Abstract
Malignant biliary obstruction (MBO) encompasses a variety of malignancies arising from the pancreaticobiliary system. This can be divided into malignant hilar biliary obstruction (MHBO) or malignant distal biliary obstruction (MDBO) biliary obstruction to which clinical outcomes and technical considerations of various biliary drainage methods may differ. EUS biliary drainage (EUS-BD) has been increasingly influential in the management of MBO together with other familiar biliary drainage methods such as ERCP and percutaneous transhepatic biliary drainage (PTBD). Conventionally, ERCP has always been the primary choice of endoscopic biliary drainage in both MHBO and MDBO and that PTBD or EUS-BD is used as a salvage method when ERCP fails for which current guidelines recommends PTBD, especially for MHBO. This review was able to show that with today's evidence, EUS-BD is equally efficacious and possesses a better safety profile in the management of MBO and should be on the forefront of endoscopic biliary drainage. Therefore, EUS-BD could be used either as a primary or preferred salvage biliary drainage method in these cases.
Keywords: malignant hilar biliary obstruction, malignant distal biliary obstruction, hilar cholangiocarcinoma, Klatskin's tumor, perihilar cholangiocarcinoma, endosonography, EUS, ERCP, EUS-guided biliary drainage
INTRODUCTION
Malignant biliary obstruction (MBO) encompasses a variety of malignancies arising from the pancreaticobiliary system. Common causes of MBO include pancreatic ductal adenocarcinoma, cholangiocarcinoma, ampullary/duodenal adenocarcinoma, gallbladder adenocarcinoma, lymphoma, and compressive metastatic proximal lymph nodes.[1] Of which in clinical practice, pancreatic ductal adenocarcinoma and cholangiocarcinoma are the most common.[2]
The incidence of pancreatic cancer was the highest in Europe (7.7/100,000 people) and North America (7.6/100,000 people). This represents 2.5% of all cancers and 80% to 90% were deem unresectable at the time of diagnosis.[3] The demographics of pancreatic cancer was also found to be similar in the Asian population as well.[4] On the other hand, the incidence of cholangiocarcinoma are reported to be highest in the Hispanic and Asian populations (2.8–3.3/100,000). Among all the cases, proximal disease occurs in about 50%, while distal disease occurs in 40% and intrahepatic disease <10%.[5] In Asia, intrahepatic cholangiocarcinomas accounts the highest in countries such as South Korea and Thailand while extrahepatic cholangiocarciomas occurs highest in Japan.[6] It is to no surprise that up to 61.4% of the cases are advanced at the time of diagnosis.[7] As a result, palliative endoscopic biliary decompression has been essential in the management of these cases.[2,8,9] Current established methods of endoscopic biliary drainage are ERCP, percutaneous transhepatic biliary drainage (PTBD) and EUS biliary drainage (EUS-BD), in which ERCP and PTBD are often the preferred choices as both methods have been established for several decades.
EUS-BD is the latest endoscopic technique comparing with the aforementioned other two. Consequently, clinical information is much less than others. Nevertheless, it has become more and more interesting as it provides an added advantage of internal biliary drainage, and its complication rates are lower when time goes by together with increasing experience by endoscopists. In some centers, it has been proposed as the primary biliary drainage modality. Therefore, in this review, we will take a look at present evidence available based on current literatures in regard to various methods of EUS-BD, their efficacy and safety as well as in comparison with conventional methods of biliary drainage in the management of MBO. Specific techniques and devices used for EUS-BD will not be discussed here.
MALIGNANT DISTAL BILIARY OBSTRUCTION VERSUS MALIGNANT HILAR BILIARY OBSTRUCTION
First, MBO can be divided into malignant distal biliary obstruction (MDBO) and malignant hilar biliary obstruction (MHBO) and the reason as such was that drainage strategies and outcomes differ from one another. For MDBO, the level obstruction occurs at the common bile duct sparing the intrahepatic ducts and relieving the obstruction is usually straightforward, providing instant clinical response and for that, often a single endoscopic procedure is usually sufficient to address the problem. On the other hand, in MHBO, achieving adequate drainage can be frustrating as intrahepatic biliary obstruction can be complex and multiple to which inadequate drainage may result in life-threatening secondary cholangitis. The common classification used is the Bismuth-Corlette (BS) classification, in which Bismuth type III–IV may involve more than one segment of intrahepatic obstruction.[10] With that, achieving adequate biliary drainage is not straightforward, which often requires drainage of more than one segment of the liver, and thus, more than one biliary drainage procedure may be needed. Moreover, to gauge the degree of biliary obstruction is often difficult in real-life clinical practice and more so in predicting adequacy of drainage. It is important to note that it has shown by achieving adequate drainage of >50% of liver segments correlates with better survival outcomes.[11]
EUS-GUIDED BILIARY DRAINAGE
EUS-BD has gained momentum over recent years and plays an important role in the management of MBO. Types of EUS-guided biliary procedures include: (1) EUS-guided choledochoduodenostomy (EUS-CDS), (2) EUS-guided hepaticogastrostomy (EUS-HGS), (3) EUS-guided hepaticoduodenostomy (EUS-HDS), (4) EUS-guided rendezvous procedure (EUS-RV) (5) EUS-guided anterograde stenting (EUS-AS). Fully covered self-expandable metal stents, partially covered metal stents, plastic stents, and lumen apposing metal stents (LAMS) are usually used for EUS-BD.[12,13] A hybrid partially half-covered and uncovered biliary self-expandable metallic stent (SEMS) or a 6 mm fully covered SEMS is commonly used in EUS-HGS.[14,15] Indications for EUS-BD include failed ERCP, inaccessible papilla by duodenal obstruction and altered surgical anatomy.[16] In this section, we will mainly highlight data that are relevant to the use of EUS-CDS and EUS-HGS, which are the most common methods of EUS-BD used in current clinical practice.
The advantage and disadvantages associated with EUS-BD are listed in Table 1. Common adverse events (AEs) associated with EUS-BD include bleeding, peritonitis, cholangitis, pneumo-peritoneum, bile leak, and stent migration or stent re-occlusion, of which bleeding is the most common of up to 11%.[17,18,19] To date, there are multiple studies carried out to evaluate the use of EUS-BD in clinical practice. However, it is important to note that many of these studies at the moment were retrospective; hence, data may seem bias; furthermore, most studies were used in the management of distal biliary obstruction with little prospective data on hilar biliary obstruction.
Table 1.
Advantages and disadvantages of EUSbiliary drainage
| Advantages | Disadvantages |
|---|---|
| Without the need of an external drainage tube | Complex procedure requiring high level of expertise |
| Lower rates of recurrent biliary obstruction and longer stent patency | Higher complications rate that ERCP (bleeding, stent migration, bile leak and pneumo-peritoneum) |
| One step procedure | |
| Lower risk of pancreatitis | |
| Altered anatomy |
Here, we look at the available evidence on the use of EUS-BD in MDBO. In two meta-analyses, it was revealed that the overall safety of EUS-BD, of which the technical success rate (TSR), clinical success rate (CSR), and AE were 90%–94%, 91.6%, and 16%–23%, respectively.[17,18] Stent migration can be a cause of concern here with the reported risk ranging from 12% to 30.8%.[18,20] Retrospective studies available have shown to have good clinical outcomes with the overall TSR, CSR, and AE ranging from 86.5% to 100%, 90%–100% and 0%–23%, respectively, though the predominant pathology was MDBO.[20,21,22,23] A review article evaluating the use of EUS-HGS showed that in 27 studies evaluated the TSR, CSR, and AE were 96%, 90%, and 18%, respectively.[24] These studies were, however, predominantly retrospective studies involving MDBO and only a small number of prospective studies. Therefore, with cautious use of EUS-BD in MDBO, it can be deemed safe and clinically efficacious.
With regard to MHBO, EUS CDS would not be feasible, and hence, we look at what are the evidence available. Minaga et al. retrospectively had 30 patients with MHBO who underwent EUS-BD after failed ERCP. The TSR, CSR, and AE rates were 96.7%, 75.9%, and 10%, respectively.[25] Moryoussef et al. prospectively recruited 18 patients who has proximal MBO for EUS-HGS. The TSR, CSR, and AE rates were 94%, 72.2%, and 16.7%, respectively.[26] In another retrospective study by Ogura et al., 10 out of 26 patients with MHBO who needed re-intervention after ERCP underwent EUS-BD and the TSR, CSR, and AE rates were 100%, 90%, and 0%, respectively.[27] A review article by Nakai et al. in which 11 studies of EUS-BD in MHBO found that the pooled TSR, CSR, and AEs of 11 available studies were 98%, 77%, and 8%, respectively.[28] EUS HGS, HDS, and bridging methods were included in this review as either an initial or rescue method after failed ERCP in the treatment of MHBO. However, it is worth to note that the cohort of patients of all these studies are small and consists of a number retrospective studies, case reports, and case series. Similar to MDBO, EUS-BD is safe and efficacious when managing MHBO. The studies are summarized in Tables 1 and 2.
Table 2.
Summary of single arm studies in EUS-biliary drainage
| Author | Study design | Patients (n) | Pathology | Intervention | Overall technical success rate, % (n) | Overall Clinical Success Rate, %(n) | Overall Adverse Events, %(n) | Stent Migration %(n) |
|---|---|---|---|---|---|---|---|---|
| Hara et al. (2011)[21] | Prospective, Single Center | 18 | MDBO | EUS-CDS | 94 (17/18) | 100 (17/17) | 17 (3/18) | 5.6 (1/18) |
| Song et al. (2012)[20] | Retrospective, Single Center | 15 | MDBO | EUS-CDS | 86.7 (13/15) | 100 (13/13) | 23.1 (3/13) | 30.8 (4/13) |
| Kunda et al. (2016)[22] | Retrospective, Multicenter | 57 | MDBO | EUS CDS | 98.2 (56/57) | 94.7 (54/57) | 9 (7/57) | 1.7 (1/57) |
| Ogura et al. (2016)[27] | Retrospective, single center | 10 | MHBO | EUS-HGS | 100 (10/10) | 90 (9/10) | 0 | NA |
| Lu et al. (2017)[23] | Retrospective, single center | 24 | MBO | 17 EUS-CDS 4 EUS-HGS | 95.8 (23/24) | 100 (23/23) | 13 (3/23) | 0 |
| Minaga et al. (2017)[25] | Retrospective, single center | 30 | MHBO | EUS-HGS | 96.7 (29/30) | 75.9 (22/29) | 10 (3/30) | 0 |
| Moryouseff et al. (2017)[26] | Prospective, single center | 18 | MHBO | EUS-HGS | 94 (17/18) | 72.2 (13/17) | 16.7 (3/18) | 0 |
MHBO: Malignant hilar biliary obstruction; NA: Not available; MBO: Malignant biliary obstruction; CDS: Choledochoduodenostomy; HGS: Hepaticogastrostomy
EUS CHOLEDOCHODUODENOSTOMY VERSUS EUS HEPATICOGASTROSTOMY
In regard to whether EUS-CDS or EUS-HGS is preferred, there are few recent studies that show a similar excellent technical and clinical success. However, it appears that the risk of AEs is higher with EUS-HGS. The TSR, CSR, and AE were 84%–100%; 77%–100%; 9.3%–32.6% in the EUS-CDS group versus 90.4%–100%; 82.1%–100%; 9.5%–35.6% in the EUS-HGS group, respectively.[19,29,30,31,32,33,34,35] These studies are summarized in Table 3.
Table 3.
Summary of studies using EUS- choledochoduodenostomy versus EUS-hepaticogastrostomy
| Authors | Study design | Patients (n) | Pathology | Intervention | Technical Success rate, % (n) | Clinical Success rate, % (n) | Adverse Events, % (n) |
|---|---|---|---|---|---|---|---|
| Dhir et al.(2014)[29] | Retrospective, Multicentre | 68 | MBO | CDS versus HGS | 96.8 (31). versus 94.4 (34), P=0.345 | NA | 9.3 (3) versus 30.5 (11), P=0.03 |
| Kawakubo et al. (2014)[30] | Retrospective, Multicentre | 64 | MDBO | CDS versus HGS | 95 (42/44) versus 95 (19/20), P=1.00 | NA | 14 (6/44) versus 30 (6/20), P=0.74 |
| Gupta et al. (2014)[19] | Retrospective, Multicentre | 240 | MBO and Benign BO | CDS versus HGS | 84.3 (75/89) versus 90.4 (132/145), P=0.15 | NA | 32.6 (29/89) versus 35.6 (52/146) |
| Artifon et al. (2015)[31] | Prospective, Single Centre | 49 | MDBO | CDS versus HGS | 91 (22/24) versus 96 (24/25), P=0.609 | 77 (17/24) versus 91 (22/25), P=0.234 | 12.5 (3/24) versus 20 (5/25), P=0.702 |
| Poincloux et al. (2015)[32] | Retrospective, single centre | 101 | MDBO | CDS versus HGS | 96.7 (29/30) versus 98.5 (65/66) | 93.1 (27/29) versus 93.8 (61/65) | 10 (3/30) versus 22.7 (15/66) |
| Khashab et al. (2016)[33] | Retrospective, Multicentre | 121 | MDBO | CDS versus HGS | 93.3 (56/60) versus 91.8 (56/61), P=0.75 | 85.5 (51/60) versus 82.1 (50/61), P=0.64 | 13.3 (8/60) versus 19.7 (12/61), P=0.37 |
| Guo et al. (2016)[34] | Retrospective, single centre | 21 | MBO | CDS versus HGS | 100 (14/14) versus 100 (7/7) | 100 (14/14) versus 100 (7/7) | 7.1 (1/14) versus 28.5 (2/7) |
| Cho et al. (2017)[35] | Prospective, single centre | 54 | MBO | CDS versus HGS | 100 (33/33) versus 100 (21/21) | 100 (33/33) versus 85.7 (18/21), P=0.054 | 15.1 (5/33) versus 9.5 (4/21), P=0.374 |
CDS: Choledochoduodenostomy; HGS: Hepaticogastrostomy; MHBO: Malignant hilar biliary obstruction; NA: Not available; MBO: Malignant biliary obstruction
The recent development of a one-step hot-cautery LAMS has made EUS-CDS a very attractive option in the management of MDBO as a one-step procedure. The TSR was reported to be 100% with a CSR of 95% with AE of 36.7%.[36] This is in contrast to performing EUS-HGS to which the learning curve is somewhat steep and require much experience to be able to achieve the required competence, desired clinical results, and safety profile[37] [Table 3].
EUS-GUIDED BILIARY DRAINAGE VERSUS ERCP
In comparison with ERCP in draining MDBO, EUS-BD similarly showed comparable efficacy and superior safety profile, especially lower risk of pancreatitis. The reported TSR, CSR, and AE were 93.4%–100%; 90.2%–100% and 6.3%–15% in the EUS-BD group versus 90.2%–94.2%; 91.3%–94.5%; 8.7%–24% in the ERCP group, respectively.[38,39,40,41] In a meta-analysis, ERCP and EUS-BD are seen as comparable in terms of CSR and AE with a significantly lower risk of pancreatitis in the EUS-BD group (0.3% vs. 7.3%).[42]
On the other hand, in MHBO, to date there are no comparative studies between EUS-BD and ERCP in MHBO. However, when ERCP is chosen, bilateral drainage results in better clinical outcomes with lower re-intervention rates compared to unilateral drainage. In a prospective study by Lee et al. involving 133 patients with malignant hilar obstruction and comparing bilateral and unilateral groups, the TSR were 95.5% vs. 100% (P = 0.244), CSR were 95.3% vs. 84.9% (P = 0.047), early AE were 6.3% vs. 27.3% (P = 0.001). The primary re-intervention rates were also lower (P = 0.049) in the bilateral group (42.6%) compared to the unilateral group (60.3%).[43] In a meta-analysis consisting of 9 studies involving 782 patients with malignant hilar obstruction showed that bilateral stenting had significantly lower re-intervention rate compared with unilateral drainage (odds ratio [OR] = 0.59, 95% confidence interval [CI]: 0.40–0.87, P = 0.009). In addition, there was no difference in the TSR (OR = 0.7, CI: 0.42–1.17, P = 0.17), early complication rate (OR = 1.56, CI: 0.31–7.75, P = 0.59), late complication rate (OR = 0.91, CI: 0.58–1.41, P = 0.56), and stent malfunction (OR = 0.69, CI: 0.42–1.12, P = 0.14).[44] Needless to say, comparative studies involving EUS-BD and ERCP in MHBO are still lacking. The studies are summarized in Table 4.
Table 4.
Summary of studies of EUS-biliary drainage versus ERCP
| Author | Study design | Patients (n) | Pathology | Intervention | Overall technical success rate, %(n) | Overallbclinical success rate, %(n) | Overall adverse events, %(n) |
|---|---|---|---|---|---|---|---|
| Dhir et al. (2015)[38] | Retrospective, single centre | 208 | MDBO | EUS BD (CDS/AS) versus ERCP | 93.4 (97/104) versus 94.2 (98/104), P=0.246 | 89.4 (93/104) versus 91.3 (95/104), P=1.00 | 8.7 (9/104) versus 8.7 (9/104), P=1.00 |
| Paik et al. (2018)[39] | Prospective, Multicentre | 125 | MDBO | EUS BD (HGS/CDS) versus ERCP | 93.8 (60/64) versus 90.2 (55/61) | 90 (54/60) versus 94.5 (52/55) | 6.3 (4/64) versus 19.7 (12/61), P=0.03 |
| Nakai et al. (2019)[40] | Prospective, Multicentre with retrospective control group | 34 | MDBO | EUS-CDS versus ERCP | 97 (33/34) | 100 (34/34) | 15 (5/34) versus 24 (6/25), P=0.50 |
| Park et al. (2018)[41] | Prospective, single centre | 30 | MBO | EUS-BD versus ERCP | 92.8 (13/14) versus 100 (14/14), P=1.00 | 100 (13/13) versus 92.8 (13/14), P=1.00 | 0 versus 0 |
BD: Biliary drainage; CDS: Choledochoduodenostomy; HGS: Hepaticogastrostomy; MHBO: Malignant hilar biliary obstruction; MBO: Malignant biliary obstruction
Combination of ERCP and EUS-BD (CERES) [Figure 1a and b] was a novel method which appears to be a feasible alternative to PTBD in the treatment of MHBO with Bismuth type III–IV disease.[45,46] This attractive option is based on the principles that internal drainage is much more desirable and alleviate the high complication and morbidity rates of using PTBD. A recent multicenter observation open-label study comparing CERES versus PTBD techniques for MHBO showed that the overall TSR, CSR, and complication rates of CERES versus PTBD were 84.2% (16/19) versus 100% (17/17) (P = 0.23), 78.9% (15/19) versus 76.5% (13/17) (P = 1), and 26.3 (5/19) versus 35.3 (6/17) (P = 0.56), respectively. Within 3 and 6 months, recurrent biliary obstruction rates of CERES versus PTBD were 26.7% (4/15) versus 88.2% (15/17), P = 0.001, and 22.2% (2/9) versus 100% (9/9), P = 0.002, respectively.[47] More studies will be needed to further evaluate the clinical use and safety of this technique [Table 4 and Figure 1a, b].
Figure 1.
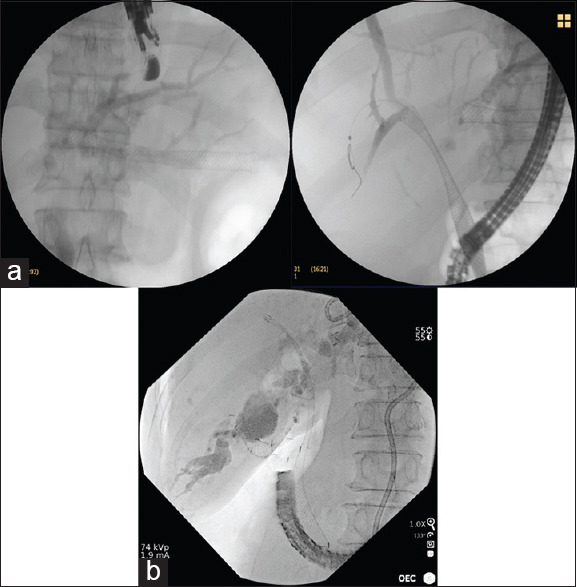
(a) EUS-hepaticogastrostomy to left intrahepatic duct combined with ERCP to the right intrahepatic duct. (b) EUS-hepaticoduodenostomy to right intrahepatic duct combined with ERCP to the right intrahepatic duct.
EUS-GUIDED BILIARY DRAINAGE VERSUS PERCUTANEOUS TRANSHEPATIC BILIARY DRAINAGE
In comparing EUS-BD and PTBD in the management of MDBO, several prospective and retrospective studies have showed comparable technical and clinical success with a lower rate of AEs favoring EUS-BD when comparing these two modalities of biliary drainage. These studies were predominantly single center, retrospective studies with a relatively small cohort of patients, the reported TSR, CSR and AE of 86.4%–100%; 62.2%–100%; 6.6%–15.3% in the EUS-BD group versus 46%–100%; 46%–100%; 25%–53.8% in the PTBD group, respectively.[48,49,50,51,52,53] In a latest prospective multi-center randomized controlled trial (RCT), Lee et al. strengthen this argument in that EUS-BD has similar clinical efficacy with lower complications compared to PTBD.[52] In a meta-analysis conducting nine studies with 483 patients, it showed that there is no difference in technical success between EUS-BD versus PTBD group (OR: 1.78; 95% CI: 0.69–4.59; I2 = 22%). However, the EUS-BD group was associated with better clinical success (OR: 0.45; 95% CI: 0.23–0.89; I2 = 0%), fewer postprocedure AEs (OR: 0.23; 95% CI: 0.12–0.47; I2 = 57%), and lower rate of reintervention (OR: 0.13; 95% CI: 0.07–0.24; I2 = 0%). This again showed that EUS-BD should be the method of choice over PTBD when ERCP fails.[54] As stated previously, the only study available that compared the use of EUS-BD and PTBD in MHBO showed that EUS-BD is as efficacious with lower rates of recurrent biliary obstruction.[47] Available studies are summarized in Table 5.
Table 5.
Summary of studies using EUS - biliary drainage versus percutaneous transhepatic biliary drainage
| Authors | Study Design | Patients (n) | Pathology | Intervention | Technical Success rate, % (n) | Clinical Success rate, % (n) | Adverse Events, % (n) |
|---|---|---|---|---|---|---|---|
| Artifon et al. (2012)[48] | Prospective, single center | 25 | MDBO | EUS-CDS versus PTBD | 100 (13/13) versus 100 (12/12) | 100 (13/13) versus 100 (12/12) | 15.3 (2/13) versus 25 (3/12), P=0.44 |
| Bapaye et al. (2013)[49] | Retrospective, single center | 50 | 50 MDBO | EUS BD (CDS/HGS) versus PTBD | 92 (23/25) versus 46 (12/26), P<0.05 | 92 (23/25) versus 46 (12/26), P<0.05 | 20 (5/25) versus 46 (12/26), P<0.05 |
| Khashab et al. (2015)[50] | Retrospective, Single Center | 73 | MDBO | EUS CDS versus PTBD | 86.4 (19/22) versus 100 (51/51), P=0.007 | 100 (19/19) versus 86.4 (47/51), P=0.40 | 18.2 (4/22) versus 39.2 (36/51), P<0.001 |
| Sharaiha et al. (2016)[51] | Retrospective, Single Center | 60 | 50 MDBO | EUS-BD (CDS/HGS) versus PTBD | 91.6 (43/47) versus 93.3 (12/13), P=1.000 | 62.2 (29/47) versus 25 (3/13), P=0.03 | 6.6 (3/47) versus 53.8 (7/13), P=0.001 |
| Lee et al. (2016)[52] | Prospective, Multicenter | 66 | MDBO | EUS CDS versus PTBD | 94.1 (32/34) versus 96.9 (31/32), P=0.008 | 87.5 (28/32) versus 87.1 (27/31), P=1.00 | 8.8 (3/34) versus 31.2 (10/32) , P=0.022 |
| Sportes et al. (2017)[53] | Retrospective, Single Center | 51 | MDBO | EUS-HGS versus PTBD | 100 (31/31) versus 100 (20/20), P=1.00 | 86 (25/31) versus 83 (15/20), P=0.88 | 16 (5/31) versus 10 (2/20) |
| Kongkam et al. (2020)[47] | Prospective, Multi-center | 36 | MHBO | EUS-BD (CERES) versus PTBD | 84.2 (16/19) versus 100 (17/17), P=0.23 | 78.9 (15/19) versus 76.5 (13/17), P=1.00 | 23.6 (5/19) versus 35.3 (6/17), P=0.56 |
BD: Biliary drainage; CERES: Combined ERCP and EUS-BD; PTBD: Percutaneous transhepatic biliary drainage; CDS: Choledochoduodenostomy; HGS: Hepaticogastrostomy; MHBO: Malignant hilar biliary obstruction; MBO: Malignant biliary obstruction
EUS RENDEZVOUS PROCEDURE
EUS Rendezvous Procedure (EUS-RV) was first described in 2004 by Mallery et al.[55] EUS-RV is indicated as a salvage technique for failed biliary cannulation during ERCP even which was performed by a skilled endoscopist. Available studies at present are mostly retrospective studies involving MDBO. Dhir et al. concluded that EUS-RV was found to be superior to precut papillotomy for single-session biliary access with a success rate of 98.3% versus 90.3%; P = 0.03.[56] The overall technical successful rate of EUS-RV across some studies were >80%.[29,57,58] Both intrahepatic and extrahepatic approaches are feasible with varying degrees of success from 44% to 82%.[57,58,59,60,61] The incidences of AEs were 10%–23%. The major complications were bleeding, bile leakage, peritonitis, pneumoperitoneum, pancreatitis, and mediastinitis.[29,57,58] Some argued that intrahepatic access is preferred due to the lower risk of bile leakage.[59,62] The major disadvantage of EUS-RV is that it involves a two-step procedure. The available studies are summarized in Table 6.
Table 6.
Summary of studies of EUS-guided rendezvous technique
| Author | Study design | Number of patients (n) | EHBD approach success % (n) | IHBD approach success % (n) | Overall technical success % (n) | Overall clinical success % (n) | Adverse events % (n) |
|---|---|---|---|---|---|---|---|
| Kahaleh et al. (2006)[59] | Retrospective, single center | 23 | 70 (7/10) | 85 (11/13) | 78 (18/23) | 100 (18/18) | 17 (4/23) |
| Dhir et al. (2012)[56] | Retrospective, single center | 58 | 98 (57/58) | - | 98.3 (57/58) | - | 3.4 (2/58) |
| Iwashita et al. (2012)[60] | Retrospective, single center | 40 | 81 (25/31) | 44 (4/9) | 72.5 (29/40) | - | 13 (5/40) |
| Khashab et al. (2013)[57] | Retrospective, two center | 13 | 100 (11/11) | 100 (2/2) | 100 (13/13) | 100 (13/13) | 15.4 (2/13) |
| Dhir et al. (2013)[58] | Retrospective, single center | 35 | 100 (18/18) | 94 (16/17) | 97 (34/35) | - | 23 (8/35) |
| Iwashita et al. (2016)[61] | Prospective, multi center | 20 | 80 (16/20) | - | 80 (16/20) | - | 15 (3/20) |
EHBD: Extrahepatic bile duct; IHBD: Intrahepatic bile duct
EUS ANTEROGRADE STENTING
EUS-AS is useful in patients who have altered anatomy or presence of duodenal obstruction and is only applicable to MDBO. In reported small retrospective studies, the overall success rate ranges from 60% to 85%, with complication rates from 0% to 15%. Cholangitis, stent occlusion, and migration are among the complications reported.[63,64] Available studies similar to EUS-RV are rather limited.
APPLICATION OF EUS-GUIDED BILIARY DRAINAGE AND PROPOSED ALGORITHM IN REAL LIFE CLINICAL PRACTICE
With the evidence presented in the above sections, how could we possibly incorporate the different methods of biliary drainage in today's landscape of managing MBO. To this day, EUS-BD has been seen as a salvage method of biliary drainage compared to ERCP and PTBD. Its availability vastly depends on the facilities and expertise available in their own respective clinical setting. Nonetheless, ERCP and PTBD have always been the preferred method of drainage compared to EUS BD. Whether ERCP or PTBD is more superior than another is still debatable and there are contrasting evidence to this. In a retrospective study, ERCP has resulted in better safety profile and clinical outcomes compared to PTBD even in centers who performs high volume of PTBD procedures.[65] However, there are some advantages of PTBD such as requiring minimal sedation, facilitating precise lobar selection, and reducing the risk of exposing the biliary tree to duodenal contents. In spite of that, the complications of PTBD are reported to be as high as 53.2% and this includes septicemia, cholangitis, bleeding, electrolyte lost, leakage, wound infection, and local discomfort.[66] Recent meta-analyses revealed that though PTBD and ERCP achieved similar results in terms of clinical outcomes, PTBD was associated with lower AEs and better safety profile compared to ERCP. The CSR and AEs of PTBD ranges from 61% to 93.9% and 12.9%–67%, respectively.[67,68] Hence, one could possibly argue that some may prefer PTBD over ERCP or when ERCP fails or is contraindicated, though by majority standards, ERCP has always been the primary choice whenever possible.
With the above considerations and conflicts surrounding the different mode of biliary drainage in daily practice, it reinforces the need to look at the application of EUS-BD in clinical practice as a modality of biliary drainage in unresectable MBO. In addition, there are no clear guidelines at the moment on how these methods can be used in different levels of MBO.
Major guidelines recommend ERCP as the primary choice of biliary drainage in MDBO. SEMSs are often preferred for this purpose. PTBD is then used when ERCP fails.[69,70] Therefore, ERCP remains the first modality used in biliary drainage for MDBO, and current guidelines do advocate that PTBD or EUS-BD will be considered if ERCP fails.[70,71,72] However, at this point, with the data presented in the earlier sections, we do recommend that EUS-BD should be preferred over PTBD.
Feasible options available for EUS-guided interventions for unresectable MDBO include: (1) EUS-BD (CDS or HGS), (2) EUS-RV, and (3) EUS-AS. However, there are a number of scenarios to be considered when deciding the choice of EUS-BD. First, whether there is the presence of duodenal obstruction, the accessibility of the papilla or the presence of a surgically altered anatomy. Second, whether the level of the distal biliary obstruction is high or low. EUS-CDS, for example, will not be possible in high-level MDBO due to difficulty in executing interventional procedures at the proximal common bile duct. With that together with the similar clinical efficacy and superior safety profile of EUS-BD over PTBD, EUS-BD should be the preferred mode of biliary drainage compare to PTBD in the event ERCP fails or any contraindication to ERCP in MDBO. Whether primary EUS-BD should be advocated over ERCP is still yet to be seen. Although this option appears to be safe and promising, more studies will be needed to evaluate this.
With regard to MHBO, biliary drainage is much more complex as mentioned previously. Bismuth type III and IV disease remains to be more challenging than type I–II as often to attain adequate clinical success, it involves draining more than one segment of the liver. Whenever possible, bilateral stenting by ERCP is better than unilateral stenting. Having said that, adequate biliary drainage may not be optimal in Bismuth Type III–IV and together with the difficulty of ERCP, the risk of contrast-induced cholangitis will invariably be increased.[73] In a retrospective study showed that percutaneous self-expandable metal stents is preferred over endoscopic technique owing to a higher success rate and lower AEs in Bismuth type III–IV disease.[74] Currently, a RCT is still being conducted to compare PTBD and ERCP in the management of MHBO.[75] At this juncture, the Asia-Pacific Consensus and ESGE guidelines recommend PTBD over ERCP in MHBO of Bismuth type III–IV disease and ERCP over PTBD in Bismuth type II disease.[70,76]
Feasible options available for EUS-guided interventions for unresectable MHBO include: (1) EUS-HGS, (2) EUS-HDS, (3) Bridging method with (EUS-HGS/HDS), (4) CERES, and (5) EUS-RV (6) EUS-AS. Evidence pertaining the EUS-BD as the primary method for biliary drainage in MHBO is still scarce at the moment. Similar to the management of MDBO, EUS-BD should be considered over PTBD if ERCP is not feasible. This is to maximize the probability of achieving optimal biliary drainage with minimal risk of cholangitis. Although studies that directly compare EUS-BD with PTBD or ERCP in the management of unresectable MHBO are still very much limited at the moment, the undesirable higher complications rate seen in PTBD as mentioned previously alone may reinforce the notion that EUS-BD should be the preferred option in such circumstance. Despite this, studies regarding the use of EUS-BD as a primary choice of drainage modality in MHBO is still very much needed to ascertain its recommendation. From the patients' point of view, it has been shown that internal drainage is more preferable than external drainage. A multicenter survey conducted looking at whether patients preference between EUS-BD or PTBD revealed that >80% preferred EUS-BD over PTBD. The reasons were less physical discomfort without percutaneous drain tube placement (78.1%), a higher success rate with relatively lower morbidity (43.8%), and the ability to be performed at the same time as the ERCP (28.3%).[77]
Even though there are strong reasons to use EUS-BD in the forefront of today's clinical practice, limitations to the application of EUS-BD is still a common obstacle in that only limited centers have the capabilities to perform such procedures. Only in high volume centers where advanced therapeutic EUS expertise are available then only EUS-BD will be performed. The complexity and difficulty of the procedure further limit its use in daily practice. As a result, in the vast majorities of centers where EUS expertise are not available, ERCP and PTBD are still the preferred choices of biliary drainage in MBO. A proposed algorithm of the position of EUS-BD in practice is shown in Figure 2.
Figure 2.
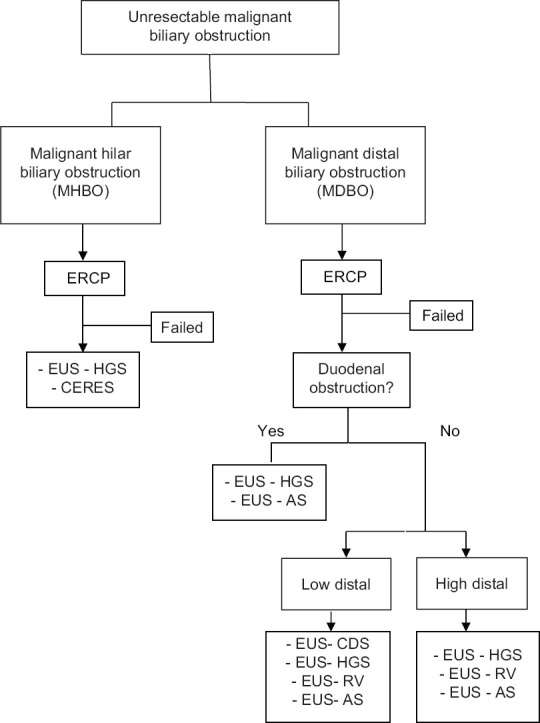
Proposed algorithm for EUS-BD in unresectable malignant biliary obstruction. AS: Anterograde stenting; CDS: Choledochoduodenostomy; EUS-BD: EUS-guided biliary drainage; CERES: Combined ERCP and EUS-BD; HGS: Hepaticogastrostomy; RV: Rendezvous procedure
CONCLUSION
Interventional EUS has come a long way over the years, and the contribution of their role to the management of pancreaticobiliary diseases has been increasingly important. We believe that with the current evidence available as discussed above, EUS-BD together with ERCP and not PTBD should be the preferred method of biliary drainage in the management of MBO and it has proven to be comparable or more efficacious and most of all safer. Unless in patients who has a poor expected survival time of <3 months or those who has poor functional status or unfit for endoscopic drainage, the use of PTBD should otherwise be discouraged. In addition, with the continuous development of improved stents such as the one-step hot-cautery LAMS and EUS-BD-specific endoscopic accessories, the choice and importance of EUS-BD cannot be overemphasized.
Further prospective randomized studies will be needed to explore not only the benefits of EUS-BD and the possibility of it being the primary choice of biliary drainage in MBO, especially in MHBO but also to look at optimum devices, techniques, and ways to minimize the complication rates of EUS-BD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pu LZ, Singh R, Loong CK, et al. Malignant biliary obstruction: Evidence for best practice. Gastroenterol Res Pract. 2016;2016:3296801. doi: 10.1155/2016/3296801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aadam AA, Liu K. Endoscopic palliation of biliary obstruction. J Surg Oncol. 2019;120:57–64. doi: 10.1002/jso.25483. [DOI] [PubMed] [Google Scholar]
- 3.Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J Oncol. 2019;10:10–27. doi: 10.14740/wjon1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kongkam P, Benjasupattananun P, Taytawat P, et al. Pancreatic cancer in an Asian population. Endosc Ultrasound. 2015;4:56–62. doi: 10.4103/2303-9027.151361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Razumilava N, Gores GJ. Cholangiocarcinoma. Lancet (London, England) 2014;383:2168–79. doi: 10.1016/S0140-6736(13)61903-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Florio AA, Ferlay J, Znaor A, et al. Global trends in intrahepatic and extrahepatic cholangiocarcinoma incidence from 1993 to 2012. Cancer. 2020;126:2666–78. doi: 10.1002/cncr.32803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagino M, Ebata T, Yokoyama Y, et al. Evolution of surgical treatment for perihilar cholangiocarcinoma: A single-center 34-year review of 574 consecutive resections. Ann Surg. 2013;258:129–40. doi: 10.1097/SLA.0b013e3182708b57. [DOI] [PubMed] [Google Scholar]
- 8.Boulay BR, Birg A. Malignant biliary obstruction: From palliation to treatment. World J Gastrointest Oncol. 2016;8:498–508. doi: 10.4251/wjgo.v8.i6.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irisawa A, Katanuma A, Itoi T. Otaru consensus on biliary stenting for unresectable distal malignant biliary obstruction. Dig Endosc. 2013;25(Suppl 2):52–7. doi: 10.1111/den.12069. [DOI] [PubMed] [Google Scholar]
- 10.Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975;140:170–8. [PubMed] [Google Scholar]
- 11.Caillol F, Bories E, Zemmour C, et al. Palliative endoscopic drainage of malignant stenosis of biliary confluence: Efficiency of multiple drainage approach to drain a maximum of liver segments. United European Gastroenterol J. 2019;7:52–9. doi: 10.1177/2050640618803812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dhir V, Isayama H, Itoi T, et al. Endoscopic ultrasonography-guided biliary and pancreatic duct interventions. Dig Endosc. 2017;29:472–85. doi: 10.1111/den.12818. [DOI] [PubMed] [Google Scholar]
- 13.Umeda J, Itoi T, Tsuchiya T, et al. A newly designed plastic stent for EUS-guided hepaticogastrostomy: A prospective preliminary feasibility study (with videos) Gastrointest Endosc. 2015;82:390–600. doi: 10.1016/j.gie.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 14.Okuno N, Hara K, Mizuno N, et al. Efficacy of the 6-mm fully covered self-expandable metal stent during endoscopic ultrasound-guided hepaticogastrostomy as a primary biliary drainage for the cases estimated difficult endoscopic retrograde cholangiopancreatography: A prospective clinical study. J Gastroenterol Hepatol. 2018;33:1413–21. doi: 10.1111/jgh.14112. [DOI] [PubMed] [Google Scholar]
- 15.De Cassan C, Bories E, Pesenti C, et al. Use of partially covered and uncovered metallic prosthesis for endoscopic ultrasound-guided hepaticogastrostomy: Results of a retrospective monocentric study. Endosc Ultrasound. 2017;6:329–35. doi: 10.4103/2303-9027.209869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Teoh AY, Dhir V, Kida M, et al. Consensus guidelines on the optimal management in interventional EUS procedures: Results from the Asian EUS group RAND/UCLA expert panel. Gut. 2018;67:1209–28. doi: 10.1136/gutjnl-2017-314341. [DOI] [PubMed] [Google Scholar]
- 17.Khan MA, Akbar A, Baron TH, et al. Endoscopic ultrasound-guided biliary drainage: A systematic review and meta-analysis. Dig Dis Sci. 2016;61:684–703. doi: 10.1007/s10620-015-3933-0. [DOI] [PubMed] [Google Scholar]
- 18.Wang K, Zhu J, Xing L, et al. Assessment of efficacy and safety of EUS-guided biliary drainage: A systematic review. Gastrointest Endosc. 2016;83:1218–27. doi: 10.1016/j.gie.2015.10.033. [DOI] [PubMed] [Google Scholar]
- 19.Gupta K, Perez-Miranda M, Kahaleh M, et al. Endoscopic ultrasound-assisted bile duct access and drainage: Multicenter, long-term analysis of approach, outcomes, and complications of a technique in evolution. J Clin Gastroenterol. 2014;48:80–7. doi: 10.1097/MCG.0b013e31828c6822. [DOI] [PubMed] [Google Scholar]
- 20.Song TJ, Hyun YS, Lee SS, et al. Endoscopic ultrasound-guided choledochoduodenostomies with fully covered self-expandable metallic stents. World J Gastroenterol. 2012;18:4435–40. doi: 10.3748/wjg.v18.i32.4435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hara K, Yamao K, Niwa Y, et al. Prospective clinical study of EUS-guided choledochoduodenostomy for malignant lower biliary tract obstruction. Am J Gastroenterol. 2011;106:1239–45. doi: 10.1038/ajg.2011.84. [DOI] [PubMed] [Google Scholar]
- 22.Kunda R, Pérez-Miranda M, Will U, et al. EUS-guided choledochoduodenostomy for malignant distal biliary obstruction using a lumen-apposing fully covered metal stent after failed ERCP. Surg Endosc. 2016;30:5002–8. doi: 10.1007/s00464-016-4845-6. [DOI] [PubMed] [Google Scholar]
- 23.Lu L, Tang X, Jin H, Yang J, Zhang X. Endoscopic ultrasound-guided biliary drainage using self-expandable metal stent for malignant biliary obstruction. Gastroenterol Res Practice. 2017;2017:84094–6284094. doi: 10.1155/2017/6284094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paik WH, Park DH. Outcomes and limitations: EUS-guided hepaticogastrostomy. Endoscopic Ultrasound. 2019;8(Suppl 1):S44–9. doi: 10.4103/eus.eus_51_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Minaga K, Takenaka M, Kitano M, et al. Rescue EUS-guided intrahepatic biliary drainage for malignant hilar biliary stricture after failed transpapillary re-intervention. Surg Endosc. 2017;31:4764–72. doi: 10.1007/s00464-017-5553-6. [DOI] [PubMed] [Google Scholar]
- 26.Moryoussef F, Sportes A, Leblanc S, et al. Is EUS-guided drainage a suitable alternative technique in case of proximal biliary obstruction? Therap Adv Gastroenterol. 2017;10:537–44. doi: 10.1177/1756283X17702614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ogura T, Onda S, Takagi W, et al. Clinical utility of endoscopic ultrasound-guided biliary drainage as a rescue of re-intervention procedure for high-grade hilar stricture. J Gastroenterol Hepatol. 2017;32:163–8. doi: 10.1111/jgh.13437. [DOI] [PubMed] [Google Scholar]
- 28.Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019;52:220–5. doi: 10.5946/ce.2018.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dhir V, Artifon EL, Gupta K, et al. Multicenter study on endoscopic ultrasound-guided expandable biliary metal stent placement: Choice of access route, direction of stent insertion, and drainage route. Dig Endosc. 2014;26:430–5. doi: 10.1111/den.12153. [DOI] [PubMed] [Google Scholar]
- 30.Kawakubo K, Isayama H, Kato H, et al. Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci. 2014;21:328–34. doi: 10.1002/jhbp.27. [DOI] [PubMed] [Google Scholar]
- 31.Artifon EL, Marson FP, Gaidhane M, et al. Hepaticogastrostomy or choledochoduodenostomy for distal malignant biliary obstruction after failed ERCP: Is there any difference? Gastrointest Endosc. 2015;81:950–9. doi: 10.1016/j.gie.2014.09.047. [DOI] [PubMed] [Google Scholar]
- 32.Poincloux L, Rouquette O, Buc E, et al. Endoscopic ultrasound-guided biliary drainage after failed ERCP: Cumulative experience of 101 procedures at a single center. Endoscopy. 2015;47:794–801. doi: 10.1055/s-0034-1391988. [DOI] [PubMed] [Google Scholar]
- 33.Khashab MA, Messallam AA, Penas I, et al. International multicenter comparative trial of transluminal EUS-guided biliary drainage via hepatogastrostomy vs.choledochoduodenostomy approaches. Endosc Int Open. 2016;4:E175–81. doi: 10.1055/s-0041-109083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo J, Sun S, Liu X, et al. Endoscopic ultrasound-guided biliary drainage using a fully covered metallic stent after failed endoscopic retrograde cholangiopancreatography. Gastroenterol Res Pract. 2016;2016:9469472. doi: 10.1155/2016/9469472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cho DH, Lee SS, Oh D, et al. Long-term outcomes of a newly developed hybrid metal stent for EUS-guided biliary drainage (with videos) Gastrointest Endosc. 2017;85:1067–75. doi: 10.1016/j.gie.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 36.Tsuchiya T, Teoh AY, Itoi T, et al. Long-term outcomes of EUS-guided choledochoduodenostomy using a lumen-apposing metal stent for malignant distal biliary obstruction: A prospective multicenter study. Gastrointest Endosc. 2018;87:1138–46. doi: 10.1016/j.gie.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 37.Oh D, Park DH, Song TJ, et al. Optimal biliary access point and learning curve for endoscopic ultrasound-guided hepaticogastrostomy with transmural stenting. Therap Adv Gastroenterol. 2017;10:42–53. doi: 10.1177/1756283X16671671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dhir V, Itoi T, Khashab MA, et al. Multicenter comparative evaluation of endoscopic placement of expandable metal stents for malignant distal common bile duct obstruction by ERCP or EUS-guided approach. Gastrointest Endosc. 2015;81:913–23. doi: 10.1016/j.gie.2014.09.054. [DOI] [PubMed] [Google Scholar]
- 39.Paik WH, Lee TH, Park DH, et al. EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: A multicenter randomized clinical trial. Am J Gastroenterol. 2018;113:987–97. doi: 10.1038/s41395-018-0122-8. [DOI] [PubMed] [Google Scholar]
- 40.Nakai Y, Isayama H, Kawakami H, et al. Prospective multicenter study of primary EUS-guided choledochoduodenostomy using a covered metal stent. Endosc Ultrasound. 2019;8:111–7. doi: 10.4103/eus.eus_17_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Park JK, Woo YS, Noh DH, et al. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: Prospective randomized controlled study. Gastrointest Endosc. 2018;88:277–82. doi: 10.1016/j.gie.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 42.Han SY, Kim SO, So H, et al. EUS-guided biliary drainage versus ERCP for first-line palliation of malignant distal biliary obstruction: A systematic review and meta-analysis. Sci Rep. 2019;9:16551. doi: 10.1038/s41598-019-52993-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee TH, Kim TH, Moon JH, et al. Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: A multicenter, prospective, randomized study (with video) Gastrointest Endosc. 2017;86:817–27. doi: 10.1016/j.gie.2017.04.037. [DOI] [PubMed] [Google Scholar]
- 44.Ashat M, Arora S, Klair JS, et al. Bilateral vs.unilateral placement of metal stents for inoperable high-grade hilar biliary strictures: A systemic review and meta-analysis. World J Gastroenterol. 2019;25:5210–9. doi: 10.3748/wjg.v25.i34.5210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Park DH. Endoscopic ultrasound-guided biliary drainage of hilar biliary obstruction. J Hepato Biliary Pancreatic Sci. 2015;22:664–8. doi: 10.1002/jhbp.271. [DOI] [PubMed] [Google Scholar]
- 46.Kongkam P, Tasneem AA, Rerknimitr R. Combination of endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-guided biliary drainage in malignant hilar biliary obstruction. Dig Endosc. 2019;31(Suppl 1):50–4. doi: 10.1111/den.13371. [DOI] [PubMed] [Google Scholar]
- 47.Kongkam P, Orprayoon T, Boonmee C, et al. ERCP plus endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage for malignant hilar biliary obstruction: a multicenter observational open-label study [published online ahead of print, 2020 Jun 8] Endoscopy. 2020 doi: 10.1055/a-1195-8197. 101055/a-1195-8197. doi:101055/a-1195-8197. [DOI] [PubMed] [Google Scholar]
- 48.Artifon EL, Aparicio D, Paione JB, et al. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: Endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768–74. doi: 10.1097/MCG.0b013e31825f264c. [DOI] [PubMed] [Google Scholar]
- 49.Bapaye A, Dubale N, Aher A. Comparison of endosonography-guided vs.percutaneous biliary stenting when papilla is inaccessible for ERCP. United Europ Gastroenterol J. 2013;1:285–93. doi: 10.1177/2050640613490928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khashab MA, Valeshabad AK, Afghani E, et al. A comparative evaluation of EUS-guided biliary drainage and percutaneous drainage in patients with distal malignant biliary obstruction and failed ERCP. Dig Dis Sci. 2015;60:557–65. doi: 10.1007/s10620-014-3300-6. [DOI] [PubMed] [Google Scholar]
- 51.Sharaiha RZ, Kumta NA, Desai AP, et al. Endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage: Predictors of successful outcome in patients who fail endoscopic retrograde cholangiopancreatography. Surg Endosc. 2016;30:5500–5. doi: 10.1007/s00464-016-4913-y. [DOI] [PubMed] [Google Scholar]
- 52.Lee TH, Choi JH, Park do H, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2016;14:1011–9000. doi: 10.1016/j.cgh.2015.12.032. [DOI] [PubMed] [Google Scholar]
- 53.Sportes A, Camus M, Greget M, et al. Endoscopic ultrasound-guided hepaticogastrostomy versus percutaneous transhepatic drainage for malignant biliary obstruction after failed endoscopic retrograde cholangiopancreatography: A retrospective expertise-based study from two centers. Therap Adv Gastroenterol. 2017;10:483–93. doi: 10.1177/1756283X17702096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: A systematic review and meta-analysis. Gastrointest Endosc. 2017;85:904–14. doi: 10.1016/j.gie.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 55.Mallery S, Matlock J, Freeman ML. EUS-guided rendezvous drainage of obstructed biliary and pancreatic ducts: Report of 6 cases. Gastrointest Endosc. 2004;59:100–7. doi: 10.1016/s0016-5107(03)02300-9. [DOI] [PubMed] [Google Scholar]
- 56.Dhir V, Bhandari S, Bapat M, et al. Comparison of EUS-guided rendezvous and precut papillotomy techniques for biliary access (with videos) Gastrointest Endosc. 2012;75:354–9. doi: 10.1016/j.gie.2011.07.075. [DOI] [PubMed] [Google Scholar]
- 57.Khashab MA, Valeshabad AK, Modayil R, et al. EUS-guided biliary drainage by using a standardized approach for malignant biliary obstruction: Rendezvous versus direct transluminal techniques (with videos) Gastrointest Endosc. 2013;78:734–41. doi: 10.1016/j.gie.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 58.Dhir V, Bhandari S, Bapat M, et al. Comparison of transhepatic and extrahepatic routes for EUS-guided rendezvous procedure for distal CBD obstruction. United European Gastroenterol J. 2013;1:103–8. doi: 10.1177/2050640613480145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kahaleh M, Hernandez AJ, Tokar J, et al. Interventional EUS-guided cholangiography: Evaluation of a technique in evolution. Gastrointest Endosc. 2006;64:52–9. doi: 10.1016/j.gie.2006.01.063. [DOI] [PubMed] [Google Scholar]
- 60.Iwashita T, Lee JG, Shinoura S, et al. Endoscopic ultrasound-guided rendezvous for biliary access after failed cannulation. Endoscopy. 2012;44:60–5. doi: 10.1055/s-0030-1256871. [DOI] [PubMed] [Google Scholar]
- 61.Iwashita T, Yasuda I, Mukai T, et al. EUS-guided rendezvous for difficult biliary cannulation using a standardized algorithm: A multicenter prospective pilot study (with videos) Gastrointest Endosc. 2016;83:394–400. doi: 10.1016/j.gie.2015.04.043. [DOI] [PubMed] [Google Scholar]
- 62.Shah JN, Marson F, Weilert F, et al. Single-operator, single-session EUS-guided anterograde cholangiopancreatography in failed ERCP or inaccessible papilla. Gastrointest Endosc. 2012;75:56–64. doi: 10.1016/j.gie.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 63.Godat S, Bories E, Caillol F, et al. Efficacy and safety in case of technical success of endoscopic ultrasound-guided transhepatic antegrade biliary drainage: A report of a monocentric study. Endosc Ultrasound. 2017;6:181–6. doi: 10.4103/2303-9027.208174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Park DH, Jeong SU, Lee BU, et al. Prospective evaluation of a treatment algorithm with enhanced guidewire manipulation protocol for EUS-guided biliary drainage after failed ERCP (with video) Gastrointest Endosc. 2013;78:91–101. doi: 10.1016/j.gie.2013.01.042. [DOI] [PubMed] [Google Scholar]
- 65.Inamdar S, Slattery E, Bhalla R, et al. Comparison of adverse events for endoscopic vs.percutaneous biliary drainage in the treatment of malignant biliary tract obstruction in an inpatient national cohort. JAMA Oncol. 2016;2:112–7. doi: 10.1001/jamaoncol.2015.3670. [DOI] [PubMed] [Google Scholar]
- 66.Heedman PA, Åstradsson E, Blomquist K, et al. Palliation of malignant biliary obstruction: Adverse events are common after percutaneous transhepatic biliary drainage. Scand J Surg. 2018;107:48–53. doi: 10.1177/1457496917731192. [DOI] [PubMed] [Google Scholar]
- 67.Liu JG, Wu J, Wang J, et al. Endoscopic biliary drainage versus percutaneous transhepatic biliary drainage in patients with resectable hilar cholangiocarcinoma: A systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. 2018;28:1053–60. doi: 10.1089/lap.2017.0744. [DOI] [PubMed] [Google Scholar]
- 68.Zhao XQ, Dong JH, Jiang K, et al. Comparison of percutaneous transhepatic biliary drainage and endoscopic biliary drainage in the management of malignant biliary tract obstruction: A meta-analysis. Dig Endosc. 2015;27:137–45. doi: 10.1111/den.12320. [DOI] [PubMed] [Google Scholar]
- 69.American Society for Gastrointestinal Endoscopy (ASGE) Standards of Practice Committee. Anderson MA, Appalaneni V, Ben-Menachem T, et al. The role of endoscopy in the evaluation and treatment of patients with biliary neoplasia. Gastrointest Endosc. 2013;77:167–74. doi: 10.1016/j.gie.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 70.Dumonceau JM, Tringali A, Papanikolaou IS, et al. Endoscopic biliary stenting: Indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline Updated October 2017. Endoscopy. 2018;50:910–30. doi: 10.1055/a-0659-9864. [DOI] [PubMed] [Google Scholar]
- 71.Mukai S, Itoi T, Baron TH, et al. Indications and techniques of biliary drainage for acute cholangitis in updated Tokyo Guidelines 2018. J Hepatobiliary Pancreat Sci. 2017;24:537–49. doi: 10.1002/jhbp.496. [DOI] [PubMed] [Google Scholar]
- 72.American Society for Gastrointestinal Endoscopy (ASGE) Standards of Practice Committee. Anderson MA, Appalaneni V, Ben-Menachem T, et al. The role of endoscopy in the evaluation and treatment of patients with biliary neoplasia. Gastrointest Endosc. 2013;77:167–74. doi: 10.1016/j.gie.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 73.Yasuda I, Mukai T, Moriwaki H. Unilateral versus bilateral endoscopic biliary stenting for malignant hilar biliary strictures. Digestive Endoscopy. 2013;25:81–5. doi: 10.1111/den.12060. [DOI] [PubMed] [Google Scholar]
- 74.Paik WH, Park YS, Hwang JH, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: A percutaneous versus endoscopic approach. Gastrointest Endosc. 2009;69:55–62. doi: 10.1016/j.gie.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 75.Al-Kawas F, Aslanian H, Baillie J, et al. Percutaneous transhepatic vs.endoscopic retrograde biliary drainage for suspected malignant hilar obstruction: Study protocol for a randomized controlled trial. Trials. 2018;19:108. doi: 10.1186/s13063-018-2473-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol. 2013;28:593–607. doi: 10.1111/jgh.12128. [DOI] [PubMed] [Google Scholar]
- 77.Nam K, Kim DU, Lee TH, et al. Patient perception and preference of EUS-guided drainage over percutaneous drainage when endoscopic transpapillary biliary drainage fails: An international multicenter survey. Endosc Ultrasound. 2018;7:48–55. doi: 10.4103/eus.eus_100_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


