Abstract
The global pandemic of COVID-19 is posing the biggest threat to humanity through its ubiquitous effect of unfathomable magnitude. Although COVID-19 is a viral disease, there might be an association between different comorbidities and the occurrence of the disease. Our study aims to determine the association between the COVID-19 infection and pre-existing comorbidities such as asthma, diabetes, liver disease, lung disease, heart disease, kidney disease, hypertension, and obesity through a web-based self-reported survey. Univariate and multivariate logistic regression analyses were done using these risk factors as independent variables. A total of 780,961 participants from 183 different countries and territories participated in this study. Among them, 1516 participants were diagnosed with COVID-19 prior to this study. A significant risk association was observed for age above 60 years, female gender, as well as different pre-existing disease conditions such as diabetes, kidney disease, liver disease, and heart diseases. Asthma and diabetes were the major dominant comorbidities among patients, and patients with existing diabetes were more likely to develop the disease than others who did not diagnose as diseased. Therefore, older adults, females, as well as people with comorbidities such as diabetes mellitus, heart disease, kidney disease, and liver disease are the most vulnerable population for COVID-19. However, further studies should be carried out to explain the pathway of these risk associations.
Keywords: COVID-19, Comorbidity, Diabetes mellitus, Heart diseases, Kidney diseases, Liver diseases
1. Introduction
After the emergence of the outbreak of novel coronavirus in December 2019 in Wuhan, China (Guan et al., 2020), the WHO had announced this outbreak as a Public Health Emergency of International Concern On 30th January 2020 (Sohrabi et al., 2020). As of 13th December 2020, there have been Seventy million cumulative confirmed cases and over 1.6 million deaths due to COVID-19 worldwide, according to the recent statistics of the World Health Organization (WHO, 2020). Several scientists have hypothesized about zoonotic transmission, although this is yet to be proven (Murdoch and French, 2020).
The Coronavirus infection disease is a highly contagious and transmittable disease caused by a betacoronavirus: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Shereen et al., 2020). Coronavirus is a group of positive single‐stranded large RNA (+ssRNA) (~30 kb) viruses (Cui et al., 2019), containing at least six open reading frames (ORF) and at least four main structural proteins: spike (S), membrane (M), envelope (E), and nucleocapsid (N) proteins (Cui et al., 2019, Chen et al., 2020). It can infect not only human hosts but also different animals (Ahmad et al., 2020). This virus belongs to the same family, composed of the severe acute respiratory syndrome coronavirus (SARS-CoV), H5N1 influenza A, H1N1 2009, and Middle East respiratory syndrome coronavirus (MERS-CoV) cause acute lung injury and acute respiratory distress syndrome (Shu et al., 2017). The transmissibility of SARS-CoV2 is higher compared to that of SARS-CoV (Liu et al., 2020). Furthermore, the mortality for COVID-19 is higher, but case mortality is higher for MERS-CoV and SARS-CoV (Mahase, 2020).
The symptoms of COVID-19 include Fever, Lower respiratory tract infection, acute respiratory infection, Cough, Shortness of breath, etc. (Guan et al., 2020, Deng et al., 2020). However, there can be COVID-19 case without any signs and symptoms, which makes the control of these pandemics challenging (Rothe et al., 2020). Geriatric population and people with severe comorbidities such as Asthma, Chronic kidney disease (CKD), chronic lung disease, Diabetes mellitus, Hemoglobin disorders, Immunity deficiency, Liver disease, Serious heart conditions, Severe obesity might be at higher risk of poor clinical outcome (NCIRD, 2019, Guan et al., 2020), increased hospital stays (Zhou et al., 2020) and higher case fatality rate (Deng et al., 2020). Along with increasing severity and mortality, these comorbidities might be associated with the incidence of COVID-19, since the immune system and systemic metabolism of the body are already compromised owing to these pre-existing conditions. For instance, Diabetic patients are more prone to infectious diseases due to impaired glycaemic control, which limits humoral immunity (Joshi et al., 1999, Shah and Hux, 2003). Furthermore, the expression of angiotensin-converting enzyme 2 (ACE2) is increased in Type 1 and Type 2 Diabetes mellitus as well as in hypertension, and the coronaviruses bind with target cells through ACE2 (Fang et al., 2020).
There are a few studies on the association between various comorbidities and COVID-19. Most of these studies were conducted solely on COVID-19 patients with fewer participants. Our study aims to determine the association between COVID-19 infection and pre-existing comorbidities using data collected from 780,961 participants from all over the world through a web-based self-reported survey.
2. Method
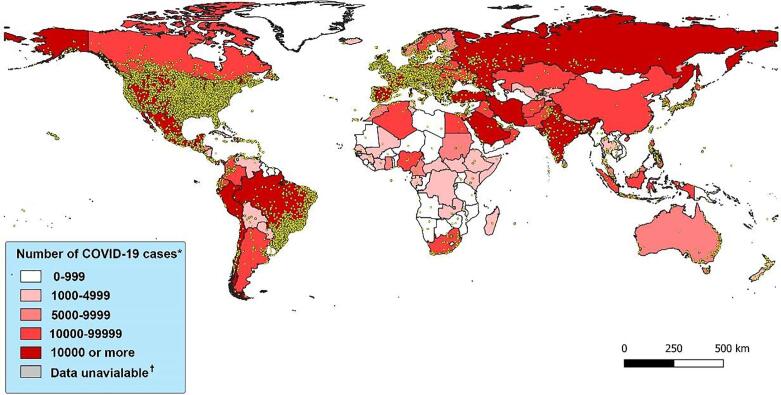
A secondary dataset from the Nexoid United Kingdom was used for this study (available at https://www.covid19survivalcalculator.com/data/master_dataset.csv). The data was collected between 25th March 2020 to 4th June 2020 by a web-based self-reported survey in order to generate a large global medical dataset for COVID-19 infection modeling. This dataset is under the “Attribution 4.0 International (CC BY 4.0)” license. In order to preserve the confidentiality of the participants, several measures were ensured, such as e-mail address, I.P. address, date of birth was kept private as well as timestamp and location data were randomly adjusted. The survey questionnaire was comprised of 30 questions regarding sociodemographic, behavioral, morbidity, clinical, and diagnostic information related to COVID-19, and the survey was conducted in English (Nexoid, 2020). Sample recruitment was done using an unrestricted self-selection method. The participants were invited through different social media platforms such as Facebook, Reddit, etc. The participants reviewed the privacy statement and agreed to participate in the study. A total of 780,961 people filled the online survey, and among them, 1516 people were diagnosed with COVID-19. A survey map was generated using the I.P. location data of the participants using the QGIS application (version 3.4.11) (Fig. 1). As the study was observational, the Institutional Ethics Committee of Noakhali Science and Technology University confirmed that no ethical approval was required.
Fig. 1.
World map according to the intensity of COVID-19 cases and sample location Note: Yellow dot represents sample locations. *Data were retrieved from worldometers website on 7th June 2020 GMT 18.00 h (Worldometer, 2020) †Data was not available for North Korea. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Age, Gender, BMI, COVID, and other disease conditions such as Asthma, Liver diseases, Lung diseases, Heart diseases, Diabetes mellitus, Hypertension data were extracted from the database. Obesity was determined from the BMI: People having a BMI of 30 or higher were considered obese.
Data analysis was carried out using IBM SPSS statistics (Version 23). Each variable was tested for descriptive statistics. The Categorical variables are presented as frequency and percentages, where continuous variables are presented as mean and standard deviation, and a t-test was done to compare the mean between COVID 19 cases and control population, who did not report as COVID-19 positive. Univariate logistic regression was carried out using COVID as a dependent variable and others as independent variables separately. The level of significance for all of the statistical tests was set at 0.05. Finally, each of the significant risk factors from univariate logistic regression was fed into a mixed multivariate logistic regression and odds ratio as well as a 95% confidence interval was calculated., A Hosmer and Lemeshow test was carried out in order to analyze the goodness of fit.
3. Result
The majority of the study population are young and under Forty years of age. Most of the participants are from North America, Europe, and South America. The United States, Brazil, Canada, and Belgium are at the top with the highest number of confirmed cases of COVID-19. Above two-thirds of the participants are male, and apart from obesity, the number of other comorbidities is higher in the COVID-19 cases (Table 1).
Table 1.
Sociodemographic and clinical characteristics of the study population.
| Characteristics | Total (n = 780961) | COVID-19 cases (n = 1516) | Control (n = 779445) |
|---|---|---|---|
| Age | |||
| Below 40 years | 463,426 (59.34) | 1097 (72.36) | 462,601 (59.35) |
| 40–59.9 years | 251,349 (32.18) | 482 (31.79) | 250,867 (32.12) |
| 60–79.9 years | 62,886 (8.05) | 143 (9.43) | 62,743 (8.03) |
| Above 80 years | 3296 (0.42) | 76 (5.01) | 3220 (0.41) |
| Region | |||
| Asia | 6328 (0.81) | 35 (2.3) | 6293 (0.8) |
| Africa | 1384 (0.17) | 4 (0.26) | 1380 (0.18) |
| Europe | 41,484 (5.31) | 205 (13.52) | 41,279 (5.3) |
| North America | 682,258 (87.36) | 1117 (73.68) | 681,141 (87.39) |
| South America | 40,623 (5.2) | 144 (9.5) | 40,479 (5.19) |
| Oceania | 8853 (1.13) | 10 (0.66) | 8843 (1.13) |
| Gender | |||
| Male | 526,317 (67.39) | 817 (53.89) | 525,500 (67.42) |
| Female | 251,730 (32.23) | 691 (45.58) | 251,039 (32.2) |
| BMI | 29.72 ± 7.92 | 30.29 ± 9.3 | 29.72 ± 7.92 |
| Comorbidity | |||
| Asthma | 123,207 (15.78) | 245 (16.16) | 122,962 (15.77) |
| Diabetes mellitus | 46,999 (6.01) | 171 (11.27) | 46,828 (6.0) |
| Kidney Disease | 2625 (0.34) | 46 (3.03) | 2529 (0.32) |
| Liver Disease | 667 (0.09) | 22 (1.45) | 645 (0.08) |
| Heart Disease | 13,131 (1.68) | 92 (6.06) | 13,039 (1.67) |
| Lung Disease | 10,424 (1.33) | 44 (2.90) | 10,380 (1.33) |
| Hypertension | 103,883 (13.3) | 273 (18.0) | 103,610 (13.29) |
| Obesity | 275,129 (35.23) | 514 (33.9) | 274,615 (35.23) |
Note: The percentages may not add up to 100% due to missing data.
From univariate logistic regression, Female participants and people age 60 or above had a higher risk of COVID-19. Except for Asthma and Obesity, other comorbidities have shown significantly elevated risk associated with the occurrence of COVID-19. Significant risk factors found in univariate logistic regression were fed into a multivariate logistic regression model. Significantly higher risk associations were observed for Age, Female gender, Diabetes, Kidney disease. Liver disease and Heart disease (Table 2). After adjustment of age and gender, the comorbidities (except asthma and obesity) were found to be associated with a higher infection rate as well. A Hosmer and Lemeshow test confirmed the goodness of fit of this model.
Table 2.
Univariate and multivariate analysis of risk factors associated with the incidence of COVID-19.
| Variable | Univariate |
Multivariate |
||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age* | 1.82 (1.58–2.1) | <0.001 | 1.36 (1.16–1.6) | <0.001 |
| Gender | 1.77 (1.6–1.96) | <0.001 | 1.69 (1.52–1.87) | <0.001 |
| Asthma‡ | 1.03 (0.9–1.18) | 0.68 | – | – |
| Diabetes mellitus‡ | 1.99 (1.70–2.33) | <0.001 | 1.46 (1.23–1.74) | <0.001 |
| Kidney Disease‡ | 9.43 (7.01–12.67) | <0.001 | 4.73 (3.38–6.61) | <0.001 |
| Liver Disease‡ | 17.78 (11.59–27.28) | <0.001 | 9.39 (5.94–14.85) | <0.001 |
| Heart Disease‡ | 3.80 (3.07–4.69) | <0.001 | 2.08 (1.63–2.66) | <0.001 |
| Lung Disease‡ | 2.22 (1.64–2.99) | <0.001 | 1.19 (0.86–1.66) | 0.29 |
| Hypertension‡ | 1.43 (1.26–1.63) | <0.001 | 0.98 (0.84–1.13) | 0.75 |
| Obesity‡ | 0.94 (0.85–1.05) | 0.28 | – | – |
*Age was classified: Below 60 years and above 60 years; Below 60 years were set as the reference for binary logistics regression.
†Male gender was set as the reference.
‡People who are not diagnosed with the disease were set as the reference.
4. Discussion
The present study investigated mostly demographic, morbidity, clinical, and diagnostic information related to COVID-19 from a handful of participants, and among them, 1516 people were diagnosed as COVID positive (+). The study compared COVID positive patients (cases) with controls and found a strong significant association with age, sex, and critical comorbidities (diabetes, kidney, liver, heart diseases, and hypertension). Though the majority of the survey participants were male (67.39%), the number of positive cases among females were pretty evenly closed (45.58%) with males. Several studies confirmed that the percentage of men suffering from this virus is higher than women (Nahian Rahman, 2020). However, our study found women were more prone to infection, and the multivariate logistic regression reveals females were 1.69 times (AOR: 1.69; 95% CI: 1.52–1.87) more likely to get infected by Covid-19 in contrast to male participants. However, this finding does not bode well with one study, which inferred women were less susceptible to this virus than men based on a different innate immunity, steroid hormones, and factors related to sex chromosomes (Conti and Younes, 2020). These contrasting findings must put more debate on this unknown condition in which the world is trying to get an answer. One population-based study conducted in Iceland between 31st January to 31st March also found a lower incidence in females and children under ten than males (Gudbjartsson et al., 2020)
Age was also found to have some effect, and participants over 60 years of age had a marginally higher risk (AOR:1.36; 95% CI: 1.16–1.6) than their younger counterparts though only around 14% of participants were above 60 years. Most of the participants were from the age group under 40 years of age, possibly because they are more accustomed to online surveys and use. The possible explanation for the higher risk of COVID-19 in the geriatric population is that most of the geriatric people dwell in nursing homes or old homes, which can trigger rapid transmissibility. One study conducted on Israeli patients concluded that younger individuals have less chance to experience severe symptoms, which requires intensive care unit hospitalization, and the recovery rate was on average faster than the older aged patients (Voinsky et al., 2020). Another study in China during the first half of February 2020, expressed a serious concern, which entails that older age and a high number of comorbidities were associated with higher severity irrespective of gender. However, men's cases tended to be more critical than women's (Jin et al., 2020).
Obesity among participants was seen pretty evenly distributed and expectedly did not warrant any substantial influence on COVID-19. Hypertension, a common comorbid situation, was also assessed to have an insignificant effect on COVID cases after controlling the influence of other predictors. These findings also contrast with one study conducted in Mainland Chain, which found hypertension as the most prevalent (16.9%) comorbidity among 1590 confirmed hospitalized COVID patients between 11th December to 31st January 2020 (Guan et al., 2020) and another study on the Chinese population during late January 2020 revealed that hypertension was even more common clinical manifestation (30%) (Zhang et al., 2020).
To put views on the effect of other comorbidities on COVID-19 in this present study reveals that participants with any of the existing comorbidities (liver, kidney, heart, lung disease, and diabetes) were observed to have more risks of this disease than participants who did not have the conditions irrespective of their gender and age. However, the number of COVID cases among kidney disease patients was low. It matches one article published in Nature Reviews Nephrology, which stressed that its involvement might result in multiple organ dysfunction and severe outcomes (Ronco and Reis, 2020). An understanding of the pathophysiology and mechanisms of kidney damage is still under scrutiny, and effective treatment is still not established (Ronco et al.). Hence, it should be taken very seriously. Our study reveals that participants with kidney problems had 9.39 times (AOR: 9.39; 95% CI: 5.94–14.85) more chance of being infected with the virus than others, and this trend of increased chances was observed with other comorbid conditions though in a lesser degree. Our findings of diabetes, another common clinical comorbidity, coincide with the results of other studies (Zhang et al., 2020). From the result, it appears that having physiological problems of different kinds had a serious aggravating effect as it increases the likelihood of getting infected by a novel coronavirus because of the weak immune system, which is susceptible to infection. Moreover, having comorbidities also correlated with poorer clinical outcomes in COVID patients (Guan et al., 2020).
There are some limitations to this study. First of all, this is an online-based self-reported study. Because of the unavailability of biochemical tests, the accuracy and validity of the data are questionable. For example, there was no option to confirm whether the participants were COVID-19 positive or not. Furthermore, the RT-PCR COVID-19 detection test can also be false positive or false negative for a variety of reasons (Tahamtan and Ardebili, 2020). Secondly, most of the study participants are from North America, Europe, and South America, but there is a current galloping trend of infection and fatality in Asia. These findings may not apply to the population of these parts of the world. The online survey requires more knowledge, technological skills, and logistics. The people from low and middle-income countries and older adults lack the logistics and technological skills for participating in these studies.
Moreover, the number of covid-19 cases among the participants was low compared to the non-covid participants in the survey. It could be due to the survey's timing when the covid-19 cases were not that severe in the countries from where more people responded. Besides, people who suffered from covid-19 might go through physical and mental trauma (Prescott and Girard, 2020), which can dissuade them from participating and revealing their experience.
Additionally, the study was conducted in English, so people who do not speak English could not participate in the survey. Some countries emphasize the laboratory testing of COVID-19 than others due to their health care policy and resource. Also, people with mental disorders had limited access to this survey. These factors might have an impact on our results. Moreover, kidney diseases, lung diseases, heart diseases, liver diseases are composed of an array of diseases. No specific disease was mentioned in this study rather than just groups of diseases. If the particular type of disease were mentioned, that would have provided a more specific and more precise picture. Finally, the study also failed to consider other epidemiological factors, e.g., participants' living conditions, types of jobs they do, and their neighborhood, which might affect the disease's transmission.
Though more specific clinical studies are required to understand this unprecedented mystery of a disease and how it affects other deadly comorbidities or whether other comorbidities had any say on this association still requires studies of different kinds to come close to any conclusive remarks. Our study attempted to shed some light on how comorbidities can come in and increases the likelihood of getting infected, and the pathways of infection require clarification, which we believe will be clarified by further studies.
Funding
The authors received no specific funding for this study.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
We would like to express our gratitude to the Nexoid United Kingdom for providing us the necessary dataset for this study.
Submission declaration and verification
The Authors hereby consents to publish this research article. This article has not been published or submitted elsewhere for publication. The authors also declare that this work does not libel anyone, violate anyone's copyright or common law rights.
Availability of data and material
The datasets generated during this study are available from the corresponding author on a reasonable request.
Authors' contribution
MRA and MRK has designed the study, acquired the secondary data, wrote the first draft of the manuscript, participated in data interpretation and revised the manuscript critically for important intellectual content. SR helped in the literature review and statistical analysis. All authors read and approved the final manuscript.
Contributor Information
Mohammad Rahanur Alam, Email: rahanur.ftns@nstu.edu.bd.
Md. Ruhul Kabir, Email: ruhul109@gmail.com.
Sompa Reza, Email: sompa.infs@gmail.com.
References
- Ahmad T., Khan M., Haroon, Musa T.H., Nasir S., Hui J., Bonilla-Aldana D.K., Rodriguez-Morales A.J. COVID-19: zoonotic aspects. Travel Med. Infect. Dis. 2020;36:101607. doi: 10.1016/j.tmaid.2020.101607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.u., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti P., Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J. Biol. Regul. Homeost. Agents. 2020;34 doi: 10.23812/Editorial-Conti-3. [DOI] [PubMed] [Google Scholar]
- Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Guangtong, Yin Mingzhu, Chen Xiang, Zeng Furong. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit. Care. 2020;24(1) doi: 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang Lei, Karakiulakis George, Roth Michael. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.-J. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur. Respir. J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.-J., Ni Z.-y., Hu Y.u., Liang W.-H., Ou C.-Q., He J.-X., Liu L., Shan H., Lei C.-L., Hui D.S.C., Du B., Li L.-J., Zeng G., Yuen K.-Y., Chen R.-C., Tang C.-l., Wang T., Chen P.-Y., Xiang J., Li S.-Y., Wang J.-L., Liang Z.-J., Peng Y.-X., Wei L.i., Liu Y., Hu Y.-H., Peng P., Wang J.-M., Liu J.-Y., Chen Z., Li G., Zheng Z.-J., Qiu S.-Q., Luo J., Ye C.-J., Zhu S.-Y., Zhong N.-S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudbjartsson D.F. Spread of SARS-CoV-2 in the icelandic population. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2027653. [DOI] [PubMed] [Google Scholar]
- J.-M. Jin, et al., 2020. Gender differences in patients with COVID-19: focus on severity and mortality. Front. Public Health 8(152). [DOI] [PMC free article] [PubMed]
- Joshi Nirmal, Caputo Gregory M., Weitekamp Michael R., Karchmer A.W. Infections in patients with diabetes mellitus. N. Engl. J. Med. 1999;341(25):1906–1912. doi: 10.1056/NEJM199912163412507. [DOI] [PubMed] [Google Scholar]
- Liu Y. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J. Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. Coronavirus: covid-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ. 2020;368:m641. doi: 10.1136/bmj.m641. [DOI] [PubMed] [Google Scholar]
- Murdoch D.R., French N.P. COVID-19: another infectious disease emerging at the animal-human interface. N. Z. Med. J. 2020;133(1510):12–15. [PubMed] [Google Scholar]
- Nahian Rahman M. Under five child mortality & its risk factors in Bangladesh and other South Asian countries: a literature review. Ind. J. Public Health Res. Dev. 2020;11(6):1374–1379. [Google Scholar]
- NCIRD, 2020. Groups at Higher Risk for Severe Illness. Coronavirus Disease 2019 (COVID-19), 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html.
- Nexoid, 2020. COVID-19 risk calculator, 07.07.2020]; Available from: https://www.covid19survivalcalculator.com/data/master_dataset.csv.
- Prescott Hallie C., Girard Timothy D. Recovery from severe COVID-19: leveraging the lessons of survival from sepsis. JAMA. 2020;324(8):739. doi: 10.1001/jama.2020.14103. [DOI] [PubMed] [Google Scholar]
- Ronco, C., Reis, T., Husain-Syed F. Management of acute kidney injury in patients with COVID-19. Lancet Respir. Med. [DOI] [PMC free article] [PubMed]
- Ronco Claudio, Reis Thiago. Kidney involvement in COVID-19 and rationale for extracorporeal therapies. Nat. Rev. Nephrol. 2020;16(6):308–310. doi: 10.1038/s41581-020-0284-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe Camilla, Schunk Mirjam, Sothmann Peter, Bretzel Gisela, Froeschl Guenter, Wallrauch Claudia, Zimmer Thorbjörn, Thiel Verena, Janke Christian, Guggemos Wolfgang, Seilmaier Michael, Drosten Christian, Vollmar Patrick, Zwirglmaier Katrin, Zange Sabine, Wölfel Roman, Hoelscher Michael. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah B.R., Hux J.E. Quantifying the risk of infectious diseases for people with diabetes. Diab. Care. 2003;26(2):510–513. doi: 10.2337/diacare.26.2.510. [DOI] [PubMed] [Google Scholar]
- Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J. Adv. Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu Y., McCauley J. GISAID: global initiative on sharing all influenza data - from vision to reality. Euro. Surveill. 2017;22(13) doi: 10.2807/1560-7917.ES.2017.22.13.30494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahamtan Alireza, Ardebili Abdollah. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev. Mol. Diagn. 2020;20(5):453–454. doi: 10.1080/14737159.2020.1757437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voinsky Irena, Baristaite Gabriele, Gurwitz David. Effects of age and sex on recovery from COVID-19: analysis of 5769 Israeli patients. J. Infect. 2020;81(2):e102–e103. doi: 10.1016/j.jinf.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2020. eekly Epidemiological Update: 21 September 2020, in Coronavirus disease 2019 (COVID-19), WHO, Editor. WHO.
- Worldometer. COVID-19 Coronavirus Pandemic, [cited 2020 07.06.2020]. Available from: https://www.worldometers.info/coronavirus/.
- Zhang Jin-jin, Dong Xiang, Cao Yi-yuan, Yuan Ya-dong, Yang Yi-bin, Yan You-qin, Akdis Cezmi A., Gao Ya-dong. Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. 2020;75(7):1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- Zhou Fei, Yu Ting, Du Ronghui, Fan Guohui, Liu Ying, Liu Zhibo, Xiang Jie, Wang Yeming, Song Bin, Gu Xiaoying, Guan Lulu, Wei Yuan, Li Hui, Wu Xudong, Xu Jiuyang, Tu Shengjin, Zhang Yi, Chen Hua, Cao Bin. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during this study are available from the corresponding author on a reasonable request.