Abstract
Objective:
This study examined the relationship between maternal anemia and fetal oxygenation status at delivery as measured by umbilical cord pO2.
Methods:
This is a secondary analysis of a prospective cohort study of singleton term deliveries with universal admission CBC and umbilical cord gases between 2010 and 2014. Maternal anemia was defined as hemoglobin ≤ 10 g/dl on admission. The primary outcomes were umbilical artery (UA) and vein (UV) pO2; secondary outcomes were acidemia (UA pH<7.1), hypoxemia (UA/UV pO2 <5th percentile), and hyperoxemia (UA/UV pO2>90th percentile). Outcomes were compared between patients with and without anemia.
Results:
Maternal anemia was associated with a significantly higher UA pO2 [median (IQR) 20 (16, 24) vs 19 (15, 24) mmHg, p=0.01] and UV pO2 [30 (25, 36) vs 29 (23, 34) mmHg, p<0.01]. Neonates born to anemic mothers were more likely to have UV hyperoxemia (15.7% vs 10.9%, aOR 1.51, 95% CI 1.26-1.81) with no difference in UA hyperoxemia. There was no difference in rates of UA or UV hypoxemia. Although maternal anemia was associated with a significant difference in UA pH (7.28 ± 0.060 vs 7.27 ± 0.065, p<0.01), there was no difference in the rate of neonatal acidemia between groups (1.6% vs 1.9%, aOR 0.93, 95% CI 0.55-1.55).
Conclusion:
Umbilical cord O2 content is higher in anemic mothers. Maternal anemia may lead to adaptations in maternal, placental and fetal physiology allowing for easier unloading of O2 to the placenta and increased O2 transfer to the fetus.
Introduction:
Anemia is one of the most commonly diagnosed comorbidities in pregnancy. A national study looking at anemia in pregnancy when hemoglobin was defined as ≤ 10 g/dL found a prevalence 22 out of 1,000 pregnancies. However, this prevalence was even higher in African American and adolescent populations.1,2
Pregnancy is associated with physiologic changes that inherently worsen anemia. Maternal blood volume expands by 50% throughout pregnancy with a greater expansion in the plasma volume, resulting in a drop in hemoglobin levels.3 There is also an increasing iron requirement during pregnancy that without adequate supplementation may result in decreased erythropoiesis.4 For these reasons, the incidence of anemia progressively increases throughout pregnancy. The USPSTF found the prevalence of iron deficiency in pregnancy to be 18%, with at least 5% of these women having concomitant anemia.5
Anemia increases the risks of obstetrical complications including intrauterine growth restriction, preterm labor, and perinatal death.6–12 In fact, Murphy et al demonstrated a 1.18-1.75-fold higher relative risk of these complications in patients diagnosed with anemia between 13-24 weeks of pregnancy.10 Additionally, studies have found that the degree of anemia directly impacts these risks, with one study showing a dose-related decrease in neonatal weight with lower hemoglobin values.11–12 For these reasons, previous studies have suggested maintaining a hemoglobin level between 10-12 g/dL throughout pregnancy to optimize pregnancy and neonatal outcomes.13
The placenta helps facilitate O2 transfer from maternal red blood cells to the fetal circulation. O2 delivery to the placenta depends on uterine blood flow and O2 content in the maternal arterial circulation, which is dependent on hemoglobin concentration.14 While studies have found that both maternal and fetal physiology may be protective against anemia and changes and O2 delivery to the placenta,15 there is little known about the effect of decreased O2 carrying capacity on intrapartum placental O2 transfer and fetal oxygenation.
We tested the hypothesis that maternal anemia decreases intrapartum placental O2 transfer through measurement of umbilical cord pO2 and pH at the time of delivery.
Methods:
This was a planned secondary analysis of a prospective cohort study conducted at a single tertiary care center between 2010 and 2014.16 This study was approved by the Washington University School of Medicine Human Research Protection Office. The primary study included patients with singleton, term, nonanomalous pregnancies admitted to Labor and Delivery for spontaneous labor or an induction of labor. Patients were excluded from this analysis if they did not have paired and validated cord gases and a universal admission CBC. Patients with sickle cell disease or sickle cell trait were excluded.
Per hospital policy, paired umbilical cord gases were collected for every patient in a standardized fashion by trained medical personnel. The umbilical cord was clamped and cut immediately following delivery. Both arterial and venous cord gases were obtained from this segment of clamped cord. These samples were collected prior to the initiation of universal delayed cord clamping at our institution. The samples were analyzed using the ABL800 benchtop gas analyzer. Cord gases were considered validated if the umbilical artery pH was at least 0.02 less than the umbilical vein pH.17
Baseline maternal demographics as well as data on the antenatal and intrapartum course were collected from medical records by trained research staff.17 The primary exposure was maternal anemia defined as hemoglobin ≤ 10 g/dl on admission.18–19 This cut-off was used in order to identify patients that were more likely to have pathologic anemia. The primary outcomes for this analysis were umbilical artery (UA) and umbilical vein (UV) pO2. Secondary outcomes were acidemia (UA pH <7.1), UA/UV hypoxemia defined as pO2 <5th percentile in this cohort, and UA/UV hyperoxemia defined as pO2 >90th percentile in this cohort, and composite neonatal morbidity defined as any of the following diagnoses: neonatal death, hypoxic ischemic encephalopathy, need for hypothermia treatment, intubation, mechanical ventilation, and meconium aspiration syndrome.17 These outcomes were compared between patients with and without anemia. To determine if placental O2 transfer is specifically affected by a common subgroup of anemia, microcytic anemia, a subgroup analysis was performed comparing outcomes between patients with and without hemoglobin ≤ 10 g/dl and mean corpuscular volume (MCV) < 80 fL. We performed a sensitivity analysis in patients with severe anemia defined as Hgb ≤ 8 g/dl.
Baseline characteristics of patients with and without anemia were compared using univariate analyses. Continuous outcomes were compared using the Student’s t test or Mann-Whitney U tests. Categorical outcomes were compared using the χ2 or Fisher exact test. Primary and secondary outcomes were compared using the Mann-Whitney U-test. Multivariable logistic regression was used to adjust for confounders. Confounders were selected on the basis of biologic plausibility and results of the univariate analyses. The variables entered into the initial regression model included hypertensive disorders of pregnancy, adolescent pregnancy, advanced maternal age, obesity, smoking, induction of labor, cesarean section, and prolonged second stage of labor. Backward step-wise elimination was used to reduce the number of variables in the model. The final model included variables that had at least a 10% effect on the magnitude of the odds ratio associated with anemia. Model fit was assessed using the Hosmer-Lemeshow goodness of fit test.
Results:
Of the 8,580 patients in the original study, 7,717 patients had paired, validated cord gases, an admission CBC, and did not have sickle cell disease or trait and were included in this analysis. Of these, 1097 (14.2%) patients were anemic and 6620 (85.8%) were not (Figure 1). Among patients with anemia, 602 (54.9%) had microcytic anemia.
Figure 1:
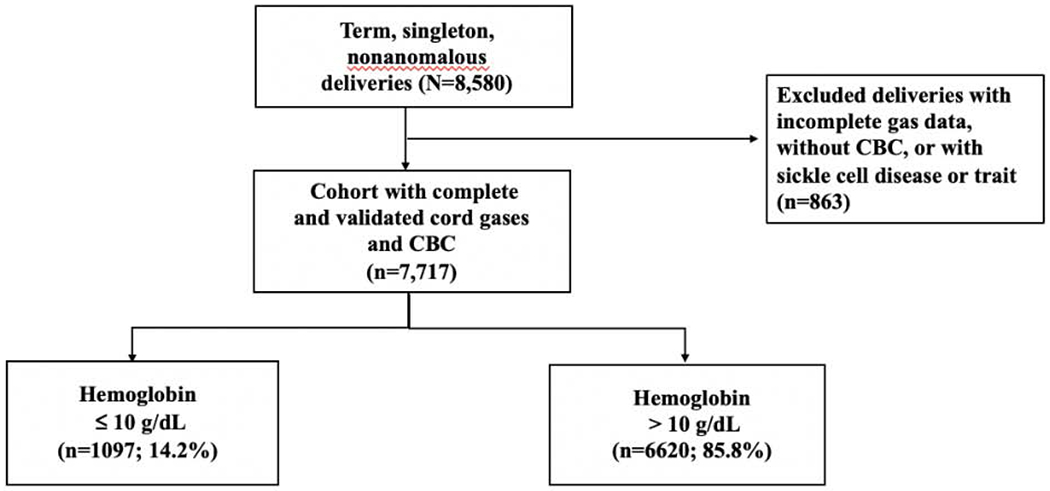
Flowchart of study participants
Baseline maternal characteristics were compared between patients with and without anemia. Patients with anemia were more likely to be younger than those without anemia, with a greater proportion of adolescents in the anemic group and a greater proportion of advanced maternal age patients in the non-anemic group. Patients with anemia were more likely to have hypertensive disorders of pregnancy, be multiparous, use tobacco, and report illicit drug use compared to those without anemia. The incidence of chronic hypertension and preexisting diabetes was similar between groups. The proportion of patients who were admitted for an induction of labor was significantly greater in the anemic group than in the nonanemic group. Patients with anemia were more likely to have a spontaneous vaginal delivery and less likely to have an operative vaginal delivery or cesarean section compared to nonanemic patients (Table 1).
Table 1:
Baseline characteristics of patients with and without anemia
| Anemia N=1097 | No anemia N=6620 | P value | |
|---|---|---|---|
| Maternal age (y) | 24 ± 5.4 | 26 ± 6.0 | <0.01 |
| AMA | 63 (5.7) | 627 (9.5) | <0.01 |
| Adolescent (≤ 19y) | 192 (17.5) | 967 (14.6) | 0.01 |
| Race | <0.01 | ||
| African American | 958 (87.6) | 4073 (62.0) | |
| Caucasian | 84 (7.7) | 1648 (25.1) | |
| Hispanic | 35 (3.2) | 512 (7.8) | |
| Other | 17 (1.6) | 332 (5.1) | |
| Gestational age (wks) | 39 ± 1.3 | 39 ± 1.2 | <0.01 |
| BMI (kg/m2) | 32 ± 7.6 | 32 ± 7.3 | <0.01 |
| Obesity | 554 (50.5) | 3831 (57.9) | <0.01 |
| Chronic HTN | 55 (5.0) | 313 (4.7) | 0.65 |
| HTN disorders of pregnancy | 198 (19.0) | 1010 (16.0) | 0.02 |
| Pre existing DM | 13 (1.2) | 107 (1.6) | 0.29 |
| Nulliparous | 327 (29.8) | 2966 (44.8) | <0.01 |
| Smoking | 179 (16.3) | 891 (13.5) | 0.01 |
| Illicit drug use | 149 (13.6) | 740 (11.2) | 0.02 |
| Alcohol | 16 (1.5) | 69 (1.0) | 0.23 |
| Induction of labor | 540 (49.2) | 2872 (43.4) | <0.01 |
| Maternal fever | 49 (4.5) | 304 (4.6) | 0.85 |
| Mode of delivery | 0.01 | ||
| SVD | 884 (80.6) | 5093 (76.9) | |
| OVD | 36 (3.3) | 333 (5.0) | |
| CS | 177 (16.1) | 1194 (18.0) | |
| Prolonged first stage of labor* | 53 (5.6) | 276 (4.9) | 0.33 |
| Prolonged second stage of labor* | 41 (4.3) | 398 (7.0) | <0.01 |
| Birthweight (g) | 3229 ± 454 | 3255 ± 464 | 0.09 |
| SGA infant weight | 138 (12.6) | 949 (14.3) | 0.12 |
| Hemoglobin (g/dl) | 9.4 (8.9, 9.8) | 11.8 (11.1, 12.6) | <0.01 |
Values represent mean ± standard deviation, median (interquartile range) or n(%)
SVD spontaneous vaginal delivery, OVD operative vaginal delivery, CS cesarean section
SGA small for gestational age
Duration >95th percentile
Patients with anemia had a significantly higher UA pO2 [median (IQR) 20 (16, 24) vs 19 (15, 24) mmHg, p=0.01] and UV pO2 [30 (25, 36) vs 29 (23, 34) mmHg, p<0.01]. Compared to neonates of nonanemic mothers, neonates born to anemic mothers were more likely to have UV hyperoxemia (15.7% vs 10.9%, aOR 1.51, 95% CI 1.26-1.81) with no difference in UA hyperoxemia (12.2% vs 11.7%, aOR 1.02, 95% CI 0.84-1.24). There was no difference in rates of UA hypoxemia (6.0% vs 7.7%, aOR 0.82, 95% CI 0.62-1.08) or UV hypoxemia (5.4% vs 6.2%, aOR 0.92, 95% CI 0.69-1.23) (Table 2).
Table 2:
Umbilical cord pO2 in anemic and non-anemic patients
| Anemia N= 1097 | No Anemia N=6620 | Unadjusted p-value | aOR (95% CI) | |
|---|---|---|---|---|
| UA pO2 | 20 (16, 24) | 19 (15, 24) | 0.01 | |
| UV pO2 | 30 (25, 36) | 29 (23, 34) | <0.01 | |
| UA pO2<5th percentile | 66 (6.0) | 511 (7.7) | 0.05 | 0.82 (0.62-1.08)* |
| UV pO2 <5th percentile | 59 (5.4) | 407 (6.2) | 0.32 | 0.92 (0.69-1.23)** |
| UA pO2 >90th percentile | 134 (12.2) | 771 (11.7) | 0.59 | 1.02 (0.84-1.24) ¥ |
| UV pO2 >90th percentile | 172 (15.7) | 720 (10.9) | <0.01 | 1.51 (1.26-1.81) |
Data represent median (interquartile range) in mmHg or n (%)
UA 5th percentile is 10 mmHg and 90th percentile is 29 mmHg
UV 5th percentile is 16 mmHg and 90th percentile 39 mmHg
Adjusted for AMA, obesity, and cesarean section
Adjusted for AMA and cesarean section
Adjusted for adolescent, induction of labor, and cesarean section
Adjusted for AMA, obesity, and cesarean section
Patients with anemia had statistically lower UA pH compared with patients without anemia (7.28 ± 0.060 vs 7.27 ± 0.065, p<0.01), however there was no difference in rates of neonatal acidemia between groups (1.6% vs 1.9%, aOR 0.93, 95% CI 0.55-1.55). UA pCO2 was lower in the anemic group compared with the nonanemic group (54 ± 8.6 vs 56 ± 9.6 mmHg, p<0.01). UA lactate was lower in the anemic group (3.0 ± 1.4 vs 3.4 ± 2.0 mmol/L, p<0.01). There was no difference in base excess between the two groups (Table 3).
Table 3:
Other umbilical artery gases
| Anemia N= 1097 | No Anemia N=6620 | p-value | |
|---|---|---|---|
| UA pH | 7.28 ± 0.060 | 7.27 ± 0.065 | <0.01 |
| UA pH<7.1 | 18 (1.6) | 123 (1.9) | 0.62* |
| UA pCO2 | 54 ± 8.6 | 56 ± 9.6 | <0.01 |
| UA base deficit | −2.9 ± 2.4 | −3.0 ± 2.6 | 0.16 |
| UA lactate | 3.0 ± 1.4 | 3.4 ± 2.0 | <0.01 |
Data represent mean ± standard deviation or n(%)
aOR 0.93 (95% CI 0.55-1.55), adjusted for hypertensive disorders of pregnancy, maternal fever, and smoking
There was no difference in composite neonatal morbidity between patients with and without anemia (1.3% vs 1.5%, p=0.73) even after adjusting for adolescent pregnancy, obesity, and cesarean delivery (aOR 1.17, 95% CI 0.68-2.01).
In a subgroup analysis comparing patients with microcytic anemia to patients without anemia, those with microcytic anemia had a significantly higher UV pO2 [median (IQR) 30 (24, 35) vs 29 (23, 34) mmHg, p<0.01] and were significantly more likely to have UV hyperoxemia (14.8% vs 10.9%, aOR 1.44, 95% CI 1.13-1.84) (Table 4).
Table 4:
Umbilical cord pO2 in patients with microcytic anemia
| Microcytic Anemia N= 602 | No Anemia N=6620 | Unadjusted p-value | aOR (95% CI)* | |
|---|---|---|---|---|
| UA pO2 | 19 (16, 24) | 19 (15, 24) | 0.37 | |
| UV pO2 | 30 (24, 35) | 29 (23, 34) | <0.01 | |
| UA pO2< 5th percentile | 34 (5.7) | 511 (7.7) | 0.07 | 0.62 (0.42-0.91) |
| UV pO2 <5th percentile | 36 (6.0) | 407 (6.1) | 0.87 | 0.88 (0.60-1.27) |
| UA pO2 >90th percentile | 64 (10.6) | 771 (11.7) | 0.46 | 0.90 (0.68-1.19) |
| UV pO2 >90th percentile | 89 (14.8) | 720 (10.9) | <0.01 | 1.44 (1.13-1.84) |
Data represent median (IQR) or n(%)
Adjusted for hypertensive disorders of pregnancy, maternal fever, and smoking
In a sensitivity analysis of patients with severe anemia, severe anemia was associated with a higher UA pO2 (median [IQR] 22 [15, 27] vs 19 [15, 24 mmHg], p=0.002) and a higher likelihood of UA and UV hyperoxemia (aOR (95% CI) 2.05 (1.11-3.71) and 2.43 (1.35-4.37)).
Discussion:
In this secondary analysis of a prospective cohort study, we found that maternal anemia is associated with a modest increase in UV O2 and UV hyperoxemia demonstrating possible increased placental O2 transfer compared to patients without anemia. This finding remains significant even when limited to patients with microcytic anemia or severe anemia. Although there were no differences in fetal acidemia or composite neonatal morbidity between patients with and without anemia, subtle differences in UA pH and lactate suggest a possible protective effect of maternal anemia in labor. Contrary to our initial hypothesis, maternal anemia at time of delivery may improve placental O2 transfer by way of more efficient O2 unloading at the maternal-fetal interface.
We initially hypothesized that anemia would result in decreased placental O2 transfer due to existing evidence that suggests increased risk for low birth weight and perinatal mortality in pregnancies complicated by anemia.20 However, previous studies looking at the relationship between maternal anemia and fetal oxygenation have yielded mixed results. Malinowski et al looked specifically at patients with sickle cell disease and found no difference in intrapartum fetal O2 saturation between patients with and without sickle cell disease.21 This was hypothesized to be secondary to the high affinity of fetal hemoglobin to O2 compared to the poor affinity of Hemoglobin S, leading to increased transfer of O2 to the fetus, particularly in cases of fetal acidemia.21–22 They did, however, find that sickle cell disease was associated with a significantly lower umbilical artery and vein pH and higher base excess.21 Another study by Ramirez-Cardich et al investigated maternal anemia and neonatal oxygenation at high altitudes. The authors found that infants born to anemic mothers at high altitudes had no change in arterial O2 saturation or respiratory rate and had significantly higher hematocrits compared to nonanemic mothers.23 To our knowledge, no studies to date have looked at the relationship between anemia, particularly microcytic anemia, and cord gases in a more generalized population. We found that severe anemia was associated with a higher likelihood of both UA and UV hyperoxemia, whereas microcytic anemia was only associated with UV hyperoxemia, raising an interesting question of whether the severity of anemia has a greater impact than the type of anemia during pregnancy.
The association between maternal anemia and higher umbilical vein O2 content is biologically plausible and may in fact be attributed to an adaptive mechanism in pregnancy physiology that causes easier unloading of O2 to the fetus. This hypothesis has been demonstrated by Paulone et al by altering maternal hematocrit and measuring uterine and umbilical blood flow as well as fetal O2 extraction in a sheep model.24 They found that when maternal hematocrit was decreased by up to 50%, fetal O2 extraction increased so as to maintain adequate fetal oxygenation. Another study in pregnant sheep by Delpapa et al demonstrated that uteroplacental O2 consumption remained unchanged in the setting of maternal anemia secondary to increases in O2 extraction.25 Additional studies in both sheep and humans have shown that the fetus can tolerate up to a 50% acute reduction in O2 delivery with a compensatory increase in O2 extraction.26–27 In fact, the rate of O2 consumption during pregnancy increases up to 20% compared to nonpregnant individuals in order to accommodate the O2 demands of the placenta and fetus.28
Compensatory adaptations in placental physiology may also play a role. Woodman et al demonstrated that iron deficiency anemia resulted in a marked increase in placental size.29 Placentas of women with anemia or chronic hypoxia have shown enhanced angiogenesis and increased capillarization, facilitating blood flow and O2 delivery to the fetus.30–31 Another study demonstrated thinning of the placental barrier to maintain fetal O2 transfer during chronic hypoxia.32
Additionally, there may be aspects of maternal and fetal physiology that contribute to our findings. When measuring O2 consumption with different degrees of anemia in fetal lambs, Edelstone et al found that fetal hemoglobin was protective against changes in O2 consumption and acid-base status because of its higher affinity to O2 compared to adult hemoglobin.15 This is because the O2-fetal hemoglobin dissociation curve is shifted leftward compared to that of adult hemoglobin, resulting in higher affinity for O2 and more extraction of O2 from adult hemoglobin.33 Maternal anemia may also cause decreased systemic perfusion and resultant mild maternal lactic acidosis.34 This acidosis could result in a compensatory rightward shift in the O2-hemoglobin dissociation curve allowing easier unloading of O2 to the fetus during labor in anemic mothers.33,35
Our study has several strengths. First, the large prospective cohort design allowed us to detect differences in umbilical cord gases and perform a meaningful subgroup analysis in a common type of anemia seen in pregnancy. An additional strength is that this study was performed in a population with a high baseline prevalence of anemia. Additionally, this study was performed in a center that practices universal admission CBC and cord gas collection, minimizing the potential for selection bias. The validation of cord gases is also a strength. Finally, this study is novel in that it is one of the first studies to look at anemia and its impact on fetal oxygenation during labor, which is critical as the physiology surrounding anemia and its adverse pregnancy outcomes remain poorly understood.
There are limitations that should be considered. We chose umbilical cord pO2 as a primary outcome in this analysis with the specific goal of understanding the impact of anemia on placental O2 transfer, however there is limited data on the predictive ability of umbilical cord pO2 on neonatal outcomes. Regardless, UA pO2 has been demonstrated to be significantly lower in patients with neonatal morbidity.36 Furthermore, it is possible that we did not have adequate power to detect meaningful differences in rare outcomes such as neonatal acidemia. However, post hoc analysis demonstrated that our sample size afforded 90% power to detect a 20% difference in neonatal acidemia between groups suggesting that our findings may reflect a true lack of clinically significant differences in acidemia risk between groups. Our study strictly focuses on peripartum placental O2 transfer, which may not reflect antenatal mechanisms that account for chronic hypoxia-related conditions such as IUGR. Additionally, we do not have information on iron studies, antenatal management of anemia or intrapartum resuscitative interventions, including O2 administration. Although we adjusted for relevant confounders that may impact fetal oxygenation or the hemoglobin dissociation curve, it is possible that residual confounders exist in the relationship between anemia and placental O2 transfer.
In conclusion, this study demonstrates increased intrapartum placental O2 transfer to the fetus in the setting of maternal anemia. Further understanding of adaptations in maternal, placental, and fetal physiology would allow for risk stratification and identification of patients who may or may not benefit from intrauterine resuscitative efforts to increase placental O2 transfer. Given that anemia is one of the most commonly diagnosed comorbidities in pregnancy and is associated with adverse pregnancy outcomes, this study calls for a deeper understanding of the impact of anemia on pregnancy physiology and fetal oxygenation status.
Acknowledgments
Funding: Dr. Raghuraman is supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K23HD098315, the Foundation for SMFM/AAOGF, and the Doris Duke Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: The authors report no conflict of interest.
Paper presentation information: Presented at the 40th Annual Pregnancy Meeting, Society for Maternal Fetal Medicine, Grapevine, Texas, February 3-8, 2020.
Condensation: Maternal anemia is associated with increased placental oxygen transfer with higher umbilical vein oxygen content at the time of delivery compared to those without anemia.
- Anemia is one of the most commonly diagnosed comorbidities in pregnancy, yet little is known about the effect of anemia on placental oxygen transfer and fetal oxygenation.
- This secondary analysis of a prospective cohort study found that umbilical cord oxygen content is higher in anemic mothers than non-anemic mothers.
- The results of this study suggest that maternal anemia may be associated with adaptations in maternal, placental, and fetal physiology that allow for easier unloading of oxygen to the placenta and improved fetal oxygenation at delivery.
References:
- 1.Adebisi OY, Strayhorn G. Anemia in pregnancy and race in the United States: Blacks at risk. Fam Med. 2005;37:655–62. [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists. Anemia in pregnancy. ACOG Practice Bulletin No. 95. Obstet Gynecol 2017. Available at: https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2008/07/anemia-in-pregnancy#. [DOI] [PubMed] [Google Scholar]
- 3.Pitkin RM. Nutritional influences during pregnancy. Med Clin North Am. 1977;61(1):3–15. [DOI] [PubMed] [Google Scholar]
- 4.Baynes RD. Iron deficiency In: Brock JH, Halliday JW, Pippard MJ, Powell LW, editors. Iron metabolism in health and disease. Philadelphia (PA): W.B. Saunders; 1994. p.189–225. [Google Scholar]
- 5.U.S. Preventive Services Task Force. Iron deficiency anemia in pregnant women: screening and supplementation. Available at: https://www.uspreventiveservicestaskforce.org/uspstf/document/evidence-summary22/iron-deficiency-anemia-in-pregnant-women-screening-and-supplementation. Retrieved April 24, 2020.
- 6.Davis LE, Hohimer AR, Morton MJ. Myocardial blood flow and coronary reserve in chronically anemic fetal lambs. Am. J. Physiol 1999;277:306–13. [DOI] [PubMed] [Google Scholar]
- 7.Mostello D, Chalk C, Khoury JC, Mack C, Siddiqi TA, Clark KE.. Chronic anemia in pregnant ewes: maternal and fetal effects. Am. J. Physiol 1991;261:1075–83. [DOI] [PubMed] [Google Scholar]
- 8.Scholl TO, Hediger ML, Rischer R, Shearer JW. Anemia vs iron deficiency: increased risk of preterm delivery in a prospective study. Am J Clin Nutr. 1992;55:985–8. [DOI] [PubMed] [Google Scholar]
- 9.Klebanoff MA, Shiono PH, Selby JV, Trachtenberg AI, Graubard BI. Anemia and spontaneous preterm birth. Am J Obstet Gynecol. 1991;164:59–63. [DOI] [PubMed] [Google Scholar]
- 10.Murphy JF, Newcombe RG, O-Riordan J, Coles EC, Pearson JF. Relation of haemoglobin levels in the first and second trimesters to outcome of pregnancy. Lancet. 1986;327:992. [DOI] [PubMed] [Google Scholar]
- 11.Allen LH. Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr. 2000;71(5):1280S–1284S. [DOI] [PubMed] [Google Scholar]
- 12.Dreyfuss M. Anemia and iron deficiency during pregnancy: etiologies and effects on birth outcomes in Nepal. PhD dissertation, Johns Hopkins University, Baltimore, 1998. [Google Scholar]
- 13.Kumar KJ, Asha N, Murphy DS, Sjatha MS, Manjunath VG. Maternal anemia in various trimesters and its effect on newborn weight maturity: an observational study. Int J Prev Med. 2013;4(2):193–199. [PMC free article] [PubMed] [Google Scholar]
- 14.Carter AM. Evolution of factors affecting placental oxygen transfer. Placenta. 2009:30;19–25. [DOI] [PubMed] [Google Scholar]
- 15.Edelstone DI, Darby MJ, Bass K, Miller K. Effects of reductions in hemoglobin-oxygen affinity and hematocrit level on oxygen consumption and acid-base status in fetal lambs. Am J Obstet Gynecol. 1989;160:820–6. [DOI] [PubMed] [Google Scholar]
- 16.Cahill AG, Tuuli MG, Stout MJ, López JD, Macones GA. A prospective cohort study of fetal heart rate monitoring: deceleration area is predictive of fetal acidemia. Am J Obstet Gynecol. 2018;218:523.e1–523.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raghuraman N, Temming LA, Stout MJ, Macones GA, Cahill AG, Tuuli MG. Intrauterine hyperoxemia and risk of neonatal morbidity. Obstet Gynecol. 2017;129:676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sifakis S, Pharmakides G. Anemia in pregnancy. Ann N Y Acad Sci. 2000;900:125–136. [DOI] [PubMed] [Google Scholar]
- 19.Moghaddam Tabrizi F, Barjasteh S. Maternal hemoglobin levels during pregnancy and their association with birth weight of neonates. Iran J Ped Hematol Oncol. 2015;5:211–217. [PMC free article] [PubMed] [Google Scholar]
- 20.Rahman MM, Abe SK, Rahman MS, Kanda M, Narita S, Bilano V et al. Maternal anemia and risk of adverse birth and health outcomes in low- and middle-income countries: systematic review and meta-analysis. Am J Clin Nutr. 2016;103(2):495–504. [DOI] [PubMed] [Google Scholar]
- 21.Malinowski AK, Cheung P, Yang J, D’Souza R, Shehata N, Ward R, et al. Cord gas parameters in infants born to women with sickle cell disease: a retrospective matched cohort study. Br J Haematol. 2019;184:653–657. [DOI] [PubMed] [Google Scholar]
- 22.Ueda Y, Nagel RL, Bookchin RM. An increased Bohr effect in sickle cell anemia. Blood. 1979;53:472–80. [PubMed] [Google Scholar]
- 23.Ramirez-Cardich ME, Saito M, Gilman RH, Escate LE, Strouse JJ, Kabrhel C, et al. Effect of maternal anemia at high altitude on infant hematocrit and oxygenation. Am J Trop Med Hyg. 2004;70:420–4. [PubMed] [Google Scholar]
- 24.Paulone ME, Edelstone DI, Shedd A. Effects of maternal anemia on uteroplacental and fetal oxidative metabolism in sheep. Am J Obstet Gynecol. 1987;156:230–6. [DOI] [PubMed] [Google Scholar]
- 25.Delpapa EH, Edelstone DI, Milley JR, Balsan M. Effects of chronic maternal anemia on systemic and uteroplacental oxygenation in near-term pregnant sheep. Am J Obstet Gynecol. 1992;166:1007–12. [DOI] [PubMed] [Google Scholar]
- 26.Almendros I, Martínez-Ros P, Farré N, Rubio-Zaragoza M, Torres M, Gutiérrez-Bautista ÁJ, et al. Placental oxygen transfer reduces hypoxia-reoxygenation swings in fetal blood in sheep model of gestational sleep apnea. J Appl Physiol. 1985;127:745–752. [DOI] [PubMed] [Google Scholar]
- 27.Carter AM. Placental gas exchange and oxygen supply to the fetus. Compr Physiol. 2015;5:1381–403. [DOI] [PubMed] [Google Scholar]
- 28.Hytten FE, Leitch I. The Physiology of Human Pregnancy. Oxford: Blackwell Scientific Publications; 1971. [Google Scholar]
- 29.Woodman AG, Care AS, Mansour Y, Cherak SJ, Panahi S, Gragasin FS, et al. Modest and severe maternal iron deficiency in pregnancy are associated with fetal anaemia and organ-specific hypoxia in rats. Sci Rep. 2017;7:46573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mayhew TM. Changes in fetal capillaries during preplacental hypoxia: growth, shape remodeling and villous capillarization in placentae from high-altitude pregnancies. Placenta. 2003;24:191–8. [DOI] [PubMed] [Google Scholar]
- 31.Lelic M, Bogdanovic G, Ramic S, Brkicevic E. Influence of maternal anemia during pregnancy on placenta and newborns. Med Arch. 2014;68:184–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kingdom JC, Kaufmann P. Oxygen and placental villous development: origins of fetal hypoxia. Placenta. 1997;18:613–21. [DOI] [PubMed] [Google Scholar]
- 33.Kaufman DP, Dhamoon AS. Physiology, Oxyhemoglobin dissociation curve. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499818/. [PubMed] [Google Scholar]
- 34.Finch CA, Gollnick PD, Hlastala MP, Miller LR, Dillmann E, Mackler B. Lactic acidosis as a result of iron deficiency. J Clin Invest. 1979;64:129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kennedy AC, Valtis DJ. The oxygen dissociation curve in anemia of various types. J Clin Invest. 1954;33:1372–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raghuraman N, Temming LA, Stout MJ, Macones GA, Cahill AG, Tuuli MG. Umbilical cord oxygen content and neonatal morbidity at term. Am J Perinatol. 2018;35:331–335. [DOI] [PubMed] [Google Scholar]


