Abstract
Objective
This study aimed to analyze the concerns and health‐related behaviors in patients with vasculitis during the early phase of the coronavirus disease 2019 (COVID‐19) pandemic in North America.
Methods
Patients with vasculitis in North America were invited to complete an online survey through the Vasculitis Patient‐Powered Research Network in collaboration with the Vasculitis Foundation and the Relapsing Polychondritis Foundation. Questions focused on concerns and behaviors related to doctors’ visits, tests, medication, and telehealth use. Factors affecting their concern and health‐related behaviors were determined.
Results
Data from 662 patients were included: 90% of patients were White, 78% were women, 83% expressed moderate or high levels of concern about COVID‐19, and 87% reported that their vasculitis moderately or extremely affected their level of concern. Older age, female sex, lung disease, and immunosuppression were associated with greater concern. Doctors’ visits, laboratory tests, and other tests were avoided by 66%, 46%, and 40% of patients, respectively. Younger age, urban location, higher income, higher concern levels, and prednisone use (>10 mg/day) were associated with greater likelihood of avoiding visits or tests. Ten percent of patients on immunosuppressive therapy stopped their medication. Twenty‐nine percent patients on rituximab avoided an infusion. Forty‐four percent of patients had telehealth visits; more visits were reported for younger patients, for patients on glucocorticoids, and in Canada versus the United States.
Conclusion
During the COVID‐19 pandemic, patients with vasculitis have high levels of concern and exhibit potentially harmful health‐related behaviors. Health care use varies across different demographic groups and geographic regions. Specific strategies are warranted to facilitate engagement of these patients with the health care system during the pandemic.
Significance & Innovation.
Patients with vasculitis were highly concerned about contracting severe acute respiratory syndrome coronavirus 2, and most patients reported that their underlying vasculitis affected their level of concern.
Many patients with vasculitis avoided doctors’ office visits, laboratory tests, and other tests and stopped or delayed receipt of immunosuppressive medications, often without a doctor’s advice.
Almost half of patients with vasculitis had a telehealth visit during the pandemic in lieu of an office visit, and most patients reported that telehealth was available to them.
INTRODUCTION
Since the first report of a novel coronavirus–induced (severe acute respiratory syndrome coronavirus 2 [SARS‐CoV‐2]) pneumonia from Wuhan, China, in December 2019, this infectious disease rapidly emerged as a global pandemic (1). Clinically, coronavirus disease 2019 (COVID‐19) ranges from asymptomatic to severe disease with pneumonia, respiratory failure, sepsis, and even death (2). Severe disease is especially prevalent among older patients and patients with preexisting chronic illnesses (3).
In the context of this rapidly evolving global health emergency, it is important to understand the plight of patients living with chronic autoimmune diseases, such as vasculitis. Vasculitis is a group of multisystem disorders characterized by inflammation of blood vessels and is often associated with organ‐ and life‐threatening manifestations. In addition to the day‐to‐day challenges of living with a chronic multisystem disease, the pandemic has created further obstacles in the lives of patients with vasculitis as they try to manage their chronic condition. Many patients face an increased risk of infection due to various factors, such as immunosuppressive medications, older age, and higher incidence of comorbidities (such as diabetes mellitus, cardiovascular disease, hypertension, or lung disease) (4, 5, 6). Difficulties in accessing medical care due to disruptions caused by social distancing and limited availability of routine care have further complicated optimal management of their disease (7).
The objective of this study was to analyze the effects of the COVID‐19 pandemic on patients with vasculitis through a questionnaire, with an emphasis on patients’ concerns and health‐related behaviors, such as avoiding doctors’ visits, laboratory tests, and other tests and stopping immunosuppressive medications. This study also determined the incidence of respiratory illnesses (COVID‐19 and others), the accessibility of testing for COVID‐19, and the availability and use of telehealth in the initial months of the pandemic.
PATIENTS AND METHODS
Study population
Adults (age 18 years and older) with vasculitis from the United States and Canada were invited to participate in an online survey through the Vasculitis Patient‐Powered Research Network (VPPRN) online research platform and two patient advocacy groups, the Vasculitis Foundation and the Relapsing Polychondritis Foundation. The protocol was reviewed and approved by the Advarra Institutional Review Board. Patients who consented to participate completed the survey through a secure website. Patients who completed the baseline survey will be sent links to follow‐up questionnaires every 2 weeks for 12 weeks and then every 4 weeks. The current report details the baseline survey findings from patients who contributed data from April 8, 2020, to May 29, 2020.
Survey elements
The survey was created by a panel of expert physicians and researchers in the fields of vasculitis and inflammatory arthritis, along with patient representatives from the Vasculitis Foundation. It included questions on demographics, comorbidities, the type of vasculitis, immunomodulatory medications, and the daily glucocorticoid dose. There were questions about recent history of any respiratory illnesses (within 2 weeks of the date of survey completion) and whether patients had been diagnosed by a physician with COVID‐19 with or without positive test results. There were also questions about barriers to testing for COVID‐19.
Patients were asked how concerned they were about the COVID‐19 pandemic and how their level of concern was affected by their underlying vasculitis, with each concern measured on a 5‐point Likert scale, including “extremely” (the maximum score of 5), “moderate” (score of 4), “somewhat” (score of 3), “slightly” (score of 2), and “not at all” (score of 1). There were questions about behavioral changes, such as whether patients stopped immunosuppressive therapy, avoided doctor appointments, infusions, or laboratory and diagnostic tests. Patients were asked about availability and use of telehealth.
Geographic data
For patients in the United States with an available 5‐digit zip code, the county of residence was obtained based on zip code tabulation areas (ZCTAs). For areas that bridged more than one county, the center of the ZCTA was used. Information on urban versus rural community residence was available through Centers for Disease Control and Prevention 2013 National Center for Health Statistics classification (online at https://www.cdc.gov/nchs/data_access/urban_rural.htm). Information on education levels and median household income was obtained from the 2014‐2018 American Community Survey 5‐year estimates based on the patient’s zip code (8). The cumulative number of cases of COVID‐19 per capita in the county on the date patients completed the survey was obtained from the publicly available USAFacts database (online at https://usafacts.org/visualizations/coronavirus‐covid‐19‐spread‐map/), accounting for the county population using 2019 Census data. Cases per capita were divided into tertiles in the United States on each day of the study period, with counties weighted by population. This measure assessed COVID‐19 activity in the patient’s county relative to all other counties in the United States on the date the survey was completed.
Statistical analysis
Patient demographics, comorbidities, the type of vasculitis, immunomodulatory treatments, and geographical data were reported for the entire cohort and separately for patients with and without recent respiratory illnesses (COVID‐19 and others). The median levels of concerns across different states and territories were compared graphically across the United States among areas with at least five patients.
Factors potentially influencing 1) patient behavior, 2) levels of concern, 3) the frequency of stopping immunosuppression (other than glucocorticoids), and 4) telehealth use were analyzed and included the type of vasculitis, the type of immunosuppression (rituximab versus other biologics, JAK inhibitors (JAKis) and/or cyclophosphamide versus traditional disease‐modifying antirheumatic drugs without biologics, JAKis, and/or cyclophosphamide versus none), the daily glucocorticoid dose, urban versus rural living, education, median household income, and county of residence (with different tertiles of COVID‐19 cases per capita). The sources of information about COVID‐19 used by patients were reported, and the relationship between telehealth use and the source of information about COVID‐19 was determined.
Kruskal‐Wallis tests were used to compare patient concerns across subgroups. Logistic regression was used to compare behavioral changes across subgroups using univariate analyses, except in the case of telehealth analyses (telehealth analyses were adjusted for the date of survey completion to account for associations between calendar time and telehealth use). χ2 tests were used to determine if telehealth use was associated with receiving COVID‐19–related information and with any health care–related behavioral changes.
RESULTS
Invitations were sent by email messages to 4225 patients; 52.0% (n = 2197) opened the emails, and 30.7% (n = 675) completed the survey. After excluding 13 patients without a diagnosis of vasculitis, 662 patients from the United States (597 patients) and Canada (65 patients) were included in the study. Among them, 91.1% were White and 77.3% were women. The mean age was 55.8 (SD ±13.9) years. The number of patients with different types of vasculitis are shown in Table 1. A total of 313 patients were treated with biologics or cyclophosphamide at the time of the survey, with rituximab being the most commonly used drug (n = 225; 73.1%). The most commonly reported comorbidities were hypertension (278 [42.0%]) and asthma (179 [27.0%]). Almost all patients with eosinophilic granulomatosis with polyangiitis (62 [96.9%]) reported coexistent pulmonary disease. Demographic data of the patients are detailed in Table 1 and Supplemental Table 1.
Table 1.
Demographic and clinical characteristics of patients
| Value | |
|---|---|
| Sample size, N | 662 |
| Age, mean ± SD, y | 55.4 ± 14.0 |
| Female sex, n (%) | 520 (78.5) |
| White, n (%) | 598 (90.3) |
| Hispanic, n (%) | 33 (5.0) |
| United States, n (%) | 597 (90.2) |
| Canada, n (%) | 65 (9.8) |
| Rural, n (%) a | 51/573 (8.9) |
| County cases of COVID‐19 per capita, n (%) a | |
| Lowest tertile | 163/573 (28.4) |
| Middle tertile | 230/573 (40.1) |
| Highest tertile | 180/573 (31.4) |
| Vasculitis types, n (%) | |
| ANCA‐associated vasculitis | |
| Granulomatosis with polyangiitis | 286 (43.2) |
| Microscopic polyangiitis | 54 (8.2) |
| Eosinophilic granulomatosis with polyangiitis | 64 (9.7) |
| Unspecified | 56 (8.5) |
| Giant cell arteritis | 30 (4.5) |
| Takayasu arteritis | 16 (2.4) |
| Relapsing polychondritis | 56 (8.5) |
| Other vasculitides b | 100 (15.1) |
| Medications, n (%) | |
| Rituximab | 225 (34.0) |
| Other biologics and/or JAKis | 77 (11.6) |
| Cyclophosphamide | 11 (1.7) |
| Methotrexate | 109 (16.5) |
| Azathioprine | 96 (14.5) |
|
Mycophenolate |
58 (8.8) |
| Glucocorticoids | |
| None | 364 (55.0) |
| ≤10 mg/day | 238 (36.0) |
| >10 mg/day | 60 (9.1) |
| NSAIDs | 114 (17.2) |
| Comorbidity, n (%) | |
| Hypertension | 278 (42.0) |
| Asthma | 179 (27.0) |
| Kidney disease | 162 (24.5) |
| Diabetes mellitus | 76 (11.5) |
| Other chronic lung disease | 73 (11.0) |
| Heart disease | 66 (10.0) |
| Chronic obstructive pulmonary disease | 45 (6.8) |
| Current smoking | 25 (3.8) |
| Malignancy | 14 (2.1) |
| Organ transplant | 14 (2.1) |
Abbreviations: ANCA, antineutrophil cytoplasmic antibody; COVID‐19, coronavirus disease 2019; JAKi, Janus kinase inhibitor; NSAID, nonsteroidal anti‐inflammatory drug.
United States data are based on zip code.
Other vasculitides included polyarteritis nodosa (n = 10), Behҫet disease (n = 10), cryoglobulinemia (n = 12), central nervous system vasculitis (n = 18), urticarial vasculitis (n = 13), and an unspecified category (n = 39).
COVID‐19 and other respiratory illnesses and SARS‐CoV‐2 testing
Seven (1.0%) patients were diagnosed with COVID‐19, of whom five had a positive SARS‐CoV‐2 test result. The remaining two patients were diagnosed by their health care providers based on their symptoms. Fifty‐nine patients (8.9%) reported having other respiratory infections within the prior 2 weeks. Twenty of 66 patients (30.3%) with a history of respiratory illness and 119 of 596 patients (20.0%) patients without a respiratory illness could not get tested for COVID‐19 because of various reasons, such as test unavailability (60 [43.2%]) and physician disapproval (45 [32.4%]) (Supplemental Table 2). There was no disparity in testing availability between the United States and Canada (P = 0.28). Within the United States, availability of testing did not differ based on rural or urban locations (P = 0.23) or incidence of (P = 0.72).
Concerns about the COVID‐19 pandemic
Most patients were either extremely (n = 328; 49.6%) or moderately concerned (n = 221; 33.4%) about the pandemic. Four‐hundred twelve patients (62.2%) reported that their vasculitis affected their level of concern extremely (Supplemental Figure 1A). Older age (Kruskal‐Wallis P < 0.01), female sex (P = 0.01), and coexisting pulmonary diseases (P < 0.01) were associated with increased levels of concern. Patients on immunosuppressive therapy (P < 0.01) and those with pulmonary diseases (P < 0.01) were more likely to report that their vasculitis affected the level of concern. Levels of concern did not differ based on use of specific immunosuppressive medications (Supplemental Figure 1B and C). Moderate‐high levels of concern were observed uniformly throughout the United States (Figure 1), and the levels of concern were not significantly different between the United States and Canada (P = 0.47). Levels of concern were similar among patients with different types of vasculitis (P = 0.58).
Figure 1.
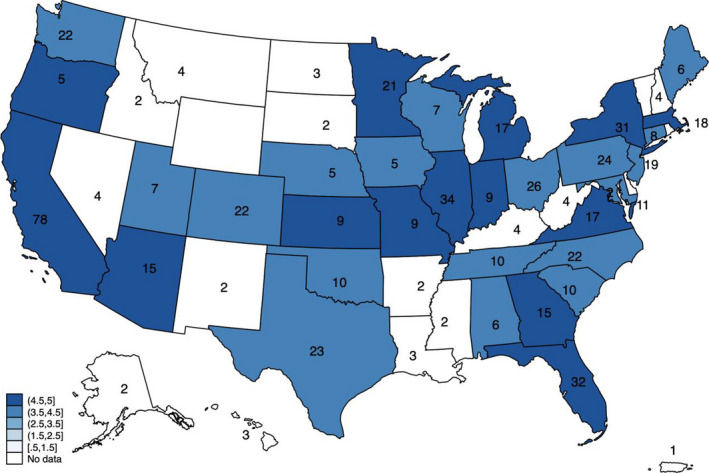
Location of patients in the United States and levels of concern due to coronavirus disease 2019 (COVID‐19) The map shows the distribution of patients within each state or territory, with the color indicating the median level of concern about COVID‐19 infection among patients there. A score of 5 indicates an extreme level of concern, a score of 4 indicates a moderate level of concern, a score of 3 indicates being somewhat concerned, a score of 2 equals being slightly concerned, and a score of 1 equals not at all concerned.
Health‐related behavioral modifications
Table 2 summarizes the findings related to health‐related behavior, and odds ratios from logistic regression models are shown in Supplemental Table 3. Two‐thirds of patients (n = 439; 66.3%) reported avoiding doctors’ visits, and 308 (46.5%) and 265 (40.0%) patients did not go for laboratory tests and other diagnostic tests, respectively. Younger patients (<60 years) were significantly more likely to avoid doctors’ visits and laboratory testing. Urban location and moderate‐high levels of concern were each associated with a significantly higher likelihood of avoiding doctors’ visits and diagnostic tests, and patients in the highest tertile of median household income were significantly more likely to avoid doctors’ visits. Glucocorticoid use (daily dose of prednisone greater than 10 mg) was associated with a significantly higher likelihood of avoiding diagnostic testing. Patients from areas of higher COVID‐19 activity were more likely to avoid going for laboratory tests and other tests.
Table 2.
Impact of COVID‐19 pandemic on patient concerns and health‐related behavior
| n | Avoided going to the doctor’s office, n (%) | Avoided getting laboratory tests, n (%) | Avoided other tests (eg, x‐ray), n (%) | Avoided receiving an infusion (patients on rituximab), n (%) | Had a telehealth visit, n (%) | Stopped medications, n (%) a | |
|---|---|---|---|---|---|---|---|
| All patients | 662 | 439 (66.3) | 308 (46.5) | 265 (40.0) | 43/225 (19.1) | 306 (46.2) | 35/450 (7.8) |
| AAV | 460 | 302 (65.7) | 209 (45.4) | 171 (37.2) | 36/205 (17.6) | 194 (42.2) | 22/333 (6.6) |
| GPA | 286 | 190 (66.4) | 131 (45.8) | 108 (37.8) | 31/145 (21.4) | 111 (38.8) | 15/205 (7.3) |
| MPA | 54 | 37 (68.5) | 24 (44.4) | 15 (27.8) | 2/20 (10.0) | 26 (48.1) | 3/36 (8.3) |
| EGPA | 64 | 45 (70.3) | 32 (50.0) | 31 (48.4) | 1/12 (8.3) | 31 (48.4) | 3/50 (6.0) |
| Unspecified | 56 | 30 (53.6) | 22 (39.3) | 17 (30.4) | 2/28 (7.1) | 26 (46.4) | 1/42 (2.4) |
| Giant cell arteritis | 30 | 19 (63.3) | 14 (46.7) | 14 (46.7) | 0/0 (0.0) | 14 (46.7) | 1/14 (7.1) |
| Takayasu arteritis | 16 | 12 (75.0) | 4 (25.0) | 4 (25.0) | 0/0 (0.0) | 8 (50.0) | 1/9 (11.1) |
| Relapsing polychondritis | 56 | 39 (69.6) | 29 (51.8) | 29 (51.8) | 1/6 (16.7) | 41 (73.2) | 6/42 (14.3) |
| Other vasculitis | 100 | 67 (67.0) | 52 (52.0) | 47 (47.0) | 6/14 (42.9) | 49 (49.0) | 5/52 (9.6) |
| Medications b | |||||||
| Rituximab | 225 | 152 (67.6) | 95 (42.2) | 84 (37.3) | 43 (19.1) | 100 (44.4) | 21/208 (10.1) |
| Other biologics, JAKi, and/or CYC | 83 | 52 (62.7) | 36 (43.4) | 31 (37.3) | N/A | 52 (62.7) | 3/77 (3.9) |
| AZA, MMF, MTX, TAC, and/or CSP | 166 | 107 (64.5) | 81 (48.8) | 74 (44.6) | N/A | 76 (45.8) | 8/147 (5.4) |
| No DMARDs | 169 | 111 (65.7) | 84 (49.7) | 66 (39.1) | N/A | 68 (40.2) | N/A |
| Glucocorticoids | |||||||
| None | 364 | 238 (65.4) | 167 (45.9) | 137 (37.6) | 26/116 (22.4) | 141 (38.7) | 19/221 (8.6) |
| ≤10 mg/d | 238 | 160 (67.2) | 111 (46.6) | 96 (40.3) | 13/87 (14.9) | 122 (51.3)* | 11/183 (6.0) |
| >10 mg/d | 60 | 41 (68.3) | 30 (50.0) | 32 (53.3)* | 4/22 (18.2) | 43 (71.7)* | 5/46 (10.9) |
| Urban county | 524 | 353 (67.4) | 246 (46.9) | 219 (41.8) | 38/190 (20.0) | 230 (43.9) | 27/360 (7.5) |
| Rural county | 51 | 25 (49.0)* | 17 (33.3) | 13 (25.5)* | 4/17 (23.5) | 20 (39.2) | 3/36 (8.3) |
| Median household income of zip code | |||||||
| Lowest tertile | 66 | 35 (53.0) | 24 (36.4) | 25 (37.9) | 7/25 (28.0) | 26 (39.4) | 4/47 (8.5) |
| Middle tertile | 111 | 72 (64.9) | 54 (48.6) | 43 (38.7) | 5/36 (13.9) | 51 (45.9) | 2/76 (2.6) |
| Highest tertile | 401 | 274 (68.3)* | 187 (46.6) | 166 (41.4) | 30/148 (20.3) | 175 (43.6) | 24/275 (8.7) |
| Education of zip code (greater than high school) | |||||||
| Lowest tertile | 37 | 20 (54.1) | 15 (40.5) | 15 (40.5) | 3/13 (23.1) | 14 (37.8) | 2/26 (7.7) |
| Middle tertile | 117 | 72 (61.5) | 51 (43.6) | 47 (40.2) | 9/38 (23.7) | 53 (45.3) | 5/86 (5.8) |
| Highest tertile | 424 | 289 (68.2) | 199 (46.9) | 172 (40.6) | 30/158 (19.0) | 185 (43.6) | 23/286 (8.0) |
| County COVID‐19 cases per capita | |||||||
| Lowest tertile | 163 | 101 (62.0) | 61 (37.4) | 55 (33.7) | 9/57 (15.8) | 69 (42.3) | 6/116 (5.2) |
| Middle tertile | 230 | 160 (69.6) | 115 (50.0)* | 105 (45.7)* | 19/90 (21.1) | 93 (40.4) | 10/158 (6.3) |
| Highest tertile | 180 | 116 (64.4) | 87 (48.3)* | 72 (40.0) | 14/60 (23.3) | 88 (48.9) | 14/122 (11.5) |
| Concerned about COVID‐19 | |||||||
| Not at all, slightly, or somewhat concerned | 113 | 54 (47.8) | 46 (40.7) | 28 (24.8) | 6/35 (17.1) | 57 (50.4) | 2/74 (2.7) |
| Moderately or extremely concerned | 549 | 385 (70.1)* | 262 (47.7) | 237 (43.2)* | 37/190 (19.5) | 249 (45.4) | 33/376 (8.8) |
| United States | 597 | 392 (65.7) | 274 (45.9) | 241 (40.4) | 43/215 (20.0) | 264 (44.2) | 33/412 (8.0) |
| Canada | 65 | 47 (72.3) | 34 (52.3) | 24 (36.9) | 0/10 (0.0) | 42 (64.6)* | 2/38 (5.3) |
| Age <60 y | 370 | 258 (69.7) | 190 (51.4) | 159 (43.0) | 27/135 (20.0) | 193 (52.2) | 26/264 (9.8) |
| Age ≥60 y | 292 | 181 (62.0)* | 118 (40.4)* | 106 (36.3) | 16/90 (17.8) | 113 (38.7)* | 9/186 (4.8) |
Abbreviations: AAV, antineutrophil cytoplasmic antibody (ANCA)‐associated vasculitis; AZA, azathioprine; COVID‐19, coronavirus disease 2019; CSP, cyclosporine; CYC, cyclophosphamide; DMARD, disease‐modifying antirheumatic drug; EGPA, eosinophilic granulomatosis with polyangiitis; GPA, granulomatosis with polyangiitis; JAKi, Janus kinase inhibitor; MMF, mycophenolate; MPA, microscopic polyangiitis; MTX, methotrexate; N/A, not applicable; TAC, tacrolimus.
Proportion stopping medications among patients who were on immunosuppression/immunomodulatory therapy and did not report a respiratory illness or diagnosis of COVID‐19.
Nineteen patients on hydroxychloroquine, sulfasalazine, leflunomide, intravenous immunoglobulin, and apremilast were excluded.
P < 0.05 versus the reference groups (granulomatosis with polyangiitis; rituximab; no glucocorticoid use; urban residence; lowest tertile of median household income, greater than high school education, or COVID‐19 cases per capita; United States; and age <60) based on logistic regression models. All were univariate analyses except for the telehealth visit analyses, which were adjusted for date of entry into the study to account for associations between calendar time and telehealth use; P values are nominal in nature and should be interpreted in an exploratory manner.
In this cohort, 10.5% of patients on immunosuppressive therapy stopped their medication. Patients with respiratory illnesses were more likely to stop medication compared with patients without a recent respiratory illness (39.5% vs 7.8%; P < 0.01). The frequency of discontinuation of different immunosuppressive drugs in patients with and without respiratory illnesses is shown in Supplemental Table 4. The most common reason for stopping immunosuppressive medications in patients who were not sick was concern for infection (n = 20; 57.1%). In 60% of patients (n = 21), drug discontinuation was not physician approved (Supplemental Table 5).
Among the 225 patients on rituximab, 17 (7.5%) temporarily discontinued the drug and an additional 30 (13.3%) patients reported avoiding receiving an infusion of rituximab. The rates of discontinuation of rituximab among patients with and without respiratory illnesses are shown in Supplemental Table 4. The various reasons cited for drug discontinuation were similar among patients prescribed rituximab and patients prescribed other immunosuppressive medications (Supplemental Table 5).
Availability and use of telehealth
The majority of patients (n = 512; 77.3%) confirmed that telehealth was available to them, 19.9% (n = 132) were not sure of the availability, and 2.7% (n = 18) said that telehealth was not available to them. Overall, 46.2% (n = 306) of patients had a telehealth visit. Telehealth visits were more frequently reported by younger patients (age less than 60 years) (52.2% vs 38.7%; P = 0.01) and patients on glucocorticoids (55.4% vs 38.7%; P < 0.01). There was no difference in telehealth use among patients with different vasculitides after adjustment for time of entry into the study. Use of telehealth was higher in Canada compared to the United States (64.6% vs 44.2%; P < 0.01) (Table 2, Supplemental Table 3).
Patients who reported a telehealth visit were more likely to avoid doctors’ visits (76.1% vs 57.8%; P < 0.01) and laboratory tests (50.6% vs 43.0%; P = 0.05). Patients who reported that telehealth was available were also more likely to avoid doctors’ visits (68.4% vs 44.4%; P = 0.04). However, use or availability of telehealth did not impact interruption of immunosuppressive therapy or avoidance of infusions (Supplemental Table 6).
Information about COVID‐19
Most patients with vasculitis obtained COVID‐19–related information from news media (n = 586; 88.5%) and government websites (n = 421; 63.6%). Half of the patients (n = 333; 50.3%) reported getting information from a health care provider. Patients who had a telehealth visit were more likely to get information from health care providers than those who did not have a telehealth visit (64.7% vs 37.9%; P < 0.01) (Supplemental Table 7).
DISCUSSION
This report describes the impact of the COVID‐19 pandemic on patients with vasculitis in North America, specifically examining their levels of concern, health‐related behavior, and access to telehealth. Patients with vasculitis are particularly vulnerable during the pandemic because of their immunosuppressed status, need for regular medical care by a multispecialty team, and requirements for frequent testing to monitor medications and evaluate the status of these potentially organ‐ or life‐threatening diseases. Although few patients in this study were diagnosed with COVID‐19, patients frequently reported disruptions or changes in their health care, with potentially important implications for outcomes related to their vasculitis.
The great majority of patients in the cohort was highly concerned about the pandemic, with greater concerns among patients who were older, were female, or had underlying lung disease. These results are not surprising given the greater risks of severe COVID‐19 in patients who are older and in those with lung disease (3). Furthermore, patients frequently reported that their vasculitis had a large impact on their level of concern, especially among patients treated with immunosuppressive medication. These results are similar to those of studies of patients with different autoimmune diseases in which immunosuppressive therapy, female sex, age, and comorbidities were associated with patient concerns (7, 9). Notably, concerns were high across the United States and Canada, and there were no significant differences by country, region, urban versus rural location, or local COVID‐19 activity.
The pandemic had significant impact on health‐related behaviors, with patients frequently avoiding doctors’ visits or testing and frequently using telehealth. Changes in health‐related behaviors were more common in patients with higher concerns about COVID‐19, and several other factors were also associated with differences in behaviors. Patients who lived in urban areas or areas of higher COVID‐19 activity were more likely to avoid office visits or tests, perhaps because of the higher incidence of COVID‐19 activity in urban areas early in the pandemic or greater restrictions on in‐office visits or testing in these areas. Younger patients were more likely to avoid office visits and more likely to use telemedicine, which could reflect greater comfort with virtual interactions with the health care system among younger patients (10). Patients receiving glucocorticoids were more likely to avoid testing and more likely to have telehealth visits, although this may reflect the greater need for visits and testing in this population.
Associations between socioeconomic status and health‐related behavior were also evaluated. Higher median household income was associated with a significantly greater likelihood of avoiding office visits and a greater likelihood of using telehealth (although telehealth results were not statistically significant). Although also not statistically significant, higher education status was similarly associated with avoidance of office visits and use of telemedicine. Notably, patients of low socioeconomic status are underrepresented in this cohort. These results are concerning and emphasize the importance of ensuring that all patients are able to safely access care, regardless of socioeconomic status, throughout the pandemic.
In the current study, many patients were receiving rituximab, and more than 20% of such patients reported that they had discontinued rituximab or avoided getting an infusion because of concerns about COVID‐19. Concern for infection was stated as the major cause of discontinuation of infusions of rituximab (73%), and almost half of these patients stopped infusions of rituximab without their doctors’ advice. Similar observations were reported in a cohort of patients with large‐vessel vasculitis in which infusions were interrupted in approximately 24% of patients on infliximab (11). The risk of severe COVID‐19 infection in patients taking immunosuppressive drugs is uncertain, although case series from Europe and the United States have not demonstrated increased severity of COVID‐19 infections in patients on immunosuppressive medications (12). In addition, although prolonged B‐cell depletion by rituximab has been a major concern during the pandemic (13), the limited published data have not demonstrated an increased susceptibility to, or severity of, COVID‐19 in patients on rituximab (14). Importantly, stopping therapy with rituximab could also lead to disease flares and higher requirements of glucocorticoids, which could increase infection risk. Recently published guidelines from the American College of Rheumatology advised continued use of immunosuppressive medications in the absence of symptoms of COVID‐19 infection (15). The high concerns of patients around immunosuppression and the continued uncertainty of the effect of immunosuppression on risk of severe COVID‐19 necessitates close communication between patients and physicians.
Most patients in this cohort reported obtaining COVID‐19–related information from news media, although this source of information would not provide information specific to patients with vasculitis or patients receiving immunosuppressive therapy. Patients who had telehealth visits, however, were more likely to get information from health care providers. Maintaining regular medical care through telehealth may help address patient concerns, allow for discussion on the use of immunosuppressive therapy during the pandemic, and ensure that patients can continue to receive information updates, important testing, and necessary treatment for their vasculitis.
This study has several strengths to note. The sample size is large for a study of vasculitides, a set of rare diseases. The study population includes patients with many forms of vasculitis and patients from across the United States and Canada, including patients in both urban and rural areas. The survey questions were drafted by physicians and patients in collaboration and address issues of substantial interest to both groups.
There are also limitations of this study to consider. The number of patients with some types of vasculitis was low, limiting comparisons across the vasculitides. The diagnosis of vasculitis was based on patient report of a physician diagnosis, although this approach has been demonstrated in the VPPRN to be accurate (16). Responders to this survey likely represent a subgroup of patients who are more active with patient support groups, live in mostly urban areas, are White, and are female. The findings may not be fully generalizable to the overall population of patients with vasculitis in North America. There is also a possibility that some patients who were sick and hospitalized did not access the survey. The effects of health care–related behaviors on patients’ underlying vasculitis were not available from these baseline data. However, follow‐up surveys are being conducted to collect information on disease course and flares during the pandemic.
In conclusion, this study of patients with vasculitis reveals that although a small number of patients had COVID‐19 infection, the pandemic has profoundly affected patients living with vasculitis. Many patients were highly concerned about COVID‐19 infection, and the level of concern was affected substantially by their underlying vasculitis. Patients reported significant health‐related behavioral modifications with potentially adverse consequences. Differential health care–related behaviors and concern levels observed in patients based on their age, sex, comorbid conditions, urban versus rural location, and socioeconomic status indicate that specific strategies are needed to facilitate ongoing engagement with the health care system to ensure optimal management of disease for this vulnerable population during the pandemic.
ACKNOWLEDGMENTS
The authors aknowledge the contributions of the patients who participated in the research.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Banerjee had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Banerjee, George, Young, Venkatachalam, Gordon, Burroughs, D. Curtis, Gavigan, Kullman, Danila, J. R. Curtis, Shaw, Nowell, Merkel.
Acquisition of data
Banerjee, George, Young, Kullman, Merkel.
Analysis and interpretation of data
Banerjee, George, Young, Venkatachalam, Ferrada, Grayson, Nowell, Merkel.
Supporting information
Fig S1
Table S1‐S7
Supplementary Material
The Vasculitis Patient‐Powered Research Network was supported by a Patient‐Centered Outcomes Research Institute award (PPRN‐1306‐04758), by the Vasculitis Foundation, and by the Vasculitis Clinical Research Consortium. This work was supported by the Vasculitis Clinical Research Consortium, which is part of the Rare Diseases Clinical Research Network, an initiative of the Office of Rare Diseases Research within the National Center for Advancing Translational Sciences. The Vasculitis Clinical Research Consortium is funded through collaboration between the National Center for Advancing Translational Sciences and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U54‐AR‐057319).
Dr. George has received a research grant from Bristol Myers Squibb. Dr. Venkatachalam, Mr. Curtis, Ms. Gavigan, and Dr. Nowell are employees of the US‐based nonprofit organization Global Healthy Living Foundation. Global Healthy Living Foundation receives grants, sponsorships, and contracts from pharmaceutical manufacturers and private foundations. A full list of Global Healthy Living Foundation funders is publicly available at https://www.ghlf.org/our‐partners/. The Autoimmune COVID‐19 Project has received sponsorship support from the Patient‐Centered Outcomes Research Institute, Eli Lilly and Company, and Janssen Pharmaceutical. Dr. Danila reports receiving grants from Pfizer, Horizon, Boehringer Ingelheim, and Genentech and reports receiving consulting fees from Novartis and Amgen. Dr. Curtis reports receiving consulting fees from AbbVie, Amgen, Bristol Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB and research support from AbbVie, Amgen, Bristol Myers Squibb, Corrona, Janssen, Lilly, Myriad, Pfizer, Regeneron, Roche, and UCB. Dr. Merkel reports receiving funds for the following activities in the past 2 years: consulting: AbbVie, AstraZeneca, Biogen, Boeringher‐Ingelheim, Bristol Myers Squibb, Celgene, ChemoCentryx, CSL Behring, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, InflaRx, Insmed, Jannsen, Kiniksa, Magenta, Pfizer, Sparrow, and Talaris; research support: AstraZeneca, Boeringher‐Ingelheim, Bristol Myers Squibb, Celgene, ChemoCentryx, Forbius, Genentech/Roche, Genzyme/Sanofi, GlaxoSmithKline, and InflaRx; and royalties: UpToDate. No other disclosures relevant to this article were reported.
REFERENCES
- 1. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment of coronavirus. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–42. [DOI] [PubMed] [Google Scholar]
- 4. Durand M, Thomas SL. Incidence of infections in patients with giant cell arteritis: a cohort study. Arthritis Care Res (Hoboken) 2012;64:581–8. [DOI] [PubMed] [Google Scholar]
- 5. Mohammad AJ, Englund M, Turesson C, Tomasson G, Merkel PA. Rate of comorbidities in giant cell arteritis: a population‐based study. J Rheumatol 2017;44:84–90. [DOI] [PubMed] [Google Scholar]
- 6. Kermani TA, Schafer VS, Crowson CS, Hunder GG, Gabriel SE, Matteson EL, et al. Increase in age at onset of giant cell arteritis: a population‐based study. Ann Rheum Dis 2010;69:780–1. [DOI] [PubMed] [Google Scholar]
- 7. Michaud K, Wipfler K, Shaw Y, Simon TA, Cornish A, England BR, et al. Experiences of patients with rheumatic diseases in the United States during early days of the COVID‐19 pandemic. ACR Open Rheumatol 2020;2:335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. US Census Bureau . ACS 2018 (5‐year estimates). URL: http://www.socialexplorer.com/pub/reportdata/HtmlResults.aspx?reportid=R12543316
- 9. Siniscalchi M, Zingone F, Savarino EV, D'Odorico A, Ciacci C. COVID‐19 pandemic perception in adults with celiac disease: an impulse to implement the use of telemedicine. Dig Liver Dis 2020;52:1071–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chun YJ, Patterson PE. A usability gap between older adults and younger adults on interface design of an Internet‐based telemedicine system. Work 2012;41 Suppl 1:349–52. [DOI] [PubMed] [Google Scholar]
- 11. Tomelleri A, Sartorelli S, Campochiaro C, Baldissera EM, Dagna L. Impact of COVID‐19 pandemic on patients with large‐vessel vasculitis in Italy: a monocentric survey. Ann Rheum Dis 2020;79:1252–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Monti S, Balduzzi S, Delvino P, Bellis E, Quadrelli VS, Montecucco C. Clinical course of COVID‐19 in a series of patients with chronic arthritis treated with immunosuppressive targeted therapies. Ann Rheum Dis 2020;79:667–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shakshouk H, Daneshpazhooh M, Murrell DF, Lehman JS. Treatment considerations for patients with pemphigus during the COVID‐19 pandemic. J Am Acad Dermatol 2020;82:e235–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Montero‐Escribano P, Matias‐Guiu J, Gomez‐Iglesias P, Porta‐Etessam J, Pytel V, Matias‐Guiu JA. Anti‐CD20 and COVID‐19 in multiple sclerosis and related disorders: a case series of 60 patients from Madrid, Spain. Mult Scler Relat Disord 2020;42:102185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mikuls TR, Johnson SR, Fraenkel L, Arasaratnam RJ, Baden LR, Bermas BL, et al. American College of Rheumatology guidance for the management of rheumatic disease in adult patients during the COVID‐19 pandemic: version 1. Arthritis Rheumatol 2020;72:1241–51. [DOI] [PubMed] [Google Scholar]
- 16. Springer JM, Kermani TA, Sreih A, Shaw DG, Young K, Burroughs CM, et al. Clinical characteristics of an Internet‐based cohort of patient‐reported diagnosis of granulomatosis with polyangiitis or microscopic polyangiitis: Observational Study. J Med Internet Res 2020;22:e17231. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Table S1‐S7
Supplementary Material


