Abstract
BACKGROUND/OBJECTIVES:
Dementia is associated with higher healthcare expenditures, in large part due to increased hospitalization rates relative to patients without dementia. Data on contemporary trends in the incidence and outcomes of potentially preventable hospitalizations of patients with dementia are lacking.
DESIGN:
Retrospective cohort study using the National Inpatient Sample from 2012 to 2016.
SETTING:
U.S. acute care hospitals.
PARTICIPANTS:
A total of 1,843,632 unique hospitalizations of older adults (aged ≥65 years) with diagnosed dementia.
MEASUREMENTS:
Annual trends in the incidence of hospitalizations for all causes and for potentially preventable conditions including acute ambulatory care sensitive conditions (ACSCs), chronic ACSCs, and injuries. In-hospital outcomes including mortality, discharge disposition, and hospital costs.
RESULTS:
The survey weighted sample represented an estimated 9.27 million hospitalizations for patients with diagnosed dementia (mean [standard deviation] age = 82.6 [6.7] years; 61.4% female). In total, 3.72 million hospitalizations were for potentially preventable conditions (40.1%), 2.07 million for acute ACSCs, .76 million for chronic ACSCs, and .89 million for injuries. Between 2012 and 2016, the incidence of all-cause hospitalizations declined from 1.87 million to 1.85 million per year (P = .04) while the incidence of potentially preventable hospitalizations increased from .75 million to .87 million per year (P < .001), driven by an increased number of hospitalizations of community-dwelling older adults. Among patients with dementia hospitalized for potentially preventable conditions, inpatient mortality declined from 6.4% to 6.1% (P < .001), inflation-adjusted median costs increased from $7,319 to $7,543 (P < .001), and total annual costs increased from $7.4 to $9.3 billion. Although 86.0% of hospitalized patients were admitted from the community, only 32.7% were discharged to the community.
CONCLUSION:
The number of potentially preventable hospitalizations of older adults with dementia is increasing, driven by hospitalizations of community-dwelling older adults. Improved strategies for early detection and goal-directed treatment of potentially preventable conditions in patients with dementia are urgently needed.
Keywords: hospitalization, dementia, healthcare utilization
Nearly 1 in 7 U.S. adults aged 70 and older has dementia, resulting in substantial healthcare utilization, individual financial burden, and health system costs.1 Increased rates of hospitalizations among older adults with diagnosed dementia2–4 are the leading contributor to higher Medicare expenditures compared with those without dementia.5 Beyond the acute illness, hospitalization poses substantial risks to older adults with dementia: functional decline, delirium, and other iatrogenic complications.6–8 Once discharged, older adults then encounter a period of heightened susceptibility to disease, adverse events, and rehospitalization.9,10 Thus reducing unnecessary hospitalizations is a crucial step toward improving patient-centered care and clinical outcomes for older adults with dementia.
Potentially preventable hospitalizations include ambulatory care sensitive conditions (ACSCs) and injuries. ACSCs include acute and chronic conditions for which high-quality ambulatory care may prevent the need for hospitalization.11–13 For acute conditions, such as pneumonia and urinary tract infections (UTIs), early outpatient detection and management may reduce the severity of illness, preventing the need for hospitalization. For chronic conditions, such as congestive heart failure and chronic obstructive pulmonary disease (COPD), optimal outpatient care may reduce the occurrence of exacerbations requiring hospital care. Injuries include trauma from falls and other accidents, as well as inadvertent medication poisonings. For traumatic injuries, prevention efforts have focused on balance, gait, and home safety evaluations as well as the use of bisphosphonates in patients with osteoporosis to mitigate the risk of traumatic injuries. Efforts to increase awareness of safe prescribing practices have sought to reduce accidental poisonings and adverse drug events.
Reducing preventable hospitalizations of older adults with dementia is a stated objective of Healthy People 2020. Over the past decade, multiple national programs broadly targeting potentially preventable hospitalizations have been introduced. Injury prevention efforts have been led by the Centers for Disease Control and Prevention through programs such as Stopping Elderly Accidents, Deaths, and Injuries (STEADI) introduced in 2013.14 As part of the Affordable Care Act (ACA), the Centers for Medicare & Medicaid Services (CMS) launched several health policy initiatives targeted at reducing preventable hospitalizations including the Hospital Readmissions Reduction Program15 and Initiative to Reduce Avoidable Hospitalizations among Nursing Facility Residents.16–18 However, despite the unique challenges in communication and care coordination faced by older adults with dementia, no national policy or programmatic initiatives have focused specifically on reducing preventable hospitalizations in this population, most of whom reside at home.
To inform the development of initiatives to reduce potentially preventable hospitalization of older adults with dementia, contemporary data on the incidence and clinical outcomes of hospitalizations are needed. However, prior studies of hospitalized patients with dementia19–22 predate the ACA and related policy initiatives that have significantly impacted hospitalization trends.15,23 To address this gap, the present study uses nationally representative hospital discharge data from 2012 to 2016 to examine national trends in all-cause and potentially preventable hospitalizations of older adults with diagnosed dementia. Given recent evidence documenting a decline in hospital transfers among nursing home residents,16–18 we further examined hospitalization trends by older adults’ residence before hospitalization.
METHODS
Data Sources
We performed a retrospective cohort study of hospitalized older adults with a diagnosis of dementia using the National Inpatient Sample (NIS). The NIS contains patient discharge-level administrative data drawn from the 47 states participating in the Agency for Healthcare Research and Quality’s (AHRQ) Healthcare Cost and Utilization Project state inpatient databases and approximates a 20% stratified sample of all discharges from community hospitals in the United States. We examined all hospitalizations for which patients were discharged from January 1, 2012, through December 31, 2016.
Study Population
We identified all hospitalizations for adults aged 65 and older with a diagnosis of dementia based on the presence of one or more International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10-CM) discharge diagnosis codes. Diagnosis codes used to identify dementia were based on a modified version of the chronic condition data warehouse (CCW) algorithm for Alzheimer’s Disease and Related Disorders (Supplementary Table S1).24 We made the following modifications to the CCW algorithm: (1) we added a diagnosis of dementia with Lewy bodies that is not included in the CCW algorithm, and (2) we excluded certain diagnoses from the CCW algorithm that are not specific to dementia (e.g., delirium, hydrocephalus, and age-related physical debility).
Outcomes
We first assessed the annual incidence of hospitalizations for all causes and for potentially preventable conditions. The latter included injuries, acute ACSCs, and chronic ACSCs. Hospitalizations for injuries were defined by the principal discharge diagnosis using AHRQ Clinical Classification Software categories (multilevel category 16: injuries and poisonings) and included fractures, other traumatic injuries (e.g., dislocations and traumatic brain injury), poisonings, and other injuries (e.g., choking and hypothermia).25,26 ACSCs were defined based on AHRQ prevention quality indicators and in accordance with prior studies.18,27,28 Chronic ACSCs included hypertension, congestive heart failure, diabetes and related complications, and COPD/asthma.27 Acute ACSCs included community-acquired pneumonia, UTI, dehydration, and sepsis.
We next examined national trends in all-cause hospitalizations and hospitalizations for potentially preventable conditions, overall and by admission source. Multiple recent national health policy interventions have sought to reduce hospital transfers from nursing homes for ACSCs.16–18 Thus we hypothesized that across the same conditions, admissions from non-acute care facilities would decline more than admissions from the community. The NIS uses reported point of origin and admission source codes provided by states to categorize the admission source for each hospitalization as not transferred (admitted from the community), transferred from an acute care hospital, transferred from non-acute care facilities (including skilled nursing, other non-acute care facility, and home health care), or unknown source.
Third, we examined outcomes related to hospital care: length of stay, performance of invasive procedures, inpatient mortality, discharge disposition, and hospitalization costs. Invasive procedures of interest included gastrostomy, tracheostomy, and intubation and ventilation. ICD procedure codes grouped by AHRQ Clinical Classification Software categories were used to identify procedures (Supplementary Table S2).25,26 Hospital costs were estimated based on reported hospital charges, using the Healthcare Cost and Utilization Project (HCUP)’s annual cost-to-charge ratio files.29
Finally, to explore the impact of residence before hospitalization on discharge disposition, we present discharge dispositions over time, overall and stratified by admission source. Discharge disposition included inpatient death, discharge home, discharge with home health, discharge to a non-acute care facility (defined by HCUP as skilled nursing facilities, intermediate care facilities, long-term care hospitals, inpatient hospice, and psychiatric hospitals), transfer to different acute care hospital, discharge against medical advice, and unknown.
Statistical Analysis
We present descriptive characteristics of all-cause hospitalizations and hospitalizations for potentially preventable conditions among older adults with diagnosed dementia.
Trends in hospitalizations are presented overall, by category (acute ACSCs, chronic ACSCs, injuries, and other conditions) and for conditions within ACSCs and injuries. Logistic regression was used to test for trend across years. Trends in hospitalizations are presented separately for patients admitted from the community and for those transferred from a non-acute care health facility.
Trends in hospital care outcomes are presented for all-cause hospitalizations and hospitalizations for potentially preventable conditions. Median costs of hospitalization were inflation adjusted to 2012 dollars to allow for assessment of trends. Total annual costs are presented in unadjusted dollars. Discharge disposition is presented for all-cause hospitalizations stratified by admission source and by condition category.
Even in ideal circumstances, not all hospitalizations for potentially preventable conditions are avoidable. To address this we conducted a sensitivity analysis to estimate the number of hospitalizations and related costs that might be saved if initiatives to reduce hospitalizations of older adults with dementia successfully prevented 25% to 75% of hospitalizations for potentially preventable conditions.
All analyses were conducted using Stata survey procedures v.14.1 to account for the complex sampling design of NIS. All analyses were weighted to compute national estimates of trends with 95% confidence intervals. Statistical significance of trends was assessed at the two-sided α = .05 level. Because the NIS data used for these analyses are fully deidentified and were not collected solely for this study, this project is not considered human subjects research and thus did not require institutional review.
RESULTS
We identified 1,853,632 hospital discharges of older adults with a diagnosis of dementia between 2012 and 2016, representing an estimated 9.27 million hospitalizations nationwide. We excluded 813 hospitalizations that were missing data for key factors such as principal discharge diagnosis (n = 234), sex (n = 242), and length of stay (n = 337).
Table 1 shows the characteristics of the all-cause and potentially preventable hospitalization cohorts. After survey weighting, the cohort included 9,268,157 all-cause hospitalizations of which 40.1% were for potentially preventable conditions. The mean age of hospitalized patients was 82.6 years (standard deviation [SD] = 6.7), 61% were female, and 93% had Medicare as the primary payer.
Table 1.
Characteristics of Hospitalizations of Older Adults with Diagnosed Dementia
| All hospitalizations | Hospitalizations for potentially preventable conditionsa | |
|---|---|---|
| Unweighted, n | 1,853,632 | 743,972 |
| Weighted, n | 9,268,157 | 3,719,859 |
| Age, mean (SD) | 82.6 (6.7) | 83.3 (6.5) |
| Female, n (weighted %) | 1,138,086 (61.4) | 479,096 (64.4) |
| Race, n (weighted %) | ||
| White | 1,341,932 (72.4) | 549,626 (73.9) |
| Black | 220,956 (11.9) | 78,094 (10.5) |
| Hispanic | 128,533 (7) | 51,979 (7.0) |
| Asian/Pacific Islander | 41,091 (2.2) | 17,683 (2.4) |
| Native American | 6,157 (.3) | 2,416 (.3) |
| Other | 40.902 (2.2) | 15,844 (2.1) |
| Missing | 73,061 (3.9) | 28,330 (3.8) |
| Primary payer, n (weighted %) | ||
| Medicare | 1,717,770 (92.7) | 691,815 (93.0) |
| Medicaid | 24,030 (1.3) | 9,277 (1.2) |
| Private insurance | 83,187 (4.5) | 31,133 (4.3) |
| Self-pay | 6,346 (.3) | 2,391 (.3) |
| No charge | 301 (<.1) | 108 (<.1) |
| Other | 21,998 (1.2) | 8,248 (1.1) |
| Admission source, n (weighted %) | ||
| Community | 1,586,548 (85.6) | 639,516 (86.0) |
| Acute care hospital (transfer) | 84,432 (4.6) | 25,159 (3.4) |
| Non-acute care facility or home health | 171,280 (9.2) | 75,043 (10.1) |
| Unknown | 11,372 (.6) | 4,254 (.6) |
| Received ED care, n (weighted %) | 1,455,115 (78.5) | 625,334 (84.1) |
| Elective hospitalization, n (weighted %) | 149,723 (8.1) | 32,653 (4.4) |
| Selected comorbidities, n (weighted %) | ||
| Hypertension | 1,497,655 (75.9) | 546,804 (73.5) |
| Diabetes | 571,753 (30.8) | 227,514 (37.6) |
| Congestive heart failure | 488,025 (26.3) | 221,673 (29.8) |
| Renal failure | 487,685 (26.3) | 201,084 (27.0) |
| Chronic obstructive pulmonary disease | 452,960 (24.4) | 194,565 (26.2) |
| Cancer | 78,218 (4.2) | 25,811 (4.7) |
| Elixhauser comorbidity score, median (IQR) | 4 (3–5) | 4 (3–5) |
Note: Unweighted sample sizes are shown with weighted proportions.
Abbreviations: ED, emergency department; IQR, interquartile range; SD, standard deviation.
Hospitalizations for potentially preventable conditions include those for injuries, acute ambulatory care sensitive conditions (ACSCs), and chronic ACSCs.
Figure 1 depicts trends in hospitalizations from 2012 and 2016, during which time the incidence of all-cause hospitalizations declined from 1.87 million to 1.85 million (P = .04), driven by a decline in non-potentially preventable conditions (1.13 million to .98 million; P < .001). The incidence of all-cause hospitalizations and hospitalizations for potentially preventable conditions increased from .75 million in 2012 to .87 million in 2016 (P < .001), with an increase in hospitalizations for acute ACSCs (from .38 million to .48 million; P < .001), a decline in chronic ACSCs (from .16 to .15 million; P < .001), and no significant change in injuries (.17 million to .19 million; P = .84) (Figure 1B). Figure 1C shows trends in individual ACSCs; there was a large increase in hospitalizations for sepsis and modest increases in heart failure and dehydration. Hospitalizations for UTIs, pneumonia, COPD, and diabetes decreased during the study period. Figure 1D shows trends in the incidence of hospitalizations for individual injury categories, all of which increased over the study period. Most of the injury hospitalizations were for fractures.
Figure 1.
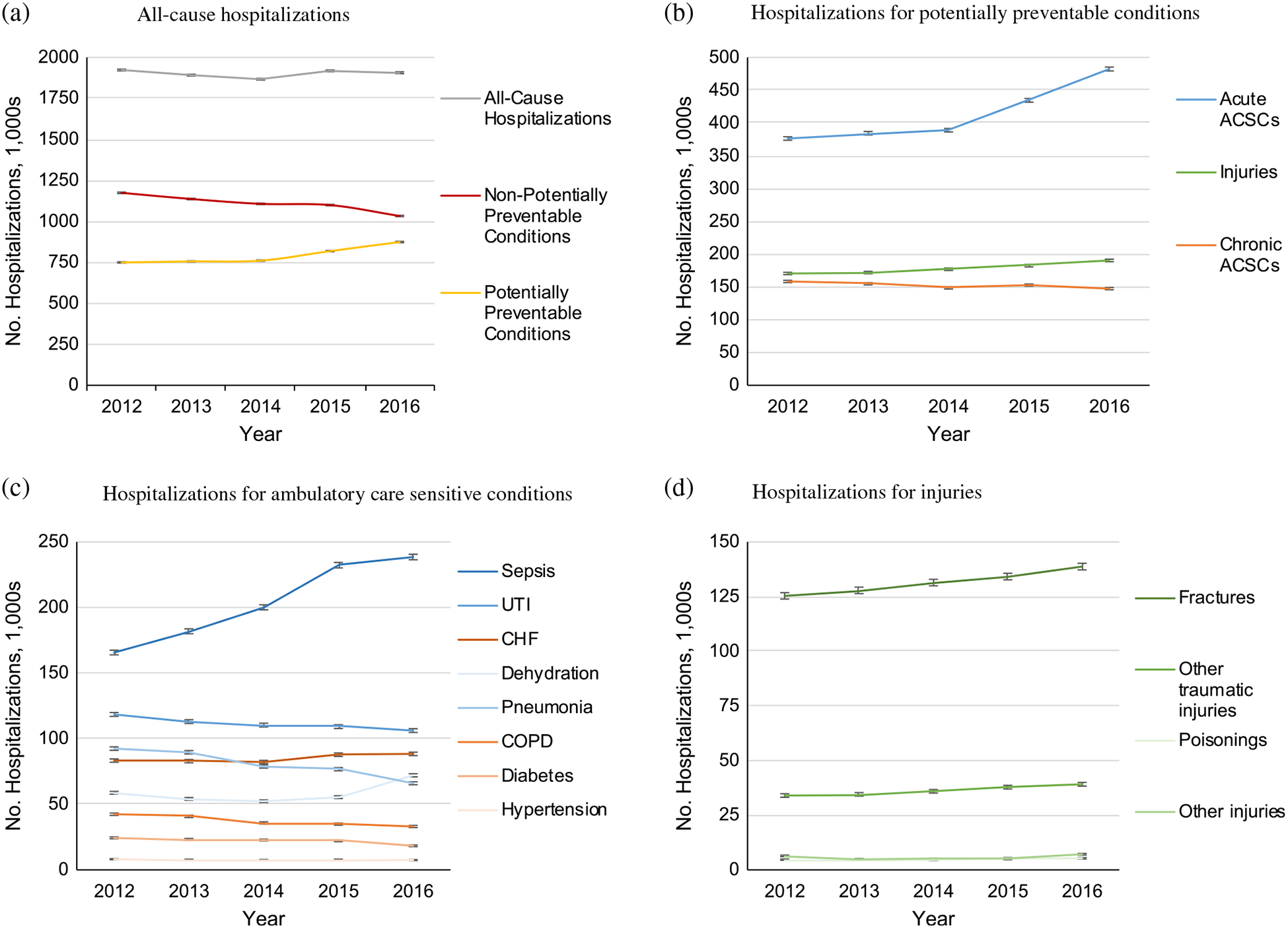
Trends in hospitalizations of older adults with diagnosed dementia, 2012 to 2016. (a) All-cause hospitalizations. (b) Hospitalizations for potentially preventable conditions. (c) Hospitalizations for ambulatory care sensitive conditions (ACSCs). (d) Hospitalizations for injuries. Note: Potentially preventable conditions include injuries, acute ACSCs, and chronic ACSCs. Non-potentially preventable conditions include all other conditions. Acute ACSCs (shown in blue) include sepsis, urinary tract infection, pneumonia, and dehydration. Chronic ACSCs (shown in red) include congestive heart failure, chronic obstructive pulmonary disease, diabetes, and hypertension. Injuries (shown in green) include fractures, other traumatic injuries, poisonings, and other injuries. All data are weighted to be nationally representative. Error bars indicate 95% confidence intervals. Panel A: P = .04 for all-cause hospitalizations, P < .001 for potentially preventable conditions, P < .001 for non-potentially preventable conditions. Panel (B): P = <.001 for acute ACSC; P = .84 for injuries and P < .001 for chronic ACSCs. Panel (C): All trends statistically significant (P < .001), except for hypertension (P = .06). Panel (D): P < .001 for fractures, P < .001 for other traumatic injuries, P = .004 for poisonings, and P < .001 for other injuries.
Figure 2 depicts trends in hospitalizations by older adults’ location before hospitalization. Most patients were admitted from the community (86%), with 9% admitted from non-acute care facilities or home health and 5% transferred from another acute care hospital (Figure 2A). Trends in reasons for hospitalization are presented for patients admitted from the community (Figure 2B) and from non-acute care facilities (Figure 2C). There was a decline in non-potentially preventable hospitalizations for both patients admitted from the community and those admitted from non-acute care facilities (P < .001 for both). There was a rise in hospitalizations for potentially preventable conditions among patients admitted from the community, driven by a rise in hospitalizations for acute ACSCs (P < .001). In contrast, that was a decline in hospitalizations for potentially preventable conditions for patients transferred from non-acute care facilities, driven by a decline in hospitalizations for chronic ACSCs (P < .001).
Figure 2.
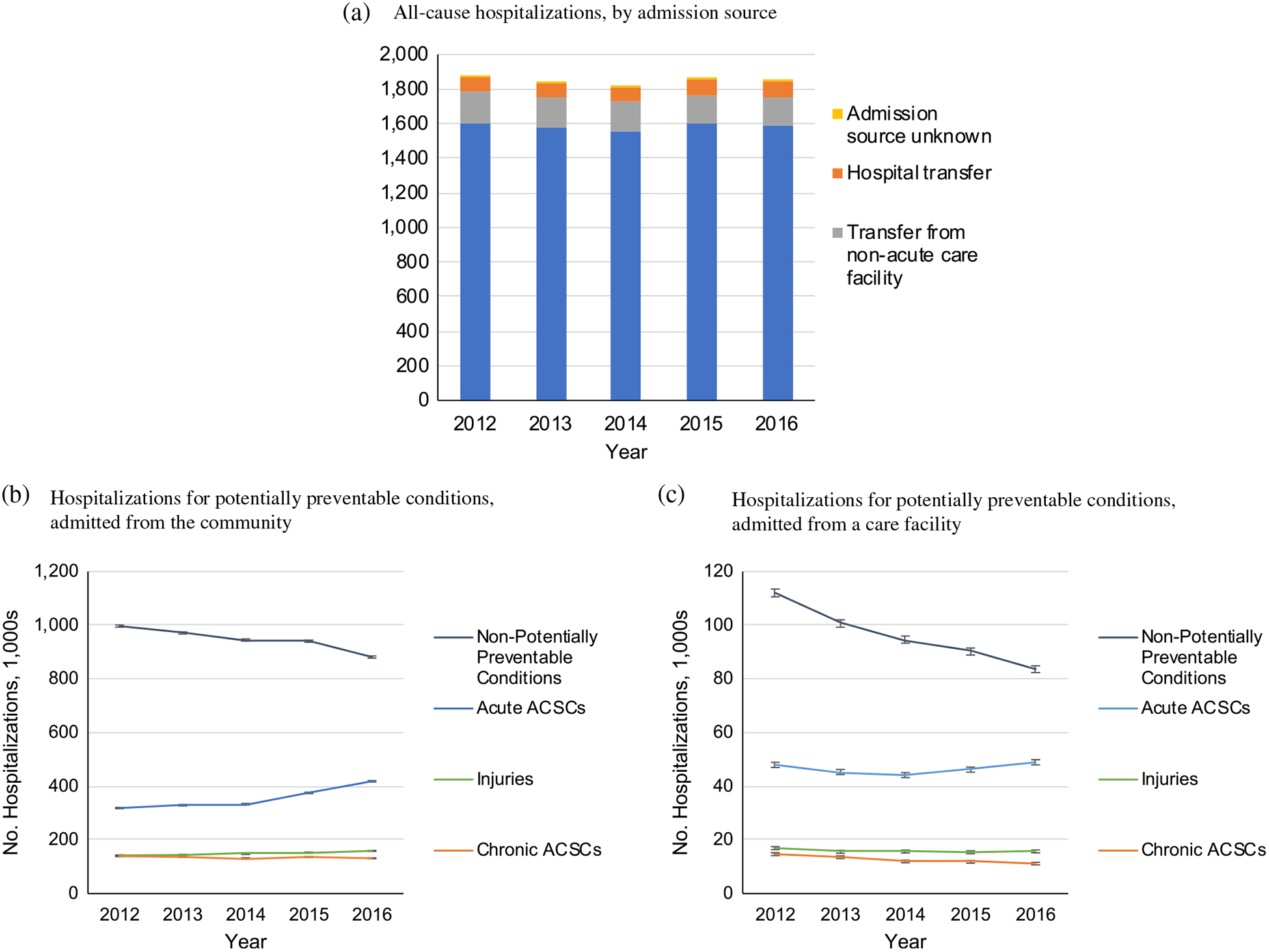
Trends in hospitalizations of older adults with diagnosed dementia, by admission source. (a) All-cause hospitalizations, by admission source. (b) Hospitalizations for potentially preventable conditions, admitted from the community. (c) Hospitalizations for potentially preventable conditions, admitted from a care facility. ACSC, ambulatory care sensitive condition. Note: Preventable conditions include injuries, acute ambulatory care sensitive conditions (ACSCs), and chronic ACSCs. Acute ACSCs include sepsis, urinary tract infection, pneumonia, and dehydration. Chronic ACSCs include congestive heart failure, chronic obstructive pulmonary disease, diabetes, and hypertension. Injuries include fractures, other traumatic injuries, medical and surgical complications, poisonings, and other injuries. Non-acute care facilities include skilled nursing, other non-acute care facility, and home health care. All data are weighted to be nationally representative. Error bars indicate 95% confidence intervals. Panel (A): All trends statistically significant (P < .001) except for admissions from source unknown (P = .80). Panel (B): All trends statistically significant (P < .001) except for injuries (P = .85). Panel (C): All trends statistically significant (P < .001).
Table 2 shows outcomes of hospital care. For all-cause hospitalizations, but not hospitalizations for potentially preventable conditions, there was a small but significant decline in the incidence of gastrostomy procedures (1.8%–1.5%; P < .001) and an increase in use of intubation and ventilation (3.3%–3.6%; P < .001). Inflation-adjusted median costs increased for both all-cause hospitalizations ($7,405 in 2016; interquartile range [IQR] = $4,667–$12,394) and hospitalizations for potentially preventable conditions ($7,543 in 2016; IQR = $4,733–$12,511).
Table 2.
Clinical Outcomes and Costs of Hospitalizations of Older Adults with Diagnosed Dementia
| 2012 | 2013 | 2014 | 2015 | 2016 | P value | |
|---|---|---|---|---|---|---|
| All-cause hospitalizations | ||||||
| Unweighted, n | 375,786 | 369,435 | 364,182 | 373,714 | 370,515 | |
| Length of stay, mean (SD) | 5.9 (6.6) | 5.9 (6.6) | 6.0 (6.9) | 6.0 (7.0) | 6.1 (7.4) | <.001 |
| Invasive procedures | ||||||
| Gastrostomy | 6,890 (1.8) | 6,510 (1.8) | 6,236 (1.7) | 6,246 (1.7) | 5,472 (1.5) | <.001 |
| Intubation and ventilation | 12,399 (3.3) | 12,877 (3.5) | 12,608 (3.5) | 12,986 (3.5) | 13,180 (3.6) | <.001 |
| Tracheostomy | 782 (.2) | 773 (.2) | 759 (.2) | 736 (.2) | 736 (.2) | .18 |
| Costs of hospitalization | ||||||
| Median cost, $, IQRa | 6,965 (4,401–11,625) | 7,060 (4,442–11,789) | 7,033 (4,432–11,737) | 7,196 (4,539–12,046) | 7,405 (4,667–12,394) | <.001 |
| Total cost, billions $b | 19 | 19.2 | 19.2 | 20.5 | 21.3 | |
| Disposition | ||||||
| Non-acute care facility | 206,700 (55.0) | 203,358 (55.0) | 200,789 (55.1) | 203,417 (54.4) | 201,001 (54.2) | <.001 |
| Home | 78,087 (20.8) | 74,184 (20.1) | 72,859 (20.0) | 74,712 (20.0) | 72,438 (19.6) | <.001 |
| Home with home health | 63,695 (16.9) | 64,720 (17.5) | 63,920 (17.6) | 67,620 (18.1) | 69,589 (18.8) | <.001 |
| Died | 18,283 (4.9) | 18,411 (5.0) | 17,995 (4.9) | 18,521 (5.0) | 18,594 (5.0) | .01 |
| Acute care hospital | 7,572 (2.0) | 7,321 (2.0) | 7,124 (2.0) | 7,164 (1.9) | 6,999 (1.9) | <.001 |
| Left against medical advice | 835 (.2) | 757 (.2) | 805 (.2) | 1,842 (.5) | 1,404 (.4) | <.001 |
| Unknown | 523 (.1) | 521 (.1) | 494 (.1) | 155 (<.1) | 138 (<.1) | <.001 |
| Hospitalizations for potentially preventable conditions | ||||||
| Unweighted, n | 141,011 | 142,199 | 142,853 | 153,906 | 164,003 | |
| Length of stay, mean (SD) | 5.6 (5.2) | 5.6 (5.3) | 5.6 (5.3) | 5.7 (5.6) | 5.7 (6.0) | <.001 |
| Invasive procedures | ||||||
| Gastrostomy | 2,088 (1.5) | 2,063 (1.5) | 2,072 (1.5) | 2,251 (1.5) | 2,284 (1.4) | .08 |
| Intubation and ventilation | 5,663 (4.0) | 5,953 (4.2) | 6,038 (4.2) | 6,572 (4.3) | 6,691 (4.1) | .25 |
| Tracheostomy | 368 (.3) | 364 (.3) | 373 (.3) | 362 (.2) | 378 (.2) | .04 |
| Costs of hospitalization | ||||||
| Median cost, $, IQRa | 7,319 (4,581–12,212) | 7,446 (4,625–12,355) | 7,430 (4,585–12,324) | 7,537 (4,707–12,531) | 7,543 (4,733–12,511) | <.001 |
| Total cost, billions $b | 7.4 | 7.6 | 7.7 | 8.6 | 9.3 | |
| Disposition | ||||||
| Non-acute care facility | 84,350 (59.8) | 84,895 (59.7) | 85,427 (59.8) | 90,037 (58.5) | 95,169 (58.1) | <.001 |
| Home | 22,888 (16.2) | 22,578 (15.9) | 22,577 (15.8) | 24,699 (16.1) | 25,917 (15.8) | .02 |
| Home with home health | 22,284 (15.8) | 23,063 (16.2) | 23,178 (16.2) | 26,247 (17.1) | 29,714 (18.1) | <.001 |
| Died | 8,970 (6.4) | 9,146 (6.4) | 9,083 (6.4) | 9,770 (6.4) | 10,006 (6.1) | .005 |
| Acute care hospital | 2,069 (1.5) | 2,047 (1.4) | 2,111 (1.5) | 2,230 (1.5) | 2,354 (1.4) | .56 |
| Left against medical advice | 224 (.2) | 209 (.1) | 208 (.1) | 744 (.5) | 570 (.3) | <.001 |
| Unknown | 196 (.1) | 216 (.2) | 199 (.1) | 58 (<.1) | 61 (<.1) | <.001 |
Note: Unweighted sample sizes are shown with weighted proportions.
Abbreviations: IQR, interquartile range; SD, standard deviation.
Inflation adjusted to 2012 dollars.
Not adjusted for inflation.
In 2016, total hospital costs for older adults with diagnosed dementia were $21.3 billion for all-cause hospitalizations and $9.3 billion for hospitalizations for potentially preventable conditions. In sensitivity analyses, varying the estimated proportion of hospitalizations of older adults with dementia that are actually preventable from 25% to 75% resulted in an estimated number of hospitalizations of 205,004 to 615,011 and estimated cost of $2.3 billion to $7.0 billion.
Disposition following hospitalization is shown in Table 2 and Figure 3. Inpatient mortality increased from 4.9% to 5.0% for all-cause hospitalizations and decreased from 6.4% to 6.1% for hospitalizations for potentially preventable conditions. There was a small decline in discharge to non-acute care facilities and discharge home that was largely offset by an increase in discharge home with home health services. Among patients admitted from the community, more than half were discharged to non-acute care facilities (Figure 3A). Most of the patients hospitalized for injuries (77%), acute ACSCs (56%), and nonpreventable conditions (51%) were discharged to non-acute care facilities (Figure 3B).
Figure 3.
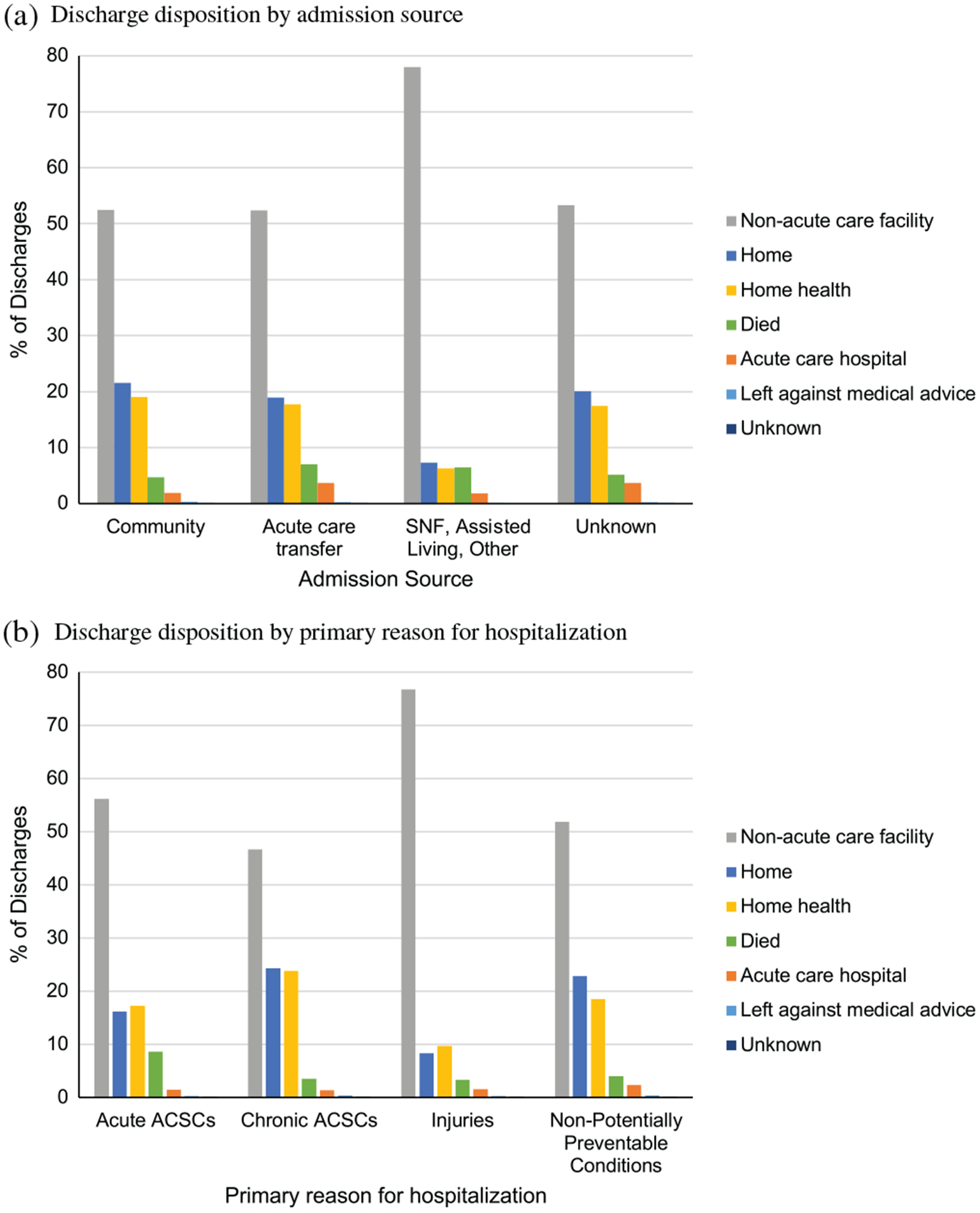
Discharge disposition of older adults with diagnosed dementia. (a) Discharge disposition by admission source. (b) Discharge disposition by primary reason for hospitalization. Note: Non-acute care facilities include skilled nursing facilities, intermediate care facilities, long-term care hospitals, inpatient hospice, and psychiatric hospitals. ACSC, ambulatory care sensitive condition; SNF, skilled nursing facility.
DISCUSSION
In this study of hospitalized older adults with diagnosed dementia, 40% of hospitalizations were for potentially preventable conditions, and although the national incidence of all-cause hospitalizations declined between 2012 and 2016, the incidence of hospitalizations for potentially preventable conditions increased. The increase in potentially preventable hospitalizations was largely driven by a greater number of hospitalizations for sepsis, injuries, and dehydration among community-dwelling older adults. Sequelae of hospitalizations for potentially preventable conditions included a 6% inpatient mortality rate, annual total costs exceeding $10 billion, and frequent discharge to non-acute care facilities. These findings indicate the urgent need for improved strategies to prevent, detect, and treat potentially preventable conditions in older adults with dementia before they require hospitalization.
Prior research has examined hospitalizations for potentially preventable conditions among older adults with dementia transferred from nursing facilities.18,30 The modest decline in transfers from nursing homes to hospitals observed in the current study is consistent with this prior research and may reflect the targeting of nursing home transfers to hospitals by both CMS policy initiatives16,17 and quality improvement programs.31 Although promising, these findings must be interpreted with the context that most older adults with dementia reside in the community, supported by family caregivers. Thus the observed increase in hospitalizations for potentially preventable conditions among community-dwelling older adults with dementia is highly concerning.
Not all ACSCs and injuries are ultimately preventable. However, improving early access to high-quality outpatient care could reduce the hundreds of thousands of potentially preventable hospitalizations observed in the current study.32,33 Our sensitivity analyses indicate a 25% reduction in potentially preventable hospitalizations of older adults with dementia that would result in annual savings of more than $2 billion. Access to high-quality primary care allows for detection and treatment of acute new problems and early decompensation of chronic conditions before they become severe enough to require hospital care.34,35 Ambulatory interventions may also impact injury rates through early recognition of gait and balance problems, reducing polypharmacy and related fall risks, and treating osteoporosis. Although all patients residing in nursing homes have access to an on-site primary care provider, access to primary care may be a major barrier for community-dwelling patients with dementia. National trends demonstrate a reduction in density of primary care physicians, particularly in rural areas,3 and a national shortage of geriatricians.36 Beyond access to primary care, continuity of care may be particularly important for reducing hospitalizations of patients with dementia.37,38
The observed high rates of hospitalizations for potentially preventable conditions may in part be due to the cognition and speech deficits faced by patients with dementia that may impair their awareness of symptoms, ability to seek care, and ability to manage chronic conditions. Resultant communication barriers may make early detection of health problems more challenging due to delays in seeking care and difficulties diagnosing the underlying cause of behavioral changes or nonspecific symptoms such as fatigue or insomnia.39,40 Overcoming these challenges will require widespread uptake of innovative outpatient care models for patients with dementia. Collaborative care models that include interdisciplinary teams with frequent patient contact and caregiver involvement were shown to improve the quality of ambulatory dementia care41,42 and may reduce healthcare utilization and ultimately be cost saving to the health system.43,44
Adding to the importance of reducing potentially preventable hospitalizations among older adults with dementia is our finding that most previously community-dwelling patients with dementia are discharged to non-acute care facilities. High rates of discharge to non-acute care facilities may reflect increased rates of hospitalization-related complications such as functional impairment and delirium6–8 and may also reflect caregiver stress.45 Most patients discharged to nursing facilities stay for more than a month, and many ultimately do not return home.46,47 Thus potentially preventable hospitalizations may be an important inflection point in patients’ overall care trajectory, and successful efforts to reduce hospitalizations of patients with dementia who reside at home may prevent or delay their transition to residence at a nursing facility.
Limitations
This study has several limitations. First, consistent with prior studies, we relied on hospital diagnosis coding to identify patients diagnosed with dementia; this approach underestimates the prevalence of dementia and does not provide information on severity of dementia.20,21 Although we used diagnosis codes specific to dementia, they are not sensitive for mild cognitive impairment that frequently goes undiagnosed in outpatient settings48 and may be misdiagnosed as delirium during hospitalization. Second, the design of the NIS allows for examination at the hospital-discharge level and does not provide unique patient identifiers, rendering us unable to estimate national rates of hospitalizations of patients with and without dementia because one patient may contribute to multiple hospitalizations. Third, given our study population, findings may not be generalizable to younger adults with dementia or to patients hospitalized at federal hospitals such as Veterans Affairs and military hospitals that are not included in the NIS. Lastly, the NIS does not capture stays for observation that was shown to increase over time, particularly for chronic ACSCs,49 and may represent additional hospital-based care received by older adults with dementia.
In conclusion, between 2012 and 2016, 40% of hospitalizations of older adults with dementia were for potentially preventable conditions. Although the number of all-cause hospitalizations decreased, the number of hospitalizations for potentially preventable conditions increased, driven by hospitalizations of community-dwelling older adults with dementia. These findings highlight the importance of injury prevention and early detection and goal-directed treatment of ACSCs as key areas for future efforts to improve ambulatory care and reduce hospitalizations for older adults with dementia.
Supplementary Material
Supplementary Table S1: Dementia Diagnosis Codes
Supplementary Table S2: Invasive Procedure Codes.
ACKNOWLEDGMENTS
Financial Disclosure: Timothy S. Anderson was supported by grants from the National Institute on Aging (NIA) (L30AG060493 and R03AG064373). Shoshana J. Herzig was supported by K23AG042459 from the NIA. Edward R. Marcantonio is supported by K24 AG035075 from the NIA. Ellen P. McCarthy is supported by the NIA under Award No. U54AG063546 that funds NIA Imbedded Pragmatic Alzheimer’s Disease and AD-Related Dementias Clinical Trials Collaboratory (NIA IMPACT Collaboratory). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sponsor’s Role: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest: The authors have declared no conflicts of interest for this article.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA. 2012;307(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng Z, Coots LA, Kaganova Y, Wiener JM. Hospital and ED use among Medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff (Millwood). 2014;33(4):683–690. [DOI] [PubMed] [Google Scholar]
- 4.Shepherd H, Livingston G, Chan J, Sommerlad A. Hospitalisation rates and predictors in people with dementia: a systematic review and meta-analysis. BMC Med. 2019;17(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, Medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187–194. [DOI] [PubMed] [Google Scholar]
- 6.Fick DM, Steis MR, Waller JL, Inouye SK. Delirium superimposed on dementia is associated with prolonged length of stay and poor outcomes in hospitalized older adults. J Hosp Med. 2013;8(9):500–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillick MR, Serrell NA, Gillick LS. Adverse consequences of hospitalization in the elderly. Soc Sci Med. 1982;16(10):1033–1038. [DOI] [PubMed] [Google Scholar]
- 8.Mecocci P, von Strauss E, Cherubini A, et al. Cognitive impairment is the major risk factor for development of geriatric syndromes during hospitalization: results from the GIFA study. Dement Geriatr Cogn Disord. 2005;20(4):262–269. [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldwater DS, Dharmarajan K, McEwen BS, Krumholz HM. Is Post-hospital Syndrome a Result of Hospitalization-Induced Allostatic Overload?. Journal of Hospital Medicine. 2018;13(5). 10.12788/jhm.2986. [DOI] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality. Prevention quality indicators technical specifications. 2019. https://www.qualityindicators.ahrq.gov/Modules/PQI_TechSpec_ICD10_v2019.aspx. Accessed February 20, 2020.
- 12.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc. 2010;58(4):627–635. [DOI] [PubMed] [Google Scholar]
- 13.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible Medicare and medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc. 2012;60(5):821–829. [DOI] [PubMed] [Google Scholar]
- 14.Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. 2013;14(5):706–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the hospital readmission reduction program and readmission rates for target and nontarget conditions. JAMA. 2016;316(24):2647–2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ingber MJ, Feng Z, Khatutsky G, et al. Initiative to reduce avoidable hospitalizations among nursing facility residents shows promising results. Health Aff (Millwood). 2017;36(3):441–450. [DOI] [PubMed] [Google Scholar]
- 17.Feng Z, Ingber MJ, Segelman M, et al. Nursing facilities can reduce avoidable hospitalizations without increasing mortality risk for residents. Health Aff (Millwood). 2018;37(10):1640–1646. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy EP, Ogarek JA, Loomer L, et al. Hospital Transfer Rates Among US Nursing Home Residents With Advanced Illness Before and After Initiatives to Reduce Hospitalizations. JAMA Internal Medicine. 2020;180(3): 385 10.1001/jamainternmed.2019.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rudolph JL, Zanin NM, Jones RN, et al. Hospitalization in community-dwelling persons with Alzheimer’s disease: frequency and causes. J Am Geriatr Soc. 2010;58(8):1542–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beydoun MA, Beydoun HA, Gamaldo AA, et al. Nationwide inpatient prevalence, predictors, and outcomes of Alzheimer’s disease among older adults in the United States, 2002–2012. J Alzheimers Dis. 2015;48(2):361–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beydoun MA, Gamaldo AA, Beydoun HA, Shaked D, Zonderman AB, Eid SM. Trends, predictors, and outcomes of healthcare resources used in patients hospitalized with Alzheimer’s disease with at least one procedure: the Nationwide Inpatient Sample. J Alzheimers Dis. 2017;57(3): 813–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Godard-Sebillotte C, Le Berre M, Schuster T, Trottier M, Vedel I. Impact of health service interventions on acute hospital use in community-dwelling persons with dementia: a systematic literature review and meta-analysis. PLoS One. 2019;14(6):e0218426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–1551. [DOI] [PubMed] [Google Scholar]
- 24.Centers of Medicare & Medicaid Services. Chronic conditions warehouse. 2019. https://www2.ccwdata.org/web/guest/condition-categories. Accessed January 17, 2020.
- 25.Healthcare Cost and Utilization Project. Clinical Classification Software (CCS) for ICD-9-CM. 2017. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed January 16, 2020.
- 26.Healthcare Cost and Utilization Project. Clinical Classification Software (CCS) for ICD-10-CM (Beta Version). 2019. http://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed January 16, 2020.
- 27.Agency for Healthcare Research and Quality. Prevention quality indicators overview. 2019. https://www.qualityindicators.ahrq.gov/Modules/pqi_resources.aspx. Accessed January 16, 2020.
- 28.Walsh EG, Wiener JM, Haber S, Bragg A, Freiman M, Ouslander JG. Potentially avoidable hospitalizations of dually eligible Medicare and Medicaid beneficiaries from nursing facility and home- and community-based services waiver programs. J Am Geriatr Soc. 2012;60(5):821–829. [DOI] [PubMed] [Google Scholar]
- 29.Healthcare Cost and Utilization Project. Cost-to-Charge Ratio Files. 2019. https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed January 16, 2020.
- 30.Givens JL, Selby K, Goldfeld KS, Mitchell SL. Hospital transfers of nursing home residents with advanced dementia. J Am Geriatr Soc. 2012;60(5): 905–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ouslander JG, Bonner A, Herndon L, Shutes J. The interventions to reduce acute care transfers (INTERACT) quality improvement program: an overview for medical directors and primary care clinicians in long term care. J Am Med Dir Assoc. 2014;15(3):162–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health. JAMA. 2011;305(20):2096–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lyketsos CG. Prevention of unnecessary hospitalization for patients with dementia: the role of ambulatory care. JAMA. 2012;307(2):197–198. [DOI] [PubMed] [Google Scholar]
- 34.Chang CH, O’Malley AJ, Goodman DC. Association between temporal changes in primary care workforce and patient outcomes. Health Serv Res. 2017;52(2):634–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basu S, Berkowitz SA, Phillips RL, Bitton A, Landon BE, Phillips RS. Association of primary care physician supply with population mortality in the United States, 2005–2015. JAMA Intern Med. 2019;179(4):506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. National and Regional Projections of Supply and Demand for Geriatricians. Rockville, MD: USDHHS: National Center for Health Workforce Analysis; 2017:2013–2025. [Google Scholar]
- 37.Amjad H, Carmichael D, Austin AM, Chang CH, Bynum JP. Continuity of care and health care utilization in older adults with dementia in fee-for-service Medicare. JAMA Intern Med. 2016;176(9):1371–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J Manag Care. 2019;25(4):e126–e134. [PubMed] [Google Scholar]
- 39.Harris DP, Chodosh J, Vassar SD, Vickrey BG, Shapiro MF. Primary care providers’ views of challenges and rewards of dementia care relative to other conditions. J Am Geriatr Soc. 2009;57(12):2209–2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chodosh J, Mittman BS, Connor KI, et al. Caring for patients with dementia: how good is the quality of care? Results from three health systems. J Am Geriatr Soc. 2007;55(8):1260–1268. [DOI] [PubMed] [Google Scholar]
- 41.Callahan CM, Boustani MA, Unverzagt FW, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care: a randomized controlled trial. JAMA. 2006;295(18):2148–2157. [DOI] [PubMed] [Google Scholar]
- 42.Vickrey BG, Mittman BS, Connor KI, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145(10):713–726. [DOI] [PubMed] [Google Scholar]
- 43.Jennings LA, Laffan AM, Schlissel AC, et al. Health care utilization and cost outcomes of a comprehensive dementia care program for Medicare beneficiaries. JAMA Intern Med. 2019;179(2):161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Boustani MA, Sachs GA, Alder CA, et al. Implementing innovative models of dementia care: the healthy aging brain center. Aging Ment Health. 2011; 15(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leggett AN, Polenick CA, Maust DT, Kales HC. Falls and hospitalizations among persons with dementia and associated caregiver emotional difficulties. Gerontologist. 2018;58(2):e78–e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Makam AN, Tran T, Miller ME, Xuan L, Nguyen OK, Halm EA. The clinical course after long-term acute care hospital admission among older Medicare beneficiaries. J Am Geriatr Soc. 2019;67(11):2282–2288. [DOI] [PubMed] [Google Scholar]
- 47.MedPAC. Report to the Congress: Medicare Payment Policy Chapter 8: Skilled nursing facility services. March 2019. http://www.medpac.gov/docs/default-source/reports/mar19_medpac_ch8_sec.pdf. Accessed March 10, 2020.
- 48.Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Figueroa JF, Burke LG, Zheng J, Orav EJ, Jha AK. Trends in hospitalization vs observation stay for ambulatory care-sensitive condition. JAMA Intern Med. 2019;179(12):1714–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Dementia Diagnosis Codes
Supplementary Table S2: Invasive Procedure Codes.


