Abstract
The COVID-19 pandemic has led to increased staffing needs in emergency departments. The question quickly arose as to whether it was appropriate to offer medical students the opportunity to assist this staff. The dilemma stems in part from the potential impact on their psychological well-being as well as their academic and clinical performances. We sought to determine the level of anxiety of medical students during the COVID-19 outbreak, and whether it was higher among the students who chose to return to the clinical setting, especially in first-line units (i.e., emergency departments and resuscitation units). In May 2020, 1180/1502 (78.5%) undergraduate medical students at Strasbourg Medical School (France) completed a questionnaire assessing their anxiety and clinical experience. A 2018 cohort of undergraduate medical students served as the baseline. The 2020 COVID cohort had higher rates of anxiety than the 2018 cohort. This difference was specifically observed in the students who chose not to return to the clinical setting during the crisis (N = 684, 59%). At linear regression, the main factors associated with anxiety were gender (p < 0.005) and perceived clinical activity personal conditions (p < 0.001). Employment site, including COVID first-line units, was not correlated with anxiety. Working in the clinical setting during the COVID-19 outbreak is not a risk factor for anxiety in medical students. Instead, it is an active coping strategy, suggesting that there are no barriers to allowing students to return to clinical settings during a pandemic, including first-line units, in terms of their psychological well-being.
Keywords: Anxiety, COVID-19, Clinical placements, Coping
Introduction
The coronavirus 2019 (COVID-19) outbreak has led to a sudden and considerable increase in human needs in acute hospital wards, particularly in emergency departments. The health and academic authorities were confronted early on with the issue of whether or not to allow undergraduate students to assist healthcare professionals with COVID-19 patients [1]. In the United States, Canada, United Kingdom, and France, as in many other countries, the authorities also decided to allow undergraduate students to return to the clinical setting on a voluntary basis [2–5].
Yet, the debate about whether or not to allocate medical students to COVID-19 first-line units is still ongoing. It is notably underpinned by psychological concerns, particularly related to the anxiety-provoking nature of the situation [6]. Anxiety is a natural emotional reaction to a stressful situation characterized by feelings of tension, worry, or apprehension, which function is to alert to potential threats, allowing the person to evaluate and respond in appropriate ways [7]. In case of inadequate response, high and persistent anxiety levels can negatively impact students’ academic performance, increase the risk of dropping out, decrease empathy, and lead to over-consumption of alcohol and drugs [8, 9]. Furthermore, anxious undergraduate students often become anxious residents and then anxious practitioners, potentially impairing performance and increasing errors [10, 11].
The COVID-19 pandemic is commonly reported as impacting anxiety among medical students owing to the disruption of academic and clinical activities, and to the redeployment of some students into COVID-related clinical activities [12–15]. Two COVID-19-related studies found that the rates of medical students showing signs of anxiety ranged from 25 to 50% [12, 16]. Beyond the wide range of the estimate, these studies did not examine the role of clinical activity, especially in COVID-19 first-line units, even though it could be a major determinant of anxiety in this type of event [17, 18]. They are also criticized for the lack of pre-COVID-19 comparison points [19].
Public health crisis related to emerging infections will become increasingly common in the coming years [20]. It is, therefore, crucial that health and academic authorities use the COVID-19 experience to improve their response capability. The aim of this study was to examine the clinical activity of undergraduate medical students in a COVID-19 hotspot and its association with anxiety. With more than 65,000 dead at the beginning of January, 2021, France is the seventh most affected country. Strasbourg and the Great East region were the initial epicenter and the most intense spot of COVID-19 circulation in France. We sought to determine whether the COVID-19 outbreak made undergraduate medical students anxious, and in particular whether allowing medical students to return to the clinical setting in COVID-19 first-line units was a risk factor for anxiety.
Methods
Study design and sample
Between May 7 and 17, 2020, we conducted a multi-institutional cross-sectional study. We recruited all undergraduate students from Strasbourg Medical School in three training stages: 2nd and 3rd year (preclinical, n = 302 and n = 303, respectively), 4th and 5th year (clinical, n = 302 and n = 300, respectively), and 6th year (graduating, with a high-stake final exam in July, n = 302) to complete an online survey. First-year students (n = 1580) were excluded since in France, they are in a selection year. Prior to the COVID-19 outbreak, all of them were allocated to clinical activities on a part-time basis. Those who chose to return working during the pandemic (referred to as “employed students”) were affected in a COVID-related clinical setting according to need, respecting their wishes. Participation in the study was elective, and responses were anonymized. Participants were informed that their completion of the questionnaire indicated their consent to participate in the study. We sent two reminders, at 4- and 8-day intervals after the first distribution, respectively, and student representatives sent reminders on social networks. Ethical approval has been granted by the Institutional Review Board of Strasbourg Medical School.
To address whether medical students were more anxious during the COVID-19 outbreak, we compared the current data with those from a survey conducted from March to May 2018 among all Strasbourg Medical School undergraduates (N = 1471, return rate 86%). The procedure was similar, with no significant changes in learning context.
Measures and survey development
The survey covered demographics (age, gender, year of study) and employment status during the COVID-19 outbreak (allocated to a health facility [employed]; not allocated [unemployed]) as well as clinical experience and anxiety. Clinical experience included employment site (COVID first-line units, i.e., emergency departments and resuscitation units; COVID medical units, i.e., other departments), primary role (usual role, i.e., role usually performed by a medical student; unusual role, i.e., role usually performed by other health professionals), supervision (yes/no), specific training (yes/no), development of new skills (yes/no), and students’ perceptions about their clinical experience.
Since there is no scale to explore perceptions about the clinical experience in times of crisis, we created a new scale—referred to as the “Crisis Experience Rating Scale” (CERS-7)—following the steps described by Artino et al. [21] and Cook et al. [22] for validation. The CERS-7 items, rated on a six-point Likert scale, were retrieved from the instructions of the health and academic authorities regarding the mobilization of medical students during the health crisis [2, 4, 5]. Item content validation was undertaken by an interprofessional panel of ten persons. Principal component analysis (Kaiser–Meyer–Olkin statistic 0.76, p < 0.001, 67% of variance explained) aggregated these items into two factors—factor 1: “CERS-Professional Experience (PROFEX)” subscale, 41% of variance explained (perceived level of preparedness, perceived competence to perform tasks, perceived helpfulness in assisting healthcare professionals treat patients, perceived level of team integration; Cronbach’s alpha = 0.82), and factor 2: “CERS-Personal Experience (PERSEX)” subscale, 26% of variance explained (perceived insecurity about infectious risk, perceived workload, sleep deprivation; Cronbach’s alpha = 0.72). The tool’s overall scale (CERS-7 total) Cronbach’s alpha was 0.75. We used the PROFEX (min = 4, max = 24) and PERSEX (min = 3, max = 18) subscales. The higher the score, the more positively the crisis experience was perceived.
For the outcome variable (anxiety), surveys for both the current and 2018 samples were based on the State–Trait Anxiety Inventory (STAI-Y), widely used to measure anxiety in medical students [11, 24]. We assessed state anxiety using the validated French version of the state anxiety subscale (STAI-A) [23]. It consists of 20 items scored on a four-point Likert scale (1 = yes to 4 = no). The total score (STAI-A Total score) ranges from 20 to 80 with females typically scoring higher than males. The higher the score, the higher the anxiety level. The STAI-A Total scores can be categorized into a three-point cutoff to detect clinically significant symptoms: below 55 (average anxiety), 56–65 (high anxiety), and above 65 (severe anxiety). Persistent high anxiety may require psychological counseling, while persistent severe anxiety must require psychological counseling. Our overall Cronbach’s alpha (α = 0.95) confirmed STAI-A’s excellent internal reliability.
For structured scales, more than 10% of non-response led to participant exclusion.
Data analysis
All analyses were performed with SPSS version 24 (IBM Corp., Armonk, NY, USA). We set statistical significance at p < 0.05 together with 95% confidence intervals (CI) for all inferential tests. We used supporting data analysis and wave analysis to assess non-response bias [24]. We used standard descriptive statistics and analysis of variance or chi-square tests for univariate comparisons to characterize and make comparisons between employed and unemployed students as well as between employment conditions and gender. We used chi-square tests for the comparative analyses with the 2018 survey on STAI-A three-point cutoff frequencies. Adjusted p values for multiple comparisons were calculated using the false discovery rate (fdr) method [25]. We used multivariate analysis of variance (MANOVA) to compare anxiety by employment status, employment sites, and gender. We used linear regression analyses (mean differences) to examine correlates of STAI-A Total score in employed students. We included variables following their clinical relevance [26]. We assessed the normality of residuals graphically using quantile–quantile plots and the Shapiro–Wilk test. We tested collinearity using the variance inlation factor (VIF) 186 and ensuring that no variable had a VIF greater than 2 [22].
Results
Of the 1180 respondents (78.5% response rate), 1165 with complete data on all variables constituted our analytic sample. Of the sample, 760 (65.2%) were females, with no significant differences between training stages. Mean (standard deviation (± SD)) age was 23 years (SD ± 6.3). The gender and age distribution mirrored that of national and local (Strasbourg) medical school data [27]. The results of a wave analysis comparing the gender and age characteristics of last-call participants with others showed no difference between the two groups.
Of the 481 (41.3%) employed students, 315 (64.9%) were females, which corresponds to the gender ratio of unemployed students. The majority were clinical students (375, 78.0%). Table 1 compares the demographic characteristics of employed and unemployed students.
Table 1.
Demographics of employed and unemployed students
| All students | Employed | Unemployed | Mean difference between employed and unemployed [95% CI] | p | |
|---|---|---|---|---|---|
| (n = 1165) | (n = 481) | (n = 684) | |||
| Gender, n (%) | |||||
| Female | 760 (65.2%) | 315 (41.4%) | 445 (58.6%) | − 17.2 [− 18.1; − 16.3] | .924 |
| Male | 405 (34.8%) | 166 (41.0%) | 239 (59.0%) | − 18.0 [− 19.2; − 16.7] | |
| Age, mean/median (± SD [range]) | |||||
| Age | 22.8/22 (± 6.3 [39–18]) | 23.4/23 (± 5.6 [39–19]) | 22.3/22 (± 6.3 [37–18]) | -0.9 [1.0;1.1] | < 0.001 |
| Training stage | |||||
| Preclinical | 531 (45.6%) | 66 (12.4%) | 465 (87.6%) | − 75.2 [− 80.2; − 70.2] | < 0.001 |
| Clinical | 471 (40.4%) | 375 (79.6%) | 96 (20.4%) | 59.2 [63.2; 55.2] | |
| Graduating | 163 (14.0%) | 40 (24.5%) | 123 (75.5%) | − 51.8 [− 57.5; − 46.1] | |
Students had been allocated to 11 hospitals, which included 6 emergency departments and 4 resuscitation units. About half of the students had been allocated to first-line units (243, 50.5%). A majority worked under supervision (416, 86.5%), and two-thirds reported that they received specific training and developed new skills. Overall, students perceived their professional and personal clinical experience as moderately positive. All significant differences between the groups were p < 0.001. There were no significant differences by gender in any of these variables. Table 2 shows students’ employment sites and clinical experience.
Table 2.
Employment sites and clinical experience characteristics
| Employed | |
|---|---|
| (n = 481) | |
| Employment site, n (%) | |
| COVID-19 first-line units | 243 (50.5%) |
| COVID-19 medical units | 238 (49.5%) |
| Clinical experience—real conditions, n (%) | |
| Primary role (usual) | 265 (55.1%) |
| Supervision (yes) | 416 (86.5%) |
| Specific training (yes) | 291 (60.5%) |
| Development of new skills (yes) | 317 (65.9%) |
| Clinical experience—perceived conditions, M/m (± SD [range]) | |
| CERS-PROFEX | 14.2/16 (± 6.5 [1;24]) |
| CERS-PERSEX | 12.4/14 (± 4.7 [1;18]) |
SD: standard deviation; CERS-PROFEX: Crisis Experience Rating Scale-Professional Experience subscale; CERS-PERSEX: Crisis Experience Rating Scale-Personal Experience subscale, M: mean; m: median
Of the 531 preclinical respondents in the analytic sample, 145 (27.3%) exceeded the average STAI-A anxiety cutoff point versus 36 of 467 (7.7%) in 2018. Similarly, of the 163 graduating respondents in the analytic sample, 60 (36.8%) exceeded the average STAI-A anxiety cutoff versus 32 of 246 (12.9%) in 2018. All p values between these groups were < 0.001. Clinical students showed a similar prevalence rate as the 2018 sample. Table 3 shows the anxiety prevalence rate by STAI-A cutoff points (95% CI) compared to the 2018 sample.
Table 3.
Comparison of anxiety between the 2020 cohort and the 2018 cohort
| STAI-A Total score | 2020 cohort | 2018 cohort | p | Adjusted p | ||
|---|---|---|---|---|---|---|
| Undergraduate N (%)/95% CI | ||||||
| All | N = 1165 | N = 1252 | ||||
| < 55 | 901 (77.3) | 74.8;79.7 | 1141 (98.2) | 89.4;92.6 | < 0.001 | < 0.001 |
| 55–65 | 178 (15.3) | 13.3;17.4 | 85 (0.7) | 5.4;8.3 | ||
| > 66 | 86 (7.4) | 5.9;9.0 | 26 (0.2) | 1.4;3.0 | ||
| Preclinical | n = 531 | n = 467 | ||||
| < 55 | 386 (72.7) | 68.7;76.4 | 431 (92.3) | 89.5;94.5 | < 0.001 | < 0.001 |
| 55–65 | 93 (17.5) | 14.4;21.0 | 27 (5.8) | 3.8;8.3 | ||
| > 66 | 52 (9.8) | 7.4;12.6 | 9 (1.9) | 0.9;3.6 | ||
| Clinical | n = 471 | n = 536 | ||||
| < 55 | 412 (87.5) | 84.1;90.3 | 493 (91.9) | 89.3;94.1 | .134 | .246 |
| 55–65 | 51 (10.8) | 8.2;14.0 | 34 (6.3) | 4.4;8.7 | ||
| > 66 | 8 (1.7) | 0.7;3.3 | 9 (1.6) | 0.7;3.1 | ||
| Graduating | n = 163 | n = 249 | ||||
| < 55 | 103 (63.2) | 55.3;70.6 | 217 (87.1) | 82.3;91.0 | < 0.001 | < 0.001 |
| 55–65 | 34 (20.9) | 14.8;27.9 | 24 (9.7) | 13.1;23.0 | ||
| > 66 | 26 (15.9) | 10.7;22.5 | 8 (3.2) | 1.4;6.2 |
CI: confidence interval
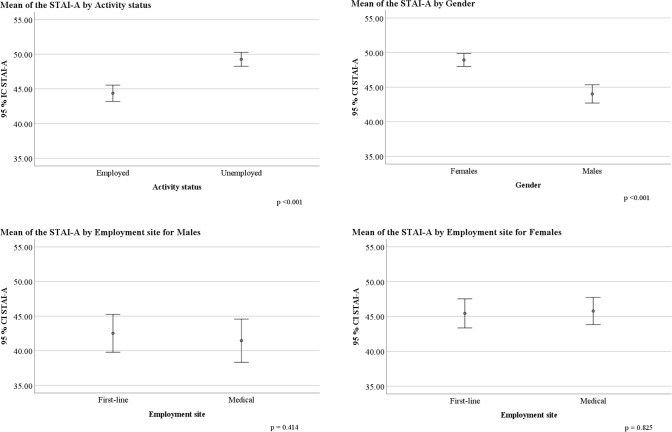
Overall, anxiety was higher in unemployed (mean difference (MD) 3.4; 95% CI 1.5; 5.5, p < 0.001) and female students (MD 5.8; 95% CI 3.7; 7.8, p < 0.001). There was no significant difference by employment sites though anxiety was still higher in employed females than males (MD 4.3; 95% CI 1.0; 6.8, p < 0.001). MANOVAs showed no interaction effects between activity status or employment site and gender. Figure 1 shows the variation in mean (95% CI) anxiety for employed and unemployed students, males and females, as well as for employment sites stratified by gender.
Fig. 1.
Plots of mean (95% CI) anxiety scores (STAI-A) by gender, activity status, and employment site stratified by gender
Answering our research question (Table 4), employment in COVID-19 first-line units was not correlated with anxiety, while being female (MD = 3.3; 95% CI 1.0; 5.7, p < 0.005), negative CERS-PROFEX (MD = − 0.2: 95% CI − 0.3; − 0.1, p < 0.030), and negative CERS-PERSEX (MD = − 0.5; 95% CI − 0.7; − 0.2, p < 0.001) were. On the contrary, none of the clinical experience real conditions were correlated with anxiety.
Table 4.
Linear regression analysis of mean difference [95% CI] in demographic, employment site, and clinical experience variables in relation to anxiety in employed students
| Variable | MD [95% CI] | p |
|---|---|---|
| Employed | ||
| Gender (female) | 3.3 [1.0; 5.7] | < 0.005 |
| Employment sites (first line) | − 0.2 [− 3.2; 3.1] | .889 |
| Primary role (usual) | − 0.1 [− 3.4; 1.5] | .435 |
| Specific training (yes) | 1.5 [− 0.8; 3.8] | .198 |
| Supervision (yes) | 1.5 [− 1.9; 4.8] | .382 |
| Development of new skills (yes) | 0.5 [− 2.0; 2.9] | .691 |
| CERS-PROFEX | − 0.2 [− 0.3; − 0.1] | < 0.030 |
| CERS-PERSEX | − 0.5 [− 0.7; − 0.2] | < 0.001 |
MD: mean difference; CI: confidence interval; CERS-PROFEX: Crisis Experience Rating Scale-Professional Experience subscale; CERS-PERSEX: Crisis Experience Rating Scale-Personal Experience subscale
Discussion
To our knowledge, our study is the first to compare the anxiety of undergraduate medical students who were allocated to COVID-19 first-line units with that of students who chose not to return to the clinical setting, with a baseline of undergraduate student anxiety prior to COVID-19. Our work revealed that the employed students were less anxious than the unemployed students, regardless of their employment site. We also showed that engaging students in COVIID-19 first-line units was not a risk factor for anxiety, as opposed to gender, and negative clinical experience perceived conditions.
Increasing attention is being paid to medical students’ well-being. In many countries, national authorities have issued recommendations to identify and prevent psychological disorders, including anxiety, in their students [28–31]. Although many personal factors have been identified as anxiety generators, academic and clinical stressors are frequently questioned [32]. The COVID-19 outbreak has characteristics of both. We found that the 2020 cohort was more anxious than the 2018 cohort, with an average increase of 14% and 7% in students with high and severe anxiety, respectively. These rates do not differ from those measured in the general population in the COVID-19 context [33]. They are also within the overall average measured in medical students outside of the COVID-19 outbreak [34]. This suggests that the impact of the pandemic on student well-being is real, but is not as significant as one might spontaneously think. Our results also confirm the well-known effect of gender, with females showing higher anxiety than males [10]. However, we provided as a result its lack of correlation with activity status and employment sites during the COVID-19 outbreak, as females were exposed to front-line conditions as much as males. This suggests that there is no gender difference in choosing to return to clinical activities during a pandemic.
Moreover, we provided findings supporting the hypothesis that employment during the COVID-19 outbreak was not a risk factor for anxiety. The difference in anxiety observed in our population concerns mainly unemployed students. Coping refers to the strategies utilized when faced with a stressor [35]. We suggest that choosing to return to the clinical setting during an outbreak is an active coping strategy, which is an adaptive way to face anxiety [36–39]. Conversely, students choosing not to return to clinical activities used less appropriate coping strategies to reduce their COVID-19-related anxiety. They may have favored avoidance strategies, which have a negative impact on anxiety [40, 41], particularly among healthcare professionals and medical students [37, 42, 43]. Those explanations support the potential benefits of implementing interventions focused on the enhancement of adaptive coping, e.g., positive reinterpretation, which is viewing a situation as an opportunity to learn new skills. These strategies could encourage students and other health professionals to return or be reallocated to clinical settings during a pandemic, and thus respond to increased staffing needs, especially in settings where the need is greatest, such as emergency departments [36, 37].
One limitation of our study is the assessment of only one of the several psychological consequences of the current health crisis, that is, anxiety. While increased anxiety is frequently observed after such events, particularly among healthcare workers, other problems have been described, including anger, depression, and suicide [44, 45]. Another limitation is the inclusion of limited protective/risk factors, essentially concerning clinical experience. Other personal and interpersonal protective/risk factors should be considered. Moreover, our study compared two partially different cohorts with a 2-year interval. This limitation must be put into perspective considering that both surveys were conducted at the same time of the year, that no major changes in the curriculum took place, and that the response rate was high in both cohorts. Finally, we did not measure student anxiety at the very beginning of the health crisis. Therefore, we cannot rule out the possibility that students who decided to work in a clinical setting were those with the lowest initial anxiety levels. However, this limitation does not call into question the relevance of our results. First, because once students become involved on a voluntary basis, their initial level of anxiety may legitimately be a factor in whether or not they become involved. Second, and assuming a lower initial level of anxiety, our data tend to show that being employed did not generate an anxiety-producing effect in these students. Finally, because, in general, it is more relevant to measure anxiety at the end of a phenomenon to determine whether adaptive mechanisms were deployed. Anxiety state is indeed variable over time (although correlated with trait anxiety, implying that people of an anxious nature are more likely to increase their anxiety contextually than others). It is, therefore, possible that students' anxiety may have been lower or higher at some point during the crisis (at the beginning or peak, for example), but when it is at the level where we measured it at the end of the crisis, this means that the coping strategies mobilized by the students were effective, which is the most important thing.
Conclusions
At the peak of the COVID-19 pandemic, 194 countries closed their universities, affecting more than 90% of the world’s student population, and exposing hospitals to a brutal workforce shortage [46]. Our results legitimize recommendations made in most countries to deal with this unprecedented situation, i.e., mobilizing only students in places where their presence is useful, and only if they are voluntary. However, our findings should lead institutions to question the level of mobilization of undergraduate medical students. They suggest that clinical activities, including in first-line units, are not anxiety risk factors. Therefore, there is no obstacle to mobilizing students in high-risk settings, as long as there is a need, their involvement is voluntary, they are and feel protected, and that supervisors remain vigilant regarding the risk of professional exhaustion.
Acknowledgements
The authors wish to thank Andréa Mignerey, Deputy Director of the Medical Affairs Department at Strasbourg University Hospital, for her help in identifying assignments for students in clinical settings. The authors also thank the undergraduate students’ representatives for their assistance in administering the survey.
Author contributions
TP contributed significantly to the design of the study and to data acquisition and interpretation. He drafted the initial version of the manuscript and oversaw revisions. JS contributed to the design of the study and to data interpretation. He reviewed manuscript drafts. EF contributed to the design of the study and to data acquisition and interpretation. She reviewed manuscript drafts. LG contributed to the design of the study and to data acquisition and interpretation. She reviewed manuscript drafts. AM contributed to the design of the study and to data acquisition and interpretation. She reviewed manuscript drafts. FS contributed to the design of the study and to data analysis. He reviewed manuscript drafts. MA contributed significantly to the design of the study and to data analysis and interpretation. She drafted the initial version of the manuscript. All authors approved the final version of the manuscript.
Funding
None.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement
All procedures performed in this study were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval has been granted by the Institutional Review Board of Strasbourg Medical School on June 13, 2017, #2017-25. An extension of ethical approval was obtained by the same board for this study on May 4, 2020.
Informed consent
Participants were informed that their completion of the questionnaire indicated their consent to participate in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baker DM, Bhatia S, Brown S, et al. Medical student involvement in the COVID-19 response. Lancet. 2020;395:1254. doi: 10.1016/S0140-6736(20)30795-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whelan A, Prescott J, Young G et al (2020) Guidance on medical students’ clinical participation: effective immediately. Association of American Medical Colleges. https://lcme.org/wp-content/uploads/filebase/March-17-2020-Guidance-on-Mediical-Students-Clinical-Participation.pdf. Accessed 22 Oct 2020
- 3.The Association of Faculties of Medicine of Canada (2020) Ten guiding principles for medical education. https://afmc.ca/sites/default/files/pdf/2020-Ten_Guiding_Principles_for_Medical_Education_COVID_Era_en.pdf. Accessed 22 Oct 2020
- 4.Medical Schools Council (2020) Advice from Medical Schools Council to UK Medical schools on actions surrounding Covid-19. https://www.medschools.ac.uk/media/2620/msc-covid-19-advice-for-uk-medical-schools.pdf. Accessed 22 Oct 2020
- 5.Ministère des Solidarités et de la Santé Coronavirus : foire aux questions pour les étudiants et les internes des filières médicales [Coronavirus: Frequently Asked Questions for Medical Students and Residents]. https://solidarites-sante.gouv.fr/IMG/pdf/covid-19_faq_etudiants_medicaux.pdf. Accessed 22 Oct 2020
- 6.Compton S, Sarraf-Yazdi S, Rustandy F, Radha Krishna LK. Medical students’ preference for returning to the clinical setting during the COVID-19 pandemic. Med Educ. 2020 doi: 10.1111/medu.14268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kazdin AE. Encyclopedia of psychology: develop-gooden. Washington: American Psychological Association; 2000. [Google Scholar]
- 8.Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein C, Brownstein A, Scott C, Lan Y-L. Anxiety and stress reduction in medical education: an intervention. Med Educ. 2007;41:258–264. doi: 10.1111/j.1365-2929.2007.02685.x. [DOI] [PubMed] [Google Scholar]
- 10.Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48:963–979. doi: 10.1111/medu.12512. [DOI] [PubMed] [Google Scholar]
- 11.Firth-Cozens J. Doctors, their wellbeing, and their stress: it’s time to be proactive about stress—and prevent it. BMJ. 2003;326:670–671. doi: 10.1136/bmj.326.7391.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bao Y, Sun Y, Meng S, et al. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tran D (2020) Managing anxiety and stress in a time of pandemic. https://students-residents.aamc.org/attending-medical-school/article/managing-anxiety-and-stress-time-pandemic. Accessed 22 Oct 2020
- 15.Clark V (2020) Prioritizing wellness in the whirlwind of COVID-19. https://students-residents.aamc.org/attending-medical-school/article/prioritizing-wellness-in-the-whirlwind-of-covid-19. Accessed 22 Oct 2020
- 16.Aker S, Mıdık Ö. The views of medical faculty students in Turkey concerning the COVID-19 pandemic. J Commun Health. 2020 doi: 10.1007/s10900-020-00841-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu W, Zhang Y, Wang P, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. 2020 doi: 10.1002/jmv.25914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976–e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ullah R, Amin S. The psychological impact of COVID-19 on medical students. Psychiatry Res. 2020;288:113020. doi: 10.1016/j.psychres.2020.113020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang ZC, Ooi SBS, Wang W. Pandemics and their impact on medical training: lessons from Singapore. Acad Med. 2020 doi: 10.1097/ACM.0000000000003441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Artino AR, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE guide no. 87. Med Teach. 2014;36:463–474. doi: 10.3109/0142159X.2014.889814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cook DA, Brydges R, Ginsburg S, Hatala R. A contemporary approach to validity arguments: a practical guide to Kane’s framework. Med Educ. 2015;49:560–575. doi: 10.1111/medu.12678. [DOI] [PubMed] [Google Scholar]
- 23.Spielberger CD, Bruchon-Schweitzer M, Paulhan I (1993) Inventaire d’anxiété État-Trait: Forme Y. ECPA, les Éditions du centre de psychologie appliquée, Paris
- 24.Phillips AW, Reddy S, Durning SJ. Improving response rates and evaluating nonresponse bias in surveys: AMEE guide no. 102. Med Teach. 2016;38:217–228. doi: 10.3109/0142159X.2015.1105945. [DOI] [PubMed] [Google Scholar]
- 25.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57:289–300. [Google Scholar]
- 26.Heinze G, Dunkler D. Five myths about variable selection. Transpl Int. 2017;30:6–10. doi: 10.1111/tri.12895. [DOI] [PubMed] [Google Scholar]
- 27.Guiberteau V, Marlat D (2020) Les étudiants inscrits dans les universités françaises en 2018–2019 [Students enrolled in French universities in 2018–2019]. Sous-direction des systèmes d’information et des études statistiques (Sies) - Ministère de l’Enseignement supérieur, de la Recherche et de l’Innovation. https://cache.media.enseignementsup-recherche.gouv.fr/file/2020/39/6/NI_2020-03_Effectifs_universitaires_1235396.pdf. Accessed 22 Oct 2020
- 28.General Medical Council (2013) Supporting medical students with mental health conditions. https://www.gmc-uk.org/-/media/documents/supporting-students-with-mental-health-conditions-0816_pdf-53047904.pdf. Accessed 22 Oct 2020
- 29.Association of American Medical Colleges (2014) Personal well-being among medical students: findings from an AAMC pilot survey. https://www.aamc.org/system/files/reports/1/april2014aib_personalwell-beingamongmedicalstudents.pdf. Accessed 22 Oct 2020
- 30.Ministère de l’Enseignement supérieur, de la Recherche et de l’Innovation (2019) Lancement du Centre national d’appui à la qualité de vie des étudiants en santé [Launch of the National Healthy Student Quality of Life Support Centre]. https://www.enseignementsup-recherche.gouv.fr/cid143914/lancement-du-centre-national-d-appui-a-la-qualite-de-vie-des-etudiants-en-sante.html. Accessed 22 Oct 2020
- 31.The Association of Faculties of Medicine of Canada (2018) Report on Mental Health Activities: focus on physician health. http://www.afmc.ca/sites/default/files/pdf/2018-AFMC_Report_on_Mental_Health_Activities_EN.pdf. Accessed 22 Oct 2020
- 32.Dyrbye LN, Sciolla AF, Dekhtyar M, et al. Medical school strategies to address student well-being: a national survey. Acad Med. 2019;94:861–868. doi: 10.1097/ACM.0000000000002611. [DOI] [PubMed] [Google Scholar]
- 33.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tian-CiQuek T, Tam WS, Tran B, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16:2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biggs A, Brough P, Drummond S. Lazarus and Folkman’s psychological stress and coping theory. In: Cooper CL, Quick J, editors. The handbook of stress and health: a guide to research and practice. New York: Wiley; 2017. [Google Scholar]
- 36.Fares J, Al Tabosh H, Saadeddin Z, et al. Stress, burnout and coping strategies in preclinical medical students. North Am J Med Sci. 2016;8:75–81. doi: 10.4103/1947-2714.177299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Erschens R, Loda T, Herrmann-Werner A, et al. Behaviour-based functional and dysfunctional strategies of medical students to cope with burnout. Med Educ Online. 2018;23:1535738. doi: 10.1080/10872981.2018.1535738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fontana MCP, Generoso IP, Sizilio A, Bivanco-Lima D. Burnout syndrome, extracurricular activities and social support among Brazilian internship medical students: a cross-sectional analysis. BMC Med Educ. 2020;20:81–87. doi: 10.1186/s12909-020-01998-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shadid A, Shadid AM, Shadid A, et al. Stress, burnout, and associated risk factors in medical students. Cureus. 2020;12:e6633. doi: 10.7759/cureus.6633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McLaughlin KA, Nolen-Hoeksema S. Rumination as a transdiagnostic factor in depression and anxiety. Behav Res Ther. 2011;49:186–193. doi: 10.1016/j.brat.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schäfer JÖ, Naumann E, Holmes EA, et al. Emotion regulation strategies in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc. 2017;46:261–276. doi: 10.1007/s10964-016-0585-0. [DOI] [PubMed] [Google Scholar]
- 42.Monteiro AMF, Santos RL, Kimura N, et al. Coping strategies among caregivers of people with Alzheimer disease: a systematic review. Trends Psychiatry Psychother. 2018;40:258–268. doi: 10.1590/2237-6089-2017-0065. [DOI] [PubMed] [Google Scholar]
- 43.Labrague LJ, McEnroe-Petitte DM, Gloe D, et al. A literature review on stress and coping strategies in nursing students. J Ment Health. 2017;26:471–480. doi: 10.1080/09638237.2016.1244721. [DOI] [PubMed] [Google Scholar]
- 44.Jeong H, Yim HW, Song Y-J, et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. 2016;38:e2016048. doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maunder RG. Was SARS a mental health catastrophe? Gen Hosp Psychiatry. 2009;31:316–317. doi: 10.1016/j.genhosppsych.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.United Nations Educational, Scientific and Cultural Organization (UNESCO) (2020) COVID-19 educational disruption and response. https://en.unesco.org/covid19/educationresponse. Accessed 22 Oct 2020