Abstract
We discuss the current understanding of COVID-19’s neurological implications, their basis, and the evolving clinical consensus with a focus on cerebrovascular stroke. We further illustrate the potential significance of these implications with the aid of an accompanying case report outlining the disease course and treatment of a COVID-19 patient suffering from ischemic stroke and pulmonary embolism. The ever-growing strain on the global healthcare system due to the spread of the novel coronavirus SARS-CoV-2 requires focused attention on urgent care of independent, coexisting, and associated comorbidities, including cerebrovascular accidents. For illustration purposes, we outline the case of a 68-year-old female presenting with COVID-19 subsequently complicated by bilateral pulmonary embolism and a right-sided cerebrovascular accident. The patient was successfully managed pharmacologically and discharged without significant neurological deficit. The evidence for a hypercoagulable state in this patient along with discussion of mechanistic bases, corroborative evidence from the literature, along with relevant guidance on screening, treatment, and prophylaxis is offered. Greater study of the pathogenesis of COVID-19-related cerebrovascular complications and revisiting current guidelines on their management including potentially heightened levels of thromboprophylaxis are warranted.
Keywords: COVID-19, Neurological, SARS-CoV-2, Stroke, Cerebrovascular accident (CVA), Acute ischemic stroke (AIS), Hypercoagulation, Pulmonary embolism, Tissue plasminogen activator (tPA), Low-molecular-weight heparin (LMWH), Anticoagulation, Fibrinolysis, Thrombolytics, Thromboprophylaxis, Case report
Introduction
After first being reported in Wuhan, China, in December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has emerged as a dominant force affecting nearly every aspect of society and millions worldwide, resulting in over 1,400,000 by the end of November 2020 [1]. Such crises often disproportionately harm the most socioeconomic and medically vulnerable patient groups [2, 3]. Given the multisystem scope of COVID-19, studies have been limited with regard to the specific mechanistic causes behind fatalities and breakdown of their clinical characteristics. While a recent study of 77 fatal cases of COVID-19 found 3.9% of deaths to be due to nervous system disease, more specific breakdowns were not provided [4]. Specifically, stroke risk has been reported to be related to disease severity in hospitalized COVID-19 patients, with an incidence of close to 1% in mild disease and up to 6% in severe infections [5]. Here, we use the case of a 68-year-old female to draw attention to the patient subpopulation whose COVID-19 disease course is complicated by acute ischemic stroke (AIS). We provide a literature review and viewpoint on the current recommendations and evolving strategies for the prevention, management, and resolution of such cases.
Case Report
Case Presentation
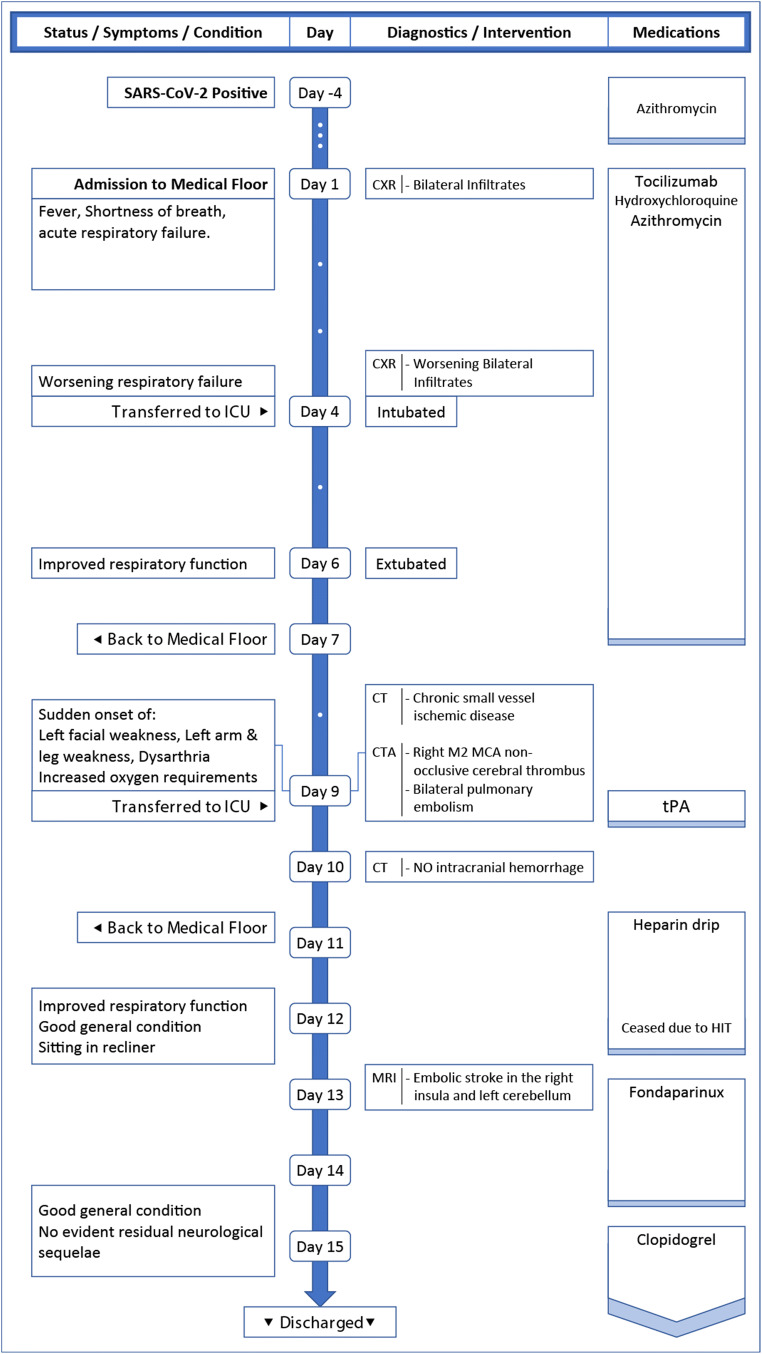
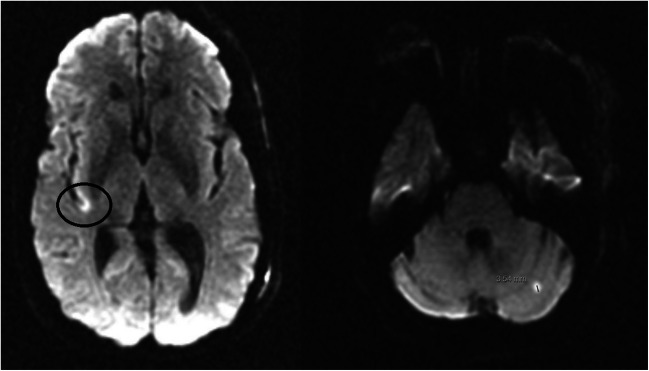
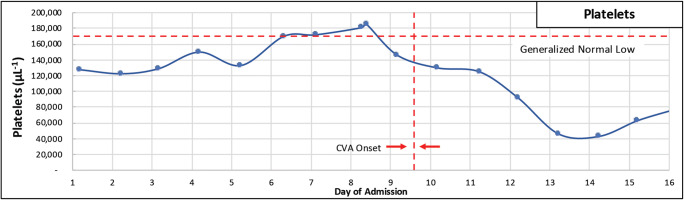
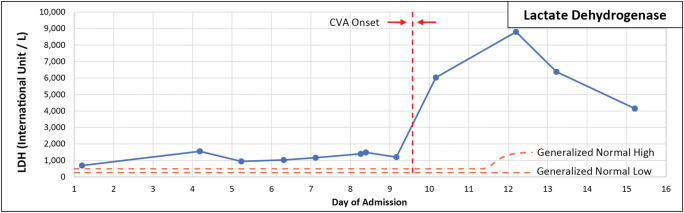
In an effort to contextualize the clinical relevance of our subsequent discussion, we have detailed the case of a 68-year-old female with a history of hypertension, hyperlipidemia, and obstructive sleep apnea positive for SARS-CoV-2. A timeline overview of the case is presented in Fig. 1. On day 1 of admission, the patient presented with symptoms of fever, shortness of breath, and acute respiratory failure due to COVID-19 pneumonia. She received tocilizumab, hydroxychloroquine, and azithromycin. On day 4, the patient was transferred to the intensive care unit (ICU) for worsening respiratory failure requiring intubation. On day 6, the patient was extubated and transferred on day 7 back to the medical floor on a non-rebreather mask with improved pancytopenia. On day 9 at 1:50 pm, while recovering on a non-rebreather mask, the patient was noted to have sudden onset of left-sided facial, arm, and leg weakness and dysarthria. Her symptoms improved transiently on the way to performing computed tomography (CT) but worsened soon after. The CT scan was unremarkable for acute hemorrhage or evolving infarct but showed signs of chronic small vessel ischemic disease. Computed tomography angiography (CTA) showed emboli in bilateral distal main and upper lobe pulmonary arteries consistent with bilateral pulmonary embolism (PE). A non-occlusive thrombus in the proximal right M2 segment of the middle cerebral artery (MCA) was also discovered (Fig. 2). The patient was able to lift left upper and lower extremities against gravity but suffering from weakness to resistance. Strength was noted as 3/5 in both upper and lower extremities, along with dysarthria. The patient was assessed with an NIH stroke scale of 8 for left-sided weakness. D-dimer levels were notably elevated. Her PE and COVID-19 status were not considered an impediment to immediate thrombolytic administration, and the tissue plasminogen activator (tPA) alteplase was ordered at 0.9 mg/kg for management of bilateral PE and right MCA non-occlusive thrombus after obtaining consent from the patient. On day 10, the patient no longer showed signs of left-sided weakness or focal neurological deficits. The next day, she was started on clopidogrel daily after CT of the head did not show intracranial hemorrhage. On day 11, the patient’s breathing improved with reduction in cough severity, but still suffering from mild tachypnea and residual shortness of breath requiring increased oxygen supplements. Dysarthria and facial asymmetry continued to be absent. C-reactive protein was also noted to continue trending downwards. On day 12, the patient was observed sitting in recliner and feeling better, though still tachycardic and mildly tachypneic. No residual symptoms were noted from the presumed stroke. MRI showed embolic stroke in the right insula and left cerebellum (Fig. 3). On day 13, she was noted to show signs of heparin-induced thrombocytopenia (HIT) with a further steady decline in platelets since initiating heparin therapy on day 11 (Fig. 5). Heparin was discontinued and the patient was started on fondaparinux with plans to switch to apixaban. HIT was later confirmed via antibody testing. On day 15, the patient was discharged in good general condition despite a positive repeat SARS-CoV-2 test, without evident neurological sequelae and was instructed to practice continued quarantine for 2 weeks.
Fig. 1.
Case timeline
Fig. 2.
Computed tomography angiography (CTA) showing non-occlusive thrombus in the proximal right M2 segment of the middle cerebral artery (MCA)
Fig. 3.
Magnetic resonance imaging (MRI) without contrast showing embolic stroke in the right insula and left cerebellum
Fig. 5.
Platelets
Case Discussion
The patient was SARS-CoV-2 positive upon admission presenting with pulmonary symptoms of COVID-19. Her treatment with hydroxychloroquine, azithromycin, and the anti-interleukin-6 antibody tocilizumab was consistent with practices and experiences of other clinicians at the time of admission [6–8]. She showed signs of improvement, extubated, and returned to the medical floor on day 7 of hospitalization. Evidence is still being gathered on the unproven efficacy, unclear mechanism, and possibly significant side effect profile of hydroxychloroquine in the treatment of COVID-19 [9, 10]. There is however further evidence for successful use of tocilizumab in a number of case reports along with a compelling theoretical basis for its efficacy [7, 8, 11].
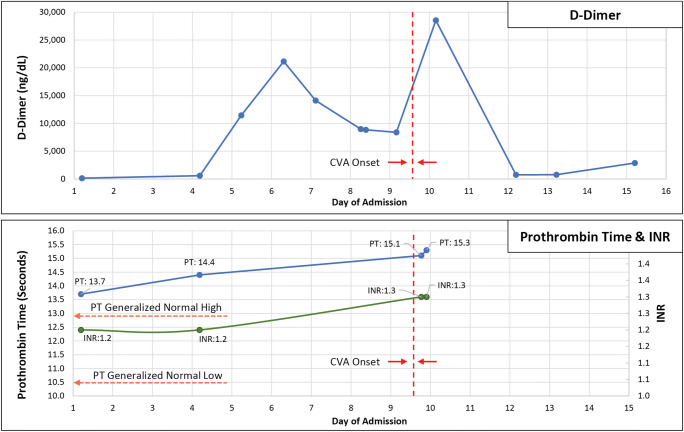
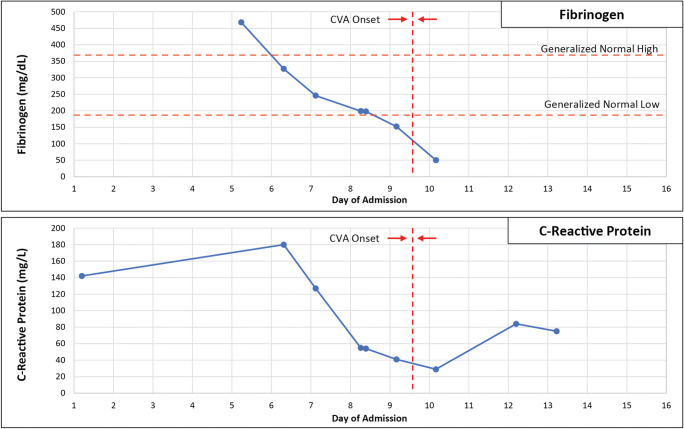
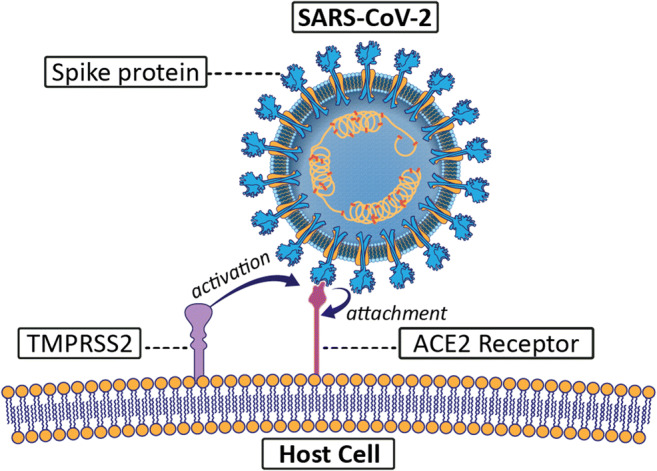
Despite the improvement in her general condition and respiratory status, the patient showed symptoms of a CVA on the ninth day of hospitalization, 2 days after returning to the medical floor. As early as 4 days prior to the manifestation of her CVA, the patient’s D-dimer, prothrombin time, and INR levels were markedly elevated indicating an existing coagulopathy at admission, with thrombocytopenia (Fig. 4 and Fig. 5). Inflammatory markers such as C-reactive protein (CRP), fibrinogen, and ferritin were also high in the days leading up to the CVA (Figs. 6 and 7). The increased levels of fibrinogen are not compatible with consumption coagulopathy such as disseminated intravascular coagulation (DIC), and instead indicate an overlapping picture of hypercoagulability in conjunction with a severe inflammatory state. This patient had multiple risk factors predisposing her to acute ischemic stroke. Her inflammatory and hypercoagulable state theoretically stemming from her COVID-19 status and a history of hypertension and hyperlipidemia are of importance. Obstructive sleep apnea itself is associated with an increased risk of hypercoagulable states as well [12, 13]. It is worthwhile to consider whether these trends in laboratory values, along with known risk factors, may have justified early prophylactic therapy to reduce the risk of acute ischemic stroke.
Fig. 4.
D-dimer, prothrombin time, and INR
Fig. 6.
Fibrinogen and C-reactive protein
Fig. 7.
Lactate dehydrogenase
Review of Literature
Neurological Manifestations of COVID-19
The novel SARS coronavirus (SARS-CoV-2)—initially known primarily as a severe viral pneumonia—has since become associated with extrapulmonary manifestations, including neurological symptoms. Among a study of 214 COVID-19 patients, 36.4% experienced some neurologic manifestations, including CNS symptoms such as dizziness, headache, impaired consciousness, CVD, ataxia, and seizure, as well as PNS symptoms such as impairment of taste, smell, and vision, and nerve pain [5]. Alterations in olfactory and gustatory senses are some of the more unique symptoms [14, 15]. In a study of 202 individuals, these alterations were observed as the solitary or earliest sign of COVID-19 in 15% of patients, and present concomitantly with other symptoms in another 23% [15]. It has also been proposed that SARS-CoV-2 could also affect the respiratory reflex pathway resulting in lack of dyspneic symptoms even in intubated patients [16, 17]. Rarer neurologic manifestations such have been linked in individual cases [5, 18]. There have also been some anecdotal accounts of delirium and cognitive decline in COVID-19 patients [19]. A recent study, which reported cognitive decline in COVID-19 patients, was limited by its cross-sectional and non-peer-reviewed nature with insufficient bases for significant confidence in its conclusions [20]. However, peer-reviewed published works do exist documenting cognitive changes in COVID-19 patients, including those who have recovered [21, 22]. It is unclear if such sequelae are likely to be subacute or chronic. Of course, there are theoretical bases for these observations, stemming from SARS-CoV-2’s potential impact via hypoxemia, coagulopathies, vascular damage, and neuroinflammation among others. The exact mechanism by which these specific neurological symptoms are linked to SARS-CoV-2 is unclear and may simply be a result of an immunological response rather than direct neuroinvasive sequela of the virus.
Of particular relevance to our discussion, in an early study of 214 patients in China, 5.7% of patients with severe COVID-19 were found to have suffered from acute cerebrovascular disease (CVD) [5]. These patients have been significantly older and more likely to have had risk factors such as diabetes, hypertension, or previous history of CVD or severe COVID-19 [23, 24], with severity of COVID-19 assessed using American Thoracic Society guidelines for community-acquired pneumonia [25]. A systemic review of 39 studies with 68,361 laboratory-confirmed COVID-19 patients found that 1.3% experienced ischemic stroke. Individual data from 129 such patients found an in-hospital mortality rate of 22.8% [26]. It is difficult to ascertain with reference to current research, whether such cerebrovascular manifestations are directly caused by the COVID-19 disease process. However, there is compelling evidence in support of COVID-19 uniquely contributing to a heightened risk of CVAs.
Review of COVID-19-Associated Hypercoagulability
Though past experiences with the 2002 SARS-CoV outbreak have yielded limited evidence due to its significantly lower number of cumulative cases (8447 worldwide) [27], a study of anecdotal cases in Singapore showed several patients with pulmonary thromboembolism and deep vein thrombosis [28]. Vascular fibrin thrombi were also a commonly found feature in over 80% of cases among a group of 20 autopsies performed in patients with the 2002 SARS-CoV virus in Toronto [29]. Of course, differences in the genetic characteristics between the 2002 SARS-CoV and SARS-CoV-2 (80% shared identity) are not insignificant and may result in varying presentations [30].
There is, however, additional evidence of a hypercoagulable state in COVID-19 pneumonia patients admitted to intensive care units. A study of 184 ICU patients in the Netherlands found a 31% incidence of thrombotic complications, despite standard thromboprophylaxis [31]. In another study by Tang et al. involving 183 COVID-19 patients, the criteria of disseminated vascular coagulation were met at a higher rate among non-survivors (71.4%) compared to survivors (0.6%) [32]. There is also an associated mild thrombocytopenia in COVID-19 patients, as with our patient [33]. Other studies have shown coagulation disturbances primarily in levels of D-dimer and fibrin degradation products (FDP) in COVID-19 patients, interpreted by the authors as consistent with consumption coagulopathy [34]. A study of 5700 patients hospitalized in New York with COVID-19 painted a similar picture with markedly elevated D-dimers, ferritin, and CRP [35]. A pathological study from Brazil of ten autopsies showed small fibrinous thrombi in small pulmonary arterioles in eight patients [36].
Given the selective patient populations analyzed some of the above studies, findings cannot be extrapolated to draw definite conclusions about the general disease process and certainly not immediately applicable to clinical decision-making without careful consideration. As an example, thromboelastography analysis from 24 patients presenting with COVID-19 admitted to the ICU in Milan, Italy, was found to be consistent with hypercoagulability in the setting of a severe inflammatory state, but not consumption coagulopathy as previously described by Tang et al. [32, 37]. Ranucci et al. reported a similarly diverging pattern of prothrombotic coagulopathy compared to what would otherwise be expected from that of DIC [38]. The increased levels of fibrinogen lend further evidence in support of this diverging pattern of coagulopathy, consistent with our own observations. Nevertheless, the overall picture of a hypercoagulable state in the most severe cases of COVID-19 is consistently apparent.
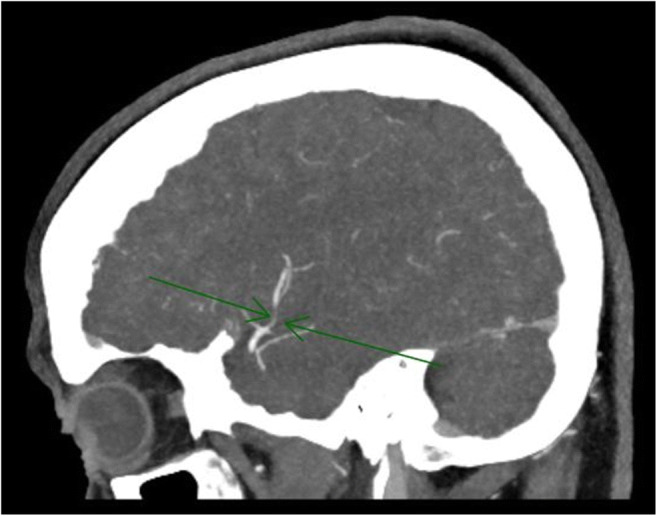
A retrospective study of 1916 patients with COVID-19 found ischemic stroke to be 7.6 times more likely as compared to patients with influenza [39]. Evidence suggests that COVID-19 presents an independent risk factor for stroke [40]. In a study of 3556 patients in one New York healthcare system, cases of stroke in COVID-19 patient were more likely to be cryptogenic (65.6%) than those without COVID-19 (30.4%, p = 0.003) and historic cases of ischemic stroke from the same time period in the preceding year (25.0%, p < 0.001) [41]. The above observations are not without a theoretical basis, and there exist plausible mechanisms by which COVID-19 may further compound CVD risk in high-risk populations. The SARS-CoV-2 virus is internalized into the host cell via the angiotensin-converting enzyme 2 (ACE2) receptor with the aid of the transmembrane protease serine 2 (TMPRSS2) protein (Fig. 8). Given the facilitative role played by TMPRSS2, its presence along with ACE2 in particular tissues potentially renders them more susceptible to viral entry and replication. Vascular smooth muscle expresses both ACE2 and TMPRSS2 priming vascular tissue for damage [42]. Cardiovascular implications of COVID-19 potentially leading to arrhythmias leading to thrombi as well as hypotension exacerbating downstream ischemic events can both contribute to the development of stroke [43]. Additionally, the inflammatory cascades and the release of proinflammatory cytokines may further contribute to the propagation of procoagulant lesions in the vasculature [7, 37, 38]. Hypoxia [31, 44, 45], thrombocytopenia [33], cytokine storm [7], and liver abnormalities [46] may each contribute to a hypercoagulable state in COVID-19 patients.
Fig. 8.
SARS-CoV-2 attachment to host cells
Clinical Implication and Practice Recommendations
Regardless of the pathological processes behind COVID-19-associated CVAs, the need to formulate an evidence-based strategy remains. Given that CVAs share overlapping risk factors with prognostic severity of disease in COVID-19 including age and chronic diseases, a focused attention on the management of new-onset acute ischemic stroke is of additional importance in light of the negative prognostic consequences. The American Heart Association (AHA) and American Stroke Association (ASA) released temporary emergency guidance to US stroke centers on March 31, 2020, in relation to protective measures against the spread of SARS-CoV-2, as well as modulated expectations in terms of adherence to treatment times [47]. A discussion on the topic is also available as a podcast [48]. However, additional guidelines are needed to address the links between COVID-19 and CVAs.
Before discussing the issue further, it is important to consider that with rising infection levels, it may be more difficult to determine if a patient’s AIS is induced by their SARS-CoV-2–positive status or whether the patient’s COVID positivity is separate from underlying disease processes responsible for their presenting stroke. Given the importance of stroke on its own account, we shall first discuss the latter scenario.
Acute Stroke as the Presenting Complaint
When it comes to a novel disease process such that of SARS-CoV-2, possible complications are not always attributable with complete certainty via a cause-and-effect relationship to the coexisting disease [49]. However, in terms of clinical management, there is a need for reciprocal screening of patients among CVA and COVID-19 populations. The standard practice of screening patients for COVID-19 obviously extends to those suspected of CVAs. As has already been discussed, COVID-19 has neurological manifestations and such patients should be carefully screened [14]. More concerning, a report from Italy showed a precipitous and counter-intuitive decline in the number of documented cases of ischemic stroke over the course of 1 month [50]. Similar observations have been made in other areas worldwide [51–53]. This is likely the combined result of patients with mild cases not seeking care for fear of being infected, cases of ischemic stroke being overlooked in the healthcare setting due to resource reallocation and overlapping cases of severe or fatal COVID-19, and stroke not being adequately tracked as cases of stroke. Public officials and healthcare professionals should do more in encouraging patients with symptoms of possible stroke to continue seeking emergency services themselves without concern for the risk of exposure to SARS-CoV-2. Telemedicine can help alleviate some patient concerns [54]. To reduce the risk to patients of unknown COVID status, some institutions have already begun using telemedicine to screen patients both in their own emergency departments and regionally [47, 55, 56]. Medical centers have already adjusted their acute stroke protocol in the emergency department to include temperature checks, oxygen saturation, and COVID-19 screening [57]. However, stroke patients may be unable to answer screening questions in which case they should ideally be considered potential carriers of SARS-CoV-2 [47]. Canadian physicians have offered a “Protected Code Stroke Pathway” [58], the implementation of which may be complicated by the limited availability of personal protective equipment (PPEs) [47, 57].
The interim guidance by AHA/ASA has called for some flexibility in algorithms and guidelines to balance the need for providing optimal care while minimizing the spread of SARS-CoV-2 [47], a goal requiring careful coordination not only within each institution but also among comprehensive hospital networks. Further recommendations have been proposed by Canadian Stroke Best Practices Advisory Council and American clinicians on hospitalization measures, transfers, rehabilitation, discharge, and secondary prevention for stroke patients during the COVID-19 pandemic [59, 60]. It is crucial that quality of care for suspected and confirmed cerebrovascular cases are not overlooked even amid a pandemic, given the uncertainty about when cases may subside and in preparation for future waves of infections.
COVID-19 Disease as the Presenting Complaint
There have been reports of patients presenting with CVAs that appear to have been triggered by an underlying SARS-CoV-2 infection [61]. Thus, COVID-19 patients should be reciprocally screened for hypercoagulable states and assessed for risk of thrombotic events. The case of the 68-year-old patient with AIS reported in this paper falls into this category. Her initial presentation and reason for hospitalization was a deteriorating respiratory function related to SARS-CoV-2. COVID-19 patients with any of the risk factors, including advanced age, diabetes, hypertension, past history of cerebrovascular disease, severe COVID-19, increased D-dimer levels, or heightened inflammatory response reflected in high CRP, are known to be at significantly increased risk of CVD [23]. It should be noted, however, that the aforementioned risk factors in this study were shared among subjects with CVD and their independent risk contribution is not well established. Clinically, however, given the urgency of the situation, justification exists for thromboprophylactic measures in all hospitalized COVID-19 patients who have been cleared of any contraindications, especially those in whom the above risk factors are clearly present. It should be noted that many questions remain unanswered on the disease mechanisms involved. Current studies are incomplete and, in certain cases, suffer from potentially imperfect analysis, and thus, clinical signs and evidence should continue to be the primary driving force behind therapeutic and prophylactic decisions in individual COVID-19 patients within the judgement of each clinician until such time that more systemic guidance is available based on larger-scale clinical trials.
It has been argued that a number of hospitalized COVID-19 patients often fit criteria for increased risk of thromboembolic events and qualify for thromboprophylaxis purely by virtue of their respiratory failure, immobilization, and acute respiratory infection [62]. A retrospective comparison of coagulation features between severe pneumonia in the setting of SARS-CoV-2 versus non-SARS-CoV-2 pneumonia showed 28-mortality reduction with the use of LMWH thromboprophylaxis compared to no thromboprophylaxis, in a subgroup of SARS-CoV-2–positive patients but only those with markedly elevated D-dimer levels [63]. There has been some disagreement among clinicians on possible interim measures when it comes to the management of hypercoagulation. Tang et al. have presented claims that LMWH is associated with better prognosis in severe COVID-19 patients, but the basis of this finding has been challenged by others [64, 65]. The International Society on Thrombosis and Haemostasis (ISTH) has issued interim guidance authored by Tang et al. for the use of LMWH in select patients, a recommendation that has been challenged by Porfidia et al. and separately called upon for modification by Barret et al. who have argued for more liberal prophylaxis beginning with unfractionated heparin even prior to significant clinical deterioration, followed by additional regimens as indicated such as the use of tPA in cases of overlapping pulmonary embolism [62, 66, 67]. It should be noted that thrice-daily unfractionated heparin is not ideal given the need to reduce patient contact during the pandemic, and thromboprophylaxis agents such as LMWH or fondaparinux may be more appropriate, at least from that point of view. Barret et al., Wang et al., and Moore et al. have gone further to suggest tPA as a treatment for COVID-19-associated ARDS [67–69]. Moore et al. have also proposed clinical trials in collaboration with Genentech Inc. in a selective cohort of patients [70]. However, the evidence in support of such a therapy is as of yet insufficient.
The American Society of Hematology (ASH) has provided guidance on this issue, calling for VTE thromboprophylaxis with LMWH or fondaparinux. At this point in time, the ASH has not taken a position regarding the use of therapeutic-intensity anticoagulation in the absence of confirmed or suspected venous thromboembolism [71]. However, the evidence from the Dutch study by Kolk et al. of 184 COVID-19 patients showed that even with standard thromboprophylaxis with LMWH, 31% of subjects experienced thrombotic complications, 27% of which were confirmed as venous thrombosis [31]. Helms et al. also found an increased risk of thrombosis despite standard anticoagulation therapy [72]. Thus, standard LMWH may be insufficient and heightened levels of prophylaxis may potentially be required. This is of particular importance for patients with correlates of elevated risk for COVID-19-associated CVD in whom laboratory indicators of coagulopathy are markedly abnormal.
Conclusions
SARS-CoV-2 has presented ever-increasing challenges to every facet of clinical medicine. CVAs are a precarious source of morbidity even in the most ideal of situations. They have become ever more significant not only due to the difficulties in maintaining optimal care during a pandemic but also due to an increased risk presented by COVID-19. Furthermore, patient apprehension has even resulted in some cases of non-COVID-19-related strokes being left unreported and untreated [53]. It is crucial and possible for standards of care to be maintained while allowing for flexibility towards balancing CVA patient care with reducing infectious spread [73].
Though it is recommended that the management of COVID-19 patients with stroke follows similar standards to patients without COVID-19, special considerations must be made. Prophylactic anticoagulation—preferably in the context of a clinical trial—may be warranted in COVID-19 patients without confirmed or suspected venous thromboembolism (VTE) and for whom contraindications have been ruled out. There has been some debate on whether prophylactic, intermediate, or therapeutic dosing is appropriate in such COVID-19 patients. At the time of this paper’s publication, the American Society of Hematology recommends prophylactic-intensity anticoagulation in critically or acutely ill COVID-19 patients without confirmed or suspected VTE, given the hypercoagulable state resulting from the disease [74]. Drug interactions with COVID-19 medications should also be taken into account. A helpful resource for COVID-19 drug interactions is found via the University of Liverpool [75]. The National Institutes of Health has further up-to-date recommendations on which clinicians can additionally rely [76]. In patients with documented evidence of acute ischemic stroke, standard stroke treatment protocols should be followed, while taking necessary precautions to limit infection spread. Special care should be taken to reduce time to treatment with the appropriate agent while ensuring that hemorrhagic stroke and risk of bleeding are ruled out [77]. There has not been any evidence thus far against the use of tPA for intravenous thrombolysis when otherwise appropriate [78, 79]. While standard stroke treatment with the complete range of pharmaceutical and surgical options is to be considered, it should be noted that the hypercoagulable state in COVID-19 could theoretically raise the possibility of reocclusion. The latter combined with the risk of hemorrhagic conversion requires close monitoring following any reperfusion therapy, within the limits of infectious disease protocols [77, 80].
Clinicians should modulate official guidelines for each individual patient based on their existing risk factors, frequent analysis of trends in the patient’s laboratory results (e.g., D-dimers), and evolving clinical picture to determine the need for prophylaxis, diagnostic imaging, and treatment. Communication and coordination with support staff to ensure detection of neurological signs in at-risk patients with frequent monitoring can further improve outcomes. The findings reported herein are sure to continue evolving in the coming months. Studies have found COVID-19-associated ischemic stroke to be more severe and result in both worse functional outcomes and higher mortality [81]. Thus, it is imperative that clinicians continue remaining up to date with present research, clinical trials, and new epidemiological findings.
Authors’ Contributions
Dr. Pooia Fattahi and Dr. Masoud Yeganegi contributed equally to the literature review, writing, and editing process of this publication. Additionally, Dr. Pooia Fattahi was responsible for acquiring material relevant to the patient case report, as well as securing the patient’s consent for its publication.
Data Availability
Not applicable.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. However, explicit consent for publication was sought and received from the patient.
Consent to Participate
Not applicable (however, consent was received for the case report contained in the publication; please see below under “Consent for publication”).
Consent for Publication
Both oral and written consent was received from the patient, who has reviewed the material prior to its publication.
Code Availability
Not applicable.
Footnotes
This article is part of the Topical Collection on Covid-19
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;0(0). doi:10.1016/s2468-2667(20)30085-2 [DOI] [PMC free article] [PubMed]
- 4.Wang K, Qiu Z, Liu J, Fan T, Liu C, Tian P, Wang Y, Ni Z, Zhang S, Luo J, Liu D, Li W. Analysis of the clinical characteristics of 77 COVID-19 deaths. Sci Rep. 2020;10(1):16384. doi: 10.1038/s41598-020-73136-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ascierto PA, Fox B, Urba W, et al. Insights from immuno-oncology: the Society for Immunotherapy of Cancer Statement on access to IL-6-targeting therapies for COVID-19. J Immunother Cancer. 2020;8(1):e000878. doi: 10.1136/jitc-2020-000878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu X, Han M, Li T, Sun W, Wang D, Fu B, Zhou Y, Zheng X, Yang Y, Li X, Zhang X, Pan A, Wei H. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci. 2020;202005615:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borba MGS, Val FFA, Sampaio VS, et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Netw Open. 2020;3(4.23):e208857. doi:10.1001/jamanetworkopen.2020.8857 [DOI] [PMC free article] [PubMed]
- 10.Fihn SD, Perencevich E, Bradley SM. Caution needed on the use of chloroquine and hydroxychloroquine for coronavirus disease 2019. JAMA Netw Open. 2020;3(4.23):e209035. doi:10.1001/jamanetworkopen.2020.9035 [DOI] [PubMed]
- 11.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alonso-Fernández A, Suquia AG, de la Peña M, Casitas R, Pierola J, Barceló A, Soriano JB, Fernández-Capitán C, Martinez-Ceron E, Carrera M, García-Río F. OSA is a risk factor for recurrent VTE. Chest. 2016;150(6):1291–1301. doi: 10.1016/j.chest.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Shitrit D, Peled N, Shitrit AB-G, Meidan S, Bendayan D, Sahar G, Kramer MR. An association between oxygen desaturation and D-dimer in patients with obstructive sleep apnea syndrome. Thromb Haemost. 2005;94(3):544–547. doi: 10.1160/TH05-02-0103. [DOI] [PubMed] [Google Scholar]
- 14.Beltrán-Corbellini Á, Chico-García JL, Martínez-Poles J, et al. Acute-onset smell and taste disorders in the context of Covid-19: a pilot multicenter PCR-based case-control study. Eur J Neurol. 2020:ene.14273. doi:10.1111/ene.14273 [DOI] [PMC free article] [PubMed]
- 15.Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, Boscolo-Rizzo P. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA. 2020;323:2089–2090. doi: 10.1001/jama.2020.6771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bertran Recasens B, Martinez-Llorens JM, Rodriguez-Sevilla JJ, Rubio MA. Lack of dyspnea in Covid-19 patients; another neurological conundrum? Eur J Neurol. 2020:ene.14265. doi:10.1111/ene.14265 [DOI] [PMC free article] [PubMed]
- 17.Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543oc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may be at least partially responsible for the respiratory failure of COVID-19 patients. J Med Virol. 2020;92:552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baker HA, Safavynia SA, Evered LA. The ‘third wave’: impending cognitive and functional decline in COVID-19 survivors. Br J Anaesth. 2020;126:44–47. doi: 10.1016/j.bja.2020.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hampshire A, Trender W, Chamberlain SR, et al. Cognitive deficits in people who have recovered from COVID-19 relative to controls: An N=84,285 online study. medRxiv. 2020:2020.10.20.20215863. doi:10.1101/2020.10.20.20215863.
- 21.Zhou H, Lu S, Chen J, Wei N, Wang D, Lyu H, Shi C, Hu S. The landscape of cognitive function in recovered COVID-19 patients. J Psychiatr Res. 2020;129:98–102. doi: 10.1016/j.jpsychires.2020.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, Coles JP, Manji H, al-Shahi Salman R, Menon DK, Nicholson TR, Benjamin LA, Carson A, Smith C, Turner MR, Solomon T, Kneen R, Pett SL, Galea I, Thomas RH, Michael BD, Allen C, Archibald N, Arkell J, Arthur-Farraj P, Baker M, Ball H, Bradley-Barker V, Brown Z, Bruno S, Carey L, Carswell C, Chakrabarti A, Choulerton J, Daher M, Davies R, di Marco Barros R, Dima S, Dunley R, Dutta D, Ellis R, Everitt A, Fady J, Fearon P, Fisniku L, Gbinigie I, Gemski A, Gillies E, Gkrania-Klotsas E, Grigg J, Hamdalla H, Hubbett J, Hunter N, Huys AC, Ihmoda I, Ispoglou S, Jha A, Joussi R, Kalladka D, Khalifeh H, Kooij S, Kumar G, Kyaw S, Li L, Littleton E, Macleod M, Macleod MJ, Madigan B, Mahadasa V, Manoharan M, Marigold R, Marks I, Matthews P, Mccormick M, Mcinnes C, Metastasio A, Milburn-McNulty P, Mitchell C, Mitchell D, Morgans C, Morris H, Morrow J, Mubarak Mohamed A, Mulvenna P, Murphy L, Namushi R, Newman E, Phillips W, Pinto A, Price DA, Proschel H, Quinn T, Ramsey D, Roffe C, Ross Russell A, Samarasekera N, Sawcer S, Sayed W, Sekaran L, Serra-Mestres J, Snowdon V, Strike G, Sun J, Tang C, Vrana M, Wade R, Wharton C, Wiblin L, Boubriak I, Herman K, Plant G. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7(10):875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y, Wang M, Zhou Y, Chang J, Xian Y, Mao L, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Lancet. 2020;19. 10.2139/ssrn.3550025. [DOI] [PMC free article] [PubMed]
- 24.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, Cooley LA, Dean NC, Fine MJ, Flanders SA, Griffin MR, Metersky ML, Musher DM, Restrepo MI, Whitney CG. Diagnosis and treatment of adults with community-acquired pneumonia. Am J Respir Crit Care Med. 2019;200(7):E45–E67. doi: 10.1164/rccm.201908-1581ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cagnazzo F, Arquizan C, Derraz I, Dargazanli C, Lefevre PH, Riquelme C, et al. Neurological manifestations of patients infected with the SARS-CoV-2: a systematic review of the literature. J Neurol. 2020;0123456789. 10.1007/s00415-020-10285-9. [DOI] [PMC free article] [PubMed]
- 27.Cleri DJ, Ricketti AJ, Vernaleo JR. Severe acute respiratory syndrome (SARS) Infect Dis Clin N Am. 2010;24(1):175–202. doi: 10.1016/j.idc.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chong PY, Chui P, Ling AE, Franks TJ, Tai DY, Leo YS, Kaw GJ, Wansaicheong G, Chan KP, Ean Oon LL, Teo ES, Tan KB, Nakajima N, Sata T, Travis WD. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128(2):195–204. doi: 10.1043/1543-2165(2004)128<195:AODDTS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Hwang DM, Chamberlain DW, Poutanen SM, Low DE, Asa SL, Butany J. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol. 2005;18(1):1–10. doi: 10.1038/modpathol.3800247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–148. doi: 10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020;0(0). doi:10.1515/cclm-2020-0188 [DOI] [PubMed]
- 35.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, and the Northwell COVID-19 Research Consortium. Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020;18:1517–1519. doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020:jth.14850. doi:10.1111/jth.14850 [DOI] [PMC free article] [PubMed]
- 38.Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020:jth.14854. doi:10.1111/jth.14854 [DOI] [PMC free article] [PubMed]
- 39.Merkler AE, Parikh NS, Mir S, et al. Risk of ischemic stroke in patients with coronavirus disease 2019 (COVID-19) vs patients with influenza. JAMA Neurol. 2020;77(11). doi:10.1001/jamaneurol.2020.2730 [DOI] [PMC free article] [PubMed]
- 40.Belani P, Schefflein J, Kihira S, Rigney B, Delman BN, Mahmoudi K, Mocco J, Majidi S, Yeckley J, Aggarwal A, Lefton D, Doshi AH. COVID-19 is an independent risk factor for acute ischemic stroke. Am J Neuroradiol. 2020;41(8):1361–1364. doi: 10.3174/ajnr.A6650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, Henninger N, Trivedi T, Lillemoe K, Alam S, Sanger M, Kim S, Scher E, Dehkharghani S, Wachs M, Tanweer O, Volpicelli F, Bosworth B, Lord A, Frontera J. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. 2020;51:2002–2011. doi: 10.1161/STROKEAHA.120.030335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu PP, Blet A, Smyth D, Li H. The science underlying COVID-19: implications for the cardiovascular system. Circulation. 2020;142:68–78. doi: 10.1161/CIRCULATIONAHA.120.047549. [DOI] [PubMed] [Google Scholar]
- 43.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta N, Zhao YY, Evans CE. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 45.Evans CE. Hypoxia and HIF activation as a possible link between sepsis and thrombosis. Thromb J. 2019;17(1):16. doi: 10.1186/s12959-019-0205-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382(17):e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Temporary emergency guidance to US stroke centers during the COVID-19 pandemic. Stroke. 2020. doi:10.1161/strokeaha.120.030023
- 48.Podcast: Interim Guidance For Stroke Centers by American Heart Association. https://soundcloud.com/americanheartstroke/interim-guidance-for-stroke. Accessed April 23, 2020.
- 49.Ellul M, Varatharaj A, Nicholson TR, Pollak TA, Thomas N, Easton A, Zandi MS, Manji H, Solomon T, Carson A, Turner MR, Kneen R, Galea I, Pett S, Thomas RH, Michael BD, CoroNerve Steering Committee Defining causality in COVID-19 and neurological disorders. J Neurol Neurosurg Psychiatry. 2020;91(8):811–812. doi: 10.1136/jnnp-2020-323667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, Colombi D, Zaino D, Michieletti E, Guidetti D. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83:1–3. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.COVID-19: are acute stroke patients avoiding emergency care? https://www.medscape.com/viewarticle/928337. Accessed April 23, 2020.
- 52.“Dial 999 for stroke emergencies despite coronavirus” - BBC News. https://www.bbc.com/news/health-52173471. Accessed April 23, 2020.
- 53.Cooper JB, Amin AG, Kim MG, Stein AA, Dominguez J, Amuluru K, Tyagi R, Mayer S, Gandhi CD, al-Mufti F. In defense of our patients: indirect negative neurological consequences of SARS-CoV-2 in the New York epicenter. J Stroke Cerebrovasc Dis. 2020;29(10):105127. doi: 10.1016/j.jstrokecerebrovasdis.2020.105127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bloem BR, Dorsey ER, Okun MS. The coronavirus disease 2019 crisis as catalyst for telemedicine for chronic neurological disorders. JAMA Neurol. 2020;77:927–928. doi: 10.1001/jamaneurol.2020.1452. [DOI] [PubMed] [Google Scholar]
- 55.Specialty guides for patient management during the coronavirus pandemic.; 2020. https://www.england.nhs.uk/coronavirus/publication/specialty-guides/. Accessed April 24, 2020.
- 56.Updated Opinion: Effects of the SARS-CoV-2 pandemic on the care of cerebrovascular diseases (Aktualisierte Stellungnahme: Auswirkungen Der SARS-CoV-2-Pandemie Auf Die Versorgung Zerebrovaskulärer Erkrankungen).; 2020. doi:10.1001/jamaneurol.2020.1127
- 57.Waldman G, Mayeux R, Claassen J, et al. Preparing a neurology department for SARS-CoV-2 (COVID-19): early experiences at Columbia University Irving Medical Center and the New York Presbyterian Hospital in New York City. Neurology. 2020:10.1212/WNL.0000000000009519. [DOI] [PMC free article] [PubMed]
- 58.Khosravani H, Rajendram P, Notario L, Chapman MG, Menon BK. Protected code stroke. Stroke. 2020;51:1891–1895. doi: 10.1161/strokeaha.120.029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith EE, Mountain A, Hill MD, Wein TH, Blacquiere D, Casaubon LK, Linkewich E, Foley N, Gubitz G, Simard A, Lindsay MP, Canadian Stroke Best Practices Advisory Council Canadian stroke best practice guidance during the COVID-19 pandemic. Can J Neurol Sci. 2020;47:1–11. doi: 10.1017/cjn.2020.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dafer RM, Osteraas ND, Biller J. Acute stroke care in the coronavirus disease 2019 pandemic. J Stroke Cerebrovasc Dis 2020;0(0):104881. doi:10.1016/j.jstrokecerebrovasdis.2020.104881, 29. [DOI] [PMC free article] [PubMed]
- 61.Zhai P, Ding Y, Li Y. The impact of COVID-19 on ischemic stroke: a case report. Res Sq. 2020. doi:10.21203/RS.3.RS-20393/V1 [DOI] [PMC free article] [PubMed]
- 62.Porfidia A, Pola R. Venous thromboembolism in COVID-19 patients. J Thromb Haemost. 2020;18:1516–1517. doi: 10.1111/jth.14842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020:3–6. 10.1007/s11239-020-02105-8. [DOI] [PMC free article] [PubMed]
- 64.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coto-Hernández R, Fábregas Ruano MT. Reply to “Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy.” J Thromb Haemost. 2020:jth.14852. doi:10.1111/jth.14852 [DOI] [PMC free article] [PubMed]
- 66.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barrett CD, Moore HB, Yaffe MB, Moore EE. ISTH interim guidance on recognition and management of coagulopathy in COVID-19: a comment. J Thromb Haemost. 2020:jth.14860. doi:10.1111/jth.14860 [DOI] [PMC free article] [PubMed]
- 68.Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, Yaffe MB, Moore HB, Barrett CD. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020;18:1752–1755. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moore HB, Barrett CD, Moore EE, McIntyre RC, Moore PK, Talmor DS, Moore FA, Yaffe MB Is there a role for tissue plasminogen activator (tPA) as a novel treatment for refractory COVID-19 associated acute respiratory distress syndrome (ARDS)? J Trauma Acute Care Surg. 2020:1. doi:10.1097/ta.0000000000002694, 713, 714. [DOI] [PMC free article] [PubMed]
- 70.Moore EE. Study of alteplase for respiratory failure in SARS-Cov2 (COVID-19). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04357730. Published 2020. Accessed April 22, 2020.
- 71.COVID-19 and VTE-anticoagulation - Hematology.org. https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation. Accessed April 25, 2020.
- 72.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients in severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Markus HS. EXPRESS: COVID-19 and stroke - a global world stroke organisation perspective. Int J Stroke. 2020;1747493020923472:361–364. doi: 10.1177/1747493020923472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.ASH guidelines on use of anticoagulation in patients with COVID-19 - hematology.Org. https://www.hematology.org/education/clinicians/guidelines-and-quality-care/clinical-practice-guidelines/venous-thromboembolism-guidelines/ash-guidelines-on-use-of-anticoagulation-in-patients-with-covid-19. Accessed December 20, 2020.
- 75.Liverpool COVID-19 Interactions. https://covid19-druginteractions.org/. Accessed December 20, 2020.
- 76.NIH COVID-19 treatment guidelines on antithrombotic therapy. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/adjunctive-therapy/antithrombotic-therapy/. Published 2020. Accessed December 20, 2020.
- 77.Dogra S, Jain R, Cao M, Bilaloglu S, Zagzag D, Hochman S, Lewis A, Melmed K, Hochman K, Horwitz L, Galetta S, Berger J. Hemorrhagic stroke and anticoagulation in COVID-19. J Stroke Cerebrovasc Dis. 2020;29(8):104984. doi: 10.1016/j.jstrokecerebrovasdis.2020.104984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, Kucher N, Studt JD, Sacco C, Bertuzzi A, Sandri MT, Barco S, Humanitas COVID-19 Task Force Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Qi X, Keith KA, Huang JH. COVID-19 and stroke: a review. Brain Hemorrhages. 2020. 10.1016/j.hest.2020.11.001. [DOI] [PMC free article] [PubMed]
- 80.Katz JM, Libman RB, Wang JJ, Sanelli P, Filippi CG, Gribko M, Pacia SV, Kuzniecky RI, Najjar S, Azhar S. Cerebrovascular complications of COVID-19. Stroke. 2020;51(9):227–231. doi: 10.1161/STROKEAHA.120.031265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ntaios G, Michel P, Georgiopoulos G, Guo Y, Li W, Xiong J, Calleja P, Ostos F, González-Ortega G, Fuentes B, Alonso de Leciñana M, Díez-Tejedor E, García-Madrona S, Masjuan J, DeFelipe A, Turc G, Gonçalves B, Domigo V, Dan GA, Vezeteu R, Christensen H, Christensen LM, Meden P, Hajdarevic L, Rodriguez-Lopez A, Díaz-Otero F, García-Pastor A, Gil-Nuñez A, Maslias E, Strambo D, Werring DJ, Chandratheva A, Benjamin L, Simister R, Perry R, Beyrouti R, Jabbour P, Sweid A, Tjoumakaris S, Cuadrado-Godia E, Campello AR, Roquer J, Moreira T, Mazya MV, Bandini F, Matz K, Iversen HK, González-Duarte A, Tiu C, Ferrari J, Vosko MR, Salzer HJF, Lamprecht B, Dünser MW, Cereda CW, Quintero ÁBC, Korompoki E, Soriano-Navarro E, Soto-Ramírez LE, Castañeda-Méndez PF, Bay-Sansores D, Arauz A, Cano-Nigenda V, Kristoffersen ES, Tiainen M, Strbian D, Putaala J, Lip GYH. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the Global COVID-19 Stroke Registry. Stroke. 2020;51:254–258. doi: 10.1161/STROKEAHA.120.031208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.