Faith and Science
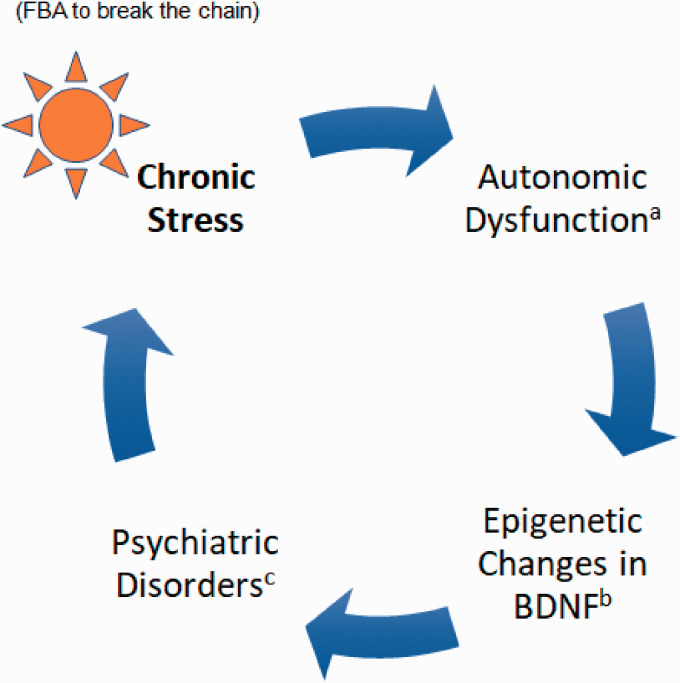
Acknowledgement of the importance of religion and spirituality in medicine is increasing. Several studies have shown a predominantly inverse relationship between faith-based activities and psychiatric disorders.1 Chronic stress alters autonomic nervous system reactivity, and changes in the dopamine systems of people undergoing chronic stress have been well documented in the literature.2 In Figure 1, we hypothesize a model regarding the vicious cycle that exists between psychiatric disorders and chronic stress.
Figure 1.
Effect of faith-based activities (FBA)1 on the chaotic internal milieu. aAutonomic nervous system dysfunction under chronic stress with the interplay between its two branches: the parasympathetic and sympathetic nervous systems.2 bEpigenetic changes in the central nervous system are crucial in the development of a myriad of psychiatric disorders.4 cPsychiatric disorders could mainly consist of mood disorders and stress-related disorders such as major depressive disorder, PTSD, and substance use disorders.
Brain-derived neurotrophic factor (BDNF) is a brain-nourishing molecule that plays an important role in synaptic plasticity, dendritic and neuronal fiber growth, and neuronal survival.1 People with mental health issues such as depression may improve their mood and behavior through faith-based activities, which are known to increase serum BDNF levels.1 The stress-related system, which includes the hypothalamic-pituitary-adrenocortical (HPA) axis and the hippocampus, and the reward system, which includes the ventral tegmental area and nucleus accumbens pathway, were found to be associated with altered BDNF expression following stress induction in animal models.3 Although the data are mixed, few studies have shown that chronic stress exposure decreases BDNF levels in brain regions implicated in mood and behavior such as the prefrontal cortex and hippocampus in rodents. Further, these findings are in agreement with results from postmortem brain studies from depressed suicide completers.4
The prefrontal cortex (PFC) assists us in completing our daily activities through thinking, reasoning, focusing, and controlling the emotions. Researchers conducted studies in a group that practices glossolalia (the phenomenon of speaking in an unknown language, especially in religious worship, practiced predominantly by Pentecostal and Charismatic Christians) as a form of deeply meaningful and intimate spiritual experience.5 Glossolalia is an unusual mental state in which individuals appear to be speaking an incomprehensible language during the most intimate praying moment. Functional magnetic resonance imaging (fMRI) scans showed that the frontal lobe, the part of the brain that controls language, was active when the participants prayed in English but fell mostly quiet when they prayed in glossolalia. Frontal lobe activity is known to increase when individuals focus on what they are saying, but this study found that when people speak in glossolalia, the words coming forth originate from a source other than the PFC. In addition, it was revealed that while blood flow to the PFC decreased, activity in the area that controls self-awareness (medial PFC/anterior cingulate cortex and medial parietal/posterior cingulate cortex) was active.5 On the contrary, it is of interest to note that an fMRI study of Carmelite nuns revealed that remembrance of spiritual, mystical experiences correlated with increased blood flow in the PFC and temporal, caudate, cingulate, and orbitofrontal cortices, which also correlate with religious experiences and positive emotions.1 These two studies show that although different modes of prayer impact both the neuroanatomical areas receiving blood flow and the nature of the spiritual experiences attained in different ways, the beneficial therapeutic outcomes are similar. These findings suggest that different behavioral and neuroanatomic circuits by which to impact BDNF expression exist in the brain and that it is worth investigating the clinical implications, both risks and benefits, of implementing faith-based activities in health care settings.
The neuronal network and its modulatory epigenetic mechanism function in such a way that leads to a chaotic internal milieu in states associated with certain psychiatric illnesses. Pharmacology is recognized as one of the important elements in the healing process of those suffering from mental health issues. Equally important are the mind-body relationship and the individual’s relation to reality as a whole.6,7 One way to change this chaotic internal milieu, a hypothetical illustration of which is depicted in Figure 1, is through faith-based interventions that include praying, meditation, and positive thinking. One of the primary goals of the faith-based and community initiatives is to train people to develop an ARTS strategy—action, reaction, and thinking smart in adversities—which could help them break the chaotic milieu, using the techniques mentioned here. We propose the further investigation and implementation of faith-based activities in the health care setting based on the preliminary findings of the studies mentioned above.
Future studies can focus on objective measurements of spirituality8 and correlate those with Patient Health Questionnaire-9 (PHQ-9) and Generalized Anxiety Disorder-7 (GAD-7) scores in various clinical settings.
Footnotes
Authors’ Contribution: Varghese prepared the first draft of the manuscript. All authors edited the manuscript with intellectual contribution and approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer: The views described in this manuscript are those of the authors and do not reflect the official policy of the Sacramento VA Medical Center or The Department of Veterans Affairs or UC Davis Health.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sajoy P. Varghese https://orcid.org/0000-0002-1230-7435
References
- 1.Mosqueiro BP, Fleck MP, Rocha NS. Increased levels of brain-derived neurotrophic factor are associated with high intrinsic religiosity among depressed inpatients. Front Psychiatry. 2019; 10:671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colombo J, Arora R, DePace NL.Vinik, AI. Clinical Autonomic Dysfunction. Kindle Edition. New York: Springer International Publishing; 2015: 791, 798. [Google Scholar]
- 3.Miao Z, Wang Y, Sun Z. The relationships between stress, mental disorders, and epigenetic regulation of BDNF. Int J Mol Sci. 2020; 21(4):1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandey GN, Ren X, Rizavi HS, Conley RR, Roberts RC, Dwivedi Y. Brain-derived neurotrophic factor and tyrosine kinase B receptor signaling in post-mortem brain of teenage suicide victims. Int J Neuropsychopharmacol. 2008; 11:1047–1061. [DOI] [PubMed] [Google Scholar]
- 5.Newberg AB, Wintering NA, Morgan D, Waldman MR. The measurement of regional cerebral blood flow during glossolalia: a preliminary SPECT study. Psychiatry Res Neuroimag. 2006; 148:67–71. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran VS. The Tell-Tale Brain: A Neuroscientist's Quest for What Makes Us Human. Kindle Edition. New York: W. W. Norton & Company. [Google Scholar]
- 7.George KM. Paulos Mar Gregorios (South Asian Theology ) Kindle Edition. Minneapolis: Fortress Press. [Google Scholar]
- 8.Koenig HG. Research on religion, spirituality, and mental health: a review. Can J Psychiatry. 2009; 54(5):283–291. [DOI] [PubMed] [Google Scholar]