erythema, and ulcers. Skin lesions are frequently located on the lateral thorax but may also be found on any region of haired skin or the nasal planum. Pruritus is a common clinical feature. The dermis contains sheets of small lymphocytes (CD3+) with fewer aggregates of C79a+ B cells. PCR for the feline T-cell receptor γ has demonstrated clonality of T cells in lesions from 14 of 20 cats with cutaneous lymphocytosis. Although the disease tends to be very slowly progressive, infiltration of internal organs by lymphocytes may occur along with clinical signs of systemic disease, such as lethargy, inappetence, and weight loss. The histologic features do not predict clinical outcome.
In dogs, indolent cutaneous T-cell lymphoma was characterized by erythematous and scaly macules patches or plaques in 8 dogs. The superficial to mid-dermis contained a band of monomorphic lymphocytes (CD3) without epitheliotropism; 7 of the 8 dogs showed T-cell receptor clonality. The lesions remained stable for years. A few dogs were euthanized because of lesion progression or development of high-grade lymphoma (one dog).
Inflamed nonepitheliotropic T-cell lymphoma is form of cutaneous lymphoma in dogs that can be difficult to differentiate morphologically from cutaneous reactive histiocytosis. The lesions are nonpruritic and range from nodules and plaques to masses, which often ulcerate. Lesions may be found on the mucocutaneous junctions of the face, extremities, neck, and trunk. Histologically, the neoplastic cells form “bottom-heavy” nodules in the dermis and subcutis, often with a Grenz zone. Atypical lymphocytes (intermediate to large) are intermixed with small lymphocytes, plasma cells, histiocytes, neutrophils, and variable numbers of eosinophils. Immunophenotyping is necessary to distinguish inflamed T-cell lymphoma from histiocytic proliferative diseases. The neoplastic cells can efface adnexal structures, but invasion into the epidermis or adnexal epithelium is very unusual. Although the clinical course is variable, the median survival time is only 9 months.
Other nonepitheliotropic cutaneous lymphomas are often of B-cell origin. An interesting form of nonepitheliotropic lymphoma is the T-cell–rich B-cell lymphoma, which is well recognized in humans and has been reported in the cat, pig, dog, and horse. In the horse, it appears to be the most common form of cutaneous lymphoma. In this form, the nodular masses are composed of large neoplastic B lymphocytes accompanied by a background population of smaller reactive T lymphocytes that usually comprise the majority of the cell population. The large neoplastic B cells exhibit cellular atypia, with large vesicular nuclei and numerous mitotic figures that are often atypical. Because the neoplastic population is often the minority population, the mitotic index should be evaluated carefully, taking into account the fact that the majority population is non-neoplastic small T lymphocytes with normal morphology and low mitotic index. These tumors also usually contain macrophages, epithelioid macrophages, and occasionally multinucleated giant cells. The mixed nature of the population can lead to this tumor being mistaken for inflammation, or a neoplasm of T lymphocytes. T-cell–rich B-cell lymphomas in the horse appear to be histologically the same as the neoplasm referred to in the older literature as equine cutaneous histiolymphocytic lymphosarcoma.
Angiocentric lymphoma (lymphomatoid granulomatosis) in the skin is usually a cutaneous manifestation of pulmonary lymphoma; however, it is thought to occur rarely as a primary cutaneous disease. Although well described in humans, this form of lymphoma has been reported infrequently in domestic animals. It is characterized by angiocentric, angioinvasive, and angiodestructive neoplastic lymphocytes in the dermis and subcutis, resulting in intramural and extravascular neoplastic infiltrates, in contrast to the luminal accumulations of lymphocytes in malignant angioendotheliomatosis. The neoplastic cells are medium- to large-sized lymphoid cells that can have a histiocytic appearance, with a cleaved or reniform nucleus. Inflammatory cells such as eosinophils, plasma cells, and small lymphocytes may accompany the neoplastic cells. In the small number of cases reported, the neoplastic lymphocytes have been identified as T lymphocytes by immunophenotyping. Clinically, the presentation is one of multiple alopecic and frequently ulcerated dermal or subcutaneous nodules. The angiodestructive nature of the neoplasm can result in multifocal necrotic or infarctive lesions.
Intravascular lymphoma (malignant angioendotheliomatosis, intravascular lymphomatosis, angiotropic large-cell lymphoma) is characterized by intravascular neoplastic lymphocytes in the vessels of the skin and other organs in the absence of a primary mass or circulating neoplastic cells. This condition is rare in humans and was originally thought to be a proliferation of endothelial cells, which lead to the original name of malignant angioendotheliomatosis. At present, it has been reported rarely in the dog and cat. Clinically, the skin lesions appear as plaques and nodules, and histologically vessels in the dermis and subcutis are partially or completely filled with large atypical lymphoid cells. In humans, the intravascular neoplastic cells are of B-lymphocyte origin; however, in dogs, the majority of cases so far have been of T-lymphocyte origin.
Cutaneous pseudolymphomas are benign reactive proliferations of lymphocytes that mimic cutaneous lymphomas histologically and sometimes clinically. These proliferations are poorly characterized in the veterinary literature, but are well recognized in humans as forming both a band-like infiltrate in the superficial dermis (T-cell pattern) and nodular-to-diffuse infiltrates in the dermis and subcutis (B-cell pattern). Pseudolymphomas in humans can be due to many antigenic stimuli, such as drug eruptions, arthropod or tick-bite reactions, and contact dermatitis. Borrelia burgdorferi–associated cutaneous pseudolymphoma has been reported in one horse; the organism was identified by PCR in the biopsy tissue taken at the site of a tick bite. Differentiation between benign inflammatory lesions and early cutaneous lymphoma can be extremely difficult. Although immunophenotyping can distinguish between T-cell and B-cell lymphomas, methods to distinguish between inflammatory and malignant lymphocyte proliferations may require PCR for analysis for clonality.
Further reading
Affolter VK, et al. Indolent cutaneous T-cell lymphoma presenting as cutaneous lymphocytosis in dogs. Vet Dermatol 2009;20:577-585.
Caniatti M, et al. Canine lymphoma: immunocytochemical analysis of fine-needle aspiration biopsy. Vet Pathol 1996;33:204-212.
Fontaine J, et al. Cutaneous epitheliotropic T-cell lymphoma in the cat: a review of the literature and five new cases. Vet Dermatol 2011;22:454-461.
Gilbert S, et al. Clinical, morphological and immunohistochemical characterization of cutaneous lymphocytosis in 23 cats. Vet Dermatol 2004;15:3-12.
Harris NL, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood 1994;84:1361-1392.
Kelley LC, Mahaffey EA. Equine malignant lymphomas: morphologic and immunohistochemical classification. Vet Pathol 1998;35:241-252.
Kiupel M, et al. Prognostic factors for treated canine malignant lymphomas. Vet Pathol 1999;36:292-300.
Latimer KS, Rakich PM. Sézary syndrome in a dog. Comp Haematol International 1996;6:115-119.
Moore PF, et al. Canine cutaneous lymphoma (mycosis fungoides) is a proliferative disorder of CD8+ T-cells. Am J Pathol 1994;144:421-429.
Moore PF, et al. Canine epitheliotropic cutaneous T-cell lymphoma: an investigation of T-cell receptor immunophenotype, lesion topography and molecular clonality. Vet Dermatol 2009;20:569-576.
Moore PF, Olivry T. Cutaneous lymphomas in companion animals. Clin Dermatol 1994;12:499-505.
Murphy KM, Olivry T. Comparison of T-lymphocyte proliferation in canine epitheliotropic lymphosarcoma and benign lymphocytic dermatoses. Vet Dermatol 2000;11:99-105.
Non-Hodgkin's lymphoma pathologic classification project. National Cancer Institute sponsored study of classifications of non-Hodgkin's lymphomas. Cancer 1982;49:2112-2135.
Peleteiro MC, et al. Two cases of cutaneous T cell lymphoma in Friesian cows in the Azores. Vet Dermatol 2000;11:299-304.
Ploysangam T, et al. Cutaneous pseudolymphomas. J Am Acad Dermatol 1998;38:877-895.
Potter K, Anez D. Mycosis fungoides in a horse. J Am Vet Med Assoc 1998;212:550-552.
Schick RO, et al. Cutaneous lymphosarcoma and leukaemia in a cat. J Am Vet Med Assoc 1993;203:1155-1158.
Sears KP, et al. A case of Borrelia-associated cutaneous pseudolymphoma in a horse. Vet Dermatol 2012;23:153-156.
Smith KC, et al. Canine lymphomatoid granulomatosis: an immunophenotypic analysis of three cases. J Comp Pathol 1996;115:129-138.
Steele KE, et al. T-cell rich B-cell lymphoma in a cat. Vet Pathol 1997;34:47-49.
Tanimoto T, Ohtsuki Y. T-cell-rich B-cell lymphoma in a pig. Vet Pathol 1998;35:147-149.
Vangessel YA, et al. Cutaneous presentation of canine intravascular lymphoma (malignant angioendotheliomatosis). Vet Dermatol 2000;11:291-297.
White SD, et al. Lymphoma with cutaneous involvement in three domestic rabbits (Oryctolagus cuniculus). Vet Dermatol 2000;11:61-67.
Willemze R, et al. EORTC classification for primary cutaneous lymphomas: a proposal from the cutaneous lymphoma study group of the European Organization for Research and Treatment of Cancer. Blood 1997;90:354-371.
Cutaneous plasmacytoma
Cutaneous plasmacytomas are common in dogs and rare in cats. Most cases are benign; however, malignant cutaneous plasmacytomas demonstrating local invasion and tissue destruction do occur. It has not been described in other species. It occurs most often in middle-aged or old dogs, with a marked predilection for the feet, ear canal, and mouth. The typical tumor is a small spherical mass grossly similar to benign cutaneous histiocytoma, but its histology is distinctive. Sheets of pleomorphic round cells are divided into solid lobules by a fine fibrous stroma. The cells often have marked variation in nuclear size and degree of basophilia, with binucleation or multinucleation, and numerous mitotic figures. At least some of the cells retain a perinuclear halo (suggesting a Golgi zone), “clockface” nucleus, and basophilic cytoplasm considered typical of plasma cells. Russell bodies are sometimes seen even in very atypical cells, and the cytoplasm of most cells is pyroninophilic. Cells recognizable as plasma cells are most easily found near the periphery (Fig. 6-164 ). A grenz zone is usually present, and there is no epithelial invasion. Electron microscopy or immunohistochemistry for canine immunoglobulin confirms the diagnosis, but seldom are these tests necessary. Occasionally, a particularly anaplastic example must be distinguished from amelanotic epithelioid melanoma or lymphoma. The distinction is critical, because even bizarre plasmacytomas are cured by excision. Immunophenotyping may be helpful. The antibody Mum-1p is reasonably specific for plasma cell tumors and appears to be superior to CD79a and CD20. Rare B-cell lymphomas can stain positively for Mum-1p. Extracellular amyloid (AL) is found in a small percentage (perhaps up to 10% of plasmacytomas). They bear no apparent relationship to multiple myeloma. Multiple tumors, rarely >2-3, have been reported, as has a very low prevalence (~5%) of local recurrence.
Figure 6-164.
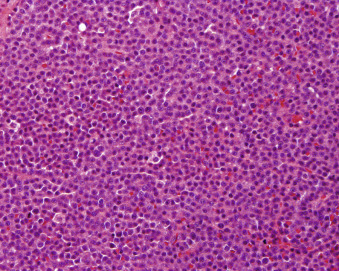
Cutaneous plasmacytoma from a dog.
Further reading
Cangul IT, et al. Clinicopathological aspects of canine cutaneous and mucocutaneous plasmacytomas. J Vet Med A Physiol Pathol Clin Med 2002;49:307-312.
Clark GN, et al. Extramedullary plasmacytomas in dogs: results of surgical excision in 131 cases. J Am Anim Hosp Assoc 1992;28:106-111.
Platz SJ, et al. Prognostic value of histopathological grading in canine extramedullary plasmacytomas. Vet Pathol 1999;36:23-27.
Rakich PM, et al. Mucocutaneous plasmacytomas in dogs: 75 cases (1980-1987). J Am Vet Med Assoc 1989;194:803-810.
Ramos-Vara JA, et al. Immunohistochemical detection of multiple myeloma 1/interferon regulatory factor 4 (MUM1/IRF-4) in canine plasmacytoma: comparison with CD79a and CD20. Vet Pathol 2007;44:875-888.
Smithson CW, et al. Multicentric oral plasmacytoma in 3 dogs. J Vet Dent 2012;29:96-110.
Merkel cell tumor
Merkel cell tumors (Merkel cell carcinoma) have rarely been reported in the dog and cat. Clinically, the tumors appear as nodular lesions that may resemble a histiocytoma. Too few cases have been reported to establish age, site, or sex predilections. Microscopically, the tumors are comprised of dermal infiltrates of round cells arranged as solid nests or clusters separated by collagenous stroma. Individual tumor cells are reported to have indistinct margins and moderate amounts of pale to vacuolated cytoplasm. The nuclei are oval or spherical with dispersed chromatin. The nucleolus may or may not be conspicuous. Anisocytosis is mild to moderate. Mitotic activity varies. Differential diagnoses include round cell tumors, such as cutaneous plasmacytoma, balloon cell melanocytoma, and metastatic neuroendocrine carcinoma.
Definitive diagnosis requires ultrastructural examination or immunohistochemistry. Merkel cell tumors label for cytokeratin (CK), CK20, chromogranin A, neuron-specific enolase, and synaptophysin. Cytokeratin 20 is specific for Merkel cells and has been shown to be useful in the diagnosis of Merkel cell carcinoma in the cat. CK 20 is a low-molecular-weight cytokeratin whose expression is restricted to the gastrointestinal epithelium, urothelium, and Merkel cell. Electron microscopic evaluation demonstrates electron-dense–core granules typical of neuroendocrine cells. Merkel cell tumors in the dog are most often benign, with only one report documenting metastasis. Multicentric cutaneous tumors have also been reported in a dog. Recurrence and metastasis has been reported in cats.
Further reading
Dohata A, et al. Clinical and pathologic study of feline merkel cell carcinoma with immunohistochemical characterization of normal and neoplastic Merkel cells. Vet Pathol 2015;pii:0300985815570484. [Epub ahead of print].
Joiner KS, et al. Multicentric cutaneous neuroendocrine (Merkel cell) carcinoma in a dog. Vet Pathol 2010;47:1090-1094.
Konno A, et al. Immunohistochemical diagnosis of a Merkel cell tumor in a dog. Vet Pathol 1998;35:538-540.
Ozaki K1, Narama I. Merkel cell carcinoma in a cat. J Vet Med Sci 2009;71:1093-1096.
Patnaik AK, et al. Clinicopathologic and electron microscopic study of cutaneous neuroendocrine (Merkel cell) carcinoma in a cat with comparisons to human and canine tumors. Vet Pathol 2001;38:553-556.
Tumors metastatic to the skin
A variety of tumors can metastasize to the skin, but the process is uncommon. Cutaneous metastasis may be the first sign of an undiagnosed visceral malignancy. The usual routes of lymphatic, hematogenous, or implantation from a surgical procedure apply. A thorough search for a primary tumor, knowledge of prior history of a tumor, and an awareness of a few unique tumor patterns of metastasis are necessary to help establish the condition as a metastatic process. Clinically, a wide array of cutaneous lesions have been reported, including erythema, papules, pustules, vesicles, dermal to subcutaneous nodules, and ulcers. Cutaneous metastases in dogs have been reported to occur with the following neoplasms: transitional cell carcinoma (TCC), mammary carcinoma, mast cell tumors, lymphoma, hemangiosarcoma, duodenal and colonic adenocarcinoma, gastric mucinous adenocarcinoma, inflammatory mammary carcinosarcoma, seminoma, osteosarcoma, nasal neuroendocrine carcinoma, and rhabdomyosarcoma.
Cutaneous metastasis of transitional cell carcinoma is uncommon in dogs; however, it has been reported to occur after previous abdominal surgery for TCC and to occur through lymphatics and blood vessels. Transepidermal metastasis has been suggested, because in most cases, cutaneous lesions are in close proximity to the vulva and prepuce. Some believe neoplastic cells from the urine may seed eroded urine scalded skin. Cutaneous lesions appear as plaques, papules, and nodules and most often occur in the perineal, inguinal, or ventral abdominal dermis or subcutis in dogs with or without history of surgery. Many affected dogs also have lymph node and distant metastasis.
Visceral hemangiosarcomas may metastasize to the subcutis in the dog. Subcutaneous hemangiosarcomas, particularly if multiple, should prompt the clinician to search for a primary visceral tumor. Metastatic tumors may be fairly well differentiated or anaplastic.
Mammary gland carcinomas in the dog may metastasize to the dermis of the inner thigh. Spread of tumor cells occurs via direct invasion of dermal lymphatics or from retrograde metastasis of tumor cells from the external inguinal lymph node. Mammary gland carcinomas in the cat may also metastasize to the ventral abdominal tissues by using similar pathways. Primary epitrichial gland carcinoma of the skin may be difficult to distinguish. Cutaneous metastasis of mammary adenocarcinoma has also been reported in a llama. The llama was 8 years old and had nonhealing ulcerative cutaneous lesions distant from the mammary gland region.
Cutaneous metastasis of internal tumors is rare in cats and have been reported in association with mammary adenocarcinoma and digestive and respiratory carcinoma. Pulmonary carcinoma is the most common cause of tumor metastasis to the skin in cats. Pulmonary carcinomas in the cat have a propensity to metastasize to the digits, often prior to onset of clinical signs referable to the primary tumor. Clinically, the lesions are suggestive of paronychia. Histologically, nests, solid sheets, and glandular structures formed by malignant epithelial cells are found in the dermis and subcutis. Bony lysis of the third phalanx may be evident radiographically and histologically. Tumor cells have abundant eosinophilic cytoplasm, basally oriented nuclei, and frequently, apical cilia. Squamous differentiation is also common. Desmoplasia is usually present.
Abdominal surgeries to remove transitional cell, colonic, or prostatic carcinomas have the potential for implantation of tumor cells in the skin at the surgical site. Tumor cells may also reach the skin via retrograde lymphatic metastasis.
Further reading
Dell'Orco M, et al. Gastric mucinous adenocarcinoma with cutaneous metastasis in a dog: diagnosis by fine-needle aspiration cytology. J Small Anim Pract 2005;46:449-453.
Favrot C, Degeorge-Rubiales F. Cutaneous metastases of a bronchial adenocarcinoma in a cat. Vet Dermatol 2005;16:183-186.
Ginel PJ, et al. Vesiculopustular dermatitis associated with cutaneous metastases of an inflammatory mammary carcinosarcoma in a bitch. Vet Rec 2000;147:550-552.
Gorman E, et al. Cutaneous metastasis of primary appendicular osteosarcoma in a dog. Vet Clin Pathol 2006;35:358-361.
Juopperi TA, et al. Extensive cutaneous metastasis in a dog with duodenal adenocarcinoma. Vet Clin Pathol 2003;32:88-91.
Koehler JW, et al. Nasal tumor with widespread cutaneous metastasis in a Golden Retriever. Vet Pathol 2012;49:870-875.
Leichner TL. Cutaneous metastases of mammary carcinoma in a llama. Can Vet J 2001;42:204-206.
Otrocka-Domagala I, et al. Aggressive, solid variant of alveolar rhabdomyosarcoma with cutaneous involvement in a juvenile Labrador Retriever. J Comp Pathol 2014;doi:10.1016/j.jcpa.2014.11.004; [Epub ahead of print].
Reed LT, et al. Cutaneous metastasis of transitional cell carcinoma in 12 dogs. Vet Pathol 2012;50:676-681.
Spugnini EP, et al. Seminoma with cutaneous metastasis in a dog. J Am Anim Hosp Assoc 2000;36:253-256.


