Abstract
Objective
Physical activity has numerous benefits for those with symptomatic knee osteoarthritis (KOA) or knee replacement, yet many individuals engage in insufficient activity. The purpose of this study was to explore beliefs about sedentary behavior, barriers to standing, and program preferences for adults with symptomatic KOA or knee replacement.
Methods
Forty‐two individuals ≥50 years with symptomatic KOA or knee replacement completed an online survey assessing current knee pain and function, sitting time, physical activity participation, beliefs about sedentary behavior, and preferences for a sedentary reduction program.
Results
Participants indicated barriers to standing were pain, discomfort, or working on a computer. Most participants shared interest to participate in a program to reduce sitting time. Participants chose education, self‐monitoring, and activity tracking as most preferable components for an intervention design.
Conclusion
Future interventions to reduce sedentary time may utilize these results to tailor programs for those with symptomatic KOA or knee replacement.
INTRODUCTION
The prevalence of knee osteoarthritis (KOA) has increased considerably over the past 20 years (1), with an estimated 14 million Americans currently living with symptomatic KOA (2). KOA is a leading cause of disability and can limit physical function and mobility as well as impair quality of life (3, 4). These limitations lead nearly half of patients with KOA to undergo total knee replacement during their lifetime (5).
Physical activity is strongly recommended as a nonpharmacologic treatment for KOA management, yet less than 20% of men and less than 10% of women with KOA meet federal physical activity guidelines (6). Even after knee replacement, the majority of patients typically do not increase their physical activity and remain either at or below presurgical activity levels (7). Individuals who have knee replacement surgery experience several barriers to activity, including pain, physical limitations, and lack of motivation, which may explain why activity levels remain unchanged after surgery (8).
In addition to low levels of physical activity, individuals with KOA spend two‐thirds of their waking day engaging in sedentary behavior, which is defined as sitting or reclined posture (3, 9). This is a proportion that remains unchanged or further increases after knee replacement (10). High levels of sedentary behavior, independent of physical activity levels, are associated with numerous health consequences, including increased risk of a negative cardiometabolic profile (11, 12) and all‐cause mortality (13). Specific to populations with knee symptoms, time spent in sedentary behavior is associated with an increased risk for disability (14), impaired physical function (3, 15), and poor quality of life (16).
Considering that individuals with knee osteoarthritis experience barriers to physical activity, reducing sedentary time may be a more feasible first‐step behavioral target for individuals with KOA and knee replacement. Several studies have started to explore ways to reduce sedentary time in older adults (17, 18, 19, 20). However, little research has focused specifically on sedentary time reduction in those with KOA or knee replacement.
To fill this gap in the literature, this study explored patients’ beliefs about sedentary behavior, their willingness to change their sedentary behavior, and their preferences for a sedentary reduction program among adults (≥50 years) with symptomatic KOA or those who had a knee replacement. Although it is believed that sedentary behavior is driven by both automatic and controlled processes (21, 22), the Theory of Planned Behavior (23, 24) may be helpful to better understand sedentary behavior (24). Therefore, this study explored behavioral beliefs and perceived behavioral control for reducing sedentary behavior and replacing sedentary time with different activities of varying duration. In addition, the study assessed this population’s preferences for technology‐supported sedentary reduction interventions given the substantial increase in the use of technology among older adults (25) and success of technology for modifying behaviors (26, 27, 28, 29, 30). The knowledge gained from this study can help to inform the development of future sedentary reduction interventions and patient‐centered clinician recommendations for those with symptomatic knee osteoarthritis or knee replacement.
PATIENTS AND METHODS
Participants and procedures
Adults older than 50 years in the southeastern United States with symptomatic KOA (at least one knee with pain, aching, or stiffness on most days of 1 month of the last 12 months) or who had undergone a knee replacement were recruited to participate in this study. Participants were recruited via email or online postings, social media flyers, or recommendations from medical staff, physicians, and nurses from local orthopedic and rehabilitation facilities. Interested candidates were directed to an online screening questionnaire to determine eligibility. If eligible, participants were automatically directed to complete the battery of online surveys, which took approximately 25 minutes to complete. On survey completion, participants were given the opportunity to enter a drawing for one of four $25 Amazon gift cards. All study procedures were approved by the University of South Carolina's Institutional Review Board.
Measures
Demographics, health history, and technology ownership
Participants were asked to report age, sex, race, ethnicity, level of education, and employment status. Height and weight were self‐reported to calculate body mass index (BMI). A brief medical and surgical history was also included to identify known medical diagnoses (eg, heart disease, cancer, hypertension, and depression/anxiety) and major surgeries (eg, knee replacement and hip replacement). Technology ownership and usage of several forms of technology (eg, smartphone, computer, and tablet) were also assessed.
Patient‐Reported Outcomes Measurement Information System
The Patient‐Reported Outcomes Measurement Information System (PROMIS) (31) was used to assess pain intensity, pain interference, and physical function and mobility. The PROMIS uses computer adaptive tests and was administered via a RedCap shared library (32). Each measure results in a T score, with a mean score of 50 (SD = 10) representing the mean of the general US population. Higher scores indicate more intense pain, increased pain interference, or higher levels of mobility.
Godin Leisure Time Exercise Questionnaire
The Godin Leisure Time Exercise Questionnaire (33) was modified for this study and was used to assess physical activity. Participants indicated the frequency and average amount of time spent engaging in strenuous (eg, jogging), moderate (eg, fast walking), and mild (eg, easy walking) exercise for at least 15 minutes over the past 7 days. The weekly total volume of time spent in strenuous and moderate exercise was calculated by multiplying the weekly frequency by duration for strenuous and moderate activities. The daily average was calculated by dividing the volume of strenuous and moderate exercise by 7.
The Sitting‐Time Questionnaire
The Sitting‐Time Questionnaire (34), which is a valid measure with high test‐retest reliability (35), was used to assess sedentary time. Participants indicated the amount of time they spend sitting on a typical weekday and weekend in various situations (eg, traveling to and from places, while at work, and during leisure time not including television watching). The average total weekly time spent sitting was calculated by multiplying the total time spent sitting on weekdays by 5 and the total time spent sitting on weekends by 2 and then summing these values. The average daily volume was obtained by dividing this sum by 7.
Beliefs about sedentary behavior
Participants’ beliefs about sedentary behavior were assessed using a questionnaire adapted from Lloyd et al (36). The adaptations made for this study included adding items related to replacing sitting time with different activities (eg, standing, light walking, and brisk walking) and excluded time lying down. Specifically, the close‐ended questionnaire assessed behavioral beliefs about the potential benefits and harms of sedentary time using a Likert scale of 1 (“not at all harmful”) to 5 (“very harmful”) and beliefs about whether reducing extended periods of sedentary behavior could improve their health (yes, no, or do not know). Additionally, the questionnaire assessed participants’ beliefs on the maximum amount of time they should spend sitting before standing up using a scale ranging from less than 30 minutes to more than 3 hours, as well as their attitude toward the amount of time they spend sedentary during work and leisure time (“I wish I could sit more,” “I wish I could sit less,” or “I do not wish to change”). Participants identified barriers (control beliefs) as to why they do not stand up more frequently (ie, “everyone else around me is sitting”, “I feel pain or discomfort from standing or easy walking,” “I am too busy at work to stand,” or “other”) and indicated their perceived behavioral control over replacing sedentary time with varying durations (eg, 2 minutes, 5 minutes, or 10 minutes) of specific activities such as standing, calisthenics, walking in place, and walking around (scale of 1 [“very unlikely”] to 5 [“very likely”]).
Interest and preferences for technology‐supported sedentary behavior reduction intervention
Participants’ interest in and preferences for technology‐supported sedentary behavior reduction intervention were obtained from a previously used questionnaire (36). Participants chose favorable potential intervention features, such as use of behavioral strategies (eg, goal setting, self‐monitoring, and tracking activity), reminders to interrupt sedentary time, use of activity trackers, and preferred activities and timing to replace sitting.
Data analysis
Descriptive statistics were calculated for demographic characteristics, health conditions, technology ownership and usage, beliefs about sedentary behavior, and sedentary behavior program preferences. χ2 or independent‐sample T tests were conducted to examine differences in demographic characteristics, physical activity, sitting behavior, and PROMIS measures between individuals with KOA and knee replacement; however, because of the small sample size, all participants were combined to explore their beliefs and preferences for reducing sedentary behavior. Missing data ranged from 0% for the majority of variables to 4.7% for indication of owning a smartphone. Data were determined to be missing at random as a result of preliminary analyses. Therefore, mean imputation was used for managing missing values. All data analysis was conducted using SPSS version 25 (37).
RESULTS
Participants
A total of 42 participants (mean = 61.8 years; SD = 7.6 years) completed the study. Participant characteristics (by knee condition) are outlined in Table 1. The majority of participants were white (93%), had graduated college or achieved higher education (74%), and had an average BMI of 31.4 kg/m2 (SD = 7.2 kg/m2). The 13 (31%) participants who had a knee replacement were significantly older (mean = 66.8 years; SD = 7.7 years) than those with KOA (mean = 59.5 years; SD = 6.5 years; P < 0.05). PROMIS measures indicated an average mobility score of 42.6 (SD = 2.3), pain intensity score of 55.1 (SD = 2.1), and pain interference score of 45.2 (SD = 2.8) among survey participants. Most of the sample owned a computer (98%) and mobile phone (93%). Of those owning a mobile phone, 87% had a smartphone. Over one‐quarter (26%) of participants also used an activity monitor (eg, Fitbit, Garmin, or Smartwatch).
Table 1.
Participant characteristics
| Overall (n = 42) | KOA (n = 29) | Knee Replacement (n = 13) | |
|---|---|---|---|
| Age, M ± SD, yr | 61.8 ± 7.6 | 59.5 ± 6.5 | 66.8 ± 7.7 |
| BMI, M ± SD, kg/m2 | 31.4 ± 7.2 | 31.0 ± 7.1 | 32.4 ± 7.5 |
| Female, n (%) | 28 (67) | 16 (55) | 12 (92) |
| Race, n (%) | |||
| White | 42 (93) | 27 (93) | 12 (92) |
| Black | 3 (7) | 2 (7) | 1 (8) |
| Education, n (%) | |||
| <College degree | 11 (26) | 8 (28) | 3 (23) |
| ≥College degree | 31 (74) | 21 (72) | 10 (77) |
| Employment Status, n (%) | |||
| Working ≥part‐time | 24 (57) | 19 (66) | 5 (38) |
| Retired | 14 (33) | 7 (24) | 7 (54) |
| Not working | 4 (10) | 3 (10) | 1 (8) |
| Technology ownership, n (%) | |||
| Computer | 41 (98) | 28 (97) | 13 (100) |
| Mobile phone | 39 (93) | 27 (93) | 12 (92) |
| Smartphone | 34 (87) | 24 (83) | 10 (77) |
| Tablet | 19 (45) | 13 (45) | 6 (46) |
| Physical activity monitor | 11 (26) | 4 (14) | 7 (54) |
| Health conditions, n (%) | |||
| Rheumatoid arthritis | 4 (10) | 2 (7) | 2 (15) |
| Hypertension | 17 (41) | 12 (41) | 5 (39) |
| Heart Disease | 3 (7) | 3 (10) | ‐ |
| Diabetes | 4 (10) | 4 (13) | ‐ |
| Depression | 7 (17) | 3 (10) | 4 (31) |
| Anxiety | 5 (12) | 3 (10) | 2 (15) |
| PROMIS Measures, M ± SD | |||
| Mobility | 42.6 ± 2.3 | 42.4 ± 2.3 | 43.1 ± 2.3 |
| Pain intensity | 55.1 ± 2.1 | 56.3 ± 1.8 | 52.6 ± 2.6 |
| Pain interference | 45.2 ± 2.8 | 46.0 ± 2.8 | 43.3 ± 2.9 |
BMI, body mass index; KOA, knee osteoarthritis; M, mean; PROMIS, Patient‐Reported Outcomes Measurement Information System.
Participant characteristics
Sedentary behavior and physical activity participation
Participants self‐reported spending an average of 129.7 minutes/week (SD = 148.8 minutes/week) engaged in strenuous or moderate exercise and 10.9 hours/day (SD = 5.3 hours/day) engaged in sedentary behavior, with no differences between individuals with KOA or knee replacement. One‐third of participants reported engaging in no strenuous or moderate exercise throughout the week, and only 29% of participants were at or above physical activity guidelines of at least 150 minutes/week of moderate to vigorous physical activity (38).
Beliefs about sedentary behavior and barriers to reducing sedentary time
Overall, most participants (86%) reported they believed sitting for an extended period of time is harmful for one’s health, with 83% of participants believing that reducing sitting time can improve general health. A higher percentage of participants believed sitting time should be replaced with light (88%) or brisk walking (86%) than those who believed it should be replaced with standing (62%).The majority of participants felt that the optimal amount time they should sit before getting up to stand or move around ranged from 30 minutes to one hour (57%) or from 1 to 2 hours (31%).
Fifty‐five percent of participants wished that they could sit less in their leisure time. Among those who are currently employed, 75% wished they could sit less at work. Participants also rated the likelihood of replacing sitting with standing, walking in place, or walking around both during work hours and during leisure time (Figure 1). Overall, at work and in leisure time, more participants indicated they would be more likely to replace sitting with brief 2‐minute activities (eg, standing, stretching, and walking) compared with activities of a longer duration (eg, 5 or 10 minutes).
Figure 1.
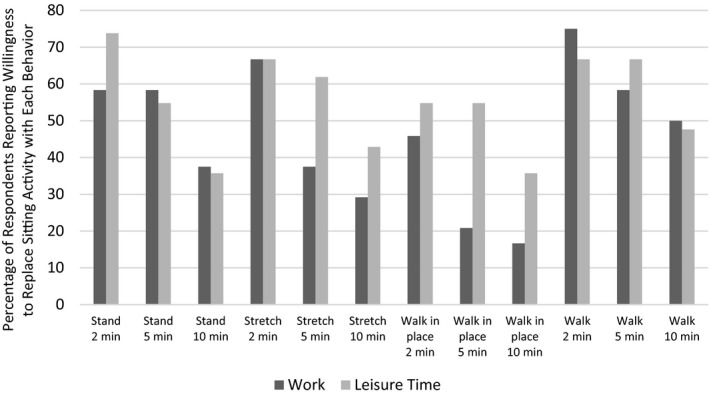
Likelihood of replacing sitting with varying durations of activities during work or leisure time.
Participants also identified their barriers to reducing sedentary time. The most common barriers were having pain or discomfort when standing (52%) and being unable to stand while working on the computer (48%). There were no differences in barriers between those with KOA or knee replacement.
Sedentary behavior program preferences
Most participants (67%) indicated they were interested in participating in a sedentary behavior reduction program. Furthermore, participants indicated the type of intervention components that they perceived would be the most helpful (Figure 2). The intervention components reported the most frequently were tracking/self‐monitoring sitting time (71%), setting a goal daily (69%), and receiving education related to sedentary behavior (67%). The intervention components that were perceived to be the least helpful to reduce sedentary time were communicating (24%) or competing (19%) with others in a sedentary reduction program.
Figure 2.
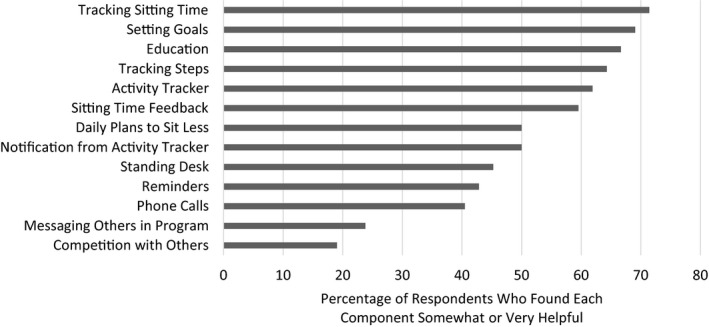
Helpfulness of sedentary reduction program features.
Nearly half of participants (45%) indicated that they would be willing to receive reminders to help them sit less. There was a trend for those who currently use a physical activity monitor to be more willing to receive reminders than those who do not (P = 0.06). Of those who would be willing to receive reminders, 47% of participants would want to receive between one and three reminders per day, and 37% would want to receive four to six reminders per day. Preferable methods of reminder delivery included via text message (74%), vibration on wrist‐worn physical activity tracker (50%), and pop‐up message on computer screen (32%). Approximately 80% of participants indicated that they preferred reminders to occur when sitting for 30 minutes to 1 hour.
DISCUSSION
This study explored the beliefs about sedentary behavior and preferences for sedentary reduction programs among adults with symptomatic KOA or knee replacement. The majority of participants (86%) believe that sitting for an extended period of time is harmful for one’s health, but intentions to change sitting behaviors was lower for both work and leisure time sedentary time (75% and 55%, respectively). Regardless of domain, participants indicated a greater willingness to replace sitting time with activities of a shorter duration (2 minutes) compared with activities that were 5 or 10 minutes in length. These exploratory results provide initial insight on beliefs and intention for reducing sedentary time that could be helpful to inform future sedentary reduction programs for this population.
From a Theory of Planned Behavior perspective, this sample appears to have strong behavioral beliefs regarding the consequences of prolonged sedentary behavior; however, their perceived behavioral control over replacing sedentary time appears to decline with activities of longer durations and may depend on whether the sedentary behavior is at work or in their leisure time. As a result, intention or willingness to change or participate in a sedentary reduction program is lower than anticipated. Intention to exercise has been found to be strongly associated with attitude, which is a result of behavioral beliefs and outcome evaluations (39), but interestingly, for sedentary behavior, subjective norms may be more predictive (24). The current study did not examine subjective norms, which may be playing a larger role in intentions to reduce sedentary time than other Theory of Behavior constructs. Future studies should be sure to explore the role of subjective norms in the prediction of intention to reduce sedentary time.
Another possible explanation for the lack of willingness to reduce sedentary time may be the higher average BMI of this sample. Excessive sedentary time may have negative effects on health indicators such as BMI (40, 41). A significant association has been found between obesity and sedentary behavior, with research indicating that obesity is a determinant of sedentary behavior as opposed to a result (42). It is important to note that the average BMI of participants in the present study falls into the obese category (>30 kg/m2), thus placing them at higher risk of the negative health consequences associated with sedentary behavior. Future research should continue to explore barriers to reducing sedentary time (eg, BMI, pain, and work) in populations with KOA and knee replacement to better inform possible intervention strategies.
The majority of participants believed that sitting for extended times can be harmful to one’s health, which suggests that the consequences of excess sitting identified over the recent years are effectively being communicated to this patient population. Many participants were also interested in receiving educational information regarding ways to sit less throughout the day. However, there has been little attention given to interventions to reduce sedentary behavior from a public health perspective (43). Although many health risks have been identified linking higher sedentary time with type II diabetes, cancer all‐cause mortality, and cardiovascular disease (44), little is known about the optimal sedentary behavior reduction level to improve health outcomes. Although an optimal level of sedentary behavior reduction to decrease disease risk is unknown, this study suggests that disseminating knowledge regarding ways to reduce sitting time could be a logical first step for decreasing sedentary behavior and health risks; however, future research is also needed to identify strategies to increase intention to reduce sedentary time in those with KOA or knee replacement.
Although US federal guidelines suggest that adults should engage in at least 150 minutes/week of moderate‐ to vigorous‐intensity physical activity, specific recommendations for sedentary behavior have yet to be determined (38). Current recommendations suggest that adults should move more and sit less but fail to acknowledge frequency of breaks and types of nonsedentary activity beneficial for improving health outcomes. The results of the current study echo those of previous studies, showing that individuals with KOA or knee replacement are highly sedentary (3, 9, 45, 46) despite behavioral beliefs that prolonged sedentary behavior may be harmful and that replacing sedentary time with other activities (eg, standing and light walking) could help to improve health. Interestingly, there were no differences in barriers to reducing sedentary time between those with KOA and knee replacement despite the clinical and symptom differences that likely exist between these populations (47, 48). Participants in the current study mentioned pain and the inability to stand while using a computer at work as top barriers to reducing sedentary time. Future interventions should consider including strategies and recommendations that may be feasible for this population and address common barriers, such as the use of an adjustable height desk or taking frequent short sedentary breaks to minimize pain.
More participants in the present study indicated a desire to reduce sitting time at work compared with those wanting to change leisure time sitting. This may indicate that during leisure time, sedentary behavior may be more intentional, whereas during working hours, sedentary behavior may be less intentional but may seem nonvolitional (24). Regardless of the type of sedentary time, participants indicated a willingness to be more likely to replace sitting time with short (2 minutes) amounts of standing, stretching, or walking around after a period of sedentary time lasting between 30 and 60 minutes compared with activities of a longer duration (5‐10 minutes). Interrupting sedentary time with brief bouts of light‐intensity activity has proven to be beneficial for functional and cardiometabolic improvements in experimental settings (49). Although this may be an acceptable intervention approach, it is unclear whether these brief interruptions of sedentary behavior would have any effect on knee symptoms or other potentially relevant health outcomes for this population.
The two most common barriers to standing more frequently reported by participants were pain and discomfort and the inability to stand while working on a computer. This is consistent with barriers to physical activity among those with KOA, such as pain and lack of motivation (50). However, as a whole, barriers to standing have not been widely assessed. Future studies are needed to evaluate whether recommending brief breaks in sedentary time are a feasible strategy for those using the computer and whether these shorter interruptions could help to reduce pain and discomfort in those with current or past knee symptoms.
The majority of participants (66.7%) indicated an interest in participating in a program to help reduce sitting time. In efforts to gain patient‐centered insight regarding programmatic design, participants were also asked to indicate which particular program components they perceived would be most helpful to reducing sitting time. Of the intervention strategies listed, nearly half (42.2%) indicated that they would be willing to receive prompts to sit less throughout the day, with text messages as the most preferable method for delivery. Given that sedentary behavior is more habitual in nature and is frequently done without intention (22), prompting can be an effective method to make individuals aware of their sedentary time. Additionally, considering the high penetration of smartphones across all age groups and demographics (25), with over 50% of every demographic group, including older adults, owning a smartphone in 2019 (25), these results provide insight into favorable intervention components that may be useful for the design and implementation of a sedentary behavior reduction program. Many participants also mentioned that they would be willing to receive a notification to sit less on a wearable physical activity tracker; however, current evidence suggests that these devices may not be effective in reducing sedentary behavior (29, 30). More research is needed to examine the effect of prompting on changes in sedentary time as well as to determine the optimal method to deliver these prompts.
This study was not without limitations. The small survey sample limits the statistical power and generalizability of these results. These preferences may not reflect those from other geographic areas, certain racial or ethnic groups, or those who are not as familiar with or comfortable using technology. Additionally, the survey used to assess beliefs about sedentary behavior has not been not tested in this population or compared with other standard Theory of Planned Behavior questionnaires, so results should be interpreted with caution. Future studies should include a larger, nationwide sample to gauge preferences from a more diverse range of individuals as well as to compare any potential differences in preferences and beliefs toward reducing sedentary behavior between those with KOA and those with knee replacement. A qualitative examination of beliefs and preferences would further the understanding of reducing sedentary time in this population as well. Objective measures of physical activity and sedentary behavior should also be used in the future to reduce self‐report bias. Additionally, interventions are needed to test the efficacy of these preferred components for sedentary behavior reduction programs in this population. This study also presented some valuable strengths as well. To our knowledge, this is the first study to examine program preferences for reducing sedentary behavior among those with KOA or those who have had a knee replacement. Furthermore, by soliciting input from those with knee issues, a patient‐centered perspective may increase the applicability and effectiveness of future interventions implemented among individuals from this population.
In conclusion, this study was the first to explore beliefs about sedentary behavior and preferences for sedentary behavior reduction program components among individuals with KOA or those who have had a knee replacement. Respondents self‐reported spending more than 10 hours/day sitting even though 83% of individuals believed that reducing sedentary time is beneficial for general health. Participants want to sit less at work and in leisure time; however, common barriers to standing included pain and inability to use a computer while standing. The majority of participants expressed interest in participating in a program to reduce the amount of time they spend sitting. Sitting behavior reduction strategies at work or during leisure time were most preferable in shorter durations (approximately 2 minutes). Finally, participants perceived tracking sitting time, goal setting, and education about sedentary behavior reduction as the most helpful strategies for reducing sedentary time. Findings from this study may be used to develop and implement future sedentary behavior reduction program among those with KOA and knee replacement.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual contact, and all authors approved the final version to be published. Drs. Powell and Pellegrini had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Powell, Larsen, Phillips, Pellegrini.
Acquisition of data
Powell, Pellegrini, Powell.
Analysis and interpretation of data
Powell, Larsen, Phillips, Pellegrini.
Supported by internal funding from the University of South Carolina Department of Exercise Science.
SMP serves as consultant on National Institutes of Health R01CA239612 and received an honorarium for speaking at the National Institutes of Health and other universities. CP serves as consultant on a Department of Defense Spinal Cord Injury Research Program Qualitative Research Award (SC160051). No other disclosures relevant to this article were reported.
REFERENCES
- 1. Nguyen U‐S, Zhang Y, Zhu Y, Niu J, Zhang B, Felson DT. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med 2011;155:725–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP, et al. Number of persons with symptomatic knee osteoarthritis in the US: impact of race and ethnicity, age, sex, and obesity. Arthritis Care Res 2016;68:1743–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee J, Chang RW, Ehrlich‐Jones L, Kwoh CK, Nevitt M, Semanik PA, et al. Sedentary behavior and physical function: objective evidence from the Osteoarthritis Initiative. Arthritis Care Res 2015;67:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zeni JA, Axe MJ, Snyder‐Mackler L. Clinical predictors of elective total joint replacement in persons with end‐stage knee osteoarthritis. BMC Musculoskelet Disord 2010;11:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, et al. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am 2013;95:385–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dunlop DD, Song J, Semanik PA, Chang RW, Sharma L, Bathon JM, et al. Objective physical activity measurement in the osteoarthritis initiative: are guidelines being met? [Original Article]. Arthritis Rheum 2011;63:3372–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paxton RJ, Melanson EL, Stevens‐Lapsley JE, Christiansen CL. Physical activity after total knee arthroplasty: a critical review. World J Orthop 2015;6:614–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pellegrini CA, Ledford G, Chang RW, Cameron KA. Understanding barriers and facilitators to healthy eating and physical activity from patients either before and after knee arthroplasty. Disabil Rehabil 2018;40:2004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Semanik PA, Lee J, Song J, Chang RW, Sohn M‐W, Ehrlich‐Jones LS, et al. Accelerometer‐monitored sedentary behavior and observed physical function loss. Am J Public Health 2015;105:560–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Harding P, Holland AE, Delany C, Hinman RS. Do activity levels increase after total hip and knee arthroplasty? [Original Article]. Clin Orthop Relat Res 2014;472:1502–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brocklebank LA, Falconer CL, Page AS, Perry R, Cooper AR. Accelerometer‐measured sedentary time and cardiometabolic biomarkers: a systematic review. Prev Med 2015;76:92–102. [DOI] [PubMed] [Google Scholar]
- 12. Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio‐metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J 2011;32:590–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009;41:998–1005. [DOI] [PubMed] [Google Scholar]
- 14. Dunlop DD, Song J, Arntson EK, Semanik PA, Lee J, Chang RW, et al. Sedentary time in US Older adults associated with disability in activities of daily living independent of physical activity. J Phys Act Health 2015;12:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Santos DA, Silva AM, Baptista F, Santos R, Vale S, Mota J, et al. Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp Gerontol 2012;47:908–12. [DOI] [PubMed] [Google Scholar]
- 16. Pinto D, Song J, Lee J, Chang RW, Semanik PA, Ehrlich‐Jones LS, et al. Association between sedentary time and quality of life from the osteoarthritis initiative: who might benefit most from treatment? [Original Article]. Arch Phys Med Rehabil 2017;98:2485–90. [DOI] [PubMed] [Google Scholar]
- 17. Barone Gibbs B, Brach JS, Byard T, Creasy S, Davis KK, McCoy S, et al. Reducing sedentary behavior versus increasing moderate‐to‐vigorous intensity physical activity in older adults: a 12‐week randomized, clinical trial. J Aging Health 2017;29:247–67. [DOI] [PubMed] [Google Scholar]
- 18. Gardiner PA, Eakin EG, Healy GN, Owen N. Feasibility of reducing older adults’ sedentary time. Am J Prev Med 2011;41:174–7. [DOI] [PubMed] [Google Scholar]
- 19. Matson TE, Renz AD, Takemoto ML, McClure JB, Rosenberg DE. Acceptability of a sitting reduction intervention for older adults with obesity. BMC Public Health 2018;18:706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J. Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. J Gerontol A Biol Sci Med Sci 2016;71:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Groves PM, Thompson RF. Habituation: a dual‐process theory. Psychol Rev 1970;77:419–50. [DOI] [PubMed] [Google Scholar]
- 22. Conroy DE, Maher JP, Elavsky S, Hyde AL, Doerksen SE. Sedentary behavior as a daily process regulated by habits and intentions. Health Psychol 2013;32:1149–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ajzen I. The Theory of Planned Behavior. Organ Behav Hum Decis Process 1991;50:179–211. [Google Scholar]
- 24. Prapavessis H, Gaston A, DeJesus S. The Theory of Planned Behavior as a model for understanding sedentary behavior. Psychology of Sport and Exercise 2015;19:23–32. [Google Scholar]
- 25. PEW Research Center . Mobile Fact Sheet. PEW Research Center; 2019. URL: https://www.pewresearch.org/internet/fact‐sheet/mobile/ [Google Scholar]
- 26. Alkhaldi G, Modrow K, Hamilton F, Pal K, Ross J, Murray E. Promoting engagement with a digital health intervention (HeLP‐Diabetes) using email and text message prompts: mixed‐methods study. Interact J Med Res 2017;6:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res 2009;11:e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Spring B, Pfammatter AF, Marchese SM, Stump T, Pellegrini CA, McFadden HG, et al. A factorial experiment to optimize remotely delivered behavioral treatment for obesity: results of the Opt‐IN study. Obesity 2020;28:1652–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brickwood K‐J, Watson G, O’Brien J, Williams AD. Consumer‐based wearable activity trackers increase physical activity participation: systematic review and meta‐analysis. JMIR MHealth Uhealth. 2019;7:e11819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ringeval M, Wagner G, Denford J, Paré G, Kitsiou S. Fitbit‐based interventions for healthy lifestyle outcomes: systematic review and meta‐analysis. J Med Internet Res 2020;22:e23954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient‐Reported Outcomes Measurement Information System (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care 2007;45 Suppl 1:S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Obeid JS, McGraw CA, Minor BL, Conde JG, Pawluk R, Lin M, et al. Procurement of shared data instruments for Research Electronic Data Capture (REDCap). J Biomed Inform 2013;46:259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985;10:141–6. [PubMed] [Google Scholar]
- 34. Marshall AL, Miller YD, Burton NW, Brown WJ. Measuring total and domain‐specific sitting: a study of reliability and validity. Med Sci Sports Exerc 2010;42:1094–102. [DOI] [PubMed] [Google Scholar]
- 35. Wijndaele K, Bourdeaudhuij ID, Godino JG, Lynch BM, Griffin SJ, Westgate K, et al. Reliability and validity of a domain‐specific last 7‐d sedentary time questionnaire. Med Sci Sports Exerc 2014;46:1248–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lloyd GR, Oza S, Kozey‐Keadle S, Pelegrini CA, Conroy DE, Penedo FJ, et al. Breast cancer survivors’ beliefs and preferences regarding technology‐supported sedentary behavior reduction interventions. AIMS Public Health 2016;3:592–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Statistical package for the social sciences: version 25.0. Chicago: SPSS; 2017. [Google Scholar]
- 38. 2018 Physical Activity Guidelines Advisory Committee . 2018 Physical Activity Guidelines Advisory Committee Scientific Report. US Department of Health and Human Services; 2018. URL: https://health.gov/sites/default/files/2019‐09/PAG_Advisory_Committee_Report.pdf. [Google Scholar]
- 39. Downs DS, Hausenblas HA. Elicitation studies and the theory of planned behavior: a systematic review of exercise beliefs. Psychology of Sport and Exercise 2005;6:1–31. [Google Scholar]
- 40. Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids 2003;38:103–8. [DOI] [PubMed] [Google Scholar]
- 41. Stamatakis E, Hamer M, Tilling K, Lawlor DA. Sedentary time in relation to cardio‐metabolic risk factors: differential associations for self‐report vs accelerometry in working age adults. Int J Epidemiol 2012;41:1328–37. [DOI] [PubMed] [Google Scholar]
- 42. Pedisic Z, Grunseit A, Ding D, Chau JY, Banks E, Stamatakis E, et al. High sitting time or obesity: Which came first? Bidirectional association in a longitudinal study of 31,787 Australian adults. Obesity 2014;22:2126–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Vallance JK, Gardiner PA, Lynch BM, D'Silva A, Boyle T, Taylor LM, et al. Evaluating the evidence on sitting, smoking, and health: is sitting really the new smoking? [Review]. Am J Public Health 2018;108:1478–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta‐analysis. Ann Intern Med 2015;162:123–32. [DOI] [PubMed] [Google Scholar]
- 45. Frimpong E, McVeigh JA, Meiring RM. Sedentary behavior in patients with knee osteoarthritis before and after total knee arthroplasty: a systematic review. J Aging Phys Act 2018;26:671–81. [DOI] [PubMed] [Google Scholar]
- 46. Webber SC, Strachan SM, Pachu NS. Sedentary behavior, cadence, and physical activity outcomes after knee arthroplasty. Med Sci Sports Exerc 2017;49:1057–65. [DOI] [PubMed] [Google Scholar]
- 47. Bachmeier CJM, March LM, Cross MJ, Lapsley HM, Tribe KL, Courtenay BG, et al. A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage 2001;9:137–46. [DOI] [PubMed] [Google Scholar]
- 48. Hammett T, Simonian A, Austin M, Butler R, Allen KD, Ledbetter L, et al. Changes in physical activity after total hip or knee arthroplasty: a systematic review and meta‐analysis of six‐ and twelve‐month outcomes. Arthritis Care Res 2018;70:892–901. [DOI] [PubMed] [Google Scholar]
- 49. White DK, Lee J, Song J, Chang RW, Dunlop D. Potential functional benefit from light intensity physical activity in knee osteoarthritis. Am J Prev Med 2017;53:689–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gay C, Eschalier B, Levyckyj C, Bonnin A, Coudeyre E. Motivators for and barriers to physical activity in people with knee osteoarthritis: a qualitative study. Joint Bone Spine 2018;85:481–6. [DOI] [PubMed] [Google Scholar]


