Abstract
Background: In the worldwide, there are the pandemic of the virus coronavirus disease 2019 (COVID-19) and there is no approved treatment for this disease. Case presentation: This study reported a new case with COVID 19 with neurological symptoms such as headache and loss of consciousness without any symptoms and imaging of COVID 19 in admission but RT-PCR COVID 19 of patient was positive and during hospitalization patient had increasing cerebrospinal fluid (CSF) volume in sub-arachnoid space, micro-hemorrhaging in basal ganglia and down ward cerebellar tonsile herniation in the brain imaging, also there were rhabdomyolysis and thrombotic thrombocytopenic purpura in the lab data. Finally, based on abnormal electroencephalogram (EEG), brain death was diagnosed for patient in end of hospitalization. In the 8th of admission day, the patients died after cardiovascular arrest. Conclusion: The COVID 19 can be associated with different symptoms such as neurological complication and brain death was unusual complication in COVID19.
Keywords: COVID 19, rhabdomyolysis, brain death, headache
Background
Coronavirus disease 2019 (COVID-19) is most common pandemic disease in the 2020 so in the year 2019 in Wuhan City, China an unspecified type of pneumonia in many patients has occurred and after a period, this very infectious disease spread in all parts of the world, it has always been increasing the prevalence of this disease and is faced with very different deaths in the world [1]. First, the name of this virus was SARS-COV-2, but the World Health Organization (WHO) called the name of the virus coronavirus disease 2019 (COVID-19) [2].
Symptoms of the disease usually are fever, cough, diarrhea and fatigue along with other respiratory symptoms, and in these patients, usually the findings of lung computed tomography (CT) are reported to be abnormal [3].
In these patients, the symptoms of neurology are not likely to occur, but it is reported that respiratory symptoms can be associated with neurological symptoms in some studies, but the point of this study was to look at a case of disease with a COVID 19 with headache and decreased level of consciousness and without any respiratory symptoms that was referred to hospital.
Case presentation
50-year-old man, medical specialist, with a history of hypothyroidism and migraine from a day before visit, after returning from work, he was suffered from severe and progressive headache, nausea and vomiting, which was improved after serum therapy and receiving the pain relief. The morning of the patient’s visit, he had more severe headaches and epigastric pain, and gradually decreased the level of consciousness that was brought to Alzahra hospital in Isfahan-Iran on April 16, 2020. Due to loss of consciousness (LOC), cardiovascular arrest was occurred after 3 h of admission and the patient’s rhythm returned to normal after 15 minutes of Cardiopulmonary resuscitation (CPR). In addition, after cardiovascular arrest, the echocardiography of patients was reposted 55% EF and LV diastolic dysfunction. Also this loss of consciousness was along with fixed-mydriasis pupil and without corneal and gag reflex, there were no other symptoms, especially respiratory symptoms based on COVID19 in the patient and other examinations were normal.
In primary laboratory test, potassium was reported 6 meq/L that according to hyperkalemia and metabolic acidosis (HCO3=4.2), insulin and glucose with sodium bicarbonate was prescribed. Considering that the patient had metabolic acidosis along with loss of consciousness and fixed-mydriasis pupil, it was suggested that the patient was poisoned with methanol and he underwent hemodialysis for 6 hours but patient s toxic panel was reported negative. In the first day of admission, based on suspicious of COVID19 chloroquine and Lopinavir/Ritonavir was prescribed for patient, but according to QT prolong, two drugs hold and meropenem and vancomycin started but lung CT (Figure 1A) of patient was clear, normal and without evidence for COVID 19, after 2 day of admission, RT-PCR COVID19 were reported positive and patient was transferred to Corona intensive care unit.
Figure 1.
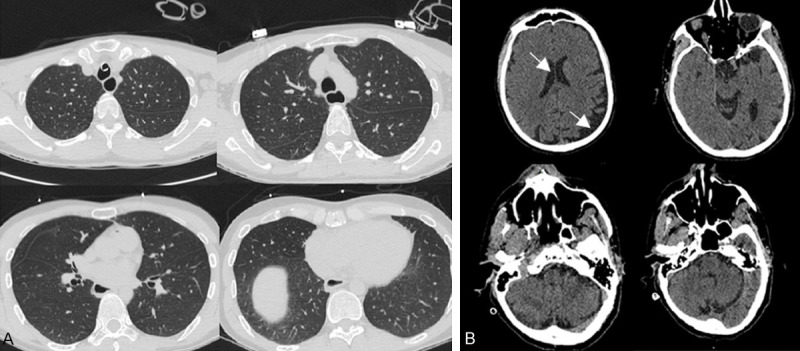
A: Coronal view of lung CT: normal lung CT and without evidence for COVID 19. B: Coronal view of brain CT: Normal brain except increased volume of CSF in subarachnoid spaces over (marked in the picture).
In the brain CT, increase cerebrospinal fluid (CSF) volume in sub-arachnoid space was reported (Figure 1B), in the brain magnetic resonance imaging (MRI) was reported micro-hemorrhaging in basal ganglia and down ward cerebellar tonsile herniation and the brain magnetic resonance angiography (MRA) was abnormal and reported “both middle cerebral artery (MCA) and anterior cerebral artery (ACA) were not seen which can be due to vasculopathy, spasm and less possibility thrombosis” which was suggested cerebral venous thrombosis (CVT), but the patient’s relatives did not give consent to posterior fossa decompression surgery.
Also, according to high level of CPK, LDH in laboratory test Rhabdomyolysis has been suggested as a possible diagnosis that the patients underwent hemodialysis for 8 times. Due to hospitalization, the patient was bradycardia and received atropine to give normal electrocardiography (ECG) rhythm. Also during of treatment patient had thrombocytopenia and peripheral blood smear was reported thrombotic thrombocytopenic purpura (TTP), in addition the blood culture of patient was reported negative.
Due to loss of consciousness, the patient had a possible diagnosis of brain death that after abnormal electroencephalogram (EEG) performing, brain death was determined. On morning of 8th day of admission patients was died because of cardiopulmonary arrest and after 45 min CPR, patient not returned to asystole rhythm.
Blood culture of patient was negative and urineanalysis was hematuria with proteinuria and few bacteria and other lab data summarized in the Table 1.
Table 1.
Lab data of patient during treatment days
| Lab data | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 |
|---|---|---|---|---|---|---|---|---|
| Alb | 2.9 | 2.8 | 2.6 | 2.5 | 2.4 | 2.4 | 2.4 | - |
| ALP | 123 | 121 | 132 | - | 225 | - | - | - |
| ALT | 10 | 81 | 144 | - | 96 | - | - | - |
| AST | 33 | 320 | 850 | - | 477 | - | - | - |
| BS | 215 | 220 | 153 | 162 | 162 | 188 | 159 | - |
| BUN | 15 | 12 | 12 | 12 | 14 | 26 | - | - |
| Ca | 9.3 | 6.5 | - | - | 7.3 | 7.0 | 7.2 | - |
| CPK | 198 | 41180 | 41240 | 25220 | 17910 | 13410 | 11460 | - |
| LDH | 526 | - | - | 2710 | 2242 | 2784 | 3480 | - |
| Cr | 2.3 | 1.9 | 2.6 | 2.4 | 2.2 | 2.9 | 3.3 | - |
| K (meq/Ls) | 6 | 3.8 | 3.6 | 3.8 | 4.2 | 4.4 | 3.7 | 5.3 |
| Lipase | 53 | - | - | - | - | - | - | - |
| Total Bill | 1.2 | 1.5 | 1.2 | 1.1 | 1.1 | - | - | - |
| Direct Bill | 0.2 | 0.2 | 0.3 | 0.3 | 0.3 | - | - | - |
| Amy | 64 | - | - | - | - | - | - | - |
| Na | 140 | 142 | 141 | 140 | 143 | 144 | 141 | 144 |
| Mg | 2.6 | 1.5 | 1.4 | 1.8 | 1.7 | 2.2 | 2 | - |
| Ph | 8.9 | 2.5 | 2.2 | 2.2 | 2.1 | 2.6 | 2.3 | - |
| WBC | 14200 | 18200 | 6900 | 8800 | 4500 | 2800 | 3300 | - |
| RBC | 4.93 | 4.41 | 4.42 | 3.98 | 3.41 | 3.24 | - | - |
| Hb | 15.5 | 13.3 | 13.9 | 12.1 | 8 | 9.4 | - | - |
| Plt | 201000 | 140000 | 49000 | 34000 | 24000 | 25000 | - | - |
| CRP | 2 | - | - | 78 | 79 | 72 | 81 | - |
| PH | 6.62 | 7.16 | 7.27 | 7.30 | 7.34 | 7.35 | 7.30 | 7.37 |
| PCO2 | 41.3 | 34.4 | 38.4 | 36.1 | 33.8 | 31.2 | 35.1 | 34.4 |
| HCO3 | 4.2 | 11.4 | 17.2 | 17.4 | 17.7 | 17 | 17.1 | 19.5 |
| PTT | 29.5 | 44 | 26 | 40 | 30 | 29.6 | 39 | - |
| PT | 10.1 | 14 | 13.5 | 10.6 | 10.0 | 9.9 | 12 | - |
| INR | 1.01 | 1.40 | 1.35 | 1.06 | 1 | 0.99 | 1.21 | - |
Discussion
In the case of this study, a patient with COVID 19 who was admitted with headache, fixed-mydriasis pupil, and dysreflexia. That the patient’s symptoms progressed sharply during 2 days. The remarkable point in this case is patient has no respiratory symptoms such as cough, shortness of breath, or fever or chills or even gastrointestinal symptoms and the patient’s symptomatic manifestations have been neurological. On the other hand, patients Chest CT did not show any evidence of COVID19 disease, but RT PCR COVID19 was reported to be positive. Apart from the symptoms that mentioned above, rhabdomyolysis, and thrombocytopenia, therefore the MCA and ACA artery thrombosis was following that brain death was happened, which is unusual signs in this disease.
In a study conducted by Ling Mao et al. to examine clinical signs of 214 patients with COVID 19 in the Wuhan City of China, 88 patients had severe respiratory infections and 126 people had not severe respiratory infections. Also, 78 patients (36.4%) of all patients had neurological symptoms. It is noteworthy that in patients who had severe infection, compared to patients who had not severe respiratory symptoms, neurological symptoms such as cerebrovascular diseases, impaired consciousness, and skeletal muscle injury were more prevalent [4]. However, in the ling mao study, it was said that in patients with severe respiratory infection symptoms, neurological symptoms could be more severe, while in the case mentioned in this study, the patient had no evidence of respiratory infection. Also in another study by Neo Poyiadji et al. Acute Hemorrhagic Necrotizing Encephalopathy for the first time in the world as Case report, was reported [5]. Conclusion: Our study reported that COVID 19 infection could be complicate neurological disorders such as brain death or CVA without respiratory complication, in this regarding COVID 19 is a novel disease with relatively high mortality rate and also this disease could be present with different complication and disorders. In this study, we suggested to work more study in related to our study.
Acknowledgements
The patient family had informed consent to access of data.
Disclosure of conflict of interest
None.
Abbreviations
- COVID 19
coronavirus disease 2019
- CSF
cerebrospinal fluid
- RT-PCR
Reverse transcription polymerase chain reaction
- EEG
electroencephalogram
- CoV
Coronavirus
- SARSCoV
severe acute respiratory Syndrome COV
- ACE2
angiotensin converting Enzyme 2
- WHO
World Health Organization
- CT
computed tomography
- LOC
loss of consciousness
- CPR
Cardiopulmonary resuscitation
- MRI
magnetic resonance imaging
- MRA
magnetic resonance angiography
- MCA
middle cerebral artery
- ACA
anterior cerebral artery
- CVT
cerebral venous thrombosis
- ECG
electrocardiography
- TTP
thrombotic thrombocytopenic purpura
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao Y, Zhao Z, Wang Y, Zhou Y, Ma Y, Zuo W. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am J Respir Crit. 2020;202:756–759. doi: 10.1164/rccm.202001-0179LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei Cl, Hui DS. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020:201187. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]