Dear Editor,
Liver abscess is a collection of infected necrotic tissue within liver parenchyma and is commonly polymicrobial or due to Entamoeba.[1] Because of being safe and efficacious image-guided percutaneous drainage (PCD) is considered as drainage procedure of choice for liver abscesses.[1] Although effective, PCD of liver abscesses is associated with significant complications including pain at catheter entry site, peri-catheter leak, bleeding, accidental dislodgement, discomfort, needle-tract infection, pleural abscess, and biliary peritonitis.[2] Moreover, abscess located in the caudate lobe is deep seated and difficult to drain percutaneously. EUS offers an excellent approach to the liver, particularly the left lobe from the stomach. Furthermore, EUS-guided drainage of liver abscess leads to internal drainage with no risk of accidental dislodgment. However, experience with EUS-guided drainage of liver abscesses is limited.[1,3,4] We retrospectively evaluated safety and efficacy of EUS-guided drainage of liver abscesses done in our unit over the past one decade.
Data base of 14 patients (mean age 40.1 ± 11.7 years; 13 males) with liver abscesses who were treated with EUS-guided drainage over the past 10 years was retrospectively reviewed. EUS-guided drainage was done either because of difficulty in performing ultrasound-guided PCD or patients preference for internal drainage. EUS-guided drainage was done with double-pigtail plastic stent/s using a therapeutic linear-array echoendoscope under endoscopic and fluoroscopic guidance. After informed consent, the liver abscess was punctured with a 19G needle [Figure 1] followed by the insertion of guidewire. After securing guidewire, access site was dilated by 4-mm biliary balloon dilator or 6 Fr cystotome followed by balloon dilatation up to 10–12 mm. This was followed by the insertion of two 7Fr double-pigtail stents.
Figure 1.
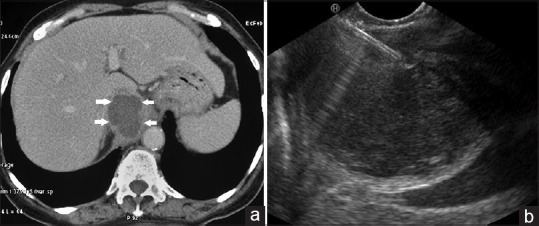
(a) Computed tomography abdomen: Amoebic liver abscess in caudate lobe (arrow). (b) EUS-guided drainage of liver abscess. The abscess being punctured with 19G needle
Of 14 patients treated with EUS-guided drainage, 11 (78.5%) patients had left lobe liver abscess and 3 (21.5%) patients had abscess in the caudate lobe with <1 cm distance between abscess and gastrointestinal lumen. The etiology of liver abscess was amoebic liver abscess in 8 (57%), infected intra-hepatic pseudocyst in 3 (21%), biloma in 2 (14%), and pyogenic liver abscess in 1 (7%) patient, respectively. Four (28.5%) patients had either multiple liver abscesses (n = 1) or co-existent intraabdominal collections (n = 3). The mean size of liver abscess was 6.1 ± 1.1 cm. EUS-guided drainage was done in four patients because of difficulty in performing ultrasound-guided PCD, whereas the remaining 10 patients preferred internal drainage. EUS-guided transgastric drainage was done in 10 patients and transesophageal drainage in four patients. The procedure was technically successful in all patients with no immediate or delayed complications. Two 7 Fr 5 cm double-pigtail plastic stents were placed in all the patients, and only one patient required repeat procedure and exchange of stents. The liver abscess in all the patients resolved within a mean period of 21.5 days, and the stents were removed at 6 weeks. There has been no recurrence of liver abscess in any patient over a follow-up period of 6–106 months. In conclusion, EUS-guided drainage of liver abscesses is technically feasible, safe, as well as effective with good long-term follow-up results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Petrone MC, Arcidiacono PG. EUS-guided drainage of liver abscesses: Ultra uncertain or sound practice? Dig Dis Sci. 2016;61:8–10. doi: 10.1007/s10620-015-3900-9. [DOI] [PubMed] [Google Scholar]
- 2.Singhal S, Changela K, Lane D, et al. Endoscopic ultrasound-guided hepatic and perihepatic abscess drainage: An evolving technique. Therap Adv Gastroenterol. 2014;7:93–8. doi: 10.1177/1756283X13506178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogura T, Masuda D, Saori O, et al. Clinical outcome of endoscopic ultrasound-guided liver abscess drainage using self-expandable covered metallic stent (with Video) Dig Dis Sci. 2016;61:303–8. doi: 10.1007/s10620-015-3841-3. [DOI] [PubMed] [Google Scholar]
- 4.Noh SH, Park DH, Kim YR, et al. EUS-guided drainage of hepatic abscesses not accessible to percutaneous drainage (with videos) Gastrointest Endosc. 2010;71:1314–9. doi: 10.1016/j.gie.2009.12.045. [DOI] [PubMed] [Google Scholar]


