Abstract
Objective
ST segment elevation myocardial infarction (STEMI) is associated with significant mortality leading to loss of productive life years, especially in younger patients. This study aims to compare the characteristics and outcomes of young versus older patients with STEMI undergoing primary percutaneous coronary intervention (PPCI) to help focus public health efforts in STEMI prevention.
Methods
Data from the Coronary Care Unit database of the National University Hospital, Singapore from July 2015 to June 2019 were reviewed. Patients were divided into young (<50 years old) or older (≥50 years old) groups.
Results
Of the 1818 consecutive patients with STEMI who underwent PPCI, 465 (25.6%) were <50 years old. Young compared with older patients were more likely to be male, current smokers, of Indian ethnicity, have family history of ischaemic heart disease (IHD) and had lower 1 year mortality (3.4% vs 10.4%, p<0.0001). Although diabetes, hypertension or dyslipidaemia was less common among young patients, the prevalence of having any one of these risk factors was high in the range of 28% to 38%. Age was an independent predictor of mortality in the older but not younger patients with STEMI, and diabetes showed a trend towards mortality in both groups.
Conclusion
Young patients with STEMI are more often smokers, of Indian ethnicity and had family history of IHD, although cardiometabolic risk factors are also prevalent. Mortality is lower, but not negligible, among the young patients with STEMI. Public health efforts are needed to reduce the prevalence of these risk factors among the constitutionally susceptible population.
Keywords: percutaneous coronary intervention, myocardial infarction, risk factors, epidemiology, acute coronary syndrome
Key questions.
What is already known about this subject?
The baseline characteristics and mortality outcomes after myocardial infarction defer between young and older patients. Less is known about the young versus older patients specifically with ST segment elevation myocardial infarction (STEMI) undergoing primary percutaneous intervention, especially in an Asian population.
What does this study add?
In our study, young patients with STEMI have significantly different baseline characteristics, although cardiometabolic risk factors are also prevalent. Mortality is lower, but not negligible, among the younger than the older patients.
How might this impact on clinical practice?
This study could help focus public health efforts in STEMI prevention, especially in the young and susceptible population.
Introduction
Primary percutaneous coronary intervention (PPCI) is the reperfusion treatment of choice for acute ST segment elevation myocardial infarction (STEMI) and the increased use of reperfusion therapy has greatly reduced mortality in the last 20 years.1 2 However, this improvement in mortality has remained relatively unchanged over the past decade and ischaemic heart disease (IHD) remains the current leading cause of death globally.2 3 Besides the direct mortality and morbidity impact of IHD on the individuals and associated healthcare cost burden to society, there is a significant indirect cost to the individuals and society through the loss of productive life years, defined as a loss of productivity that results from individuals not being able to participate in the labour force because of their medical conditions.4 This burden has a greater impact when a young person, who may be the main income provider in the family, suffers from acute STEMI leading to a sudden loss of income. In contrast to the general perception that prognosis for these young patients with STEMI is good, the 15 years mortality could be as high as 30% among those with diabetes and poor left ventricular ejection fraction (LVEF).5 Young patients with myocardial infarction (MI) remain at significantly greater risk of long-term mortality compared with an age-matched background population, with young patients with first-time MI having a twofold increased long-term mortality (1 to 10 years after first MI) relative to the general population.6 7 In a recent cohort analysis of patients hospitalised for acute myocardial infarction (AMI) over a 20-year period, there was a trend of increase in patients who were <55 years of age.8 These young patients also had high prevalence of cardiometabolic comorbidities with 1 year mortality approaching 10%.8
While previous studies have described the characteristics and outcomes of young patients with MI, there is a lack of contemporary data among young Asian patients with STEMI who are treated with PPCI.8–15 There is also no universal definition of a young patient with MI and previous studies have used a cut-off age of 45 to 55 years.8–15 We therefore aim to assess the characteristics of young patients with STEMI and their outcomes after PPCI to help identify areas to focus public health efforts in STEMI prevention within our population.
Methods
Study population
This is a retrospective study on consecutive multiethnic Asian patients admitted with acute STEMI to the coronary care unit (CCU) and treated with PPCI at the National University Hospital, Singapore from 1 July 2015 to 30 June 2019 as part of the Western STEMI network, which provides network PPCI services to three acute hospitals in the western part of Singapore. This study was approved by the National Healthcare Group Domain Specific Review Board and the requirement for informed consent was waived (Reference number 2020/00942).
Data collection and definitions
Patient demographics, prior medical history, clinical characteristics, cardiac catheterisation data, inpatient mortality and complications were obtained from the National University Hospital CCU database, which captures data from all patients admitted to the CCU for STEMI and planned for or underwent PPCI. Patient comorbidities included both pre-existing conditions and conditions that were newly diagnosed during the STEMI admission. Outcomes after discharge and follow-up data were obtained from the hospital electronic medical records and mortality at 30 days and at 1 year were recorded. STEMI was defined in accordance with the fourth universal definition of MI.16 Patients aged less than 50 years old were defined as the ‘young STEMI’ group while patients aged 50 years and older were defined as the ‘older STEMI’ group.
Statistical analysis
Statistical analyses of categorical variables were performed with χ2 test and are presented as frequencies with percentages. Continuous variables are presented as mean±SD or median with IQR depending on the data distribution and statistical analyses were performed with Mann-Whitney U test. Kaplan-Meier curves were used to describe the cumulative all-cause mortality during the available follow-up period, and the log-rank test was used to assess for any significant difference between the two groups. The multivariate Cox regression analysis was used to compare factors that were clinically relevant and associated with all-cause mortality between the young and older STEMI groups, adjusted for age, gender, ethnicity, smoking status, hypertension, diabetes, dyslipidaemia, family history of IHD, previous AMI, stroke, chronic kidney disease, atrial fibrillation, door-to-balloon time (DTBT) ≥90 min and multivessel disease. All statistical analyses were performed using IBM SPSS Statistics for Windows, V.25.0 (IBM Corp, Armonk, New York, USA). A p value of <0.05 was considered significant for all analyses.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting or dissemination plans of our research.
Results
Baseline characteristics
Of the 2327 patients identified over the 4-year period, we excluded 221 patients who were reclassified as non-STEMI, 135 patients who did no undergo PPCI, 115 patients with incomplete data and 38 patients who were initially admitted for reasons other than MI. A total of 1818 consecutive patients with STEMI received PPCI and were included in the analysis. The baseline demographic and clinical characteristics of these patients are summarised in table 1. The mean age of the cohort was 58±12.2 years and 1587 (87.3%) were male. We identified 465 (25.6%) young patients with STEMI with a mean age of 43±4.9 years compared with 63.2±9.4 years in the older STEMI group. Compared with the older patients with STEMI, young patients with STEMI were more likely to be male (94% vs 85%, p<0.0001), of Indian ethnicity (32% vs 16.3%, p<0.0001) and current smokers (61.1% vs 42.6%, p<0.0001). Young patients with STEMI were less likely to have prior history of hypertension (31.6% vs 56.6%, p<0.0001), diabetes mellitus (28.2% vs 36.9%, p=0.001), dyslipidaemia (38.3% vs 55%, p<0.0001), AMI (7.5% vs 14.9%, p<0.0001), stroke (1.3% vs 5.2%, p<0.0001), chronic kidney disease (1.5% vs 7.1%, p<0.0001) and atrial fibrillation (0.2% vs 2.4%, p=0.002) compared with older patients, but they were more likely to have a family history of IHD (18.1% vs 9.5%, p<0.0001).
Table 1.
Baseline characteristics of patients with STEMI treated with PPCI
| Baseline characteristics | Total (n=1818) | Age <50 (n=465) | Age ≥50 (n=1353) | P value |
| Age, mean±SD (years) | 58.1±12.2 | 43.0±4.9 | 63.2±9.4 | <0.0001 |
| Gender: male | 1587 (87.3%) | 437 (94%) | 1150 (85%) | <0.0001 |
| Ethnicity | ||||
| Chinese | 948 (52.1%) | 160 (34.4%) | 788 (58.2%) | <0.0001 |
| Malay | 357 (19.6%) | 87 (18.7%) | 270 (20%) | <0.0001 |
| Indian | 369 (20.3%) | 149 (32%) | 220 (16.3%) | <0.0001 |
| Others | 144 (7.9%) | 69 (14.8%) | 75 (5.5%) | <0.0001 |
| Smoking status | ||||
| Non-smoker | 742 (40.8%) | 144 (31%) | 598 (44.2%) | <0.0001 |
| Current smoker | 861 (47.4%) | 284 (61.1%) | 577 (42.6%) | <0.0001 |
| Ex-smoker | 215 (11.8%) | 37 (8.0%) | 178 (13.2%) | <0.0001 |
| Risk factors | ||||
| Hypertension | 913 (50.2%) | 147 (31.6%) | 766 (56.6%) | <0.0001 |
| Diabetes mellitus | 630 (34.7%) | 131 (28.2%) | 499 (36.9%) | 0.001 |
| Dyslipidaemia | 922 (50.7%) | 178 (38.3%) | 744 (55%) | <0.0001 |
| Family history of IHD | 212 (11.7%) | 84 (18.1%) | 128 (9.5%) | <0.0001 |
| Past history | ||||
| Previous AMI | 227 (12.5%) | 35 (7.5%) | 192 (14.9%) | <0.0001 |
| Previous PCI | 239 (13.1%) | 35 (7.5%) | 204 (15.1%) | <0.0001 |
| Previous CABG | 26 (1.4%) | 0 (0%) | 26 (1.9%) | 0.003 |
| Stroke | 76 (4.2%) | 6 (1.3%) | 70 (5.2%) | <0.0001 |
| Chronic kidney disease | 103 (5.7%) | 7 (1.5%) | 96 (7.1%) | <0.0001 |
| Atrial fibrillation | 34 (1.9%) | 1 (0.2%) | 33 (2.4%) | 0.002 |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; IHD, ischaemic heart disease; PCI, percutaneous coronary intervention; PPCI, primary percutaneous coronary intervention; STEMI, ST segment elevation myocardial infarction.
Procedural characteristics
There were more young patients with STEMI presenting with the left anterior descending coronary artery as the culprit vessel (51% vs 45.2%, p=0.025, table 2). Young patients with STEMI had less multivessel disease compared with older patients (31% vs 40.7%, p<0.0001), while prevalence of significant left main disease was similar in both groups. The procedural success rates (99.4% vs 98.4%, p=0.139) were similar between the young and older patients with STEMI and median DTBT were the same for both groups. The proportion of young compared with older patients who had DTBT ≥90 min was also similar (20.4% vs 21.6%, p=0.601). Compared with the older patients, young patients were less likely to require periprocedural insertion of an intra-aortic balloon pump (4.9% vs 9.7%, p=0.01) or undergo coronary artery bypass graft surgery (0.6% vs 2.4%, p=0.02).
Table 2.
Procedural characteristics of patients with STEMI treated with PPCI
| Procedural characteristics | Total (n=1818) | Age <50 (n=465) | Age ≥50 (n=1353) | P value |
| Culprit vessel | 0.025 | |||
| Left main | 28 (1.5%) | 6 (1.3%) | 22 (1.6%) | |
| Left anterior descending | 848 (46.6%) | 237 (51%) | 611 (45.2%) | |
| Left circumflex | 215 (11.8%) | 63 (13.5%) | 152 (11.2%) | |
| Right coronary | 708 (38.9%) | 157 (33.8%) | 551 (40.7%) | |
| Ramus intermedius | 7 (0.4%) | 2 (0.4%) | 5 (0.4%) | |
| Bypass graft | 12 (0.7%) | 0 (0%) | 12 (0.9%) | |
| Number of vessel disease | <0.0001 | |||
| 1-vessel disease | 1123 (61.8%) | 321 (69.0%) | 802 (59.3%) | |
| 2-vessel disease | 520 (28.6%) | 118 (25.4%) | 402 (29.7%) | |
| 3-vessel disease | 175 (9.6%) | 26 (5.6%) | 149 (11.0%) | |
| Any left main >50% | 73 (4.0%) | 18 (3.9%) | 55 (4.1%) | 0.854 |
| Multivessel disease | 695 (38.2%) | 144 (31.0%) | 551 (40.7%) | <0.0001 |
| DTBT, median with IQR (minutes) | 56 (36–77) | 56 (37–76) | 56 (36–77) | 0.608 |
| DTBT ≥90 min | 387 (21.3%) | 95 (20.4%) | 292 (21.6%) | 0.601 |
| Procedural success | 1794 (98.7%) | 462 (99.4%) | 1332 (98.4%) | 0.139 |
| Use of IABP | 154 (8.5%) | 23 (4.9%) | 131 (9.7%) | 0.01 |
| CABG done | 35 (1.9%) | 3 (0.6%) | 32 (2.4%) | 0.02 |
CABG, coronary artery bypass graft surgery; DTBT, door to balloon time; IABP, intra-aortic balloon pump; PPCI, primary percutaneous coronary intervention; STEMI, ST segment elevation myocardial infarction.
Clinical complications and mortality
In general, the young patients with STEMI had fewer clinical complications compared with older patients as they were less likely to suffer from acute pulmonary oedema (5.2% vs 12.3%, p<0.0001), cardiogenic shock (7.1% vs 13.2%, p<0.0001) or require endotracheal intubation (6.7% vs 13.8%, p<0.0001). Compared with the older patients, young patients had better post-MI LVEF (in percentages, 49.5±10.7 vs 47.8±11.6, p=0.007). There were also fewer bleeding events (4.7% vs 11.2%, p<0.0001) and acute kidney injury (6% vs 13.4%, p<0.0001) in young compared with older patients. Overall, young patients with STEMI had more favourable mortality outcomes compared with older patients, with lower in-hospital (2.8% vs 8%, p<0.0001), 30-day (3% vs 8.1%, p<0.0001) and 1 year (3.4% vs 10.4%, p<0.0001) mortality (table 3). Figure 1 shows the Kaplan-Meier curves comparing all-cause mortality between the young and older patients with STEMI which shows that longer-term mortality is also lower among the young patients with STEMI when compared with older patients (log rank test, p<0.0001). Independent predictors of all-cause mortality for both young and older patients with STEMI are shown in table 4. In both the young (HR: 5.42, CI: 1.97 to 14.93, p=0.001) and older patients with STEMI (HR: 2.07, CI: 1.51 to 2.84, p<0.0001), a DTBT ≥90 min was associated with mortality. In young patients with STEMI, prior stroke (HR: 19.17, CI: 2.69 to 85.68, p=0.003) and multivessel disease (HR: 3.21, CI: 1.13 to 9.08, p=0.028) were significantly associated with mortality whereas in older patients with STEMI, age (HR: 1.05, CI: 1.03 to 1.07, p<0.0001) and chronic kidney disease (HR: 2.58, CI: 1.73 to 3.81, p<0.0001) were significantly associated with mortality. Among the traditional metabolic risk factors, diabetes showed the strongest trend towards mortality in both the young (HR: 2.77, CI: 0.90 to 8.53, p=0.077) and older (HR: 1.31, CI: 0.95 to 1.89, p=0.102) patients with STEMI.
Table 3.
Clinical complications and mortality of patients with STEMI treated with PPCI
| Complications and mortality | Total (n=1818) | Age <50 (n=465) | Age ≥50 (n=1353) | P value |
| Mortality | ||||
| In-hospital | 121 (6.7%) | 13 (2.8%) | 108 (8.0%) | <0.0001 |
| At 30 days | 123 (6.8%) | 14 (3.0%) | 109 (8.1%) | <0.0001 |
| At 1 year | 157 (8.6%) | 16 (3.4%) | 141 (10.4%) | <0.0001 |
| Time to death or censored, median with IQR (days) | 709 (335–1083) | 661 (241–1082) | 727 (365–1090) | 0.277 |
| Length of hospitalisation, median with IQR (days) | 4 (2–6) | 4 (3–5) | 5 (3–7) | <0.0001 |
| 30-day readmission (days) | 423 (23.3%) | 82 (17.6%) | 341 (25.2%) | 0.001 |
| LVEF post-STEMI, mean±SD (%) | 48.2±11.4 | 49.5±10.7 | 47.8±11.6 | 0.007 |
| Complications | ||||
| Acute pulmonary oedema | 191 (10.5%) | 24 (5.2%) | 167 (12.3) | <0.0001 |
| Cardiogenic shock | 211 (11.6%) | 33 (7.1%) | 178 (13.2) | <0.0001 |
| Endotracheal intubation | 218 (12%) | 31 (6.7%) | 187 (13.8) | <0.0001 |
| Stroke | 0.746 | |||
| Ischaemic | 20 (1.1%) | 4 (0.9%) | 16 (1.2%) | |
| Haemorrhagic | 6 (0.3%) | 1 (0.2%) | 5 (0.4%) | |
| Bleeding | 174 (9.6%) | 22 (4.7%) | 152 (11.2%) | <0.0001 |
| Acute kidney injury | <0.0001 | |||
| Requiring RRT | 37 (2.0%) | 5 (1.1%) | 32 (2.4%) | |
| Not requiring RRT | 172 (9.5%) | 23 (4.9%) | 149 (11.0%) | |
| Atrial fibrillation | 117 (6.4%) | 7 (1.5%) | 110 (8.1%) | <0.0001 |
| Ventricular tachycardia | 0.005 | |||
| Sustained | 78 (4.3%) | 14 (3%) | 64 (4.7%) | |
| Non-sustained | 139 (7.6%) | 50 (10.8%) | 89 (6.6%) | |
| Ventricular fibrillation | 143 (7.9%) | 30 (6.5%) | 113 (8.4%) | 0.189 |
LVEF, left ventricular ejection fraction; PPCI, primary percutaneous coronary intervention; RRT, renal replacement therapy; STEMI, ST segment elevation myocardial infarction.
Figure 1.
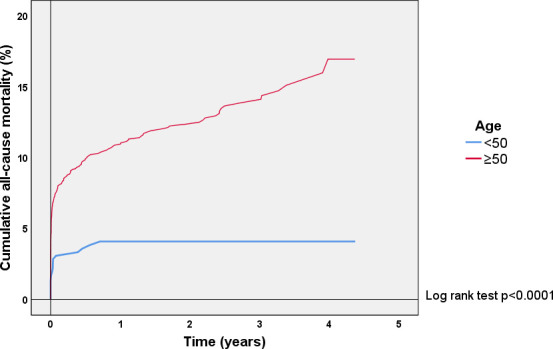
Kaplan-Meier curves showing cumulative all-cause mortality after primary percutaneous coronary intervention in young (aged <50 years) compared with older (aged ≥50) patients presenting with ST segment elevation myocardial infarction.
Table 4.
Multivariate COX regression analysis of factors associated with all-cause mortality in young (aged <50) compared with older (aged ≥50) patients with STEMI treated with PPCI
| Age <50 | Age ≥50 | |||
| Adjusted HR (95% CI) | P value | Adjusted HR (95% CI) | P value | |
| Age, per 1 year increase | 0.93 (0.85–1.02) | 0.134 | 1.05 (1.03–1.07) | <0.0001 |
| Female gender | 1.34 (0.29–7.97) | 0.667 | 0.63 (0.41–0.97) | 0.037 |
| Indian ethnicity | 0.83 (0.25–2.55) | 0.756 | 1.47 (0.97–2.23) | 0.070 |
| Current smoker | 0.74 (0.31–2.43) | 0.567 | 0.78 (0.54–1.12) | 0.185 |
| Hypertension | 0.61 (0.16–2.05) | 0.467 | 1.01 (0.71–1.44) | 0.939 |
| Diabetes mellitus | 2.77 (0.90–8.53) | 0.077 | 1.31 (0.95–1.89) | 0.102 |
| Dyslipidaemia | 0.46 (0.12–1.49) | 0.235 | 1.02 (0.73–1.42) | 0.911 |
| Family history of IHD | 0.20 (0.03–1.62) | 0.133 | 0.60 (0.28–1.29) | 0.191 |
| Previous AMI | 1.48 (0.24–8.33) | 0.672 | 0.74 (0.48–1.14) | 0.172 |
| Previous stroke | 19.17 (2.69–85.68) | 0.003 | 1.24 (0.75–2.04) | 0.409 |
| Chronic kidney disease | 0.05 (0.01–72.23) | 0.987 | 2.58 (1.73–3.81) | <0.0001 |
| Atrial fibrillation | 0.05 (0.01–42.67) | 0.997 | 1.18 (0.58–2.43) | 0.649 |
| DTBT ≥90 min | 5.42 (1.97–14.93) | 0.001 | 2.07 (1.51–2.84) | <0.0001 |
| Multivessel disease | 3.21 (1.13–9.08) | 0.028 | 1.06 (0.78–1.43) | 0.720 |
AMI, acute myocardial infarction; DTBT, door to balloon time; IHD, ischaemic heart disease; PPCI, primary percutaneous coronary intervention; STEMI, ST segment elevation myocardial infarction.
Discussion
In our contemporary real-world cohort of consecutive patients with STEMI treated with PPCI, approximately one in four were younger patients aged <50 years. There were significant differences in the baseline characteristics between young and older patients with STEMI, with higher rates of smoking, Indian ethnicity and family history of IHD, but lower rates of hypertension, diabetes and dyslipidaemia in the young than the older patients. Young patients with STEMI had better in-hospital and short-term and medium-term survival, and less likely to experience complications of STEMI when compared with older patients. The long-term mortality was also lower in the young compared with older patients with STEMI with few of them died beyond 1 year of their index STEMI.
To our knowledge, this is the first large cohort study investigating the characteristics, short-term and long-term outcomes of young patients with STEMI (age <50) undergoing PPCI in a multiethnic South East Asian population. The majority of previous studies of young patients with STEMI included mixed MI presentations, or were studies done in predominantly Caucasian populations.7–15 17 18 There were few prior studies on our local population with STEMI and these were focused on differences in more elderly patients (age ≥65),19 or did not study characteristics and outcomes in young compared with older patients with STEMI.20 21
Our study showed the high prevalence (61.1%) of current smokers among the young patients with STEMI and this is similar to previous studies on young patients with MI with prevalence of smoking ranging from 47% to 83%.7–15 17–19 A recent retrospective cohort study by Biery et al showed that young patients with MI who quit smoking after their MI had significantly lower all-cause and cardiovascular mortality compared with those who continued to smoke.22 Studies on national health policies in raising legal age of smoking showed that delayed smoking initiation in youths would reduce adult smoking prevalence in the long term.23 24 In Singapore, the Health Ministry had raised the minimum legal age of smoking from 18 to 20 years old from 1 January 2020, and this would be subsequently raised to 21 years old on 1 January 2021.25 Our study found that smoking was the most prevalent modifiable risk factor in our young patients with STEMI and these recent policies to raise the legal smoking age could decrease smoking prevalence in the future.
A previous study looking at ethnic differences and trends in our local population showed a higher STEMI incidence rate in the Indian ethnic group (126 per 100 000 population) compared with the Chinese (58 per 100 000 population).20 Our study also showed that young patients with STEMI were more likely to be of Indian ethnicity and had family history of IHD. The Indian ethnic group in Singapore comprises of largely South Asian ancestry and this ethnic group has been shown to have higher rates of young patients with MI regardless of the geographical location.7 12 14 17 19 26 Prior studies from various countries have consistently found that the prevalence of family history of IHD was higher, in the range of 20% to 48%, among the young patients with MI when compared with older patients with MI.7 10 12 15 17 Similarly, 18.1% of young patients with STEMI in our study had a family history of IHD and this was twice more than that in older patients.
It is not surprising that our young patients with STEMI had lower rates of hypertension, diabetes and dyslipidaemia as incidence of these metabolic risk factors increases with age. However, about one-third of our young patients with STEMI had at least one of these metabolic risk factors. In particular, 28.2% of young patients with STEMI in our cohort had diabetes and this is higher than the reported rates of diabetes of around 9% in other similar studies on young patients with STEMI in predominantly Caucasian populations.17 18 In a study by Ding et al, young patients with diabetes mellitus had poorer health status before and during hospitalisation for AMI.27 Diabetes was also shown in our study to have a strong trend towards all-cause mortality in both the young and older patients with STEMI and similar studies showed that young patients with STEMI with diabetes had higher mortality during follow-up.17–19 Our study is also the first to show the prevalence of multivessel disease in young patients with STEMI within our population.19–21 Almost a third (31%) of our young patients with STEMI had multivessel disease whereas in other similar studies done in predominantly Caucasian populations, the prevalence of multivessel disease in young patients with STEMI was around 22%.17 18 Young patients with STEMI who had multivessel disease also had worse mortality outcomes compared with those with single vessel disease. Data from our study could therefore support public health programmes to educate the public on the risk factors in young patients with STEMI, particular those with family history of IHD and of Indian ethnicity, and to place greater emphasis of early detection and screening for these metabolic risk factors before MI occurs.
It is encouraging that the short-term and long-term mortality of our young patients with STEMI remains significantly lower than older patients, and this lower mortality in young patients with MI was noted in many previous studies.7–15 17–19 Young patients with STEMI suffered from fewer complications, had better post-MI LVEF and had a significantly shorter length of hospitalisation compared with older patients. Mortality after 1 year was very low in our young patients with STEMI which is consistent with other similar studies.17 18 However, mortality in our young patients with STEMI was not negligible, with mortality at 2.8% inpatient, 3% at 30 days and 3.4% at 1 year. Most of the deaths in the young STEMI cohort occurred before discharge, and 7 (53.8%) out of 13 in-hospital deaths occurred within the first 24 hours; in comparison, 55 (50.9%) out of 108 in-hospital deaths in the older patients with STEMI occurred in the first 24 hours (data not shown). This shows that a significant proportion of deaths in the young patients with STEMI occurred during the first 24 hours of presentation despite receiving PPCI. A DTBT ≥90 min was also a strong independent predictor of mortality in our young patients with STEMI. Our hypothesis is that while young patients with STEMI have better reserves and are more able to tolerate the effects of MI, these patients may ignore their symptoms and a proportion of young patients with STEMI may present late or only after suffering a cardiac arrest. Future studies should focus on the factors contributing to early mortality in young patients with STEMI and the health-seeking behaviours, such as seeking early treatment or calling for an ambulance, in this population.
Interestingly, age was found to be an independent predictor of mortality in the older but not younger patients with STEMI. This suggests that other constitutional and modifiable risk factors are as, if not more, important in young patients with STEMI as mortality is not due to age alone. The prevalence of atherosclerotic risk factors has been increasing and the mean age decreasing in patients presenting with either AMI or acute ischaemic stroke.28 Our study also found a very significant association of prior stroke with mortality in young patients with STEMI, therefore highlighting the extremely high risk of early death in these patients. Mortality in young patients with STEMI represents a tragedy not just to the patient, but also to the family and dependents as these patients are in their peak earning years and are more likely to be the main income provider for the family. Our study provides insights into the characteristics of young patients with STEMI and their outcomes after PPCI. This could form the basis for future public health efforts in STEMI and ultimately coronary artery disease prevention within our population.
Limitations
This is a single-centre, retrospective cohort study of patients with STEMI who underwent PPCI over 4 years and therefore subject to the usual limitations as any retrospective, observational study. Our study excluded 135 patients who did no undergo PPCI and 115 patients with incomplete data, and while these exclusions could theoretically lead to a biased sample, the numbers were small compared with the overall cohort. There could also be a potential selection bias as older patients, especially the very elderly, would more likely be managed with medical therapy compared with younger patients, and hence be excluded from our study. All patients with STEMI who underwent PPCI would be captured in our CCU database, including patients who presented with out-of-hospital cardiac arrest (OOHCA) in which cardiac aetiology, including STEMI, was suspected as the cause and hence underwent coronary angiography. However, patients with OOHCA who were not referred for coronary angiography would not be included in our database and while some of these patients might have undiagnosed STEMI, such cases were rare. While data from the CCU database was generally robust, it did not have data on all known risk factors for AMI. In particular, we do not have data on obesity or body mass index, which were previously studied in other young MI cohorts.7 14 15 18 Though obesity has been shown to be a risk factor for AMI, its effect is modest compared with smoking and other cardiometabolic risk factors like hypertension, diabetes and dyslipidaemia.26 Finally, the limitations of available hospital electronic medical records meant that we were unable to analyse potential confounders affecting outcomes following discharge and long-term mortality such as the adherence to guideline-directed medical therapy or dynamic risk from optimal control of cardiovascular risk factors after STEMI and PPCI.
Conclusion
One in four of our patients with STEMI are younger than 50 years old and they are more often smokers, of Indian ethnicity and have family history of IHD, although other cardiometabolic risk factors are also prevalent. Although mortality is lower among the young compared with older patients, it is not negligible. Public health efforts are needed to reduce the prevalence of smoking and address other risk factors early especially among the constitutionally susceptible population.
Acknowledgments
Cardiology and Emergency Medicine Department colleagues in Alexandra Hospital, Ng Teng Fong General Hospital and National University Hospital for their invaluable contributions to the Western STEMI Network. Nursing and allied health staff of the cardiac catheterisation laboratory and coronary care unit of the National University Hospital for their excellent care of our cardiac patients.
Footnotes
Contributors: BWLT, ZYN and PHL contributed to the initial study design, literature review, analysis and interpretation of data and drafting of the manuscript. WK, KWS and WS contributed to the acquisition, verification and analysis of data. S-PC contributed to the statistical analysis and interpretation of data. KHC, MC, WK, RL, JPL, AFL, KKP, ET, HCT and T-CY contributed to the critical revision of the manuscript for important intellectual content. All the authors contributed in the final approval of the manuscript submitted and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. BWLT is the corresponding first author and is responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1.Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165. 10.1093/eurheartj/ehy394 [DOI] [PubMed] [Google Scholar]
- 2.Puymirat E, Cayla G, Cottin Y, et al. Twenty-year trends in profile, management and outcomes of patients with ST-segment elevation myocardial infarction according to use of reperfusion therapy: data from the FAST-MI program 1995-2015. Am Heart J 2019;214:97–106. 10.1016/j.ahj.2019.05.007 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organisation Top 10 global causes of deaths, 2016. Available: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death [Accessed 8 Jul 2020].
- 4.Schofield D, Cunich M, Shrestha R, et al. The indirect costs of ischemic heart disease through lost productive life years for Australia from 2015 to 2030: results from a microsimulation model. BMC Public Health 2019;19:802. 10.1186/s12889-019-7086-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cole JH. Miller JI 3rd, Sperling LS, Weintraub WS. Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol 2003;41:521–8. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt M, Szépligeti S, Horváth-Puhó E, et al. Long-term survival among patients with myocardial infarction before age 50 compared with the general population: a Danish nationwide cohort study. Circ Cardiovasc Qual Outcomes 2016;9:523–31. 10.1161/CIRCOUTCOMES.115.002661 [DOI] [PubMed] [Google Scholar]
- 7.Jing M, Gao F, Chen Q, et al. Comparison of Long-Term Mortality of Patients Aged ≤40 Versus >40 Years With Acute Myocardial Infarction. Am J Cardiol 2016;118:319–25. 10.1016/j.amjcard.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 8.Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation 2019;139:1047–56. 10.1161/CIRCULATIONAHA.118.037137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malmberg K, Båvenholm P, Hamsten A. Clinical and biochemical factors associated with prognosis after myocardial infarction at a young age. J Am Coll Cardiol 1994;24:592–9. 10.1016/0735-1097(94)90002-7 [DOI] [PubMed] [Google Scholar]
- 10.Zimmerman FH, Cameron A, Fisher LD, et al. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (coronary artery surgery study registry). J Am Coll Cardiol 1995;26:654–61. 10.1016/0735-1097(95)00254-2 [DOI] [PubMed] [Google Scholar]
- 11.Awad-Elkarim AA, Bagger JP, Albers CJ, et al. A prospective study of long term prognosis in young myocardial infarction survivors: the prognostic value of angiography and exercise testing. Heart 2003;89:843–7. 10.1136/heart.89.8.843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan MY, Woo KS, Wong HB, et al. Antecedent risk factors and their control in young patients with a first myocardial infarction. Singapore Med J 2006;47:27–30. [PubMed] [Google Scholar]
- 13.Morillas P, Bertomeu V, Pabón P, et al. Characteristics and outcome of acute myocardial infarction in young patients. The PRIAMHO II study. Cardiology 2007;107:217–25. 10.1159/000095421 [DOI] [PubMed] [Google Scholar]
- 14.Wong CP, Loh SY, Loh KK, et al. Acute myocardial infarction: clinical features and outcomes in young adults in Singapore. World J Cardiol 2012;4:206–10. 10.4330/wjc.v4.i6.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matsis K, Holley A, Al-Sinan A, et al. Differing clinical characteristics between young and older patients presenting with myocardial infarction. Heart Lung Circ 2017;26:566–71. 10.1016/j.hlc.2016.09.007 [DOI] [PubMed] [Google Scholar]
- 16.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018;72:2231–64. 10.1016/j.jacc.2018.08.1038 [DOI] [PubMed] [Google Scholar]
- 17.Rathod KS, Jones DA, Gallagher S, et al. Atypical risk factor profile and excellent long-term outcomes of young patients treated with primary percutaneous coronary intervention for ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care 2016;5:23–32. 10.1177/2048872614567453 [DOI] [PubMed] [Google Scholar]
- 18.Waziri H, Jørgensen E, Kelbæk H, et al. Short and long-term survival after primary percutaneous coronary intervention in young patients with ST-elevation myocardial infarction. Int J Cardiol 2016;203:697–701. 10.1016/j.ijcard.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 19.Pek PP, Zheng H, Ho AFW, et al. Comparison of epidemiology, treatments and outcomes of St segment elevation myocardial infarction between young and elderly patients. Emerg Med J 2018;304:emermed-2017-206754–296. 10.1136/emermed-2017-206754 [DOI] [PubMed] [Google Scholar]
- 20.Zheng H, Pek PP, Ho AF, et al. Ethnic differences and trends in ST-segment elevation myocardial infarction incidence and mortality in a multi-ethnic population. Ann Acad Med Singap 2019;48:75–85. [PubMed] [Google Scholar]
- 21.Ho AFW, Loy EY, Pek PP, et al. Emergency medical services utilization among patients with ST-segment elevation myocardial infarction: observations from the Singapore myocardial infarction registry. Prehosp Emerg Care 2016;20:454–61. 10.3109/10903127.2015.1128032 [DOI] [PubMed] [Google Scholar]
- 22.Biery DW, Berman AN, Singh A, et al. Association of smoking cessation and survival among young adults with myocardial infarction in the partners YOUNG-MI registry. JAMA Netw Open 2020;3:e209649. 10.1001/jamanetworkopen.2020.9649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad S, Billimek J. Limiting youth access to tobacco: comparing the long-term health impacts of increasing cigarette excise taxes and raising the legal smoking age to 21 in the United States. Health Policy 2007;80:378–91. 10.1016/j.healthpol.2006.04.001 [DOI] [PubMed] [Google Scholar]
- 24.Beard E, Brown J, Jackson S, et al. Long-term evaluation of the rise in legal age-of-sale of cigarettes from 16 to 18 in England: a trend analysis. BMC Med 2020;18:85. 10.1186/s12916-020-01541-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministry of Health, Singapore Minimum legal age for tobacco raised to 20 years old from 1 January 2020. Available: https://www.moh.gov.sg/news-highlights/details/minimum-legal-age-for-tobacco-raised-to-20-years-old-from-1-january-2020/ [Accessed 8 Jul 2020].
- 26.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–52. 10.1016/S0140-6736(04)17018-9 [DOI] [PubMed] [Google Scholar]
- 27.Ding Q, Funk M, Spatz ES, et al. Association of diabetes mellitus with health status outcomes in young women and men after acute myocardial infarction: results from the VIRGO study. J Am Heart Assoc 2019;8:e010988. 10.1161/JAHA.118.010988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Agarwal S, Sud K, Thakkar B, et al. Changing trends of atherosclerotic risk factors among patients with acute myocardial infarction and acute ischemic stroke. Am J Cardiol 2017;119:1532–41. 10.1016/j.amjcard.2017.02.027 [DOI] [PubMed] [Google Scholar]


